APPENDICES - NIHR Health Technology Assessment Programme
APPENDICES - NIHR Health Technology Assessment Programme
APPENDICES - NIHR Health Technology Assessment Programme
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
DOI: 10.3310/hta14370 <strong>Health</strong> <strong>Technology</strong> <strong>Assessment</strong> 2010; Vol. 14: No. 37<br />
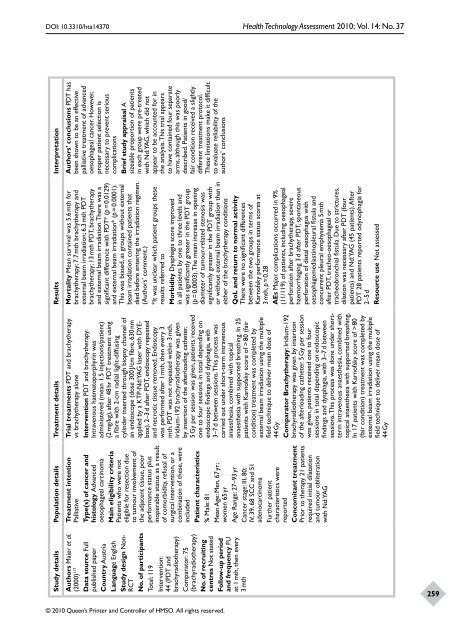
Study details Population details Treatment details Results Interpretation<br />
Authors’ conclusions PDT has<br />
been shown to be an effective<br />
palliative treatment of advanced<br />
oesophageal cancer. However,<br />
proper patient selection is<br />
necessary to prevent serious<br />
complications<br />
Brief study appraisal A<br />
sizeable proportion of patients<br />
in each group were pre-treated<br />
with Nd:YAG, which did not<br />
appear to be accounted for in<br />
the analysis. This trial appears<br />
to have contained four separate<br />
arms, although this was poorly<br />
described. Patients in good/<br />
fair condition received a slightly<br />
different treatment protocol.<br />
These limitations make it difficult<br />
to evaluate reliability of the<br />
authors’ conclusions<br />
Mortality Mean survival was 5.6 mth for<br />
brachytherapy; 7.7 mth brachytherapy and<br />
external beam irradiation; 6.3 mth PDT<br />
brachytherapy; 13 mth PDT, brachytherapy<br />
and external beam irradiation. There was a<br />
significant difference with PDT* (p = 0.0129)<br />
and external beam irradiation* (p = 0.0001).<br />
This was biased, as groups without external<br />
beam irradiation contained patients that<br />
died before entering the irradiation regimen.<br />
(Authors’ comment.)<br />
*It was unclear which patient groups these<br />
results referred to<br />
Morbidity Dysphagia score improved<br />
in all patients by one to three levels and<br />
was significantly greater in the PDT group<br />
(p = 0.0003). The mean increase in opening<br />
diameter of tumour-related stenosis was<br />
significantly greater in the PDT group with<br />
or without external beam irradiation than in<br />
either of the brachytherapy conditions<br />
QoL and return to normal activity<br />
There were no significant differences<br />
between the two groups in terms of<br />
Karnofsky performance status scores at<br />
3 mth, p = 0.28<br />
AEs Major complications occurred in 9%<br />
(11/119) of patients, including oesophageal<br />
perforation after brachytherapy, severe<br />
haemorrhaging 3 d after PDT, spontaneous<br />
perforation of distal oesophagus with<br />
oesophagomediastinopleural fistula and<br />
concurrent pleural emphysema 5 mth<br />
after PDT, tracheo-oesophageal or<br />
tracheobronchial fistula. Due to strictures,<br />
dilation was necessary after PDT (four<br />
patients) and Nd:YAG (45 patients). After<br />
PDT 28 patients reported odynophagia for<br />
2–5 d<br />
Resource use Not assessed<br />
Trial treatments PDT and brachytherapy<br />
vs brachytherapy alone<br />
Intervention PDT and brachytherapy:<br />
Intravenous haematoporphyrin was<br />
administered (mean 1.5 injections/patient)<br />
(2 mg/kg), after 48 hr PDT treatment using<br />
a fibre with 2-cm radial light-diffusing<br />
cylinder inserted through biopsy channel of<br />
an endoscope (dose 300 J/cm fibre, 630 nm<br />
applied by a KTP-Nd:YAG laser with DYEbox).<br />
2–3 d after PDT, endoscopy repeated<br />
and necrotic tissue removed. Endoscopy<br />
was performed after 1 mth, then every 3<br />
mth. PDT was not repeated within 3 mth.<br />
Iridium-192 brachyradiotherapy was given<br />
by insertion of the afterloading catheter.<br />
5 Gy per session was given, patients received<br />
one to four sessions in total depending on<br />
endoscopic findings and dysphagia, with<br />
3–7 d between sessions. This process was<br />
carried out under short-term intravenous<br />
anaesthesia, combined with topical<br />
anaesthesia with supported breathing. In 25<br />
patients with Karnofsky score of > 80 (fair<br />
condition) treatment was completed by<br />
external beam irradiation using the multiple<br />
field technique to deliver mean dose of<br />
44 Gy<br />
Comparator Brachytherapy: Iridium-192<br />
brachyradiotherapy was given by insertion<br />
of the afterloading catheter. 5 Gy per session<br />
was given, patients received one to four<br />
sessions in total depending on endoscopic<br />
findings and dysphagia, with 3–7 d between<br />
sessions. This process was done under shortterm<br />
intravenous anaesthesia, combined with<br />
topical anaesthesia with supported breathing.<br />
In 17 patients with Karnofsky score of > 80<br />
(fair condition) treatment was completed by<br />
external beam irradiation using the multiple<br />
field technique to deliver mean dose of<br />
44 Gy<br />
Treatment intention<br />
Palliative<br />
Type(s) of cancer and<br />
histology Advanced<br />
oesophageal carcinoma<br />
Main eligibility criteria<br />
Patients who were not<br />
eligible for resection due<br />
to tumour involvement of<br />
the adjacent tissue, poor<br />
performance status plus<br />
inoperable status as a result<br />
of comorbidity, refusal of<br />
surgical intervention, or a<br />
combination of these, were<br />
included<br />
Patient characteristics<br />
% Male: 81<br />
Mean Age: Men, 67 yr;<br />
women 65 yr<br />
Age Range: 27–93 yr<br />
Cancer stage: III, 80;<br />
IV, 39. 68 SCC and 51<br />
adenocarcinoma<br />
Further patient<br />
characteristics were<br />
reported<br />
Concomitant treatment<br />
Prior to therapy 21 patients<br />
required initial dilatation<br />
and tumour obliteration<br />
with Nd:YAG<br />
Authors Maier et al.<br />
(2000) 117<br />
Data source Full<br />
published paper<br />
Country Austria<br />
Language English<br />
Study design Non-<br />
RCT<br />
No. of participants<br />
Total: 119<br />
Intervention:<br />
44 (PDT and<br />
brachyradiotherapy)<br />
Comparator: 75<br />
(brachyradiotherapy)<br />
No. of recruiting<br />
centres Not stated<br />
Follow-up period<br />
and frequency FU<br />
at 1 mth, then every<br />
3 mth<br />
© 2010 Queen’s Printer and Controller of HMSO. All rights reserved.<br />
259