FINAL ND Module 09-10.pdf - AaronsWorld.com
FINAL ND Module 09-10.pdf - AaronsWorld.com
FINAL ND Module 09-10.pdf - AaronsWorld.com
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
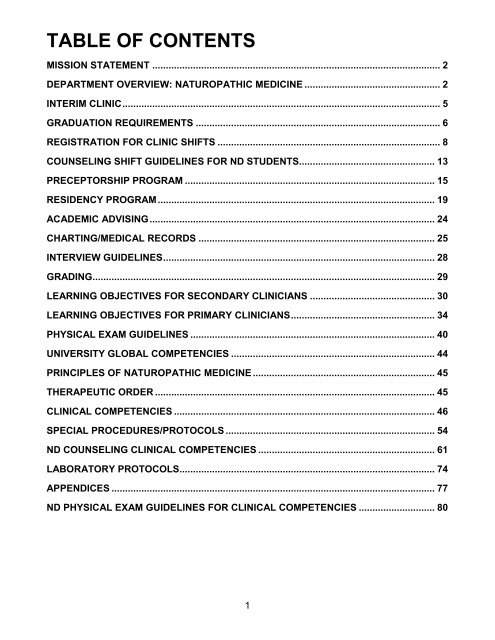
TABLE OF CONTENTS<br />
MISSION STATEMENT .......................................................................................................... 2<br />
DEPARTMENT OVERVIEW: NATUROPATHIC MEDICINE .................................................. 2<br />
INTERIM CLINIC..................................................................................................................... 5<br />
GRADUATION REQUIREMENTS .......................................................................................... 6<br />
REGISTRATION FOR CLINIC SHIFTS .................................................................................. 8<br />
COUNSELING SHIFT GUIDELINES FOR <strong>ND</strong> STUDENTS.................................................. 13<br />
PRECEPTORSHIP PROGRAM ............................................................................................ 15<br />
RESIDENCY PROGRAM...................................................................................................... 19<br />
ACADEMIC ADVISING......................................................................................................... 24<br />
CHARTING/MEDICAL RECORDS ....................................................................................... 25<br />
INTERVIEW GUIDELINES.................................................................................................... 28<br />
GRADING.............................................................................................................................. 29<br />
LEARNING OBJECTIVES FOR SECO<strong>ND</strong>ARY CLINICIANS .............................................. 30<br />
LEARNING OBJECTIVES FOR PRIMARY CLINICIANS..................................................... 34<br />
PHYSICAL EXAM GUIDELINES .......................................................................................... 40<br />
UNIVERSITY GLOBAL COMPETENCIES ........................................................................... 44<br />
PRINCIPLES OF NATUROPATHIC MEDICINE ................................................................... 45<br />
THERAPEUTIC ORDER ....................................................................................................... 45<br />
CLINICAL COMPETENCIES ................................................................................................ 46<br />
SPECIAL PROCEDURES/PROTOCOLS ............................................................................. 54<br />
<strong>ND</strong> COUNSELING CLINICAL COMPETENCIES ................................................................. 61<br />
LABORATORY PROTOCOLS.............................................................................................. 74<br />
APPE<strong>ND</strong>ICES ....................................................................................................................... 77<br />
<strong>ND</strong> PHYSICAL EXAM GUIDELINES FOR CLINICAL COMPETENCIES ............................ 80<br />
1
Mission Statement of the School of Naturopathic Medicine<br />
We educate future naturopathic physicians who care for the health and well-being of their <strong>com</strong>munities<br />
and advance our profession.<br />
Vision Statement of the School of Naturopathic Medicine<br />
The School of Naturopathic Medicine will be a leading academic center for inspired and scholarly<br />
learning in the cultivation of naturopathic doctors. We will ac<strong>com</strong>plish this through education, research,<br />
professional leadership, <strong>com</strong>munity and clinical services that bridge the worlds of science, nature and<br />
spirit.<br />
DEPARTMENT OVERVIEW: NATUROPATHIC MEDICINE<br />
The naturopathic clinical program provides training in general naturopathic practice for naturopathic<br />
medical students of Bastyr University. Naturopathic medical students at the Bastyr Center for Natural<br />
Health progress through their training in observing, supporting, and then managing roles. Each role<br />
assumes increasing responsibility for provision of patient care. Prior to graduation, students are able to<br />
safely, <strong>com</strong>petently, and efficiently direct all aspects of patient diagnosis, treatment and management<br />
in a general care setting. This training includes integration of philosophy into practice and treatment<br />
modalities including physical medicine, homeopathy, botanical medicine, nutrition and counseling.<br />
Emerging from naturopathic clinical training, each clinician will exemplify the integration of<br />
traditional naturopathic philosophy and principles of healing with conventional medical knowledge<br />
and skills. At the core of this integration is the self-reflective approach to life-long learning that allows<br />
clinicians to provide the highest quality of care.<br />
2
PROCEDURAL SECTION<br />
3
CLINICAL REQUIREMENTS<br />
ATTE<strong>ND</strong>ANCE REQUIREMENTS<br />
Student clinicians are required to attend at least 80 percent of each assigned quarterly shift in order to<br />
receive a grade of achieved <strong>com</strong>petency for the quarterly shift. Exceptional circumstances resulting in<br />
additional absence for educational purposes may be approved at the discretion of the supervisor.<br />
The supervisor is not required to grant exception to the policy, and will determine permission based on<br />
student participation and performance on the shift. The hours for ALL absences must be made up.<br />
Holidays and emergency closures do not count against the total quarter’s attendance, but the<br />
missed hours must still be made up. A student must demonstrate <strong>com</strong>petence in their weekly<br />
performance in order to obtain a passing grade. A student missing more than the number of approved<br />
absences for the quarterly weekly shifts will receive a grade of failure for the quarter. A grade of<br />
failure for a quarterly shift means the student will lose all hours and patient contacts for that shift, and<br />
the entire quarterly shift will need to be repeated. Please note that 100 percent of students’ required<br />
clinical hours must be <strong>com</strong>pleted before re<strong>com</strong>mendation for graduation.<br />
Students who arrive more than 30 minutes late for their assigned shift will receive a written warning<br />
for a first event and need to make up missed time. Students will receive a clinic sanction for a second<br />
event in the same quarter. (For more information, please see the sanctions section.)<br />
EXCUSED ABSENCES<br />
It is the responsibility of every student clinician to inform their assigned supervisor of any absence<br />
from the center prior to that absence. Notification of a supervisor of an absence after a daily shift has<br />
begun may result in the absence being designated an unexcused absence.<br />
For planned absences:<br />
1. Fill out the bottom portion of the form titled “absence/substitution form—student clinician.” A<br />
separate form must be <strong>com</strong>pleted for each shift you will miss. A sample of this form is included in<br />
the appendix.<br />
2. Have the supervisor sign in the appropriate space.<br />
3. Primary <strong>ND</strong> clinicians must secure a substitute to cover their shift and the substitute must sign<br />
the form as well.<br />
4. Student substitutes on counseling shifts is at the discretion of the supervisor. Students must<br />
check with the supervisor in advance of the projected absence, and the need to arrange a substitute<br />
5. Primary clinicians are also responsible for contacting the patients who are <strong>com</strong>ing in specifically<br />
to see them. Patient phone numbers can be obtained by requesting the patient’s chart. If the phone<br />
number listed is incorrect, clinicians may check with the front desk for phone numbers listed in the<br />
<strong>com</strong>puter. Ask patients to contact the front desk if they wish to reschedule their appointments.<br />
Primary clinicians must also notify the secondary/observation clinicians of their absence.<br />
6. Secondary/observation clinicians must also secure a substitute to cover shifts, if possible, and the<br />
substitute must sign the form. In addition, secondary clinicians must notify the primary student<br />
clinician on their shift of their absence.<br />
7. Once the form is <strong>com</strong>pleted, submit it to the faculty administrative assistant in S206. The form<br />
will be retained through the quarter for future reference. Students should provide an email or<br />
written copy of the absence form to their substitute clinician before turning in the form.<br />
8. Students who are unable to attend their scheduled shifts during the first week of a quarter must<br />
<strong>com</strong>plete and turn in a form prior to the date of the absence. A student will automatically be given<br />
a grade of failure and dropped from the shift if no arrangements are made with the supervisor by<br />
the second week of the quarter.<br />
4
UNEXCUSED ABSENCES<br />
An unexcused absence occurs when a student fails to notify the shift supervisor of their absence prior<br />
to the start of the shift. This includes the circumstance of a substitute clinician who signs to cover a<br />
shift and does not show up for the shift.<br />
The first unexcused absence during a term will result in the student clinician being required to<br />
<strong>com</strong>plete makeup hours for the missed shift (4 hours) with the additional sanction of a penalty of two<br />
makeup shifts (8 hours) for a total of 12 hours.<br />
A second unexcused absence will result in an F grade for the quarter shift and the loss of all hours and<br />
contacts earned during the quarter. If the absent student is a substitute clinician, they may be<br />
subject to a higher hourly penalty for not showing up for the shift.<br />
Supervising clinical faculty members may, at their discretion, accept notification of an absence after<br />
the start of the clinic shift in the event of an emergency. The student will need to provide<br />
documentation. Even if the student calls the supervising clinical faculty member immediately prior to<br />
the missed shift, the supervisor reserves the right to define the missed shift as unexcused absence and<br />
assign sanctions.<br />
Midwifery students must have a substitute available on an “immediate-notice” basis for all shifts<br />
missed due to their attendance at a birth. Sanctions will be assigned for any shifts missed for a birth<br />
without appropriate back-up in place.<br />
INCLEMENT WEATHER POLICY-See global handbook<br />
INTERIM CLINIC<br />
Interim clinic is the time during which the clinic operates and no academic courses are offered.<br />
Students will be responsible for interim clinic shifts during the same days/times they were scheduled<br />
for shifts during the preceding quarter. Absence requests must be approved by the student’s supervisor<br />
and submitted two weeks prior to the start of the interim period. Interim clinic occurs at the end of each<br />
quarter, allowing the center to provide on-going care to patients during academic breaks.<br />
Students are RESPONSIBLE FOR SHIFT COVERAGE for their interim shifts and are<br />
required to find substitutes as indicated in the attendance policy.<br />
<strong>ND</strong> interim clinic requirements for graduation:<br />
Credits: 2 Hours: 44<br />
Hours are to be <strong>com</strong>pleted over the course of all weeks of interim clinic. The last opportunity that<br />
June graduates have for obtaining interim clinic hours is at the end of winter quarter, during<br />
spring break.<br />
Note: Students are automatically registered for interim clinic credits (2) during the spring quarter of<br />
their fourth year. This will appear on the registration form as interim patient care.<br />
Interim clinic is currently offered during the following times:<br />
• Winter break, between fall and winter quarter, for 2-3 weeks<br />
• Spring break, between winter and spring quarter, for 1 week<br />
Interim clinic time sheets are tracked on a separate form than regular patient care hours. Patients seen<br />
during interim clinic on patient care shifts are counted in the summary total of patient contacts.<br />
Students should use the “patient summary” form to keep a record of the patient contacts.<br />
Additional interim hours (above 44) can be used to make up shift hour deficits from current or past<br />
quarters. These hours should be tracked on the interim shift form, and patient contacts on the summary<br />
of patient contacts form. At the end of each interim clinic period, all paperwork must be turned in to<br />
the clinic registration staff to receive credit for the work performed. Hours above the required 44 will<br />
automatically be added to your sub and extra hour’s bank.<br />
Any unexcused absence during interim clinic will result in the assignment of sanctions, to include a<br />
requirement to make up the four hours missed plus an additional 8 hours of clinic shifts for each<br />
missed shift for a total of 12 hours. These hours are in addition to the required interim hours for<br />
each program.<br />
5
<strong>ND</strong>/AOM dual-track students need to <strong>com</strong>plete 44 hours of <strong>ND</strong> interim clinic and 36 hours of AOM<br />
interim clinic.<br />
PLEASE NOTE: Due to calendar changes, interim weeks are subject to change without notice.<br />
Please be advised of this possibility.<br />
GRADUATION REQUIREMENTS<br />
Before graduation, students must:<br />
•Have all clinical <strong>com</strong>petencies <strong>com</strong>pleted and documented. Students will not graduate until all<br />
requirements have been met and the clinical faculty has re<strong>com</strong>mended the student for graduation.<br />
•Complete all clinical hours, all patient contact requirements, and submit all required paperwork.<br />
•Pass a standardized “clinic exit examination” or OSCE. This exam will be offered before spring<br />
quarter during a student’s final year in clinic. Students will be given the opportunity to remediate<br />
this exam one time if they fail to pass. If they fail the exam a second time, the student will be<br />
referred to the student progress <strong>com</strong>mittee. The exam is offered once a year at a designated time<br />
between clinical quarters or during winter quarter. The student must participate in the exam at this<br />
time in order to graduate.<br />
The following is a summary of specific requirements that need to be met in order to graduate and be<br />
eligible to take board examination:<br />
SUMMARY:<br />
Total number of shifts: 21 clinic shifts<br />
Total number of hours: 1,224.5 (includes patient care, 132 hours preceptor, and interim clinic)<br />
Total number of patient contacts: 350<br />
Pass OSCE Exam: 1<br />
GRADUATION ROTATION/SHIFT REQUIREMENTS<br />
Total number of rotations/shifts:<br />
•21 clinic rotations/shifts which includes 17 general patient care and 4 Physical medicine<br />
shifts. General patient care shifts include one mandatory counseling shift. A student may<br />
include one additional counseling shift and/or up to four homeopathy shifts as long as they<br />
exhibit <strong>com</strong>petence in their general patient care shifts.<br />
•3 Clinical Laboratory Diagnosis with Labs<br />
•3 Preceptor Rotations/Shifts<br />
•44 hours of Interim patient care-currently available only during winter and spring breaks.<br />
Required for clinical laboratory diagnosis:<br />
•One lab rotation (3 quarters of lab portion of the Clinical Lab Diagnosis course)<br />
•99 hours, including class<br />
•This lab rotation occurs on campus<br />
Interim clinic requirements:<br />
•All 44 hours must be <strong>com</strong>pleted in patient care and/or physical medicine<br />
•Interim clinic is part of your quarterly shift requirement. Students must attend the same<br />
weekly shifts as scheduled the preceding quarter. Unapproved absences during interim will<br />
result in a requirement to make up the four hours missed plus an additional 8 hours of clinic<br />
shift time in addition to the interim hours requirement. A second violation results in failure of<br />
the quarterly shift with loss of all hours and contacts.<br />
• Students are required to <strong>com</strong>plete the interim hours before the spring quarter of their<br />
graduating year. There is no interim clinic between spring and summer quarter.<br />
•An AC for interim depends upon successful <strong>com</strong>pletion of all required interim hourly shifts.<br />
6
2. HOUR REQUIREMENTS<br />
Clinic Entry I and II 25.5<br />
Patient care hours 924<br />
Lab rotation 99<br />
Preceptor hours 132<br />
Interim clinic hours 44<br />
Total Hours 1,224.5<br />
3. CREDIT REQUIREMENTS<br />
Clinic entry I and II 2<br />
Patient care shifts 42<br />
Clinical lab diagnosis 9 (including class)<br />
Preceptor shifts 3<br />
Interim clinic 2<br />
4. PATIENT CONTACTS REQUIRED<br />
Total number of patient contacts: 350<br />
This includes patients seen in the 21 patient care shifts (homeopathy, counseling, physical medicine,<br />
substitute and extra hours, and interim). A minimum of 175 must be primary contacts. This does not<br />
include patient contacts gained in preceptor. This averages 16.7 patients for each shift.<br />
MEDICAL RECORDS<br />
Filing Forms in the Medical Record (Proper Placement) Patient records are divided into four<br />
sections: Front-Left; Front-Right; Back-Left; & Back-Right. Location for each form is below.<br />
Front-Left (from bottom to top)<br />
(Referrals)<br />
Authorization to Bill Third-Party Payer<br />
Acknowledgement of Receipt for Notice of Privacy Practices<br />
(Any specialty consent forms or authorization forms)<br />
Consent for Treatment<br />
Observation and Imaging Consent Form<br />
Patient Information Form (PIF)<br />
Patient Profile<br />
Pediatric/Adult Health Data Sheet<br />
Supplement and Medication List<br />
Patient Visit Summary<br />
Patient Intra-Clinic Referral Form<br />
Front-Right (Forms in this section are always filed in chronological order with most recent<br />
documentation on top. Documentation for the same DOS should be filed with progress notes on<br />
the top and copies of prescriptions, herbal formulas and treatment plans on the bottom.)<br />
Initial Consultation and Interview Form<br />
Progress Notes for FOC and ROC visits<br />
Prescriptions and Herbal Formulas (copies)<br />
Treatment Plans and Instructions (copies)<br />
(other reference information given to patient-noted by name on treatment plan)<br />
Referral Letters/Other Correspondence<br />
Diet Diaries (and other information, except outside hardcopy medical records provided by patient)<br />
Back-Left (from bottom to top)<br />
Notices of Disclosures<br />
Labs and Referred Procedures (most recent on top)<br />
Back-Right (in chronological order with most recently received information on top)<br />
7
Copies of Authorization Forms for Releases Processed<br />
Copies of authorization forms for pending in<strong>com</strong>ing record requests<br />
Outside Medical Records (copies of records received from other practitioners)<br />
REGISTRAR<br />
REGISTRATION FOR CLINIC SHIFTS - GENERAL NFORMATION<br />
1. To register for clinic shifts, students must first register with the academic registration staff.<br />
2. After viewing the faculty schedule, all students will submit to clinic registration staff their<br />
requests for supervisors and shift times for the up<strong>com</strong>ing year before the registration deadline.<br />
These requests must align with the student’s assigned academic track and course schedule.<br />
3. The clinic registration staff coordinates registration for clinic shifts. They attempt to meet<br />
students’ requests when scheduling shifts but this cannot be guaranteed.<br />
4. Student clinician pairings are subject to final approval of the program and associate dean(s).<br />
5. The <strong>com</strong>pleted schedule is approved by the clinic associate dean for naturopathic medicine.<br />
Changes to the student's schedule after the registration date will only be allowed documented<br />
family or medical emergencies. Documentation is required.<br />
6. No student in any program may have more than two shifts in one day. Shift times may not<br />
overlap with other shifts or courses. An adequate amount of time must be maintained for travel<br />
between the clinic, campus and external site locations.<br />
7. It is important to note that the assigned academic track for students and assigned clinic shifts<br />
for all students are not amenable to changes necessitated by other considerations such as outside<br />
employment schedules, child care schedules, etc. It is, therefore, incumbent upon every student to<br />
make whatever arrangements are necessary in order to ac<strong>com</strong>modate his or her assigned academic<br />
and clinic schedules.<br />
8. Students may only withdraw from the clinic if they have a verifiable emergency. They must<br />
obtain a letter signed by the program dean or their designate approving this withdrawal.<br />
9. Information on interim clinic registration is in the interim clinic section of this handbook.<br />
10. Students may register for clinic elective shifts or observation shifts in other programs, on a<br />
space available basis.<br />
ADDITIONAL INFORMATION FOR <strong>ND</strong> REGISTRATION<br />
The goal is to have a primary and secondary student clinician in each room in general patient care,<br />
homeopathy and counseling; and to have three to four primary and three to four secondary student<br />
clinicians on each physical medicine shift. There may be co-primary clinicians assigned together.<br />
Note: Co-primary designation does not imply that both clinicians function in the role of primary for<br />
each patient. Students may never share primary patient contacts. Co-primaries alternate taking the role<br />
of primary and secondary clinicians.<br />
Students will have the opportunity to add elective shifts, trade <strong>com</strong>parable shifts with fellow clinicians,<br />
or drop shifts with a financial penalty, after the initial shift assignment process is <strong>com</strong>pleted. More<br />
information is distributed by the registrar’s office prior to the shift change period.<br />
In general, each <strong>ND</strong> student will be registered for a minimum of two shifts and a maximum of four<br />
shifts per quarter. The only exception to this rule is <strong>ND</strong> students in their first year at the clinic. They<br />
will have one to two shifts per quarter, with a maximum of six total shifts in that year. Each <strong>ND</strong><br />
student will be registered for at least one patient care shift per quarter, which could include one<br />
counseling shift during that year. It is highly re<strong>com</strong>mended that students have at least two shifts in<br />
general patient care before shifting into the primary role.<br />
Primary student clinicians who are also on-call as midwifery interns must be paired with a co-primary<br />
on all <strong>ND</strong> shifts or have a back-up on immediate call. The co-primary must be informed in advance<br />
and accept the responsibility for last minute coverage if the midwifery intern is called out on a birth<br />
before the midwifery student will be allowed an approved absence for the birth.<br />
8
APPOINTMENTS WITH THE CLINIC REGISTRATION STAFF<br />
At least one advising session is required with the clinic registration staff before graduation. It is<br />
re<strong>com</strong>mended that students meet with the clinic registration staff near the beginning of their clinical<br />
experience in order to clarify and understand the clinic education requirements, and to understand how<br />
their progress is tracked each quarter. Each quarter the clinic registration office will provide all<br />
students with a summary of their <strong>com</strong>pleted requirements. It is the student’s responsibility to check<br />
the summary for accuracy on a quarterly basis. Additional advising sessions are re<strong>com</strong>mended in<br />
order to stay current with <strong>com</strong>pleted and remaining outstanding requirements. Graduating students<br />
are required to meet with the clinic registration staff early in their last year to verify they are on<br />
track for graduation.<br />
Homeopathy:<br />
•Up to 4 general patient care shifts may be taken in homeopathy.<br />
•Homeopathy may also be taken as elective audit shifts and shift requirements must be<br />
followed elective or audit shifts. Additional shifts must be approved by the homeopathy chair.<br />
•Prerequisites must be <strong>com</strong>pleted prior to entering a homeopathy shift. Homeopathy classes<br />
1-3 are required prerequisites, and Homeopathy 4 is highly re<strong>com</strong>mended.<br />
•All students who are registered for a homeopathy shift are required to be registered and<br />
participate in Homeopathy Grand Rounds. Other students may enroll in Grand Rounds with<br />
approval of the instructor. Grand Rounds hours do not count as clinical patient care hours.<br />
Physical Medicine Requirements:<br />
•Students must take two physical medicine shifts each year for two clinical years, for a total<br />
of 4 shifts. (see additional shift request info below)<br />
•Only one physical medicine shift should be taken in any quarter.<br />
Registration Requirements by Quarter:<br />
Students must be registered for a minimum of one shift, and a maximum of four shifts, in any quarter<br />
in which they are clinic eligible and enrolled at Bastyr University. Students in their first year of clinic<br />
are allowed to take only six shifts in that year. For an outline of shift assignment per quarter see the<br />
shift requirement chart following. At least one of the assigned quarterly clinic shifts must be a patient<br />
care shift. Students may not be registered for more than two shifts in one day. Students wishing to take<br />
more than four shifts per quarter must submit a written request to the clinical associate dean prior to<br />
registration. Failure to follow re<strong>com</strong>mended shift registration will delay graduation date.<br />
Registration in Additional Shifts:<br />
Students wishing to take additional shifts beyond the maximum number (homeopathy, counseling,<br />
patient care or physical medicine) must submit requests to the clinic registrar and clinical associate<br />
dean at least one month in advance of registration.<br />
EXTERNAL SITE ROTATIONS/SHIFTS<br />
External site clinics fulfill clinic requirements. External sites currently include: Ballard Senior Center,<br />
Consejo Center, Country Doctor, Mary’s Place, Providence Marianwood Senior Center, 45 th St.<br />
Homeless Youth Clinic, Cascade Natural Medicine, West Seattle Teen Clinic, Shoreline Senior Center,<br />
Snohomish Valley Senior Center, Carolyn Downs Clinic and YWCA Women’s Wellness Center.<br />
These sites may change from time to time as the external site program is expanded or modified.<br />
Students are required to take at least one external clinic shift during their clinical training. Clinical<br />
faculty reserve the right to restrict the number of external shifts in which a student participates, if<br />
student progress is in question.<br />
9
CLINIC AUDIT OR ELECTIVE SHIFTS<br />
If positions are available, students may take additional clinic shifts as clinical elective or as elective<br />
audit shifts. The clinic registrar should be contacted for information regarding the availability of these<br />
shifts. If you take the shift for elective credit, then the first 36 hours of the shift go towards fulfilling<br />
the elective requirement and may not be used as sub hours. You must <strong>com</strong>plete 36 hours to get an AC<br />
for the shift/class. Any hours over 36 may be used as sub hours. Shifts taken as an elective audit do<br />
not qualify for financial aid but all hours may be used as sub hours. Students are held to the same<br />
standards in attendance and performance as all other shifts.<br />
SHIFT REQUIREMENTS – QUARTERLY BREAKDOWN<br />
For 4-year track and 5-year track option A:<br />
Year/Quarter<br />
Number of Clinic Shifts<br />
Year 3 of 4 or Year 4 of 5:<br />
Summer 1 or 2<br />
Fall 1 or 2<br />
Winter 1 or 2<br />
Spring 1 or 2<br />
Note: no more than 6 shifts total in the first year of any <strong>ND</strong> track<br />
Year 4 of 4 or Year 5 of 5:<br />
Summer 3-4<br />
Fall 3-4<br />
Winter 3-4<br />
Spring 3-4<br />
For 5-year track, option B: You may choose to begin clinic in summer quarter. This is<br />
re<strong>com</strong>mended for dual track students in Acupuncture or midwifery. If you begin clinic in the fall, you<br />
will be<strong>com</strong>e a primary the following year in the fall.<br />
Year/Quarter<br />
Number of Clinic Shifts<br />
Year 3 of 5:<br />
Summer 0<br />
Fall 1-2<br />
Winter 1-2<br />
Spring 1-2<br />
Note: no more than 6 shifts total in the first year of any <strong>ND</strong> track<br />
Year 4 of 5:<br />
Summer 1-2<br />
Fall 1-2<br />
Winter 1-2<br />
Spring 1-2<br />
Year 5 of 5:<br />
Summer 3-4<br />
Fall 2-3<br />
Winter 2-3<br />
Spring 2-3<br />
10
MIDWIFERY<br />
All midwifery student clinicians who are also on-call as midwifery interns must be paired with a coprimary<br />
on all <strong>ND</strong> shifts. The co-primary must be informed in advance and accept the responsibility<br />
for last minute coverage if the midwifery intern is called out on a birth. If no co-primary is assigned,<br />
the student must have student back up for immediate on-call coverage of their clinical shifts. Only two<br />
daily clinic shifts per quarter may be missed on a quarterly shift. The supervisor has the right to<br />
authorize a third excused absence if individual circumstances warrant that absence. The supervisor is<br />
not obligated to authorize a third absence from a quarterly shift.<br />
If a midwifery student does not have substitution coverage and misses a shift to fulfill duties in the<br />
midwifery program, the hours missed will be counted as an unexcused absence and the student will<br />
incur all sanctions noted in the attendance section of this book. In addition, the chair of the midwifery<br />
department will be notified, and further sanctions may occur in that department.<br />
Midwifery students may use documented hours obtained in the clinical pre-and post-partum exam care<br />
of their birthing clients as sub and extra hours to cover their clinic absences due to births. As these<br />
hours are not used in the midwifery department for credit, this policy does not allow double credit for<br />
the work. These hours do not include birthing hours. No more than 120 hours may be used during a<br />
student’s entire clinical training. The hours must be documented and signed by the midwife preceptor.<br />
These hours must then be co-signed by the associate clinical dean and submitted to the registrar’s<br />
office. No hours will be accepted without the co-signature.<br />
Clinical Training Eligibility<br />
•Naturopathic medicine students must <strong>com</strong>plete and achieve <strong>com</strong>petency in all required Classes<br />
prior to entering clinic. This includes all classes in the 1 st and 2 nd year if on the 4-year track. It<br />
includes all classes of the first 3 years of the 5A track, and first 2 years of the 5B track. Students<br />
must be in good academic standing in order to begin the clinical training portion of the program.<br />
Questions about didactic prerequisites for clinical <strong>ND</strong> training should be addressed to the<br />
registrar’s office on campus.<br />
•Students need to <strong>com</strong>plete all pre-clinic requirements including: background check; TB test<br />
series; and other immunizations as required by elected external site clinics.<br />
•Students must <strong>com</strong>plete and achieve <strong>com</strong>petency in Clinic Entry II and in the clinic entrance<br />
exam.<br />
•All advanced standing/transfer students must meet all clinical training requirements and be in<br />
good academic standing. Advanced standing students will not be granted waivers of any clinical<br />
training credits, hours or other requirements.<br />
•Students must <strong>com</strong>plete the Medical Procedures Course or have proof of <strong>com</strong>pletion of an<br />
equivalent that includes current requirements for professional rescuer’s level CPR training.<br />
Questions about what constitutes an eligible equivalent experience should be addressed to the<br />
Associate Dean or Associate Clinical Dean by email.<br />
•A copy of the current CPR/first aid card, or written approval to substitute equivalent experience<br />
for the course, must be turned in to the clinic registration office on campus.<br />
Please note: Bastyr Center for Natural Health requires that all supervisors and student clinicians be<br />
recertified each year at the level stated above, even when the card issued by the certifying agency<br />
states that the card is valid for a period longer than a year.<br />
•Students must <strong>com</strong>plete a Washington State Patrol (WSP) criminal background check. There is<br />
no charge for this service. Forms will be distributed to all students enrolled in Clinic Entry II.<br />
Forms are also available in the registrar’s office. Questions about the WSP background check<br />
should be addressed to the registrar’s office on campus.<br />
•TB screening and hepatitis immunization forms/waivers will be distributed during the<br />
Physical/Clinical Diagnosis 3 Lab course or in CE II. Students must have <strong>com</strong>pleted TB screening.<br />
You must have received the immunization series or signed a waiver for hepatitis B immunization.<br />
11
Questions regarding TB screening and hepatitis immunization should be directed to the Associate<br />
Clinical Dean at BCNH.<br />
•A signed clinic contract (appendix 1 of the Student Clinician Handbook global module) must be<br />
turned in to your Clinic Entry II instructor.<br />
•All <strong>ND</strong> students must <strong>com</strong>plete 20 hours of preceptor observation experience prior to the start<br />
of their first quarter in the clinic. Preceptor packets with full instructions are available from the<br />
preceptor coordinator’s office at the BCNH, or the wall display outside of the registrar’s office on<br />
campus. Questions about Preceptor shifts should be addressed to the preceptor coordinator at the<br />
clinic.<br />
•All <strong>ND</strong> students must be enrolled in at least one patient care shift during all quarters in which<br />
they are clinic eligible through graduation unless they are on a leave of absence. Exceptions to this<br />
quarterly clinic attendance requirement are reserved for extenuating circumstances. Students who<br />
do not register for clinic every quarter will delay the date of their graduation.<br />
To apply for a leave of absence from the university, contact the registrar’s office.<br />
Clinic registration forms will be placed in the main campus student mailboxes of all students eligible to<br />
enter clinic. The forms must be turned in to the registrar’s office by the deadline listed on the form. If<br />
you are clinic eligible and do not receive a clinic registration form, contact the clinic registration office<br />
immediately.<br />
CLINIC ENTRY COURSES<br />
<strong>ND</strong> CLINIC ENTRY I<br />
This course is registered and paid for the first quarter of the first year of the four- and five-year track<br />
and is to be <strong>com</strong>pleted by the end of spring quarter of the first year.<br />
Credits: 1.0<br />
Hours: 14.5<br />
Course Objectives:<br />
•To provide students with a well-rounded experience as a patient at Bastyr Center for<br />
Natural Health. This course is designed as an experiential class. Students may choose not to<br />
receive the re<strong>com</strong>mended treatment. A student may choose to have a wellness program<br />
designed if they have no specific health concerns.<br />
•To provide students with experience in the medicine they are studying.<br />
•To prepare students for Clinic Entry II, the next prerequisite for entry into the clinic after<br />
achieving <strong>com</strong>petency in CE 1.<br />
•To expose students to basic medical terminology.<br />
Course Requirements:<br />
Attendance at all class meetings: one per quarter and one finals week of the last quarter: 4.0 hr<br />
•First office call: 1.5 hr<br />
•Return office call: 1.0 h<br />
•A return office call in any clinic department: 2.0 hr<br />
•3 counseling sessions at the campus student counseling center: 3.0 hr<br />
•3 case previews: 1.5 hr<br />
•3 case reviews: 1.5 hr<br />
Each student is required to write several short evaluative papers discussing their clinic experience.<br />
These papers are to be turned in to the CE I instructor at the class meetings.<br />
Students will receive a CE I tracking sheet to record the requirements as they are met. It needs to be<br />
initialed and dated at each visit.<br />
The class will meet with the instructor at the end of spring quarter for a final discussion group. Course<br />
tracking sheets and clinic evaluation papers are at this time.<br />
12
<strong>ND</strong> CLINIC ENTRY II<br />
Prerequisites:<br />
•<strong>ND</strong> Clinic Entry I<br />
•All students must have <strong>com</strong>pleted the entire body of course work through the winter quarter<br />
when they be<strong>com</strong>e clinic eligible to enroll in Clinic Entry II.<br />
Credits: 1.0<br />
Hours: 3 hrs/week x 3 weeks; 9 hrs + 2 hr exam = 11 total hours<br />
Required Text: Student Clinician Handbook, Global and <strong>ND</strong> modules<br />
Course Objectives:<br />
•Students will gain a broader understanding of naturopathic medicine as it relates to clinical<br />
practice.<br />
•Students will gain a perspective on clinic purpose, administration and function at BCNH.<br />
•The role of the student clinician will be clearly defined.<br />
•Students will be introduced to skills that will allow them to be<strong>com</strong>e familiar with case<br />
management and charting, as performed at Bastyr Center for Natural Health.<br />
•Students will know the role of each person in the clinic structure.<br />
•Students will learn the clinic policies, procedures, and clinical education requirements.<br />
•Students will be exposed to the ethical and moral issues of medicine and clinical practice<br />
and how these issues relate to the clinical experience.<br />
•Students are encouraged to develop and broaden their own personal philosophy of<br />
naturopathic medicine.<br />
Students will be required to pass a clinic entrance practical exam in order to receive an AC in Clinic<br />
Entry II. This exam is structured to allow the student to demonstrate <strong>com</strong>petence in physical exam,<br />
differential diagnosis, laboratory diagnosing, charting, and <strong>com</strong>munication skills.<br />
Students must receive a grade of achieved <strong>com</strong>petency in CE II in order to enter the clinic.<br />
Students must purchase required medical equipment for use in their clinical education.<br />
COUNSELING REQUIREMENTS<br />
COUNSELING SHIFT GUIDELINES FOR <strong>ND</strong> STUDENTS<br />
Absences: Clinic attendance policies must be followed on all counseling shifts. Students must<br />
<strong>com</strong>plete a Student Clinician Absence/Substitute Form when they will miss a shift. (See counseling<br />
substitute policy below) All missed counseling shift hours must be made up to receive credit. Students<br />
are encouraged to make up these hours on a counseling shift, but hours can be made up on any regular<br />
clinic shift. The requirement for student substitutes on counseling shifts is at the discretion of the<br />
supervisor. Substitutes may be necessary if two or more other students from the same shift have<br />
already obtained permission to be absent for the same day. Students must check with the supervisor in<br />
advance for approval of the projected absence, and the potential need to arrange for a substitute<br />
External Counseling Shifts: When available, these shifts can be elected by student clinicians who<br />
have finished their first counseling shift at BCNH.<br />
Interim Shifts: Interim counseling shifts are required for those clinicians currently on a counseling<br />
shift. They are also available to those needing to make up any previous counseling absences.<br />
Second Shift Requests: Students wishing to take a second shift may do so depending upon the<br />
availability of openings. Students should sign up through the registrar’s office. Counseling Shift<br />
Assignments: Students will be randomly assigned a counseling shift, during their first clinical year,<br />
and must take the shift during the quarter assigned.<br />
Interaction Between BCNH and Student Counseling Center on Campus: Students as clients<br />
should have the choice of seeing a counselor at either the Student Counseling Center on Campus or at<br />
BCNH, but not both.<br />
13
Students cannot receive counseling from their current clinical supervisors.<br />
Neither staff nor student trainees are allowed to self-refer to their private practices. Referrals may be<br />
made to other clinicians in the <strong>com</strong>munity.<br />
PRECEPTORSHIP<br />
Advanced Preceptor Shift in Lieu of Patient Care Shift<br />
A student may request an advanced preceptor shift in place of a regularly scheduled patient care shift if<br />
they have met the requirements below:<br />
• All 132 hours (3 credits) of the required preceptor hours must be <strong>com</strong>pleted, submitted and on<br />
the student transcript.<br />
• Eleven patient care shifts must be <strong>com</strong>pleted with a grade of achieved <strong>com</strong>petency for each.<br />
Physical medicine shifts cannot be included in this count.<br />
• The student must be in good academic standing<br />
• The site must be pre-approved through the preceptor coordinator.<br />
• The site must offer hands-on patient care experience that is <strong>com</strong>parable to what would be<br />
obtained in the Bastyr Natural Health Clinic.<br />
The site must provide evaluation on standard clinic evaluation forms.<br />
All student requests for advanced preceptor shifts must be typewritten and submitted to the Associate<br />
Clinical Dean. Email submission is acceptable. The request must include:<br />
• Your purpose in requesting the shift that defines the skills or knowledge you will obtain at the<br />
designated site.<br />
• Information stating that all requirements listed above are met.<br />
• The name, address and contact information of the external clinic site and supervising clinician<br />
or program manager.<br />
• The number of hours to be <strong>com</strong>pleted. Each shift must be equivalent to 44 hours.<br />
• Each advanced preceptor shift must be requested independently.<br />
• A maximum of two shifts is allowed. They may be taken at one facility and with one<br />
supervisor or at two sites with two supervisors.<br />
• A letter from the supervising physician that outlines the nature and extent of hands-on<br />
experience and skills the student will obtain. It should also outline the number of contact hours,<br />
estimated number of patients, and a description of the active supervision and management the<br />
student will receive from the supervisor.<br />
All the above elements must be present for the site to qualify as an advanced preceptor site. The<br />
Associate Clinical Dean will review the student’s request with clinical faculty. The student will be<br />
notified of the out<strong>com</strong>e in writing or by email.<br />
If the site is approved, the associate clinical dean will notify the clinic registrar. The student will be<br />
advised and must <strong>com</strong>plete the required paperwork.<br />
All external clinic shifts must be registered and paid for as a general patient care shift (2 credits per<br />
shift/44 hours). Hours <strong>com</strong>pleted above the 44 hours cannot be used as substitution or extra hours.<br />
Students must keep careful records of the patient contacts during the external shift. The summary of<br />
patient contacts and hours form must be <strong>com</strong>pleted by the preceptor and submitted to the clinic<br />
registrar at the end of the shift for grading. The associate dean and preceptor program coordinator<br />
should be notified at the end of the shift so that a thank you note may be sent to the preceptor.<br />
14
PRECEPTOR<br />
BASTYR UNIVERSITY’S NATUROPATHIC MEDICINE PRECEPTORSHIP PROGRAM<br />
STUDENT PACKET<br />
Preceptorships provide students with the opportunity to observe established health care practitioners in<br />
their private practice or other <strong>com</strong>munity settings. These experiences offer many benefits to<br />
<strong>com</strong>plement the clinical training received on patient care shifts. By preceptoring, students are able to<br />
observe a variety of physician-patient <strong>com</strong>munication styles, therapeutic modalities and clinical<br />
conditions, as well as day-to-day business practices. Additionally, many preceptors offer advanced<br />
students hands-on experience with their patients.<br />
<strong>ND</strong> Preceptorship graduation requirements are as follows:<br />
1. A total of 132 hours (3 credits) of documented preceptorship experience.<br />
2. At least 88 preceptorship hours must be spent with an <strong>ND</strong>.<br />
3. You may have up to 44 hours credited with non-<strong>ND</strong> practitioners.<br />
4. You must precept at a minimum of 3 different sites/locations.<br />
5. A minimum of 20 hours are required at any given site.<br />
6. You may precept with more than one pre-approved preceptor at one site/location as long you<br />
earn at least 20 hours A<strong>ND</strong> you go to at least 3 different sites overall.<br />
7. You must <strong>com</strong>plete 20 hours prior to beginning clinic shifts.<br />
8. Pre-clinic training preceptorships are limited to 40 credited hours.<br />
Finding and Setting up Preceptorships:<br />
There are many practitioners who have already volunteered to be preceptors for Bastyr <strong>ND</strong> students,<br />
and students are always encouraged to develop new sites. We have <strong>ND</strong>s, MDs, chiropractors,<br />
acupuncturists, homeopaths, osteopaths, nurse practitioners and more. You may precept in the Seattle<br />
area and/or in other states, provinces and countries. You may precept during the school year and/or<br />
during official school breaks.<br />
There are different ways to learn about <strong>ND</strong> preceptorship opportunities. Many students hear about<br />
preceptors from other students, a wonderful natural referral system! You are also invited to contact the<br />
<strong>ND</strong> Preceptor Coordinator for suggestions and information about site placements as well as other aspects<br />
of the preceptorship program. There is also a Preceptor Information Site available on the Bastyr<br />
Intranet at the Center and Campus, which you can access through Internet Explorer at<br />
http://precept/. Here you can browse and search for pre-approved preceptors by different criteria,<br />
including name, credentials (e.g. <strong>ND</strong>, LAc, MD etc), specialties, location, and student class level<br />
accepted.<br />
Before contacting a preceptor, review their information page for any special requirements and<br />
opportunities, as well as the appropriate contact person for requesting a preceptorship. Keep in mind<br />
that, although approved preceptors have volunteered to precept Bastyr <strong>ND</strong> students, they are not<br />
required to accept a certain number of students. Unless noted otherwise, the student is responsible for<br />
arranging a schedule that works for both you and your preceptor. It is wise to plan ahead and be as<br />
flexible as possible with your schedule.<br />
If you know of a practitioner who you think has accepted students in the past but do not find him/her<br />
listed on the Information Site, please contact the <strong>ND</strong> Preceptor Coordinator. If you would like to suggest<br />
a new preceptor, you may either contact the <strong>ND</strong> Preceptor Coordinator or give a Preceptor Application<br />
packet directly to the prospective practitioner. Application packets are available outside the <strong>ND</strong><br />
Preceptorship office at the clinic and outside the Registrar’s office on campus. Please note that ALL<br />
NEW PRECEPTORS (practitioners) MUST BE APPROVED BEFORE YOU BEGIN YOUR PRECEPTORSHIP in<br />
order to receive credit and insure professional liability coverage. Also, please note that individual<br />
practitioners are approved as preceptors so this does not necessarily mean that all practitioners at a<br />
particular clinic/site participate in our program. If in doubt, please check with the <strong>ND</strong> Preceptor<br />
Coordinator before starting a preceptorship.<br />
Paperwork and Documentation:<br />
The Student Packet contains the following forms: <strong>ND</strong> Student’s Preceptorship Evaluation, <strong>ND</strong> Student’s<br />
Clinical Timesheet and <strong>ND</strong> Student’s Patient Contacts. You must submit a full packet for each<br />
preceptorship that you <strong>com</strong>plete. For your benefit, you should <strong>com</strong>plete the learning objective portion<br />
of the <strong>ND</strong> Student’s Preceptorship Evaluation prior to starting your experience. However, this form is<br />
15
not submitted until you finish your preceptorship and <strong>com</strong>plete the remaining evaluation portion. All<br />
forms are submitted at the same time ---- at the end of your preceptorship.<br />
Please keep track of your hours and patient contacts on the forms provided. Your preceptor needs to<br />
initial each day’s hours and patient contacts as well as sign the timesheet. When you finish a<br />
preceptorship, double check that you and the preceptor have signed and dated all forms, make copies of<br />
all forms for your own records and submit originals to the <strong>ND</strong> Preceptorship office. Please submit<br />
<strong>com</strong>pleted packets within a month of <strong>com</strong>pletion. DO not wait until just before graduation to submit<br />
your forms or your graduation date could be delayed. You can drop off packets, or send them through<br />
interdepartmental mail or the regular mail to the address below. After your paperwork is processed, you<br />
will receive, in your student mailbox, a printout of your total hours and patient contacts to date. This<br />
information is forwarded to the Registrar to be added to your transcript.<br />
The university has a blood born pathogen exposure incident policy in place in the unlikely event of<br />
your exposure to a blood born pathogen while at a preceptor site. Please note that the policy is in<br />
effect whether you are precepting in the Seattle metro area or another state, country or province.<br />
Some sites may have their own policy in place, and if so, you should follow their policy and check in<br />
with the blood born pathogen officer or counselor for follow up as soon as you return to the university.<br />
A counselor may be reached 24 hours a day by calling the resident on call at (206) 200-7067. All<br />
information on an incident or exposure is <strong>com</strong>pletely confidential and will not affect your standing in<br />
the program.<br />
All of our preceptors have graciously opened up their practice to help students get a broader view of the practice of medicine. Be sure to<br />
acknowledge your preceptor’s time and generosity!<br />
For more information, please contact:<br />
Martha Diehl, <strong>ND</strong> Preceptor Coordinator<br />
Office of Graduate and Community Medicine<br />
Room 326<br />
Bastyr Center for Natural Health<br />
1307 N 45th Street<br />
Seattle, WA 98103<br />
Phone 206.834.4103<br />
FAX 206.834.4107<br />
mdiehl@bastyr.edu<br />
revised 8/1/05<br />
Additional Student Packets and Preceptor Applications are available outside the Registrar’s office on campus<br />
and outside the <strong>ND</strong> Preceptorship office at the clinic.<br />
16
BASTYR UNIVERSITY’S NATUROPATHIC MEDICINE PRECEPTORSHIP PROGRAM<br />
<strong>ND</strong> Student’s Preceptorship Evaluation<br />
Name of Student: _____________________________________________________________________<br />
Telephone Number: _______________________ Anticipated Graduation (Quarter/Year): ____________<br />
Current Class Level (e.g. 2nd/4th): ____________Clinic Entry Date (Quarter/Year):__________________<br />
Name of Preceptor: ___________________________________________ Title (e.g. <strong>ND</strong>, MD): _________<br />
Clinic/Site Name: _____________________________________________________________________<br />
Address: _____________________________________________________________________________<br />
_____________________________________________________________________________<br />
Dates of Preceptorship: ________________________________________________________________<br />
Learning Objectives for this Preceptor Site: _________________________________________________<br />
_________________________________________________________________________________________<br />
_________________________________________________________________________________________<br />
__________________________________________________________________________<br />
Using the following scale, how would you rate your experience with this Preceptor?<br />
5. Excellent<br />
4. Above Average<br />
3. Average<br />
2. Below average<br />
1. Poor<br />
N/A Not Applicable<br />
A. Mentoring style 5 4 3 2 1 N/A<br />
B. Informative/ability to explain procedures 5 4 3 2 1 N/A<br />
C. Patient rapport/support 5 4 3 2 1 N/A<br />
D. Clinical Skill 5 4 3 2 1 N/A<br />
E. Time Management 5 4 3 2 1 N/A<br />
F. Receptivity to new ideas 5 4 3 2 1 N/A<br />
G. Integration of <strong>ND</strong> philosophy into practice 5 4 3 2 1 N/A<br />
~ Continued on reverse ~<br />
Type of Experience: _______ Shadow/Observe _______ Limited Hands-On _______Hands-On<br />
Please briefly describe your experience with the preceptor’s teaching style, kinds of patients seen in practice,<br />
modalities used, etc:<br />
Did the experience meet your learning objectives?<br />
Would you re<strong>com</strong>mend this preceptor to other students? Why or why not?<br />
Total number of hours: ________ Total patient contacts: ________<br />
Student’s Signature: ________________________________________________ Date: _____________<br />
<strong>ND</strong> Preceptor Coordinator’s Signature: __________________________________ Date: _____________<br />
revised 8/1/05<br />
17
BASTYR UNIVERSITY’S NATUROPATHIC MEDICINE PRECEPTORSHIP PROGRAM<br />
<strong>ND</strong> Student’s Clinical Time Sheet<br />
(Be sure to total your hours and patient contacts and have your preceptor initial and sign where applicable on<br />
both sides of this form.)<br />
Student: ___________________________________________________________________________<br />
Preceptor: ________________________________________________________Title: ______________<br />
Date In Out Total Hours Total Patients Preceptor’s Initials<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
___________ _____ _____ _________ __________ ______________<br />
Total: _________ __________<br />
Optional Comments by Preceptor: ________________________________________________<br />
____________________________________________________________________________<br />
_________________________________________________________________________________<br />
_______________________________________________________________________<br />
____________________________________________________________________________<br />
Preceptor’s Signature: ___________________________________________ Date: ________________<br />
<strong>ND</strong> Preceptor Coordinator’s Signature: _______________________________ Date: _______________<br />
revised 8/1/05<br />
~Student Patient Contact Form on reverse~<br />
BASTYR UNIVERSITY’S NATUROPATHIC MEDICINE PRECEPTORSHIP PROGRAM<br />
<strong>ND</strong> Student’s Preceptorship Patient Contacts<br />
Documentation of ALL Patient Contacts is required for credit. Please document your level of participation (Observed,<br />
Assisted, or Performed) under headings in each SOAP (Subjective, Objective, Assessment, and Plan) column.<br />
Do NOT list any patient names or initials.<br />
Student: ____________________________________________________________________________<br />
Preceptor: _______________________________________________________ Title: ______________<br />
Preceptor’s Initials<br />
Date Medical Assessment S O A P<br />
revised 8/1/05<br />
18
RESIDENCY PROGRAM<br />
Bastyr University is a CNME recognized sponsor of postgraduate medical education. This recognition<br />
has provided the university with the authority to grow its residency program by increasing the number<br />
of affiliate residency training sites. The residency program at the Bastyr Center for Natural Health<br />
(BCNH) is a CNME approved program. Through the residencies at BCNH and its affiliate programs,<br />
the university is able to offer both first-year and second-year residency training opportunities. The<br />
Bastyr University residencies are highly <strong>com</strong>petitive and attract graduates from other educational<br />
institutions as well as from Bastyr.<br />
The residency program at BCNH is a closely supervised mentorship program. Each resident evolves<br />
from an observational role into an independent practitioner over the course of the year. This<br />
progression is monitored and facilitated by a faculty mentor and by the Director of Graduate and<br />
Community Medicine. A second year of naturopathic residency consists of greater clinical autonomy<br />
with continued skill development. All residents have opportunities to do rotations in other local clinics<br />
and medical centers.<br />
The BCNH residency program is designed to provide an opportunity for naturopathic medical school<br />
graduates to strengthen their skills as a naturopathic physician. The program will provide residents the<br />
opportunity to enhance their knowledge and skills in general medicine, application of naturopathic<br />
philosophy, teaching, and practice management. The residency has specific knowledge, skill, and<br />
professional <strong>com</strong>petencies that are consistent with the progressive level of training throughout the<br />
course of the residency.<br />
GOALS OF THE BCNH RESIDENCY PROGRAM<br />
1. To develop ethical naturopathic physicians who are highly <strong>com</strong>petent in the practice of general<br />
naturopathic medicine, and in the management of emergent health conditions.<br />
2. To develop skilled clinical educators in the natural health sciences that integrate mind, body,<br />
spirit, and nature.<br />
3. To teach our residents core skills essential to leadership roles in a wide range of health care<br />
systems.<br />
4. To maintain an emotionally supportive environment, encourage intellectual debate, and foster<br />
life-long professional development.<br />
5. To give our residents the opportunity to provide high quality naturopathic care to the people of<br />
our <strong>com</strong>munity, regardless of socioeconomic status.<br />
6. To develop collegial relationships with other members of the clinical staff in order to enhance<br />
the quality of medical care to our <strong>com</strong>munity.<br />
7. To foster advanced <strong>com</strong>munication skills with healthcare providers outside the Bastyr Center<br />
for Natural Health.<br />
Moreover, one of the long-term goals of the university is to provide residency opportunities for every<br />
naturopathic graduate. As a CNME recognized sponsor, the university continues to develop training<br />
opportunities through affiliations with established institutions and clinics. The current affiliate<br />
residency sites are CNME approved that base their training on the supervised mentorship model as<br />
well. These affiliate sites range in size from small private clinic-based programs to hospital-based<br />
residencies. Each program has an affiliate residency director who is responsible for ensuring the<br />
quality of the clinical training. Though semi-autonomous, these programs regularly <strong>com</strong>municate with<br />
the Director of Graduate and Community Medicine to ensure <strong>com</strong>pliance with the CNME training<br />
standards. The goals of each affiliate program are described in each site-specific residency training<br />
manual.<br />
19
ONCOLOGY/CANCER<br />
NATUROPATHIC TREATMENT OF MALIGNANCY<br />
Chapter 18.57 or 18.71 RCW of the naturopathic licensing law states:<br />
“The practice of naturopathy includes manual manipulation (mechanotherapy), the prescription,<br />
administration, dispensing, and use, except for the treatment of malignancies or neoplastic disease, of<br />
nutrition and food science, physical modalities, homeopathy, certain medicines of mineral, animal, and<br />
botanical origin, hygiene and immunization, <strong>com</strong>mon diagnostic procedures, and suggestion; however,<br />
nothing in this chapter shall prohibit consultation and treatment of a patient in concert with a<br />
practitioner licensed under chapter 18.57 or 18.71 RCW.”<br />
Upon review by Bastyr University law firm, the statutory limitation in this aspect of our law is that a<br />
<strong>ND</strong> may not "treat malignancies” except “in concert with” an MD or DO. Therefore, if an <strong>ND</strong> is<br />
providing care to a cancer patient for any purpose other than treatment of his or her malignancy, there<br />
is no unusual limitation to the <strong>ND</strong>’s scope of practice.<br />
However, when a <strong>ND</strong> is providing curative treatment for the malignancy, the <strong>ND</strong> is within his or her<br />
scope only if the curative treatments are “in concert with” an MD or DO. There is no formal guidance<br />
on what it means to be acting “in concert with” an MD or DO from either the courts or the department<br />
of health. Mr. Burgon has advised us in this regard as follows.<br />
At a minimum, the <strong>ND</strong> must be confident that she or he is fully aware of the MD’s prescribed<br />
course of treatment. This is likely to require interaction with the MD or DO in order to obtain<br />
the necessary medical records or other direct knowledge of the patient’s treatment.<br />
In light of this interpretation, we have revised the informed consent form for the treatment of<br />
malignancies (see appendix). It is your responsibility to ensure that any patient for whom you are<br />
treating malignancy, the symptoms thereof, or the side effects of their conventional treatment for their<br />
malignancy, sign this consent form prior to your treatment.<br />
In order to treat patients with malignancy, naturopathic providers must:<br />
Have full awareness of the patient treatment as re<strong>com</strong>mended by their MD or DO documented<br />
in the patient’s medical record. It may also be listed as a documented conversation held with<br />
the patient’s MD or DO.<br />
As long as a patient is under the care of an MD or DO for their malignancy, naturopathic providers<br />
may treat this patient’s malignancy. If a patient has refused the treatment re<strong>com</strong>mended by an MD or<br />
DO, naturopathic providers must document the voluntary informed refusal of that treatment.<br />
Naturopathic providers must then continue to adhere to the above stated <strong>com</strong>munication guidelines in<br />
the care of this patient.<br />
• Regularly inform the patient’s MD or DO of the treatment being provided to the patient.<br />
• It is important to note that the <strong>ND</strong> does not have to be subservient to the MD’s direction. The<br />
<strong>ND</strong> must only provide treatment that is in harmony with the medical regimen and must inform the<br />
MD of the treatment being provided.<br />
And, to summarize your role:<br />
We provide treatment that is in harmony with the patient’s conventional treatment (to the best of<br />
the medical profession’s current state of knowledge).<br />
20
STUDENT ACADEMIC ISSUE RESOLUTION POLICY<br />
When a student has an academic-related issue and is seeking a venue in which to formally address this<br />
issue, it is the responsibility of the student to initiate the process outlined below in a step-by-step<br />
manner. Examples of academic related issues may include grade disputes, interpersonal<br />
<strong>com</strong>munication difficulties with faculty or supervisors or deans or difficulties <strong>com</strong>plying with program<br />
or department policies or procedures. Students are re<strong>com</strong>mended to meet with the Vice President of<br />
Student Affairs to receive assistance in preparing for the meeting and for creating a written request for<br />
resolution. The student is also wel<strong>com</strong>ed to request the support of the VPSA during all meetings and<br />
steps in the process. If the student suspects the issue may involve sexual harassment, the student is<br />
encouraged to review the Sexual Harassment Policy in the student handbook.<br />
In the event that a faculty member does not respond to a student request to arrange an informal<br />
meeting, or if a student does not receive a response from the lead faculty, chair or dean within the<br />
prescribed time line, the student may progress to the next step in the process. Documentation must be<br />
provided to show that the time lines were not met.<br />
Step 1<br />
The first step in resolving an academic related issue is for the student to arrange a formal meeting with<br />
the faculty regarding the issue of concern. A simple resolution to the issue may occur after this<br />
meeting. Once the issue is raised by the student, the faculty member and the student should meet so<br />
the issue is resolved within five days. If the issue occurs at a break where clinic is not in session the<br />
issue should be resolved by the 5 th working day after classes/clinic resumes. If it is a grade dispute, the<br />
student must raise the issue by 5 PM of the Friday of the first week of the following quarter, including<br />
summer quarter. All discussions and issues occurring during the formal meeting will be documented<br />
by the faculty member.<br />
Step 2<br />
If the issue is not resolved between the student and faculty member, the next step is for the student to<br />
submit a written request to the department chair, lead faculty or associate dean supervising the faculty<br />
member. The letter should state the issue of concern and the student’s re<strong>com</strong>mendation for resolution<br />
of the issue. After receiving the documentation, the supervisor will meet with the student and faculty<br />
in question. The department chair, lead faculty or associate dean will analyze the information and<br />
inform the student and faculty member in writing within 5 working days of the meeting. If the issue<br />
<strong>com</strong>es forward the week prior to a break or holiday, the issue should be resolved by the 5 th day after<br />
classes/clinic resume. All discussions will be documented by the chair/lead/associate dean.<br />
Step 3<br />
If the issue is not resolved according to step 2 within the 5 working days, the student will submit a<br />
written request to the Dean that clearly outlines the issue and re<strong>com</strong>mends resolution for the issue.<br />
The Dean will review the documentation from step 1 and step 2, the Dean will meet with the student<br />
faculty member and chair/lead/associate dean. The Dean will render a decision and inform the<br />
participants in writing within 5 working days of the meeting. In the event that an issue is presented<br />
during the week prior to a holiday or break, the issue should be resolved within 5 days after<br />
classes/clinic resume. In the case of a grade dispute, the decision of the Dean is binding and not<br />
subject to further appeal. All discussion and decisions rendered will be documented by the Dean. If<br />
the Dean is the instructor, the student should go directly to step 4.<br />
Step 4<br />
As previously stated grades are not subject to further appeal unless the dean is the instructor. If the<br />
student does not agree with the decision of the dean regarding other issues they may submit a written<br />
request to the office of the Vice President for Academic Affairs/Provost that clearly states the issue and<br />
re<strong>com</strong>mends a resolution of the issue. The VPAA or their designee will review the documentation<br />
received from the step 1-3 proceedings, request a meeting if it seems warranted, and will render a<br />
decision within 10 working days of receipt of the request. The decision of the VPAA is final and<br />
21
inding and not subject to further appeal. All discussions and decisions rendered will be documented<br />
by the VPAA or their designee.<br />
In the case of a grade dispute a student who remediates a PC grade to an AC status may still appeal the<br />
original grade. Students must initiate grade appeals with the program or department providing the<br />
course. The prefix designation of the course number signifies the department/program offering the<br />
course. Questions of judgment concerning course content, instructional method and appropriateness of<br />
performance standards are not subject to appeal.<br />
For further information, see the university student handbook.<br />
22
CLINICAL SECTION<br />
23
ACADEMIC ADVISING<br />
APPOINTMENTS WITH CLINICAL FACULTY ADVISORS<br />
Each student clinician will be assigned to a clinical faculty advisor. You may find out who you are<br />
assigned to through the registrar’s office or by checking with the clinic faculty assistant. If the student<br />
desires to change that assignment, contact the main campus registrar’s office. Advising sessions are an<br />
opportunity for students to share any suggestions or issues and to practice skills and review<br />
<strong>com</strong>petencies. Appointments may be made with your advisor in person or by email. Advisors are a<br />
resource to mentor students and supervise mini exam <strong>com</strong>petencies. If a student is at risk of failure,<br />
they are required to meet with their advisor on a regular basis as outlined in their learning contract. It<br />
is the student’s responsibility to contact the advisor and make an appointment. All the faculty members<br />
have posted office hours for student drop in visits, or will make appointments with students through<br />
email. The faculty assistant can also assist students in making appointments with faculty or with the<br />
associate clinical dean.<br />
CODE OF CO<strong>ND</strong>UCT<br />
Student clinicians are expected to function within the code of conduct expected of a professional<br />
physician. This includes awareness and integration of the standards of the profession, and honesty in<br />
their behavior and interactions with staff, patients, supervisors and colleagues. Clinicians will<br />
integrate integrity and responsibility in their interactions and uphold those standards with their<br />
supervisors and other clinicians. The practitioner will also disclose all potential conflicts of interest or<br />
potential for secondary gain that may arise during practice and patient treatment. A patient may not be<br />
referred to an outside resource that may provide benefit to the clinician or practitioner. Failure to abide<br />
by these standards will lead to sanction or even to dismissal.<br />
DOCUMENTATION<br />
TIME SHEETS<br />
•Students are responsible for having their time sheets at each shift.<br />
•Four hours is the maximum number of hours that may be counted for each shift, unless<br />
otherwise noted.<br />
•Students need to have the supervising faculty member initial the time sheet each week.<br />
•Any time missed on a shift due to absence, tardiness, or holiday will result in an IP grade<br />
<br />
for the shift. These hours will be made up with substitution or extra interim shift hours.<br />
Time Sheets must be turned in to the supervising faculty by the last day of each quarter. If a<br />
student does not submit their time sheet, the registrar will send a request to the student. If there is<br />
no response within a week, the Associate Clinical Dean or their designate will be notified. The AD<br />
or their designate will investigate whether the time sheet is held by the faculty or student. If the<br />
student has not submitted their time sheet and does not respond to the AD the registrar’s office will<br />
record an N (no Grade) grade. The financial Aid office will be notified in order to calculate<br />
whether this affects the status of the student’s financial aid. The student is required to meet with<br />
the AD or their designate to change the grade from N to IP or AC. If the student is found to be<br />
negligent in their responsibility a fee may be charged.<br />
HA<strong>ND</strong> WASHING/SANITATION<br />
The student applies proper awareness and observance of public health and sanitation rules by washing<br />
their hands, cleaning the tables and equipment before and after each exam and shift. The equipment<br />
may include lights, gynecological lights, tables, mirrors, and personal medical equipment including<br />
their stethoscope. Proper hand washing includes washing for 20 seconds, rinsing and drying the hands<br />
thoroughly. There are hand sanitation stations throughout the clinic that may be used up to two times<br />
before washing with water.<br />
24
HOURS/PATIENT CONTACTS<br />
Students are required to keep a summary of patient contacts from all shifts, interim clinic, substitution,<br />
and extra time. These are to be recorded on the “summary of patient contacts” form, and each patient<br />
contact must be initialed by the supervising faculty member. Students must designate each contact as<br />
either primary (P) or secondary (S) and use a separate form for each shift.<br />
IMMUNIZATIONS-SEE THE GLOBAL HA<strong>ND</strong>BOOK FOR POLICIES, REQUIREMENTS<br />
A<strong>ND</strong> PROCEDURES<br />
Charting/Medical Records<br />
PROCEDURES<br />
All chart entries must be made in black ink on the appropriate form. Computerized chart notes must be<br />
<strong>com</strong>pleted on clinic read-only templates installed on clinic library <strong>com</strong>puters or on your PC. Charting<br />
may not be stored on personal <strong>com</strong>puters or PDA’s unless it is <strong>com</strong>pletely de-identified. This<br />
policy is to protect the confidentiality of patient medical records in <strong>com</strong>pliance with HIPPA privacy<br />
guidelines.<br />
All charting corrections or changes made by a student or supervising faculty in a chart on the day of<br />
the original entry are to be made as follows:<br />
1. Draw one line through the entry to be changed.<br />
2. Write the new entry beside the old entry.<br />
3. Initial the change.<br />
4. Please refer to the medical abbreviations list in the appendix of the global module for<br />
approved medical abbreviations in charting.<br />
For all chart changes made in a chart after the day of the original entry by the supervising faculty:<br />
1. Draw one line through the entry to be changed.<br />
2. Write the new entry beside the old entry.<br />
3. Initial and date the change.<br />
4. No changes can be made after the provider has signed the chart. Any additions or changes to<br />
the charting must be made on a new page and signed by the supervising faculty and inserted<br />
into the charting with appropriate referencing to the original chart notes.<br />
No patient may be treated without the following:<br />
1. A “consent to treatment” form signed by the patient or the patient’s designated signatory.<br />
2. A <strong>com</strong>pleted patient intake form and patient billing/insurance form.<br />
CHARTING/MEDICAL RECORD KEEPING<br />
FORMAT<br />
We utilize the SOAP format for all charting in the clinic.<br />
Each chart should have a subjective (S), Objective (O), Assessment (A), Plan (P), Future Plan (FP) and<br />
Impression (I). Note that within the SOAP format, there are variable styles of charting.<br />
1. Subjective (S): This section includes what the patient tells you about their health and symptoms.<br />
In the large category, this is the history of the present illness (HPI).<br />
a. It includes the chief <strong>com</strong>plaint (ex: my stomach hurts), and the seven attributes of that <strong>com</strong>plaint.<br />
The attributes include: location, quality, quantity or severity, timing (onset, duration and<br />
frequency), setting, aggravating and alleviating factors and associated manifestations.<br />
(Ex: the pain began yesterday and was 3/10 in intensity, now it is 7/10. The pain is dull, aching and<br />
fluctuates in intensity. I took Pepto Bismol and felt better for a while and then I vomited and<br />
had diarrhea two times. I got back from Mexico four days ago. I was traveling in the country<br />
25
and ate at local restaurants and stands. I did not have access to bottled water, but I have an old<br />
filter I used to use when I went camping.) .<br />
It should include the attributes for every <strong>com</strong>plaint a patient presents with in the clinic. Ex: I have a<br />
stomach ache, a headache and diarrhea. My knee also hurts when I walk down stairs. These<br />
extra <strong>com</strong>plaints would be noted as Complaints #2, 3, and 4. If associated with the chief<br />
<strong>com</strong>plaint, example: diarrhea, it may be noted with all its attributes on the associated symptom<br />
portion of the related <strong>com</strong>plaint.<br />
b. It also includes the past medical history, family history, allergies, lifestyle, social history, current<br />
medications (correctly spelled), current supplement and over the counter drug use and a review<br />
of systems. Please see Bates for details regarding professional charting the patient history.<br />
2. Objective (O): This section includes the information you gather using your senses-what you see,<br />
hear, smell and feel while conducting a physical examination of the patient. It is <strong>com</strong>pleted using<br />
clinical language. Terms must be spelled correctly.<br />
3. Assessment (A): The assessment is one of the most important aspects of the chart. All active<br />
diagnoses, with a correct ICD-9 code for each, must be recorded in the assessment section. They<br />
must correspond with the diagnoses that are recorded on the superbill.<br />
Clinicians may consider their diagnosis likely but not certain, in which case they should precede<br />
the stated diagnosis with an indicative term such as “working” diagnosis, “presumptive” or<br />
“probable” diagnosis. In this event, the Assessment would also include rule/out(s) or a differential<br />
diagnosis. For example: “Probable Diagnosis: Atypical Migraine Headache, Rule/Out increased<br />
intra-ocular pressure.” Record your diagnostic rationale after each diagnosis or tentative diagnosis.<br />
Every rule/out diagnosis requires a corresponding action in the treatment plan. Differential<br />
diagnoses may or may not require action on the treatment plan. Finally, all active or resolved<br />
diagnoses and problems are recorded and tracked on the patient’s “health data sheet,” which<br />
appears on the left side of the front section of the patient’s chart. They are also included in the<br />
assessment section and noted as resolved.<br />
4. Problems: At BCNH, we follow a system that includes a problem list. It is described by Rakel<br />
in Essentials of Family Practice. A problem is defined as “anything that requires diagnosis or<br />
management or that interferes with quality of life as perceived by the patient. It is any physiologic,<br />
pathologic, psychological, or social item of concern to either the patient or the physician.” Rakel<br />
delineates further that a problem can be anatomic (hernia), physiologic (undiagnosed jaundice), a<br />
specific diagnosis, a sign, a symptom, economic (financial stress), social (family discord),<br />
psychiatric, a physical handicap, an abnormal lab or imaging finding, or a risk factor (personal or<br />
family). Note that “problem” is a more inclusive term than “diagnosis.”<br />
A diagnosis <strong>com</strong>municates the provider’s certainty of the existence of a specific disease entity. A<br />
problem can be a diagnosis, or it can be a variety of assessments in progress, some requiring<br />
further evaluation.<br />
a. If the purpose of the charted visit was to follow-up on a previously listed problem from a<br />
problem list, and the problem has resolved by inclusion in another diagnosis, or by cure or<br />
disappearance, this should be noted in your assessment<br />
b. Assessment: (Rationale or ddx)<br />
Diagnoses: GERD—Rationale: secondary to suspected food intolerance and possible weak<br />
sphincter muscle tone and reduced HCl/pepsin production<br />
Problems: headache—ddx: a typical migraine, chronic sinus infection, eyestrain<br />
5. Impression (I): After you indicate your active diagnoses and problems, you may then, give your<br />
impression of the patient. Remember to write this section professionally and respectfully. Nothing<br />
should be included in this section that you would not directly tell your patient. This includes the<br />
naturopathic diagnosis and the principles utilized in the case.<br />
6. Plan (P): All actions re<strong>com</strong>mended or prescribed at the present patient visit must be noted in the<br />
plan section of the patient’s chart. This will include instructions for diet or lifestyle modification or<br />
26
intervention; any medication (herbal/botanical, homeopathic, nutraceutical, or prescription<br />
medication) with <strong>com</strong>plete and correct name of product, key ingredients(s) and amount(s) as<br />
appropriate, number of units, dose and instructions, duration of dosing, and important side effects<br />
about which the patient was informed and what they were instructed to do if they occur; therapeutic<br />
application or self-treatment (with detailed instructions); referrals for treatment; consultation with<br />
specialist(s); and laboratory testing or imaging. Remember that the plan must contain an action<br />
corresponding to every problem, diagnosis, or rule/out evaluated or managed at that visit; even if<br />
the action is simply to watch and wait (do nothing).<br />
a. As students create and record this plan, they should consider the hierarchy of therapeutics<br />
(therapeutic order) and naturopathic principles, and how these principles guide the plan.<br />
b. If care to be offered in the future has been decided on, it is charted as “future plan.” This<br />
includes all of the future planned actions for the clinician and their team, including any<br />
intended follow-up, when the team will next see the patient in the clinic, any planned phone<br />
calls to the patient, referral, research activities and coordination of care.<br />
c. This is where you include the determinants of health to validate your choice of treatment and<br />
your future plan.<br />
7. The supplement and medication list needs to be updated at each patient visit. If a patient<br />
discontinues a medication/supplement, it should be noted in the medication/supplement sheet on<br />
the left of the chart.<br />
a. Spelling must be accurate.<br />
b. All paperwork must be filled out in its entirety before turning the medical record in to<br />
supervisors for their signature. This includes the patient’s name, date, supervisor’s full name<br />
and student’s full name on every page, a copy of the treatment plan, patient visit summary with<br />
correct ICD-9 code/s used that day, medication/supplement sheet filled out with dosing<br />
schedule, doctor’s name, self-prescribed medication, adult health data sheet or pediatric health<br />
data sheet <strong>com</strong>pleted or brought up to date, and drug allergies. Treatment plans in the chart<br />
must include dosages in terms of metric measurement (mg/grams), not just “3 caps TID”,<br />
unless it is a <strong>com</strong>bination product.<br />
c. Do not leave any preparation notes in the medical record.<br />
d. All of the documentation must be <strong>com</strong>pleted within the borders of the note page. Any<br />
information outside of the borders (i.e., the dark thick line) may not copy when medical<br />
records are requested from another provider.<br />
e. All <strong>ND</strong> student clinicians must <strong>com</strong>plete chart notes for all patient visits and phone contacts<br />
within 1 hour of the contact. In<strong>com</strong>plete charts must be appropriately labeled and notes and<br />
treatment plan from the visit must be in the chart. Once the chart is signed and <strong>com</strong>pleted, the<br />
student fills out a chart action review form for their supervising faculty member, and leaves it<br />
in the supervising clinical faculty’s mailbox.<br />
f. Violation of these policies will result in a clinic sanction, resulting in loss of that day's shift<br />
hours and patient contacts. Repeated violations of this policy will result in a failure of the<br />
entire quarterly shift including loss of those shift hours and patient contacts. Students who<br />
<strong>com</strong>mit repeated violations may be considered as candidates for expulsion from the program.<br />
The medical record is a legal document.<br />
8. Charts need to be legible, clear and concise. If your handwriting is illegible you should <strong>com</strong>plete<br />
your charting by typing or <strong>com</strong>puter. You must follow the patient confidentiality guidelines as<br />
required by HIPPA when you utilize the clinic format for <strong>com</strong>puterized chart notes.<br />
27
PATIENT INTERVIEW GUIDELINES<br />
PRIMARY CLINICIAN<br />
The primary student needs to direct the interview. While it is important to hear the patient’s story, it is<br />
inefficient to let the patient run the interview. If a patient is not answering your questions, politely<br />
redirect them. This may mean that you do this several times during an interview.<br />
Remember that FOCs should actually take no more than 75 minutes and ROCs should take only 45<br />
minutes. The interview portion of an FOC should generally be no longer than 30 minutes and for<br />
ROCs no more than 10-15 minutes. This leaves time to perform PE, formulate your diagnosis and<br />
treatment plan, discuss the treatment plan with your supervisor and to present it to the patient.<br />
Time management is one of the most important tools for managing a successful practice. It may not be<br />
possible to obtain all of the patient information in one visit. If the patient has a <strong>com</strong>plicated history, let<br />
them know that another visit may be required in order to <strong>com</strong>plete all the information. Their main<br />
<strong>com</strong>plaint or urgent problems must be addressed in the first visit.<br />
Never discuss any treatment with a patient during the interview without consulting the<br />
supervising clinical faculty member. To do so is to practice medicine without a license and infraction<br />
of this policy is taken seriously as a matter of public safety and respect for the supervisor’s ability to<br />
practice medicine. Students who violate this policy are subject to sanctions. Repeated violation of this<br />
policy will result in failure of the shift and consideration for expulsion by the Academic Progress<br />
Committee.<br />
SECO<strong>ND</strong>ARY <strong>ND</strong> CLINICIAN<br />
The role of the secondary clinician during the interview is to support and learn from the primary<br />
clinician. You may ask questions when it is appropriate and help to fill in gaps that may have been<br />
overlooked by the primary. The expectation is that the secondary clinician assists the primary in<br />
maintaining the interview without disrupting the flow of the interview.<br />
It is also a secondary responsibility to help keep the interview on track. Remember that an FOC lasts<br />
75 minutes and an ROC is no longer than 45 minutes. This means that the interview portion of an FOC<br />
should last no longer than 30 minutes and in an ROC no more than 10-15 minutes. Assist the primary<br />
in leaving time to perform PE, formulate a diagnosis and treatment plan, discuss the treatment plan<br />
with the supervisor and present the plan to the patient.<br />
Never discuss any treatment with a patient during the interview without consulting the primary and<br />
supervising faculty member. See the section above regarding sanctions.<br />
Secondary clinicians are responsible for <strong>com</strong>pletion of the patients’ paperwork. This includes the<br />
superbill, treatment plan and dispensary sheet. Please obtain blank copies of these forms before the<br />
shift so they are available. Each should be filled out <strong>com</strong>pletely and accurately. Treatment plans must<br />
be legible, with the provider’s full name. It must include a rationale for each treatment re<strong>com</strong>mended<br />
to maximize patient <strong>com</strong>pliance. You may request assistance in <strong>com</strong>pleting paperwork from other team<br />
members in order to maximize time management for the visit.<br />
MEDICAL RECORD KEEPING RESPONSIBILITIES - PRIMARY CLINICIANS<br />
Primary student clinicians are responsible for ensuring that all medical records are <strong>com</strong>pleted in<br />
accordance with clinic policy and that all forms are filed properly in the chart when generated. All<br />
corresponding recording must be <strong>com</strong>pleted by the primary student clinician within 1 hour and should<br />
be signed by the supervising physician within 2 hours after each patient shift. The supervisor will<br />
notify the student by note or email of any charting deficits. The supervisor will discuss the issues and<br />
assist the primary clinician with necessary information to ensure immediate correction. Clinicians who<br />
fail to correct such deficits in charting practices will be warned in writing of the deadline for the<br />
expected changes. If the chart is not corrected within that time, the student is eligible to receive a clinic<br />
sanction.<br />
28
SCOPE OF PRACTICE OF A CLINICIAN<br />
The student must recognize at all times that they are practicing under the license of a supervisor. This<br />
means that any advice or re<strong>com</strong>mendation made to a patient without the prior approval of a supervisor<br />
is practicing medicine without a license. By utilizing this behavior in the clinic, the student is placing<br />
themselves at risk for sanctions, up to and including dismissal.<br />
Students may not prescribe treatment that benefits their own business interests or refer a patient to their<br />
private practice or business. This constitutes a conflict of interest and is not tolerated by BCNH.<br />
GRADING HA<strong>ND</strong>BOOK FOR CLINICIANS<br />
Grading criteria for primary and secondary clinicians in naturopathic medicine are outlined in this<br />
section. Achieved <strong>com</strong>petency is reached by incorporating all skills into each shift. Secondary<br />
clinicians are evaluated as early secondary and late secondary clinicians. Primary Clinicians are<br />
evaluated as early, middle and late primary clinicians. An early primary is a clinician who has been a<br />
primary in patient care for 0-2 quarters, usually corresponding to patient care shifts 5-8. A mid-primary<br />
clinician is enrolled in patient care shifts 9-12 and a late primary is enrolled in shifts 13-17.<br />
Naturally, an early primary clinician will demonstrate less skill in all areas than a late primary, and the<br />
grading system takes this into account. Please see the table below for a visual of the grading system<br />
used at the clinic and the performance differences between the grades of AC, PC and F.<br />
Clinic<br />
Grade Earned<br />
Level AC PC F<br />
Early<br />
Primary<br />
All skills w/coaching<br />
on at least 80% of cases<br />
All skills w/coaching on at<br />
least 70-79% of cases<br />
All skills w/coaching on<br />
less than 70% of cases<br />
All skills w/ minimal All skills w/ minimal All skills w/ minimal<br />
Mid<br />
coaching on at least 80% coaching on at least coaching on less than 70%<br />
Primary<br />
of cases<br />
70-79% of cases<br />
of cases<br />
Late<br />
Primary<br />
Early<br />
Secondary<br />
Late<br />
Secondary<br />
All skills w/out coaching<br />
on at least 80% of cases<br />
All skills w/ assistance on<br />
at least 80% of cases<br />
All skills w/out assistance<br />
on at least 80% of cases<br />
All skills w/out coaching<br />
on at least 70-79% of<br />
cases<br />
All skills w/ assistance on<br />
at least 70-79% of cases<br />
All skills w/out assistance<br />
on at least 70-79% of<br />
cases<br />
29<br />
All skills w/out coaching on<br />
less than 70% of cases<br />
All skills w/ assistance on<br />
less than 70% of cases<br />
All skills w/out assistance<br />
on less than 70% of cases<br />
The student must receive an AC grade to obtain credit for each of the quarterly shifts. The skills<br />
necessary to demonstrate <strong>com</strong>petence are raised each quarter to ensure that students attain all necessary<br />
basic skills to be a safe and effective naturopathic physician. If a student is performing under the level<br />
of <strong>com</strong>petence, a letter will be sent to them that indicates the area(s) of deficiency and makes<br />
re<strong>com</strong>mendations for improving their performance. If the student cannot raise their level of<br />
performance by the end of the quarter a grade of PC or F will be given.<br />
When a student receives a PC grade for a quarterly shift, the student must follow all re<strong>com</strong>mendations<br />
listed by the supervisor to change the PC to an AC by the fifth week of the following quarter. This<br />
policy differs from the time line of didactic courses. If the student cannot rectify those inadequacies,<br />
the grade will change to an F, and the student will lose credit for all hours and patient contacts.<br />
When a student receives an F grade for the quarterly shift, they will lose all patient contacts and hours<br />
attained during the quarter. The entire shift must be repeated, and the date of graduation will be set
ack at least one quarter. During the repeat shift, the student will be graded at the same level as the<br />
failed shift. Failure of a clinic shift places the student on academic probation and a learning contract is<br />
developed with the assistance of the associate clinical dean. Failure of two clinic shifts automatically<br />
places the student on final probation status and they must meet with the associate clinical dean and<br />
with the naturopathic medicine academic progress <strong>com</strong>mittee to determine whether they may remain in<br />
the program.<br />
LEARNING OBJECTIVES FOR SECO<strong>ND</strong>ARY CLINICIANS<br />
During their careers at Bastyr Center for Natural Health, all clinicians must demonstrate <strong>com</strong>petence in<br />
numerous clinical skills. We track this expanding expertise by a system of skills/performance<br />
evaluations to be <strong>com</strong>pleted sequentially by term. Below is a time line for all <strong>ND</strong> student clinicians.<br />
The clinic supervisor, advisor or resident will sign for the <strong>com</strong>petencies they have observed.<br />
Secondary Quarter/Shift 1<br />
Development and Application of Communication Skills<br />
Knowledge and utilization of all aspects of clinic operational procedures<br />
Incorporates Professional Attitudes and Behaviors<br />
Knowledge and Practice of Physical Exam Skills<br />
Development of Charting Skills<br />
Building Knowledge of Treatment Modalities and Application<br />
Secondary Quarter/Shift 2<br />
All the preceding skills and:<br />
Responsibility and Participation in active patient care<br />
Present cases at preview and review-Professional Communication Skills<br />
Further development of Charting Skills<br />
Further develop knowledge of Treatment Modalities<br />
Application of treatment skills<br />
Secondary Quarters/Shifts 3 & 4<br />
All the preceding skills and:<br />
Application of Interview and <strong>com</strong>munication skill<br />
Charting Skills applied at Early Primary Level<br />
Physical Exam Skills intact and ready for assuming primary role<br />
Contribute actively to diagnostic and therapeutic work-up of patient cases<br />
Interactive application of treatment skills<br />
Begin limited primary work with supervision<br />
Secondary <strong>com</strong>petency achievement on general naturopathic medicine shifts is noted on a tracking<br />
form which is included for in the appendix of this notebook. There are separate <strong>com</strong>petency tracking<br />
forms for homeopathy shifts, counseling shifts and physical medicine shifts. Each secondary clinician<br />
will <strong>com</strong>plete one form for each general naturopathic patient care shift they have each quarter. If you<br />
have no patient care shifts in a quarter you do not <strong>com</strong>plete a form. The forms are turned in to the<br />
clinic program supervisor when they are <strong>com</strong>pleted. They must be on record with the clinic registration<br />
staff before you may advance to primary status. Please see the Associate Clinical Dean with questions<br />
regarding this policy<br />
30
SECO<strong>ND</strong>ARY SKILLS<br />
1. Professional Skills<br />
A. Initiative and Responsibility in Role as Secondary Clinician<br />
B. Communication Skills with supervising physician, peers and staff<br />
C. Communication skills with patients<br />
2. Clinical Skills<br />
A. Physical Exam Skills<br />
B. Integration of Didactic Knowledge into the Clinical Setting<br />
C. Medical Record Keeping Skills<br />
D. Participation in Case Discussion<br />
PROFESSIONAL SKILLS-Secondary Clinician<br />
These are skills that are necessary in creating rapport with patients, supervisors and colleagues<br />
throughout your professional life. The grading in this category is oriented to provide optimal flow to<br />
patient care. The skills themselves are necessary adjuncts to success in the professional world.<br />
Initiative and Responsibility in Role-Secondary Clinician<br />
This skill is necessary in the clinic for student education and quality of patient care. Grading for this<br />
criterion includes, but is not limited to:<br />
• The student studies and prepares for shifts by reading patient charts and researching<br />
<strong>com</strong>plaints and conditions, reviewing the pathophysiology of disease processes, biochemistry<br />
of illness and treatments, differential diagnosis, and treatment for the <strong>com</strong>plaints, conditions<br />
and diagnoses of the patients.<br />
• The student demonstrates self-motivation in pursuing knowledge to enhance patient care and<br />
their own education.<br />
• The student demonstrates familiarity with cases and can present the cases seen that day in<br />
case preview and review when requested to do so by their supervisor.<br />
• The student utilizes clinical resources to enhance their skill and knowledge during down time<br />
on the shifts by pursuing self study, practicing physical exam skills and studying treatment<br />
modalities.<br />
There is no remediation or PC grade available for this skill.<br />
This skill is a necessary attribute for a practicing physician as our skill set is never mastered.<br />
Continual study is a necessity for a safe and viable practitioner.<br />
Communication Skills with Supervising Faculty, Peers and Staff-Secondary Clinician<br />
• The student exhibits an understanding and mastery of professional <strong>com</strong>munication in their<br />
verbal, non-verbal and written <strong>com</strong>munication.<br />
• The student assists the supervisor and their peers in processing paperwork and enhancing the<br />
effectiveness and timeliness of the patient visit.<br />
• The student elicits feedback on their performance from the supervisor and their peer clinicians.<br />
• The student exhibits professionalism and collegiality in all their interactions with clinic staff,<br />
peers and supervisor.<br />
• The student incorporates clinical policies and procedures smoothly into the patient care and<br />
learning process.<br />
Communication Skills with Patients-Secondary Clinician<br />
• The student participates in the patient visit in a professional manner that enhances, and does<br />
not impede the visit progress.<br />
• The student actively follows the case taking and inserts appropriate questions at indicated<br />
times during the visit.<br />
31
• The student notes requests by the patient during the visit and informs the primary and<br />
supervisor so that those needs may be addressed.<br />
• The student observes the patient during the interview and reports pertinent observations to the<br />
primary and supervisor.<br />
• The student demonstrates <strong>com</strong>munication skills that emphasize patient needs and are<br />
culturally and socially sensitive to patient gender, lifestyle, culture, race and socioeconomic<br />
status.<br />
Remediation of this skill may include, but is not limited to, auditing portions of counseling courses,<br />
pursuing skills workshops in counseling or <strong>com</strong>munication skills, tutoring on <strong>com</strong>munication skills<br />
and diversity training through the school tutoring center or an outside resource.<br />
Communication skills are one of the most important attributes of a successful physician and are<br />
a necessary ingredient for smooth flow and optimal function of a multidisciplinary teaching<br />
clinic.<br />
CLINICAL SKILLS-Secondary Clinician<br />
Physical Exam Skills<br />
The student is adept in taking the vital signs of each patient on each visit in a timely manner, using<br />
the appropriate equipment accurately.<br />
• The student reports abnormal vital signs to the supervisor and ensures that the information is<br />
recorded appropriately in the patient chart.<br />
• The student demonstrates proper technique and knowledge of exams when asked to repeat<br />
physical exams during the patient visit and when achieving their <strong>com</strong>petency sign-off<br />
requirements.<br />
• The student demonstrates their ability to integrate the information obtained in physical exam<br />
into the differential diagnosis and treatment plan for each patient as a part of the clinical team.<br />
• The student is prepared to participate in exams by bringing their diagnostic equipment in good<br />
working order to each daily shift.<br />
The student applies proper awareness and observance of public health and sanitation rules by<br />
washing their hands, cleaning the tables and equipment after each exam and shift. The equipment<br />
may include lights, gynecological lights, tables, mirrors, and personal medical equipment including<br />
their stethoscope. Proper hand washing includes washing for 20 seconds, rinsing and drying the<br />
hands thoroughly.<br />
Remediation for this skill in the event a student receives a PC includes demonstration of appropriate<br />
technique in performing physical exam <strong>com</strong>petencies and in obtaining vital signs and accurate charting<br />
of information in a patient chart. If PC is given because of damage or lack of equipment the student<br />
must demonstrate that their equipment is in good working order.<br />
It is mandatory that a safe and successful physician exhibit excellent physical exam skills and an<br />
understanding of how information obtained in a physical exam contributes to the development of<br />
a differential diagnosis and treatment plan for each patient.<br />
Integration of Didactic Knowledge Into the Clinical Setting-Secondary Clinician<br />
• The student demonstrates understanding and integration of pathophysiology, anatomy, and<br />
biochemistry as they relate to patient <strong>com</strong>plaints and diagnosis during case discussion, case<br />
preview and case review.<br />
• The student demonstrates evidence of case preparation by including knowledge obtained<br />
through research into case discussion.<br />
• The student suggests appropriate lab or diagnostic testing during case discussions and can<br />
explain the procedures and purpose of testing to the patient if asked to do so.<br />
• The student exhibits their grasp of knowledge in case discussions, case preview and case<br />
review.<br />
32
A PC grade in this skill is rectified by the student <strong>com</strong>pleting an assignment of three case analyses with<br />
supervisor or their agent. The cases will include the following <strong>com</strong>ponents:<br />
• Identify the chief <strong>com</strong>plaint and seven attributes and how the review of systems is integrated<br />
into the development of a differential diagnosis.<br />
• Describe objective findings utilizing appropriate terminology.<br />
• Formulate and defend a differential diagnosis and how testing is integrated into the<br />
confirmation process.<br />
This skill is mandatory for both the success of the physician and to guard public safety.<br />
Medical Record Keeping Skills (Charting)-Secondary Clinician<br />
• The student charts vital signs appropriately in the medical record<br />
• The student demonstrates mastery of the SOAP charting format by presenting cases in Case<br />
Preview and Review in that form when called upon to do so.<br />
• The student demonstrates their <strong>com</strong>petence in medical record keeping by recording findings<br />
during physical exam when asked to do so by the primary clinician.<br />
• The student demonstrates a grasp of medical record keeping requirements as outlined in this<br />
handbook when submitting required charting for <strong>com</strong>petency evaluation.<br />
A PC in this category is rectified by presenting two <strong>com</strong>pleted return office call records and first office<br />
call record that <strong>com</strong>plies with clinic medical record keeping guidelines.<br />
Clinical record keeping skills are mandatory for the successful physician for ethical and legal<br />
reasons. The record is a physician’s and a patient’s protection as it documents patient- physician<br />
interactions.<br />
Participation in Case Discussion-Secondary Clinician<br />
• The student demonstrates <strong>com</strong>petence in explaining the principles of naturopathic medicine<br />
and how they apply to each case when presenting in case preview and review.<br />
• The student demonstrates <strong>com</strong>petence in discussing the Therapeutic Order and how they<br />
apply in each case during case preview and review when asked to do so by the supervising<br />
physician or peers.<br />
• The student demonstrates their ability to present cases within the SOAP format during case<br />
preview and review discussion when called upon to do so by the supervisor.<br />
• The student demonstrates the integration of didactic knowledge into each patient interaction<br />
during case discussions.<br />
• The student exhibits a willing participation in case discussion during shift and during case<br />
preview and review.<br />
A PC in this skill is remediated by practicing case presentation and analysis under the supervision<br />
of the supervising faculty or the associate clinical dean. Large gaps in knowledge may require<br />
attendance of a portion of didactic classes pertaining to the area of weak knowledge or the addition<br />
of a case analysis and management course.<br />
The ability to synthesis patient data and discuss reasoning for your clinical choices is a<br />
primary skill of a safe and effective physician.<br />
33
GRADING CRITERIA PRIMARY CLINICIANS<br />
• An AC grade is given when students have successfully demonstrated <strong>com</strong>petence in all the<br />
clinical categories relevant to their clinical status.<br />
• A PC grade is given if one non-critical skill is assessed as inadequate.<br />
• An F grade is given if critical clinical skills are assessed as unsatisfactory.<br />
• If a PC grade is given, a letter detailing requirements for changing the PC grade to an AC will<br />
ac<strong>com</strong>pany the grade. Refer to the clinic SOP and grading section in the global manual for<br />
<br />
details.<br />
If an F grade is given, a letter detailing the reasoning for the grade will follow assignment of<br />
the grade. Refer to the clinic grading section and policy sections in the global and <strong>ND</strong> manuals<br />
for details.<br />
LEARNING OBJECTIVES FOR PRIMARY CLINICIANS<br />
Early Primary<br />
• Practice application and integrate skill in the interview, PE, development of differential<br />
diagnosis, and medical charting of patients seen in clinical rotations.<br />
• Formulate basic treatment plans utilizing nutrition, homeopathy, counseling, botanical<br />
medicine and/or physical medicine that are pertinent to the patient.<br />
• Demonstrate skills in application and explanation of diagnosis and treatment to the<br />
supervising physician and to the patient<br />
• Develop confidence in personal skill development<br />
• Demonstrate integration of lifelong learning skills<br />
• Enhance <strong>com</strong>munication skills and professional demeanor<br />
• Integrate <strong>com</strong>munication skills with empathy and unconditional regard into the patient<br />
<br />
encounter.<br />
Integrate the principles of naturopathic medicine and therapeutic order into discussion and decision<br />
making.<br />
Mid level Primary<br />
All of the above skills and:<br />
• Apply scientific research in <strong>com</strong>munication of etiology (cause), diagnosis and treatment of<br />
disease<br />
• Demonstrate effective time management into the patient interview<br />
• Integrate evaluation of the vis into the assessment, diagnosis, and treatment of each patient.<br />
• Mastery in application of assessment skills utilizing the determinants of health, therapeutic<br />
order and the principles of naturopathic medicine into patient evaluation and treatment.<br />
• Integrate wellness and prevention in evaluation and management.<br />
Advanced Primary<br />
All the preceding skills and:<br />
• Master effective patient management skills that utilize the principles of naturopathic medicine<br />
and the therapeutic order in individualized assessment, treatment and management.<br />
• Integrate self-confidence into your role as a clinician.<br />
• Demonstrate the ability to function independently, developing treatment plans and case<br />
management with minimal assistance from the supervisor.<br />
PRIMARY SKILLS<br />
1. Professional Skills<br />
A. Communication with Patient<br />
B. Communication with Supervisor, Staff and Colleagues<br />
34
C. Motivation, Initiative and Responsibility in the Patient Care Setting<br />
D. Teamwork-Incorporation of Policies and Procedures<br />
2. Clinical Skills<br />
A. Interview Skills<br />
B. Physical Exam Skills<br />
C. Overall Case Management<br />
D. Medical Record Keeping (Charting)<br />
E. Incorporation of Academic and Didactic Knowledge into Clinical Practice<br />
F. Application of Naturopathic Therapeutics<br />
PROFESSIONAL SKILLS-Primary Clinician<br />
These skills are necessary in creating rapport with patients, supervisors and colleagues throughout your<br />
professional life. The skills are necessary adjuncts to success in the professional world.<br />
Communication with Patients-Primary Clinician<br />
• The student speaks clearly to the patient and establishes patient rapport.<br />
• The student uses language and terminology in order to improve patient knowledge and<br />
understanding of their health and illness.<br />
• The student <strong>com</strong>municates specific patient care re<strong>com</strong>mendations as authorized by the<br />
supervising physician accurately to the patient and does not volunteer or direct additional<br />
treatment to the patient without physician authorization.<br />
• The student demonstrates good listening skills during the patient interview by including all<br />
patient concerns in the charting and case discussion.<br />
• The student demonstrates empathy with the patient during the interview and exam. For<br />
example, this may be done by emphasizing respect, and an understanding of the patient’s<br />
circumstances into the conversation in a non-judgmental and accepting manner.<br />
• The student conducts themselves in an open, non-judgmental way to all information disclosed<br />
by the patient.<br />
• The student ensures that all the needs of the patient have been elicited before the end of the<br />
visit.<br />
• The student demonstrates <strong>com</strong>munication skills that emphasize patient needs and are<br />
culturally and socially sensitive to patient gender, lifestyle, culture, race and socioeconomic<br />
status.<br />
Remediation of this skill may include, but is not limited to, auditing portions of counseling courses,<br />
pursuing skills workshops in counseling or <strong>com</strong>munication skills, tutoring on <strong>com</strong>munication skills<br />
and diversity training through the school tutoring center or an outside resource. The student will<br />
demonstrate these skills in at least four of five interviews.<br />
Communication skills are one of the most important attributes of a successful physician and are<br />
a necessary ingredient for smooth flow and optimal function of a multidisciplinary teaching<br />
clinic.<br />
Communication with Supervisors, Staff, and Colleagues-Primary Clinician<br />
• The student demonstrates respect and collegiality in their <strong>com</strong>munications and interactions<br />
with supervisors, staff and colleagues.<br />
• The student demonstrates the ability to work as part of the team to optimize patient care.<br />
• The student demonstrates an articulate and summarized presentation of cases in preview and<br />
review.<br />
• The student demonstrates the ability to summarize the patient’s case to the supervisor in a<br />
<strong>com</strong>plete, coherent and concise manner.<br />
• The student responds to supervisor’s requests or assignments in a timely and professional<br />
manner.<br />
35
• The student follows the attendance policy and is responsible and thorough in <strong>com</strong>munication<br />
regarding absences and its impact on patient care.<br />
• The student <strong>com</strong>municates specific patient care re<strong>com</strong>mendations as authorized by the<br />
supervising physician accurately to the patient and does not volunteer or direct additional<br />
treatment to the patient without physician authorization.<br />
There is no PC in this category. If a student demonstrates a deliberate lack of cooperation and<br />
professionalism with others that results in delay, confusion, error, omission, conflict or creates extra<br />
work in patient management and/or jeopardizes patient rapport, further sanctions will be given on the<br />
first offense. The sanctions will be appropriate to the violation and may include a warning letter, a<br />
failure event or referral to the appropriate progress <strong>com</strong>mittee as decided by the supervisor. Additional<br />
episodes during the remainder of the clinical training will result in failure of the quarterly shift in<br />
which the episode occurs and potential dismissal from the program.<br />
Motivation and Initiative in Learning-Primary Clinician<br />
• The student demonstrates initiative and responsibility in aspects of patient care including, but<br />
not limited to - researching conditions, treatments, and disease processes and integrates this<br />
information into case discussion, preview and review.<br />
• The student demonstrate initiative and responsibility in the time management areas of patient<br />
care including, but not limited to – attendance, and appropriate time management for each visit.<br />
• The student reads patient charts, reviews diagnostic testing and is prepared for patient visits,<br />
contributing the information to case preview, review and discussion.<br />
• The student conducts research into etiology and treatment and integrates that information into<br />
case discussion and management, preview and review.<br />
• The student has integrates the information obtained from the chart on past treatment and<br />
out<strong>com</strong>es and incorporates that information into patient management.<br />
• The student reviews in<strong>com</strong>ing medical records and integrates the information into case<br />
discussion by the next patient visit.<br />
• The student utilizes down time on the shift to improve clinical knowledge and skills by<br />
practicing physical exams, hands on treatment, research, treatment modalities and/or<br />
pathophysiology without supervisor stimulus.<br />
• The student sits in on case discussions of other primary clinicians using the time to learn and<br />
contribute to the group education.<br />
The student is respectful of their role and the roles of other members of the team, and supports<br />
them in the fulfillment of their duties.<br />
To rectify a PC in this category, the student must be observed on each shift actively pursuing<br />
improvement of their clinical skills for an equal number of hours that were not well spent on their<br />
clinical shift. They will turn in two case studies they have evaluated. The supervisor in question has the<br />
option of creating a different process for rectification of this skill as meets the needs of the student in<br />
question. Other supervisors may be the monitors of this activity.<br />
This skill is mandatory for a practicing physician. Self-motivation and life-long learning are<br />
hallmarks of a <strong>com</strong>petent and safe practitioner.<br />
Incorporation of Clinic Policies and Procedures-Teamwork-Primary Clinician<br />
• The student will demonstrate <strong>com</strong>petence in this area by adhering to all clinic and university<br />
policies outlined in the clinic student handbooks and catalogues.<br />
• The student will follow the attendance and substitution policy of the clinic.<br />
• The student focuses on utilizing regulations and teamwork to enhance the quality of the<br />
patient visit and to ensure patient safety.<br />
36
The student will demonstrate professional code of conduct and ethics in the manner they conduct<br />
their practice and professional activities. This will include honesty, integrity and responsibility for<br />
individual judgments and actions. The practitioner will disclose all potential conflicts of interest<br />
that may arise during patient treatment.<br />
To rectify a PC in this area, the student must score 80% or more on a quiz that will cover the policies<br />
and procedures outlined in the clinic student handbook. No further violations of policy or procedure<br />
may occur during the duration of clinical training. As noted in the handbook, certain violations are<br />
subject to immediate failure or dismissal from the clinical training program and the university.<br />
CLINICAL SKILLS-Primary Clinician<br />
Interview Skills<br />
• The student obtains a thorough case history on the initial office visit as outlined in this manual<br />
and in “A Guide to Physical Examination and History Taking” by Bates, that includes, but is<br />
not limited to:<br />
HPI-History of the Present Illness<br />
Past Medical History<br />
Family History<br />
Psychosocial and Lifestyle History<br />
Pertinent Review of Systems<br />
Current Medication and Supplement dosing<br />
• The student demonstrates integrates special interview techniques in gynecology, drug and alcohol<br />
dependence, STD risk profile, psychological risk and history, etc.<br />
• The student can ascertain the present risk to safety of the patient and others when it is indicated to<br />
do so.<br />
• The student integrates pertinent positive and pertinent negative information obtained during the<br />
interview to focus questioning toward development of a diagnostic and treatment plan.<br />
• The student assimilates the written and verbal information gathered during the patient visit into<br />
their differential during the visit to maximize use of the allotted visit time.<br />
• The student obtains this information during the interview in a respectful and non-judgmental<br />
manner.<br />
To rectify a PC grade, the student will participate in three mock interviews to demonstrate the above<br />
skills. The conditions utilized in the interview will be taken from the condition list in the clinic<br />
notebook. The student must demonstrate these skills successfully in two of the three cases if an early to<br />
mid-primary and in all cases if a mid to late primary.<br />
Physical Examination Skills-Primary Clinician<br />
• The student <strong>com</strong>petently performs an exam within accepted performance guidelines on<br />
request of the supervisor, or as indicated by patient chief <strong>com</strong>plaint, within a reasonable time<br />
frame.<br />
• The student has all equipment in working order.<br />
• The student notifies the supervisor of all positive findings so they may be reviewed during the<br />
patient visit by the supervisor. Failure to do so makes the clinician eligible for sanctions.<br />
• The student performs all exams as required and adapts to individual patient circumstances and<br />
<strong>com</strong>fort.<br />
• The student has appropriate faculty supervision before performing any breast exam or male or<br />
female genital exam. Failure to obtain supervision for genitourinary examinations will result in<br />
sanctions being applied to the student.<br />
The student applies proper awareness and observance of public health and sanitation rules by<br />
washing their hands, cleaning the tables and equipment after each exam and shift. The equipment<br />
may include lights, gynecological lights, tables, mirrors, and personal medical equipment including<br />
37
their stethoscope. Proper hand washing includes washing for 20 seconds, rinsing and drying the<br />
hands thoroughly.<br />
To rectify a PC the student must perform three exams, reflecting the appropriate skill level, during<br />
interim or substitute shifts. The student must pay for the services of a model to perform the exams. In<br />
some circumstances the student may use the male and female pelvic models to practice these skills if<br />
authorized by a resident or physician.<br />
Overall Case Management-Primary Clinician<br />
• The student reveals integration of information and knowledge in their management of<br />
treatment by monitoring patient progress and suggests alterations to the plan when<br />
circumstances indicate change is due.<br />
• The student integrates clinical application of patient management techniques by following up<br />
on referrals, diagnostic testing, and re<strong>com</strong>mending change to the plan as indicated by patient<br />
progress and/or test out<strong>com</strong>e with faculty supervision and authorization.<br />
• The student follows up with authorized phone calls to the patient when indicated by the<br />
supervisor to do so.<br />
• The student integrates individual pathophysiology and lifestyle factors into their consideration<br />
of treatment changes.<br />
• The student continues to research and integrate new information into the treatment plan as<br />
indicated necessary by patient progress.<br />
• The student monitors patient progress and stimulates change or referral when patients do not<br />
respond to treatment in a timely manner.<br />
• The student must demonstrate the ability to take an appropriate history, perform the<br />
appropriate physical exam(s), meet with supervisor for case discussion, make an assessment<br />
and diagnosis, create a treatment plan, and successfully <strong>com</strong>municate that information to the<br />
patient within the allotted period of time.<br />
• The student presents the clinical cases in the prescribed format at case preview and review<br />
and actively participates in discussion of cases managed by other students.<br />
• The student integrates the principles of naturopathic medicine and the therapeutic order into<br />
their case management and can discuss how they impact the management of the case.<br />
<br />
The student demonstrates an understanding and application of ethical behavior in the management<br />
of patient care.<br />
To rectify a PC grade, the student will present treatment plans for three FOC cases as assigned by the<br />
supervising faculty or their designate. They will adapt those treatment plans through two ROC visits.<br />
The plans will be graded for <strong>com</strong>plexity and knowledge based on the current educational status of the<br />
student.<br />
Medical Record Keeping (Charting)-Primary Clinician<br />
• The student must <strong>com</strong>plete the medical record within 24 hours of the patient visit unless<br />
exception is granted by the supervisor. Corrections or changes made to the chart must be<br />
<strong>com</strong>pleted within 24 hours unless exception is granted by the supervisor.<br />
• Record notes with basic case information, including assessment and plan, are to be left in an<br />
in<strong>com</strong>plete chart.<br />
• NO MEDICAL RECORD IS TO LEAVE CLINIC PREMISES. SANCTIONS WILL BE<br />
INVOKED WITH VIOLATION OF THIS POLICY.<br />
• The medical record is to be <strong>com</strong>pleted in the accepted clinic SOAP format as defined in the<br />
earlier section of this handbook. The pages are to be properly organized in the record folder.<br />
• The student will write in black ink only and handwriting must be legible or typed charting<br />
notes utilized.<br />
38
• The student will use the current accepted forms for each visit and note the patient name, date<br />
of birth, and date of visit on each page.<br />
• If more than one page is used to record a ROC, each page will be numbered.<br />
• The supporting record pages including the visit summary sheet, medication list, and patient<br />
health profile sheet are to be brought up to date for each visit.<br />
• Accepted medical terminology as noted in the global edition of the handbook, including<br />
abbreviations, is to be used in record keeping.<br />
• Spelling and grammar are correct and appropriate, including names of medication.<br />
• Treatment section of the medical record should be <strong>com</strong>pleted, including the formula for any<br />
tincture or tea prescribed. It is not appropriate to refer readers to the treatment plan or previous<br />
visit notes for this information.<br />
• Patient treatment plan should include the rationale for each re<strong>com</strong>mendation and how long it<br />
should be continued. They should also include any previously prescribed medication that is to<br />
be continued as well as any that are to be discontinued. Each treatment plan should stand alone.<br />
To rectify a PC grade the student must <strong>com</strong>plete three medical records appropriately. The records must<br />
be <strong>com</strong>pleted on substitution or interim shifts.<br />
Incorporation of Academic and Didactic Knowledge in the Clinical Setting-Primary Clinician<br />
• The student must demonstrate integration of didactic knowledge as they relate to patient<br />
<strong>com</strong>plaints and diagnosis during case discussion, case preview and review.<br />
• The student must demonstrate the ability to triage acute patients in the clinical setting.<br />
• The student must regularly demonstrate evidence of case preparation by including their<br />
pertinent research into case discussions.<br />
• The student must integrate laboratory and diagnostic testing and the impact of the results of<br />
that testing on diagnosis and treatment of the patient.<br />
• The student must demonstrate integration of their knowledge of the psychological aspects of<br />
patient <strong>com</strong>plaints, diagnoses and methods of intervention.<br />
The student must integrate the principles of naturopathic medicine and therapeutic order into<br />
case discussions and management.<br />
To rectify a PC the student must demonstrate the above skills on two to four cases as indicated by the<br />
supervisor that are included on the required conditions list, to supervising faculty or their designate.<br />
Application of Naturopathic Therapeutics-Primary Clinician<br />
• The student exhibits a growing depth and breadth of knowledge in all aspects of naturopathic<br />
therapeutics.<br />
• The student prepares and presents therapeutic options for each case and can discuss rationale,<br />
strategy and therapeutic goal during presentation in case discussion and case preview.<br />
• The student demonstrates the ability to apply therapies appropriate to each patient’s<br />
circumstances.<br />
• The student is able to prepare a pertinent treatment plan in an acute situation within the given<br />
time constraints.<br />
• The student is familiar with the contents of supplement formulas prescribed for the patient.<br />
• The student is a safe practitioner and exhibits understanding of actual and potential<br />
interactions between medications, supplements, food, nutrients and botanical medicines.<br />
• The student is able to identify all of the treatment modalities that may be appropriate for<br />
treatment of the individual patient condition and can discuss the rationale and any indicated<br />
safety concerns for the use of each modality.<br />
• The student is able to re<strong>com</strong>mend effective and safe doses of supplements, botanicals and<br />
homeopathic remedies.<br />
39
• The student incorporates the use of the naturopathic principles and the therapeutic order into<br />
the treatment plan and can document their action over time.<br />
To rectify a PC grade, the student will be assigned five cases from the supervisor’s caseload and be<br />
required to formulate specific alternative treatment plants for the given conditions. These treatments<br />
will be reviewed and discussed with the supervisor. The skills indicated above must be demonstrated in<br />
at least four of the cases.<br />
SANCTIONS/FAILURE EVENTS<br />
If a student does not adequately perform one or more of any of the critical shift <strong>com</strong>petencies on any<br />
given day or does not achieve <strong>com</strong>petency on any two or more of the non-critical <strong>com</strong>petencies, the<br />
supervisor has the right to issue a sanction to the student. A written warning may precede this sanction,<br />
though that depends on the nature of the event. A second incident must result in a written sanction. A<br />
written sanction results in the loss of all of the daily shift hours and patient contacts for the shift under<br />
review, and may include additional penalties. Two sanctions on the same shift will automatically result<br />
in a failure grade for that entire shift with the loss of all patient contacts and hours earned on that shift.<br />
This means the student must pay for and retake an entire shift.<br />
Students will be issued a sanction when they are found to have violated any of the policies of the clinic,<br />
including, but not limited to:<br />
• Breaching patient confidentiality.<br />
• Removing any patient ID information from the clinic.<br />
• Acting in an unprofessional or disrespectful manner to patients, staff, faculty and peers at any<br />
time, including when present in the clinic and not on shift.<br />
<br />
• Failing to <strong>com</strong>ply with Blood Borne Pathogen and other safety policies and procedures.<br />
Practicing medicine without a license.<br />
The severity of the sanction will depend on the severity of the offense and may range from loss of<br />
clinical hours and patient contacts to suspension from the clinic or school. The involved supervisor and<br />
the program dean, or their designate, will determine the type of sanction.<br />
Sanctions are not grades and therefore are not subject to appeal under the appeal of grade policy. A<br />
student may issue a grievance according to the grievance procedure as outlined in the student<br />
handbook.<br />
PHYSICAL EXAM GUIDELINES<br />
Clinicians are expected to know all physical exams. The Physical/Clinical Diagnosis class teaches<br />
clinicians to perform a thorough PE. Even if clinicians haven’t performed this type of exam recently,<br />
they must be adept in performance of each exam at all times, so constant practice is re<strong>com</strong>mended.<br />
Vitals must be taken at each visit, including physical medicine shifts. Vitals include height and weight.<br />
Clinicians must have their equipment in working order for each shift. It should be checked the day<br />
before to ensure that everything works well, batteries are recharged, etc.<br />
A doctor must be present in the room during breast and genitourinary exams of both male and<br />
female patients. This is to guard the safety of the patient, protect the clinic, clinician and supervisor<br />
legally and to ensure accurate performance and education.<br />
Alert the supervisor of all questionable or abnormal findings obtained during the physical examination.<br />
The attending physician must recheck all positive findings. Failure to notify the physician of<br />
abnormal findings obtained during a physical exam so they can verify those findings makes the<br />
student eligible for sanctions. Repeated failure to notify the supervisor of positive findings will<br />
result in sanctions that may include failure of the shift.<br />
40
Contract for Blood Borne Pathogen and Injection Safety<br />
This contract is to be signed by each student after they have received the blood<br />
borne pathogen and injection safety review update. All students at any clinical site<br />
associated with Bastyr University must have a signed copy of this contract on file<br />
with the safety office to continue their clinical education.<br />
I have participated in the biohazard and blood borne pathogen safety review. I agree to<br />
follow the biohazard and blood borne pathogen safety procedures at all times and<br />
recognize that failure to do so will result in sanctions being imposed upon me.<br />
Student Name (print) ________________________________<br />
Signature _________________________________ Date _____________________<br />
Return this <strong>com</strong>pleted form to:<br />
Bastyr Center for Natural Health<br />
Faculty Administrative Assistant<br />
Room S206<br />
41
SAFETY<br />
Please review the general clinic safety section in the Global <strong>Module</strong> Handbook for the clinic policies and<br />
regulations.<br />
In the event a blood borne pathogen accident or incident occurs and you or the patient may have been<br />
exposed, immediately notify your supervisor, who will ensure the health and safety of all involved in the<br />
incident. Please follow the BBP incident procedure outlined elsewhere in this handbook.<br />
The following two charts are a review of the Blood Borne Pathogen safety policy and procedures. Please<br />
note that deliberate failure to <strong>com</strong>ply with Blood Borne Pathogen safety policies and procedures may<br />
result in a sanction.<br />
Blood Glucose Check Procedure:<br />
1. Assemble equipment next to patient. Place sharps container no more than ½ step away from<br />
injection area.<br />
2. Wash and glove hands.<br />
3. Insert testing strip into glu<strong>com</strong>eter. There must be a flashing drop of blood on the<br />
glu<strong>com</strong>eter screen in order to proceed with test.<br />
4. Swab lateral part of patient’s 4th fingertip with alcohol.<br />
5. Using lancet, prick swabbed area.<br />
6. Immediately, put lancet into sharps container.<br />
7. Touch and hold the drop of blood to the edge of the “Comfort Curve” on the testing strip.<br />
8. Apply a cotton ball and/or band aid to bleeding site.<br />
9. After reading blood glucose level, immediately put testing strip and soiled cotton ball into<br />
biohazard container.<br />
10. Clean up after yourself and put equipment away.<br />
11. Wash hands.<br />
12. Document procedure and test results.<br />
42
L/B<br />
<br />
HOW TO: INJECTIONS A<strong>ND</strong> FINGERPRICKS<br />
EQUIPMENT NEEDED:<br />
1. SHARPS CONTAINER<br />
2. SUPERVISOR<br />
3. GLOVES<br />
4. Band aid<br />
5. Cotton balls<br />
6. Alcohol<br />
7. a. Syringe and needle (B12/Complex injection) OR<br />
b. Lancet (blood glucose check)<br />
9. a. Bottle of B12 and/or B <strong>com</strong>plex OR<br />
b. Glu<strong>com</strong>eter kit (blood glucose check)<br />
IF YOU ARE MISSING ANY ITEMS ON THIS LIST,<br />
YOU MAY NOT PROCEED!!<br />
B12/B Complex Injection Procedure:<br />
1. Assemble equipment next to patient. Place sharps container no more than ½ step away from<br />
injection area.<br />
2. Check vial for expiration date.<br />
3. Wash and glove hands.<br />
4. Expose injection site.<br />
5. Palpate lateral aspect of tissue between greater trochanter and PSIS, feeling for muscular tissue<br />
with minimal adipose tissue and no bone palpable.<br />
6. Swab area with alcohol.<br />
7. Swab top of vial(s) with alcohol.<br />
8. Push appropriate amount of air into vial (Ex: 1:1 ratio air:vitamin in multi dose vial; 1:2 ratio<br />
air:vitamin in single dose vial).<br />
9. Draw up appropriate amount of B12 or B <strong>com</strong>plex.<br />
10. Withdraw needle from vial.<br />
11. Repeat steps 7-9 if also using B <strong>com</strong>plex.<br />
12. Flick syringe to allow bubbles to escape.<br />
13. With a flick of the wrist, inject needle into swabbed area, pull back to ensure no blood/not in a<br />
vein. If no blood retracts, inject at a moderate rate. Use distraction by scratching area local to<br />
injection with gloved finger.<br />
14. Continue to depress plunger, needle will automatically retract.<br />
15. Immediately put syringe into sharps container.<br />
16. Apply cotton ball and/or band aid to injection site as needed.<br />
17. Clean up after yourself and put supplies away.<br />
18. Wash hands.<br />
19. Document injection.<br />
(Ex: 1 cc B12 and 1 cc B <strong>com</strong>plex injected IM R gluteal m. Lot #: ___; Expiration date: ___. Pt<br />
tolerated injection well, or describe any problems that occurred during the injection).<br />
43
COMPETENCIES<br />
Students at Bastyr Center for Natural Health will demonstrate <strong>com</strong>petence in the clinical skills required<br />
for proficiency in their chosen degree.<br />
UNIVERSITY GLOBAL COMPETENCIES<br />
Communications skills<br />
Students at BCNH will develop writing and speaking skills that will enable them to <strong>com</strong>municate in a<br />
professional, appropriate and effective manner to colleagues, other health care providers, patients, and the<br />
public. Students will be able to actively listen to their patients, colleagues, other health care providers and<br />
the public and to integrate this information into their case management. Students will develop their<br />
clinical intuition. Students will develop literacy in medical and professional information.<br />
Critical Thinking<br />
Students at BCNH will demonstrate the ability to think critically illustrating their knowledge,<br />
<strong>com</strong>prehension, application, analysis, synthesis and evaluation of information.<br />
Professional Behavior<br />
Students at BCNH will conduct themselves professionally and responsibly with regards to medical ethics,<br />
<strong>com</strong>passionate behavior, cross-cultural differences, respectful <strong>com</strong>munication and personal health and<br />
wellness.<br />
CLINIC QUALITIES<br />
Heritage<br />
Students at BCNH will develop an understanding and acknowledgement of the rich heritage inherent in<br />
naturopathic medicine as well as all other forms of medicine. Students will appreciate the philosophy and<br />
essence of holism that naturopathic medicine embodies.<br />
Integration<br />
Students at BCNH will develop the skills and professional <strong>com</strong>petence necessary to demonstrate<br />
integration between disciplines, modalities and philosophies.<br />
Career Management<br />
Students at BCNH will develop <strong>com</strong>petence relating to professional responsibilities, career and business<br />
management. The students will participate in their professional <strong>com</strong>munity.<br />
44
PRINCIPLES OF NATUROPATHIC MEDICINE<br />
The Healing Power of Nature [Vis Medicatrix Naturae] Naturopathic medicine recognizes an inherent<br />
ability in the body which is ordered and intelligent. Naturopathic physicians act to identify and remove<br />
obstacles to recovery and to facilitate and augment this healing ability.<br />
Identify and Treat the Causes [Tolle Causam] The naturopathic physician seeks to identify and remove<br />
the underlying causes of illness, rather than to eliminate or merely suppress symptoms.<br />
First Do No Harm [Primum Non Nocere] Naturopathic medicine follows three principles to avoid<br />
harming the patient:<br />
1. utilize methods and medicinal substances which minimize the risk of harmful side effects<br />
2. avoid, when possible, the harmful suppression of symptoms<br />
3. acknowledge and respect the individual’s healing process, using the least force necessary to<br />
diagnose and treat illness.<br />
Doctor as Teacher [Docere] Naturopathic physicians educate the patient and encourage selfresponsibility<br />
for health. They also acknowledge the therapeutic value inherent in the doctor - patient<br />
relationship.<br />
Treat the Whole Person Naturopathic physicians treat each individual by taking into account physical,<br />
mental, emotional, genetic, environmental, social and other factors that affect health. Since total health<br />
also includes spiritual health, naturopathic physicians encourage individuals to pursue their personal<br />
spiritual path.<br />
Prevention Naturopathic physicians emphasize the prevention of disease, assessing the risk factors and<br />
hereditary susceptibility to disease and making appropriate interventions to prevent illness. Naturopathic<br />
medicine strives to create a healthy world in which humanity may thrive.<br />
Wellness Naturopathic medicine seeks to establish and maintain optimum health and balance; wellness is<br />
a state of being healthy, characterized by a balance in emotion, thought and action. Wellness is inherent in<br />
everyone, no matter what disease(s) is/are being experienced. If wellness is recognized and experienced<br />
by an individual, they will more quickly heal a given disease than direct treatment of the disease alone.<br />
(This principle was adopted by Bastyr University and added to the six principles.)<br />
THERAPEUTIC ORDER<br />
The therapeutic order is used to assist developing clinicians to focus their treatment method using the<br />
lowest possible force to assist patients in regaining their health. The treatment chosen is one that best<br />
addresses the needs of the patient at one moment in time. The force of the chosen treatment may decrease<br />
as patients regain their health.<br />
Determinants of Health<br />
Assess/Stimulate the Healing Power of Nature<br />
Tonify Systems<br />
Correct Structural Integrity<br />
Symptom Based Naturopathic Treatment<br />
Symptom Based Synthetic Treatment<br />
Higher Force Interventions<br />
45
CLINICAL COMPETENCIES<br />
During clinical training at the Bastyr Center for Natural Health, naturopathic medicine students are<br />
required to demonstrate <strong>com</strong>petence in numerous clinical skills. Those skills begin with the secondary<br />
skills and advance to the primary skills, each building upon the next. Skill <strong>com</strong>petence is tracked on the<br />
following sheets. These requirements are not linked to the clinic shift grades. They are a separate<br />
requirement, and a signed <strong>com</strong>petency does not assure a grade of AC on any clinic shift.<br />
Patient care, counseling, homeopathy, and physical medicine all have specific forms to help document<br />
that skill development. Supervising faculty will evaluate and confirm your <strong>com</strong>petence on a quarterly<br />
basis. Each quarter the sheet is signed by your supervising physician. Keep a copy for yourself and turn<br />
the original in to the clinic registration staff to prove <strong>com</strong>pletion of the <strong>com</strong>petencies. Following you will<br />
find the clinical <strong>com</strong>petencies for secondary clinicians and primary clinicians and the timelines we<br />
suggest you follow in order to <strong>com</strong>plete them in time for graduation.<br />
All secondary <strong>com</strong>petencies must be signed before a clinician may advance to primary status.<br />
All primary <strong>com</strong>petencies must be signed before a primary may graduate.<br />
Tracking Clinical Competencies<br />
Each quarter you receive an updates from the registrars office that notes <strong>com</strong>petencies you have<br />
<strong>com</strong>pleted. Check that each quarter to ensure that you are being credited appropriately.<br />
Tracking for Secondary Clinicians Clinical <strong>com</strong>petencies (3 or 4) Patient Care<br />
Clinical <strong>com</strong>petencies -Physical Medicine<br />
Clinical <strong>com</strong>petencies - Counseling<br />
Clinical <strong>com</strong>petencies - Dispensary<br />
Tracking for Primary Clinicians (On your quarterly updates from the registrar)<br />
Clinical <strong>com</strong>petencies - Patient Care<br />
Clinical <strong>com</strong>petency - Counseling<br />
Clinical <strong>com</strong>petency - Physical Medicine<br />
Elective <strong>com</strong>petency – Homeopathy<br />
Clinical <strong>com</strong>petencies – Conditions<br />
Clinical <strong>com</strong>petencies - Physical Examination<br />
Clinical <strong>com</strong>petency – OSCE examination<br />
46
SECO<strong>ND</strong>ARY<br />
COMPETENCIES<br />
PATIENT CARE 1 PATIENT CARE 2 PATIENT CARE 3<br />
Dispensary<br />
<strong>com</strong>petency (3) Have supervisor initial when Completed------- -------------------------<br />
Build patient<br />
treatment notebookelectronic<br />
or written (3)<br />
FOC charting One Chart Two Charts Two Charts<br />
ROC charting Two Charts Three Charts Three Charts<br />
HEENT exam<br />
(perform 1)<br />
Respiratory Exam<br />
(perform 1)<br />
Cardiac Exam<br />
(perform 1)<br />
Neuro Exam<br />
(perform 1)<br />
Abdominal Exam<br />
(perform 1)<br />
Musculoskeletal<br />
Exam (1)<br />
Update CPR (annually)<br />
47
STUDENT EVALUATION -- PRIMARY <strong>ND</strong> PATIENT CARE COMPETENCY Grade each category as: AC /<br />
PC / F<br />
STUDENT’S NAME: DATE: / / QUARTER: F W SP SU<br />
(Please Print)<br />
(Circle or Bold)<br />
DAY: M T W TH F S SHIFT: 1.0 1.1 2.0 2.1 3.0 3.1 Offsite:<br />
(Circle or Bold) (Circle or Bold) (Name Of External Site)<br />
I. PROFESSIONAL SKILLS<br />
A. COMMUNICATION SKILLS<br />
1. Demonstrates empathy to the patient and speaks clearly to effectively establish<br />
rapport<br />
2. Uses appropriate language and terminology to teach patient about their health<br />
(Docere)<br />
3. Effectively <strong>com</strong>municates treatment re<strong>com</strong>mendations to the patient as directed by<br />
the supervisor<br />
4. Demonstrates listening skills and includes all the patient concerns in charting and<br />
discussion<br />
5. Conducts self in an open and non-judgmental manner in obtaining and<br />
<strong>com</strong>municating information<br />
6. Demonstrates professionalism, respect and collegiality in all interactions with<br />
supervisor, staff and peers<br />
7. Demonstrates the ability to articulate and summarize case presentations using<br />
accurate medical terminology<br />
B. MOTIVATION A<strong>ND</strong> INITIATIVE SKILLS<br />
1. Demonstrates self-initiative and responsibility in all aspects of patient care<br />
2. Integrates their research and all information in the patient chart before each visit<br />
3. Tracks and follows through on all laboratory and diagnostic testing that is ordered<br />
4. Reviews charts and all requested medical records and assimilates that information<br />
into diagnosis and treatment<br />
5. Utilizes down time on rotations to improve clinical knowledge and skills<br />
6. Demonstrates initiative and responsibility in time management in all areas of<br />
patient care<br />
C. INCORPORATION OF CLINIC POLICIES A<strong>ND</strong> PROCEDURES<br />
1. Adheres to policies to enhance patient experience and student education<br />
49<br />
2. Utilizes regulations and teamwork to ensure patient safety<br />
II. CLINICAL SKILLS<br />
A. INTERVIEW SKILLS<br />
1. Obtains a thorough case history during initial and return office visit<br />
2. Demonstrates the ability to perform special interview techniques as needed<br />
3. Demonstrates the ability to obtain information to ascertain the patient’s risk and/or<br />
safety<br />
4. Demonstrates the ability to effectively assimilate the written and verbal information<br />
obtained in the visit to develop a plan<br />
5. Demonstrates the ability to obtain all necessary information in a respectful and timely<br />
manner<br />
B. PHYSICAL EXAM SKILLS (FIRST DO NO HARM & FI<strong>ND</strong> THE CAUSE)<br />
1. Demonstrates the ability to perform a <strong>com</strong>petent exam as indicated by needs of<br />
patient within a reasonable time<br />
2. Has all equipment in working order and equipment necessary on hand in the room<br />
prior to the visit<br />
3. Notifies a supervisor of all positive and pertinent negative findings in a timely<br />
manner so they may be reviewed<br />
4. Competently performs all exams as needed for the visit adapting to individual patient<br />
need and <strong>com</strong>fort level<br />
5. Has appropriate faculty supervision before performing any male or female exam<br />
C. OVERALL CASE MANAGEMENT SKILLS (TREAT THE WHOLE PERSON)<br />
1. Demonstrates understanding of treatment goals and monitors patient progress<br />
2. Indicates <strong>com</strong>petence in following through on referrals and laboratory and diagnostic<br />
testing<br />
3. Integrates pertinent pathophysiology in their consideration of treatment choice and
change<br />
4. Continues to research and integrate new information into the treatment plan<br />
C. OVERALL CASE MANAGEMENT SKILLS (TREAT THE WHOLE PERSON)<br />
(CONTINUED)<br />
5. Monitors patient progress and re<strong>com</strong>mends to supervisor changes or referrals when patients do<br />
not progress as expected<br />
6. Demonstrates the ability to perform all aspects of a visit with in the allotted time frame<br />
7. Meets with the supervising physician as needed to monitor progress and provide<br />
optimal medical care<br />
8. Integrates principles of naturopathic medicine and the Therapeutic Order into the<br />
development, application and management of treatment<br />
D. CHARTING SKILLS<br />
1. Completes charting following clinic guidelines within the allotted time frame<br />
2. Charting is <strong>com</strong>pleted using the accepted SOAP format<br />
3. Charting is demonstrated as professional by incorporating appropriate information,<br />
language, spelling and grammar<br />
E. INCORPORATING ACADEMIC A<strong>ND</strong> DIDACTIC KNOWLEDGE INTO<br />
CLINICAL SETTING<br />
1. Regularly demonstrates understanding of pathophysiology, anatomy, biochemistry and<br />
physical diagnosis and integrates this into case discussion, preview and review and<br />
evaluation and management of the patient<br />
E. INCORPORATING ACADEMIC A<strong>ND</strong> DIDACTIC KNOWLEDGE INTO<br />
CLINICAL SETTING (CONTINUED)<br />
2. Regularly demonstrates the ability to triage patient <strong>com</strong>plaints correctly identifying and<br />
prioritizing problems and actions<br />
3. Regularly demonstrates case preparation by familiarity with medical record and by<br />
including research into discussions accurately for each patient<br />
4. Demonstrates skill by accurately ordering appropriate laboratory and diagnostic testing<br />
and incorporating results to monitor patient progress<br />
5. The student demonstrates integration of the psychological and spiritual aspects of<br />
patient care into case management<br />
F. APPLICATION OF NATUROPATHIC THERAPEUTICS<br />
1. Demonstrates expanding depth and breadth of knowledge of therapeutics throughout<br />
the quarter<br />
2. Prepares and presents therapeutic options in a timely manner and can effectively<br />
discuss rationale and strategy for each<br />
3. Demonstrates safety an knowledge in their choice of treatment, prescribed dosage and<br />
duration of treatment<br />
4. Demonstrates the integration of naturopathic principles and therapeutic order into each<br />
plan<br />
5. Integrates naturopathic principles, philosophy and Therapeutic Order into evaluation,<br />
management and treatment of each patient<br />
COMMENTS: (*FACULTY – please attach a separate sheet with the student’s information at the top if you choose to make additional <strong>com</strong>ments beyond this space.)<br />
SUPERVISOR’S NAME:<br />
(PLEASE PRINT)<br />
SUPERVISOR’S SIGNATURE:<br />
50
<strong>ND</strong> PRIMARY CLINICAL COMPETENCIES<br />
Student Name:<br />
Competency<br />
1. Recertified CPR status (current<br />
CPR) each year. Must present card to<br />
supervisor.<br />
2. Communicates knowledge of risk<br />
and safety in prescription of injections<br />
and demonstrates safety and<br />
<strong>com</strong>petence in provision of<br />
intramuscular injection &/or IV<br />
therapy &/or Minor office procedures.<br />
3. Has demonstrated <strong>com</strong>petence in<br />
writing referral letters to other<br />
physician/specialists.<br />
4. Has demonstrated skill & ability in<br />
writing treatment summary letters for<br />
physicians or chart summary.<br />
5. Discuss birth control options,<br />
efficacy and safety with patient<br />
including protection from STDs.<br />
6. Effectively utilizes and integrates<br />
multiple methodologies and/or<br />
modalities within patient management.<br />
7. Acts within ethical parameters (see<br />
the ethics benchmark).<br />
8. Demonstrates CPT and ICD-9<br />
coding knowledge in billing and<br />
charting.<br />
9. Integrates quality of service into<br />
case discussion with patients.<br />
10. Effectively applies homeopathic<br />
prescribing into the treatment of<br />
patients.<br />
11. Creates and prescribes effective<br />
botanical formulas into the treatment<br />
of patients.<br />
Quarter/Year:<br />
Quarter 4/5 Quarter 6/7 Quarter 8<br />
Supervisor<br />
Sig/Date<br />
Comments<br />
Supervisor<br />
Sig/Date<br />
Comments<br />
Supervisor<br />
Sig/Date<br />
Comments<br />
51
<strong>ND</strong> PRIMARY CLINICAL COMPETENCIES - CO<strong>ND</strong>ITIONS<br />
A thorough knowledge of the etiology, assessment or diagnosis, management and treatment of each of<br />
the following categories of disease or conditions must be demonstrated by each student. For credit the<br />
student should have seen the patient for an initial and at least 1 follow up visit.<br />
Acute conditions do not require a follow-up in person, but may be made by telephone. The student<br />
must also present standard and naturopathic treatment options, risks and benefits<br />
Student Name:<br />
Quarter/Year:<br />
Supervisor Competency - may include but is not limited to the listed diagnoses.<br />
Initial/Date If line follows a category, must present at least two cases.<br />
Cardiovascular disease: (HTN, hypercholesterolemia, coronary artery disease, angina, etc.)<br />
Dysglycemia: (diabetes-NIDDM or IDDM, or hypoglycemia)<br />
Upper gastrointestinal disorder: (GER, GERD, PUD, dyspepsia)<br />
Lower gastrointestinal disorder: (IBD, IBS, Crohn’s, UC, Celiac, constipation, diarrhea)<br />
(2 nd -Upper or lower)<br />
Hepatobiliary disease: (cholelithiasis, hepatitis, metabolic liver disease)<br />
Cancer prevention and/or treatment<br />
Skin diseases: (eczema, psoriasis, exanthums, acne, etc...)<br />
Hematological disorders: (anemia, leukemia, dyscrasias, etc…)<br />
Osteoporosis or osteopenia<br />
Female gynecological conditions: (FBD, menopausal management, PMS, polycystic<br />
ovary disease, dysmenorrhea, endometriosis, management of abnormal pap smear,<br />
etc.)<br />
Male genitourinary conditions: (prostate disorder, epididymitis, varicocele, etc...)<br />
Acute Respiratory Tract Disorder: (otitis media, pharyngitis, bronchitis, etc…)<br />
Chronic Respiratory Tract Disorder: (chronic bronchitis, asthma, emphysema, chronic<br />
sinusitis, allergies, etc…)<br />
Nutritional deficiencies or inadequacies<br />
Acute Urinary tract and/or kidney disorders: (UTI, pyelonephritis, glomerulonephritis,<br />
etc.)<br />
Mental/emotional illness<br />
Nervous system disorder: (insomnia, dizziness, seizure, paresthesia, etc…)<br />
HIV: (opportunistic infections associated with HIV+, HIV risk assessment)<br />
Endocrine disorders<br />
Auto-immune Disease: (RA, SLE, Hashimoto’s, etc…)<br />
Musculoskeletal conditions - acute<br />
Musculoskeletal conditions - chronic<br />
52
Physical Exam Benchmark Competencies<br />
Each exam is listed in the Physical Exam outline section(see Appendix). The exams are to be<br />
performed from memory and observed in full by the supervising doctor. The exams must be performed<br />
<strong>com</strong>petently. Clinicians are encouraged to <strong>com</strong>plete their exams well in advance of their last patient<br />
care shift. A copy of this page is given to the Clinic registration staff upon <strong>com</strong>pletion.<br />
Supervisor<br />
Initial /<br />
Date<br />
Benchmark Primary Physical Exam Competencies<br />
Part of Exit Exam Prior to Graduation (last 4 quarters)<br />
Breast Exam (10 minutes)<br />
Female Gynecological Exam, pelvic (20 minutes)<br />
Male Reproductive Exam (20 minutes)<br />
Well Child Check-up, including developmental mile-stone assessment (20<br />
minutes)<br />
Complete Screening exam (30 minutes)<br />
HEENT Exam (10 minutes)<br />
Abdominal Exam (10 Minutes)<br />
Respiratory Exam (10 Minutes)<br />
Cardiovascular Exam (15 minutes)<br />
Musculoskeletal Exam (20 minutes)<br />
Neurological Exam 15 minutes)<br />
53
SPECIAL PROCEDURES/PROTOCOLS<br />
GYNECOLOGICAL CYTOLOGY SERVICES<br />
Papanicolaou (PAP) staining of endocervical, ectocervical and vaginal smears is an important aspect of<br />
women’s health care. Please see the attached description of the re<strong>com</strong>mended examination in the<br />
physical exam section of this notebook. A separate cytology notebook details the services offered, and<br />
is available from the client services staff. It includes sections on:<br />
•General information<br />
•Specimen collection<br />
•Patient statistical and follow-up reports<br />
•Terminology/classification standards<br />
•Special services<br />
Collection supplies including slides or SurePath/LiquiPap liquid medium, broom or cytobrush,<br />
modified Ayre spatula, and Pap Paks are available at no charge from the laboratory.<br />
PAP PROCEDURAL DIRECTIONS<br />
Almost all cancers of the cervix begin near the squamo-columnar junction. It is imperative, therefore,<br />
that smears be taken from this area. There are two collection media available: Pap Pak and SurePath<br />
Liquid Pap.<br />
Instructions for Using Pap Pak<br />
Prior to obtaining the cervical sample:<br />
•Write the patient’s name in pencil on the frosted end of the glass.<br />
•Have a Pap Pak open.<br />
•Indicate on the request form all pertinent information about the patient such as last menstrual<br />
period, radiation therapy, IUD, clinical cancer, hormone therapy and previous abnormal cytology.<br />
•Excess mucus should be removed from the uterine cervix and vagina before the samples are<br />
taken.<br />
Ectocervical Sample – Using a modified wooden Ayre spatula, obtain a sample from the ectocervix.<br />
Rotate and scrape the external OS. The sample material should be spread evenly along the length of the<br />
slide in a thin layer.<br />
Endocervical Sample – Using a cytobrush, obtain a second sample from the endocervix. Rotate within<br />
the endocervical canal. Please note that a cytobrush should not be used on pregnant patients. Roll the<br />
brush to spread the sample along the length of the slide in an even and thin layer. It is not an issue for<br />
evaluation if you mix the samples from the two areas.<br />
Fix immediately with the fixative from the Pap Pak or a spray.<br />
If hormonal evaluation is needed, an additional smear may be obtained by scraping the lateral vaginal<br />
wall. This sample should be thinly spread on a separate slide and fixed immediately with the fixative<br />
from the Pap Pak or spray. Label slide M.I. (Maturation Index) and note the request on the lab<br />
requisition form.<br />
Water based lubricant can be used on the speculum to enhance patient <strong>com</strong>fort. It does not obscure<br />
detail.<br />
The use of a cytobrush can significantly improve the collection of endocervical cells at the<br />
squamocolumnar junction. The following cautions govern their use:<br />
•You may want to inform your patients that there may be some minor painless spotting for a day<br />
or two following the PAP test.<br />
•NEVER reuse the cytobrush.<br />
•Insufficient clinical data exists regarding its use on pregnant patients. DO NOT USE on<br />
pregnant patients.<br />
•The cytobrush MUST NOT be used for sampling from the endometrium.<br />
54
Instructions for Using SurePath or LiquiPap<br />
Cervical Sample Collection: Insert the Rovers Cervix-Brush® into the endocervical canal. Apply<br />
gentle pressure until the bristles form against the cervix. Maintaining gentle pressure, hold the stem<br />
between the thumb and forefinger. Rotate the brush a full rotation in a clockwise direction. Placing<br />
your thumb against the back of the brush pad, gently disconnect the entire brush from the stem into the<br />
SurePath® preservative vial. Dispose of the stem. The spiral cytobrush may also be used to gather<br />
endocervical samples. The brush is swished thoroughly through the liquid medium to release cells.<br />
Cap and label vial: Place the cap on the vial and tighten. Label the vial and lab requisition form with<br />
patient name and/or number, physician name and date if desired.<br />
Lubricant: A small amount of water based lubricant may be used on the speculum in this collection<br />
without diminishing the quality of the sample collected.<br />
Exam Components:<br />
Each annual gynecological examination is ac<strong>com</strong>panied by a screening history that should include<br />
evaluation of current health status, lifestyle risk factors, health habits, and family history. The patient<br />
also receives screening exams that include HEENT, neck and lymph, cardiac, respiratory, abdominal<br />
and breast exams. The patient is also evaluated for the need of any additional screening tests indicated<br />
by the patient history.<br />
Other annual or preventive laboratory testing and/or imaging should be ordered at this time.<br />
WASHINGTON BREAST A<strong>ND</strong> CERVICAL HEALTH PLAN<br />
Bastyr Center for Natural Health is a participating site for the Washington Breast and Cervical Health<br />
Plan which offers gynecological exams and mammograms at no cost to underserved women between<br />
the ages of 40 and 64 years of age. The candidates must be screened by Dr. Jennifer Powell in medical<br />
records to ensure they qualify for the program. The program pays for the pap, mammogram and any<br />
care necessary after a positive finding on either exam. Please check with the Associate Clinical Dean<br />
or Dr. Powell to find out more about this program.<br />
55
<strong>ND</strong> PHYSICAL MEDICINE COMPETENCIES<br />
Mission Statement: To offer specialized care in physical medicine modalities in an atmosphere of<br />
excellence, professionalism and <strong>com</strong>passion, while simultaneously developing these skills and<br />
attributes in naturopathic medicine student clinicians.<br />
Clinical Competencies:<br />
• Skillful performance of listed hydrotherapy treatments<br />
• Skillful performance of listed physiotherapy treatments<br />
• Skillful performance of soft tissue assessment and integration of findings into treatment<br />
• Demonstrates knowledge and integration of orthopedic tests<br />
• Demonstrate knowledge and integration of neurological tests<br />
• Demonstrate skill in assessment of joint dysfunction due to subluxation/fixation through static and motion palpation<br />
• Demonstrate skill in formulation of a working diagnosis, prescribe and administer diagnostic<br />
testing and appropriate treatment (including hydrotherapy, physiotherapy, soft tissue manipulation,<br />
joint manipulation, nutrition, botanicals and homeopathy)<br />
Student Name:<br />
Supervisor<br />
Initial/Date<br />
HYDROTHERAPY TREATMENTS<br />
56<br />
Quarter/Year:<br />
Constitutional Hydrotherapy<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Hyperthermia (including Peat immersions)<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Wet Sheet Pack<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Colon Hydrotherapy<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Local Contrast<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Plasters and Poultices (peat, castor oil)<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Other Office and Home treatments (heating <strong>com</strong>press [wet sock], neutral bath,<br />
Epsom salts soak, contrast showers, other contrast applications)<br />
a. applications<br />
b. primary indications<br />
c. contraindications (continued on next page)
Student Name:<br />
Supervisor<br />
Initial/Date<br />
ELECTROTHERAPY TREATMENTS<br />
Diathermy<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Ultrasound (including phonophoresis)<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Low Volt NEMS<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Interferential NMES<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
DC (Galvanic) Iontophoresis<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
Low Level Laser Therapy (LLLT)<br />
a. application<br />
b. primary indications<br />
c. contraindications<br />
MANUAL THERAPIES<br />
Soft Tissue Assessment<br />
a. tissue texture evaluation<br />
b. muscle tension evaluation<br />
c. active/passive/resisted joint range of motion<br />
d. Indications for treatment<br />
e. Contraindications of treatment<br />
Local Tissue Release Techniques<br />
a. NMT<br />
b. Swedish massage basic techniques<br />
Muscle Energy (stretching) Technique (MES/MET)<br />
a. lower extremity/low back muscles<br />
b. upper extremity/neck/shoulders muscles<br />
ORTHOPEDIC ASSESMENT<br />
a. knee<br />
• Ant /Post drawer sign (continued on next page)<br />
Quarter/Year:<br />
57
Student Name:<br />
Supervisor<br />
Initial/Date<br />
ORTHOPEDIC ASSESMENT cont’d<br />
• Apley’s <strong>com</strong>pression/distraction tests<br />
• patella femoral grind<br />
• Lachman’s test<br />
• ballotable patella test (major effusion)<br />
• bulge test (minor effusion)<br />
b. hip/pelvis/SI<br />
• trendelenburg<br />
• test for leg length discrepancy<br />
• Patrick (Patrick-FABER) test<br />
• Ely’s test<br />
• Gaenslen’s test<br />
• Hibb’s test<br />
• Ober’s test<br />
• Ortolani click<br />
• pelvic rock test<br />
• Thomas’ test<br />
• Yoeman’s test<br />
c. low back/sciatica<br />
• Lasegue’s test (SLR)<br />
• straight leg raise<br />
• valsalva test<br />
• Bragard’s test<br />
• Bechterew’s test<br />
• Minor’s sign<br />
• Kemp’s test<br />
• Milgram’s test<br />
• Nachlas Test<br />
• Kernig’s test<br />
LBP Malingering Tests<br />
• Hoover’s sign<br />
• Burn’s bench test<br />
d. shoulder<br />
• Apley’s scratch test<br />
• Drop arm test (Codman’s)<br />
• Glenohumoral apprehension test<br />
• impingement test (Neer’s, Hawking-Kennedy)<br />
• Lippman’s test<br />
• Speed’s test<br />
• Yergason’s test<br />
e. neck/TOS testing (continued on next page)<br />
Quarter/Year:<br />
58
Student Name:<br />
Supervisor<br />
Initial/Date<br />
ORTHOPEDIC ASSESMENT cont’d<br />
f. ankle/foot<br />
• vertebral artery test<br />
• cervical spine (foraminal) <strong>com</strong>pression test<br />
• cervical spine (foraminal) distraction test<br />
• Lindner’s test (Brudzinski’s sign)<br />
• Adson’s/reverse Adson’s (thoracic outlet)<br />
• East’s test (Roos’ test) (thoracic outlet)<br />
• Posterior drawer test<br />
• anterior drawer test<br />
• tibial torsion test<br />
• dorsiflexion<br />
• Homan’s sign<br />
59<br />
Quarter/Year:<br />
• Forefoot squeeze test (Morton’s test)<br />
h. elbow/wrist/hand<br />
• Cozen’s test (lateral epicondylitis)<br />
• Mill’s test (lateral epicondylitis)<br />
• Golfer’s elbow test (medial epicondylitis)<br />
• Finkelstein’s test (stenosing tenosynovitis)<br />
• varus/valgus stress tests<br />
• Phalen’s test<br />
• Tinel’s sign<br />
NEUROLOGIC ASSESSMENT<br />
a. DTR’s<br />
b. Romberg<br />
c. Babinski<br />
d. muscle strength testing<br />
e. sensation testing<br />
OSSEOUS MANIPULATION ASSESSMENT<br />
a. static palpation<br />
b. motion palpation<br />
OSSEOUS MANIPULATION TECHNIQUE<br />
(know indications, contraindications, correct manipulation set up, and technique)<br />
a. joint manipulation set up<br />
b. joint manipulation<br />
• cervical spine<br />
• thoracic spine<br />
• ribs<br />
• lumbar spine<br />
• sacrum (SI joints)<br />
PATIENT EDUCATION RE: PREVENTION OF MUSCULOSKELETAL PROBLEMS<br />
a. Prevention (continued on next page)
Student Name:<br />
Supervisor<br />
Initial/Date<br />
ORTHOPEDIC ASSESMENT cont’d<br />
• Activity Modification<br />
• Correct lifting<br />
• Ergonomic work stations<br />
• Functional training<br />
• Postural training<br />
• Rest<br />
Quarter/Year:<br />
60
<strong>ND</strong> COUNSELING CLINICAL COMPETENCIES<br />
Mission Statement: The mission of the Counseling Department is to train naturopathic medical<br />
students in relationship-centered care and help students achieve personal integration. During their first<br />
rotation the students will meet the following <strong>com</strong>petencies. Any further advanced counseling shifts<br />
will expand these <strong>com</strong>petencies.<br />
BASTYR UNIVERSITY<br />
BASTYR CENTER FOR NATURAL HEALTH<br />
<strong>ND</strong> COUNSELING: CORE CLINCIAL COMPETENCIES<br />
Student:<br />
Quarter/Year:<br />
Supervisor:<br />
___________________________________<br />
___________________________________<br />
___________________________________<br />
Competence in Basic Counseling Skills<br />
Establish rapport, which includes demonstrating counseling characteristics of:<br />
Congruence<br />
Empathy<br />
Positive regard<br />
Reinforcing individual strengths<br />
Collaboration<br />
Demonstrate <strong>com</strong>munication skills:<br />
Attending Behavior (eye contact, vocal qualities, verbal tracking, body language)<br />
Open and Closed Questions<br />
Encouraging, Paraphrasing, & Summarizing<br />
Reflection of Feeling<br />
Confrontation<br />
Focusing<br />
Interpretation/Reframe<br />
Appropriate Use of Self-Disclosure<br />
Feedback<br />
Offers Appropriate Information/Advice<br />
Directives<br />
Reflection of Meaning<br />
Collaborative Goal Setting<br />
Competence in Psychological Assessment<br />
Conduct and Document Initial Assessment Interview, including:<br />
Psychiatric History<br />
Etiology<br />
Symptom Presentation (Frequency, Intensity, Duration)<br />
Precipitants/Triggers<br />
Diagnostic Impression/Dynamic Formulation<br />
Treatment Plan<br />
Mental Status Exam<br />
Recognize indicators of psychological conditions, assess according to current DSM and naturopathic<br />
perspective, and make appropriate treatment plan.<br />
61
Demonstrate Competency in Assessing the following areas:<br />
Axis I Clinical Syndromes and V Codes<br />
Axis II Personality Disorders<br />
Axis III Related Medical Conditions and Holistic Assessment of Functioning<br />
Axis IV Psychological Stressors<br />
Axis V Global Assessment of Functioning<br />
Demonstrate appropriate charting skills including:<br />
Ongoing treatment/SOAP notes<br />
CPT Codes<br />
Demonstrate the ability to differentiate and articulate symptoms from cause:<br />
Identify stages of change demonstrated by the patient.<br />
Demonstrate the ability to assess and refer for suicidal behavior.<br />
Demonstrate the ability to assess and refer for homicidal behavior.<br />
Demonstrate the ability to assess and refer for domestic violence.<br />
Demonstrate the ability to assess and refer for child/elder abuse.<br />
Competence in Whole Person Healing and Integration of Naturopathic Principles<br />
Discuss and apply counseling principles within the context of Naturopathic Medicine:<br />
1. Vis Medicatrix Naturae (the Healing Power of Nature)<br />
2. Tolle Causum (Treat the Cause)<br />
3. Tolle Totem (Treat the Whole Person)<br />
4. Primum Non Nocere (First Do No Harm)<br />
5. Docere (Doctor as Teacher)<br />
6. Prevention<br />
Articulate spiritual considerations as they relate to patient wellness.<br />
Competence in Professional Consultation and Referrals<br />
Demonstrate the ability to determine when a referral is necessary and to refer out to appropriate mental<br />
health providers.<br />
Identify <strong>com</strong>munity and internet resources for providers and for patients.<br />
Competence in Professional Conduct, Ethics, and Legal Matters<br />
Recognize and maintain personal/professional limitations and boundaries.<br />
Demonstrate personal maturity and emotional integration congruent with University policies and<br />
professional standards.<br />
Demonstrate behavior consistent with promoting health and appropriate self-care.<br />
Demonstrate openness to present one’s work for ongoing critique, as well as an ability to hear and<br />
incorporate feedback in clinical supervision and with peers.<br />
Demonstrate time management skills.<br />
Demonstrate ability to obtain and articulate informed consent (including principles of confidentiality).<br />
Competence in Culture and Diversity<br />
Demonstrate awareness of how one’s cultural background and experiences have influenced attitudes,<br />
values, and biases about psychological processes.<br />
Demonstrate awareness of own negative and positive emotional reactions toward other cultural.<br />
groups/areas of diversity that may prove detrimental or challenging to the counseling relationship.<br />
Recognize and use culturally appropriate assessment and intervention strategies.<br />
62
DISPENSARY CLINICAL COMPETENCIES - SECO<strong>ND</strong>ARY<br />
The dispensary <strong>com</strong>petency is required during your secondary year of clinical training. You will sign<br />
up for 4 small group discussions during the year. One of those discussions must cover Quality<br />
Assurance Standards. This discussion group will be offered multiple times during the year. Other<br />
topics will be offered in rotation and are based on a systems approach to treatment. You will attend<br />
three other discussion groups during the year on topics of your choice. Only 12-15 students are<br />
allowed per discussion group, and priority is given those who sign up. The <strong>com</strong>petency will be<br />
awarded on the following points.<br />
Attendance<br />
Preparation<br />
Participation in Discussion-the student must participate in active discussions on three<br />
conditions<br />
o The student must be prepared to present information on three products chosen to treat a<br />
condition. The products chosen may include encapsulated products, loose herbs,<br />
tinctures, glycerites, solid extracts, homeopathics, flower remedies, drainage remedies<br />
or topical treatments. Each discussion must include the following information:<br />
•Ingredients<br />
•Mechanism of action<br />
•Desired beneficial effects<br />
•Contraindications, if any<br />
•Undesired effects, if any<br />
•The above information may be applied to any of the following diagnoses or<br />
conditions, though are not limited to these conditions. You may choose other<br />
conditions under the general topic that you are interested in<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Cardiovascular disease (hypertension, hyperlipidemia, coronary artery<br />
disease, angina, etc.)<br />
Dysglycemia (DM, IDDM, hypoglycemia<br />
Upper gastrointestinal disorder (GER, GERD, PUD, dyspepsia)<br />
Lower gastrointestinal disorder (IBD, IBS, Crohn’s, UC, Celiac,<br />
constipation, diarrhea, etc…)<br />
Hepatobiliary disease (cholelithiasis, hepatitis, metabolic liver disease, etc.)<br />
Cancer prevention or treatment<br />
Skin diseases (eczema, psoriasis, exanthums, acne, etc…)<br />
Hematological disorders (anemia, leukemia, dyscrasias, etc…)<br />
Bone disorders (osteoporosis, osteomalacia, osteopenia, rickets)<br />
Female gynecological conditions (fibroids, FBD, menopause, PMS,<br />
PCO/PCOS, dysmenorrhea, abnormal pap, etc…)<br />
Male genitourinary conditions (BPH, prostatitis, epididymitis, etc…)<br />
Acute Respiratory Tract disorder<br />
Chronic Respiratory tract disorder<br />
Nutritional deficiency<br />
Acute urinary tract or kidney disorder<br />
Mental or emotional illness<br />
Nervous system disorder (insomnia, dizziness, seizure, paresthesia, etc…)<br />
HIV<br />
Endocrine disorders<br />
Autoimmune conditions<br />
Acute musculoskeletal disorders<br />
Chronic musculoskeletal disorders<br />
63
The project is required to increase knowledge of products available to treat <strong>com</strong>mon conditions and to<br />
allow the student practice integrating and <strong>com</strong>municating their knowledge of botanical, nutritional, and<br />
homeopathic treatment modalities in the clinical setting before they be<strong>com</strong>e primary clinicians. The<br />
learning objectives for the project include the following:<br />
1. Integrate mechanism of action, safety and physiology to the choice and application of treatment<br />
to a mock patient pathological condition or case.<br />
2. Create treatment plans that may be applied to patient care in the clinical setting.<br />
3. Articulate and define individual circumstances of treatment application based on the<br />
naturopathic principles and determinants of health.<br />
The <strong>com</strong>petency is presented and managed by a naturopathic physician with years of clinical and<br />
preceptor and teaching experience. You must utilize professional demeanor and <strong>com</strong>munication in all<br />
your interactions with your instructor and each other during these discussions.<br />
When you have <strong>com</strong>pleted the <strong>com</strong>petency as outlined, your instructor will sign off a section of the<br />
overall <strong>com</strong>petency. If you do not <strong>com</strong>plete the <strong>com</strong>petency during the discussion to the satisfaction<br />
of the moderator, you may repeat the section without sanction until you attain the <strong>com</strong>petency. You<br />
must <strong>com</strong>plete this entire <strong>com</strong>petency before moving into the primary role.<br />
Quality Assurance Discussion Group 2 Discussion Group 3 Discussion Group 4<br />
Signature/Date Signature/Date Signature/Date Signature/Date<br />
Databases that may be helpful in preparing for your project:<br />
www.naturaldatabase.<strong>com</strong><br />
www.naturalstandard.<strong>com</strong><br />
www.consumerlab.<strong>com</strong><br />
You are wel<strong>com</strong>e to use other resources and share those resources with others in the group.<br />
Kathie Golden, <strong>ND</strong><br />
64
HOMEOPATHY CLINICAL COMPETENCIES (OPTIONAL A<strong>ND</strong> ELECTIVE)<br />
Mission Statement: Homeopathy is an integral part of naturopathic medicine and a vital tool used by<br />
naturopathic doctors in healing their patients. Bastyr University is <strong>com</strong>mitted to teaching homeopathy<br />
with the highest standards in order to graduate naturopathic doctors who are <strong>com</strong>petent and skilled in<br />
the use of homeopathic medicines. Note that All homeopathic student clinicians are required to<br />
attend a minimum of five sessions of Grand Rounds for each homeopathy shift in order to enhance<br />
their clinical case study and analysis experience in Homeopathy. Primary clinicians are required to<br />
attend Homeopathic Grand Rounds whenever they have a case that needs study and analysis<br />
beyond the homeopathic clinic office call procedure.<br />
REQUIREMENTS TO ENROLL IN OPTIONAL HOMEOPATHY SPECIALTY SHIFTS<br />
Student Name:<br />
Quarter/Year:<br />
Supervisor<br />
Initial/Date<br />
Requirements<br />
To register for a homeopathy shift as a secondary student clinician:<br />
Complete Homeopathy III. Registration in Homeopathy IV is preferred.<br />
Attend Homeopathy Grand Rounds as assigned each quarter<br />
To be<strong>com</strong>e primary clinician <strong>com</strong>plete all the following requirements. This may occur<br />
your first quarter in homeopathy:<br />
Fulfill the responsibilities of a secondary clinician.<br />
Complete and turn in written analysis on 2 cases that you have observed.<br />
Act as primary clinician on one office call. Includes taking and analyzing the case, and<br />
writing up the patient’s chart notes.<br />
Be available for case discussion with supervising doctor.<br />
Demonstrate the ability to remain present and receptive to the patient.<br />
HOMEOPATHY CLINICAL COMPETENCIES - SECO<strong>ND</strong>ARY<br />
Student Name:<br />
Supervisor<br />
Initial/Date<br />
Requirements<br />
65<br />
Quarter/Year:<br />
The following requirements are the same as for a general Patient Care Shift:<br />
• Attendance is required, as described in the Student Clinician Handbook.<br />
• Ensure appropriate forms are available for signature. (dispensary/consent forms & treatment plans)<br />
• Track patient contacts.<br />
• Professional Cooperation with the colleagues and the supervising doctor.<br />
• Participate in taking the case - demonstrate active listening and appropriate questioning.<br />
• Participate in case preview/review - prepared for preview familiar with patient charts.<br />
The following requirements are unique to a Homeopathy Specialty Shift:<br />
• Take the patient’s case with appropriate homeopathic underlining, observations, etc. on<br />
all patient visits.<br />
• Study the case alone, or with a primary clinician, and be prepared to discuss and analyze<br />
the case with the supervising doctor in case preview/review.<br />
• All homeopathic student clinicians are required to attend a minimum of five<br />
sessions of Grand Rounds per shift. Primary clinicians may be required to attend<br />
additional Grand Rounds when they have a case that needs study and analysis beyond<br />
clinic.<br />
• All homeopathic clinicians should be able to demonstrate adequate knowledge and use<br />
of the repertory and materia medica as it applies to the patient’s symptoms
HOMEOPATHY CLINICAL COMPETENCIES - PRIMARY<br />
Student Name:<br />
Supervisor<br />
Initial/Date<br />
Competency<br />
Quarter/Year:<br />
The following requirements are the same as for a general Patient Care shift:<br />
• Assume responsibility for attendance, charting, and tracking the number of patient<br />
visits according to clinic policy<br />
• Track patient contacts and ensure that you have seen an adequate number of patients.<br />
• Professional cooperation with colleagues and supervising doctor.<br />
• Participate in case preview/review.<br />
• Adequately chart the patient’s visit in a timely fashion (within 24 hours)<br />
Communication skills:<br />
• Explain homeopathy treatment to the patient in clear and understandable terms.<br />
• Instruct patients how to take the medicine appropriately and what to expect from their<br />
treatment.<br />
• Discuss with the patient what we expect from them in terms of life-style habits, making<br />
follow-up appointments, when they can phone the clinic, etc.<br />
• Display open and cooperative <strong>com</strong>munications with peers and with supervising<br />
doctors.<br />
• All students will be held to the highest standards of professional and ethical behavior.<br />
These include: patient confidentiality, personal responsibility, impartiality,<br />
professional accountability and an appropriate understanding and respect of ethical<br />
personal boundaries.<br />
Case taking skills:<br />
• Establish adequate rapport with patient.<br />
• Demonstrate proper use of open ended and confirmatory questions, listening skills and<br />
full homeopathic case taking plus review of systems, past medical history, family<br />
medical history, etc.<br />
• Be able to take a full case in a reasonable amount of time.<br />
• Demonstrate good charting skills, including underlining and <strong>com</strong>pleteness of<br />
information that is readable and relevant.<br />
Case assessment and analysis skills:<br />
• Medical differential diagnosis.<br />
• Proper lab and other testing in order to confirm the diagnosis.<br />
• Proper physical examinations.<br />
• Identify acute vs. chronic prescribing.<br />
• Identify the patient’s <strong>com</strong>plaints from a homeopathic perspective. This includes the<br />
chief <strong>com</strong>plaint, the center of gravity, the etiology, the recognition of general,<br />
particular, and mental/emotional symptoms; the differentiation of strange, rare, and<br />
peculiar symptoms from <strong>com</strong>mon symptoms; identification of the miasmatic basis of<br />
the patient’s disease, and an assessment of the strength of the patient’s Vital Force.<br />
• Demonstrate an adequate knowledge and use of the repertory and materia medica as it<br />
applies to the patient’s symptoms.<br />
(continued on next page)<br />
67
Student Name:<br />
Supervisor<br />
Initial/Date<br />
Competency<br />
Quarter/Year:<br />
• Demonstrate the systematic thought processes of homeopathic assessments: essence,<br />
keynote, totality, etiology, reliable symptoms, etc.<br />
• Demonstrate adequate knowledge of <strong>com</strong>parative materia medica, and confirmatory<br />
and keynote symptoms, in order to arrive at the proper selection of the medicine.<br />
• Give rationale for potency selection.<br />
• Give evaluation of prognosis of treatment.<br />
• Document all of the above in chart for each visit.<br />
Follow-up case skills:<br />
• Show initiative and persistence in following up with supervisor and patients.<br />
• Take follow-up case appropriately and <strong>com</strong>prehensively.<br />
• Evaluate the action of the remedy within appropriate timelines.<br />
• Demonstrate the ability to effectively <strong>com</strong>municate with other medical<br />
professionals, and to refer to them when appropriate, in order to ensure optimal<br />
patient care.<br />
68
BUSINESS SECTION<br />
69
BILLING<br />
CURRENT PROCEDURAL TERMINOLOGY (CPT)<br />
Bastyr Center for Natural Health uses CPT codes according to the standards agreed upon by CMS and<br />
associated medical groups. The chosen CPT codes reflect the level of service provided during each<br />
patient visit. The supervising clinician is responsible for choosing the correct CPT code for the visit,<br />
and for recording it on the patients billing and lab forms.<br />
Important principles for choosing CPT codes include:<br />
• A new patient is one who has not received any professional services from the clinician or<br />
another clinician of the same specialty who belongs to the same group practice within the past<br />
three years.<br />
• Counseling is defined as a discussion with a patient and/or family concerning diagnostic<br />
results, impressions or re<strong>com</strong>mendations, prognosis, risks evaluation and risk reduction.<br />
PATIENT CARE CPT CODING WORKSHEET<br />
[Used to calculate visit fee - Not to be filed with the Medical Records]<br />
On the following four pages, you will find the BCNH Patient Care CPT Coding Worksheet. It is to be<br />
optionally used by supervisors or student clinicians on shift as a guide to choosing the correct CPT<br />
code for the level of visit <strong>com</strong>plexity, the number of history elements obtained, and the number of<br />
physical exam elements performed. All criteria included in the tables are derived from the<br />
documentation guidelines.<br />
NEW PATIENTS:<br />
Requires all three Key Components – History, Physical Exam and Decision Complexity.<br />
Decision<br />
Code History Physical Exam<br />
Complexity<br />
CC:<br />
99201<br />
1 System/Area<br />
Straight<br />
HPI [1-3]<br />
Focused<br />
[1-5 elements]<br />
Forward<br />
areas<br />
99202 Expanded<br />
Problem Focused<br />
99203<br />
Detailed<br />
99204<br />
Comprehensive<br />
99205<br />
Comprehensive<br />
CC:<br />
HPI [1-2]<br />
ROS [1]<br />
areas<br />
CC:<br />
HPI [4-7]<br />
ROS [2-<br />
9]<br />
PFSH [1]<br />
areas<br />
CC:<br />
HPI [4-7]<br />
ROS [10]<br />
PFSH [3]<br />
CC:<br />
HPI [4-7]<br />
ROS [10]<br />
1+ Systems<br />
[6 elements]<br />
6 Systems/Areas w/2<br />
Elements or 2 Systems/Areas<br />
w/12 Elements<br />
9 Systems/Areas<br />
w/2+ Elements<br />
9 Systems/Areas<br />
w/2+ Elements<br />
Straight<br />
Forward<br />
Low<br />
Moderate<br />
High<br />
Counseling<br />
[Health]<br />
10 minutes<br />
20 minutes<br />
30 minutes<br />
45 minutes<br />
60 minutes<br />
70
RETURN PATIENTS:<br />
Requires 2 of the following 3 Key Components – History, Physical Exam and Decision Complexity.<br />
Decision Counseling<br />
Code History Physical Exam<br />
Complexity [Health]<br />
99212<br />
1 System/Area<br />
Straight<br />
CC: HPI<br />
10 minutes<br />
Focused<br />
[1-5 elements]<br />
Forward<br />
99213 Expanded<br />
Problem Focused<br />
99214<br />
Detailed<br />
99215<br />
Comprehensive<br />
CC:<br />
HPI<br />
ROS [1]<br />
CC:<br />
HPI<br />
ROS [2-9]<br />
PFSH [1]<br />
CC:<br />
HPI<br />
ROS [10]<br />
PFSH [3]<br />
1+ Systems<br />
[6 elements]<br />
6 Systems/Areas w/2<br />
Elements or 2<br />
Systems/Areas w/12<br />
Elements<br />
9 Systems/Areas<br />
w/2+ Elements<br />
Low<br />
Moderate<br />
High<br />
15 minutes<br />
25 minutes<br />
40 minutes<br />
History of Present Illness [HPI]<br />
Includes the Elements Listed Below<br />
Location<br />
Quality<br />
Severity<br />
Duration<br />
Timing<br />
Context<br />
Modifying Factors<br />
Associated Signs and Symptoms<br />
HPI Notes<br />
Brief HPI: The medical record should describe 1-3 elements<br />
of the present illness.<br />
Extended HPI: Description should include at least 4<br />
elements of the HPI or the status of at least 3 chronic or<br />
inactive conditions.<br />
Past Family and/or Social History (PFSH)<br />
Consists of a Review of 3 Areas<br />
Past History: The patients past experiences with<br />
illnesses, operation, injuries, and treatments<br />
Family History: A review of medical events in the<br />
patients family, including diseases which may be<br />
hereditary of place the patient at risk<br />
Social History: An age appropriate review of past<br />
and current activities<br />
PFSH Notes<br />
Pertinent PFSH: At least one specific item<br />
from any of the three history areas must be<br />
documented of a pertinent PFSH.<br />
Complete PFSH: At least one specific item<br />
from each of the three history areas must be<br />
documented.<br />
71
Review of Systems [ROS]<br />
Includes the Systems listed below<br />
Constitutional Symptoms [e.g.<br />
fever, weight loss, etc.]<br />
Eyes<br />
Ears, Nose, Mouth, Throat<br />
Cardiovascular<br />
Respiratory<br />
Gastrointestinal<br />
Genitourinary<br />
Musculoskeletal<br />
Integumentary<br />
Neurological<br />
Psychiatric<br />
Endocrine<br />
Hematological/Lymphatic<br />
Allergic/Immunologic<br />
Other Comments/Additional<br />
Instructions:<br />
ROS Notes<br />
Problem Pertinent ROS: The patient's positive responses and<br />
pertinent negatives for the system related to the problem should<br />
be documented.<br />
Extended ROS: The patients positive responses and pertinent<br />
negatives for 2 – 9 systems should be documented<br />
Complete ROS: At least 10 organ systems must be reviewed.<br />
Those systems with positive or pertinent negative responses<br />
must be individually documented. For the remaining systems, a<br />
notation indicating all other systems are negative is permissible.<br />
In the absence of such a notation, at least 10 systems must be<br />
individually documented.<br />
Notes for Coding<br />
Problem Focused: A limited examination of the affected body<br />
area or segment or organ system. 1-5 elements.<br />
Expanded Problem Focused: A limited examination of the<br />
affected body area or organ system and any other symptomatic<br />
or related body area or organ. 6+ elements.<br />
Detailed: An extended examination of the affected body area of<br />
organ system and any other symptomatic or related body area or<br />
organ system. At least 2 elements from each of the 6 areas or at<br />
least 12 elements in 2+ areas.<br />
Comprehensive: A general multi-system examination of a<br />
single organ system and other symptomatic or related body area<br />
or organ system. All elements in at least 9 areas.<br />
72
FEES A<strong>ND</strong> PAYMENT<br />
•Three <strong>com</strong>ponents of an office visit are key to determining the level of E/M (Evaluation and<br />
Management) service. They are: History, Examination, and Medical Decision<br />
Making/Complexity of Case as docu.<br />
• The quantity of detail, counted as elements, in areas of History of Present Illness/Chief<br />
Complaint (HPI/CC), Past/Family/Social History (PFSH), Review of Systems (ROS), and<br />
Physical Examination further impacts the level of CPT chosen.<br />
•Time, in reference to a patient visit, equals face-to-face time working with the patient.<br />
•There are five E/M levels of risk and <strong>com</strong>plexity: Minimal, Self-Limited, Low, Moderate,<br />
and High.<br />
• To select a CPT code for a new patient visit, the E/M services provided must meet or<br />
exceed established criteria in all three key <strong>com</strong>ponents described above. A return office visit<br />
must meet or exceed only two, and one must be the level of medical decision<br />
making/<strong>com</strong>plexity.<br />
• In the case where counseling and/or coordination of care constitutes more than 50 percent<br />
of the clinician/patient and/or family encounter (face-to-face time), then time alone be<strong>com</strong>es<br />
the determining CPT factor. Quantity of time must be documented.<br />
•The CPT code series most used at Bastyr Center for Natural Health in <strong>ND</strong> patient care are<br />
Office or Other Outpatient Services (99201-205, 99221-215), Preventive Medicine Services<br />
(99381-387, 99391-397), and Counseling and/or Risk Reduction Intervention (99401-404).<br />
BILLING DOCUMENTATION GUIDELINES (DG)<br />
•Pertinent factors of Complexity of Medical Decision Making including Number of<br />
Diagnoses or Management Options, Amount and/or Complexity of Data to be Reviewed, and<br />
Risk of Significant Complications, Morbidity, and/or Mortality.<br />
•An Encounter Dominated by Counseling or Coordination of Care, particularly the element<br />
of time.<br />
• The correct number of elements of CC, HPI, ROS, PFSH, and Examinations to correspond<br />
with the Complexity of Medical Decision Making and CPT chosen.<br />
INTERNATIONAL CLASSIFICATION OF DISEASES (ICD-9)<br />
• Every condition actively addressed during the patients present clinic visit, and only those<br />
conditions, must be assigned a specific ICD-9 code. All ICD-9 codes pertaining to an individual<br />
patient visit must be recorded in the required locations in the written record, including the<br />
assessment section. However, only four ICD-9 codes should be listed on the billing form.<br />
• All ICD-9 codes must be numbered by priority on each billing form and in the patient chart.<br />
73
LABORATORY PROTOCOLS<br />
HOURS OF OPERATION<br />
Laboratory hours of operation are as follows:<br />
Open: 8:30 a.m. to 8:30 p.m. Monday, Tuesday, and Thursday<br />
8:30 a.m. to 4:30 p.m. Wednesday, Friday<br />
8:30 a.m. to 12:30 p.m. Saturday<br />
Closed: 12:30 until 1:30 on Monday through Friday<br />
5:00 until 5:30 on Monday, Tuesday, Thursday<br />
LABORATORY PROCEDURES<br />
BCNH has an affiliation with Pacific Physicians Laboratory (PPL). With this relationship, there will be<br />
a PPL phlebotomist in the lab area for most hours that the clinic is open for patients. The phlebotomists<br />
are employees of PPL and are here to assist the clinic in the care of our patients. They are not clinic<br />
employees and cannot be used for services outside the lab.<br />
There are two general categories of lab services that we provide: Outside Labs (Reference Laboratory,<br />
including PPL and other labs) and In-House labs (Waived tests). Waived tests are those tests that<br />
physician practitioners are legally able to perform in their offices.<br />
• All outside lab specimens will go through PPL including non-reference labs (Great Smokies,<br />
Immunolabs, etc.). These will all be collected, prepared, and processed by the phlebotomist.<br />
• Waived tests can be performed here in the lab area by physicians with the assistance of<br />
student clinicians, or may be sent out to PPL. When we elect to do a waived test here, it is our<br />
responsibility to make the appropriate diagnosis from the lab result.<br />
• Only physicians can use the microscope to interpret lab results, students and the medical<br />
assistant (MA) can look but CANNOT interpret the results. A physician must record the lab<br />
results on the results sheet.<br />
Waived tests include the following and are to be performed only in the lab area:<br />
• UA-dipstick and micro<br />
• KOH preps<br />
• wet preps<br />
• hematocrit<br />
• rapid strep<br />
• guiac<br />
• fern<br />
• glu<strong>com</strong>eter<br />
• nasal smear<br />
• pregnancy<br />
• pinworm<br />
After your clinical diagnosis class, you should be reasonably <strong>com</strong>fortable doing dipsticks, wet mounts,<br />
KOH, guiac, rapid strep and PG tests-though only your supervisor can report the results. The<br />
following tests require a higher level of skill and your supervisor may <strong>com</strong>plete them personally or<br />
may choose to send them out: UA-microscopy, nasal smear, hematocrit and fern. There may be<br />
situations where a second opinion is desired. BCNH encourages calling the techs/pathologist at PPL,<br />
rather than relying on specific faculty with lab expertise.<br />
74
When a supervisor needs to do a waived lab test performed in-house, the physician will decide how to<br />
proceed:<br />
• They can collect and prepare the sample themselves, and interpret the result-providing<br />
educational opportunities for their students.<br />
• Or, if the test involves microscopy, they can contact the in-house on-call resident to prepare<br />
and interpret the result. The on-call resident may be covering a shift, and therefore, not always<br />
available. Students may be directed to review the findings for educational purposes.<br />
• In all cases, the lab results must be reviewed and recorded on the results sheet by the<br />
supervising physician, signed by the supervisor, and placed in the patient chart.<br />
In the event that a provider requires an ASAP lab test performed, the phlebotomist can arrange to send<br />
the sample to PPL in a taxi. (As a reminder: ASAP tests, results of which should be available within<br />
one hour, cover a broad range of tests. Results of ASAP tests can offer definitive diagnostic<br />
information and direct specific therapy. STAT tests <strong>com</strong>prise those procedures for which results are<br />
needed within seconds to minutes. When dealing with life-threatening conditions, these test results<br />
may be essential in guiding therapy in the crucial first few minutes after a clinically unstable patient<br />
arrives in the center.) In the case where a STAT test is required, in all likelihood, the supervisor should<br />
arrange for the patient to be transported by 911 to an emergency department.<br />
Students may, with the permission of their supervisor and under direct supervision from the same,<br />
perform phlebotomy on their patients. All students must adhere to the following guidelines prior to<br />
drawing any samples:<br />
• Notify the phlebotomist first before taking the draw kit<br />
• The phlebotomist must double check the paperwork<br />
• The phlebotomist must double check that the students are drawing the correct samples<br />
• PPL will be billing the patient for the draw fee as they are providing the materials<br />
• The clinic blood borne pathogen safety procedures will be followed at all times. See the<br />
safety section to review those rules.<br />
LAB PAPERWORK<br />
All waived tests that are done in-house must be charged for on the superbill, and there is no need for a<br />
lab requisition form.<br />
All labs to be sent to outside facilities (PPL or otherwise) must be ac<strong>com</strong>panied by a lab requisition<br />
form that is properly filled out in pen. The white copy goes to the phlebotomist in the lab or is placed<br />
in the “Lab Requisitions” file above the phlebotomist’s desk, the yellow copy goes into the chart, and<br />
the pink copy goes to the patient (this is especially important if the patient is going to a different<br />
facility for their draw or if they are returning to BCNH at a later date for their draw). Ensure that all<br />
copies of the form are <strong>com</strong>pleted accurately through the three layers of the form.<br />
All Pap and other samples to be sent to pathology require information sections of the lab specimen<br />
identification form be <strong>com</strong>pleted by the physician.<br />
LABORATORY WORKFLOW<br />
The lab tech is in the lab during open clinic hours except during the designated lunch and dinner breaks.<br />
All patients needing draws should be scheduled through the front desk to ensure that there is time and<br />
space to see them immediately. Students may draw blood for any tests under the supervision of<br />
supervising faculty. All specimens are to be labeled and placed on the bench with appropriately<br />
<strong>com</strong>pleted forms. LABEL: patient last name, first name; date collected; source. Samples collected<br />
from patients in exam/ treatment areas must be handled following blood borne pathogen safety<br />
procedures and transported to the lab in accordance with OSHA guidelines. This includes containing<br />
samples <strong>com</strong>pletely and transporting in a gloved hand(s). Every lab procedure that is performed or<br />
sent out must be coded and billed appropriately. Even though the student or provider may draw the<br />
specimen and/or perform a lab test, we must charge for the resources that have been utilized. Any<br />
75
discounts or special rates will be determined by the clinic policies in place and managed through the<br />
phlebotomist or front desk staff. Obtaining and processing of a sample can take up to 30 minutes,<br />
depending on the request. It is during the immediate post-closing time that work already requested is<br />
finished, and the laboratory is cleaned and disinfected for the next day. All lab work is to be brought to<br />
the lab or requested 30 minutes prior to the lab’s posted closing time. Should there be an emergency<br />
that may require the lab to remain open past its closing time, please notify the lab personnel as soon<br />
as possible. Poor time management is no reason for staff to stay later than their posted time.<br />
For patients who need laboratory work during closure hours, please refer them to the front desk for a<br />
lab appointment time.<br />
LABORATORY TEST FEES A<strong>ND</strong> BILLING<br />
Whenever an outside lab is ordered, the patient must be informed that additional fees will be incurred<br />
and that they will be billed for these fees.<br />
Only laboratory personnel will quote test fees with the patient. The supervising physician may research<br />
the cost and give an estimated cost to the patient.<br />
Reference laboratories may have a multi-tiered fee schedule. In such cases, a discussion with<br />
laboratory personnel is required to clarify which schedule to apply. Criteria to determine such an<br />
application include:<br />
•Insurance coverage<br />
•Payment at time of service option<br />
• Payment included with specimen option<br />
• Specific reference laboratory offering the requested test(s)<br />
Laboratory personnel bill patients for laboratory testing. Any tests that are subsequently requested will<br />
be billed to the patient by the testing entity.<br />
LABORATORY TEST RESULTS<br />
Original reports of lab test results will be placed in the ordering physician’s mailbox for review,<br />
response and signature. A copy of the test results will be placed under the physician’s name in the<br />
folding blue file in the faculty assistant’s office for students to review. The physician will route the<br />
reports to the patient’s chart for filing by placing the signed report in the loose paperwork medical<br />
records box hanging on the outside of the chartroom door. Duplicate copies of all lab reports are stored<br />
for two months in the lab.<br />
76
APPE<strong>ND</strong>ICES<br />
1. Student Clinician Absence/Substitute Form<br />
2. <strong>ND</strong> Physical Exam Guidelines for Clinical Competencies<br />
3. Naturopathic Treatment of Malignancy Consent Form<br />
77
Appendix 1<br />
BASTYR CENTER FOR NATURAL HEALTH<br />
Student Clinician Absence / Substitute Form<br />
It is the responsibility of every Student Clinician to inform their assigned Supervisor<br />
of any planned absence from the clinic, and give this form to the Faculty<br />
Administrative Assistant.<br />
Please follow the procedures outlined below:<br />
1. Fill out the bottom portion of this form <strong>com</strong>pletely, otherwise it will be<br />
returned to you for further clarification. Fill out a separate form for each shift<br />
and planned absence.<br />
2. Notify the Supervisor of each shift you plan to miss, and have him/her sign<br />
the appropriate space below.<br />
3. Primary and Secondary Student Clinicians must obtain a substitute for each<br />
shift you plan to miss, and have the substitute sign the appropriate space below.<br />
A copy of the <strong>com</strong>pleted form or confirmatory email should be sent to the sub by<br />
the absent clinician.<br />
4. Once the form is <strong>com</strong>plete, submit it to the Faculty Administrative Assistant in<br />
room S 206 (second floor). The form is retained on a quarterly basis.<br />
5. All of these procedures must be followed in advance of the planned<br />
absence.<br />
6. If you are suddenly ill or have a personal emergency, you must call your<br />
supervisor and the front desk at the clinic as soon as possible to notify them in<br />
person.<br />
7. An unexcused absence will result in an automatic fail for the quarter.<br />
Name of Student (Please Print): ______________________________________________<br />
Today’s Date: _______________<br />
Date of Absence: ______________<br />
Department (Please Circle):<br />
Acupuncture/Oriental Medicine Dispensary Counseling<br />
Naturopathic Patient Care Homeopathy Nutrition<br />
Physical Medicine<br />
Lab<br />
Shift (Please Circle): Morning Afternoon Evening<br />
Reason for Absence: ____________________________________________________________<br />
Signature of Supervisor: _____________________________________________________<br />
Name of Substitute (Please Print): ___________________________________________<br />
Signature of Substitute: _____________________________________________________<br />
78
Appendix 2<br />
BASTYR CENTER FOR NATURAL HEALTH<br />
STUDENT DAILY SHIFT CHECK-OFF EVALUATION FORM – PATIENT CARE<br />
STUDENT NAME: ______________________________ DATE: _____________<br />
QUARTER/YEAR: ______________ SHIFT: ____________________________<br />
NUMBER OF PATIENTS SEEN ON SHIFT: ____________________________<br />
RATING SCALE:<br />
NA = not applicable<br />
1 = unsatisfactory (F)<br />
2 = adequate (AC)<br />
3 = good (AC)<br />
4 = excellent (AC)<br />
An AC grade is given if the student has successfully demonstrated <strong>com</strong>petency (2, 3 or 4 on scale<br />
above) in all the clinical categories appropriate to her/his status in clinic. A PC grade is given if all<br />
critical clinical skills are successfully demonstrated and one non-critical skill is assessed as<br />
unsatisfactory (1 on scale above). An F grade is given if one or more critical clinical skill is assessed as<br />
unsatisfactory, or if two or more non-critical clinical skills are assessed as unsatisfactory at a level<br />
appropriate to the student’s status in clinic. If a PC grade is given, a letter detailing requirements for<br />
changing the PC to an AC must ac<strong>com</strong>pany the grade. See the Clinic Handbook and grading manual<br />
for details.<br />
Supervisor<br />
Initial/Date<br />
Objective<br />
Clinical Skills<br />
Initiative, motivation, responsibility<br />
Communications skills and rapport with patients<br />
Interview skills (S)<br />
Physical exam (O)<br />
Differential diagnosis/assessment skills (A)<br />
Knowledge of naturopathic therapeutics and their proper application<br />
Patient case preparation and follow up<br />
Familiarity with clinic policies and procedures and efficiency in following them<br />
Listening skills<br />
Time management skills<br />
Proper use of lab, diagnostic studies, etc.<br />
Ability to make an appropriate referral when needed and ability to write up referral<br />
Charting technique (<strong>com</strong>pleteness and clarity)<br />
Participation and input in case discussions on shift, case preview and case review<br />
Summary <strong>com</strong>ments: This space for <strong>com</strong>ments/suggestions/re<strong>com</strong>mendations and/or<br />
to explain and clarify ratings above. Supervising Clinic<br />
al Faculty must sign & date.<br />
Supervisor’s Signature ________________________________ Date ________________<br />
79
Appendix 3: <strong>ND</strong> PHYSICAL EXAM GUIDELINES FOR CLINICAL COMPETENCIES<br />
The Abdominal Examination Benchmark<br />
Basics:<br />
The abdominal Examination proceeds through look, listen, then feel. Ensure the following throughout<br />
the examination.<br />
Patient <strong>com</strong>fort is maximized<br />
Patient is supine, draped and only the abdomen is exposed<br />
Their head is supported by a pillow<br />
Their knees are slightly flexed to relax abdominal muscles<br />
Their hands are on their chest or by their side<br />
Your hands are WARM<br />
Watch the patient’s face throughout the exam for signs of distress<br />
The painful or tender area is examined LAST<br />
A. Inspection:<br />
1. DO: Observe for:<br />
Patient distress (does it hurt the patient to move or cough?<br />
Abdominal distension, if present, is it localized or generalized?<br />
Scars<br />
Masses<br />
Visible organomegaly<br />
2. KNOW:<br />
The abdomen is typically divided into 4 quadrants-R & LLQ, R & LUQ<br />
And additional three middle or central regions-epigastium, peri-umbilical &<br />
hypogastrium/supra-pubic<br />
A localized bulge in the abdominal wall may suggest a hernia<br />
Patients with peritonitis have increased pain with sudden movements of the abdomen,<br />
like coughing, walking, or when bed is bumped<br />
B. Auscultation<br />
1. Do:<br />
Listen in one place with the diaphragm of the stethoscope until you hear bowel sounds.<br />
Listen for bruits in the epigastrium and both upper quadrants<br />
2. KNOW:<br />
Normal bowel sounds rate and sound<br />
In bowel obstruction, bowel sounds may be high pitched and tinkling<br />
In <strong>com</strong>plete obstruction, there may be no bowel sounds, but you may have to listen for 2<br />
minutes to make sure there are no sounds<br />
An isolated systolic bruit heard in the epigastrium can be regularly heard in normal<br />
persons.<br />
C. Percussion<br />
1. DO:<br />
Percuss the abdomen lightly in all four basic quadrants<br />
Percuss, in the mid-clavicular line, the upper liver margin superiorly and the lower liver<br />
margin inferiorly. OR you may palpate the lower liver margin inferiorly.<br />
Measure the distance between the upper liver margin and the lower liver margin in the<br />
mid clavicular line.<br />
If you suspect ascites on the basis of bilateral flank bulging or dullness to percussion,<br />
then also perform one of the following tests:\<br />
80
Fluid Wave:<br />
Have the patient place the edge of their own hand on their anteriofr abdominal<br />
wall to dampen false positive soft tissue waves<br />
Lightly place your right hand on the right lateral side of the patient’s abdomen.<br />
With the fingertips of your left hand, briskly tap the left lateral side of the<br />
patient’s abdomen<br />
In the presence of ascites, you will feel a tap against your right hand as the fluid<br />
wave generated by your left hand travels through the ascites<br />
Shifting dullness:<br />
In the presence of ascites, air filled bowel loops float above the ascites fluid<br />
In the supine patient, percuss the bowel bluid level on the patient’s lateral<br />
abdominal wall (percussing from anterior to posterior) noting where the<br />
percussion note changes from tympanitic (bowel loops anteriorly) to dull<br />
(ascetic fluid posteriorly). Make a small mark with your pen to delineate this<br />
line.<br />
Have the patient assume a partial decubitus position angled towards you.<br />
Again percuss the lateral abdominal wall and see if the bowel bluid interace<br />
level has changed. If it has, it suggests that there is freely moving fluid (ascites)<br />
within the abdomen.<br />
2. KNOW:<br />
The normal abdomen should have both tympanitic areas (gas filled bowel) and<br />
dull areas (fluid filled bowel).<br />
A protuberant abdomen that is diffusely tmpanitic suggests intestinal obstruction.<br />
Localized percussion tenderness suggests peritoneal inflammation<br />
The causes of ascites include liver disease, renal disease, inflammation, and<br />
decreased intravascular oncotic pressure.<br />
The determination of a given patient’s liver span varies between observers. The<br />
more consistent you are in using the same method with every patient you<br />
evaluate, the less variable your own examination be<strong>com</strong>es in assessing liver size.<br />
Current references list different normal liver spans in the mid clavicular line as<br />
follows:<br />
Bates’ Guide to Physical Examination and History Taking: 6-12 cm<br />
Evidence-Based Physical Diagnosis: 6-15 cm<br />
Physical Diagnosis Secrets: less than 12-13 cm<br />
D. Palpation<br />
1. DO:<br />
a. Palpate all four quadrants superficially once, then palpate them more deeply<br />
b. Palpate the lower liver edge in the RUQ<br />
Technique: Place your left hand behind the patient, along and just below their<br />
11 th -12 th ribs<br />
Ask the patient to relax, and press your left hand forward as they exhale<br />
Place your right hand on the patient’s right abdomen in the mid clavicular line<br />
Begin your palpation well below the lower border of liver dullness as<br />
determined by percussion<br />
Ask the patient to breath inward as you feel for their liver edge <strong>com</strong>ing down to<br />
meet your right fingertips<br />
Repeat several times as necessary, keeping your left hand in the same place, but<br />
adjusting your right hand’s position until the edge is palpated. Note whether it<br />
is tender to the patient and the characteristics edge: soft, smooth, hard, nodular<br />
c. Palpate for an enlarged spleen in the LUQ by using a similar technique except reach<br />
across the patient with your left had, supporting and pressing forward with your left<br />
81
hand on the patient’s left lower rib cage and adjacent soft tissues. Attempt to<br />
palpate the spleen with your right hand in the LUQ<br />
d. Assess the abdominal aorta for enlargement in people over 50 years of age or with<br />
risk factors for cardiovascular disease<br />
Technique:<br />
Press inward in the epigastric region slightly left of the midline to identify aortic<br />
pulsations<br />
Now place your hands on either side of the aorta, and press inwards, attempting to<br />
determine the width of the palpated pulsations being transmitted through overlying<br />
tissue<br />
Remember that you are feeling pulsations through multiple overlying tissues, so<br />
even the normal adult aorta (less than 2.5-3.0 cm diameter) will feel wider than it is.<br />
An aorta more than 5 cm diameter on ultrasound needs a vascular surgery consult<br />
e. Elicit Murphy’s sign, McBurney’s sign and Rosvig’s sign if indicated by tenderness<br />
on palpation<br />
2. KNOW:<br />
Definition and medical meaning of:<br />
Peritonitis<br />
Tenderness<br />
Guarding<br />
Rebound<br />
Rigidity<br />
McBurney’s Point<br />
Murphy’s sign<br />
82
Cardiac Exam Benchmark<br />
Basics:<br />
Places table in appropriate position for exam<br />
The student explains benefit of examining in each of three positions.<br />
A. Inspect & Palpate<br />
DO: Demonstrates inspection<br />
Palpates precordial region for lifts/heaves and thrills in appropriate regions<br />
Palpates the PMI (point of maximal impulse) at the cardiac apex<br />
2. Know<br />
Definitions:<br />
Heave or Lift (defines perimeters and location)<br />
Thrill (defines perimeters and location)<br />
Normal PMI (defines perimeters and location)<br />
B. Auscultate<br />
1. DO: Listen at four basic locations using the diaphragm of the stethoscope. At each<br />
location, auscultate the normal heart sounds (S1, S2). At each location listen carefully for<br />
murmurs and rubs.<br />
Aortic area (R 2 nd ICS, upper right sternal border)<br />
Pulmonic area (L 2 nd ICS, upper left sternal border)<br />
At the pulmonic area, listen for the physiologic split of S2<br />
Tricuspid area (l 5 th ICS, lower left sternal border)<br />
Cardiac apex (mitral valve area)<br />
Use the bell of the stethoscope and auscultate for S3 or S4<br />
2. DO: If a murmur is heard, grade the murmur<br />
3. KNOW: The physiologic actions that create S1 and S2<br />
The normal S1-S2 sounds and where they are best heard<br />
Difference between a physiologic and pathological split sound<br />
Definition of a rub, where it is best heard<br />
Definition of an S3, where it is best heard<br />
Definition of an S4, where it is best heard<br />
Definition of the five characteristics of a murmur and the location of the classic<br />
murmurs<br />
C. Assess Neck Veins and Determine JVP<br />
1. Do:<br />
Position and light the patient to visualize the neck and veins<br />
Determine the JVP<br />
2. The definition of the normal JVP<br />
D. Palpate & Auscultate Carotid Arteries<br />
1. Do:<br />
Palpate each artery with appropriate technique<br />
Auscultate each artery<br />
2. Know:<br />
Definition and location of murmurs heard in the Carotid Arteries<br />
Definition, health considerations and location of bruit<br />
E. Palpate Peripheral Arteries<br />
1. Do: Palpate peripheral arteries with appropriate technique<br />
2. Know:<br />
Health considerations of absent pulses<br />
83
Ethics Benchmark<br />
As professionals, there are specific expectations regarding ethical knowledge and behavior.<br />
Overall, we expect students will be able to:<br />
Recognize ethical issues when they arrive in clinical practice<br />
Reason through ethical dilemmas<br />
Understand their responsibility to act (guiding principles of the profession)<br />
Respond in ethically appropriate ways (carry out the appropriate action)<br />
A. Ethics Knowledge: the student is familiar with ethics concepts presented in the first two years<br />
(pre-clinical) of medical school, including:<br />
1. Ethical issues in the physician-patient relationship.<br />
a. Informed consent<br />
i. Right to refuse<br />
ii. Decision making capacity<br />
iii. Surrogate decision makers<br />
b. Confidentiality<br />
c. Truth telling<br />
2. Ethical issues at the end of life<br />
a. DNR orders<br />
b. Futility<br />
c. Withholding and withdrawing treatment<br />
B. Ethics Tools: the discipline of ethics relies on specific methods as tools to reason through<br />
dilemmas and guide behavior in practice. Students will be familiar with:<br />
1. Ethical principles that guide health care professionals, including students in training, in<br />
appropriate care for patients in the clinical setting.<br />
a. Respect for person (autonomy): respect for autonomy and self-determination<br />
b. Nonmaleficence (first, do no harm): prevent harm, or minimize harm.<br />
c. Beneficence: be of benefit to patients<br />
d. Justice: Treat patients with integrity and fairness<br />
2. A case-based method to work through ethical dilemmas. The student will be able to:<br />
a. Describe core topic information in a case. Core topics are present in every clinical<br />
encounter.<br />
Medical considerations<br />
Patient preferences<br />
<br />
<br />
Quality of life<br />
Contextual feature such as the family, the law, clinic policy, third party payers<br />
and cultural traditions<br />
b. Identify core issue or dilemma in case<br />
c. Find relevant resources such as books, current articles, consultants<br />
d. Propose and justify a course of action<br />
C. Ethical Behaviors: recognizing ethical issues and knowing what is appropriate is only part<br />
of what is expected of medical professionals and physicians in training. You must also be<br />
able to act appropriately. This includes:<br />
a. Understand and maintain professional boundaries with patients<br />
b. Maintain patient confidentiality<br />
c. Admit mistakes, lack of knowledge, errors, and omissions, and seek to correct them.<br />
84
Head & Neck Examination Benchmarks<br />
I. Basics<br />
a. The head and neck examination is usually performed in the seated patient. Parts of the<br />
neck examination and palpation of the thyroid gland may be performed with the<br />
examiner standing behind the patient.<br />
b. The cranial nerve examination may occur at the time of the head & neck examination or<br />
separately as part of the Neurological examination. For the purposes of <strong>com</strong>petency<br />
examination, the cranial nerve exam is performed with the neurological examination.<br />
II.<br />
III.<br />
IV.<br />
Initial Inspection<br />
a. DO:<br />
i. Inspect the size and shape of the head<br />
ii. Look for symmetry, masses and signs of trauma.<br />
iii. Note any difficulty with breathing or speech.<br />
b. KNOW - (the following terms):<br />
i. Normocephalic: a normal sized and shaped calvaium<br />
ii. Stridor: noise with breathing that is high-pitched, fine, and originates at the<br />
level of the glottis or subglottis<br />
iii. Hoarseness: arises from swelling or masses on the true or false vocal cords<br />
Face<br />
a. DO:<br />
i. Inspect for symmetry and lesions.<br />
ii. Palpate bony prominences, parotid glands, and temporomandibular joints (TMJ).<br />
iii. Percuss the paranasal sinuses in the following areas for tenderness: above the<br />
eyes (frontal), between the eyes (ethmoid), over the malar eminences (maxillary).<br />
b. KNOW:<br />
i. An acute facial fracture may result in point tenderness, step-offs, edema,<br />
crepitus, and/or facial numbness.<br />
Ears<br />
a. DO:<br />
i. Inspect the auricle and mastoid.<br />
ii. Palpate the pinna and tragus for tenderness.<br />
iii. With the otoscope examine the external auditory calans (EAC), tympanic<br />
membranes (TMs), and note any middle ear structures visualized through the<br />
TMs.<br />
iv. Assess hearing one ear at a time with a tuning fork (512 Hz), ticking watch, or<br />
light finger rubbing.<br />
v. If hearing is asymmetrical or otherwise clinically deficient, perform the Weber<br />
and Rinne Tests assessing for sensorineural or conductive hearing loss:<br />
1. Weber’s Test: A 512 Hz vibrating tuning fork is placed on the patient’s<br />
forehead, nasal bridge, or upper teeth and the patient is asked where the<br />
sound is heard best. Normally the sound should be heard equally well in<br />
each ear. If the sound is heard asymmetrically, it means one of two<br />
things:<br />
a. KNOW: there is sensorineural loss on the side with the<br />
decreased sound OR there is conductive hearing loss on the side<br />
with the increased sound<br />
2. Rinne’s Test: the vibrating tuning fork is placed on the mastoid process.<br />
It is then held just lateral to the ear and the patient is asked which<br />
position produced the loudest sound. A positive Rinne’s test is a normal<br />
test: Air conduction85<br />
is greater than bone conduction.
The Neurological Exam Benchmark<br />
Basics:<br />
Parts of the Neurological Examination may be interspersed, depending on timing, exposure and<br />
clinician preference with other segments of the health examination (E.g., cranial nerve exam at the<br />
time of the HEENT exam, strength with the MS exam). The <strong>com</strong>plete neurological benchmark must<br />
be <strong>com</strong>pleted for <strong>com</strong>petency to be awarded.<br />
A. Basic Mental Status<br />
1. Do: An assessment of:<br />
Level of Consciousness<br />
Orientation to person, place and time (Day, date, month and year)<br />
Memory: short term (Three-word recall tests - items after 5 minutes)<br />
long term (health history)<br />
Language & Speech<br />
2. Know: The following level of consciousness terms:<br />
a. Alert<br />
b. Lethargic<br />
c. Stuporous<br />
d. Comatose<br />
3. Know: The following language/speech terms<br />
a. Aphasia<br />
b. Dysphonia<br />
c. Dysarthria<br />
B. Cranial Nerves II-XII<br />
DO:<br />
1. CNI – Olfactory – smell with alternate nostrils – coffee, mint, lemon etc…<br />
2. CNII: visual acuity, visual fields, papillary reaction & Fundi<br />
3. CNIII, IV & VI: ocular alignment, lid pupillary reaction & extra ocular movements<br />
4. CN V: facial sensation (3 distributions – forehead, cheek, lateral jaw) & muscles of<br />
mastication<br />
5. CN VII: muscles of facial expression<br />
6. CN VIII: hearing, nystagmus & balance<br />
7. CN IX & X: palateal rise to phonation & coordinated swallowing<br />
8. CN XI: sternocleidomastoid & upper trapezius strength<br />
9. CN XII: tongue size and movement<br />
KNOW:<br />
a. The parasympathetic nervous system and the sympathetic nervous system<br />
involvement in function of each nerve<br />
b. Know which muscles and movements are controlled by CN III, IV & VI<br />
10. Motor Function<br />
DO:<br />
a. Assess the following for each major muscle group of the upper and lower<br />
extremities<br />
i. Muscle bulk<br />
ii. Muscle tone<br />
iii. Strength (Myotomes)<br />
Upper extremities: Deltoids, biceps, triceps, wrist flexors, wrist extensors,<br />
hand grip, interossei muscles<br />
Lower extremities: Hip flexors, hip extensors, quadriceps, hamstrings, ankle<br />
dorsiflexors, ankle plantar flexors<br />
86
The Pelvic Examination Benchmark<br />
I. Basics & Preparation<br />
Encourage your patient to void prior to this examination.<br />
Wash your hands before the exam, and wear gloves on both hands, as indicated below.<br />
Be attentive and ensure your patient’s <strong>com</strong>fort and modesty with draping and exposure.<br />
Have appropriate supplies readily at hand: speculum, light source, cotton swabs, water soluble<br />
lubricant, culture equipment (GC, Chlamydia, HSV) and for sampling the vaginal pool (swab in<br />
test tube and carrier), and pap supplies (pap pak and liquid-pap supplies)<br />
1. Have the patient disrobe, either <strong>com</strong>pletely or to socks, as indicated by physician choice.<br />
The gown should close in the front or back, indicated by physician preference.<br />
2. Assist the patient onto the table and adjust the pillow and stirrups to fit the patient’s body<br />
size and positional <strong>com</strong>fort. Then perform any exam preceding the pelvic examination.<br />
Keep movements smooth and gentle.<br />
3. Give as much control as possible to the patient. Instruct her to let you know if you are<br />
inadvertently hurting her, or causing dis<strong>com</strong>fort. Provide reasonable explanations of your<br />
movements and intentions as you proceed through the exam.<br />
II. Examination-DO<br />
1. Vulva & Introitus<br />
A. Inspect:<br />
1.Hair pattern over lower abdomen, groin and mons pubis.<br />
2.Skin changes or concerning nevi<br />
3.labia majora and minora<br />
4.size of clitoris<br />
5.inspect perineal region for lesions or scars<br />
6.inspect the perianal region for external hemorrhoids or fissures<br />
B. Palpate:<br />
1.SBU-Skene’s gland, Bartholin’s gland, periurethral gland<br />
2.Introitus-check for hymen<br />
3.Check for location of cervix<br />
4.Evaluate for pelvic floor relaxation-cystocele, rectocele and cervical descent or<br />
prolapse<br />
2. Speculum Examination-DO<br />
A. Choose an appropriately sized speculum, and lubricated with a small amount of<br />
lubricant (water based only).<br />
B. Gently insert the speculum with the blades of the speculum oriented transversely and<br />
the gyn light turned on.<br />
C. Insert the speculum smoothly with the pressure downwards to avoid the sensitive<br />
urethral area<br />
D. Pass the speculum along the axis of the vagina, and gently rotate the speculum as it is<br />
being moved inward so that the blades be<strong>com</strong>e horizontal in orientation.<br />
E. Adjust the speculum and light as needed to visualize the cervix.<br />
F. Examine the cervix:<br />
1.Note the shape of the os, squamocolumnar junction, and any apparent lesions.<br />
2.Obtain cultures from the endocervical region for GC and Chlamydia (leave swabs in<br />
place for 30 seconds before withdrawing).<br />
3.Obtain the Papanicolaou (Pap) smear.<br />
a.Pap Slide-Spatula-Place longer end of spatula into cervical os and scrape 360<br />
degree circle, then spread cells from blade to slide along one side of the slide.<br />
Brush-then insert the brush inside the endocervix and turn 360 degrees. Wipe<br />
the brush by rolling it down the slide. Drop on or spray with fixative.<br />
87
Respiratory Clinical Benchmark Exam<br />
Basics:<br />
Table and patient are placed in the appropriate position for each section of the exam.<br />
The student can explain the reason for position changes during the respiratory exam.<br />
A. Inspection Posterior Chest:<br />
a. DO: inspect for signs of respiratory distress<br />
Inspect lips for color and nails for color and shape<br />
Inspect the posterior thorax and lungs with patient arms crossed anteriorly over the<br />
chest and hands placed on the opposite shoulder or arm<br />
Listen to the patient’s breathing for wheezing or stridor<br />
Inspect the neck for contraction of the sternocleidomastoid contraction or other use of<br />
accessory muscles<br />
Inspect the shape and movement of the chest for unbalanced movement or deformity<br />
b. KNOW: Normal resting respiratory range for adult and child<br />
Meaning of cyanosis and clubbing of the nails<br />
Meaning of wheezing and stridor and accessory muscle use<br />
Retraction of the interspaces indicates severe asthma, COPD or upper airway<br />
obstruction<br />
B. Palpation Posterior Chest:<br />
a. DO: Palpate for tenderness, masses and fremitus<br />
Test for chest expansion<br />
i. Technique: Place thumbs at the level of the 10 th rib with fingers lateral<br />
and parallel to the rib cage. Slide hands medially until there is a loose<br />
fold of skin between thumbs and spine on each side. Have the patient<br />
inhale deeply and observe the area between the thumbs for symmetry of<br />
movement to evaluate for underlying fibrosis, pleural effusion, lobar<br />
pneumonia, and unilateral bronchial obstruction.<br />
Test for tactile fremitus<br />
i. Technique: Using the ball or ulnar surface of the palm, palpate for<br />
vibrations in the 8 points (4 on each side) on the posterior thorax for<br />
symmetry, increase, decrease or absent sounds.<br />
b. KNOW: Causes of unilateral decrease or delay in expansion<br />
i. chronic fibrosis of lung or pleura, pleural effusion, lobar pneumonia,<br />
bronchial obstruction<br />
C. Percussion Posterior Chest:<br />
a. DO: Percuss the posterior chest, in 14 points (7 on each side) as for auscultation, for<br />
intensity, pitch and duration. (for technique, refer to “Guide for Physical Examination<br />
and History Taking by Bates”). Evaluate each sound for dullness and hyper resonance.<br />
b. KNOW: notes and characteristics of each note<br />
i. Definitions:<br />
1. Hyper resonance<br />
2. dullness<br />
D. Auscultation Posterior Chest:<br />
a. Do: Auscultate the 14 points previously percussed differentiating for intensity, pitch,<br />
and duration of inspiration and expiration and for adventitious sounds.<br />
b. Know: Identification of vesicular, bronchovesicular, bronchial and tracheal<br />
sounds.<br />
Meaning of adventitious sounds including crackles (rales), wheezes and rhonchi and<br />
how to utilize characteristics to focus diagnosis or rule out of pathology.<br />
88
E. Examine, Palpate, Percuss and Auscultate the Anterior chest demonstrating respect for<br />
anatomical differences of male and female patients.<br />
Know: Techniques for clinical assessment of pulmonary function including vital<br />
capacity, spirometry and imaging.<br />
F: Perform special maneuvers-whispered pectoriloquy, egophony and bronchophony<br />
Know: indications of positive results from special maneuvers.<br />
G: Pearls:<br />
Normal resting respiratory rate in an adult is 14-20 resps/minute<br />
Cyanosis indicates hypoxia. It is most apparent in the lips and nails<br />
Stridor is a high-pitched wheeze that is a sign of obstruction or secretions in the larynx<br />
or trachea<br />
Wheeze indicates constriction of the bronchioles<br />
Crackles suggest lung pathology including pneumonia, fibrosis, early CHF or of the<br />
airways as in bronchitis or bronchiectasis<br />
Clearing of crackles, wheezes or rhonchi after coughing or percussion indicates<br />
bronchitis or atelectasis.<br />
89
Multi-System Screening Examination<br />
Patient Seated<br />
1. Check height and weight<br />
2. Wash hands<br />
3. Inspect general appearance<br />
4. Check oral temperature<br />
5. Palpate, <strong>com</strong>pare, count radial pulse<br />
6. Count respiratory rate<br />
7. Measure blood pressure<br />
8. Inspect skin and nails<br />
9. Inspect and palpate the hair, scalp, skull and face<br />
10. Inspect eyes (position alignment, lids, conjunctiva, sclera)<br />
11. Inspect cornea, lens, PERRLA, corneal reflections<br />
12. Funduscopic exam<br />
13. Inspect and palpate external ears<br />
14. Otoscopic exam<br />
15. Inspect nose and palpate sinuses<br />
16. Inspect lips, tongue, teeth, buccal and labial mucosa, pharynx<br />
17. Palpate tongue, buccal and labial mucosa, palate, floor of mouth<br />
18. Inspect neck (trachea, veins)<br />
19. Inspect and palpate thyroid<br />
20. Inspect and palpate posterior chest<br />
21. Percuss posterior and lateral chest<br />
22. Auscultate posterior and lateral chest<br />
Patient Supine<br />
23. Inspect and palpate the precordium (measure PMI)<br />
24. Percuss cardiac border<br />
25. Auscultate heart<br />
26. Auscultate carotid arteries<br />
27. Auscultate abdomen, mid-epigastrium and femoral areas<br />
28. Palpate tibial and pedal pulses<br />
29. Check for pedal, tibial and pre-tibial edema<br />
30. Inspect and percuss abdomen<br />
31. Palpate abdomen<br />
32. Palpate bimanually for liver<br />
33. Palpate bimanually for spleen<br />
34. Palpate for cervical nodes<br />
35. Palpate axillary and epitrochlear nodes<br />
36. Palpate femoral nodes<br />
37. Inspect and palpate joints<br />
38. Test ROM of lower extremity<br />
91
Patient Seated<br />
39. Test ROM of upper extremity<br />
40. Inspect and percuss spine and renal angles<br />
41. Test ROM of cervical spine<br />
42. Test ROM of lumbar spine<br />
43. Check visual acuity (CN II)<br />
44. Test EOM (CN III, IV, VI)<br />
45. Check strength of temporalis and masseter (CN V)<br />
46. Check facial muscles (CN VII)<br />
47. Check auditory acuity (CN VIII)<br />
48. Check phonation, uvula, tongue (CN IX, X, XII)<br />
49. Check strength of SCM and trapezius (CN XI)<br />
50. Check DTR at biceps, triceps, patellar, achilles (C 6 / 7 / 8 ) (L 3 / 4 ) (S 1 )<br />
51. Check sensory with sharp and light touch on face and extremities<br />
Patient Standing<br />
52. Check gait<br />
53. Assess judgment and insight<br />
54. Assess orientation to person, place, and time<br />
55. Assess recent and remote memory<br />
56. Assess mood<br />
Equipment Needed for this Exam<br />
Thermometer<br />
Blood Pressure Cuff<br />
Rosenbaum Card<br />
Pen Light<br />
Ophthalmoscope<br />
Otoscope<br />
Nasal Speculum<br />
Tongue Blade<br />
Gloves<br />
Stethoscope<br />
Cotton-Tipped Applicator<br />
Reflex Hammer<br />
92
Appendix 4<br />
Naturopathic Treatment of Malignancy Consent Form<br />
In accordance with the Washington state licensing law of naturopathy, naturopathic doctors may treat<br />
malignancy only in concert with an M.D. or D.O.<br />
I, ______________________, request naturopathic care at the Bastyr Center for Natural Health.<br />
(patient’s name)<br />
An oncologist has diagnosed me with _________________________ cancer.<br />
(type of cancer)<br />
I am currently under the care of Dr. _____________________________ (M.D. or D.O.) for my cancer.<br />
(name of doctor)<br />
I understand that Washington law requires that any naturopathic care that I receive at the Bastyr Center for<br />
Natural Health for the treatment of cancer be rendered in concert with a medical or osteopathic doctor. My<br />
signature below attests to my understanding of this important relationship between my health care<br />
professionals and my <strong>com</strong>mitment to cooperate with my care providers in this collaborative treatment.<br />
Date<br />
Patient’s Name (Print)<br />
Guardian’s Name (Print)<br />
Patient’s Signature<br />
Guardian’s Signature<br />
93
I<strong>ND</strong>EX<br />
A<br />
absence · 4, 12, 33, 36, 78<br />
see unexcused<br />
B<br />
blood borne pathogen · 41<br />
C<br />
CPT codes · 70<br />
E<br />
external sites · 9<br />
F<br />
failure · 4, 24, 27, 30, 36<br />
L<br />
laboratory · 74<br />
I<br />
P<br />
patient contacts · 4, 5, 6, 7, 25<br />
Q<br />
quarterly breakdown · 10<br />
S<br />
sanction · 40<br />
substitute · 4, 5, 13, 78<br />
T<br />
time sheets · 5, 24<br />
U<br />
unexcused absence · 5<br />
W<br />
warning · 4, 36, 40<br />
interim · 5<br />
94