Facilitator - WHO Western Pacific Region - World Health Organization
Facilitator - WHO Western Pacific Region - World Health Organization
Facilitator - WHO Western Pacific Region - World Health Organization
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
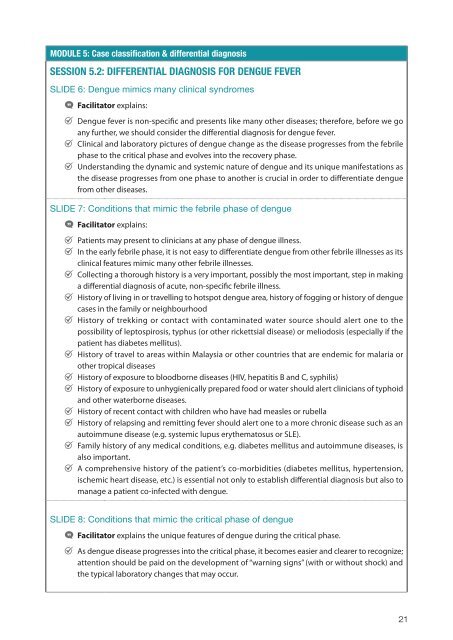
MODULE 5: Case classification & differential diagnosis<br />
SESSION 5.2: DIFFERENTIAL DIAGNOSIS FOR DENGUE FEVER<br />
SLIDE 6: Dengue mimics many clinical syndromes<br />
•<strong>Facilitator</strong><br />
•<br />
explains:<br />
•Dengue fever is non-specific and presents like many other diseases; therefore, before we go<br />
•<br />
any further, we should consider the differential diagnosis for dengue fever.<br />
•Clinical and laboratory pictures of dengue change as the disease progresses from the febrile<br />
•<br />
phase to the critical phase and evolves into the recovery phase.<br />
•Understanding the dynamic and systemic nature of dengue and its unique manifestations as<br />
the disease progresses from one phase to another is crucial in order to differentiate dengue<br />
from other diseases.<br />
SLIDE 7: Conditions that mimic the febrile phase of dengue<br />
•<strong>Facilitator</strong><br />
•<br />
explains:<br />
•<br />
•Patients may present to clinicians at any phase of dengue illness.<br />
•In the early febrile phase, it is not easy to differentiate dengue from other febrile illnesses as its<br />
•<br />
clinical features mimic many other febrile illnesses.<br />
•Collecting a thorough history is a very important, possibly the most important, step in making<br />
•<br />
a differential diagnosis of acute, non-specific febrile illness.<br />
•History of living in or travelling to hotspot dengue area, history of fogging or history of dengue<br />
•<br />
cases in the family or neighbourhood<br />
•History of trekking or contact with contaminated water source should alert one to the<br />
possibility of leptospirosis, typhus (or other rickettsial disease) or meliodosis (especially if the<br />
•<br />
patient has diabetes mellitus).<br />
•History of travel to areas within Malaysia or other countries that are endemic for malaria or<br />
•<br />
other tropical diseases<br />
•History of exposure to bloodborne diseases (HIV, hepatitis B and C, syphilis)<br />
•History of exposure to unhygienically prepared food or water should alert clinicians of typhoid<br />
•<br />
and other waterborne diseases.<br />
•History of recent contact with children who have had measles or rubella<br />
•History of relapsing and remitting fever should alert one to a more chronic disease such as an<br />
•<br />
autoimmune disease (e.g. systemic lupus erythematosus or SLE).<br />
•Family history of any medical conditions, e.g. diabetes mellitus and autoimmune diseases, is<br />
•<br />
also important.<br />
•A comprehensive history of the patient’s co-morbidities (diabetes mellitus, hypertension,<br />
ischemic heart disease, etc.) is essential not only to establish differential diagnosis but also to<br />
manage a patient co-infected with dengue.<br />
SLIDE 8: Conditions that mimic the critical phase of dengue<br />
• •<strong>Facilitator</strong> explains the unique features of dengue during the critical phase.<br />
• •As dengue disease progresses into the critical phase, it becomes easier and clearer to recognize;<br />
attention should be paid on the development of “warning signs” (with or without shock) and<br />
the typical laboratory changes that may occur.<br />
21