« Maladie de Lyme » Borréliose
« Maladie de Lyme » Borréliose
« Maladie de Lyme » Borréliose
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>«</strong> <strong>Maladie</strong> <strong>de</strong> <strong>Lyme</strong> <strong>»</strong><br />
<strong>Borréliose</strong><br />
E. Denes
Vecteur et bactérie
Ixo<strong>de</strong>s ricinus<br />
7
Coucou !<br />
8
Distribution d’Ixo<strong>de</strong>s ricinus<br />
9
Cycle<br />
10
Borrelia<br />
11
Distribution <strong>de</strong>s Borrelia<br />
n Borrelia burgdorferi stricto sensu<br />
n Etats-Unis<br />
n Borrelia burgdorferi sensu lato<br />
n France<br />
n Afzelii (50%)<br />
n Garinii (29,6%)<br />
n Valaisana (18,5%)<br />
12
Transmission<br />
n Tiques porteuses (France) :<br />
n 10 – 15 %<br />
n Fixation < 24 h : Pas <strong>de</strong> transmission<br />
n Fixation > 72 h : Transmission<br />
n Risque <strong>de</strong> transmission en France<br />
n 7 - 10 %<br />
13
Borrelia et Clinique<br />
14
Inci<strong>de</strong>nce en France<br />
15
Distribution <strong>de</strong> Borrelia<br />
16
Clinique
Quand évoquer un <strong>Lyme</strong> ?
Contexte<br />
n Notion <strong>de</strong> morsure <strong>de</strong> tique<br />
n Manifestations cliniques compatibles<br />
n M Pas d’immunité efficace<br />
n Réinfection possible<br />
19
Différents sta<strong>de</strong>s<br />
n Sta<strong>de</strong> primaire<br />
n Sta<strong>de</strong> secondaire<br />
n Sta<strong>de</strong> tertiaire<br />
20
Phase primaire<br />
n Erythème chronique migrant<br />
n Pathognomonique<br />
21
Erythème chronique migrant<br />
n > 5 cm (jusqu’à 75 cm)<br />
n Délai d’apparition<br />
n 3 j – 1 mois<br />
n Retrouvé dans 30 % <strong>de</strong>s cas<br />
n +/- Syndrome grippal et ganglions <strong>de</strong><br />
drainage<br />
n Sérologie inutile<br />
n Biologie : RAS<br />
22
Erythème chronique migrant<br />
23
Phase précoce disséminée<br />
n Erythèmes multiples<br />
n Myalgies, arthralgies<br />
n Radiculite<br />
n Atteinte articulaire (arthrite)<br />
n Atteinte cardiaque<br />
n Neuroborréliose précoce<br />
24
Phase secondaire<br />
n Si phase primaire non traitée ou passée<br />
inaperçue<br />
n Infection tissulaire focalisée<br />
n Unique<br />
n Multiple<br />
n Neurologique<br />
n Articulaire<br />
25
n Neurologique<br />
n Meningo-radiculite<br />
n Méningite isolée<br />
n Méningo-myélite<br />
n Méningoencéphalite<br />
n Ponction lombaire à Méningite lymphocytaire<br />
n Sauf pour PF<br />
26
Atteinte articulaire<br />
n Rare en Europe<br />
n Grosses articulations (genou, …)<br />
n Mono ou oligo-articulaire<br />
n Arthrite intermittente<br />
n HLA-DR2 ou DR4<br />
27
n Plus rarement<br />
n Lymphocytome (oreilles – mamelons – OGE)<br />
n Atteinte cardiaque<br />
n Trouble du rythme et conduction<br />
n Myocardite, péricardite<br />
n Atteinte oculaire<br />
n Atteinte <strong>de</strong> toutes les structures <strong>de</strong> l’oeil<br />
28
Phase tertiaire<br />
n Neurologique<br />
n Encéphalomyélite chronique<br />
n Encéphalite (subaiguë, chronique, trouble cognitif,<br />
trouble <strong>de</strong> la mémoire)<br />
n Polyradiculonévrite sensitives axonales<br />
n Douleur radiculaire<br />
n LCR : anomalies<br />
n Synthèse intra-téchale d’Ac<br />
29
n Acro<strong>de</strong>rmatite atrophiante<br />
30
n Arthrites<br />
n Aigues<br />
n Chroniques<br />
n Récidivantes<br />
31
Quand ne pas y penser ...<br />
n Symptômes chroniques<br />
n Adénopathie<br />
n Fièvre<br />
n Fatigue chronique<br />
n Fibromyalgie<br />
n ...<br />
n Petite histoire… (diplopie)<br />
32
Syndrome post <strong>Lyme</strong><br />
n Asthénie<br />
n Algies diffuses<br />
n Plaintes cognitives<br />
n Lien direct avec B. burgdorferi ?<br />
n Pas <strong>de</strong> nouveau traitement antibiotique<br />
33
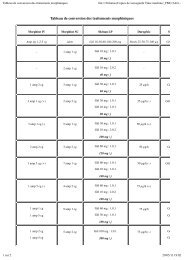
Symptomes cliniques<br />
Kalish 2001 Selzer 2000 Shadick1994<br />
Suivi 10-20<br />
ans<br />
M+51 Suivi à 6 ans<br />
N = 84 N = 678 N = 50<br />
Douleur musculo-squeletique 56% 40% 21%<br />
Tbl mémoire 30% 23%<br />
Fatigue 43% 24% 9%<br />
Céphalées 20% 19%<br />
Douleur cou 15%<br />
Pb d’appétit 6%<br />
Pb trouver mots 30%<br />
Pb nommer objets 25%<br />
Pb au travail 6%<br />
Pb pour dormir 36% 23% 16%<br />
Pb concentration 13% 2%<br />
34
Symptômes cliniques<br />
Kalish 2001 Selzer 2000 Shadick1994<br />
Suivi 10-20<br />
ans<br />
M+51 Suivi à 6 ans<br />
N = 84 N = 678 N = 50<br />
Douleur musculo-squeletique 56% 44% 40% 28% 21%<br />
61%<br />
Tbl mémoire 30% 36% 23% 21%<br />
Fatigue 43% 46% 24% 16% 9%<br />
26%<br />
Céphalées 20% 16% 19% 13%<br />
Douleur cou 15% 14%<br />
Pb d’appétit 6% 4%<br />
Pb trouver mots 30% 22%<br />
Pb nommer objets 25% 17%<br />
Pb au travail 6% 5%<br />
Pb pour dormir 36% 28% 23% 13% 16%<br />
47%<br />
Pb concentration 13% 20% 2%<br />
16%<br />
35
Diagnostic
Type <strong>de</strong> test<br />
n Détection antigènes boréliens<br />
n ELISA<br />
n Western Blot<br />
n Détection directe<br />
n PCR<br />
n Pas en routine (recherche / formes atypiques)<br />
n Pas <strong>de</strong> syndrome inflammatoire franc<br />
37
ELISA<br />
n Nécessité d’une Se > 90 %<br />
n Attention réaction croisée<br />
n Ban<strong>de</strong> 41 kD<br />
n Antigénicité croisée avec<br />
n Autres micro-organisme flagellés<br />
n Tissus <strong>de</strong> l’hôte (SNC, synovial, myocar<strong>de</strong>)<br />
n Ban<strong>de</strong> 39 kD<br />
n Variabilité inter espèce<br />
38
ELISA<br />
n Attention<br />
n Réactions croisées<br />
n Syphilis, EBV, CMV, M. pneumoniae, Syphilis<br />
n Stimulations polyclonales (FR)<br />
n Pathologies dys-immunitaires (Lupus)<br />
n Persistances IgG/IgM<br />
n Mois / années<br />
n Même si traitement (Cicatrice sérologique)<br />
n Attention kit pour LCR<br />
39
Western Blot<br />
n Confirmation <strong>de</strong> la spécificité <strong>de</strong>s Ac<br />
n Pas <strong>de</strong> critère d’interprétation défini<br />
n Nb <strong>de</strong> ban<strong>de</strong>s<br />
n Types <strong>de</strong> ban<strong>de</strong>s<br />
n Spécificité : 99%<br />
n IgM anti OspC et 41 kD : infection<br />
débutante<br />
41
Démarche diagnostic<br />
n 1er : ELISA<br />
n - : Pas <strong>de</strong> test <strong>de</strong> confirmation<br />
n + / douteux : WB<br />
42
Pas d’indication<br />
n Sujets asymptomatiques<br />
n Dépistage systématique<br />
n Piqûre <strong>de</strong> tique sans clinique associée<br />
n ECM typique<br />
n Contrôle <strong>de</strong> sérologie <strong>de</strong>s patients traités<br />
43
Term Clinical Case Definition Laboratory evi<strong>de</strong>nce essential Laboratory evi<strong>de</strong>nce supporting<br />
Erythema<br />
(chronicum)<br />
migrans<br />
Borrelial<br />
lymphocytoma<br />
Early<br />
neuroborreliosis<br />
Expanding red or bluish-red patch, often with<br />
central clearing. Advancing edge typically<br />
distinct, often intensely coloured, not markedly<br />
elevated.<br />
Rare, painless bluish-red nodule or plaque,<br />
usually ear lobe, ear helix, nipple or scrotum<br />
more frequent in children (especially on ear)<br />
than in adults.<br />
Painful meningo-radiculoneuritis with or without<br />
facial palsy or other cranial neuritis (Garin-<br />
Bujadoux-Bannwarth syndrome). In children<br />
mostly meningitis, isolated unilateral<br />
(sometimes bilateral) facial palsy, other cranial<br />
neuritis.<br />
<strong>Lyme</strong> carditis Acute onset of atrio-ventricular (II-III) conduction<br />
disturbances, rhythm disturbances, sometimes<br />
myocarditis or pancarditis.<br />
<strong>Lyme</strong> arthritis Recurrent brief attacks of objective joint<br />
swelling in one, or a few, large joints,<br />
occasionally progressing to chronic arthritis.<br />
Acro<strong>de</strong>rmatitis<br />
chronica<br />
atrophicans<br />
Chronic<br />
neuroborreliosis<br />
Long-standing red or bluish-red lesions, usually on<br />
the extensor surfaces of extremities. Possible initial<br />
doughy swelling. Lesions eventually become<br />
atrophic. over bony prominences.<br />
A very rare condition. Long-standing encephalitis,<br />
encephalomyelitis, meningoencephalitis,<br />
radiculomyelitis.<br />
http://www.oeghmp.at/eucalb/diagnosis_case-<strong>de</strong>finition-outline.html<br />
None. Culture from skin biopsy.<br />
*Significant change in levels of<br />
specific antibodies or presence of<br />
specific IgM.<br />
*Significant change in levels of<br />
specific antibodies or presence of<br />
specific IgM.<br />
+ Intrathecally produced specific<br />
antibodies.<br />
*Significant change in levels of specific<br />
IgG antibodies.<br />
Presence of specific IgG antibodies<br />
(usually high levels)<br />
Presence of specific IgG antibodies<br />
(usually high levels)<br />
Lymphocytic pleocytosis in CSF.<br />
+ Intrathecally produced specific<br />
antibodies.<br />
Specific serum IgG.<br />
Histology. Culture from skin biopsy.<br />
Intrathecal total IgM and IgG.<br />
Specific oligoclonal bands in CSF.<br />
*Significant change in levels of<br />
specific antibodies or presence of<br />
specific IgM.<br />
Culture from CSF.<br />
Culture from endomyocardial biopsy.<br />
Culture from synovial fluid and/or<br />
tissue.<br />
Histology, culture from skin biopsy.<br />
Specific oligoclonal bands in CSF.<br />
45
Traitement
Oter la tique...<br />
Ne pas utiliser d’éther : risque <strong>de</strong> régurgitation<br />
47
Antibiotiques actifs<br />
n Pénicilline G<br />
n Amoxicilline<br />
n Ceftriaxone<br />
n Doxycycline<br />
48
Indication Thérapeutique<br />
n Erythème Chronique Migrans (ECM)<br />
n Neuro-borréliose<br />
n Arthrite<br />
n Atteinte cardiaque<br />
49
Non indication thérapeutique<br />
n Sérologie positive isolée<br />
n Prophylaxie après morsure <strong>de</strong> tique<br />
50
ECM<br />
n Doxycycline 200 mg/j<br />
n Amoxicilline p.o<br />
n 3-4 g/j (France)<br />
n Durée : 14 - 21 j<br />
51
Neuro-borréliose<br />
n Ceftriaxone : 2 g/j en parentéral pendant 4<br />
semaines<br />
n Doxycycline : 200 - 300 mg / j pendant 28<br />
j<br />
n Carlson, Neurology 1994; 44 : 1203-07<br />
n Avec Pru<strong>de</strong>nce …<br />
n Paralysie faciale isolée : traitement oral<br />
52
Arthrite<br />
n Doxycycline 200 mg/j<br />
n Amoxicilline p.o<br />
n Durée : 14 - 28 j<br />
53
Atteinte cardiaque<br />
n BAV du 1er <strong>de</strong>gré<br />
n Traitement par voie oral 21 j<br />
n BAV 2ème et 3ème <strong>de</strong>gré<br />
n Traitement par voie parentérale 21 jours<br />
n Son<strong>de</strong> d’entraînement<br />
54
Vaccination<br />
n Vaccin à partir <strong>de</strong> la lipoprotéine OspA<br />
n protéine <strong>de</strong> surface<br />
n Efficacité +<br />
n Mis sur le marché en 98 (USA)<br />
n retiré en 2002<br />
n Sigal / Steere : NEJM 1998 ; 339<br />
55
Phase primaire<br />
56
Phases secondaires et tertiaires<br />
57
Prophylaxie<br />
n ATB systématique après morsure n’est<br />
pas recommandée<br />
n Femme enceinte<br />
n Pas d’indication mais …<br />
n Enfant <strong>de</strong> moins <strong>de</strong> 8 ans<br />
n Pas d’indication mais …<br />
n Immunodéprimé :<br />
n Risque théorique<br />
60
<strong>Lyme</strong> Anxiety<br />
Extensive (often inaccurate) publicity about both the risks and the outcomes of <strong>Lyme</strong> disease<br />
has produced consi<strong>de</strong>rable anxiety about this disease (many states with no en<strong>de</strong>mic disease<br />
have <strong>Lyme</strong> disease support groups organized by patients). This concern has also led to<br />
inappropriate use of serological tests for <strong>Lyme</strong> disease as a screening test (often or<strong>de</strong>red as a<br />
result of requests by patients) in an attempt to i<strong>de</strong>ntify the cause of wi<strong>de</strong>ly prevalent,<br />
nonspecific symptoms such as pain and fatigue. This has, in turn, led to a virtual epi<strong>de</strong>mic of<br />
overdiagnosis and overtreatment of patients for <strong>Lyme</strong> disease, which only serves to perpetuate<br />
the myth that <strong>Lyme</strong> disease is commonly associated with severe, long-term morbidity. Most<br />
studies indicate that with rare exceptions, the outcomes for persons with <strong>Lyme</strong> disease are<br />
excellent. It is important for clinicians to consi<strong>de</strong>r what evi<strong>de</strong>nce (both clinical and<br />
epi<strong>de</strong>miological) there is to "rule in" <strong>Lyme</strong> disease before serological tests are or<strong>de</strong>red to rule<br />
out the diagnosis. Persons with only nonspecific symptoms and no objective signs of <strong>Lyme</strong><br />
disease are very unlikely to have <strong>Lyme</strong> disease, regardless of the results of serological tests.<br />
Inappropriate use of these tests frequently will result in misdiagnosis of <strong>Lyme</strong> disease and may<br />
prevent or <strong>de</strong>lay the patient from receiving appropriate care for the true problem.<br />
E. D. Shapiro and M. A. Gerber. <strong>Lyme</strong> Disease. Clinical Infectious Diseases<br />
2000;31:533-542<br />
62
www.eucalb.com<br />
n Media reports have coloured European public<br />
perceptions of LB by suggesting that the infection is<br />
difficult to diagnose and treat and has a high morbidity,<br />
but this applies only to a tiny minority of cases. Some of<br />
these misconceptions are due to misdiagnosis (mainly<br />
overdiagnosis) which may occur because clinical<br />
presentations of LB are not unique to that condition.<br />
Diagnosis is primarily clinical and takes into account the<br />
risk of tick bite. Supporting evi<strong>de</strong>nce is provi<strong>de</strong>d by<br />
laboratory investigation, usually antibody tests.<br />
n EUROPEAN UNION CONCERTED ACTION ON LYME BORRELIOSIS<br />
63
Référence<br />
n U.R. Hengee et al. <strong>Lyme</strong> borreliosis. The Lancet<br />
Infectious Diseases 2003; 3 : 489-500<br />
n G. Staneck, F. Strie. <strong>Lyme</strong> borreliosis. The<br />
Lancet. 2003 ; 362 : 1639 - 1647<br />
n G.P. Wormser et al. Practice gui<strong>de</strong>lines for the<br />
treatment of <strong>Lyme</strong> disease. Clinical Infectious<br />
Diseases. 2000 ; 31(suppl 1) : S1 - S14<br />
n A.C. Steere. <strong>Lyme</strong> disease. NEJM. 2001 ; 345 :<br />
115 - 125<br />
64
Références (suite)<br />
n http:// www.maladies-a-tiques.com/<br />
n http://www.oeghmp.at/eucalb/<br />
65