Facilitator - WHO Western Pacific Region - World Health Organization
Facilitator - WHO Western Pacific Region - World Health Organization
Facilitator - WHO Western Pacific Region - World Health Organization
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
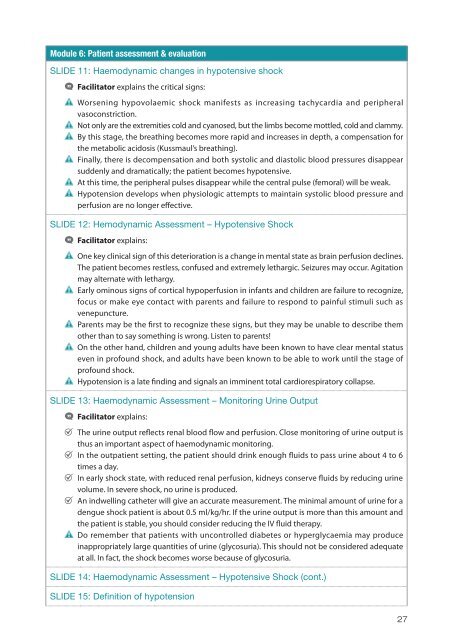
Module 6: Patient assessment & evaluation<br />
SLIDE 11: Haemodynamic changes in hypotensive shock<br />
•<strong>Facilitator</strong><br />
•<br />
explains the critical signs:<br />
•Worsening hypovolaemic shock manifests as increasing tachycardia and peripheral<br />
•<br />
vasoconstriction.<br />
•Not only are the extremities cold and cyanosed, but the limbs become mottled, cold and clammy.<br />
•By this stage, the breathing becomes more rapid and increases in depth, a compensation for<br />
•<br />
the metabolic acidosis (Kussmaul’s breathing).<br />
•Finally, there is decompensation and both systolic and diastolic blood pressures disappear<br />
•<br />
suddenly and dramatically; the patient becomes hypotensive.<br />
•<br />
•At this time, the peripheral pulses disappear while the central pulse (femoral) will be weak.<br />
•Hypotension develops when physiologic attempts to maintain systolic blood pressure and<br />
perfusion are no longer effective.<br />
SLIDE 12: Hemodynamic Assessment – Hypotensive Shock<br />
•<strong>Facilitator</strong><br />
•<br />
explains:<br />
•One key clinical sign of this deterioration is a change in mental state as brain perfusion declines.<br />
The patient becomes restless, confused and extremely lethargic. Seizures may occur. Agitation<br />
•<br />
may alternate with lethargy.<br />
•Early ominous signs of cortical hypoperfusion in infants and children are failure to recognize,<br />
focus or make eye contact with parents and failure to respond to painful stimuli such as<br />
•<br />
venepuncture.<br />
•Parents may be the first to recognize these signs, but they may be unable to describe them<br />
•<br />
other than to say something is wrong. Listen to parents!<br />
•On the other hand, children and young adults have been known to have clear mental status<br />
even in profound shock, and adults have been known to be able to work until the stage of<br />
•<br />
profound shock.<br />
•Hypotension is a late finding and signals an imminent total cardiorespiratory collapse.<br />
SLIDE 13: Haemodynamic Assessment – Monitoring Urine Output<br />
•<strong>Facilitator</strong><br />
•<br />
explains:<br />
•The urine output reflects renal blood flow and perfusion. Close monitoring of urine output is<br />
•<br />
thus an important aspect of haemodynamic monitoring.<br />
•In the outpatient setting, the patient should drink enough fluids to pass urine about 4 to 6<br />
•<br />
times a day.<br />
•In early shock state, with reduced renal perfusion, kidneys conserve fluids by reducing urine<br />
•<br />
volume. In severe shock, no urine is produced.<br />
•An indwelling catheter will give an accurate measurement. The minimal amount of urine for a<br />
dengue shock patient is about 0.5 ml/kg/hr. If the urine output is more than this amount and<br />
•<br />
the patient is stable, you should consider reducing the IV fluid therapy.<br />
•Do remember that patients with uncontrolled diabetes or hyperglycaemia may produce<br />
inappropriately large quantities of urine (glycosuria). This should not be considered adequate<br />
at all. In fact, the shock becomes worse because of glycosuria.<br />
SLIDE 14: Haemodynamic Assessment – Hypotensive Shock (cont.)<br />
SLIDE 15: Definition of hypotension<br />
27