The use of ultrasound imaging prior to percutaneous ... - JICS
The use of ultrasound imaging prior to percutaneous ... - JICS
The use of ultrasound imaging prior to percutaneous ... - JICS
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
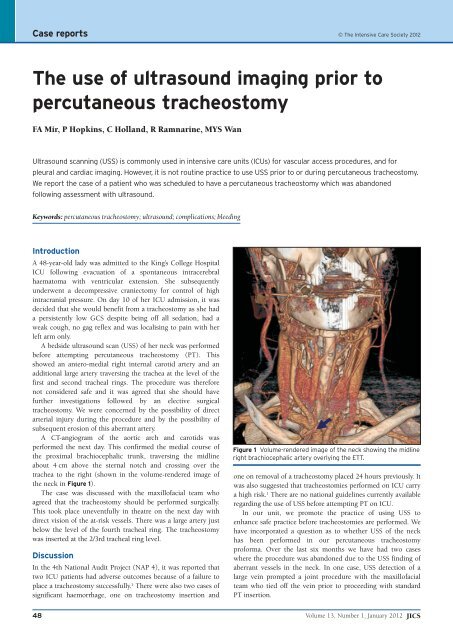
Case reports © <strong>The</strong> Intensive Care Society 2012<strong>The</strong> <strong>use</strong> <strong>of</strong> <strong>ultrasound</strong> <strong>imaging</strong> <strong>prior</strong> <strong>to</strong><strong>percutaneous</strong> tracheos<strong>to</strong>myFA Mir, P Hopkins, C Holland, R Ramnarine, MYS WanUltrasound scanning (USS) is commonly <strong>use</strong>d in intensive care units (ICUs) for vascular access procedures, and forpleural and cardiac <strong>imaging</strong>. However, it is not routine practice <strong>to</strong> <strong>use</strong> USS <strong>prior</strong> <strong>to</strong> or during <strong>percutaneous</strong> tracheos<strong>to</strong>my.We report the case <strong>of</strong> a patient who was scheduled <strong>to</strong> have a <strong>percutaneous</strong> tracheos<strong>to</strong>my which was abandonedfollowing assessment with <strong>ultrasound</strong>.Keywords: <strong>percutaneous</strong> tracheos<strong>to</strong>my; <strong>ultrasound</strong>; complications; bleedingIntroductionA 48-year-old lady was admitted <strong>to</strong> the King’s College HospitalICU following evacuation <strong>of</strong> a spontaneous intracerebralhaema<strong>to</strong>ma with ventricular extension. She subsequentlyunderwent a decompressive craniec<strong>to</strong>my for control <strong>of</strong> highintracranial pressure. On day 10 <strong>of</strong> her ICU admission, it wasdecided that she would benefit from a tracheos<strong>to</strong>my as she hada persistently low GCS despite being <strong>of</strong>f all sedation, had aweak cough, no gag reflex and was localising <strong>to</strong> pain with herleft arm only.A bedside <strong>ultrasound</strong> scan (USS) <strong>of</strong> her neck was performedbefore attempting <strong>percutaneous</strong> tracheos<strong>to</strong>my (PT). Thisshowed an antero-medial right internal carotid artery and anadditional large artery traversing the trachea at the level <strong>of</strong> thefirst and second tracheal rings. <strong>The</strong> procedure was thereforenot considered safe and it was agreed that she should havefurther investigations followed by an elective surgicaltracheos<strong>to</strong>my. We were concerned by the possibility <strong>of</strong> directarterial injury during the procedure and by the possibility <strong>of</strong>subsequent erosion <strong>of</strong> this aberrant artery.A CT-angiogram <strong>of</strong> the aortic arch and carotids wasperformed the next day. This confirmed the medial course <strong>of</strong>the proximal brachiocephalic trunk, traversing the midlineabout 4 cm above the sternal notch and crossing over thetrachea <strong>to</strong> the right (shown in the volume-rendered image <strong>of</strong>the neck in Figure 1).<strong>The</strong> case was discussed with the maxill<strong>of</strong>acial team whoagreed that the tracheos<strong>to</strong>my should be performed surgically.This <strong>to</strong>ok place uneventfully in theatre on the next day withdirect vision <strong>of</strong> the at-risk vessels. <strong>The</strong>re was a large artery justbelow the level <strong>of</strong> the fourth tracheal ring. <strong>The</strong> tracheos<strong>to</strong>mywas inserted at the 2/3rd tracheal ring level.DiscussionIn the 4th National Audit Project (NAP 4), it was reported thattwo ICU patients had adverse outcomes beca<strong>use</strong> <strong>of</strong> a failure <strong>to</strong>place a tracheos<strong>to</strong>my successfully. 1 <strong>The</strong>re were also two cases <strong>of</strong>significant haemorrhage, one on tracheos<strong>to</strong>my insertion andFigure 1 Volume-rendered image <strong>of</strong> the neck showing the midlineright brachiocephalic artery overlying the ETT.one on removal <strong>of</strong> a tracheos<strong>to</strong>my placed 24 hours previously. Itwas also suggested that tracheos<strong>to</strong>mies performed on ICU carrya high risk. 1 <strong>The</strong>re are no national guidelines currently availableregarding the <strong>use</strong> <strong>of</strong> USS before attempting PT on ICU.In our unit, we promote the practice <strong>of</strong> using USS <strong>to</strong>enhance safe practice before tracheos<strong>to</strong>mies are performed. Wehave incorporated a question as <strong>to</strong> whether USS <strong>of</strong> the neckhas been performed in our <strong>percutaneous</strong> tracheos<strong>to</strong>mypr<strong>of</strong>orma. Over the last six months we have had two caseswhere the procedure was abandoned due <strong>to</strong> the USS finding <strong>of</strong>aberrant vessels in the neck. In one case, USS detection <strong>of</strong> alarge vein prompted a joint procedure with the maxill<strong>of</strong>acialteam who tied <strong>of</strong>f the vein <strong>prior</strong> <strong>to</strong> proceeding with standardPT insertion.48Volume 13, Number 1, January 2012 <strong>JICS</strong>
Case reportsPT is considered <strong>to</strong> be a safer and better alternative <strong>to</strong>surgical tracheos<strong>to</strong>my as shown by several studies. 2 In theEuropean ‘Prevalence <strong>of</strong> Infection in Intensive Care’ (EPIC)study 3 in 1995, 12.6% <strong>of</strong> all critically ill patients had atracheos<strong>to</strong>my. Fatal haemorrhage is a rare complication <strong>of</strong> PT(0.25% in a series reported in 2005), 4 but is believed <strong>to</strong> beunder-reported. In one study, bleeding from injury <strong>to</strong> bloodvessels, which could have possibly been identified if <strong>ultrasound</strong>was <strong>use</strong>d, was considered significant in 24 <strong>of</strong> 497 (5%) PTsperformed without pre-procedure US evaluation. Six out <strong>of</strong>these 24 patients required conversion <strong>to</strong> surgical tracheos<strong>to</strong>my. 5<strong>The</strong>re are case reports which have demonstrated the benefits<strong>of</strong> using <strong>ultrasound</strong> before PT. Bertram et al 6 showed in theirseries <strong>of</strong> patients that about 15% <strong>of</strong> patients had the commoncarotid artery less than 10.5 mm from the fourth tracheal ringand anticipated that the neck extension required for PDTwould result in these vessels coming closer <strong>to</strong> the level <strong>of</strong> theupper tracheal rings. This was deemed <strong>to</strong> pose a higher risk <strong>of</strong>bleeding complications.Another advantage <strong>of</strong> the <strong>use</strong> <strong>of</strong> USS for PT is the real-time<strong>imaging</strong> <strong>of</strong> the needle path through the anterior neck tissues <strong>to</strong>define levels <strong>of</strong> puncture <strong>of</strong> the trachea. Studies have been doneon models which show that in subjects with simulatedunidentifiable anterior neck airway ana<strong>to</strong>my and trachealdeviation, the <strong>use</strong> <strong>of</strong> USS improves speed and success <strong>of</strong> cannulaplacement and reduces the number <strong>of</strong> attempts required. 7Conclusion<strong>The</strong> routine <strong>use</strong> <strong>of</strong> USS is <strong>of</strong> benefit in identifying overlying orvulnerable adjacent structures such as the thyroid gland andisthmus, and blood vessels. Imaging can also guide needles anddila<strong>to</strong>rs away from at-risk structures. 8,9 In view <strong>of</strong> theincreasing availability <strong>of</strong> USS and expertise in its <strong>use</strong>, werecommend that it is <strong>use</strong>d routinely for PT.Declaration <strong>of</strong> interestsNo conflict <strong>of</strong> interest <strong>to</strong> declare.References1. Harper J, Rangasami J, Cook T. Major airway events in patients with atracheos<strong>to</strong>my. In: Report and Findings <strong>of</strong> the 4th National Audit Project <strong>of</strong><strong>The</strong> Royal College <strong>of</strong> Anaesthetists. RCoA London 2011: p 126-27.2. Delaney A, Bagshaw SM, Nalos M. Percutaneous dilatationaltracheos<strong>to</strong>my versus surgical tracheos<strong>to</strong>my in critically ill patients: asystematic review and meta-analysis. Crit Care 2006,10:R55.3. Vincent JL, Bihari DJ, Suter PM et al. <strong>The</strong> prevalence <strong>of</strong> nosocomialinfection in intensive care units in Europe. Results <strong>of</strong> the EuropeanPrevalence <strong>of</strong> Infection in Intensive Care (EPIC) study. JAMA 1995;274:639-44.4. McCormick B, Manara AR. Mortality from <strong>percutaneous</strong> dilatationaltracheos<strong>to</strong>my. A report <strong>of</strong> three cases. Anaesthesia 2005;60:490-95.5. Muhammad JK, Major E, Wood A, Pat<strong>to</strong>n DW. Percutaneous dilatationaltracheos<strong>to</strong>my: haemorrhagic complications and the vascular ana<strong>to</strong>my <strong>of</strong>the anterior neck. A review based on 497 cases. Int J Oral Maxill<strong>of</strong>ac Surg2000,29:217-22.6. Bertram S, Emsh<strong>of</strong>f R, Norer B. Ultrasonographic ana<strong>to</strong>my <strong>of</strong> theanterior neck. J Oral Maxill<strong>of</strong>ac Surg 1995;53:1420-24.7. Rajajee V, Fletcher JJ, Rochlen LR, Jacobs TL. Real-time <strong>ultrasound</strong>guided<strong>percutaneous</strong> dilatational tracheos<strong>to</strong>my: a feasibility study. CritCare 2011;15:R67.8. Dinsmore J, Heard AMB, Green RJ.<strong>The</strong> <strong>use</strong> <strong>of</strong> <strong>ultrasound</strong> <strong>to</strong> guide timecriticalcannula tracheo<strong>to</strong>my when anterior neck airway ana<strong>to</strong>my isunidentifiable. Eur J Anaesthesiol 2011;28:506-10.9. Mallick A, Bodenham AR. Tracheos<strong>to</strong>my in critically ill patients. Eur JAnaesthesiol 2010;27:676-82.Fauzia Ahmad Mir Specialist Registrar Intensive Carefauziamir@nhs.netPhilip Hopkins Consultant Intensive CareChris<strong>to</strong>pher Holland Consultant Intensive CareRaymond Ramnarine Specialist Registrar RadiologyMing Young Simon Wan Specialist Registrar RadiologyKings College Hospital, LondonCommentary: Ultrasound guidance for practical proceduresThis report rightly emphasises the potential value <strong>of</strong><strong>ultrasound</strong> visualisation <strong>of</strong> pre-tracheal blood vessels <strong>prior</strong><strong>to</strong> <strong>percutaneous</strong> tracheos<strong>to</strong>my (Figure 2). Such vessels, ifarterial, may be palpable or visibly pulsatile. <strong>The</strong> <strong>use</strong> <strong>of</strong><strong>ultrasound</strong> <strong>to</strong> guide needles in<strong>to</strong> the trachea at the correct levelis also described. Higher-resolution devices now enable goodvisualisation <strong>of</strong> individual tracheal cartilages. <strong>The</strong> true utility <strong>of</strong>such approaches is still hampered by the probe footprint sizeand shape applied <strong>to</strong> the root <strong>of</strong> the neck, and the inability <strong>of</strong><strong>ultrasound</strong> <strong>to</strong> enable <strong>imaging</strong> within the air-filled trachea.Clinicians should also consider the <strong>use</strong> <strong>of</strong> high-resolution<strong>ultrasound</strong> <strong>prior</strong> <strong>to</strong> other invasive procedures <strong>to</strong> reduce therisk <strong>of</strong> bleeding, eg identification <strong>of</strong> vessels in the chest orabdominal wall in the liver failure patient with portalhypertension <strong>prior</strong> <strong>to</strong> ascitic or pleural drain insertion.Andrew Bodenham Direc<strong>to</strong>r <strong>of</strong> Intensive Care, Consultant inAnaesthesia, Leeds General InfirmaryFigure 2 Cross-section <strong>ultrasound</strong> image <strong>of</strong> the neck showing aplexus <strong>of</strong> large anterior jugular veins (arrow) in front <strong>of</strong> thetrachea in a patient with tricuspid regurgitation.<strong>JICS</strong> Volume 13, Number 1, January 2012 49