ANTIHISTAMINES - rEMERGs
ANTIHISTAMINES - rEMERGs
ANTIHISTAMINES - rEMERGs
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
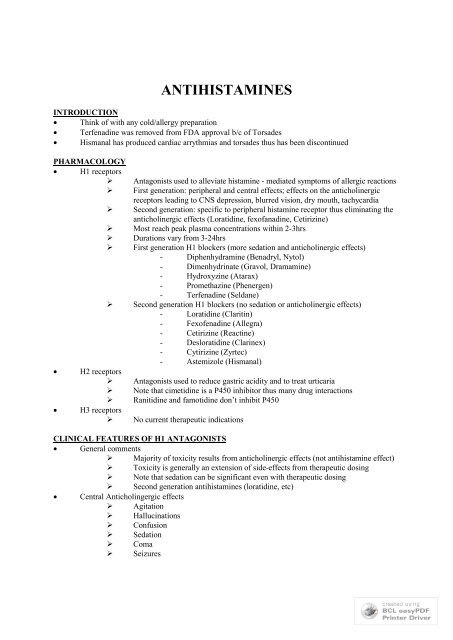
<strong>ANTIHISTAMINES</strong>INTRODUCTION Think of with any cold/allergy preparation Terfenadine was removed from FDA approval b/c of Torsades Hismanal has produced cardiac arrythmias and torsades thus has been discontinuedPHARMACOLOGY H1 receptors‣‣‣‣‣‣‣H2 receptors‣‣‣H3 receptors‣Antagonists used to alleviate histamine - mediated symptoms of allergic reactionsFirst generation: peripheral and central effects; effects on the anticholinergicreceptors leading to CNS depression, blurred vision, dry mouth, tachycardiaSecond generation: specific to peripheral histamine receptor thus eliminating theanticholinergic effects (Loratidine, fexofanadine, Cetirizine)Most reach peak plasma concentrations within 2-3hrsDurations vary from 3-24hrsFirst generation H1 blockers (more sedation and anticholinergic effects) Diphenhydramine (Benadryl, Nytol) Dimenhydrinate (Gravol, Dramamine) Hydroxyzine (Atarax) Promethazine (Phenergen) Terfenadine (Seldane)Second generation H1 blockers (no sedation or anticholinergic effects) Loratidine (Claritin) Fexofenadine (Allegra) Cetirizine (Reactine) Desloratidine (Clarinex) Cytirizine (Zyrtec) Astemizole (Hismanal)Antagonists used to reduce gastric acidity and to treat urticariaNote that cimetidine is a P450 inhibitor thus many drug interactionsRanitidine and famotidine don’t inhibit P450No current therapeutic indicationsCLINICAL FEATURES OF H1 ANTAGONISTS General comments‣ Majority of toxicity results from anticholinergic effects (not antihistamine effect)‣ Toxicity is generally an extension of side-effects from therapeutic dosing‣ Note that sedation can be significant even with therapeutic dosing‣ Second generation antihistamines (loratidine, etc) Central Anticholingergic effects‣ Agitation‣ Hallucinations‣ Confusion‣ Sedation‣ Coma‣ Seizures
Peripheral Anticholinergic Effects‣ Tachycardia: decreases vagal stimulation to heart‣ Hyperthermia: agitation + inability to sweat‣ Mydriasis:‣ Can’t see: loss of accomodation + mydriasis‣ Dry, flushed skin‣ Hypertension‣ Urinary retension‣ Decreased bowel activity: ileus, absent bowel soundsCardiovascular Effects‣ Sinus tachycardia very common (vagolytic effects)‣ May be hypertensive or hypotensive‣ Wide QRS and prolonged QT can occur Thought to be a function of Na+ channel blockade Treat with bicarbNotes on Diphenhydramine (Bendadryl) Overdoses‣ Retrospective review of 136 cases: 55% developed CNS depression, 15%developed catatonic stupor‣ Pediatric patients more susceptible to seizures, respiratory complications, CNSstimulation, and anticholinergic symptoms‣ Wide QRS, prolonged QT, ventricular dysrhytmias have all occurred‣ Vertical and horizontal nystagmus noted‣ Rhabdomyolysis has occurred: patients were very agitatedDry as a bone:dry skinRed as a beet: flushedMad as a hatter: agitationBlind as a bat: mydriasis,accomodationHot as a hare: feverMANAGEMENT General‣‣‣‣‣‣‣‣‣‣Cardiac monitorWatch for seizures, prolonged QT, wide QRSNeed [APAP] level b/c of cold preps often have acetaminophenWatch temp and HR as predictors of who will be more toxicMost managed with only supportive careActivated charcoal is indicated (may require intubation and NG administration ifthere is significant CNS depression)Consider MDAC as anticholinergic effects with delay gastric motility and GIabsorptionFluids for dehydrationFluids +/- pressors for hypotensionGastric Lavage only for MASSIVE overdose that presents early
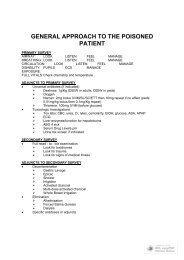
‣ Benzos for severe agitation‣ Benzos for seizures‣ Temp: cold water mist, fansCardiac Toxicity‣ Wide QRS, prolonged QT‣ Bolus bicarbonate until effect‣ Hypertonic salinePhysostigmine‣ Acetylcholinesterase inhibitor (central and peripheral) which increases the amountof acetylcholine in the synapse‣ Can effectively reverse anticholinergic toxicity‣ Initially was used to counteract atropine poisoning‣ Only used for SEVERE toxicity: benefit must clearly outweigh the risks‣ Risks: cholinergic crisis (DUMBELS)‣ Contraindications: wide QRS, history of exposure to TCAs or any IA or ICantiarrthmics, exposure to any other potential Na+ channel blocker (cocaine,carbamezepine, thioridazine, etc), underlying cardiac conduction disorders‣ Increased mortality when TCAs on board (how can you be sure they aren’t?)‣ Must be on cardiac monitor with atropine at bedside for cholinergic crisis‣ Dose: 1-2 mg in adults, 0.5 mg in children; repeat q10 min prnDECONGESTANTSPHARMACOLOGY Sympathomimetics that act on alpha adrenergic receptors to produce vasoconstriction in themucous membranes and improve airflow In therapuetic doses they can have systemic affects in addition to local effects Ephedrine and Pseudoephedrine: alpha 1,2 and beta 1,2 agonism Phenylephrine: powerful alpha agonist with very little beta effects Phenylpropanolamine: alpha 1,2 agonism with no beta agonism Imidazoline sympathomimetics: topical applicaitons (oxymetazoline, tetrahydrozoline,naphazoline); pure alpha 2 agonist that are primarily used as nasal decongestants NOTE: weight lifters and athletes are abusing these Onset of symptoms usually within few hours and resolve by 8-24hrsCLINICAL MANIFESTATIONS Rarely cause systemic toxicity b/c of poor absorption CNS stimulation common Cardiac stimulation: tachycardia, HTN Bradycardia possible with pure alpha agonists (reflexic response to hypertension) Requires 4-5 Xs recommended dose to see significant effects Headache is most common initial symptom that is reported by those that become toxic Severe exposures: ventricular arrythmias, seizure, intracranial hemorrhages, ischemic gut, MisMANAGEMENT Activated charcoal Benzodiazepines for sedation, seizures
Nitroprusside or phentolamine for hypertensive emergenciesHypertensive + Bradycardic: note that atropine may not be a good idea b/c bradycardia is aresponse to the hypertension from the pure alpha effect; atropine may result in massive increase inBP if the bradycardia is a reflexic responseANTICHOLINERGICSINTRODUCTION Belladonna alkaloids = prototypical anticholinergics; atropine, scopolamine, hysocyamine Jimson week: contains scopolamineCOMMON CAUSES OF ANTICHOLINERGIC SYNROME Plants‣ Jisonweed‣ Angel’s tumptt‣ Jasmine‣ Mandrake‣ Deadly nightshade‣ Etc Belladona Alkaloids‣ Atropine‣ Scopolamine‣ Homatropine‣ Cyclopentolate‣ Tropicamide‣ Ipratropium Antihistamines‣ Benadryl‣ Atarax‣ Gravol‣ Dramamine‣ Antivert‣ Brompheniramine Phenothiazines Aniparkinson agents‣ Cogentin‣ Artane‣ Kemadrin‣ EtcANTICHOLINERGIC EFFECTS AS PART OF TOXIDROME Flexeril Tegretol Amitriptyline Imipramine Doxepin Amoxapine
DesipramineNortripyltinMellarilSerentilThoraxineCompazineCOMMON OTC SLEEP AIDS Pyrilamin (Sominex) Diphenhydramine (Nytol, Benadryl) Cyclizine (Marezine)PRINCIPLES OF DISEASE Muscarinic effects Do not have nicotinic effects (paralysis, weakness, resp failure) b/c there is no blockage at theNMJ Muscarinic blockade‣ Tachycardia‣ Mydriasis‣ Absent bowel sounds‣ HOT and DRY SKIN (can’t sweat!) (sympathomimetic is wet)‣ Urinary retention‣ Decreased ability for visual accomodation‣ Dry mucous membranes Central effects‣ Seizures‣ Delirium‣ Coma‣ Agitation‣ Fever Delirium‣ Elderly patient with delirium‣ May be due to antiparkinsonian drugs, antipsychotic drugs, or TCAs‣ Common overlooked Fever‣ Can be afebrile or severe temperature elevation‣ Severe hyperthermia associated with cerebral edema, rhabdo, DIC‣ Requires aggressive sedation, coolingDDXSympathomimetic sweaty, anticholinergic dry (sympathomimetics can be dry if dehydrated)Seritonin syndrome has hypereflexia and increased tone, anticholinergics usually don’tThyroid storm, meningitis, encephalitis, etcMANAGMENT Agitation: benzos are drug of choice Hyperthermia: temps q1hr, ice to groin, fans, cooling blankets, bzd, intubation and paralysis Decontamination: activated charcoal; avoid sorbitol if there are no bowel sounds; MDAC may be aproblem b/c of decreases gut motility (enemas may help)
Physostigmine‣ Acetylcholinesterase inhibitor thus increases acethylcholine at synapse‣ Physostigmine is the ONLY agent that can cross the BBB for a central effect‣ Risk: can cause seizures; asystole reported after TCA ingestion;‣ Benefit: reverses delirium in 96% of patients thus is diagnostic and therapeutic‣ Dose: 1-2 mg iv and repeat prn‣ Contraindications: blocks on ECG (risk of asystole); suspected TCA ingestionDisposition: observe 4-6 hrs unless it is a delayed onset agent like Datura stramonium seeds