FINAL Global Module 10-11.pdf - AaronsWorld.com
FINAL Global Module 10-11.pdf - AaronsWorld.com
FINAL Global Module 10-11.pdf - AaronsWorld.com
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
TABLE OF CONTENTS<br />
TABLE OF CONTENTS 1<br />
I. INTRODUCTION 3<br />
MISSION AND VISION STATEMENTS 3<br />
WELCOME 3<br />
PURPOSE OF THE HANDBOOK 3<br />
II. CLINIC SHIFT POLICIES AND PROCEDURES 4<br />
CODE OF ETHICS 4<br />
PROFESSIONAL CODE OF CONDUCT 5<br />
SCOPE OF PRACTICE AND CONFLICT OF INTEREST 5<br />
DRESS, HYGIENE, AND APPEARANCE REQUIREMENTS 6<br />
REGISTERING FOR SHIFTS/ROTATIONS 7<br />
ATTENDANCE REQUIREMENTS AND GRADES 9<br />
ABSENCES <strong>10</strong><br />
GRADING AND STUDENT PERFORMANCE 12<br />
ON-SHIFT POLICIES, ROLES, AND PROCEDURES 16<br />
PATIENT SCHEDULING AND REFERRALS 23<br />
III. SAFETY, ACCIDENTS, AND EMERGENCIES 25<br />
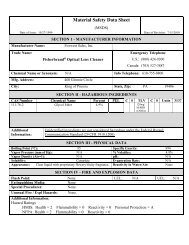
BLOOD BORNE PREVENTION PROCEDURE 25<br />
NEEDLES 26<br />
ACCIDENT / ILLNESS 27<br />
SUICIDAL/HOMICIDAL PATIENT POLICY AND PROCEDURE 29<br />
REPORTING A PATIENT/VISITOR ACCIDENT OR ILLNESS 33<br />
EMERGENCIES: WEATHER, EARTHQUAKE, DISEASE 34<br />
IV. CONFIDENTIALITY, MEDICAL RECORDS, AND TREATMENT OF MINORS 37<br />
CONFIDENTIALITY 37<br />
MEDICAL RECORDS 42<br />
TREATMENT OF MINORS 47<br />
V. MISCELLANEOUS CLINIC POLICIES: GRIEVANCE, PARKING, FUNDRAISING 50<br />
GRIEVANCE/COMPLAINT POLICIY 50<br />
FACILITIES, EQUIPMENT AND PARKING 51<br />
CULTIVATION AND SOLICITATION POLICY (FUNDRAISING) 52<br />
VI. APPENDICES 54<br />
CLINIC CONTRACT 55<br />
STUDENT HEPATITIS B CHECKLIST 56<br />
STUDENT CLINICIAN ABSENCE / SUBSTITUTE FORM 57<br />
MEDICAL ABBREVIATIONS 58<br />
PATIENT CO-MANAGEMENT: TEMPLATES AND ETIQUETTE GUIDELINES 64<br />
VII. INDEX 71
MISSION AND VISION STATEMENTS<br />
I. INTRODUCTION<br />
THE MISSION OF BASTYR CENTER FOR NATURAL HEALTH<br />
To create an extraordinary environment <strong>com</strong>mitted to excellence in health care and clinical education<br />
that assists and empowers individuals and the <strong>com</strong>munity to achieve better health and a higher quality<br />
of life.<br />
THE MISSION OF BASTYR UNIVERSITY<br />
We educate future leaders in natural health arts and sciences. Respecting the healing power of nature<br />
and recognizing that body, mind and spirit are intrinsically inseparable, we model an integrated<br />
approach to education, research and clinical service.<br />
THE VISION OF BASTYR UNIVERSITY<br />
As the world’s leading academic center for advancing and integrating knowledge n the natural health<br />
arts and sciences, Bastyr University will transform the health and well-being of the human <strong>com</strong>munity.<br />
WELCOME<br />
Wel<strong>com</strong>e to Bastyr Center for Natural Health! You are about to begin a very exciting part of your<br />
training at Bastyr University. Bastyr Center for Natural Health, also known as “the clinic" or “BCNH”,<br />
will provide more than 35,000 patient visits this year. The services of each clinical program and the<br />
integration between programs provide some of the best natural medicine care to be found anywhere!<br />
The staff and faculty of BCNH are excited about your entry into the clinical portion of your training<br />
and look forward to working together while you make your unique and important contributions to our<br />
mission.<br />
PURPOSE OF THE HANDBOOK<br />
The purpose of the Student Clinician Handbook is to outline the policies, standards, and requirements<br />
for student clinician performance and conduct in the clinic. The handbook consists of four modules: a<br />
global module that applies to all student clinicians, and three department-specific modules: AOM, ND,<br />
and Nutrition. Student clinicians are responsible for knowing and adhering to all of the guidelines and<br />
requirements described in the current global module of the Student Clinician Handbook as well as<br />
those in the module(s) for their specific program(s).<br />
This handbook governs all student clinicians and supersedes previous editions. The policies and<br />
procedures contained within are subject to change during the year. Changes to policy will be sent by<br />
email to all students in clinical training and will be posted on the university intranet. A signed copy of<br />
the clinic contract found in the appendix of this module is required for OM 4800 AOM Clinic Entry<br />
and ND 6804 Clinic Orientation for students to be eligible to begin clinical training.<br />
The Student Clinician Handbook and other clinic files can be found online. Log in to your student<br />
account, double-click on ‘My Computer’ and then double-click on the N drive which connects to<br />
\\middleearth.prv\bastyr\campus\data\public\clinic. You can also access the same information at this<br />
location: MyBU > Home > Clinical Education > Documents.<br />
3
II. CLINIC SHIFT POLICIES AND PROCEDURES<br />
CODE OF ETHICS<br />
The purpose of the Bastyr Center for Natural Health code of ethics is to provide a framework within<br />
which all students and staff at the Bastyr Center for Natural Health can learn and work in a safe,<br />
nurturing, and supportive environment. Ethical behavior is critical to the quality of interactions among<br />
individuals and groups within the university and clinic. Individual behaviors also reflect the quality of<br />
health care provided to the patients of the clinics. As individuals and as an institution, we strive for<br />
excellence. The code of ethics provides guidance in achieving excellence. The code may also be found<br />
in the university’s Student Handbook, under Bastyr Center for Natural Health.<br />
Code of Ethics<br />
o The natural health-care practitioner’s primary purpose is to restore, maintain and<br />
optimize health in human beings.<br />
o The natural health-care practitioner acts to restore, maintain and optimize health by<br />
providing individualized care, according to his/her ability and judgment.<br />
o The natural health-care practitioner shall endeavor to first do no harm and to provide<br />
the most effective health care available with the least risk to his/her patients at all<br />
times.<br />
o The natural health-care practitioner shall recognize, respect and promote the healing<br />
power of nature inherent in each human being. The natural health-care practitioner<br />
shall strive to identify and remove the causes of illness, rather than to merely<br />
eliminate or suppress symptoms.<br />
o The natural health-care practitioner shall educate her/his patients, inspire rational<br />
hope and encourage self-responsibility for health.<br />
o The natural health-care practitioner shall treat each person by considering all<br />
individual health factors and influences.<br />
o The natural health-care practitioner shall promote personal well-being and the<br />
prevention of disease for the individual, <strong>com</strong>munity and our world.<br />
o The natural health-care practitioner shall acknowledge the worth and dignity of every<br />
person.<br />
o The natural health-care practitioner shall safeguard the patient’s right to privacy and<br />
only disclose confidential information when either authorized by the patient or<br />
mandated by law.<br />
o The natural health-care practitioner shall act judiciously to protect the patient and the<br />
public when health care quality and safety are adversely affected by in<strong>com</strong>petent or<br />
unethical practice by any person. The natural health-care practitioner shall maintain<br />
<strong>com</strong>petence in her/his field and strive for professional excellence through<br />
assessment of personal strengths, limitations and effectiveness and by advancement<br />
of professional knowledge.<br />
o The natural health-care practitioner shall conduct his/her practice and professional<br />
activities with honesty, integrity and responsibility for individual judgments and<br />
actions.<br />
4
o The natural health-care practitioner shall respect all ethical, qualified health care<br />
practitioners and cooperate with other health professionals to promote health for the<br />
individual, the public and the global <strong>com</strong>munity.<br />
o The natural health-care practitioner shall strive to exemplify personal well-being,<br />
ethical character and trustworthiness as a health care professional.<br />
PROFESSIONAL CODE OF CONDUCT<br />
This is the code of conduct for all members of the Bastyr University <strong>com</strong>munity. Please see the<br />
University Catalogue and Student Handbook for further information regarding our code of conduct.<br />
The privilege of working in the Bastyr University Clinic Program requires full <strong>com</strong>pliance with all<br />
clinic policies and procedures. Loss of privileges, specified disciplinary actions, or separation from<br />
Bastyr University may be imposed on any University member whose conduct on or off campus<br />
adversely affects the Bastyr University <strong>com</strong>munity, in particular when it includes blatant disregard for<br />
the welfare of others.<br />
Fundamental types of misconduct that may lead to suspension or dismissal include:<br />
o Physical and/or verbal abuse, intimidation, or harassment of another person or group.<br />
o Racist and/or derogatory remarks and/or behavior towards another person or group.<br />
o Deliberate or careless endangerment, tampering with safety alarms or equipment,<br />
violation of specific safety regulations, and/or failure to render reasonable<br />
cooperation in an emergency.<br />
o Obstruction or forcible disruptions of regular Bastyr University activities, including<br />
teaching, research, administration, clinic services, discipline, organized events, and<br />
the operation and maintenance of facilities.<br />
o Interference with the free speech and movement of any academic and/or <strong>com</strong>munity<br />
members.<br />
o Dishonesty, including provision of false information, alteration or misuse of<br />
documents.<br />
o Plagiarism and/or other academic cheating, impersonation, misrepresentation, or<br />
fraud.<br />
o Theft, abuse of, or unauthorized use of personal or Bastyr University property.<br />
o Use of illicit drugs or being on the premises in a drug or alcohol-intoxicated state.<br />
SCOPE OF PRACTICE AND CONFLICT OF INTEREST<br />
While at the Bastyr Center for Natural Health, a Bastyr University external shift site, or an approved<br />
preceptor shift, the intern clinician’s scope of practice is limited to the scope of practice of his or her<br />
supervisor and shift. An intern clinician may not exceed the scope of practice of the supervising<br />
clinician nor the scope of practice provided as care on the shift.<br />
Note: Students may not refer a patient to their private practice in another licensed profession. This<br />
constitutes a conflict of interest and will result in disciplinary action, jeopardizing the student’s status<br />
in their degree program, up to and including dismissal from the university.<br />
5
DRESS, HYGIENE, AND APPEARANCE REQUIREMENTS<br />
The purpose of the dress code is to develop and convey professionalism and to support an attitude of<br />
respect toward patients, the clinic, and natural medicine. All clinical staff, faculty, and students<br />
working when the clinic is open for business must <strong>com</strong>ply with the dress code. If staff, faculty, or<br />
students are not on duty and stop by the clinic when not dressed professionally, they should avoid<br />
lingering where patients are present. All interns must be dressed appropriately for the duration of their<br />
entire shift, including preview and review.<br />
The dress code requires that students wear clean, neatly pressed and professional clothing in good<br />
condition. Clothing should be dressy rather than casual. In <strong>com</strong>pliance with health department<br />
regulations, open-toed sandals or shoes are not permitted in the clinic. Backs, abdomens, and mid to<br />
lower chests should not be revealed by the cut of one’s clothing. Women’s breasts or underwear should<br />
not be visible when bending forward.<br />
Clothing considered too casual for the clinic includes: denim material of any color, jeans-style pants,<br />
athletic footwear, slipper-type footwear, deck shoes without socks, athletic clothing including casual<br />
T-shirts, polo shirts, tank tops, sweat shirts, sweat pants, shorts, spaghetti strap sundresses and shirts,<br />
cropped tops, and low-riders or low cut pants. Undergarments should not show through clothing. If belt<br />
loops are visible, a belt or suspenders must be worn.<br />
Men are required to wear a shirt and tie unless they are wearing a dress shirt that does not require a tie.<br />
Allowable exceptions to a shirt and tie include turtlenecks, turtleneck sweaters, and mandarin collar or<br />
collarless dress shirts. Wearing medical smocks or surgical scrubs and clean athletic footwear is<br />
allowable on physical medicine shifts in ND clinic only.<br />
Women are required to wear an appropriate top (sweater, blouse, or shirt) and bottom (dress slacks,<br />
pants, or skirts). Skirts and dresses must be of modest cut and length. Clothing should never be tight<br />
fitting or revealing. An appropriate dress or skirt of modest length must cover tights and leggings. No<br />
leggings or tights may be worn alone as slacks or pants.<br />
All clinicians in the Acupuncture and Oriental Medicine clinic must wear a white lab coat of knee<br />
length with lapels over their street clothing as described above. This coat must be clean and pressed at<br />
all times. The student is responsible for his or her own lab coat and its care (washing and pressing). It<br />
is not permissible to borrow another clinician’s lab coat without the owner’s permission.<br />
It is preferable that clinicians have no visible piercing or tattoo. Earrings and modest nose piercings are<br />
the exception. Visible tattoos must be minimal and tasteful, since many patients find them offensive.<br />
Extensive or dramatic tattoos must be covered by clothing, such as long sleeves, wherever possible.<br />
Please be aware of breath and body odors when at the clinic. The Bastyr Center for Natural Heath is a<br />
scent free workplace. Do not wear any scents or perfumes in the clinic. Keep hair, beards, and<br />
fingernails clean and neatly trimmed. Tie or pin back long hair, whether you are male or female. Hair<br />
should not be shocking or outrageous in style or color.<br />
Photo ID badges are required at all times while in the clinic. Some external clinics may specify and<br />
provide their own ID badges that should be worn instead of badges issued by the Bastyr Center for<br />
Natural Health. Consult your site supervisor for specifics.<br />
Dress code adherence is mandatory when representing Bastyr Center for Natural Health or Bastyr<br />
University at external sites or events, unless the site has different dress requirements.<br />
No food or beverage consumption is allowed in the exam rooms. Keep the exam rooms free of nonclinical<br />
personal items. Cupboards are present in the exam rooms to store your belongings.<br />
6
DRESS CODE VIOLATIONS<br />
It is up to each individual to follow this code. The clinical faculty, Dean and Associate Dean, or their<br />
designee, will respond to incidences of non-adherence to this dress code on a case-by-case basis.<br />
Violations of the dress code can result in the following:<br />
For a first offense, students receive a written warning and can be sent home for the shift. If sent home,<br />
this shift will count as an unexcused absence. Students will lose all hours and patient contacts for that<br />
day’s shift.<br />
For a second offense, a student will be sent home and fail the shift.<br />
REGISTERING FOR SHIFTS/ROTATIONS<br />
The following information pertains to all students registering for clinic shifts at the Bastyr Center for<br />
Natural Health. For program-specific shift registration requirements, please see the respective Student<br />
Clinician Handbook module for your program.<br />
Bastyr University utilizes two-quarter scheduling. Clinic shift and didactic course registration is<br />
<strong>com</strong>pleted for all clinic-eligible students for summer/fall and winter/spring.<br />
Clinicians have the opportunity to request supervisors for their clinical shifts. While every effort will<br />
be made to meet these requests, there are no guarantees that these requests will be met.<br />
Each clinician may be assigned at least one, and could be assigned more, Saturday shifts during each<br />
year of their clinical training. Exception will be made for clinicians who have religious obligations that<br />
prevent their working on Saturday. Primary clinicians are required to enroll in external/offsite shifts as<br />
outlined by their respective program, unless they do not meet requirements. Should a new offsite shift<br />
be<strong>com</strong>e available after clinical assignments, the clinic Associate Registrar reserves the right to move<br />
clinicians to the new location, as long as it does not cause any undue time conflicts with didactic<br />
courses, or violate the religious restrictions described above. In addition the clinic Associate Registrar<br />
reserves the right to alter student clinical shift schedules during the year.<br />
It is the responsibility of the student to turn in his or her registration form by the posted deadline. If<br />
registration forms are received after deadlines, shift assignments can be affected and late fees will be<br />
assessed.<br />
SPECIALTY SHIFTS/ROTATIONS<br />
The following are considered specialty shifts, and requests by the clinician are required if he or she is<br />
interested in being assigned to a shift:<br />
ND Clinics:<br />
Diabetes and Cardiovascular Health – Students must send a short email to Dr. Ryan Bradley and/or Dr.<br />
Natalie Freedman explaining why they are interested in participating in this shift. Additional reading<br />
and work outside of the shift time is required, and the shift requires an additional 30 minutes<br />
attendance time due to patient schedule requirements. Additional clinical credit may not be given for<br />
this extra time.<br />
Homeopathy – This rotation is open to both primary and secondary students. Students may request a<br />
two-quarter block or a single quarterly shift. Permission from the Chair of Homeopathy is necessary<br />
for clinicians who wish to pursue the study of homeopathy further and is dependent on space<br />
availability.<br />
7
Integrated care shift – This shift is supervised by an MD who has trained in integrative medicine and<br />
focuses on minor surgery and management of other health care issues.<br />
IWC/ND<br />
Students are re<strong>com</strong>mended to <strong>com</strong>plete the AIDS and Alternative Medicine elective prior to selecting<br />
the HIV/AIDS integrated wellness shift. Final assignments are determined in conjunction with an ND /<br />
IWC Supervisor. ND students must be willing to <strong>com</strong>mit to this shift for two consecutive quarters.<br />
The Immune Wellness Clinic shift (IWC) allows low-in<strong>com</strong>e people living with HIV/AIDS to receive<br />
free or low cost care at the clinic and discounts at both dispensaries. This program is subsidized by<br />
Bastyr University. To qualify for this program, patients must have gross in<strong>com</strong>e less than 200% of the<br />
federal poverty in<strong>com</strong>e guidelines. Patients apply by <strong>com</strong>pleting applications processed by the<br />
business office. The patients are referred by their <strong>com</strong>munity case managers (medical social workers),<br />
doctors, or friends in the program. The Thursday evening IWC shift is an integrated shift involving ND,<br />
AOM, and Nutrition supervisors and students. Case Review integrates all students into a group review<br />
process. The program supports over 150 visits each month.<br />
There are certain guidelines for working with IWC patients:<br />
o All IWC patients are encouraged to have visits in Naturopathy, Acupuncture and<br />
Oriental Medicine, and Nutrition.<br />
o Most patients use this program and its resources responsibly and excessive selfreferred<br />
visits are not allowed. The provider overseeing the care of such a patient<br />
who may be abusing the system is responsible for developing and directing the care<br />
plan.<br />
The IWC program does not pay for laboratory or diagnostic testing. The business office will provide<br />
accurate information to questions about coverage.<br />
ND/AOM– These shifts are only available to dual-track students who are primary-eligible in both<br />
programs. The ND/AOM shift (located in ND Team Care) counts as a patient care shift in the ND<br />
program and the AOM/ND shift (located in AOM Team Care) as an intern shift in the MSA or<br />
MSAOM program.<br />
Research Shift – This shift focuses on patients involved in a research protocol.<br />
IV Therapy – This shift provides general patient care and on provision of IV Therapies to patients. It<br />
is only open to primary eligible students.<br />
Biofeedback – This is the counseling portion of the Integrated Pain Management Shift.<br />
Visceral Manipulation – This shift is open to both primary and secondary clinicians who will provide<br />
both general patient care and their visceral manipulation skills.<br />
Pain Management Shift – This is an integrated AOM/ND(PMed)/NTR/Counseling shift held at BCNH<br />
focused on the treatment of patients who experience chronic pain. Gathering of information associated<br />
with research studies may be part of the student’s duties.<br />
AOM Clinics:<br />
IWC/AOM – Students must have taken the Public Health Issues in AOM course, or must receive<br />
permission of the Associate Dean or AOM/IWC supervisor for this shift.<br />
8
AOM/ND – These shifts are only open to dual-track students who are primary-eligible in both<br />
programs. The ND/AOM shift counts as a patient care shift in the ND program, and the AOM/ND as<br />
an intern shift in the MSA or MSAOM program.<br />
Pain Management Shift – This is an integrated AOM/ND(PMed)/NTR/Counseling shift held at BCNH.<br />
Gathering of information associated with research may be a part of the student’s duties.<br />
Offsite/External Clinics:<br />
External Sites – ND and AOM clinicians may be required to do offsite shifts when there are openings<br />
at times the clinician has indicated availability, and the intern meets the requirements for the shift.<br />
EXTERNAL SITES/ROTATIONS<br />
Standard policies on attendance, evaluation of students and instructors, professional behavior, and<br />
discipline apply at all Bastyr external sites. The clinic program supervisor provides the instructor and<br />
student with the forms necessary for documenting these processes. Instructors at external sites know<br />
internal clinic shift procedures, such as case preview/review and documentation guidelines, and are<br />
encouraged to follow these procedures, as feasible to the site. The instructor may develop special<br />
procedures that meet the unique needs of a site. All external site registration occurs during clinic<br />
registration, and some supervisors may require an extra screening step such as a letter of intention,<br />
from the student. Most external sites require additional screening such as documentation and<br />
vaccinations. Some external clinics require an additional onsite orientation. A list of current external<br />
sites is provided to students during the clinic registration process.<br />
ATTENDANCE REQUIREMENTS AND GRADES<br />
All student clinicians will be required to attend at least 80 percent of each assigned quarterly shift,<br />
including clinic assistant, observation, intern, and patient care shifts, in order to receive a grade of<br />
Achieved Competency (AC) or In Progress (IP), for the shift. Hours missed because of holidays and<br />
emergency or other administrative closures do not count against the total quarter’s attendance for the<br />
purpose of assigning a grade, but all missed hours, including university holidays and administrative<br />
closures must be made up. A student must attend at least nine daily shifts for each quarterly shift in<br />
order to pass that shift.<br />
A student who does not attend at least 80 percent of the quarterly shift (two excused absences) will<br />
normally receive a failure for that quarterly shift, lose all hours and patient contacts and the entire<br />
quarterly shift will need to be repeated. Exceptional circumstances resulting in a third absence requires<br />
approval by the supervisor. Please note that students must <strong>com</strong>plete <strong>10</strong>0 percent of their required<br />
clinical hours before they will receive a re<strong>com</strong>mendation for graduation.<br />
An in<strong>com</strong>plete grade may only be awarded for documented medical necessity and must meet the<br />
guidelines published by the university. Students must apply to the Associate Dean or clinic<br />
administrator in their respective program in order to apply for a grade of in<strong>com</strong>plete. See the Bastyr<br />
University Catalog for more information on in<strong>com</strong>plete grades.<br />
Students will receive a grade of IP (in progress) if they miss any shifts, whether the absence was due to<br />
a holiday, administrative clinic closure or personal absence. Clinic grades of IP will be changed to AC<br />
at the end of the program if a review of the student’s records has shown that the clinic shifts have been<br />
made up.<br />
Clinic grades of IP will be changed to AC at the end of the program if a review of the student’s records<br />
has shown that missing hours have been <strong>com</strong>pleted.<br />
9
Students will receive a grade of AC (achieved <strong>com</strong>petency) only if they are in attendance for the entire<br />
quarter and all clinical work reflects the required skill level.<br />
Students who are 15 minutes late to their assigned shift will receive a written warning for a first event<br />
and need to make up missed time. A clinic sanction will be given for a second event in the same<br />
quarter. If a third event occurs, the student is eligible to fail the quarterly shift. (For more information,<br />
see page 14, the Sanctions section under Grading & Student Performance.)<br />
ABSENCES<br />
It is the responsibility of every student clinician to inform their assigned supervisor of any absence.<br />
PLANNED ABSENCES<br />
Complete the bottom portion of the Student Clinician Absence/Substitution Form. Complete a separate<br />
form for each shift you will miss. (A sample of this form is included in the appendix on page 57.)<br />
Complete the bottom portion, including your name, ID#, today’s date, date of expected absence, shift,<br />
program, and reason for absence.<br />
Notify the supervisor and have him or her sign in the appropriate space. Primary ND and AOM interns<br />
must secure a substitute to cover their shift and the substitute must sign the form. In the case of dual<br />
primary assignment (two primaries assigned to one treatment room), the supervisor may or may not<br />
require a sub. If a substitute does not sign the form and does not show up for the shift, the student<br />
assigned to the shift is held responsible and will receive sanctions for an unexcused absence. Once the<br />
form is signed by the substitute student, the substitute is responsible for attending the shift.<br />
Once the form is <strong>com</strong>pleted, give it to the faculty administrative assistant in room S206 at the clinic,<br />
who keeps it for the quarter.<br />
Primary clinicians are also responsible for contacting the patients who are <strong>com</strong>ing in specifically to see<br />
them. Patient phone numbers are available from the front desk. Ask patients to contact the front desk if<br />
they wish to reschedule their appointments. Primary clinicians must also notify a<br />
secondary/observation clinician of their intended absence.<br />
Secondary/observation clinicians must also secure a substitute to cover shifts, and <strong>com</strong>plete the<br />
required form including signatures. In addition, secondary clinicians must notify the supervisor and<br />
primary student clinician of their absence.<br />
If students are not able to attend their scheduled shifts during the first week of a quarter, an<br />
“absence/substitution” form must be <strong>com</strong>pleted and handed in prior to the date of the absence. A<br />
student will automatically receive a grade of failure, and be dropped from the shift if no notification<br />
has been received and the absence extends to the second week of the quarter.<br />
UNEXCUSED ABSENCES<br />
An unexcused absence is defined as failing to notify the scheduled supervising clinical faculty member<br />
of the absence prior to the start of the shift. The first unexcused absence during a term results in the<br />
student clinician being required to <strong>com</strong>plete three makeup shifts (12 hours). A second unexcused<br />
absence will result in a grade of F for the quarter and the loss of the entire shift’s hours and patient<br />
contacts. The shift will need to be repeated and paid for a second time. Supervising clinical faculty<br />
members may, at their discretion, accept notification of an absence after the start of the clinic shift in<br />
the event of an emergency. Even if the student calls the supervising clinical faculty member prior to<br />
the missed shift, the supervisor reserves the right to define the missed shift as an unexcused absence<br />
<strong>10</strong>
and assign sanctions. Two failure grades for clinical training shifts automatically place a student on<br />
final probation with eligibility for dismissal from the program.<br />
A substitute intern who is absent for the shift they agreed to cover and fails to notify the clinical<br />
faculty member is also subject to the unexcused absence policy.<br />
Midwifery students must have a substitute available on an “immediate-notice” basis for all shifts<br />
missed due to their attendance at a birth.<br />
EMERGENCY LEAVES<br />
When an emergency or illness prevents students from attending a shift, they must notify their<br />
supervisor prior to the start of the shift.<br />
Notifying the Supervisor:<br />
In the event of an emergency, the intern must notify her or his supervisor. The supervisor may be<br />
contacted by calling the clinic and asking that the supervisor be contacted. In the event the supervisor is<br />
not available, the intern may, 1) leave a voice mail and an email for the supervisor and 2) contact the<br />
Associate Dean/lead faculty member by email regarding the nature of your emergency. If possible, please<br />
provide a substitute for a missed shift. Be aware there may be additional requirements for specific clinical<br />
programs (ND, AOM, Nutrition, or Health Psychology) which are outlined in the program specific<br />
handbook.<br />
SUBSTITUTE/EXTRA HOURS<br />
Students receive full credit for all hours that they substitute for another student. Substitute hours make<br />
up shift hour deficits.<br />
Students should record the substitute/extra time on their regular time sheet under the substitute/extra<br />
hour section. Only four hours may be recorded for any one daily shift.<br />
AOM sub shifts must go on an AOM time sheet. CHM sub shifts must go on a CHM time sheet. ND<br />
sub shifts must go on an ND time sheet. Do not mix AOM, CHM and ND shifts on one time sheet.<br />
The supervising clinical faculty must sign for the hours and patient contacts received on each day.<br />
All patients that clinicians see on substitute shifts count towards the total patient contact requirements<br />
(350 patients for ND students and 400 patients for AOM students). These patient contacts are tracked<br />
on a summary of patient contacts form, separate from those received for their regularly scheduled shift.<br />
Hours that accumulate in the substitute/extra “bank” may not be used to construct a new shift. These<br />
hours are only used to make up shift hour deficits or may be accumulated to meet future deficits.<br />
The clinic registrar will automatically transfer substitute and extra hours into areas showing a deficit of<br />
hours. These changes are documented at your quarterly update.<br />
All interim shift hours are logged on the Interim timesheet. Excess Interim hours count towards sub<br />
hours once all Interim hour requirements are met.<br />
Interim hours (hours <strong>com</strong>pleted during the week after the end of the academic/didactic term during fall,<br />
winter and summer terms) must be made up by substituting on another interim shift. You may not use<br />
substitute hours <strong>com</strong>pleted during a regular quarterly shift to <strong>com</strong>plete interim requirements.<br />
AOM: You must <strong>com</strong>plete all observation hours, including observation interim hours, prior to<br />
beginning work on your first primary treatment shift. It is important to verify how many hours you<br />
must make up on your observation shifts, and then <strong>com</strong>plete them before you are scheduled to start as<br />
a primary intern.<br />
11
GRADING AND STUDENT PERFORMANCE<br />
Clinic grading is an achieved <strong>com</strong>petency system. Each student must receive a grade of achieved<br />
<strong>com</strong>petency (AC) in order to receive credit and proceed to the next shift. The achieved <strong>com</strong>petency<br />
grading system is not a pass/fail grading system. A grade of AC means that all clinical skills for each<br />
level are successfully mastered, <strong>com</strong>mensurate with the student’s current status at the clinic.<br />
In the event that a student receives an evaluation of partial <strong>com</strong>petency (PC) for any skill listed in their<br />
evaluation for that term, they will receive a grade of PC for that shift. A learning contract will be<br />
developed by the Associate Dean/Clinical Lead for the remediation of the shift. The student will have<br />
until the end of the following term (counted as the Friday of the 11 th week) to <strong>com</strong>plete remediation as<br />
outlined in the learning contract. A grade of F may be assigned if the student:<br />
o has received a grade of PC for more that one to three skills<br />
o has failed to achieve a grade of AC for the same specific skill in more than one term<br />
o has a skill deficit that the faculty member does not feel can be remediated within the time<br />
allowed<br />
At the end of the quarter, the periodic evaluations are a reference for the supervisor when <strong>com</strong>pleting<br />
each student’s quarterly performance evaluation. The student will receive a performance evaluation<br />
each quarter.<br />
A student can receive the following quarterly grades:<br />
AC - Achieved <strong>com</strong>petency<br />
PC - Partial <strong>com</strong>petency<br />
IP - In progress<br />
I - In<strong>com</strong>plete<br />
W - Withdraw<br />
F - Failure<br />
Here is a brief summary of the meaning of each grade. Please refer to the Bastyr University catalog for<br />
the <strong>com</strong>plete grading policy.<br />
Achieved Competency (AC): Students receive an AC upon demonstrating mastery of all the clinical<br />
knowledge, skills and attitudes outlined on the evaluation form <strong>com</strong>mensurate with the student’s<br />
current level in their clinic program, and they have missed no clinic time during the regular eleven<br />
weeks of the clinical academic term.<br />
Partial Competency (PC): To receive a grade of PC, the student will have received an assessment of<br />
PC on one or more of the mandatory skills in their evaluation. The student may be deficient in no more<br />
than three skills which the supervisor feels can be successfully remediated within one term of the<br />
student receiving the grade of PC. The student must meet with the associate dean or program lead<br />
within the first week of the next quarter to create a learning contract. The student will be required to<br />
successfully meet the terms of the learning contract no later than the end of the term after receiving the<br />
PC grade.<br />
In Progress (IP): An IP grade means a student has achieved <strong>com</strong>petency but has missed one or more<br />
weeks during the academic term, resulting in <strong>com</strong>pleting less than 44 hours for the shift in question.<br />
When <strong>10</strong>0 percent of hours and/or patient contact requirements are <strong>com</strong>plete, the grade will change to<br />
12
an AC. This change will be <strong>com</strong>pleted by the clinic registrar towards the end of the student’s program,<br />
and will not be <strong>com</strong>pleted on a term by term basis.<br />
In<strong>com</strong>plete (I): Students will receive an in<strong>com</strong>plete only for medical or other verifiable emergencies.<br />
In order to receive an in<strong>com</strong>plete grade for a clinic shift, a student must contact the Associate Dean<br />
and provide written documentation of illness or personal emergency. An in<strong>com</strong>plete grade may only be<br />
assigned after the seventh (7 th ) week in the quarter. The student must be in good academic standing<br />
and will not apply to a student who is failing a class or clinic shift. All in<strong>com</strong>plete grades not<br />
successfully <strong>com</strong>pleted by the end of the third week of the following quarter will convert to a failure (F)<br />
grade. In the event of an ongoing medical or family emergency, in<strong>com</strong>pletes may be extended beyond<br />
the third week of the following term by the Associate Dean or Dean of the program in which the<br />
in<strong>com</strong>plete occurred.<br />
Withdraw (W): A student officially withdraws by notifying the clinic registration staff, who will then<br />
notify the registrar, supervisors and faculty members. The student must also obtain approval from the<br />
Dean of their program. Withdrawal requests are allowed for documented emergency purposes only and<br />
occur only through the eighth week of the quarter. An approved withdraw allows a student to keep all<br />
patient contacts. Hours <strong>com</strong>pleted to date will be used as substitute/extra hours. The only exception to<br />
this is when the student has received a mid-quarter letter identifying areas of deficient <strong>com</strong>petency<br />
prior to a withdrawal, and has not demonstrated that these areas of deficiency are at AC level at the<br />
time of withdrawal. In this case, all patient contacts and hours prior to the withdrawal will be forfeit.<br />
Note: When a student officially drops a shift after the deadline, the result will be a loss of all clinic<br />
credits/hours/patient contacts for the entire quarter shift.<br />
Failure (F): The student does not satisfactorily demonstrate <strong>com</strong>petence as outlined for their level of<br />
training. At the discretion of the Dean or Associate dean, a grade of failure may also be applied in the<br />
event of an egregious infraction of clinic policy that endangers a patient or violates state or federal law.<br />
This results in a loss of all clinic credits, hours, and patient contacts for the entire shift, and will require<br />
a repeat shift at Bastyr Center for Natural Health. The failure of a clinic shift places the student on<br />
academic probation. Two quarterly shift failures will automatically place the student on final<br />
probation. In addition the dean, or their designee, will make a re<strong>com</strong>mendation to the school<br />
promotions <strong>com</strong>mittee regarding dismissal from the university. In the event that the student is not<br />
dismissed, a learning contract is developed for the student. The student must successfully meet the<br />
requirements of the learning contract to avoid dismissal.<br />
FAILURE RISK<br />
To provide time to improve their performance, students who are at risk for failing a quarterly shift are<br />
notified verbally and in writing by their supervising clinical faculty of their deficiency. The letter will<br />
make suggestions for improvement and provide a timeline for the student. The notification is made as<br />
soon as the deficiency is evident, preferably mid-quarter, unless the deficiencies are not evident until<br />
after that time. If a student is having difficulty meeting the requirements of their clinical training, they<br />
should seek assistance from their clinic advisor or the associate clinical dean or program lead. A copy<br />
of this letter is sent to the student’s advisor, the program dean or their designee, and to the registrar's<br />
office (for the student’s clinic file). The notification letter will identify each area of concern and will<br />
provide clear guidelines about what is required in order to achieve <strong>com</strong>petency. Students must meet<br />
with their supervisor and/or advisor if they receive notice of risk of failing a shift. It is solely the<br />
student’s responsibility to arrange this meeting.<br />
AOM: All interns must get a midterm letter for each of their shifts.<br />
13
If students wish to file a grievance or appeal a clinic grade, they must follow the university’s academic<br />
grievance and appeal of grade procedure as outlined in the Student Handbook.<br />
GRADING & TIME SHEETS<br />
Clinicians receive a pre-printed clinic time sheet for each assigned shift and are responsible for<br />
accurately entering hours and patient contacts on this form. Supervisors must initial each shift and<br />
patient contact for the student to receive credit. Once the quarterly shift is <strong>com</strong>pleted, the supervisor<br />
will assign a grade for the shift. The time sheet and the grade recorded on it are submitted by the<br />
supervisor to the clinic registrar for processing of grades and credit.<br />
Clinicians are required to turn in all original paperwork to their supervisor in a timely manner at the<br />
end of each quarter. The clinic registrar does not accept copies of clinic paperwork. Upon <strong>com</strong>pletion<br />
by the supervisor, the registrar’s office records the grades for each shift. A student who fails to turn in<br />
their clinic paperwork does not receive credit for the quarter. Failing to respond to requests to turn in<br />
paperwork may result in an appearance before the student progress <strong>com</strong>mittee.<br />
In the event a clinician loses his or her paperwork, the clinician is responsible for recreating the<br />
paperwork with all appropriate signatures. A new form can be obtained from the registrar.<br />
Interim paperwork is due at the end of each interim period. Only one quarter of interim hours entered<br />
on a single form is acceptable.<br />
Completed forms left in the basket outside S206 on the second floor are collected by the clinic<br />
program supervisor and go to the clinic registrar on campus daily. Students should keep copies of all<br />
<strong>com</strong>pleted forms and clinic-related paperwork for their own records.<br />
STUDENT PROMOTIONS COMMITTEE<br />
The Student Promotions Committee consists of faculty within a specific school, including the Dean<br />
and Associate Dean or Clinic Lead. This <strong>com</strong>mittee evaluates student academic performance of those<br />
students with academic concerns in the previous quarter(s). This <strong>com</strong>mittee will look at the entire<br />
academic record of the student and make a determination as to the appropriate course of action. The<br />
course of action can include, but is not limited to, a warning, learning contract, probation, or<br />
re<strong>com</strong>mendation for suspension and/or dismissal from the program. The student should contact the<br />
Vice President of Student Affairs for counseling and advice if they should be called to meet with this<br />
<strong>com</strong>mittee.<br />
SANCTION/FAILURE EVENT(S)<br />
If a student <strong>com</strong>mits an actionable violation of clinic policy, the student will receive a written sanction<br />
by the supervisor, with a copy to the Associate Dean/Clinic Lead. At the discretion of the supervisor,<br />
the sanction may result in loss of all contacts and hours on the shift for the day in which the event<br />
occurred. Additional penalties may be assigned by the supervisor. A second written sanction on the<br />
same shift will result in a grade of F with the loss of all hours and contacts for the entire shift.<br />
Student will be issued a sanction when they are found to have violated any of the policies of the clinic,<br />
including but not limited to:<br />
o Breaching patient confidentiality.<br />
o Removing any patient ID information from the clinic.<br />
o Acting in an unprofessional or disrespectful manner at any time, including when offshift.<br />
14
o Failing to <strong>com</strong>ply with Blood Borne Pathogen safety policies and procedures, or any<br />
other actions that affect patient, intern, or staff safety.<br />
o Unexcused absence from a clinical shift.<br />
The severity of the sanction will depend on the severity of the offense and can range from loss of<br />
clinical hours and patient contacts, to suspension from the clinic or expulsion from the university. The<br />
involved supervisor and the program Associate Dean, or their designee, will determine the type of<br />
sanction. Sanctions are not grades and are, therefore, not subject to appeal under the appeal of grade<br />
policy. A student may issue a grievance according to the grievance procedure as outlined in the student<br />
handbook.<br />
FAILURE EVENT<br />
A failure event results in a loss of credit for the daily shift including hours and patient contacts.<br />
Additional penalty may include a sanction of up to eight additional hours. The Associate Dean must<br />
initial all sub hours used to remediate the failure event on the failure event time sheet, available from<br />
the clinic registrar or associate dean.<br />
MIDTERM/WARNING LETTER<br />
A warning letter is provided to the student by clinical faculty in the event that the student is not<br />
performing up to AC level in any area for which the intern is being evaluated. The letter is provided as<br />
early in the quarter as the deficient performance be<strong>com</strong>es evident. In the School of Acupuncture and<br />
Oriental Medicine a midterm letter evaluating performance is given to all students, regardless of<br />
academic performance.<br />
LOSS OF CREDIT, SUSPENSION, DISMISSAL<br />
There are specific actions and behaviors that can result in partial loss of credit, failure (F) for an entire<br />
shift, suspension and/or dismissal from the clinic. The following actions will result in a clinic sanction:<br />
o Failure to follow the clinic attendance and absence/substitution policy.<br />
o Failure to follow the clinic policies and procedures as described in the <strong>Global</strong> <strong>Module</strong><br />
Handbook or the school specific handbook.<br />
o Failure to follow the instructions or re<strong>com</strong>mendations of the supervising<br />
doctor/physician/faculty.<br />
o Causing intentional harm to a clinic patient, neglect of a patient’s care and safety, or<br />
any form of verbal abuse.<br />
o Inappropriate behavior or unethical conduct when interacting with clinical faculty,<br />
staff, patients, or students.<br />
o Failure to follow the telephone and email contact policies and procedures.<br />
The following violations will result in loss of clinic credit, suspension, and/or dismissal, depending on<br />
the circumstances and severity of the violation. In the case where suspension or dismissal may be<br />
appropriate, the program Associate Dean, Dean or their designee will make a re<strong>com</strong>mendation to the<br />
Vice President for Academic Affairs according to the circumstances of each incident:<br />
o Dishonest conduct.<br />
o Practicing medicine without a license. This includes practicing clinically outside of<br />
school prior to <strong>com</strong>pletion of a degree or certificate.<br />
15
o Violation of the Bastyr Center for Natural Health code of ethics.<br />
o Breach of patient confidentiality, which includes the removal of any identifying<br />
patient material from the clinic.<br />
o Willful refusal to <strong>com</strong>ply with the instructions of the student’s supervisor, Associate<br />
Dean, Dean, safety officer, or clinic staff.<br />
ON-SHIFT POLICIES, ROLES, AND PROCEDURES<br />
CASE PREVIEW AND REVIEW PROTOCOLS<br />
The following are re<strong>com</strong>mendations to make case preview a better learning and teaching experience:<br />
o Case preview is the first 30 minutes of each four-hour shift. Case review is the last 30<br />
minutes of each four-hour shift.<br />
o Supervising clinical faculty members are responsible for starting and ending case<br />
preview on time. Clinic supervisors and students should be familiar with the day’s<br />
cases.<br />
o Students are required to start on time with all of their cases reviewed in advance of<br />
preview. All lab results and medical records should be in the chart and the students<br />
ready to discuss them.<br />
o The student team from each room presents a brief identification of their patients<br />
scheduled on the shift.<br />
o Patient age, sex and other relevant data<br />
o Chief and secondary <strong>com</strong>plaint(s)<br />
o Then, one room at a time, the primary student clinician will present the purpose of<br />
the days’ visit for each patient scheduled. The clinician should include other<br />
relevant information for each case, such as diagnostic testing and previous treatment<br />
results.<br />
o If this is an ROC, a short summary should be presented of past data pertinent to<br />
understanding the assessment, and the response of the patient to the treatment. In<br />
addition, note future plans. A discussion of that day’s plan should be presented.<br />
o If this is an FOC, a discussion of the <strong>com</strong>plaint should occur that includes possible<br />
differential diagnosis, confirmatory exams and therapeutic ideas.<br />
o All the other student clinicians should be attentive to each case.<br />
o By the end of case preview, all the cases will have been discussed as a group, and the<br />
students will be prepared to start the first scheduled patient’s care.<br />
o If students are more than 15 minutes late for case preview without prior arrangement<br />
or an emergency, there will be no credit given for case preview, and the 30 minutes<br />
time will need to be made up at a future date. Shift supervisor will mark absent on<br />
the CP (case preview) section of the attendance sheet for that shift. Case preview is<br />
valuable educational time to prepare the student clinicians for the day’s patients.<br />
o Case presentations must be concise and <strong>com</strong>pleted within six to seven minutes<br />
16
CHECK-OUT AND PAYMENT FOR SERVICES<br />
When the patient visit is <strong>com</strong>pleted, the primary or secondary student clinician must ac<strong>com</strong>pany the<br />
patient to the “Please Wait Here” sign at the front desk for rescheduling and checkout. Be sure to<br />
personally deliver the <strong>com</strong>pleted superbill to the front desk staff before the end of the patient’s<br />
treatment. The intern is responsible for ensuring the superbill is accurately <strong>com</strong>pleted, with all<br />
diagnostic and procedure codes. Students should not linger at the front desk and should only wait there<br />
if assistance is required for patients with a special scheduling need. No information regarding<br />
diagnosis or treatment is to be discussed outside of the exam room other than that needed to schedule<br />
an appointment. If there is a line of patients waiting, the student should leave the patient at the “Please<br />
Wait Here” sign and return to shift.<br />
All patients must check out at the front desk before leaving the clinic. Student clinicians are<br />
responsible for notifying the front desk of any late patient checkouts.<br />
Students must not discuss fees or payment arrangements with patients. The patient services department,<br />
prior to the patient visit, arranges all payments or discounts on services.<br />
TIME MANAGEMENT<br />
Student clinicians are responsible for beginning and ending patient visits on time.<br />
o A regular FOC last up to 80 minutes.<br />
o Homeopathy FOC’s last up to 1<strong>10</strong> minutes.<br />
o Nutrition FOC’s last up to 50 minutes.<br />
o An acute FOC lasts up to 50 minutes.<br />
o A regular ROC lasts up to 50 minutes.<br />
o An acute ROC lasts up to 20 minutes.<br />
An “introduction visit” lasts 15-20 minutes. The purpose of this visit is to answer patient questions and<br />
provide general information. No diagnosis or treatment is given. This visit is available in Naturopathic<br />
Team Care only.<br />
As each patient visit is <strong>com</strong>pleted, the exam room is organized, cleaned and prepared for the next<br />
patient. All equipment previously used, should be disinfected.<br />
Time should be managed so that the student clinicians are done and are ready for case review for the<br />
last 30 minutes of the shift.<br />
Students cannot determine the length of a visit. This is the responsibility of the supervising provider.<br />
When a patient schedules and is seen for a visit, the length of the visit should not be changed without<br />
the supervising provider’s consent.<br />
CLINICIANS - PRESENCE OR ABSENCE OF STUDENT<br />
Requests by Patients<br />
When a patient initiates a request that student clinicians not be present for portions of the office call, it<br />
is appropriate for the attending physician to honor the request and facilitate meeting it. It must be<br />
assumed that the patient has a legitimate reason for making this request. If the request was made to the<br />
student clinician, it is acceptable for the supervisor to clarify this request with the patient. However, it<br />
is not appropriate for staff, students, or faculty to initiate or encourage any patient to ask for changes<br />
from the assigned schedule, or for a different clinician arrangement. Any special arrangement<br />
requested by a patient must be approved by the Associate Dean or the Clinic Director (ND) after the<br />
first office call.<br />
17
CLINICIAN RESPONSIBILITIES - PRIMARY/INTERN STUDENT<br />
Primary student clinicians are responsible for presenting their cases in case preview and review,<br />
directing patient interviews, taking the case notes and assessing the patient both subjectively and<br />
objectively. After collecting this information, students meet with the supervising faculty to discuss the<br />
diagnostic strategy, and once a diagnosis is reached, establish the plan. Primary student clinicians are<br />
encouraged to think through and develop their own strategy and management of the case, although the<br />
supervising clinical faculty makes the final decisions and is responsible for all aspects of case<br />
management. Specifically, primary student clinicians:<br />
o Preview the case with the attending clinical faculty member and secondary student<br />
clinician during case preview before initiating contact with the patient.<br />
o Monitor the electronic patient schedule and physically check the reception area for<br />
the first 15 minutes of a scheduled appointment in the event of a late patient. If a<br />
patient arrives more than 20 minutes late for their appointment, the receptionist will<br />
page the supervisor. The supervisor will determine the viability of starting the<br />
appointment or the need to reschedule the appointment.<br />
o Meet the patient in the reception area and escort the patient to the exam room.<br />
Clinicians should explain to a new patient how the clinic operates, how patient visits<br />
are conducted, and how many supervisors and/or observers will be attending the<br />
visit. (From this point onward, the patient is not left unattended, except for the<br />
purpose of providing privacy during disrobing and dressing when indicated by a<br />
procedure, when the student clinicians and supervisor discuss the case in private<br />
consultation, or during the resting phase of an acupuncture treatment.) Make sure to<br />
tell all patients to wait until the clinician returns before climbing onto the<br />
exam/massage table. Additionally, do not leave patients with limited physical or<br />
mental capacities unattended for more than brief periods of time. Young or<br />
profoundly mentally handicapped patients must not be left alone in the treatment<br />
room at any time.<br />
o Take case notes in black pen only, neatly, and in an organized manner, following the<br />
standard SOAP formats. An S, O, A, or P should be written for the appropriate<br />
section on the progress form. Draw a single line through any corrections and initial<br />
the correction. Do not scratch out any part of the chart notes.<br />
o Charts must be <strong>com</strong>pleted within 24 hours. Any unfinished charts including<br />
unfinished chart notes must be returned to Medical Records one hour after shift, or<br />
checked out with your name and your clinic location noted.<br />
o Carry out your supervisor’s instructions with respect to interviewing the patient,<br />
performing a physical exam, diagnostic studies, and making referrals and treatment<br />
plans.<br />
o Familiarize the secondary student clinician with their style of case management, and<br />
direct/support the secondary student clinician’s role as an observer and facilitator.<br />
o Sign the chart when it is <strong>com</strong>pleted, fill in the summary of patient contact “health<br />
data and medication list” forms on the inside cover of the chart, make certain that<br />
the superbill is <strong>com</strong>pleted correctly, including CPT and ICD9 codes, and obtain the<br />
supervisor’s signature on all forms and case notes.<br />
o Re<strong>com</strong>mend that the patient is rescheduled after consultation with the supervisor.<br />
For the Naturopathic Team Care clinic, re<strong>com</strong>mend that the patient is rescheduled at<br />
18
a time that the supervisor and, if possible, the primary and/or secondary student<br />
clinicians are present. The supervisor, with the knowledge and consent of the patient,<br />
must approve exceptions. In the Acupuncture or CHM Team Care clinics, attempt to<br />
schedule on a shift with the primary intern unless specifically instructed otherwise<br />
by the supervisor.<br />
o Follow-up by telephone with the patient, with supervisor approval, when there is a<br />
cancellation or no-show for a scheduled visit (both FOC and ROC), to discover why<br />
the patient was unable to <strong>com</strong>e in, determine the state of their health, and to<br />
reschedule an appointment. Limit the length of all phone calls to/from patients to no<br />
more than 3 minutes. Major changes or alterations to treatment plans should only be<br />
made during a patient care visit. All phone contacts need to be pre-approved by the<br />
supervising clinical faculty. Be certain to record any phone contact information in<br />
the patient chart and have it signed by the supervising clinical faculty. (Patients<br />
appreciate personal care and interest shown in their health care.) Check with the<br />
reception staff before proceeding to contact a patient as their reason for absence<br />
may already be known. Chart all phone contacts on a progress note that is signed by<br />
the supervisor.<br />
o Have the time sheet and summary of patient contacts signed off by the<br />
supervisor/clinical faculty at the end of each shift.<br />
o Properly drape patients and pull blinds when patients are to change into a gown.<br />
o Be<strong>com</strong>e familiar with clinic resources, such as patient protocols, therapeutic<br />
notebooks, forms, etc.<br />
o Only practice modalities in which coursework has been <strong>com</strong>pleted and that<br />
supervisors have approved (i.e., utilizing cranial sacral therapy and specialized<br />
techniques such as the use of tuning forks on acupuncture shifts should only occur<br />
on shifts when the supervisor is also proficient).<br />
IMPORTANT: No treatment modality is applied, supplement re<strong>com</strong>mended, nor instruction<br />
given to the patient without the prior approval of the supervisor. This is practicing medicine<br />
without a license and sanctions would be placed on the student.<br />
19
CLINICIAN RESPONSIBILITIES - SECONDARY/OBSERVING STUDENT<br />
Secondary student clinicians have an observer/facilitator role. It is their responsibility to discuss with<br />
primary student clinicians on each shift exactly what role they are to take during the patient visit.<br />
Specifically, secondary student clinicians must:<br />
o Be<strong>com</strong>e familiar with each case on each shift before case preview.<br />
o Make certain that the exam room is in order and that all the necessary supplies are in<br />
the room. In the Naturopathic Team Care clinic, there is a list of supplies for each<br />
room in the cabinet above the sink. Insure that the paging telephone volume is at an<br />
audible level.<br />
o Attend case preview to provide input on each case with the primary student clinician<br />
and supervising clinical faculty.<br />
o Oversee the dispensary care, entering all dispensary items on the prescription form.<br />
Obtain supervisor’s signature on the form, seeing that the date, item, and refill<br />
section are <strong>com</strong>plete. In Naturopathic Team Care, make a copy of the prescription<br />
form for the chart. Secondary clinicians also should take the <strong>com</strong>pleted and signed<br />
forms to the CHM dispensary (AOM or CHM) or give the original <strong>com</strong>pleted and<br />
signed form to the patient (ND).<br />
o At the conclusion of the office visit, ac<strong>com</strong>pany the patient to the front desk to have<br />
the return office visit scheduled, and check out. The student does not need to wait<br />
with the patient. In the event there is a patient being seen by all available Patient<br />
Services Representatives (PSRs), the patient should be taken to the privacy sign<br />
near the front desk.<br />
o Instruct the patient that they will have to obtain and pay for their dispensary items<br />
separately from the visit fees. The secondary student should also direct the patient to<br />
the dispensary.<br />
o Make certain that the room is cleaned and disinfected and ready for use by the next<br />
patient or shift.<br />
o Attend case review during the last half-hour of the shift.<br />
o At the end of the shift, is responsible for having the time sheet and summary of<br />
patient contacts signed off by the supervising clinical faculty.<br />
o Anticipate the paper work that needed on a shift and have it ready: release of records,<br />
diet diary, clinic referral form, etc.<br />
o Complete all information on the “records release form” and have patient sign and<br />
date the form, and when <strong>com</strong>plete obtain supervisor’s initials before copying for<br />
chart and forwarding to Medical Records. Note the name of the requesting primary<br />
clinician on the form.<br />
o If a patient has a second appointment in another department following your<br />
appointment, personally take the patient’s chart to the practitioner or clinician with<br />
your chart notes included and give a brief update to the supervisor or clinicians.<br />
IMPORTANT: No treatment modality is applied nor instruction given to the patient without the prior<br />
approval of the supervisor.<br />
20
SUPERBILL INSTRUCTIONS<br />
Listed below are the fields that must be reviewed and <strong>com</strong>pleted by students and/or supervisors for<br />
each patient visit.<br />
Provider Name: Clearly print the supervising provider name and have the supervisor sign the<br />
bill.<br />
License #: Clearly print the license number of the supervising provider.<br />
Department: Circle the department and/or program that saw the patient.<br />
Patient Information: Make sure that the <strong>com</strong>pleted information is correct, and <strong>com</strong>plete any missing<br />
fields.<br />
Name: Patient’s legal name, printed legibly. Do not use nicknames.<br />
Date of Birth: Verify that the date of birth written on the superbill and patient chart match.<br />
Date of Service: Verify that the date of service is correct.<br />
ICD-9 Codes: List each ICD-9 code in descending order of priority or relevance as related to the chief<br />
presenting illness. Only list four diagnoses on the superbill even if the chart notes indicate more than<br />
four diagnoses. A list of <strong>com</strong>mon diagnoses with ICD-9 codes is located on the back of the superbill. If<br />
a diagnosis is not on the back of the superbill, consult the on-line diagnostic support program to find<br />
the correct code. In the event that the case is a referral from a gatekeeper from a third party payer, the<br />
approved diagnostic code given by the gatekeeper must be listed first. For AOM providers, list only<br />
the approved diagnostic code. In the event of a personal injury claim, list only the billable diagnostic<br />
codes.<br />
AOM: Use only the diagnosis code for the <strong>com</strong>plaint or <strong>com</strong>plaints being treated at that contact. Be<br />
sure to prioritize pain codes when applicable. For personal injury claims and insurance claims, treat<br />
and code for the <strong>com</strong>plaints that were approved by the payor.<br />
Procedure CPT Codes: Circle all procedures performed during the visit. In the column labeled “Dx#,”<br />
indicate the associated diagnosis (1, 2, 3, or 4). As above in #5, only one Dx# per CPT even if more<br />
than one diagnosis relates to the procedure. The Dx# should indicate only the diagnosis that is the most<br />
significant to the service performed. There may be additional diagnoses listed above that are not tied to<br />
a procedure.<br />
Version: Check version date at lower right corner to ensure using the latest revision. In the event you<br />
believe you do not have the latest version, contact the Medical Records Office to obtain the most up to<br />
date version of the superbill.<br />
INSURANCE AND CODING<br />
Bastyr Center for Natural Health participates in third party reimbursement systems. All providers at<br />
BCNH, including residents, are credentialed for this purpose. Interns are required to be aware of the<br />
insurance status of the patients they work with, and consult with their supervisor regarding the proper<br />
coding of superbills generated for a patient resulting form each contact.<br />
21
DOCUMENTATION GUIDELINES (DG)<br />
Bastyr Center for Natural Health uses documentation guidelines for evaluation and management<br />
services as agreed upon by CMS and the AMA. The clinic’s medical record instruments accurately<br />
model the principles of these guidelines, including the clinic ROS and PE forms. Summaries of DG<br />
appear at the corresponding location in these instruments for the clinician’s convenience. Clinicians are<br />
to ensure that each patient’s medical record <strong>com</strong>plies with these guidelines at each visit. In accordance<br />
with the documentation guidelines for evaluation and management services, proper medical records<br />
keeping include:<br />
o History of Chief Complaint (CC), Secondary Complaint (SC) and Tertiary Complaint<br />
(TC) if applicable.<br />
o History of Present Illness (HPI). Include pertinent elements of location, quality,<br />
severity, duration, timing, context, modifying factors, and associated signs and<br />
symptoms.<br />
o Pertinent elements of Past, Family, and/or Social History (PFSH).<br />
o INTERNATIONAL CLASSIFICATION OF DISEASES (ICD-9)<br />
o Bastyr Center for Natural Health uses ICD-9 codes, or diagnosis codes, according to<br />
the standards agreed upon by the World Health Organization and relies upon<br />
reference texts to describe these standards.<br />
During each patient visit, the clinician is responsible for choosing the correct ICD-9 code for the visit,<br />
with supervisor approval, and recording it in the medical record and on the patient billing form.<br />
Instructions for choosing ICD-9 codes are included in reference texts- hard copy or on-line. Important<br />
principles for choosing ICD-9 codes include:<br />
o Scope of practice.<br />
o Identifying the most specific code available for the patient's condition.<br />
o The first diagnostic code referenced on the billing form must describe the primary or<br />
most important reason for the care provided. This is the Primary Diagnosis.<br />
o The ICD-9 code chosen must be consistent with and substantiated by information<br />
recorded in the subjective, objective, assessment, and plan sections of the patient’s<br />
written record.<br />
o For more detailed information, please refer to Documentation Guidelines for<br />
Evaluation and Management Services in the appendix.<br />
INTERPRETER SERVICES POLICY<br />
Under Title VI of the Civil Rights Act of 1964, the Office for Civil Rights has determined that<br />
language assistance is appropriate when language barriers cause persons with limited English<br />
proficiency (LEP) exclusion from or denied access to clinical services. The key to providing equal<br />
access for the LEP client is to ensure that the service provider and the LEP client can <strong>com</strong>municate<br />
effectively. The LEP client should be given information about, and be able to understand, the services<br />
that can be provided by the provider and must be able to <strong>com</strong>municate his/her situation to the provider.<br />
A health care provider is required to obtain informed consent prior to <strong>com</strong>mencing treatment. The<br />
clinic’s Informed Consent form is in English. It is imperative that an interpreter translate this form in<br />
22
its entirety to the LEP patient, so that the patient is able to give informed consent to treatment (or nontreatment).<br />
Consent given by the patient’s signature is on the Informed Consent form.<br />
In order to meet the guidelines for services provided to LEP patients by Bastyr Center for<br />
Natural Health providers, there are several interpreter options:<br />
While the provider cannot require a patient to use family members or friends as interpreters, a family<br />
member or friend may be an interpreter. It is important that the use of a family member or friend not<br />
<strong>com</strong>promise the patient’s confidentiality or the effectiveness of services. According to Washington<br />
state law on patient confidentiality, a <strong>com</strong>promise of patient’s confidentiality by the use of a family<br />
member or a friend as an interpreter occurs if discussing highly sensitive areas, such as HIV/AIDS,<br />
sexually transmitted diseases, drug and alcohol treatment and mental health issues. Given these<br />
guidelines, the supervising faculty provider must assess <strong>com</strong>promising the confidentiality or<br />
effectiveness of services by a patient using a family member or friend as an interpreter. Pursue other<br />
options for interpreters if confidentiality or effectiveness of services is deemed <strong>com</strong>promised.<br />
A student proficient in the patient’s language and in the English language and who is familiar with<br />
medical terminology is a <strong>com</strong>petent interpreter. Thus, student clinicians may act as interpreters for<br />
LEP patients with the permission of the patient and the approval of the supervising faculty member.<br />
The AT&T Language Line is available to provide interpretation and translation for patients. This<br />
service is pre-arranged by the front desk staff in coordination with the patient. Any costs incurred in<br />
the interpretation are the responsibility of the patient.<br />
LEP patients may use certified interpreters. The patient is responsible for making arrangements for<br />
these interpreters and for paying these interpreters. The front desk will provide contact information for<br />
interpreter services to interested patients. Under the American Disabilities Act (ADA), all clinical<br />
service providers are required to provide sign language interpreters for all deaf persons. The cost of<br />
these interpreters is the responsibility of the clinic and in some cases shared with the patient’s health<br />
insurer.<br />
PATIENT SCHEDULING AND REFERRALS<br />
SCHEDULING<br />
Student clinicians are encouraged to bring in their own patients through <strong>com</strong>munity education, public<br />
talks, participating in wellness clinics, health fairs, and talking to friends. Students may also review<br />
past clinic schedules and call patients, with permission from their supervisor.<br />
When a patient needs to be referred to another student clinician, because the attending student clinician<br />
is moving to another shift, an external clinic, or is graduating, the attending student clinician must<br />
facilitate a smooth transition to a clinician on the same shift or to another shift where the attending<br />
student clinician will be on duty. This decision is made with the agreement of the supervisor on the<br />
original shift, while considering patient scheduling needs, insurance coverage, and specialty care that<br />
may be indicated. All patients schedule through Patient Services Representatives. Student clinicians do<br />
not make their own scheduling <strong>com</strong>mitments.<br />
The front desk has a system of scheduling FOC’s that is fair for everyone. Student clinicians may not<br />
make any requests to restrict FOC assignment in their rooms.<br />
If arranging an appointment for a patient, students need to have the patient call to schedule an<br />
appointment. Students must never schedule appointments. It is fine to arrange tentatively with a patient<br />
regarding a time to <strong>com</strong>e in, but the patient must actually contact the front desk to schedule the<br />
appointment. Students must have patients scheduled during regular clinic shift time.<br />
23
REFERRALS<br />
Patient Referral To BCNH<br />
Clinicians should show appreciation to physicians who refer patients to BCNH with typed thank you<br />
letters after the FOC. When the referred patient has <strong>com</strong>pleted several visits (3) or after pertinent<br />
diagnostic or therapeutic out<strong>com</strong>es are achieved, the clinician then should send another letter to the<br />
referring physician, summarizing the patient’s visit and/or treatments to date. All correspondence must<br />
be approved and signed by the supervisor.<br />
Patient Referral Outside BCNH<br />
To refer a patient to a provider outside of BCNH, a typewritten letter must be <strong>com</strong>pleted by the<br />
primary or secondary student clinician. This letter should follow the standards of a professional<br />
referral letter including the patient’s identifying information, the presenting <strong>com</strong>plaint and other<br />
relevant subjective information, any objective findings, the assessment or rule-outs (differential<br />
diagnosis, depending on the scope of the supervising clinical faculty member), the reason for the<br />
referral, and what treatments, tests or diagnostic procedures are to be performed (again within the<br />
scope of the referring supervisor). The letter should indicate whether or not the recipient provider<br />
should institute treatment as he or she sees appropriate, or whether he or she should consult with the<br />
referring supervisor first. This letter must be signed by the referring provider. It must be photocopied,<br />
with the copy placed in the chart. The original is sent with the patient to be hand delivered or is mailed.<br />
Templates and sample letters are in the appendix of this module or are available from your supervisor.<br />
Intra-clinic Referrals<br />
Student clinicians are encouraged to consider referrals to other departments within the clinic. All such<br />
referrals require an intra-clinic referral letter (see templates and examples in the appendix of this<br />
handbook), <strong>com</strong>pleted and signed by the supervisor. The clinicians / supervisor teams are encouraged<br />
to write treatment summary notes at the conclusion of their evaluation or treatment to the referring<br />
supervisor and clinicians.<br />
24
III. SAFETY, ACCIDENTS, AND EMERGENCIES<br />
SAFETY<br />
Everyone in the clinic is required to follow the guidelines for universal precautions against infectious<br />
diseases, safety standards, and sterile technique standards. Please review these guidelines.<br />
HAND WASHING AND DISINFECTION<br />
All students and supervisors are required to wash their hands with soap and warm water for 20 seconds<br />
then rinsing thoroughly and drying the hands before and after every patient visit, before and after<br />
performing PE, and any clean or sterile procedure. Disinfection of surfaces (exam tables, equipment,<br />
sink and countertops, lamps, etc.) must be performed between each patient and at the end of shift.<br />
Refer to infection control manual located in the lab for details. Chemical hand sanitizing stations are<br />
located throughout the clinic for use when water is not available.<br />
BLOOD BORNE PREVENTION PROCEDURE<br />
o Wipe all working surfaces down with germicide before and after working with (or<br />
possible exposure to) blood, body fluids or tissues (urine, vaginal fluids, semen,<br />
stool, etc).<br />
o Wear a ¾ length buttoned lab coat when in the acupuncture clinic, or handling or<br />
testing blood or body fluids (even a urine dipstick or vaginal wet prep).<br />
o Dispose of ALL SHARPS (lancet, vacutainer needles, syringes, etc.) in a puncture<br />
resistant SHARPS container.<br />
o Make sure you have EVERYTHING you need (bandaids, gauze, alcohol, Sharps<br />
container, tourniquet, needle, holder, acupuncture needles etc.) in front of you<br />
before starting venipuncture or other invasive procedure.<br />
o NEVER be more than an arm’s length away from a SHARPS container when using<br />
any kind of sharp (needle, lancet, acupuncture needle etc.).<br />
o NEVER walk or turn with an acupuncture needle, syringe or other sharp in your hand.<br />
o NEVER (under any circumstance), recap the needle on a syringe or reinsert an<br />
acupuncture needle into an insertion tube after using it. Even one handed recap is<br />
strictly forbidden.<br />
o NEVER unscrew needle from hub of syringe or vacutainer holder. If it is stuck,<br />
throw out entire apparatus. (average cost is $1.00)<br />
o All non-sharp biohazard items (items exposed to blood or body fluids like urine<br />
dipsticks or bloody gauze) are thrown away in BIOHAZARD (red) BAG, not sharps<br />
containers.<br />
o NEVER put or stuff anything into already full sharps container.<br />
o When Biohazard bag or Sharps container is ¾ full, close it, tape it shut and dispose<br />
of appropriately.<br />
o When in doubt about any of these procedures, ask your supervisor.<br />
25
NEEDLES<br />
NEEDLE STICK OR EXPOSURE INCIDENT<br />
If an incident occurs:<br />
Have someone notify your supervisor who will arrange for another clinician to take over patient care.<br />
Wash the injured area with soap and warm running water for at least two minutes. Squeezing the<br />
wound does not provide any protection.<br />
During clinic hours contact the resident physician on call at 206-834-4<strong>10</strong>0. If after clinic hours,<br />
contact the physician on call at 206-200-7067. If no answer, call the BBP officer at 206-422-8763.<br />
You must talk with a physician within a half hour of the incident.<br />
Provide details and information regarding any other person involved to your supervisor while<br />
<strong>com</strong>pleting the incident report. The BBP officer will contact the source person regarding provision of<br />
serum for testing at no cost to them.<br />
The doctor on call or the BBP officer will order blood tests for HIV status, Hepatitis B and Hepatitis C<br />
to be done within 48 hours. Repeat testing will be done at 6 weeks, 3 months and potentially at 6<br />
months, all at no cost to you.<br />
Decisions as to whether you need referral to an emergency room for prophylactic treatment against<br />
HIV need to be made within 30 minutes. Exposure to Hepatitis B or C needs to be addressed within<br />
one week of exposure.<br />
All information and reports will be kept in a locked file in the office of the BBP Officer, separate from<br />
your medical file. Copies will be provided to you upon request. Copies of the source person’s tests<br />
will not be provided.<br />
External sites may have their own policy, which should be observed. The incident report and followup<br />
testing should occur through BCNH.<br />
For more information, contact the BBP or Safety Officer.<br />
CLEAN NEEDLE TECHNIQUE AND BIOHAZARD WASTE HANDLING<br />
Students are responsible for knowing the OSHA/WISHA guidelines for blood borne pathogens and are<br />
required to view a training video and sign a document acknowledging that they understand these<br />
guidelines. Please follow the clinic policies for handling biohazard materials by placing disposables in<br />
the biohazard bags located in each exam room. Immediately take reusable instruments to the<br />
appropriate collection site for cleaning and sterilization. Biohazard materials include all supplies and<br />
instruments exposed to patient body fluids, such as blood, urine, vaginal secretions, saliva, etc. See the<br />
safety manual in the laboratory or ask the current infection control representative for details.<br />
ACUPUNCTURE NEEDLE POLICY<br />
Acupuncture needle counts occur prior to any treatment, and the number initialed by the intern before<br />
insertion. Interns must record any needles added or removed during the treatment. After all needles are<br />
removed, interns must make a final count and, along with the supervisor, initial it. This information<br />
must be recorded on the chart notes for every visit.<br />
Any lost needle requires the attention of the supervisor. When a needle is lost, the garbage must be<br />
flagged and deposited in the blood borne pathogens collections “box.” The laundry from the room<br />
26
must also be flagged. A special notice alerting the janitorial crew to the lost needle in the room must be<br />
posted on the door. On rare occurrences, it is possible a patient will take a needle home that dropped<br />
into a pants cuff or elsewhere in clothing. The supervisor makes a decision about whether to call the<br />
patient and alert him or her to this possibility. The supervisor records “Lost Needle” incidents and<br />
notifies the Associate Dean for AOM Clinical Education immediately. The Associate Dean will record<br />
the incident and send a copy to the clinic registration staff for the student’s record. Any pattern of<br />
occurrences of lost needles will result in clinical sanctions. If a needle is found to be related to a<br />
specific room or shift, clinical sanctions for the clinicians in that room can result.<br />
All Practitioner Care acupuncturists working at Bastyr Center for Natural Health will be alerted to this<br />
policy and the clinic’s concern. The clinic director is notified if needles are found, in order to initiate<br />
proper feedback.<br />
ACCIDENT / ILLNESS<br />
REPORTING AN OCCUPATIONAL ACCIDENT/ILLNESS<br />
This procedure is for any occupational injury or illness occurring to a student clinician, staff, or faculty<br />
member on the clinic premises or caused by the working environment.<br />
IN CASE OF STUDENT ILLNESS<br />
Notify the supervisor.<br />
The student shall be seen by a provider of their choice as needed (at the clinic or elsewhere).<br />
IN CASE OF ACCIDENT<br />
Notify the supervisor.<br />
In the event of an accident the intern or observer immediately notifies their clinic supervisor. In the<br />
event their clinic supervisor is not available, the intern should notify the nearest clinic supervisor, the<br />
associate dean, or clinic lead for the program. The supervisor immediately determines the nature of the<br />
emergency and if necessary calls 9 - 911. If the supervisor is able to safely do so, they should begin<br />
provide emergency care for the patient. The student clinicians should follow all instructions from the<br />
clinic supervisor during the emergency.<br />
The front desk is responsible for the following:<br />
o Furnishing an Occupational Illness/Injury Report form to the provider/supervisor.<br />
o Arranging for an exam room.<br />
o Contacting appropriate emergency responders per provider’s instructions.<br />
The supervisor and provider will begin appropriate paperwork with the employee as soon as possible<br />
following the accident. The supervisor will forward the paperwork to the clinic safety coordinator<br />
within 24 hours of the incident. The Medical Director, Director of Facilities and Safety or a designated<br />
administrator will continue the evaluation process.<br />
The emergency transport of a patient will be a 911 vehicle. Students, faculty or staff may not drive a<br />
patient to the emergency room in a personal vehicle.<br />
27
IN CASE OF A SENTINEL EVENT<br />
A sentinel event is an unexpected occurrence involving death, physical or psychological injury, or the<br />
risk thereof. “Sentinel” events signal the need for immediate investigation and response.<br />
The front desk, once notified, is responsible for the following:<br />
o Paging the clinic lead for that program.<br />
o Arranging for exam room.<br />
o Furnishing the Occupational Illness/Injury Report form to the provider/supervisor.<br />
o Contacting an appropriate emergency responder per instructions from provider.<br />
The following administrators must be notified immediately:<br />
Paperwork requirements:<br />
o Clinic Director/Medical Director.<br />
o Practice management manager.<br />
o Clinic facilities manager.<br />
o Program lead / Associate Dean(s).<br />
o The supervisor or provider must <strong>com</strong>plete the Occupational Illness/Injury Report<br />
form, including: Date, time, and place of incident.<br />
o Complete, detailed description of incident, including any objects involved.<br />
o Nature of incident.<br />
o Basic cause and any contributing cause(s).<br />
The Medical Director, Director of Facilities and Safety or their designee <strong>com</strong>pletes the investigation of<br />
events, conducts interviews with all persons directly involved, and presents an evaluation to the<br />
clinic’s Safety Committee, which is responsible for:<br />
o Evaluation of Review.<br />
o Developing action plans and establishing timelines for <strong>com</strong>pletion, including but not<br />
limited to the documentation of response to the incident, identification of<br />
deficiencies, suggestions for improvement(s) to the response, and writing<br />
re<strong>com</strong>mendation(s).<br />
o Sending the findings to the supervisor/ provider directly involved, the program<br />
coordinator, clinic director, and practice management manager.<br />
The OSHA 2000 Log and Summary form must be <strong>com</strong>pleted for each event. This is the responsibility<br />
of the Director of Facilities and Safety or the director’s designate. A copy of all paperwork is<br />
forwarded to the Bastyr University Health and Safety Office on campus.<br />
Contact the Medical Director and Director of Facilities and Safety immediately in the event of serous<br />
injury/illness or fatality. All fatalities, or if it is expected someone will die of their injury/illness, must<br />
be reported to Labor and Industries within eight hours of the event or first knowledge of the event.<br />
The Medical Director or Director of Facilities and Safety is to ac<strong>com</strong>pany the Regulatory Agency<br />
representative and assist during the investigation. In such an event, leave the area untouched. Photos<br />
of the scene are required to record the environment at the time. Pertinent instructions will be given<br />
when the Medical Director and Director of Facilities and Safety are notified.<br />
28
SUICIDAL/HOMICIDAL PATIENT POLICY AND PROCEDURE<br />
As of January 19, 2007, it is the policy for all health care providers at the Bastyr Center for Natural<br />
Health and providers at the Bastyr University campus and clinic to follow the procedure listed below<br />
when any patient presents with suicidal ideations, or might otherwise be a hazard to self or others. If a<br />
clinic supervisor determines that further evaluation must be made, evaluation may only be made by a<br />
mental health professional. A MHP is defined as a psychologist, therapist, or mental health<br />
professional designated by the clinic administration as qualified to make this determination. Please see<br />
the flow charts below.<br />
Life contracts are not effective and are not used.<br />
29
SUICIDAL/HOMICIDAL PATIENT PROCEDURE<br />
Who<br />
Does What<br />
Patient 1. Expresses suicidal ideation<br />
Student/Intern 2. Reports suicidal/homicidal ideation to supervisor<br />
Supervisor 3. Interviews patient and assesses the seriousness of the situation, determining if<br />
the patient is a hazard to self or others.<br />
4. If the patient is deemed to not be a hazard to self or others by the supervisor, go<br />
to step 5. If the supervisor believes the patient may be a hazard to self or others,<br />
go to step <strong>10</strong>.<br />
5. Determines if the patient is under care of a health care professional. If yes go to<br />
step 6. If no, go to step 9.<br />
6. Refer patient to current healthcare professional, noting referral in faculty<br />
member’s <strong>com</strong>ment on progress note.<br />
7. Approve treatment.<br />
Student/Intern 8. Complete approved treatment, charting referral to current health care<br />
professional in plan.<br />
Supervisor 9. If patient is not under care of a mental health professional, refer patient to<br />
mental health professional for follow up. If the patient does not have mental<br />
health resources, include referral to the King County Crisis Line 206.461.3222.<br />
Supervisor<br />
<strong>10</strong>. If the supervisor determines that the patient is a hazard to self or others,<br />
determine if there is a mental health provider on site at the clinic. If yes go to<br />
step 11. If no go to step 13.<br />
11. Request immediate assistance from on site mental health provider.<br />
On Site<br />
Mental Health<br />
Professional<br />
Supervisor<br />
12. Evaluates patient and determines best course of action. This may include but is<br />
not limited to calling for immediate assistance from emergency providers,<br />
referral for crisis intervention or referral back to supervisor to continue<br />
treatment.<br />
13. Calls 911 to report a patient that may be at risk of doing harm to self or others to<br />
get assistance.<br />
30
FLOW CHART FOR REVISED SUICIDAL/HOMICIDAL PATIENT PROCEDURE<br />
Patient expresses<br />
suicidal/homicidal<br />
ideation<br />
Student/Intern<br />
reports<br />
suicidal/homicidal<br />
ideation to<br />
supervisor.<br />
Patient answers "yes" to any of the<br />
following Questions:<br />
1. Do you have a plan for how you would<br />
harm yourself/others?<br />
2. Do you know when you would harm<br />
yourself/others?<br />
3. Do you have the means to carry out<br />
this plan?<br />
4. Do you have a history of a suicide<br />
attempt/ harming others?<br />
Supervisor<br />
interviews patient<br />
and assesses<br />
the seriouslness<br />
of the situation.<br />
Continue<br />
treatment.<br />
NO<br />
Is patient hazard<br />
to self or others?<br />
Yes<br />
Unsure<br />
Patient must be<br />
seen immediately by<br />
mental health<br />
professional.<br />
Is patient under<br />
care of mental health<br />
professional?<br />
Mental health<br />
professional on<br />
site?<br />
Yes Yes<br />
No No<br />
Request patient to<br />
contact mental<br />
health<br />
professional.<br />
Refer to mental<br />
health<br />
professional, or<br />
the King County<br />
Crisis Clinic at<br />
(206) 461-3222.<br />
Request immediate<br />
assistance from on<br />
site mental health<br />
professional.<br />
Call 911.<br />
Someone must<br />
remain with<br />
patient.<br />
31
EMERGENCY PROCEDURE PROTOCOL FLOW SHEET<br />
Is 911<br />
required?<br />
(if in any doubt,<br />
call them!)<br />
YES<br />
Dial 9 – 911. Don’t hang<br />
up until operator instructs<br />
you to do so.<br />
If this a Blood-Borne Pathogen Incident<br />
(exposure to someone else’s bodily fluid)<br />
follow this procedure and the Blood-Borne<br />
Pathogen Flow Chart located in each exam room.<br />
Is this a potentially<br />
dangerous situation<br />
involving a violent or<br />
threatening individual?<br />
NO<br />
Call the clinic Emergency Phone<br />
at 206-200-7067. Follow their<br />
instructions and notify them<br />
whether 911 has been called.<br />
YES<br />
Use paging system or ask<br />
Appointment Desk to do so:<br />
“Paging Dr. Armstrong. Please<br />
call PHONE EXTENSION or<br />
report to LOCATION.”<br />
If no response within 30 seconds,<br />
page the on-call resident.<br />
If no response within 30 seconds,<br />
send someone to physically locate<br />
a faculty member, resident,<br />
or other ND.<br />
If no response within 1 minute, send<br />
someone to physically locate<br />
“Dr. Armstrong”<br />
(a resident, ND, or Facilities/Security staff)<br />
Fill out an INCIDENT REPORT form<br />
immediately after the incident, while it’s<br />
fresh in your mind. Forms are in each<br />
Review/Preview room or at the Appt. Desk.<br />
Submit the form to the Clinic Safety<br />
Coordinator within 24 hours.<br />
`<br />
32
REPORTING A PATIENT/VISITOR ACCIDENT OR ILLNESS<br />
This protocol applies to any injury or illness occurring on the clinic’s premises or as a result of clinical<br />
services or a product purchased from the Bastyr Dispensary or the Chinese Herbal Dispensary.<br />
IN CASE OF ILLNESS/ACCIDENT ON THE PREMISES OF THE CLINIC<br />
The front desk should be notified and is responsible for the following:<br />
o Arranging for an exam room.<br />
o Furnishing an Incident Report form to the provider of record. The provider of record<br />
<strong>com</strong>pletes the top portion of the form and forwards the paperwork to the clinic<br />
safety coordinator within 24 hours of the incident.<br />
o The Director of Facilities and Safety is responsible for contacting the university’s<br />
liability insurance <strong>com</strong>pany.<br />
o The Director of Facilities and Safety shall copy all paperwork to the clinic director<br />
and practice management manager within 24 hours.<br />
o The emergency transport of the patient will be a 911 vehicle. An emergency vehicle<br />
should be called by the provider making the initial emergency assessment or her or<br />
his designee<br />
IN CASE OF INJURY FROM OR ADVERSE REACTION TO ANY PRODUCT PURCHASED FROM THE CLINIC<br />
Dispensary staff should notify the supervisor or clinic lead to discuss the event with the patient.<br />
The supervisor is responsible for the following:<br />
o Determining the extent of the problem; refer to the emergency manual located in the<br />
Clinic laboratory.<br />
o Referring patients to a provider, if necessary, to discuss the specific nature of the<br />
problem.<br />
o Either the dispensary staff and/or the supervisor is responsible for the following:<br />
o Completing the top portion of the Incident Report form.<br />
o Forwarding paperwork to the Medical Director within 24 hours of the incident.<br />
The following administrators must be notified immediately:<br />
o Medical Director.<br />
Paperwork requirements:<br />
o Practice management manager.<br />
o Clinic facilities manager.<br />
o Program Lead / Associate Dean.<br />
o The supervisor or provider must <strong>com</strong>plete the top portion of the Incident Report form,<br />
including:<br />
o The date, time, and place of the incident.<br />
o A <strong>com</strong>plete detailed description of incident, including any object(s) or machinery<br />
involved.<br />
33
o The nature of the incident.<br />
o The basic cause and any contributing cause(s).<br />
The Medical Director, Director of Facilities and Safety or designees is responsible for the following:<br />
o Completing the investigation of events.<br />
o Conducting interviews with all persons directly involved.<br />
o Presenting an evaluation to the clinic or campus Safety Committees, which is<br />
responsible for reviewing the evaluation, developing action plans and establishing<br />
time lines for <strong>com</strong>pletion, documenting the response to the incident, identifying<br />
deficiencies, suggesting improvement(s) to the response and writing<br />
re<strong>com</strong>mendations.<br />
o Sending its findings to:<br />
o The supervisor/provider who was directly involved.<br />
o The clinic program supervisor.<br />
o The Medical Director.<br />
o The Director of Facilities and Safety<br />
o The Director of Facilities and Safety will follow up, as re<strong>com</strong>mended by the<br />
<strong>com</strong>mittee.<br />
o The Medical Director shall contact the patient as deemed necessary to ensure patient<br />
satisfaction.<br />
o Copies of all paperwork will be forwarded to the Bastyr University Health and Safety<br />
Office on campus.<br />
EMERGENCIES: WEATHER, EARTHQUAKE, DISEASE<br />
INCLEMENT WEATHER POLICY AND PROCEDURE<br />
In the event of severe inclement weather conditions, Bastyr University President and the Medical<br />
Director will together determine whether it is indicated for clinic to close. Closure will occur only in<br />
the event of extremely severe weather conditions. There will be every effort to keep the Clinic open to<br />
meet the needs of the clinic’s patients as long as it is safe to do so.<br />
A decision to close will put the following closure procedures into effect:<br />
For all clinic closures, the status of both the clinic and campus will be posted on the<br />
www.schoolreport.org website, which is the source of TV and radio reports.<br />
Closure information for both the campus and clinic is on Bastyr University’s weather message line at<br />
(206) 274-1213 by 6 a.m.<br />
The clinic’s public voicemail system (206) 834-4<strong>10</strong>0 will be up-to-date with closure information by<br />
7:30 a.m. Clinic staff members will <strong>com</strong>e in to call and inform scheduled patients of clinic closure and<br />
will post signs on clinic doors.<br />
Closure decisions made during clinic business hours will follow the following:<br />
o Signs will be posted immediately on clinic doors<br />
34
o The clinic’s master voicemail message will be modified immediately<br />
o Scheduled patients will be called and informed of closure<br />
o People at the clinic will be notified by others in the building<br />
o Campus will post signs for students near the cafeteria and at the DART bus stop<br />
Decisions to close on a Saturday will follow the same procedures.<br />
In the event of a power and/or phone outage, <strong>com</strong>munications with employees, patients, and students<br />
will be limited. Clinic staff will post signs and do their utmost to have someone available to meet<br />
anyone who <strong>com</strong>es in.<br />
In general, off-site/external shifts will also close when the clinic closes due to inclement weather. Any<br />
shift hours missed due to inclement weather will need to be made-up. Additionally, a site supervisor<br />
may close a site at their discretion. Off-site clinics will also close when the host institution is closed.<br />
Contact the ND External Site Coordinator at (206) 834-4188 for the latest information on ND external<br />
shifts. Contact the Associate Dean in the School of Acupuncture and Oriental Medicine for the status<br />
of AOM off-site clinics.<br />
EARTHQUAKE RESPONSE PLAN<br />
When an earthquake occurs, drop to the floor and take cover under a sturdy desk or table, or stand<br />
under an interior or exterior door frame. Hold on to the desk or table, as it might be moving. If a desk<br />
or table is not available, seek cover against an interior wall and protect your head and neck with your<br />
arms. Avoid danger spots such as windows, mirrors, hanging objects, or tall furniture that could topple<br />
over.<br />
If treating a patient, stop any procedure you are performing immediately, Remove acupuncture needles<br />
or other equipment from the patient. Help the patient to the floor, and get the patient to a safe area<br />
under a table or in an internal doorway. Do not take cover without attempting to assist patients who<br />
cannot help themselves. Once the shaking has stopped, depart the building immediately, via the safest,<br />
closest emergency exit.<br />
If conditions are not hazardous, floor safety wardens will sweep the clinic. Students, staff, and patients<br />
will meet in the safe zone to await instructions from the Medical Director, Facilities Manager or their<br />
designees. On campus, instructions will be provided by the Director of Facilities and Safety or the<br />
Director’s designee.<br />
COMMUNICABLE DISEASE OUTBREAK<br />
These guidelines are for dispensing information to Bastyr University and Bastyr Center for Natural<br />
Health employees and students in the event of a <strong>com</strong>municable disease outbreak:<br />
o The testing facility should notify the clinic laboratory of a positive test result.<br />
o The Bastyr clinical laboratory notifies the provider of the record and the Medical<br />
Director.<br />
o The Medical Director should notify:<br />
o The clinic and campus personnel via e-mail/voice mail.<br />
o Clinic students via written notices on the bulletin board in the student lounge and via<br />
e-mail.<br />
o The university Health and Safety Office via e-mail.<br />
35
o The student services office.<br />
o The university health and safety office of the student services office notifies students<br />
via written messages on various designated bulletin boards, i.e. the white board and<br />
others.<br />
IMMUNIZATION POLICY<br />
These policies are to protect the health and safety of employees and students who might be exposed to<br />
certain bio-hazardous agents in the campus and clinic working environments.<br />
TUBERCULOSIS SCREENING<br />
Bastyr University and the Bastyr Center for Natural Health mandate annual tuberculosis (TB) tests of<br />
all faculty, staff, and students working in Bastyr University clinics or affiliated clinical areas. TB<br />
screening information/forms for students are part of the Clinic Entry course or clinic orientation.<br />
Faculty and staff are required to provide documentation to the Clinic Safety Officer. The University<br />
Safety Officer or Clinic Safety Coordinator can answer TB screening questions. Students pay $<strong>10</strong><br />
towards the cost of their PPD TB test at the clinic. TB screening forms are available at the medical<br />
records desk. The Quanti-FERON test is available at a higher cost.<br />
To review the <strong>com</strong>plete TB screening policy, see TB Procedure.doc in the Clinic Information folder at<br />
\\middleearth.prv\bastyr\campus\data\public\clinic. (see page 3 of this handbook for access details)<br />
Once the required testing is <strong>com</strong>plete, it is the responsibility of students, staff and faculty to submit a<br />
copy of their documentation to the safety office on campus, or to the TB Results drop box near the<br />
clinic Medical Records window.<br />
HEPATITIS B IMMUNIZATIONS<br />
All students, faculty, and staff who are Category I (those who have daily exposure to blood or body<br />
fluids) and Category II (those who have occasional exposure to blood or body fluids) are required to<br />
either take the Hepatitis B immunization series, provide documentation that they have had such<br />
immunizations, or sign a waiver signifying that they refuse the HBV immunization, along with a<br />
release of liability form.<br />
Bastyr University agrees to pay for 50% of the cost of immunization for students (up to the amount<br />
charged by the King county Health Department). Contact the Facilities Office on campus regarding<br />
reimbursement.<br />
Commencement of the immunization series (or submission of a waiver) and TB screening shall occur<br />
before the first day of work for all faculty and staff, before all students begin their clinical training, and<br />
with the start of fall quarter of each year for entering ND students. Documentation of immunization<br />
must be <strong>com</strong>pleted by entering AOM students by the deadline specified during the AOM Clinic Entry<br />
class. For AOM students not taking Clinic Entry during their first term at Bastyr University, all<br />
immunization and TB screening records must be <strong>com</strong>pleted before beginning a clinic shift. Hepatitis<br />
immunization questions can be directed to the blood borne pathogen safety officer. Requests for forms<br />
can be addressed to Director of Facilities and Safety, or the Clinic lead/Associate Dean. Anyone who<br />
elects to waive the immunization series has the option to change that election at any time and <strong>com</strong>plete<br />
the immunization series.<br />
For external clinic shifts or preceptor sites that require any other kind of immunization or proof of<br />
immunity, the student is required to pay for all costs involved in testing for antibody levels, if they<br />
choose to check for immunity, as well as costs for immunizations.<br />
36
IV. CONFIDENTIALITY, MEDICAL RECORDS,<br />
AND TREATMENT OF MINORS<br />
CONFIDENTIALITY<br />
As a healthcare facility, the Bastyr Center for Natural Health is a member of the public trust. To<br />
preserve this trust, Bastyr University is <strong>com</strong>mitted to the highest standards of confidentiality. Breaches<br />
of these policies can permanently jeopardize any individual’s position at Bastyr. Further, Bastyr<br />
University clinics are in <strong>com</strong>pliance with the Health Insurance Portability and Accountability Act of<br />
1996 (HIPAA), a federal law mandating specific requirements with respect to patient privacy.<br />
CONFIDENTIALITY POLICIES<br />
Clinicians handle personal and sensitive medical information in the course of providing care to patients.<br />
It is the responsibility of all faculty members and student clinicians to conduct themselves in a<br />
professional manner and abide by the clinic’s confidentiality policies. Clinicians who are unclear about<br />
a policy or procedure are to utilize the resources available to them to clarify any misunderstanding they<br />
might have. Moreover, clinicians have a responsibility to intervene or report policy violations or<br />
wrongful disclosures when and if it is known to them. Unprofessional practices reflect poorly on<br />
everyone at the clinic, and in their profession. It can also damage the clinic’s relationship with patients,<br />
and put the institution at legal and financial risk, including substantial penalties under federal law<br />
(HIPAA). Direct all questions related to medical records or confidentiality policies to the Medical<br />
Records Office at (206) 834-4151. Bastyr is dedicated to upholding the professional standards of the<br />
medical <strong>com</strong>munity as well as ensuring the safety and well-being of all its patients.<br />
BREACHES OF POLICY<br />
Clinicians who violate clinic confidentiality policies will be subject to disciplinary action. Depending<br />
on the circumstances and severity of the violation, student clinicians can be subject to any or all of the<br />
following: loss of clinic credit, a failure event, or suspension or dismissal from the university.<br />
DE-IDENTIFICATION POLICY<br />
The following de-identification guidelines are to protect patient confidentiality. All notes taken down<br />
by students for self-study and all case summaries submitted for publication in the Bastyr Center for<br />
Natural Health Journal must adhere to these guidelines.<br />
No full-face photographic images or <strong>com</strong>parable images may be used.<br />
Note: Partial pictures showing unique tattoos or piercings may not be appropriate. When in doubt,<br />
check with the Medical Director regarding the use of images in any publication.<br />
Omit the names of any of the following parties:<br />
o Patient<br />
o Patient’s relatives<br />
o Patient’s employer(s)<br />
o Patient’s household members<br />
o Known close acquaintances*<br />
37
*Names of Bastyr clinicians and faculty involved in treating the patient may be included as long as<br />
none of the above relationships is identified. Contributor consent is required.<br />
All geographic subdivisions smaller than a state level are omitted.<br />
o Stating a patient is from Washington State, for example, is acceptable, but including a<br />
patient’s city, county, precinct, zip code, street address, or equivalent geo-code is<br />
not.<br />
Omit all of the following date elements (except year*):<br />
o Birth date<br />
o Admission date<br />
o Discharge date<br />
o Date of death<br />
*A patient’s age and year of birth may be stated as long as the patient is 89 years of age or younger. If<br />
a patient is 90 or more years of age, the patient’s age or birth year may not be used. For example,<br />
stating “a 95-year-old man <strong>com</strong>ing in for treatment of insomnia” would not be permissible and should<br />
instead be reported as “an elderly man <strong>com</strong>ing in for treatment of insomnia.”<br />
Omit all of the following elements:<br />
o Patient phone numbers<br />
o Patient fax numbers<br />
o E-mail address<br />
o Social security numbers<br />
o Medical records numbers<br />
o Patient account numbers<br />
o Biometric identifiers<br />
o Any other uniquely identifying numbers, characteristics or codes<br />
RECORD HANDLING RESTRICTIONS<br />
Access<br />
Patient medical information is available to clinicians on a ‘need-to-know’ basis. Clinicians may request<br />
patient records from the chartroom as needed to prepare for, document, or provide patient care.<br />
Clinicians may access patient records for <strong>com</strong>piling chart summaries for grand rounds and teaching<br />
purposes, provided they currently have or have had a treatment relationship with the patient, and the<br />
record is not designated as ‘restricted.’ Clinicians who wish to access other patient records or perform<br />
chart reviews for other purposes must contact the clinic director to secure pre-approval for such access.<br />
Patients must follow clinic policy to access their own medical information and chart.<br />
Use and Return<br />
Return all charts to the appropriate chart return area or chartroom at the end of each business day. This<br />
is necessary to ensure adequate accounting of all patient records. Patient records used on an AOM shift<br />
must be <strong>com</strong>plete, including supervisor charting and signatures, and returned to the Medical Records<br />
area in AOM or the Medical Records office at the end of each shift.<br />
38
Photocopying<br />
Direct copying of any patient medical information, progress notes, or lab work is prohibited. It is not<br />
acceptable to directly photocopy patient medical information and subsequently redact (blacken) the<br />
patient’s name or other unique identifiers. This does not adequately ensure patient privacy and is a<br />
prohibited practice at the clinic. If a clinician wishes to retain patient medical information for<br />
educational purposes or therapeutic research, the medical information contained in any progress notes,<br />
lab work, or chart documents not described above must be transcribed to a separate sheet of paper or<br />
electronic document and include no uniquely identifying elements. (See clinic de-identification policy<br />
for a <strong>com</strong>plete list of uniquely identifying elements.)<br />
Transporting Records<br />
All uniquely identifiable patient information, including patient charts, loose chart notes, administrative<br />
reports, or other documentation in hardcopy or electronically stored format must remain in the building<br />
at all times. The medical records manager, or Medical Director or their designee must authorize any<br />
activities that require transportation or removal of such clinic records from the clinic. Unauthorized<br />
transportation of patient records or removal of patient information from the clinic is a wrongful<br />
disclosure and is strictly prohibited.<br />
Note: If a student clinician removes a chart or chart notes that contain any patient identifying<br />
information from the premises, disciplinary action will result as follows:<br />
For a first offense, student clinicians will receive a failure in clinic for one entire quarter shift,<br />
including loss of credit for clinic shift hours and patient contacts.<br />
For a second offense, clinician will receive a failure event as described above and be subject to<br />
immediate suspension from the institution.<br />
Secure Vs. Non-Secure Areas<br />
Uniquely identifiable patient information, as described above, must not be left in non-secure zones of<br />
the clinic. Non-secure, public zones include all hallways not designated as ‘staff only’ areas, waiting<br />
rooms, classrooms, conference rooms, treatment rooms, lounges and break rooms, libraries, restrooms,<br />
main dispensary shopping areas, stairwells, elevators, or any other area not expressly designated as a<br />
secure zone. Designated secure zones include assigned preview-review areas, the clinic laboratory, the<br />
chartroom, and all faculty and administrative offices of authorized personnel. Please note that while<br />
preview-review discussions occasionally occur in classrooms and conference rooms, these areas are<br />
not designated preview-review areas or secure zones. Patient records must never be left unattended in<br />
unsecured classrooms or conference rooms. All identifiable patient information must be removed from<br />
preview/review rooms at the end of each daily shift.<br />
Disposal<br />
All notes and documents that are no longer needed and containing unique patient identifiers, as<br />
outlined in the de-identification policy, are shredded after use or placed in a secure, blue, shred only<br />
bin. Placing such documents in trash or recycle bins is a wrongful disclosure of patient information and<br />
is prohibited.<br />
Wrongful Disclosures<br />
All clinicians are required to report any known wrongful disclosures to the medical records manager.<br />
Wrongful disclosures include any uniquely identifiable patient information that has been lost, stolen,<br />
wrongfully made public, or improperly handled.<br />
39
Patient Access<br />
Clinicians may not give patients unsupervised access to their charts at any time. Leaving charts<br />
unattended in the treatment room with patients jeopardizes the integrity of the record, because patients<br />
may alter or remove parts of the clinic’s official treatment documentation. Similarly, clinicians may<br />
not bring one patient’s chart into the treatment room while treating another patient. If patients wish to<br />
view their records, please have them contact the medical records manager or medical records<br />
coordinator to schedule an appointment to view them.<br />
COMMUNICATION RESTRICTIONS<br />
Preview-Review Sessions<br />
Patient information is discussed only in preview-review sessions in a manner that omits uniquely<br />
identifying information. Discussions should be limited to the patient’s age, gender, and medically<br />
relevant information necessary for learning and conducive to the advancement of clinic <strong>com</strong>petency.<br />
Clinicians may refer to patients using the initials of the first and last names for clarification in<br />
discussion. It is not appropriate, however, to use a patient’s name, date of birth, or personal account<br />
information in preview-review discussions. Moreover, discussions may not include names of relatives<br />
or known acquaintances, specific occupational information, or any other uniquely identifying acts. (See<br />
clinic de-identification policy for <strong>com</strong>plete list of uniquely identifying elements.)<br />
Records designated (i.e. labeled) as ‘restricted’ may not be discussed in preview-review sessions. Restricted<br />
records include records of students, staff, faculty, and their immediate relatives. Such records are only<br />
discussed among the clinicians directly involved in the patient’s care. Similarly, restricted records may<br />
not be used for grand rounds summaries or discussed among clinicians not directly involved in the<br />
restricted patient’s care – even if this discussion does not include uniquely identifying elements.<br />
Faculty may opt to restrict access to an individual’s chart by notifying the medical records manager.<br />
The medical records office will make the necessary changes and grant the chart ‘restricted’ status. A<br />
student clinician may not grant a record restricted status.<br />
Public vs. Private Areas<br />
Patient cases may only be discussed freely in private areas. Treatment rooms, private offices,<br />
designated preview-review areas, or closed classrooms and conference rooms are sufficiently private to<br />
allow free discussion of patient information. It is inappropriate to discuss patient cases in hallways,<br />
waiting rooms, or other public, non-secure areas using any uniquely identifying information.<br />
Clinicians must never discuss medical treatment with a patient in a public area at the clinic, even if the<br />
patient consents to such discussion. Not only could such a discussion result in a misunderstanding<br />
about what was acceptable subject matter, but could also present a poor image to other patients.<br />
Discussion of patient cases outside the clinic must be done in a manner that excludes all uniquely<br />
identifying elements. Students are to refrain from discussing other student cases outside the clinic<br />
entirely – even in a de-identified fashion.<br />
Minimum Necessary Standard<br />
Clinicians are required to abide by a ‘minimum necessary standard’ when discussing patient<br />
information with other clinicians not involved in the patient’s health care or when discussing such<br />
information with staff members of various departments. Clinicians may only discuss patient<br />
information to the extent necessary to ac<strong>com</strong>plish the task at hand. It is inappropriate to discuss patient<br />
medical information with staff or faculty not directly involved in a patient’s health care, if disclosing<br />
such information is not necessary in order for that staff or faculty member to perform his or her<br />
40
essential work duties. Clinicians shall use their professional judgment in determining what information<br />
is necessary and appropriate to <strong>com</strong>municate.<br />
Releasing Information<br />
Clinicians are prohibited from releasing patient information, with the exception of releasing<br />
information to a patient, the patient’s legal representative, or another health care provider involved in<br />
the patient’s care, when the release is either verbal (in person or over the phone) or in the form of a<br />
summary/referral letter (i.e., does not involve copying chart notes). The medical records office must<br />
process all other releases including faxes. All other inquiries for patient information are made by<br />
contacting the medical records helpline at (206) 834-4151. If a clinician wishes to enclose chart notes<br />
along with a summary/referral letter, the medical records office must provide the enclosure and mail<br />
the letter on the clinician’s behalf. All questions concerning representative authority are directed to the<br />
medical records office. (See Medical Records section below for more information on records releases.)<br />
Faxing of patient information<br />
Clinicians who need summary and referral letters faxed to other health care providers and a copy of the<br />
correspondence placed in the chart, should request this of medical records Students must first call and<br />
verify all fax numbers with the receiving party prior to faxing. Clinicians are not to fax copies of chart<br />
notes, such as labs, progress notes, or other uniquely identifiable information to any third party,<br />
including other health care providers. All such releases must go through the medical records office. All<br />
in<strong>com</strong>ing faxes containing patient medical information must go to the medical records office at (206)<br />
834-4131. In<strong>com</strong>ing faxes containing any patient information should NOT be directed to the any other<br />
clinic fax number.<br />
E-mailing patient information<br />
Clinicians are prohibited from e-mailing patient information unless the <strong>com</strong>munication is with an<br />
authorized clinician or staff member, and the e-mail correspondence is neither directed to, nor<br />
originates from, an external server. For example, a clinician may use an assigned faculty or student e-<br />
mail account (@bastyr.edu) to e-mail patient information to another authorized staff member or<br />
clinician within the organization (@bastyr.edu). E-mailing patient information from or to an e-mail<br />
account at external servers, however, such as Hotmail©, Yahoo©, America Online©, etc., is prohibited<br />
and constitutes a wrongful disclosure.<br />
In addition, when a clinician or authorized staff use e-mail for patient follow up (e.g. Supervisor e-<br />
mails student that patient’s labs are in, please call patient with these directions) they must ensure that<br />
all e-mails de-identify patient information.<br />
For example: if Sue Smith was seen in the first hour in room three of Dr. Robert’s Thursday afternoon<br />
shift, the e-mail could state: Labs are in for JS, first hour patient on your Thursday 2.0 shift from<br />
March 5 th . Please call her and ask her to make a follow up appointment to review the labs and set up a<br />
treatment plan. Please document the phone call and forward the chart to me to sign.<br />
Please Note: this internal email <strong>com</strong>munication is not part of the medical record and should not go into<br />
the chart.<br />
Student clinicians may not correspond with patients via e-mail and must direct any such<br />
<strong>com</strong>munications to their faculty supervisor upon receipt.<br />
41
MEDICAL RECORDS<br />
The medical records department includes file clerks and office staff who are responsible for chartroom<br />
workflow and health information management at the clinic. This includes all records at Bastyr Center<br />
for Natural Health. Key contact information is below:<br />
Medical Records & Billing Manager 206-834-4164<br />
(questions concerning clinic policies, departmental management, and staffing)<br />
HIPPA Compliance Officer 206-850-2955<br />
(questions concerning legal matters, medical record policies, and safety)<br />
Medical Records Helpline 206-834-4151<br />
(questions regarding general medical records services)<br />
Medical Records Fax Number 206-834-4131<br />
Medical Records Fax Number 206-834-4131<br />
(all non-billing* related faxes that contain patient information)<br />
Billing Office Fax Number 206-834-4136<br />
(*billing faxes, including referrals, credentialing, and corrected claims issues)<br />
The medical records department is dedicated to accounting for all medical records. If you suspect that<br />
a patient’s medical record might be missing, report it to the medical records office immediately.<br />
SERVICES AND SCOPE OF THE MEDICAL RECORDS DEPARTMENT<br />
The medical records office handles all requests for medical records releases from the clinic to third<br />
parties. The medical records department is also responsible for:<br />
o General chart maintenance and standardization.<br />
o Storage, transportation, and ultimate destruction of the physical patient record.<br />
o Answering questions about proper charting procedures, confidentiality issues, or the<br />
release of medical information from the clinic.<br />
Clinicians are not to release or loan medical records to any third parties, including the patient. Direct<br />
patient requests to the medical records office for processing. (See section on release of records and the<br />
section on confidentiality policies for more details.)<br />
The medical records office serves all faculty members, student clinicians, and patients. Clinicians who<br />
have special requests or circumstances are wel<strong>com</strong>e to call (extension 4151) or visit the department.<br />
The medical records office will:<br />
o Bring records to clinicians that are currently seeing a patient.<br />
o Contact clinicians with follow-up information as requested.<br />
o Assist clinicians in determining current addresses and phone numbers for other health<br />
care providers.<br />
o Help clinicians avoid many <strong>com</strong>mon mistakes in directing correspondence to large<br />
facilities.<br />
42
o Mail or fax any correspondence (including referral letters, summary letters, and<br />
physician statements) on behalf of clinicians, and/or make a copy of the<br />
correspondence for the chart upon request.<br />
ACTIVE RECORDS AND CHART STORAGE<br />
Medical records for patients who have visited the clinic within the last 18 months are ‘active’ records<br />
and are stored on site in the chartroom located on the second floor. Older, ‘inactive’ records are stored<br />
at an off-site storage facility. When a patient schedules an appointment, inactive charts are retrieved<br />
from storage and reactivated. However, if a clinician needs a chart from archives for other purposes,<br />
such as an Institutional Review Board (IRB) approved chart review, clinicians must submit their<br />
request for the record to the medical records office using the Record Request slip. See below.<br />
REQUESTING PATIENT RECORDS FROM THE CHARTROOM<br />
Patient charts pulled and prepped for up<strong>com</strong>ing scheduled appointments are placed in the designated<br />
room slots for their corresponding shift 24 hours in advance of the patient’s appointment. There are<br />
occasions that warrant a clinician to request a chart outside of scheduled appointment times. Clinicians<br />
will often need to request charts to <strong>com</strong>plete charting for appointments, make calls to patients, review<br />
outside medical records, or prepare for an up<strong>com</strong>ing appointment.<br />
To request a patient’s record from the second floor chartroom, clinicians must <strong>com</strong>plete a Record<br />
Request slip and submit it to the proper slot in the chartroom. All request slips must include the<br />
patient’s first name, at least the first three letters of the patient’s last name, the date of birth OR the<br />
patient’s ID#, the date of request, and the name of the individual requesting the chart. Illegible or<br />
in<strong>com</strong>plete Record Request slips are not processed. Therefore, these slips must be written legibly and<br />
include all required information.<br />
The Record Request slip shown below is to request charts from the chartroom. Terms of checkout and<br />
instructions for using the slip are on the back of the form.<br />
Record Request<br />
Patient Information:<br />
Date: _______________<br />
First Name: ___________________________ Last Name: ______________________<br />
(minimum of first 3 letters of last name required)<br />
DOB: _____________ ID#: _____________ Type: (see back) ________________________________<br />
(not needed if requesting most recent volume of record)<br />
BASTYR VIS MEDICATRIX NATURAE<br />
Out to: ___________________<br />
(Please write legibly to avoid unnecessary delays in processing your request.)<br />
43
Faculty providers frequently receive Patient Chart Requires Action (PCRA) slips from student<br />
clinicians, medical records staff, and patient services representatives. These slips indicate specific<br />
actions that must be taken regarding a patient’s record. These actions can include providing missing<br />
signatures and chart entries or following up on patient callbacks and reviewing outside medical records.<br />
A PCRA slip also serves as a record request slip for a patient's chart, in lieu of the actual Record<br />
Request slip. Please note that some patients have multiple volume charts. Unless otherwise indicated,<br />
clinicians receive the patient’s most recent chart volume. A request for multiple chart volumes for a<br />
patient must ac<strong>com</strong>pany a Record Request slip or PCRA slip for each volume requested. CHM<br />
students may request up to six charts from the chartroom at one time. All other student clinicians may<br />
request up to three charts at a time. Please note that requests can take up to 20 minutes to process, and<br />
all charts must be returned to the chartroom by the end of the day. Student clinicians are NOT to<br />
remove patient records from the building. Removing patient records from the clinic will result in<br />
disciplinary action. (See page 39, transporting records section.)<br />
PCRA Slip: The Patient Chart Requires Action slip requests that supervisors <strong>com</strong>plete a special<br />
follow-up. When submitted, this form can serve as a chart request in lieu of a Records Request Slip.<br />
Patient Chart Requires Action<br />
To: ______________________________<br />
Patient’s Name:<br />
_________________________________<br />
Patient’s DOB: _______________<br />
(Required)<br />
From: ___________________________<br />
What is needed:<br />
Today’s<br />
Date:<br />
_______________________<br />
Your signature on visit notes<br />
Your entry in patient visit summary<br />
Your signature on phone contact notes<br />
Your review of outside medical records<br />
Other: __________________________________________<br />
(date of visit): _________________<br />
(date of visit): _________________<br />
(date of contact): ______________<br />
(date received): _______________<br />
RECIPIENT, SIGN & DATE HERE TO REQUEST THIS<br />
CHART:<br />
_________________________________________________<br />
DATE: ______________<br />
44
REQUESTING A PATIENT’S RECORDS FROM ANOTHER PROVIDER<br />
If clinicians would like to receive a patient’s medical records from another healthcare facility or<br />
practitioner, they must have the patient <strong>com</strong>plete an Authorization to Release Confidential Health<br />
Information form. Clinicians should verify that the patient has filled the form out <strong>com</strong>pletely*, make a<br />
copy for the chart and the patient, and submit the original <strong>com</strong>pleted form to the Medical Records<br />
mailbox marked ‘Requests and Signature Returns’ (located diagonal to the chartroom window on the<br />
second floor). A sample <strong>com</strong>pleted authorization form is posted across from the Medical Records<br />
mailboxes for reference.<br />
*When reviewing authorization forms for <strong>com</strong>pleteness, clinicians should verify that the patient signed<br />
AND dated the form, and information is clearly written on the form. These elements are frequently<br />
overlooked and cause unnecessary delays in processing. It is not necessary to provide a <strong>com</strong>plete<br />
address for major facilities and providers, if the facility’s full name and location, or the provider’s full<br />
name and location of practice are indicated. Medical Records keeps addresses on file and provides this<br />
information as needed. Clinicians must ensure, however, that the information provided is sufficient to<br />
identify the individual or institution involved. The Medical Records office logs all requests for records,<br />
so clinicians may follow up on a previously submitted request at any time by checking with the<br />
Medical Records office.<br />
Procedure Summary<br />
Have the patient fill out an Authorization to Release Confidential Health Information form.<br />
Check the form for <strong>com</strong>pleteness and accuracy. In<strong>com</strong>plete forms result in processing delays.<br />
Make two copies of the authorization form, one to be given to the patient, the other to be filed in the<br />
patient’s chart (in the back on the right).<br />
Submit the original form to the Medical Records mailbox marked “Requests and Signature Returns.”<br />
Note: Average turn-around-time for receiving records is two weeks. Faculty supervisors receive notice<br />
when the records arrive.<br />
Expediting Requests<br />
Medical Records will try to ac<strong>com</strong>modate urgent or special requests for records as needed. If Medical<br />
Records has submitted a request for records to another individual or facility, the staff will try to obtain<br />
the records in time for the patient appointment. Faculty may call a facility to follow up on a request,<br />
but records must <strong>com</strong>e through the medical records office when they arrive. In<strong>com</strong>ing faxes containing<br />
patient information go to (206) 834-4131 in Medical Records.<br />
Similarly, a request may be given priority status by writing ‘RUSH’ at the top of the authorization<br />
form upon initial submission to the medical records office. This option is only for times when normal<br />
processing substantially <strong>com</strong>promises patient care.<br />
RELEASING RECORDS TO PATIENTS AND OTHER THIRD-PARTIES<br />
Medical Records must process all records releases. If a faculty or clinician receives a request for<br />
records from an outside third party, the faculty member must direct the request to Medical Records for<br />
processing. If patients wish to receive copies of their own medical records, a faculty member must<br />
approve the release, which can result in a delay in processing the request. Clinicians should either<br />
direct patients to the second floor appointment desk or initiate the request process as follows:<br />
Have the patient <strong>com</strong>plete an Authorization to Release Confidential Health Information form.<br />
45
Check the form for <strong>com</strong>pleteness.<br />
Have the faculty member initial the form in the top right space next to their printed name, signifying<br />
their approval of the release in advance. (This is an optional step initially, although it expedites the<br />
process. Supervisors may either approve the release in advance by initialing the form in the top right,<br />
or wait to approve it later. Medical Records will subsequently forward the request to the faculty<br />
supervisor, so the faculty member can review and initial it at that time.) There might be a charge for<br />
patients wanting records for personal use. A patient may inquire about fees for records at the second<br />
floor appointment desk. There is always a charge to send patient information to parties not directly<br />
involved in patient care.<br />
Submit the original <strong>com</strong>pleted form to the Medical Records mailbox labeled “Requests and Signature<br />
Returns,” located near the chartroom window on the second floor.<br />
Processing of all record releases is performed by the medical records office. Providers are not to<br />
release records directly to patients, because this <strong>com</strong>promises the clinic’s efforts to maintain quality<br />
control and <strong>com</strong>ply with applicable state and federal health information management laws. The clinic<br />
will not re-disclose medical information from other health care facilities directly to patients except<br />
under extraordinary circumstances. Patients are to contact the original facility to obtain copies of such<br />
information.<br />
As a professional courtesy, copies sent to other clinic/health care practitioners are sent at no charge. A<br />
patient who wants information for personal use may receive up to <strong>10</strong> pages at no charge. Copies in<br />
excess of <strong>10</strong> pages are charged the regular rate. There is no charge for patients who hand-deliver<br />
records to another health care provider, after confirmation of the patient’s appointment with the other<br />
provider. All copies sent to parties not directly involved in patient care are charged the full rate.<br />
Record releases to patients can take up to two weeks to process.<br />
LOOSE CHARTING<br />
Sometimes a chart is not available at the time of an appointment. In this case, the progress notes from<br />
the patient’s visit should be submitted to “loose charting.” Loose charting goes in the Labs and Loose<br />
Charting box, located in the hallway by the second floor copier outside the chartroom door. Loose<br />
charting on the first floor goes in the loose charting tray near the chart shelf.<br />
X-RAYS AND OTHER RADIOGRAPHIC IMAGING<br />
Active x-rays and other radiographic images are stored in the physical medicine department<br />
supervisor’s office for convenience and easy access for up to 30 days. After that time, medical records<br />
staff either returns the images to the facility that has loaned the records to the clinic, or forwards them<br />
to archives for long-term storage, if the clinic owns the record. Faculty supervisors will receive notice<br />
from the medical records office when x-rays and or other radiographic images arrive.<br />
46
DECEASED PATIENTS<br />
Initial Notification<br />
Clinicians, as well as all other staff members, must notify the medical records office if they receive<br />
notice that a patient is deceased. They should be prepared to provide the following information:<br />
Actions Taken<br />
o Identifying who provided notification that the patient was deceased.<br />
o Who at Bastyr received the original notification.<br />
o When the reporting party received notification.<br />
Once notified, the medical records office will:<br />
Provider Follow-Up<br />
o Notify the patient’s primary care provider, if s/he did not provide notification.<br />
o Notify the patient services representatives.<br />
o Place a notice in the patient’s chart that s/he is deceased.<br />
o Flag the patient’s Millbrook account for deceased status.<br />
Upon notification, the primary care provider may choose to contact surviving family members, send a<br />
card, attend the service, or take other actions as the provider deems appropriate. The provider will<br />
inform students and other providers at his/her discretion.<br />
PATIENT FORMS<br />
Patient forms are located in the south corner of the building on each floor. On the first floor, they are in<br />
the AOM storage area. On the second floor, they are on the south side of the preview/review rooms.<br />
Please contact the Medical Records Department or HIPAA Compliance Officer for questions regarding<br />
these forms.<br />
TREATMENT OF MINORS<br />
POLICY AND PROCEDURES ON PROVIDING HEALTH SERVICES<br />
These policies and procedures establish efficient and consistent mechanisms for the care and treatment<br />
of minors at Bastyr Center for Natural Health and privacy-related issues involving a minor's health<br />
records. Any person under the age of eighteen (18) is considered a minor at the Bastyr Center for<br />
Natural Health.<br />
MINORS PROVIDING THEIR OWN CONSENT<br />
General Rule<br />
Persons under the age of 18 may not consent to their own medical treatment unless one of the<br />
exceptions listed below applies. If none of the exceptions apply, parental consent to medical treatment<br />
is necessary for the provision of medical services to persons under the age of 18.<br />
47
Exceptions<br />
Below is a list of the exceptions that stipulate when persons under the age of 18 may consent to their<br />
own medical treatment:<br />
Age. A minor's consent is valid if the minor is over the age of eighteen (18). RCW 26.28.015.<br />
Emancipation. A minor's consent is valid for an emancipated minor. RCW 13.64.060. In Washington,<br />
evidence of a minor’s emancipation is through:<br />
o A Judicial Determination. The minor must submit a court order evidencing minor's<br />
Emancipation; or<br />
o A Clinical Determination. The healthcare provider considers that the minor is<br />
emancipated for purposes of receiving medical treatment, and documents in the<br />
patient's medical records, the age, maturity, intelligence, training, experience,<br />
economic independence, and the freedom from parental control that the minor<br />
exercises. Smith v. Seilby, 72 Wn.2d 16, 431 P.2d 719 (1967).<br />
o Marriage. A minor's consent is valid if the minor is married to a spouse 18 years or<br />
older. RCW 26.28.020. A minor married to a minor may give consent if emancipated<br />
(see “emancipation” above).<br />
Life-Threatening Emergency. Consent for care is implied by law when immediate treatment is<br />
required to preserve life or to prevent serious impairment of bodily functions, and when it is<br />
impossible to obtain the consent of the minor, the parent, or the legal guardian. RCW 18.71.220.<br />
Minor with Sexually Transmitted Disease (STD). A minor 14 years or older may consent to<br />
examination and treatment for an STD without the consent or knowledge of parent or guardian. RCW<br />
70.24.1<strong>10</strong>.<br />
Gynecological Services. Provided she is capable of giving informed consent, an unmarried minor 14<br />
years or older may consent to gynecological care, including examination and prescriptions for birth<br />
control.<br />
Reproductive Services. Provided she is capable of giving informed consent, an unmarried minor of<br />
any age may consent to treatment involving the reproductive autonomy of the minor.<br />
Minor Seeking Drug or Alcohol Abuse Outpatient Treatment. A minor 13 years of age or older<br />
may consent to counseling, care, treatment, or rehabilitation for outpatient treatment for conditions and<br />
problems caused by drug or alcohol abuse. RCW 70.96A.095.<br />
Mental Health Testing and Treatment. A minor 13 years or older may consent to inpatient and<br />
outpatient mental health treatment. RCW 71.34.030 and RCW 71.34.042.<br />
AUTHORIZATION TO CONSENT ON BEHALF OF A MINOR<br />
Any of the following individuals may consent to a minor’s medical treatment:<br />
o Either one of the parents, mother or father, of the minor patient.<br />
o A divorced parent with legal custody.<br />
o A divorced non-custodial parent, where the custodial parent cannot be reached and<br />
custodial parent has not previously objected to medical treatment. RCW 26.09.3<strong>10</strong>.<br />
o A minor parent that is married to a spouse 18 years or older. If the minor parent is<br />
married to a minor (dual minor parents), valid consent is determined by the<br />
emancipation factors above.<br />
48
How Consent is Given<br />
o Legal guardian. A signed copy of the court order establishing guardianship must be<br />
filed with the minor's medical records. RCW 26.09.3<strong>10</strong>.<br />
o Authorized department of social and health services (DSHS) representative. A court<br />
order establishing the minor as custody of DSHS and an authorized DSHS<br />
representative may consent to medical treatment for the minor. A copy of the court<br />
order must be filed with the minor's medical record.<br />
The individuals listed in Sections A-H above ("authorized individual(s)") may consent to treatment on<br />
behalf of a minor by signing a written consent form on the minor's first visit to the clinic. Please refer<br />
to the clinic’s informed consent policy for additional requirements. If an authorized individual is<br />
unavailable and delegates authority to consent on behalf of a minor to another individual (e.g., a<br />
grandparent), then the authorized individual shall provide a written delegation statement authorizing<br />
the other individual to consent to treatment on behalf of the minor. The delegation statement signed<br />
and dated by the authorized individual should state:<br />
“I, [name of parent] am the parent or legal guardian of [name of child] and am authorized to consent to<br />
diagnosis and medical treatment on their behalf. If I am personally unable or unavailable to provide<br />
such consent, I hereby authorize [name of designee] to consent to [name of child]'s medical treatment<br />
at the Bastyr Center for Natural Health.”<br />
A required written consent form or delegation statement may be waived in emergency situations or at<br />
the discretion of the clinic director.<br />
ACCESS TO A MINOR’S MEDICAL RECORDS<br />
Minors Control Their Medical Records and/or Health Information<br />
If the minor consented to the treatment pursuant to one of the exceptions above, the minor has the<br />
rights of access and control of disclosure regarding his or her medical records and/or health<br />
information (RCW 70.02.130). The clinic treats requests for disclosure from anyone other than the minor<br />
like any other request for patient information from someone other than the patient.<br />
Parent/Legal Guardian Control Minor's Medical Records and/or Health Information<br />
If parent or legal guardian has authority to act on behalf of the minor in making decisions related to<br />
health care, then the parent or legal guardian may access and control disclosure of the minor's medical<br />
records and/or health information.<br />
If a minor, authorized to consent for his or her own medical treatment, is a dependent for insurance<br />
purposes, the clinic may submit information to the insurance <strong>com</strong>pany for reimbursement in the<br />
ordinary course. Additionally, the clinic should submit all necessary and customary information to<br />
obtain payment for services rendered, even if the services were for a minor under an exception listed<br />
above.<br />
Disclosure Under Insurance Policy<br />
Submission of Health Information by Provider. Providers submit all necessary and required health<br />
information for processing claims with health plans and insurers.<br />
Duty of Health Plans and Insurers. Under the Washington State Patient's Bill of Rights, health plans<br />
and insurers may not send an explanation of benefits form to a policyholder if it would violate the<br />
privacy rights of a covered dependent. RCW 48.43.021<br />
49
GRIEVANCE/COMPLAINT POLICIY<br />
V. MISCELLANEOUS CLINIC POLICIES:<br />
GRIEVANCE, PARKING, FUNDRAISING<br />
GRIEVANCE POLICIES - STUDENT<br />
This policy enables students, to voice their concerns about policies, procedures, or other matters, and<br />
have their concerns addressed fairly.<br />
If students have a concern about an occurrence while on a patient care shift, a clinic assistant rotation,<br />
an external clinic shift, or preceptor shift, they should first discuss the matter in private with the<br />
supervising clinical faculty member. If it is not resolved, then students must meet with the Associate<br />
Dean, or their designee, by first submitting a letter outlining the situation, then scheduling a meeting to<br />
discuss the letter’s contents.<br />
If students have a concern about a policy or procedures or clinic operations in general, they should<br />
email a letter to the appropriate Associate Clinical Dean or lead and schedule an appointment to<br />
discuss it with them. If still unresolved, students should forward their letter with an explanation from<br />
the Associate Clinical Dean or clinic lead and schedule a meeting with the Medical Director.<br />
Student concerns about hours, number of shifts, credits, registration, clinic grades, or attendance<br />
should be discussed with the clinic registration staff on campus.<br />
Student concerns regarding the preceptor program are addressed to the preceptor coordinator in each<br />
respective school.<br />
GRIEVANCE POLICIES - PATIENTS<br />
If patients have a grievance, the attending supervisor or the student clinician provides a clinic <strong>com</strong>ment<br />
form for them to <strong>com</strong>plete. The forms are clearly labeled and on display in the patient waiting area. If<br />
the <strong>com</strong>ment is business-related, the <strong>com</strong>pleted form is routed to the practice management manager. If<br />
the <strong>com</strong>ment is related to health care services, it is routed to the clinic director and the Associate Dean<br />
or clinic lead for the program in which the <strong>com</strong>plaint related contact and procedure occurred. One of<br />
these two individuals or their designee addresses the matter. Once the concern is addressed, the patient<br />
is notified in writing.<br />
The patient services department and the front desk staff also handle many minor patient grievances.<br />
Upon a patient’s first visit to Bastyr Center for Natural Health, the patient services department gives<br />
the patient a patient information handout. On this handout is a list of patient rights and responsibilities.<br />
Therefore, patients are informed in writing of their right to bring forth any grievance that might arise<br />
regarding their care, service, health plan, or provider network.<br />
Please refer to the Student Handbook for other information regarding grievances, sanction, and appeals<br />
policies.<br />
50
FACILITIES, EQUIPMENT AND PARKING<br />
COPY MACHINE USAGE<br />
The copy machines are for clinic business only. Personal copies, including copies of class notes, must<br />
occur outside of the clinic. Unique codes have been provided for students, staff and faculty to aid in<br />
tracking copy use.<br />
PARKING AND BICYCLES<br />
Students must use on-street parking. The underground parking lot is for patient parking only. Cars will<br />
be towed if this rule is violated. Suggestions for student clinicians include: carpooling, using Metro or<br />
the Bastyr University Shuttle, or bicycling to the clinic if possible. There is a bike rack in the basement<br />
parking area. Do not park bikes against the handrail outside the front door, along the ramp leading to<br />
the front of the clinic, or anywhere along the street where the sidewalk or entrance might be partially<br />
blocked.<br />
TELEPHONE CONTACT POLICY<br />
Please observe the following rules for phone contact:<br />
The clinic’s phones are for clinic business only.<br />
All calls to patients must be pre-approved by the supervising clinical faculty member.<br />
If the patient’s residence is a long distance from the clinic, students must obtain permission from a<br />
supervisor to call and use a clinical faculty office phone.<br />
Calls to/from patients should be limited to three minutes. These calls should be limited to determining<br />
the status of the patient, reporting test results, clarifying treatment instructions, or re<strong>com</strong>mending<br />
follow up. If the call is longer than this, consider scheduling the patient for an office call or<br />
consultation. A phone contact should not replace an office visit.<br />
Clinicians are legally responsible for phone advice. A note in the chart must be made with the date,<br />
reason for the call, and any pertinent information or advice. Student clinicians and the supervising<br />
physician/clinical faculty members should both sign the note. Do not offer any new treatment advice or<br />
change any treatment plan without approval from the supervising clinical faculty member.<br />
There is a student phone in the lounge that may be used for local personal calls.<br />
Students should never give their home phone numbers to patients. Any business that a clinician needs<br />
to discuss with a patient should take place at the clinic, in person, or by phone.<br />
PAGERS/CELL PHONE USAGE<br />
All pagers and cell phones must be on vibratory alert mode (silent alert) or turned off while in the<br />
clinic, except preview/review and lounge areas. Furthermore, it is not permissible to answer these calls<br />
in a room with a patient during a patient visit. Answer urgent calls outside of patient care rooms.<br />
51
CLINIC CLOSING TIME<br />
In general, the clinic closes one hour after the last shift has ended. Students are required to leave the<br />
building prior to the last walk around by clinic facilities at the end of each business day. Facilities<br />
personnel will alert people of closing time about 15 minutes ahead of the actual closing. Students need<br />
to finish their work and charts and return them to medical records so that they can be out of the<br />
building by the appropriate time. AOM clinicians must finish all charting on a specific patient chart by<br />
the end of the shift when the patient was seen. There may be exceptions if students are working<br />
directly with a clinic faculty member after hours. In this case, students must be in direct proximity of<br />
the faculty member and must leave when they leave.<br />
Current hours are listed below and can change at any time.<br />
Day Last Shift Ends Closing Time<br />
M, T, Th 9 pm <strong>10</strong> pm<br />
W, F 5 pm 6 pm<br />
Sat 1 pm 2 pm<br />
CULTIVATION AND SOLICITATION POLICY (FUNDRAISING)<br />
All fundraising activities must be coordinated through the Development Department at campus.<br />
All departments, faculty, staff, and students must contact the Development Department before<br />
cultivating or soliciting any prospect or donor for any project or campaign. The Development<br />
Department coordinates all fundraising to ensure that those prospects are cultivated and solicited<br />
appropriately. Without this coordination, donor relations can be damaged if, for instance, more than<br />
one person solicits the same prospect/donor at the same time for different Bastyr projects.<br />
Coordination also ensures that Development can assist any person or department properly with<br />
cultivation and solicitation activities.<br />
DONATIONS<br />
The Development Department creates a file for each gift in our donor database. If someone wants to<br />
make a donation, have him or her simply write out a check to Bastyr University or contact<br />
Development at 425-602-3051. If a donor wants to contribute to a specific department or program<br />
only (and not the Operating Fund), they need to specify which department/program they intend in a<br />
note or letter.<br />
52
IN-KIND DONATIONS<br />
If a <strong>com</strong>pany or individual wishes to make an in-kind donation, please follow this procedure before<br />
acceptance:<br />
Gifts-in-Kind (furniture, equipment, securities, real estate, books, etc.) must be reviewed with special<br />
care by the Development and Finance Departments to ensure that acceptance will not involve financial<br />
<strong>com</strong>mitments in excess of budgeted items or other obligations disproportionate to the usefulness of the<br />
gift. Bastyr does not automatically accept all in-kind donations. The University must first determine if<br />
the item(s) is something needed. If so, contact the Development Department at 425-602-3051, and you<br />
will be given an in-kind donation form to fill out and return. The donor’s estimation of the dollar value,<br />
along with what you consider the item(s) dollar value to be, will be needed. When gifts-in-kind are<br />
given to this organization with the donor intent of receiving a tax deduction, it shall be the<br />
responsibility of the donor, not the organization, to obtain an appraisal of the gift. It is in the donor's<br />
best interest that the Bastyr not provide directly, nor be responsible for securing, the services of<br />
appraisers in connection with gifts to the university. Development will send out thank you letters<br />
within 48-hours upon receipt of the item(s) and copy your department.<br />
ACKNOWLEDGEMENT LETTERS<br />
The Development Department sends acknowledgement letters for all donations within 48 hours of<br />
receipt of contribution. The President of Bastyr University or Vice President for Development and/or<br />
other appropriate persons sign the letters.<br />
VOLUNTEER OPPORTUNITIES AND RECRUITMENT<br />
The Development Department identifies specific ways volunteers can be utilized for stewardship and<br />
fund raising. The goals for involvement of volunteers in fund raising efforts are:<br />
o Relationship building.<br />
o Social interaction with other donors, faculty, alumni, staff, and students.<br />
o Prospect identification and development.<br />
o Broadening our network of donors/prospects.<br />
COMMENTS AND FEEDBACK<br />
If you receive a <strong>com</strong>ment or <strong>com</strong>plaint regarding a fundraising event or solicitation, please contact the<br />
Vice president of Development at 425.601.3008.<br />
53
VI. APPENDICES<br />
I. CLINIC CONTRACT<br />
II.<br />
III.<br />
IV.<br />
STUDENT IMMUNIZATION CHECKLIST<br />
STUDENT CLINICIAN ABSENT/SUBSTITUTE FORM<br />
MEDICAL ABBREVIATIONS<br />
V. CO-MANAGEMENT: TEMPLATES AND ETIQUETTE GUIDELINES AND<br />
REFERRAL LETTERS<br />
54
Appendix 1<br />
CLINIC CONTRACT<br />
By signing this document, I am verifying that I have thoroughly read and familiarized myself with the<br />
Student Clinician Handbook, have attended the CE II class or clinic orientation, and received the<br />
information provided therein.<br />
I have especially noted the following areas and their differences between academic classroom policy<br />
and procedures, and clinic policy and procedures:<br />
Clinic Registration Process and Policies<br />
Add/Drop Process and Deadline Policies<br />
Paperwork Due Dates<br />
Clinical Competencies<br />
All Confidentiality Procedures and Policies<br />
Professional Conduct and Code of Ethics<br />
I will adhere to all confidentiality procedures and policies, knowing that all patient information,<br />
including electronically stored information, is confidential and should never be removed from, or<br />
discussed outside of the clinic.<br />
I understand and agree that I am responsible for knowing, understanding, and following all the<br />
information contained within the Student Clinician Handbook global module and department module(s)<br />
for my program(s), including all revisions and updates. I understand I am accountable for following<br />
and adhering to these policies and procedures. I also agree and acknowledge that any intentional<br />
falsification in my clinical <strong>com</strong>petency, documentation of patient contact hours, and/or clinic time<br />
sheets is cause for denial of all related clinic hours and may lead to additional disciplinary sanctions.<br />
Signature: ___________________________________________ Date: ______________________<br />
Printed Name: ________________________________________Degree Program(s): ____________<br />
A signed copy of this form, given to your instructor, is a requirement to pass the Clinic Entry course(s)<br />
and clinic orientation (OM4800-AOM or NM6804-ND). This signed copy will be on file with the<br />
clinic registration staff, and is a requirement for entering clinic.<br />
55
Appendix 2<br />
Bastyr University Health and Safety Department<br />
STUDENT HEPATITIS B CHECKLIST<br />
It is re<strong>com</strong>mended that health care workers exposed to blood or body fluids be vaccinated against<br />
Hepatitis B. Medical providers and students fall into this risk category both in the Bastyr Clinic and in<br />
some classes. Immunization provides <strong>10</strong>0% protection of contracting Hepatitis B. Therefore, each<br />
student should consider vaccination. Vaccination for Hepatitis B consists of a series of three injections.<br />
Please check one box below:<br />
I am immunized against Hepatitis B already, or am in the process of receiving the series. Attached<br />
is a copy of my immunization record or positive HB surface antibody test. I <strong>com</strong>pleted the Hepatitis B<br />
Vaccine Series on _________________________ (date).<br />
I was Hepatitis B Surface Antibody-positive on ________________________ (date).<br />
I had Hepatitis B on ______________________________________________ (date).<br />
I wish to receive the series of 3 Hepatitis B vaccinations. I have read the information about<br />
Hepatitis B and the Hepatitis B vaccine. I have had the opportunity to ask questions and understand the<br />
benefits and risks of Hepatitis B immunization. I understand I must have three doses of vaccine to<br />
confer optimum immunity, and I may be tested to document my susceptibility to Hepatitis B before<br />
receiving the vaccine. I understand there is no guarantee I will develop immunity to Hepatitis B by<br />
receiving this vaccine. I also understand I may experience an adverse side effect from the vaccine. I<br />
request that it be given to me, or to the person named below, of whom I am parent or guardian.<br />
(1) Given by: ________________________ Lot number ___________________ Date: _______<br />
(2) Given By: ________________________ Lot number ___________________ Date: _______<br />
(3) Given by: ________________________ Lot number ___________________ Date: _______<br />
I understand that due to my occupational exposure to blood and body fluids which are potentially<br />
infectious, I may be thus at risk for contracting Hepatitis B (HBV) infection, which is a serious disease.<br />
However, I decline HBV vaccine at this time. I understand that by declining the vaccine I continue to<br />
be at risk for contracting Hepatitis B. I also understand that I may change my mind and receive the<br />
vaccination at any time.<br />
This does not apply to me in the work that I do.<br />
Printed Name: _____________________________________<br />
Signature: _________________________________________ Date: ___________<br />
Witness: ___________________________________________ Date: ___________<br />
56
Appendix 3<br />
Bastyr Center for Natural Health<br />
STUDENT CLINICIAN ABSENCE / SUBSTITUTE FORM<br />
It is the responsibility of every Student Clinician to inform their assigned Supervisor of any planned<br />
absence from the clinic, and give this form to the Faculty Administrative Assistant.<br />
Please follow the procedures outlined below:<br />
Fill out the bottom portion of this form <strong>com</strong>pletely, otherwise it will be returned to you for further<br />
clarification. Fill out a separate form for each shift and planned absence.<br />
Notify the Supervisor of each shift you plan to miss, and have him/her sign the appropriate space.<br />
Primary and Secondary Student Clinicians must obtain a substitute for each shift you plan to miss, and<br />
have the substitute sign the appropriate space below.<br />
Once the form is <strong>com</strong>plete, submit it to the Clinic Faculty Administrative Assistant in S206. The form<br />
is kept on a quarterly basis.<br />
All of these procedures must be followed in advance of the planned absence.<br />
If you are suddenly ill or have a personal emergency, you must call your supervisor and the front desk<br />
at the clinic to page your supervisor as soon as possible.<br />
An unexcused absence will result in an automatic fail for the quarter.<br />
Name of Student (Please Print): _______________________________________________________<br />
Today’s Date: ___________________________<br />
Date of Absence: __________________________<br />
Department (Please Circle):<br />
Acupuncture/Oriental Medicine Dispensary Counseling<br />
Naturopathic Patient Care Homeopathy Nutrition<br />
Physical Medicine<br />
Lab<br />
Shift (Please Circle): Morning Afternoon Evening<br />
Reason for Absence: ______________________________________________________________<br />
Signature of Supervisor: ___________________________________________________________<br />
Name of Substitute (Please Print): ___________________________________________________<br />
Signature of Substitute: ____________________________________________________________<br />
57
Appendix 4<br />
MEDICAL ABBREVIATIONS<br />
The use of medical and scientific abbreviations is<br />
time saving and often a standard practice in the<br />
healthcare industry. A number of the abbreviations<br />
may appear with or without periods and with either<br />
capital or small letters.<br />
Abbreviation Meaning<br />
AAMA<br />
AB, ab<br />
ABC<br />
ABG<br />
ac<br />
AC<br />
Acc<br />
ACG<br />
ACS<br />
ACTH<br />
AD<br />
ad-lib<br />
adeno-CA<br />
ADH<br />
AE<br />
AFB<br />
AFP<br />
AIDS<br />
AK<br />
AKA<br />
ALL<br />
AMA<br />
AMI<br />
ANS<br />
AP<br />
AandP<br />
ARDS<br />
American Association of Medical Assistants<br />
abortion<br />
aspiration biopsy cytology<br />
arterial blood gas<br />
before meals (ante cibum)<br />
air conduction<br />
ac<strong>com</strong>modation<br />
angiocardiography<br />
American Cancer Society<br />
adrenocorticotropic hormone<br />
right ear (auris dextra)<br />
as desired<br />
adenocarcinoma<br />
antidiuretic hormone<br />
above the elbow<br />
acid-fast bacillus<br />
alpha-fetoprotein<br />
acquired immunodeficiency syndrome<br />
above the knee<br />
above-knee amputation<br />
acute lymphocytic leukemia<br />
American Medical Association<br />
acute myocardial infarction<br />
autonomic nervous system<br />
anteroposterior<br />
auscultation and percussion<br />
adult respiratory distress syndrome<br />
58<br />
ARMD<br />
AS<br />
sinistra)<br />
ASD<br />
ASHD<br />
Astigm<br />
ATN<br />
AV<br />
AVR<br />
BaE<br />
baso<br />
BBB<br />
BE<br />
bid<br />
BIN, bin<br />
BK<br />
BKA<br />
BM<br />
BMR<br />
BNO<br />
BP<br />
BPH<br />
BUN<br />
bx<br />
C1, C2 to C8<br />
CA, Ca<br />
CAD<br />
CAT, CT<br />
CBC<br />
cc<br />
<strong>com</strong>plaint<br />
cc<br />
CCU<br />
CDC<br />
CDH<br />
CEA<br />
CHD<br />
age-related macular degeneration<br />
aortic stenosis; left ear (auris<br />
atrial septal defect<br />
arteriosclerotic heart disease<br />
astigmatism<br />
acute tubular necrosis<br />
atrioventricular, arteriovenous<br />
aortic valve replacement<br />
barium enema<br />
basophil<br />
bundle-branch block<br />
below the elbow<br />
twice a day<br />
twice a night<br />
below the knee<br />
below-knee amputation<br />
bowel movement<br />
basal metabolic rate<br />
bladder neck obstruction<br />
blood pressure<br />
benign prostatic hyperplasia<br />
blood urea nitrogen<br />
biopsy<br />
cancer, calcium<br />
coronary artery disease<br />
<strong>com</strong>puterized axial tomography<br />
<strong>com</strong>plete blood count<br />
cardiac catheterization; chief<br />
cubic centimeter<br />
coronary care unit<br />
Centers for Disease Control<br />
congenital dislocation of the hip<br />
carcinoembryonic antigen<br />
coronary heart disease
CHF<br />
congestive heart failure<br />
CI<br />
chlorine<br />
cm<br />
centimeter<br />
CMA<br />
certified medical assistant<br />
CMML<br />
chronic myelomonocytic leukemia<br />
CNS<br />
central nervous system<br />
CO 2<br />
carbon dioxide<br />
COLD<br />
chronic obstructive lung disease<br />
COPD<br />
chronic obstructive pulmonary disease<br />
CP<br />
cerebral palsey<br />
CPD<br />
cephalopelvic disproportion<br />
CPR<br />
cardiopulmonary resuscitation<br />
CS, C-section cesarean section<br />
CSF<br />
cerebrospinal fluid<br />
CT<br />
<strong>com</strong>puted tomography<br />
CTS<br />
carpal tunnel syndrome<br />
CV<br />
cardiovascular<br />
CVA<br />
cerebrovascular accident<br />
CVD<br />
cardiovascular disease<br />
CWP<br />
childbirth without pain<br />
CXR<br />
chest x-ray<br />
cysto<br />
cystoscopy<br />
D<br />
diopter (lens strength)<br />
do<br />
discontinue<br />
/d per day<br />
DandC<br />
dilation and curettage<br />
DDS<br />
Doctor of Dental Surgery<br />
DandE<br />
dilation and evacuation<br />
Derm<br />
dermatology<br />
DI<br />
diabetes insipidus; diagnostic imaging<br />
diff<br />
differential count (white blood cells)<br />
DM<br />
diabetes mellitus<br />
DO<br />
doctor of osteopathy<br />
DOA<br />
dead on arrival<br />
DOB<br />
date of birth<br />
DPT<br />
diphtheria, pertussis, tetanus<br />
59<br />
DRGs<br />
DUB<br />
DVT<br />
dx<br />
EBV<br />
ECG, EKG<br />
ECF<br />
facility<br />
EDC<br />
confinement<br />
EEG<br />
EENT<br />
EMG<br />
ENT<br />
EOM<br />
eosin<br />
ESR<br />
EST<br />
ET<br />
F<br />
FACP<br />
Physicians<br />
FAGS<br />
Surgeons<br />
FBS<br />
FDA<br />
FEF<br />
FEKG<br />
FEV<br />
FH<br />
FHR<br />
FHT<br />
FS<br />
FSH<br />
FTND<br />
FUO<br />
FVC<br />
Fx<br />
diagnostic related groups<br />
dysfunctional uterine bleeding<br />
deep vein thrombosis<br />
diagnosis<br />
Epstein-Barr virus<br />
electrocardiogram<br />
extracellular fluid; extended care<br />
estimated or expected date of<br />
electroencephalogram<br />
eye, ear, nose, and throat<br />
electromyogram<br />
ear, nose, and throat<br />
extraocular movement<br />
eosinophil<br />
erythrocyte sedimentation rate<br />
electric shock therapy<br />
esotropia<br />
Fahrenheit<br />
Fellow, American College of<br />
Fellow, American College of<br />
fasting blood sugar<br />
Food and Drug Administration<br />
forced expiratory flow<br />
fetal electrocardiogram<br />
forced expiratory volume<br />
family history<br />
fetal heart rate<br />
fetal heart tone<br />
frozen section<br />
follicle-stimulating hormone<br />
full-term normal delivery<br />
fever of undetermined origin<br />
forced vital capacity<br />
fracture
GB<br />
gallbladder<br />
GC<br />
gonorrhea<br />
GH<br />
growth hormone<br />
GI<br />
gastrointestinal<br />
gm<br />
gram<br />
gr<br />
grain<br />
GTT<br />
glucose tolerance test<br />
Gtt<br />
drops (guttae)<br />
GU<br />
genitourinary<br />
Gyn<br />
gynecology<br />
H<br />
hypodermic; hydrogen<br />
h<br />
hour<br />
HCG<br />
human chronic gonadotropin<br />
HCI<br />
hydrochloric acid<br />
HCO<br />
bicarbonate<br />
HCT, hot hematocrit<br />
HD<br />
hip disarticulation; hemodialysis; hearing<br />
distance; Hodgkin's disease<br />
HDL<br />
high-density lipoprotein<br />
HEENT head, eyes, ears, nose, and throat<br />
Hg<br />
mercury<br />
Hgb, Hb hemoglobin<br />
HIV<br />
human immunodeficiency virus<br />
HMD<br />
hyaline membrane disease<br />
HNP<br />
herniated nucleus pulposus (herniated disk)<br />
HP<br />
hemipelvectomy<br />
hs<br />
at bedtime<br />
HSG<br />
hysterosalpingography<br />
HSV<br />
herpes simplex virus<br />
hypo<br />
hypodermically<br />
IAS<br />
interatrial septum<br />
IBD<br />
inflammatory bowel disease<br />
ICF<br />
intracellular fluid<br />
ICSH<br />
interstitial cell-stimulating hormone<br />
ICU<br />
intensive care unit<br />
IandD<br />
incision and drainage<br />
ID<br />
intradermal<br />
IDDM<br />
Ig<br />
IH<br />
IM<br />
inj<br />
IOL<br />
iop<br />
IPPB<br />
breathing<br />
IQ<br />
IRDS<br />
syndrome<br />
IS<br />
IUD<br />
IV<br />
IVC<br />
cholangiography<br />
IVF<br />
IVP<br />
IVS<br />
K<br />
KD<br />
kg<br />
KS<br />
KUB<br />
l<br />
insulin-dependent diabetes mellitus<br />
immunoglobulin<br />
infectious hepatitis<br />
intramuscular<br />
injection<br />
intraocular lens<br />
intraocular pressure<br />
intermittent positive-pressure<br />
intelligence quotient<br />
infant respiratory distress<br />
intercostal space<br />
intrauterine device<br />
intravenous<br />
inferior vena cava, intravenous<br />
in vitro fertilization<br />
intravenous pyelogram<br />
interventricular septum<br />
potassium<br />
knee disarticulation<br />
kilogram<br />
Kaposi's sar<strong>com</strong>a<br />
kidney ureter bladder<br />
liter<br />
L1, L2 to L5 first lumbar vertebra, second<br />
lumbar vertebra through fifth lumbar vertebra<br />
LA<br />
LandA<br />
LAT, lat<br />
LB<br />
LDL<br />
LE<br />
extremity<br />
LH<br />
LLQ<br />
LMP<br />
left atrium<br />
light and ac<strong>com</strong>modation<br />
lateral<br />
large bowel<br />
low-density lipoprotein<br />
lupus erythematosus, lower<br />
luteinizing hormone<br />
left lower quadrant<br />
last menstrual period<br />
60
LP<br />
lumbar puncture<br />
Ortho, ORTH<br />
orthopedics<br />
LPN<br />
Licensed Practical Nurse<br />
OS<br />
left eye (oculus sinister)<br />
LRQ<br />
lower right quadrant<br />
os<br />
mouth; opening; bone<br />
LUQ<br />
left upper quadrant<br />
Oto<br />
otology<br />
LV<br />
left ventricle<br />
OU<br />
both eyes (oculi unitas)<br />
lymphs<br />
lymphocytes<br />
OV<br />
office visit<br />
MCH<br />
mean corpuscular hemoglobin<br />
oz<br />
ounce<br />
MCHC<br />
concentration<br />
MCV<br />
MD<br />
mets<br />
mg<br />
MH<br />
MI<br />
mix. astig<br />
ml<br />
mm<br />
mono<br />
MRI<br />
MS<br />
MSH<br />
MVP<br />
Myop<br />
Na<br />
NPH<br />
NPO<br />
NSAID<br />
O 2<br />
OA<br />
OB<br />
OB-GYN<br />
OCPs<br />
OD<br />
mean corpuscular hemoglobin<br />
mean corpuscular volume<br />
Medical Doctor<br />
metastases<br />
milligram (1/<strong>10</strong>00 gram)<br />
marital history<br />
myocardial infarction; mitral insufficiency<br />
mixed astigmatism<br />
milliliter (1/<strong>10</strong>00 liter)<br />
millimeter (1/<strong>10</strong>00 meter; 0.039 inch)<br />
monocyte<br />
magnetic resonance imaging<br />
mitral stenosis; multiple sclerosis<br />
melanocyte-stimulating hormone<br />
mitral valve prolapse<br />
myopia<br />
sodium<br />
neutral prolamine Hagedorn (insulin)<br />
nothing by mouth (nulla per os)<br />
nonsteroidal anti-inflammatory drug<br />
oxygen<br />
osteoarthritis<br />
obstetrics<br />
obstetrics and gynecology<br />
oral contraceptive pills<br />
right eye (oculus dexter); overdose<br />
P<br />
PA<br />
Pap smear<br />
paren<br />
PAT<br />
Path<br />
PBI<br />
PC<br />
PCP<br />
PCV<br />
PD<br />
PE<br />
PET<br />
PGH<br />
pH<br />
PID<br />
PKU<br />
PMN<br />
PMP<br />
PND<br />
PNS<br />
PO<br />
poly<br />
pp<br />
prn<br />
PT<br />
Therapy<br />
pulse<br />
posteroanterior<br />
Papanicolaou's smear<br />
parenterally<br />
paroxysmal atrial tachycardia<br />
pathology<br />
protein-bound iodine<br />
after meals<br />
Pneumocystis carinii pneumonia<br />
packed cell volume (hematocrit)<br />
peritoneal dialysis<br />
physical examination<br />
positron emission tomography<br />
pituitary growth hormone<br />
hydrogen ion concentration<br />
pelvic inflammatory disease<br />
phenylketonuria<br />
polymorphonuclear neutrophil<br />
previous menstrual period<br />
paroxysmal nocturnal dyspnea<br />
peripheral nervous system<br />
orally<br />
polymorphonuclear neutrophil<br />
postprandial (after meals)<br />
as required<br />
prothrombin time; Physical<br />
od<br />
once a day<br />
PTH<br />
parathyroid hormone<br />
OHS<br />
open heart surgery<br />
PTT<br />
partial thromboplastin time<br />
OR<br />
operating room<br />
PVC<br />
premature ventricular contraction<br />
61
q (spell out)<br />
qam<br />
qd<br />
qh<br />
q2h<br />
qid<br />
qpm<br />
qns<br />
R, rt right<br />
RA<br />
rad<br />
RAI<br />
RBC<br />
RD<br />
REM<br />
RLQ<br />
R.N.<br />
RNA<br />
R/O<br />
ROM<br />
RP<br />
RU<br />
RUQ<br />
RV<br />
Rx<br />
s<br />
every, daily<br />
every morning<br />
every day (quaque die)<br />
every hour<br />
every two hours<br />
four times a day<br />
every night<br />
quantity not sufficient<br />
right atrium, rheumatoid arthritis<br />
radiation absorbed dose<br />
radioactive iodine<br />
red blood cell; red blood count<br />
respiratory disease<br />
rapid eye movement<br />
right lower quadrant<br />
registered nurse<br />
ribonucleic acid<br />
rule out<br />
range of motion<br />
retrograde pyelogram<br />
routine urinalysis<br />
right upper quadrant<br />
right ventricle<br />
prescription, treatment, therapy<br />
without<br />
S1, S2 to S5 first sacral vertebra, second sacral vertebra<br />
through fifth sacral vertebra<br />
SA<br />
SC<br />
SCD<br />
SD<br />
seg<br />
SGOT<br />
SGPT<br />
SH<br />
SLE<br />
sinoatrial node<br />
subcutaneous<br />
sudden cardiac death<br />
shoulder disarticulation<br />
polymorphonuclear neutrophil<br />
serum glutamic-oxaloacetic transaminase<br />
serum glutamic-pyruvic transaminase<br />
serum hepatitis<br />
systemic lupus erythematosus<br />
SOB<br />
SOS<br />
sp. gr.<br />
SR<br />
St<br />
staph<br />
stat<br />
STD<br />
strep<br />
subcu, subq<br />
Svc<br />
SVD<br />
T<br />
shortness of breath<br />
if necessary<br />
specific gravity<br />
sedimentation rate<br />
strabismus (esotropia)<br />
staphylococcus<br />
immediately<br />
sexually transmitted disease<br />
streptococcus<br />
subcutaneous<br />
superior vena cava<br />
spontaneous vaginal delivery<br />
temperature<br />
T1, T2 to T12 first thoracic vertebra, second<br />
thoracic vertebra through twelfth thoracic vertebra<br />
T 3<br />
T 4<br />
TAH<br />
T and A<br />
TB<br />
THA<br />
THR<br />
TIA<br />
tid<br />
TKA<br />
TKR<br />
TNM<br />
top<br />
TPN<br />
TPR<br />
respiration<br />
TPUR<br />
TSH<br />
TSS<br />
TUR, TURP<br />
prostate<br />
TX<br />
triiodothyronine<br />
thyroxine<br />
total abdominal hysterectomy<br />
tonsillectomy and adenoidectomy<br />
tuberculosis<br />
total hip arthroplasty<br />
total hip replacement<br />
transient ischemic attack<br />
three times a day<br />
total knee arthroplasty<br />
total knee replacement<br />
tumor, nodes, metastasis<br />
topically<br />
total parenteral nutrition<br />
temperature, pulse, and<br />
transperineal urethral resection<br />
thyroid-stimulating hormone<br />
toxic shock syndrome<br />
transurethral resection of the<br />
tumor cannot be assessed<br />
62
U (spell out)<br />
units<br />
VHD<br />
ventricular heart disease<br />
UA<br />
urinalysis<br />
VLDL<br />
very-low-density lipoprotein<br />
UC<br />
uterine contractions<br />
VSD<br />
ventricular septal defect<br />
UGI<br />
ULQ<br />
ung<br />
URI<br />
UTI<br />
UV<br />
VA<br />
VC<br />
VD<br />
upper gastrointestinal<br />
upper left quadrant<br />
ointment<br />
upper right quadrant<br />
urinary tract infection<br />
ultraviolet<br />
visual acuity<br />
vital capacity<br />
venereal disease<br />
WBC<br />
blood count<br />
wt<br />
w/v<br />
x<br />
XP<br />
XT<br />
XX<br />
XY<br />
white blood cell (count); white<br />
weight<br />
weight by volume<br />
multiplied by<br />
xeroderma pigmentosa<br />
exotropia<br />
female sex chromosomes<br />
male sex chromosomes<br />
VF<br />
visual field<br />
63
Appendix 5<br />
PATIENT CO-MANAGEMENT: TEMPLATES AND ETIQUETTE GUIDELINES<br />
In order to facilitate professional and appropriate <strong>com</strong>munications between Bastyr Center for Natural<br />
Health providers and other healthcare providers, we all need to use similar standards for referral and<br />
treatment summary letters. Following this introduction, you will find copies of a model for a treatment<br />
summary letter, a model for a referral-to-a-specialist letter, and examples of both letters.<br />
The following are elements of professional etiquette:<br />
It is customary to write a treatment summary letter to the referring primary care doctor shortly after the<br />
first referred visit. If the initial strategy of the case management can only be summarized after several<br />
visits, the treatment summary is <strong>com</strong>pleted after the second or third visit. This summary letter is<br />
applicable to all referrals from primary care doctors.<br />
After you have received written consent from the patient, you should write a treatment summary to this<br />
patient’s primary care doctor even if the patient is seeing you outside of a referral. This is essential for<br />
safe and effective co-managed care.<br />
You should periodically send treatment summary updates to the patient’s primary care provider. The<br />
interval of these letters is dependent upon the nature of the case.<br />
Treatment summary letters to primary care doctors may not instruct the primary care doctor in the care<br />
of the patient. Treatment summary letters summarize your findings and management in order to inform<br />
the primary care physician. You should not re<strong>com</strong>mend general screening tests or interventions outside<br />
the scope of the referral to the patient or to the referring primary care physician. You may inquire about<br />
the primary care physician’s intended screening or case management strategies. The language of<br />
treatment summary letters should be deferential; after all, you are seeing “their” patient as a specialist.<br />
If you are the primary care physician writing a letter to a specialist, it is important to summarize all<br />
relevant findings so that the time your patient spends with the specialist is productive and effective.<br />
Your letter should be instructive and should contain copies of relevant diagnostic reports.<br />
64
Today’s date<br />
Doctor Name<br />
Address<br />
RE: patient name DOB: of patient ICD-9: referred ICD-9 diagnosis<br />
Dear Dr. ________,<br />
We thank you for the opportunity to see your patient, Jane Doe, for <strong>com</strong>plementary naturopathic care at<br />
Bastyr Center for Natural Health – Team Care.<br />
HX: Start with a statement of the total number of visits and the dates of the visits. Re-state presenting<br />
CC, which must be the same as the referred diagnosis. Discuss history of present illness (i.e. summary of<br />
chief <strong>com</strong>plaint attributes). Also list the relevant and associated secondary diagnoses/<strong>com</strong>plaints.<br />
ROS (significant): List significant past medical history as well as pertinent negatives.<br />
PMHX: List pertinent or significant past medical history<br />
FAM HX: List pertinent or significant family history<br />
MEDS/SUPPLMNTS: Upon initial visit, list the medications and supplements patient was taking. List<br />
any known allergies to medications in CAPITAL FONT.<br />
PE: Summary of relevant PE findings at first, or most recent, visit<br />
MNGMNT: Summary of case management, including responses to treatments, new PE findings, and<br />
progression of treatments.<br />
RECOMMENDATIONS: Overall summary of patient response to naturopathic/acupuncture/nutrition<br />
treatment and your request for additional referrals if necessary.<br />
Please contact us if you have any further questions or concerns.<br />
Sincerely,<br />
Doctor’s Name & Credentials<br />
Supervising Faculty<br />
Student’s Name<br />
Student Clinician<br />
CC: patient<br />
65
Today’s Date<br />
Dr. Primary Care Doctor<br />
<strong>10</strong>01 1st Ave.<br />
Seattle, WA 98111<br />
RE:<br />
Jane Doe<br />
DOB: 1/1/01 ICD-9: 564.1 (irritable bowel syndrome)<br />
Dear Dr. Primary Care Doctor,<br />
I thank you for the opportunity to see your patient, Jane Doe, for <strong>com</strong>plementary naturopathic care at<br />
Bastyr Center for Natural Health – Team Care.<br />
HX: I have seen Jane Doe three times (2/3/01, 3/8/01, and 4/15/01). She first presented on 2/3/01 with a<br />
diagnosis of irritable bowel syndrome (564.1). On February 3 rd , Ms. Doe reported that her IBS symptoms<br />
began during the winter of 1999. She experienced 2 episodes of the stomach flu within 1 month of each<br />
other. Subsequent to these flu episodes, Ms. Doe has experienced gastrointestinal problems. She<br />
described constant eructation, sore and irritating pressure in her epigastric area, and flatulence. Her<br />
symptoms present somewhat intermittently without any identifiable pattern. She reported that she had<br />
tested negative for giardia and H. pylori. She also has had a negative endoscopy and biopsy. Finally, a<br />
24-hour pH test revealed weakened LES and a gastric emptying test revealed delayed gastric emptying.<br />
Ms. Doe explained that antacids and doxepin were mildly helpful in temporarily alleviating her<br />
symptoms. She also informed me that various food eliminations and a decrease in caffeine and alcohol<br />
were somewhat helpful. Ms. Doe expressed concern that this past summer, she experienced two<br />
episodes of diarrhea, which was a new symptom for her. Ms. Doe denied stabbing, crampy, or burning<br />
pain. She denied nausea or vomiting. She reported 2-3 bowel movements weekly that were well formed<br />
and without abnormalities. In general, Ms. Doe reported excellent lifestyle habits. Her diet was<br />
sufficient in calories, although very limited in variety. She reported regular exercise and sleep. Ms.<br />
Doe’s primary goal was to regain normal, asymptomatic digestive function.<br />
ROS (significant): History of dysthymia; currently mild. No significant symptoms reported with regards<br />
to cardiovascular, dermatological, musculoskeletal, urinary, or reproductive functions.<br />
PMHX: Ms. Doe had a benign breast cyst diagnosed in July 2001. Ms. Doe reported PMS symptoms for<br />
which she recently has been prescribed oral contraceptives.<br />
FAM HX: Mother with HTN, diagnosed at age 45. Paternal grandfather with ulcerative colitis.<br />
MEDS/SUPPLMNTS: Upon initial visit – LoEstrin 28, B vitamin supplement (50 mg daily), Calcium<br />
supplement (1500 mg daily). ALLERGIC TO ERYTHROMYCIN.<br />
PE: bp: <strong>10</strong>0/64, p: 52; reg., t: 98.3, rr: 16. Heart: rrr, no extra sounds. Thyroid: non-palpable. Abdomen:<br />
bs x 4; no shifting dullness, no masses, negative hepatic or splenic enlargement, mild tenderness to deep<br />
palpation of RLQ and suprapubic regions.<br />
MNGMNT: Based upon the presentation of the IBS symptoms and the onset of the symptoms after<br />
repeated viral infections, we presumed that the IBS symptoms developed as a result of intestinal<br />
dysbiosis, decreased intestinal mucosal integrity and an associated prostaglandin pro-inflammatory<br />
imbalance. At Ms. Doe’s first visit, we re<strong>com</strong>mended oral acidophilus supplementation (HMF Forte), a<br />
digestive stimulant, mild laxative, and carminative herbal tincture (Rumex crispus: Foeniculum vulgare),<br />
an extract of licorice (Glycyrrhiza glabra) for its anti-inflammatory and mucosal healing properties, and<br />
an omega-3 fatty acid supplement.<br />
66
After a month on this plan, Ms. Doe returned on March 8 th , when she reported some improvement. She<br />
was having a bowel movement every other day and experiencing a con<strong>com</strong>itant decrease in flatulence.<br />
Her abdominal dis<strong>com</strong>fort was still present; however, it was decreased in intensity. She reported no<br />
change in her eructation. She also reported a 14-day menses after taking the oral contraceptives for 2<br />
weeks. She was fully <strong>com</strong>pliant with the treatment. Based upon this response, we re<strong>com</strong>mended that she<br />
continue with the current plan with the exception of the licorice extract, which we discontinued. We<br />
re<strong>com</strong>mended the addition of Filipendula officinalis herbal tincture (gastrointestinal nervine, herbal<br />
antacid, and anti-inflammatory) and a plant-based digestive enzyme supplement. We re<strong>com</strong>mended that<br />
she increase the variety of vegetables and fruit in her diet. Ms. Doe returned in another month on April<br />
15 th . At this visit, she reported some further improvement in her abdominal dis<strong>com</strong>fort, flatulence and<br />
reported that she was not burping as frequently as previously.<br />
Overall, she estimated her improvement at 50%. Most of her symptoms only occurred with the<br />
consumption of certain foods, namely some raw vegetables, pizza, and chocolate chip cookies. At this<br />
visit, we discussed Ms. Doe’s stress level and determined that, despite excellent stress management<br />
practices; she tended to internalize work stress. At this point, we surmised that the dysbiosis and<br />
mucosal integrity of her intestinal track were somewhat improved. However, we suspected that her<br />
internalized stress and physiologically caused inflammation from certain foods were triggering increased<br />
levels of CRF and associated IL-1 release. These molecules are known to bind to 5-HT receptors in the<br />
digestive tract causing constipation and diarrhea depending on the receptor subtype. We further<br />
suspected that her symptoms were aggravated by functional HCl and pancreatic enzyme deficiencies,<br />
given the preponderance of eructation and the epigastric dis<strong>com</strong>fort. Based upon these suspected<br />
etiologies of her IBS, we re<strong>com</strong>mended that Ms. Doe continue the acidophilus, omega-3 and pancreatic<br />
enzymes. We made new re<strong>com</strong>mendations for nervine and adaptogenic botanicals (Eleutherococcus<br />
senticosus and Avena sativa) and betaine HCl. Finally, we emphasized the importance of additional<br />
stress management at work and shared some additional techniques with Ms. Doe.<br />
RECOMMENDATIONS: It appears as though Ms. Doe is responding well to naturopathic treatment of<br />
her irritable bowel syndrome. We suspect that Ms. Doe will need additional time for the healing process<br />
to continue. We would very much like to continue to support Ms. Doe with naturopathic medical<br />
treatment. An additional referral for 3 visits to begin in July 2001 and to occur over a period of 6 months<br />
would best enable us to provide this naturopathic care to Ms. Doe.<br />
Please contact us if you have any further questions or concerns.<br />
Sincerely,<br />
Doctor’s Name, & Credentials<br />
Supervising Faculty<br />
CC: Jane Doe<br />
Student’s Name,<br />
Student Clinician<br />
67
Today’s Date<br />
Doctor Name<br />
Doctor Address<br />
RE: patient name<br />
Scheduled appt. time and date<br />
DOB: patient birth date<br />
Dear Dr. ________,<br />
I am referring ____ to you for further evaluation of symptoms consistent with (diagnosis or presumptive<br />
diagnosis with ICD-9).<br />
Pertinent Hx: List HPI, relevant PMHx, relevant ROS, and relevant FamHx<br />
Physical Exam and Labs: List significant findings<br />
Interventions: List all current medications and supplements. (Include state t regarding any known drug<br />
allergies)<br />
Impression: List suspected rule-outs, requested evaluations, examinations, and follow-up. In regard to<br />
evaluation of this patient, please provide us with the following:<br />
_____ a brief written report on findings (with verbal report if desired).<br />
_____ treatment.<br />
_____ periodic status reports on the patient if she/he remains under your care.<br />
Thank you for agreeing to see _______. For further information, please contact Dr. _ (ND supervisor)<br />
__ at doctor’s phone #. Thank you so much for your help in the care of this patient.<br />
Sincerely,<br />
Doctor’s Name & Credentials<br />
Supervising Faculty<br />
Student’s name<br />
Student Clinician<br />
CC: Patient<br />
68
Dr. GI Specialist<br />
GI Specialist Building<br />
123 1 st Ave.<br />
Seattle, WA 98111<br />
Today’s Date<br />
RE: Jane Doe DOB: 2/3/50 SS#: 202-20-0220<br />
Dear Dr. GI Specialist,<br />
I am referring Jane Doe to you for further evaluation of abdominal pain (789.00.<br />
Pertinent Hx: Ms. Doe first presented with abdominal pain on September 22, 2001. She reported that she<br />
had experienced intermittent abdominal pain since March of 2001. The pain was located in her right<br />
lower quadrant. She described it as achy, occasionally sharp. The pain was noticeably worse prior to<br />
menses, in the morning upon waking. She reported some relief with hot showers. She described<br />
associated dis<strong>com</strong>fort in her low back. She also described a 4-month history of constipation, with one<br />
difficult to pass bowel movement every 3 rd day. She denied association of her abdominal pain with<br />
defecation or eating. Her menses is regular every 23 to 26 days. She also denied fever, nausea, or<br />
bloating. Ms. Doe has a long-standing history of GER with ingestion of certain foods and is status post<br />
cholestectomy in 1999 secondary to cholelithiasis. During my most recent visit with Ms. Doe, on<br />
October 3 rd , she reported that her abdominal pain was more frequent (daily) and was worse than<br />
previously in the mornings. In a recent phone call, Ms. Doe reported that her pain had be<strong>com</strong>e more<br />
severe and more constant. She reported being awakened by her pain after more than 3 hours of sleep.<br />
Sitting up provided some relief. Other pertinent history includes moderate obesity, cholethiasis<br />
(cholestectomy 2000) with splenic enlargement in 2000 (see enclosed ultrasound report), and<br />
microcytic anemia (diagnosed 9/25/01).<br />
Physical Exam and Labs Physical examination on October 31, 2001 revealed the following significant<br />
findings: Abdominal examination: normal b.s. x 4 but diminished, no masses, tenderness to deep<br />
palpation of RLQ and pain reported in RLQ upon deep palpation of LLQ, -HSM Gynecological<br />
examination: without abnormalities. Uterus was partially palpable without tenderness or apparent<br />
enlargement. Ovaries were not palpable bilaterally; however deep palpation did not elicit any dis<strong>com</strong>fort.<br />
Interventions: Ms. Doe has been taking a multivitamin and an herbal formula for<br />
______Days/weeks/months/years. On October 3 rd , 2001, she began taking Iron citrate (200 mg<br />
elemental iron daily). Ms. Doe has no known drug allergies.<br />
69
Impression: I am concerned about the worsening pain pattern that Ms. Doe is experiencing. I am also<br />
concerned about the recent finding of microcytic anemia. In particular, I would like to rule out colonic<br />
carcinoma, appendicitis or colitis. In light of the worsening symptoms, I have also scheduled an<br />
abdominal CT for Ms. Doe on October 20, 2001. I will have the written report of this CT faxed to you as<br />
well. In regard to evaluation of this patient, please provide:<br />
brief written or verbal report on findings.<br />
diagnostic work-up as indicated.<br />
periodic status reports on the patient if she/he remains under your care.<br />
Ms. Doe has an appointment with you on October 28, 2001. Your re<strong>com</strong>mendations would be<br />
appreciated. If further information is needed, please contact me. Thank you so much for your help in the<br />
care of this patient.<br />
Sincerely,<br />
Doctor’s Name<br />
Credentials Supervising Faculty<br />
Student’s Name<br />
Student Clinician<br />
CC: patient<br />
Enclosure: Abdominal ultrasound written report of 2/99; CBC with differential of 9/25/01<br />
70
VII. INDEX<br />
A<br />
absence · 9<br />
planned · <strong>10</strong><br />
sub form · 57<br />
unexcused · <strong>10</strong><br />
accident<br />
patient/visitor · 33<br />
C<br />
case preview/review · 16<br />
clinic contract · 55<br />
<strong>com</strong>municable disease outbreak · 35<br />
copy machine · 51<br />
D<br />
deceased patients · 47<br />
dress code · 6<br />
violations · 7<br />
E<br />
earthquake response plan · 35<br />
email · 41<br />
ethics · 5<br />
external sites · 9<br />
F<br />
failure · 13, 15<br />
G<br />
grievance, policy for students · 50<br />
H<br />
handwashing · 25<br />
HEP B · 36<br />
I<br />
immunization checklist · 56<br />
interpreter services policy · 22<br />
L<br />
loose charting · 46<br />
M<br />
medical records · 42<br />
Midterm Letter · 15<br />
minors · 47<br />
mission<br />
Bastyr Center for Natural Health · 3<br />
Bastyr University · 3<br />
N<br />
needle policy · 26<br />
P<br />
parking · 51<br />
patient referrals<br />
intraclinic · 24<br />
to outside providers · 24<br />
R<br />
records release · 45<br />
records request from another provider · 45<br />
S<br />
sanctions · 14<br />
scheduling · 7<br />
specialty shifts · 7<br />
scope of practice · 5<br />
sentinel event · 28<br />
superbill instructions · 21<br />
T<br />
TB screening · 36<br />
telephone contact policy · 51<br />
time management · 17<br />
timesheets · 14<br />
71
CLINIC PHONE DIRECTORY<br />
Bastyr Center for Natural Health………………………………………………..…………..206-834-4<strong>10</strong>0<br />
CHM Dispensary……………………….…....………………………..…....…………………...…….4169<br />
Dispensary …….…………………....…………….…………………..…....…………………...…….4114<br />
In-house Lab …….................................................................................................................................5382<br />
PPL Lab…….........................................................................................................................................4113<br />
Business Office Help Line …………………………………………………………………………... 4183<br />
Medical Records Help Line.....………………………….......….……...…................…………...……4151<br />
Medical Questions Line (internal voicemail access only) ...…....……………..………..…………….4668<br />
ND Resident Pager (urgent calls from patients only) …….................................….…….….206-200-7067<br />
Administration:<br />
Jamey Wallace, ND, Clinic Director (Core) .............................................……………….……..….....4141<br />
Judy Colchin, Clinic Administrator & Projects Manager ………………................….………..……..4118<br />
Anita Blair, Clinic Program Supervisor ……...........…...........……………………………………..…4119<br />
Claudia Starkey, Faculty Administrative Assistant ..............................................................................4139<br />
Kathie Golden, ND, Product Review Coordinator …….............….….……………….………….…. 4156<br />
Marci Wedel, Finance & Clinic Senior Accountant ..........……………..….……....4150 or 425-602-3377<br />
Gary Garcia, MD, Director of Graduate and Community Medicine.….............…..........…………….4124<br />
Martha Diehl, Placement/Preceptor Coordinator……………............….…………....………………..4<strong>10</strong>3<br />
Melissa McCarty, ND Off-Site Coordinator.....……………...........….....…………………….………4<strong>10</strong>4<br />
Seth McOmber, Marketing Communications Coordinator... ...........…….....…………..……………..4163<br />
Ginny (Virginia) Norman, Medical Assistant………….………………..................…..……………...4111<br />
Clinic Safety:<br />
Will Wilson, Clinic Safety Officer ………………………………...………………………. 206-617-9455<br />
Sandi Cassidy, Compliance Officer (HIPPA) ………………………………………………………...4164<br />
Daniel Clark, Safety Director ……………………………………………………………….425-602-3064<br />
Debra Brammer, ND, Blood Borne Pathogen Officer (BBP)……………………………….206-422-8763<br />
Clinic Facilities:<br />
Will Wilson, Clinic Facilities Manager.………………..………...................…..…………………….4157<br />
Norm Chambers, Clinic Facilities Technician II …...................…………..………………………….41<strong>10</strong><br />
Rosemary Saldaña, Clinic Facilities Technician II.............…………..……………………...……….4130<br />
72
Patient Services:<br />
Martin Imbach, Manager.…..................................................................….…………………………...4142<br />
Medical Records & Billing Office:<br />
Sandi Cassidy, Manager……………………………………….………........…….....….......................4164<br />
Medical Records Helpline………….………………………………………………………………….4151<br />
Robyn Tannous, Insurance A/R Specialist ...........................................................................................4186<br />
Rebecca Million, Collections Specialist ……....................…….....………………..…………………4165<br />
Sharon Ruffin, Billing and A/R Specialist …........................…….…………….…...………………..4126<br />
Helen Jones, Credentialing Coordinator …...................…………………..….……………………….4177<br />
Business Help Line …………………………….….............. …………………………...……………4183<br />
Chinese Herbal Dispensary:<br />
Allen Sayigh, LAc, Dispensary Manager..…........................................................................................4121<br />
Matt Ferguson, Dispensary Coordinator ……………………………………………………………...4169<br />
Dispensary Assistants:<br />
Renata Chung, LAc…..…………..........………………………………………………..……………..4169<br />
Sean Seery, LAc………………….................…………………………………………...…………….4169<br />
Lisa Nicodemus, LAc ....................…….…..…………………………………………………..……..4169<br />
Dispensary:<br />
Ann Busch, Dispensary Manager ………........................………………………………….................4145<br />
Barbara Nims, Dispensary Supervisor..………………………………………………........................5848<br />
Lead Dispensary Assistants:<br />
Michelle Seligman….….................……………………………………………….…………………..5513<br />
Kristin Ishibashi ……….…....................………………………………..………...…..………………5160<br />
Dispensary Assistants:<br />
Jennifer Kemnitz……………….........………………...………………………………………………5130<br />
Haydn Engelke .................................................................................................................. …………...4114<br />
Erika Boynton ………….…....................……………………………………………………………..5137<br />
Gillian Mamacos………..................…………………………………………….....………………….5767<br />
Karl Morrison ……………………………………………………………………………………….5538<br />
73
AOM Clinical Faculty:<br />
Terry Courtney, LAc, Dean Acupuncture and Oriental Medicine (Core)……...............……………..4162<br />
Steve Given, DAOM, LAc, Associate Dean for AOM Clinical Education (Core)...…........................4179<br />
Benjamin (Boonchai) Apichai, LAc (Adjunct)………..……….................…………………………..5704<br />
Sara Bayer, LAc (Adjunct)……………....................……………….………………………………...52<strong>10</strong><br />
Qiang Cao, LAc (Core)……………...........…………..……………………………………………….4197<br />
Wei Yi Ding, LAc (Core)…………….........................……………………………………………….5535<br />
James Dowling, LAc (Adjunct)……….............………….…………………………………………...5826<br />
Angela Hughes, LAc, (Adjunct) ….................………………………………………………………..5156<br />
Susan Kaetz, LAc (Adjunct)……….......................…………………………………………………...5211<br />
Chongyun Liu, LAc (Core)……......................……………….……………………………………….4196<br />
Yuan Ming Lu, LAc (Adjunct)……….....................………………………………………………….5567<br />
Kathleen Lumiere, DAOM, LAc (Adjunct)...............……………..……………………......................5<strong>10</strong>4<br />
Rosey (Xin Dong) Ma, LAc (Adjunct)….......................……..……………………………………….5116<br />
Eric Martin, LAc (Adjunct) …………………………….………………………….............................4122<br />
Andrew McIntyre, LAc (Core)…………………..........…..…………………………………………..4125<br />
Kyo (Richard) Mitchell, DAOM, LAc (Core)…................…………………………………………...4176<br />
Hazel Philp, ND, LAc (Adjunct) ..........................................................................................................5<strong>10</strong>3<br />
Shad Reinstein, LAc (Adjunct)………………….....……..…………………………………………...5152<br />
Lee Hullender Rubin, DAOM, LAc (Adjunct) ……………………………………………………….5112<br />
Allen Sayigh, LAc, (Adjunct) ........................................................... ...…............................................4121<br />
Angela Tseng, DAOM, LAc (Core)……..................…………….....………………………………...5214<br />
Ying Wang, LAc (Core)……….................…………...…………………….………………………...4122<br />
Sue Yang-Eng, DAOM, LAc (Core) …….............………....…...……………..…………..…………4192<br />
AOM Residents:<br />
Hong Yu, DAOM, LAc 2 nd year....................................................................... ………...…………….4146<br />
74
ND Clinical Faculty:<br />
Sarah Acosta, ND (Adjunct) .................................................................................................................5218<br />
Paul Anderson, ND (Core).....................................................................................................................5152<br />
Debra Brammer, ND, Associate Clinical Dean for Clinical Education (Core)…….…………………4198<br />
Cristopher Bosted, ND (Adjunct).......................................................................................................... 5169<br />
Ryan Bradley, ND (Core) ..................................................................................................................... 5170<br />
Matt Brignall, ND (Adjunct) …………………..........……..…………………………….……………5141<br />
Kevin Connor, ND (Adjunct)……………......................………………...……..…………................ 4661<br />
Laurie Cullen, ND (Core) ………....................………….………………….………………………... 4159<br />
Tamara Cullen, ND (Adjunct)……................……………………………….……………………….. 5143<br />
Alyssa DiRienzo, ND (Adjunct)…….................…….………………….…………….……………… 5207<br />
Christian Dodge, ND (Core) ….........……...………………………………………..….......................4660<br />
Patrick Donovan, ND (Adjunct) ................................................................................... 5<strong>10</strong>6<br />
Jill Fresonke, ND (Adjunct) ………………..…................……….….…………………...…. ………. 5145<br />
Alicia Gonzalez, ND (Adjunct) ............................................................................................................ 5164<br />
Jane Guiltinan, ND, Dean and Professor, School of Naturopathic Medicine ……...4<strong>10</strong>5 or 425-602-3386<br />
John Hibbs, ND (Core)…………...........………………………………..………….…..…………….. 4158<br />
Eric Jones, ND (Core)…………………..………..............…………………………..………………. 4129<br />
David Kiefer, MD (Adjunct) ................................................................................................................ 4666<br />
Mark Lamden, ND (Adjunct)………....................………..……………….………………...425-823-6163<br />
Richard Mann, ND (Core) ………….............…………………….………….………………………. 4135<br />
Masahiro Takakura, ND, LAc (Core) ....................................................................................425-602-3293<br />
Nancy Mercer, ND (Adjunct) …….......………….……….……………………………….................. 5204<br />
Steve Milkis, ND (Adjunct) ……….......………….…….………….………………………………… 4148<br />
Jana Nalbandian, ND, Chair of Clinical Sciences (Core) …................……….……..……………….. 4170<br />
Dean Neary, ND, Physical Medicine Chair (Core) …..……................….…………………………… 5183<br />
Andrew Parkinson, ND (Core)……….….…...........…………………………………………………. 4123<br />
Hazel Philp, ND, LAc (Adjunct) .......................................................................................................... 5<strong>10</strong>3<br />
Katie Shaff, ND (Adjunct)……….....………...........………..…………………………...…………… 5<strong>10</strong>9<br />
Nancy Welliver, ND (Adjunct) ……..............………………………….…………………..………… 5182<br />
Phoebe Yin, ND (Core) ………………............……………………………………………………… 4153<br />
75
ND Residents:<br />
Jessica Bean, ND 1st year ……..…………...............………..............…………………………… 4168<br />
Amanda Heep, ND, LAc 1st year ……...…..………………..……………………....................... 4<strong>10</strong>8<br />
Miranda Marti, ND, LAc 1st year.......................................................................................................... 4143<br />
Kelly Moyaert, ND 1st year………….............………………………………………………… 4112<br />
Brendan Smith, ND 1st year.....…………….............…….………………………………………… 4172<br />
Bill Walter, ND 1st year ………......................…………………………......……………………….. 4187<br />
Kimberly Sandstrom, ND 2nd year........................................................................................... 4174<br />
Brandy Webb, ND 2nd year ……..................………..…….........………...……...………............. 4128<br />
Nutrition Clinical Faculty:<br />
Kelly Morrow, MS, RD, Clinic Nutrition Coordinator (Core) …...............……...…….…………….. 4133<br />
Doris Piccinin, MS, RD (Core) ............................................................................................................. 5<strong>10</strong>8<br />
Michelle Babb, MS, RD, (Adjunct) ………..............……………………………................................ 5113<br />
Heather King, MS, RD (adjunct) ………..............……………………………....................................5115<br />
Psychology Clinical Faculty:<br />
Eliza Carlson, RD, MS …………………………………………………………………….………… 5705<br />
Christy Hofsess, PhD (Core)................................................................................................................. 5138<br />
Dan Rosen, PhD (Core)...........................................................................................................425-602-3255<br />
Brad Lichtenstein, ND (Core)…......................………………...……..…. .…….………………...…..5198<br />
Aaron Strong, MA …………………………………………………………………………………… 5181<br />
76