Most Frequent RTP Reason Codes - Palmetto GBA
Most Frequent RTP Reason Codes - Palmetto GBA
Most Frequent RTP Reason Codes - Palmetto GBA
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
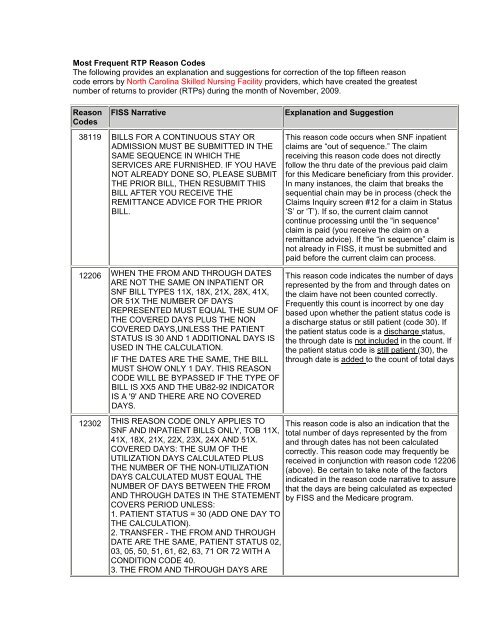
<strong>Most</strong> <strong>Frequent</strong> <strong>RTP</strong> <strong>Reason</strong> <strong>Codes</strong><br />
The following provides an explanation and suggestions for correction of the top fifteen reason<br />
code errors by North Carolina Skilled Nursing Facility providers, which have created the greatest<br />
number of returns to provider (<strong>RTP</strong>s) during the month of November, 2009.<br />
<strong>Reason</strong><br />
<strong>Codes</strong><br />
FISS Narrative<br />
Explanation and Suggestion<br />
38119 BILLS FOR A CONTINUOUS STAY OR<br />
ADMISSION MUST BE SUBMITTED IN THE<br />
SAME SEQUENCE IN WHICH THE<br />
SERVICES ARE FURNISHED. IF YOU HAVE<br />
NOT ALREADY DONE SO, PLEASE SUBMIT<br />
THE PRIOR BILL, THEN RESUBMIT THIS<br />
BILL AFTER YOU RECEIVE THE<br />
REMITTANCE ADVICE FOR THE PRIOR<br />
BILL.<br />
12206 WHEN THE FROM AND THROUGH DATES<br />
ARE NOT THE SAME ON INPATIENT OR<br />
SNF BILL TYPES 11X, 18X, 21X, 28X, 41X,<br />
OR 51X THE NUMBER OF DAYS<br />
REPRESENTED MUST EQUAL THE SUM OF<br />
THE COVERED DAYS PLUS THE NON<br />
COVERED DAYS,UNLESS THE PATIENT<br />
STATUS IS 30 AND 1 ADDITIONAL DAYS IS<br />
USED IN THE CALCULATION.<br />
IF THE DATES ARE THE SAME, THE BILL<br />
MUST SHOW ONLY 1 DAY. THIS REASON<br />
CODE WILL BE BYPASSED IF THE TYPE OF<br />
BILL IS XX5 AND THE UB82-92 INDICATOR<br />
IS A '9' AND THERE ARE NO COVERED<br />
DAYS.<br />
12302 THIS REASON CODE ONLY APPLIES TO<br />
SNF AND INPATIENT BILLS ONLY, TOB 11X,<br />
41X, 18X, 21X, 22X, 23X, 24X AND 51X.<br />
COVERED DAYS: THE SUM OF THE<br />
UTILIZATION DAYS CALCULATED PLUS<br />
THE NUMBER OF THE NON-UTILIZATION<br />
DAYS CALCULATED MUST EQUAL THE<br />
NUMBER OF DAYS BETWEEN THE FROM<br />
AND THROUGH DATES IN THE STATEMENT<br />
COVERS PERIOD UNLESS:<br />
1. PATIENT STATUS = 30 (ADD ONE DAY TO<br />
THE CALCULATION).<br />
2. TRANSFER - THE FROM AND THROUGH<br />
DATE ARE THE SAME, PATIENT STATUS 02,<br />
03, 05, 50, 51, 61, 62, 63, 71 OR 72 WITH A<br />
CONDITION CODE 40.<br />
3. THE FROM AND THROUGH DAYS ARE<br />
This reason code occurs when SNF inpatient<br />
claims are “out of sequence.” The claim<br />
receiving this reason code does not directly<br />
follow the thru date of the previous paid claim<br />
for this Medicare beneficiary from this provider.<br />
In many instances, the claim that breaks the<br />
sequential chain may be in process (check the<br />
Claims Inquiry screen #12 for a claim in Status<br />
‘S’ or ‘T’). If so, the current claim cannot<br />
continue processing until the “in sequence”<br />
claim is paid (you receive the claim on a<br />
remittance advice). If the “in sequence” claim is<br />
not already in FISS, it must be submitted and<br />
paid before the current claim can process.<br />
This reason code indicates the number of days<br />
represented by the from and through dates on<br />
the claim have not been counted correctly.<br />
<strong>Frequent</strong>ly this count is incorrect by one day<br />
based upon whether the patient status code is<br />
a discharge status or still patient (code 30). If<br />
the patient status code is a discharge status,<br />
the through date is not included in the count. If<br />
the patient status code is still patient (30), the<br />
through date is added to the count of total days<br />
This reason code is also an indication that the<br />
total number of days represented by the from<br />
and through dates has not been calculated<br />
correctly. This reason code may frequently be<br />
received in conjunction with reason code 12206<br />
(above). Be certain to take note of the factors<br />
indicated in the reason code narrative to assure<br />
that the days are being calculated as expected<br />
by FISS and the Medicare program.
<strong>Reason</strong><br />
<strong>Codes</strong><br />
FISS Narrative<br />
THE SAME BUT NO CONDITION CODE 40<br />
PRESENT.<br />
38117 THE TOB IS EQUAL TO AN SNF, OR THE<br />
CLAIM IS FOR A NON-PPS INPATIENT, OR<br />
AN IPF PPS. THE ADMISSION DATE IS ON<br />
OR AFTER 040195, AND THE STATEMENT<br />
COVERS FROM DATE IS GREATER THAN<br />
THE ADMISSION DATE. THERE IS A PRIOR<br />
CLAIM PENDING, AND THE PRIOR CLAIM'S<br />
THRU DATE IS 1 DAY LESS THAN THIS<br />
CLAIM'S FROM DATE, AND THE REASON<br />
CODE AUTHORIZATION FIELD (CLAIM<br />
PAGE 9) DOES NOT CONTAIN THIS<br />
REASON CODE.<br />
Explanation and Suggestion<br />
The admission date in FL 17 is prior to the<br />
statement from date of this claim. **OR** The<br />
prior claim in the series shows a thru date that<br />
is one day less than<br />
31486 THE CLAIM IS AN SNF CLAIM WITH A<br />
STATEMENT COVERS FROM DATE OF<br />
7/1/98 OR GREATER AND THE SUM OF ALL<br />
REVENUE CODES 0022 DOES NOT EQUAL<br />
THE CLAIM COVERED DAYS COUNT.<br />
15202 FOR 11X, 18X, OR 21X BILLS, THE<br />
COVERED DAYS (FLD 7) MUST<br />
EQUAL THE ACCOMMODATION UNITS (FLD<br />
46) FOR REVENUE CODES<br />
10X - 21X. PLEASE MAKE CORRECTIONS<br />
AND RESUBMIT/REKEY.<br />
HARDCOPY SUBMITTORS RESUBMIT <strong>RTP</strong><br />
REPORT WITH CORRECTIONS.<br />
W7K01 STANDARD NARRATIVE: THE OPPS<br />
VERSION OF OCE HAS DETECTED<br />
AN ERROR IN THE ADMITTING DIAGNOSIS.<br />
This reason code can indicate that the units<br />
field billed on the revenue line for the HIPPS<br />
code (revenue code 0022) does not match the<br />
number of covered days shown on page 1 of<br />
the claim in FISS. However, for most of the<br />
claims receiving this reason code the problem<br />
is that a non-covered claim is being billed, but<br />
the provider is showing covered units (field<br />
name = COV UNIT) for revenue code 0022. If<br />
the claim is a totally non-covered claim, please<br />
remove all covered units.<br />
Provider should be certain that the units<br />
(including covered units on page 2 of claim in<br />
FISS) billed with accommodation revenue<br />
codes (10X-21X) equal the number of covered<br />
days (page 1) billed on the claim. If all of the<br />
days and the units appear to be correct but this<br />
reason code is still returned, contact the<br />
Provider Contact Center (PCC) for assistance.<br />
This reason code indicates that the admitting<br />
diagnosis code (the code in the ADMITTING<br />
DIAGNOSIS field on claim page 03) for the<br />
date of service billed does not match a valid<br />
code in the OPPS version of the Outpatient<br />
Code Editor (OCE). Check this code against<br />
the FISS ICD-9-CM code file (Menu Option<br />
#15) and correct it accordingly<br />
11801 IF THE TYPE OF BILL IS EQUAL TO 11X, OR<br />
41X IF THE ADMISSION TYPE IS EQUAL TO<br />
1, 2, 3, OR 9, THEN THE ADMISSION<br />
SOURCE MUST BE EQUAL TO 1 THRU 9;<br />
OR<br />
IF THE ADMISSION TYPE IS EQUAL TO 4,<br />
Generally the receipt of this reason code<br />
means that the admission source code was not<br />
included on this claim. Please add the<br />
appropriate admission source code to allow the<br />
claim to continue processing. If the admission<br />
source code is present on the claim, please
<strong>Reason</strong><br />
<strong>Codes</strong><br />
FISS Narrative<br />
THEN THE ADMISSION SOURCE MUST BE<br />
EQUAL TO 1, 2, 3, OR 4;<br />
OR<br />
IF THE TYPE OF BILL IS EQUAL TO 13X,<br />
14X, 83X, OR 85X, AND THE DATE OF<br />
SERVICE IS GREATER THAN 02/28/91,<br />
THEN THE ADMISSION SOURCE MUST BE<br />
EQUAL TO 1 THRU 8;<br />
OR<br />
IF THE TYPE OF BILL IS EQUAL TO 18X,<br />
21X, 28X, OR 51X, THEN THE ADMISSION<br />
SOURCE MUST BE A SPACE OR EQUAL TO<br />
AN 'A' OR 1 THRU 9.<br />
OR<br />
IF THE TYPE OF BILL IS EQUAL TO 3X2 OR<br />
3X9, AND THE DATE OF SERVICE IS<br />
10/01/00 OR GREATER THEN THE<br />
ADMISSION SOURCE MUST BE 1 THRU 9,<br />
A, B, OR C.<br />
OR<br />
IF THE DATE OF SERVICE IS EQUAL TO OR<br />
GREATER THAN 1/1/08 THE ADMISSION<br />
SOURCE CODE OF 'A' OR '3' IS NO LONGER<br />
VALID.<br />
32404 ACCORDING TO THE REVENUE CODE FILE<br />
A HCPC IS REQUIRED. HOWEVER, THE<br />
HCPC THAT WAS ENTERED ON THE CLAIM<br />
WAS NOT FOUND ON THE HCPC FILE<br />
CORRECTIONS WITH REPORT.<br />
32200 WHEN DIAGNOSIS CODE 'V048' OR 'V0382'<br />
IS PRESENT ON A CLAIM, A CONDITION<br />
CODE 'A6' IS REQUIRED FOR THE<br />
FOLLOWING BILL TYPES:<br />
12X, 13X, 14X, 22X, 23X, 24X, 34X, 72X, 74X,<br />
75X, 85X.<br />
Explanation and Suggestion<br />
review the conditions listed in the reason code<br />
narrative to determine if the code is correct<br />
according to the other factors/data elements<br />
included on the claim, and change the code<br />
accordingly.<br />
Please refer to the most current CPT-4 HCPCS<br />
coding book to verify that the HCPCS being<br />
billed is valid for the dates of service on the<br />
claim. Make any necessary corrections and<br />
resubmit. Hardcopy submittors resubmit.<br />
Diagnosis codes ‘V048’ and ‘V0382’ are used<br />
to indicate that the patient involved is in need of<br />
a vaccination (influenza and pneumonia,<br />
respectively). Medicare billing guidelines<br />
require that the special program indicator,<br />
condition code ‘A6’, be included on all claims<br />
billing for these services. Therefore, this reason<br />
code is generated whenever these diagnosis<br />
codes are present and condition code ‘A6’ is<br />
not. Add condition code ‘A6’ and the claim<br />
should proceed to payment, or the diagnosis<br />
codes should be removed if the vaccinations<br />
were not provided.<br />
32415 CONDITION CODE A6 IS REQUIRED WHEN<br />
ONE OR MORE OF THE FOLLOWING<br />
HCPCS ARE PRESENT ON THE CLAIM:<br />
HCPC Q0124 WITH FROM DATE LESS THAN<br />
010195 OR 90657, 90658, 90659, 90669,<br />
90724, 90732, G0008 OR G0009.<br />
This reason code occurs because the provider<br />
has not included condition code ‘A6’ (special<br />
program indicator for vaccine billing –<br />
deductible and coinsurance do not apply) on<br />
the claim but there is a pneumonia vaccine or<br />
influenza vaccine being billed. Either the<br />
‘A6’should be added, or the listed HCPCS/CPT<br />
codes should be removed from the claim.
<strong>Reason</strong><br />
<strong>Codes</strong><br />
FISS Narrative<br />
Explanation and Suggestion<br />
153#1 TOTAL CHARGES: THE TOTAL CHARGES<br />
ON REVENUE CODE 001 MUST BE EQUAL<br />
TO THE SUM OF ALL THE CHARGES<br />
ABOVE IT.<br />
30949 TYPE OF BILL EQUALS XX7 OR XX8 BUT<br />
NO CONDITION CODE IS PRESENT ON THE<br />
BILL. PLEASE INCLUDE THE APPROPRIATE<br />
CONDITION CODE OF<br />
D0 - CHANGES TO SERVICE DATES<br />
D1 - CHANGES IN CHARGES<br />
D2 - CHANGES IN REVENUE CODE/HCPC<br />
D3 - SECOND OR SUBSEQUENT INTERIM<br />
PPS BILL<br />
D4 - CHANGE IN GROUPER INPUT (DRG)<br />
D5 - CANCEL ONLY TO CORRECT A HIC OR<br />
PROVIDER NUMBER<br />
D6 - CANCEL ONLY - DUPLICATE<br />
PAYMENT, OUTPATIENT TO INPATIENT<br />
OVERLAP, OIG OVERPAYMENT<br />
D7 - CHANGE TO MAKE MEDICARE<br />
SECONDARY PAYER<br />
D8 - CHANGE TO MAKE MEDICARE<br />
PRIMARY PAYER<br />
D9 - ANY OTHER CHANGES.<br />
PLEASE MAKE CORRECTIONS AND<br />
RESUBMIT/REKEY.<br />
13314 FOR OCCURRENCE SPAN CODE<br />
70(QUALIFYING STAY DATE) THE "FROM"<br />
DATE IS GREATER THAN THE "THROUGH"<br />
DATE. *VERIFY THE QUALIFYING STAY<br />
THRU DATE (REPORTED WITH<br />
OCCURRENCE CODE 70) IS GREATER<br />
THAN THE ADMISSION DATE OF THE<br />
CLAIM.<br />
OR<br />
THIS IS A SNF, AND THE OCCURRENCE<br />
SPAN CODE 80 (PRIOR SAME-SNF STAY)<br />
FROM DATE IS GREATER THAN THE CLAIM<br />
ADMISSION FROM DATE.<br />
31094 TOTAL COVERED CHARGES CANNOT BE<br />
GREATER THAN ZERO IF THE THIRD<br />
POSITION OF THE TYPE OF BILL (TOB)<br />
EQUALS ZERO. PLEASE VERIFY THE TYPE<br />
This reason code indicates that the Total<br />
Charges revenue line (0001) contains a charge<br />
that is not the sum total of the line items on this<br />
claim. This may be an indication that some line<br />
item changes were made but the Total Charge<br />
line was not “deleted” and re-entered with the<br />
corrected total charge amount. If the Total<br />
Charge line item is not “corrected” in the same<br />
manner as all other line items, this reason code<br />
is likely to occur.<br />
In this instance, the provider is submitting an<br />
adjustment (type of bill = xx7) or a paid claim<br />
cancellation (xx8), but they have failed to<br />
include the claim change condition code (FL<br />
24-30) that explains the adjustment or<br />
cancellation. Please add one of the condition<br />
codes listed in the reason code narrative to<br />
your claim.<br />
On most of the claims receiving this reason<br />
code the Admission Date billed on the claim is<br />
BEFORE the qualifying stay date (occurrence<br />
code 70) which is incorrect. It appears that an<br />
”old” (prior) admit date is being used rather<br />
than the admit date that relates to the from and<br />
through dates on the current claim. Please<br />
review the admit date, the qualifying stay date<br />
and the from and through date on the claim to<br />
assure that the appropriate, current dates are<br />
being used and that they are in the proper<br />
sequence.<br />
This reason code is received because the claim<br />
is billed with a zero (0) in the third position of<br />
the type of bill (TOB) indicating a no pay and/or<br />
non-covered claim, but the charges on the
<strong>Reason</strong><br />
<strong>Codes</strong><br />
FISS Narrative<br />
OF BILL AND/OR THE TOTAL COVERED<br />
CHARGES REPORTED. PLEASE CORRECT<br />
AND RESUBMIT/REKEY. HARDCOPY<br />
SUBMITTORS RESUBMIT <strong>RTP</strong> REPORT<br />
WITH CORRECTIONS.<br />
Explanation and Suggestion<br />
claim are listed as covered charges. In some<br />
cases the type of bill may be reported<br />
incorrectly. If this is the case please update the<br />
type of bill (TOB). If this is in fact a no pay<br />
and/or non-covered claim, the charges must be<br />
moved to the non-covered column.<br />
If you encounter some other reason code that you are unable to decipher, please submit it to us<br />
using the “I Have a Question” form included in the Medicare Advisory.