GENERAL APPROACH TO THE POISONED PATIENT - rEMERGs
GENERAL APPROACH TO THE POISONED PATIENT - rEMERGs
GENERAL APPROACH TO THE POISONED PATIENT - rEMERGs
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
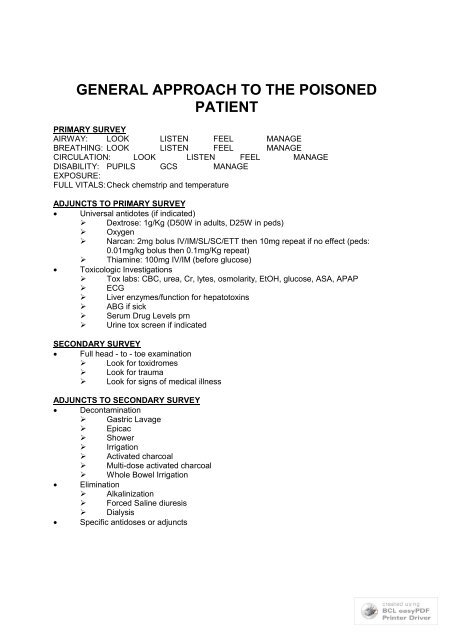
<strong>GENERAL</strong> <strong>APPROACH</strong> <strong>TO</strong> <strong>THE</strong> <strong>POISONED</strong><strong>PATIENT</strong>PRIMARY SURVEYAIRWAY: LOOK LISTEN FEEL MANAGEBREATHING: LOOK LISTEN FEEL MANAGECIRCULATION: LOOK LISTEN FEEL MANAGEDISABILITY: PUPILS GCS MANAGEEXPOSURE:FULL VITALS:Check chemstrip and temperatureADJUNCTS <strong>TO</strong> PRIMARY SURVEY Universal antidotes (if indicated)‣ Dextrose: 1g/Kg (D50W in adults, D25W in peds)‣ Oxygen‣ Narcan: 2mg bolus IV/IM/SL/SC/ETT then 10mg repeat if no effect (peds:0.01mg/kg bolus then 0.1mg/Kg repeat)‣ Thiamine: 100mg IV/IM (before glucose) Toxicologic Investigations‣ Tox labs: CBC, urea, Cr, lytes, osmolarity, EtOH, glucose, ASA, APAP‣ ECG‣ Liver enzymes/function for hepatotoxins‣ ABG if sick‣ Serum Drug Levels prn‣ Urine tox screen if indicatedSECONDARY SURVEY Full head - to - toe examination‣ Look for toxidromes‣ Look for trauma‣ Look for signs of medical illnessADJUNCTS <strong>TO</strong> SECONDARY SURVEY Decontamination‣ Gastric Lavage‣ Epicac‣ Shower‣ Irrigation‣ Activated charcoal‣ Multi-dose activated charcoal‣ Whole Bowel Irrigation Elimination‣ Alkalinization‣ Forced Saline diuresis‣ Dialysis Specific antidoses or adjuncts
CLINICAL FEATURES OF <strong>TO</strong>XICOLOGY<strong>TO</strong>XICOLOGICAL HIS<strong>TO</strong>RY Overdose details: What, when, route, dose, co-ingestants, why EMS should bring all prescription bottles Get pharmacy printout Identify pills and make sure pills equal label Look through medications on old chart Ask family/friend about possible ingestants Ask what else is available in the house (INH example) Bring in containers Search the patient Have family or police search the patient’s house Consider body packing/stuffing if ingestant unknown Specifically ask about SLOW - RELEASE preparations<strong>TO</strong>XICOLOGICAL EXAMINATION Accurate vital signs essential Look for signs of trauma: head trauma important Look for signs of medical illness Look for body packing/stuffing Look for toxidromes = constellations of signs and symptoms associated with a class ofdrug or toxin‣ Level of consciousness‣ HR, BP, temp‣ Pupils‣ Skin‣ Bowel sounds‣ Reflexes, rigidity Odors in OverdosesAlmondsCyanideCarrotsWater hemlockFishyZinc or aluminumFruityEtOH, acetone, isopropanol, hydrocarbonsGarlicArsenic, etcGlueToluene, solventsPearsChloral hydrate, paraldehydeRotten eggs H2S, NACShoe polish Nitro benzeneWintergreen Methyl salicylate
<strong>TO</strong>XINS CAUSING SEIZURESCAPITCyclic antidepressantsCholinergics:organophosphatesCaffeineCamphorAmphetaminesAntihistaminesAmoxapinePhenothiazinesPropranololPhenylpropanolaminePiroxicamIsoniazid (think inaboriginals, refractoryseizures, or anyone onTB Rx)Theophylline<strong>TO</strong>XINS CAUSING TEMP CHANGES Hyperthermia‣ Anitcholinergics‣ Sympathomimetics‣ Seritonin syndrome‣ Salicylates‣ Methylxanthines‣ Thyroxoine‣ NMS Hypothermia‣ CO‣ Opiates‣ Oral hypoglycemics‣ Insulin‣ Alcohol‣ Sedatives‣ Hypnotics‣ Phenothiazines<strong>TO</strong>XINS AND CV CHANGESTACHYCARDIABRADYCARDIAWCT<strong>TO</strong>XINS CAUSING PINPOINTPUPILS (MIOSIS)ClonidineOpiates (except demerol)OrganophosphatesPCPPhenothiazinesPilocarpineTCAPhenothiazineTheophyllineChloral HydrateAny stimulantSSRIsSNRIsCholinergicsBeta BlockersCCBsDigoxinNa channelblockersOpiatesSedative/hypnoticsAlpha agonistsGHBTrazadoneTCAsAntihistaminesCocainesOther stimulantsBBCCBDigoxinCarbemazepineQuinineChloroquinePhenothiazines
<strong>TO</strong>XICOLOGY AND <strong>THE</strong> LABDRUG SCREENS NOT ROUTINELY INDICATED‣ Lab doesn’t screen for most drugs‣ Initial screen may be negative if done soon after the ingestion‣ Positive findings may not be the cause of the presentation (cocaine +ve inurine for days after use)‣ Expensive‣ Rarely change clinical managmentANION GAP The difference between measured cations and anions There truly is no difference b/c electrical neutrality is maintained but we don’t measure all cationsand anions thus a measured gap is evident Cations: Na+ is vast majority (Ca, Mg, K are minority) Anions: Cl-, HC03- Anion Gap made up mostly of albumin: thus hypoalbuminemic patients have a lower anion gapand increased AGMA may not be picked up (AG may go from 5 to 10 but is still within thenormal range) Low anion gap ( +6: simultaneous metabolic alkalosis or respiratory acidosis‣ low delta G < -6: simultaneous respiratory alkalosis or low AG state Other‣ CO/CN: oxidative phosphorylation inhibition‣ EtOH: ethyl alcohol donates an H+ thus mild direct acidosis; also respiratorydepression and dehydration thus mild indirect acidosis‣ Paraldehyde: acetic and chloracetic acid‣ Methanol: formic acid‣ Ethylene glycol: oxalic acid‣ Isoniazid: > 30 mg/kg causes lifethreatening acidosis, acidosis is secondary tolactate production during seizure; pyridoxine and dialysis as treatment‣ Iron: inhibits oxidative phosphrylation, negative ionotrope, dehydrated, GIbleeding/hypovolemia, and Fe2+ —> F3 + + H+ all contribute to acidosis‣ ASA: acetylsalicylic acid, salicylic acid, also inhibits oxidative phosphorylationthus lactic acidosis (major mechanism), ketoacidosis, aminoacids (catabolic statedue to inhibition of oxidative phosphyrlation); note combined A/B disorder b/c ofstimulation of respiratory centers and respiratory alkalosis‣Toluene-inhaled hydrocarbon; often abused
-acrylic paints, glues, adhesives, paint, varnish, laquers-sniffing (breath over a container), huffing (sniff from a rag) or bagging(sniff from a bag)-rapid absorption to lungs, CNS intoxication for hours-CNS: stupor, intoxication, sz, ataxia, headache, hallucination-CVS: arrythmias and sudden death (SENSITIZED MYOCARDIUM tocatecholamines); inhaled hydrocarbon then exertion —> sudden deathToxins that increase AGMA independent of lactate‣ ASA‣ Methanol‣ Ethylene glycolDIFFERENTIAL DIAGNOSIS OF INCREASED AGMAAMUDPILECA<strong>TO</strong>AKA, ASA, alcohol intoxicationMethanolUremiaDKAParadehyde, Phenformin (Metformin)Iron, Isoniazid, Ibuprofen (rare)Lactic acidosis (any cause)Ethylene glycolCO, CNASAToluene, TheophyllineOther H2S MetforminOSMOLAR GAP Osmolality = measured osmolality‣ Lab measurement of moles of solute/kg of solvent‣ Measured by freezing point depression‣ Can also be measured by vapor pressure but this is less reliable b/cerroneously low results will occur with volatile substances (alcohols) Osmolarity = osmolarity calculated‣ Calculated moles of solute/L of solution‣ Different formulas exist‣ Calgary lab uses: 1.86Na + BUN + glucose + 9 + EtOH (this assumesNa+ Cl- ionized forms which is more accurate)
PASCALAProteinsAlcohols- Ethanol- Methanol- Isopropanol- Propylene glycol (plumming antifreeze, diluant for many drugs)- Diethylene glycol- Triethylene glycolSurgars- Mannitol- Glycerol- SorbitolContrast dyeAcidosis- Lacticacidosis- Ketoacidosis (DKA, AKA)LipidsAcetone
<strong>TO</strong>XICOLOGICAL TESTS Immunoassays‣ Uses antibodies to detect drugs or metabolites Chromatography‣ Analyte specificity is achieved by physical separation‣ Major advantage: multiple substances can be detected in a singleprocedure‣ Can look for many different compounds thus more useful for generalscreening‣ Thin Layer Chromatography: substance put on thin layer plate, solvent isdrawn up the plate by capillary action; compared to controls; slow andlabor intensive‣ High Performance Liquid Chromatography: similar idea but the mobilephase is pumped through under high pressure; peaks are detecteddepending on how far the substance “moved” down the plate and arecompared to controls‣ Gas Chromatography: similar idea but the moving phase is a gas‣ Mass spectrometer: a highly sensitive “detector” to detect very smallquantities; mas spec uses electromagnetic filtering to determine the massof the ions; ultimately produces peaks on graph that are characteristic ofcertain drugs Urine Tox screens‣ Vary with each lab‣ Most urine screens use immunoassays‣ Confirmatory Gas chromatography and mass spec is done ifimmunoassay is +ve
DECONTAMINATION<strong>GENERAL</strong> Definition‣ Decontamination is the prevention of absorption into the bloodstream Factors to consider‣ Is this a dangerous toxin?‣ Is there likely to be further absorption?‣ How long from the time of ingestion?‣ Is there an effective antidote?‣ Has the clinical course excluded the posibility of toxicity? Gastric Emptying‣ Most studies show that minimal drug is in stomach after 2-4 hours‣‣Vomiting‣‣‣‣‣Time in stomach varies with drugDrugs that SLOW gastric emptying and increase the possible time forgastric empyting to be effective Anticholinergics Opiates Sedative/hypnotics Gastric concretions: ASA, iron, phenobarbitalSelf induced vomiting and ipecac are never indicatedUnlikely to removed significant amount of toxinRisk of aspirationIpecac hinds administration of charcoalRisk of MWTs, esophageal ruptureGASTRIC LAVAGE Technique of Gastric Lavage‣ Large gastric tube (36 french)‣ Left lateral position‣ Tap water or saline‣ 300 cc in, clamp, drain by gravity‣ Continue until clear; follow lavage with activated charcoal Potential Complications‣ Injury to pharynx‣ Esophageal tears‣ Gastric perforation‣ Aspiration Evidence Behind and Controversies‣ Shown to decrease drug absorption in volunteers‣ Only (limited) clinical benefit has been shown if done LESS than one hour‣ Has been trends toward clinical improvements in serious overdoses‣ Some people advocate never using gastric lavage, BUT!!‣ ACEP policy statement: little to indicate value; selective use only‣ Study limitations Small sample sizes thus not powered to exclude clinicallyimportant differences
Include multiple different overdoses Exclude critically ill patients (where it is really needed!!) Poor controls, poor randomization Hasn’t been specifically studied where it makes moresense (enteric coated, pylorospasms, gastric concretions,etc)Indications for gastric lavage‣ No universal indications can be given‣‣Case-by-case consideration is appropriateConsiderations FOR gastric lavage Potentially lethal overdose NO effective antidote Patient currently symptomatic Time since ingestions < 1-2 hours Charcoal ineffective (Li, Fe) Gastric concretions (ASA, Fe, enteric coated, phenobarb) Pylorospasm (ASA) No antecedant vomiting Delayed gastric absorption (anticholinergics, narcotics,enteric coated preparations)Contraindications‣ Inability to protect airway (ie; must intubate)ACTIVATED CHARCOAL Dose‣ No universal correct dose; no maximum dose known‣ Ideal charcoal:drug ratio is 10:1‣ Most common initial doses: 0.5 - 1.0 g/kg (Adults = 50 gm)‣ Use larger doses (1.5 - 2.0 g/kg) for dangerous large ingestions of agentswell absorbed by charcoal: ASA, theophylline, verapamil SR How beneficial is activated charcoal?‣ Lowers absorption, lower peak serum levels, decreased area under thecurve‣ Beneficial only if substance still present in the GI tract and binds tocharcoal‣ Many animal studies showing benefit‣ Many human studies showing decreased absorption‣ Limited studies to show clinical benefit Indications‣ Should be administered in virtually all cases of potentially toxic overdoses‣ More effective earlier but history is so inaccurate, reasonable to give evenwith later presentations‣ Consider using for overdose of toxin that doesn’t bind charcoal b/c ofpossibility of co-ingestant Drugs NOT absorbed by charcoal‣ C Caustics‣ H Hydrocarbons
‣ I Iron‣ L Lithium, Lead‣ E EthanolMultidose Activated Charcoal (MDAC)‣ Doses and frequency varies with indication‣ Can be given by continuous NG infusion‣ Massive ingestion: one dose won’t be enough‣ Sustained release: delayed release of drug‣ Gastric concretions‣ Enhanced elimination: prevents enterohepatic reabsorption of active drugor metabolites?Contraindications‣ Caustic ingestions: doesn’t bind, obscures endoscopy‣ Unprotected airway‣ Hydrocarbons: increased risk of aspiration and ARDSComplications‣ Very safe‣ GI upset‣‣Bowel obstruction: case reports with MDACAspiration is biggest risk Trivial aspiration very common Significant aspiration rareCATHARTICS Purpose = increase GI transit speed, decrease transit time No proven benefit Effect on activated charcoal: occasionally benefitial, usually no effect, occasionallyharmful Only three used with any frequency: sorbital, magnesium sulfate, magnesium citrate Sorbital: 1 gm/kg; repeat dose X 1 only at 0.5 mg/kg with MDAC if no ileus/obstruction No evidence of harm for single use if no contraindications Complications: dehydration, electrolyte changes, GI upset, abdominal distension Children have more problems with fluid and electrolyte shifts Relative contraindications:‣ Bowel obstruction‣ Ileus (absent bowel sounds)‣ Diarrhea (uneccessary)‣ Infants and young childrenWHOLE BOWEL IRRIGATION General‣ More effective than clearing bowel than cathartic‣ PEG-ELS solution is electrolyte and osmolarity balanced thus nofluid/electrolyte shifts (isotonic components); huge volumes are notdangerous‣ Components are not absorbed‣ Mechanical washout of bowel (doesn’t draw in fluid or stimulate motility) Indications for WBI: serious overdoses, poor binding to charcoal, sustained release
‣‣‣‣‣IronLithiumBody packersBody stuffersSlow release preparations ASA CCBs Valproic acidO<strong>THE</strong>R GI DECONTAMINATION Endoscopic removal: difficult to remove concretions and body packs; complications ofprocedure usually outweigh potential benefit; rarely indicated (very durable packs withbody packers) Surgical removal: rarely body packs causing bowel obstruction or intestinal ischemia Surgery post GI perforation after caustic ingestionsELIMINATION<strong>GENERAL</strong> Elimination = removal of toxin after it has been absorbed Indications‣ Patients who fail supportive care‣ Patients in whom the normal route of elimination is impaired (renal failure)‣ Patients in whom the toxin is expected to be very significant‣ Patients that are not expected to tolerate the physiologic effects Methods of Elimination‣ MDAC‣ Hemodialysis‣ Urine alkalinization‣ Peritoneal dialysis‣ Charcoal hemoperfusion‣ Hemofiltration‣ Plasmapheresis‣ Exchange transfusion‣ Diuresis‣ Chelation Ion Trapping = Urine Alkalinization‣ ASA‣ Barbituates‣ Formic acid (methanol): minor role‣ Methotrexate‣ Chlorpropamide (Diabenese - oral hypoglycemic)HEMODIALYSIS What are features of dialyzable drugs?‣ Low Vd‣ Low protein binding‣ Small molecular weights‣ Water soluble
‣ Single compartment kinetics‣ Low endogenous clearanceAdv of hemodialysis over other extracorporeal techniques‣ Corrects acid - base abnormalities‣ Corrects electrolyte abnormalities‣ Removes MORE drug than CRRT (continous hemofiltration)Toxins well removed by HEMODIALYSIS‣ Methanol‣ Ethylene Glycol‣ Isopropranol‣ ASA‣ Lithium‣ Valproic acid‣ TheophyllinDIALYZABLE OVERDOSESM MethanolE Ethylene GlycolT TheophyllineI IsopropranolV Valproic AcidA ASAL LithiumPossibly effective dialysis‣ Amanita mushroom toxin‣ Tegretol‣ BB: atenolol, sotalol‣ Paraquat‣ Phenytoin‣ Phenobarbital‣ Procainamide‣ Methotrexate
DIAGNOSTIC IMAGING AND <strong>TO</strong>XICOLOGYRADIOPAQUE INGESTIONSCChloral hydrate, Calcium carbonateHHeavy metals (iron, lead, arsenic, lithium, zinc), barium, bisthmusIIronPPlay-dohPPhenothiazines, Potassium chlorideEEnteric coated pillsDDental amalgamED MANAGEMENT Approach: see ToNotes Decontamination(1) Ipecac: NO role in ED b/c emesis will only dec absp by 30%. May beindicated for use at the home(2) Gastric Lavage‣ orogastric hose 30 - 40 F‣ infuse 300ml until fluid is clear‣ adv: immediate recovery of gastric material, control lavageduration, direct access for instillation of charcol‣ disadv: invasive, efficacy is questionable a/f 1-2h postingestion,aspiration risk (decreased by trendelenberg)(3) Shower Decrease Absorption(1) Activated Charcol‣ agent of choice for gastrointestinal decontamination inacute‣ may reduce absorption by 50% alone‣ dose: 1g/Kg‣ disadv: poor pt acceptance, messy(5) Cathartics‣ theory: speed up GI motility :. shortening time forabsorption‣ but: not shown to improve pt outcome and may increaseabsortpion‣ disadv: frequent liquid stools, dehydration and lyteimbalances esp in children(6) Whole Bowel Irrigation‣ used in body stuffers and sustained-release or enteridccoatedmedication overdoses‣ NG tube then goGo-Litely @ 1-2 L/hr until objects
emoved or effluent clearIncreased Elimination(1) Dialysis(2) Forced Diuresis(3) Alkalinization of serum‣ TCA example: changing pH from 7.45 to 7.50 increasesalbumin binding from 95 - 96% of drug :. free drug (whichis active) goes from 5% to 4% which is a 20% reduction inthe amount of free drug.‣ Alkalinization also changes the intracellular pH and allowsthe open of H/M ? gates of the Na+ channel and release ofthe TCA(4) Alkalinization of the urine‣ Ion Trapping of ASA in the urine b/c the alkalinized formis not reabsorbed as well.Supportive Care(1) Oxygen, IV, Monitor(2) Management of Respiratory Complications‣ Airway protection: intubation if necessary‣‣Ventilation may be necessaryARDS: high-flow oxygen, +ve pressure ventilation,consider PEEP(3) CV Complications‣ arrythmias as per ACLS‣ hypotension: fluids only (vassopressors rare)‣ hypertension: nitroprusside, CCBs(4) Neuro Complications‣ coma: airway etc‣ seizures: very dangerours, standard tx w/ benzos andphenobarb, paralyzing agents may be needed initially tocontrol prolonged sz (pancuronium)‣behavioural abnormailities: chemical sedation is dangerousb/c of cardioresp compromise :. use physical restraints ifpossible: ativan and haloperidol are effective if necessaryDiagnostic Studies‣ Drug Screens: urine and blood‣ Routine labs‣ ABGs importantDefinitive Care‣ Antagonists: see table 129-2, pp740‣ All poisoned pts should get oxygen, glucose, and naloxozone (narcan)‣ Elimination: example is alkalinization of urine in ASA od