FEMTO-LASIK and BEYOND - Carl Zeiss, Inc.
FEMTO-LASIK and BEYOND - Carl Zeiss, Inc.
FEMTO-LASIK and BEYOND - Carl Zeiss, Inc.
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
24<br />
Ophthalmology WORLD REPORT<br />
International Refractive User Symposium<br />
Kuala Lumpur, Malaysia<br />
VisuMax<br />
in Keratoplasties<br />
Dr Khaled Ben Amor on “Keratoplasties<br />
with VisuMax”<br />
“Even in DLK, the results of<br />
femtosecond laser are very nice<br />
optically <strong>and</strong> we have much more<br />
success rate with the technique.”<br />
Keratoplasties with VisuMax: : Dr Ben Amor shared his<br />
experiences about the keratoplasty with VisuMax which<br />
according to him is “the obligation of the VisuMax,<br />
much beyond refractive surgery”. Discussing the advantages<br />
of the VisuMax he said that it offered a curved corneal interface<br />
<strong>and</strong> a planar cut. He then showed the high performance<br />
optics in ZEISS that was the key to optimum cut. He shared<br />
videos showing how it was easy to lift a donor graft <strong>and</strong> those<br />
for keratoconus hydrops, corneal scarring, bullous keratopathy<br />
<strong>and</strong> adherent leucoma. Dr Ben Amor also discussed the<br />
advantages of the femto penetrating keratoplasty due to the<br />
regular side cut. “Better centration <strong>and</strong> better donor recipient<br />
fit give a nice optical result better than that with a manual<br />
keratoplasty,” he said.<br />
Deep lamellar keratoplasty (DLK): He explained the principle<br />
approach in a DLK which required the separation of<br />
the endothelium from the stroma by injecting a bubble. In<br />
manual DLK, the bubble layer is seen in around 52% cases<br />
which necessitate desiccation of the rest of the stroma. According<br />
to him, Femto DLK ensures precision during surgery.<br />
Dpt<br />
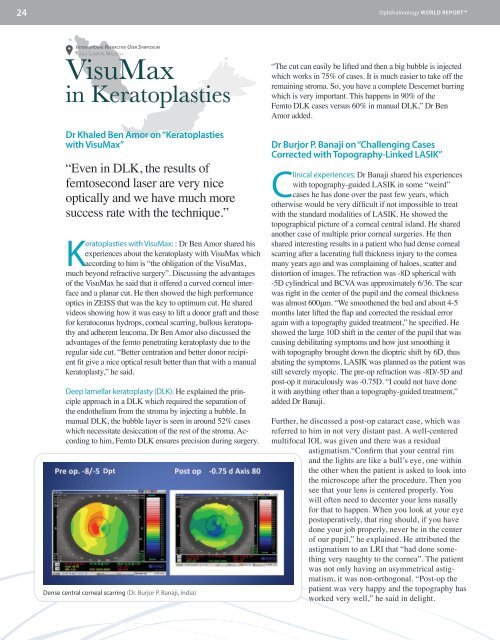
Dense central corneal scarring (Dr. Burjor P. Banaji, India)<br />
“The cut can easily be lifted <strong>and</strong> then a big bubble is injected<br />
which works in 75% of cases. It is much easier to take off the<br />
remaining stroma. So, you have a complete Descemet barring<br />
which is very important. This happens in 90% of the<br />
Femto DLK cases versus 60% in manual DLK,” Dr Ben<br />
Amor added.<br />
Dr Burjor P. Banaji on “Challenging Cases<br />
Corrected with Topography-Linked <strong>LASIK</strong>”<br />
Clinical experiences: Dr Banaji shared his experiences<br />
with topography-guided <strong>LASIK</strong> in some “weird”<br />
cases he has done over the past few years, which<br />
otherwise would be very difficult if not impossible to treat<br />
with the st<strong>and</strong>ard modalities of <strong>LASIK</strong>. He showed the<br />
topographical picture of a corneal central isl<strong>and</strong>. He shared<br />
another case of multiple prior corneal surgeries. He then<br />
shared interesting results in a patient who had dense corneal<br />
scarring after a lacerating full thickness injury to the cornea<br />
many years ago <strong>and</strong> was complaining of haloes, scatter <strong>and</strong><br />
distortion of images. The refraction was -8D spherical with<br />
-5D cylindrical <strong>and</strong> BCVA was approximately 6/36. The scar<br />
was right in the center of the pupil <strong>and</strong> the corneal thickness<br />
was almost 600μm. “We smoothened the bed <strong>and</strong> about 4-5<br />
months later lifted the flap <strong>and</strong> corrected the residual error<br />
again with a topography guided treatment,” he specified. He<br />
showed the large 10D shift in the center of the pupil that was<br />
causing debilitating symptoms <strong>and</strong> how just smoothing it<br />
with topography brought down the dioptric shift by 6D, thus<br />
abating the symptoms. <strong>LASIK</strong> was planned as the patient was<br />
still severely myopic. The pre-op refraction was -8D/-5D <strong>and</strong><br />
post-op it miraculously was -0.75D. “I could not have done<br />
it with anything other than a topography-guided treatment,”<br />
added Dr Banaji.<br />
Further, he discussed a post-op cataract case, which was<br />
referred to him in not very distant past. A well-centered<br />
multifocal IOL was given <strong>and</strong> there was a residual<br />
astigmatism.“Confirm that your central rim<br />
<strong>and</strong> the lights are like a bull’s eye, one within<br />
the other when the patient is asked to look into<br />
the microscope after the procedure. Then you<br />
see that your lens is centered properly. You<br />
will often need to decenter your lens nasally<br />
for that to happen. When you look at your eye<br />
postoperatively, that ring should, if you have<br />
done your job properly, never be in the center<br />
of our pupil,” he explained. He attributed the<br />
astigmatism to an LRI that “had done something<br />
very naughty to the cornea”. The patient<br />
was not only having an asymmetrical astigmatism,<br />
it was non-orthogonal. “Post-op the<br />
patient was very happy <strong>and</strong> the topography has<br />
worked very well,” he said in delight.