Full text - JICS - The Intensive Care Society
Full text - JICS - The Intensive Care Society
Full text - JICS - The Intensive Care Society
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
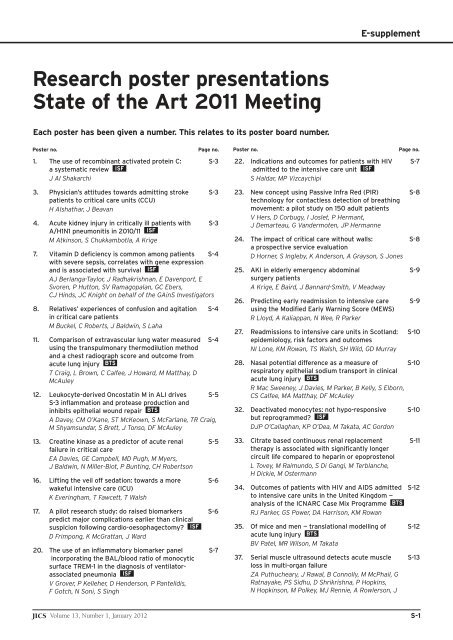
E-supplement<br />
Research poster presentations<br />
State of the Art 2011 Meeting<br />
Each poster has been given a number. This relates to its poster board number.<br />
Poster no. Page no. Poster no. Page no.<br />
1. <strong>The</strong> use of recombinant activated protein C: S-3<br />
a systematic review ISF<br />
J Al Shakarchi<br />
3. Physician’s attitudes towards admitting stroke S-3<br />
patients to critical care units (CCU)<br />
H Alshathar, J Beavan<br />
4. Acute kidney injury in critically ill patients with S-3<br />
A/H1N1 pneumonitis in 2010/11 ISF<br />
M Atkinson, S Chukkambotla, A Krige<br />
7. Vitamin D deficiency is common among patients S-4<br />
with severe sepsis, correlates with gene expression<br />
and is associated with survival ISF<br />
AJ Berlanga-Taylor, J Radhakrishnan, E Davenport, E<br />
Svoren, P Hutton, SV Ramagopalan, GC Ebers,<br />
CJ Hinds, JC Knight on behalf of the GAinS Investigators<br />
8. Relatives’ experiences of confusion and agitation S-4<br />
in critical care patients<br />
M Buckel, C Roberts, J Baldwin, S Laha<br />
11. Comparison of extravascular lung water measured S-4<br />
using the transpulmonary thermodilution method<br />
and a chest radiograph score and outcome from<br />
acute lung injury BTS<br />
T Craig, L Brown, C Calfee, J Howard, M Matthay, D<br />
McAuley<br />
12. Leukocyte-derived Oncostatin M in ALI drives S-5<br />
S-3 inflammation and protease production and<br />
inhibits epithelial wound repair BTS<br />
A Davey, CM O’Kane, ST McKeown, S McFarlane, TR Craig,<br />
M Shyamsundar, S Brett, J Tonso, DF McAuley<br />
13. Creatine kinase as a predictor of acute renal S-5<br />
failure in critical care<br />
EA Davies, GE Campbell, MD Pugh, M Myers,<br />
J Baldwin, N Miller-Biot, P Bunting, CH Robertson<br />
16. Lifting the veil off sedation: towards a more S-6<br />
wakeful intensive care (ICU)<br />
K Everingham, T Fawcett, T Walsh<br />
17. A pilot research study: do raised biomarkers S-6<br />
predict major complications earlier than clinical<br />
suspicion following cardio-oesophagectomy ISF<br />
D Frimpong, K McGrattan, J Ward<br />
20. <strong>The</strong> use of an inflammatory biomarker panel S-7<br />
incorporating the BAL/blood ratio of monocytic<br />
surface TREM-1 in the diagnosis of ventilatorassociated<br />
pneumonia ISF<br />
V Grover, P Kelleher, D Henderson, P Pantelidis,<br />
F Gotch, N Soni, S Singh<br />
22. Indications and outcomes for patients with HIV S-7<br />
admitted to the intensive care unit ISF<br />
S Haldar, MP Vizcaychipi<br />
23. New concept using Passive Infra Red (PIR) S-8<br />
technology for contactless detection of breathing<br />
movement: a pilot study on 150 adult patients<br />
V Hers, D Corbugy, I Joslet, P Hermant,<br />
J Demarteau, G Vandermoten, JP Hermanne<br />
24. <strong>The</strong> impact of critical care without walls: S-8<br />
a prospective service evaluation<br />
D Horner, S Ingleby, K Anderson, A Grayson, S Jones<br />
25. AKI in elderly emergency abdominal S-9<br />
surgery patients<br />
A Krige, E Baird, J Bannard-Smith, V Meadway<br />
26. Predicting early readmission to intensive care S-9<br />
using the Modified Early Warning Score (MEWS)<br />
R Lloyd, A Kaliappan, N Wee, R Parker<br />
27. Readmissions to intensive care units in Scotland: S-10<br />
epidemiology, risk factors and outcomes<br />
NI Lone, KM Rowan, TS Walsh, SH Wild, GD Murray<br />
28. Nasal potential difference as a measure of S-10<br />
respiratory epithelial sodium transport in clinical<br />
acute lung injury BTS<br />
R Mac Sweeney, J Davies, M Parker, B Kelly, S Elborn,<br />
CS Calfee, MA Matthay, DF McAuley<br />
32. Deactivated monocytes: not hypo-responsive S-10<br />
but reprogrammed ISF<br />
DJP O’Callaghan, KP O’Dea, M Takata, AC Gordon<br />
33. Citrate based continuous renal replacement S-11<br />
therapy is associated with significantly longer<br />
circuit life compared to heparin or epoprostenol<br />
L Tovey, M Raimundo, S Di Gangi, M Terblanche,<br />
H Dickie, M Ostermann<br />
34. Outcomes of patients with HIV and AIDS admitted S-12<br />
to intensive care units in the United Kingdom —<br />
analysis of the ICNARC Case Mix Programme BTS<br />
RJ Parker, GS Power, DA Harrison, KM Rowan<br />
35. Of mice and men — translational modelling of S-12<br />
acute lung injury BTS<br />
BV Patel, MR Wilson, M Takata<br />
37. Serial muscle ultrasound detects acute muscle S-13<br />
loss in multi-organ failure<br />
ZA Puthucheary, J Rawal, B Connolly, M McPhail, G<br />
Ratnayake, PS Sidhu, D Shrikrishna, P Hopkins,<br />
N Hopkinson, M Polkey, MJ Rennie, A Rowlerson, J<br />
<strong>JICS</strong> Volume 13, Number 1, January 2012 S-1
Research poster presentations<br />
Poster no. Page no. Poster no. Page no.<br />
Moxham, S Harridge, N Hart, H Montgomery<br />
38. Patterns of gene expression associate with risk S-13<br />
of death in patients with severe sepsis due to<br />
community-acquired pneumonia ISF<br />
J Radhakrishnan, E Svoren, P Ellis, C Langford,<br />
P Hutton, C Garrard, CJ Hinds, JC Knight, on behalf<br />
of the GAinS Investigators<br />
42. Gender differences in inflammation in a model S-14<br />
of acute lung injury induced by inhaled<br />
lipopolysaccharide in healthy volunteers BTS<br />
E O’Brien, M Shyamsundar, CM O’Kane, DF McAuley<br />
43. Capillary lactate in critical care ISF<br />
S-14<br />
D Soo, J Baldwin, N Miller-Biot, E Shardlow,<br />
E Davies, P Bunting, S Laha<br />
44. Does the prophylactic use of Octenisan skin S-14<br />
washes reduce the incidence of bacteraemias<br />
and MRSA acquisition in critical care ISF<br />
C Spencer, D Orr, S Hallam, E Tillmans<br />
45. Regionalisation of ICU and ECMO services in S-15<br />
the UK; beliefs about the evidence, benefits<br />
and harm — a national survey<br />
N Stewart, K Gunning, BH Cuthbertson<br />
46. Protocols for the prevention of contrast-induced S-15<br />
nephropathy: a 2011 survey of intensive care units<br />
in the United Kingdom<br />
Strachan JM, Crilley T, Parvizi S, DeVile MPJ<br />
47. Decreased levels in elafin due to proteolytic S-16<br />
cleavage may contribute to alveolar inflammation<br />
in the pulmonary compartment in patients with<br />
ALI BTS<br />
This poster will now be displayed on Wednesday<br />
A Kerrin, C O’Kane, M Shyamsundar, T Craig,<br />
DF McAuley, CC Taggart<br />
48. An audit of infection characteristics in patients S-16<br />
with acute liver failure secondary to paracetamol<br />
overdose ISF<br />
E <strong>The</strong>ocharidou, B Agarwal, AK Burroughs, A Walecka<br />
50. Airflow distribution with manual hyperinflation S-16<br />
as assessed through gamma camera imaging BTS<br />
H Van Aswegen, A Van Aswegen, H Du Raan,<br />
R Du Toit, M Spruyt, R Nel, MED Maleka<br />
53. Outcomes and APACHE II scores for patients S-17<br />
with alcoholic liver disease and ICU admission; a<br />
retrospective observational cohort study<br />
J Welbourne, K Gunning<br />
55. Deep vein thrombosis (DVT) in critically ill patients S-17<br />
R Moroi, M Takeda, T Harada, M Namiki, A Yaguchi<br />
56. Airway device and quality of cardiopulmonary S-17<br />
resuscitation<br />
J Yeung, G Perkins, F Gao<br />
57. Professional background of team leader and S-18<br />
quality of CPR<br />
J Yeung, G Perkins, F Gao<br />
58. Feedback and prompt devices and quality of S-19<br />
chest compressions<br />
J Yeung, G Perkins, F Gao<br />
Key:<br />
ISF<br />
BTS<br />
— Abstracts relating to the International Sepsis Forum<br />
— Abstracts relating to the British Thoracic <strong>Society</strong><br />
S-2<br />
Volume 13, Number 1, January 2012 <strong>JICS</strong>
Research poster presentations<br />
1. <strong>The</strong> use of recombinant activated protein C:<br />
a systematic review<br />
J Al Shakarchi<br />
Good Hope Hospital, Birmingham, UK<br />
Although recombinant activated protein C has been used in numerous<br />
intensive care units, its use in septic patients remain controversial. We<br />
aimed to evaluate whether recombinant activated protein C is effective in<br />
the treatment of sepsis in adult patients.<br />
We searched Medline, Embase and DOAJ for randomised control trials<br />
comparing the additional use of recombinant activated protein C against<br />
placebo in the treatment of sepsis in adult patients. Strict inclusion criteria<br />
and thorough appraisal of the reviews was required to ensure comparability<br />
of the included papers.<br />
Our dataset comprised of individual data on 4,633 patients from four<br />
randomised controlled trials that compared the additional use of<br />
recombinant activated protein C in the treatment of sepsis in adult<br />
patients. Only one of the papers showed statistically significant<br />
improvement in survival with the use of recombinant activated protein C.<br />
<strong>The</strong> other three studies did not show statistically significant results.<br />
However the point estimate favoured its use in only one of the three<br />
remaining studies.<br />
From the data we have gathered it may be reasonable to conclude that<br />
the current evidence does not support the use of recombinant activated<br />
protein C in addition to standard therapy in adult patients with sepsis.<br />
<strong>The</strong>refore until there is more evidence for its use, intensive care units<br />
should refrain from using this therapy.<br />
3. Physician’s attitudes towards admitting stroke<br />
patients to critical care units (CCU)<br />
H Alshathar*, J Beavan †<br />
*Tunbridge Wells Hospital, Kent, UK. † Royal Derby Hospital, Derby, UK<br />
Patients with stroke in the UK are rarely admitted to critical care units.<br />
Acute stroke treatment has changed with thrombolysis and more medical,<br />
neurovascular and neurosurgical interventions. <strong>The</strong>se recent changes may<br />
have led to acute stroke patients accessing more critical care beds. We<br />
explored physician’s attitudes to such access.<br />
A web-based questionnaire survey of intensivists, anaesthetists with<br />
critical care sessions, stroke physicians, neuorologists and geriatricians<br />
through email and specialty websites of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>, British<br />
Association of Stroke Physicians and British Geriatrics <strong>Society</strong>.<br />
Respondents were asked to rate four stroke cases (differences in age,<br />
comorbidity and aetiology/potential intervention of stroke) for the<br />
likelihood of considering ICU admission as well as requesting comments.<br />
Two hundred and ten physicians in the UK took part in the survey;<br />
(122/210 (58%) intensivists/anaesthetists with critical care sessions,<br />
60/210(29%) stroke physicians, 16/210 (8%) neurologists and 12/2010<br />
(6%) geriatricians). <strong>The</strong> majority (132/208 (64%)) were consultants;<br />
101/207 (49%) worked in district general hospitals, 69/207 (33%) in<br />
teaching hospitals with or without 37/207 (18%) neurosurgical services.<br />
Most (170/206 (83%)) had admitted patients with acute stroke to a<br />
ICU. Overall 160/208 (77%) had been involved with thrombolysis for<br />
acute stroke, but 55% of anaesthetists. Most had experience of post<br />
thrombolysis monitoring in a stroke unit hyperacute bay (116/169<br />
(68.5%)).<br />
Case one described neurological deterioration in a young person with a<br />
large stroke where the outcome is uncertain, but may be good if support is<br />
provided. Stroke physicians (86%) and neurologists (86%) were more<br />
likely to admit/consider ICU admission than intensivists (60%),<br />
anaesthetists (62%), and geriatricians (66%).<br />
Case two described a situation suspicious of basilar artery thrombosis<br />
requiring urgent medical and neurovascular intervention with poor<br />
prognosis without intervention. Neurologists (88%) and stroke physicians<br />
(85%) were much more likely to consider support, than intensivists (33%)<br />
or anaesthetists (52%). <strong>The</strong>re was no difference in respondents working in<br />
neurosurgical centres.<br />
Case three had been recovering well from his stroke and had developed<br />
a potentially reversible condition (pneumonia). Intensivists (62%) and<br />
anaesthetists (54%) were more likely to consider admission than stroke<br />
physicians (41%), neurologists (38%) and geriatricians (33%).<br />
<strong>The</strong> fourth case had dementia and large intracranial haemorrhage with<br />
poor prognostic features. <strong>The</strong> majority of physicians (96.55%) agreed<br />
against admission to ICU.<br />
A third of respondents provided us with comments. <strong>The</strong>mes raised<br />
included difficulty in predicting prognosis, communication, the decision<br />
being in the hands of neurosurgeons, rationing/capacity of ICU beds,<br />
differing referral patterns depending on the status/geography of the stroke<br />
service.<br />
Our survey showed that many physicians involved in stroke and critical<br />
care are considering critical care support to stroke patients, but decisions<br />
are affected by service as well as patient factors. Critical care teams need to<br />
be guided by evidence based advice from stroke teams on patient selection<br />
for ICU and should be included in planning of stroke services.<br />
4. Acute kidney injury in critically ill patients with<br />
A/H1N1 pneumonitis in 2010/11<br />
M Atkinson*, S Chukkambotla † , A Krige †<br />
*North Western Deanery, Manchester, UK. † Royal Blackburn Hospital,<br />
Blackburn, UK<br />
A/H1N1 infection is a major seasonal cause of illness requiring critical care<br />
admission. A high proportion of A/H1N1 positive patients develop acute<br />
kidney injury (AKI). 1 Following the model of a single season, multicentre<br />
observational study, 1 we retrospectively examined all A/H1N1 positive<br />
admissions to a district general hospital (DGH) critical care unit for three<br />
months starting December 2010 for incidence of AKI using the creatinine<br />
score from the risk, injury, failure, loss of function and end-stage (RIFLE)<br />
criteria and its associations with mortality, incidence and duration of<br />
intermittent positive pressure ventilation (IPPV), duration of critical care<br />
admission and provision of renal replacement therapy (RRT).<br />
Twenty-seven patients were admitted to the critical unit who tested<br />
positive for A/H1N1. Fourteen (52%) met RIFLE criteria for AKI. Of these,<br />
three (11%) met the RIFLE criterion for risk (>150% change in creatinine),<br />
three (11%) met the criterion for injury (>200% change in creatinine), and<br />
eight (30%) met the criterion for failure (>300% change in creatinine).<br />
Nine (33% of all patients, 64% of AKI patients) received RRT. Critical care<br />
mortality was three out of 14 (21%) in patients with AKI and one out of 13<br />
(8%) in patients without AKI. This difference was not statistically<br />
significant. Thirteen out of 20 (65%) ventilated patients developed AKI,<br />
compared with one out of seven (14%) non-ventilated patients. This<br />
difference was statistically significant (p=0.0329). Excluding fatalities, the<br />
duration of IPPV was longer in patients with AKI (median 11 days, range<br />
0-54 days) than in patients without AKI (median one day, range 0-20<br />
days). This difference was statistically significant (p
Research poster presentations<br />
balances in patients with acute lung injuries, as our study examined<br />
patients a year later than Petillä.<br />
Reference<br />
1. Pettilä V, Webb SAR, Bailey M et al. Acute kidney injury in patients with influenza A<br />
(H1N1) 2009. <strong>Intensive</strong> <strong>Care</strong> Med 2011;37:763-67.<br />
7. Vitamin D deficiency is common among patients<br />
with severe sepsis, correlates with gene<br />
expression and is associated with survival<br />
AJ Berlanga-Taylor*, J Radhakrishnan*, E Davenport*, E Svoren † ,<br />
P Hutton † , SV Ramagopalan § , GC Ebers § , CJ Hinds † , JC Knight* on behalf<br />
of the GAinS Investigators<br />
*Wellcome Trust Centre for Human Genetics, University of Oxford,<br />
Oxford, UK. † Queen Mary University of London, Barts and <strong>The</strong> London<br />
School of Medicine and Dentistry, William Harvey Research Institute, UK.<br />
‡<br />
John Radcliffe Hospital, Oxford, UK. § University of Oxford, Oxford, UK.<br />
Deficiency of vitamin D is common and has been linked to many diseases<br />
at the epidemiological and molecular levels. 1-2 Vitamin D levels are often<br />
low in hospitalised patients and deficiency of this vitamin is particularly<br />
severe among intensive care unit patients. 3-4 We hypothesized that vitamin<br />
D deficiency might be a contributing factor to all cause mortality in<br />
patients with severe sepsis. Genome wide gene expression was used to<br />
identify functional correlates of vitamin D deficiency.<br />
Clinical data, serum and leukocyte RNA was collected from 144<br />
patients with severe sepsis due to community acquired pneumonia (n=78)<br />
or faecal peritonitis (n=66) admitted to intensive care and recruited to the<br />
Genomic Advances in Sepsis (GAinS) study. Using the first available<br />
sample on admission to intensive care, the hydroxylated form of vitamin D<br />
(25(OH)D 3<br />
) was measured with liquid chromatography mass spectrometry,<br />
peripheral blood leukocytes were isolated at the bedside using the<br />
LeukoLock filter system (Ambion) and RNA hybridisation was carried out<br />
on Illumina Human WG6 V3 arrays. We performed uni- and multi-variate<br />
analysis of the distribution of 25(OH)D 3<br />
according to survival and<br />
correlated serum 25(OH)D 3<br />
levels to whole genome transcriptome<br />
measurements.<br />
Patients had a median age of 64 years, 51% male, 93% Caucasian and<br />
an overall mortality rate at hospital discharge of 24%. Analysis of serum<br />
levels of 25(OH)D 3<br />
showed that 97% of patients were deficient<br />
(
Research poster presentations<br />
using the chest radiograph and the transpulmonary thermodilution<br />
method predict mortality in patients with ALI/ARDS.<br />
A retrospective longitudinal study of 59 ALI patients was performed.<br />
Clinical data were collected within 48 hours of ALI diagnosis and once<br />
daily up to 14 consecutive days. A panel of two clinicians systematically<br />
scored each chest radiograph for the degree of alveolar oedema. <strong>The</strong> single<br />
indicator transpulmonary thermodilution technique (PiCCO Pulsion<br />
Medical Systems, Munich, Germany) was also used to measured EVLW<br />
which was indexed to predicted body weight.<br />
<strong>The</strong> chest radiograph score had only a modest, positive correlation with<br />
the EVLWI measurements (r=0.35, p
Research poster presentations<br />
population. Early diagnosis and intervention may prevent ARF, reducing<br />
morbidity and mortality. Previous retrospective studies have only used<br />
confirmed cases of rhabdomyolysis with clinically significant<br />
concentrations of CK. 3<br />
This prospective observational pilot study collected data from patients<br />
aged ≥18 years with arterial or central venous pressure lines in situ. Total<br />
serum CK was analysed on admission and every two days using Trust<br />
reference ranges for males (38-173 U/L) and females (26-140 U/L).<br />
Corresponding creatinine and ARF were recorded. Data was analysed with<br />
2-tailed t-tests.<br />
Twenty-four patients were recruited (thirteen [54.2%] males, 20<br />
[83.3%] postoperative, age 57 [49-65], BMI 26.8 [24.0-30.0], APACHE II<br />
12.7 [9.5-15.0], length of stay 2.2 [1.2-4.3] days, CK 144.1 [± 95.0] U/L).<br />
<strong>The</strong>re was a high incidence (37.5%) of elevated CK on admission to the<br />
unit. Two (8.3%) participants developed ARF during their admission.<br />
<strong>The</strong>re was no significant difference between groups with and without ARF.<br />
However, the sample did not allow an adequate range of CK values to<br />
determine true significance. Serial data in one participant with ARF<br />
showed an apparent relationship between CK and creatinine (Figure 1).<br />
Figure 1. Example of serial CK (dashed line) and creatinine (solid line) in<br />
patient with ARF.<br />
Further work is indicated with a larger sample and the collection of<br />
additional data such as mortality. More serial data will be helpful in<br />
determining the predictive value of CK in acute renal failure.<br />
Acknowledgements: This project was funded by Lancashire Teaching<br />
Hospitals NHS Foundation Trust.<br />
References<br />
1. Reha WC, Mangano FA, Zehman RK, Pahira JJ. Rhabdomyolysis: Need for high index<br />
of suspicion. Urology 1989;35:292-96.<br />
2. Huerta-Alardin AL, Varon J, Marik PE. Bench-to-bedside review: Rhabdomyolysis – an<br />
overview for clinicians. Crit <strong>Care</strong> 2005;9:158-69.<br />
3. de Meijer AR, Fikkers BG, Keijzer MH et al. Serum creatine kinase as a predictor of<br />
clinical course in rhabdomyolysis: a 5-year intensive care survey. Intens <strong>Care</strong> Med<br />
2003;29:1121-25.<br />
16. Lifting the veil off sedation: towards a more<br />
wakeful intensive care (ICU)<br />
K Everingham, T Fawcett, T Walsh<br />
University of Edinburgh, Edinburgh, Scotland<br />
Strategies to reduce sedation are associated with improved patient<br />
outcomes during critical illness. 1 <strong>The</strong> implementation of daily sedation<br />
reviews and sedation holds is frequently challenging, despite inclusion in<br />
National Patient Safety Programmes. 2 Sedation management is<br />
predominantly a nurse-led activity, but few studies have specifically<br />
explored critical care nurses experiences and feelings surrounding sedation<br />
management and the clinical decisions they make. <strong>The</strong>se issues are key to<br />
successful implementation of systematic changes in care.<br />
We aimed to provide insight into beliefs surrounding sedation<br />
practices, especially sedation ‘holds’, among ICU nurses focusing on how<br />
the environment, nursing behaviours, knowledge and personal experiences<br />
S-6<br />
influence their clinical decisions.<br />
Sixteen qualitative interviews were completed employing a<br />
phenomenological approach whereby an individual’s lived experience of<br />
their world is explored to gain a deeper understanding, interpretation and<br />
meaning of phenomena. Nurses of varying ages, gender and nursing<br />
experience were interviewed at the bedside. Taped interviews were<br />
transcribed, repeatedly listened to and supported by field notes. Non-verbal<br />
gestures and intonations were incorporated. Using an interpretive analysis,<br />
commonality of themes and meanings were exposed and the con<strong>text</strong>ual<br />
implications of the findings explored.<br />
<strong>The</strong>mes emerged from the data that demonstrate that the lived<br />
experience of the critical care nurses can militate against optimal sedation<br />
interventions and patient outcomes. <strong>The</strong> nurses’ perceived a more wakeful<br />
ICU population to increase their workload without increased support. A<br />
pressure of obligation from medical staff to perform sedation holds<br />
emerged, even if it conflicted with their own professional judgement. <strong>The</strong>re<br />
was a perception that sedation holds were ‘expected of them’. Related to<br />
this, traditional power relations between nurses and doctors were still<br />
evident, wherein the nurses felt they were being perceived as ‘lazy or<br />
‘wanting an easy shift’ if they opposed sedation holds. <strong>The</strong>se feelings<br />
manifested as a loss of autonomy and feelings of detachment around the<br />
process of sedation assessment and management. “Negative” consequences<br />
of reduced sedation, especially agitation, were strongly associated with less<br />
sedation. Agitation was elicited as a source of fear, both for nurse’s safety<br />
and patient safety. Nurses recalled instances where adverse events, such as<br />
unintentional tube and line removal, occurred as a result of agitation.<br />
Nurses grappled with feelings of guilt, blame and failure to protect their<br />
patients from harm, which developed into resentment and apprehension<br />
in regards to future sedation holds. Each of these feelings impinged<br />
upon the clinical decisions made and constituted barriers to optimal<br />
sedation management.<br />
Despite the evidence demonstrating that less sedation equates to better<br />
patient outcomes, and although nurses are ideally placed to drive a change<br />
of practice, there are clear identified barriers that impede them delivering<br />
optimal sedation care.<br />
References<br />
1. Kress J, Pohlman A, O’Connor M et al. Daily interruption of sedative infusions in<br />
critically ill patients undergoing mechanical ventilation. N Engl J Med 2000;342:1471-77.<br />
2. NHS Scotland (2009) Scottish Patient Safety Alliance [online] Available from:<br />
http://www.patientsafetyalliance.scot.nhs.uk/programme [accessed 2nd July 2011].<br />
17. A pilot research study: do raised biomarkers<br />
predict major complications earlier than clinical<br />
suspicion following cardio-oesophagectomy<br />
D Frimpong*, K McGrattan † , J Ward †<br />
*University of Manchester, Manchester, UK. † Lancashire Teaching<br />
Hospitals NHS Foundation Trust, Preston, UK<br />
Oesophageal cancer is a common cancer that affects 7500 people per year<br />
in the UK. 1 Radical treatment can involve surgery (cardiooesophagectomy).<br />
2 Cardio-oesophagetomy is associated with major<br />
complications. <strong>The</strong> main objective of the study is to determine if<br />
inflammatory markers, released in response to surgery, infection and<br />
inflammation, can predict complications before clinical suspicion. Earlier<br />
detection of complications can potentially avoid further invasive<br />
investigations and reduce morbidity and mortality.<br />
Nine participants completed the study over an eight-week period. Each<br />
participant had ten samples; two preoperative samples to determine a<br />
baseline and eight postoperative samples starting 48 hours postoperatively.<br />
Participant hospital notes were used to collect information on<br />
complications.<br />
In general there was a rise in the inflammatory markers postoperatively<br />
followed by a rapid decline. Eight of the nine patients developed<br />
complications; 55% of the participants had arrhythmias in the first four<br />
postoperative days. One patient had an anastomotic leak and a<br />
bronchopleural fistula. CRP remained elevated in this patient and PCT<br />
Volume 13, Number 1, January 2012 <strong>JICS</strong>
Research poster presentations<br />
showed a secondary rise. Rises in CRP, PCT and neutrophils correlated<br />
well with complications however did not precede clinical suspicion.<br />
Inflammatory markers are raised following cardio-oesophagectomy,<br />
peaking in the first two to three days and declining rapidly. Although some<br />
correlated with complications none consistently preceded clinical<br />
suspicion. This study is limited by population size and a large multi centre<br />
trial is recommended.<br />
References<br />
1. Cancer Research UK. Oesophageal Cancer – UK incidence statistics. [Online]. Updated 17<br />
December 2010. Accessed 01/07/11. Available from: http://info.cancerresearchuk.org/<br />
cancerstats/types/oesophagus/incidence/<br />
2. Lancashire and South Cumbria Cancer Network. UGI Specialist MDT Operational<br />
Policy. June 2011.<br />
20. <strong>The</strong> use of an inflammatory biomarker panel<br />
incorporating the BAL/blood ratio of monocytic<br />
surface TREM-1 in the diagnosis of ventilatorassociated<br />
pneumonia<br />
V Grover* † , P Kelleher †‡ , D Henderson †‡ , P Pantelidis †‡ , F Gotch † , N Soni*,<br />
S Singh*<br />
*Chelsea and Westminster NHS Foundation Trust, London, UK. † Imperial<br />
College London, UK. ‡ Imperial College Healthcare NHS Trust, London,<br />
UK<br />
Diagnosis of ventilator-associated pneumonia (VAP) is slow and fraught<br />
with difficulty. Biomarkers may speed up diagnosis. <strong>The</strong> Triggering<br />
Receptor Expressed on Myeloid Cells-1 (TREM-1) is elevated in<br />
extracellular infections 1 and is a putative biomarker. It exists as a surface<br />
protein on monocytes and neutrophils, together with a soluble isoform.<br />
<strong>The</strong> diagnostic utility of bronchoalveolar lavage (BAL) soluble TREM-1 is<br />
controversial. No data exists on BAL surface TREM-1 in VAP. We<br />
investigated whether BAL surface TREM-1 expression increases in VAP and<br />
whether the BAL/blood ratio improves diagnostic accuracy. We also aimed<br />
to identify a diagnostic biomarker panel given that a single analyte is<br />
unlikely to classify all VAP cases.<br />
Ninety-one adults were recruited into four groups and paired BAL and<br />
blood obtained: 27 with VAP (diagnosed by Clinical Pulmonary Infection<br />
Score and positive semi-quantitative microbiology), 18 ventilated without<br />
infection (ventilated control, VC), 15 ventilated with non-pulmonary<br />
infection (ventilated sepsis elsewhere, VSE) and 27 non-ventilated noninfected<br />
patients with chronic lung disease (non-ventilated control, NVC).<br />
Soluble biomarkers (IL-1β, IL-6, IL-8, soluble TREM-1 and procalcitonin)<br />
and surface markers (monocytic and neutrophilic surface TREM-1, CD11b<br />
and CD62L) were assayed in each sample, together with peripheral white<br />
cell count and CRP. Receiver-operator characteristic (ROC) curves were<br />
constructed for each marker. Data was assessed using the Kruskal-Wallis<br />
and Mann-Whitney tests, with Dunn’s post-hoc analysis for multiple<br />
comparisons. <strong>The</strong> VAP group was compared to VC and VSE groups<br />
individually. As no significant difference existed, VC and VSE groups were<br />
combined into a non-VAP group. Fisher discriminant analysis was used to<br />
construct a diagnostic biomarker panel. 2<br />
Monocytic surface TREM-1 (mTREM-1) had an area under ROC<br />
curve (AUC) of 0.89 for diagnosing VAP, improving to 0.94 with the<br />
mTREM-1 BAL/blood ratio. Other individual markers had AUCs of<br />
0.56-0.80. A six-marker panel incorporating the BAL/blood ratio of<br />
mTREM-1 and monocytic CD11b (mCD11b), BAL soluble TREM-1 and<br />
IL-1β, blood IL-6 and CRP differentiated VAP, non-VAP and NVC groups.<br />
For VAP, the AUC (95% CI) of this panel was 0.98 (0.96-1.00).<br />
Sensitivity, specificity and likelihood ratio (LR) were 95%, 93% and 12.9.<br />
Cross-validation and use of training and validation cohorts confirmed the<br />
robustness of the panel.<br />
In conclusion, the BAL/blood ratio of surface mTREM-1 may be useful<br />
in VAP diagnosis and differentiation from non-pulmonary sepsis. A<br />
diagnostic biomarker panel incorporating the BAL/blood ratio of mTREM-<br />
1 and mCD11b, BAL soluble TREM-1 and IL-1b, blood IL-6 and CRP has<br />
clinical utility in identifying VAP.<br />
Figure 1. mTREM-1 expression in BAL and the BAL/blood ratio. Box-whisker<br />
(Tukey) plots of the BAL mTREM-1 levels and the BAL/blood ratio in VAP,<br />
ventilated control (VC), ventilated sepsis elsewhere (VSE) and non-ventilated<br />
control (NVC) patients. Medians and inter-quartile ranges are indicated.<br />
p
Research poster presentations<br />
Patient demographics and HIV risk factors (n=90)<br />
Age (mean, SD) 49 (10.9)<br />
Male Sex (%, n) 83 (75/90)<br />
Black ethnicity (%, n) 29 (26/90)<br />
Country of origin UK (%, n) 53 (48/90)<br />
Africa (%, n) 20 (18/90)<br />
Other (%, n) 27 (24/90)<br />
HIV risk group Heterosexual (%, n) 36 (31/85)<br />
Homosexual (%, n) 58 (49/85)<br />
IVDU (%, n) 6 (5/85)<br />
HepBSAg+ (%, n) 12 (7/59)<br />
HepCAb+ (%, n) 10 (6/58)<br />
CD4 cell count at time of ICU admission (median, IQR) 168 (30.5, 351)<br />
History of AIDS defining illness (%, n) 56 (47/84)<br />
First AIDS defining illness in ICU (%, n) 25 (18/72)<br />
New diagnosis of HIV in ICU (%, n) 19 (17/90)<br />
Criteria for HAART met at admission CD4
Research poster presentations<br />
significant additional critical care workload. With increasing trust wide<br />
adoption, corresponding education and safety initiatives, a trend towards<br />
reduction has been seen in duration of stay and cumulative mortality for<br />
all unplanned admissions.<br />
References<br />
1. Kumar A, Roberts D, Wood KE et al. Duration of hypotension before initiation of<br />
effective antimicrobial therapy is the critical determinant of survival in human septic<br />
shock. Crit <strong>Care</strong> Med 2006;34:1589-96.<br />
2. McQuillan P, Pilkington S, Allan A. Confidential enquiry into the quality of care before<br />
intensive care unit admission. Br Med J 1998;316:1853-58.<br />
3. Subbe CP, Davies RG, Williams E et al. Effect of introducing the modified early warning<br />
score on clinical outcomes, cardiopulmonary arrests and intensive care utilisation in<br />
acute medical admissions. Anaesthesia 2003;58:797-802.<br />
25. AKI in elderly emergency abdominal surgery<br />
patients<br />
A Krige, E Baird, J Bannard-Smith, V Meadway<br />
Royal Blackburn Hospital, Blackburn, UK<br />
Acute kidney injury (AKI) occurs in 1% of all non cardiac surgical patients<br />
and is associated with higher morbidity and mortality. 1 Development of<br />
new acute renal failure still carries a morality of up to 50%. <strong>The</strong> impact of<br />
AKI on the health economy is significant, with renal replacement therapy<br />
costing approximately £850/day. 2 Optimising renal blood flow and oxygen<br />
delivery peri-operatively, aggressively managing severe sepsis, and avoiding<br />
nephrotoxic drugs may reduce the incidence. <strong>The</strong> recent NCEPOD report<br />
highlights continued failure to provide the above and report an incidence<br />
of 36.6% in the elderly undergoing emergency surgery.<br />
We undertook a retrospective case note review of patients over the age<br />
of 65, undergoing emergency, non-vascular, abdominal surgery in a district<br />
general hospital. Using the ORMIST theatre computer system, 149 patients<br />
were identified between Nov 2007 and March 2009. Ninety-five sets of<br />
notes were available of which 27 were incorrectly coded and two were<br />
unacceptable due to excessive data omission. <strong>The</strong> remaining 66 case notes<br />
were systematically reviewed and additional information retrieved from the<br />
ICE blood results system and ORMIST. Data is reported as mean (SD) or<br />
median (IQR). <strong>The</strong> Chi-squared test was used to compare mortality<br />
between RIFLE classes 2 and the Kruskall-Wallis tests for LOS between<br />
RIFLE classes. 3<br />
<strong>The</strong> mean age of the 66 patients analysed was 78.24 years, 53% were<br />
female and 47% were admitted to critical care post-operatively. <strong>The</strong> overall<br />
incidence of AKI was 36.4% in this high-risk population. Twenty-four<br />
(38.7%) of 62 cases adequately documented had abdominal sepsis. This<br />
group had 33% unadjusted mortality in comparison with 13% mortality in<br />
the group without abdominal sepsis. Table 1 summarises all other results.<br />
RIFLE Classes 0 Risk Injury Failure<br />
n 42 12 7 5<br />
Age (years)* 79.45 (6.3) 77.42 (8.4) 77.14 (5.52) 72.6 (7.89)<br />
pPOSSUM (%)* 20.22 (22.11) 15.5 (17.36) 46.57 (45) 44.4 (28.33)<br />
Time to source 64.5 (20.75- 55 (33.75-90) 8 (5-35) 12 (10.5-104.5)<br />
control (mins) κ 182.75)<br />
Pre-op IV fluid 2829 (1450) 3091 (1868) 1917 (801) 4600 (2632)<br />
volume (mL)*<br />
Hospital LOS (days) κ 18 (12.75-35.5) 20.5 (10.25 14 (5-25) 32 (18.5-34.5)<br />
-39.5)<br />
Hospital survival (%)* Δ 88 (32.8) 75 (45.2) 43 (53.5) 80 (44.7)<br />
* mean (SD); κ median (IQR); Δ p=0.045<br />
Table 1. Process and outcome data according to RIFLE categories.<br />
<strong>The</strong> incidence of AKI in our dataset mirrors the recent NCEPOD<br />
report 4 and the difference in mortality between RIFLE groups reaches<br />
statistical significance (see Table 1) with a stepwise increase in mortality<br />
moving through RIFLE categories until we see a contradictory reduction in<br />
mortality in RIFLE F. However there are only five patients in this group.<br />
<strong>The</strong>re may also be selection bias, ie three patients in RIFLE F received RTT,<br />
indicating they were an elderly group whose baseline function was<br />
sufficient to provide aggressive multi-organ support where treatment<br />
limitations may have been deemed more appropriate in other patients. In<br />
keeping with NCEPOD 4 our series also shows lengthy delays to source<br />
control and frequently inadequate fluid management.<br />
References<br />
1. Brienza N, Gigilio M, Marucci M et al. Preventing kidney injury after non cardiac<br />
surgery. Current Opin Crit <strong>Care</strong> 2010;16:353-58.<br />
2. NHS Blood and Transplant: Organ Donation. http://www.organdonation.nhs.uk<br />
3. Acute Dialysis Quality Initiative. http://www.adqi.net<br />
4. NCEPOD – An age old problem. 2011.<br />
26. Predicting early readmission to intensive care<br />
using the Modified Early Warning Score (MEWS)<br />
R Lloyd*, A Kaliappan † , N Wee*, R Parker ‡<br />
*Ipswich Hospital, Ipswich, UK. † Addenbrooke’s Hospital, Cambridge,<br />
UK. ‡ University of Cambridge, UK<br />
<strong>The</strong> Modified Early Warning Score (MEWS) is a physiological scoring<br />
system based on simple observations of a patient’s vital signs. It is widely<br />
used across the UK by critical care outreach and ward nursing teams as a<br />
track and trigger score to alert medical teams to a deteriorating patient and<br />
to escalate levels of care. Higher scores have been associated with increased<br />
risk of death, ICU admission and cardiac arrests. 1 <strong>The</strong> usefulness of MEWS<br />
within Critical <strong>Care</strong> setting has not been adequately studied. It is not<br />
common practice to calculate the MEWS when planning to discharge a<br />
patient back to the ward after their ICU stay.<br />
After gaining local research ethics committee approval, we investigated<br />
the association of the MEWS score calculated at the point of discharge<br />
from intensive <strong>Care</strong> Unit (ICU) and readmission to ICU within 48 hours.<br />
We retrospectively analysed all the ward discharges from our ICU for the<br />
year 2009 (n=532) and calculated their MEWS score before ICU discharge.<br />
Out of a total 673 admissions, we excluded the 88 patients who died in<br />
the ICU, 34 who died on the ward following ICU discharge and 19 patients<br />
who were transferred to other ICUs. <strong>The</strong> remaining admissions (n=532)<br />
were included in the analysis. <strong>The</strong>re were 50 readmissions in total. Of<br />
these 10 were early readmissions within 48 hours. MEWS at discharge<br />
ranged between 0 to 10 with 1 and 2 being the most frequent score.<br />
A logistic regression model was used with early readmissions as the<br />
outcome variable and MEWS as the explanatory variable. After using<br />
Generalised Estimating Equations to adjust for clustering, we found a<br />
statistically significant relationship between MEWS and early readmissions<br />
with an odds ratio for MEWS 1.35(95% confidence interval 1.07-1.69) and<br />
a robust Z score 2.58.<br />
MEWS odds 95% CI of Robust Z<br />
ratio odds ratio score<br />
MEWS 1.35 1.07-1.69 2.58<br />
Adjusted for age and gender 1.35 1.07-1.70 2.52<br />
Adjusted for risk of death (ROD) score 1.41 1.11-1.81 2.76<br />
Adjusted for BMI (log10 transformed) 1.49 1.17-1.90 3.18<br />
A group of patients with MEWS score one unit higher than another<br />
group of patients, are expected to have odds of early readmission 1.35<br />
times higher on average (95% CI 1.07 to 1.69) than for the other group of<br />
patients. MEWS was still found to be a significant predictor of early<br />
readmission even after separately adjusting for age and gender, ROD score<br />
and BMI. This study shows that it may be beneficial to use the MEWS<br />
when planning to discharge an ICU patient to the ward. Further studies are<br />
needed to evaluate if there is a threshold MEWS score above which early<br />
readmission is more likely.<br />
Reference<br />
1. Cullinane M, Findlay G, Hargraves C, Lucas S. An Acute Problem National Confidential<br />
Enquiry into Patient Outcome and Death. 11th May 2005. www.ncepod.org.uk/2005report<br />
(accessed 1/07/2011).<br />
<strong>JICS</strong> Volume 13, Number 1, January 2012 S-9
Research poster presentations<br />
27. Readmissions to intensive care units in Scotland:<br />
epidemiology, risk factors and outcomes<br />
NI Lone*, KM Rowan † , TS Walsh*, SH Wild*, GD Murray*<br />
*University of Edinburgh. † <strong>Intensive</strong> <strong>Care</strong> National Audit and Research<br />
Centre (ICNARC), London, UK<br />
Readmission to intensive care is associated with poorer outcomes and<br />
increased resource use. Early readmission is used as an indicator of quality<br />
of care. Studies investigating patients readmitted to intensive care have<br />
been limited to using only ICU audit databases to determine risk factors<br />
and outcomes. In Scotland, there is the unique opportunity to link the ICU<br />
database to other national healthcare databases. Our aim was to use data<br />
linkage to assess the validity of records coded as readmissions in the ICU<br />
database, and to identify risk factors for and report outcomes of patients<br />
readmitted to all ICUs in Scotland in 2005.<br />
We used a retrospective cohort design. <strong>The</strong> national database of ICU<br />
admissions, SICSAG (Scottish <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong> Audit Group), was<br />
linked to the Scottish acute hospital discharges and death registry<br />
databases. <strong>The</strong> cohort comprised patients >16 years old admitted to a<br />
Scottish ICU in 2005. We excluded those who were not at risk of future<br />
ICU readmission i.e. those dying during their first admission and those<br />
discharged after 31/12/2005. We used binary logistic regression to identify<br />
risk factors for readmission and to adjust outcomes for important<br />
confounders. <strong>The</strong> outcome was three year mortality after ICU discharge.<br />
Validity of the readmission field was checked against the linked<br />
hospital dataset using patients whose hospital admission started and ended<br />
during 2005.<br />
<strong>The</strong>re were 8992 ICU admission episodes in the SICASG database in<br />
2005 of which 6554 had a valid linkage and fulfilled inclusion criteria.<br />
<strong>The</strong>re were 5894 (89.9%) first admissions; 660 (10.1%) readmission<br />
episodes and 566 (9.6%) patients had at least one readmission during the<br />
12-month study period (range 0-9). One quarter of patients (n=148) had<br />
their first readmission within 48 hours of ICU discharge. In multivariable<br />
analysis, only out-of-hours discharge (OR1.4, p=0.02), prior<br />
cardiopulmonary resuscitation (OR0.5, p=0.03), discharge destination<br />
(p=0.003) and Charlson comorbidity (p=0.001) were independent risk<br />
factors for readmission. Patients with at least one readmission during the<br />
12-month study period were significantly more likely to die at three years<br />
post-ICU discharge than those with no readmissions (mortality 54.1% vs<br />
30.7%, logrank-χ2 175.6, p
Research poster presentations<br />
including soluble (sol)-TNF and the adhesion molecule L-selectin. We<br />
sought to determine whether TACE activity and substrate shedding in<br />
critically ill patients would be altered when compared to healthy controls.<br />
Blood samples (day 0, 2, 4 and 6) were taken from mechanically<br />
ventilated patients (n=5) who had the systemic inflammatory response<br />
syndrome (SIRS). Purified blood monocytes were obtained by magnetic<br />
CD14 positive bead selection from peripheral blood mononuclear cells<br />
(PBMCs). Monocytes were washed and exposed to a LPS stimulus (1µg/mL<br />
for 60 minutes) before having their TACE activity quantified using a cellbased<br />
fluorometric catalytic activity assay. 3,4 Monocyte expression levels of<br />
HLA-DR and of pre and post-LPS TACE and L-selectin were determined<br />
via flow cytometry. PBMC’s were also placed in 16-hour LPS culture and<br />
had sol-TNF production quantified by ELISA.<br />
Funding sources: Both Dr O’Callaghan and Dr Gordon have received<br />
research support from the <strong>Intensive</strong> <strong>Care</strong> Foundation. Dr Gordon is in<br />
receipt of an NIHR Clinician Scientist Fellowship award and is grateful for<br />
funding through the NIHR-BRC funding scheme.<br />
References<br />
1. Volk H, Reinke, P, Krausch D et al. Monocyte deactivation-rationale for a new<br />
therapeutic strategy in sepsis. <strong>Intensive</strong> <strong>Care</strong> Med 1996;22:S474-81.<br />
2. Black R, Rauch C, Kozlosky C et al. A metalloproteinase disintegrin that releases<br />
tumour-necrosis factor-alpha from cells. Nature 1997;385:729-33.<br />
3. Alvarez-Iglesias A, Wayne G, O’Dea KP et al. Continuous real-time measurement of<br />
tumour necrosis factor-α converting enzyme activity on live cells. Lab Invest<br />
2005;85:1440-48.<br />
4. Scott A, O’Dea KP, O’Callaghan D et al. Reactive oxygen species and p38 MAPK mediate<br />
TNF-alpha converting enzyme (TACE/ADAM17) activation in primary human<br />
monocytes. J Biol Chem 2011: Epub 26/08/2011.<br />
33. Citrate based continuous renal replacement<br />
therapy is associated with significantly longer<br />
circuit life compared to heparin or epoprostenol<br />
L Tovey, M Raimundo, S Di Gangi, M Terblanche, H Dickie, M Ostermann<br />
Guy’s and St Thomas’ Hospital, London, UK<br />
Figure 1a and 1b. TACE activity changes over sampling time course (mean +<br />
SD), n=3-5. (a): Baseline (un-stimulated) activity levels. (b) Activity increase<br />
from baseline (%) on LPS exposure. * p
Research poster presentations<br />
34. Outcomes of patients with HIV and AIDS<br />
admitted to intensive care units in the United<br />
Kingdom — analysis of the ICNARC Case Mix<br />
Programme<br />
RJ Parker*, GS Power † , DA Harrison † , KM Rowan †<br />
*Aintree University Hospitals NHS Foundation Trust, Liverpool, UK. † <strong>Intensive</strong><br />
<strong>Care</strong> National Audit and Research Centre (ICNARC), London, UK<br />
<strong>Intensive</strong> care unit (ICU) outcome due to human immunodeficiency virus<br />
infection (HIV) and the acquired immunodeficiency syndrome (AIDS) was<br />
initially extremely poor. Subsequent data suggest it is now similar to that of<br />
other general medical patients on ICU. 1 Whether due to better ICU<br />
management or the availability in developed countries of highly active<br />
antiretroviral therapy remains debated. 1<br />
<strong>The</strong> ICNARC Case Mix Programme (CMP) is the national clinical audit<br />
of adult critical care units in England, Wales and Northern Ireland.<br />
Following extensive validation, data are pooled into the CMP Database.<br />
Since 2006, whether an admission has HIV or AIDS has been collected as<br />
part of the CMP dataset.<br />
Of 304,435 admissions to 200 critical care units between 1 April 2006<br />
and 31 December 2010 893 patients with HIV and 152 with AIDS were<br />
identified (
Research poster presentations<br />
References<br />
1. Ware LB, Matthay MA. <strong>The</strong> acute respiratory distress syndrome. N Engl J Med<br />
2000;342:1334-49.<br />
2. Matute-Bello G, Downey G, Moore BB et al. An Official American Thoracic <strong>Society</strong><br />
Workshop Report: features and measurements of experimental acute lung injury in<br />
snimals. Am J Respir Cell Mol Biol 2011; 44:725-38.<br />
3. Ware LB. Modeling human lung disease in animals. Am J Physiol Lung Cell Mol Physiol<br />
2008;294:L149-50.<br />
4. Matute-Bello G, Frevert CW, Martin TR. Animal models of acute lung injury. Am J<br />
Physiol Lung Cell Mol Physiol 2009;295:L379-99.<br />
37. Serial muscle ultrasound detects acute muscle<br />
loss in multi-organ failure<br />
ZA Puthucheary* § , J Rawal*, B Connolly † , M McPhail ‡ , G Ratnayake † ,<br />
PS Sidhu § , D Shrikrishna ∞ , P Hopkins § , N Hopkinson ∞ , M Polkey ∞ , MJ<br />
Rennie # , A Rowlerson § , J Moxham § , S Harridge § , N Hart † , H Montgomery*<br />
*University College London, Whittington Hospital NHS Trust, London,<br />
UK. † Guy’s and St Thomas’ and King’s College London, NIHR<br />
Comprehensive Biomedical Research Centre, St Thomas’ Hospital,<br />
London, UK. ‡ Imperial College London, Hammersmith Hospital NHS<br />
Trust, UK. § King’s College London, UK. ∞ Royal Brompton Hospital,<br />
Imperial College London, UK. # University of Nottingham, UK.<br />
Muscle wasting and weakness is a debilitating consequence of critical<br />
illness. However, tests for the early identification and tracking of muscle<br />
loss are lacking. Manual muscle testing is currently advocated, but requires<br />
patient co-operation, which is difficult in the early stages of critical illness.<br />
Muscle ultrasound is potentially a useful clinical tool as it not only<br />
provides an objective measure but is also inexpensive and portable. We<br />
hypothesised that serial muscle ultrasound would be able to identify and<br />
track muscle loss.<br />
Critically ill patients were recruited from a district general hospital and<br />
a university teaching hospital within the first 24 hours of admission.<br />
Inclusion criteria were (i) likely to remain intubated ≥48 hours (ii) likely<br />
to remain in critical care ≥7 days. Patients were excluded if they i) were<br />
pregnant ii) had disseminated malignancy iii) suffered from a primary<br />
neuromuscular disease. Serial measurements of rectus femoris cross<br />
sectional area (RF CSA<br />
) were taken using B-mode ultrasound, on days 1, 3, 7<br />
and 10 of admission. Bedside physiological data was collected, allowing<br />
patients to be stratified by numbers of failed organ systems. <strong>The</strong> primary<br />
endpoint was a change of 15% of RF CSA<br />
in 10 days.<br />
Twenty-six patients were recruited and fulfilled entry criteria at 10 days.<br />
Using the Sequential Organ Failure Assessment (SOFA) score, six patients<br />
had single organ failure, and 20 had ≥2 organ failure. Patients with ≥2 had<br />
significantly greater loss of muscle at 10 days than those with single organ<br />
failure (19.4±1.94% vs 1.79±1.75%, p=0.003) as shown in Figure 1. Subgroup<br />
analysis comparing 2-3 organ failure to 4-6 organ failure<br />
demonstrated no significant difference in muscle loss (-18.1%±5.3 vs<br />
-20.9%±11.7, p=0.355). No difference was seen in age (52.4±17.6 vs<br />
54.4±20.8) or Medical Research Council sum scores at day 10 between<br />
groups (47±17.8 vs 51±9.8, p=0.57).<br />
Figure 1. Time course of acute muscle loss during ICU stay: single organ vs<br />
multi-organ failure.<br />
RF CSA<br />
is a clinically useful tool for monitoring muscle loss in critically<br />
ill patients. Substantial muscle loss occurs in patients with ≥2 organ failure<br />
within the first few days with 19% loss in RF CSA<br />
by day 10. No change in<br />
RFCSA was observed in patients with single organ failure. <strong>The</strong> lack of<br />
difference in MRC sum score between the groups could indicate that the<br />
contractile properties of the muscle are maintained despite the loss of<br />
cross-sectional area.<br />
38. Patterns of gene expression associate with risk of<br />
death in patients with severe sepsis due to<br />
community-acquired pneumonia<br />
J Radhakrishnan*, E Svoren § , P Ellis † , C Langford † , P Hutton ‡ , C Garrard ‡ ,<br />
CJ Hinds § , JC Knight∗, on behalf of the GAinS Investigators<br />
*University of Oxford, UK. † University of Cambridge, UK. ‡ John Radcliffe<br />
Hospital, Oxford, UK. § Barts and the London School of Medicine, Queen<br />
Mary University, London, UK<br />
Despite advances in supportive management, mortality rates in patients<br />
with severe sepsis remain high. <strong>The</strong> mechanisms underlying the<br />
pathogenesis of sepsis and in particular the basis of adverse outcomes are<br />
incompletely understood. <strong>The</strong>re is evidence that genetic factors are<br />
important and may influence sepsis susceptibility and outcome.<br />
After ethics approval and gaining informed consent, 74 adult patients<br />
admitted to intensive care with severe sepsis due to community-acquired<br />
pneumonia (CAP) were recruited. Pregnant patients and those with preexisting<br />
immune compromise were excluded. Peripheral blood leukocyte<br />
samples (n=129) were collected at the bedside using a leukodepletion filter<br />
system (LeukoLOCK, Ambion) on days 1, 3 and 5 following admission to<br />
the intensive care unit (ICU). Genome wide gene expression was measured<br />
by hybridising the extracted RNA to whole genome bead arrays (Illumina<br />
HT12 v4) that interrogate ~48,000 unique transcripts. <strong>The</strong> findings were<br />
validated in an additional 55 samples from 30 patients using Illumina<br />
WGA v3 bead arrays.<br />
After normalisation, exploratory analysis was performed by hierarchical<br />
clustering of the principal components contributing to the observed<br />
variance. Differences between groups of interest were examined using<br />
Bayesian analysis by fitting hierarchical mixed models with Markov Chain<br />
Monte Carlo sampling using a Gibbs sampler. Gene set enrichment<br />
analysis and the DAVID functional gene annotation system were used to<br />
cluster significant genes into biologically informative pathways. All results<br />
were confirmed in the validation data set.<br />
<strong>The</strong> overall mortality was 17.6% (n=13). <strong>The</strong> median age was 60<br />
(IQR=20) years in survivors (S) and 64 (IQR=28) in non-survivors (NS) (p<br />
>0.05). NS showed significantly higher relative neutrophil counts (87.5 vs<br />
82.1), lower monocyte counts (4.5 vs 7.6), and a worse oxygenation index<br />
(14.9 vs 20.6). <strong>The</strong>re were no other significant differences between S and<br />
NS in terms of demographics, microbiology, organ failures or severity<br />
scores.<br />
Exploratory factor analysis by unsupervised clustering revealed a<br />
previously unidentified substructure in the global gene expression data set<br />
for the 74 patients. Three distinct clusters of differentially expressed genes<br />
were defined which displayed a graded increase in mortality rates (5%,<br />
10%, 33% respectively for each cluster group). Analysis of the validation<br />
data set using genes defining the clusters in the training set (~2800)<br />
showed an identical substructure with the same proportional differences in<br />
mortality rates. Clustering was explained by differences in the expression<br />
of genes associated with mitochondrial ribosomes, mitochondrial<br />
membrane associated proteins, and vesicle processing in association with<br />
class II MHC genes. Poor outcome was also associated with changes in<br />
glucose metabolism and DNA repair mechanisms related to oxidative<br />
damage. Significant sex-specific effects on gene expression were noted.<br />
We have shown how analysis of gene expression can resolve a clinically<br />
homogeneous cohort of patients with severe sepsis into distinct clusters<br />
predictive of risk of death. Differential expression of genes associated with<br />
mitochondrial function made an important contribution to the clustering.<br />
<strong>The</strong>se findings highlight some convincing mechanistic explanations for<br />
adverse outcomes in sepsis and could potentially be used to stratify<br />
patients according to risk of death on admission to ICU.<br />
<strong>JICS</strong> Volume 13, Number 1, January 2012 S-13
Research poster presentations<br />
Acknowledgements: Dr Radhakrishnan was in receipt of a Wellcome<br />
Trust Training Fellowship. <strong>The</strong> study was also supported by funding from<br />
the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>, the UKCRN, the Sainsbury Family Trusts and<br />
Sirius Genomics.<br />
42. Gender differences in inflammation in a model of<br />
acute lung injury induced by inhaled<br />
lipopolysaccharide in healthy volunteers<br />
E O’Brien, M Shyamsundar, CM O’Kane, DF McAuley<br />
Queens University of Belfast, UK<br />
Conflicting findings on the effect of gender difference on outcome in<br />
patients with sepsis and ALI have been reported in observational studies.<br />
However in patients exposed to infection, females are less likely to progress<br />
to severe sepsis. <strong>The</strong> objective of this study was to assess the effect of<br />
gender on the inflammatory response in a model of ALI induced by<br />
inhaled lipopolysaccharide (LPS).<br />
Thirty healthy volunteers from the placebo arms of two clinical trials<br />
(ISRCTN21056528 and ISRCTN98813895) were included in this study.<br />
Subjects inhaled 50µg LPS and bronchoalveolar lavage (BAL) was<br />
performed at six hours after LPS inhalation. Cytokines were measured by<br />
using cytometric bead array (R&D Systems). Total white cell count<br />
(WCC) was determined using a haemocytometer. Data are mean [±SD] or<br />
median [IQR].<br />
Figure 1.<br />
Fourteen (47%) of the volunteers were male. BAL IL-8 (pg/mL) was<br />
significantly higher in females (Figure 1). <strong>The</strong>re was no difference in BAL<br />
TNF α, IL-1β, IL-6, MCP-1 and IL-1ra. BAL IL-10 levels were below the<br />
limit of detection. <strong>The</strong>re was no difference in BAL WCC or neutrophils.<br />
We have shown that in a model of ALI induced by inhaled LPS, female<br />
subjects mounted a higher cytokine response as evidenced by a higher BAL<br />
IL-8 level. <strong>The</strong> increase in BAL IL-8 may promote a more pro-inflammatory<br />
alveolar milieu. Increased alveolar inflammation in females may account<br />
for both reduced progression from infection to severe sepsis through<br />
improved bacterial clearance, but in those who do progress to severe sepsis<br />
the exaggerated inflammatory response might result in increased organ<br />
dysfunction and account for poor outcome. Understanding gender<br />
determined differences in response to infection might highlight new<br />
therapies for sepsis and ALI.<br />
Funded by the UK <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong> and NI R&D Office.<br />
43. Capillary lactate in critical care<br />
D Soo*, J Baldwin*, N Miller-Biot † , E Shardlow*, E Davies † , P Bunting*,<br />
S Laha*<br />
*Lancashire Teaching Hospitals NHS Trust, Preston, UK. † University of<br />
Manchester, Manchester, UK<br />
S-14<br />
<strong>The</strong> measurement of lactate levels has an established role in the assessment<br />
of the critically ill patient, both in indicating risk of mortality, 1-3 and in<br />
guiding treatments such as entry into sepsis protocols. 4 Hand-held devices<br />
have been designed to measure lactate at the bedside. Analysis of capillary<br />
blood samples on such devices, if shown to be accurate, could have<br />
advantages over currently used methods, such as increased turn-around<br />
times which would facilitate decision making. <strong>The</strong> aim of this study was to<br />
ascertain whether capillary lactate analysed on a hand-held device can<br />
produce results that correlate sufficiently with the gold-standard method<br />
(arterial blood analysed by the laboratory) to be considered reliable.<br />
Adult patients admitted to the critical care unit of a teaching hospital,<br />
and requiring arterial lines as part of their normal care, were enrolled<br />
prospectively during the study period March-July 2011. From each patient<br />
capillary, arterial and venous samples were taken. Capillary samples were<br />
measured on the Roche ® Accutrend hand-held lactate analyser. Venous and<br />
arterial samples, taken by venepuncture and withdrawn from the arterial<br />
line respectively, were tested on the hand-held device and sent to the<br />
hospital's laboratory for testing (Roche ® Modular P Unit lactate analyser).<br />
Agreement between the lactate measurement methods were assessed<br />
using inter-method reliability coefficients (ICCs) and Bland-Altman plots.<br />
Correlation was estimated through calculations of r 2 .<br />
From a cohort of 36 patients, capillary lactate levels measured on the<br />
hand held device (range=1 to 4.6) showed poor agreement (ICC=0.16) and<br />
poor correlation (r 2 =0.34) with laboratory tested arterial samples<br />
(range=0.47 to 3.58 mmol/L). Results from venous blood analysed on the<br />
hand-held device compared with venous blood measured in the laboratory<br />
were analysed as part of the secondary outcomes. Agreement and<br />
correlation were better, though not statistically significant (ICC 0.75, limits<br />
of agreement -0.24 and 1.46, r 2 =0.84).<br />
<strong>The</strong> poor correlation between capillary measured lactate and the goldstandard,<br />
excludes the possibility for it to replace current practice.<br />
However, venous blood analysed on the hand-held lactate meter had better<br />
correlation with laboratory results. This is a promising finding and will be<br />
the subject of future research projects in the same department.<br />
References<br />
1. Bakker J, Gris P, Coffernils M et al. Serial blood lactate levels can predict the<br />
development of multiple organ failure following septic shock. Am J Surg 1996;171:<br />
221-26.<br />
2. Smith I, Kumar P, Molloy S et al. Base excess and lactate as prognostic indicators for<br />
patients admitted to the intensive care. <strong>Intensive</strong> <strong>Care</strong> Med 2001;27:74-83.<br />
3. Khosravani H, Shahpori R, Stelfox HT et al. Occurrence and adverse effect on outcome<br />
of hyperlactatemia in the critically ill. Crit <strong>Care</strong> 2009;13:90.<br />
4. Dellinger RP, Levy MM, Carlet JM et al. Surviving Sepsis Campaign: international<br />
guidelines for management of severe sepsis and septic shock. Crit <strong>Care</strong> Med 2008;36:<br />
296-327.<br />
44. Does the prophylactic use of Octenisan skin<br />
washes reduce the incidence of bacteraemias and<br />
MRSA acquisition in critical care<br />
C Spencer, D Orr, S Hallam, E Tillmans<br />
Lancashire Teaching Hospitals, Preston, UK<br />
Routine daily body-washes with the antiseptic, chlorhexidine, have been<br />
previously shown to be associated with a reduction in MRSA (methicillin<br />
resistant Staphylococcus aureus) and VRE (vancomycin resistant<br />
Enterococcus) acquisition and bacteraemia. 1 Octenisan ® (Schulke & Mayr,<br />
Germany) is an antiseptic in widespread clinical use as part of MRSA<br />
eradication therapy. <strong>The</strong> active ingredient, octenidine has a wide spectrum<br />
of antibacterial and antifungal action but is particularly active against<br />
MRSA without inducing resistance. 2<br />
We performed this retrospective, uncontrolled study in a 24-bedded<br />
mixed critical care unit with tertiary neurosciences, at Lancashire Teaching<br />
Hospitals. From 1st June 2009 to 1st June 2010 all elective and emergency<br />
patients admitted, were washed with soap and water. From 1st June 2010<br />
to 1st June 2011 all elective and emergency admissions were washed with<br />
soap and water only if visibly soiled, then washed from the neck down<br />
with Octenisan, with a contact time of three minutes before being washed<br />
off. Measured outcomes were:<br />
Volume 13, Number 1, January 2012 <strong>JICS</strong>
Research poster presentations<br />
MRSA acquisition – defined as a patient with no previous history of<br />
MRSA, who had negative surveillance swabs (skin, nose, perineum) on<br />
unit admission, who later cultured MRSA from any site.<br />
ICU-acquired bacteraemias – defined as a positive blood culture,<br />
obtained >48 hours post admission to the unit.<br />
Chi squared test was used for testing for statistical significance.<br />
Soap and water Octenisan<br />
(2009/10) (2010/11)<br />
Patients admitted 1206 1225<br />
MRSA acquisitions 29 7 (p=0.0002)<br />
MRSA bacteraemias 3 0<br />
Total blood cultures taken 322 336<br />
>48 hours post ICU admission<br />
Number of bacteraemias 37 31 (p=0.4669)<br />
>48 hours post ICU admission<br />
<strong>The</strong> 76% reduction in MRSA acquisitions and reduction in bacteraemia<br />
may be due to reducing the bio-burden, or even eradication of MRSA, on<br />
patients skin, reducing risk of further transmission and colonisation.<br />
Infection control practices, including barrier nursing precautions, did not<br />
change across this period. It must be noted however, that MRSA<br />
bacteraemias in the hospital at large did reduce across this period, a<br />
possible confounding factor.<br />
ICU-acquired bacteraemias reduced, although non-significantly. <strong>The</strong><br />
frequency of blood culture sampling did not change during the study<br />
period. <strong>The</strong> largest reduction in bacteraemias was mainly due to a<br />
reduction in coagulase negative staphylococcal (CNS) bacteraemias from<br />
14 to 8 per year (p=0.200). This may be due to a lower skin bio-burden of<br />
CNS leading to fewer inadvertent cultures of skin contaminants, or less<br />
opportunity for invasive CNS infection.<br />
This study shows that routine/prophylactic antiseptic washes with<br />
Octenisan may have a role in programs for MRSA reduction in critical care<br />
units.<br />
Acknowledgements: No funding, no involvement of Schulke-Mayr.<br />
References<br />
1. Climo M, Sepkowitz K, Zuccotti G et al. <strong>The</strong> effect of daily bathing with chlorhexidine<br />
on the acquisition of methicillin-resistant Staphylococcus aureus, vancomycin-resistant<br />
Enterococcus, and healthcare-associated bloodstream infections: Results of a quasiexperimental<br />
multicenter trial. Crit <strong>Care</strong> Med 2009;37:1858-65.<br />
2. Al-Doori Z, Goroncey-Bermes P, Gemmell CG et al. Low-level exposure of MRSA to<br />
octenidine dihydrochloride does not select for resistance. J Antimicrob Chemother<br />
2007;59:1280-81.<br />
45. Regionalisation of ICU and ECMO services in the<br />
UK; beliefs about the evidence, benefits and harm<br />
— a national survey<br />
N Stewart*, K Gunning † , BH Cuthbertson ‡<br />
*Aberdeen Royal Infirmary, Aberdeen, UK. † Addenbrooke’s Hospital,<br />
Cambridge, UK. ‡ Sunnybrook Health Sciences Centre, Toronto, Canada<br />
Extra-corporeal membrane oxygenation (ECMO) has been used<br />
sporadically as rescue therapy for adults with severe acute respiratory<br />
failure in adults. During the recent H1N1 influenza pandemics existing<br />
ECMO capacity has often been saturated. We aimed to determine the views<br />
of <strong>Intensive</strong> <strong>Care</strong> clinicians’ on the development of adult ECMO services.<br />
A UK national survey of all members of the UK <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong> was<br />
conducted.<br />
A total of 2,148 participants were invited to complete the survey with<br />
691 respondents (32.7%). Among respondents: 65% believe adult ECMO<br />
services should be expanded; 42.5% of respondents agreed that ICU<br />
services in the UK should be regionalised while 63.8% agreed the UK<br />
should develop regional ventilatory care centres including ECMO services.<br />
Of these 52.8% believe the development of such centres would lead to<br />
improved outcomes despite only 38.1% agreeing that current evidence base<br />
supports the use of ECMO. Most (72%) agree there is a requirement for<br />
further trials in this area. Experience during H1N1 influenza pandemics<br />
was the factor respondents most frequently identified as driving ECMO<br />
expansion (61.1%). <strong>The</strong> majority (60.1%) believe that expanded ECMO<br />
service should be provided in 5-10 supra-regional centres. Patient safety,<br />
resources, guidelines and transportation of sick patients were also seen as<br />
important issues.<br />
In conclusion, there is support for centralisation of ICU services and for<br />
expansion in ECMO services for adults with severe acute respiratory failure<br />
in the UK. If expansion of ECMO services is envisaged, clinicians support<br />
appropriate funding, investment in transport services and development of<br />
national guidelines.<br />
46. Protocols for the prevention of contrast-induced<br />
nephropathy: a 2011 survey of intensive care<br />
units in the United Kingdom<br />
Strachan JM*, Crilley T † , Parvizi S † , DeVile MPJ ‡<br />
*Royal Berkshire Hospital, Reading, UK. † Milton Keynes General Hospital,<br />
Milton Keynes, UK. ‡ John Radcliffe Hospital, Oxford, UK<br />
Computerised tomography is a common investigation on the intensive care<br />
unit (ICU), frequently exposing patients to intravenous contrast media.<br />
Contrast-induced nephropathy (CIN) is an important cause of renal failure<br />
in the critically ill, and significantly increases mortality. 1 However current<br />
evidence for measures taken to prevent CIN are conflicting and we<br />
hypothesised that wide variation in practice exists throughout the country<br />
with a lack of formal protocols.<br />
We therefore undertook a web-based survey to determine the existence<br />
of protocols on ICUs for the prevention of CIN and also to gauge current<br />
practice. We directed the survey at all units capable of taking level 3<br />
patients across the UK, as defined by the most recent Critical <strong>Care</strong><br />
Directory (2008), via the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong> website and by emailing<br />
individual hospitals. Ethical approval was not thought to be necessary.<br />
During April, May and June 2011 we received responses from 117<br />
individual ICUs from a possible 329 units; a 36% response rate. From these<br />
117 individual ICUs, 32 (27.4%) claimed to have a protocol while 85<br />
(72.6%) did not. Protocols were more likely in specialist ICUs – 10 of 17<br />
units (58.8%) – than teaching hospital ICUs – eight of 32 units (25% ) – or<br />
district general ICUs – 14 of 68 units (20.6%). Of the 32 units that claimed<br />
to have a protocol, 18 (56%) used N-acetylcysteine (NAC) in a variety of<br />
dosing regimens, and the remaining 14 (44%) did not use NAC. In units<br />
with a protocol 1.26% sodium bicarbonate was the preferred fluid type –<br />
used in 11 units (34%), followed by Hartmann’s solution – used in 10 units<br />
(31%) in a wide variety of volumes and regimen timings. Only five units<br />
(16%) with protocols did not use fluid boluses. Of the 85 units that did not<br />
have a protocol, no consensus on the available evidence was stated as the<br />
reason by 48 (41%) while 20 units (17%) felt this is a decision taken by<br />
radiology. Of these units without formal protocols, 17 (20%) still gave<br />
NAC, whereas 68 (80%) did not. A fluid regimen was used by 39 (46%)<br />
while 46 (54%) did not give fluid boluses at all. <strong>The</strong>mes from free <strong>text</strong><br />
comments included the feeling that the evidence is not yet convincing for<br />
widespread use of standardised preventative measures as well as that taking<br />
a “risk benefit” approach, rather than using specific creatinine cut off<br />
values, ought to determine contrast use.<br />
Protocols for the prevention of CIN are not commonplace on ICUs in<br />
the UK. However it appears that many clinicians are thinking about CIN<br />
and freely prescribing some form of prophylaxis. More evidence is<br />
therefore needed to convince the majority of ICU physicians that to follow<br />
a standardised approach in order to prevent renal injury from contrast<br />
media is worthwhile.<br />
Acknowledgement: We acknowledge and thank the <strong>Intensive</strong> <strong>Care</strong><br />
<strong>Society</strong> for promoting the survey online. None of the authors have any<br />
conflicts of interest to declare.<br />
Reference<br />
1. Lakhal K, Ehrmann S, Chaari A et al. Acute Kidney Injury Network definition of<br />
contrast-induced nephropathy in the critically ill: Incidence and outcome. J Crit <strong>Care</strong><br />
Available online 6 July 2011; doi:10.1016/j.jcrc.2011.05.010.<br />
<strong>JICS</strong> Volume 13, Number 1, January 2012 S-15
Research poster presentations<br />
47. Decreased levels in elafin due to proteolytic<br />
cleavage may contribute to alveolar inflammation<br />
in the pulmonary compartment in patients<br />
with ALI<br />
A Kerrin, C O’Kane, M Shyamsundar, T Craig, DF McAuley, CC Taggart<br />
Queen’s University of Belfast, Northern Ireland<br />
Unregulated protease activity may drive dysregulated pulmonary<br />
inflammation implicated in acute lung injury (ALI). Elafin is a potent<br />
serine protease inhibitor produced locally in the lung by epithelial and<br />
inflammatory cells with anti-inflammatory properties. In this study we<br />
assessed the temporal changes in elafin concentration in patients with ALI<br />
and evaluate whether a decrease in elafin levels are due to proteolytic<br />
degradation. We also evaluated the ability of elafin to down-regulate<br />
inflammation in alveolar macrophages.<br />
Patients with ALI within 48 hours of onset of ALI (n=37), day 3 (n=19)<br />
and day 7 (n=9) as well as five healthy volunteers underwent<br />
bronchoalveolar lavage fluid (BALF). Elafin was measured by ELISA. To<br />
determine whether elafin was susceptible to proteolytic cleavage, western<br />
blot analysis of recombinant elafin was incubated with BALF ± protease<br />
inhibitors. Alveolar macrophages from healthy volunteers were isolated<br />
and pre-treated with 10 µg/mL elafin for one hour, followed by 24 hour<br />
stimulation with 100 ng/mL LPS. IL-8 was measured in supernatants by<br />
ELISA.<br />
Elafin was significantly increased at the onset of ALI compared to<br />
healthy volunteers (39±5 ng/mL vs 0.5±0.1 ng/ml; p
Research poster presentations<br />
lungs were noted between the two MHI circuits. Tc-99m uptake was<br />
generally more in the right lung fields (62.7% and 63% respectively) than<br />
in the left lung fields (37.3% and 37% respectively) for all patients and was<br />
least in the left lower segments (4.3% and 6.9% respectively) on both<br />
occasions. No statistically significant differences in HR, MAP or C D<br />
were<br />
noted between the two MHI circuits.<br />
<strong>The</strong> Mapleson-C and Laerdal MHI circuits using PEEP of 7.5 cmH 2<br />
O<br />
and PIP of 25 cmH 2<br />
O in mechanically ventilated patients in the supine<br />
position proved to be equally effective with regards to airflow distribution<br />
through the tracheobronchial tree. <strong>The</strong> supine position however might not<br />
be optimal in the treatment of left lower lobe pathology with MHI as little<br />
airflow was observed to this area during this study.<br />
Acknowledgements: <strong>The</strong> researchers thank all the patients, medical,<br />
nursing and physiotherapy personnel of the multidisciplinary ICU,<br />
Universitas Hospital who participated in this project. Thanks also to<br />
Professor Anton Otto, Head of Nuclear Medicine, Universitas Hospital for<br />
his support to this project. This project was funded by the University of the<br />
Witwatersrand Faculty of Health Sciences Research Committee Individual<br />
Research Grant.<br />
References<br />
1. Berney S, Denehy L, Pretto J. Head-down tilt and manual hyperinflation enhance<br />
sputum clearance in patients who are intubated and ventilated. Aust J Physiother<br />
2004;50:9-14.<br />
2. Choi JSP, Jones AYM. Effects of manual hyperinflation and suctioning on respiratory<br />
mechanics in mechanically ventilated patients with ventilator-associated pneumonia.<br />
Aust J Physiother 2005;51:25-30.<br />
3. Savian C, Chan P, Paratz J. <strong>The</strong> effect of positive end-expiratory pressure level on peak<br />
expiratory flow during manual hyperinflation. Anesth Analg 2005;100:1112-16. DOI:<br />
10.1213/01.ANE.0000147505.98565.AC<br />
53. Outcomes and APACHE II scores for patients<br />
with alcoholic liver disease and ICU admission;<br />
a retrospective observational cohort study<br />
J Welbourne, K Gunning<br />
Addenbrookes Hospital, Cambridge, UK<br />
Analysis of the ICNARC database has shown that intensive care unit (ICU)<br />
admissions with alcoholic liver disease (ALD) increased from 0.65% in<br />
1996 to 1.35% in 2005. 1 <strong>The</strong> Office of National Statistics reports that<br />
alcohol related deaths rose from 6.9 per 100,000 in 1991 to 12.9 per<br />
100,000 in 2005. 2 Available data suggests very poor outcomes for patients<br />
with ALD admitted to ICU. 3<br />
A retrospective observational cohort study was performed between June<br />
2006 and June 2011 in a UK ICU with specialist hepatology care. This<br />
single specialist unit (‘JVF’) data has been compared to national data<br />
(Table 1).<br />
Number of ICU mortality Hospital Mean APACHE II<br />
patients mortality score<br />
ICNARC 118 43.2% 64.9% 20.0<br />
JVF data 46 28% p>0.05 41% p=0.005 20.03 p>0.05<br />
Table 1. National data 2005 and JVF data for patients with alcoholic hepatitis<br />
or alcoholic cirrhosis who are admitted to ICU.<br />
This study shows improved hospital mortality for patients with ALD<br />
admitted to a centre with hepatology care as compared to national data.<br />
Further prospective study is indicated to examine outcomes when patients<br />
with ALD admitted to general ICUs are transferred to a specialist<br />
hepatology centre. This is an area of interest as the number of patients with<br />
ALD admitted to ICU is increasing.<br />
References<br />
1. Welch C, Harrison D, Short A, Rowan K. <strong>The</strong> increasing burden of alcoholic liver<br />
disease on United Kingdom critical care units: secondary analysis of a high quality<br />
clinical database. J Health Serv Res Policy 2008;13 Suppl 2:40-44.<br />
2. Alcohol-related deaths in the United Kingdom, 2000-2009. Office of National Statistics. Jan<br />
2011.<br />
3. Mackle D, Swann. One year outcome of intensive care patients with decompensated<br />
alcoholic liver disease. Br J Anaesth 2006;97:496-98.<br />
55. Deep vein thrombosis (DVT) in critically ill patients<br />
R Moroi, M Takeda, T Harada, M Namiki, A Yaguchi<br />
Tokyo Women’s Medical University, Japan<br />
<strong>The</strong> diagnosis of DVT (deep vein thrombosis) is important to prevent<br />
pulmonary embolism (PE) which eventually causes death in hospitalised<br />
patients. Especially, there is a high incidence of DVT in critically ill<br />
patients, because almost all the patients in the ICU have risk factors for<br />
DVT and limitations of their activities of daily living due to unstable vital<br />
status, controlled with analgesia, or multiple injuries. However, the<br />
prophylaxis and the treatment for DVT are sometimes difficult for ICU<br />
patients because of their underlying disease such as intracranial<br />
hemorrhage, trauma and gastrointestinal hemorrhage. <strong>The</strong> aim of the<br />
present study is to evaluate the backgrounds of DVT patients in ICU and to<br />
assess the prophylaxis and the treatment for DVT in critically ill patients.<br />
Ninety-one ICU patients (57 men (63%), 34 women (37%); age 65 [49-<br />
77]) were included in this study. <strong>The</strong> duplex ultrasound scans (ALOKA ® ,<br />
Tokyo) were performed within one week after admission to the ICU and<br />
DVT was diagnosed by duplex ultrasonography. D-dimer levels (µg/mL)<br />
were measured by latex agglutination test (Sekisui Medical ® , Tokyo)<br />
(normal
Research poster presentations<br />
Quality parameter ETT (n=50) LMA (n=25) BVM (n=25)<br />
Before After P value Before After P value Before After P value<br />
Continuous 0 (0%) 50 (100%) 0 (0%) 25 (100%) 0 (0%) 0 (0%)<br />
compressions, n (%)<br />
Compression depth (mm) 44.39±13.3 44.42±13.1 0.978 44.24±13.7 45.52±13.1 0.565 48.53±14.9 53.20±17.3 0.103<br />
Compression rate 113.6±16.3 115.0±12.8 0.544 116.9±18.8 118.9±13.0 0.576 118.3±13.3 118.1±13.0 0.923<br />
Prop comp depth
Research poster presentations<br />
Doctors Advanced clinical P value<br />
(n=114)<br />
practitioners<br />
(n=80)<br />
No flow time (sec) 221.7±80.6 177±49.7 0.672<br />
No flow ratio 0.19 (0.1,0.24) 0.16 (0.11, 0.29) 0.944<br />
Mean compression depth (mm) 42.37±11.9 41.28±12.8 0.366<br />
Proportions of compressions 0.17 (0.02, 0.52) 0.27 (0.04, 0.54) 0.233<br />
with depth