Acute liver failure following hepatic resection - JICS - The Intensive ...
Acute liver failure following hepatic resection - JICS - The Intensive ...
Acute liver failure following hepatic resection - JICS - The Intensive ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
© <strong>The</strong> <strong>Intensive</strong> Care Society 2013<br />
Review articles<br />
<strong>Acute</strong> <strong>liver</strong> <strong>failure</strong> <strong>following</strong> <strong>hepatic</strong><br />
<strong>resection</strong>: incidence, presentation,<br />
prevention and management in ICU<br />
C Jones, L Kelliher, C Bigham, N Quiney<br />
<strong>The</strong> incidence of <strong>liver</strong> <strong>failure</strong> <strong>following</strong> <strong>liver</strong> <strong>resection</strong> has been reported to be between 8-32%, depending on the number<br />
of segments resected, the health of the patient and the incidence of <strong>hepatic</strong> ischaemic/reperfusion injury. This article<br />
outlines the evidence surrounding classification, prevention and management of this condition.<br />
Keywords: <strong>liver</strong> <strong>resection</strong>; <strong>liver</strong> <strong>failure</strong>; intensive care<br />
Introduction<br />
Mild <strong>liver</strong> dysfunction is occasionally seen <strong>following</strong> major<br />
surgery. <strong>Acute</strong> <strong>liver</strong> <strong>failure</strong> is much rarer. Patients at greatest<br />
risk of developing postoperative <strong>liver</strong> <strong>failure</strong> are those<br />
undergoing <strong>liver</strong> <strong>resection</strong>, where the risk can be as high as<br />
32%. 1 When it does occur, acute <strong>liver</strong> <strong>failure</strong> is a devastating<br />
complication, with a high morbidity and mortality.<br />
<strong>The</strong> spectrum of <strong>liver</strong> dysfunction post-<strong>hepatic</strong> <strong>resection</strong><br />
encompasses everything from a transient rise in <strong>liver</strong> enzymes<br />
to fulminant <strong>liver</strong> <strong>failure</strong> and death. <strong>The</strong> features include<br />
coagulopathy, hyperbilirubinaemia, encephalopathy and<br />
associated multiple organ <strong>failure</strong>. <strong>The</strong> most effective way to<br />
reduce the impact of this complication is to prevent it<br />
developing in the first instance, which requires a careful and<br />
considered approach. Early identification of patients at risk and<br />
prompt and appropriate management of those developing acute<br />
<strong>liver</strong> <strong>failure</strong> is key.<br />
<strong>The</strong> incidence of <strong>liver</strong> <strong>resection</strong> surgery is increasing as a<br />
treatment for certain benign and malignant <strong>liver</strong> lesions. <strong>The</strong><br />
most common indication in the UK is for treatment of <strong>liver</strong><br />
metastases associated with colorectal cancer. Approximately<br />
3,600 patients per year fit into this category, a figure that will<br />
only increase with improvements in chemotherapy regimens. 2<br />
Hepatic <strong>resection</strong> is also performed in live-donor <strong>liver</strong><br />
transplantation.<br />
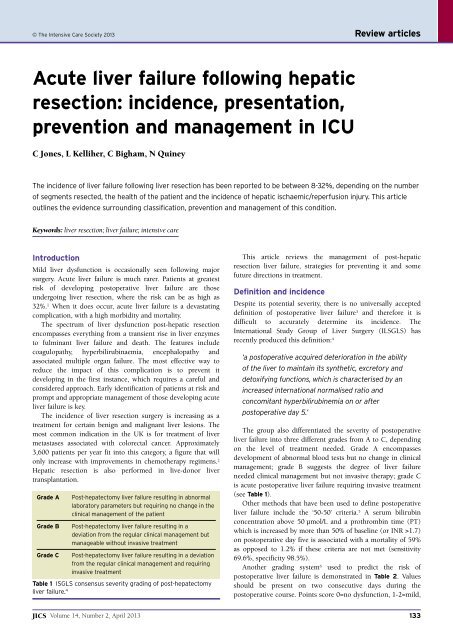
Grade A<br />
Grade B<br />
Grade C<br />
Post-hepatectomy <strong>liver</strong> <strong>failure</strong> resulting in abnormal<br />
laboratory parameters but requiring no change in the<br />
clinical management of the patient<br />
Post-hepatectomy <strong>liver</strong> <strong>failure</strong> resulting in a<br />
deviation from the regular clinical management but<br />
manageable without invasive treatment<br />
Post-hepatectomy <strong>liver</strong> <strong>failure</strong> resulting in a deviation<br />
from the regular clinical management and requiring<br />
invasive treatment<br />
Table 1 ISGLS consensus severity grading of post-hepatectomy<br />
<strong>liver</strong> <strong>failure</strong>. 4<br />
This article reviews the management of post-<strong>hepatic</strong><br />
<strong>resection</strong> <strong>liver</strong> <strong>failure</strong>, strategies for preventing it and some<br />
future directions in treatment.<br />
Definition and incidence<br />
Despite its potential severity, there is no universally accepted<br />
definition of postoperative <strong>liver</strong> <strong>failure</strong> 3 and therefore it is<br />
difficult to accurately determine its incidence. <strong>The</strong><br />
International Study Group of Liver Surgery (ILSGLS) has<br />
recently produced this definition: 4<br />
‘a postoperative acquired deterioration in the ability<br />
of the <strong>liver</strong> to maintain its synthetic, excretory and<br />
detoxifying functions, which is characterised by an<br />
increased international normalised ratio and<br />
concomitant hyperbilirubinemia on or after<br />
postoperative day 5.’<br />
<strong>The</strong> group also differentiated the severity of postoperative<br />
<strong>liver</strong> <strong>failure</strong> into three different grades from A to C, depending<br />
on the level of treatment needed. Grade A encompasses<br />
development of abnormal blood tests but no change in clinical<br />
management; grade B suggests the degree of <strong>liver</strong> <strong>failure</strong><br />
needed clinical management but not invasive therapy; grade C<br />
is acute postoperative <strong>liver</strong> <strong>failure</strong> requiring invasive treatment<br />
(see Table 1).<br />
Other methods that have been used to define postoperative<br />
<strong>liver</strong> <strong>failure</strong> include the ‘50-50’ criteria. 5 A serum bilirubin<br />
concentration above 50 µmol/L and a prothrombin time (PT)<br />
which is increased by more than 50% of baseline (or INR >1.7)<br />
on postoperative day five is associated with a mortality of 59%<br />
as opposed to 1.2% if these criteria are not met (sensitivity<br />
69.6%, specificity 98.5%).<br />
Another grading system 6 used to predict the risk of<br />
postoperative <strong>liver</strong> <strong>failure</strong> is demonstrated in Table 2. Values<br />
should be present on two consecutive days during the<br />
postoperative course. Points score 0=no dysfunction, 1-2=mild,<br />
<strong>JICS</strong> Volume 14, Number 2, April 2013 133
Review articles<br />
Points 0 1 2<br />
Total serum bilirubin (µmol/L) ≤20 21-60 >60<br />
Prothrombin time 6<br />
(seconds above normal)<br />
Serum lactate (mmol/L) ≤1.5 1.6-3.5 >3.5<br />
Encephalopathy severity grade None 1 and 2 3 and 4<br />
Table 2 Severity of postoperative <strong>hepatic</strong> dysfunction score. 6<br />
3-4=moderate, >4= severe dysfunction.<br />
<strong>The</strong> incidence of acute <strong>liver</strong> <strong>failure</strong> <strong>following</strong> <strong>hepatic</strong><br />
<strong>resection</strong> has been reported to be as high as 32% by some<br />
authors, 1 although others suggest it is nearer 8%. Schindl and<br />
colleagues believe that the risk should be quoted as less than<br />
1% in patients with no parenchymal disease and having small<br />
<strong>resection</strong>s; 10% when four segments are being resected and<br />
30% for those having five or more segments resected. 6<br />
With advances in surgical and anaesthetic techniques,<br />
mortality rates <strong>following</strong> <strong>liver</strong> <strong>resection</strong> surgery have decreased<br />
from 20% in the 1970s 8 to approximately 2% today. 9<br />
Postoperative <strong>hepatic</strong> insufficiency/<strong>failure</strong> accounts for between<br />
60 and 100% of these deaths. 5,6,10-12 Morbidity <strong>following</strong> <strong>liver</strong><br />
<strong>resection</strong> remains high, with rates between 15-35%. 13-15<br />
Causes of post-<strong>hepatic</strong> <strong>resection</strong> <strong>liver</strong> <strong>failure</strong><br />
Liver dysfunction is seen occasionally after any major surgery.<br />
Periods of intraoperative hypoxia, hypotension, the use of<br />
blood transfusions or development of sepsis can all result in<br />
<strong>liver</strong> ischaemia and/or cellular dysfunction. Following <strong>liver</strong><br />
<strong>resection</strong>, intra-operative blood loss of more than one litre with<br />
the need for blood transfusion increases the risk of<br />
postoperative <strong>liver</strong> <strong>failure</strong> and sepsis. 16,17 Sepsis has a<br />
detrimental effect on <strong>liver</strong> function (by inhibiting Kupffer cell<br />
function) and affects <strong>hepatic</strong> cell regeneration. 18<br />
A normal subject with no other risk factors can have up to<br />
75% of their <strong>liver</strong> resected safely. 19 <strong>The</strong> <strong>liver</strong> has a great<br />
capacity to regenerate, and the remnant can increase by 100%<br />
in size in as little as a week (although this is not reflected in a<br />
concomitant increase in synthetic function).<br />
<strong>The</strong> most important risk factors for postoperative <strong>liver</strong><br />
<strong>failure</strong> are: 3,12<br />
• <strong>The</strong> size of <strong>resection</strong><br />
• Evidence of preoperative <strong>liver</strong> parenchymal disease (eg<br />
cirrhosis)<br />
• Hepatic ischaemia/reperfusion injury.<br />
Removal of four or more segments (out of eight) is<br />
associated with an increased risk of postoperative <strong>liver</strong> <strong>failure</strong>.<br />
If the <strong>liver</strong> remnant is too small, there may not be enough<br />
functioning hepatocytes for adequate synthesis, excretion and<br />
detoxification. Another problem with small <strong>liver</strong> remnants is<br />
hyperperfusion; 20 the relative increase in blood flow causes<br />
sinusoidal dilatation, haemorrhagic infiltration, centrilobar<br />
necrosis and prolonged cholestasis, causing further impaired<br />
synthetic function and inhibition of cell proliferation. 3,20<br />
Underlying <strong>liver</strong> disease reduces the functional and<br />
regenerative capacity of the <strong>liver</strong> and therefore makes it more<br />
susceptible to damage. A larger remnant volume needs to be<br />
present at the end of surgery. 3,18 Chemotherapy also affects <strong>liver</strong><br />
parenchyma and reduces its regenerative capacity. A recent<br />
French study looked at 101 patients undergoing intensive<br />
chemotherapy (≥6 cycles of the newer chemotherapy agents:<br />
oxaliplatin and irinotecan) prior to undergoing <strong>liver</strong> <strong>resection</strong>.<br />
<strong>The</strong>y found that 50% of patients developed sinusoidal<br />
obstruction syndrome and 10% steatohepatitis on histological<br />
analysis (5% had both). 20 Both sinusoidal injury and steatosis<br />
from chemotherapy reduce the regenerative capacity of the<br />
<strong>liver</strong> remnant and therefore increase the likelihood of<br />
postoperative <strong>failure</strong>. 3,22,23 Sinusoidal injury may also occur as a<br />
result from ‘small-for-size syndrome,’ when dysfunction occurs<br />
after a living-donor partial graft. It is thought to be due to<br />
portal hyperperfusion of the graft, combined with poor venous<br />
outflow, resulting in sinusoidal congestion and endothelial<br />
dysfunction. 24 A similar picture can be seen after extensive<br />
<strong>hepatic</strong> <strong>resection</strong> with a small <strong>liver</strong> remnant.<br />
Vascular occlusive techniques used to reduce intraoperative<br />
bleeding comprise either total occlusion of both inflow and<br />
outflow, or total inflow occlusion. <strong>The</strong> ‘Pringle’ manoeuvre<br />
refers to the total occlusion of inflow, ie occlusion of <strong>hepatic</strong><br />
artery and portal vein inflow to the <strong>liver</strong>. This limits blood<br />
supply to the <strong>liver</strong>, with the result that bleeding will principally<br />
be a result of <strong>hepatic</strong> venous pressure, which itself can be<br />
reduced by maintaining a low CVP intraoperatively. Occlusion<br />
induces ischaemia in the <strong>liver</strong> remnant, 25 resulting in <strong>hepatic</strong><br />
ischaemia/reperfusion injury, the generation of free radicals and<br />
subsequent <strong>liver</strong> dysfunction. For this reason, the Pringle<br />
manoeuvre is now used much less frequently 26 and for less<br />
than forty-five minutes in total during surgery. 27<br />
Other risk factors for postoperative <strong>liver</strong> <strong>failure</strong> include<br />
age over sixty-five, as the ability of the <strong>liver</strong> to regenerate<br />
decreases with age, 28 diabetes mellitus and poor nutritional<br />
status. 3,18 Being male doubles the risk of developing<br />
postoperative <strong>liver</strong> <strong>failure</strong>. 29<br />
Rarely, postoperative <strong>liver</strong> <strong>failure</strong> can result from altered<br />
vascular supply. Portal or <strong>hepatic</strong> vein obstruction can occur<br />
either through thrombosis, torsion or surgical injury. It is<br />
worth considering these options and excluding them with an<br />
ultrasound scan. Postoperative cholestasis can also ‘muddy the<br />
waters.’ It is often drug-induced (eg penicillin, erythromycin<br />
and NSAIDs), but can occasionally be a result of the surgery<br />
itself, or <strong>following</strong> total parenteral nutrition on the intensive<br />
care unit. Occasionally an isolated increase in bilirubin can<br />
occur, for example <strong>following</strong> a blood transfusion or in a patient<br />
with Gilbert’s syndrome. Gilbert’s syndrome is present in 2-5%<br />
of the population. A decreased activity of <strong>hepatic</strong> glucuronyl<br />
transferase leads to an increase in unconjugated bilirubin.<br />
Preventative strategies<br />
Careful patient selection to ensure adequate<br />
residual <strong>liver</strong> volume<br />
In patients with normal <strong>liver</strong> parenchyma, a remnant as small<br />
as 26% of the original <strong>liver</strong>’s volume can be safely left. 6<br />
However those with parenchymal diseases require a larger<br />
residual volume (approximately 40%) to avoid postoperative<br />
<strong>liver</strong> <strong>failure</strong>; 19 a similar volume has been suggested for those<br />
patients who have received intensive chemotherapy treatment<br />
134<br />
Volume 14, Number 2, April 2013 <strong>JICS</strong>
Review articles<br />
(>6 cycles) prior to <strong>liver</strong> <strong>resection</strong> surgery. 21 In that study, the<br />
authors found that residual volumes of 44.8%, 43.1% and<br />
37.7% were independent predictors of overall morbidity, sepsis<br />
and <strong>liver</strong> <strong>failure</strong> respectively.<br />
In patients with cirrhosis, <strong>resection</strong>s should only be offered<br />
in those with stable disease (ie Child-Pugh class A); only very<br />
small <strong>resection</strong>s in selected patients should be offered to patients<br />
with Child-Pugh class B, and avoided in class C patients.<br />
Where an extensive <strong>resection</strong> is planned, avoiding the<br />
problems associated with a potentially small remnant can be<br />
achieved by employing strategies such as preoperative<br />
neoadjuvant chemotherapy to reduce the volume of tumour,<br />
performing a staged hepatectomy or a preoperative portal vein<br />
embolisation (PVE). PVE is one of the most useful strategies<br />
there is in preventing postoperative <strong>liver</strong> dysfunction and<br />
involves embolising one of the portal veins to induce <strong>liver</strong><br />
atrophy on the operative side and hypertrophy in the intended<br />
remnant section. 30<br />
Choice of anaesthetic agents<br />
<strong>The</strong> volatile anaesthetic agents metabolised in the <strong>liver</strong> are<br />
known to alter <strong>hepatic</strong> blood flow and induce transient<br />
changes in <strong>liver</strong> enzymes. <strong>The</strong> use of halothane, which on<br />
repeated exposure may cause hepatitits (so-called ‘halothane<br />
hepatitis’) is now uncommon. Other volatile agents, including<br />
isoflurane, sevoflurane and desflurane, have minimal <strong>hepatic</strong><br />
metabolism and there is a lack of evidence demonstrating<br />
hepatotoxicity. 31 Total intravenous anaesthesia (TIVA) has been<br />
advocated by some as a preferred option in <strong>liver</strong> surgery, but to<br />
date there is no evidence to support this.<br />
Minimise blood loss<br />
Postoperative blood transfusions have an immunosuppressive<br />
effect 16 and, as stated above, the requirement for blood<br />
transfusion <strong>following</strong> major blood loss increases the risk of<br />
postoperative <strong>liver</strong> <strong>failure</strong>. 16,17 Strategies to reduce blood loss<br />
include: maintaining a low central venous pressure<br />
(
Review articles<br />
there are localising signs. Cerebral oedema is a worrying<br />
complication, which is more prevalent the more acute the <strong>liver</strong><br />
<strong>failure</strong>. Increased ammonia may be involved in the<br />
development of cerebral oedema by both cytotoxic and<br />
vasogenic mechanisms.<br />
Cardiovascular<br />
Distributive shock develops with severe peripheral shunting. A<br />
high cardiac output, decreased oxygen extraction, and low<br />
systemic vascular resistance are all features. <strong>The</strong> origin of the<br />
peripheral shunting is unclear. It may be the result of<br />
platelet/fibrin plugs, and abnormal vasomotor tone. 44 <strong>The</strong><br />
result is poor peripheral extraction of oxygen.<br />
Renal<br />
<strong>Acute</strong> kidney injury is common. This is multifactorial; the<br />
common reasons are pre-renal renal <strong>failure</strong> and acute tubular<br />
necrosis. Hepato-renal syndrome (HRS) can occur in fulminant<br />
<strong>liver</strong> <strong>failure</strong> and is associated with high morbidity and<br />
mortality. 45 HRS is more typically associated with<br />
decompensated chronic <strong>liver</strong> disease, portal hypertension and<br />
spontaneous bacterial peritonitis. Differentiating HRS from prerenal<br />
<strong>failure</strong> that progresses to ATN can be difficult. Urine<br />
sodium analysis and microscopy can be helpful. HRS typically<br />
takes longer to resolve, if it does at all, being associated with<br />
greater than 50% mortality. When acute <strong>liver</strong> <strong>failure</strong> develops<br />
<strong>following</strong> a <strong>resection</strong>, it will be acute (within 28 days),<br />
so manifestations more commonly linked to chronic <strong>liver</strong><br />
disease are less likely to be present, such as portal hypertension<br />
and tense ascites. However, if they occur (as the underlying<br />
architecture of the remaining <strong>liver</strong> may be compromised)<br />
then they should be managed appropriately. If tense ascites<br />
is present, then reducing intra-abdominal pressure can<br />
improve renal function. Hypophosphataemia can also<br />
sometimes be seen after <strong>liver</strong> <strong>resection</strong> due to increased renal<br />
excretion of phosphate.<br />
Infection<br />
Immunocompromise is a feature of acute <strong>liver</strong> <strong>failure</strong> 12 and<br />
consequently bacterial and fungal infections are more<br />
prevalent. Infection can also be harder to detect as there<br />
is a blunted systemic inflammatory response in this population.<br />
A high index of suspicion is required; for management,<br />
see below.<br />
Pharmacology<br />
A number of drugs are metabolised in the <strong>liver</strong>. This results in<br />
prolonged effects of sedation, certain neuromuscular blockers<br />
and a number of ‘housekeeping’ ICU drugs, eg omeprazole.<br />
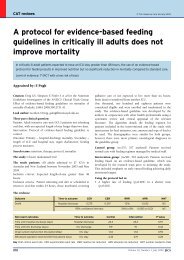
Supportive management of acute <strong>liver</strong> <strong>failure</strong><br />
In most centres, patients undergoing <strong>liver</strong> <strong>resection</strong> will be<br />
admitted to a level 2 bed for initial postoperative care. <strong>The</strong><br />
majority of patients will pass through without complication. If<br />
acute <strong>liver</strong> <strong>failure</strong> develops, then supportive management<br />
(Table 3) is required until either the <strong>liver</strong> regenerates, a<br />
treatable cause of the <strong>liver</strong> <strong>failure</strong> is established or (if<br />
appropriate) an orthotic <strong>liver</strong> transplant is performed.<br />
Airway<br />
Intubation will be required when the airway is no longer<br />
protected in grade 3/4 encephalopathy, or if the airway is<br />
compromised in another way.<br />
Respiratory<br />
Hypoxia may be a problem due to concomitant pneumonia,<br />
pulmonary oedema or pulmonary haemorrhage. Due to the<br />
concern over the possibility of cerebral oedema, PaCO 2 will<br />
have to be controlled tightly at 4.5-5 kPa and minimal<br />
achievable PEEP should be used.<br />
Cardiovascular<br />
Distributive shock usually develops and appropriate fluid<br />
loading and vasopressors will be needed. A cerebral perfusion<br />
pressure of 50-60 mm Hg will be required for neuroprotection.<br />
Neurological<br />
As previously stated, encephalopathy, cerebral oedema,<br />
intracranial haemorrhage and seizures can occur. In acute <strong>liver</strong><br />
<strong>failure</strong>, the level of encephalopathy and degree of oedema are<br />
closely linked. If cerebral oedema is suspected, neuroprotective<br />
strategies should be implemented such as the aforementioned<br />
control of carbon dioxide levels and arterial blood pressure<br />
control. Other aspects include maintaining blood sugar levels<br />
of less than 10 mmol/L (avoiding hypoglycaemia), keeping the<br />
head up at 30 degrees and avoiding ties for the endotracheal<br />
tube. An intracranial pressure monitor may be inserted;<br />
however, risks of intracranial bleeding and infection are higher<br />
in the <strong>liver</strong> <strong>failure</strong> population. It can be a useful monitor<br />
provided that it is used to guide use of aggressive therapy, such<br />
as hypertonic saline to achieve a sodium level of 145-<br />
155 mmol/L, mannitol, cooling to 32-34 degrees or deep<br />
sedation to achieve burst suppression. Other monitors can also<br />
be used, such as the transcranial Doppler or jugular bulb<br />
oxygen saturation monitor, to guide therapy. Encephalopathy is<br />
typically graded from 0 to 4, and is thought to result from a<br />
number of metabolites not cleared by the <strong>liver</strong>; this improves<br />
as <strong>liver</strong> function returns. Administration of regular lactulose<br />
may be helpful. Seizures should be initially controlled with<br />
phenytoin and minimal doses of benzodiazepines (due to their<br />
prolonged action). An electroencephalogram may be required<br />
to prove termination of seizures if any doubt exists. <strong>The</strong> cause<br />
for the seizures should be established, including brain imaging.<br />
Biochemistry<br />
Bicarbonate infusions can be used, but often, renal replacement<br />
therapy is required to provide the appropriate support for<br />
acidosis, fluid and electrolyte control. Anticoagulation of the<br />
filter circuit may not be required or, depending on the platelet<br />
count, prostacyclin may be used.<br />
Coagulopathy<br />
In the early postoperative period, it is reasonable to treat an<br />
INR of >1.5. However, others suggest that it is not necessary to<br />
correct clotting abnormalities (provided there is no bleeding)<br />
unless invasive procedures are planned or the coagulopathy is<br />
profound. 2 In fulminant <strong>liver</strong> <strong>failure</strong>, coagulopathy can be<br />
profound (and resistant to Vitamin K). In this unit, we correct<br />
136<br />
Volume 14, Number 2, April 2013 <strong>JICS</strong>
Review articles<br />
Problem<br />
Circulatory disturbances<br />
Management/Aim<br />
CVP 8-12 mm Hg<br />
MAP 65-90 mm Hg<br />
Haematocrit ≥30%<br />
Central venous oxygen saturation ≥70%<br />
Respiratory dysfunction Arterial oxygen saturation ≥93%<br />
Renal dysfunction<br />
Liver protection<br />
Sepsis<br />
Urine output ≥0.5 mL/kg/hr<br />
N-acetylcysteine infusion for 72 hours: 150 mg/kg loading dose over<br />
one hour, 12.5 mg/kg/hr for four hours, 6.25 mg/kg/hr subsequently<br />
Septic screen: CXR, sputum, urine and blood culture<br />
Ascitic fluid from drain site<br />
Consider CT abdomen<br />
Start antibiotics if worsening of encephalopathy or SIRS parameters<br />
Coagulopathy Platelet count ≥50 x 10 9 /L<br />
(correct if bleeding or invasive procedure) International standardised ratio ≤1.5<br />
Ascites<br />
Encephalopathy/cerebral oedema<br />
If grade 3-4<br />
Paracentesis if severe pain or respiratory/renal compromise<br />
Start lactulose<br />
Neuroprotective strategies: keep PaO 2 >10 kPa, PaCO 2 4.5-5 kPa,<br />
cerebral perfusion pressure >50-60 mm Hg, blood sugar 6-10 mmol/L,<br />
head up, no neck ties<br />
Consider ICP monitor and/or other cerebral monitoring tools.<br />
Resistant ICP treatments include hypertonic saline, mannitol and<br />
cooling to 32-24°C<br />
Nutrition<br />
Stress ulcer prophylaxis<br />
Enteral energy supply of 2,000 kcal/day<br />
Enteral is preferred to parenteral route<br />
Maintain euglycaemia and other electrolytes within normal<br />
range (K + /PO -3 4 /Mg ++ )<br />
Start proton pump inhibitor<br />
Table 3 Goal directed therapy, adapted from: van den Broek, 48 Hammond. 3<br />
the coagulopathy if haemostasis is required or for<br />
interventional procedures. Fresh frozen plasma (FFP) and<br />
cryoprecipitate can be used, but give a significant volume load.<br />
Consequently, recombinant factor VIIa and fibrinogen<br />
concentrate can be useful. Early thrombocytopenia is often not<br />
corrected until levels are below 50 x 10 9 /L and haemostasis is a<br />
concern. Thrombocytopenia that develops later can have lower<br />
limits prior to correction. Platelet dysfunction can be<br />
quantified by using appropriate thrombo-elastogram<br />
preparations or platelet function analysers.<br />
Renal dysfunction<br />
<strong>Acute</strong> kidney injury should be managed by the three basic<br />
principles:<br />
• Providing an adequate blood pressure<br />
• Optimal cardiac output with appropriate fluid loading<br />
• Avoiding nephrotoxic drugs.<br />
If severe <strong>liver</strong> <strong>failure</strong> develops, continuous haemofiltration is<br />
usually required for a number of reasons, most commonly,<br />
profound acidosis. It is not clear whether haemodiafiltration or<br />
high volume exchanges provide any significant survival<br />
advantage. If HRS is suspected, then there is limited evidence to<br />
suggest that terlipressin is a useful vasopressor and that albumin<br />
is a useful replacement fluid. 46 This can be 4.5% albumin if<br />
hypovolaemia is suspected and 20% albumin otherwise.<br />
In the event of tense ascites, drainage should be performed<br />
to prevent a high intra-abdominal pressure, but it is unclear<br />
whether high-volume or low-volume ascites removal (with<br />
appropriate albumin replacement) is beneficial.<br />
Infection<br />
Patients with <strong>liver</strong> <strong>failure</strong> are at particular risk of developing<br />
sepsis due to a combination of immunoparesis, poor<br />
nutritional status and increased gut translocation. Sepsis can<br />
arise as a result of both bacterial and fungal pathogens (see<br />
Table 4). Some studies have demonstrated that prophylactic<br />
antibiotics can reduce the incidence of infective complications<br />
in patients with established postoperative <strong>liver</strong> <strong>failure</strong>, 3,7,47,48<br />
however they are not routinely recommended as they have not<br />
been shown to improve outcomes or survival. 3,49,50 Equally,<br />
some studies have suggested a role for routine antifungal<br />
prophylaxis, although conclusive evidence is lacking. 51<br />
<strong>JICS</strong> Volume 14, Number 2, April 2013 137
Review articles<br />
Fungal<br />
Candidia albicans<br />
Aspergillus<br />
Bacterial<br />
Escherichia coli<br />
Staphylococcus<br />
Pseudomonas<br />
secondary to relative hyperperfusion may be successfully<br />
managed by decreasing portal venous inflow through<br />
embolisation of the splenic artery as described in two case<br />
series. 67,68 Surprisingly, neither of these reported any serious<br />
complications such as splenic infarction, but this was not<br />
been replicated in another, smaller case series. 69<br />
Table 4 Commonest pathogens in <strong>liver</strong> <strong>failure</strong>. 52<br />
Diagnosing sepsis in this population is difficult and regular<br />
surveillance cultures are recommended with an early escalation<br />
of antibiotic therapy and antifungals.<br />
Nutrition<br />
Poor nutritional status can affect outcome after major cancer<br />
surgery. 53 It is associated with an altered immune response and<br />
can reduce regeneration of <strong>liver</strong> cells. 54-56 Early enteral feeding<br />
can preserve the integrity of the gut barrier and so reduce<br />
postoperative infection rates. 57,58 Those developing <strong>liver</strong> <strong>failure</strong><br />
should have regular high-dose lactulose (start at 20 mL tds) to<br />
produce 3-4 soft stools per day.<br />
N-acetylcysteine (NAC)<br />
Glutathione is an anti-oxidant found in the <strong>liver</strong> and plays an<br />
important role in the cellular defence mechanisms against<br />
oxidative damage from free radicals. 59,60 Glutathione is oxidised<br />
by oxygen-free radicals; its oxidised form is then reduced by<br />
NADPH (reduced nicotinamide adenine dinucleotide<br />
phosphate) forming an oxidation/reduction cycle that serves to<br />
‘mop up’ harmful free radicals. During hypoxia, glutathione<br />
stores are consumed, which can add to oxidative injury on<br />
reperfusion. 61,62 NAC is a precursor to glutathione and, when<br />
given as an infusion postoperatively, may reduce <strong>liver</strong><br />
dysfunction. NAC also has an anti-inflammatory action<br />
inhibiting chemotaxis. This, in turn, decreases the generation<br />
of oxygen-free radicals by phagocytic cells. 63 In other nonparacetamol-induced<br />
causes of acute <strong>liver</strong> <strong>failure</strong>, both<br />
intravenous and oral NAC have been shown to improve<br />
transplant-free survival and appear safe and well tolerated. 64,65<br />
However, the evidence for the routine use of NAC to reduce<br />
ischaemia/reperfusion injury and prevent complications after<br />
major surgery is inconclusive. 62 Many units still use this as a<br />
routine therapy until normal <strong>liver</strong> function has returned. 35<br />
<strong>Acute</strong> postoperative <strong>liver</strong> <strong>failure</strong> amenable to<br />
treatment<br />
It is important to rule out any treatable cause of post-<strong>resection</strong><br />
<strong>liver</strong> <strong>failure</strong>:<br />
• Portal vein thrombosis: This will give rise to ischaemia and<br />
possible infarction. <strong>The</strong> diagnosis can be made using either<br />
ultrasound Doppler or CT scan. <strong>The</strong> debate over whether<br />
early postoperative portal vein thrombosis is best managed<br />
with surgical de-obstruction or anticoagulation remains<br />
unresolved. 24<br />
• Venous outflow obstruction: Where this is due to rotation of<br />
the remnant <strong>liver</strong> segment, surgical intervention is<br />
indicated. <strong>The</strong>re is also a role for endovascular stenting to<br />
improve venous outflow. 66<br />
• ‘Small-for-size’ remnant: <strong>The</strong>re is some evidence that<br />
patients with a small remnant and venous congestion<br />
Liver transplantation<br />
Liver <strong>resection</strong> is often performed for the removal of metastatic<br />
malignancy and in these circumstances, consideration for <strong>liver</strong><br />
transplant is often not appropriate. However, provided there<br />
are no contraindications, <strong>liver</strong> transplantation can be<br />
considered and has been successfully used as the treatment of<br />
postoperative <strong>liver</strong> <strong>failure</strong>. 24 <strong>The</strong> Milan criteria, developed in<br />
patients undergoing <strong>resection</strong>s for hepatocellular carcinoma to<br />
help identify those suitable for transplantation, are as follows:<br />
• Single lesion hepatocellular carcinomas of
Review articles<br />
system, which also uses the principle of albumin dialysis,<br />
where lipophilic albumin-bound toxins (eg bilirubin, etc) are<br />
filtered and then adsorbed with a second circuit, to clean the<br />
albumin before being returned to the patient. SPAD is a Single-<br />
Pass Albumin Dialysis system which uses a similar circuit to<br />
MARS ® , except it uses normal machines and no perfusion<br />
pump systems, and uses a counter-current flow of albumin<br />
solution. Studies have shown that SPAD can achieve greater<br />
clearance of ammonia and bilirubin than MARS ® , although<br />
clearance of water-soluble substances was similar between the<br />
two methods. 76<br />
Conclusion<br />
Despite vast improvements in the perioperative care of patients<br />
undergoing <strong>liver</strong> <strong>resection</strong> surgery, there remains a significant<br />
risk of developing postoperative <strong>liver</strong> <strong>failure</strong>. Best estimates<br />
place the incidence at about 8%. Preoperative <strong>liver</strong> function<br />
and <strong>resection</strong> size are the most important factors in the risk<br />
associated with postoperative <strong>liver</strong> <strong>failure</strong>, although a number<br />
of pre- and peri-operative factors are also important, such as<br />
the presence of diabetes mellitus or the use of vaso-occlusive<br />
techniques. With advances in chemotherapy, patients who<br />
traditionally would not have been considered operable are<br />
becoming amenable to surgical treatment. Careful patient<br />
selection and optimisation, for example using portal vein<br />
embolisation, are important in reducing the incidence of<br />
postoperative <strong>liver</strong> <strong>failure</strong>.<br />
If acute <strong>liver</strong> <strong>failure</strong> occurs, then treatable conditions (such<br />
as segment torsion) should be considered and appropriate<br />
supportive care provided. Preventing and managing<br />
complications (commonly infective or haemorrhagic) are also<br />
an important aspect of care. Fulminant post-<strong>resection</strong> <strong>liver</strong><br />
<strong>failure</strong> has a very poor prognosis, accounting for the majority<br />
of post-<strong>liver</strong> <strong>resection</strong> deaths.<br />
References<br />
1. Schroeder RA, Marroquin CE, Bute BP et al. Predictive indices of<br />
morbidity and mortality. Ann Surg 2006;243:373-79.<br />
2. Garden OJ, Rees M, Poston GJ et al. Guidelines for <strong>resection</strong> of<br />
colorectal cancer <strong>liver</strong> metasteses. Gut 2006;55:Siii1-8.<br />
3. Hammond JS, Guha IN, Beckingham IJ, Lobo DN. Prediction,<br />
prevention and management of post<strong>resection</strong> <strong>liver</strong> <strong>failure</strong>. Br J Surg<br />
2011;98:1188-200.<br />
4. Rahbari NN, Garden OJ, Padbury R et al. Posthepatectomy <strong>liver</strong> <strong>failure</strong>:<br />
a definition and grading by the International Study Group of Liver<br />
Surgery (ISGLS). Surgery 2011;145:713-24.<br />
5. Balzan S, Belghiti J, Farges O et al. <strong>The</strong> ’50-50 criteria’ on postoperative<br />
day 5: an accurate predictor of <strong>liver</strong> <strong>failure</strong> and death after hepatectomy.<br />
Ann Surg 2005;242:824-29.<br />
6. Schindl M, Redhead D, Fearon K et al. Edinburgh Liver Surgery and<br />
Transplantation Experimental Research Group (eLISTER). <strong>The</strong> value of<br />
residual <strong>liver</strong> volume as a predictor of <strong>hepatic</strong> dysfunction and infection<br />
after major <strong>liver</strong> <strong>resection</strong>. Gut 2005;54:289-96.<br />
7. Schreckenbach T, Liese J, Bechstein WO, Moench C. Posthepatectomy<br />
<strong>liver</strong> <strong>failure</strong>. Dig Surg 2012;29:79-85.<br />
8. Foster JH. History of <strong>liver</strong> surgery. Arch Surg 1991;126:381-87.<br />
9. Karanjia ND, Lordan JT, Fawcett WJ et al. Survival and recurrence after<br />
neo-adjuvant chemotherapy and <strong>liver</strong> <strong>resection</strong> for colorectal metastases –<br />
a ten year study. Eur J Surg Oncol 2009;35:838-43.<br />
10.McCall J, Koea J, Gunn K et al. Liver <strong>resection</strong>s in Auckland 1998-2001:<br />
mortality, morbidity and blood product use. N Z Med J 2001;114:266-72.<br />
11.Sun HC, Qin LX, Wang L et al. Risk factors for postoperative<br />
complications after <strong>liver</strong> <strong>resection</strong>. Hepatobiliary Pancreat Dis Int<br />
2005;4:370-74.<br />
12.Mullen JT, Ribero D, Reddy SK et al. Hepatic insufficiency and mortality<br />
in 1,059 noncirrhotic patients undergoing major hepatectomy. J Am Coll<br />
Surg 2007;204:854-62.<br />
13.Parikh AA, Gentner B, Wu T et al. Perioperative complications in<br />
patients undergoing major <strong>liver</strong> <strong>resection</strong> with or without neoadjuvant<br />
chemotherapy. J Gastrointest Surg 2003;7:1082-88.<br />
14.Benoist S, Nordlinger B. Neodjuvant treatment before <strong>resection</strong> of <strong>liver</strong><br />
metastases. Eur J Surgical Oncol 2008;33: S35-S41.<br />
15.Nordlinger B, Sorbye H, Glimelius B et al. Perioperative chemotherapy<br />
with FOLFOX4 and surgery vs surgery alone for resectable <strong>liver</strong><br />
metastases from colorectal cancer (EORTC Intergroup trial 40983): a<br />
randomised controlled trial. Lancet 2008;371:1007-16.<br />
16.Jensen LS, Anderson AJ, Christiansen PM et al. Postoperative infection<br />
and natural killer cell function <strong>following</strong> blood transfusion in patients<br />
undergoing elective colorectal surgery. Br J Surg 1992;79:513-16.<br />
17.Kooby DA, Stockman J, Ben-Porat L et al. Influence of transfusions on<br />
perioperative and long-term outcome in patients <strong>following</strong> <strong>hepatic</strong><br />
<strong>resection</strong> for colorectal metastases. Ann Surg 2003;237:860-69.<br />
18.Garcea G, Maddern GJ. Liver <strong>failure</strong> after major <strong>hepatic</strong> <strong>resection</strong>.<br />
J Hepatobil Pancreat Surg 2009;16:145-55.<br />
19.Clavien PA, Emond J, Vauthey JN et al. Protection of the <strong>liver</strong> during<br />
<strong>hepatic</strong> surgery. J Gastrointest Surg 2004;8:313-27.<br />
20.Clavien PA, Oberkofler CE, Raptis DA et al. What is critical for <strong>liver</strong><br />
surgery and partial <strong>liver</strong> transplantation: size or quality Hepatol<br />
2010;52:715-29.<br />
21.Narita M, Oussoultzoglou E, Fuchshuber P et al. What is a safe future<br />
<strong>liver</strong> remnant size in patients undergoing major hepatectomy for<br />
colorectal <strong>liver</strong> metastases and treated by intensive preoperative<br />
chemotherapy Ann Surg Oncol 2012;19:526-38.<br />
22.Behrns KE, Tsiotos GG, DeSouza NF et al. Hepatic steatosis as a<br />
potential risk factor for major <strong>hepatic</strong> <strong>resection</strong>. J Gastrointest Surg<br />
1998;2:292-98.<br />
23.Karoui M, Penna C, Amin-Hashem M et al. Influence of preoperative<br />
chemotherapy on the risk of major hepatectomy for colorectal <strong>liver</strong><br />
metastases. Ann Surg 2006;243:1-7.<br />
24.Paugam-Burtz C, Wendon J, Belghiti J, Mantz J. Case Scenario:<br />
postoperative <strong>liver</strong> <strong>failure</strong> after <strong>liver</strong> <strong>resection</strong> in cirrhotic patient.<br />
Anesthesiology 2012;116:705-11.<br />
25.Brooks AJ, Hammond JS, Girling K, Beckingham IJ. <strong>The</strong> effect of <strong>hepatic</strong><br />
vascular inflow occlusion on <strong>liver</strong> tissue pH, carbon dioxide, and oxygen<br />
partial pressures: defining the optimal clamp/release regime for<br />
intermittent portal clamping. J Surg Res 2007;141:247-51.<br />
26.Lordan JT, Worthington TR, Quiney N et al. Operative mortality, blood<br />
loss and the use of Pringle manoeuvres in 526 consecutive <strong>liver</strong><br />
<strong>resection</strong>s. Ann R Coll Surg Engl 2009;91:578-82.<br />
27.Sugiyama Y, Ishizaki Y, Imamura H et al. Effects of intermittent Pringle’s<br />
manoeuvre on cirrhotic compared with normal <strong>liver</strong>. Br J Surg<br />
2010;97:1062-69.<br />
28.Iakova P, Awad SS, Timchenko NA. Aging reduces proliferative capacities<br />
of <strong>liver</strong> by switching pathways of C/EBPalpha growth arrest. Cell<br />
2003;113:495-506.<br />
29.Yokoyama Y, Schwacha MG, Samy TS et al. Gender dimorphism in<br />
immune responses <strong>following</strong> trauma and hemorrhage. Immunol Res<br />
2002;26:63-76.<br />
30.Abulkhir A, Limongelli P, Healey AJ et al. Preoperative portal vein<br />
embolization for major <strong>liver</strong> <strong>resection</strong>: a meta-analysis. Ann Surg<br />
2008;247:49-57.<br />
31.Kharasch ED. Adverse drug reactions with halogenated anaesthetics. Clin<br />
Pharmacol <strong>The</strong>r 2008;84:158-62.<br />
32.Jones RM, Moulton CE, Hardy KJ. Central venous pressure and its effect<br />
on blood loss during <strong>liver</strong> <strong>resection</strong>. Br J Surg 1998;85:1058-60.<br />
33.Jones CN, Kelliher L, Thomas R, Quiney N. Perioperative management<br />
of <strong>liver</strong> <strong>resection</strong> surgery. J Perioper Prac 2011;21:198-202.<br />
<strong>JICS</strong> Volume 14, Number 2, April 2013 139
Review articles<br />
34.Wu CC, Ho WM, Cheng SB et al. Perioperative parenteral tranexamic<br />
acid in <strong>liver</strong> tumour <strong>resection</strong>: A prospective randomized trial toward a<br />
“blood transfusion”-free hepatectomy. Ann Surg 2006;243:173-80.<br />
35.Hartog A, Mills G. Anaesthesia for <strong>hepatic</strong> <strong>resection</strong> surgery. Contin Educ<br />
Anaesth Crit Care Pain 2009;9:1-5.<br />
36.Abbasoglu O, Sayek I. Parenchymal transection with ultrasonic scalpel in<br />
<strong>liver</strong> <strong>resection</strong>. HPB (Oxford) 2003; 5:167-69.<br />
37.Izzo F, Di Giacomo R, Falco P et al. Efficacy of a haemostatic matrix for<br />
the management of bleeding in patients undergoing <strong>liver</strong> <strong>resection</strong>: results<br />
from 237 cases. Curr Med Res Opin 2008;24:1011-15.<br />
38.Little SA, Jarnagin WR, Dematteo RP et al. Diabetes is associated with<br />
increased perioperative mortality but equivalent long-term outcome after<br />
<strong>hepatic</strong> <strong>resection</strong> for colorectal cancer. J Gastrointest Surg 2002;6:88-94.<br />
39.Michalopoulos GK. Liver regeneration. J Cell Physiol 2007;213:286-300.<br />
40.Fisette A, Hassanain M, Metrakos P et al. High-dose insulin therapy<br />
reduces postoperative <strong>liver</strong> dysfunction and complications in <strong>liver</strong><br />
<strong>resection</strong> patients through reduced apoptosis and altered inflammation.<br />
J Clin Endocrinol Metab 2012;97:212-26.<br />
41.Jaeschke H. Molecular mechanisms of <strong>hepatic</strong> ischaemia-reperfusion<br />
injury and preconditioning. Am J Physiol Gastrointest Liver Physiol<br />
2003;284:G15-G26.<br />
42.Selzner N, Rudiger H, Graf R, Clavien P-A. Protective strategies against<br />
ischemic injury of the <strong>liver</strong>. Gastroenterology 2003;125:917-36.<br />
43.Koti RS, Seifalian AM, Davidson BR. Protection of the <strong>liver</strong> by ischaemic<br />
preconditioning: a review of mechanisms and clinical applications. Dig<br />
Surg 2003;20:383-96.<br />
44.Wendon J, Alexander GJM, Williams R. Cardiovascular monitoring and<br />
local blood flow. In: Williams R, Hughes RD, eds. <strong>Acute</strong> <strong>liver</strong> <strong>failure</strong>:<br />
improved understanding and better therapy. London: Miter Press; 1991:<br />
39-41.<br />
45.Wilkinson SP, Blendis LM, Williams R. Frequency and type of renal and<br />
electrolyte disorders in fulminant <strong>hepatic</strong> <strong>failure</strong>. BMJ 1974;1:186-89.<br />
46.Sanyal AJ, Boyer T, Garcia-Tsao G et al. for the Terlipressin Study Group.<br />
A randomized, prospective, double-blind, placebo-controlled trial for<br />
terlipressin for type 1 hepatorenal syndrome. Gastroenterology<br />
2008;134:1360-68.<br />
47.Rolando N, Gimson A, Wade J et al. Prospective controlled trial of<br />
selective parenteral and enteral antimicrobial regimen in fulminant <strong>liver</strong><br />
<strong>failure</strong>. Hepatology 1993;17:196-201.<br />
48.van den Broek MAJ, Olde Damink SWM, Dejong CHC et al. Liver<br />
<strong>failure</strong> after partial <strong>hepatic</strong> <strong>resection</strong>: definition, pathophysiology, risk<br />
factors and treatment. Liver Int 2008;28:767-80.<br />
49.Wu CC, Yeh DC, Lin MC et al. Prospective randomized trial of systemic<br />
antibiotics in patients undergoing <strong>liver</strong> <strong>resection</strong>. Br J Surg 1998;85:<br />
489-93.<br />
50.Patton H, Misel M, Gish RG. <strong>Acute</strong> <strong>liver</strong> <strong>failure</strong> in adults: an evidencebased<br />
management protocol for clinicians. Gastroenterol Hepatol<br />
2012;8:161-72.<br />
51.Fisher NC, Cooper MA, Hastings JG, Mutimer DJ. Fungal colonisation<br />
and fluconazole therapy in acute <strong>liver</strong> disease. Liver 1998;18:320-25.<br />
52.Heard J, Bellamy M. Liver <strong>failure</strong> in the intensive care unit. Trends Anaes<br />
Crit Care 2011;1:135-40.<br />
53.Chen Y, Liu BL, Shang B et al. Nutritional support in surgical patients<br />
with colorectal cancer. World J Gastroenterol 2011;17:1779-86.<br />
54.Fan ST, Lo CM, Lai E et al. Perioperative nutritional support in patients<br />
undergoing hepatectomy for hepatocellular carcinoma. N Engl J Med<br />
1994;331:1547-52.<br />
55.Bozzetti F. Rationale and indications for preoperative feeding of<br />
malnourished surgical cancer patients. Nutrition 2002;18:953-59.<br />
56.Awad S, Constantin-Teodosiu D, Macdonald IA, Lobo DN. Short-term<br />
starvation and mitochondrial dysfunction – a possible mechanism leading<br />
to postoperative insulin resistance. Clin Nutr 2009;28:497-509.<br />
57.Xu DZ, Lu Q, Deitch EA. Elemental diet-induced bacterial translocation<br />
associated with systemic and intestinal immune suppression. JPEN<br />
1998;22:37-41.<br />
58.Hu Q-G, Zheng Q-C. <strong>The</strong> influence of enteral nutrition in postoperative<br />
patients with poor <strong>liver</strong> function. World J Gastroenterol 2003;9:843-46.<br />
59.Ross D. Glutathione, free radicals and chemotherapeutic agents.<br />
Mechanisms of free-radical induced toxicity and glutathione dependent<br />
protection. Pharmacol <strong>The</strong>r 1988;37:231-49.<br />
60.Hammond CL, Lee TK, Ballatori N. Novel roles for glutathione in gene<br />
expression, cell death, and membrane transport of organic solutes. J<br />
Hepatol 2001;34:946-54.<br />
61.Demir S, Inal-Erden M. Pentoxifylline and N-acetylcysteine in <strong>hepatic</strong><br />
ischemia/reperfusion injury. Clin Chim Acta 1998;275:127-35.<br />
62.McKay A, Cassidy D, Sutherland F, Dixon E. Clinical results of N-<br />
acetylcysteine after major <strong>hepatic</strong> surgery: a review. J Hepatobiliary<br />
Pancreat Surg 2008;15:473-78.<br />
63.Kharazmi A, Nielsen H, Schiotz PO. N-Acetylcysteine inhibits human<br />
neutrophil and monocyte chemotaxis and oxidative metabolism. Int J<br />
Immunopharmacol 1988;10:39-46.<br />
64.Lee WM, Hynan LS, Rossaro L et al. for the <strong>Acute</strong> Liver Failure Study<br />
Group. Intravenous N-acetylcysteine improves transplant-free survival in<br />
early stage non-acetaminophen acute <strong>liver</strong> <strong>failure</strong>. Gastroenterology<br />
2009;137:856-64.<br />
65.Mumtaz K, Azam Z, Hamid S et al. Role of N-acetylcysteine in adults<br />
with non-acetaminophen-induced acute <strong>liver</strong> <strong>failure</strong> in a center without<br />
the facility of <strong>liver</strong> transplantation. Hepatol Int 2009;3:563-70.<br />
66.Wang JK, Truty MJ, Donohue JH. Remnant torsion causing Budd-Chiari<br />
syndrome after right hepatectomy. J Gastrointest Surg 2010;14:910-12.<br />
67.Gruttadauria S, Mandala’ L, Miraglia R et al. Successful treatment of<br />
small-for-size syndrome in adult-to-adult living-related <strong>liver</strong><br />
transplantation: single center series. Clin Transplant 2007;21:761-66.<br />
68.Umeda Y, Yagi T, Sadamori H, Matsuka H et al. Effects of prophylactic<br />
splenic artery modulation on portal overperfusion and <strong>liver</strong> regeneration<br />
in small-for-size graft. Transplantation 2008;86:673-80.<br />
69.Singhal A, Goyal N, Gupta VV. Delayed splenic artery occlusion for<br />
treatment of established small-for-size syndrome after partial <strong>liver</strong><br />
transplantation. Liver Transpl 2009; 15:1381-82.<br />
70.Mazzaferro V, Regalia E, Doci R et al. Liver transplantation for the<br />
treatment of small hepatocellular carcinomas in patients with cirrhosis.<br />
N Engl J Med 1996;334:693-99.<br />
71.Hughes RD, Mitry RR, Dhawan A. Current status of hepatocyte<br />
transplantation. Transplantation 2012;93:342-47.<br />
72.Chari RS, Collins BH, Magee JC et al. Brief report: Treatment of <strong>hepatic</strong><br />
<strong>failure</strong> with ex vivo pig-<strong>liver</strong> perfusion followed by <strong>liver</strong> transplantation.<br />
N Engl J Med 1994;331:234-37.<br />
73.Sutcliffe RP, Antoniades CG, Deshpande R et al. Liver and<br />
Pancreatobiliary Surgery with Liver Transplantation. Oxford University<br />
Press 2010.<br />
74.van de Kerkhove MP, de Jong KP, Rijken AM et al. MARS treatment in<br />
posthepatectomy <strong>liver</strong> <strong>failure</strong>. Liver International 2003;23(suppl 3):44-51.<br />
75.Chiu A, Chan LM, Fan ST. Molecular adsorbent recirculating system<br />
treatment for patients with <strong>liver</strong> <strong>failure</strong>: the Hong Kong experience. Liver<br />
Int 2006;26:695-702.<br />
76.Sauer IM, Goetz M, Steffan I et al. In vitro comparison of the molecular<br />
adsorbent recirculation system (MARS) and single-pass albumin dialysis<br />
(SPAD). Hepatology 2004;39:1408-14.<br />
Chris Jones Clinical Research Fellow<br />
drchrisnjones@yahoo.co.uk<br />
Leigh Kelliher Clinical Research Fellow<br />
Colin Bigham Locum Consultant in Anaesthesia and <strong>Intensive</strong><br />
Care<br />
Nial Quiney Consultant in Anaesthesia and <strong>Intensive</strong> Care<br />
Royal Surrey County Hospital NHS Foundation Trust<br />
140<br />
Volume 14, Number 2, April 2013 <strong>JICS</strong>