Volume 7 Number 2 July 2006 - JICS - The Intensive Care Society
Volume 7 Number 2 July 2006 - JICS - The Intensive Care Society
Volume 7 Number 2 July 2006 - JICS - The Intensive Care Society
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong><br />
<strong>Volume</strong> 7<br />
<strong>Number</strong> 2<br />
<strong>July</strong> <strong>2006</strong><br />
Price £15<br />
● Lessons Learned From <strong>The</strong> London Bombings<br />
● Organ Donation - Time For A Rethink?<br />
● <strong>The</strong> ACUTE Initiative<br />
● Best Interests - Who Decides?<br />
This issue is supported by<br />
an educational grant from<br />
Lilly Critical <strong>Care</strong><br />
● Tight Glycaemic Control<br />
● Pericardial Tamponade
Journal produced by <strong>The</strong> <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>.<br />
29B Montague Street, London, WC1B 5BW.<br />
Tel: 020 7291 0690 Fax: 020 7580 0689 Website: www.ics.ac.uk<br />
Editor: Dr. Bruce Taylor, Consultant in <strong>Intensive</strong> <strong>Care</strong> and Anaesthesia.<br />
Department Of Critical <strong>Care</strong> Medicine, Queen Alexandra Hospital, Cosham, Portsmouth, Hampshire PO6 3LY.<br />
Email: bruce.taylor@porthosp.nhs.uk<br />
Editorial Assistant: Jemma Regan Email: jemma@ics.ac.uk
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Editorial 3<br />
Contents<br />
Editorial / President’s Report<br />
03 Editorial B Taylor<br />
04 President’s Report A Batchelor<br />
Meetings Reports<br />
06 Annual Spring Meeting Report T Jackson<br />
09 Annual Spring Meeting Exhibition Report M Moore<br />
10 Poster Presentation Winner<br />
11 SKINT Workshop D Goldhill<br />
Research & Development Update<br />
12 Tracman Update L Morgan<br />
Surveys & Audits<br />
13 Designated Consultants for the Inter-Hospital G Allen, P Farling<br />
Transfer of Patients with Brain Injury – a survey of B A Mullan<br />
practice among neurosurgical units in the UK and Ireland<br />
16 Tight Glycaemic Control in Scottish ICUs E S Jack, M J E Neil<br />
19 An Audit of Hypoglycaemia in Critical <strong>Care</strong> A N Thomas<br />
E M Boxall<br />
G Sabbagh<br />
J Eddleston<br />
T Dunne, A Stevens,<br />
P Murphy<br />
Original Articles<br />
23 Best Interests -Who Decides? C Danbury<br />
25 <strong>The</strong> Point of Death J Radcliffe Richards<br />
27 Pakistan Earthquake A Charters<br />
29 Not Left to Your Own Devices S Ludgate<br />
30 Diagnosis and Management of PVL-associated C Day<br />
Staphylococcal Infections<br />
32 Reflections on the clinical learning points from the PJ Shirley, M Thavasothy<br />
Royal London Hospital <strong>Intensive</strong> <strong>Care</strong> Unit D McAuley, D Kennedy<br />
following <strong>July</strong> 7th 2005 terrorist attacks<br />
G Mandersloot<br />
V Verma, M Healy<br />
35 Cardiac Tamponade Following Insertion of An R Davis, M B Walker<br />
Implantable Defibrillator<br />
37 Bedside Ultrasound of Pleural Effusions by UK D Y Ellis<br />
Intensivists; How Much Training Do we Need? R M Grounds<br />
A Rhodes<br />
38 Update on the ACUTE initiative G Perkins<br />
40 Lemmingaid - Kafka and the Clinical Director Wood & Trees<br />
(Metamorphosis)<br />
CATmaker Reviews<br />
42 Rescue Angioplasty vs Repeat Thrombolysis in A Gershlick<br />
Acute MI?<br />
44 Furosemide and albumin improve oxygenation in D MacNair<br />
a small group of patients with Acute Lung Injury B H Cuthbertson<br />
46 Corticosteroids in late ARDS K Steinberg<br />
48 Non-invasive ventilation in patients with acute J L Moran<br />
cardiogenic pulmonary oedema: a meta-analysis<br />
Manpower<br />
50 Manpower Census R Kishen<br />
Correspondence<br />
51 Aussie Training – a Perspective from Down-Under S Blakeley<br />
52 National Critical Incidents Reporting Scheme J Mitchell<br />
52 National Critical Incidents Reporting Scheme A N Thomas<br />
53 Guidelines for clearing suspected spinal injury in E Thomas<br />
unconscious patients<br />
Miscellaneous<br />
55 Industry Members 60 Secretariat Report<br />
56 Council Members 62 Meetings Diary<br />
58 Advertising and Sponsorship Rate Card<br />
<strong>JICS</strong> Editorial Board<br />
Bruce Taylor (Editor)<br />
Jemma Regan (Editorial Assistant)<br />
Carl Waldmann<br />
David Goldhill<br />
CAT reviews;<br />
Chris Cairns<br />
Brian Cuthbertson<br />
Sheena Hubble<br />
<strong>The</strong> Editor writes<br />
It is with great sadness that we heard of the recent death of another<br />
popular and highly respected colleague. We hope to include a tribute<br />
to Fiona Clarke in the next edition – which will be the second time in<br />
just over a year that that we have reflected on the death of a young,<br />
talented intensivist who, for reasons that remain enigmatic, chose to<br />
end their own life. Such a devastating loss causes us to stop and<br />
think; the common characteristic in both instances seems to be that<br />
even close colleagues didn’t see it coming – which inevitably leads us<br />
all to think about our own colleagues, and whether we should have<br />
concerns about their (and perhaps even our own) wellbeing.<br />
It also at least raises the question of whether we are as resilient about<br />
the effects of the job that we do as we might like to think we are. You<br />
don’t choose a career in intensive care unless you enjoy a challenge,<br />
and the unpredictably of the work that goes with the territory.<br />
However, an integral part of the work also includes difficult decisions,<br />
and the management of situations that can be both harrowing and<br />
distressing for all involved. Asking colleagues how they cope with<br />
such challenges produces responses ranging between ‘I don’t do<br />
stress’ from some of the more outwardly robust, to that of a capable<br />
and enthusiastic SpR trainee who decided not to pursue their<br />
preferred career because they felt unable to handle the emotional<br />
pressures that come with the job. Most of us probably fit somewhere<br />
between these extremes, and have developed our own strategies for<br />
coping with the ups and downs of our everyday work; there will be few<br />
of us who have not accumulated a private, personal collection of<br />
memories that will always remain with us.<br />
When we spend so much of our time caring for patients who are<br />
critically ill because of accidents, bad luck or complications, do we<br />
really walk away as unscathed as we would like to believe? I suspect<br />
not. Most colleagues (if persuaded to discuss this largely ‘no go’<br />
area) admit to having rather distorted perspectives about things<br />
like accident risks, family health and life expectancy, and many<br />
acknowledge that these do affect their worries about everyday<br />
activities. It seems that we cope in different ways – from fastidious<br />
fitness training to music-making, skiing to scuba diving. It also seems<br />
clear that the peer support from working in a cohesive team plays an<br />
important part in attenuating the effects of difficult days. Within the<br />
‘bell curve’ distribution of personalities, it is perhaps inevitable that<br />
there will be some who will be at the vulnerable end, and we can only<br />
speculate on what influences the development of depressive illness<br />
that leads them to end their life – but it seems clear that we should all<br />
do everything that we can to identify colleagues who may be at risk,<br />
and to help them in any way that we can.<br />
Two articles in this edition provide us with retrospective commentary<br />
on other, tragic unexpected events, with an analysis of the clinical<br />
lessons learned from the <strong>July</strong> London bombings and of the huge<br />
practical difficulties that had to be tackled by volunteers in the<br />
aftermath of the Pakistan Earthquake. Those of you who attended<br />
the excellent Gilston Lecture at the Spring Meeting will have been<br />
impressed by the science that underpins the concept of intensive<br />
insulin therapy, and two articles are included which focus on its<br />
implementation and potential complications in intensive care practice.<br />
Also included is an analysis of the implications of the latest legal ruling<br />
in the Baby MB case, a thought-provoking perspective on organ<br />
donation, updates on PVL staphylococcal infection, the ACUTE<br />
initiative, and medical device malfunction. And for those of you who<br />
may be considering taking on the role of Clinical Director, Wood and<br />
Trees offer some advice that you may wish to consider!<br />
B Taylor<br />
bruce.taylor@porthosp.nhs.uk<br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
4<br />
Report<br />
President’s Report<br />
President -<br />
Anna Batchelor<br />
It’s hard to believe that a year has gone by already.<br />
This is a great job and I am really enjoying it, but<br />
it’s hard work! I am writing this in a hotel room in<br />
London, having got the 0718 train this morning<br />
from Newcastle and attended the Critical <strong>Care</strong><br />
Stakeholders forum (CCSF) meeting, after which<br />
I had tea and a “catch up” with Keith Young from<br />
the Department of Health and Jane Eddleston,<br />
the Department advisor for Critical <strong>Care</strong>. When<br />
ensconced in my room (I am rapidly becoming an<br />
expert on the hotels of Bloomsbury) I did about 2<br />
hours of electronic “paper work” and dealing with<br />
emails before getting down to writing this report.<br />
Tomorrow I am having breakfast with Kathy Rowan<br />
from ICNARC, followed at 1030 by chairing the<br />
Education and Competence group for the assistant<br />
critical care practitioners’ stream of New Ways of<br />
Working in Critical <strong>Care</strong>, and late afternoon hoping<br />
to make the Royal College of Anaesthetists Critical<br />
<strong>Care</strong> Committee. With luck and a following wind I<br />
will get the 1700 train and be home about 2015 just<br />
in time to put my baby to bed. I will have to miss the<br />
Royal College of Physicians Critical <strong>Care</strong> Committee<br />
meeting tomorrow morning unless I can clone myself<br />
before then. Cloning would actually be very useful<br />
because if I had stayed in Newcastle today I would<br />
have done a 0900 to 2100 day in theatre which of<br />
course has been left to my colleagues back at the<br />
ranch. Last week had just 1 day away and next<br />
week is similar, but the following one I am away 4<br />
days. <strong>The</strong> representation work increases year on<br />
year, a reflection of the value placed on the <strong>Society</strong>’s<br />
advocatory role for Critical <strong>Care</strong> clinicians. You<br />
could ask why more is not done on email, but<br />
sometimes meeting face to face just gets the job<br />
done quicker and sometimes interesting things<br />
happen at meetings - but more of that later.<br />
Saxon Ridley has now left Council and Jane Harper<br />
has been elected to fill my former place. I am<br />
particularly pleased that I have replaced by another<br />
woman - for some reason very few stand for<br />
election. I am sure Jane will be a useful addition<br />
to the <strong>Society</strong> and as Chair of the Network Medical<br />
Leads will bring the strands back together which I<br />
hope will lead to a stronger force for Critical <strong>Care</strong>.<br />
At the CCSF today we heard that several networks<br />
are struggling to find funding and some have just<br />
ceased to be. This is a great pity as networking is<br />
something intensivists do well and the benefits are<br />
there for commissioners to see if only they would<br />
take the trouble to look. I very much hope that the<br />
combined efforts of the <strong>Society</strong>, the Medical Leads<br />
and the CCSF may be able to help these networks<br />
get back up and running.<br />
<strong>The</strong> Spring meeting in Harrogate went well, and we<br />
still have the Focus meeting on Transplantation, the<br />
Trainees’ Meeting and State of the Art to come. This<br />
year we are also introducing some small seminars in<br />
the new College on Clinical Excellence Awards,<br />
Education and Management, so look out for those<br />
too. We are very aware that access to study leave<br />
may be less generous than previously and that you<br />
need good value from the meetings you do attend,<br />
so I hope the <strong>Society</strong> can deliver this.<br />
<strong>The</strong> National Burn <strong>Care</strong> Review is coming to a<br />
conclusion and Specialised Commissioners are<br />
working with providers to fit their local service into<br />
the Centre/Unit/Facility model. I was concerned to<br />
see that there were apparently less beds for burns<br />
critical care in the Jan 06 KH03a compared to Jan<br />
05, and we must guard against the possibility of<br />
having less provision for burn critical care at the end<br />
of this review than we had at the beginning. I would<br />
be keen to hear of any problems colleagues have<br />
experienced.<br />
<strong>The</strong> New Ways of Working Programme continues<br />
and the Advanced Critical <strong>Care</strong> Practitioner<br />
Education and Competence Framework which is<br />
currently going through the Government ‘Gateway’<br />
should be available in both hard copy and<br />
electronically very soon. I hope you will look at it<br />
and feed back. I strongly believe we need to look<br />
towards practitioners who are appropriately trained<br />
and supervised helping us with the service delivery<br />
gap which will be left by Modernising Medical<br />
<strong>Care</strong>ers and the EWTD. As with many things with<br />
the DH, there is of course no money to continue the<br />
programme and fund second wave pilots. I hope the<br />
framework is strong enough to enable the production<br />
of a high quality transferable practitioner workforce.<br />
Having completed that we are now working on the<br />
Assistant Practitioner documentation and this should<br />
be available in the late summer.<br />
We are hoping that NICE will be able to take on<br />
“<strong>The</strong> <strong>Care</strong> of the Unexpectedly Acutely Ill Patient<br />
in Hospital” as a fast track programme. <strong>The</strong> initial<br />
vibes are good and we await ministerial approval.<br />
NICE are a powerful body whose edicts must be<br />
followed. Unfortunately we cannot tell them what to<br />
put in their guidance but we hope that the results of<br />
the NCEPOD report along with the considerable<br />
amount of expertise now available will result in a<br />
process that leads to benefits for patients.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Report continued 5<br />
<strong>The</strong> Critical <strong>Care</strong> Contingency Planning Group<br />
continues to work on the complicated issues that<br />
may arise from an unexpected sudden increase in<br />
demand for intensive care beds, and is due to<br />
produce the first draft guidance in the near future.<br />
<strong>The</strong> group wishes it to be clear that this should be<br />
regarded as ‘work in progress’ and that feedback<br />
and suggestions for future amendments will be<br />
welcomed and encouraged.<br />
Professor David Menon continues to do excellent<br />
work representing the specialty concerning the<br />
Human Tissue Act, Mental Capacity Act, the Clinical<br />
Trials Directive, and the Data Protection Act. <strong>The</strong>se<br />
are very complex documents and I am grateful to<br />
David for his diligence and expertise in guiding us<br />
through these issues.<br />
At the beginning I said sometimes meetings can be<br />
interesting... ...last week’s away day proved to be<br />
very unexpectedly so. You may have heard of Skills<br />
for Health, a Sector Skills Council for Health - one<br />
of 27 such projects covering the whole UK economy<br />
(that’s plumbers, electricians and just about<br />
everyone with the possible exception of politicians).<br />
This body have been in existence for some time,<br />
writing competences (sic) for all health care workers<br />
including doctors. It was clear at the meeting that<br />
many people had just woken up to the existence of<br />
this organisation and they were not too impressed<br />
with the product. You may wish to look at the<br />
website http://www.skillsforhealth.org.uk/. I would<br />
be very grateful for feedback which I can add to that<br />
I have already provided. For those of you who<br />
cannot face this I will just tell you there are 92<br />
competences for Emergency Urgent and Scheduled<br />
<strong>Care</strong>, of which giving an anaesthetic is one and<br />
taking a blood sample is another. Quite why out<br />
of only 92, removing organs deserves a whole<br />
competency I will leave you to guess.<br />
So that’s it, a few days in the life of the ICS<br />
President, till the next issue TTFN.<br />
A Batchelor<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
6<br />
Meeting Report<br />
Harrogate ICS Spring Meeting<br />
<strong>2006</strong> Report<br />
T Jackson<br />
Harrogate was once again chosen to host the<br />
Spring ICS meeting this year. Having enjoyed the<br />
successful SKINT meeting, delegates gathered amid<br />
the decidedly changeable weather for the two day<br />
conference. A packed programme boasted parallel<br />
sessions with such diverse themes as trauma and<br />
climate change (ironic in the context of the change<br />
of weather from Monday to Tuesday!) and promised<br />
an array of expert speakers.<br />
<strong>The</strong> Harrogate International Centre has developed<br />
since the last ICS meeting, with the addition a year<br />
ago of the Queens Suite adding to the flexible<br />
conference facilities. <strong>The</strong> first session here centred<br />
on trauma, starting with Prof Monty Mythen’s<br />
presentation of the pitfalls in evidence for volume<br />
resuscitation strategies based on certain well-quoted<br />
trials. <strong>The</strong> general consensus was carried into the<br />
questions, namely that minimal resuscitation should<br />
not be mistakenly interpreted as under-resuscitation.<br />
Prof Pete Giannoudis developed a comprehensive<br />
journey through the genetic basis of trauma<br />
responses, from the history of trauma management<br />
strategies to the future expectations of genetic<br />
markers of inflammatory responses. <strong>The</strong> session<br />
was concluded with a poignant reminder of the<br />
recent London terrorist bombs from Dr Hugh<br />
Montgomery, with the chilling message that many<br />
of our colleagues in the capital knew a terrorist<br />
attack was a certainty, and the place that drills and<br />
preparation played in the response to those attacks.<br />
Having watched the events unfold in the media that<br />
day, as many of us will remember, it was fascinating<br />
to hear first hand experience of the dynamics of<br />
casualty flows and intensive care activity at such a<br />
testing time.<br />
<strong>The</strong> parallel session in the main auditorium<br />
concerned outreach issues, with presentations on<br />
the lack of evidence for efficacy of outreach in the<br />
light of the antipodean MERIT study, the spectrum<br />
of musculoskeletal dysfunction in the ICU setting<br />
and some potential avenues for impacting on these<br />
difficult conditions, and discussion of the commonly<br />
applied ‘track and trigger’ scoring systems applied<br />
to patients at risk of critical illness.<br />
<strong>The</strong> refreshment break provided the first<br />
opportunity to view the range of industry exhibitors,<br />
although there was some debate as to who would<br />
pluck up courage to visit the rectal tube vendors<br />
with confidence!<br />
<strong>The</strong> second session of the day fell to a choice of<br />
matters nephrological or scanning the horizon for<br />
areas of forthcoming impact on the critical care<br />
world. <strong>The</strong> former, began with a talk from Dr<br />
Andrew Davenport concerning the haemodynamic<br />
instability associated with renal replacement therapy.<br />
<strong>The</strong>re were some useful insights into methods of<br />
minimising this potentially serious complication.<br />
Dr Andy Lewington from Leeds spoke on the<br />
interplay between nephrologists and intensivists in<br />
the management of the critically ill patient with renal<br />
failure, although it was clear that not all shared his<br />
experience of joint care. Following on from this was<br />
Prof Didier Payen from Paris presenting his work on<br />
whether early renal replacement has any impact on<br />
the progression of organ dysfunction in sepsis.<br />
On the background of various theories why<br />
haemofiltration might be effective was clear<br />
evidence to the contrary, however he ended by<br />
suggesting that high-volume filtration may offer<br />
some as yet unproven benefit.<br />
Lunch was followed by an intriguing look at how<br />
climate change may affect the spectrum of infectious<br />
diseases presenting to UK ICUs. This was put into<br />
context by a talk from Prof Ken Carslaw from Leeds<br />
University’s school of Earth and Environment,<br />
detailing how the evidence for global warming has<br />
developed over the years, and predictions of how<br />
our impact on the climate is likely to progress. With<br />
increasing coverage of this field in the media, it was<br />
interesting to hear expert opinion on a politically ‘hot’<br />
topic. Following this, Dr Philip Stanley presented<br />
illustrative cases of diseases associated with foreign<br />
travel which may already necessitate ICU admission<br />
in a small group of individuals, a theme which was<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Meeting Report continued 7<br />
developed by Prof Jon Cohen, who discussed<br />
reasons why infectious diseases with which we are<br />
unfamiliar may become more commonplace in the<br />
face of a climate more associated with North African<br />
countries. He used the examples of West Nile virus<br />
and Hantavirus to illustrate how climate change can<br />
have a direct impact on disease presentation.<br />
<strong>The</strong> highlight of the afternoon was the Gilston<br />
Lecture, where Prof Greet Van den Berghe<br />
presented a very comprehensive account of her<br />
compelling research into glycaemic control in<br />
intensive care.<br />
<strong>The</strong>re was a noticeable paucity of delegates at the<br />
pre-conference coffee on day two. I’m not sure if<br />
this was related to over-indulgence at the dinner<br />
dance the night before, or to casualties of the<br />
fun-run earlier that morning.<br />
<strong>The</strong> Fun Run - raring to go...!<br />
Day two promised further interesting topics, and I<br />
began to wish I could clone myself and attend both<br />
parallel sessions. <strong>The</strong> aspects of training and<br />
revalidation were received well, particularly in the<br />
current climate of modernising medical careers<br />
and contract issues. However, I elected to join the<br />
neurosciences session. Dr Peter Andrews<br />
presented an overview of potential advances in<br />
neurocritical care, including the disappointing results<br />
of several important trials, suggesting alternative<br />
ways of assessing outcome to improve the yield of<br />
trials in the future. He also concentrated on the role<br />
of decompressive craniectomy in the management of<br />
traumatic brain injury, and ended with outlines of<br />
agents which may show some promise, including<br />
statins which are being assessed for use in<br />
vasospasm related to subarachnoid haemorrhage.<br />
Professor Carl Hendrik Nordstrom presented the<br />
theory and practice of the Lund approach to<br />
managing traumatic brain injury, which differs<br />
from the standard North American teaching on<br />
maintenance of cerebral perfusion pressure. He<br />
described the protocol for manipulating capillary<br />
hydrostatic pressure, including the use of metoprolol<br />
and clonidine accepting cerebral perfusion pressures<br />
down to 50mmHg. It was clear from the lively<br />
discussion which was initiated (but sadly not<br />
concluded due to time constraints) that neither Lund<br />
nor North American approaches suit all brain-injured<br />
patients. <strong>The</strong> session was completed by Dr Steve<br />
Wilson with a round-up of the evidence base (or lack<br />
thereof) for various elements of the management<br />
of traumatic brain injury. <strong>The</strong> most compelling<br />
evidence seemed to be from the TARN database<br />
study suggesting significant reduction in mortality in<br />
patients managed in a neurosurgical centre,<br />
although Dr Wilson presented some obvious<br />
caveats.<br />
Next, I attended the session on trainee issues.<br />
This caught my eye largely for the echo talk, and<br />
didn’t disappoint. It was heartening to hear Dr<br />
Robert Orme talk of his quest to become trained in<br />
echocardiography, although this personal account<br />
also reinforced what I and many colleagues have<br />
found, which is that it isn’t easy to acquire the<br />
necessary exposure to train and then remain<br />
validated in such techniques. Dr Orme also<br />
imparted some useful resources for anyone<br />
interested in achieving echo competence. This<br />
was followed by an interesting presentation by Mrs<br />
Carole Boulanger detailing her metamorphosis from<br />
experienced intensive care sister to advanced critical<br />
care practitioner. It is clear both from her talk and<br />
some of the questions that there is some unease at<br />
the origin of these new roles from various quarters,<br />
but as manpower issues become more prevalent,<br />
ACCPs may well become more commonplace.<br />
Delegates assemble in the lecture area<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
8<br />
Meeting Report continued<br />
<strong>The</strong>re then followed a pair of lunchtime symposia.<br />
I was surprised that nobody seemed to adopt the<br />
Latin derivation of this term (a drinking party) and<br />
instead we all tucked into our packed lunches with<br />
as little rustling as possible, so as to hear the<br />
industry sponsored presentations. <strong>The</strong> Queen’s<br />
Suite auditorium hosted two presentations regarding<br />
remifentanil based sedation regimes. Firstly, Dr Atul<br />
Kapila described the experience in Reading of the<br />
introduction of a sedation protocol and subsequent<br />
audit cycles, highlighting the issues surrounding<br />
education for the nursing staff. This was followed by<br />
Dr Wolfram Wilhelm from Lunen in Germany, who<br />
presented his unit’s experience of more widespread<br />
use of remifentanil in ICU. In the parallel lunchtime<br />
session Dr Duncan Wyncoll summarised the results<br />
of the XPRESS study, an investigation into the<br />
administration of Activated Protein C with or without<br />
heparin.<br />
into the breach at very short notice, describing the<br />
‘Lo-Trach’ endotracheal tube and its role in<br />
minimising the impact of ventilator associated<br />
pneumonia, for which he presented a compelling<br />
argument. Following this, Prof Van den Berghe<br />
again took to the platform to reprise her glycaemic<br />
control research, this time including discussion of<br />
some of the studies which have disagreed with her<br />
work, and answering some of the criticisms that<br />
have been levelled at it. Finally, Dr Sapsford also<br />
returned, to discuss the myths and developments in<br />
arrhythmia management, centring on various rhythm<br />
disturbances and the emerging role of<br />
radiofrequency ablation techniques to provide more<br />
long-term relief. Of more relevance to critical care<br />
were his discussion of atrial fibrillation and the<br />
evolution of the rate versus rhythm control debate,<br />
which currently favours the former (probably!).<br />
<strong>The</strong> meeting was a resounding success with some<br />
very stimulating presentations from a wide range of<br />
nationally and internationally renowned speakers.<br />
Thanks must go to Prof Mark Bellamy and Ms Judith<br />
Thornton for their work in developing the programme<br />
and also for the hard work put in by the ICS<br />
secretariat and meetings committee. Here’s to a<br />
repeat performance next year at Bournemouth!<br />
As usual, the poster presentations attracted lots of interest<br />
After lunch, there were parallel sessions on<br />
cardiology and IT in critical care. <strong>The</strong> cardiology<br />
session began with Echoardiography in ICU<br />
presented by Dr Sean Bennett with a<br />
complementary view to Dr Orme earlier; he<br />
presented several clinical examples of how echo<br />
diagnosis can affect ICU management. <strong>The</strong> second<br />
presentation was from Dr Rob Sapsford regarding<br />
the management of acute coronary syndromes,<br />
and brought together some of the changes in<br />
nomenclature and investigations which have evolved<br />
over the last few years. Rounding off the session<br />
was a presentation by Prof Alistair Hall on<br />
biomarkers of coronary disease, introducing the<br />
markers which can further refine the management of<br />
patients presenting with acute coronary syndromes,<br />
and the future for multi-marker profiling.<br />
<strong>The</strong> final session of the day centred on myths<br />
and new developments in critical care. Dr Duncan<br />
Wyncoll performed magnificently having stepped<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Meeting Report continued 9<br />
Exhibition Report<br />
M Moore<br />
Harrogate International Centre held this year’s<br />
Spring <strong>2006</strong> Conference on 22 nd - 24 th May, which<br />
included the Skills for Intensivists Workshops and<br />
the Annual Spring <strong>2006</strong> Meeting, successfully filling<br />
the trade hall with 49 exhibitors with a mixture of<br />
Corporate, Company and non industry members.<br />
After hours of build up, constructing the stands for<br />
the exhibition, we finally produced a trade hall with<br />
some amazing purpose built stands. AstraZenca’s<br />
stand was one of the impressive designs that<br />
appeared very appealing to the delegates with<br />
interactive technology and a modernised style.<br />
Although the weather was clearly not on our side<br />
throughout, delegates still arrived first thing to attend<br />
this year’s event. Everything ran smoothly as<br />
delegates weaved through the whole venue covering<br />
the exhibition hall and both main sessions.<br />
Tuesday evening mellowed down to the sound of<br />
Jazz at our Annual Dinner and Dance accompanied<br />
by appetising food and drink and a lively atmosphere<br />
on the dance floor.<br />
It was a bright and early start on Wednesday<br />
morning for those who took part in the <strong>Intensive</strong><br />
<strong>Care</strong> Foundation Fun Run around the muddy fields<br />
of Harrogate. <strong>The</strong>re was just enough time for a<br />
quick change, then it was back to the Centre for the<br />
final day of educational and research sessions.<br />
<strong>The</strong> ICS would like to thank all exhibitors and<br />
sponsors for contributing to this event and their<br />
continuing support throughout the years. We greatly<br />
appreciate the involvement from our Industry<br />
Members and look forward to welcoming new<br />
associates to our Corporate and Company<br />
Membership Schemes.<br />
Thank you to the following exhibitors:<br />
Abbott Point of <strong>Care</strong><br />
Anmedic UK Ltd<br />
Arrow International UK Ltd<br />
AstraZeneca UK Ltd<br />
B. Braun Medical Ltd<br />
Beaver Medical<br />
BOC Medical Plc<br />
Cardiac Services<br />
Codan Ltd<br />
ConvaTec Ltd<br />
Cook UK<br />
Delta Surgical Ltd<br />
DOT Medical<br />
Dräger Medical UK Ltd<br />
Edwards Lifesciences Ltd<br />
Eli Lilly & Co Ltd<br />
Eumedica Pharmaceuticals<br />
Fresenius Kabi Ltd<br />
Fresenius Medical <strong>Care</strong><br />
Fukuda Denshi UK<br />
Gambro Hospal Ltd<br />
GE Healthcare<br />
Gilead Sciences Ltd<br />
GlaxoSmithKline Ltd<br />
Henleys Medical Supplies Ltd<br />
IMPACT<br />
Inspiration Healthcare Ltd<br />
Johnson & Johnson Wound Management<br />
Kapitex Healthcare Ltd<br />
Lidco Ltd<br />
Maquet Ltd<br />
Norvartis Medical Nutrition<br />
Novo Nordisk Ltd<br />
Pfizer Ltd<br />
Pulsion Medical<br />
Respironics UK Ltd<br />
Roche Diagnostics Ltd<br />
SLE Ltd<br />
Smiths Medical<br />
SonoSite Ltd<br />
Spacelabs Medical UK Ltd<br />
Teleflex Medical Systems Ltd<br />
<strong>The</strong> CESAR Trial<br />
TracMan Trial<br />
Trumpf Medical Systems Ltd<br />
Viasys Healthcare<br />
Vital Signs Ltd<br />
Wisepress Ltd<br />
Zeneus Pharma Ltd<br />
M Moore<br />
Events & Marketing Administrator<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
10<br />
Meeting Report continued<br />
Spring <strong>2006</strong> Clinical Practice Poster Presentation Winner<br />
Congratulations to:<br />
Dr Rachid Berair and Dr Michael Lim<br />
Audit on physician prescription of sedation scores in mechanically ventilated patients<br />
Spring <strong>2006</strong> Research Poster Presentation Winner<br />
Congratulations to:<br />
Dr Elaine Harrison, Dr Samuel Pambakian, Dr Justin Woods and Dr William Fellingham<br />
Comparison between pulmonary artery catheter and Vigileo – FloTrac<br />
<strong>The</strong> <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong><br />
Annual Spring <strong>2006</strong> Meeting<br />
Delegate Badge Prize Draw Winner<br />
Congratulations to Dr Paul Knight from<br />
Calderdale Royal Hospital, whose badge was<br />
drawn out to receive the £25 book token.<br />
We thank all those delegates who return their<br />
badges at the end of each conference.<br />
This ensures the badge holders are re-used at<br />
future events and helps to keep costs down.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Meeting Report continued 11<br />
SKINT - Skills for Intensivist Workshops<br />
D Goldhill<br />
<strong>The</strong> workshops have now been running for two<br />
years and have all been held in conjunction with<br />
one of the ICS meetings. <strong>The</strong> equipment-based<br />
workshops are designed to be practical hands-on<br />
sessions providing an opportunity to work with a<br />
range of equipment and to get first-hand advice<br />
from experts.<br />
<strong>The</strong> ultrasound-guided vascular access workshop<br />
At the recent conference in Harrogate four<br />
workshops were held. <strong>The</strong>y were;<br />
1. Advanced ventilation:<br />
This year the workshops was expanded and<br />
started in the morning and ran until late afternoon.<br />
Topics covered included non-invasive ventilation,<br />
COPD/asthma, automated weaning, prone<br />
entilation, lung recruitment and oscillation. <strong>The</strong>re<br />
was the opportunity to work with machines from<br />
Drager, Respironics. Maquet, Viasys and GE.<br />
2. Percutaneous tracheostomy:<br />
This popular workshop was based around<br />
Cook and Portex kits with key lectures and<br />
demonstrations using models, bronchoscopes<br />
and the tracheostomy kits themselves.<br />
<strong>The</strong> workshops took place on Monday 23 rd May,<br />
the day before the main conference. Most places<br />
were taken and feedback from all of them has been<br />
excellent. As well as these workshops, Intracranial<br />
Pressure Monitoring has been run several times.<br />
Future planned workshops are on Non-invasive<br />
Cardiac Output Monitoring and Echocardiography.<br />
<strong>The</strong>ir success is due to three things. Firstly the<br />
enthusiasm and hard work of individuals who<br />
devised and organised the individual workshops.<br />
For Ventilation this was Peter Macnaughton, for<br />
Percutaneous Tracheostomy Alf Shearer, for<br />
Ultrasound Andy<br />
Bodenham, for Intracranial<br />
Pressure Monitoring Carl<br />
Waldmann and for the<br />
PBL Monty Mythen.<br />
<strong>The</strong>se individuals have<br />
been joined by a team of<br />
helpers who have freely<br />
given of their time and<br />
expertise for little reward.<br />
<strong>The</strong> percutaneous<br />
tracheostomy workshop<br />
<strong>The</strong> final element in the<br />
package is the support<br />
of industry who have<br />
supplied the equipment<br />
and educational materials.<br />
<strong>The</strong>se workshops are a superb opportunity to learn<br />
or revise some essential skills, and to play with the<br />
necessary toys. <strong>The</strong>y will be run again. If you want<br />
to help with any of the current workshops, or if you<br />
have ideas for workshops you would like to run,<br />
please contact the ICS.<br />
D Goldhill<br />
SKINT_Meister<br />
3. Ultrasound-guided vascular access:<br />
This workshop has been run on several previous<br />
occasions. ‘Phantoms’ and volunteers allowed<br />
the participants to get excellent training in<br />
ultrasound anatomy, needle visualisation and<br />
techniques for vascular access. <strong>The</strong> session<br />
ended with an introduction to echocardiography.<br />
4. Problem-based clinical scenarios (PBL):<br />
This was a new innovation consisting of an<br />
interesting review of current sepsis treatment<br />
options followed by an interactive discussion of<br />
three case presentations. This was a marvellous<br />
opportunity to learn from experts about their<br />
approach to real clinical cases.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
12<br />
Research & Development Update<br />
TracMan: Tracheostomy<br />
Management in Critical <strong>Care</strong><br />
Update<br />
Dear All,<br />
Over 60 <strong>Intensive</strong> <strong>Care</strong> Units (ICUs) around the UK are now collaborating in the TracMan Trial with a total of<br />
335 patients recruited (at 25 May). Terrific effort from the ICS community we think!<br />
Our top recruiting ICUs January to April <strong>2006</strong> are:<br />
Month<br />
Jan 06<br />
Feb 06<br />
Mar 06<br />
Apr 06<br />
Hospital and Lead Consultant/Nurse<br />
Whiston Hospital, Prescot (Dr R MacMillan)<br />
Southampton General Hospital (Dr T Woodcock & Mrs K de<br />
Courcy-Golder)<br />
Joint top recruiters:<br />
Derriford Hospital, Plymouth (Dr P D Macnaughton & Mrs N Donlin)<br />
St Thomas Hospital, London (Dr D Wyncoll & Mr T Sherry)<br />
Southampton (Dr T Woodcock & Mrs K de Courcy-Golder)<br />
Derriford Hospital, Plymouth (Dr P D Macnaughton & Mrs N Donlin)<br />
Our thanks go to these and all our collaborators for their efforts and enthusiasm! We are well on our way to<br />
addressing the important question concerning the timing of tracheostomy.<br />
If your ICU is not currently involved in TracMan and you would like to know more, please do not hesitate to<br />
contact me on Tel: 01865 857627, email: Lesley.morgan@nda.ox.ac.uk.<br />
Look forward to hearing from you!<br />
L Morgan<br />
TracMan Trial Manager<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Surveys & Audits 13<br />
Designated Consultants for the Inter-Hospital Transfer of<br />
Patients with Brain Injury: A Survey of Practice Among<br />
Neurosurgical Units in the UK and Ireland<br />
G Allen, P Farling, B A Mullan<br />
Summary<br />
In 1996 the Association of Anaesthetists of<br />
Great Britain and Ireland, in conjunction with the<br />
Neuroanaesthesia <strong>Society</strong>, produced a set of<br />
recommendations for the inter-hospital transfer of<br />
brain injured patients. Ten years on we surveyed<br />
neurosurgical units in the UK and Ireland to assess<br />
their compliance with the recommendations. Thirty<br />
three out of a possible 36 units participated in the<br />
survey, which revealed that a significant proportion<br />
of neurosurgical units still do not have a consultant<br />
with overall responsibility for standards relating to<br />
transfer. <strong>The</strong> presence of such a person would<br />
appear to facilitate audit and training and improve<br />
patient safety. Importantly, the infrastructure to<br />
support the role of the designated consultant is<br />
currently inadequate.<br />
Introduction<br />
In the UK moderate and severe head injuries<br />
have a yearly incidence of 15 per 100,000 of the<br />
population 1 . It has been estimated that 11,000<br />
inter-hospital transfers of critically ill patients may<br />
occur in a year 2 . Approximately 10% of these<br />
may be for isolated head injuries 3 . In 1996 the<br />
Association of Anaesthetists of Great Britain<br />
and Ireland (AAGBI), in conjunction with the<br />
Neuroanaesthesia <strong>Society</strong>, produced<br />
recommendations for the safe transfer of patients<br />
with brain injury 4 . An audit of the ability of UK<br />
hospitals to implement these recommendations<br />
was published in 1999 5 . It showed that many<br />
hospitals had responded to the guidelines and were<br />
attempting to implement them. However, it also<br />
concluded that designated consultants, with<br />
responsibility for overseeing the conduct of transfers<br />
and staff training, were not readily identifiable. It is<br />
now 10 years since the publication of the initial<br />
recommendations. A revised, up-to-date set, are<br />
due to be published this year. We therefore felt that<br />
it would be timely to undertake a survey of the<br />
neurosurgical units in the UK and Ireland to assess<br />
their current compliance with the appointment of<br />
lead clinicians responsible for inter-hospital<br />
transfers. <strong>The</strong> units also provided information on<br />
the education, training and audit activities related to<br />
neuro-transfers, and the local infrastructure in place<br />
to support these activities.<br />
Methods<br />
<strong>The</strong>re are 36 neurosurgical units in the UK and<br />
Ireland (Table 1). <strong>The</strong> Neuroanaesthesia <strong>Society</strong><br />
of Great Britain and Ireland (NASGBI) has a<br />
representative in each of these units. This<br />
representative was contacted and asked if they<br />
would participate in a telephone questionnaire<br />
survey at a time which was convenient. <strong>The</strong><br />
representative could delegate the questionnaire<br />
to a more appropriate consultant if applicable.<br />
A single investigator (GA) collected all the data.<br />
As Northern Ireland has a well-established regional<br />
critical care transport service, we also surveyed the<br />
district general hospitals (DGHs) in Northern Ireland<br />
with a functioning Emergency Department. <strong>The</strong> lead<br />
clinicians in the Departments of Anaesthesia at<br />
these hospitals were identified and their participation<br />
requested. A separate questionnaire was developed<br />
for the DGHs.<br />
Results<br />
Thirty three of the 36 neurosurgical units participated<br />
in the survey. Failure to achieve a 100% response<br />
rate was due to our inability to contact the<br />
appropriate NASGBI representative for that unit<br />
and to identify a suitable substitute.<br />
Seventeen units (52 %) had a designated consultant<br />
with overall responsibility for the inter-hospital<br />
transfer of head injured patients. Only 3 of these<br />
units (18 %) had this activity recognised in the<br />
consultant’s job plan. No units were able to identify<br />
specific budget allowances for the role of the<br />
designated consultant. Units involved in regional<br />
critical care transfer services did have separate<br />
funding arrangements for these activities. Three<br />
adult units (Table 1) are currently involved in the<br />
retrieval of head injured patients. In all cases this<br />
was by way of a general transfer service for the<br />
critically ill, which would on occasion transport<br />
head injured patients if the acuity of the situation<br />
permitted.<br />
A total of 16 units (49 %) were participating in formal<br />
education and training of junior medical staff<br />
involved in the transfer of head injured patients: 13<br />
of the 17 units (76 %) with a designated consultant,<br />
and 3 of the 16 units (19 %) without a designated<br />
consultant. Audit was performed at 27 units (82 %):<br />
13 of these units were regularly auditing transfers<br />
and 14 were auditing occasionally. All units with a<br />
designated consultant performed audit, whereas only<br />
10 of the 16 units without a designated consultant<br />
undertook audit (63%).<br />
Of the DGHs surveyed, 7 out of 11 hospitals<br />
participated in the survey (64% response rate).<br />
Only 1 of the hospitals (14 %) had a designated<br />
consultant. 2 hospitals audited their transfers (29%).<br />
All senior house officers in the Northern Ireland<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
14<br />
Surveys & Audits continued<br />
School of Anaesthesia receive formal lectures on<br />
inter-hospital transfer and on the management of<br />
head injured patients. <strong>The</strong> transfers were normally<br />
performed by consultants in 1 hospital (14 %), by<br />
senior house officers in 2 hospitals (29 %) and by<br />
specialist registrars in the remaining 4 hospitals (57<br />
%). On occasions all 7 hospitals had used the<br />
regional general critical care transfer service to<br />
transport acute head injuries. <strong>The</strong> decision to use<br />
the service or not was taken by the neurosurgeon<br />
on-call, and was determined by the perceived<br />
urgency of the situation. All 7 hospitals felt that<br />
regular formal feedback form the receiving<br />
neurosurgical unit would be helpful.<br />
Discussion<br />
Trauma services in the UK and Ireland are<br />
organised regionally. <strong>The</strong>refore patients with brain<br />
injury who require definitive treatment may have to<br />
be transferred from a receiving hospital to a<br />
neurosurgical unit. Many studies have shown that<br />
such transfers may be poorly conducted and hence<br />
patients may be exposed to secondary insults 6,7 .<br />
<strong>The</strong>se insults include raised intracranial pressure,<br />
hypotension, hypoxia, hypercapnea, hyperpyrexia<br />
and hyperglycaemia. <strong>The</strong> risk of secondary brain<br />
damage can be reduced if the transfer is of high<br />
quality and based on sound principles. In 1996<br />
the AAGBI and the NASGBI published a set of<br />
recommendations for the safe transfer of patients<br />
with acute head injuries to neurosurgical units 4 .<br />
One of the recommendations was that there should<br />
be designated consultants in the referring hospitals<br />
and the neurosurgical units with overall responsibility<br />
for transfers. It was envisaged that this individual<br />
would have an important role in the clinical<br />
management of transfers, the education and<br />
training of nursing and medical staff, and in<br />
auditing the quality of inter-hospital transfers.<br />
<strong>The</strong> recommendations also stated that trusts should<br />
recognise that appropriate time and funding is<br />
required to support these activities. Our survey<br />
has revealed that almost 10 years on from the<br />
publication of the recommendations a significant<br />
proportion of neurosurgical units still do not have a<br />
designated consultant. <strong>The</strong> figures were even more<br />
disappointing for the acute DGHs in Northern<br />
Ireland. In those units that could identify a<br />
designated consultant, it would appear that little<br />
recognition or support for the activity is being<br />
provided by the healthcare trusts. This situation<br />
is untenable for the future. Without adequate<br />
resources it is extremely difficult to have a good<br />
quality service. <strong>The</strong> activities of the designated<br />
consultants involve a substantial time commitment<br />
and should be reflected in their job plans.<br />
A survey by Knowles et al in 1999 5 revealed that<br />
many referring hospitals in the UK thought that the<br />
formation of transfer teams to transport severe<br />
head injuries would have some merit. Currently<br />
only 3 adult units are involved in the retrieval of<br />
head injured patients. However, they are all general<br />
transfer services for the critically ill and are not<br />
specific for neurotrauma. Given the clinical urgency<br />
of some brain injury transfers, even if it were<br />
possible to establish specific neuro-transfer teams,<br />
there would still be occasions where the referring<br />
hospital would have to undertake the transfer<br />
themselves. Transfer teams cannot absolve<br />
DGHs of all their transfer responsibilities. Indeed,<br />
education and training would become even more<br />
important for these hospitals if the frequency with<br />
which they performed inter-hospital transfers was<br />
reduced.<br />
Conclusions<br />
Many neurosurgical units, and possibly many<br />
peripheral hospitals, do not yet have a designated<br />
consultant with overall responsibility for the transfer<br />
of patients with brain injuries. Our results suggest<br />
that the presence of this consultant facilitates<br />
education, training and audit, all of which are<br />
crucial to improving the standards of transfer. <strong>The</strong><br />
infrastructure to support the designated consultant<br />
is currently poor, with few units recognizing the role<br />
in the consultant’s job plan. Urgent attention is<br />
required to rectify this situation and future healthcare<br />
planners need to be made aware of the necessary<br />
resource implications.<br />
G Allen a , P Farling b , BA Mullan b<br />
a. Specialist Registrar<br />
b. Consultant, Department of Anaesthesia &<br />
<strong>Intensive</strong> <strong>Care</strong> Medicine, <strong>The</strong> Royal Group of<br />
Hospitals, Grosvenor Road, Belfast, BT12 6BA.<br />
References<br />
1. Jennett B, MacMillan R. Epidemiology of head injury. Br Med J<br />
(Clin Res Ed). 1981;10: 101-4.<br />
2. <strong>Intensive</strong> care society. Guidelines for transport of the critically ill<br />
adult. ICS 1997.<br />
3. McGinn GH, MacKenzie RE, Donelly JA, Smith EA, Runcie<br />
CJ.Interhospital transfer of the critically ill trauma patient: the<br />
potential role of a specialist transport team in a trauma system.<br />
J Accid Emerg Med. 1996;13:90-2.<br />
4. Jenkinson JL, Saunders DA, Wallace PGM, et al.<br />
Recommendations for the transfer of patients with acute head<br />
injuries to neurosurgical units. AAGBI. 1996<br />
5. Knowles PR, Bryden DC, Kishen R, Gwinutt CL. Meeting the<br />
standards for interhospital transfer of adults with severe brain<br />
injury in the United Kingdom. Anaesthesia 1999; 54: 280 – 283.<br />
6. Gentleman D, Jennett B. Hazards of inter hospital transfer of<br />
comatose head-injured patients. Lancet 1981; 2: 853 – 855.<br />
7. Vyvyan HAL, Kee S & Bristow A. A survey of secondary<br />
transfers of head injured patients in the south of England.<br />
Anaesthesia 1991; 46: 728-731.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Surveys & Audits continued 15<br />
Table 1<br />
List of neurotrauma centers in the UK and Ireland.<br />
* Units with general critical care transfer services which occasionally transfer acute head injuries<br />
Aberdeen Dublin * Nottingham<br />
Atkinson Morley Dundee Oldchurch<br />
Barts & <strong>The</strong> London Edinburgh Oxford<br />
Belfast * Glasgow * Plymouth<br />
Birmingham Haywards Heath Preston<br />
Birmingham Child Hull Queen Square<br />
Bristol Kings Royal Free<br />
Cambridge Leeds Sheffield<br />
Cardiff Liverpool Southampton<br />
Charing Cross Manchester Stoke<br />
Cork Middlesbrough Swansea<br />
Coventry Newcastle Great Ormond St<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
16<br />
Surveys & Audits continued<br />
Tight Glycaemic Control in Scottish<br />
<strong>Intensive</strong> <strong>Care</strong> Units<br />
E S Jack, M J E Neil<br />
Abstract<br />
Recent work has shown a mortality benefit in<br />
critically ill patients when hyperglycaemia is<br />
prevented. We performed a telephone survey of<br />
all ICUs in Scotland to identify methods of glucose<br />
control, their ability to achieve target ranges, and<br />
any related audit processes. In 23 of 26 adult ICUs<br />
blood glucose is controlled by formalised insulin<br />
protocols, mostly (19/26) similar to that described by<br />
Van Den Berghe. Few units are auditing the quality<br />
of this inexpensive and effective intervention.<br />
Keywords: Insulin; normoglycaemia; critical illness<br />
Figure 1: Methods of controlling normoglycaemia<br />
Introduction<br />
It has long been recognised that hyperglycaemia is<br />
associated with increased mortality in a variety of<br />
critical illnesses, e.g. acute myocardial infarction 1 ,<br />
stroke 2 and trauma 3 . Recent evidence has shown<br />
a mortality benefit in general intensive care patients<br />
by using insulin protocols to gain and maintain tight<br />
normoglycaemia 4,5 .<br />
Aims<br />
Our three primary aims were to establish:<br />
1. <strong>The</strong> methods of controlling blood glucose in use in<br />
Scottish ICUs.<br />
2. <strong>The</strong> blood glucose target ranges set by individual<br />
units.<br />
3. Whether target blood glucose levels are achieved<br />
and the audit processes used to measure this.<br />
ICU units<br />
Beds<br />
Rigid Protocol 19 145<br />
Individual approach 4 25<br />
Sliding scale 3 16<br />
Target Ranges<br />
<strong>The</strong>re is a considerable variation in the target range<br />
adopted by units. Of 23 units (91.4% beds) using a<br />
target range (rigid protocol or individualised system)<br />
the majority [19 units, 134 beds (78.8%)] set a<br />
lower limit of
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Surveys & Audits continued 17<br />
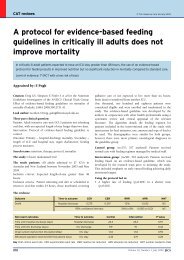
Figure 3: ‘Tightness’ targeted<br />
Range (mmol.l -1 ) <strong>Number</strong> of units Beds<br />
1.5 –1.9 4 26<br />
2 – 2.4 8 60<br />
2.5 – 2.9 4 47<br />
3 – 3.4 3 16<br />
3.5 – 3.9 3 17<br />
4 1 4<br />
Audit of control<br />
Only 5 out of 26 (19%) units were aware of recent or<br />
ongoing audit of glycaemic control. All of these were<br />
units that had instigated a rigid protocol of control.<br />
Figure 4: Audit or survey of degree of control<br />
<strong>The</strong> remaining units had no observational study<br />
done within the previous 12 months, or if one had<br />
been performed its results had not been published<br />
within that unit.<br />
Discussion<br />
General intensive care has seen some significant<br />
advances over the recent past, including the first<br />
large scale randomised controlled trials involving<br />
the sickest of patients. This research has led the<br />
adoption of interventions proven to reduce<br />
mortality and morbidity, e.g. ARDSnet protocol for<br />
ventilation in acute respiratory distress syndrome 6 ,<br />
recombinant activated protein C for sepsis 7 , low<br />
dose corticosteroids for inotrope-dependent<br />
sepsis-related circulatory failure 8 , and maintenance<br />
of tight control of normoglycaemia with insulin 4 .<br />
Many of these have been integrated in the<br />
international ‘Surviving Sepsis Campaign’ 9 . <strong>The</strong><br />
acceptance and implementation of this evidence by<br />
the majority (23/26, 91.4% of beds) of Scottish units<br />
is encouraging. <strong>The</strong> absence of published evidence<br />
on the benefits of a rigid protocol versus an<br />
individualised daily scale limits conclusions about<br />
the decision to favour differing methods of glucose<br />
control.<br />
Target Ranges<br />
<strong>The</strong> wide variety of ranges of glucose concentration<br />
reported to be beneficial to patients is reflected in<br />
Scottish critical care practice. <strong>The</strong>re are significant<br />
variations in both the absolute limits set and the<br />
‘tightness’ of the range, often arising as a result of<br />
alterations made during implementation of protocols.<br />
Although these variations restrict comparison of the<br />
degree of control, the fact that 4 units set tolerance<br />
ranges of less than 2mmol.l -1 between upper and<br />
lower limits suggests that very tight control of<br />
acceptable glucose levels is practicable. Resistance<br />
to using tight limits has centred on the possibility of<br />
overt hypoglycaemia, but with good implementation<br />
this would seem avoidable.<br />
Audit<br />
In the absence of reliable audit of the<br />
implementation of this intervention, and only a<br />
minority of units (5 out of 26) appearing to<br />
disseminate information on results, concern must<br />
exist about overall achievement of tight glycaemic<br />
control. Although medical students, trainees or<br />
nurses may have indeed been diligently collecting<br />
data and performing small scale surveys, without the<br />
dissemination of such information to the wider staff<br />
progress is inevitably limited. It is the responsibility<br />
of all units to audit how well they are achieving their<br />
target levels (no matter which range they are using),<br />
and to keep all involved workers informed about the<br />
results, so that they can attempt to constantly<br />
improve. Our survey suggested that only one unit<br />
re-audited levels of control on a month-to-month<br />
basis; their control levels were up to 80% of all<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
18<br />
Surveys & Audits continued<br />
glucose results being within their set range (a very<br />
tight range of only 1.7mmol.l -1 ). Only 5 of the 26<br />
units had recollection of a survey/audit being<br />
completed within the previous12 months, with<br />
control levels ranging from 55% to 85%. This would<br />
seem to indicate scope for further improvements in<br />
achieving targets, and that very tight ranges can be<br />
applied in a general intensive care unit.<br />
Conclusions<br />
Most ICUs (23 of 26, 91.4% of beds) in Scotland<br />
use formalised approaches to maintaining<br />
normoglycaemia, with only 3 units (8.6% of beds)<br />
having no formal control mechanism. Discrepancies<br />
were identified in the definitions of normoglycaemia<br />
as well as the tolerance range (i.e. between 1.5 &<br />
4mmol.l -1 ) accepted. Although there is scope for<br />
improving the audit of glycaemic control within<br />
Scottish ICUs, the practice of tight control has to be<br />
seen in the wider context of overall intensive care.<br />
E S Jack a , M J E Neil b<br />
a. SpR <strong>Intensive</strong> <strong>Care</strong> Unit, Victoria Infirmary,<br />
Glasgow. G42 9TY. 0141 201 5320<br />
correspondence to ewanwendy@supanet.com<br />
b. SpR Department of Anaesthesia, Ninewells<br />
Hospital, Dundee. 01382 60111<br />
References<br />
1. Malmberg K, Ryden L, Hamsten A, et al. Effects of insulin<br />
treatment on cause-specific one-year mortality and morbidity<br />
in diabetic patients with acute myocardial infarction. DIGAMI<br />
(Diabetes Insulin-Glucose in Acute Myocardial Infarction) Study<br />
Group. Eur Heart J 1996; 17: 1337–1344<br />
2. Scott, J. F.; Gray, C. S.; O'Connell, J. E.; Alberti, K. G. M. M.<br />
Glucose and insulin therapy in acute stroke; why delay further?<br />
Qjm 1998; 91: 511-515<br />
3. Laird AM. Miller PR. Kilgo PD. Meredith JW. Chang MC.<br />
Relationship of early hyperglycemia to mortality in trauma<br />
patients. J Trauma-Injury Infection & Critical <strong>Care</strong> 2004; 56:<br />
1058-62.<br />
4. Van den Berghe, G; Wouters, P; Weekers, F et al. <strong>Intensive</strong><br />
Insulin <strong>The</strong>rapy in Critically Ill Patients. NEJM 2001. 345:<br />
1359-1367.<br />
5. Cariou, A; Vinsonneau, C; Dhainaut, J-F. Adjunctive therapies in<br />
sepsis: An evidence-based review. CCM 2004; 32: S562-S570.<br />
6. <strong>The</strong> Acute Respiratory Distress Syndrome Network: Ventilation<br />
with lower tidal volumes as compared with traditional tidal<br />
volumes for acute lung injury and the acute respiratory distress<br />
syndrome. N Engl J Med 2000; 342: 1301-1308.<br />
7. Bernard GR, Vincent JL, Laterre PF, et al: Efficacy and safety<br />
of recombinant human activated protein C for severe sepsis. N<br />
Engl J Med 2001; 344: 699–709<br />
8. Annane D. Sebille V. Charpentier C. et al. Effect of treatment<br />
with low doses of hydrocortisone and fludrocortisone on<br />
mortality in patients with septic shock. JAMA 2002; 288(7):<br />
862-71.<br />
9. http://www.survivingsepsis.org/<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Surveys & Audits continued 19<br />
An Audit and Review of Hypoglycaemia<br />
in Critical <strong>Care</strong><br />
A N Thomas, E M Boxall, G Sabbagh, Dr J<br />
Eddleston, T Dunne, A Stevens, P Murphy<br />
Summary<br />
<strong>The</strong> incidence of hypoglycaemia during critical<br />
illness was audited by asking staff across a critical<br />
care network to complete pre-printed forms attached<br />
to glucose vials used to treat this complication.<br />
Twenty eight episodes were identified in 2764<br />
patient days, with a median blood glucose 2.3<br />
mmol.l -1 , (range 1.3 to 4.0 mmol.l -1 ). A more<br />
complete record of the circumstances associated<br />
with hypoglycaemia was obtained than from<br />
reviewing 22 unstructured critical incident reports.<br />
<strong>The</strong> importance of maintaining calorie intake and<br />
monitoring night time glucose were identified as<br />
potentially preventative measures in 76<br />
hypoglycaemic episodes. A risk register was<br />
produced to provide recommendations on how such<br />
events can be avoided. Details of the database and<br />
pre-printed forms can be found on the ICS website 1 .<br />
Key Words<br />
Glucose, hypoglycaemia, insulin, intensive care,<br />
adverse events, critical incident, glucometer.<br />
Tight control of blood glucose has been shown to<br />
improve survival and reduce morbidity in critical<br />
illness 2 . <strong>Intensive</strong> insulin protocols are, however,<br />
associated with the risk of hypoglycaemia 2,3,4 .<br />
This paper describes a structured method of auditing<br />
hypoglycaemia and reviews the circumstances<br />
associated with hypoglycaemic episodes. A<br />
literature review revealed other potential situations<br />
where hypoglycaemia may occur; these situations<br />
are described and strategies to minimise these risks<br />
are discussed.<br />
Methods<br />
<strong>The</strong> study was part of a wider investigation into<br />
intravenous drug administration in critical care,<br />
conducted with local research ethics committee<br />
approval across the Greater Manchester critical care<br />
network. Pre-printed forms (available on the ICS<br />
web site 1 ) requesting details of hypoglycaemic<br />
episodes were attached to vials of strong glucose<br />
solution used in their treatment. Staff accessing<br />
these vials to treat hypoglycaemia completed the<br />
forms and placed them in their unit’s critical incident<br />
box. <strong>The</strong> data was entered into an Access database<br />
(Microsoft Access, Microsoft inc. Seattle USA). <strong>The</strong><br />
study was conducted for a 4-week period in units<br />
across the network at times staggered between the<br />
start of February and mid April 2005. To obtain a<br />
larger sample of hypoglycaemic episodes than would<br />
be found in such a short audit period, critical incident<br />
forms in one ICU were hand-searched to identify all<br />
hypoglycaemic episodes reported from August 2002<br />
until January 2005. For similar reasons, a second<br />
unit also prospectively reviewed their observation<br />
charts during March 2004 to identify all episodes<br />
where the blood glucose fell below 3.0 mmol.l -1 .<br />
We therefore collected episodes of hypoglycaemia<br />
by prospective audit using pre-printed forms, by<br />
retrospective review of critical incidents, and by<br />
review of observation charts. <strong>The</strong> information from<br />
all of the episodes identified using these 3 methods<br />
were then entered on an SPSS spreadsheet (SPSS<br />
for Windows 11.4. SPSS inc. Chicago Il) for<br />
subsequent analysis.<br />
Results<br />
A total of 76 hypoglycaemic episodes were<br />
identified, 28 from completed pre-printed from the<br />
glucose vials, 26 from the retrospective review of<br />
critical incidents and 22 from the prospective chart<br />
review. <strong>The</strong> median blood hypoglycaemic level<br />
recorded using the pre-printed forms was 2.3 mmol.l<br />
-1<br />
(range 1.3 to 4.0 mmol.l -1 ). Reports were<br />
received from 8 intensive care units with a median of<br />
3 per unit (range 1 to 6). <strong>The</strong>se units had a total of<br />
97 beds open at the time with an occupancy rate of<br />
95%, so the 28 episodes occurred in approximately<br />
2764 bed days. All of the units were using tight<br />
glucose control protocols (target range 4.0 to 8.0<br />
mmol.l -1 ). <strong>The</strong> median hypoglycaemic level for the<br />
single unit retrospective record review was 2.1<br />
mmol.l -1 (range 1.1 – 3.9 mmol.l -1 ).<br />
To increase the sample size and facilitate<br />
identification of factors associated with<br />
hypoglycaemia we included results from previous<br />
hypoglycaemia critical incidents and a retrospective<br />
chart review with the main audit from the glucose<br />
bottle forms (76 episodes in total). From within this<br />
combined record the median hypoglycaemic level at<br />
the time of recording was 2.5 mmol.l -1 (range 1.1-4.0<br />
mmol.l -1 ). <strong>The</strong> median blood glucose concentration<br />
recorded before the episode of hypoglycaemia was<br />
5.4 mmol.l -1 (range 2.4 – 13 mmol.l -1 ) in the 60<br />
incidents where this information was available.<br />
<strong>The</strong> median time between this reading and the<br />
hypoglycaemic episode was 3 hours (range 1 to 6<br />
hours) in the 39 records where this could be<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
20<br />
Surveys & Audits continued<br />
calculated. Of the 32 records where it was<br />
recorded, 25 had been receiving insulin for less than<br />
24 hours and 17 for more than 24 hours. In the<br />
63 records where the time of hypoglycaemia was<br />
recorded, 35 were reported between 21:00 and<br />
07:00, 17 were reported between 07:00 and 14:00<br />
and 11 were reported between 14:00 and 21:00. In<br />
3 of 10 patients who were not receiving insulin at the<br />
time of the incident other conditions were known to<br />
have caused hypoglycaemia. In the 44 patients<br />
where the insulin dose was recorded the median<br />
dose was 3 units/hr (range 1 to 14 units/hr) at the<br />
time of hypoglycaemia. <strong>The</strong> method of glucose<br />
measurement was recorded in 50 patients; in 31<br />
glucose was measured using a blood gas analyser,<br />
20 by glucometer (both methods used in 1 case).<br />
One glucometer reading was checked by laboratory<br />
measurement. Where the information was recorded,<br />
28 of 71 patients had experienced interruptions to<br />
their calorie intake in the previous two hours, and<br />
14 of 50 patients were receiving steroids.<br />
Using the old reported critical incidents it was<br />
not possible to establish the time between<br />
measurements or the method of measurement for<br />
any of the incidents. <strong>The</strong> measurement intervals<br />
could, however, be established in 18 of 28 episodes<br />
reported using the pre-printed forms, all of which<br />
reported the measurement method. Insulin dosage<br />
was not recorded in 12 of 22 of the old unstructured<br />
forms but was in all of the pre-printed forms.<br />
Older critical incident forms failed to document the<br />
important observation that the patient’s calorie intake<br />
had not been altered, and none reported on a<br />
patient’s steroid medication. <strong>The</strong> record of<br />
information required to describe the circumstances<br />
of each episode was therefore more complete when<br />
the pre-printed forms were used.<br />
Discussion<br />
A number of advantages arise from the use of<br />
pre-printed forms adhered to glucose vials to collect<br />
information on hypoglycaemic episodes. Firstly,<br />
a more comprehensive representation of the<br />
circumstances of hypoglycaemia is established<br />
than was previously possible by reviewing free text<br />
reports, where important details of the circumstances<br />
around the hypoglycaemic episode may be omitted.<br />
Secondly, a clear reminder is provided to report the<br />
incident and it is possible to track the use of all<br />
glucose vials and associated clinical indications to<br />
establish the completeness of the record. Thirdly, it<br />
highlights for review incidents where glucose was<br />
administered when glucose levels exceeded 3.0<br />
mmol/l -1 , which are not normally associated with<br />
symptoms of hypoglycaemia 5 . Finally the form<br />
fields can be matched to a prewritten database to<br />
allow easy incident recording and analysis.<br />
<strong>The</strong> method described does have some<br />
disadvantages. Firstly, completed forms had to be<br />
reliably returned. Although relatively simple in units<br />
with “critical incident boxes”, for those with electronic<br />
records there may be nowhere to put the forms.<br />
This could be resolved by replacing forms with<br />
prompts to enter required information into an<br />
electronic incident report, or by providing envelopes<br />
for the forms to be sent to an allocated individual<br />
who could enter them onto the database.<br />
Alternatively, staff could enter information directly<br />
onto the database, but we avoided this request as it<br />
would have increased workload and would also have<br />
required additional training and computer access.<br />
<strong>The</strong> system described is relatively simple to run and<br />
could be widely adapted across many ICUs so that,<br />
over time, it would produce a clear picture of the<br />
circumstances leading to hypoglycaemia and the<br />
processes required to reduce these episodes.<br />
None of the incidents reported in this study resulted<br />
in any demonstrable long-term harm to patients, in<br />
keeping with studies describing the implementation<br />
of tight glycaemic control 2,3,4 . Hypoglycaemia is,<br />
however, a potentially devastating side effect of<br />
insulin use and has been associated with many<br />
deaths and considerable disability 6,7,8 .<br />
A potential risk register for hypoglycaemia, based on<br />
consideration of the process involved in glucose<br />
control, is summarised in Table 1. This highlights<br />
potential risks with examples, the level of risk should<br />
an event occur, how likely is it to occur, and steps to<br />
minimise the potential risk. It demonstrates clearly<br />
that although hypoglycaemic episodes arising from<br />
tight glycaemic control may be relatively common,<br />
they are not the major source of risk of injury to<br />
the patient. Rarer problems such as inaccurate<br />
measurement of blood glucose, missed diagnosis<br />
of hypoglycaemia, major errors in insulin<br />
administration, or mechanical malfunction of infusion<br />
systems are more likely to result in permanent<br />
neurological damage.<br />
In summary we have described a simple system to<br />
systematically record episodes of hypoglycaemia,<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Surveys & Audits continued 21<br />
the details of which are freely available on the ICS<br />
web site. <strong>The</strong> wider adoption of this audit tool would<br />
improve understanding of the incidence and causes<br />
of hypoglycaemia in intensive care. We have also<br />
reviewed situations where hypoglycaemia may occur<br />
and how these episodes may be minimised.<br />
Acknowledgements<br />
We are grateful for the assistance of medical,<br />
nursing and pharmacy staff in the following hospitals’<br />
critical care units in <strong>The</strong> Greater Manchester<br />
Critical Network. We particularly grateful to Dr S<br />
Nagesh for her help in conducting the single hospital<br />
prospective audit.<br />
This study was conducted under the direction of the<br />
safety committee of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong> and<br />
was funded by the Greater Manchester supra-district<br />
audit committee.<br />
A N Thomas a , E M Boxall b , G Sabbagh c , Dr J<br />
Eddleston d , T Dunne e , A Stevens f , P Murphy g<br />
a. Clinical Director, <strong>Intensive</strong> <strong>Care</strong>, Hope Hospital,<br />
Stott Lane, Salford. M6 8HD, UK<br />
b. Critical <strong>Care</strong> Pharmacist, Pharmacy Department,<br />
Hope Hospital, Stott Lane, Salford, M6 8HD.UK<br />
c. Project manager, Greater Manchester Critical<br />
<strong>Care</strong> Network<br />
d. Network lead, Greater Manchester Critical <strong>Care</strong><br />
Network.<br />
e. Critical <strong>Care</strong> Pharmacist, Pharmacy Department,<br />
Manchester Royal Infirmary. Oxford Rd.<br />
Manchester<br />
f. Network Manager. Greater Manchester Critical<br />
<strong>Care</strong> Network<br />
g. Lead Nurse. Greater Manchester Critical <strong>Care</strong><br />
Network<br />
References<br />
1. http://www.ics.ac.uk/committees_menu/safety_committee.asp<br />
2. Van den Berghe, G., Wouters, P Weekers, F. et al. <strong>Intensive</strong><br />
insulin therapy in critically ill patients. N Engl J Med 2001; 345:<br />
1359-1367.<br />
3. Krinsley, J. S. Effect of an intensive glucose management<br />
protocol on the mortality of critically ill adult patients. Mayo Clin<br />
Proc 2004; 79: 992-1000.<br />
4. Goldberg, P. A., Siegel, M. D., Sherwin, R. S. et al.<br />
Implementation of a safe and effective insulin infusion protocol<br />
in a medical intensive care unit. Diabetes <strong>Care</strong> 2004; 27:<br />
461-467.<br />
5. Auer, R. N. Hypoglycemic brain damage. Forensic Sci Int<br />
2004;146: 105-110.<br />
6. Fischer, K. F., Lees, J. A. Newman, J. H. Hypoglycemia In<br />
Hospitalized-Patients - Causes And Outcomes. N Engl J Med<br />
1986;315: 1245-1250.<br />
7. Bates, D. W., Chassin, M. R. Becher, E. C. Unexpected<br />
hypoglycemia in a critically ill patient: <strong>The</strong> wrong patient. Ann<br />
Intern Med 2002;136: 826-833.<br />
8. Batalis, N. I., Prahlow J. A. Accidental insulin overdose. J<br />
Forensic Sci 2004; 49: 1117-20.<br />
9. Ridley, S. A., Booth S. A., Thompson, C. M. Prescription errors<br />
in UK critical care units. Anaesthesia 2004; 59: 1193-1200.<br />
10. Disse E., Thivolet C. Hypoglycemic coma in a diabetic patient<br />
on peritoneal dialysis due to interference of icodextrin<br />
metabolites with capillary blood glucose measurements.<br />
Diabetes <strong>Care</strong> 2004; 27:2279,<br />
11. Levy, W. J., Gardner, D., Moseley, J. Dix, J. Gaede, S. E.<br />
Unusual problems for the physician in managing a hospital<br />
patient who received a malicious insulin overdose. Neurosurgery<br />
1985; 17: 992-6.<br />
12. Waring, W. S., Alexander, W.D. Emergency presentation of an<br />
elderly female patient with profound hypoglycaemia. Scot Med J<br />
2004; 49: 105-7.<br />
13. Clothier C, MacDonald C A, Shaw D A. Allitt inquiry:<br />
independent inquiry relating to deaths and injuries on the<br />
children's ward at Grantham and Kesteven General Hospital<br />
during the period February to April 1991. London: HMSO 1994.<br />
Correspondence to: Dr Antony Thomas. <strong>Intensive</strong><br />
care unit, Hope Hospital, Stott Lane, Salford M6<br />
8HD, UK. (e-mail: tony.thomas@srht.nhs.uk)<br />
Fax:01612065072.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
22<br />
Surveys & Audits continued<br />
Table 1: RISK REGISTER FOR POSSIBLE CAUSES OF HYPOGLYCAEMIA IN CRITICAL CARE.<br />
(Risk of hyperglycaemia also included to allow consideration of balance of risks)<br />
RISK LEVEL OFRISK EXAMPLES HOW COMMONLY PREVENTION<br />
TO PATIENT ENOUNTERED<br />
Poorly controlled Increased chance Hyperglycaemia associated Common Robust evidence based policies and protocols to control blood<br />
hyperglycaemia of death 1 with critical illness glucose. Education and adherence to protocol. Frequent<br />
review of glucose control within each ICU.<br />
Poor prescribing of Low Illegible prescription Common 9 Training of medical staff. Nurses asking for ambiguous<br />
insulin prescriptions to be rewritten. Standard strength of insulin.<br />
Electronic prescribing or pre printed insulin prescriptions<br />
Hypoglycaemia within Low Hypoglycaemia some hours Common 2,3,4 Avoid rest periods with feeds. Consider giving steroids by<br />
normal variation of after a bolus dose of steroids infusion. Use glucose 10%, 1 mg/kg/hr during interruptions<br />
tight glycaemic control to feed. Make sure glucose is measured at night. Avoid<br />
unnecessary sedation or paralysis that would mask symptoms.<br />
Technical problems Medium Malfunctioning syringe driver Rare Good equipment and regular maintenance policies. Limit<br />
with insulin delivery delivers contents of syringe in nsulin syringes to 30 units in 30mls, thereby i limiting the total<br />
systems 5 minutes dose that could be given by a malfunctioning syringe.<br />
Preparation and Medium Confusion of insulin with another Rare Checking procedures. Ensure one type of insulin available.<br />
administration errors. drug to be given by bolus Clear labeling of syringes. Use of pre-filled syringes.<br />
Confusion over labeling administration 7,8 Limit insulin in syringe. Always use the same concentration of<br />
or contents of syringes insulin and ensure insulin in date.<br />
or working of syringe<br />
pumps or preparation<br />
of syringes<br />
Systematic errors in High Glucometer test strips Rare Awareness of possibly. <strong>Care</strong> of glucometers and test strips.<br />
measurement contaminated with glucose Training and audit of use of glucometers. Checking<br />
containing feeds. Lines primed unexpected glucose values by a second measurement<br />
with glucose. Cross reaction with methods and other sample sites<br />
other sugar in peritoneal dialysis 1<br />
Unexpected medical Medium Insulinoma .Unrecognised use Rare Awareness of possibly. Regular measure of glucose in<br />
conditions or effects of of subcutaneous insulin or other patients not receiving insulin. Active investigation of<br />
drugs, other medication hypoglycaemic drug unexpected hypoglycaemia<br />
errors<br />
Criminal Intent High Surreptitious Injection of insulin Very Rare Awareness of possibly. Active investigation of unexplained<br />
by staff member or visitor, by hypoglycaemia. Good appraised and other employment<br />
any route 11,12,13 practices13]. Proper storage of insulin13.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Original Articles 23<br />
Withdrawal of Treatment in Critical <strong>Care</strong> -<br />
Who Decides?<br />
C Danbury, C Newdick<br />
Defining patients’ best interests in light of the<br />
Baby MB case.<br />
Commenting on patients who lack the capacity to<br />
consent, Lord Donaldson, Master of the Rolls, said<br />
in 1993, ‘<strong>The</strong> doctors… have both the right and the<br />
duty to treat him in accordance with what in the<br />
exercise of their clinical judgment they consider to<br />
be his best interests.’ 1 In the same case he said,<br />
‘Consultation with the next of kin… may reveal<br />
information as to the personal circumstances of the<br />
patient… Neither the personal circumstances of the<br />
patient nor a speculative answer to the question<br />
"What would the patient have chosen?’ can bind the<br />
practitioner in his choice of whether or not to treat…’<br />
In recent years these statements have been<br />
subject to challenge. <strong>The</strong> definition of what are<br />
a patient’s best interests has been clarified by the<br />
courts and now extends beyond that of a simple<br />
medically-defined best interest. Dame Butler-Sloss,<br />
has clarified that<br />
Although this is helpful, the recent case of Burke v<br />
General Medical Council has caused some<br />
confusion. Mr Burke requested the GMC’s guidance<br />
on withholding and withdrawing treatment be<br />
declared unlawful. Mr Burke has cerebellar ataxia.<br />
He does not wish for artificial nutrition and hydration<br />
to be withdrawn against his wishes. <strong>The</strong> GMC<br />
guidance implies that is lawful for doctors to do this,<br />
when it is deemed that Mr Burke lacks competence<br />
to make decisions for himself. <strong>The</strong> court of first<br />
instance held in Mr Burke’s favour. This was<br />
subsequently overturned by the Court of Appeal.<br />
However, this subsequent judgement held an<br />
anomaly, specifically at paragraphs 53 and 55.<br />
Paragraph 53 states,<br />
‘We have indicated that, where a competent patient<br />
indicates his or her wish to be kept alive by the<br />
provision of ANH [Artificial Nutrition and Hydration]<br />
any doctor who deliberately brings that patient’s life<br />
to an end by discontinuing the supply of ANH will not<br />
merely be in breach of duty but guilty of murder.’<br />
This appears to be contradicted at paragraph 55,<br />
‘Best interests are not limited to best medical<br />
interests.’ 2<br />
and,<br />
‘If mental capacity is not in issue and the patient,<br />
having been given the relevant information and<br />
offered the available options, chooses to refuse the<br />
treatment, that decision has to be respected by the<br />
doctors. Considerations that the best interests of the<br />
patient would indicate that the decision should be to<br />
consent to treatment are irrelevant.’ 3<br />
<strong>The</strong>refore, though an individual’s best interests are<br />
not confined to the narrow spectrum of medical best<br />
interests, they are still determined by doctors if the<br />
patient is not competent. In an attempt to determine<br />
what best interests are, the UK government has said<br />
that they should encompass:<br />
‘the ascertainable past and present wishes and<br />
feelings of the person concerned and the factors the<br />
person would consider if able to do so... the views of<br />
other people whom it is appropriate and practical to<br />
consult about the person’s wishes and feelings and<br />
what would be in his or her best interests.’ 4<br />
‘…Clearly the doctor would need to have regard to<br />
any distress that might be caused as a result of<br />
overriding the expressed wish of the patient.<br />
Ultimately, however, a patient cannot demand that<br />
a doctor administer a treatment which the doctor<br />
considers is adverse to the patient’s clinical needs.<br />
This said, we consider that the scenario that we<br />
have just described is extremely unlikely to arise<br />
in practice.’<br />
It is important to remember that the earlier case of<br />
Bland 6 , heard by the House of Lords, established<br />
categorically that ANH was medical treatment.<br />
<strong>The</strong>refore, on the one hand that Court of Appeal is<br />
telling us that we may not withdraw treatment<br />
against the patient’s wishes and on the other saying<br />
that patients may not insist on treatment. When<br />
considering these statements, it is important to<br />
remember that the courts make no distinction<br />
between withholding and withdrawing treatment.<br />
<strong>The</strong> Court of Appeal heard this case in <strong>July</strong> of 2005,<br />
and the scenario that was held to be ‘extremely<br />
unlikely’ has taken eight months before appearing in<br />
the High Court as the case of An NHS Trust v MB<br />
[<strong>2006</strong>] EWHC 507 (FAM).<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
24<br />
Original Articles continued<br />
Baby MB was born with spinal muscular atrophy<br />
(SMA). SMA is an autosomal recessive disorder,<br />
with an incidence of 1 in 6000 live births and in<br />
MB’s case the disease is so severe that it will be<br />
ultimately fatal. <strong>The</strong> view of 14 consultants,<br />
including 4 expert witnesses, the senior sister of the<br />
PICU and the guardian ad litem, was that MB should<br />
be permitted to die. Against this were the parents,<br />
who felt that MB still had a quality of life and were<br />
opposed to this remedy. Although the judge held<br />
that ‘<strong>The</strong>re is thus a formidable body of medical<br />
evidence of very high quality,’ he found in the<br />
parents favour. Notwithstanding the judge’s view<br />
that his decision was not was not “policy based”, this<br />
finding has implications for the practice of medicine<br />
in this country. Justice Holman said,<br />
‘I actually go further and consider that currently it<br />
is positively in his best interests to continue with<br />
continuous pressure ventilation and with the nursing<br />
and medical care that properly go with it, including<br />
suctioning and deep suctioning when required,<br />
replacement of the tube as necessary, and chest<br />
and lung physiotherapy to clear his secretions.<br />
Although that is my opinion, I cannot and do not<br />
make an order or declaration to that effect. I merely<br />
state it.’<br />
By refusing to grant a declaration that it is lawful<br />
for doctors to withdraw care, the judge effectively<br />
makes a declaration that doctors must continue<br />
treating MB. Extrapolating the Court of Appeal’s<br />
decision in Burke, any doctor who now withdraws<br />
care on MB, may be committing a crime. Who<br />
therefore, will consider withdrawal of treatment<br />
without the family’s express permission?<br />
<strong>The</strong> law relating to best interests and treatment is<br />
now less clear than ever. In light of the Mental<br />
Capacity Act 2005, there will soon be another group<br />
of individuals who will be involved in the process of<br />
deciding about different treatments. This decision<br />
has wider implications than for one individual. If this<br />
judgement stands, then the best interests test<br />
becomes unhelpful. If the best interest of the patient<br />
is determined by relatives, then we have adopted<br />
substituted judgement of the USA. Such a standard<br />
raises the prospect of continuation of treatment<br />
well beyond the point that is currently considered<br />
appropriate.<br />
C Danbury<br />
Consultant Intensivist, Royal Berkshire Hospital and<br />
Clinical Research Fellow, School of Law, University<br />
of Reading<br />
C Newdick<br />
Reader in Health Law, School of Law, University<br />
of Reading<br />
References<br />
1. In re T (adult refusal of treatment). [1993] Fam. 95<br />
2. Re MB (Medical Treatment). [1997] 2 FLR 426<br />
3. Ms B v An NHS Hospital Trust. [2002] WL 347038<br />
4. <strong>The</strong> Lord Chancellor‚s Department. Making Decisions (Cm<br />
4465) October 1999<br />
5. R (on the application of Burke) v General Medical Council.<br />
[2004] All ER (D) 588 (Jul)<br />
6. Aidale NHS Trust v Bland. [1993] AC. 789<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Original Articles continued 25<br />
<strong>The</strong> Point of Death<br />
J Radcliffe Richards<br />
One great success of intensive care is its<br />
contribution to surgery that would otherwise be<br />
impossible, such as cardiac and neurosurgery, and<br />
the more sophisticated kinds of transplant. But the<br />
connection with transplants is an odd one, because<br />
it is probably the only case in which the failure of<br />
one group of doctors to save their patient is a<br />
necessary condition of another’s saving theirs. If the<br />
patient whose care is the raison d’etre for one team<br />
is a potential source of spare parts for the other,<br />
there is in the nature of things a certain tension. It is<br />
hardly surprising if mutterings occasionally surface<br />
from transplanters who suspect intensivists of letting<br />
potential donors slip through their fingers; or from<br />
intensivists who resent the surgeons who descend<br />
to ransack their dead patients and disappear to<br />
life-saving glory, leaving the colleagues on whom<br />
their work depends to cope with the mess and grief<br />
that remain.<br />
Some of these tensions are inevitable; others,<br />
probably, could be sorted out by a good course in<br />
communication skills. But a quite different kind of<br />
difficulty, for both sides, lies in a mass of legal,<br />
ethical and cultural constraints on their activities.<br />
Several of these are, arguably, not reasonable<br />
demands of principle, but residues of ancient habits<br />
and beliefs that are actually incompatible with much<br />
present day moral and scientific thinking.<br />
For instance, one of the worst aspects of donation<br />
for all concerned is the need to ask relatives for<br />
consent. This is still required by ‘good practice’<br />
(though no longer law) even when the donor has<br />
already consented. But the common law principle<br />
that bodies cannot be property, and bequeathed like<br />
other possessions, derives from a time when people<br />
expected the literal resurrection of the dead at the<br />
Last Judgment, and when bodies were anyway of no<br />
use to anyone else. <strong>The</strong> situation is now radically<br />
different, and we already have requirements for<br />
consent to the use of bodies that look suspiciously<br />
like property rights. <strong>The</strong>re seems no good reason<br />
for not completing the change. If people owned<br />
and could bequeath their bodies, the jarring and<br />
unpleasant matter of seeking consent from the<br />
bereaved would disappear, and in time families<br />
would probably think no more about what was going<br />
on behind the scenes than they do now about the<br />
activities of pathologists and undertakers. And if the<br />
change were combined with an opting out system –<br />
also long overdue, since it would not remove the<br />
right to refuse – it would probably considerably<br />
increase the organ supply.<br />
But the non-ownership of bodies is perhaps the least<br />
important residue of ancient thinking that adversely<br />
affects both transplantation and intensive care.<br />
Much more fundamental is the legal and moral<br />
importance given to the idea of a firm boundary<br />
between life and death, and inalienable obligations<br />
to the living.<br />
<strong>The</strong> most obvious of these obligations is the<br />
prohibition on killing – actively pushing someone<br />
over the threshold of death – and hence the<br />
requirement for donors to be already dead. Another<br />
is the legal requirement to consider only the interests<br />
of the patient when making treatment decisions<br />
before death. Both of these mean that potentially<br />
transplantable organs deterioriate, often beyond use,<br />
during the dying process. Many people are now<br />
challenging (or stretching, or disregarding) the<br />
prohibition on treating patients with a view to their<br />
becoming donors; a few are even questioning the<br />
dead donor rule. But what really needs<br />
reconsideration is the traditional assumptions<br />
about life and death that underlie both of them.<br />
Dying is a process, during which different functions<br />
close down gradually and at different rates. Some,<br />
like hair growth, continue even after death. If life<br />
dwindles gradually, how can we know exactly when<br />
it has gone? <strong>The</strong> traditional approach to this<br />
problem was to err on the side of caution. Because<br />
it is worse to treat the living as dead than the other<br />
way round (worse to bury the living than leave the<br />
dead unburied), people waited until the body<br />
reached a point in the closing down process from<br />
which experience showed there was no return.<br />
What that point was depended on the state of<br />
scientific understanding.<br />
This approach was adequate for most of human<br />
history, but the situation has radically changed.<br />
Transplantation has for the first time made it urgent<br />
to identify death at the earliest possible stage in the<br />
closing down process. As long as the purpose of<br />
pronouncing death was proclaiming the next king, or<br />
passing on property, or burying the corpse, a few<br />
hours here or there made little difference. Now that<br />
we need both a dead donor and live organs, we<br />
need to establish exactly when death occurs.<br />
At the same time, the technology that makes both<br />
transplantation and intensive care possible has,<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
26<br />
Original Articles continued<br />
paradoxically, made identifying a point of death even<br />
harder. In the natural process of dying, the final<br />
elements of the closing down process come fairly<br />
close together; but we can now draw out those<br />
different elements, often independently, while<br />
monitors allow us to watch what is going on in<br />
previously impossible detail. <strong>The</strong> range from<br />
which to choose the point of death has expanded<br />
immeasurably.<br />
<strong>The</strong> resulting controversies about the point of death<br />
can become passionate, because holders of different<br />
views regard their opponents as doing serious,<br />
unjustified harm. People who accept the brain stem<br />
criterion, for instance, think that innumerable organs<br />
are lost to slow deterioration while ventilators<br />
maintain cardiopulmonary function, or monitors show<br />
the last flickers of cortical activity, in a patient<br />
already dead. Others with more conservative views<br />
– including many potential donors and their families<br />
– think their opponents are recommending the<br />
murder of dying patients.<br />
<strong>The</strong> only way out of this impasse involves<br />
recognizing a much more fundamental point: that<br />
science cannot establish a point of death. <strong>The</strong><br />
traditional view is that there is an objective fact<br />
about the matter: death is the final departure of<br />
some undetectable soul or élan vital. But if such<br />
things exist, science has no way of observing them.<br />
If, on the other hand, life is – as scientists<br />
increasingly believe – a function of the organization<br />
of material parts, there simply is no point of<br />
transition between life and death. Trying to pin it<br />
down is like trying to determine the point at which<br />
red becomes orange on a spectrum. On the<br />
traditional account, the question of when death<br />
occurs in the closing down process is scientifically<br />
unanswerable; on the more recent one, it is<br />
meaningless. Either way, it should be abandoned.<br />
<strong>The</strong> whole problem can then be approached from a<br />
different direction. Why are we so anxious to know<br />
whether someone is alive or dead? <strong>The</strong> reason,<br />
obviously, is our concern to treat the living and the<br />
dead appropriately.<br />
Instead of trying to keep the familiar categories and<br />
force the transitional states into them, we should<br />
address directly the problem of how people in those<br />
states should be treated. This question is not<br />
scientific, but moral. Science can tell us what states<br />
people are in and (with different degrees of certainty,<br />
and subject to change) whether those can be<br />
stabilized or reversed. It cannot answer the moral<br />
question of how we should treat people in those<br />
states.<br />
Traditional believers in an objective point of death<br />
will probably answer the moral question by<br />
maintaining an absolute prohibition on active<br />
hastening of death, and always presuming life in<br />
case of uncertainty. But for anyone who accepts<br />
that there is no definite point of death, but only a<br />
shading between clearly alive and clearly dead,<br />
moral judgments will need a different basis. <strong>The</strong><br />
most plausible view is that what matters is people’s<br />
interests.<br />
This kind of idea, when followed through, has<br />
radically different implications from those of the<br />
traditional view. <strong>The</strong>y can overlap in many areas,<br />
but in the penumbra between life and death, the two<br />
approaches come apart. When patients reach the<br />
point of having no interest in further treatment to<br />
reverse or delay the closing down process, they<br />
usually have no interest in whether it is further<br />
delayed, or accelerated, or redirected. From their<br />
point of view, accelerating the closing down process<br />
beyond the point of their interests is no more killing,<br />
in any morally relevant respect, than is accelerating<br />
the closing down of hair growth by cremation. At the<br />
same time, other people may have considerable<br />
interest in how the process happens – not only<br />
because of transplants, but because of the<br />
enormous resources that currently go into end-of-life<br />
care. From their point of view it matters a great deal<br />
whether we treat the dying according to their<br />
interests as we understand them, or rule out certain<br />
possibilities altogether until some (highly elusive)<br />
objective point of death.<br />
Law and professional practice already give great<br />
weight to patients’ interests, and most doctors would<br />
say those interests were the purpose of their work.<br />
But much of what is legally required and actually<br />
done has nothing to do with interests, and may<br />
actually work against them, because of ancient<br />
assumptions about an objective point of death and<br />
its moral relevance.<br />
Since every day extends our ability to separate and<br />
draw out the different elements of the closing down<br />
process that is death, it is essential to replace the<br />
anachronistic, apparently scientific debate about<br />
when death really occurs with the explicitly moral<br />
debate that it should be.<br />
J Radcliffe Richards<br />
Centre for Biomedical Ethics and Philosophy UCL<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Original Articles continued 27<br />
Shaken and Stirred – Experience from<br />
the Pakistan Earthquake<br />
A Charters<br />
On 8 th October 2005 an earthquake measuring 7.6<br />
on the Richter scale struck the northeast of Pakistan<br />
95 km away from the capital Islamabad.<br />
Muzabfarabad, the area’s capital, was extensively<br />
hit. <strong>The</strong> whole of the infrastructure of this region<br />
had been destroyed including fresh water facilities,<br />
electricity, houses, health facilities, sanitation and<br />
food supplies. <strong>The</strong> government of Pakistan<br />
estimated that over 23,000 people lost their lives.<br />
Four million people where affected, with over 42,000<br />
confirmed injured. This disaster rivalled the tsunami<br />
in its gravity, yet the world was slow to respond.<br />
of my initial enquiry my application was accepted<br />
and I was invited to join other volunteers at Merlin<br />
HQ, where we received a briefing about how NGOs<br />
work and what we were expected to do. Within<br />
hours of having received every vaccination known<br />
to man I found myself queuing alongside an<br />
orthopaedic consultant ready to board a plane<br />
that would take us to Pakistan.<br />
On 10 th October an assessment team, consisting of<br />
an A&E consultant, public health specialist and a<br />
communications officer with a logistician, was sent<br />
out to the Neelam valley (approximately 46 km away<br />
from Muzabfarabad) to asses the local health needs.<br />
<strong>The</strong> area had been cut off from accessible health<br />
provision as a result of 140 landslides which had<br />
destroyed roads and all local facilities. From the<br />
valley population of approximately120,000 it was<br />
estimated that at least 10,000 had died and 20,000<br />
were injured, but these figures could not be<br />
confirmed and the reality may have been worse.<br />
<strong>The</strong> only access to the valley was by helicopter, but<br />
a reasonable supply chain was established because<br />
of the pre-existing high military presence on the<br />
Kashmir boarder.<br />
I received an email on the 18 th of OCT from the<br />
lead of the RCN oncology forum alerting us to the<br />
fact that Merlin were in desperate need of paediatric<br />
trauma specialists - either nurses or doctors - to<br />
establish field hospitals in Kashmir for the<br />
traumatised survivors. I immediately contacted Trust<br />
management who agreed to my release from work.<br />
<strong>The</strong> initial response from Merlin was a little reticent<br />
as I had no previous field experience and normally<br />
aid agencies use workers who have had previous<br />
involvement in disasters or aid programmes.<br />
However, having submitted my CV, within a few days<br />
We were met by a representative from Merlin and<br />
escorted to our hotel, which was very basic and to<br />
be honest made the tents that we slept in for the<br />
next month feel luxurious! <strong>The</strong> next day we had<br />
further briefings, including one on UN security,<br />
following which we were flown out to a village called<br />
Devlian where our base was situated in military<br />
camp, hence hosted and protected by the Pakistan<br />
army.<br />
We were assigned an army liaison officer who<br />
became such an invaluable asset that I honestly<br />
don't know how we could have achieved what we<br />
did without him. During the very difficult first few<br />
days we set up a clinic with two consulting room<br />
tents; one was assigned as a pharmacy tent, where<br />
we organised an assortment of drugs most of which<br />
I hadn't seen for years (chloramphenicol, procaine<br />
penicillin, doxycycline etc.); the other was a patient<br />
tent in which we subsequently received 150 - 200<br />
patients a day. This basic primary care centre<br />
gradually grew into something that even the military<br />
would have been proud of, with a medical tent,<br />
surgical tent, pharmacy, four inpatient tents,<br />
vaccination clinic, store tents and a patient education<br />
tent, along with 3 patient latrines and a large<br />
(unreliable) Chinese generator. Once the primary<br />
care centre was up and running we were seeing<br />
over 250 patient a day. Some patients had walked<br />
or had to be carried over 30 km to reach us,<br />
prompting a decision to set up an outreach service<br />
and satellite clinics.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
28<br />
Original Articles continued<br />
<strong>The</strong> conditions we saw out in the valley were also<br />
very challenging. Although most of the patients with<br />
traumatic injuries had been air-lifted out, we still<br />
received an average of 60 patients day with old<br />
fractures and necrotic wounds. A surprising number<br />
of patients had dislocated hips or femoral fractures<br />
(a consequence of their house falling on top of<br />
them). Most had been waiting in the remnants of<br />
their homes since the earthquake, but when help<br />
failed to arrive and word spread of our centre they<br />
were often carried 10 - 30 km to us on makeshift<br />
stretchers. As we initially had no morphine (and the<br />
culture was against opioid analgesia) we depended<br />
on intramuscular non-steroidal anti inflammatory<br />
drugs and oral paracetamol before arranging aerial<br />
transfers.<br />
Other conditions we treated included diphtheria - a<br />
very worrying condition that brought back memories<br />
of treating very sick children with epiglottitis in<br />
Melbourne in the early 1990s - except we had no<br />
intensive care, no ENT surgeons, limited oxygen<br />
supplies and no tracheotomy tubes. All we could<br />
provide for these children were antibiotics and<br />
transfer to Muzabfarabad on the next available<br />
helicopter. Typhoid, dysentery, and malaria were<br />
also common as were a great deal of primary care<br />
conditions.<br />
Another aim of our mission was to establish public<br />
health programmes, and consequently our team<br />
vaccinated over 1500 children, provided over 1000<br />
hygiene kits and aided in the digging of countless<br />
latrines. Merlin subsequently established three<br />
further primary care centres in more mountainous<br />
sites to vaccinate and provide health care for<br />
patients that simply could not reach the base areas.<br />
To date over 15,000 patients have been cared for in<br />
these clinics with the intention being that they<br />
continue until they are no longer required.<br />
My experience working alongside the Pakistani<br />
doctors, receptionists, pharmacist and staff will stay<br />
with me for ever. I learnt a great deal about<br />
conditions I have never seen before, and will never<br />
complain about a full waiting room again. I would<br />
encourage any one that is offered the chance to do<br />
relief or emergency work to take it up - for your own<br />
benefit as well as the people you will help. Although<br />
without doubt one of the most challenging things I<br />
have ever done, it was also the most rewarding.<br />
My practice was concentrated mainly on children<br />
who were often very sick, and my cannulation skills<br />
were severely challenged on several occasions.<br />
It proved essential to concentrate on history-taking<br />
and physical examination rather than relying on<br />
investigations and diagnostic imaging as we had<br />
no labs or x-ray facilities. With patients attending<br />
the centre between the hours of 0900 - 1600 the<br />
workload was high on most days but consistently<br />
rewarding. Patients admitted to our inpatient tents,<br />
normally were normally those who required isolation<br />
(e.g. measles) or those with typhoid or malaria who<br />
were simply too ill to go home.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Original Articles continued 29<br />
Not Left to Your Own Devices?<br />
Dr S Ludgate<br />
<strong>The</strong> purchase and maintenance of medical devices<br />
makes up a significant percentage of the annual<br />
NHS and social care budget. Last year, for<br />
example, acquisition was estimated at some £10<br />
billion. Yet, whilst the medical professional is fully<br />
aware of the strict controls covering the licensing<br />
of drugs and the “Yellow Card” system for reporting<br />
side effects that result from their use, fewer<br />
clinicians appear to be aware that a similar system<br />
exists for the regulation of medical devices and,<br />
importantly, for the reporting and investigation of<br />
adverse events involving their use.<br />
One of the main problems is that not everyone is<br />
sure exactly what is included in the definition of a<br />
“medical device”. This term covers any product,<br />
other than a medicine, that is used in the healthcare<br />
environment for the diagnosis, treatment, prevention<br />
or monitoring of illness or disease, or alleviation of a<br />
handicap. It, therefore, encompasses a huge variety<br />
of products (it has been estimated that there are<br />
somewhere in the region of almost 90,000 devices<br />
available on the market) ranging from needles and<br />
syringes, to anaesthetic machines, central venous<br />
lines, patient monitors and vaporisers to name just a<br />
few.<br />
<strong>The</strong> Medicines and Healthcare products Regulatory<br />
Agency (MHRA) is an executive agency of the<br />
Department of Health, formed by the merger of the<br />
Medical Devices Agency and the Medicines Control<br />
Agency which, on the devices side, is entrusted with<br />
safeguarding public health by working with clinicians,<br />
regulators and manufacturers to ensure that all<br />
medical devices used in the Health Service meet<br />
appropriate standards of safety, quality and<br />
performance and comply with provisions of the<br />
European Medical Devices Directives.<br />
One of the Agency’s main functions in carrying out<br />
this aim, is its management of an Adverse Incident<br />
Centre which currently receives almost 9,000 device<br />
related adverse incidents each year. Each incident<br />
is investigated on a priority scale, determined after<br />
discussion with the reporter and any relevant clinical<br />
or technical staff involved. Investigations may result<br />
in a number of actions being taken, including the<br />
issuing of advice to the Health Service by means<br />
of a Device Alert, or working with manufacturers to<br />
prevent recurrence of a problem through<br />
modification or recall of a device. As a result of<br />
adverse incidents reported last year, 72 Device<br />
Alerts were issued, covering advice on a wide range<br />
of subjects, including overfilling of anaesthetic<br />
vaporisers, entrapment of anaesthetic breathing<br />
systems between operating tables and patient<br />
trolleys, prevention of hypoxic gas mixtures, issues<br />
relating to heat and moisture exchangers and filters<br />
and a variety of concerns involving infusion pumps.<br />
Additionally, there were over 400 product recalls or<br />
field corrections involving MHRA’s supervision or<br />
active involvement, 260 cases requiring the provision<br />
of advice on safer device use or improved staff<br />
training by MHRA and, in 740 cases, manufacturers<br />
undertook to improve designs, manufacturing<br />
processes or quality systems, directly as a result<br />
of the conclusions from MHRA investigations.<br />
Although the Adverse Incident Centre receives a<br />
number of device-related adverse incident reports<br />
directly from manufacturers, these relate mainly to<br />
problems arising from shortcomings in the device or<br />
its instructions for use. Increasingly, we know that<br />
adverse incidents also occur as a result of user<br />
practices, conditions of use, inappropriate storage<br />
or maintenance, or difficulties with cleaning,<br />
decontamination or sterilisation. If improvements<br />
are to be made in design, function, materials,<br />
ergonomics and instructions for use, therefore, it is<br />
vital that the Agency continues to receive reports<br />
directly from users who have experience with the<br />
device. We, therefore, urge you to let us know<br />
of any device related adverse event, however<br />
apparently trivial, since we have many examples of<br />
MHRA being the first globally to identify problems,<br />
mainly as a result of user reporting. It could not be<br />
easier. <strong>The</strong>se reports can be made by the MHRA<br />
website (www.mhra.gov.uk), which will enable the<br />
reporter to receive an automatic acknowledgement<br />
and a unique reference number. Alternatively, a<br />
standard user report form can be downloaded from<br />
the website and e-mailed to the Adverse Incident<br />
Centre (AIC) (aic@mhra.gsi.gov.uk), faxed to AIC on<br />
020 7084 3109, or posted to:<br />
Adverse Incident Centre<br />
MHRA<br />
2/2G Market Towers<br />
1 Nine Elms Lane<br />
London SW8 5NQ<br />
Please help us to improve patient and user safety<br />
when it comes to medical devices<br />
Dr S Ludgate<br />
Clinical Director, Devices<br />
MHRA<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
30<br />
Original Articles continued<br />
Diagnosis and Management of PVL-<br />
Associated Staphylococcal Infections<br />
C Day, M Morgan<br />
Panton-Valentine Leucocidin (PVL) is a toxin which<br />
destroys white blood cells. A new pattern of disease<br />
due to PVL producing staphylococcus aureus is<br />
emerging and a working group of the Health<br />
Protection Agency (HPA) is producing evidence -<br />
based guidance after reviewing of a number of<br />
cases in England.<br />
PVL can be produced by both methicillin sensitive<br />
staphylococcus aureus (MSSA) and methicillin<br />
resistant staphylococcus aureus (MRSA), but the<br />
majority of strains causing infection in the UK to<br />
date have been MSSA. Community-acquired MRSA<br />
(C-MRSA) are more likely to produce PVL than<br />
hospital-acquired MRSA.<br />
PVL strains are normally associated with necrotising<br />
pyogenic cutaneous infections classically presenting<br />
as recurrent folliculitis or abscess formation, and<br />
occasionally with cellulitis or tissue necrosis 2 .<br />
However, they can cause severe invasive infections<br />
such as septic arthritis, septicaemia and toxic shock,<br />
or community-acquired necrotising pneumonia,<br />
which is when affected patients are most likely to<br />
need intensive care 3,4 .<br />
Skin Infections<br />
PVL-associated staphylococcal infection should be<br />
suspected if a patient has recurrent furuncles or<br />
abscesses, especially if in a high-risk group.<br />
Contact sport athletes, residents of institutions such<br />
as military camps, prisons and care homes seem to<br />
have increased carriage of PVL-producing SA.<br />
Necrotising Pneumonia<br />
PVL-producing strains of staphylococcus aureus are<br />
associated with rapidly progressive, haemorrhagic,<br />
necrotising community acquired pneumonia in young<br />
immunocompetent patients, with a mortality rate as<br />
high as 75%. Most patients developing necrotising<br />
pneumonia have no history of skin sepsis.<br />
In primary care, treatment for a post-viral bacterial<br />
pneumonia should include cover for staphylococcal<br />
infection. Antibiotics such as co-amoxyclav or<br />
clarithromycin or related macrolide may be used, or<br />
if necessary flucloxacillin may be added to the local<br />
regimen for community-acquired pneumonia.<br />
Early clinical diagnosis is difficult but essential<br />
for survival. Typically the following features in a<br />
previously fit young patient suggest the diagnosis:<br />
Non-specific findings of flu-like illness, (fever of<br />
>39°C, tachycardia >140 beats/min myalgia,<br />
chills). Diarrhoea and vomiting may be due to<br />
associated toxic shock, which in the setting of<br />
a significantly raised serum creatine kinase<br />
suggests myositis.<br />
Haemoptysis<br />
Hypotension<br />
Marked leucopenia<br />
Multilobar infiltrates on chest X-ray, usually<br />
accompanied by effusions, and later cavitation<br />
Very high C-reactive protein level (>250-300 g/L)<br />
(not found in viral infection)<br />
Gram film of sputum reveals sheets of<br />
staphylococci<br />
N.B. <strong>The</strong> CURB65 score may be misleadingly low<br />
in young adults on admission.<br />
Clinical Management (mainly supportive)<br />
Some patients deteriorate with alarming rapidity<br />
making early admission desirable<br />
Early appropriate antibiotic therapy - see below<br />
Activated Protein C may be helpful but active<br />
pulmonary haemorrhage may preclude its use.<br />
Intravenous immunoglobulin (IVIG) - see below<br />
Standard surgical masks should be worn during<br />
intubation and physiotherapy. Closed tracheal<br />
suction should be used since secondary cases<br />
may occur.<br />
Antibiotic <strong>The</strong>rapy<br />
Various combinations of vancomycin, clindamycin,<br />
linezolid, rifampicin and co-trimoxazole in high doses<br />
have been used 3,4,5,6,7 . Intravenous flucloxacillin<br />
(2gm 4-6 hourly) may be useful for bactericidal<br />
action in combination with linezolid (600 mg bd iv)<br />
and / or rifampicin (300 mg bd iv). Whilst linezolid<br />
covers MRSA pending antibiotic sensitivity results,<br />
clindamycin 1.2 g qds may be used as an alternative<br />
suppressor of toxin production once sensitivity is<br />
confirmed. Vancomycin should not be used alone 7 .<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Original Articles continued 31<br />
Intravenous Immunoglobulin (IVIG)<br />
IVIG should be considered in addition to intensive<br />
care support and high dose antibiotic therapy<br />
because of the high mortality of the infection.<br />
<strong>The</strong> dosage of 2g/kg of IVIG recommended in<br />
streptococcal toxic shock syndrome may be useful<br />
for PVL-producing staphylococcus aureus infections,<br />
neutralizing exotoxins and superantigens 7,8,9 .<br />
8. Norrby-Teglund A, et al. Intravenous immunoglobulin adjunctive<br />
therapy in sepsis, with special emphasis on severe invasive<br />
Group A streptococcal infections. Scand J Infect Dis 2003; 35:<br />
683-689.<br />
9. Darenberg J et al. Differences in potency of intravenous<br />
polyspecific immunoglobulin G against streptococcal and<br />
staphylococcal superantigens: implications and therapy of toxic<br />
shock syndrome. Clin Infect Dis 2004; 38: 826-42<br />
Further Information<br />
Isolates of Staphylococcus aureus from cases which<br />
may be PVL - related (including community -<br />
acquired skin infections or pneumonia) should be<br />
sent to Dr Angela Kearns at the HPA Laboratory of<br />
Healthcare Associated Infection (LHCAI) at<br />
Colindale, telephone 0208 327 7227.<br />
C Day a , M Morgan b<br />
a. Director of <strong>Intensive</strong> <strong>Care</strong><br />
b. Consultant in Microbiology<br />
Royal Devon and Exeter Hospital<br />
References<br />
1. Holmes A et al. Staphylococcus aureus carrying Panton-Valentine<br />
Leukocidin genes (PVL) in England and Wales: frequency,<br />
characterisation and association with clinical disease. J Clin<br />
Micro 2005; 43:2384-2390.<br />
2. Reichert B, Birrell G. Severe non-pneumonic necrotising<br />
infections in children caused by Panton-Valentine Leukocidin<br />
producing Staphylococcus aureus strains. J Infection 2005;<br />
50:438-442.<br />
3. Gillet Y et al. Association between Staphylococcus aureus strains<br />
carrying gene for Panton-Valentine leukocidin and highly lethal<br />
necrotising pneumonia in young immunocompetent patients.<br />
Lancet 2002; 359: 753-759.<br />
4. Klein JL et al. Severe community-acquired pneumonia caused by<br />
Panton-Valentine Leukocidin-positive Staphylococcus aureus:<br />
first reported case in the United Kingdom. Int <strong>Care</strong> Med 2003;<br />
29:1399.<br />
5. Francis JS et al. Severe community-onset pneumonia in healthy<br />
adults caused by methicillin - resistant Staphylococcus aureus<br />
carrying the Panton -Valentine leukocidin genes. Clin Infect Dis<br />
2005; 40:100-7.<br />
6. Wargo KA, Eiland EH. Appropriate therapy for community<br />
acquired methicillin resistant Staphylococcus aureus carrying the<br />
Panton Valentine leukocidin gene. Clin Infect Dis 2005; 40:<br />
1376-7.<br />
7. Micek AT Dunne M Kollef MH. Pleuropulmonary complications<br />
and Panton-Valentine Leucocidin -Positive Community - Acquired<br />
Methicillin-Resistant Staphylococcus aureus: importance of<br />
treatment with antimicrobials inhibiting exotoxin production.<br />
Chest 2005; 128:2732-2738.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
32<br />
Original Articles continued<br />
Reflections on the clinical learning points from the the Royal<br />
London Hospital <strong>Intensive</strong> <strong>Care</strong> Unit following <strong>July</strong> 7th 2005<br />
terrorist attacks<br />
P J Shirley, M Thavasothy, D McAuley,<br />
D Kennedy, G Mandersloot, V Verma, M Healy<br />
Background<br />
<strong>The</strong> <strong>July</strong> 7 th bombings resulted in sudden,<br />
significant increased pressures on emergency care<br />
resources at Royal London Hospital (RLH), including<br />
critical care services. A lengthy period of reflection<br />
has resulted in some observations and learning<br />
points from these events.<br />
<strong>The</strong> RLH has 16 level 3 critical care beds, and a<br />
six-bedded surgical HDU managed separately by<br />
surgical teams. Of 703 ICU admissions in 2004,<br />
98% were emergencies, approximately 30% being<br />
trauma-related. This workload, coupled with a 95%<br />
occupancy rate, means that capacity expansion at<br />
short notice is difficult.<br />
Major Incident Preparation<br />
On 7 th <strong>July</strong> the first RLH intensive care unit (ICU)<br />
admission occurred at 1300, the initial response<br />
having commenced with the major incident<br />
declaration at approximately 0930. Of 15 patients<br />
in the ICU, 10 were ventilated, 3 of whom were<br />
considered fit for transfer to St Bartholomew’s or<br />
the London Chest (LCH) Hospitals, where level 3<br />
capacity had been increased by cancelling all<br />
elective cardiothoracic surgery. Fortuitously,<br />
regional anaesthetic registrars attending training<br />
were available to assist in patient transfers, and LCH<br />
also despatched transport teams. A total of 7 ICU<br />
consultants attended to assist, but none learned by<br />
paging or mobile phones that a major incident had<br />
been declared until late in the day (runners proved<br />
more efficient in disseminating this information). It<br />
was subsequently revealed that mobile networks<br />
were blocked to prevent overload and to preserve<br />
communications for emergency services.<br />
Five non-ventilated patients were transferred to<br />
ward areas. Five HDU beds were upgraded to level<br />
3 status by moving patients to ward care, and 4<br />
further level 3 beds were established in theatre<br />
recovery. Although only staffed for 16 patients, the<br />
main RLH ICU has 18 physical bed spaces, allowing<br />
2 extra beds to be created. Three unrelated cardiac<br />
arrest calls required attendance by the critical care<br />
team during this period.<br />
<strong>The</strong> ICU team were involved in the early<br />
management of patients in the Emergency<br />
Department (ED), subsequently managing patients<br />
through triaging, CT scanning, and operating<br />
theatres. This resulted in improved communication<br />
with the ICU prior to admission as well as providing<br />
continuity thereafter.<br />
Clinical Load<br />
Of 195 patients seen at the RLH, 27 were admitted,<br />
and 7 required Level 3 critical care post-operatively<br />
(Table 1). <strong>The</strong> average ICU stay was 12 days; one<br />
patient stayed for 22 days and one died from<br />
secondary brain injury resulting from prolonged<br />
hypoxia and two pre-hospital cardiac arrests.<br />
Learning Points<br />
1. ED – TRAUMA<br />
After ‘ABCDE’ management rapid transfer to<br />
theatre, ideally accompanied by the same team<br />
throughout. Secondary and tertiary surveys<br />
should be performed / repeated in theatre and ICU<br />
as initial ED surveys were often incomplete owing<br />
to instability.<br />
Send blood / urine for urgent toxicology (ED<br />
should have Rapid Test Assay).<br />
2. THEATRES – SURGERY<br />
Appropriate decisions by trauma-experienced<br />
surgeons on limb salvage, debridement and early<br />
fasciotomies will improve functional limb outcome<br />
and reduce systemic complications. Ensure all<br />
entry / exit wounds are adequately explored, as<br />
correlated with tertiary survey.<br />
Frequent repeat debridements likely to be<br />
required, necessitating close liaison with specialist<br />
surgeons.<br />
3. ICU<br />
Anticipate massive fluid requirements; early<br />
invasive haemodynamic monitoring.<br />
If haemodynamically unstable consider FAST scan<br />
and transthoracic echocardiogram (TOE if high<br />
risk of blunt cardiac injury).<br />
If transfusion requirements are high, consider<br />
mediastinal / chest wall, retroperitoneal or femoral<br />
haematomas.<br />
Have a low threshold of suspicion for barotrauma<br />
(pneumothoraces, perforated viscus).<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Original Articles continued 33<br />
Consider diagnostic peritoneal lavage (DPL) if<br />
bowel perforation suspected but unconfirmed<br />
on CT, checking fluid for soiling, white cells and<br />
amylase.<br />
Check limb compartments regularly, distal pulses<br />
at least four-hourly; track creatinine kinase (CK)<br />
levels as early indicators of compartment<br />
syndrome / rhabdomyolysis.<br />
Repeat surgical exploration if muscle ischaemia /<br />
necrosis suspected.<br />
Early DVT prophylaxis, low threshold of suspicion<br />
for DVT / fat embolus.<br />
Protective lung ventilation strategies to reduce risk<br />
of acute lung injury (ALI).<br />
4. RADIOLOGY<br />
Established protocols can ensure appropriate<br />
investigations and reporting by senior radiologists<br />
(minimum screening in all multi-injured or<br />
obtunded patients is CT C-spine with<br />
reconstruction, and anteroposterior / lateral X-rays<br />
of thoracic and lumbar spine.)<br />
Ensure orbit and facial views requested at initial<br />
CT scan depending on secondary survey and time<br />
available, balanced by additional acquisition time<br />
and need to image large numbers of patients.<br />
X-ray reporting best recorded digitally to<br />
centrally-accessible storage media, to facilitate<br />
information retrieval.<br />
5. INFECTION<br />
Prophylactic antibiotics.<br />
Virology input – bone / body parts from other<br />
victims may be embedded in patients, hence risk<br />
of HIV, hepatitis B & C. Send baseline samples<br />
for each and give empiric hepatitis B<br />
immunoglobulin with vaccination.<br />
Tetanus booster for every patient.<br />
6. ANCILLARY INJURIES<br />
Ophthalmology review of every patient to detect<br />
‘x-ray invisible’ foreign bodies.<br />
ENT otoscopy to check for ruptured eardrums<br />
(may indicate other injuries, related to blast force /<br />
proximity).<br />
7. SERUM MONITORING<br />
Regular CK levels<br />
Pregnancy test for women of childbearing age<br />
(trans-vaginal ultrasound scan if positive)<br />
Central venous saturations (ScvO 2 ) as early<br />
indicator of global perfusion adequacy.<br />
Discussion<br />
Our patients demonstrated injury patterns consistent<br />
with well-publicised pathophysiology reports of blast<br />
injuries. <strong>The</strong>se can be divided into primary,<br />
(barotrauma from initial blast wave), secondary<br />
(projectiles created by the wave) and tertiary (victims<br />
projected by the wave into stationary objects).<br />
<strong>The</strong> nature of the injuries was dependent on the<br />
proximity of the bomber to the victim and whether<br />
there were solid structures or other bodies between<br />
the bomber and victim.<br />
Following a bomb blast, traumatic limb amputation<br />
normally only occurs very close to the explosion 2 .<br />
Patients requiring amputation had massive fluid<br />
requirements from evaporative and third space<br />
losses. ScvO2 proved a useful early indicator of<br />
global perfusion adequacy (> 70%) prior to more<br />
invasive haemodynamic monitoring.<br />
Gas-containing organs such as ears, lungs and<br />
bowel are most vulnerable to primary blast injury.<br />
Consequently, in anticipation of ALI lung-protective<br />
ventilation strategies were adopted, using low tidal<br />
volume ventilation to limit plateau pressures. Blast<br />
lung as a discrete entity has been reported in up to<br />
50% of injuries occurring within enclosed spaces 3 ,<br />
but early ALI was not a feature in any of our<br />
patients. Four patients developed some features of<br />
ALI at a later stage.<br />
Although it is established RLH policy for all<br />
intubated, polytrauma patients to have radiological<br />
C-spine clearance by a senior radiologist within 24<br />
hrs 4 this was not achieved for all ICU admissions,<br />
resulting in significant increases in nursing workload<br />
to maintain spinal protection. Hard copies of X-ray<br />
films and scans were often removed by surgical<br />
teams, and were therefore not available to others for<br />
review. Ideally they should have been housed in a<br />
single area to enable immediate access.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
34<br />
Original Articles continued<br />
Limb compartments and distal pulses were<br />
fastidiously checked. Over the ensuing 48 hours<br />
all ICU patients with limb injuries required repeat<br />
surgical interventions to ensure early resection of<br />
non-viable and infected tissue, with most requiring<br />
repeat debridements. CK values > 5000 were<br />
treated with fluid, frusemide AND repeat surgical<br />
review. In several cases delayed compartment<br />
syndromes were diagnosed by a combination of<br />
clinical vigilance and rising serial CK levels,<br />
prompting revised surgical inspection and further<br />
debridement.<br />
Up to 28% of blast survivors have eye injuries 5 ,<br />
and hence every patient received slit-lamp<br />
ophthalmological examination for undetected foreign<br />
bodies. Otoscopy confirmed at least one perforated<br />
tympanic membrane in all ICU patients, indicating<br />
close proximity to the blasts. Although tympanic<br />
membrane rupture serves as a marker of blast<br />
exposure, it does not predict progression to<br />
pulmonary complications 5 and there were no<br />
subsequent ICU referrals of patients treated for<br />
tympanic perforations elsewhere in the hospital who<br />
then developed pulmonary pathology. In the Madrid<br />
bombings, of 17 critically ill patients with pulmonary<br />
complications, 13 had ruptured tympanic<br />
membranes and 4 did not 6 .<br />
Conclusion<br />
A number of factors contributed to successful<br />
outcomes for most ICU patients, including the<br />
relatively low number of seriously injured casualties<br />
and the ability to contain them within one unit. Major<br />
incident training / practices concentrate on the first 6<br />
hours, yet few patients reached the ICU by this time.<br />
<strong>The</strong>re is little emphasis on what is now termed ‘the<br />
prolonged-care phase,’ or the days (and weeks)<br />
following ICU admission. Useful advice has<br />
subsequently been obtained from clinicians who<br />
face such situations more frequently, and from their<br />
excellent published reviews 8,9 . Recently visits of<br />
survivors to the ICU or the critical care follow-up<br />
clinic have proved valuable for patients and<br />
relatives, as well as many staff members. <strong>The</strong><br />
psychological response to the attacks amongst the<br />
patients seems variable and after this elapsed time<br />
there seems to be evidence, unsurprisingly, of<br />
post-traumatic stress in some 10 .<br />
Allogenic bone fragments were recovered at surgery<br />
in several patients, raising concern over blood-borne<br />
infections. All patients consequently received<br />
hepatitis B vaccination with serum samples stored<br />
for later testing if necessary (this was agreed after<br />
a risk assessment meeting on <strong>July</strong> 8th with Health<br />
Protection Agency (HPA) representatives7).<br />
<strong>The</strong> decision to withhold anti-retrovirals was in<br />
accordance with HPA guidance on post-exposure<br />
prophylaxis in bomb victims.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Original Articles continued 35<br />
Cardiac Tamponade Following Insertion of an Implantable<br />
Defibrillator in a Patient with Hypertrophic Cardiomyopathy<br />
R Davis, M B Walker<br />
Case Report<br />
A 24-year-old female with hypertrophic<br />
cardiomyopathy (HCM) had been diagnosed in<br />
early adolescence as a result of family screening.<br />
At age 22 symptomatic broad complex tachycardia<br />
was confirmed by a 7-day loop recorder following<br />
episodes of palpitations with dizziness. Initial<br />
treatment with bisoprolol failed to suppress the<br />
dysrhythmia episodes and amiodarone therapy had<br />
caused thyroid complications. To reduce the risk of<br />
sudden death the patient therefore underwent an<br />
uneventful procedure to insert an implantable<br />
cardio-debrillator (ICD), following which she was<br />
discharged home.<br />
Five days after insertion of the ICD she presented<br />
to the local Emergency Department with a 48-hour<br />
history of diarrhoea and vomiting. On assessment<br />
she was dehydrated, and abdominal examination<br />
was unremarkable; a diagnosis of gastroenteritis<br />
was made and intravenous fluid replacement was<br />
commenced. She was admitted to a general<br />
medical ward, where despite receiving 4 litres of<br />
intravenous crystalloid she continued to feel unwell,<br />
and after 12 hours developed abdominal cramps<br />
with right upper quadrant pain. Biochemical<br />
abnormalities were alkaline phosphatase 78 mmol.<br />
L -1 , bilirubin 20 mmol.L -1 and aspartate<br />
transaminase 240 mmol.L -1 . Arterial blood gases<br />
results were pH 7.2, PaO 2 14.5 kPa and PaCO 2 2.3<br />
kPa on 15L per minute of oxygen with a lactate 5.0<br />
mmol.L -1 . Serum amylase was normal and an<br />
erect chest radiograph was unremarkable. Her<br />
vital signs remained stable with a heart rate 110<br />
bpm (sinus rhythm), blood pressure 110/60 mmHg<br />
and a GCS of 15, but she had become tachypnoeic<br />
with a respiratory rate of 30 breaths per minute. An<br />
urgent surgical opinion was requested, but before<br />
the surgical review could take place she<br />
deteriorated rapidly, developing pulmonary oedema<br />
and hypotension with a blood pressure of 80/50<br />
mmHg, but her GCS remained 15. In view of the<br />
rapidity of her clinical deterioration a decision was<br />
made to transfer her to the critical care unit.<br />
Shortly after arriving she sustained a<br />
cardiorespiratory arrest and cardiopulmonary<br />
resuscitation was commenced. Ventricular<br />
fibrillation was identified and external DC<br />
defibrillation converted the rhythm to ventricular<br />
tachycardia, but with no palpable pulse. Further<br />
external defibrillation resulted in PEA which<br />
subsequently deteriorated to asystole despite<br />
continued full resuscitation sequences. <strong>The</strong>re<br />
was no electrocardiographic evidence of activation<br />
of the ICD during this time. Echocardiography<br />
performed during the resuscitation demonstrated<br />
fluid within the pericardium. Pericardiocentesis<br />
was attempted and 10 mls of blood was aspirated<br />
with difficulty, but cardiac output was not restored.<br />
After 45 minutes cardiopulmonary resuscitation was<br />
discontinued on the grounds of futility. Subsequent<br />
interrogation of the ICD revealed that no shocks<br />
had been delivered since its insertion.<br />
Post mortem examination demonstrated a<br />
distended pericardium containing 250mls of clotted<br />
blood as a result of perforation of the right atrial<br />
appendage by the ICD atrial anchoring wire.<br />
Examination of the alimentary tract showed<br />
oedema of the mesentery and the colonic wall with<br />
no evidence of mucosal inflammation in the large or<br />
small bowel. <strong>The</strong> liver and spleen showed marked<br />
venous congestion and mottling. It was concluded<br />
that the cause of death was cardiac tamponade<br />
due to a slow persistent leak from the right atrium<br />
following perforation by a helical screw wire. <strong>The</strong><br />
abdominal symptoms were the result of venous<br />
congestion of the bowel and liver caused by<br />
impaired venous return. Failure of activation of the<br />
ICD probably resulted from lack of contact between<br />
the lead and the atrial wall after perforation.<br />
Discussion<br />
HCM is a disease of cardiac structure<br />
characterized by left and/or right ventricular<br />
hypertrophy involving primarily the interventricular<br />
septum. <strong>The</strong> primary haemodynamic disturbance<br />
caused by muscle hypertrophy is diastolic<br />
dysfunction, leading to increased filling pressures<br />
and decreased ventricular compliance. However,<br />
only 25% of patients with HCM have dynamic left<br />
ventricular outflow obstruction with a systolic<br />
pressure gradient.<br />
Histological appearances of HCM are of myocyte<br />
hypertrophy with myocardial fibre disarray, most<br />
pronounced in the interventricular septum. In the<br />
later stages of the disease there is considerable<br />
myocardial fibrosis and increased loose connective<br />
tissue. Around half the cases are familial with<br />
autosomal dominant inheritance but variable<br />
penetrance and expression. <strong>The</strong> remaining cases<br />
are sporadic. Half of the familial cases arise from<br />
mutations in the gene coding for the heavy chain of<br />
ß-myosin on chromosome 14.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
36<br />
Original Articles continued<br />
Patients with HCM usually present between 30<br />
and 40 years of age with chest pain, exertional<br />
dyspnoea and syncope. However, it can also occur<br />
in children with a similar presentation occurring<br />
during adolescence. Some cases present with<br />
sudden death 1 . Onset of symptoms in early<br />
childhood is associated with a greater risk of<br />
mortality; the 10-year mortality for children<br />
diagnosed before 14 years of age is 50 percent.<br />
Syncopal events appear to be related to myocardial<br />
ischaemia and/or ventricular tachycardia. <strong>The</strong><br />
predisposition to arrhythmias arises from several<br />
factors including hypertrophy, myocardial fibre<br />
disarray and interstitial fibrosis.<br />
Patients with HCM at high risk of sudden cardiac<br />
death (Table 1) may be candidates for an ICD.<br />
<strong>The</strong> ACC/ESC guidelines state that this is the most<br />
effective and reliable treatment option available for<br />
this group 2 . In this case ICD was offered after<br />
complications secondary to medical therapy for<br />
arrhythmia control.<br />
Table 1: Risk factors for sudden cardiac death in<br />
patients with HCM<br />
Risk factors for SCD in HCM<br />
Family history of HOCM with SCD<br />
History of Syncope<br />
Massive Left Ventricular Hypertrophy >30mm<br />
Survival of Previous SCD<br />
Symptomatic non sustained Ventricular tachycardia<br />
Hypotension in response to exercise<br />
Cardiac perforation is a recognised but rare<br />
complication of pacemaker and defibrillator<br />
insertion 3,4 but the presentation of cardiac<br />
tamponade is usually recognised acutely 5 .<br />
Cardiac tamponade following a penetrating<br />
myocardial injury classically presents with Beck’s<br />
triad of hypotension, muffled heart sounds and<br />
jugular venous distension. However, in this case,<br />
the presentation was delayed, with the patient<br />
initially becoming unwell 3 days after ICD insertion<br />
and the presenting symptoms and signs were<br />
primarily of a gastrointestinal nature. This led to<br />
an initial misdiagnosis of gastroenteritis. <strong>The</strong><br />
pericardial collection inhibited normal cardiac<br />
filling, and continued fluid resuscitation for<br />
presumed dehydration in the face of an already<br />
poorly-compliant ventricle resulted in severe<br />
pulmonary oedema.<br />
Despite evidence of a pericardial collection on<br />
ultrasonography during the resuscitation, aspiration<br />
attempts were unsuccessful. <strong>The</strong> post mortem<br />
revealed that the blood in the pericardium was<br />
clotted, which probably explains why<br />
pericardiocentesis proved ineffective.<br />
In summary, in this case of subacute cardiac<br />
tamponade following apparently uneventful ICD<br />
insertion, the clinical symptoms and signs were<br />
delayed and atypical, with primarily gastrointestinal<br />
manifestations. A high index of suspicion of<br />
cardiac tamponade should be maintained by<br />
clinicians in the early postoperative period following<br />
ICD insertion.<br />
In patients presenting with apparent non-cardiac<br />
symptoms soon after ICD insertion there should be<br />
a low threshold for performing echocardiography<br />
and ICD interrogation.<br />
References<br />
1. Maron BJ, Shen W-K, Link MS, et al. Efficacy of implantable<br />
cardioverter-defibrillators for the prevention of sudden death in<br />
patients with hypertrophic cardiomyopathy. N Engl J Med 2000;<br />
342: 365-73.<br />
2. Maron BJ, McKenna W, Danielson GK, et al. ACC/ESC clinical<br />
expert consensus document on hypertrophic cardiomyopathy: a<br />
report of the American College of Cardiology Task Force on<br />
Clinical Expert Consensus Documents and the European<br />
<strong>Society</strong> of Cardiology Committee for Practice Guidelines<br />
(Committee to Develop an Expert Consensus Document on<br />
Hypertrophic Cardiomyopathy). J Am Coll Cardiol 2003; 42:<br />
1687-1713.<br />
3. Dilling-Boer D, Ector H, Willems R, Heidbuchel H. Pericardial<br />
effusion and right-sided pneumothorax resulting from an atrialfixation<br />
lead. Europace 2003; 5: 419-23.<br />
4. Irwin SM, Green GS, Lolue SE. Atrial lead perforation: A case<br />
report. Pacing Clinical Electrophysiology.1987; 10: 1378-81.<br />
5. Tran NT, Zivin A, Mozzafferian D, Karmy-Jones R. Right atrial<br />
perforation secondary to implantable cardioverter defibrillator<br />
insertion. Can Resp J 2001; 8: 283-5.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Original Articles continued 37<br />
Bedside Ultrasound of Pleural Effusions by UK<br />
Intensivists: How much training do we need?<br />
D Y Ellis, R M Grounds, A Rhodes<br />
Bedside (or handheld) ultrasonography is being used<br />
in the ICU with increasing frequency, and areas of<br />
interest include echocardiography, vascular access,<br />
focussed abdominal ultrasound in trauma (FAST)<br />
and bladder scanning 1,2 .<br />
A recent paper showed that bedside ultrasonography<br />
by intensivists was able to detect and size pleural<br />
effusions in critically ill patients 3 . However in this<br />
study all intensivists performing bedside ultrasound<br />
scanning had ‘level III’ echocardiography training (12<br />
months training, 300 scans performed, 750<br />
interpreted 4 ) and an accompanying editorial<br />
therefore questioned how applicable this study was<br />
to ‘general intensivists who may have less training<br />
and experience’ 5 . This raises the question of how<br />
much training is required to allow general intensivists<br />
to accurately judge the presence and size of pleural<br />
effusions using ultrasound technology?<br />
One of the authors (DYE) is a specialist registrar in<br />
<strong>Intensive</strong> <strong>Care</strong> and Emergency Medicine, and has<br />
had minimal training in bedside ultrasound consisting<br />
of a 1 day FAST and central venous line placement<br />
course and a 2 day emergency echocardiography<br />
course, both in 2004. Since then he has undertaken<br />
limited scans in both the emergency department<br />
and the ICU (total of approximately 50 mostly<br />
unsupervised scans including ECHO, FAST, chest<br />
scans and scans to assess the size of the abdominal<br />
aorta), and has been entering the cases in a log<br />
book. Usually, the scans are performed<br />
independently whilst awaiting formal radiology<br />
department imaging. Over the last year (2005), DYE<br />
has worked on a London teaching hospital ICU,<br />
periodically performing bedside chest ultrasound<br />
scans using a Sonosite 180 ultrasound machine.<br />
A retrospective analysis of DYE’s logbook was<br />
performed and comparison made with the radiology<br />
reports in the patients’ notes. If no formal ultrasound<br />
report was available then other confirmation of the<br />
presence or absence of pleural fluid was looked for<br />
(e.g. CT scan, drainage of effusion or effusion noted<br />
on echocardiography). <strong>The</strong> results are illustrated in<br />
Table 1. This data suggests that the presence of an<br />
effusion is unlikely to be missed by an intensivist<br />
with minimal training using bedside ultrasound<br />
techniques. Comparing accuracy on sizing the<br />
effusions was more difficult in this analysis due to<br />
gaps in the data.<br />
It is our belief that bedside ultrasound imaging<br />
should be viewed as an extension of the<br />
stethoscope, and therefore as a part of clinical<br />
examination when indicated. Clinicians should not<br />
be afraid of having a ‘quick look’ with the ultrasound<br />
probe as long as they are aware of its (and their)<br />
limitations.<br />
Table 1: Breakdown of pleural ultrasound scans<br />
performed<br />
CT – computed tomography, TTE – transthoracic<br />
echocardiography, TOE – transeosophageal<br />
echocardiography<br />
D Y Ellis, R M Grounds, A Rhodes<br />
General <strong>Intensive</strong> <strong>Care</strong> Department, St George’s<br />
Hospital, London<br />
References<br />
1. Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU: part<br />
1. Chest 2005; 128: 881-95.<br />
2. Beaulieu Y, Marik PE. Bedside ultrasonography in the ICU: part<br />
2. Chest 2005; 128:1766-81.<br />
3. Vignon P, Chastagner C, Berkane V et al. Quantitative<br />
assessment of pleural effusion in critically ill patients by means of<br />
ultrasonography. Crit <strong>Care</strong> Med 2005; 33: 1757-63.<br />
4. Stewart WJ, Douglas PS, Sagar K et al. Echocardiography in<br />
emergency medicine: a policy statement by the American <strong>Society</strong><br />
of Echocardiography and the American College of Cardiology. J<br />
Am Coll Cardiol 1999; 33: 586-8.<br />
5. Jones AE, Kline JA Pleural effusions in the critically ill: the<br />
evolving role of bedside ultrasound. Crit <strong>Care</strong> Med 2005; 33:<br />
1874-5.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
38<br />
Original Articles continued<br />
Update on the ACUTE Initiative<br />
Dr G Perkins, Dr J Bion<br />
Recent reports have highlighted serious limitations<br />
to the care provided for the critically ill patient on<br />
hospital wards. In many cases, this is related to a<br />
failure to recognise and intervene in simple aspects<br />
of acute care such as managing airway, breathing<br />
and circulation problems 1,2 . This is compounded by<br />
poor organisation, a failure to appreciate the clinical<br />
urgency of a situation, lack of supervision, failure to<br />
seek advice and poor communication 3,4 . Recent<br />
surveys of acute care knowledge and skills amongst<br />
medical students and junior doctors demonstrate<br />
poor understanding of even simple aspects of care<br />
4,5<br />
, of particular concern as juniors are often the first<br />
responders to an acutely or critically ill patient 6 .<br />
<strong>The</strong> General Medical Council has for some time<br />
required medical undergraduates to be able to<br />
recognise and manage acute illness, and perform<br />
resuscitation on completion of their training 7 .<br />
However, there is no national or international<br />
agreement about what undergraduates should be<br />
taught to enable them to care for acutely ill patients<br />
after graduation 8,9 .<br />
<strong>The</strong> Acute <strong>Care</strong> Undergraduate Teaching initiative<br />
was launched as a joint project between the<br />
Resuscitation Council (UK) and Intercollegiate<br />
Board for Training in <strong>Intensive</strong> <strong>Care</strong> Medicine in<br />
response to increasing concerns about the general<br />
care of the critically ill patient. <strong>The</strong> project sought<br />
to develop a framework of core competencies for<br />
medical undergraduates in the care of acutely ill<br />
or arrested patient on the premise that improved<br />
education during undergraduate training would better<br />
prepare the newly-qualified doctor for the demands<br />
of clinical practice in today’s NHS. A national<br />
competency framework for undergraduates should<br />
also help smooth the transition from undergraduate<br />
training to the educational programs supporting<br />
Foundation Year Training.<br />
Proposals for competencies were invited as part<br />
of a modified Delphi survey from doctors, nurses,<br />
medical students, resuscitation officers and<br />
university teachers. Suggested competencies<br />
(defined in terms of knowledge, attitudes or skills)<br />
were submitted electronically via a website hosted<br />
by the Resuscitation Council (UK). Over 250<br />
respondents contributed 2629 competency<br />
suggestions. <strong>The</strong>se were condensed into 95<br />
representative competency statements under the<br />
themes listed in Table 1.<br />
<strong>The</strong> competency statements were rated individually<br />
by a nominal group composed of experts in<br />
resuscitation, education and intensive care.<br />
Competency statements were then classified as<br />
essential or optional elements of the curriculum<br />
based on the nominal group median ratings.<br />
This resulted in 71 essential and 16 optional<br />
competencies. Examples are given for airway and<br />
oxygenation domain in Table 2. Full details of the<br />
competencies can be found in the original paper 10<br />
or at the Resuscitation Council (UK) website<br />
(http://www.resus.org.uk/acute/projrept.pdf).<br />
<strong>The</strong> project team hope that these competencies will<br />
provide a focus for tutors responsible for developing<br />
training programmes in the care of the critically ill<br />
patient at undergraduate level. By defining the<br />
outcomes rather than the process of training,<br />
standardisation of the end product is encouraged<br />
whilst respecting diversity of local approaches to<br />
content delivery and integration with the<br />
undergraduate curriculum as a whole.<br />
Dr G Perkins<br />
Lecturer in Respiratory and Critical <strong>Care</strong> Medicine<br />
Dr J Bion<br />
Reader in <strong>Intensive</strong> <strong>Care</strong> Medicine<br />
University of Birmingham, Birmingham, B15 2TT<br />
Acknowledgement<br />
We would like to acknowledge the help and support<br />
of the ACUTE steering group and members of the<br />
Nominal Group: Catherine Baldock, Hannah Barrett,<br />
Ian Bullock, Matthew Cooke, Brian Cuthbertson,<br />
David Gabbott, Sheena Hubble, Sarah Mitchell,<br />
Jerry Nolan, Chris Smith, Alasdair Short.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Original Articles continued 39<br />
Table 1: Competency proposals grouped by themes<br />
Airway and oxygenation<br />
Breathing and ventilation<br />
Circulation<br />
Confusion and coma<br />
Drugs therapeutics and protocols<br />
Clinical examination and monitoring<br />
Team working and organisation<br />
Patient and societal needs<br />
Trauma<br />
Equipment<br />
Infection and inflammation.<br />
Table 2: An example of competencies in one domain<br />
(Airway and Oxygenation). Essential competencies<br />
are shown in normal type; optional competencies are<br />
shown in italics<br />
<strong>The</strong> Trainee<br />
Describes the signs of airway obstruction<br />
Demonstrates safe use of simple airway<br />
manoeuvres / adjuncts (head-tilt, chin lift, suction,<br />
oropharyngeal, nasopharyngeal airway)<br />
Describes the indications and rationale for safe<br />
oxygen therapy in the critically ill patient<br />
Describes the principles of controlled oxygen<br />
therapy in the patient with COPD emphasising the<br />
importance of alleviating life threatening hypoxia)<br />
Demonstrates basic treatment for simulated<br />
choking<br />
Demonstrates safe and effective use of laryngeal<br />
mask airway<br />
Describes the indications for and method of<br />
needle cricothyroidotomy<br />
Describes the indications for and method of<br />
surgical cricothyroidotomy<br />
Demonstrates safe and effective tracheal<br />
intubation.<br />
References<br />
1. Neale G. Risk management in the care of medical emergencies<br />
after referral to hospital. J R Coll Physicians Lond 1998; 32:<br />
125-9.<br />
2. McGloin H, Adam SK, Singer M. Unexpected deaths and<br />
referrals to intensive care of patients on general wards. Are<br />
some cases potentially avoidable? J R Coll Physicians Lond<br />
1999; 33: 255-9.<br />
3. Vincent C, Neale G, Woloshynowych M. Adverse events in<br />
British hospitals: preliminary retrospective record review. BMJ<br />
2001; 322: 517-9.<br />
4. Smith GB, Poplett N. Knowledge of aspects of acute care in<br />
trainee doctors. Postgrad Med J 2002; 78: 335-8.<br />
5. Ringsted C, Schroeder TV, Henriksen J et al. Medical students'<br />
experience in practical skills is far from stakeholders'<br />
expectations. Med Teach 2001; 23: 412-6.<br />
6. National Confidential Enquiry into Patient Outcome and Death.<br />
An Acute Problem. http://www.ncepod.org.uk/2005report/. 2005.<br />
7. General Medical Council. Tomorrow’s doctors:<br />
Recommendations for Undergraduate Education. London:<br />
General Medical Council, 2003.<br />
8. Shen J, Joynt GM, Critchley LA, Tan IK, Lee A. Survey of<br />
current status of intensive care teaching in English-speaking<br />
medical schools. Crit <strong>Care</strong> Med 2003; 31: 293-8.<br />
9. Frankel HL, Rogers PL, Gandhi RR, Freid EB, Kirton OC,<br />
Murray MJ. What is taught, what is tested: findings and<br />
competency-based recommendations of the Undergraduate<br />
Medical Education Committee of the <strong>Society</strong> of Critical <strong>Care</strong><br />
Medicine. Crit <strong>Care</strong> Med 2004; 32: 1949-56.<br />
10. Perkins GD, Barrett H, Bullock I et al. <strong>The</strong> Acute <strong>Care</strong><br />
Undergraduate TEaching (ACUTE) Initiative: consensus<br />
development of core competencies in acute care for<br />
undergraduates in the United Kingdom. Int <strong>Care</strong> Med 2005; 31:<br />
1627-33.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
40<br />
Lemmingaid<br />
Kafka and the Clinical Director<br />
In this new world of appraisal, audit and reflective<br />
life-long learning it often seems that we have ample<br />
opportunity to take a long hard look at ourselves in<br />
the mirror and deduce what we are ‘really’ like –<br />
strengths, weaknesses, vices and virtues. Complete<br />
nonsense, of course. Forthright criticism we dismiss<br />
as ‘unfair’ whereas gentler criticism normally comes<br />
from those too serpentine to be easily understood.<br />
So, we potter along unconscious of our impact,<br />
unknowing of our capabilities and unaware of<br />
whether we are liked, possibly admired or merely<br />
tolerated. <strong>The</strong>se soul-searchings are mostly of no<br />
great consequence except when the spinning bottle<br />
of clinical management happens to point to you<br />
when it stops.<br />
Clinical management is something most doctors<br />
avoid – and rightly. Given the choice between<br />
stabbing yourself in the neck with a biro, wetting<br />
your nose and sticking it in a light socket or<br />
becoming a clinical manager, clearly the last is the<br />
least attractive. <strong>The</strong>re are up-sides; your jaded<br />
clinical job seems like paradise- lost, people know<br />
who you are and once in a decade you might make<br />
some small difference. <strong>The</strong> down-sides are; lots<br />
more work, the people who know who you are now<br />
want something from you and you don’t make a<br />
difference. (It is claimed that clinical managers merit<br />
award application sometimes get binned by the<br />
powerful whom they have cheesed off along the<br />
way).<br />
How did all this happen? I will share my reflections<br />
with you, dear reader, so that you can be broadly<br />
forewarned when the spinning bottle stops at you.<br />
As for myself, a collective whim of the department<br />
fatally combined with managerial acquiescence<br />
resulting in me becoming Clinical Director. <strong>The</strong><br />
barely suppressed mirth of those who congratulated<br />
me was frankly repulsive.<br />
To be honest, I was flattered – so, no reflective<br />
cognition here. To date, I had shown no managerial<br />
interest / experience / capability... the list of qualities<br />
necessary for the job, which I surely did not<br />
possess, could stretch from here to Budapest in<br />
size 12 Font. <strong>The</strong> outgoing Clinical Director made<br />
transparently facetious assertions like: ‘You’ll<br />
enjoy it’ and ‘It will be good for you’. Ha! Proper<br />
self-awareness would have screamed ‘No!’ at the job<br />
I was taking on.<br />
<strong>The</strong> day he quit, I entered a Kafka-esque world<br />
where people thought, spoke and did things<br />
differently. <strong>The</strong> months turned into years and, it<br />
was an embarrassingly long time before I realised<br />
you only need one quality to succeed in clinical<br />
management – a taste for the absurd. And so here<br />
are random thoughts painfully gleaned.<br />
Power. An old proverb from Pakistan roughly<br />
translates as: Always vote for the man that doesn’t<br />
want the job. If you are a power-junky, then you’re<br />
probably crazy. Consultant colleagues are your<br />
equals; attempting to cajole them against their<br />
wishes usually results in an intransitive prepositional<br />
exclamatory phrase beginning and ending with ‘F’.<br />
Invoking an esprit de corps is about your only hope -<br />
doctors are more concerned with what their<br />
colleagues think of them than what management<br />
thinks of them.<br />
Reputations. <strong>The</strong>se are achieved very quickly – but<br />
can take a lifetime to shake off. As Mark Twain<br />
said: Get yourself a reputation as an early riser and<br />
thereafter you can sleep ‘til lunch. Actions speak<br />
louder than words – so just telling everyone how<br />
fantastic and hard working you are will earn you a<br />
reputation, but not the one you’re looking for. A<br />
small effort at the beginning of your consultant life<br />
could earn you the reputation as someone who<br />
has ‘guts’ – failure to make this effort can tend to a<br />
reputation for being one end of the alimentary tract<br />
or the other, which is not so nice.<br />
Hard work. All doctors are mildly delusional. We<br />
all believe we work very, very, very hard. Some<br />
doctors do work very, very, very hard; others work<br />
very, very hard and the rest work very hard. You<br />
can distinguish these three groups because they are<br />
exhausted, quiet and bellicose respectively. <strong>The</strong>re<br />
is an inverse relationship between ‘very’ count and<br />
bellicosity. As any biological characteristic is<br />
normally distributed in any population then hard<br />
work is unlikely to be different. Curiously, everyone<br />
knows who is at the lower end of the effort bell curve<br />
except those individuals who are there. If you then<br />
begin to compare what consultants within your own<br />
specialty do with other specialties you feel both<br />
furious (some specialties are a bit of a doss) and<br />
humble (some specialties really work their socks off).<br />
Finance. Budgets are an illusion. I don’t suggest<br />
that financial control isn’t a worthy occupation. No,<br />
but if all the anaesthetic monitors blow a fuse or<br />
there are no anaesthetists to watch them then<br />
money will be found, and it doesn’t matter how<br />
many digits in the red your directorate is. <strong>The</strong>re is<br />
a pot and it isn’t at the end of a rainbow – it’s just<br />
that you may need to produce reams of supporting<br />
documentation which often turns out be more<br />
expensive than the thing you want money for.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Lemmingaid continued 41<br />
Meetings. It is a mistake to attend all meetings –<br />
of which there are squillions. I did this at first but<br />
my psychiatrist became worried and advised me to<br />
be more selective. After following his advice, I<br />
cancelled my subscription to ‘Rifle’ magazine and<br />
stopped stockpiling weapons in the garden shed.<br />
Trust Executive meetings follow a familiar seasonal<br />
pattern: Summer – hot, lazy and boring. Autumn –<br />
half-yearly financial position declared, year-end<br />
predictions computed. Winter – Yikes! Predictions<br />
are now way off the map. Extra waiting lists! No<br />
cancelled operations! Close ITU beds! Arrrgh!<br />
Spring: - Phew, we just made it, again. Its familiar<br />
repetition almost became comforting after a while.<br />
Employment law. This is an area where familiarity<br />
leads to utter contempt. I shall not expound widely<br />
on this, suffice to say that being on sick leave does<br />
not prevent you going skiing, on a Mediterranean<br />
cruise or a diving holiday in Tobago. I would have<br />
thought it did – but I was wrong. And be careful how<br />
you ask someone if they would please turn up to<br />
work and do the job they are paid to do – that is<br />
probably bullying as defined by the ‘Dignity at work’<br />
policy.<br />
Holidays. Statutory and religious holidays. All<br />
faiths are equal but some have more holidays.<br />
Every faith group must be allowed time off to<br />
celebrate their religious holidays – ‘fair enough’, I<br />
say. No NHS employee should have more time off<br />
than any other equivalent worker – ‘fair enough’, I<br />
say again. No one wants to work Christmas day –<br />
Erm… try squaring that circle year after year?<br />
Annual leave is an even greater giggle – thankfully<br />
not in our department; but a Surgical Consultant<br />
baulked at filling in leave forms, commenting<br />
unaffectedly that: ‘A Gentleman takes as much<br />
holiday as he needs’ (!)<br />
Higher Awards. Who said modern medicine<br />
excludes those with a poetic bent? <strong>The</strong>se forms are<br />
a tribute to poetic licence and creative thinking.<br />
People who have time to fill in the form are lying on<br />
the form. This is not exactly fair, I recognise – but<br />
there is a skill to filling in the form. Humility and<br />
dyslexia, often the domain of deserving individuals,<br />
just doesn’t cut it. Highest Award holders are mostly<br />
distinguished by the company they keep. (That’s<br />
blown my chances, then).<br />
laity, as this should not be an option and runs<br />
counter to ‘Patient Choice’. Dealing with complaints<br />
is the Directors turf. Often the complaints are<br />
tendentious. But beware smugness; complaints are<br />
rarely malicious, some do have reasonable grounds<br />
- but so often the real medical Lulu’s go unnoticed<br />
and are never mentioned in the letters.<br />
Miscellaneous. A few translations: Drill down –<br />
all the data we have collected up to now is<br />
meaningless…we’ll have to start again. Think<br />
outside the box - start again. Suggestion –<br />
something sensible to ignore. Contribution –<br />
something useless to ignore. Sharing – something<br />
senseless that will inform the whole project design.<br />
Business Plan – a ritual designed to exhaust<br />
clinicians, delay and ultimately refuse what they<br />
need and warn them off ever making such spurious<br />
claims in the future. Patients – these are not the<br />
sick people in beds but the representatives who sit<br />
on every damn project committee including the Toilet<br />
Rebuild 2007 project. <strong>The</strong>se representatives will<br />
never sit on the rebuilt toilets, however - because<br />
they’re not real patients.<br />
Why is the acronym for the Department of Health<br />
the same thing Homer Simpson says when he<br />
realises he’s done something stupid? ‘;DoH!’ Most<br />
documents it produces talk of ‘strategy’ – and is as<br />
useful as the strategy developed by a blindfolded<br />
convict tied to a post in front of a firing squad.<br />
Having befriended and flattered another colleague<br />
into being Clinical Director, I’ve now left Kafka’s<br />
world. I will leave you with a quote from Albert<br />
Einstein when returning a loaned copy of a Kafka<br />
novel to its owner: ‘I couldn’t read it for its perversity.<br />
<strong>The</strong> Human mind isn’t complicated enough.’ I<br />
feel that about the NHS – perverse, chaotic and<br />
complex. Like the young crab said on the edge<br />
of the pool of tears in Alice’s Adventures in<br />
Wonderland: ‘It’s enough to try the patience of an<br />
oyster!’ But you’ve got to love it too – what else are<br />
you going to do?<br />
Wood and Trees<br />
Complaints. Healthy people are usually outside<br />
hospitals and sick ones are inside. Increasing<br />
sickness has a positive correlation with morbidity<br />
and mortality. It comes as no surprise that<br />
sometimes patients don’t get better, they may<br />
even die. <strong>The</strong> force of this logic often eludes the<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
42<br />
CATmaker Reviews<br />
Rescue Angioplasty vs Repeat<br />
Thrombolysis in Acute MI?<br />
In patients with failed primary thrombolysis<br />
following an acute MI, when compared with<br />
non-PCI management (pooled results of<br />
conservative management & repeat<br />
thrombolysis), PCI reduces cardiac and cerebral<br />
events (NNT=12) and “all-cause” mortality (NNT<br />
= 16). However, when compared directly with<br />
either conservative management OR repeat<br />
thrombolysis there was no mortality benefit.<br />
Level of Evidence: 1 + (RCT with a low risk of<br />
bias)<br />
Citation: Gershlick AH, Stephens-Lloyd A, Hughes<br />
S et al for the REACT Trial Investigators. Rescue<br />
angioplasty after failed thrombolytic therapy for acute<br />
myocardial infarction. N Engl J Med 2005; 353:<br />
2758-68<br />
Lead author's name and email: Anthony Gershlick,<br />
agershlick@aol.com<br />
Three-part Clinical Question:<br />
Patients: Suffering from an acute ST elevation<br />
myocardial infarction that failed to show >50%<br />
resolution of ST segment elevation within 90 minutes<br />
of receiving thrombolysis.<br />
Treatment: Percutaneous Intervention (PCI) vs.<br />
Repeat Thrombolysis vs. Conservative Management<br />
Outcomes: Primary = Composite of cardiac and<br />
cerebrovascular events (all cause mortality, cardiac<br />
<strong>The</strong> Evidence<br />
mortality, recurrent myocardial infarction,<br />
cerebrovascular event and severe heart failure).<br />
Secondary = risk of major and minor bleeding and<br />
need for revascularisation.<br />
Search Terms: Myocardial infarction, management,<br />
PCI, thrombolysis<br />
<strong>The</strong> Study: Double-blinded concealed randomised<br />
controlled trial with intention-to-treat.<br />
<strong>The</strong> Study Patients: All patients with an acute<br />
ST-elevation infarction who received thrombolysis<br />
within 6 hours of the onset of chest pain but in whom<br />
there had been less than 50% resolution of ST<br />
segments 90 minutes after starting thrombolysis.<br />
Exclusion criteria included cardiogenic shock, LBBB<br />
and a haemoglobin >1.5g/dl below the normal range<br />
within the previous 6 hours.<br />
Control group (N = 283; 283 analysed):<br />
Conservative management (intravenous heparin<br />
titrated to an APTT ratio of 1.5-2.5) or repeat<br />
thrombolysis using a fibrin-specific thrombolytic<br />
agent plus intravenous heparin.<br />
Experimental group (N = 144; 144 analysed):<br />
Coronary angiography, +/- angioplasty, +/- adjuvant<br />
therapy (stenting or glycoprotein IIb/IIIa inhibitors)<br />
determined at the time of PCI.<br />
Outcome Time to Outcome CER EER RRR ARR NNT<br />
Cardiac and 6 months 0.233 0.153 34% 0.080 12<br />
Cerebrovascular<br />
events 95% Confidence Intervals: 1% to 67% 0.003 to 0.157 6 to 303<br />
Mortality 6 months 0.127 0.063 50% 0.064 16<br />
(all cause)<br />
95% Confidence Intervals: 7% to 94% 0.009 to 0.119 8 to 118<br />
Mortality 6 months 0.102 0.056 45% 0.046 NS<br />
(cardiac cause)<br />
95% Confidence Intervals: ns ns ns<br />
Non-Event Time to outcome/s Control group Experimental P-value<br />
Outcomes<br />
group<br />
22.4% (Conservative)<br />
Revascularisation 6 months<br />
25.6% (Repeat Thrombolysis)<br />
13.8% p=0.05<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
CATmaker Reviews continued 43<br />
Comments:<br />
1. Do the methods allow accurate testing of the<br />
hypothesis? Yes<br />
2. Do the statistical tests correctly test the results<br />
to allow differentiation of statistically significant<br />
results? Yes<br />
3. Are conclusions valid in light of the results? Yes<br />
- their primary outcome measure was a<br />
composite of death, recurrent MI, severe heart<br />
failure and cerebrovascular events.<br />
4. Did results get omitted, and why? Yes. Patients<br />
randomized to one arm were allowed to have<br />
another treatment if the investigators thought<br />
that it was clinically indicated, for instance, due<br />
to ongoing chest pain or the development of<br />
cardiogenic shock. However, analyzing on an<br />
intention-to-treat basis did not change the<br />
statistical outcome.<br />
5. Did they suggest areas of further research? No,<br />
although given the trend towards reduced<br />
mortality, repeating this study with mortality as<br />
the sole primary outcome measure may lead to<br />
a positive answer. Unfortunately this trial was<br />
stopped early due to problems with recruitment<br />
and funding.<br />
10. What grade of recommendation can I make<br />
when this study is considered along with other<br />
available evidence? B<br />
11. Should I change my practice because of these<br />
results? Only if all patients who don’t receive<br />
adequate reperfusion after thrombolysis go on to<br />
receive rescue PCI as routine management.<br />
<strong>The</strong>re is insufficient evidence to recommend this<br />
at present. Conservative management is as<br />
effective as repeat thrombolysis.<br />
12. Should I audit my current practice because of<br />
these results? Yes, although you may have too<br />
few patients to come up with any meaningful<br />
outcome.<br />
Appraised by: Stephen Harris, Department of<br />
Anaesthesia & Critical <strong>Care</strong> Medicine, Torbay<br />
Hospital, Lawes Bridge, Torquay, DEVON TQ2 7AA.;<br />
14 January <strong>2006</strong><br />
Email: stepharr@hotmail.com<br />
Kill or Update By: Jan 2010<br />
Reviewed & Edited by CC & BT<br />
6. Did they make any recommendations based on<br />
the results and were they appropriate? Yes.<br />
Rescue PCI is indicated in failed thrombolysis.<br />
Given that this reduces recurrent MI but not<br />
outcome measures such as morbidity or<br />
mortality, this needs to be interpreted with<br />
caution.<br />
7. Is the study relevant to my clinical practice? Yes<br />
8. What level of evidence does this study<br />
represent? 1 + (RCT with a low risk of bias)<br />
9. What grade of recommendation can I make on<br />
this result alone? B<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
44<br />
CATmaker Reviews continued<br />
Furosemide and Albumin Improve Oxygenation in<br />
a Small Group of Patients with Acute Lung Injury<br />
Using furosemide combined with albumin in<br />
the treatment of hypoproteinaemic patients with<br />
acute lung injury improves oxygenation. Further<br />
studies are required to determine clinical<br />
outcomes such as survival and duration of<br />
mechanical ventilation.<br />
Level of evidence: 1 - (RCT with a high risk of<br />
bias)<br />
Citation/s: Martin GS, Moss M, Wheeler A, Mealer<br />
M, Morris J, Bernard G: A randomised, controlled<br />
trial of furosemide with or without albumin in<br />
hypoproteinaemic patients with acute lung injury.<br />
Crit <strong>Care</strong> Med. 2005; 33:1681-7<br />
Three-part Clinical Question:<br />
Patients: Hypoproteinaemic patients with acute lung<br />
injury.<br />
Intervention: Treatment of furosemide with or without<br />
albumin.<br />
Outcome: Improved oxygenation.<br />
Search Terms: acute respiratory distress syndrome;<br />
acute lung injury, albumin; blood proteins;<br />
hydrostatic pressure; hypoproteinaemia; lung<br />
diseases; osmotic pressure<br />
<strong>The</strong> Evidence<br />
<strong>The</strong> Study: Double-blinded concealed randomised<br />
multi-centred controlled trial with intention-to-treat.<br />
In 11 medical, surgical and trauma ICUs in North<br />
America.<br />
<strong>The</strong> Study Patients: Patients were eligible that had<br />
each of the following criteria: American-European<br />
Consensus Conference definition for ALI, serum total<br />
protein level ≤6.0g/dl, ongoing nutritional support<br />
and mechanical ventilation for >24hrs. Patients<br />
were excluded for haemodynamic instability, renal or<br />
liver disease, allergy, pregnancy, age
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
CATmaker Reviews continued 45<br />
EBM Questions:<br />
1. Do the methods allow accurate testing of the<br />
hypothesis? Yes<br />
2. Do the statistical tests correctly test the results to<br />
allow differentiation of statistically significant<br />
results? Yes<br />
3. Are conclusions valid in light of the results? Yes<br />
4. Did results get omitted, and why? No<br />
5. Did they suggest areas of further research? Yes.<br />
<strong>The</strong>ir suggestion is that a large-scale randomised<br />
trial is warranted to determine clinical benefit in<br />
mechanical ventilation.<br />
6. Did they make any recommendations based on<br />
the results and were they appropriate? No<br />
7. Is the study relevant to my clinical practice? To a<br />
limited extent, Yes. <strong>The</strong> small number of patients<br />
in this study (n=40) with the large number of<br />
excluded patients (n=309) make this a minority<br />
subgroup of hypoproteinaemic patients with acute<br />
lung injury but without shock. Additionally, there<br />
was no proven improvement in patient survival.<br />
10. What grade of recommendation can I make<br />
when this study is considered along with other<br />
available evidence? None<br />
11. Should I change my practice because of these<br />
results? No<br />
12. Should I audit my current practice because of<br />
these results? Yes, if you use furosamide and<br />
albumin in ALI patients you should review your<br />
practice<br />
Appraised by: David MacNair and Dr BH<br />
Cuthbertson, <strong>Intensive</strong> <strong>Care</strong> Unit, Aberdeen Royal<br />
Infirmary, Foresterhill, Aberdeen AB25 2ZN ; 13<br />
September 2005<br />
Email: davidmacnair@doctors.net.uk<br />
Kill or review by: May 2010<br />
Reviewed & edited by CC & BT.<br />
8. What level of evidence does this study<br />
represent? Level 1- (RCT with a high risk of bias<br />
due to small sample size.)<br />
9. What grade of recommendation can I make on<br />
this result alone? None<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
46<br />
CATmaker Reviews continued<br />
Corticosteroids in Late ARDS<br />
<strong>The</strong> treatment of late ARDS with<br />
methylprednisolone does not improve mortality<br />
but may reduce the duration of ventilation.<br />
Level of evidence: 1+ (RCT with a low risk of<br />
bias)<br />
Citation/s: <strong>The</strong> National Heart, Lung, and Blood<br />
Institute Acute Respiratory Distress Syndrome<br />
(ARDS) Clinical Trials Network. Efficacy and Safety<br />
of Corticosteroids for Persistent Acute Respiratory<br />
Distress Syndrome. NEJM <strong>2006</strong>; 354: 1671-1684.<br />
Lead author: Kenneth Steinberg<br />
Three-part Clinical Question:<br />
Patients: Patients with late stage ARDS<br />
Intervention: High dose methylprednisolone<br />
Outcome: (Primary) Mortality, (Secondary)<br />
ventilator-free days, organ-failure-free days.<br />
Search Terms: ARDS; therapy.<br />
<strong>The</strong> Study: Single-blinded randomised controlled<br />
trial with intention-to-treat.<br />
<strong>The</strong> Study Patients: Late stage ARDS according to<br />
American European Consensus Conference criteria<br />
still requiring mechanical ventilation for 7-28 days<br />
after onset of ARDS.<br />
Control group (N = 91; 91 analysed): No specified<br />
ventilatory strategy (probably not controlled) until<br />
1999 then standard ARDSnet ventilation strategy<br />
after 1999 and weaned according to a standardised<br />
weaning protocol.<br />
Experimental group (N = 89; 89 analysed):<br />
No specified ventilatory strategy (probably not<br />
controlled) until 1999 then standard ARDSnet<br />
ventilation strategy after 1999 and weaned according<br />
to a standard weaning protocol plus the addition of<br />
corticosteroids. Methylprednisolone 2mg/kg as one<br />
off dose followed by 0.5mg/kg six hourly for 14 days,<br />
0.5mg/kg twelve hourly for 7 days then tapered to off<br />
over 4 days if still ventilated or over 2 days if not<br />
ventilated or patient had developed fungal infection<br />
or septic shock.<br />
<strong>The</strong> Evidence<br />
Outcome Time to Outcome CER EER RRR ARR NNT<br />
Mortality 60 days 0.286 0.292 -2% -0.006 NS<br />
Oxygenation<br />
95% Confidence Intervals: ns ns ns<br />
Mortality in early 60 days 0.364 0.273 25% 0.091 NS<br />
group randomised<br />
between 7-13 days 95% Confidence Intervals: ns ns ns<br />
Mortality in late 60 days 0.080 0.348 -335% -0.268 -4<br />
group randomised<br />
between 14 and 95% Confidence Intervals: -612% to -58% -0.490 to -0.046 -22 to -2<br />
28 days<br />
Non-Event Outcomes Time to outcome/s Control group Experimental group p-value<br />
Ventilator- free days 28 days 6.8 11.2
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
CATmaker Reviews continued 47<br />
Comments:<br />
1. Do the methods allow accurate testing of the<br />
hypothesis? This is in question. <strong>The</strong> study ran<br />
for 7 years partly due to factors outside the<br />
control of the authors and clinical practice<br />
changed markedly in this time (i.e. the<br />
publication of the ARDSnet study in 2000).<br />
Study patients were changed to ARDSnet<br />
ventilation after 1999 and their ventilation was<br />
not protocolised before this time. Further, the<br />
patient number for the entire study and for all<br />
subgroups is far below the original power<br />
calculation. Although not fully explained they<br />
probably relate to poor recruitment rather than<br />
any genuine change in estimated mortality. <strong>The</strong><br />
trial only recruited 5% of available patients so<br />
limiting the trial results applicability. <strong>The</strong> late<br />
treatment subgroup (14-28 days) was clearly<br />
post-hoc as it was not stated in the trial protocol<br />
with all the problems associated with such<br />
analysis. With a total of 48 patients in the 14-28<br />
day subgroup (2 deaths in control group and 8 in<br />
treatment) this result should not be considered<br />
valid as it is grossly underpowered. One extra<br />
death in control group would make this<br />
non-significant.<br />
2. Do the statistical tests correctly test the results<br />
to allow differentiation of statistically significant<br />
results? Yes.<br />
3. Are conclusions valid in light of the results?<br />
<strong>The</strong>y conclude that the results do not support<br />
the routine use of methlyprednisolone in<br />
prolonged ARDS. This is a reasonable<br />
conclusion. <strong>The</strong>y also conclude that starting<br />
methylprednisolone more than two weeks after<br />
onset of ARDS may increase mortality. This may<br />
lack validity due to very small event numbers.<br />
4. Did results get omitted, and why? No.<br />
5. Did they suggest areas of further research? No.<br />
6. Did they make any recommendations based on<br />
the results and were they appropriate? Yes.<br />
<strong>The</strong>y concluded that results did not support the<br />
routine use of methyprednisolone in ARDS.<br />
This seems a reasonable recommendation. Is<br />
the study relevant to my clinical practice? <strong>The</strong>y<br />
recruited from a group of all comers with ARDS<br />
who are still ventilated after 7 days but they only<br />
recruited 5% of the available patients thus<br />
limiting the generalisability of the result.<br />
Extrapolating the lack of clinical benefit in such<br />
a highly selected group of patients to all ARDS<br />
patients may be questionable. What level of<br />
evidence does this study represent? 1 + .<br />
7. What grade of recommendation can I make on<br />
this result alone? B. Steroids do not improve<br />
mortality in late (>7 days) ARDS who still require<br />
mechanical ventilation. <strong>The</strong>re appears to be<br />
some benefit in terms of the secondary<br />
outcomes of duration of ventilation and ICU<br />
stay although late readmission to ICU in the<br />
treatment group makes this non-significant at<br />
180 days.<br />
8. What grade of recommendation can I make<br />
when this study is considered along with other<br />
available evidence? B also as this study is the<br />
only valid randomised controlled trial in this<br />
group of patients. <strong>The</strong> previous study by Meduri<br />
et al was extremely small and lacked internal or<br />
external validity.<br />
9. Should I change my practice because of these<br />
results? Yes. If you use steroids in late ARDS<br />
you should review your practice. <strong>The</strong> further use<br />
of this therapy depends on the interpretation of<br />
the importance of the effects on duration of<br />
ventilation at 28 days. In light of the lack of<br />
effect on other clinically important outcomes and<br />
the presence of some serious side effects such<br />
as myopathies (which may lead to an increased<br />
requirement for re-ventilation during the study<br />
period), this reviewer suggests that this<br />
treatment should not be used for this indication.<br />
10. Should I audit my current practice because of<br />
these results? Yes. If you use steroids you<br />
should consider auditing your results. If you<br />
intend to start using steroids for the ventilatory<br />
benefits you should also audit your results<br />
prospectively including the presence of side<br />
effects such as weakness syndromes, sepsis,<br />
hyperglycaemia etc. and longer term outcomes<br />
such a 180 day mortality, ventilatory status and<br />
ICU stay.<br />
Appraised by: BH Cuthbertson, <strong>Intensive</strong> <strong>Care</strong> Unit,<br />
Aberdeen Royal Infirmary, Aberdeen, Scotland. 44<br />
(0)1224 554580; 08 May <strong>2006</strong><br />
Email: b.h.cuthbertson@abdn.ac.uk<br />
Kill or Update By: 8th May 2008<br />
Reviewer & edited by CC & BT<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
48<br />
CATmaker Reviews continued<br />
Non-Invasive Ventilation in Patients with Acute<br />
Cardiogenic Pulmonary Oedema: A Meta-Analysis<br />
<strong>The</strong> use of CPAP in cardiogenic pulmonary<br />
oedema significantly reduces mortality. Bi-level<br />
ventilation is associated with a non significant<br />
trend towards reduced mortality<br />
Level of Evidence: 1 + (meta-analysis with low<br />
risk of bias)<br />
Citation/s: John V. Peter, et al. Effect of noninvasive<br />
positive pressure ventilation ( NIPPV)<br />
on mortality in patients with acute cardiogenic<br />
pulmonary oedema: a meta-analysis. Lancet <strong>2006</strong>;<br />
367: 1155-63<br />
Lead author: John L Moran<br />
Three-part Clinical Question:<br />
Patients: Patients with cardiogenic pulmonary<br />
oedema.<br />
Intervention: NIPPV (CPAP and Bi-level)<br />
Outcomes: Reduce mortality, need for IPPV, length<br />
of hospital stay and what are the associated failure<br />
rates plus incidence of new MI.<br />
Search Terms: Pulmonary oedema, heart<br />
<strong>The</strong> Evidence:<br />
failure, respiratory insufficiency, positive pressure<br />
ventilation, continuous positive airway pressure,<br />
non-invasive ventilation, non-invasive positive<br />
pressure ventilation, nasal ventilation and BIPAP<br />
<strong>The</strong> Review:<br />
Data Sources: Cochrane Library, Medline, Embase,<br />
Citation Index, hand search, non-English sources,<br />
Am. Coll. Of Physicians (ACP) J Club, DARE<br />
Study Selection: Randomised trials on acute<br />
cardiogenic pulmonary oedema. Comparing<br />
standard therapy (oxygen by facemask, diuretics,<br />
nitrates and other supportive care) with CPAP or<br />
Bi-level NIPPV. Only trials reporting hospital<br />
mortality or need for IPPV were included. Trials<br />
classified into 3 groups: (i) CPAP versus standard<br />
therapy, (ii) bi-level ventilation versus standard<br />
therapy and (iii) CPAP versus bi-level ventilation.<br />
Data Extraction: <strong>The</strong> studies were reviewed by<br />
two investigators, differences in opinion settled by<br />
consensus. <strong>The</strong>y were tested for heterogeneity.<br />
Comparison Mortality RR (95% CI) p-value NNT<br />
CPAP vs standard therapy 0.59 (0.38-0.90) 0.015 10<br />
Bi-level ventilation vs 0.63 (0.37-1.10) 0.11 NS<br />
standard therapy<br />
Bi-level ventilation 0.75 (0.40-1.43) 0.38 NS<br />
vs CPAP<br />
Other results comments: No comment made<br />
on mode of delivery of NIPPV. Study sample sizes<br />
relatively small. Included studies appear of<br />
intermediate quality. No difference in mortality<br />
between CPAP and BiPAP. Significant reduction<br />
in need for IPPV for both CPAP and BIPAP. No<br />
significant difference in hospital stay between<br />
treatment groups. Weak evidence of an increase<br />
in new MI with Bi-level ventilation.<br />
EBM Comments:<br />
1. Do the methods allow accurate testing of the<br />
hypothesis? Yes<br />
2. Do the statistical tests correctly test the results<br />
to allow differentiation of statistically significant<br />
results? Yes<br />
3. Are conclusions valid in light of the results? Yes<br />
4. Did results get omitted, and why? Yes. Studies<br />
not randomised or inappropriate endpoints.<br />
Descriptive studies.<br />
5. Did they suggest areas of further research? Yes.<br />
Role of PEEP/EPAP in relation to increased<br />
incidence of MI. Role of BiPAP in hypercapnic<br />
patients.<br />
6. Did they make any recommendations based on<br />
the results and were they appropriate? Yes. That<br />
the British Thoracic Societies recommendations<br />
are appropriate: CPAP should be used in<br />
patients with cardiogenic pulmonary oedema<br />
who still have hypoxia despite the best medical<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
CATmaker Reviews continued 49<br />
treatment, and reserve the use of bilevel<br />
ventilation for patients in whom CPAP is<br />
unsuccessful.<br />
7. Is the study relevant to my clinical practice? Yes<br />
8. What level of evidence does this study<br />
represent? 1 + (meta-analysis with a low risk of<br />
bias)<br />
9. What grade of recommendation can I make on<br />
this result alone? A<br />
10. What grade of recommendation can I make<br />
when this study is considered along with other<br />
available evidence? A<br />
11. Should I change my practice because of these<br />
results? Yes. If you are not currently using NIV in<br />
the management of cardiogenic pulmonary<br />
oedema, you should consider adding it to your<br />
medical treatment.<br />
12. Should I audit my current practice because of<br />
these results? Yes<br />
Appraised by: Brian Digby, SpR in Anaesthesia &<br />
<strong>Intensive</strong> <strong>Care</strong>, Stirling Royal Infirmary ; 24 April<br />
<strong>2006</strong><br />
Email: briandigby@hotmail.com<br />
Kill or Update By: May, 2011<br />
Reviewed & Edited by CC & BT.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
50<br />
Manpower<br />
It is that time again!<br />
Manpower Census <strong>2006</strong><br />
Dear Colleagues,<br />
I have written about Manpower census on many<br />
occasions. In the past, it has mostly been about the<br />
new online Manpower census that is available on the<br />
<strong>Society</strong>’s website. <strong>The</strong> census runs yearly and yes,<br />
it is time to be counted again.<br />
Manpower census is an important venture of your<br />
<strong>Society</strong> on behalf of the profession. This important<br />
information will be useful in planning for the future of<br />
the speciality as well as in organising the training,<br />
especially as the training of doctors is undergoing<br />
massive changes.<br />
<strong>The</strong> online census will go live later on towards the<br />
end of <strong>July</strong> <strong>2006</strong> and I urge you all to fill in the forms<br />
to make this data gathering venture a success. Due<br />
to a changeover to a new database, this year I<br />
request you to fill in the form again. You will need<br />
your GMC registration number as a unique identifier.<br />
This is to make sure that there are no repetitions.<br />
Periodically, emails will go out to remind colleagues<br />
to fill in the forms, if not done already. I believe the<br />
web-based census will be a success as last year<br />
about one fifth of the forms were filled by those<br />
colleagues who are not yet members of the society.<br />
<strong>The</strong>re will be other initiatives to complement the<br />
manpower census. One example of these initiatives<br />
will be to send out a set of questions to the Linkmen.<br />
I assure the Linkmen that there are only a few<br />
simple questions to fill in. <strong>The</strong> questions are<br />
designed to get basic information about the<br />
workforce in your ICU.<br />
I thank you all for your cooperation and hope to<br />
present meaningful data about intensive care<br />
manpower in my next report.<br />
R Kishen<br />
Chair, Manpower Committee<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Correspondence 51<br />
Aussie Training - A Perspective<br />
from Down-Under<br />
Dear Sir,<br />
I was interested to read the article “Working in a UK<br />
Critical <strong>Care</strong> Department – a Perspective from<br />
Down-Under”, as I am in a similar, albeit reverse<br />
position. Having completed my CCST, 18 months<br />
ago I ventured down-under to work in an Australia.<br />
My first hurdle was the amount of form filling and<br />
applications for various authorities, all of which were<br />
alien to me. I have to say I still only have only a<br />
faint understanding of what they were all for.<br />
Bizarrely I found the easiest thing to do was open a<br />
bank account - I didn’t even need a dollar!<br />
I had not expected to find as many differences in the<br />
UK and Australian medical systems as I did. Some<br />
were trivial differences, such as having to use mmHg<br />
rather than kPa for blood gas measurements, which<br />
was actually a lot harder than I had imagined.<br />
Generic names for drugs were often not used, and<br />
so there was a ‘relearning’ of drug names. I also<br />
discovered that the Australians are even worse at<br />
using three-letter-abbreviations than the Europeans.<br />
Language shouldn’t have been an issue but there<br />
were times I did wonder if we were all speaking in<br />
the same tongue!<br />
Referring to Dr McGloughlin’s comment regarding<br />
the SHO post, I noticed differences in the description<br />
of training levels. Many doctors did not have the<br />
opportunity or expectation to gain practical skills<br />
whilst in the resident (SHO) post. Some UK<br />
graduates who had been SHOs in the UK were<br />
surprised to find themselves in Registrar posts in<br />
Australia, but were certainly able to cope.<br />
You get a better feel for the size of the country living<br />
and working here. With most of the population<br />
clustered around the major cities, you start to look<br />
at the transfer of patients in a different light. For<br />
example, most multi-trauma in Victoria is brought to<br />
one of the trauma hospitals within Melbourne. This<br />
could mean regularly transferring an unstable patient<br />
300km from the east or west, or even 500km from<br />
the north. When you consider some of the distances<br />
to be covered in outback Australia, you develop a<br />
tremendous respect for the air retrieval services<br />
such as the Royal Flying Doctor Service.<br />
Neurosurgery and cardiothoracic surgery are<br />
likewise centralised, which means the families<br />
are also often travelling great distances.<br />
I would thoroughly recommend a period of overseas<br />
training, and it is good to see more formal links<br />
being made through the Australia and New Zealand<br />
<strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>. I have met numerous<br />
Australian doctors who have spent time working in<br />
the UK, and they all have a story to tell regarding<br />
their time overseas. I hope that on my return, I too<br />
can spin a few yarns and sink a few bevvies with<br />
Australian doctors working up-top.<br />
S Blakeley<br />
Senior Registrar <strong>Intensive</strong> <strong>Care</strong><br />
Melbourne, Australia<br />
Having solely worked in a public system with very<br />
little expose to the private sector, I found it strange<br />
coming to a system with such a split public and<br />
private system. I have now seen both the Australian<br />
public and private ICU systems and have formed my<br />
own opinions. However, you come to realise how<br />
relatively shielded you are from the grisly concept of<br />
money as a trainee in the NHS - something which<br />
has its good and bad points!<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
52<br />
Correspondence continued<br />
National Critical Incidents Reporting Scheme<br />
Dear Sir,<br />
National Critical Incidents Reporting Scheme<br />
I read with interest the article by Thomas and<br />
others 1 about the development and analysis of a<br />
database to record critical incidents associated<br />
with intravenous drug administration in critically<br />
ill patients.<br />
<strong>The</strong>re is no mention in this article of the National<br />
Patient Safety Agency’s National Reporting &<br />
Learning System (http://www.npsa.nhs.uk/health/<br />
reporting), which has been rolled out to a significant<br />
majority of NHS Trusts. Anonymised data from all<br />
incidents reported within all participating NHS Trusts<br />
is being sent in a semi-automatic fashion to the<br />
National Patient safety Agency, and it is very likely<br />
that the Trusts involved in this article are already<br />
submitting incident data (including that related to<br />
intravenous drug administration in critical care).<br />
I strongly recommend that the <strong>Intensive</strong> <strong>Care</strong><br />
<strong>Society</strong> works with the National Patient Safety<br />
Agency to improve the reporting rate of adverse<br />
incidents within all UK critical care areas within the<br />
framework of the National Reporting & Learning<br />
System, rather than attempting to develop an<br />
additional isolated database.<br />
Yours sincerely<br />
Dr J Mitchell<br />
Lead Clinician in Clinical Risk<br />
Harefield Hospital<br />
References<br />
1. Thomas AN, Boxall EM, Sabbagh G et al, Journal of <strong>Intensive</strong><br />
<strong>Care</strong> <strong>Society</strong>, <strong>2006</strong> 7: 22-24<br />
A Reply from the Author<br />
Dear Sir,<br />
A national critical incident reporting system for<br />
<strong>Intensive</strong> <strong>Care</strong> would have very significant<br />
advantages for our patients. It would seem<br />
appropriate for this to be run by the National<br />
Patient Safety Agency and this should be the<br />
way forward if:<br />
1. This allowed staff to report incidents with out<br />
having to classify them at the time they are<br />
submitting them.<br />
2. <strong>The</strong> classification of incidents is relevant to<br />
critical care.<br />
3. Information about the nature and frequency of<br />
incidents is provided in a timely manner back to<br />
critical care units in a way that could allow them<br />
to benchmark with other units and to improve<br />
patient care.<br />
I note from the NPSA website that its national<br />
reporting system has been in operation since 2004.<br />
I am a Clinical Director of a large <strong>Intensive</strong> <strong>Care</strong> Unit<br />
in a hospital that submits critical incidents to this<br />
scheme. Unfortunately I have yet to see any feed<br />
back from this NPSA scheme as to the nature of<br />
critical incidents in <strong>Intensive</strong> <strong>Care</strong> or any idea of<br />
their frequency.<br />
<strong>The</strong> database described in our paper 1 provides a<br />
simple system to collect and classify critical incidents<br />
associated with IV Medications. Its use in a small<br />
number of units over a short period of time allowed<br />
us to disseminate information that could improve<br />
patient care. It also allowed the units involved to<br />
compare their levels or reporting with the other<br />
units involved.<br />
<strong>The</strong> process of completing the database has in no<br />
way interfered with a central reporting of incidents<br />
to the NPSA, so there is no reason why the two<br />
systems should not work in parallel. <strong>The</strong> database<br />
is freely available now on the ICS website<br />
(http://www.ics.ac.uk/committees_menu/safety_committee.asp<br />
) and would allow the retrospective or<br />
prospective collection of thousands of medication<br />
related critical incidents in <strong>Intensive</strong> <strong>Care</strong> to allow a<br />
better understanding of these incidents.<br />
It is my understanding that the ICS has already<br />
approached the NPSA to collaborate to improve<br />
the reporting of adverse incidents in critical care.<br />
While waiting for this to result in constructive<br />
dialogue, the use of the database described in our<br />
paper would allow some progress to be made in our<br />
understanding of critical incidents relating to<br />
medication use in <strong>Intensive</strong> <strong>Care</strong>.<br />
Yours sincerely,<br />
Dr Thomas<br />
Clinical Director ICU<br />
References<br />
1. Thomas A.N., Boxall EM, Sabbagh G et al. <strong>JICS</strong> <strong>2006</strong>; 7: 22-24a<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Correspondence continued 53<br />
<strong>The</strong> Editor,<br />
Clearing Suspected Spinal Injury in Unconscious<br />
Patients<br />
Further to the useful guidance provided by Morris<br />
et al 1 , members may be interested in viewing our<br />
imaging protocol that was signed up to by Radiology,<br />
Neurosurgery, A&E and ourselves in 2003. This was<br />
been rolled out to our critical care and neuroscience<br />
networks and is also freely available on the<br />
neuroscience smart group website. <strong>The</strong>re was initial<br />
resistance from peripheral radiologists but once it<br />
was made clear that it was the availability of the<br />
imaging facility 24/7 and that 9-5 reporting would be<br />
adequate things have improved significantly. As a<br />
neuroscience centre we now very rarely have to<br />
repeat scans. We have recently reviewed this<br />
protocol and decided to make no changes,<br />
particularly as a recent paper from the Baltimore<br />
group 2 would support thin slice helical CT with<br />
reconstruction sensitive enough to 'clear' spines.<br />
E Thomas<br />
Lead Consultant for Neuro ICU<br />
<strong>Intensive</strong> <strong>Care</strong> Unit<br />
Derriford Hospital<br />
Plymouth<br />
Reference<br />
1. http://www.ics.ac.uk/downloads/Standards/Clearing%20<br />
the%20spine%20-%20Consensus.pdf<br />
2. Hogan GJ, Mirvis SE, Shanmuganathan K, Scalea TM.<br />
Radiology 2005; 237:106-113<br />
Guidelines for Clearing Suspected Spinal<br />
Injury in Unconscious Patients<br />
<strong>The</strong>se guidelines provide a consistent and largely<br />
evidence-based approach to clearing cervical and<br />
other spinal injuries in unconscious patients.<br />
<strong>The</strong> following guidelines should be utilised as a<br />
means of ‘clearing’ the cervical spine (and where<br />
appropriate thoraco-lumbar spine) in the majority of<br />
unconscious patients.<br />
should be no requirement for additional plain<br />
view x-rays.<br />
Unconscious isolated head injury presenting to A&E<br />
Quad CT<br />
Routine head protocol<br />
Each patient should be assessed and the decision<br />
making regarding imaging must be individualised.<br />
Imaging should be completed as soon as possible<br />
and in all cases within 48 hours of injury (as long as<br />
the patient’s condition allows). <strong>The</strong> images should<br />
be reported by a suitably trained radiologist and the<br />
report clearly documented in the patient’s<br />
contemporaneous clinical notes.<br />
Unconscious polytrauma patient presenting to A&E<br />
Quad CT<br />
Routine head protocol<br />
C-spine @ 1mm slices from cranio-cervical junction<br />
to cervico-thoracic junction (must include posterior<br />
elements of C7 and T1) with sagittal and coronal<br />
reconstructions.<br />
Thorax and abdomen (after oral contrast down<br />
oro-gastric tube in A&E and intravenous contrast in<br />
CT) @ 2.5mm slices allowing sagittal reconstruction<br />
of thoracic and lumbar spines.<br />
This imaging protocol should be able to clear all<br />
bony injuries to the spinal column and there<br />
C-spine @ 1mm slices from cranio-cervical junction<br />
to cervico-thoracic junction (must include posterior<br />
elements of C7 and T1) with sagittal and coronal<br />
reconstruction.<br />
If the patient is going to theatre immediately<br />
from the CT scanner then a lateral c-spine<br />
scanogram and/or the sagittal recons must<br />
accompany the patient to theatre.<br />
Should the rest of the spine need to be imaged, in<br />
the first instance, use departmental plain AP and<br />
lateral radiographs of thoracic and lumbar spine.<br />
Any suspicious areas can then be imaged further<br />
with focused thin slices using the Quad scanner as<br />
above, when circumstances permit.<br />
Patients transferred from other institutions<br />
Assume spine has not been cleared unless these<br />
guidelines have been followed and the results<br />
documented fully in the patients notes.<br />
Clearing ligamentous injury<br />
Utilising the Quad CT as recommended in these<br />
guidelines is likely to exclude all unstable injuries.<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
54<br />
Correspondence continued<br />
If there is a high clinical or radiological suspicion of<br />
an unstable cervical injury then further imaging<br />
should be considered.<br />
This should be individualised following discussion<br />
between all clinicians caring for the patient and may<br />
include MRI, fluoroscopy or static flexion / extension<br />
views.<br />
Supporting documentation:<br />
www.sign.ac.uk/guidelines (go to full text,<br />
guideline No 46 section 5.6<br />
www.east.org/tpg/chap3.pdf<br />
D’Alise MD et al; J Neurosurgery (Spine 1) (1999)<br />
91:54-59,<br />
Mirvis SE; Emergency Radiology (2001) 8: 3-5<br />
Lee JL et al; Emergency Radiology (2001) 8:<br />
311-314<br />
Ptak T et al; Emergency Radiology (2001) 8:<br />
315-319<br />
Blackmore CC et al; Skeletal Radiol (2000) 29:<br />
632-639<br />
E Thomas<br />
Lead Consultant in Neuro <strong>Intensive</strong> <strong>Care</strong><br />
November 2005<br />
(review date January 2008)<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Miscellaneous 55<br />
Industry Membership<br />
<strong>The</strong> <strong>Society</strong> is extremely grateful to the following Industry Members for their continued support.<br />
Corporate Members<br />
Company Members<br />
B Braun Medical Ltd<br />
BOC Medical<br />
Dräger Medical UK Ltd<br />
Edwards Lifesciences<br />
Eli Lilly & Co<br />
Fresenius Kabi<br />
GlaxoSmithKline Ltd<br />
Maquet Critical <strong>Care</strong> Ltd<br />
Novartis Consumer Health<br />
Novo Nordisk<br />
Roche Diagnostics<br />
Trumpf Medical Systems Ltd<br />
Wyeth Pharma<br />
Zeneus Pharma<br />
Arrow International UK Ltd<br />
Astra Zeneca UK Limited<br />
Convatec<br />
Cook UK<br />
Fukuda Denshi<br />
Gambro Hospal<br />
GE Healthcare<br />
Gilead Sciences<br />
Pulsion Medical UK<br />
Smiths Medical<br />
Corporate Member News Page on the ICS Website<br />
Each of the <strong>Society</strong>’s Corporate Members, subject to the <strong>Society</strong>’s editorial control, may publicise relevant<br />
items of news information which are considered to be of interest to the <strong>Society</strong>’s membership. We hope that<br />
our Corporate Members will soon submit items of news, so please do visit the Industry section and<br />
Corporate Member area of the website periodically. Corporate Members who wish to submit any information<br />
concerning new products or clinical trials, product developments or corporate news should email Pauline<br />
Kemp, Administration Manager via Pauline@ics.ac.uk with their item for consideration.<br />
Interested in finding out the benefits of Industry Membership of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>?<br />
Contact: Pauline Kemp, Administration Manager, on 020 7291 0690 or email: Pauline@ics.ac.uk<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
56<br />
ICS Council Members / Ex-Officio Members<br />
<strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong> Council Members<br />
Anna Batchelor (Royal Victoria Infirmary, Newcastle upon Tyne)<br />
Robert Winter (Queen’s Medical Centre, Nottingham)<br />
Carl Waldmann (Royal Berkshire Hospital, Reading)<br />
David Goldhill (Royal National Orthopaedic Hospital, Stanmore)<br />
Sam Waddy (John Radcliffe Hospital, Oxford)<br />
Richard Griffiths (Whiston Hospital, Prescot)<br />
Kevin Gunning (Addenbrooke’s Hospital, Cambridge)<br />
Roop Kishen (Hope Hospital, Manchester)<br />
Bruce Taylor (Queen Alexandra Hospital, Portsmouth)<br />
Peter Macnaughton (Derriford Hospital, Plymouth)<br />
David Menon (Addenbrookes Hospital, Cambridge)<br />
Monty Mythen (University College London)<br />
Jane Harper (Royal Liverpool University Hospital)<br />
President<br />
Council Chair<br />
Executive Committee Chair<br />
Honorary Secretary<br />
IT & Website Editorial Board Chair<br />
President Elect<br />
Honorary Treasurer<br />
Meetings Committee Chair<br />
CritPaL Executive Secretary<br />
Trainees’ Division Chair<br />
Research Committee Chair<br />
Safety Committee Chair<br />
Standards Committee Assistant<br />
to Chair<br />
Manpower Committee Chair<br />
Linkman Co-ordinator<br />
Standards Committee Chair<br />
<strong>JICS</strong> Editor<br />
Education and Training Chair<br />
Meetings Committee Assistant<br />
to Chair<br />
ICS ACCEA Chair<br />
Industry Liaison Council<br />
Representative<br />
Council Member<br />
Ex-officio Members<br />
Louie Plenderleith (Western Infirmary, Glasgow)<br />
Ian Greenway (Morriston Hospital, Wales)<br />
Brian McCloskey (Royal Victoria Hospital, N Ireland)<br />
President, Scottish <strong>Intensive</strong> <strong>Care</strong><br />
<strong>Society</strong><br />
President, Welsh <strong>Intensive</strong> <strong>Care</strong><br />
<strong>Society</strong><br />
President, Irish <strong>Intensive</strong> <strong>Care</strong><br />
<strong>Society</strong><br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
2nd Royal Berkshire Hospital<br />
& Reading University meeting on<br />
Ethics in Critical <strong>Care</strong> Medicine<br />
Venue TBA<br />
November 17th <strong>2006</strong><br />
Introduction Dr A D Lawson, Chairman 09:30<br />
TBA Medical Ethics - Four Principles Virtues and Rights 09:45<br />
Dr Piers Benn Medical Ethics - Utilitarianism 10:30<br />
Coffee 11:00<br />
Dr C Newdick: Decision making by patients and proxies 11:30<br />
Dr C Danbury: Legality of Stopping Treatment 12:00<br />
Dr J Griffiths Post Discharge <strong>Care</strong>: A moral duty? 12:30<br />
Q & A Session on morning 13:00<br />
Lunch 1330<br />
Prof D Oderberg: Killing or Letting Die Morally Different? 14:45<br />
Dr A D Lawson: Futility - a bankrupt concept? 15:15<br />
TBA Should the cost of treatment dictate withdrawal? 15:45<br />
Panel Discussion of Invited Questions 16:15<br />
Tea 16:45 - 17:15<br />
Keynote Debate: Does Industrial Sponsorship bias the ethical 17:15 - 18:00<br />
practice of <strong>Intensive</strong> <strong>Care</strong> Medicine?<br />
Chair: Dr C Waldman<br />
Proposer: Dr Neil Soni, Opposer Prof Monty Mythen<br />
Enquiries to conference organizer: Dr Andrew D Lawson<br />
andrew.lawson@rbbh-tr.nhs.uk Tel: 0118 322 7065<br />
Registration:<br />
Registration forms via website http://icuethics.com/<br />
or Emmahooley2@aol.com<br />
£150 - Consultants, £100 Trainees, Nurses & Students £50
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
58<br />
Advertising & Sponsorship Rate Card<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Advertising & Sponsorship Rate Card continued 59<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
60<br />
Miscellaneous continued<br />
Secretariat Report<br />
Staffing<br />
With further staff changes, I’m pleased to welcome<br />
Michele Moore to our Team as Events and Marketing<br />
Administrator. Michele will be working closely with<br />
our Industry members and building on the existing<br />
relationships and hopefully creating new ones.<br />
Industry is very important to the <strong>Society</strong> in terms of<br />
financially supporting our educational grants and<br />
helping to keep the Meeting registration fees as low<br />
as possible.<br />
We also have Helen Harvey starting as Events and<br />
Committee Administrator and I’m sure those who<br />
attend our Meetings and Seminars will soon meet<br />
and welcome Helen to the <strong>Society</strong>.<br />
We also welcome Stephanie Hooff who will be<br />
temping at the <strong>Society</strong> during the coming months.<br />
Stephanie is covering for Stephanie Antonio during<br />
her extended Leave to Brazil this summer and for a<br />
few months thereafter. We hope having two<br />
Stephanies will not cause too much confusion!<br />
<strong>The</strong>refore, our current staff structure (Shaba Haque<br />
still on maternity leave) is:<br />
Pauline Kemp, Administration Manager<br />
email: pauline@ics.ac.uk<br />
Thomas Heiser, Interim Educational Events Team<br />
Manager (part time)<br />
email: Thomas@ics.ac.uk<br />
Adeeba Sajad, Educational Events Administrator<br />
email: Adeeba@ics.ac.uk<br />
Stephanie Antonio, Membership and Office Support<br />
Administrator<br />
email: Steph@ics.ac.uk<br />
Helen Harvey, Events and Committee Administrator<br />
email: Helen@ics.ac.uk<br />
Jemma Regan, Assistant to Administration Manager<br />
email: Jemma@ics.ac.uk<br />
Christine Wilson, Finance Administrator<br />
email: Christine@ics.ac.uk<br />
Stephanie Hooff, Temporary Office Support Assistant<br />
email: StephTemp@ics.ac.uk<br />
Please visit the Secretariat section of the website for<br />
a summary of ‘who does what’ in the <strong>Society</strong>.<br />
IT<br />
Having successfully moved our IT servers off-site<br />
we aim to start work improving our website in the<br />
coming months. Your suggestions and comments<br />
are always welcome.<br />
Office Move<br />
We aimed to be moving to the new offices in <strong>July</strong>,<br />
but due to unforeseen circumstances beyond our<br />
control, this date has now been pushed back to<br />
August.<br />
P Kemp<br />
Administration Manager<br />
Michele Moore, Events and Marketing Administrator<br />
email: Michele@ics.ac.uk<br />
Trainee Offer<br />
Special Offer for ICS Trainee Members!<br />
<strong>The</strong> <strong>Society</strong> has negotiated a special half price subscription rate to <strong>Intensive</strong> <strong>Care</strong> Monitor<br />
for ICS Trainee Members of only £30 instead of the usual price of £60.<br />
Existing Trainee Members may fill in the form opposite<br />
and return by mail, post or fax to:<br />
INTENSIVE CARE MONITOR<br />
14 Temple Fortune Lane<br />
London<br />
NW11 7UD<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
62<br />
Miscellaneous continued<br />
Forthcoming <strong>Intensive</strong> <strong>Care</strong><br />
<strong>Society</strong> Events <strong>2006</strong> / 2007<br />
17 <strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Focus <strong>2006</strong> Meeting - Organ Donation<br />
<strong>The</strong> <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong> &<br />
<strong>The</strong> British Transplantation <strong>Society</strong><br />
Royal College of Surgeons, London<br />
14 – 15 September <strong>2006</strong><br />
<strong>The</strong> Trainees’ Annual Meeting<br />
<strong>The</strong> Macdonald Burlington Hotel, Birmingham<br />
Please see inside front cover for more details<br />
3 October <strong>2006</strong><br />
Essential information for the ICBTICM Tutor<br />
ICS Seminars at Churchill House<br />
Churchill House, London<br />
14 November <strong>2006</strong><br />
Dealing with Difficulty<br />
ICS Seminars at Churchill House<br />
Churchill House, London<br />
11 – 12 December <strong>2006</strong><br />
<strong>The</strong> State of the Art <strong>2006</strong> Meeting<br />
Hilton London Metropole, London<br />
9 – 11 May 2007<br />
<strong>The</strong> ICS SKINT (9 May)<br />
Annual Spring Meeting (10 / 11 May)<br />
Bournemouth International Centre, Bournemouth<br />
For further information and registration forms please visit<br />
the ICS website Meetings page at www.ics.ac.uk or contact<br />
Tel: 020 7291 0690 Fax: 020 7580 0689 Email: events@ics.ac.uk<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Miscellaneous continued 63<br />
Other Meeting of Interest<br />
<strong>2006</strong><br />
PgCert/PgDip/MSc in Critical <strong>Care</strong><br />
University of Wales College of Medicine<br />
An interdisciplinary, interprofessional distance learning course. <strong>The</strong> course is modular and involves a number<br />
of residential components where key speakers are invited and a variety of teaching methods employed. It<br />
has been running since 2003 and the evaluations to date have demonstrated that it is a suitable course for<br />
all health care professionals with an interest in critical care. Further details by email: msccritcare@cf.ac.uk<br />
26 - 27 June <strong>2006</strong>: ARDS - Mechanisms & Management<br />
<strong>The</strong> Bloomsbury Institute of <strong>Intensive</strong> <strong>Care</strong> Medicine<br />
A major two day conference with an international panel of experts discussing the latest developments.<br />
Registration fee: Consultants: £330 - before May 1st/ after May 1st -£400<br />
Trainees, PAMs. Scientists: £250 - before May 1st/ after May 1st- £300 (includes lunch and refreshments)<br />
Venue: <strong>The</strong> Royal <strong>Society</strong>, 6 - 9 Carlton House Terrace, London , SW1<br />
For further details, please contact:<br />
Brenda Roberts, Bloomsbury Institute of <strong>Intensive</strong> <strong>Care</strong> Medicine, Room 512, 5th Floor, Jules Thorn Building<br />
Middlesex Hospital, Mortimer Street, London W1T 3AA<br />
Tel: 020 7679 9666 Fax: 020 7679 9660 email: b.roberts@ucl.ac.uk<br />
28 - 30 June <strong>2006</strong>: AMBEX <strong>2006</strong>, the Ambulance Service Association's major forum for all<br />
professionals working in pre-hospital and emergency care<br />
Harrogate International Centre, Harrogate<br />
For further details please visit www.ambex.net<br />
4 <strong>July</strong> <strong>2006</strong>: Major Incident Management<br />
<strong>The</strong> Critical <strong>Care</strong> Directorate and the University of Wales College of Medicine have organised a one day<br />
meeting on key aspects of major incident management. Issues presented include: Planning, on-scene<br />
medical management, biological and chemical weapon attacks and psychological support. Lessons learnt<br />
from the most recent terrorist outrages in London will also be discussed.<br />
<strong>The</strong> meeting is presented by an expert faculty at the Millennium Stadium Cardiff. Full details can be obtained<br />
from Gaynor Mathieu email: Gaynor.Mathieu@CardiffandVale.wales.nhs.uk<br />
6 <strong>July</strong> <strong>2006</strong>: Challenges and Dilemmas of the Long Term Critical <strong>Care</strong> Patient<br />
Walkers Stadium, Leicester City Football Club, Leicester, UK<br />
Cost: £75.00 per person including lunch and refreshments<br />
Aims: To review current research and practice in long term ICU care and to generate debate into different<br />
ways to manage long term patients. Also, to challenge current thinking and practice.<br />
During the event, participants will improve their understanding of the management of the long term critical<br />
care patients and consider new ways of working to improve outcomes.<br />
For further details and bookings please contact:<br />
Mr Sam Whitfield. Tel: 0116 2502305<br />
email: sam.whitfield@uhl-tr.nhs.uk<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
64<br />
Miscellaneous continued<br />
6 <strong>July</strong> <strong>2006</strong>: Paediatric <strong>Intensive</strong> <strong>Care</strong> Trainees Meeting<br />
Leeds General Infirmary, Leeds<br />
<strong>The</strong>re in no charge for this meeting. Please email Wendy.Dickinsen@leedsth.nhs.uk to register.<br />
A programme can be downloaded by email to Dickinsen@leedsth.nhs.uk<br />
6-7 <strong>July</strong> <strong>2006</strong>: 5th Evidence Based Peri-Operative Medicine Conference<br />
Savoy Place (IEE), London<br />
Full program, venue and registration details (including on-line booking) available at:<br />
www.ucl.ac.uk/anaesthesia/meetings<br />
11-13 September <strong>2006</strong>: British Association of Critical <strong>Care</strong> Nurses - Conference <strong>2006</strong><br />
Newcastle Racecourse - Newcastle upon Tyne<br />
For further details via www.baccnconference.org.uk<br />
19 September <strong>2006</strong>: PICS Trainee Day<br />
THEME: NEURO-INTENSIVE CARE<br />
Alder Hey Children’s Hospital – Education centre<br />
Full programme available.<br />
For further details please contact Andrew Selby:<br />
Tel: + 44 151 228 4811 X 2555<br />
Fax: + 44 151 252 5771<br />
email: Andrew.Selby@rlc.nhs.uk for more details<br />
20 September <strong>2006</strong>: MASTICS (Midlands & South Trent <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>) - State of the<br />
Art Meeting<br />
<strong>The</strong> Yew Lodge Hotel, Kegworth, Derby.<br />
Click for emails email: Shirley.Goddard@derbyhospitals.nhs.uk for more information<br />
24-27 September <strong>2006</strong>: <strong>The</strong> European <strong>Society</strong> of <strong>Intensive</strong> <strong>Care</strong> Medicine - 19th Annual Congress<br />
CCIB Congress Centre in Barcelona, Spain<br />
Abstract deadline: 15 April <strong>2006</strong><br />
Full details are available from www.esicm.org<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
Notes 65<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>
<strong>Volume</strong> 7 <strong>Number</strong> 2<br />
66<br />
Notes continued<br />
<strong>July</strong> <strong>2006</strong><br />
<strong>The</strong> Journal of the <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong>