- Page 1 and 2: EMPLOYEE HANDBOOK OF SUMMARY PLAN D
- Page 3 and 4: Table of Contents Eligibility .....
- Page 5 and 6: Your cost for optional life insuran
- Page 7 and 8: This coverage is available for elig
- Page 9 and 10: For example, let’s assume: • Yo
- Page 11 and 12: • The disability is considered to
- Page 13 and 14: • If the Plan is terminated by th
- Page 15 and 16: Conversion portability feature for
- Page 17: conversion period ends. Ported cove
- Page 21 and 22: Table of Contents Eligibility .....
- Page 23 and 24: • Suffered by the employee within
- Page 25 and 26: Upon the death of a covered depende
- Page 27 and 28: insane • Commission or attempt to
- Page 29 and 30: administrator will give no deferenc
- Page 31 and 32: APPENDIX A (cont.) Schedule of Insu
- Page 33 and 34: * A loss is defined as: • For a h
- Page 35 and 36: Felonious Assault and Violent Crime
- Page 37 and 38: hospital confinement (or part of a
- Page 39 and 40: SUMMARY PLAN DESCRIPTION Huntington
- Page 41 and 42: This Summary Plan Description (SPD)
- Page 43 and 44: 10. May the designated beneficiary
- Page 45 and 46: extension of time for processing th
- Page 47 and 48: APPENDIX A — Schedule of Insuranc
- Page 49 and 50: APPENDIX B — Additional Benefits
- Page 51 and 52: Rehabilitation Benefit: The benefit
- Page 53 and 54: SUMMARY PLAN DESCRIPTION Huntington
- Page 55 and 56: This Summary Plan Description (SPD)
- Page 57 and 58: How are benefits payable Benefits a
- Page 59 and 60: Appeal Procedure 15. What procedure
- Page 61 and 62: Table of Weekly Disability Insuranc
- Page 63 and 64: SUMMARY PLAN DESCRIPTION Huntington
- Page 65 and 66: This Summary Plan Description (SPD)
- Page 67 and 68: How the EAP Works The EAP provides
- Page 69 and 70:
• A specific description of the E
- Page 71 and 72:
Type of Claim Time to Appeal from D
- Page 73 and 74:
Throughout the review process, the
- Page 75 and 76:
Table of Contents OVERVIEW ........
- Page 77 and 78:
Your Contributions If you choose to
- Page 79 and 80:
⎯ Removal of lead-based paint to
- Page 81 and 82:
• Any other expenses considered n
- Page 83 and 84:
Ineligible Dependent Day Care Expen
- Page 85 and 86:
account, you cannot also claim the
- Page 87 and 88:
Health Care FSA Example Assume the
- Page 89 and 90:
enefits, you will have to manually
- Page 91 and 92:
• In addition, you contributed $2
- Page 93 and 94:
SUMMARY PLAN DESCRIPTION Huntington
- Page 95 and 96:
Introduction In accordance with the
- Page 97 and 98:
hours you are paid for working and
- Page 99 and 100:
savings on a before-tax basis can m
- Page 101 and 102:
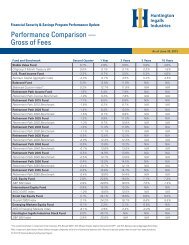
Effective Date June 7, 2004 July 11
- Page 103 and 104:
securities of foreign issuers. It m
- Page 105 and 106:
how long you intend to have the fun
- Page 107 and 108:
withdrawals are subject to taxes (S
- Page 109 and 110:
in which you terminate employment o
- Page 111 and 112:
e taxable in the year of the sale.
- Page 113 and 114:
The request for appeal must include
- Page 115 and 116:
• Bonding of Plan officials, •
- Page 117 and 118:
writing. Participants in the Huntin
- Page 119 and 120:
Table of Contents Eligibility .....
- Page 121 and 122:
• You become an active, full-time
- Page 123 and 124:
• Normal Retirement ⎯ Refer to
- Page 125 and 126:
• January 1, 1994−December 31,
- Page 127 and 128:
Calendar Year Months Hours per mont
- Page 129 and 130:
Your Minimum Benefit will be reduce
- Page 131 and 132:
join the Pension Plan on July 1, 19
- Page 133 and 134:
If you retire early and begin your
- Page 135 and 136:
20. For all types of retirement, ar
- Page 137 and 138:
• A pension at your Normal Retire
- Page 139 and 140:
You will receive a notice of suspen
- Page 141 and 142:
• The Pension Plan is terminated
- Page 143 and 144:
• A legible copy of your spouse
- Page 145 and 146:
A Joint and Survivor (J&S) with Pop
- Page 147 and 148:
The Participant’s estimated Socia
- Page 149 and 150:
The Participant receives a monthly
- Page 151 and 152:
If the Participant marries after co
- Page 153 and 154:
The spouse may elect to defer comme
- Page 155 and 156:
• A description of additional mat
- Page 157 and 158:
Administration of the Plan 48. How
- Page 159 and 160:
Benefits under this Plan are insure
- Page 161 and 162:
Rollovers by Non-Spouse Beneficiari
- Page 163 and 164:
Table of Contents Introduction ....
- Page 165 and 166:
Plan. The plan document sets forth
- Page 167 and 168:
4. What is included in hours paid f
- Page 169 and 170:
investment performance could result
- Page 171 and 172:
Vesting 16. What is “vesting” a
- Page 173 and 174:
Besides having the right to appeal,
- Page 175 and 176:
Subject to the terms of the Collect
- Page 177 and 178:
SUMMARY PLAN DESCRIPTION Huntington
- Page 179 and 180:
which agreement is effective Octobe
- Page 181 and 182:
Applying for Your Retirement Benefi
- Page 183 and 184:
Top Heavy Rules ...................
- Page 185 and 186:
Vesting If you participated in the
- Page 187 and 188:
DETAILS ABOUT THE CASH BALANCE PLAN
- Page 189 and 190:
30-year Treasury Bond Annual Rate F
- Page 191 and 192:
Points on August 31, 2008 (age plus
- Page 193 and 194:
• Hire date: November 29, 2004
- Page 195 and 196:
Once you become vested, you are alw
- Page 197 and 198:
• If you have 10 or more years of
- Page 199 and 200:
payment or even a forfeiture of ben
- Page 201 and 202:
50% joint and survivor annuity with
- Page 203 and 204:
3. To determine the amount your spo
- Page 205 and 206:
Calculating 75% Joint and Survivor
- Page 207 and 208:
The factors shown in this table are
- Page 209 and 210:
In the chart, age 65 corresponds to
- Page 211 and 212:
Type of Approved Leave Qualifying m
- Page 213 and 214:
• You have 75 points (refer to
- Page 215 and 216:
cannot be determined, you receive e
- Page 217 and 218:
• Individuals hired by an outside
- Page 219 and 220:
Vesting in Your Benefit Vesting mea
- Page 221 and 222:
Your Total Contributions multiplied
- Page 223 and 224:
Age at Which You Begin Receiving Be
- Page 225 and 226:
• A legible copy of your marriage
- Page 227 and 228:
level income option. However, your
- Page 229 and 230:
For example, let’s assume: • Yo
- Page 231 and 232:
• $875.00 + ($1,000.00 x 0.590) =
- Page 233 and 234:
Factors for Calculating Certain and
- Page 235 and 236:
Type of Approved Leave Unpaid famil
- Page 237 and 238:
The amount of your spouse's monthly
- Page 239 and 240:
Final Monthly Rate From Through Mon
- Page 241 and 242:
Hours for this purpose are usually
- Page 243 and 244:
There are specific requirements tha
- Page 245 and 246:
Appealing Claims Decisions If you d
- Page 247 and 248:
When plan amendments are made that
- Page 249 and 250:
COMMONLY USED ACRONYMS Following ar
- Page 251 and 252:
Table of Contents Plan Description
- Page 253 and 254:
Claims Administrator Vision Service
- Page 255 and 256:
How to Use the Vision Plan If you w
- Page 257 and 258:
Fiduciary Responsibility The Plan A
- Page 259 and 260:
Additional Information about the Ap
- Page 261 and 262:
Table of Contents Plan Description
- Page 263 and 264:
• Debt Collection Defense • Doc
- Page 265 and 266:
The Group Legal Plan gives you acce
- Page 267 and 268:
WILL AND ESTATE MATTERS Probate (10
- Page 269 and 270:
issues; or any matter where the cre
- Page 271 and 272:
Mortgages This service covers the p
- Page 273 and 274:
INSURANCE MATTERS Insurance Claims
- Page 275 and 276:
Juvenile Court Defense This service
- Page 277 and 278:
EXCLUSIONS Excluded services are th
- Page 279 and 280:
this Plan. However, if you are elig
- Page 281 and 282:
SUMMARY PLAN DESCRIPTION (Supplemen
- Page 283 and 284:
Medicare Premium Reimbursement Prog
- Page 285 and 286:
Administrative This summary plan de
- Page 287 and 288:
SUMMARY PLAN DESCRIPTION Huntington
- Page 289 and 290:
This Summary Plan Description (SPD)
- Page 291 and 292:
What is Covered The following items
- Page 293 and 294:
would pay $0, so the Plan would pay
- Page 295 and 296:
If services under the Plan are deni
- Page 297 and 298:
Post-Service Claims. There are two
- Page 299 and 300:
Appendix I: List of Participating P
- Page 301 and 302:
SUMMARY PLAN DESCRIPTION Huntington
- Page 303 and 304:
Introduction The benefit plans desc
- Page 305 and 306:
• Gives you the right to sue for
- Page 307 and 308:
Security Administrator (formerly kn
- Page 309 and 310:
HIPAA Privacy Rights Title II of th
- Page 311 and 312:
Your Rights Under HIPAA You have th
- Page 313 and 314:
If you are on a leave of absence du
- Page 315 and 316:
Event Within 31 days of the qualifi
- Page 317 and 318:
Benefit Option What Happens During
- Page 319 and 320:
Benefit Option Weekly Disability In
- Page 321 and 322:
Dependent Day Care Flexible Spendin
- Page 323 and 324:
If You Transfer If you transfer fro
- Page 325 and 326:
If Your Employment Ends Due to a La
- Page 327 and 328:
If Your Employment Ends Due to Disa
- Page 329 and 330:
continues provided the required pre
- Page 331 and 332:
Newly Eligible Child If you, the fo
- Page 333 and 334:
efore the end of the original 18-mo
- Page 335 and 336:
Uniformed Services Employment and R
- Page 337 and 338:
change the amount of required emplo
- Page 339 and 340:
Contact Information: Vision Plan ER
- Page 341 and 342:
Contact Information: Dependent Care
- Page 343 and 344:
Contact Information: Business Trave
- Page 345 and 346:
Source of Contributions: Premiums a
- Page 347 and 348:
Contact Information: Employee Assis
- Page 349 and 350:
Plan Sponsor/Employer EIN 90-060700
- Page 351 and 352:
Plan Number: 107 Plan Name: Plan Ad
- Page 353 and 354:
Contact Information: Retiree Prescr