Prefrontal Cortex, Thalamus, and Cerebellar Volumes in ...
Prefrontal Cortex, Thalamus, and Cerebellar Volumes in ...
Prefrontal Cortex, Thalamus, and Cerebellar Volumes in ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
0145-6008/05/2909-1590$03.00/0<br />
ALCOHOLISM: CLINICAL AND EXPERIMENTAL RESEARCH<br />
<strong>Prefrontal</strong> <strong>Cortex</strong>, <strong>Thalamus</strong>, <strong>and</strong> <strong>Cerebellar</strong> <strong>Volumes</strong><br />
<strong>in</strong> Adolescents <strong>and</strong> Young Adults with Adolescent-Onset<br />
Alcohol Use Disorders <strong>and</strong> Comorbid Mental Disorders<br />
Michael D. De Bellis, An<strong>and</strong>hi Narasimhan, Dawn L. Thatcher, Matcheri S. Keshavan, Paul Soloff, <strong>and</strong> Duncan B. Clark<br />
Background: In adults, prefrontal, thalamic, <strong>and</strong> cerebellar bra<strong>in</strong> <strong>in</strong>jury is associated with excessive<br />
ethanol <strong>in</strong>take. As these bra<strong>in</strong> structures are actively matur<strong>in</strong>g dur<strong>in</strong>g adolescence, we hypothesized that<br />
subjects with adolescent-onset alcohol use disorders, compared with control subjects, would have smaller<br />
bra<strong>in</strong> volumes <strong>in</strong> these areas. Thus, we compared prefrontal-thalamic-cerebellar measures of adolescents<br />
<strong>and</strong> young adults with adolescent-onset alcohol use disorders (AUD, def<strong>in</strong>ed as DSM-IV alcohol dependence<br />
or abuse) with those of sociodemographically similar control subjects.<br />
Methods: Magnetic resonance imag<strong>in</strong>g was used to measure prefrontal cortex, thalamic, <strong>and</strong> cerebellar<br />
volumes <strong>in</strong> 14 subjects (eight males, six females) with an AUD (mean age, 17.0 � 2.1 years) <strong>and</strong> 28 control<br />
subjects (16 males, 12 females; 16.9 � 2.3 years). All AUD subjects were recruited from substance abuse<br />
treatment programs <strong>and</strong> had comorbid mental disorders.<br />
Results: Subjects with alcohol use disorders had smaller prefrontal cortex <strong>and</strong> prefrontal cortex white<br />
matter volumes compared with control subjects. Right, left, <strong>and</strong> total thalamic, pons/bra<strong>in</strong>stem, right <strong>and</strong><br />
left cerebellar hemispheric, total cerebellar, <strong>and</strong> cerebellar vermis volumes did not differ between groups.<br />
There was a significant sex-by-group effect, <strong>in</strong>dicat<strong>in</strong>g that males with an adolescent-onset AUD compared<br />
with control males had smaller cerebellar volumes, whereas the two female groups did not differ <strong>in</strong><br />
cerebellar volumes. <strong>Prefrontal</strong> cortex volume variables significantly correlated with measures of alcohol<br />
consumption.<br />
Conclusions: These f<strong>in</strong>d<strong>in</strong>gs suggest that a smaller prefrontal cortex is associated with early-onset<br />
dr<strong>in</strong>k<strong>in</strong>g <strong>in</strong> <strong>in</strong>dividuals with comorbid mental disorders. Further studies are warranted to exam<strong>in</strong>e if a<br />
smaller prefrontal cortex represents a vulnerability to, or a consequence of, early-onset dr<strong>in</strong>k<strong>in</strong>g.<br />
Key Words: Alcohol Use Disorders, Alcohol Abuse or Dependence, <strong>Prefrontal</strong> <strong>Cortex</strong>, Cerebellum,<br />
Adolescence.<br />
INTRODUCTION<br />
ADOLESCENT-ONSET ALCOHOL USE disorders<br />
(AUD, def<strong>in</strong>ed as DSM-IV alcohol dependence or<br />
abuse) are prevalent <strong>and</strong> serious problems among adolescents<br />
(Clark, 2004; Johnston et al., 2003; Rohde et al.,<br />
1996). Adult AUD usually beg<strong>in</strong> dur<strong>in</strong>g adolescence (Wagner<br />
<strong>and</strong> Anthony, 2002). Studies focus<strong>in</strong>g on bra<strong>in</strong> structure<br />
<strong>and</strong> function associated with ethanol use have been<br />
From the Department of Psychiatry <strong>and</strong> Behavioral Sciences, Duke University<br />
Medical Center, Durham, North Carol<strong>in</strong>a; <strong>and</strong> Western Psychiatric<br />
Institute <strong>and</strong> Cl<strong>in</strong>ic, University of Pittsburgh Medical Center, Pittsburgh,<br />
Pennsylvania .<br />
Received for publication February 19, 2005; accepted June 6, 2005.<br />
Presented <strong>in</strong> part at the 2002 Annual Meet<strong>in</strong>g of the American Psychiatric<br />
Association, May 2002.<br />
Supported <strong>in</strong> part by NIMH grants K08MHO1324 <strong>and</strong> RO1AA12479<br />
(MDB), RO1MH01180 <strong>and</strong> RO1MH43687 (MSK), <strong>and</strong> K02AA00291 <strong>and</strong><br />
R01DA14635 (DBC) <strong>and</strong> P50AA08746 (DBC, PS).<br />
Repr<strong>in</strong>t requests: Dr. Michael D. De Bellis, Department of Psychiatry <strong>and</strong><br />
Behavioral Sciences, Duke University Medical Center, Box 3613, Durham,<br />
NC, 27710; Fax: 919-419-0165; E-mail: debel002@mc.duke.edu.<br />
Copyright © 2005 by the Research Society on Alcoholism.<br />
DOI: 10.1097/01.alc.0000179368.87886.76<br />
Vol. 29, No. 9<br />
September 2005<br />
done primarily <strong>in</strong> adults. Several studies demonstrated<br />
adult AUD is associated with abnormalities of the prefrontal<br />
cortex (PFC) (Pfefferbaum et al., 1997), thalamus (Sullivan<br />
et al., 2003), <strong>and</strong> the cerebellar hemispheres (Nicolas,<br />
2000; Torvik, 1986). Studies have demonstrated frontal<br />
gray <strong>and</strong> white matter neuroanatomical deficits primarily <strong>in</strong><br />
the adult samples (Harper, 1987; Pfefferbaum et al., 1997).<br />
One study showed differences between younger (age, 26 to<br />
44 years) <strong>and</strong> older alcoholics (age, 45 to 63 years); the<br />
older group had cortical volume deficits <strong>in</strong> both gray <strong>and</strong><br />
white matter with greatest tissue volume loss occurr<strong>in</strong>g <strong>in</strong><br />
the frontal lobes, whereas the younger group had deficits <strong>in</strong><br />
only the gray matter (Pfefferbaum et al., 1997). A prom<strong>in</strong>ent<br />
f<strong>in</strong>d<strong>in</strong>g <strong>in</strong> adult alcohol-dependent patients is hypometabolism<br />
<strong>in</strong> the medial frontal region of the cerebral<br />
cortex (Gilman et al., 1990). In another study, smaller<br />
volumes of prefrontal gray but not white matter were seen<br />
<strong>in</strong> 25 men, 22 to 41 years of age, with polysubstance use<br />
disorders (the majority of subjects used coca<strong>in</strong>e, but 13 of<br />
the 25 drank six or more dr<strong>in</strong>ks a week) compared with 14<br />
healthy volunteers (Liu et al., 1998). Smaller thalami <strong>and</strong><br />
pons (Sullivan et al., 2003), cerebellar neuronal loss (Baker<br />
1590 Alcohol Cl<strong>in</strong> Exp Res, Vol 29, No 9, 2005: pp 1590–1600
BRAIN VOLUMES IN YOUTHS 1591<br />
et al., 1999), <strong>and</strong> compromised pontocerebellar <strong>and</strong> cerebellothalamocortical<br />
systems (Sullivan 2003) were reported<br />
<strong>in</strong> adults with an AUD.<br />
PFC <strong>and</strong> the cerebellar hemispheres are bra<strong>in</strong> regions<br />
that undergo active developmental changes dur<strong>in</strong>g adolescence<br />
(Durston et al., 2001; Giedd et al., 1999; Paus et al.,<br />
2001; Pfefferbaum et al., 1994; Thompson et al., 2000). The<br />
acquisition of executive cognitive functions, which reflect<br />
the maturation of the prefrontal-thalamic-cerebellar structures,<br />
encompass higher cognitive functions (Miller <strong>and</strong><br />
Cohen, 2001; Schmahmann, 1997). Adolescents with AUD<br />
show deficits <strong>in</strong> cognitive functions, <strong>in</strong>clud<strong>in</strong>g lower IQ <strong>and</strong><br />
achievement scores <strong>in</strong> read<strong>in</strong>g than control subjects (Moss<br />
et al., 1994) <strong>and</strong> neurocognitive deficits <strong>in</strong> attention, visuospatial,<br />
<strong>and</strong> memory function<strong>in</strong>g (Brown et al., 2000). In a<br />
prospective study of adolescents with AUD, ages 14 to 17<br />
years, many of whom had at least one other substance use<br />
disorder (60% had significant cannabis use), substance use<br />
disorders predicted poorer performances on tests of memory<br />
<strong>and</strong> attention (Tapert et al., 2002b). On the other h<strong>and</strong>,<br />
subjects who were offspr<strong>in</strong>g of <strong>in</strong>dividuals with alcoholism,<br />
<strong>and</strong> so were at high familial risk for an AUD, perform<br />
poorly on measures of executive cognitive function (Giancola<br />
et al., 1996; Harden <strong>and</strong> Pihl 1995; Hill, 2004; Tarter et<br />
al., 1999). This raises speculation that as a result of <strong>in</strong>herent<br />
prefrontal-thalamic-cerebellar vulnerabilities, there may be<br />
a predisposition to an adolescent-onset AUD (Wiers et al.,<br />
1994).<br />
Consequently, as prefrontal-thalamic-cerebellar structures<br />
are actively matur<strong>in</strong>g dur<strong>in</strong>g adolescence, we compared<br />
volume measures of these regions of <strong>in</strong>terest <strong>in</strong><br />
adolescents <strong>and</strong> young adults with adolescent-onset AUD<br />
with those of matched comparison subjects. It was hypothesized<br />
that adolescents with an AUD will have structural<br />
deficits <strong>in</strong> these structures compared with sociodemographically<br />
similar healthy control subjects. Given that<br />
adult females with an AUD may show disproportionately<br />
negative effects on bra<strong>in</strong> structure <strong>and</strong> function from excessive<br />
dr<strong>in</strong>k<strong>in</strong>g than adult males with an AUD (Harper et<br />
al., 1990; Hommer et al., 1996; Hommer, 2003; Mann, et<br />
al., 1992), a comparison of sex differences was also planned.<br />
MATERIALS AND METHODS<br />
Subjects<br />
Adolescents (def<strong>in</strong>ed as age 13 to 17 years) <strong>and</strong> young adults (def<strong>in</strong>ed<br />
as age 18 to 21 years) with an adolescent-onset AUD <strong>and</strong> healthy comparison<br />
subjects were recruited (Table 1). Because of the high degree of<br />
known variability <strong>in</strong> volume of bra<strong>in</strong> structures (Lange et al., 1997), two<br />
healthy comparison subjects were case-matched for each subject with an<br />
AUD for age (with<strong>in</strong> six months), sex, <strong>and</strong> h<strong>and</strong>edness. Groups were<br />
similar on height, weight, socioeconomic status (SES) <strong>and</strong> full-scale IQ.<br />
The comparison group was recruited by advertisement from the community<br />
<strong>and</strong> these subjects had no lifetime histories of psychiatric disorders,<br />
<strong>in</strong>clud<strong>in</strong>g alcohol <strong>and</strong> substance use disorders.<br />
Table 1. Demographic Characteristics of Subjects with an Adolescent Onset AUD <strong>and</strong> Matched Comparison Subjects<br />
AUD AUD males AUD females Control Control males Control females AUD vs.Controls p<br />
N 14 8 6 28 16 12 X2�0 NS<br />
Age (years)(range <strong>in</strong> years) 17.0 � 2.1 (14.0 - 20.6) 16.4 � 2.1 (14.0 - 19.1) 17.8 � 2.0 (15.0 - 20.9) 16.9 � 2.3 (13.5 - 21) 15.9 � 1.9 (13.5 - 19.7) 18.1 � 2.2 (15.5 -21) T40� 0.21 0.84<br />
Weight (kg) 68.5 � 11.5 66.0 � 13.2 71.9 � 8.8 68.4 � 17.6 71.8 � 17.8 64.0 � 17.2 T40� 0.02 0.99<br />
Height (cm) 169.6 � 11.0 173.9 � 13.1 163.8 � 2.3 170.1 � 10.2 174.5 � 8.1 164.3 � 10.0 T40�-0.16 0.88<br />
SES 34.3 � 7.5 32.0 � 5.8 37.7 � 8.5 37.8 � 8.8 38.6 � 8.1 36.8 � 9.9 T40�-1.35 0.18<br />
Fullscale IQ 105.6 � 13.0 107.6 � 12.8 103 � 14.1 111.8 � 16.4 112 � 15.9 111 � 17.8 T40�-1.24 0.22<br />
Age of onset of AUD (years) 15.6 � 2.4 14.6 � 2.7 16.6 � 2.2 ––<br />
Duration of AUD (years) 1.4 � 0.7 1.5 � 0.6 1.2 � 0.9 ––<br />
Average number of dr<strong>in</strong>ks<br />
7.3 � 3.0 (3 - 13) 7.6 � 2.6 (5 - 13) 6.9 � 3.7 (3 - 13) 0.27 � 0.38 (0 - 1) 0.25 � 0.33 (0 - 1) 0.30 � 0.48 (0 - 1)<br />
per dr<strong>in</strong>k<strong>in</strong>g occasion(range)<br />
Number of dr<strong>in</strong>ks per maximum 12.1 � 6.8 (5.0 - 25) 13.6 � 7.9 (6.0 - 25) 10.0 � 5.0 (5.0 - 18) 0.54 � 0.8 (0 - 2) 0.5 � 0.7 (0 - 2) 0.6 � 0.9 (0 - 2)<br />
dr<strong>in</strong>k<strong>in</strong>g episode(range)<br />
Yearly alcohol quantity/frequency<br />
group<strong>in</strong>g (number <strong>in</strong> each group)<br />
Absta<strong>in</strong>ers<br />
0<br />
0<br />
0<br />
18<br />
8<br />
10<br />
Less than 1 dr<strong>in</strong>k/week<br />
0<br />
0<br />
0<br />
6<br />
4<br />
2<br />
Less than 0.5 dr<strong>in</strong>k/day<br />
2<br />
1<br />
1<br />
4<br />
4<br />
0<br />
0.5 to 1.5 dr<strong>in</strong>ks/day<br />
4<br />
2<br />
2<br />
0<br />
0<br />
0<br />
2.0� dr<strong>in</strong>ks/day<br />
8<br />
5<br />
3<br />
0<br />
0<br />
0<br />
SES, socioeconomic status.
1592 DE BELLIS ET AL.<br />
Cl<strong>in</strong>ical Evaluation<br />
Substance use disorder diagnoses were determ<strong>in</strong>ed us<strong>in</strong>g a modified<br />
form of the Structured Cl<strong>in</strong>ical Interview for the DSM-IV (Mart<strong>in</strong> et al.,<br />
2000). Information was gathered by direct <strong>in</strong>terviews because family <strong>in</strong>formants<br />
typically underreport alcohol <strong>and</strong> drug <strong>in</strong>volvement (Kosten et<br />
al., 1992). For each symptom, ages of onset were recorded to the nearest<br />
month. The <strong>in</strong>terviewers had Masters-level education <strong>in</strong> mental healthrelated<br />
fields <strong>and</strong> were <strong>in</strong>dividually tra<strong>in</strong>ed to obta<strong>in</strong> greater than 90%<br />
agreement with an experienced <strong>in</strong>terviewer. Interrater reliabilities were<br />
high for <strong>in</strong>dividual DSM-IV symptoms (� � 0.84 to 1.0) <strong>and</strong> for AUD<br />
diagnoses (� � 0.94) (Mart<strong>in</strong> et al., 2000). Other Axis I mental disorders<br />
were assessed us<strong>in</strong>g a modified version of the Schedule for Affective<br />
Disorders <strong>and</strong> Schizophrenia for School-Age, Present Episode (K-<br />
SADS-P) (Chambers et al., 1985) <strong>and</strong> Lifetime Version (K-SADS-E)<br />
(Orvaschel <strong>and</strong> Puig–Antich, 1987) <strong>in</strong>terview, with both adolescent <strong>and</strong><br />
parent(s) as <strong>in</strong>formants. An exp<strong>and</strong>ed assessment of posttraumatic stress<br />
disorder (PTSD) was completed as part of the K-SADS Present <strong>and</strong><br />
Lifetime Version (Kaufman et al., 1997). Consensus diagnoses were<br />
reached among the <strong>in</strong>terviewer, the assessment coord<strong>in</strong>ator, <strong>and</strong> a cl<strong>in</strong>ically<br />
experienced faculty psychiatrist or psychologist us<strong>in</strong>g the best estimate<br />
method (Clark, 1999; Kosten <strong>and</strong> Rounsaville, 1992), <strong>in</strong> which a date<br />
of onset, def<strong>in</strong>ed as the time at which diagnostic criteria were first met, is<br />
determ<strong>in</strong>ed for each disorder (Clark et al., 2001). The Lifetime History of<br />
Alcohol Use Interview (Sk<strong>in</strong>ner, 1982) was used to collect supplemental<br />
<strong>in</strong>formation on alcohol <strong>and</strong> other abused substances, <strong>in</strong>clud<strong>in</strong>g the average<br />
quantity <strong>and</strong> frequency of use <strong>and</strong> the maximum frequency <strong>and</strong><br />
quantity of use for alcohol <strong>and</strong> seven other drug classes (stimulates<br />
[caffe<strong>in</strong>e, nicot<strong>in</strong>e], sedatives [barbiturates], opioids [hero<strong>in</strong>, morph<strong>in</strong>e,<br />
code<strong>in</strong>e], hypnotics [Valium], halluc<strong>in</strong>ogens/PCP, cannabis [marijuana],<br />
<strong>in</strong>halants) for each year of a subject’s life. The Alcohol Consumption<br />
Questionnaire (ACQ), which was based on survey <strong>in</strong>struments that Cahalan<br />
(1981) developed, was used to measure the quantity <strong>and</strong> frequency<br />
of alcohol consumption <strong>in</strong> the past year (Cahalan, 1981). The ACQ is a<br />
self-report <strong>in</strong>ventory designed to categorize the average frequency, average<br />
quantity, maximum quantity, frequency of maximum quantity, <strong>and</strong><br />
type of alcohol used <strong>in</strong> the past 12 months to form a yearly alcohol<br />
quantity/frequency group<strong>in</strong>g (Table 1). The quantity <strong>and</strong> frequency of<br />
alcohol consumption <strong>and</strong> other alcohol consumption variables were measured<br />
by a questionnaire us<strong>in</strong>g face valid items found to have acceptable<br />
psychometric properties <strong>in</strong> other studies (Grant et al., 1995; Has<strong>in</strong> <strong>and</strong><br />
Carpenter, 1998). Quantity variables were based on 0.6-oz. (17-g) ethanol<br />
“st<strong>and</strong>ard dr<strong>in</strong>ks” (one 12-oz. [340-g] beer, one 5-oz. [142-g] glass of table<br />
w<strong>in</strong>e [12% alcohol by volume], or one 1.5 oz. [42.5 g] of 80-proof hard<br />
liquor), <strong>and</strong> the frequency variables were calculated as number of occasions<br />
per month.<br />
The alcohol use disorder group consisted of n<strong>in</strong>e with lifetime alcohol<br />
dependence (five males, four females) <strong>and</strong> five with lifetime alcohol abuse<br />
(three males, two females). AUD subjects were recruited from treatment<br />
programs <strong>in</strong> the Pittsburgh Area. Comorbidity is common <strong>in</strong> adolescent<br />
AUD; other studies have shown that a substantial percentage of adolescents<br />
with AUD are comorbid with other substance use disorders (particularly<br />
cannabis), conduct disorder, attention deficient hyperactivity disorder,<br />
mood disorders, <strong>and</strong> posttraumatic stress disorder (Clark et al., 1997).<br />
In our sample, subjects had a mean of 4.1 � 2.4 <strong>and</strong> range of 2 to 9 lifetime<br />
Axis I disorders. Comorbidity <strong>in</strong>cluded the follow<strong>in</strong>g: other substance<br />
abuse or dependence (cannabis [n � 11], eight males, three females) or<br />
halluc<strong>in</strong>ogens (n � 2, males), major depressive disorder (n � 10; five<br />
males, five females), conduct disorder (n � 8; six males, two females),<br />
posttraumatic stress disorder (n � 7; five males, two females), attentiondeficit<br />
hyperactivity disorder (n � 7; six males, one female), oppositional<br />
defiant disorder (n � 2; two males), generalized anxiety disorder (n � 2;<br />
two females), <strong>and</strong> bipolar disorder (n � 1, male). It should be noted that<br />
there was overlap <strong>in</strong> that all AUD subjects with ADHD had conduct<br />
disorder or oppositional defiant disorder, that all AUD subjects with<br />
PTSD except one had major depression, <strong>and</strong> all AUD subjects with major<br />
depression had a cannabis use disorder except three. The age of onset for<br />
Table 2. Cl<strong>in</strong>ical characteristics of adolescents <strong>and</strong> young adults with an<br />
adolescent-onset AUD<br />
AUD AUD males<br />
(n � 8)<br />
AUD females<br />
(n � 6)<br />
Alcohol abuseAlcohol<br />
dependence<br />
59 35 24<br />
Number of co-morbid<br />
axis I disorders<br />
4.1 � 2.4 4.6 � 1.8 3.3 � 3.0<br />
Number with CUD 11 8 3<br />
Halluc<strong>in</strong>ogen abuse 2 2 0<br />
Number with MDD 10 5 5<br />
Number with PTSD 7 5 2<br />
Number with ADHD 7 6 1<br />
Number with CD 8 6 2<br />
Number with ODD 2 2 0<br />
Number with GAD 2 0 2<br />
Number with bipolar disorder 1 1 0<br />
CUD, Cannabis use disorder; MDD, major depressive disorder; PTSD, posttraumatic<br />
stress disorder; ADHD, attention deficit hyperactivity disorder; CD,<br />
conduct disorder; ODD, oppositional defiant disorder; GAD, generalized anxiety<br />
disorder.<br />
an alcohol use disorder was 15.6 � 2.4 years. Although the mean age of<br />
onset for the 11 subjects with cannabis use disorder was 15.0 � 2.2 years,<br />
for n<strong>in</strong>e of these subjects the alcohol use disorder diagnosis preceded their<br />
cannabis use disorder. Some comorbid disorders preceded (ADHD) or<br />
co-occurred with the AUD (major depression, conduct disorder, bipolar<br />
disorder). See Table 2. Bra<strong>in</strong> structural (cerebral, amygdala, hippocampal,<br />
lateral ventricle) volumes <strong>and</strong> corpus callosum areas for 12 of the 14<br />
subjects with alcohol use disorder <strong>and</strong> 24 of the 28 healthy comparison<br />
subjects were previously reported (De Bellis et al., 2000a).<br />
Subjects were excluded from the study if the follow<strong>in</strong>g were found: 1)<br />
AUD subjects were admitted to the University of Pittsburgh Medical<br />
Center’s General Cl<strong>in</strong>ical Research Center to ensure that they did not use<br />
drugs or alcohol before the MRI scan. Thus, AUD subjects were excluded<br />
from the study if the follow<strong>in</strong>g were found: the use of drugs dur<strong>in</strong>g the two<br />
weeks before the MR scan (confirmed by a negative ur<strong>in</strong>e drug screen 12<br />
hours before the MRI scan), <strong>and</strong> the use of alcohol with<strong>in</strong> 12 hours of the<br />
MRI scan (confirmed by a negative alcohol breathalyzer test); 2) presence<br />
of a significant medical or neurological illness; 3) gross obesity (weight<br />
greater than 150% of ideal body weight) or growth failure (height under<br />
third percentile); 4) full-scale <strong>in</strong>telligence below 80, as estimated by the<br />
short form of the Wechsler Intelligence Scale for Children, Third Edition,<br />
or the Wechsler Adult Intelligence Scale, Third Edition; 5) pregnancy; <strong>and</strong><br />
6) <strong>in</strong>sufficient English skills for consent<strong>in</strong>g to the protocol. This protocol<br />
was approved by the University of Pittsburgh Institutional Review Board.<br />
Subjects or their parent(s) or legal guardian(s) gave written <strong>in</strong>formed<br />
consent. Adolescents under age 14 years assented before participat<strong>in</strong>g <strong>in</strong><br />
this protocol. Adolescents 14 years of age <strong>and</strong> older gave written <strong>in</strong>formed<br />
consent along with the written <strong>in</strong>formed consent of their parent or legal<br />
guardian. Subjects aged 18 years or older gave written <strong>in</strong>formed consent.<br />
Thus, no subject was consented to participate <strong>in</strong>dependently of a parent or<br />
legal guardian. Subjects received monetary compensation for participation.<br />
MRI Acquisition<br />
All volumetric MRI scans were performed with the use of a GE<br />
1.5-Tesla Unit (Signa System, General Electric Medical Systems, Milwaukee,<br />
WI) runn<strong>in</strong>g version 5.4 software located at the University of Pittsburgh<br />
Medical Center (UPMC) MR Research Center. The subject’s head<br />
was aligned <strong>in</strong> a head holder with foam padd<strong>in</strong>g, us<strong>in</strong>g soft towels <strong>and</strong> ch<strong>in</strong><br />
<strong>and</strong> forehead straps to m<strong>in</strong>imize head movement. The subject’s nose was<br />
positioned at the 12 o’clock position for alignment, <strong>and</strong> a gradient echo<br />
localiz<strong>in</strong>g axial slice verified this plane. A sagittal series (us<strong>in</strong>g TE � 18<br />
msec, TR � 400 msec, flip angle � 90 degrees, acquisition matrix � 256<br />
� 192, NEX � 1, FOV � 20 cm, slices � 21) verified patient position,
BRAIN VOLUMES IN YOUTHS 1593<br />
cooperation, <strong>and</strong> image quality. We required that the midsagittal slice<br />
show full visualization of the cerebral aqueduct <strong>and</strong> the anterior <strong>and</strong><br />
posterior commissures, <strong>in</strong> which a l<strong>in</strong>e was estimated requir<strong>in</strong>g the<br />
anterior-commissure-posterior-commissure l<strong>in</strong>e to be with<strong>in</strong> three degrees<br />
of 180. If these criteria were not met, the subject was realigned until these<br />
criteria were met. A three-dimensional spoiled gradient recalled acquisition<br />
<strong>in</strong> the steady-state pulse sequence was used to obta<strong>in</strong> 124 contiguous<br />
images with slice thickness of 1.5 mm <strong>in</strong> the coronal plane for region of<br />
<strong>in</strong>terest measures (TE � 5 msec, TR � 25 msec, flip angle � 40 degrees,<br />
acquisition matrix � 256 � 192, number of excitations � 1, field of vision<br />
� 24 cm). Coronal sections were obta<strong>in</strong>ed perpendicular to the anteriorcommissure-posterior-commissure<br />
l<strong>in</strong>e to provide a more reproducible<br />
guide for image orientation. Axial proton density <strong>and</strong> T 2-weighted images<br />
were obta<strong>in</strong>ed to enable exclusion of structural abnormalities on MRI. A<br />
neuroradiologist reviewed all scans <strong>and</strong> ruled out cl<strong>in</strong>ically significant<br />
abnormalities. All subjects tolerated the procedure well. No sedation was<br />
used.<br />
The imag<strong>in</strong>g data from the coronal sections were transferred from the<br />
MRI unit to a computer workstation (PowerMac<strong>in</strong>tosh, Apple Computer)<br />
<strong>and</strong> analyzed with the use of IMAGE software (version 1.61) developed at<br />
the NIH (Rasb<strong>and</strong>, 1996) that provides valid <strong>and</strong> reliable volume measurements<br />
of specific structures us<strong>in</strong>g a manually operated (h<strong>and</strong> trac<strong>in</strong>g)<br />
approach. Tra<strong>in</strong>ed <strong>and</strong> reliable raters who were bl<strong>in</strong>ded to subject <strong>in</strong>formation<br />
made all measurements. These methods were previously described<br />
by our group (De Bellis et al., 1999; De Bellis et al., 2002; De Bellis et al.,<br />
2001) <strong>and</strong> are briefly presented here.<br />
Intracranial volumes were calculated by first manually trac<strong>in</strong>g the<br />
<strong>in</strong>tracranial volume of each coronal slice after exclusion of skull <strong>and</strong> dura,<br />
then summ<strong>in</strong>g these areas of successive coronal slices, <strong>in</strong>clud<strong>in</strong>g GM <strong>and</strong><br />
WM <strong>and</strong> cerebral sp<strong>in</strong>al fluid (CSF) volumes, <strong>and</strong> multiply<strong>in</strong>g by slice<br />
thickness. These measures <strong>in</strong>cluded frontal, parietal, temporal, occipital<br />
cortex, subcortical structures, cerebellum, <strong>and</strong> bra<strong>in</strong>stem.<br />
Cerebral volumes were measured after manual exclusion of CSF volumes,<br />
cerebellum, <strong>and</strong> bra<strong>in</strong>stem <strong>in</strong> the same manner <strong>and</strong> <strong>in</strong>cluded cortical<br />
<strong>and</strong> subcortical structures.<br />
<strong>Prefrontal</strong> cortex volumes were calculated by summ<strong>in</strong>g up areas of<br />
successive coronal slices, <strong>in</strong>clud<strong>in</strong>g gray <strong>and</strong> white matter <strong>and</strong> CSF volumes<br />
<strong>and</strong> multiply<strong>in</strong>g by slice thickness. The anterior boundary of the<br />
prefrontal cortex was def<strong>in</strong>ed as the most anterior coronal section conta<strong>in</strong><strong>in</strong>g<br />
gray matter. The coronal slice show<strong>in</strong>g the genu of the corpus<br />
callosum was used to mark the posterior limit of the prefrontal cortex<br />
(Rosenberg et al., 1997). <strong>Prefrontal</strong> white <strong>and</strong> gray matter volumes were<br />
calculated by us<strong>in</strong>g a semiautomated segmentation algorithm. This computerized<br />
segmentation technique uses mathematically derived cutoffs for<br />
gray matter–white matter–CSF partitions with histograms of signal <strong>in</strong>tensities.<br />
This computerized segmentation technique is both labor <strong>in</strong>tensive<br />
<strong>and</strong> manually operated. It uses an <strong>in</strong>teractive method <strong>in</strong> which mathematically<br />
derived cutoffs for gray matter–white matter–CSF partitions from<br />
histograms of signal <strong>in</strong>tensities are used to <strong>in</strong>dividually select gray matter,<br />
white matter, <strong>and</strong> CSF areas from each coronal slice. Gray matter, white<br />
matter, <strong>and</strong> CSF areas are thus separately calculated <strong>and</strong> multiplied by<br />
slice thickness for the <strong>in</strong>dividual subject’s gray matter, white matter, <strong>and</strong><br />
CSF volumes. In this way, we can m<strong>in</strong>imize the <strong>in</strong>herent limitations on<br />
qualify<strong>in</strong>g white matter signal hypo<strong>in</strong>tensities as gray matter on T 1weighted<br />
MRI scans by visual <strong>in</strong>spection of slices (i.e., so that hypo<strong>in</strong>tensity<br />
artifacts <strong>in</strong> corpus callosum or cerebral white matter are not calculated<br />
as gray matter). This approach has been validated by us<strong>in</strong>g both a stereology<br />
technique for bra<strong>in</strong> morphometric measurements <strong>and</strong> a phantom<br />
with known absolute volumes (Keshavan et al., 1995) <strong>and</strong> has been used <strong>in</strong><br />
several published neuroimag<strong>in</strong>g studies (De Bellis et al., 1999; De Bellis et<br />
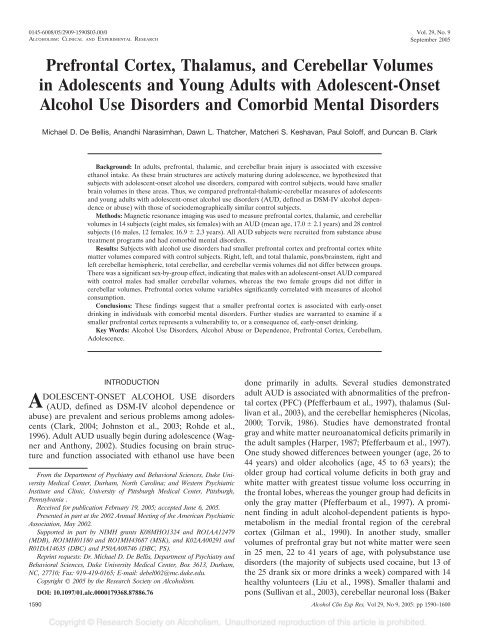
al., 2001; Rosenberg et al., 1997). See Fig. 1.<br />
The boundaries of the thalamus were previously described (Gilbert et<br />
al., 2000). The boundaries of the thalamus were def<strong>in</strong>ed as follows: The<br />
mammillary bodies <strong>and</strong> the <strong>in</strong>terventricular foramen def<strong>in</strong>ed the anterior<br />
boundary; the <strong>in</strong>ternal capsule def<strong>in</strong>ed the lateral boundary; the third<br />
ventricle def<strong>in</strong>ed the medial boundary; the hypothalamus def<strong>in</strong>ed the<br />
<strong>in</strong>ferior boundary; the lateral ventricle def<strong>in</strong>ed the superior boundary; <strong>and</strong><br />
Fig. 1. Manual trac<strong>in</strong>gs of PFC. PFC volumes were calculated by summ<strong>in</strong>g up<br />
areas of successive coronal slices <strong>and</strong> multiply<strong>in</strong>g by slice thickness. The anterior<br />
boundary of the prefrontal cortex was def<strong>in</strong>ed as the most anterior coronal<br />
section conta<strong>in</strong><strong>in</strong>g gray matter. The coronal slice show<strong>in</strong>g the genu of the corpus<br />
callosum was used to mark the posterior limit of the prefrontal cortex. <strong>Prefrontal</strong><br />
white <strong>and</strong> gray matter volumes were calculated by us<strong>in</strong>g a semiautomated<br />
segmentation algorithm (not shown).<br />
the crus fornix def<strong>in</strong>ed the posterior boundary of the thalamus. Every<br />
coronal slice that <strong>in</strong>cluded the thalamus was manually traced, <strong>and</strong> total<br />
volume was computed by summ<strong>in</strong>g up successive areas <strong>and</strong> multiply<strong>in</strong>g by<br />
slice thickness.<br />
The volumes of the cerebellum, vermis, <strong>and</strong> bra<strong>in</strong>stem were calculated<br />
by summ<strong>in</strong>g up areas of successive coronal slices after trac<strong>in</strong>g the region<br />
of <strong>in</strong>terest <strong>and</strong> exclud<strong>in</strong>g CSF as previously described (Hardan et al.,<br />
2001). Briefly, measurements began as the cerebellum appeared laterally<br />
to the pons. The tentorium cerebelli acted as the superior limit <strong>and</strong> the<br />
base of the cerebellum itself as the <strong>in</strong>ferior limit. The cisterna magna <strong>and</strong><br />
transverse s<strong>in</strong>us were excluded. The last slice <strong>in</strong>cluded was the one at<br />
which the cerebellum was no longer dist<strong>in</strong>guishable from the transverse<br />
s<strong>in</strong>us or disappeared. The measurement of the vermis began at the slice<br />
where the anterior <strong>and</strong>/or <strong>in</strong>ferior posterior lobes appeared. The gray<br />
matter of the vermis structures, determ<strong>in</strong>ed by mathematically derived<br />
cutoffs for gray matter–white matter–CSF partitions from histograms of<br />
signal <strong>in</strong>tensities as previously described (De Bellis et al., 2001), were<br />
traced separately until the slice where the fourth ventricle was no longer<br />
visible. The cerebellar medullary body <strong>and</strong> the deep cerebellar nuclei were<br />
excluded. Measurements were made around the vermis until it was no<br />
longer visible. The first slice of the bra<strong>in</strong>stem was measured where the<br />
pons first appeared with<strong>in</strong> the suprasellar cistern. The cerebellar peduncles,<br />
<strong>in</strong>clud<strong>in</strong>g the brachium pontis (middle), were <strong>in</strong>cluded <strong>in</strong> the<br />
bra<strong>in</strong>stem. In the anterior plane, the superior limit of the pons was a<br />
straight l<strong>in</strong>e connect<strong>in</strong>g the ambient cisterns from left to right. Posterior<br />
measurements <strong>in</strong>cluded the cerebral aqueduct <strong>and</strong> the superior colliculus.<br />
No separate volumetric measurements were made for the midbra<strong>in</strong>, pons,<br />
<strong>and</strong> medulla oblongata. See Fig. 2.<br />
Intraclass correlation of <strong>in</strong>terrater <strong>and</strong> <strong>in</strong>trarater reliability for <strong>in</strong>dependent<br />
designation of regions on segmented images obta<strong>in</strong>ed from 20<br />
subjects were 0.99 <strong>and</strong> 0.99 for <strong>in</strong>tracranial volume, cerebral volume,<br />
cerebral CSF, prefrontal lobe volume, prefrontal lobe gray matter, prefrontal<br />
lobe white matter, prefrontal CSF; 0.96 <strong>and</strong> 0.98 respectively, for<br />
right, left, <strong>and</strong> total thalamus volumes; 0.91 <strong>and</strong> 0.95 respectively, for right,<br />
left, <strong>and</strong> total cerebellum; 0.89 <strong>and</strong> 0.94 respectively, for pons/bra<strong>in</strong>stem;<br />
<strong>and</strong> 0.91 <strong>and</strong> 0.92 respectively, for cerebellar vermis.<br />
Statistical Methods<br />
Demographic variables were compared by means of Student’s t test <strong>and</strong><br />
Pearson 2 as appropriate. Histograms were obta<strong>in</strong>ed to assess normality of<br />
the data <strong>and</strong> to observe any outly<strong>in</strong>g observations. There were no significant<br />
outliers, <strong>and</strong> we did not exclude any cases <strong>in</strong> our data analyses.<br />
Formal hypothesis test<strong>in</strong>g was carried out by t tests <strong>in</strong> two stages, first with<br />
the raw data, then aga<strong>in</strong> adjust<strong>in</strong>g for total cerebral volume, to determ<strong>in</strong>e<br />
differences between AUD subjects <strong>and</strong> control subjects. In test<strong>in</strong>g for<br />
covariate effects such as sex <strong>and</strong> <strong>in</strong>teractions (sex-by-group), multivariate<br />
regression analysis was used. Bra<strong>in</strong> structural means, which differed significantly<br />
between the groups (e.g., PFC volumes), were adjusted for<br />
cerebral volume to correct for <strong>in</strong>dividual differences <strong>in</strong> bra<strong>in</strong> size with<br />
regard to gender <strong>and</strong> then correlated with cl<strong>in</strong>ical data us<strong>in</strong>g Spearman<br />
correlation coefficients. All significance test<strong>in</strong>g <strong>in</strong>volv<strong>in</strong>g the ma<strong>in</strong> hypoth-
1594 DE BELLIS ET AL.<br />
Fig. 2. Manual trac<strong>in</strong>gs of cerebellum, vermis, <strong>and</strong> bra<strong>in</strong>stem. The volumes of the cerebellum, vermis, <strong>and</strong> bra<strong>in</strong>stem were calculated by summ<strong>in</strong>g up areas of<br />
successive coronal slices after trac<strong>in</strong>g the region of <strong>in</strong>terest. Measurements began as the cerebellum appeared laterally to the pons (not shown). The last slice <strong>in</strong>cluded<br />
was the one at which the cerebellum was no longer dist<strong>in</strong>guishable from the transverse s<strong>in</strong>us or disappeared (not shown). The measurement of the vermis began at<br />
the slice where the anterior <strong>and</strong>/or <strong>in</strong>ferior posterior lobes appeared (A). This slice <strong>in</strong>cluded the bra<strong>in</strong>stem. The gray matter of the vermis structures, determ<strong>in</strong>ed by<br />
mathematically derived cutoffs for gray matter–white matter–CSF partitions from histograms of signal <strong>in</strong>tensities, were traced separately (B, C, D, E). Measurements<br />
were made around the vermis until it was no longer visible with<strong>in</strong> the cerebellar hemispheres (F). The first slice of the bra<strong>in</strong>stem was measured where the pons first<br />
appeared with<strong>in</strong> the suprasellar cistern (not shown). The cerebellar peduncles, <strong>in</strong>clud<strong>in</strong>g the brachium pontis (middle), were <strong>in</strong>cluded <strong>in</strong> the bra<strong>in</strong>stem (A). Posterior<br />
measurements <strong>in</strong>cluded the cerebral aqueduct <strong>and</strong> the superior colliculus. No separate volumetric measurements were made for the midbra<strong>in</strong>, pons, <strong>and</strong> medulla<br />
oblongata.<br />
esis was two-tailed with � 0.05. All data are presented as mean � SD<br />
unless otherwise specified.<br />
RESULTS<br />
Subjects with an adolescent-onset AUD had smaller PFC<br />
(p � 0.02) <strong>and</strong> PFC white matter (p � 0.007) volumes <strong>and</strong><br />
greater amounts of PFC CSF (p � 0.01) compared with<br />
healthy comparison subjects. Smaller PFC (p � 0.02), PFC<br />
white matter (p � 0.004), <strong>and</strong> larger PFC CSF (p � 0.001)<br />
volumes persisted when controll<strong>in</strong>g for cerebral volume.<br />
See Table 3. These results also persisted when controll<strong>in</strong>g<br />
for cerebral volume <strong>and</strong> age, sex, <strong>and</strong> sex-by-group <strong>in</strong>teractions<br />
for smaller PFC (F 1,36 � 5.8, p � 0.02) <strong>and</strong> PFC<br />
white matter (F 1,36 � 9.0, p � 0.005), <strong>and</strong> larger PFC CSF<br />
(F 1,36 � 12.0, p � 0.001) volumes. No effects of age, sex, or<br />
sex-by-group were seen <strong>in</strong> these analyses.<br />
Given that both major depression (Ste<strong>in</strong>gard et al., 2002)<br />
<strong>and</strong> ADHD (Castellanos et al., 1996; Mostofsky et al., 2002;<br />
Sowell et al. 2003a) <strong>in</strong> adolescents has been associated with<br />
smaller frontal volumes, multivariate regression analysis<br />
was used to further exam<strong>in</strong>e the results us<strong>in</strong>g comorbidity<br />
(number of comorbid disorders), sex, sex-by-group, <strong>and</strong><br />
us<strong>in</strong>g PFC outcome variables least squares adjusted for<br />
cerebral volume. Although these analyses have decreased<br />
power, the results did confirm larger PFC CSF (F 1,37 �<br />
5.27, p � 0.03) <strong>in</strong> subjects with an adolescent-onset AUD<br />
<strong>and</strong> suggested that subjects with an adolescent-onset AUD<br />
had smaller PFC (F 1,37 � 2.73, p � 0.1) <strong>and</strong> smaller PFC<br />
white matter volumes (F 1,37 � 2.4, p � 0.1), compared with<br />
healthy comparison subjects. Furthermore, multivariate regression<br />
analysis exam<strong>in</strong><strong>in</strong>g PFC variables us<strong>in</strong>g comorbidity<br />
(presence of major depression, presence of ADHD),<br />
presence of a cannabis use disorder, <strong>and</strong> controll<strong>in</strong>g for sex<br />
<strong>and</strong> cerebral volume did confirm larger PFC CSF (F 1,34 �<br />
9.0, p � 0.005) <strong>in</strong> subjects with an adolescent-onset AUD<br />
<strong>and</strong> suggested that subjects with an adolescent-onset AUD<br />
had smaller PFC suggested smaller PFC (F 1,34 � 2.4, p �<br />
0.1), compared with healthy comparison subjects. The estimates<br />
for these comorbidities <strong>in</strong> these above regression<br />
models were not significant. To further explore this issue of<br />
comorbidity, we ran the follow<strong>in</strong>g analyses. There were no<br />
significant differences when PFC volumes (adjusted for<br />
cerebral volumes) <strong>in</strong> AUD subjects with major depression<br />
(mean, 162.2 � 14.2 cm 3 ) <strong>and</strong> without major depression<br />
(mean, 155.7 � 15.2 cm 3 )(t 1,12 � -0.77, p � 0.45) were<br />
compared with<strong>in</strong> AUD groups or when AUD subjects with<br />
ADHD (mean, 159.9 � 9.2 cm 3 ) <strong>and</strong> without ADHD<br />
(mean, 161.0 � 18.7 cm 3 )(t 1,12 � 0.13, p � 0.89) were<br />
compared with<strong>in</strong> AUD groups. There were no significant<br />
differences when PFC volumes adjusted for cerebral volumes<br />
<strong>in</strong> AUD subjects with a cannabis use disorder (mean,<br />
160.7 � 16.1 cm 3 ) <strong>and</strong> without a cannabis use disorder<br />
(mean, 159.3 � 3.5 cm 3 ) were compared with<strong>in</strong> AUD<br />
groups (t 1,12 � -0.14, p � 0.89). Furthermore, there were no
BRAIN VOLUMES IN YOUTHS 1595<br />
Table 3. Bra<strong>in</strong> structures of subjects with an adolescent-onset AUD <strong>and</strong> matched comparison subjects<br />
Structures (cm 3 ) AUD AUD males AUD females Control Controlmales Controlfemales AUD vs.controls Covariate, t 1,39, p value<br />
Intracranial volume 1477.8 � 105.4 1503.0 � 117.2 1444.2 � 185.3 1547.7 � 135.0 1618.9 � 104.8 1452.8 � 115.1 t � -1.68 p � 0.1 —<br />
Cerebral volume 1283.5 � 103.2 1307.0 � 116.7 1252.2 � 81.1 1322.0 � 153.3 1404.5 � 89.0 1211.9 � 154.1 t � -0.85 p � 0.40 —<br />
Cerebral CSF 37.7 � 12.8 36.7 � 15.3 39.0� 9.9 41.2 � 11.8 39.3 � 11.9 45.7 � 11.4 t � -0.82 p � 0.42 —<br />
PFC volume 157.1 � 18.1 158.1 � 18.0 155.7 � 19.8 175.9 � 26.6 184.2 � 23.2 164.9 � 27.7 t � -2.38 p � 0.02 Group: t � -2.47, p � 0.0 Cerebral<br />
Vol: t � 6.23, p � 0.0001<br />
PFC gray matter 107.1 � 12.1 106.6 � 12.9 107.8 � 12.2 114.9 � 17.6 117.1 � 15.9 111.8 � 20.0 t 40 � -1.48 p � 0.15 Group: t � -1.19, p � 0.24 Cerebral<br />
Vol: t � 4.14, p � 0.0002<br />
PFC white matter 50.0 � 8.2 51.5 � 8.0 47.9 � 8.9 61.0 � 13.2 67.1 � 10.8 53.0 � 12.1 t 40 � -2.86 p � 0.007 Group: t � -3.09, p � 0.004 Cerebral<br />
Vol: t � 5.99, p � 0.0001<br />
PFC CSF 8.3 � 4.1 8.1 � 3.6 8.6 � 4.9 5.0 � 2.0 4.6 � 2.2 5.6 � 1.4 t 1 � 2.83 p � 0.01 Group: t � 3.48, p � 0.001 Cerebral<br />
Vol: t � 0.25, p � 0.80<br />
<strong>Thalamus</strong> (total) 8.4 � 2.0 8.5 � 1.9 8.2 � 2.2 7.4 � 2.0 7.4 � 1.8 7.4 � 2.3 t 40 � 1.34 p � 0.19 Group: t � 1.38, p � 0.18 Cerebral<br />
Vol: t � 0.61, p � 0.54<br />
Right thalamus 4.2 � 1.0 4.2 � 1.1 4.1 � 1.1 3.7 � 1.0 3.7 � 0.9 3.8 � 1.2 t 40 � 1.28 p � 0.21 Group: t � 1.30, p � 0.20 Cerebral<br />
Vol: t � 0.46, p � 0.64<br />
Left thalamus 4.2 � 1.0 4.2 � 0.9 4.1 � 1.2 3.7 � 1.1 3.8 � 0.9 3.7 � 1.2 t 40 � 1.32 p � 0.20 Group: t � 1.37, p � 0.18 Cerebral<br />
Vol: t � 0.73, p � 0.47<br />
Pons/bra<strong>in</strong>stem 26.1 � 2.5 26.5 � 2.3 25.5 � 2.9 26.2 � 2.9 27.1 � 3.2 25.0 � 2.0 t 40 � -0.12 p � 0.90 Group: t � 0.10, p � 0.92 Cerebral<br />
Vol: t � 1.67, p � 0.1<br />
Cerebellum(total) 141.3 � 9.1 141.0 � 10.1 141.7 � 8.5 143.8 � 13.3 150.7 � 13.1 134.7 � 6.3 t 40 � -0.63 p � 0.53 Group: t � -0.26, p � 0.79 Cerebral<br />
Vol: t � 3.24, p � 0.002<br />
Right cerebellum 70.9 � 4.9 70.8 � 5.9 71.0 � 3.8 72.3 � 6.9 75.7 � 6.7 67.7 � 4.2 t 40 � -0.67 p � 0.51 Group: t � -0.33, p � 0.74 Cerebral<br />
Vol: t � 2.99, p � 0.005<br />
Left cerebellum 69.7 � 5.2 69.6 � 6.0 69.9 � 4.3 71.4 � 6.7 74.6 � 6.4 67.1 � 4.3 t 40 � -0.80 p � 0.43 Group: t � -0.47, p � 0.64 Cerebral<br />
Vol: t � 2.91, p � 0.006<br />
<strong>Cerebellar</strong> vermis 7.86 � 0.59 7.84 � 0.67 7.9 � 0.51 7.34 � 1.25 7.64 � 1.04 6.95 � 1.45 t 40 � 1.46 p � 0.15 Group: t � 1.65, p � 0.1 Cerebral<br />
(total)<br />
Vol: t � 1.43, p � 0.16<br />
CV, cerebral volume.<br />
significant differences when PFC volumes adjusted for cerebral<br />
volumes <strong>in</strong> AUD subjects with PTSD (mean, 163.2 �<br />
18.6 cm 3 ) <strong>and</strong> without PTSD (mean, 163.2 � 8.4 cm 3 )(t 1,12<br />
� -0.73, p � 0.48) or with conduct disorder (mean, 159.3 �<br />
12.5 cm 3 ) <strong>and</strong> without conduct disorder (mean, 163.2 �<br />
19.8 cm 3 )(t 1,12 � 0.45, p � 0.66) were compared with<strong>in</strong><br />
AUD groups.<br />
Right, left <strong>and</strong> total thalamic, pons/bra<strong>in</strong>stem, right <strong>and</strong><br />
left cerebellar hemispheres <strong>and</strong> total cerebellum <strong>and</strong> cerebellar<br />
vermis volumes did not differ between groups. See<br />
Table 3. There was a significant sex-by-group effect, <strong>in</strong>dicat<strong>in</strong>g<br />
that males with an adolescent-onset AUD compared<br />
with control males had smaller cerebellar volumes (male<br />
AUD mean: 141.8 � 8.5 cm 3; male control mean: 150.7 �<br />
13.1 cm 3 )(F � 4.16, df � 1,37, p � 0.05), whereas the two<br />
female groups were not different on this variable (female<br />
AUD mean: 141.0 � 10.1 cm 3; female control mean: 134.7<br />
� 6.3 cm 3 ). It should be noted six of the eight AUD males<br />
also had comorbid attention deficit hyperactivity disorder,<br />
comb<strong>in</strong>ed type, whereas only one adolescent female had<br />
this diagnosis. No other significant sex-by-group <strong>in</strong>teractions<br />
were seen.<br />
PFC variables adjusted for cerebral volume to correct for<br />
<strong>in</strong>dividual differences <strong>in</strong> bra<strong>in</strong> size with regard to gender<br />
were correlated with six alcohol consumption variables (age<br />
of onset of AUD, duration of an AUD, average number of<br />
dr<strong>in</strong>k per dr<strong>in</strong>k<strong>in</strong>g episode, most number of dr<strong>in</strong>ks per<br />
maximum dr<strong>in</strong>k<strong>in</strong>g episode, quantity/frequency group<strong>in</strong>g,<br />
<strong>and</strong> lifetime number of dr<strong>in</strong>ks), us<strong>in</strong>g Spearman correlation<br />
coefficients. The average number of dr<strong>in</strong>ks per dr<strong>in</strong>k<strong>in</strong>g<br />
episode significantly correlated with the PFC gray matter<br />
volume (r s � -0.6, df � 12, p � 0.03). The number of dr<strong>in</strong>ks<br />
per maximum dr<strong>in</strong>k<strong>in</strong>g episode significantly correlated with<br />
the PFC volume (r s � -0.57, df � 12, p � 0.03) <strong>and</strong> PFC<br />
gray mater volume (r s � -0.78, df � 12, p � 0.0009). See<br />
Fig. 4. Quantity/frequency group<strong>in</strong>g negatively correlated<br />
with the PFC gray matter volume (r s � -0.71, df � 12, p �<br />
0.005). No significant relationships were seen between<br />
PFC, PFC gray, or prefrontal white matter measures with<br />
age of onset of an AUD or duration of an AUD. No<br />
significant relationships were seen between PFC gray or<br />
white matter measures with age of onset or duration of<br />
cannabis use disorder. Fig. 3<br />
DISCUSSION<br />
Adolescents <strong>and</strong> young adults with adolescent-onset<br />
AUD <strong>and</strong> comorbid mental disorders were found to have<br />
significantly smaller PFC <strong>and</strong> PFC white matter volumes<br />
<strong>and</strong> greater amounts of PFC CSF compared with healthy<br />
comparison subjects. The f<strong>in</strong>d<strong>in</strong>gs of greater PFC CSF<br />
persisted when controll<strong>in</strong>g for comorbidity. PFC volume<br />
variables significantly <strong>and</strong> negatively correlated with the<br />
most number of dr<strong>in</strong>ks per maximum dr<strong>in</strong>k<strong>in</strong>g episode.<br />
Right, left, <strong>and</strong> total thalamic, pons/bra<strong>in</strong>stem, right <strong>and</strong><br />
left cerebellar hemispheres, <strong>and</strong> total cerebellum <strong>and</strong> cer-
1596 DE BELLIS ET AL.<br />
Fig. 3. PFC volumes (cm 3 ) adjusted for cerebral volume of adolescents <strong>and</strong><br />
young adults with an adolescent-onset AUD <strong>and</strong> comparison subjects. Female<br />
subjects are shown <strong>in</strong> circles. Male subjects are shown <strong>in</strong> squares. Subjects <strong>in</strong><br />
blue <strong>in</strong>dicate history of major depression; open circles or squares <strong>in</strong>dicate history<br />
of ADHD.<br />
Fig. 4. Correlation between PFC gray matter volume (cm 3 ) adjusted for cerebral<br />
volume of adolescents <strong>and</strong> young adults with an adolescent-onset AUD with<br />
the most number of dr<strong>in</strong>ks per maximum dr<strong>in</strong>k<strong>in</strong>g episode (r s � -0.78, df � 12,<br />
p � 0.0009). Female subjects are shown <strong>in</strong> circles. Male subjects are shown <strong>in</strong><br />
squares. Subjects <strong>in</strong> blue <strong>in</strong>dicate history of major depression; open circles or<br />
squares <strong>in</strong>dicate history of ADHD.<br />
ebellar vermis volumes did not differ between groups.<br />
There was a significant sex-by-group effect for males with<br />
an adolescent-onset AUD to have smaller cerebellar volumes<br />
than control males. To our knowledge, this is the first<br />
study to exam<strong>in</strong>e the association of an adolescent-onset<br />
AUD on the prefrontal, thalamic, <strong>and</strong> cerebellar morphology<br />
of adolescents <strong>and</strong> young adults.<br />
There are several possible explanations for the smaller<br />
PFC volumes <strong>and</strong> PFC white matter volumes found <strong>in</strong><br />
adolescents <strong>and</strong> young adults with adolescent-onset AUD.<br />
S<strong>in</strong>ce the PFC is matur<strong>in</strong>g dur<strong>in</strong>g adolescence, PFC maturation<br />
may be impeded by the neurotoxic effects of alcohol,<br />
despite the significantly different dr<strong>in</strong>k<strong>in</strong>g patterns seen <strong>in</strong><br />
adolescents, who tend to b<strong>in</strong>ge dr<strong>in</strong>k relative to adults, who<br />
are more likely to dr<strong>in</strong>k daily. Alcohol affects N-methyl-D-<br />
aspartate (NMDA) receptors, a subclass of glutamate receptors<br />
<strong>in</strong> the PFC that are matur<strong>in</strong>g dur<strong>in</strong>g adolescence<br />
(Breese et al., 1995; Lov<strong>in</strong>ger, 1993). Alcohol withdrawal<br />
leads to <strong>in</strong>creased excitatory transmission through its effects<br />
on NMDA receptors. This process can result <strong>in</strong> discrete<br />
excitotoxic neuronal damage or a more severe <strong>and</strong><br />
complicated alcohol withdrawal syndrome <strong>in</strong>clud<strong>in</strong>g withdrawal<br />
seizures (Becker, 1999). B<strong>in</strong>g<strong>in</strong>g, or chronic <strong>in</strong>termittent<br />
alcohol exposure, may be more neurotoxic to adolescent<br />
neurons secondary to many brief episodes of<br />
withdrawal (Lundqvist et al., 1995; Lundqvist et al., 1994).<br />
However, only two of our AUD subjects had symptoms of<br />
withdrawal. Adolescence is a period of active myel<strong>in</strong>ation<br />
<strong>in</strong> PFC regions (Paus et al., 2001). Alcoholism is also<br />
associated with white matter loss (Hard<strong>in</strong>g et al., 1997).<br />
Although the f<strong>in</strong>d<strong>in</strong>gs of smaller PFC volumes did not<br />
correlate with age of onset or duration of an AUD, significant<br />
negative correlations were seen between PFC <strong>and</strong><br />
PFC gray matter volume measures with alcohol consumption<br />
variables. Thus, we may speculate that the smaller PFC<br />
volumes may be a result of the adverse effects of an AUD<br />
on the adolescent PFC either through a direct or <strong>in</strong>direct<br />
(via withdrawal) toxic effects on adolescent PFC development.<br />
Another explanation for the smaller PFC <strong>and</strong> PFC<br />
white matter volumes may be that PFC maturation is<br />
impeded by the neurotoxic effects of other illicit substances<br />
on the adolescent bra<strong>in</strong>. Eleven of the 14 subjects<br />
<strong>in</strong> this study also had cannabis abuse or dependence. The<br />
active component of the marijuana plant, cannabis sativa, is<br />
9-tetrahydrocannab<strong>in</strong>ol, which affects growth factor gene<br />
expression <strong>in</strong> the adult rat forebra<strong>in</strong> (Mailleux et al., 1994).<br />
Precl<strong>in</strong>ical data suggest that cannab<strong>in</strong>oids modulate the<br />
release of neurotransmitters (i.e., L-glutamate, GABA, noradrenal<strong>in</strong>e,<br />
dopam<strong>in</strong>e, seroton<strong>in</strong>, <strong>and</strong> acetylchol<strong>in</strong>e) from<br />
axon term<strong>in</strong>als (Iversen, 2003). Although GABA functions<br />
primarily as an <strong>in</strong>hibitory neurotransmitter, it can also act<br />
as a trophic factor dur<strong>in</strong>g nervous system development to<br />
<strong>in</strong>fluence events such as proliferation, migration, differentiation,<br />
synapse maturation, <strong>and</strong> cell death (Owens <strong>and</strong><br />
Kriegste<strong>in</strong>, 2002). Thus, cannabis use disorder through its<br />
effects on GABA <strong>and</strong> other neurotransmitters may negatively<br />
<strong>in</strong>fluence adolescent bra<strong>in</strong> development. Although<br />
multivariate regression analysis exam<strong>in</strong><strong>in</strong>g the results controll<strong>in</strong>g<br />
for the presence of a cannabis use disorder as well<br />
as comorbidity also suggested smaller PFC <strong>and</strong> smaller<br />
PFC gray <strong>and</strong> white matter volumes <strong>in</strong> the AUD subjects<br />
compared with control subjects, because no adolescentonset<br />
AUD subject had an alcohol use disorder only, it is<br />
not impossible to conclude that an adolescent-onset AUD<br />
is toxic to PFC maturation.<br />
A third explanation for the smaller PFC <strong>and</strong> PFC white<br />
matter volumes of adolescents <strong>and</strong> young adults with an<br />
adolescent-onset AUD is an <strong>in</strong>herent vulnerability for delayed<br />
PFC maturation that enhances the risk for poorer<br />
executive cognitive function<strong>in</strong>g <strong>and</strong> adolescent substance
BRAIN VOLUMES IN YOUTHS 1597<br />
use disorders. Impulsivity is thought to be closely associated<br />
with PFC development dur<strong>in</strong>g adolescence (Spear, 2000).<br />
Increased impulsivity, which may contribute to early-onset<br />
dr<strong>in</strong>k<strong>in</strong>g, is seen <strong>in</strong> subjects with frontal lobe excisions<br />
(Miller, 1992). Alcoholism has been conceptualized as a<br />
frontal lobe condition (Moselhy et al., 2001). Neuroimag<strong>in</strong>g<br />
studies across modalities have demonstrated the PFC to be<br />
<strong>in</strong>volved <strong>in</strong> <strong>in</strong>toxication, crav<strong>in</strong>g, <strong>and</strong> withdrawal with respect<br />
to alcohol <strong>and</strong> other drugs (Goldste<strong>in</strong> <strong>and</strong> Volkow,<br />
2002). In a review of the literature on impulsivity <strong>and</strong><br />
addiction <strong>in</strong> adolescence, Chambers et al. (2003) concluded<br />
that substance use disorders constitute neurodevelopmental<br />
disorders <strong>and</strong> suggested that the common neurobiological<br />
mechanisms <strong>in</strong>volv<strong>in</strong>g PFC motivational bra<strong>in</strong> circuitry<br />
could be substrates for both normative impulsivity <strong>and</strong><br />
addictive behavior among adolescents. In our study, PFC<br />
volume variables adjusted for cerebral volumes significantly<br />
correlated with the most number of dr<strong>in</strong>ks per maximum<br />
dr<strong>in</strong>k<strong>in</strong>g episode, a measure of dis<strong>in</strong>hibition <strong>and</strong> impulsivity.<br />
High-risk studies with subjects with family histories of<br />
substance use disorders support this idea. Young subjects,<br />
who are offspr<strong>in</strong>g of fathers with alcoholism <strong>and</strong> are at high<br />
familial risk for AUD perform poorly on measures of executive<br />
cognitive function (Giancola et al., 1996; Harden<br />
<strong>and</strong> Pihl, 1995; Hill, 2004). Individuals at high relative risk<br />
for substance use disorders demonstrated impulsive problems<br />
<strong>in</strong>clud<strong>in</strong>g conduct disorders (Clark et al., 1998), antisocial<br />
behaviors (Clark et al., 1999), <strong>and</strong> neurobehavioral<br />
dis<strong>in</strong>hibition (Tarter et al., 2003) <strong>in</strong> late childhood. Deficits<br />
<strong>in</strong> PFC-mediated executive functions of decision-mak<strong>in</strong>g,<br />
susta<strong>in</strong>ed attention, verbal fluency abstraction, behavioral<br />
<strong>in</strong>hibition, work<strong>in</strong>g memory, regulation of motivation, <strong>and</strong><br />
motor control are seen <strong>in</strong> ADHD (Barkley, 1997; Ernst et<br />
al., 2003; P<strong>in</strong>eda et al., 1998), conduct disorder (Dery et al.,<br />
1999; Morgan <strong>and</strong> Lilienfeld, 2000), major depression<br />
(Rogers et al., 2004), <strong>and</strong> posttraumatic stress disorder<br />
(Beers <strong>and</strong> De Bellis, 2002), the most common comorbid<br />
disorders <strong>in</strong> our AUD subjects. Imag<strong>in</strong>g studies also suggest<br />
PFC abnormalities <strong>in</strong> all these heterogeneous mental<br />
disorders (De Bellis et al., 2000b; Nolan et al., 2002; Schulz<br />
et al., 2004; Sowell et al., 2003b; Spalletta et al., 2001).<br />
Similar results have been atta<strong>in</strong>ed <strong>in</strong> community adolescents,<br />
where neurocognitive deficits <strong>in</strong> measures of attention<br />
ability predicted substance use disorders 8 years later<br />
(Tapert et al., 2002a). Thus, these childhood psychopathologies<br />
may lead to early substance use disorders <strong>and</strong><br />
substance-related problems <strong>in</strong> adolescence, due to preexist<strong>in</strong>g<br />
PFC vulnerability. Thus, unlike our previous f<strong>in</strong>d<strong>in</strong>gs<br />
<strong>in</strong> this sample, where we reported that the adolescent<br />
hippocampus may be more vulnerable to the toxic effects of<br />
an adolescent-onset AUD than an adult with similar years<br />
of dr<strong>in</strong>k<strong>in</strong>g (De Bellis et al., 2000a) because hippocampal<br />
volumes correlated positively with the age of onset <strong>and</strong><br />
negatively with the duration of an AUD, the f<strong>in</strong>d<strong>in</strong>gs of<br />
smaller PFC did not correlate with age of onset or duration<br />
of an AUD. This leads to the speculation that delayed PFC<br />
maturation (less myel<strong>in</strong>ation of the PFC) may be an <strong>in</strong>herent<br />
vulnerability that enhances the risk for poorer executive<br />
cognitive function<strong>in</strong>g <strong>and</strong> an adolescent-onset AUD.<br />
In this particular study, the negative overall cerebellum<br />
f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> adolescents with an AUD are <strong>in</strong> contrast with<br />
adult f<strong>in</strong>d<strong>in</strong>gs (Parks et al., 2002). This may be because of<br />
a longer period of exposure to alcohol consumption is<br />
required to cause alterations <strong>in</strong> the cerebellum or because<br />
of adolescent cerebellar plasticity (Hansel et al., 2001).<br />
However, we note that there was a significant sex-by-group<br />
effect for males with an adolescent-onset AUD to have<br />
smaller cerebellar volumes than control males. It should be<br />
noted that six of the eight AUD males also had comorbid<br />
ADHD, comb<strong>in</strong>ed type. Alteration <strong>in</strong> the frontal-striatal<br />
circuitry underlies the psychopathology of ADHD <strong>and</strong><br />
probably causes the related deficits of higher cognitive<br />
functions <strong>in</strong> these <strong>in</strong>dividuals (Berqu<strong>in</strong> et al., 1998; Castellanos<br />
et al., 1996). ADHD boys have a smaller cerebellar<br />
vermis compared with healthy control boys (Berqu<strong>in</strong> et al.,<br />
1998; Castellanos et al., 1996), <strong>and</strong> <strong>in</strong> most studies, the<br />
difference is limited to the <strong>in</strong>ferior posterior vermis of the<br />
cerebellum (Castellanos et al., 1996; Mostofsky et al.,<br />
1998). The difference <strong>in</strong> cerebellar volume <strong>in</strong> boys with<br />
ADHD has been replicated <strong>in</strong> girls with similar symptom<br />
severity (Castellanos et al., 2001). A longitud<strong>in</strong>al study<br />
found that both smaller cerebral <strong>and</strong> cerebellar volumes <strong>in</strong><br />
subjects with ADHD persisted over time <strong>and</strong> were unrelated<br />
to stimulant treatment (Castellanos et al., 2002).<br />
Overall, recent studies suggest a possible modulat<strong>in</strong>g cerebellar<br />
<strong>in</strong>fluence on the predom<strong>in</strong>antly right frontal-striatal<br />
circuits <strong>in</strong>volved <strong>in</strong> ADHD (Giedd et al., 2001). S<strong>in</strong>ce<br />
premorbid ADHD is a risk factor for substance use disorders<br />
<strong>in</strong> adolescent <strong>and</strong> young adults (Biederman et al.,<br />
1997; Clark et al., 1999), any possible relation between<br />
AUD <strong>and</strong> other comorbid conditions should be considered<br />
when evaluat<strong>in</strong>g structural MRI f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> <strong>in</strong>dividuals with<br />
AUD. Our study is limited by the fact that our adolescent<br />
AUD group had extensive comorbidity with other Axis I<br />
disorders. It should be noted that it is rare for an adolescent<br />
with alcohol abuse or dependence not to have another<br />
mental disorder (Clark et al., 1997). Imag<strong>in</strong>g studies of<br />
adult <strong>and</strong> adolescent AUD are only beg<strong>in</strong>n<strong>in</strong>g to address<br />
the issues of comorbidity by exam<strong>in</strong><strong>in</strong>g adults with early<br />
<strong>and</strong> late onset alcohol dependence. However, studies of<br />
very large samples are needed to exam<strong>in</strong>e these issues.<br />
Given that most MRI studies of adults with an AUD do not<br />
exam<strong>in</strong>e histories of childhood-onset mental disorders<br />
(ADHD, major depression) <strong>in</strong> their samples, this is an<br />
important <strong>and</strong> overlooked research issue that may have<br />
<strong>in</strong>fluenced the known bra<strong>in</strong> structural f<strong>in</strong>d<strong>in</strong>gs <strong>in</strong> the adult<br />
AUD literature.<br />
In summary, unlike <strong>in</strong> the mature bra<strong>in</strong>, <strong>in</strong> which chronic<br />
AUD is characterized by a cont<strong>in</strong>uum of graded bra<strong>in</strong><br />
dysmorphology, our prelim<strong>in</strong>ary f<strong>in</strong>d<strong>in</strong>gs suggest that structural<br />
deficits <strong>in</strong> the adolescent PFC are associated with an<br />
adolescent-onset AUD <strong>in</strong> <strong>in</strong>dividuals with comorbid mental
1598 DE BELLIS ET AL.<br />
disorders. We speculate that smaller PFC may represent a<br />
vulnerability to, or a consequence of, early-onset dr<strong>in</strong>k<strong>in</strong>g<br />
<strong>in</strong> these vulnerable <strong>in</strong>dividuals. However, given that our<br />
sample lacked an AUD group without comorbidity, we<br />
cannot conclude that a smaller PFC is a causal factor for an<br />
adolescent-onset AUD. Further studies are warranted to<br />
exam<strong>in</strong>e if a smaller PFC represents a vulnerability to or a<br />
consequence of early-onset dr<strong>in</strong>k<strong>in</strong>g. Future MRI studies<br />
of <strong>in</strong>dividuals with an adolescent-onset AUD that control<br />
for comorbidity <strong>and</strong> <strong>in</strong> <strong>in</strong>dividuals at high familial risk for<br />
AUD are warranted.<br />
ACKNOWLEDGMENTS<br />
The authors thank Grace Moritz, M.S.W., Cara Renzelli,<br />
M.S.Ed., Julie Hall, B.A., <strong>and</strong> the staff of the University of<br />
Pittsburgh Medical Center’s General Cl<strong>in</strong>ical Research Center<br />
Staff for their assistance <strong>in</strong> this work.<br />
REFERENCES<br />
Baker KG, Hard<strong>in</strong>g AJ, Halliday GM, Kril JJ, Harper CG (1999) Neuronal<br />
loss <strong>in</strong> functional zones of the cerebellum of chronic alcoholics with<br />
<strong>and</strong> without Wernicke’s encephalopathy. Neuroscience 91:429–438.<br />
BarkleyRA (1997) Behavioral <strong>in</strong>hibition, susta<strong>in</strong>ed attention, <strong>and</strong> executive<br />
functions: construct<strong>in</strong>g a unify<strong>in</strong>g theory of ADHD. Psychol Bull<br />
121:65–94.<br />
Becker HC (1999) Alcohol withdrawal: neuroadaptation <strong>and</strong> sensitization.<br />
CNS Spectrums 4:38–65.<br />
Beers SR, De Bellis MD (2002) Neuropsychological function <strong>in</strong> children<br />
with maltreatment-related posttraumatic stress disorder. Am J Psychiatry<br />
159:483–486.<br />
Berqu<strong>in</strong> PC, Giedd JN, Jacobsen LK, Hamburger SD, Kra<strong>in</strong> AL, Rapoport<br />
JL, et al (1998) Cerebellum <strong>in</strong> attention-deficit hyperactivity<br />
disorder: a morphometric MRI study. Neurology 50:1087–1093.<br />
Biederman J, Wilens T, Mick E, Farone S, Weber W, Curtis S, et al (1997)<br />
Is ADHD a risk factor for psychoactive substance use disorders? F<strong>in</strong>d<strong>in</strong>gs<br />
from a four year prospective follow-up study. J Am Acad Child<br />
Adolesc Psychiatry 36:21–29.<br />
Breese CR, Freedman R, Leonard SS (1995) Glutamate receptor subtype<br />
expression <strong>in</strong> human postmortem bra<strong>in</strong> tissue from schizophrenics <strong>and</strong><br />
alcohol abusers. Bra<strong>in</strong> Res 674:82–90.<br />
Brown S, Tapert SF, Granholm E, Delis D (2000) Neurocognitive function<strong>in</strong>g<br />
of adolescents: Effects of protracted alcohol use. Alcohol Cl<strong>in</strong><br />
Exp Res 24:164–171.<br />
Cahalan D (1981) Quantify<strong>in</strong>g alcohol consumption: Patterns <strong>and</strong> problems.<br />
Circulation 64:7–14.<br />
Castellanos FX, Giedd JN, Berqu<strong>in</strong> PC, Walter JM, Sharp W, Tran T, et<br />
al (2001) Quantitative bra<strong>in</strong> magnetic resonance imag<strong>in</strong>g <strong>in</strong> girls with<br />
attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 58:289–<br />
295.<br />
Castellanos FX, Giedd JN, Marsh WL, Hamburger SD, Vaituzis AC,<br />
Dickste<strong>in</strong> DP, et al (1996) Quantitative bra<strong>in</strong> magnetic resonance imag<strong>in</strong>g<br />
<strong>in</strong> attention-deficit hyperactivity disorder. Arch Gen Psychiatry<br />
53:607–616.<br />
Castellanos FX, Lee PP, Sharp W, Jeffries NO, Greenste<strong>in</strong> DK, Clasen<br />
LS, et al (2002) Developmental trajectories of bra<strong>in</strong> volume abnormalities<br />
<strong>in</strong> children <strong>and</strong> adolescents with attention-deficit/hyperactivity disorder.<br />
JAMA 288:1740–1748.<br />
Chambers RA, Taylor JR, Potenza MN (2003) Developmental neurocircuitry<br />
of motivation <strong>in</strong> adolescence: a critical period of addiction vulnerability.<br />
Am J Psychiatry 160:1041–1052.<br />
Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambros<strong>in</strong>i PJ, Tabrizi<br />
MA, et al (1985) The assessment of affective disorders <strong>in</strong> children <strong>and</strong><br />
adolescents by semi-structured <strong>in</strong>terview: Test-retest reliability of the<br />
schedule for affective disorders <strong>and</strong> schizophrenia for school-age children,<br />
present episode version. Arch Gen Psychiatry 42:696–702.<br />
ClarkDB (1999) Psychiatric Assessment. In Sourcebook on Substance<br />
Abuse: Etiology, Epidemiology, Assessment, <strong>and</strong> Treatment (Ott PJ,<br />
Tarter RE, Ammerman RT, eds), pp 197–211. Allyn & Bacon, Needham<br />
Heights, MA.<br />
Clark DB (2004) The natural history of adolescent alcohol use disorders.<br />
Addiction 99:5–22.<br />
Clark DB, Kirisci L, Moss HB (1998) Early adolescent gateway drug use<br />
<strong>in</strong> sons of fathers with substance use disorders. Addict Behav 23:561–<br />
566.<br />
Clark DB, Parker AM, Lynch KG (1999) Psychopathology <strong>and</strong> substancerelated<br />
problems dur<strong>in</strong>g early adolescence: A survival analysis. J Cl<strong>in</strong><br />
Child Psychol 28:333–341.<br />
Clark DB, Pollock N, Bukste<strong>in</strong> OG, Mezzich AC, Bromberger JT, Donovan<br />
JE (1997) Gender <strong>and</strong> comorbid psychopathology <strong>in</strong> adolescents<br />
with alcohol dependence. J Am Acad Child Adolesc Psychiatry 36:1195–<br />
1203.<br />
Clark DB, Pollock NK, Mezzich A, Cornelius J, Mart<strong>in</strong> C (2001) Diachronic<br />
assessment <strong>and</strong> the emergence of substance use disorders. J Child<br />
Adolesc Substance Abuse 10:13–22.<br />
De Bellis MD, Clark DB, Beers SR, Soloff P, Bor<strong>in</strong>g AM, Hall J, et al<br />
(2000a) Hippocampal volume <strong>in</strong> adolescent onset alcohol use disorders.<br />
Am J Psychiatry 157:737–744.<br />
De Bellis MD, Keshavan M, Clark DB, Casey BJ, Giedd J, Bor<strong>in</strong>g AM, et<br />
al (1999) A.E. Bennett Research Award: Developmental Traumatology,<br />
II: Bra<strong>in</strong> development. Biol Psychiatry 45:1271–1284.<br />
De Bellis MD, Keshavan M, Shifflett H, Iyengar S, Dahl R, Axelson DA,<br />
et al (2002) Superior temporal gyrus volumes <strong>in</strong> pediatric generalized<br />
anxiety disorder. Biol Psychiatry 51:553–562.<br />
De Bellis MD, Keshavan MS, Beers SR, Hall J, Frustaci K, Masalehdan A,<br />
et al (2001) Sex differences <strong>in</strong> bra<strong>in</strong> maturation dur<strong>in</strong>g childhood <strong>and</strong><br />
adolescence. Cereb <strong>Cortex</strong> 11:552–557.<br />
De Bellis MD, Keshavan MS, Spencer S, Hall J (2000b) N-acetylaspartate<br />
concentration <strong>in</strong> the anterior c<strong>in</strong>gulate <strong>in</strong> maltreated children <strong>and</strong><br />
adolescents with PTSD. Am J Psychiatry 157:1175–1177.<br />
Dery M, Toup<strong>in</strong> J, Pauze R, Mercier H, Fort<strong>in</strong> L (1999) Neuropsychological<br />
characteristics of adolescents with conduct disorder: Association<br />
with attention-deficit-hyperactivity <strong>and</strong> aggression. J Abnorm Child<br />
Psychol 27:225–236.<br />
Durston S, Hulshoff Pol, HE Casey BJ, Giedd JN, Buitelaar JK, van<br />
Engel<strong>and</strong> H (2001) Anatomical MRI of the develop<strong>in</strong>g human bra<strong>in</strong>:<br />
what have we learned? J Am Acad Child Adolesc Psychiatry 40:1012–<br />
1020.<br />
Ernst M, Kimes AS, London ED, Matochik JA, Eldreth D, Tata S, et al<br />
(2003) Neural substrates of decision mak<strong>in</strong>g <strong>in</strong> adults with attention<br />
deficit hyperactivity disorder. Am J Psychiatry 160:1061–1070.<br />
Giancola P, Moss HB, Mart<strong>in</strong> C, Kirisci L, Tarter RE (1996) Executive<br />
cognitive function<strong>in</strong>g predicts reactive aggression <strong>in</strong> boys at high risk for<br />
substance abuse: A prospective study. Alcohol Cl<strong>in</strong> Exp Res 20:740–<br />
744.<br />
Giedd JN, Blumenthal J, Jeffries NO, Castellanos X, Liu H, Zijdenbos A,<br />
et al (1999) Bra<strong>in</strong> development dur<strong>in</strong>g childhood <strong>and</strong> adolescence: a<br />
longitud<strong>in</strong>al MRI study. Nat Neurosci 2:861–863.<br />
Giedd JN, Blumenthal J, Molloy E, Castellanos FX (2001) Bra<strong>in</strong> imag<strong>in</strong>g<br />
of attention deficit/hyperactivity disorder. Ann N Y Acad Sci 931:33–49.<br />
Gilbert AR, Moore GJ, Keshavan MS, Paulson LA, Narula V, Mac<br />
Master FP, et al (2000) Decrease <strong>in</strong> thalamic volumes of pediatric<br />
patients with obsessive-compulsive disorder who are tak<strong>in</strong>g paroxet<strong>in</strong>e.<br />
Arch Gen Psychiatry 57:449–456.<br />
Gilman S, Adams K, Koeppe RA, Berent S, Klu<strong>in</strong> KJ, Modell JG, et al<br />
(1990) <strong>Cerebellar</strong> <strong>and</strong> frontal hypometabolism <strong>in</strong> alcoholic cerebellar<br />
degeneration studied with positron emission tomography. Ann Neurol<br />
28:775–785.<br />
Goldste<strong>in</strong> RZ, Volkow ND (2002) Drug addiction <strong>and</strong> its underly<strong>in</strong>g<br />
neurobiological basis: neuroimag<strong>in</strong>g evidence for the <strong>in</strong>volvement of the<br />
frontal cortex. Am J Psychiatry 159:1642–1652.
BRAIN VOLUMES IN YOUTHS 1599<br />
Grant B, Harford T, Dawson D, Chou P, Picker<strong>in</strong>g R (1995) The Alcohol<br />
Use Disorder <strong>and</strong> Associated Disabilities Interview Schedule (AUDA-<br />
DIS): Reliability of alcohol <strong>and</strong> drug modules <strong>in</strong> a general population<br />
sample. Drug Alcohol Depend 39:37–44.<br />
Hansel C, L<strong>in</strong>den DJ, D’Angelo E (2001) Beyond parallel fiber LTD: The<br />
diversity of synaptic <strong>and</strong> non-synaptic plasticity <strong>in</strong> the cerebellum. Nat<br />
Neurosci 4:467–475.<br />
Hardan AY, M<strong>in</strong>shew NJ, Harenski K, Keshavan M (2001) Posterior fossa<br />
magnetic resonance imag<strong>in</strong>g <strong>in</strong> autism. J Am Acad Child Adolesc<br />
Psychiatry 40:666–672.<br />
Harden PW, Pihl RO (1995) Cognitive function, cardiovascular reactivity<br />
<strong>and</strong> behavior <strong>in</strong> boys at high risk for alcoholism. J Abnorm Psychol<br />
104:94–103.<br />
Hard<strong>in</strong>g A, Wong A, Svoboda M, Kril JJ, Halliday GM (1997) Chronic<br />
alcohol consumption does not cause hippocampal neuron loss <strong>in</strong> humans.<br />
Hippocampus 7:78–87.<br />
Harper C, Kril J, Daly J (1987) Are we dr<strong>in</strong>k<strong>in</strong>g our neurons away? Br<br />
Med J 294:534–536.<br />
Harper CG, Smith NA, Kril JJ (1990) The effects of alcohol on the female<br />
bra<strong>in</strong>: a neuropathological study. Alcohol Cl<strong>in</strong> Exp Res 25:445–448.<br />
Has<strong>in</strong> D, Carpenter KM (1998) Difficulties with questions on usual dr<strong>in</strong>k<strong>in</strong>g<br />
<strong>and</strong> the measurement of alcohol consumption. Alcohol Cl<strong>in</strong> Exp<br />
Res 22:580–584.<br />
Hill SY (2004) Trajectories of alcohol use <strong>and</strong> electrophysiological <strong>and</strong><br />
morphological <strong>in</strong>dices of bra<strong>in</strong> development: dist<strong>in</strong>guish<strong>in</strong>g causes from<br />
consequences. Ann N Y Acad Sci. 1021:245–259.<br />
Hommer D, Momenan R, Rawl<strong>in</strong>gs R, et al (1996) Decreased corpus<br />
callosum size among alcoholic women. Arch Neurol 53:359–363.<br />
Hommer DW (2003) Male <strong>and</strong> female sensitivity to alcohol-<strong>in</strong>duced bra<strong>in</strong><br />
damage. Alcohol Res Health J Natl Inst Alcohol Abuse Alcohol 27:<br />
181–185.<br />
Iversen L (2003) Cannabis <strong>and</strong> the bra<strong>in</strong>. Bra<strong>in</strong> 126:1252–1270.<br />
JohnstonLD,O’MalleyPM,BachmanJG (2003) The Monitor<strong>in</strong>g the Future<br />
National Survey Results on Adolescent Drug Use: Overview of Key F<strong>in</strong>d<strong>in</strong>gs<br />
2002. National Institute on Drug Abuse: Bethesda MD.<br />
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al (1997)<br />
Schedule for affective Disorders <strong>and</strong> Schizophrenia for school-age<br />
children-present <strong>and</strong> lifetime version (K-SADS-PL): Initial reliability<br />
<strong>and</strong> validity data. J Am Acad Child Adolesc Psychiatry 36:980–988.<br />
Keshavan MS, Anderson S, Beckwith C, Nash K, Pettegrew J, Krishnan<br />
KRR (1995) A comparison of stereology <strong>and</strong> segmentation techniques<br />
for volumetric measurements of bra<strong>in</strong> ventricles. Psychiatry Res Neuroimag<strong>in</strong>g<br />
61:53–60.<br />
Kosten TA, Anton SF, Rounsaville BJ (1992) Ascerta<strong>in</strong><strong>in</strong>g psychiatric<br />
diagnoses with the family history method <strong>in</strong> a substance abuse population.<br />
Psych Res 26:135–147.<br />
Kosten TA, Rounsaville BJ (1992) Sensitivity of psychiatric diagnosis<br />
based on the best estimate procedure. Am J Psychiatry 149:1225–1227.<br />
Lange N, Giedd JN, Castellanos FX, Vaituzis AC, Rapoport JL (1997)<br />
Variability of human bra<strong>in</strong> structure size: ages 4-20 years. Psychiatry<br />
Res Neuroimag<strong>in</strong>g Sect 74:1–12.<br />
Liu X, Matochik JA, Cadet JL, London ED (1998) Smaller volume of<br />
prefrontal lobe <strong>in</strong> polysubstance abusers: a magnetic resonance imag<strong>in</strong>g<br />
study. Neuropsychopharmacology 18:243–252.<br />
Lov<strong>in</strong>ger DM (1993) Excitotoxicity <strong>and</strong> alcohol-related bra<strong>in</strong> damage.<br />
Alcohol Cl<strong>in</strong> Exp Res 17:19–27.<br />
Lundqvist C, All<strong>in</strong>g C, Knoth R, Volk B (1995) Intermittent ethanol<br />
exposure of adult rats: hippocampal cell loss after one month of treatment.<br />
Alcohol Cl<strong>in</strong> Exp Res 30:737–748.<br />
Lundqvist C, Volk B, Knoth R, All<strong>in</strong>g C (1994) Long-term effects of<br />
<strong>in</strong>termittent versus cont<strong>in</strong>uous ethanol exposure on hippocampal synapses<br />
of the rat. Acta Neuropathol 87:242–249.<br />
Mailleux P, Preud’homme X, Albala N, V<strong>and</strong>erw<strong>in</strong>den JM, V<strong>and</strong>erhaeghen<br />
JJ (1994) Delta-9-Tetrahydrocannab<strong>in</strong>ol regulates gene expression<br />
of the growth factor pleiotroph<strong>in</strong> <strong>in</strong> the forebra<strong>in</strong>. Neurosci Lett 175:<br />
25–27.<br />
Mann K, Batra A, Gunthner A, Schroth G (1992) Do women develop<br />
alcoholic bra<strong>in</strong> damage more readily than men? Alcohol Cl<strong>in</strong> Exp Res<br />
16:1052–1056.<br />
Mart<strong>in</strong> CS, Pollock NK, Bukste<strong>in</strong> OG, Lynch KG (2000) Inter-rater<br />
reliability of the SCID alcohol <strong>and</strong> substance use disorders section<br />
among adolescents. Drug Alcohol Depend 54:173–176.<br />
Miller EK, Cohen JD (2001) An <strong>in</strong>tegrative theory of prefrontal function.<br />
Ann Rev Neurosci 24:167–202.<br />
Miller LA (1992) Impulsivity, risk-tak<strong>in</strong>g, <strong>and</strong> the ability to synthesize<br />
fragmented <strong>in</strong>formation after frontal lobectomy. Neuropsychologia 30:<br />
69–72.<br />
Morgan AB, Lilienfeld SO (2000) A meta-analytic review of the relation<br />
between antisocial behavior <strong>and</strong> neuropsychological measures of executive<br />
function. Cl<strong>in</strong> Psychol Rev 20:113–136.<br />
Moselhy HF, Georgiou G, Kahn A (2001) Frontal lobe changes <strong>in</strong> alcoholism:<br />
a review of the literature. Alcohol Alcohol 36:357–368.<br />
Moss HB, Kirisci L, Gordon HW, Tarter RE (1994) A neuropsychological<br />
profile of adolescent alcoholics. Alcohol Cl<strong>in</strong> Exp Res 18:159–163.<br />
Mostofsky SH, Cooper KL, Kates WR, Denckla MB, Kaufmann WE<br />
(2002) Smaller prefrontal <strong>and</strong> premotor volumes <strong>in</strong> boys with attentiondeficit/hyperactivity<br />
disorder. Biol Psychiatry 52:785–794.<br />
Mostofsky SH, Reiss AL, Lockhart P, Denckla MB (1998) Evaluation of<br />
cerebellar size <strong>in</strong> attention-deficit hyperactivity disorder. J Child Neurol<br />
13:434–439.<br />
Nicolas JM, Fern<strong>and</strong>ez-Sola J, Antunez E, Cofan M, Cardenal C,<br />
Sacanella E, Estruch R, Urbano-Marquez A (2000) High ethanol <strong>in</strong>take<br />
<strong>and</strong> malnutrition <strong>in</strong> alcoholic cerebellar shr<strong>in</strong>kage. QJM 93:449–456.<br />
Nolan CL, Moore GJ, Madden R, Farchione T, Bartoi M, Lorch E, et al<br />
(2002) <strong>Prefrontal</strong> cortical volume <strong>in</strong> childhood-onset major depression:<br />
prelim<strong>in</strong>ary f<strong>in</strong>d<strong>in</strong>gs. Arch Gen Psychiatry 59:173–179.<br />
OrvaschelH, Puig-Antich (1987) Schedule for Affective Disorder <strong>and</strong><br />
Schizophrenia for School-Age Children, Epidemiologic Version.<br />
K-SADS-E Fourth Version.<br />
Owens DF, Kriegste<strong>in</strong> AR (2002) Is there more to GABA than synaptic<br />
<strong>in</strong>hibition? Nat Rev Neurosci 3:715–727.<br />
Parks MH, Dawant BM, Riddle WR, Hartmann SL, Dietrich MS, Nickel<br />
MK, et al (2002) Longitud<strong>in</strong>al bra<strong>in</strong> metabolic characterization of<br />
chronic alcoholics with proton magnetic resonance spectroscopy. Alcohol<br />
Cl<strong>in</strong> Exp Res 26:1368–1380.<br />
PausT,Coll<strong>in</strong>sDL,EvansAC, LeonardG,PikeB,ZijdenbosA (2001) Maturation<br />
of white matter <strong>in</strong> the human bra<strong>in</strong>: a review of magnetic resonance<br />
studies. Bra<strong>in</strong> Res Bull 54:255–266.<br />
Pfefferbaum A, Mathalon DH, Sullivan EV, Rawles JM, Zipursky RB,<br />
Lim KO (1994) A quantitative magnetic resonance imag<strong>in</strong>g study of<br />
changes <strong>in</strong> bra<strong>in</strong> morphology from <strong>in</strong>fancy to late adulthood. Arch<br />
Neurol 51:874–887.<br />
Pfefferbaum A, Sullivan EV, Mathalon DH, Lim KO (1997) Frontal lobe<br />
volume loss observed with magnetic resonance imag<strong>in</strong>g <strong>in</strong> older chronic<br />
alcoholics. Alcohol Cl<strong>in</strong> Exp Res 21:521–529.<br />
P<strong>in</strong>eda D, Ardila A, Rosselli M, Cadavid C, Mancheno S, Mejia S (1998)<br />
Executive dysfunctions <strong>in</strong> children with attention deficit hyperactivity<br />
disorder. Int J Neurosci 96:177–196.<br />
Rasb<strong>and</strong> W (1996) NIH IMAGE Manual. National Institutes of Health.<br />
Bethesda, MD.<br />
Rogers M, Kasai K, Koji M, Fukuda R, Iwanami A, Nakagome K, et al<br />
(2004) Executive <strong>and</strong> prefrontal dysfunction <strong>in</strong> unipolar depression: A<br />
review of neuropsychological <strong>and</strong> imag<strong>in</strong>g evidence. Neurosci Res 50:<br />
1–11.<br />
Rohde P, Lew<strong>in</strong>sohn PM, Seeley JR (1996) Psychiatric comorbidity with<br />
problematic alcohol use <strong>in</strong> high school students. J Am Acad Child<br />
Adolesc Psychiatry 35:101–109.<br />
Rosenberg DR, Keshavan MS, O’Hearn KM, Dick EL, Bagwell WW,<br />
Seymour AB, et al (1997) Frontostriatal measurement <strong>in</strong> treatmentnaive<br />
children with obsessive-compulsive disorder. Arch Gen Psychiatry<br />
54:824–830.<br />
Schmahmann JD (1997) The Cerebellum <strong>and</strong> Cognition, International<br />
Review of Neurobiology, Vol 41. San Diego CA: Academic Press.
1600 DE BELLIS ET AL.<br />
Schulz KP, Fan J, Tang CY, Newcorn JH, Buchsbaum MS, Cheung AM,<br />
et al (2004) Response <strong>in</strong>hibition <strong>in</strong> adolescents diagnosed with attention<br />
deficit hyperactivity disorder dur<strong>in</strong>g childhood: an event-related FMRI<br />
study. Am J Psychiatry 161:1650–1657.<br />
Sk<strong>in</strong>ner H (1982) Development <strong>and</strong> Validation of a Lifetime Alcohol Consumption<br />
Assessment Procedure. Toronto: Addiction Research Foundation.<br />
Sowell ER, Thompson PM, Welcome SE, Henkenius AL, Toga AW,<br />
Peterson BS (2003a) Cortical abnormalities <strong>in</strong> children <strong>and</strong> adolescents<br />
with attention-deficit hyperactivity disorder. Lancet 362:1699–1707.<br />
Sowell ER, Thompson PM, Welcome SE, Henkenius AL, Toga AW,<br />
Peterson BS (2003b) Cortical abnormalities <strong>in</strong> children <strong>and</strong> adolescents<br />
with attention-deficit hyperactivity disorder. Lancet 362:1699–1707.<br />
Spalletta G, Pas<strong>in</strong>i A, Pau F, Guido G, Mengh<strong>in</strong>i L, Caltagirone C (2001)<br />
<strong>Prefrontal</strong> blood flow dysregulation <strong>in</strong> drug naive ADHD children<br />
without structural abnormalities. J Neural Transm 108:1203–1216.<br />
Spear LP (2000) The adolescent bra<strong>in</strong> <strong>and</strong> age-related behavioral manifestations.<br />
Neurosci Biobehav Rev 24:417–463.<br />
Ste<strong>in</strong>gard RJ, Renshaw PF, Hennen J, Lenox M, C<strong>in</strong>tron CB, Young AD,<br />
et al (2002) Smaller frontal lobe white matter volumes <strong>in</strong> depressed<br />
adolescents. Biol Psychiatry 52:413–417.<br />
Sullivan EV (2003) Compromised pontocerebellar <strong>and</strong> cerebellothalamocortical<br />
systems: speculations on their contributions to cognitive <strong>and</strong><br />
motor impairment <strong>in</strong> nonamnesic alcoholism. Alcohol Cl<strong>in</strong> Exp Res<br />
27:1409–1419.<br />
Sullivan EV, Rosenbloom MJ, Serventi KL, Deshmukh A, Pfefferbaum A<br />
(2003) Effects of alcohol dependence comorbidity <strong>and</strong> antipsychotic<br />
medication on volumes of the thalamus <strong>and</strong> pons <strong>in</strong> schizophrenia.<br />
Am J Psychiatry 160:1110–1116.<br />
Tapert SF, Baratta MV, Abrantes AM, Brown SA (2002a) Attention<br />
dysfunction predicts substance <strong>in</strong>volvement <strong>in</strong> community youth. J Am<br />
Acad Child Adolesc Psychiatry 41:680–686.<br />
Tapert SF, Granholm E, Leedy NG, Brown SA (2002b) Substance use <strong>and</strong><br />
withdrawal: Neuropsychological function<strong>in</strong>g over 8 years <strong>in</strong> youth. J Int<br />
Neuropsychol Soc 8:873–883.<br />
Tarter R, Vanyukov M, Giancola P, Dawes M, Blackson T, Mezzich A, et<br />
al (1999) Epigenetic model of substance use disorder etiology. Dev<br />
Psychopathol 11:657–683.<br />
Tarter RE, Kirisci L, Mezzich A, Cornelius JR, Pajer K, Vanyukov M, et<br />
al (2003) Neurobehavioral dis<strong>in</strong>hibition <strong>in</strong> childhood predicts early age<br />
at onset of substance use disorder. Am J Psychiatry 160:1078–1085.<br />
Thompson PM, Giedd JN, Woods RP, MacDonald D, Evans AC, Toga<br />
AW (2000) Growth patterns <strong>in</strong> the develop<strong>in</strong>g bra<strong>in</strong> detected by us<strong>in</strong>g<br />
cont<strong>in</strong>uum mechanical tensor maps. Nature 404:190–193.<br />
Torvik A, Torp S (1986) The prevalence of alcoholic cerebellar atrophy: A<br />
morphometric <strong>and</strong> histological study of autopsy material. J Neurol Sci<br />
75:43–51.<br />
Wagner FA, Anthony JC (2002) From first drug use to drug dependence:<br />
developmental periods of risk for dependence upon marijuana, coca<strong>in</strong>e,<br />
<strong>and</strong> alcohol. Neuropsychopharmacology 26:479–488.<br />
Wiers RW, Sergeant JA, Gunnung WB (1994) Psychological mechanisms<br />
of enhanced risk of addiction <strong>in</strong> children of alcoholics: A dual pathway?<br />
Acta Paediatr Sc<strong>and</strong> Suppl 404:9–13.