SoA abstracts - JICS - The Intensive Care Society
SoA abstracts - JICS - The Intensive Care Society
SoA abstracts - JICS - The Intensive Care Society
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
State of the Art 2010 <strong>abstracts</strong> © <strong>The</strong> <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong> 2011<br />
ICS medal and research abstract presentations<br />
Research Gold Medal Presentations winner<br />
Unravelling the paradox, how inflammation<br />
leads to immuno-suppression and<br />
secondary infection<br />
A Conway Morris University of Edinburgh, Edinburgh, UK<br />
Nosocomial infections occur in 25-35% of patients admitted to intensive<br />
care, 1 similar to rates found in neutropenic patients. 2 Notably the<br />
predominant organisms causing nosocomial infections differ from those<br />
causing community-acquired infections in immuno-competent people. 3<br />
<strong>The</strong> high rates of nosocomial infection, and the specific organisms<br />
involved argue for the influence of host vulnerabilities. However, most<br />
critically ill patients who acquire nosocomial infection are not classically<br />
immuno-suppressed (eg HIV infection or neutropaenia), suggesting that<br />
they suffer from a more subtle, as yet poorly defined, immune dysfunction.<br />
Paradoxically, many illnesses that precipitate intensive care admission are<br />
accompanied by immune hyper-activity. 4<br />
Animal models of sepsis and trauma have implicated the endogenous,<br />
pro-inflammatory molecule C5a in neutrophil dysfunction. 5,6 Due to the<br />
rapid clearance (2-3 minute half life) of C5a from the circulation,<br />
measurement of plasma concentrations gives an imprecise account of<br />
neutrophil exposure to this molecule. 7 However, when C5a binds to its<br />
predominant receptor CD88, the receptor is internalised and surface<br />
expression decreased, 7 with a strong inverse correlation to exposure, so<br />
acting as a proxy marker for C5a exposure. 8<br />
I hypothesised that excessive release of C5a would act to inhibit<br />
neutrophil function in humans, as seen in animal models. 5,6 Second, I<br />
hypothesised that C5a drives a defect in phagocytosis by inhibiting RhoA,<br />
the key mediator of actin polymerisation in complement-facilitated<br />
phagocytosis and that similar defects would be seen in neutrophils from<br />
critically ill patients. Third, I hypothesised that C5a-mediated neutrophil<br />
dysfunction would predict those at greatest risk of nosocomial infection, and<br />
act additively with other immune dysfunctions (monocyte deactivation 9 and<br />
elevated immuno-suppressive regulatory T-cells 10 ) in this manner.<br />
C5a mediates neutrophil dysfunction in ventilator-associated<br />
pneumonia<br />
<strong>The</strong> initial year’s work involved a cohort of 73 critically ill patients with<br />
suspected ventilator-associated pneumonia (VAP). 8 I demonstrated that<br />
these patients had neutrophils that were unable to effectively phagocytose<br />
or produce reactive oxygen species, and these defects correlated<br />
significantly with the marker of C5a exposure, CD88 (Figure 1a). This<br />
relationship was specific to CD88, as there was no correlation with other<br />
markers of neutrophil activation (eg CD11b). However, the neutrophils<br />
retained capacity for tissue toxicity, 8 and patients with confirmed VAP<br />
displayed an intense alveolar inflammation. 11,12<br />
Exploring the mechanism of C5a-mediated neutrophil dysfunction<br />
<strong>The</strong> apparent paradoxical finding of a pro-inflammatory molecule driving<br />
dysfunction required exploration of potential underpinning mechanisms,<br />
occurring in years 2 and 3. Recombinant human C5a (rhC5a) applied to<br />
healthy neutrophils was able to impair phagocytosis, and reproduce the<br />
correlation with CD88 and phagocytosis seen in the patients with VAP8.<br />
C5a inhibited RhoA and actin polymerisation in response to a phagocytic<br />
target, effects which could be prevented by blocking PI3K‰ with the<br />
isoform specific small molecule inhibitor, IC87114 (Figure 1b). 13 Similarly<br />
PI3Kδ inhibition prevented the inhibition of phagocytosis. Granulocytemacrophage<br />
colony stimulating factor (GM-CSF) was able to reverse the<br />
inhibition of RhoA and actin polymerisation and restore phagocytosis when<br />
applied after C5a exposure. 14<br />
<strong>The</strong> correlation of phagocytosis with CD88 was confirmed in<br />
neutrophils obtained from a new cohort of critically ill patients (see<br />
below), and similar inhibition of RhoA and actin polymerisation to that<br />
seen in-vitro was demonstrated, alongside ex-vivo resurrection of<br />
phagocytosis by GM-CSF. 14<br />
C5a-mediated neutrophil dysfunction precedes and predicts<br />
nosocomial infection<br />
<strong>The</strong> VAP study recruited patients at time of clinical diagnosis, and only<br />
included those with a single nosocomial infection. As such I could not<br />
determine whether the neutrophil dysfunction preceded infection, or was<br />
simply an epiphenomenon. In the final year I undertook a further study<br />
examining the prevalence of neutrophil dysfunction in a group of 95<br />
critically ill patients (patients requiring support of ≥1 organ systems for<br />
≥48 hours), taking serial blood samples. C5a mediated neutrophil<br />
dysfunction was determined by measuring surface CD88 expression using<br />
flow cytometry, and occurred in 73% of the patients examined. It occurred<br />
in those with both sterile and septic inflammation. 15 Infection was<br />
determined by pre-defined criteria, in cases of dubiety an expert consensus<br />
panel adjudicated. Patient data was censored from 48 hours before<br />
nosocomial infection occurred to reduce the risk of infection itself causing<br />
the effect seen.<br />
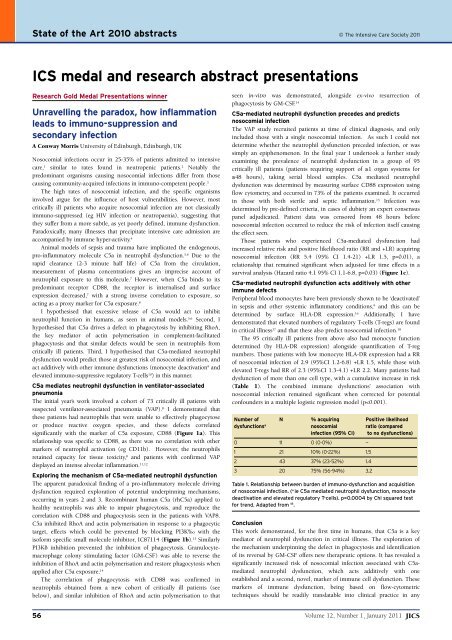
Those patients who experienced C5a-mediated dysfunction had<br />
increased relative risk and positive likelihood ratio (RR and +LR) acquiring<br />
nosocomial infection (RR 5.4 (95% CI 1.4-21) +LR 1.5, p=0.01), a<br />
relationship that remained significant when adjusted for time effects in a<br />
survival analysis (Hazard ratio 4.1 95% CI 1.1-6.8, p=0.03) (Figure 1c).<br />
C5a-mediated neutrophil dysfunction acts additively with other<br />
immune defects<br />
Peripheral blood monocytes have been previously shown to be ‘deactivated’<br />
in sepsis and other systemic inflammatory conditions, 9 and this can be<br />
determined by surface HLA-DR expression. 16 Additionally, I have<br />
demonstrated that elevated numbers of regulatory T-cells (T-regs) are found<br />
in critical illness 17 and that these also predict nosocomial infection. 18<br />
<strong>The</strong> 95 critically ill patients from above also had monocyte function<br />
determined (by HLA-DR expression) alongside quantification of T-reg<br />
numbers. Those patients with low monocyte HLA-DR expression had a RR<br />
of nosocomial infection of 2.9 (95%CI 1.2-6.8) +LR 1.5, while those with<br />
elevated T-regs had RR of 2.3 (95%CI 1.3-4.1) +LR 2.2. Many patients had<br />
dysfunction of more than one cell type, with a cumulative increase in risk<br />
(Table 1). <strong>The</strong> combined immune dysfunctions’ association with<br />
nosocomial infection remained significant when corrected for potential<br />
confounders in a multiple logistic regression model (p
State of the Art 2010 <strong>abstracts</strong><br />
suitably equipped laboratory. Future work will focus on immune profile<br />
guided therapeutic trials for immuno-dysfunction as well as an exploration<br />
of whether the immune defects identified are simply additive or if there is<br />
synergism between them.<br />
Funding and acknowledgements: This work was funded by an academic<br />
clinical training fellowship from the Chief Scientist Office (CAF/08/13), the<br />
Sir Jules Thorn Charitable Trust and NHS Lothian Research and<br />
Development.<br />
Figures for this abstract can be accessed at www.ics.ac.uk/<br />
Meetings_Seminars/main_meetings/gold_medal_ab<br />
References<br />
1. Vincent JL. Nosocomial infection in adult intensive-care units. Lancet 2003;361:2068-77.<br />
2. EORTC International Antimicrobial <strong>The</strong>rapy Project Group. Three antibiotic regimens in<br />
the treatment of infections in febrile granulocytopenic patients with cancer. J Infect Dis<br />
1978;137:14-29.<br />
3. Torres A, Rello J. Update in community-acquired and nosocomial pneumonia. 2009. Am<br />
J Respir Crit <strong>Care</strong> Med 2010;181:782-87.<br />
4. Adibconquy M, Cavaillon J. Stress molecules in sepsis and systemic inflammatory<br />
response syndrome. FEBS Lett 2007;581:3723-33.<br />
5. Huber-Lang MS, Younkin EM, Sarma JV et al. Complement-induced impairment of<br />
innate immunity during sepsis. J Immunol 2002;169:3223-31.<br />
6. Flierl MA, Perl M, Rittirsch D et al. <strong>The</strong> role of C5a in the innate immune response after<br />
experimental blunt chest trauma. Shock 2007;29:25-31.<br />
7. Oppermann M, Götze O. Plasma clearance of the human C5a anaphylatoxin by binding<br />
to leucocyte C5a receptors. Immunology 1994;82:516-21.<br />
8. Conway Morris A, Kefala K, Wilkinson T et al. C5a mediates peripheral blood<br />
neutrophil dysfunction in critically ill patients. Am J Respir Crit <strong>Care</strong> Med 2009;180:<br />
19-28.<br />
9. Döcke WD, Randow F, Syrbe Uet al. Monocyte deactivation in septic patients:<br />
restoration by IFN-gamma treatment. Nat Med 1997;3:678-81.<br />
10. Venet F, Chung C-S, Kherouf H et al. Increased circulating regulatory T cells contribute<br />
to lymphocyte anergy in septic shock patients. <strong>Intensive</strong> <strong>Care</strong> Med 2009;35:678-86.<br />
11. Conway Morris A, Kefala K, Wilkinson TS et al. Diagnostic importance of pulmonary<br />
interleukin-1 beta and interleukin-8 in ventilator-associated pneumonia. Thorax 2010;65:<br />
201-07.<br />
12. Conway Morris A, Kefala K, O’Kane C et al. Ventilator-associated pneumonia is<br />
characterised by elevated neutrophil proteases. (Abstract (oral presentation), ICS State of<br />
the Art Meeting 2009). <strong>JICS</strong> 2010;11:58-59.<br />
13. Conway Morris A, Rossi AG, Walsh TS, Simpson AJ. C5a drives phagocytic dysfunction<br />
via a PI3K delta-dependent inhibition of actin polymerization. (Abstract, ICS State of the<br />
Art Meeting 2009). <strong>JICS</strong> 2010;11:61.<br />
14. Conway Morris A, Rossi AG, Walsh TS, Simpson AJ. Inhibition of Rho-A by C5a leads<br />
to defective neutrophil phagocytosis in critically ill patients. (Abstract (oral presentation),<br />
ESICM Annual Congress 2010). <strong>Intensive</strong> <strong>Care</strong> Med in press.<br />
15. Conway Morris A, Antonelli J, Brittan M et al. C5a mediated neutrophil dysfunction<br />
precedes and predicts nosocomial infection in critical illness. (Abstract, ESICM Annual<br />
Congress 2010). <strong>Intensive</strong> <strong>Care</strong> Med in press.<br />
16. Caille V, Chiche J-D, Nciri N et al. Histocompatibility leukocyte antigen-D related<br />
expression is specifically altered and predicts mortality in septic shock but not in other<br />
causes of shock. Shock 2004;22:521-26.<br />
17. Conway Morris A, Brittan M, Antonelli J et al. Immuno-suppressive regulatory<br />
(CD4 + CD25 + FOXP3 + ) T-cells are elevated in septic and non-septic critical illness. Abstract<br />
submitted for ICS State of the Art Meeting 2010.<br />
18. Conway Morris A, Brittan M, Antonelli J et al. Combined immuno-phenotyping of<br />
neutrophils, monocytes and T-cells enables accurate prediction of the risk of nosocomial<br />
infection. Abstract submitted for ICS State of the Art Meeting 2010.<br />
Research Gold Medal Presentations<br />
Iron is an important factor in pulmonary<br />
physiology<br />
TG Smith, Nuffield Department of Anaesthetics, John Radcliffe Hospital,<br />
Oxford, UK<br />
Scientific background<br />
<strong>The</strong> interaction between hypoxia and pulmonary physiology is central to<br />
intensive care medicine. Physiological responses to hypoxia include an<br />
increase in pulmonary arterial pressure caused by hypoxic pulmonary<br />
vasoconstriction. This phenomenon is important in intensive care<br />
medicine, such as in patients with acute respiratory distress syndrome<br />
(ARDS), 1 as well as in other areas of anaesthesia and medicine. 2 However it<br />
can become pathological – pulmonary hypertension frequently complicates<br />
hypoxic lung disease and worsens patient survival. 3-5 <strong>The</strong> mechanisms<br />
underlying pulmonary responses to hypoxia are poorly understood. This<br />
body of work has investigated these mechanisms and their therapeutic<br />
implications. Our original hypothesis was that the hypoxia-inducible factor<br />
Figure 1. Effect of intravenous iron on systolic pulmonary artery pressure and<br />
serum ferritin in healthy sea-level residents during altitude hypoxia at 4,340<br />
metres. Baseline measurements (Day 0) were made at sea level prior to<br />
ascent to high altitude. Dashed lines and open symbols indicate pre-infusion<br />
measurements, while solid lines and closed symbols indicate post-infusion<br />
measurements. Infusions were given immediately after measurements were<br />
made on the morning of Day 3 (indicated by the dotted vertical line). Black<br />
lines and symbols indicate the group that received an infusion of iron sucrose<br />
200 mg (n=11), while grey lines and symbols indicate the group that received a<br />
placebo infusion (n=11). Infusion with iron reversed much of the elevation in<br />
pulmonary artery systolic pressure caused by hypoxia (p
State of the Art 2010 <strong>abstracts</strong><br />
Figure 2. Effect of venesection on systolic pulmonary artery pressure and<br />
serum ferritin in chronic mountain sickness patients during altitude hypoxia<br />
at 4,340 metres. Eleven patients with chronic moutain sickness were studied.<br />
Measurements shown in this figure are those made prior to any iron or<br />
placebo infusions. <strong>The</strong> black bar indicates the period over which staged<br />
isovolaemic venesection of two litres of blood occurred. Over the following<br />
two weeks, a progressive reduction in ferritin (p
State of the Art 2010 <strong>abstracts</strong><br />
Extracellular myeloperoxidase and markers<br />
of inflammation in the sepsis syndromes<br />
NS MacCallum, National Heart and Lung Institute, Imperial College,<br />
London, UK<br />
Introduction<br />
<strong>The</strong> systemic inflammatory response syndrome (SIRS) and its sequelae<br />
represent a formidable problem, together constituting the leading cause of<br />
morbidity and mortality in critically ill patients. 1-3 SIRS, which is clinically<br />
indistinguishable from sepsis, is seen in association with a variety of noninfective<br />
insults, 4 including surgery necessitating cardiopulmonary-bypass<br />
(CPB). 5 <strong>The</strong> incidence is insult dependent, with 15-27% 6-7 of critically ill<br />
patients suffering from severe sepsis, and up to 96% of ICU admissions 2,5<br />
affected by SIRS.<br />
Neutrophils are activated early in the host immune response, and are<br />
central to the pathogenesis of sepsis/SIRS. 8 <strong>The</strong> neutrophil capacity for<br />
bacterial killing lacks selectivity, despite stringent regulation; and thereby<br />
carries the potential to inflict collateral damage to and destruction of host<br />
tissue, 9 through generation of pro-oxidant mediators. 10<br />
Myeloperoxidase (MPO) generated hypochlorous acid (HOCl) is the<br />
most bactericidal oxidant produced by the neutrophil. HOCl and an array<br />
of oxidant molecules generated by MPO/HOCl 10,11 are implicated in altered<br />
cell signalling, growth arrest and tissue damage. 12,13 Caeruloplasmin (CP)<br />
has been shown to have an affinity for MPO; when bound it compromises<br />
the enzymatic activity of MPO. 14,15 CP therefore plays a potentially key role<br />
in redox regulation, modulating pro-inflammatory responses related to<br />
HOCl under certain defined circumstances. 16,19<br />
Hypothesis<br />
We hypothesised that excess release of extracellular (plasma) MPO,<br />
produces a net increase in HOCl production, resulting in redox imbalance<br />
in favour of pro-oxidant forces. A sub-optimal anti-oxidant response,<br />
specifically CP, places patients at greater risks of developing organ<br />
dysfunction. We investigated the following:<br />
Aims<br />
First, using in vitro experiments we explored the relationship between<br />
MPO protein and activity, MPO-CP binding, and the effect of the latter on<br />
MPO activity.<br />
Second, two populations with SIRS (sepsis and post-CPB) were<br />
recruited in order to elucidate the relationship between MPO exposure,<br />
MPO activity, and CP; to place these within the framework of associated<br />
inflammatory mediators; and to demonstrate their relationship to SIRSinduced<br />
organ dysfunction.<br />
Methods<br />
Research ethical approval: Royal Brompton Hospital Research Ethics<br />
Committee.<br />
Populations: Severe sepsis, n=44; post-CPB, n=52; healthy controls, n=21;<br />
non-cardiac surgical controls, n=8.<br />
Morbidity: Defined within the sequential organ failure assessment score<br />
(SOFA). 20<br />
Biochemical techniques: Spectrophotometry (enzyme kinetics, spectral<br />
absorbance); immunoprecipitation; ELISA; radial-immunodiffusion; gelchromatography;<br />
Western blotting; nondenaturing electrophoresis; gaschromatography–mass-spectroscopy.<br />
Results<br />
Methodology<br />
An assay was developed to determine MPO activity using the chromogen<br />
tetramethylbenzidine, with validation by detection of chromogen oxidation<br />
product by spectral absorbance, and the absence of activity following<br />
immunoprecipitation of MPO from a purified protein solution. Hemeproteins<br />
in the plasma peroxidase-pool 21 contribute to measured activity.<br />
Plasma from healthy controls and patients with SIRS was therefore<br />
subjected to immunoprecipitation of MPO. <strong>The</strong> MPO fraction, 35% of the<br />
measured activity, correlated with total activity (Figure 1a). <strong>The</strong>re was no<br />
relationship between plasma MPO protein and activity.<br />
MPO activity<br />
Inhibited in protein solution by CP in a dose dependent manner (Figure 1b<br />
and c); this was not reproducible in plasma or blood. MPO–CP binding<br />
affinity was confirmed in a purified protein system by (a) gelchromatography;<br />
(b) immunoprecipitation of MPO/CP by anti-CP/MPO<br />
antibody respectively, followed by immuno-detection (ELISA, Western<br />
blot); (c) and nondenaturing electrophoresis. Detection of the MPO–CP<br />
complex in plasma was inconclusive.<br />
MPO exposure<br />
Patients with severe sepsis and those post-CPB were divided into groups<br />
based on cumulative MPO exposure over the 72 hour study period.<br />
Group 1: In severe sepsis greater MPO exposure was associated with an<br />
increase and/or non-resolution in: leukocyte count, CRP, and IL-6. <strong>The</strong>re<br />
was no difference in MPO activity, CP, IL-8, TNF, and IL-10. MPO exposure<br />
was associated with non-resolution of organ dysfunction and increased 3-<br />
chlorotyrosine (a marker of HOCl-induced oxidative damage 22 ) Figure 2a<br />
and b. By contrast, a relative increase in CP was associated with lower MPO<br />
exposure and a decrease in organ dysfunction (1.4 SOFA points). MPO<br />
activity was decreased compared to controls, and demonstrated no<br />
relationship to MPO or CP protein.<br />
Group 2: Post-CPB, greater MPO exposure was associated with an<br />
increase and/or non-resolution in: leucocyte count, CRP, and IL-6, IL-8, and<br />
IL-10; only the former differed between groups. MPO activity and CP<br />
decreased significantly, with no difference between groups, nor discernable<br />
relationship between indices. <strong>The</strong>re was no difference in organ dysfunction<br />
or 3-chlorotyrosine.<br />
Figure 2a and b. Relationship of neutrophil count to plasma myeloperoxidase<br />
protein and activity over time: MPO grouping. Mean –SEM of neutrophil count,<br />
plasma MPO and plasma MPO activity for group A – higher (n=20), group B –<br />
lower (n=20) plasma MPO AUC during the 72 hour study period. Group A had<br />
a greater neutrophil response (p=0.051) and MPO concentration (p
State of the Art 2010 <strong>abstracts</strong><br />
Discussion<br />
In the validated plasma MPO activity assay, the activity due to MPO and the<br />
total measured activity correlated well. <strong>The</strong> proportion of measured activity<br />
attributable to MPO was similar in health and SIRS, despite differing<br />
plasma concentrations of MPO protein. This may reflect a functional<br />
capacity of MPO, supporting a role during normal physiological states. 23-29<br />
CP inhibited MPO activity in solution but not plasma; possibly due to the<br />
presence of endogenous CP, dysfunctional exogenous CP, 30 or plasma<br />
factors. CP binding affinity to MPO was confirmed in protein solution, with<br />
MPO-CP complex visualisation for the first time.<br />
In the SIRS populations studied, MPO was associated with an increase<br />
of inflammatory indices. Greater plasma MPO appears to be detrimental in<br />
terms of non-resolution of organ dysfunction and CRP in severe sepsis, but<br />
exerts no impact on inflammatory indices or morbidity post-CPB. MPO<br />
activity was decreased in both populations, despite leukocyte response and<br />
elevated MPO protein. Post-CPB the activity did not return to pre-operative<br />
levels, a phenomenon not previously documented.<br />
CP appears to neither to modulate MPO activity in SIRS post-CPB, nor<br />
in severe sepsis. Thus, despite in vitro data confirming the ability if CP to<br />
inhibit MPO activity, no such evidence could be demonstrated in patient<br />
plasma. <strong>The</strong> data presented here did not support a role for the modulation<br />
of MPO by CP within 72 hours of onset of the syndromes studied. A rise in<br />
CP was however associated with a decrease in MPO protein in sepsis,<br />
perhaps, in conjunction with its binding affinity, conferring a regulatory<br />
role of the former in the elimination of extracellular MPO protein.<br />
<strong>The</strong> reduced enzymatic capacity of MPO during SIRS may be due to<br />
diminished functional capacity of MPO (eg molecular damage); 31-34<br />
reduction of substrate or co-factor availably; 35 or inhibition. 14,15,33,36-38 MPO<br />
activity may be subject to regulation. However, the evidence of chlorination<br />
indicates that this population may also be either more susceptible to, or<br />
subject to, elevated HOCl-induced oxidative damage. 39 This paradox<br />
possibly relates to substrate availability, 40 a mechanism that would support<br />
the increased production of HOCl.<br />
<strong>The</strong> data highlight further evidence for a regulatory role of MPO<br />
activity. MPO activity levels on resolution of organ dysfunction and<br />
systemic inflammation are similar to, and indeed return to those levels seen<br />
pre-operatively and in health. <strong>The</strong> ‘excess’ MPO detectable in plasma is<br />
enzymatically dysfunctional, retaining an intact epitope detectable<br />
immunologically. Increased release of MPO into plasma may be<br />
physiological, compensating for the limited enzymatic lifespan and<br />
associated molecular damage sustained. <strong>The</strong> mechanism of MPO clearance<br />
remains undetermined. Dysfunctional MPO protein may thus remain in<br />
plasma for a prolonged time period until cleared.<br />
Conclusion<br />
<strong>The</strong> relationship between plasma MPO and its measured activity remains to<br />
be further elucidated. What seems clear from the data presented here is that<br />
plasma MPO protein is not representative of activity in severe sepsis or post-<br />
CPB; and that maintenance of a constant activity, or return to a ‘normal’<br />
activity following resolution of disease process seems to be desirable.<br />
Acknowledgements: This research was generously funded by the British<br />
Heart Foundation through Clinical Research Fellowship. NSM conducted<br />
all experiments over a three year period with PhD supervision by Dr GJ<br />
Quinlan and Professor TW Evans. <strong>The</strong> Royal Marsden Hospital and Dr MB<br />
Hacking for access to surgical control patients. <strong>The</strong> staff from the Unit of<br />
Critical <strong>Care</strong> research group and the Royal Brompton Hospital.<br />
Figures 1a, b and c and 2c can be accessed at www.ics.ac.uk/<br />
Meetings_Seminars/main_meetings/gold_medal_ab<br />
References<br />
1. Angus DC, Linde-Zwirble WT, Lidicker J et al. Epidemiology of severe sepsis in the<br />
United States: analysis of incidence, outcome, and associated costs of care. Crit <strong>Care</strong> Med<br />
2001;29:1303-10.<br />
2. Brun-Buisson C. <strong>The</strong> epidemiology of the systemic inflammatory response. <strong>Intensive</strong> <strong>Care</strong><br />
Med 2000;26 Suppl 1:S64-74.<br />
3. Martin GS, Mannino DM, Eaton S et al. <strong>The</strong> epidemiology of sepsis in the United States<br />
from 1979 through 2000. N Engl J Med 2003;348:1546-54.<br />
4. Bone RC, Balk RA, Cerra FB et al. Definitions for sepsis and organ failure and guidelines<br />
for the use of innovative therapies in sepsis. <strong>The</strong> ACCP/SCCM Consensus Conference<br />
Committee. American College of Chest Physicians/<strong>Society</strong> of Critical <strong>Care</strong> Medicine.<br />
Chest 1992;101:1644-55.<br />
5. MacCallum NS, Gordon SE, Quinlan GJ et al. Abstract 23: <strong>The</strong> Systemic Inflammatory<br />
Response Syndrome Following Cardiac Surgery. Circulation 2007;116<br />
(16_MeetingAbstracts):II_928-.<br />
6. Brun-Buisson C, Meshaka P, Pinton P et al. EPISEPSIS: a reappraisal of the epidemiology<br />
and outcome of severe sepsis in French intensive care units. <strong>Intensive</strong> <strong>Care</strong> Med<br />
2004;30:580-88.<br />
7. Padkin A, Goldfrad C, Brady AR et al. Epidemiology of severe sepsis occurring in the<br />
first 24 hrs in intensive care units in England, Wales, and Northern Ireland. Crit <strong>Care</strong><br />
Med 2003;31:2332-38.<br />
8. Das UN. Critical advances in septicemia and septic shock. Crit <strong>Care</strong> 2000;4:290-96.<br />
9. Marshall JC. Neutrophils in the pathogenesis of sepsis. Crit <strong>Care</strong> Med 2005;33(12<br />
Suppl):S502-5.<br />
10. MacCallum NS, Quinlan GJ, Evans TW. <strong>The</strong> role of neutrophil-derived myeloperoxidase<br />
in organ dysfunction and sepsis. In: Vincent JL, ed. Yearbook of <strong>Intensive</strong> <strong>Care</strong> and<br />
Emergency Medicine: Springer: 2007;173-78.<br />
11. Weiss SJ, Lampert MB, Test ST. Long-lived oxidants generated by human neutrophils:<br />
characterization and bioactivity. Science 1983;222:625-28.<br />
12. Pullar JM, Vissers MC, Winterbourn CC. Living with a killer: the effects of<br />
hypochlorous acid on mammalian cells. IUBMB Life 2000;50:259-66.<br />
13. Vissers MC, Pullar JM, Hampton MB. Hypochlorous acid causes caspase activation and<br />
apoptosis or growth arrest in human endothelial cells. Biochem J 1999;344 Pt 2:443-49.<br />
14. Griffin SV, Chapman PT, Lianos EA et al. <strong>The</strong> inhibition of myeloperoxidase by<br />
ceruloplasmin can be reversed by anti-myeloperoxidase antibodies. Kidney Int<br />
1999;55:917-25.<br />
15. Segelmark M, Persson B, Hellmark T et al. Binding and inhibition of myeloperoxidase<br />
(MPO): a major function of ceruloplasmin Clin Exp Immunol 1997;108:167-74.<br />
16. Baker CS, Evans TW, Haslam PL. Measurement of ceruloplasmin in the lungs of patients<br />
with acute respiratory distress syndrome: is plasma or local production the major source<br />
Respiration 2000;67:533-38.<br />
17. Festa M, Mumby S, Nadel S et al. Antioxidant protection against iron in children with<br />
meningococcal sepsis. Crit <strong>Care</strong> Med 2002;30:1623-29.<br />
18. Gutteridge JM, Quinlan GJ, Mumby S et al. Primary plasma antioxidants in adult<br />
respiratory distress syndrome patients: changes in iron-oxidizing, iron-binding, and free<br />
radical-scavenging proteins. J Lab Clin Med 1994;124:263-73.<br />
19. Pepper JR, Mumby S, Gutteridge JM. Sequential oxidative damage, and changes in ironbinding<br />
and iron-oxidising plasma antioxidants during cardiopulmonary bypass surgery.<br />
Free Radic Res 1994;21:377-85.<br />
20. Vincent JL, Moreno R, Takala J et al. <strong>The</strong> SOFA (Sepsis-related Organ Failure<br />
Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group<br />
on Sepsis-Related Problems of the European <strong>Society</strong> of <strong>Intensive</strong> <strong>Care</strong> Medicine. <strong>Intensive</strong><br />
<strong>Care</strong> Med 1996;22:707-10.<br />
21. Peroxidase activity of hemoproteins released into plasma as sources of oxidative stress in<br />
sepsis: a preliminary report. A60. Annual Congress <strong>Society</strong> of Critical <strong>Care</strong> Medicine;<br />
2007; Orlando, FL, USA. SCCM.<br />
22. Winterbourn CC, Kettle AJ. Biomarkers of myeloperoxidase-derived hypochlorous acid.<br />
Free Radic Biol Med 2000;29:403-09.<br />
23. Claesson R, Karlsson M, Zhang Y, et al. Relative role of chloramines, hypochlorous acid,<br />
and proteases in the activation of human polymorphonuclear leukocyte collagenase. J<br />
Leukoc Biol 1996;60:598-602.<br />
24. Arnhold J. Properties, functions, and secretion of human myeloperoxidase. Biochemistry<br />
(Mosc) 2004;69:4-9.<br />
25. Eiserich JP, Baldus S, Brennan ML et al. Myeloperoxidase, a leukocyte-derived vascular<br />
NO oxidase. Science 2002;296:2391-94.<br />
26. Midwinter RG, Vissers MC, Winterbourn CC. Hypochlorous acid stimulation of the<br />
mitogenactivated protein kinase pathway enhances cell survival. Arch Biochem Biophys<br />
2001;394:13-20.<br />
27. Schoonbroodt S, Legrand-Poels S, Best-Belpomme M et al. Activation of the NF-kappaB<br />
transcription factor in a T-lymphocytic cell line by hypochlorous acid. Biochem J<br />
1997;321(Pt 3):777-85.<br />
28. Schildknecht S, Ullrich V. Peroxynitrite as regulator of vascular prostanoid synthesis.<br />
Arch Biochem Biophys 2009;484:183-89.<br />
29. Evans TJ, Buttery LD, Carpenter A et al. Cytokine-treated human neutrophils contain<br />
inducible nitric oxide synthase that produces nitration of ingested bacteria. Proc Natl<br />
Acad Sci USA 1996;93:9553-58.<br />
30. Sengelov H, Kjeldsen L, Borregaard N. Control of exocytosis in early neutrophil<br />
activation. J Immunol 1993;150:1535-43.<br />
31. Marchetti C, Patriarca P, Solero GP et al. Genetic characterization of myeloperoxidase<br />
deficiency in Italy. Hum Mutat 2004;23:496-505.<br />
32. Nauseef WM, Root RK, Malech HL. Biochemical and immunologic analysis of hereditary<br />
myeloperoxidase deficiency. J Clin Invest 1983;71:1297-307.<br />
33. Galijasevic S, Maitra D, Lu T et al. Myeloperoxidase interaction with peroxynitrite:<br />
chloride deficiency and heme depletion. Free Radic Biol Med 2009; In Press, Corrected<br />
Proof.<br />
34. Chapman AL, Hampton MB, Senthilmohan R et al. Chlorination of bacterial and<br />
neutrophil proteins during phagocytosis and killing of Staphylococcus aureus. J Biol<br />
Chem 2002;277:9757-62.<br />
35. Zhang R, Shen Z, Nauseef WM et al. Defects in leukocyte-mediated initiation of lipid<br />
peroxidation in plasma as studied in myeloperoxidase-deficient subjects: systematic<br />
identification of multiple endogenous diffusible substrates for myeloperoxidase in<br />
plasma. Blood 2002;99:1802-10.<br />
36. Park YS, Suzuki K, Mumby S et al. Antioxidant binding of caeruloplasmin to<br />
myeloperoxidase: myeloperoxidase is inhibited, but oxidase, peroxidase and<br />
immunoreactive properties of caeruloplasmin remain intact. Free Radic Res 2000;33:<br />
261-65.<br />
37. Qian M, Eaton JW, Wolff SP. Cyanate-mediated inhibition of neutrophil myeloperoxidase<br />
activity. Biochem J 1997;326(Pt 1):159-66.<br />
60<br />
Volume 12, Number 1, January 2011 <strong>JICS</strong>
State of the Art 2010 <strong>abstracts</strong><br />
38. Andrews PC, Krinsky NI. A kinetic analysis of the interaction of human<br />
myeloperoxidase with hydrogen peroxide, chloride ions, and protons. J Biol Chem<br />
1982;257:13240-45.<br />
39. Winterbourn CC. Biological reactivity and biomarkers of the neutrophil oxidant,<br />
hypochlorous acid. Toxicology 2002;181-82:223-27.<br />
40. Pascual C, Karzai W, Meier-Hellmann A et al. A controlled study of leukocyte activation<br />
in septic patients. <strong>Intensive</strong> <strong>Care</strong> Med 1997;23:743-48.<br />
What determines poor psychological<br />
outcomes after admission to the intensive<br />
care unit<br />
D Wade*, R Raine*, J Weinman † , R Hardy*, R Tupprasoot ‡ , M Mythen ‡ ,<br />
DCJ Howell ‡<br />
*University College London, UK. † Institute of Psychiatry, King’s College<br />
London, UK. ‡ University College Hospital NHS Foundation Trust, London,<br />
UK<br />
Background<br />
It is well documented that the mental health and quality of life of ICU<br />
survivors may be poor. 1,2 Extreme psychological reactions such as<br />
terror, panic and confusion can occur during ICU admission. 3 Subsequently,<br />
patients may suffer from depression, anxiety and posttraumatic stress<br />
disorder (PTSD). A national guideline 4 requires that intensive care patients<br />
should be assessed for risk of psychological morbidity and offered<br />
rehabilitation. To provide support for patients and improve outcomes, more<br />
evidence is needed about the psychological impact of intensive care.<br />
<strong>The</strong>refore the aims of this research were to assess the prevalence of<br />
psychological morbidity three months after a level 3 intensive care<br />
admission and to identify clinical, psychological and socio-economic<br />
predictors of poor outcome. An additional aim was to investigate the<br />
formation of intrusive memories of intensive care as a key process in the<br />
development of PTSD. <strong>The</strong> work was carried out as an MRC-funded PhD<br />
by DW between September 2007 and September 2010.<br />
Methods<br />
Initially a systematic review was conducted of studies of psychological<br />
morbidity and quality of life following intensive care admission.<br />
Subsequently, a prospective cohort study of 157 consecutive ICU patients,<br />
who received level 3 care, was performed. At ICU discharge, patients were<br />
assessed for mood, stress, delirium and memory distortions. Data about<br />
illness, treatment and drugs in the ICU were collected.<br />
At three months, PTSD, depression, anxiety, quality of life<br />
and socioeconomic circumstances (SEC) were assessed. A total of<br />
100 patients (64%) participated in the follow-up assessment, ensuring that<br />
the study was fully-powered. Statistical analysis included the detection of<br />
univariable associations between predictors and outcomes, multiple<br />
regression to identify independent risk factors and mediation analysis. 5<br />
Finally seventeen cohort participants who developed intrusive memories<br />
of the ICU were interviewed at 4-5 months for a qualitative study.<br />
Results<br />
<strong>The</strong> systematic review of 46 studies found few high quality studies and<br />
estimates of prevalence of PTSD ranged from 0% to 62%. Depression was<br />
found in 3%-47%, and anxiety in 5%-43% of patients. Few risk factors were<br />
reported and evidence for clinical predictors was inconsistent.<br />
<strong>The</strong> cohort study showed that during level 3 ICU admissions the<br />
incidence of mood disturbance, delirium and physical stress was 47%, 66%<br />
and 56% respectively. At three months, the prevalence of PTSD was 27.1%<br />
(CIs: 18.3, 35.9%), of depression 46.3% (CIs: 36.5-56.1%) and of anxiety<br />
44.4% (CIs: 34.6%-54.2%). PTSD was predicted by <strong>The</strong>rapeutic<br />
Intervention Scoring System (TISS) score, number of organs supported,<br />
number of drug groups received in ICU and sepsis markers. C-Reactive<br />
Protein (CRP) at admission (r=0.248, p=0.014), and noradrenaline use<br />
(mean difference=5.1, p=0.033) both predicted PTSD, as did highest CRP<br />
and white cell count (WCC) during admission.<br />
Table 1 shows that the strongest clinical predictor of PTSD was days of<br />
sedation (r=0.268, p=0.008). Benzodiazepine usage was the strongest<br />
clinical predictor of depression (mean difference: 7.44 (CIs: 1.81, 13.07),<br />
p=0.010) and inotrope usage predicted worse anxiety (mean difference:<br />
7.63 (CIs:1.90,13.37), p=0.01). Steroids predicted better physical quality of<br />
life (5.57 (9.96,1.18), p=0.029), as did anaesthetics (4.45(0.04,8.94)).<br />
<strong>The</strong>re was a trend for opioid analgesia to be associated with better<br />
depression, anxiety and mental health scores (7-8 points difference).<br />
Psychological risk factors for PTSD included extreme ICU reactions<br />
such as mood disturbance (r=0.495, p
State of the Art 2010 <strong>abstracts</strong><br />
Strengths of the cohort study include the representativeness of the<br />
sample, achieved by approaching every level 3 patient admitted to ICU over<br />
a ten month period. Participants were assessed at ICU discharge, reducing<br />
risk of recall bias. A comprehensive group of risk factors was explored,<br />
robust methods of outcome assessment were employed and a rigorous<br />
follow-up system ensured a good response rate. Limitations were that the<br />
sample size was not large and many statistical associations were found,<br />
increasing the risk of type 1 errors.<br />
<strong>The</strong> finding that different clinical factors correlate with post-ICU PTSD,<br />
depression and anxiety is of particular interest and the biological<br />
mechanisms behind these observations should be investigated further. This<br />
research also suggests that modifications in clinical practice to reduce the<br />
intensity of ICU interventions, to use inotropes and sedatives judiciously<br />
and prescribe appropriate opiate analgesia, may improve psychological<br />
outcome. In the meantime patients should be routinely assessed for<br />
psychological distress and offered support in ICU and post discharge. A<br />
clinical and psychological intervention based on these findings should be<br />
designed and evaluated in a randomised controlled trial.<br />
References<br />
1. Dowdy DW, Eid MP, Sedrakyan A et al. Quality of life in adult survivors of critical<br />
illness: a systematic review of the literature. <strong>Intensive</strong> <strong>Care</strong> Med 2005;31:611-20.<br />
2. Jackson JC, Hart RP, Gordon SM et al. Post-traumatic stress disorder and post-traumatic<br />
stress symptoms following critical illness in medical intensive care unit patients: assessing<br />
the magnitude of the problem. Crit <strong>Care</strong> 2007;11:R27.<br />
3. Granberg A, Engberg IB, Lundberg D. Patients’ experience of being critically ill or<br />
severely injured and cared for in an intensive care unit in relation to the ICU syndrome.<br />
Part 1. <strong>Intensive</strong> Crit <strong>Care</strong> Nursing 1998;14:294-307.<br />
4. National Institute for Health and Clinical Excellence. Clinical Guideline 83:<br />
Rehabilitation after critical illness. NICE 2009.<br />
5. Baron RM, Kenny DA. <strong>The</strong> moderator-mediator variable distinction in social<br />
psychological research. J Personality Social Psychol 1986;51:1173-82.<br />
6. Ware JE, Sherbourne CD. <strong>The</strong> MOS 36-item short-form health survey(SF-36). 1.<br />
Conceptual framework and item selection. Medical <strong>Care</strong> 1992;6:473-83.<br />
Developing novel renoprotective agents for<br />
the prevention of post cardiac surgery<br />
acute kidney injury<br />
NN Patel*, T Toth † , C Jones*, H Lin*, P Ray ‡ , SJ George*, G Welsh † ,<br />
SC Satchell † , GD Angelini*, GJ Murphy*<br />
*Bristol Royal Infirmary, Bristol, UK. † Southmead Hospital, Bristol, UK.<br />
‡<br />
Weston General Hospital, Weston-Super-Mare, UK<br />
Background<br />
Acute kidney injury (AKI) following cardiac surgery, defined as a >25%<br />
reduction in glomerular filtration rate, is associated with a four-fold<br />
increase in postoperative mortality. Despite the importance of this clinical<br />
problem, our understanding of the underlying processes is poor and there<br />
is no effective treatment. This is a reflection of the poor homology between<br />
rodent models, the mainstay of research into kidney injury, and that which<br />
occurs in humans, and it has been suggested that large animal models of<br />
AKI with closer homology to humans are required if clinical progress is to<br />
be achieved.<br />
<strong>The</strong> aim of this programme of research was:<br />
1. To undertake a systematic review of the evidence from randomised<br />
controlled clinical trials that have evaluated pharmacological agents for<br />
the prevention of AKI post cardiac surgery.<br />
2. To characterise post-cardiopulmonary bypass (CPB) AKI in a novel<br />
porcine recovery model with potentially greater homology to cardiac<br />
surgery patients.<br />
3. To determine the effect of endothelin-A (ET-A) receptor blockade on<br />
post CPB AKI in swine.<br />
4. To determine the effect of phosphodiesterase-5 (PDE-5) inhibition on<br />
post CPB AKI in swine.<br />
Methods<br />
Systematic review<br />
We searched PubMed, Embase and the Cochrane Central Register of<br />
Controlled Trials for randomised controlled trials comparing renoprotective<br />
pharmacological interventions with control in adult patients undergoing<br />
cardiac surgery with cardiopulmonary bypass. We extracted data for<br />
mortality, need for renal replacement therapy (RRT), incidence of AKI, and<br />
creatinine clearance at 24-48 hours. <strong>The</strong> meta-analysis was performed in<br />
line with recommendations from the Cochrane Collaboration and the<br />
Quality of Reporting of Meta-analyses guidelines with standard software.<br />
Porcine recovery model of post-CPB AKI<br />
Plan of investigation<br />
Pigs (n=8 per group) were randomised to the following groups:<br />
Group 1. Sham operation. Pigs underwent a neck dissection under<br />
general anaesthesia.<br />
Group 2. CPB only. Pigs underwent 2.5 hours of CPB.<br />
Group 3. CPB plus sitaxsentan sodium (ET-A antagonist). Pigs<br />
underwent 2.5 hours of CPB. Each pig received an infusion of sitaxsentan<br />
sodium 0.7 mg/kg over 30 minutes, at commencement of CPB.<br />
Group 4. CPB plus sildenafil citrate (PDE-5 inhibitor). Pigs underwent<br />
2.5 hours of CPB. Each pig received an infusion of sildenafil 10 mg over 30<br />
minutes, at commencement of CPB.<br />
Experimental methods<br />
Thirty-two adult female Large White Landrace crossbred pigs weighing 50-<br />
70 kg were used. Minimally invasive CPB was achieved via Smart<br />
Cannulae ® (Smartcanula LLC, Lausanne, Switzerland) placed in the aorta<br />
and right atrium via the right internal carotid artery and external jugular<br />
vein respectively. Heparinisation, priming, temperature, perfusion pressure,<br />
pump flows and acid base balance were managed according to standard<br />
protocols. Total CPB time was 2.5 hours. Sham procedure animals<br />
underwent similar general anaesthesia, surgical dissection and<br />
heparinisation as CPB operated animals. Urine output was measured via a<br />
urethral catheter. Animals were recovered, re-anaesthetised and reevaluated<br />
at 24 hours.<br />
Collection of serum and urine samples and measurement of renal and<br />
endothelial function, oxygenation, and perfusion occured at four time<br />
points: Baseline, the end of CPB, 1.5 hours post CPB and 24 hours post<br />
CPB. Organ harvest was performed prior to euthanasia.<br />
Outcomes<br />
1. Renal function: Creatinine clearance (primary outcome), free water<br />
clearance and fractional sodium excretion were calculated from urine<br />
volumes and serum samples taken at the four specified time points<br />
using standard formulae.<br />
2. Renal injury: H&E stained 5 µm formalin fixed, paraffin embedded<br />
sections were scored for tubular injury by a renal histopathologist<br />
blinded to treatment allocation. Urinary IL-18, albumin and protein<br />
were measured in the urine.<br />
3. Renal endothelial function: Renal blood flow was recorded using a<br />
Transonic flow probe placed on the renal artery via a mini-laparotomy.<br />
Endothelial dysfunction was determined by the change in renal blood<br />
flow in response to a supra-renal aortic infusion of acetylcholine<br />
(0.1-10 µg/kg/min). Cortical perfusion and medullary oxygenation was<br />
measured by cortical surface probes and O 2 sensors connected to a dual<br />
channel tissue monitoring system (Oxylite, Oxford Optronix, Oxford<br />
UK).<br />
4. Mechanisms:<br />
Endothelial injury – immunocytochemistry (ICC) for lectin Dolichos<br />
biflorus agglutinin, Pecam-1 and ve-Cadherin. Nitric oxide (NO)<br />
bioavailability was assessed by measuring urinary nitrate/nitrite<br />
concentration using the Greiss reaction.<br />
Endothelial activation – ICC for endothelin-1, eNOS and iNOS,<br />
Inflammatory cell infiltrate – ICC for MAC-387.<br />
High energy phosphates – will be measured using HPLC of snap frozen<br />
tissue,<br />
Apoptosis – assessed using In-Situ End Labelling (ISEL).<br />
Results<br />
Systematic review<br />
Forty-nine randomised controlled trials involving 4,605 patients were<br />
included. Pharmacological interventions included dopamine, fenoldopam,<br />
62<br />
Volume 12, Number 1, January 2011 <strong>JICS</strong>
State of the Art 2010 <strong>abstracts</strong><br />
Mean (SEM) Sham CPB alone CPB + CPB + P value P value<br />
sitaxsentan sildenafil (sitax) (sildenafil)<br />
Creatinine +22.4 -27.6 +39.7 +19.3 0.010 0.009<br />
clearance Δ 24 hr (13.4) (15.0)* (11.0)** (7.8)**<br />
(mL/min)<br />
Proteinuria Δ 24 +5.36 +29.26 -7.68 -0.2
State of the Art 2010 <strong>abstracts</strong><br />
3. To investigate the effects of flow targeted haemodynamic therapies on<br />
tissue microvascular flow and oxygenation and plasma markers of<br />
inflammation in patients following major abdominal surgery.<br />
4. To investigate changes in sublingual microvascular flow in patients with<br />
sepsis and severe sepsis within six hours of hospital admission and<br />
compare these data to that of healthy volunteers.<br />
5. To investigate the dose related effects of noradrenaline on tissue<br />
microvascular flow and oxygenation in patients with septic shock.<br />
Methods and results<br />
All studies received relevant approvals from the local audit committee,<br />
Research ethics committees and the Medical and Healthcare products<br />
Regulatory Agency as appropriate. In each of the clinical investigations<br />
cutaneous PtO 2 was measured continuously using a Clark electrode<br />
(TCM400, Radiometer, Denmark). Microvascular flow was measured<br />
intermittently using cutaneous laser Doppler flowmetry (MoorLab,<br />
Moor Instruments, UK) and visualised using sublingual sidestream<br />
darkfield imaging (Microscan, Microvision Medical Netherlands). Cardiac<br />
output and DO 2 I were measured continuously using lithium indicator<br />
dilution and pulse power analysis (LiDCOplus, LiDCO Ltd, UK) in<br />
studies 2, 3 and 5 and supra sternal Doppler (USCOM Ltd, Australia) in<br />
study 4.<br />
Study 1: Characterisation of the high-risk surgical population in a<br />
large NHS Trust<br />
Data describing in-patient non-cardiac surgical procedures performed in<br />
our NHS Trust between April 2002 and March 2005 were obtained from<br />
hospital and critical care databases. Healthcare Resource Groups (HRG)<br />
codes were extracted and then ranked according to mortality rates. HRGs<br />
with ≥5% mortality were prospectively defined as high-risk. <strong>The</strong> high-risk<br />
surgical population accounted for 75.4% of deaths in hospital but only<br />
9.3% of admissions. Although the high-risk population accounted for less<br />
than 10% of cases they utilised 23% of in-patient bed days. Only 35.3% of<br />
the high-risk patients were admitted to a critical care unit at any stage after<br />
surgery. Of 294 high-risk patients who died, only 144 (49.0%) were<br />
admitted to critical care at any time. Mortality rates were high amongst<br />
patients admitted to critical care following initial management on a<br />
standard ward (29.9%).<br />
Study 2: Observational study of peri-operative changes in tissue<br />
microvascular flow and oxygenation<br />
Measurements were made prior to and at 0, 2, 4, 6 and 8 hours after major<br />
abdominal surgery. Patients received usual clinical care. Of 25 patients<br />
recruited, two died (8%) and 14 (56%) developed post-operative<br />
complications. In patients who developed complications, sublingual<br />
microvascular flow index (MFI) (small vessels
State of the Art 2010 <strong>abstracts</strong><br />
6. Pearse R, Dawson D, Fawcett J et al. Early goal-directed therapy after major surgery<br />
reduces complications and duration of hospital stay. A randomised, controlled trial<br />
[ISRCTN38797445]. Crit <strong>Care</strong> 2005;9:R687-693.<br />
7. Wilson J, Woods I, Fawcett J et al. Reducing the risk of major elective surgery:<br />
randomised controlled trial of preoperative optimisation of oxygen delivery. BMJ 1999;<br />
318:1099-103.<br />
8. Boyd O, Grounds RM, Bennett ED. A randomized clinical trial of the effect of deliberate<br />
perioperative increase of oxygen delivery on mortality in high-risk surgical patients.<br />
JAMA 1993;270:2699-707.<br />
9. De Backer D, Creteur J, Preiser JC et al. Microvascular blood flow is altered in patients<br />
with sepsis. Am J Respir Crit <strong>Care</strong> Med 2002;166:98-104.<br />
10. Rivers E, Nguyen B, Havstad S et al. Early goal-directed therapy in the treatment of<br />
severe sepsis and septic shock. N Engl J Med 2001;345:1368-77.<br />
11. Landry DW, Oliver JA. <strong>The</strong> pathogenesis of vasodilatory shock. N Engl J Med 2001;<br />
345:588-95.<br />
12. Dellinger RP, Levy MM, Carlet JM et al. Surviving Sepsis Campaign: international<br />
guidelines for management of severe sepsis and septic shock: 2008. Crit <strong>Care</strong> Med 2008;<br />
36:296-27.<br />
Muscle dysfunction in severe sepsis<br />
P S Zolfaghari, University, College London, London, UK<br />
Introduction<br />
Recent evidence suggests mitochondrial dysfunction and subsequent<br />
cellular metabolic shutdown may be important pathophysiological<br />
mechanisms of multi-organ failure. 1-4 This may underlie the profound<br />
muscle dysfunction seen in these critically ill patients. 5<br />
Mitochondria supply adenosine triphosphate (ATP) to meet cell<br />
metabolic demands. By oxidising substrates, the mitochondrial respiratory<br />
chain generates a proton gradient across the inner mitochondrial<br />
membrane (the mitochondrial membrane potential – Δψ m ) that provides<br />
energy to drive ATP synthesis. 6 Cycling of phosphate to form ATP is vital<br />
for muscle function as its accumulation causes a reduction in the force of<br />
contraction. 7 <strong>The</strong> respiratory chain is inhibited/damaged by reactive<br />
species 8 produced excessively in sepsis. 1,9,10 Mitochondrial dysfunction can<br />
also result from lack of substrate, decreased protein turnover, and increased<br />
uncoupled (non-ATP generating) respiration – ‘proton leak’.<br />
Previous studies have examined mitochondrial function ex-vivo, using<br />
isolated mitochondria or homogenised tissue samples. I have extended<br />
this scope by applying new techniques to investigate temporal effects of<br />
sepsis on:<br />
1. Whole animal metabolism and muscle function.<br />
2. Transmembrane potential difference (Δψ m ) in freshly isolated living<br />
skeletal muscle (diaphragm)<br />
3. Mitochondrial proton leak and phosphorylation kinetics.<br />
Methods<br />
Experiments were performed on 30-week male C57-black mice under<br />
Home Office guidelines. Sepsis was induced by intraperitoneal (i.p.)<br />
injection of 20 mL/kg caecal slurry. Two groups of sham animals (fed and<br />
starved) received i.p. 0.9% saline. All animals received subcutaneous 0.82%<br />
saline/5% dextrose (50 mL/kg) at 6 hr and 18 hr. Mice were housed in<br />
metabolic cages to measure whole body oxygen consumption (VO 2 ) and<br />
carbon dioxide production (VCO 2 ).<br />
Echocardiography was performed at 0 hr, 6 hr and 24 hr post-induction<br />
of sepsis under brief (but equi-depth) isoflurane anaesthesia. Core<br />
temperature was also measured.<br />
At 24h, sepsis severity was scored using a panel of clinical variables<br />
based on individual appearance, behaviour and biochemical data. 3 Animals<br />
were then sacrificed, diaphragm muscle removed intact and 1.5 mm wide<br />
strips of muscle dissected and attached to an ergometer force transducer<br />
continuously superfused with oxygenated Krebs’ solution. Maximal tetanic<br />
isometric force and the power generated while imposing length changes<br />
(simulating in-vivo functional movement of the diaphragm) were<br />
measured. 11 Fatigue testing involved measuring power output during one<br />
minute of repetitive length changes, with 2Hz electrical stimulation<br />
corresponding to the mouse’s respiratory rate.<br />
<strong>The</strong> role of the ryanodine receptor in muscle dysfunction was explored<br />
by measuring isometric force generation following exposure to 30 mM<br />
caffeine.<br />
Δψ m was measured in freshly isolated oxygenated diaphragm strips by<br />
multiphoton confocal microscopy using a voltage-dependent fluorescent<br />
probe, tetramethylrhodamine methylester (TMRM) 100nM. 12 Increased dye<br />
fluorescence is indicative of a higher Δψ m .<br />
Changes in Δψ m were explored using modular kinetic analysis of proton<br />
leak and phosphorylation in mitochondria isolated from skeletal muscle. 13<br />
This involved energisation of mitochondria by the Complex II substrate<br />
succinate (together with the Complex I inhibitor, rotenone) in a chamber<br />
allowing simultaneous measurement of oxygen consumption and Δψ m .<br />
Changes in oxygen consumption were measured in the presence (State III)<br />
and absence (State IV respiration) of ADP during alterations in Δψ m<br />
achieved by sequential inhibition of the respiratory chain.<br />
Results<br />
Profound (60-70%) decreases in VO 2 were observed in severely septic mice<br />
within hours, corresponding with development of hypothermia. At 24 hr,<br />
core temperature was 37.5±0.2°C [sham] vs 31.5±1.2°C [severe septic]<br />
(p
State of the Art 2010 <strong>abstracts</strong><br />
References<br />
1. Brealey D, Brand M, Hargreaves I et al. Association between mitochondrial dysfunction<br />
and severity and outcome of septic shock. Lancet 2002;360:219-23.<br />
2. Crouser ED. Mitochondrial dysfunction in septic shock and multiple organ dysfunction<br />
syndrome. Mitochondrion 2004;4:729-41.<br />
3. Brealey D, Karyampudi S, Jacques TS et al. Mitochondrial dysfunction in a long-term<br />
rodent model of sepsis and organ failure. Am J Physiol Regul Integr Comp Physiol 2004;<br />
286:R491-497.<br />
4. Callahan LA, Supinski GS. Sepsis induces diaphragm electron transport chain<br />
dysfunction and protein depletion. Am J Respir Crit <strong>Care</strong> Med 2005;172:861-68.<br />
5. Lanone S, Taillé C, Boczkowski J et al. Diaphragmatic fatigue during sepsis and septic<br />
shock. <strong>Intensive</strong> <strong>Care</strong> Med 2005; 31:1611-17.<br />
6. Duchen MR. Mitochondria in health and disease: perspectives on a new mitochondrial<br />
biology. Mol Aspects Med 2004;25:365-451.<br />
7. Martyn DA, Gordon AM. Force and stiffness in glycreated rabbit psoas fibres. Effect of<br />
calcium and elevated phosphate. J Gen Phsyiol 1992;99:795-816.<br />
8. Brown GC. Regulation of mitochondrial respiration by nitric oxide inhibition of<br />
cytochrome c oxidase. Biochim Biophys Acta 2001;1504:46-57.<br />
9. Haden DW, Suliman HB, Carraway MS et al. Mitochondrial biogenesis restores oxidative<br />
metabolism during Staphylococcus aureus sepsis. Am J Respir Crit <strong>Care</strong> Med 2007;176:<br />
768-77.<br />
10. Boczkowski J, Lisdero CL, Lanone S et al. Endogenous peroxynitrite mediates<br />
mitochondrial dysfunction in rat diaphragm during endotoxemia. FASEB J 1999;13:1637-<br />
46.<br />
11. Stevens ED, Faulkner JA. <strong>The</strong> capacity of mdx mouse diaphragm muscle to do<br />
oscillatory work. J Physiol 2000;522:457-66.<br />
12. Duchen MR, Surin A, Jacobson J. Imaging mitochondrial function in intact cells. Meth<br />
Enzymol 2003;361:353-89.<br />
13. Parker N, Affourtit C, Vidal-Puig A et al. Energization-dependant endogenous activation<br />
of proton conductance in skeletal muscle mitochondria. Biochem J 2008;412:131-39.<br />
14. Kreymann, G, Grosser S, Buggisch P et al. Oxygen consumption and resting metabolic<br />
rate in sepsis, sepsis syndrome and septic shock. Critical <strong>Care</strong> Med 1993;21:1012-19.<br />
15. Peres Bota D, Lopes Ferreira F, Melot C et al. Body temperature alterations in the<br />
critically ill. <strong>Intensive</strong> <strong>Care</strong> Med 2004;30:811-16.<br />
16. Callahan LA, Stofan DA, Szweda LI et al. Free radicals alter maximal diaphragmatic<br />
mitochondrial oxygen consumption in endotoxin-induced sepsis. Free Radic Biol Med<br />
2001;30:129-38.<br />
17. Friedrich O. Critical illness myopathy: what is happening Curr Opin Clin Nutr Metab<br />
<strong>Care</strong> 2006;9:403-09.<br />
18. Zink W, Kaess M, Hofer S et al. Alterations in intracellular Ca2+-homeostasis of skeletal<br />
muscle fibers during sepsis*. Critical <strong>Care</strong> Med 2008;36:1559-63.<br />
Research Free Paper Presentations Winner<br />
Combined immuno-phenotyping of<br />
neutrophils, monocytes and T-cells enables<br />
accurate prediction of the risk of<br />
nosocomial infection<br />
A Conway Morris*, M Brittan*, J Antonelli † , C McCulloch † , IF<br />
Laurenson † , DG Swann † , A Hay † , TS Walsh † , AJ Simpson*<br />
*MRC Centre for Inflammation Research, University of Edinburgh,<br />
Edinburgh, UK. † Royal Infirmary of Edinburgh, Edinburgh, UK<br />
Nosocomial infection is a significant problem in intensive care units and is<br />
thought to be linked to critical illness-associated immune dysfunction. This<br />
study aimed to examine the relationship between three immune cell types<br />
(neutrophils, monocytes and regulatory T-cells) and acquisition of<br />
nosocomial infection.<br />
Ninety-five critically ill patients (patients requiring support of ≥1 organ<br />
systems for ≥48 hours) were recruited within 48 hours of admission to<br />
intensive care. Serial blood samples were taken, and measures made of<br />
markers of neutrophil dysfunction (low CD88 expression 1 ), monocyte<br />
deactivation (low HLA-DR expression 2 ) and levels of immunosuppressive<br />
regulatory T-cells (T-regs). Infection was determined by pre-defined criteria.<br />
Patient data were censored from 48 hours before nosocomial infection<br />
occurred to reduce the risk of infection itself causing the effect seen.<br />
Thirty-three patients developed nosocomial infection. Neutrophil<br />
dysfunction was associated with a relative risk (RR) and Likelihood ratio<br />
(LR) of nosocomial infection of 5.4 (95%CI 1.4-21, LR1.5) compared to<br />
patients without dysfunction, monocyte deactivation an RR of 2.9 (95%CI<br />
1.2-6.8, LR 1.5) and elevated T-regs with an RR of 2.3 (95%CI 1.3-4.1, LR<br />
2.2). Many patients had dysfunction of more than one cell type, with a<br />
cumulative increase in risk (Table). <strong>The</strong> relationship was significant when<br />
adjusted for potential confounders in a logistic regression analysis (p8 units, and coagulopathy and a greater ICU mortality, but did not<br />
directly compare transfused with non-transfused patients.<br />
In order to make this comparison Kaplan-Meier survival estimates were<br />
plotted. Patients transferred/discharged or in ICU over 30 days (the cut-off<br />
in ISOC data collection) were censored. <strong>The</strong> curves were compared using<br />
the log rank test, and a Hazard Ratio (HR) was calculated using Cox<br />
regression, with RBCT as the only covariate. To adjust for potential<br />
confounding a Cox model adjusted for RBCT, Apache II score, and the<br />
presence of coagulopathy was fitted. <strong>The</strong> HR for RBCT in the unadjusted<br />
and adjusted models was compared.<br />
<strong>The</strong> Kaplan-Meier Plot suggested patients receiving RBCT had better<br />
survival. Figure 1 shows the curves separating early and diverging until day<br />
15, after which the numbers at risk (and precision of estimates) was low.<br />
66<br />
Volume 12, Number 1, January 2011 <strong>JICS</strong>
State of the Art 2010 <strong>abstracts</strong><br />
<strong>The</strong> unadjusted HR suggested that receiving RBCT reduced the relative risk<br />
of all cause mortality by 29% (95% CI 11 to 43). After adjusting for<br />
APACHE II score and coagulopathy this association was strengthened<br />
(unadjusted HR 0.71 (95% CI: 0.57 to 0.89); adjusted HR 0.54 (0.43 to<br />
0.68). Our data suggest an association between receiving RBCT and greater<br />
ICU survival. <strong>The</strong>se finding could be explained by residual confounding,<br />
however they are consistent with the results of recent studies that used<br />
more comprehensive statistical adjustment. 4 It is likely that the<br />
combination of these findings and the study cited supports the need for<br />
further large pragmatic trials of RBCT in the critically ill.<br />
Numbers at risk:<br />
Non RBCT 1290 189 67 25 9 4 0<br />
RBCT 633 313 201 130 81 58 6<br />
Log rank x 2 =8.82, p=0.03<br />
Hazard ratio = 0.71 (95% CI 0.57 to 0.89)<br />
Figure 1. Kaplan-Meier survival estimates in patients receiving RBCT and<br />
those not receiving RBCT.<br />
Acknowledgements: This work was done as part of the first author’s<br />
Masters Dissertation. Thanks is owed to the individuals involved in the<br />
original ISOC study, and to Professor Robin Prescott for extracting the data<br />
from the original ISOC dataset.<br />
References<br />
1. Hebert PC, Wells G, Blajchman MA et al. A multicentre, randomized, controlled clinical<br />
trial of transfusion requirements in critical care. N Engl J Med 1999;340:409-17.<br />
2. Vincent JL, Baron JF, Reinhart K et al. Anemia and blood transfusion in critically ill<br />
patients. JAMA 2002;288:1499-507.<br />
3. Corwin HL, Gettinger A, Pearl RG et al. <strong>The</strong> CRIT Study: Anemia and blood transfusion<br />
in the critically ill – Current clinical practice in the United States. Crit <strong>Care</strong> Med<br />
2004;32:39-52.<br />
4. Sakr Y, Lobo S, Knuepfer S et al. Anemia and blood transfusion in a surgical intensive<br />
care unit. Crit <strong>Care</strong> 2010;14:R92.<br />
5. Walsh TS, Stanworth SJ, Prescott RJ et al. Prevalence, management and outcomes of<br />
critically ill patients with prothrombin time prolongation in United Kingdom intensive<br />
care units. Crit <strong>Care</strong> Med 2010; in press.<br />
Long-term effects of organ failure in the<br />
critically ill<br />
NI Lone, TS Walsh<br />
Centre for Population Health Sciences, University of Edinburgh,<br />
Edinburgh, UK<br />
<strong>The</strong> Sequential Organ Failure Assessment (SOFA) score has been shown to<br />
be associated with ICU mortality. 1 However, few studies have investigated<br />
the relationship between SOFA score and long-term mortality. <strong>The</strong> aims of<br />
this study were to report the relationship between organ failure and longterm<br />
mortality in ICU patients, and to investigate if the total burden of<br />
organ failure had an ongoing effect on mortality.<br />
We undertook a secondary analysis of a dataset collected prospectively<br />
for a multicentre cohort study. We excluded those with a neurological<br />
diagnosis and those under 16. Daily SOFA score was calculated<br />
prospectively for each patient and the worst SOFA score during the ICU<br />
stay for each of the five organs was recorded in the dataset. A measure of<br />
total organ failure burden was derived as the sum of the worst SOFA scores<br />
at any time point during the stay. Individual organ SOFA scores were<br />
classified into three categories: 0, 1-2, and 3-4. Total organ failure burden<br />
was categorised into mild (0-5), moderate (6-11) and severe (≥12). Death<br />
status was retrieved by linking the original study dataset to the Scottish<br />
Death Registry database. Short and long-term mortality were defined as<br />
death at three months and five years from ICU admission. A logistic<br />
regression model was used to adjust for the following confounders: age,<br />
sex, and APACHE II score on admission to ICU.<br />
Of 1023 admissions during the study period, 151 (15%) were excluded<br />
(neurological diagnosis n=141). <strong>The</strong> mean age was 59, 380 (44%) were<br />
female, and the mean APACHE II score on admission was 20.3. ICU<br />
mortality was 26%. Short-term mortality was 40%, and long-term mortality<br />
was 58%. In multivariable analyses (n=745 due to missing data),<br />
cardiovascular (p
State of the Art 2010 <strong>abstracts</strong><br />
Mean (SEM) Sham (n=7) CPB alone CPB + Sildenafil P value<br />
(n=7) (n=7)<br />
Creatinine clearance +22.2 (11.6) -29.1 (13.1)* +19.3 (7.8)** 0.009<br />
Δ 24 hr (mL/min)<br />
Urinary IL-18 post 27.5 (13.5) 236.9 (37.0)* 0.02 (0.003)**
State of the Art 2010 <strong>abstracts</strong><br />
presence of sepsis, admission haemoglobin, length of ICU stay and<br />
study centre.<br />
Binary logistic regression was used. Two regression models were fitted,<br />
the first included variables present at admission to ICU and the second<br />
included all ten variables. Additionally, a unifactorial association of each of<br />
the predictor variables with RBCT was estimated to aid interpretation of the<br />
multifactorial models.<br />
Results are shown in Table 1, on the previous page. For baseline data<br />
age, admission Hb, Apache II score and study centre were independent<br />
predictors of RBCT in ICU. <strong>The</strong> second model upheld these predictors and<br />
additionally suggested ICU stay over two days, bleeding in ICU and ICU<br />
coagulopathy as further independent predictors of RBCT. Gender, weight<br />
and sepsis were not significant predictors.<br />
Illness severity, age, admission haemoglobin, presence of coagulopathy<br />
and length of ICU stay have been described previously as independent<br />
predictors of RBCT and/or are biologically plausible. 4,5 <strong>The</strong> apparent<br />
association with study centre was interesting and could have resulted from<br />
case mix. An alternative explanation is variation in clinical practice<br />
between centers.<br />
Acknowledgements: This work was done as part of the first author’s<br />
Masters Dissertation. Thanks is owed to the individuals involved in the<br />
original ISOC study, and to Professor Robin Prescott for extracting the data<br />
from the original ISOC dataset.<br />
References<br />
1. Vincent JL, Sakr Y, Sprung C et al. Are blood transfusions associated with greater<br />
mortality rates Anesthesiology 2008;108:31-39.<br />
2. Sakr Y, Lobo S, Knuepfer S et al. Anemia and blood transfusion in a surgical intensive<br />
care unit. Crit <strong>Care</strong> 2010;14:R92.<br />
3. Walsh TS, Stanworth SJ, Prescott RJ et al. Prevalence, management and outcomes of<br />
critically ill patients with prothrombin time prolongation in United Kingdom intensive<br />
care units. Crit <strong>Care</strong> Med 2010; In Press.<br />
4. Walsh TS, Saleh E-E-D. Anaemia during critical illness. Bri J Anaesthesia 2006;97:<br />
278-91.<br />
5. Chant C, Wilson G, Friedrich JO. Anemia, transfusion and phlebotomy practices in<br />
critically ill patients with prolonged ICU length of stay: a cohort study. Crit <strong>Care</strong><br />
2006;10:R140.<br />
Long-term survival of alcoholic liver<br />
disease following critical care admission: a<br />
national cohort study<br />
AM Shaik-Dawood*, NI Lone † , TS Walsh*<br />
*Edinburgh Royal Infirmary, Edinburgh, UK. † Centre for Population<br />
Health Sciences, University of Edinburgh, Edinburgh, UK<br />
<strong>The</strong> number of patients with alcoholic liver disease (ALD) admitted to<br />
critical care is increasing in line with an increase in alcohol consumption<br />
in the United Kingdom. 1 <strong>The</strong>re is little published literature on long-term<br />
outcomes for ALD patients following intensive care unit (ICU) admission<br />
at a national level. <strong>The</strong> aim of this study was to report long-term<br />
outcomes and resource utilisation for ALD patients requiring ICU<br />
admission in Scotland.<br />
<strong>The</strong> Scottish <strong>Intensive</strong> <strong>Care</strong> <strong>Society</strong> Audit Group (SICSAG)<br />
prospectively collects data on all ICU admissions to all participating ICUs<br />
in Scotland. Data were extracted for all patients admitted during a threeyear<br />
period (1/1/2005 to 31/12/2007) meeting at least one of the<br />
following diagnostic codes: ALD, alcohol dependence (AD), upper gastrointestinal<br />
bleed (GIB), cirrhosis, hepatic encephalopathy, portal<br />
hypertension and liver transplant. We selected the study cohort by<br />
including only patients with a diagnostic code of ALD. In addition, those<br />
with a diagnostic code of alcohol dependence combined with a code<br />
indicating cirrhosis ± complications were included. Sepsis-related and<br />
upper GIB diagnoses were defined by a process of consensus. Survival<br />
analyses were undertaken using the long-rank test to compare Kaplan-<br />
Meier plots. Death status was retrieved by linking the dataset to the<br />
Scottish Death Registry database. <strong>The</strong> shortest period of follow up was<br />
19-months, the longest 57-months. <strong>The</strong>refore 18-month mortality data<br />
was available for all cases.<br />
Of 2872 admissions in the extract, 1699 (59.2%) were excluded<br />
(transplants, isolated AD, unspecified GIB and non-alcoholic liver diseases).<br />
<strong>The</strong> remaining cohort (n=1173) comprised the ALD study cohort, of whom<br />
16 (1.4%) were missing outcome data. <strong>The</strong> mean age was 52.0, 759 (65%)<br />
were male and the mean APACHE II score was 23.3. <strong>The</strong> prevalence of<br />
mechanical ventilation, cardiovascular-support and haemofiltration was<br />
85%, 60% and 19% respectively and 17% received all three. <strong>The</strong> prevalence<br />
of a sepsis-related diagnosis was 48.3% and GIB 25.1%. <strong>The</strong> mean length of<br />
stay was 6.2 (ICU) and 18.3 (hospital) days. Short-term mortality was 42.9%<br />
(ICU), 55.2% (hospital) and long-term mortality was 64.4% (one year),<br />
67.1% (18 months). <strong>The</strong> short-term mortality was higher than the whole<br />
Scottish ICU and hospital mortality between 2005 and 2007.2,3 Eighteenmonth<br />
mortality increased with number of organs supported (chi-square<br />
test-for-trend p
State of the Art 2010 <strong>abstracts</strong><br />
annually. 1 Further costs to the criminal justice system, social care and the<br />
economy bring the total ARH expenditure to approximately £20 billion.<br />
<strong>The</strong>se harms are not gender or age specific and as a result form part of the<br />
caseload for many NHS staff. 2<br />
<strong>The</strong> North West has been identified as having the second highest rates<br />
of admissions to hospital in the UK. 1 This audit was conducted to assess<br />
the impact that ARH have upon an ICU within this area.<br />
Data was collected during an eight week prospective audit from patients<br />
identified by staff as having an ARH. Patients with a significant history of<br />
alcohol excess were also included in this study as it has been shown that<br />
these patients respond less well to treatment. 3 Information was collected<br />
regarding the reason for admission, maximum number of organs supported,<br />
age, diagnosis, gender, postcode, date admitted, whether the ICU admission<br />
was planned or related to trauma, whether self harm was involved, whether<br />
the patient was post operative and the patient outcome.<br />
Of the 200 admissions, 21 were alcohol related; one of which was<br />
planned. <strong>The</strong> mean cost per admission was £5,007.84 for non alcohol<br />
related and £13,457.46 for alcohol related admissions. <strong>The</strong> mean age of<br />
alcohol related admissions was 50 compared to 62 for non alcohol related.<br />
Of the alcohol related admissions, 38% died compared to 10% of non<br />
alcohol related. <strong>The</strong>re were 15 admissions related to trauma, seven were<br />
alcohol related. Fourteen percent of non alcohol related admissions were<br />
admitted on a weekend compared to 62% of alcohol related.<br />
Alcohol played a significant role in the ICU workload over the 8 weeks<br />
studied. ARH patients were younger, were more likely to die during the<br />
admission, be unplanned and be as a result of trauma. Alcohol related<br />
admissions cost considerably more. Further study is required as the sample<br />
size was small.<br />
To reduce the impact that ARH have upon the ICU, further emphasis<br />
needs to be put upon primary prevention such as a minimum price for<br />
alcohol and tighter regulations for sponsorship to decrease both<br />
affordability and awareness. <strong>The</strong>re is no fast acting and simple solution to<br />
this culture of excessive drinking, but it is clear that these significant<br />
monetary and human costs caused by alcohol related harms cannot<br />
continue.<br />
References<br />
1. NHS Confederation and Royal College of Physicians. Too much of the hard stuff: what<br />
alcohol costs the NHS. [Online]. 2010 [Cited 11/07/2010] http://www.nhsconfed.org/<br />
Publications/Documents/Briefing_193_Alcohol_costs_the_NHS.pdf<br />
2. House of Commons Health Committee. Alcohol. Report of first session 2009-2010.<br />
[Online]. 2010 [Cited 11/07/2010] http://www.publications.parliament.uk/pa/<br />
cm200910/cmselect/cmhealth/151/151i.pdf<br />
3. Uusaro A, Parviainen I, Tenhunen JJ, Ruokonen E. <strong>The</strong> proportion of intensive care unit<br />
admissions related to alcohol use: a prospective cohort study. Acta Anaesthesiol Scand<br />
2005;49:1236-40..<br />
Research Poster Presentations winner<br />
Interactions between allogenic red cell<br />
transfusion and cardiopulmonary bypass in<br />
post cardiac surgery acute kidney injury<br />
NN Patel*, H Lin*, T Toth † , C Jones*, P Ray ‡ , SC Satchell † , GI Welsh † , R<br />
Cardigan § , SJ George*, GD Angelini*, GJ Murphy*<br />
*Bristol Royal Infirmary, Bristol, UK. † Southmead Hospital, Bristol, UK.<br />
‡<br />
Weston General Hospital, Weston-Super-Mare, UK. § National Health<br />
Service Blood and Transplant<br />
Acute kidney injury (AKI) post cardiac surgery is associated with mortality<br />
rates approaching 20%. Clinical studies have demonstrated associations<br />
between allogenic red blood cell (RBC) transfusion and AKI in patients<br />
undergoing cardiac surgery, however causality has not been established.<br />
<strong>The</strong> aim of this study was to determine whether transfusion has a causal<br />
effect on the development of AKI in a large animal experimental model of<br />
post cardiopulmonary bypass (CPB) AKI with significant homology to that<br />
which occurs in cardiac surgery patients.<br />
Adult pigs were randomised to undergo Sham procedure, CPB, Sham +<br />
RBC Transfusion or CPB + RBC Transfusion in a factorial model design<br />
with recovery and reassessment at 24 hours.<br />
CPB reduced renal perfusion pressure and the circulating haematocrit<br />
resulting in endothelial injury and activation, increased endothelin-1 and<br />
cortical adenosine expression, global endothelial dysfunction and<br />
vasoconstriction, medullary hypoxia, glomerular inflammatory cell<br />
infiltration and sequestration of activated platelets, proteinuria, tubular<br />
epithelial cell stress and a 47% reduction in creatinine clearance (CrCl), or<br />
a mean reduction of 64.9 mL/min (95% CI 20.2-109.6) at 24 hours.<br />
Transfusion did not cause significant endothelial activation and injury<br />
however it did result in glomerular inflammation and platelet<br />
sequestration, a reduction in cortical microvascular flow, increased<br />
endothelin-1 expression, medullary hypoxia and a reduction of CrCl –<br />
30.53 mL/min (-58.47 to -2.59), p=0.034, at 24 hours. Transfusion in CPB<br />
pigs increased renal perfusion pressure, reduced endothelial injury and<br />
expression of cortical vasoconstrictors attributed to CPB and improved<br />
medullary oxygenation at 24 hours. This was associated with a<br />
reduction in glomerular inflammation, proteinuria and markers of tubular<br />
epithelial stress, although the improvement in CrCl relative to CPB was<br />
not significant (mean difference 33.5 mL/min, 95% CI -13.7 to 80.77,<br />
p=0.141)<br />
In this model RBC transfusion and CPB cause acute kidney injury<br />
via distinct mechanisms. Transfusion reverses some of the pathophysiological<br />
processes attributable to CPB induced oxygen supply<br />
dependency. <strong>The</strong>se findings highlight the complexity of acute kidney<br />
injury and suggest novel therapeutic targets: endothelial dysfunction and<br />
platelet activation.<br />
Research Poster Presentations<br />
Applicability of palliative quality measures<br />
to end-of-life care in ICUs in the UK and<br />
Israel<br />
Up to 90% of patient deaths in ICU involve ‘end-of-life’ decision-making.<br />
Previous studies have demonstrated that there are differences in intensive<br />
care units between and within countries in: patient and family members’<br />
preference for involvement in decisions about end of life care; end-of-life<br />
care practices and the role of health professionals in shared decision<br />
making. 1-4 <strong>The</strong> Department of Health strategy for end-of-life care places<br />
emphasis on conducting timely discussions to allow patients’ wishes to be<br />
met; studies comparing end of life care across countries identify ICUs in<br />
Israel as having higher rates of withholding treatment at end-of-life (the<br />
ETHICUS study 3,4 ). <strong>The</strong> original study team acknowledge that these<br />
differences may be due to religious affiliation of physicians; however, these<br />
data do suggest that there are lessons that can be learnt from colleagues in<br />
Israel regarding the conduct of timely discussions with carers and, where<br />
possible, patients.<br />
Studies have shown that the quality of ICU end-of-life care needs to be<br />
improved. In order to improve the quality of care, some method must be<br />
developed to measure it. An extensive body of work in the United States<br />
(US) has identified a series of Palliative Quality Measures (PQM) for end of<br />
life care in intensive care units. This study examined whether the palliative<br />
quality measures identified in the US apply in Israel and the UK.<br />
<strong>The</strong> study was conducted in three phases:<br />
Phase 1: Medical Record Review (n=84 records) to examine validity,<br />
reliability of the PQM tool in Israel and UK<br />
Phase 2: Focus Group Interviews with ICU Nurses (n=48-54<br />
participants) to examine what is considered as a ‘good death’ in ICUs in<br />
Israel and the UK<br />
Phase 3: Observation of nurse-to-nurse handover (n=120 observations<br />
across six ICUs) to examine verbal communication of PQM.<br />
Data collection is Israel was undertaken in April/May 2010; UK data<br />
collection commenced in November 2010.<br />
References<br />
1. Azoulay E, Pochard F, Chevret S, Adrie C et al. Half the family members of intensive<br />
care unit patients do not want to share in the decision-making process: a study in 78<br />
70<br />
Volume 12, Number 1, January 2011 <strong>JICS</strong>
State of the Art 2010 <strong>abstracts</strong><br />
French intensive care units. Crit <strong>Care</strong> Med 2004;32:1832-38.<br />
2. Pochard F, Azoulay E, Chevret S, Lemaire F et al. Symptoms of anxiety and depression<br />
in family members of intensive care unit patients: ethical hypothesis regarding decisionmaking<br />
capacity. Crit <strong>Care</strong> Med 2001;29:1983-97.<br />
3. Benbenishty J, Ganz FD, Lippert A et al. Nurse involvement in end-of-life decision<br />
making: the ETHICUS study. <strong>Intensive</strong> <strong>Care</strong> Med 2006;32:129-32.<br />
4. Sprung CL, Woodcock T, Sjokvist P et al. Reason, considerations, difficulties and<br />
documentation of end-of-life decisions in European intensive care units: the ETHICUS<br />
study. <strong>Intensive</strong> <strong>Care</strong> Med 2008;34:271-77.<br />
Sodium bicarbonate is as effective as<br />
hypertonic saline for reduction of raised<br />
intracranial pressure after traumatic<br />
brain injury<br />
CP Bourdeaux, JM Brown<br />
Frenchay Hospital, Bristol, UK<br />
In a previous study we demonstrated that 8.4% sodium bicarbonate (HSB)<br />
was effective at reducing raised intracranial pressure (ICP) after severe<br />
traumatic brain injury (TBI). 1 In this randomised controlled trial we<br />
compared the effects of an equiosmolar dose of 8.4% sodium bicarbonate<br />
with our standard treatment of 100mL of 5% sodium chloride (HS) for the<br />
treatment of raised ICP after TBI.<br />
Ethical approval was granted by the research ethics committee for<br />
Wales and the medical and healthcare products regulatory agency approved<br />
the use of 8.4% sodium bicarbonate. Patents were recruited to the trial if<br />
they had suffered severe TBI (GCS 20 mm Hg for >5 minutes) patients were randomised to receive<br />
either HS (100 mL 5% saline) or HSB (85 mL 8.4% sodium bicarbonate).<br />
Patients were studied for six hours after each dose, monitoring ICP,<br />
mean arterial pressure (MAP) and cerebral perfusion pressure (CPP).<br />
Patients could be re-randomised, treated and studied for further episodes<br />
every 24 hours. <strong>The</strong> primary outcome measure was change in ICP<br />
after treatment.<br />
Twenty episodes of raised ICP were studied in 11 patients. Ten episodes<br />
were treated with HS and 10 episodes were treated with HSB. Six patients<br />
had suffered a road traffic collision and five patients had fallen from a<br />
height. Baseline variables were not different between the treatment groups.<br />
Intracranial pressure (mm Hg)<br />
25<br />
20<br />
15<br />
10<br />
Figure 1. Mean intracranial pressure vs time.<br />
Hypertonic saline<br />
Sodium bicarbonate<br />
0 100 200 300 400<br />
Time (minutes)<br />
All patients responded to initial therapy (ICP 20 mm Hg. No patients required a second dose of HSB.<br />
Analysis of the data using a 2 way ANOVA indicates that there was a<br />
statistically significant fall in ICP from baseline at all time points, p
State of the Art 2010 <strong>abstracts</strong><br />
This work confirms the finding of elevated T-regs in human sepsis. It<br />
extends this finding to patients with non-septic critical illness, suggesting<br />
that this is part of a stereotyped counter-regulatory response to systemic<br />
inflammation. It contributes to the growing understanding of immune<br />
suppression among the critically ill.<br />
Funding: This work was funded by the Chief Scientist Office.<br />
Reference<br />
1. Venet F, Chung C-S, Kherouf H et al. Increased circulating regulatory T cells contribute<br />
to lymphocyte anergy in septic shock patients. <strong>Intensive</strong> <strong>Care</strong> Med 2009;35:678-86.<br />
Neutrophil microparticles and their<br />
contents as potential novel biomarkers in<br />
sepsis<br />
J Dalli*, J Radhakrishnan* † , X Yin ‡ , M Mayr ‡ , JC Knight † , C Hinds* † ,<br />
M Perretti*<br />
William Harvey Research Institute, Barts and the London School of<br />
Medicine and Dentistry, London, UK. † Wellcome Trust Centre for Human<br />
Genetics, University of Oxford, Oxford, UK. ‡ King’s College British Heart<br />
Foundation Centre and Centre for Bioinformatics, School of Physical<br />
Sciences and Engineering, London, UK<br />
Microparticles were originally described as platelet dust, but it is now<br />
recognised that they are more than inert by-products of cellular<br />
activation. 1,2 Studies conducted in a number of inflammatory conditions<br />
have shown that plasma levels of neutrophil derived microparticles are<br />
elevated in these patients, suggesting that they might be playing an<br />
important pathogenic role. To date, very little is known about the<br />
contents of neutrophil-derived microparticles. We therefore analysed the<br />
protein content of microparticles derived from activated human<br />
neutrophils.<br />
First neutrophils were stimulated with 1 mmol fLMP under two<br />
distinct conditions, either in suspension or post adhesion to human<br />
umbilical endothelial cells. Microparticles were extracted from<br />
supernatant using ultracentrifugation and then subjected to proteomic<br />
analysis (liquid chromatography followed by mass tandem spectrometry).<br />
Among the many candidates (shared or unique for each population) two<br />
proteins differentially expressed between the two groups and two that<br />
were equally expressed were identified by Western blotting and flow<br />
cytometry. We then proceeded to analyse protein expression in plasma<br />
microparticles obtained from healthy volunteers and patients suffering<br />
from sepsis recruited to the Genomic Advances in Sepsis (GAinS) study.<br />
<strong>The</strong> initial proteomic analysis showed that there were over 600<br />
different proteins present in these microstructures of which more then<br />
200 were significantly enriched between the two populations of<br />
stimulated neutrophils. Western blotting and flow cytometry confirmed<br />
the presence of ceruloplasmin and alpha-2-macroglobulin in plasmaderived<br />
microparticles and demonstrated differential microparticle<br />
associated protein expression between healthy volunteers and patients<br />
with sepsis (n=10; P
State of the Art 2010 <strong>abstracts</strong><br />
TACE activity — a potential indicator of<br />
monocyte inflammatory status during<br />
sepsis<br />
DJP O’Callaghan, KP O’Dea, AJ Scott, M Takata, AC Gordon<br />
Imperial College, London, UK<br />
<strong>The</strong> immune response during sepsis is comprised of both a systemic<br />
inflammatory response syndrome (SIRS) and a compensatory antiinflammatory<br />
response syndrome (CARS). Monocytes can display an<br />
altered response status, eg a state of priming or tolerance, when challenged<br />
with an inflammatory stimulus. <strong>The</strong>se states, as measured using in-vitro<br />
assays, may be considered representative of those occurring in SIRS and<br />
CARS respectively.<br />
Tumour necrosis factor-α (TNF) converting enzyme (TACE) is<br />
responsible for the shedding of membrane proteins, including TNF and its<br />
receptors, and is expressed on monocytes. 1 Selective substrate shedding<br />
can have opposing effects, potentially allowing TACE to dictate monocyte<br />
inflammatory balance.<br />
To determine TACE activity within a two-hit lipopolysaccharide (LPS)<br />
model, human monocytes were isolated from whole blood via density<br />
gradient centrifugation and magnetic activated cell sorting utilising CD14<br />
positive bead selection. Cells were re-suspended and placed in nonadhesive<br />
conditions, with variable doses of LPS (low dose 1 ng/mL, high<br />
dose 1 µg/mL, and nil as control) for 16 hours.<br />
n=5 for all groups, data display as mean ± standard error. For each group:<br />
grey bar represents baseline activity afer 16 hour pre-treatment, black bar<br />
represents activity after LPS 1μg/mL for one hour.<br />
Monocytes were washed and exposed to a further LPS stimulus<br />
(1 µg/mL for one hour) before having their TACE activity quantified using<br />
a cell based fluorometric catalytic activity assay. 2 TACE expression levels<br />
were determined via flow cytometry. A t-test was used for analysis.<br />
LPS stimulation induced up-regulation of TACE activity in controls and<br />
in the low-dose LPS group. In the high-dose LPS group baseline TACE<br />
activity remained elevated and did not increase on further stimulation.<br />
<strong>The</strong>re were no significant differences in TACE expression after pretreatment<br />
between groups.<br />
<strong>The</strong>se findings suggest that TACE has a memory of previous LPS<br />
exposure at two levels: activity is higher and cannot be re-induced.<br />
Furthermore monocyte inflammatory status can be assessed at the level<br />
of altered cellular protein processing activity, suggesting TACE activity<br />
may be a novel and useful indicator of such status during the course<br />
of sepsis.<br />
References<br />
1. Black R, Rauch C, Kozlosky C et al. A metalloproteinase disintegrin that releases<br />
tumour-necrosis factor-alpha from cells. Nature 1997;385:729-33.<br />
2. Alvarez-Iglesias A, Wayne G, O’Dea KP et al. Continuous real-time measurement of<br />
tumour necrosis factor-a converting enzyme activity on live cells. Lab Invest<br />
2005;85:1440-48.<br />
Prevention of post-cardiopulmonary<br />
bypass acute kidney injury and endothelial<br />
dysfunction using sitaxsentan sodium, an<br />
endothelin-a receptor antagonist<br />
NN Patel*, T Toth † , C Jones*, H Lin*, P Ray ‡ , SJ George*, G Welsh † , SC<br />
Satchell † , GD Angelini*, GJ Murphy*<br />
*Bristol Royal Infirmary, Bristol, UK. † Southmead Hospital, Bristol, UK.<br />
‡<br />
Weston General Hospital, Weston-Super-Mare, UK<br />
Acute kidney injury (AKI) post cardiac surgery is associated with mortality<br />
rates approaching 20%. Our objective was to characterise post cardiopulmonary<br />
bypass (CPB) AKI in an animal model with significant<br />
homology to cardiac surgery patients and to assess the effect of Sitaxsentan<br />
Sodium, an endothelin-A receptor antagonist on these changes.<br />
Adult White-Landrace pigs (50-70 kg, n=21) were randomised to<br />
undergo either: a) sham procedure, b) 2.5 hours of CPB, or c) 2.5 hours of<br />
CPB + sitaxsentan sodium (0.7 mg/kg). Perfusion pressure and hydration<br />
were standardised. Endpoints included serial functional and biochemical<br />
measures of AKI. All pigs were recovered for 24 hours prior to in-vivo<br />
measurement of renal endothelial function, nephrectomy and histological<br />
assessment.<br />
Mean (±95% CI) Sham CPB alone CPB + Sitaxsentan p value<br />
(n=7) (n=7) (n=7)<br />
Creatinine clearance +22.4 -27.6 +39.7 0.010<br />
Δ 24 hrs (mL/min) (-10.4, +55.3) (-64.4, +9.1)* (+9.3, +70.2)**<br />
Proteinuria Δ +5.36 +29.26 *-7.68
State of the Art 2010 <strong>abstracts</strong><br />
Pharmacological therapies for the<br />
prevention of acute kidney injury following<br />
cardiac surgery: a systematic review<br />
NN Patel, CA Rogers, GD Angelini, GJ Murphy<br />
Bristol Royal Infirmary, Bristol, UK<br />
Post cardiac surgery acute kidney injury (AKI) is common, is associated<br />
with a significant increase in morbidity and mortality. We aimed to<br />
systematically review randomised trials that assessed the renoprotective<br />
utility of pharmacological agents in patients undergoing cardiac surgery.<br />
A systematic review of all randomised trials comparing renoprotective<br />
pharmacological interventions with control in patients undergoing cardiac<br />
surgery with cardiopulmonary bypass was undertaken.<br />
47 randomised controlled trials involving 3942 patients were included.<br />
Pharmacological interventions included dopamine, fenoldopam, calcium<br />
channel antagonists, natriuretic peptides, diuretics, and N-acetylcysteine.<br />
Most trials were of poor quality, with small sample sizes, under reporting<br />
of randomisation procedure, allocation concealment and method of<br />
blinding. <strong>The</strong>re was marked variation in interventions being compared,<br />
populations receiving the intervention and outcomes being measured.<br />
No pharmacological intervention was associated with a significant<br />
reduction in mortality or incidence of AKI. Fenoldopam and Atrial<br />
Natriuretic Peptide (ANP) were associated with a 70% (NNT 21, 95% CI<br />
11.3, 83.0) and 73% (NNT 14, 95% CI 8.6, 81.0) reduction, respectively,<br />
in the need for RRT. Fenoldopam and sodium nitroprusside (SNP) were<br />
associated with a significant increase of 26.04 mL/min (95% CI 18.94,<br />
33.15) and 6.60 mL/min (95% CI 2.41, 10.79), respectively in creatinine<br />
clearance at 24-48 hr, whereas dopamine was associated with a significant<br />
reduction (-4.26 mL/min, 95% CI -7.14, -1.39).<br />
Vasodilatory agents, such as fenoldopam and ANP show evidence of<br />
renoprotection in patients undergoing cardiac surgery. Evidence does<br />
not support the use of dopamine, diuretics or N-acetylcysteine. Further<br />
studies evaluating the effect of novel renoprotective strategies on<br />
clinical outcomes in adequately powered randomised controlled trials<br />
are required.<br />
Genetic polymorphism of the beta-2<br />
adrenoreceptor may affect alveolar fluid<br />
clearance and mortality in the acute<br />
respiratory distress syndrome<br />
W Backman*, Z Puthucheary † , J Skipworth † , J Rawal † , J Palmen † , M Hill † , S<br />
Humphries † , R Chambers † , H Montgomery* †<br />
*University College London Medical School, London, UK. † University<br />
College London, London, UK<br />
Acute respiratory distress syndrome (ARDS) is defined by the acute<br />
onset of non-cardiogenic pulmonary oedema and consequent hypoxaemia.<br />
Impaired alveolar fluid clearance (AFC) has been postulated to play<br />
a key pathogenenic role. AFC is mediated by apical membrane epithelial<br />
sodium channels (ENaC) and basal membrane Na + /K + ATPase,<br />
upregulated by the intracellular signalling molecules cAMP. cAMP levels<br />
rise with β2 adrenoceptor (β2R)and type 2A adenosine receptor<br />
(A 2A R) stimulation.<br />
Adenosine is catabolised by adenosine deaminase (ADA). Single<br />
nucleotide polymorphisms (SNPs) exist in the genes for A2AR, ADA, and<br />
β2R. <strong>The</strong> β2R rs1042717 SNP (G→A) is associated with β2R<br />
desensitisation. We aimed to identify a role for AFC in human ARDS by<br />
seeking association of genetic variation in β2R, A 2A R and ADA with the<br />
development of ARDS or mortality in ARDS cases.<br />
DNA samples were collected from 111 ARDS patients and 72 ICU<br />
control patients and genotyped using a PCR sequencing detection system<br />
with custom-made probes. No association was found between ADA SNPs<br />
rs244076 (p=0.28) and rs11086932 (p=0.188), the A2AR SNP rs5751876<br />
(p=0.698) or the β2R SNP rs1042717 (p=0.68), and the presence of ARDS<br />
nor (using a dominant allele model) with ARDS-related mortality.<br />
However, a trend for a mortality-association was noted with the β2R SNP<br />
(p=0.075) (Figure 1). Such an association of a marker of adrenoceptor<br />
desensitization with improved outcome would be consistent with recent<br />
data from the BALTI trial investigators – where beta-adrenoceptor<br />
activation may be associate with an excess ARDS mortality.<br />
% mortality<br />
45<br />
40<br />
35<br />
30<br />
25<br />
20<br />
15<br />
10<br />
5<br />
0<br />
GG<br />
AG/AA<br />
Expected<br />
Observed<br />
Figure 1. AG/AA genotype of β2R tends towards decreased mortality<br />
compared to GG. Expected (overall) mortality: 31%. GG mortality: 38.6%.<br />
AG/AA mortality: 18.5%. p=0.075 by Chi-square test for independence.<br />
No specific therapies (other than those which are supportive) are yet<br />
available which influence the development of ARDS or outcome from it.<br />
Our results show a trend in mortality with β2R desensitisation. Further<br />
studies with greater numbers (likely necessitating international<br />
collaborations) are necessary to confirm the importance of genetic control<br />
of alveolar fluid clearance in ARDS.<br />
<strong>The</strong> relationship between agitation and<br />
pain during physiotherapy in intensive care<br />
L Salisbury*, K Everingham † , P Lapinlampi ‡ , I Cornwall † , F Frame § ,<br />
T Walsh †<br />
*University of Edinburgh, Edinburgh, UK. † NHS Lothian, Edinburgh, UK.<br />
‡<br />
GE Healthcare, Helsinki, Finland. § University of Leicester, Leicester, UK<br />
<strong>The</strong> occurrence and causes of distress in critically ill patients are not well<br />
described or understood. Identified stressors include physiotherapy, 1,2 but<br />
no standards for management of sedation or analgesia during<br />
physiotherapy exist. Recent evidence supporting routine ICU management<br />
at ‘lighter’ levels of sedation potentially increases the importance of<br />
interventions to avoid distress during interventions such as physiotherapy.<br />
<strong>The</strong> aim of this study was to explore the relationships between agitation<br />
and pain during physiotherapy.<br />
A prospective observational study was undertaken. Patients admitted to<br />
the ICU requiring mechanical ventilation and physiotherapy were recruited<br />
into the study. A single session of physiotherapy was observed by an<br />
independent assessor. Agitation was measured using the Richmond<br />
Agitation Sedation Scale (RASS) and pain using the Behavioural Pain Scale<br />
(BPS). <strong>The</strong> RASS and BPS were collected immediately prior to the<br />
commencement of physiotherapy (Baseline) and after each treatment<br />
intervention undertaken during the single physiotherapy session.<br />
Spearman’s rank correlation coefficients were undertaken to explore the<br />
relationships between baseline RASS and BPS scores and the change in and<br />
worse scores of RASS and BPS during the physiotherapy session.<br />
Forty-nine patients were recruited into the study (32 males; age<br />
57.4±13.9 years; APACHE II 22.5±6.2; physiotherapy duration<br />
14.9±4.7 mins; sedation received for 24 hours prior to physiotherapy<br />
74<br />
Volume 12, Number 1, January 2011 <strong>JICS</strong>
State of the Art 2010 <strong>abstracts</strong><br />
128.7±126.5 mL; opiates received for 24 hours prior to physiotherapy<br />
39.1±37.3 mL; ICU admission to study 100.9±97.6 hours). Table 1<br />
summarises the Spearman Rank correlation coefficients.<br />
Table 1. Spearman Rank correlation coefficients<br />
Weak associations were found between baseline RASS and BPS scores<br />
and subsequent RASS and BPS scores during a single physiotherapy<br />
session, with the exception of the association between baseline RASS and<br />
worse RASS score during physiotherapy.<br />
In patients who are mechanically ventilated and receiving<br />
physiotherapy their baseline RASS was moderately associated with their<br />
worse RASS score during physiotherapy. This indicates that a patient’s<br />
conscious level at baseline is likely to increase during a single session of<br />
physiotherapy. As a result physiotherapists should consider whether<br />
patients at ‘lighter’ levels of sedation may require a bolus prior to<br />
commencing physiotherapy to prevent agitation during the treatment<br />
session. More work is required exploring the measurement and<br />
management of pain during physiotherapy in intensive care.<br />
References<br />
1. Novaes et al. <strong>Intensive</strong> <strong>Care</strong> Med 1999;25:1421-26.<br />
2. van de Leur et al. Crit <strong>Care</strong> 2004;8:R467-R473.<br />
Treating delayed gastric emptying in<br />
critical illness: metoclopramide,<br />
erythromycin and bedside (Cortrak)<br />
nasointestinal tube placement<br />
S Taylor, A Manara, J Brown<br />
Frenchay Hospital, Bristol, UK<br />
Baseline RASS<br />
Baseline BPS<br />
Change in RASS during physiotherapy 0.27 0.24<br />
Worse RASS during physiotherapy 0.65 0.17<br />
Change in BPS during physiotherapy 0.35 0.10<br />
Worse BPS during physiotherapy 0.39 0.26<br />
Nasointestinal feeding can overcome delayed gastric emptying common to<br />
critical illness. This improves outcome associated with early enteral<br />
nutrition but current methods of tube placement have failed to gain<br />
widespread success or use. 1 We determined whether the<br />
electromagnetically-guided nasointestinal tube (EGNT-Cortrak) system<br />
was effective in improving enteral feed retention compared to nasogastric<br />
feeding plus prokinetics.<br />
In ICU patients with gastric residual volumes >200 mL we compared<br />
two treatment cohorts: a) IV metoclopramide±erythromycin; or b)<br />
Nasointestinal feeding when EGNT became available. We retrospectively<br />
determined placement success, feed retention and gastric residual volumes.<br />
Of 69 EGNT placements in 62 patients, 87% reached the small<br />
intestine. Enteral fluid input rose in all groups from ~700 mL pretreatment<br />
to >1600 mL d10. In contrast, more feed was retained by the<br />
EGNT group (metoclopramide: d1-3, 5-7; p=0.0001-0.02; erythromycin:<br />
d1-2, 6-8; p=0.006-0.041) despite higher gastric residual volumes<br />
(metoclopramide: pre-treatment day 2+1 and d2-3, 5; p=0.0001-0.03;<br />
erythromycin: pre-treatment d2+1 and d2-4; p0.0002-0.04).<br />
<strong>The</strong> median percentage of the enteral nutrition goal retained d1-10<br />
was higher following EGNT (80-100%) than metoclopramide (n=58,<br />
40-87%: days 1-2, 5-7, p†0.018) or erythromycin (n=38, 48-98%; days 1<br />
and 5, p
T he <strong>Intensive</strong> Car e <strong>Society</strong><br />
State of the Art 2010 <strong>abstracts</strong><br />
Pre-alarm ward round Post-alarm ward round<br />
intervention<br />
intervention<br />
Total alarms Alarms/bed/hour Total alarms Alarms/bed/hour<br />
Median<br />
Median<br />
(interquartile<br />
(interquartile<br />
range)<br />
range)<br />
Total alarms 1013 7.0* (2.0–15.0) 604 3.5* (1.0–11.0)<br />
Nuisance alarms 878 6.0** (1.0–13.5) 502 2.0** (1.0–9.0)<br />
Relevant alarms 135 1.0 † (0.0–2.0) 102 1.0† (0.0–2.0)<br />
* Difference significant at p=0.0025, ** Difference significant at p=0.0022, † p = 0.41<br />
and total alarms is presented in the table. ‘Total alarms’ is the sum of<br />
alarms over 15 hours.<br />
Our results show that introducing an alarm ward round significantly<br />
reduces the amount of alarms occurring at night on a general <strong>Intensive</strong><br />
<strong>Care</strong> Unit. Of importance is that the alarm round decreases the frequency<br />
of nuisance alarms without decreasing the frequency of relevant alarms.<br />
References<br />
1. Imhoff M, Kuhls S. Alarm algorithms in critical care monitoring. Anesth Analg<br />
2006;102:1525-37.<br />
2. Meredith C, Edworthy J. Are there too many alarms in the intensive care unit An<br />
overview of the problems. J Adv Nurs 1995;21:15-20.<br />
3. Balogh D, Kittinger E, Benzer A, Hackl JM. Noise in the ICU. <strong>Intensive</strong> <strong>Care</strong> Med<br />
1993;19:343-46.<br />
Become a member and...<br />
...in addition to becoming part of a growing network of medical professionals working within<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
of up to £1,000,000 in the event of death or<br />
disability during a patient transfer.<br />
<br />
informative journal.<br />
at the <strong>Society</strong>’s meetings and events.<br />
to keep members informed of recent<br />
developments in <strong>Intensive</strong> <strong>Care</strong> as well as forthcoming meetings, events and<br />
opportunities such as grants and prizes and other news.<br />
– a two way communication channel from the<br />
<strong>Society</strong> to its members and vice versa.<br />
<br />
grade of membership.<br />
at a<br />
<br />
further details .<br />
<br />
76<br />
Volume 12, Number 1, January 2011 <strong>JICS</strong>