Neoplasms of the Meninges James G. Smirniotopoulos, MD
Neoplasms of the Meninges James G. Smirniotopoulos, MD
Neoplasms of the Meninges James G. Smirniotopoulos, MD
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>Neoplasms</strong> <strong>of</strong> <strong>the</strong> <strong>Meninges</strong><br />
<strong>James</strong> G. <strong>Smirniotopoulos</strong>, <strong>MD</strong><br />
Pattern Analysis: Location<br />
• Basic Approach<br />
‣ Where is <strong>the</strong> lesion?<br />
<br />
Intraaxial<br />
<br />
Extraaxial<br />
<br />
Intraventricular<br />
‣ Where is <strong>the</strong> lesion ?<br />
<br />
Supratentorial<br />
<br />
Infratentorial<br />
‣ How old is <strong>the</strong> patient ?<br />
<br />
Child<br />
<br />
Adult<br />
‣ What about Sex?<br />
Extra-axial ~ Non-Glial<br />
• Meningioma<br />
‣ Hemangiopericytoma<br />
• Schwannoma<br />
• Pituitary<br />
• Cysts<br />
‣ Epidermoid, Dermoid<br />
‣ Colloid, Craniopharyngioma<br />
‣ Arachnoid<br />
• Chordoma<br />
• Pineal<br />
Educational Objectives<br />
• Meningioma is <strong>the</strong> most common non-glial<br />
primary tumor<br />
• Meningioma is <strong>the</strong> most common<br />
extraaxial neoplasm<br />
• Most meningiomas have “typical imaging”<br />
‣ Hemispheric, homogeneous, broad<br />
based on <strong>the</strong> dura, hyperostosis,<br />
hormonally sensitive<br />
• Some meningiomas have “atypical<br />
imaging”<br />
• Hemangiopericytoma is NOT a<br />
meningioma<br />
Meningioma<br />
• 75% are histologically typical<br />
• 75% are radiologically typical<br />
‣ CT<br />
‣ MR<br />
‣ Angiography<br />
• Atypical Imaging =/= Atypical Histology<br />
• “The atypical appearance <strong>of</strong> a common<br />
lesion may be seen more <strong>of</strong>ten than <strong>the</strong><br />
classic appearance <strong>of</strong> an uncommon<br />
lesion.”<br />
Primary Meningeal <strong>Neoplasms</strong><br />
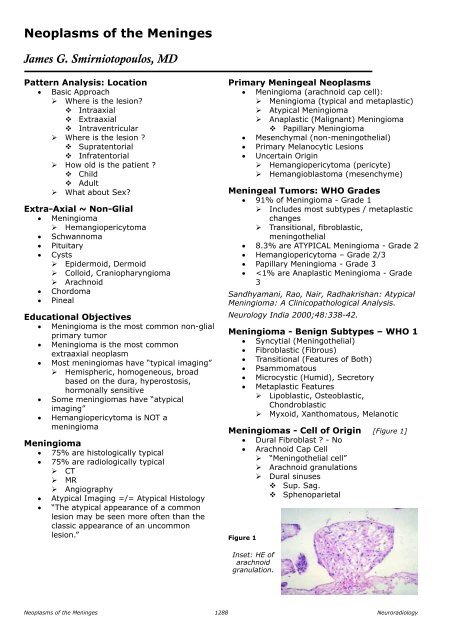
• Meningioma (arachnoid cap cell):<br />
‣ Meningioma (typical and metaplastic)<br />
‣ Atypical Meningioma<br />
‣ Anaplastic (Malignant) Meningioma<br />
<br />
Papillary Meningioma<br />
• Mesenchymal (non-meningo<strong>the</strong>lial)<br />
• Primary Melanocytic Lesions<br />
• Uncertain Origin<br />
‣ Hemangiopericytoma (pericyte)<br />
‣ Hemangioblastoma (mesenchyme)<br />
Meningeal Tumors: WHO Grades<br />
• 91% <strong>of</strong> Meningioma - Grade 1<br />
‣ Includes most subtypes / metaplastic<br />
changes<br />
‣ Transitional, fibroblastic,<br />
meningo<strong>the</strong>lial<br />
• 8.3% are ATYPICAL Meningioma - Grade 2<br />
• Hemangiopericytoma – Grade 2/3<br />
• Papillary Meningioma - Grade 3<br />
•
Meningioma - Etiologic Factors<br />
• Trauma<br />
• Radiation<br />
• Viruses<br />
• Familial (Non-NF2) Meningioma<br />
• Neur<strong>of</strong>ibromatosis – Type - 2<br />
‣ MISME Syndrome<br />
Meningioma - Radiation<br />
• Low Dose (2000 cGray = 2000 RADS)<br />
‣ Used for Skull Base Tumors<br />
‣ Pituitary Adenoma<br />
Meningioma - Molecular Biology<br />
• Postulate Tumor suppressor Gene<br />
• Chromosome 22 – deletion in tumor cells<br />
‣ Both sporadic and inherited<br />
‣ W/ or w/o NF-2<br />
• Homozygous for TWO wild-type copies is<br />
normal<br />
• Heterozygous for 22 develops neoplasm<br />
‣ Because <strong>the</strong>re is a subsequent loss <strong>of</strong><br />
<strong>the</strong> OTHER wild-type gene<br />
• Inherited (germline) deletion <strong>of</strong> 22<br />
‣ W/Schwannoma = NF2<br />
Meningiomas<br />
• 1/7 to 1/4 <strong>of</strong> all Intracranial Primary<br />
‣ ~ 6/ 100k / year<br />
‣ Small ones in ~ 1.4% <strong>of</strong> autopsies<br />
• 1/4 – 1/3 <strong>of</strong> all Intraspinal Tumors<br />
• Middle age (40-60)<br />
• Female > Male<br />
‣ Cranial 2-4:1<br />
‣ Spinal 4-8:1<br />
‣ Progesterone receptors in 2/3<br />
‣ Estrogen receptors less common<br />
Meningioma – Sharp Margin [Figure 2]<br />
• Wonton wrapper<br />
• Tortilla<br />
• Arepa (Colombia)<br />
• Sopapilla (Chile)<br />
• Bolo de milho (Brazil)<br />
• Pita (Greece and Middle East)<br />
• Naan (India)<br />
• Lavaash (Farsi/Iranian)<br />
• Injera (Ethiopia)<br />
Meningioma - CT Imaging<br />
• Non-Contrast<br />
‣ Sharply Circumscribed<br />
‣ Homogeneous<br />
‣ Hyperdense (+/- Ca++)<br />
<br />
NOT from psammoma bodies !<br />
‣ Broad Dural Surface<br />
‣ Bone Changes (Hyperostosis)<br />
• Enhanced CT<br />
‣ Homogeneous Enhancement<br />
Meningioma – Early CT [Figure 3]<br />
Figure 3 A & B<br />
Meningioma – with classic features <strong>of</strong> hyperdensity<br />
and hyperostosis.<br />
Psammomatous Meningioma<br />
[Figure 4]<br />
Figure 2 A & B<br />
Meningioma – parasagittal.<br />
Meningioma - “En plaque”<br />
• En plaque (like a flat bread)<br />
• Pancake<br />
• Crepe<br />
Figure 4 A & B<br />
Spinal masses.<br />
Neuroradiology<br />
1289<br />
<strong>Neoplasms</strong> <strong>of</strong> <strong>the</strong> <strong>Meninges</strong>
Meningioma: Vasogenic Edema<br />
• VASCULAR<br />
‣ Parasitization <strong>of</strong> MCA, etc.<br />
‣ Compression <strong>of</strong> cortical aa./vv.<br />
• COMPRESSIVE TRAUMA<br />
• SECRETORY EFFECT<br />
• “TRANSCORTICAL FLOW”<br />
‣ Close apposition <strong>of</strong> tumor to brain<br />
‣ Thinned cortex<br />
‣ +/- infiltration <strong>of</strong> brain<br />
‣ Fluid gradient from meningioma into<br />
brain<br />
Meningioma and Edema [Figure 5]<br />
Figure 5 A, B & C<br />
Meningioma. WHO Grade 1 – benign, yet with<br />
extensive vasogenic edema.<br />
Meningioma and Edema<br />
Edema and Prognosis<br />
• Edema =/= Histology<br />
• Edema =/= Size<br />
• Edema ~ Pial Vascularity<br />
• Edema IS Related to Resectability<br />
‣ Smaller “pseudocapsule”<br />
‣ Surgical “cleavage plane”<br />
‣ Tumor “sticks” to underlying brain<br />
• Resectability IS Related to Prognosis<br />
• Edema IS INDIRECTLY Related to<br />
Prognosis<br />
Meningiomas: MR Imaging<br />
• “Meningiomas are ISO-intense.”<br />
‣ Usually on T1W<br />
‣ Vary pulse sequence to see<br />
• EXTRA-axial Features<br />
‣ Gray-matter buckling<br />
‣ Pseudo-capsule <strong>of</strong> vessels<br />
‣ Meningeal/dural “TAIL”<br />
• GADOLINIUM ENHANCEMENT<br />
Tentorial Meningioma [Figure 6]<br />
Meningioma: Peri-tumoral Edema<br />
• Male > Female (p = 0.026)<br />
• Hyperintense to GM on T2W (p = 0.016)<br />
• Pial blood supply (p = 0.001)<br />
‣ Statistically significant<br />
• Pathology<br />
‣ Grade 1: 23/79 cases had edema<br />
(32% G1)<br />
‣ Grade 2-3: 7/79 had edema (87% G2-<br />
3)<br />
Lee K, Joo W, Rha H, et al: Peritumoral brain<br />
edema in meningiomas …<br />
Surgical Neurology 2008;69:350-5.<br />
Figure 6 A & B<br />
Gross Courtesy Tom Naidich, Mt. Sinai, NY.<br />
Meningioma – Pre and Post Gd<br />
[Figure 7]<br />
Figure 7 A & B<br />
Frontal Meningioma - notice <strong>the</strong> bone thickening<br />
(hyperostosis) under <strong>the</strong> center <strong>of</strong> <strong>the</strong> lesion.<br />
<strong>Neoplasms</strong> <strong>of</strong> <strong>the</strong> <strong>Meninges</strong> 1290<br />
Neuroradiology
MR Signal and Meningioma Types<br />
• Most are Isointense to GM<br />
‣ On both T1W & T2W<br />
• Hyperintense to GM on T1W<br />
‣ “Lipoblastic” (Fatty) Meningioma<br />
‣ Hemorrhage into Meningioma<br />
• Hypointense on T2W<br />
‣ Fibroblastic<br />
‣ Transitional<br />
• Hyperintense on T2W<br />
‣ Meningo<strong>the</strong>lial<br />
‣ “Angioblastic”<br />
• Microcystic (“Humid”)<br />
Meningioma - Dural Tail [Figure 8]<br />
Dural tail: Histology [Figure 9]<br />
Figure 9<br />
Dural Tail: Differential Diagnosis<br />
• Extraaxial Lesions<br />
‣ Meningioma<br />
<br />
Most common lesion w/dural tail<br />
<br />
Most common lesions overall<br />
‣ Schwannoma<br />
‣ Hemangiopericytoma<br />
‣ Sarcoidosis<br />
‣ Dural Lymphoma and metastases<br />
‣ Gumma (syphilis)<br />
• Intraaxial Lesions<br />
‣ Pleomorphic Xanthoastrocytoma<br />
‣ Superficial cerebral astrocytoma<br />
‣ GBM (rare)<br />
Cavernous Sinus Meningioma<br />
[Figure 10]<br />
Figure 8 A, B, C & D<br />
Meningioma - Dural Tail.<br />
The upper right image shows branching hypointensities<br />
that may represent flow voids from tumor vessels.<br />
Dural Tail<br />
• Curvilinear enhancement<br />
• “Dural flair”<br />
• First reported w/meningioma<br />
• First reported to be neoplastic invasion<br />
• What is it REALLY?<br />
‣ Thickening <strong>of</strong> <strong>the</strong> dura<br />
‣ Vasocongestion <strong>of</strong> <strong>the</strong> dura<br />
‣ Edema <strong>of</strong> <strong>the</strong> dura<br />
Figure 10 A & B<br />
Cavernous Sinus Meningioma with extensive dural<br />
enhancement along <strong>the</strong> tentorium.<br />
Meningioma CT & MR Features<br />
• Mass effect 88% 90%<br />
• Extraaxial Location 42% 70%<br />
• Broad Dural Attach. 74% 98%<br />
• Typical Dense./Intensity 92% 74%<br />
• Hyperostosis 10% 14%<br />
• Homogeneous 76% 76%<br />
• Enhancement 96%(78%) 96%(80%)<br />
(Homogeneous)<br />
• Meningeal. Enhance (tail) 2% 50%<br />
• “Capsule” 14% 68%<br />
Neuroradiology 1990;32:467-73.<br />
Neuroradiology<br />
1291<br />
<strong>Neoplasms</strong> <strong>of</strong> <strong>the</strong> <strong>Meninges</strong>
O<strong>the</strong>r Locations for Meningioma<br />
• Intraventricular<br />
• Orbit<br />
‣ Intraconal<br />
‣ Periorbital<br />
• Nasal Cavity<br />
Intraventricular: ~ 5% [Figure 11]<br />
• Usually Adult<br />
• F > M<br />
• Usually Lateral Ventricle<br />
• Usually Trigone/Atrium<br />
• ALWAYS attached to Choroid Plexus<br />
• Vascular pedicle from choroid<br />
Figure 11<br />
Figure 12 A & B<br />
Meningioma – Supplied by branches <strong>of</strong> <strong>the</strong> ECA,<br />
showing classic spoke-wheel vascularity.<br />
Intraventricular<br />
Meningioma.<br />
Figure 13<br />
Optic Nerve Meningioma<br />
Meningioma Arterial Supply<br />
• External Carotid 85%<br />
• Internal Carotid 63%<br />
• Tumor Blush 95%<br />
Meningioma<br />
– Venous<br />
phase, showing<br />
persistent and<br />
dense tumor<br />
blush.<br />
Delayed Washout [Figure 14]<br />
Meningioma - Angiography – Transit<br />
Time [Figure 12]<br />
• Blush or Stain<br />
‣ Early arterial<br />
‣ Prominent in VENOUS phase<br />
‣ Capillaries/sm. arterioles<br />
‣ (Too small to see individually)<br />
• Venous Filling<br />
‣ Characteristic if delayed<br />
‣ May fill with or before Nl. veins<br />
Meningioma - Angiography – Long<br />
Transit Time [Figure 13]<br />
• Venous Filling (Stattin, 1996)<br />
‣ 170 Meningiomas<br />
‣ Delayed in 136 (80%)<br />
‣ With Nl. vv. In 10 (6%)<br />
‣ Earlier in 24 (14%)<br />
‣ (8 in early arterial phase)<br />
• Leeds & Taveras (1969)<br />
‣ EDV in 6/36 (16%)<br />
Figure 14 A to E<br />
MR Perfusion study, showing delayed washout from<br />
meningioma. Courtesy <strong>of</strong> Dra. Perla Salgado, Mexico<br />
City, Mexico.<br />
<strong>Neoplasms</strong> <strong>of</strong> <strong>the</strong> <strong>Meninges</strong> 1292<br />
Neuroradiology
Meningioma: Effect on Skull<br />
[Figure 15]<br />
• Hyperostosis (15-25%)<br />
‣ With or without micro invasion<br />
• Pressure Erosion<br />
‣ Periosteal remodeling<br />
• Bone Destruction<br />
‣ Microscopic invasion<br />
Meningioma: Mostly Intraosseous<br />
[Figure 17]<br />
Figure 17 A, B & C<br />
57 y.o. woman, long Hx <strong>of</strong> seizures.<br />
Figure 15<br />
Variable patterns <strong>of</strong> hyperostosis from meningioma:<br />
Inner table, inner and outer table, diploic space,<br />
combinations.<br />
Hyperostosis [Figure 16]<br />
Meningioma Hyperostosis<br />
• Does NOT mean invasion <strong>of</strong> bone<br />
• Implies CHRONICITY<br />
‣ And benign behavior<br />
• Skull Base<br />
‣ Invasion via HAVERSIAN CANALS<br />
Meningioma: Atypical Imaging (Yet,<br />
typical Histology)<br />
Meningioma – WHO 1 [Figure 18]<br />
Figure 16 A & B<br />
Hyperostosis from meningioma.<br />
“En plaque” Meningioma<br />
• Meningioma:<br />
‣ Intradural s<strong>of</strong>t-tissue mass<br />
‣ Extradural s<strong>of</strong>t-tissue mass<br />
• Fibrous Dysplasia:<br />
‣ Intra-osseous lesion<br />
‣ No extra-osseous mass<br />
Figure 18 A & B<br />
Meningioma with typical histology – yet aggressive<br />
radiologic appearance.<br />
Neuroradiology<br />
1293<br />
<strong>Neoplasms</strong> <strong>of</strong> <strong>the</strong> <strong>Meninges</strong>
Meningioma Atypical Imaging<br />
• Focal Lucency Outside (arachnoid cyst)<br />
• Focal Lucency Inside (necrosis, cyst)<br />
• Hypodensity (“humid”, lipoblastic)<br />
• Focal Hyperdensity (metaplasia,<br />
hemorrhage)<br />
• Heterogeneous<br />
• Hyperintensity on T1W<br />
• Hyperintensity on T2W<br />
Hemangiopericytoma [Figure 20]<br />
• Syn: “angioblastic meningioma”<br />
• Cell <strong>of</strong> Origin – perivascular pericyte <strong>of</strong><br />
Zahn and/or Zimmerman<br />
• < 1% <strong>of</strong> primary CNS<br />
• M 1.4:1 F<br />
• Age – 40’s<br />
• Dural based, bone destruction, lobulated<br />
Fatty Metaplasia [Figure 19]<br />
Figure 19 A & B<br />
WHO Grade 1 Meningioma with Fatty Metaplasia.<br />
Meningioma with Cysts<br />
• Inside <strong>of</strong> neoplasm<br />
‣ (rim enhancement)<br />
• Between tumor and brain<br />
‣ (”arachnoid cysts”)<br />
• Inside Brain<br />
‣ PIA separates tumor from brain<br />
‣ ?? Results <strong>of</strong> chronic Edema<br />
‣ Vacuolization <strong>of</strong> White Matter<br />
Meningioma: Atypical Histology<br />
• Atypical Meningioma ~ 5-7%<br />
• Anaplastic Meningioma ~ 1-3%<br />
• ~ 0.2% / 100k per year<br />
• Higher incidence <strong>of</strong> Recurrence<br />
• Shorter time to Recurrence<br />
• “Atypical Histology”<br />
‣ Necrosis<br />
‣ Excessive mitoses<br />
‣ Invasion into brain*<br />
“Malignant Meningioma”<br />
• < 3% <strong>of</strong> all Meningioma<br />
• Anaplastic (Malignant) Meningioma<br />
• Papillary Meningioma<br />
• “Benign” Metastasizing Meningioma<br />
• Hemangio-Peri-Cytoma (HPC)<br />
• Malignant Fibrous Histiocytoma MFH)<br />
<strong>Neoplasms</strong> <strong>of</strong> <strong>the</strong> <strong>Meninges</strong> 1294<br />
Figure 20 A, B, C & D<br />
Hemangiopericytoma. WHO 2,3<br />
Top: Lobulated Mass - narrow attachment base.<br />
Hemangiopericytoma (HPC)<br />
• Narrow dural base (“Mushrooming”)<br />
• No Hyperostosis<br />
• No Calcification in tumor<br />
• Lobulated (not hemispheric)<br />
• Internal Signal Voids (on MRI)<br />
‣ Irregular and multiple<br />
Meningioma: Radiologic Features - CT<br />
• Feature Benign/”Malignant”<br />
• Homogeneous Enhance 72% / 36%<br />
• Heterogeneous Enhance 23% / 64%<br />
• Hyperostosis 18% / 7%<br />
• Calcification 27% / 0%<br />
• “Mushrooming” 0% / 57%<br />
‣ Narrow attachment and larger “cap”<br />
‣ Invaginating into brain<br />
Parkway Delight vs. Rueben<br />
• Parkway Delight Rueben<br />
• Pastrami Corned Beef<br />
• Coleslaw Sauerkraut<br />
• Thousand Island Russian<br />
• Muenster Swiss cheese<br />
• Pumpernickel Rye Bread<br />
Neuroradiology
HPC vs. Meningioma<br />
HPC<br />
Meningioma<br />
Narrow base Broad base<br />
Lobulated Hemispheric<br />
Heterogeneous Homogeneous<br />
Bone destruction, Hyperostosis<br />
No Ca++<br />
Psammomatous,<br />
No Ca++<br />
Irregular vessels Spoke Wheel vessels<br />
Meningioma<br />
• The 4H+ Tumor<br />
• Homogeneous<br />
• Hyperdense<br />
• Homogeneous enhancement<br />
• Hemispheric shape<br />
• Hyperostosis<br />
• Hormonally modulated<br />
References<br />
1. Ahmadi J, Hinton DR, Segall HD, Couldwell WT. Surgical implications <strong>of</strong> magnetic resonance-enhanced<br />
dura. Neurosurgery. 1994 Sep;35(3):370-7;discussion 377.<br />
2. Aoki S, Sasaki Y, Machida T, Tanioka H. Contrast-enhanced MR images in patients with meningioma:<br />
importance <strong>of</strong> enhancement <strong>of</strong> <strong>the</strong> dura adjacent to <strong>the</strong> tumor. AJNR Am J Neuroradiol 1990 Sep-<br />
Oct;11(5):935-8.<br />
3. Asari S, Yabuno N, Ohmoto T. Magnetic resonance characteristics <strong>of</strong> meningiomas arising from <strong>the</strong><br />
falcotentorial junction. Comput Med Imaging Graph 1994 May-Jun;18(3):181-5.<br />
4. Berger MS. Perfusion MR and <strong>the</strong> evaluation <strong>of</strong> meningiomas: is it important surgically? AJNR Am J<br />
Neuroradiol 2003;24:1499-500.<br />
5. Goldsher D, Litt AW, Pinto RS, Bannon KR, Kricheff II. Dural “tail” associated with meningiomas on Gd-<br />
DTPA-enhanced MR images: characteristics, differential diagnostic value, and possible implications for<br />
treatment. Radiology 1990 Aug;176(2):447-50.<br />
6. Helie O, Soulie D, Sarrazin JL, Derosier C, Cordoliani YS, Cosnard G. [Magnetic resonance imaging and<br />
meningiomas <strong>of</strong> <strong>the</strong> posterior cerebral fossa. 31 cases] J Neuroradiol 1995 Dec;22(4):252-70. French.<br />
7. Hutzelmann A, Palmie S, Buhl R, Freund M, Heller M. Dural invasion <strong>of</strong> meningiomas adjacent to <strong>the</strong><br />
tumor margin on Gd-DTPA-enhanced MR images: histopathologic correlation. Eur Radiol 1998;8(5):746-<br />
8.<br />
8. Hutzelmann A, Palmie S, Freund M, Buhl R, Heller M. [Dura thickening adjacent to intracranial, para-dural<br />
space-occupying lesions in MRI. Histologic correlation] Aktuelle Radiol 1997 Nov;7(6):305-8. German.<br />
9. Hutzelmann A, Palmie S, Zimmer C, Benz T, Leweke F, Freund M. [The meningeal sign: a new appraisal]<br />
R<strong>of</strong>o 1996 Apr;164(4):314-7. German.<br />
10. Ildan F, Tuna M, Gocer AP, Boyar B, Bagdatoglu H, Sen O, Haciyakupoglu S, Burgut HR. Correlation <strong>of</strong> <strong>the</strong><br />
relationships <strong>of</strong> brain-tumor interfaces, magnetic resonance imaging, and angiographic findings to predict<br />
cleavage <strong>of</strong> meningiomas. J Neurosurg 1999 Sep;91(3):384-90.<br />
11. Kawahara Y, Niiro M, Yokoyama S, Kuratsu J. Dural congestion accompanying meningioma invasion into<br />
vessels: <strong>the</strong> dural tail sign. Neuroradiology 2001 Jun;43(6):462-5.<br />
12. Maiuri F, et al. Intracranial meningiomas: correlations between MR imaging and histology. Eur J Radiol<br />
1999;31:69-75.<br />
13. Nagele T, Petersen D, Klose U, Grodd W, Opitz H, Voigt K. The “dural tail” adjacent to meningiomas<br />
studied by dynamic contrast-enhanced MRI: a comparison with histopathology. Neuroradiology 1994<br />
May;36(4):303-7.<br />
14. Nakasu S, Nakasu Y, Matsumura K, Matsuda M, Handa J. Interface between <strong>the</strong> meningioma and <strong>the</strong> brain<br />
on magnetic resonance imaging. Surg Neurol 1990 Feb;33(2):105-16.<br />
15. Nakau H, Miyazawa T, Tamai S, Tsuchiya K, Shima K, Shirotani T, Chigasaki H. Pathologic significance <strong>of</strong><br />
meningeal enhancement (“flare sign”) <strong>of</strong> meningiomas on MRI. Surg Neurol 1997 Dec;48(6):584-90;<br />
discussion 590-1.<br />
16. Quekel LG, Versteege CW. The “dural tail sign” in MRI <strong>of</strong> spinal meningiomas. J Comput Assist Tomogr.<br />
1995 Nov-Dec;19(6):890-2.<br />
17. Sakai K, Tada T, Fukasaku K, Kyoshima K, Kobayashi S. Histological examination <strong>of</strong> <strong>the</strong> gadoliniumenhanced<br />
dura mater around meningiomas on magnetic resonance imaging. Neurol Med Chir (Tokyo)<br />
1993 Jul;33(7):429-33.<br />
18. Sandhyamani, Rao, Nair, Radhakrishan: Atypical Meningioma: A Clinicopathological Analysis.Neurology<br />
India 2000;48:338-42.<br />
19. Sato M, Matsumoto M, Kodama N. Meningeal enhancement surrounding meningiomas on Gd-DTPA MRI.<br />
Fukushima J Med Sci. 1998 Jun;44(1):1-11.<br />
20. Sekiya T, Manabe H, Iwabuchi T, Narita T. [The dura mater adjacent to <strong>the</strong> attachment <strong>of</strong> meningiomas:<br />
its enhanced MR imaging and histological findings] No Shinkei Geka 1992 Oct;20(10):1063-8. Japanese.<br />
Neuroradiology<br />
1295<br />
<strong>Neoplasms</strong> <strong>of</strong> <strong>the</strong> <strong>Meninges</strong>
21. Takeguchi T, Miki H, Shimizu T, Kikuchi K, Mochizuki T, Ohue S, Ohnishi T. The dural tail <strong>of</strong> intracranial<br />
meningiomas on fluid-attenuated inversion-recovery images. Neuroradiology 2004 Feb;46(2):130-5. Epub<br />
2004 Jan 28.<br />
22. Wilms G, Lammens M, Marchal G, Van Calenbergh F, Plets C, Van Fraeyenhoven L, Baert AL. Thickening <strong>of</strong><br />
dura surrounding meningiomas: MR features. J Comput Assist Tomogr 1989 Sep-Oct;13(5):763-8.<br />
23. Yamaguchi N, Kawase T, Sagoh M, Ohira T, Shiga H, Toya S. Prediction <strong>of</strong> consistency <strong>of</strong> meningiomas<br />
with preoperative magnetic resonance imaging. Surg Neurol 1997 Dec;48(6):579-83.<br />
<strong>Neoplasms</strong> <strong>of</strong> <strong>the</strong> <strong>Meninges</strong> 1296<br />
Neuroradiology