published
published
published
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
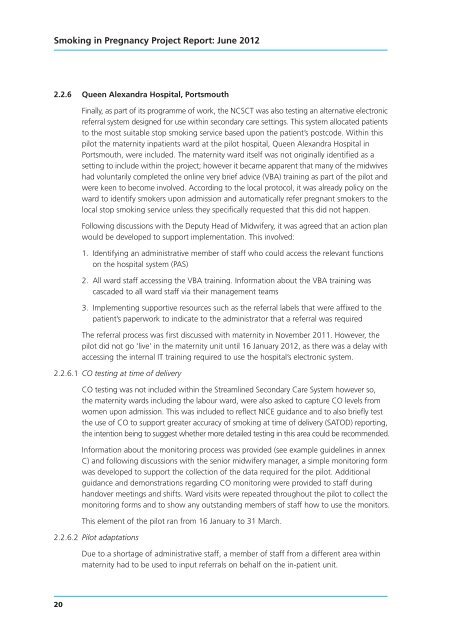
Smoking in Pregnancy Project Report: June 2012<br />
2.2.6 Queen Alexandra Hospital, Portsmouth<br />
Finally, as part of its programme of work, the NCSCT was also testing an alternative electronic<br />
referral system designed for use within secondary care settings. This system allocated patients<br />
to the most suitable stop smoking service based upon the patient’s postcode. Within this<br />
pilot the maternity inpatients ward at the pilot hospital, Queen Alexandra Hospital in<br />
Portsmouth, were included. The maternity ward itself was not originally identified as a<br />
setting to include within the project; however it became apparent that many of the midwives<br />
had voluntarily completed the online very brief advice (VBA) training as part of the pilot and<br />
were keen to become involved. According to the local protocol, it was already policy on the<br />
ward to identify smokers upon admission and automatically refer pregnant smokers to the<br />
local stop smoking service unless they specifically requested that this did not happen.<br />
Following discussions with the Deputy Head of Midwifery, it was agreed that an action plan<br />
would be developed to support implementation. This involved:<br />
1. Identifying an administrative member of staff who could access the relevant functions<br />
on the hospital system (PAS)<br />
2. All ward staff accessing the VBA training. Information about the VBA training was<br />
cascaded to all ward staff via their management teams<br />
3. Implementing supportive resources such as the referral labels that were affixed to the<br />
patient’s paperwork to indicate to the administrator that a referral was required<br />
The referral process was first discussed with maternity in November 2011. However, the<br />
pilot did not go ‘live’ in the maternity unit until 16 January 2012, as there was a delay with<br />
accessing the internal IT training required to use the hospital’s electronic system.<br />
2.2.6.1 CO testing at time of delivery<br />
CO testing was not included within the Streamlined Secondary Care System however so,<br />
the maternity wards including the labour ward, were also asked to capture CO levels from<br />
women upon admission. This was included to reflect NICE guidance and to also briefly test<br />
the use of CO to support greater accuracy of smoking at time of delivery (SATOD) reporting,<br />
the intention being to suggest whether more detailed testing in this area could be recommended.<br />
Information about the monitoring process was provided (see example guidelines in annex<br />
C) and following discussions with the senior midwifery manager, a simple monitoring form<br />
was developed to support the collection of the data required for the pilot. Additional<br />
guidance and demonstrations regarding CO monitoring were provided to staff during<br />
handover meetings and shifts. Ward visits were repeated throughout the pilot to collect the<br />
monitoring forms and to show any outstanding members of staff how to use the monitors.<br />
This element of the pilot ran from 16 January to 31 March.<br />
2.2.6.2 Pilot adaptations<br />
Due to a shortage of administrative staff, a member of staff from a different area within<br />
maternity had to be used to input referrals on behalf on the in-patient unit.<br />
20