Volume 6 Issue 3 - Australasian Society for Ultrasound in Medicine
Volume 6 Issue 3 - Australasian Society for Ultrasound in Medicine
Volume 6 Issue 3 - Australasian Society for Ultrasound in Medicine
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
<strong>Ultrasound</strong> evaluation of neck lymph nodes<br />
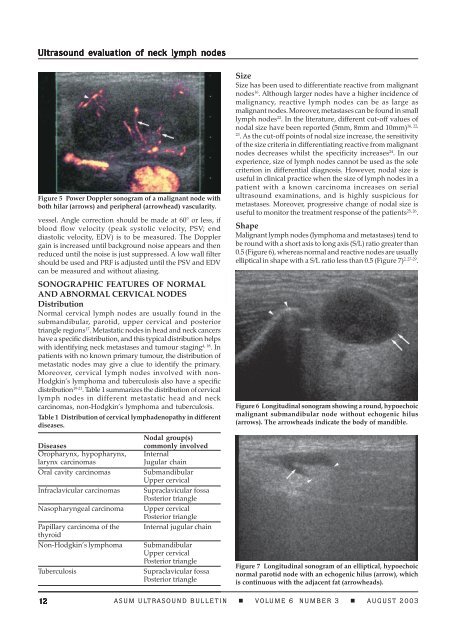
Figure 5 Power Doppler sonogram of a malignant node with<br />
both hilar (arrows) and peripheral (arrowhead) vascularity.<br />
vessel. Angle correction should be made at 60° or less, if<br />
blood flow velocity (peak systolic velocity, PSV; end<br />
diastolic velocity, EDV) is to be measured. The Doppler<br />
ga<strong>in</strong> is <strong>in</strong>creased until background noise appears and then<br />
reduced until the noise is just suppressed. A low wall filter<br />
should be used and PRF is adjusted until the PSV and EDV<br />
can be measured and without alias<strong>in</strong>g.<br />
SONOGRAPHIC FEATURES OF NORMAL<br />
AND ABNORMAL CERVICAL NODES<br />
Distribution<br />
Normal cervical lymph nodes are usually found <strong>in</strong> the<br />
submandibular, parotid, upper cervical and posterior<br />
triangle regions 17 . Metastatic nodes <strong>in</strong> head and neck cancers<br />
have a specific distribution, and this typical distribution helps<br />
with identify<strong>in</strong>g neck metastases and tumour stag<strong>in</strong>g 4, 18 . In<br />
patients with no known primary tumour, the distribution of<br />
metastatic nodes may give a clue to identify the primary.<br />
Moreover, cervical lymph nodes <strong>in</strong>volved with non-<br />
Hodgk<strong>in</strong>’s lymphoma and tuberculosis also have a specific<br />
distribution 19-21 . Table 1 summarizes the distribution of cervical<br />
lymph nodes <strong>in</strong> different metastatic head and neck<br />
carc<strong>in</strong>omas, non-Hodgk<strong>in</strong>’s lymphoma and tuberculosis.<br />
Table 1 Distribution of cervical lymphadenopathy <strong>in</strong> different<br />
diseases.<br />
Diseases<br />
Oropharynx, hypopharynx,<br />
larynx carc<strong>in</strong>omas<br />
Oral cavity carc<strong>in</strong>omas<br />
Infraclavicular carc<strong>in</strong>omas<br />
Nasopharyngeal carc<strong>in</strong>oma<br />
Papillary carc<strong>in</strong>oma of the<br />
thyroid<br />
Non-Hodgk<strong>in</strong>’s lymphoma<br />
Tuberculosis<br />
Nodal group(s)<br />
commonly <strong>in</strong>volved<br />
Internal<br />
Jugular cha<strong>in</strong><br />
Submandibular<br />
Upper cervical<br />
Supraclavicular fossa<br />
Posterior triangle<br />
Upper cervical<br />
Posterior triangle<br />
Internal jugular cha<strong>in</strong><br />
Submandibular<br />
Upper cervical<br />
Posterior triangle<br />
Supraclavicular fossa<br />
Posterior triangle<br />
Size<br />
Size has been used to differentiate reactive from malignant<br />
nodes 16 . Although larger nodes have a higher <strong>in</strong>cidence of<br />
malignancy, reactive lymph nodes can be as large as<br />
malignant nodes. Moreover, metastases can be found <strong>in</strong> small<br />
lymph nodes 22 . In the literature, different cut-off values of<br />
16, 22,<br />
nodal size have been reported (5mm, 8mm and 10mm)<br />
23<br />
. As the cut-off po<strong>in</strong>ts of nodal size <strong>in</strong>crease, the sensitivity<br />
of the size criteria <strong>in</strong> differentiat<strong>in</strong>g reactive from malignant<br />
nodes decreases whilst the specificity <strong>in</strong>creases 24 . In our<br />
experience, size of lymph nodes cannot be used as the sole<br />
criterion <strong>in</strong> differential diagnosis. However, nodal size is<br />
useful <strong>in</strong> cl<strong>in</strong>ical practice when the size of lymph nodes <strong>in</strong> a<br />
patient with a known carc<strong>in</strong>oma <strong>in</strong>creases on serial<br />
ultrasound exam<strong>in</strong>ations, and is highly suspicious <strong>for</strong><br />
metastases. Moreover, progressive change of nodal size is<br />
useful to monitor the treatment response of the patients 25, 26 .<br />
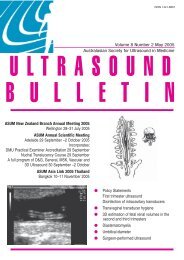
Shape<br />
Malignant lymph nodes (lymphoma and metastases) tend to<br />
be round with a short axis to long axis (S/L) ratio greater than<br />
0.5 (Figure 6), whereas normal and reactive nodes are usually<br />
elliptical <strong>in</strong> shape with a S/L ratio less than 0.5 (Figure 7) 2, 27-29 .<br />
Figure 6 Longitud<strong>in</strong>al sonogram show<strong>in</strong>g a round, hypoechoic<br />
malignant submandibular node without echogenic hilus<br />
(arrows). The arrowheads <strong>in</strong>dicate the body of mandible.<br />
Figure 7 Longitud<strong>in</strong>al sonogram of an elliptical, hypoechoic<br />
normal parotid node with an echogenic hilus (arrow), which<br />
is cont<strong>in</strong>uous with the adjacent fat (arrowheads).<br />
12 ASUM ULTRASOUND BULLETIN VOLUME 6 NUMBER 3 AUGUST 2003