EDI - European Association of Dental Implantologists
EDI - European Association of Dental Implantologists
EDI - European Association of Dental Implantologists
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ISSN 1862-2879<br />
Issue 3/2008 Vol. 4<br />
<strong>EDI</strong> Journal<br />
<strong>European</strong> Journal for<br />
<strong>Dental</strong> <strong>Implantologists</strong><br />
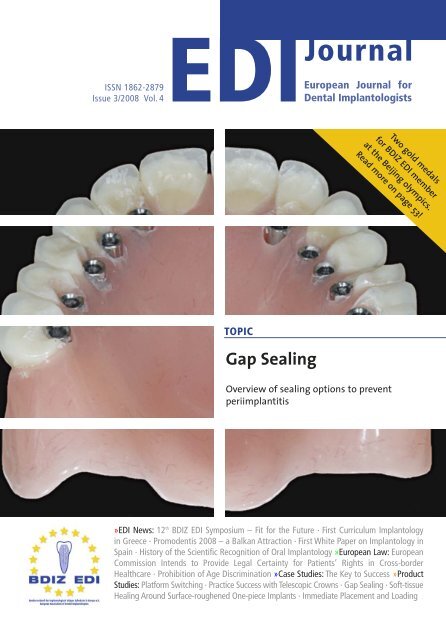
TOPIC<br />
Gap Sealing<br />
Two gold medals<br />
for BDIZ <strong>EDI</strong> member<br />
at the Beijing olympics.<br />
Read more on page 53!<br />
Overview <strong>of</strong> sealing options to prevent<br />
periimplantitis<br />
»<strong>EDI</strong> News: 12 th BDIZ <strong>EDI</strong> Symposium – Fit for the Future · First Curriculum Implantology<br />
in Greece · Promodentis 2008 – a Balkan Attraction · First White Paper on Implantology in<br />
Spain · History <strong>of</strong> the Scientific Recognition <strong>of</strong> Oral Implantology »<strong>European</strong> Law: <strong>European</strong><br />
Commission Intends to Provide Legal Certainty for Patients’ Rights in Cross-border<br />
Healthcare · Prohibition <strong>of</strong> Age Discrimination »Case Studies: The Key to Success »Product<br />
Studies: Platform Switching · Practice Success with Telescopic Crowns · Gap Sealing · S<strong>of</strong>t-tissue<br />
Healing Around Surface-roughened One-piece Implants · Immediate Placement and Loading
In 2009, Germany will be<br />
coming down with a<br />
monster that will benefit<br />
practically nobody and be<br />
a royal pain for most – the<br />
Federal Health Fund. A<br />
giant bureaucracy will be<br />
born that no other <strong>European</strong><br />
country has in quite<br />
the same form and to quite the same extent. We are talking about<br />
one <strong>of</strong> the most far-reaching social reforms <strong>of</strong> the post-WW2 era<br />
that will affect more people than the current pension discussion in<br />
Germany. Even before its arrival, this Federal Health Fund is spreading<br />
horror amongst members <strong>of</strong> the health pr<strong>of</strong>essions, employers<br />
and employees, health insurers, voters and even amongst many<br />
politicians who – at the very last moment, it would seem – have<br />
realized that the Fund has long since become a symbol for a glaring<br />
anachronism: Ulla Schmidt, the Federal Minister for Health,<br />
may be speaking <strong>of</strong> increased competition within the German<br />
health care system, but what she really means is nationalization,<br />
just like in socialist countries. Firmly by her side: Chancellor Angela<br />
Merkel, who despite resistance across the country is unwilling to<br />
give up on this unspeakable “healthcare reform”, which has nothing<br />
good in store for the 71 million people affected and which will<br />
bring, in addition to pronounced increases in premiums, a noticeable<br />
reduction in the quality <strong>of</strong> medical care throughout the country,<br />
as experts have warned. To say nothing <strong>of</strong> the pecuniary losses<br />
within entire regions or <strong>of</strong> the reductions in income for physicians<br />
and dentists.<br />
In October, a uniform premium will be determined for statutory<br />
health insurance that will probably amount to almost 16 percent<br />
<strong>of</strong> most employees’ gross pay and, consequently, mean higher cost<br />
both for them and for their employers, who are picking up almost<br />
half <strong>of</strong> the tab. Throughout the country, physicians and other medical<br />
personnel have been taking to the streets – 20,000 joined the<br />
protest demonstrations held in Munich’s Olympic Stadium in June<br />
alone. But any attempts to stop the monster appear to be too late:<br />
The Federal Health Fund, the coming centralized collecting institution<br />
for all healthcare premiums, has already taken up its work<br />
with 95 employees.<br />
In Bavaria, the second most populous German state, voters are<br />
expected to turn out in droves against the ruling conservative<br />
party in September to punish it for its links to the Berlin coalition<br />
who introduced the Fund. Christa Stewens, Bavarian State Minister<br />
<strong>of</strong> Labour and Social Welfare, had voiced her reservations against<br />
the Fund from the beginning, but all this brought her was reprimands<br />
from the Chancellor. Her ministry in Munich is therefore<br />
trying very hard to distance itself from the monster that originated<br />
in Berlin (see also the interview on page 42).<br />
Die Zeit, a renowned German weekly, has recently reported on<br />
the negative attitudes even among statutory health insurers,<br />
using the company health insurance fund <strong>of</strong> Audi, the car manufacturer,<br />
as an example. At present, the premium for their quarter<br />
million insurance contracts is 13.1 percent <strong>of</strong> gross pay, which is<br />
comparatively low. Now it seems as if everybody will have to pay<br />
an extra 350 euros a year – and that on top <strong>of</strong> rising energy prices,<br />
an increase that makes everybody’s blood boil, especially since the<br />
ruling coalition in Berlin had originally promised to reduce nonwage<br />
labour costs in Germany, in part by reducing health insurance<br />
premiums.<br />
The cost <strong>of</strong> the bureaucracy will also increase. The statutory<br />
health insurers will have to reinvent the way they collect their premiums<br />
– a logistical tour de force. At present, employers withhold<br />
the employee’s share <strong>of</strong> the premiums from wages and forward it<br />
to health insurers along with their own share. Because the health<br />
insurers will be able, and <strong>of</strong>ten forced, to charge supplementary<br />
premiums in the future, they must provide for collecting these premiums,<br />
generating individual accounts for all policyholders. One<br />
health insurer alone stated that this accounting changeover cost<br />
them 40 million euros. The current government actually inherited<br />
the idea <strong>of</strong> the Health Fund from its predecessor, the “Red/Green”<br />
government in power until 2005. The Social Democrats had set out<br />
to force private health insurers to pay substantial amounts <strong>of</strong><br />
money to bail out some <strong>of</strong> the less fortunate statutory health<br />
insurers. The Christian Democrats, by contrast, wanted to introduce<br />
flat per-capita premiums that were independent <strong>of</strong> policyholders’<br />
incomes and not co-financed by employers. But in the<br />
end, neither <strong>of</strong> these ideas was realized. Today, many politicians<br />
might wish to close their eyes and see if their own Federal Health<br />
Fund maybe simply goes away. But burying your head in the sand<br />
no longer works – the masses <strong>of</strong> those who are affected will take<br />
care <strong>of</strong> that. The health insurers themselves. Physicians and medical<br />
personnel. And the voters, who will be seeing plenty <strong>of</strong> headlines<br />
shouting out the news <strong>of</strong> rising premiums and <strong>of</strong> chaos and<br />
turmoil in those organizations they depend on for their health.<br />
The year 2009 will see federal elections and millions <strong>of</strong> policyholders<br />
<strong>of</strong> statutory health insurers will be witnessing “quite<br />
annoying things”, as Die Zeit predicts by way <strong>of</strong> genteel understatement.<br />
The voters might be the only ones that can make the<br />
government back away from its plans – for a while anyway.<br />
Sincerely,<br />
Christian Berger, Kempten/Germany<br />
President <strong>of</strong> BDIZ <strong>EDI</strong><br />
<strong>EDI</strong><br />
Editorial<br />
Germans are Turning<br />
away in Horror<br />
3
4 <strong>EDI</strong><br />
Table <strong>of</strong> Content<br />
<strong>EDI</strong> News<br />
<strong>Dental</strong> Medicine in Focus – Fit for the Future<br />
12 th BDIZ <strong>EDI</strong> Symposium/Hesse Dentists’ Congress 8<br />
A Greek-German Joint Venture<br />
Pilot project: Curriculum Implantology in Greece 14<br />
Motivated to their Fingertips<br />
Attendants <strong>of</strong> the first Greek Curriculum<br />
Implantology 17<br />
Promodentis 2008 – a Balkan Attraction<br />
<strong>Dental</strong> trade show and congress in Novi Sad 18<br />
First White Paper on Implantology in Spain 21<br />
History <strong>of</strong> the Scientific Recognition <strong>of</strong> Oral<br />
Implantology<br />
Foreword 22<br />
Committed to our Tradition – Looking Back on<br />
the History <strong>of</strong> the BDIZ <strong>EDI</strong> 24<br />
Looking Back and Looking Forward 30<br />
The Tübingen Implant 36<br />
Federal Health Fund: “Dispose <strong>of</strong> it Properly!”<br />
Interview with Christa Stewens 42<br />
Are we Threatened by a New Wave <strong>of</strong> Regulations?<br />
<strong>European</strong> Commission to strengthen<br />
patients’ rights 46<br />
18 th Expert Symposium University and<br />
Clinical Practice<br />
Fuerteventura 2008 50<br />
Quintessenz-TV: Online Video Library 52<br />
Implantologist Wins Two Gold Medals<br />
BDIZ <strong>EDI</strong> congratulates Hinrich Peter Romeike 53<br />
Europe-Ticker 54<br />
<strong>European</strong> Law<br />
<strong>European</strong> Commission Intends to Provide Legal<br />
Certainty for Patients’ Rights in Cross-border<br />
Healthcare 58<br />
Prohibition <strong>of</strong> Age Discrimination 62<br />
Case Studies<br />
The Key to Success<br />
Anterior maxilla reconstructed with autogenous<br />
calvarial bone block grafts restored with dental<br />
implants 64<br />
Product Studies<br />
Platform Switching<br />
Clinical and biomechanical outcomes 72<br />
Practice Success with Telescopic Crowns<br />
Prosthodontic reconstruction <strong>of</strong> the edentulous<br />
maxilla with a removable denture 78<br />
Gap Sealing<br />
Overview <strong>of</strong> sealing options to prevent periimplantitis<br />
84<br />
S<strong>of</strong>t-tissue Healing Around Surface-roughened<br />
One-piece Implants 88<br />
Immediate Placement and Loading<br />
A basis for predictable esthetic transitional<br />
contour 92<br />
Business & Events<br />
Making New Discoveries<br />
Astra Tech World Congress 2008 96<br />
Groundbreaking Technology<br />
BioHorizons Global Symposium 2008 98<br />
CARS 2008, Barcelona 99<br />
EAO 17 th Annual Scientific Meeting, Warsaw 100<br />
The camlog foundation Research Award<br />
2008/2009 101<br />
SimPlant Academy World Conference on<br />
3D Digital Dentistry 102<br />
An Investment to the Future 104<br />
Camlog Invests in the Future <strong>of</strong> its<br />
Wimsheim Site 105<br />
News and Views<br />
Editorial: Germans are Turning away in Horror 3<br />
Imprint 6<br />
Product Reports 106<br />
Product News 114<br />
Calendar <strong>of</strong> Events 122<br />
Publishers Corner 122
6<br />
<strong>EDI</strong><br />
Imprint<br />
<strong>EDI</strong><br />
<strong>European</strong> Journal for <strong>Dental</strong> <strong>Implantologists</strong><br />
a BDIZ <strong>EDI</strong> publication<br />
published by teamwork media GmbH, Fuchstal<br />
<strong>Association</strong>: The <strong>European</strong> Journal for <strong>Dental</strong> <strong>Implantologists</strong> (<strong>EDI</strong>)<br />
is published in cooperation with BDIZ <strong>EDI</strong><br />
Publisher Board<br />
Members:<br />
Christian Berger<br />
Pr<strong>of</strong> Dr Dr Joachim E. Zöller<br />
Dr Detlef Hildebrand, Dr Thomas Ratajczak<br />
Editor in Chief: Ralf Suckert, r.suckert@teamwork-media.de<br />
Editors: Anita Wuttke, Phone +49 89 72069-888, wuttke@bdizedi.org<br />
Simone Stark, Phone +49 8243 9692-34, s.stark@teamwork-media.de<br />
Scientific Board: Pr<strong>of</strong> Dr Alberico Benedicenti, Genoa Dr Marco Degidi, Bologna<br />
Dr Eric van Dooren, Antwerp Pr<strong>of</strong> Dr Rolf Ewers, Vienna<br />
Pr<strong>of</strong> Dr Antonio Felino, Porto PD Dr Jens Fischer, Bern<br />
Dr Roland Glauser, Zurich Pr<strong>of</strong> Dr Dr Ingrid Grunert, Innsbruck<br />
Dr Detlef Hildebrand, Berlin Dr Axel Kirsch, Filderstadt<br />
Pr<strong>of</strong> Dr Ulrich Lotzmann, Marburg Pr<strong>of</strong> Dr Edward Lynch, Belfast<br />
Dr Konrad Meyenberg, Zurich Pr<strong>of</strong> Dr Georg Nentwig, Frankfurt<br />
Dr Jörg Neugebauer, Cologne Pr<strong>of</strong> Dr Georgios Romanos, Rochester<br />
MDT Luc and Patrick Rutten, Tessenderlo Dr Henry and Maurice Salama, Atlanta<br />
Dr Ashok Sethi, London<br />
Pr<strong>of</strong> Dr Dr Joachim Zöller, Cologne<br />
Ralf Suckert, Fuchstal<br />
All case reports and scientific documentations are peer reviewed by the international editorial board<br />
<strong>of</strong> “teamwork – Journal <strong>of</strong> Multidisciplinary Collaboration in Restorative Dentistry“<br />
Project Management<br />
& Advertising:<br />
Marianne Steinbeck, MS Media Service, Badstraße 5, D-83714 Miesbach,<br />
Phone +49 8025 5785, Fax +49 8025 5583, msmedia@aol.com<br />
Publishers: teamwork media Verlags GmbH, Hauptstr. 1, D-86925 Fuchstal<br />
Phone +49 8243 9692-11, Fax +49 8243 9692-22<br />
service@teamwork-media.de; www.teamwork-media.de<br />
Layout: Sigrid Eisenlauer; teamwork media GmbH<br />
Printing: J. Gotteswinter GmbH; Munich<br />
Publication Dates: March, June, September, December<br />
Subscription Rates: Annual subscription: Germany € 40.- including shipping and VAT. All other countries € 58.- including shipping. Subscription<br />
payments must be made in advance. Ordering: in written form only to the publisher. Cancellation deadlines:<br />
in written form only, 8 weeks prior to end <strong>of</strong> subscription year. Subscription is governed by German law. Past issues<br />
are available. Complaints regarding nonreceipt <strong>of</strong> issues will be accepted up to 3months after date <strong>of</strong> publication.<br />
Current advertising rate list No. 1, from 1/01/05<br />
ISSN 1862-2879<br />
Payments: to teamwork media GmbH;<br />
Raiffeisenbank Fuchstal BRC 733 698 54 Account No.100 416746<br />
Copyright and<br />
Publishing Rights:<br />
All rights reserved. The magazine and all articles and illustrations therein are protected by copyright. Any utilization<br />
without the prior consent <strong>of</strong> editor and publisher is inadmissible and liable to prosecution. No part <strong>of</strong> this publication<br />
may be produced or transmitted in any form or by any means, electronic or mechanical including by photocopy, recording,<br />
or information storage and retrieval system without permission in writing from the publisher. With acceptance <strong>of</strong><br />
manuscripts the publisher has the right to publish, translate, permit reproduction, electronically store in databases, produce<br />
reprints, photocopies and microcopies. No responsibility shall be taken for unsolicited books and manuscripts. Articles<br />
bearing symbols other than <strong>of</strong> the editorial department or which are distinguished by the name <strong>of</strong> the authors represent<br />
the opinion <strong>of</strong> the afore-mentioned, and do not have to comply with the views <strong>of</strong> BDIZ <strong>EDI</strong> or teamwork media<br />
GmbH. Responsibility for such articles shall be borne by the author. All information, results etc. contained in this publication<br />
are produced by the authors with best intentions and are carefully checked by the authors and the publisher. All<br />
cases <strong>of</strong> liability arising from inaccurate or faulty information are excluded. Responsibility for advertisements and other<br />
specially labeled items shall not be borne by the editorial department.<br />
Copyright: teamwork media GmbH . Legal Venue: Munich
8<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
12 th BDIZ <strong>EDI</strong> Symposium/Hesse Dentists’ Congress, Frankfurt<br />
<strong>Dental</strong> Medicine in Focus –<br />
Fit for the Future<br />
The title <strong>of</strong> this year’s BDIZ <strong>EDI</strong> symposium should be taken quite literally: Fit for the Future – when it comes to the German<br />
standard fee schedule for dentists, GOZ. BDIZ <strong>EDI</strong> is aiming to prepare symposium attendants for working with the new GOZ.<br />
And there is an innovation this year: For the first time, BDIZ <strong>EDI</strong> holds its annual symposium jointly with the Hesse Chamber <strong>of</strong><br />
Dentists. The 12 th BDIZ <strong>EDI</strong> Symposium and Hesse Dentists’ Congress (Hessischer Zahnärztetag) will take place at the Congress<br />
Center <strong>of</strong> Messe Frankfurt on 7 and 8 November 2008 – very much in line with the BDIZ <strong>EDI</strong> tradition, addressing health-care<br />
policy, legal and accounting matters and <strong>of</strong>fering a comprehensive scientific program.<br />
The imminent introduction <strong>of</strong> the new standard fee<br />
schedule is probably the topic currently most discussed<br />
among German dentists. Originally planned<br />
for 1 January 2008, the Federal Ministry <strong>of</strong> Health is<br />
now proposing a starting date <strong>of</strong> 1 January 2009, but<br />
even this starting date may be difficult to realize.<br />
Nevertheless, GOZ is certain to take effect some time<br />
next year. Unfortunately, looking at the second GOZ<br />
draft currently circulated by the Ministry, hopes are<br />
slim for the new fee schedule to achieve more than<br />
shuffling around a bunch <strong>of</strong> already existing items.<br />
GOZ in daily practice<br />
On the whole, it must be stated that, while dentistry<br />
has made enormous progress in many fields during<br />
the past 20 years, the GOZ draft does not really take<br />
this into account. The only thing we will get is a re -<br />
organization <strong>of</strong> GOZ that is “volume neutral”. Moreover,<br />
fears are justified that GOZ, which applies to private<br />
contract for dental service, will be made to conform<br />
more closely to the much-denounced BEMA, a<br />
catalogue <strong>of</strong> service point values that is applicable to<br />
patients covered by statutory health insurance. For<br />
these reasons, an entire day during the symposium is<br />
dedicated to GOZ alone. What does GOZ 2009 actually<br />
say? How is it structured and – most importantly –<br />
what will its effects be? These topics will be discussed<br />
by a round <strong>of</strong> experts consisting <strong>of</strong> Dr Rataj -<br />
czak, Dr Sobek, Dr Winzen and Dr Brodmann, on the<br />
morning <strong>of</strong> 7 November.<br />
Highly practical aspects will be addressed on the<br />
afternoon <strong>of</strong> the same day. Clinical cases from perio -<br />
dontology, restorative dentistry and oral implantology<br />
will be presented, followed by discussions <strong>of</strong> the<br />
corresponding accounting issues pursuant to GOZ<br />
2009 and HOZ (which is the German <strong>Dental</strong> <strong>Association</strong>’s<br />
fee schedule). These sessions and the subsequent<br />
discussion will be hosted by the respective<br />
president <strong>of</strong> the Hesse Chamber <strong>of</strong> Dentists and BDIZ<br />
<strong>EDI</strong>, Dr Michael Frank and Christian Berger. For a list <strong>of</strong><br />
speakers, please consult the following program.<br />
Annual General Meeting<br />
This year’s Annual General Meeting <strong>of</strong> BDIZ <strong>EDI</strong><br />
will take place at the Congress Center <strong>of</strong> Messe<br />
Frankfurt on 7 November 2008 between 12:30 pm<br />
and 2 pm. Conspicuous signs will guide participants<br />
to the appropriate room.<br />
Pure science<br />
The scientific program on Saturday, 8 November<br />
2008 will be very much in line with the motto <strong>of</strong> the<br />
symposium, Fit for the Future. Clinical concepts for<br />
the dental <strong>of</strong>fice will be presented in the morning,
EDA Testing<br />
starting with a discussion <strong>of</strong> parallels between general<br />
medicine and dentistry (Pr<strong>of</strong> Gerlach, Frankfurt)<br />
and the diagnosis <strong>of</strong> diseases <strong>of</strong> the oral mucosa<br />
(Pr<strong>of</strong> Wagner, Mainz). After that, several speakers will<br />
present their own treatment concepts: on current<br />
restorative treatment options (Pr<strong>of</strong> Mehl, Zürich), on<br />
current issues in endodontics (Dr Zehnder, Zürich)<br />
and on microbiological diagnostic concepts in perio -<br />
dontal therapy (Dr Ehmke, Münster). The morning<br />
segment concludes with a summary by BDIZ <strong>EDI</strong> vice<br />
president Pr<strong>of</strong> Joachim E. Zöller (University <strong>of</strong> Cologne)<br />
and a discussion <strong>of</strong> the presentations held during the<br />
morning.<br />
The afternoon segment is dedicated entirely to oral<br />
implantology, featuring two highly interesting com-<br />
As previously, the 12 th BDIZ <strong>EDI</strong> Symposium <strong>of</strong>fers the perfect<br />
opportunity to take the certification exam for EDA Expert in<br />
Implantology (<strong>European</strong> <strong>Dental</strong> <strong>Association</strong>). Interested dentists<br />
should learn more about the admission requirements available<br />
at www.bdizedi.org/Education or by contacting the BDIZ <strong>EDI</strong> <strong>of</strong>fice<br />
in Bonn. Registration forms and admission requirement information<br />
are also available via e-mail from <strong>of</strong>fice-bonn@bdizedi.org.<br />
parisons: “Dialogue on correct implant prosthetics –<br />
restorative dentist and dental surgeon” (Dr Hildebrand,<br />
Berlin) and “Dialogue on correct implant<br />
surgery – dental surgeon and restorative dentist”<br />
(Dr Neugebauer, Köln). These dialogues will then lead<br />
to a discussion in which members <strong>of</strong> the audience<br />
are welcome to participate.<br />
The highlight <strong>of</strong> the day, and its culmination, will<br />
be a live implant restoration session. Dr Paul Weigl<br />
(Frankfurt) will be presenting a correct course <strong>of</strong><br />
implant and restorative treatment, step by step, from<br />
bite registration to insertion. The final discussion will<br />
be hosted by Christian Berger and Dr Michael Frank.<br />
Workshops and dental exhibition<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Participants <strong>of</strong> the two-day symposium will have an<br />
opportunity to register for one <strong>of</strong> the traditional four<br />
workshops held under the auspices <strong>of</strong> the dental<br />
industry on Friday morning between 9 am and noon.<br />
A visit to the dental exhibition is highly recommended<br />
during the breaks on Saturday. The program for<br />
the 12 th BDIZ <strong>EDI</strong> Symposium can be found in the following<br />
section.<br />
9
10<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Friday, 7 November 2008<br />
“Fit for Future”: GOZ 2009<br />
GOZ Forum 2009<br />
9:00 AM – noon Introduction: The GOZ-Forum<br />
Dr M. Frank, Lampertheim<br />
C. Berger, Kempten<br />
GOZ 2009: Content – Structure – Consequences<br />
Dr J.M. Sobek, Hamm<br />
Dr O. Winzen, Frankfurt<br />
Dr G. Brodmann, Bad Dürkheim<br />
Dr T. Ratajczak, Sindelfingen<br />
12:30 – 2:00 PM BDIZ <strong>EDI</strong> General Meeting<br />
GOZ in daily practice<br />
2:00 – 2:15 PM Welcoming address<br />
C. Berger<br />
Dr M. Frank<br />
2:15 – 2:45 PM The perio case – clinical aspects<br />
Dr B. Ehmke, Münster<br />
2:45 – 3:15 PM The perio case: Billing according to GOZ 2009/HOZ<br />
Dr O. Winzen, Frankfurt<br />
3:15 – 3.45 PM Break<br />
3:45 – 4:15 PM The prosthetic case – clinical aspects<br />
Dr D. Hildebrand, Berlin<br />
4:15 – 4:45 PM The prosthetic case: Billing according to GOZ 2009/HOZ<br />
Dr J.M. Sobek, Hamm<br />
4:45 – 5:15 PM The implant case – clinical aspects<br />
Pr<strong>of</strong>essor J.E. Zöller, Cologne<br />
5:15 – 5:45 PM The implant case: Billing according to GOZ 2009/HOZ<br />
Dr Christian Foitzik, Darmstadt<br />
5:45 PM Discussion and summary<br />
Dr M. Frank<br />
C. Berger<br />
6:30 PM Get-together party in the Congress Foyer<br />
8:00 PM Social event for participants<br />
Friday, 7 November 2008<br />
Pre-congress Workshops<br />
9:00 AM – noon Workshop 1 Microbiological diagnostics in periodontal therapy<br />
Gaba Dr P.M. Jervøe-Storm<br />
9:00 AM – noon Workshop 2 Regeneration techniques using stem cells<br />
Geistlich N.N.<br />
9:00 AM – noon Workshop 3 Natural aesthetics in anterior reconstructions made easy<br />
American <strong>Dental</strong> Systems Dr H. Klinge<br />
9:00 AM – noon Workshop 4<br />
N.N.<br />
Implantology
12<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Saturday, 8 November 2008<br />
“Fit for Future”: Scientific Program<br />
Fax to:<br />
+49 228 9359 246<br />
or mail to<br />
BDIZ <strong>EDI</strong> Geschäftsstelle Bonn<br />
An der Esche 2<br />
53111 Bonn<br />
Germany<br />
Clinical concepts for practitioners (chair: Pr<strong>of</strong>essor J.E. Zöller)<br />
9:00 – 9:15 AM Welcoming address<br />
Dr M. Frank, Lampertheim<br />
C. Berger, Kempten<br />
9:15 – 9:45 AM The future is chronic: Parallels between general medicine and dentistry<br />
Pr<strong>of</strong>essor F.M. Gerlach, MPH, Frankfurt<br />
9:45 – 10:15 AM Oral medicine: Diagnosing diseases <strong>of</strong> the oral mucosa<br />
Pr<strong>of</strong>essor W. Wagner, Mainz<br />
10:15 – 10:45 AM Break · <strong>Dental</strong> exhibition visit<br />
10:45 – 11:15 AM Current concepts in restorative treatment<br />
Pr<strong>of</strong>essor A. Mehl, Zürich<br />
11:15 – 11:45 AM Current concepts in endodontics<br />
Dr M. Zehnder, Zürich<br />
11.15 AM – 12:15 PM Microbiological diagnostic concepts in periodontal therapy<br />
Dr B. Ehmke, Münster<br />
12.15 – 12:30 PM Discussion <strong>of</strong> the morning presentations<br />
Pr<strong>of</strong>essor J.E. Zöller, Cologne<br />
12:30 – 2:00 PM Break · <strong>Dental</strong> exhibition visit<br />
Implantology – from the planning stage to the prosthetic result (chair: Dr M. Frank)<br />
2:00 – 2:30 PM Dialog on correct implant prosthetics – Restorative dentist and dental surgeon<br />
Dr D. Hildebrand, Berlin<br />
2:30 – 2:45 PM Discussion<br />
Dr C. Foitzik, Darmstadt<br />
2:45 – 3:15 PM Dialog on correct implant surgery – <strong>Dental</strong> surgeon and restorative dentist<br />
Pr<strong>of</strong>essor J.E. Zöller, Cologne<br />
3:15 – 3:30 PM Discussion<br />
Dr M. Frank<br />
3:30 – 4:00 PM Break · <strong>Dental</strong> exhibition visit<br />
Live implant restoration session<br />
4:00 – 5:00 PM Correct implant restorations<br />
Step-by-step: From bite registration to insertion<br />
Dr P. Weigl, Frankfurt<br />
5:00 PM Final discussion<br />
Dr M. Frank<br />
C. Berger<br />
Please register the following persons for the 12th BDIZ <strong>EDI</strong> Symposium (Frankfurt, 7/8 November 2008).<br />
I understand that the registration is binding.<br />
Please complete or tick as appropriate<br />
Family name —————————————————— Title ————— Given name ————————————————<br />
Street address —————————————————— Postal code/City —————————————————————<br />
Phone (home phone if necessary) —————— Fax ————————— E-mail ——————————————————–<br />
–––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––––<br />
Office seal<br />
Please enter my order for ____ tickets<br />
for the evening program on 7 November.<br />
I will be attending the General Meeting.<br />
BDIZ <strong>EDI</strong> would like to refer you to its Terms and Conditions for the 12 th<br />
BDIZ <strong>EDI</strong> Symposium. For rates and the symposium program, please visit<br />
www.bdizedi.org.<br />
Dentist/physician<br />
Member BDIZ <strong>EDI</strong><br />
Non-member<br />
assistant<br />
Workshop to attend (please choose one):<br />
1 2 3 4<br />
(Available only for congress registrants)<br />
Date/Signature ———————————————––––––——————————
14<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Pilot project: Curriculum Implantology in Greece<br />
A Greek-German Joint Venture<br />
The first Curriculum Implantology in Greece, jointly<br />
arranged by the BDIZ <strong>EDI</strong> and the University <strong>of</strong> Cologne,<br />
was successfully concluded in the Greek capital <strong>of</strong><br />
Athens in July this year. The 26 graduates received their<br />
certificates from BDIZ <strong>EDI</strong> president Christian Berger<br />
personally in a solemn ceremony at the Parthenon<br />
Hotel. But whilst the BDIZ <strong>EDI</strong> assisted the Greek side in<br />
getting started, there was certainly no intention simply<br />
to implement the German setup one-to-one. While<br />
preserving the guidelines laid down in the curriculum <strong>of</strong><br />
the Consensus Conference on <strong>Dental</strong> Implantology, the<br />
concept implemented gave special regard to the<br />
specifics <strong>of</strong> the Greek environment. The driving force<br />
behind the scenes was Dr Peter Ehrl from Berlin.<br />
This first series <strong>of</strong> courses had been kicked <strong>of</strong>f on<br />
28 October 2007 and was completed by 26 graduates<br />
with an intensive session on infection control in the<br />
operating theatre on 12 July 2008. During this time,<br />
the Greek dentists completed 124 hours <strong>of</strong> training.<br />
Within the framework <strong>of</strong> the individual continuingeducation<br />
modules, the participants also visited the<br />
clinic <strong>of</strong> Dr Ehrl in Berlin and the dental <strong>of</strong>fice <strong>of</strong> BDIZ<br />
<strong>EDI</strong> secretary general Dr Detlef Hildebrand to sit in on<br />
live surgery performed by the pros. The tremendous<br />
The city <strong>of</strong> contrasts: Old Athens and new Athens.<br />
The Acropolis, high above the ro<strong>of</strong>s <strong>of</strong> Athens.<br />
number <strong>of</strong> applications for the Curriculum shows<br />
how interested the Greek dentists are in dental<br />
implantology. Curriculum 2 has been going on for several<br />
months now, while Curriculum 3 has just started.<br />
From idea to implementation<br />
Everything started when BDIZ <strong>EDI</strong> and Yannis Roussis<br />
<strong>of</strong> the Greek dental publisher Omnipress took contact<br />
during a session <strong>of</strong> the BDIZ <strong>EDI</strong> <strong>European</strong> Committee<br />
in Munich in 2006. At the time, Roussis was<br />
looking to open up opportunities for Greek dentists<br />
to embark on studies in innovative fields, such as<br />
dental implantology, in their own country. BDIZ <strong>EDI</strong><br />
had promised support. The chance came, and was<br />
seized immediately, when Dr Peter Ehrl held a presentation<br />
on implantology in Athens and was contacted<br />
by Yannis Roussis. Within half a year, Dr Ehrl and the<br />
BDIZ <strong>EDI</strong> developed a complete concept, including a<br />
timeline and a line-up <strong>of</strong> speakers, which included<br />
Dr Efstratios Papazoglou, a young Greek dentist who<br />
had both studied and taught in the US and who was<br />
now to be responsible for the implementation <strong>of</strong> the<br />
Curriculum in his home country. Omnipress was<br />
responsible for organizing the individual modules in<br />
Athens; Dr Ehrl organized the one-week practical<br />
module in Berlin, where the participants engaged in
16<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
hands-on studies at the clinic <strong>of</strong> Dr Ehrl and at the<br />
dental <strong>of</strong>fices <strong>of</strong> Dr Hildebrand and Dr Steffen Köhler.<br />
Many <strong>of</strong> the participants placed their first implants<br />
during the Curriculum. Dr Ehrl had given them two<br />
specific tasks to complete: one task included the<br />
placement <strong>of</strong> a single-tooth implant, complete with<br />
photographic case documentation and a presentation<br />
before the group, and the second task included<br />
the placement <strong>of</strong> implants in an edentulous jaw, also<br />
with documentation and presentation. Each case<br />
was comprehensively discussed in the group.<br />
Greek-German team <strong>of</strong> presenters<br />
The implementation <strong>of</strong> this first Curriculum worked<br />
beautifully, with praise due to its architects, Dr Peter<br />
A. Ehrl <strong>of</strong> Berlin and Dr Efstratios Papazoglou <strong>of</strong><br />
Athens. The team they had assembled cooperated<br />
across national boundaries in an easy and uncomplicated<br />
manner. The Greek speakers were Dr Ioannis<br />
Fakitsas, Dr Giorgos Goumenos, Dr Syridon Karatzas,<br />
Dr Konstantin Lagios, Dr Efstratios Papazoglou, Dr Stavros<br />
Pelekanos, Dr Nick Petrou and Dr Nick Raptis. The German<br />
speakers were Dr Peter A. Ehrl, Christian Berger,<br />
Dr Detlef Hildebrand, Dr Steffen Köhler and Pr<strong>of</strong>essor<br />
Joachim E. Zöller.<br />
Conclusions<br />
Looking back on this successful pilot project, Dr Ehrl<br />
could not help but be satisfied. The goal had not been<br />
“to impose German structures on other countries but<br />
to create <strong>European</strong> structures that are accessible to<br />
all countries”. This also happens to be the objective<br />
that BDIZ <strong>EDI</strong> pursues – and it would be great if we<br />
gave a chance to implantological associations in<br />
Europe to build similar structures where this is<br />
desired. BDIZ <strong>EDI</strong> is ready to help.<br />
Graduates<br />
Dr Stavros Bletsas<br />
Dr Ioannis Triantafyllou<br />
Dr Georgios Kontorinis<br />
Dr Spyros Danias<br />
Dr Paraskevi Margellou<br />
Dr Christiana Constantinou<br />
Dr Iliana Gkevreki<br />
Dr Georgios Vasilopoulos<br />
Dr Ioannis Tzikopoulos<br />
Dr Harilaos Pashardis<br />
Dr Georgios Magouliotis<br />
Dr Vasilios Gogos<br />
Highly motivated and attentive participants – until the very last day.<br />
Successful graduates <strong>of</strong> the first Greek Curriculum Implantology and their teachers.<br />
Dr Nikolaos Michalopoulos<br />
Dr Christina Kagelari<br />
Dr Dimitrios Kristallis<br />
Dr Ilias Liakouras<br />
Dr Aikaterini Gkova<br />
Dr Panagiotis Dedes<br />
Dr Vasiliki Papavasileiou<br />
Dr Konstantinos Kyriopoulos<br />
Dr Mersini Tourvali<br />
Dr Konstantinos Dellis<br />
Dr Vasilious Vasiloudes<br />
Dr Theodora Karakousoglou<br />
Dr Ioannis Diamantopoulos<br />
Our first implant:<br />
These two young<br />
dentists will go a<br />
long way!
Attendants <strong>of</strong> the first Greek Curriculum Implantology<br />
Motivated to their Fingertips<br />
The high level <strong>of</strong> motivation on the part <strong>of</strong> the twenty-six<br />
participants <strong>of</strong> the first Greek Curriculum Implantology –<br />
some <strong>of</strong> whom had actually placed their very first implant<br />
during the Curriculum – was impressive even for lecturer<br />
Dr Peter Ehrl from Berlin. “We have learned something from<br />
you as well”, he said as he took leave from his students <strong>of</strong><br />
this first Curriculum.<br />
We would like to present one <strong>of</strong> these highly motivated dentists:<br />
Dr Vasilis Vasiloudes from Cyprus, who studied dentistry in Freiburg,<br />
Germany 20 years ago, then returned to his home country after<br />
graduation to open his own practice. Ten years ago he started getting<br />
involved in oral implantology. “That was the right decision to<br />
make”, he says today. Having mastered periodontology, he wanted<br />
to be active in the surgical field, placing implants and directing the<br />
restorative process. His small <strong>of</strong>fice in Nicosia, with a single treatment<br />
room and two assistants, is growing thanks to the increasing<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
demand for implantological treatments.<br />
He is planning to add a<br />
second treatment room soon: „This<br />
course has given me plenty <strong>of</strong> selfconfidence!”<br />
By way <strong>of</strong> confirmation,<br />
he recounts that he had placed a<br />
hundred implants in five years.<br />
Meanwhile, he places at least that<br />
many in a single year.<br />
The Cypriot dentist plans to attend<br />
more continued-education events in Dr Vasilis Vasiloudes<br />
the field <strong>of</strong> dental im plantology. He is<br />
considering the certification exam for EDA Expert in Implantology<br />
(<strong>European</strong> <strong>Dental</strong> <strong>Association</strong>), which requires many years <strong>of</strong> prior<br />
experience and the placement <strong>of</strong> a large number <strong>of</strong> implants and<br />
implant-supported restorations every year. Despite being a father<br />
<strong>of</strong> three, he is willing to travel long distances to attend continuingeducation<br />
events, as his participation at the Curriculum has shown<br />
– he had to fly from Nicosia to Athens every week to attend.<br />
17
18<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
<strong>Dental</strong> trade show and congress in Novi Sad<br />
Promodentis 2008 –<br />
a Balkan Attraction<br />
June 2008 saw the fifth incarnation <strong>of</strong> Promodentis – Novi Sad, the dental trade show with its integrated<br />
congress for dentists and dental technicians that has become known far beyond the limits <strong>of</strong> the Balkans,<br />
presenting innovations in the technical as well as in the dental scientific and practical fields.<br />
For three days, 34 experts from Serbia, Germany,<br />
Romania, Italy, Slovenia, the Serbian constituent<br />
republic <strong>of</strong> Bosnia-Herzegovina and Macedonia presented<br />
clinical cases and technical innovations from<br />
dentistry and dental technology. The 650 congress<br />
participants were able to sample an overview <strong>of</strong><br />
dental developments in Europe, at the same time<br />
demonstrating that the field <strong>of</strong> dental implantology<br />
is looming in the Balkans.<br />
Meeting point on the Danube<br />
With its 350,000 inhabitants, Novi Sad (“New Garden”)<br />
is Serbia’s second-largest city, which has long<br />
since emerged from the shadows <strong>of</strong> Serbia’s capital<br />
Belgrade, which is only 70 km away. In addition to the<br />
annual Promodentis event, the inter national Pro -<br />
medika trade show has been held for 16 years now –<br />
a trade show where protagonists <strong>of</strong> medicine meet<br />
the pharmaceutical industry. Despite its historically<br />
young age – it was founded at the end <strong>of</strong> the 17 th century<br />
– Novi Sad can look back on a turbulent history<br />
(see box). The city was founded as a meeting point for<br />
traders and craftsmen under the protection <strong>of</strong> the<br />
Petrovaradin fortress, located on the other side <strong>of</strong> the<br />
Danube River. Today, the city is a focal point for innovative<br />
medical, pharmaceutical and dental technology.<br />
Fruitful cooperation<br />
Politicians and academic representatives <strong>of</strong> the medical<br />
and dental faculties <strong>of</strong> several Balkan universities<br />
had followed the invitation to participate at Promodentis<br />
2008. The congress was organized by the Serbian<br />
medical society DLVSLD, founded in 1872, by the<br />
Serbian <strong>Association</strong> <strong>of</strong> dental technicians and by the<br />
partner association <strong>of</strong> BDIZ <strong>EDI</strong>, the implantological<br />
society UOI-SCG-<strong>EDI</strong>.<br />
Germany was represented by BDIZ <strong>EDI</strong> president<br />
Christian Berger. This was the second time that Berger<br />
attended Promodentis Novi Sad as the personal<br />
guest <strong>of</strong> UOI-SCG-<strong>EDI</strong> president Dr Dusan Vasiljevic.<br />
He spoke on “Decisions: preserve or implant?” The<br />
presentation also addressed unresolved questions in<br />
dental implantology: Can peri-implantitis be prevented?<br />
How can peri-implantitis be treated, and what<br />
effect does this treatment have on the prognosis <strong>of</strong><br />
the implant? The cooperation <strong>of</strong> the two partner<br />
Dr Branislav Kardasevic<br />
and Dr Dusan Vasiljevic.<br />
Meeting at Promodentis,<br />
Novi Sad: Congress<br />
visitors.
20 <strong>EDI</strong><br />
<strong>EDI</strong> News<br />
20<br />
Christian Berger in a discussion with Vitomir Konstantinovic,<br />
pr<strong>of</strong>essor for oral and maxill<strong>of</strong>acial surgery and oral implantology<br />
at the dental school <strong>of</strong> the University <strong>of</strong> Belgrade.<br />
associations BDIZ <strong>EDI</strong> and UOI-SCG-<strong>EDI</strong> has yielded<br />
very positive results. The membership <strong>of</strong> the Serbian<br />
implantological association has increased markedly<br />
over the past few years.<br />
Conclusions<br />
In addition to the technical and scientific presentations<br />
by internationally renowned speakers, the congress<br />
also <strong>of</strong>fered 60 poster presentations selected<br />
Novi Sad – “New Garden”<br />
The city <strong>of</strong> Novi Sad was founded in the 17 th century<br />
as a settlement <strong>of</strong> traders and craftsmen serving<br />
or working at the close-by military fortress <strong>of</strong><br />
Petrovaradin in the nearby Southern Pannonian<br />
plain. Protected by this fortress, a small settlement<br />
was founded on the left bank <strong>of</strong> the Danube in<br />
1694. The region had become part <strong>of</strong> the Austro-<br />
Hungarian Empire shortly before, in 1687, after the<br />
end <strong>of</strong> the Ottoman rule. In 1748, the citizens gave<br />
their settlement its current name and, on payment<br />
<strong>of</strong> a fee, obtained the status <strong>of</strong> a Free Royal City. In<br />
this manner, Novi Sad became the hub <strong>of</strong> the<br />
mainly agricultural Vojvodina region. The city was<br />
particularly characterized by its multiethnic popu-<br />
The dental fair.<br />
and introduced by a jury consisting <strong>of</strong> three pr<strong>of</strong>essors<br />
representing different specializations within<br />
dentistry. Both the organizers and the participants<br />
considered Promodentis 2008 in Novi Sad a big success.<br />
It is planned to continue the trade show and<br />
congress tradition during the upcoming years. The<br />
dental trade show 2008 had more than 50 exhibitors<br />
and considerably more than 1,500 visitors. A big dental<br />
symposium is being planned for 2009.<br />
Dr Branislav Kardasevic<br />
lation – its inhabitants were Serbs, Hungarians,<br />
Germans, Jews, Slovaks, Ruthenians, Greeks, Armenians<br />
and others. Following World War I and the<br />
defeat <strong>of</strong> the Austro-Hungarian Empire, the region<br />
became part <strong>of</strong> the Kingdom <strong>of</strong> Serbs, Croats, and<br />
Slovenes, and later <strong>of</strong> Yugoslavia. Novi Sad became<br />
the capital <strong>of</strong> the Danube Banovina province, later<br />
known as Vojvodina. Because Novi Sad and environs<br />
are, or were, the site <strong>of</strong> strategically important<br />
bridges across the Danube River and <strong>of</strong> important<br />
petrochemical plants, the city was the target <strong>of</strong><br />
NATO bombardments during the Kosovo war <strong>of</strong><br />
1999. Novi Sad was affected particularly badly, with<br />
bombardments affecting administrative buildings<br />
and TV stations in the city centre; the attack on the<br />
oil refinery released immense amounts <strong>of</strong> poisonous<br />
substances. The destruction <strong>of</strong> the bridges not<br />
only resulted in a complete traffic breakdown, but<br />
also in massive water supply problems. Today, Novi<br />
Sad is predominantly known as a centre <strong>of</strong> Serbian<br />
culture, which is sometimes jocularly dubbed “the<br />
Serbian Athens”.<br />
Miscellaneous sources
The Spanish <strong>Dental</strong> Implant Society (SEI) conducted prospective study<br />
First White Paper<br />
on Implantology<br />
in Spain<br />
Araceli Morales Sánchez, PhD, MD, DDS, President<br />
<strong>of</strong> the Spanish <strong>Dental</strong> Implant Society (SEI)<br />
The Spanish <strong>Dental</strong> Implant Society (Sociedad Española de<br />
Implantes, SEI) has conducted a prospective study on dental<br />
implantology in Spain. The interest in such a publication has<br />
been considerable, given the enormous interest in dental<br />
implants today – not only amongst dental practitioners, but<br />
throughout the entire industry.<br />
Spain appears to have the third highest number <strong>of</strong> dental<br />
implants <strong>of</strong> any <strong>European</strong> country – although it is very difficult<br />
to come up with precise figures. This White Paper, however, has<br />
established some very interesting facts. <strong>Dental</strong> implantology<br />
has significantly changed the way dental clinics work. Implant<br />
treatment has become more widespread and is increasingly<br />
considered the treatment <strong>of</strong> choice.<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Implant treatment is undoubtedly a highly satisfactory therapeutic<br />
modality, <strong>of</strong>fering great clinical benefits to patients and dentists<br />
alike. However, concerns about risks and failures are statistically<br />
greater amongst dental practitioners than normally admitted.<br />
The success rates published in the scientific literature are at<br />
odds with the perceptions generally held by dentists, who <strong>of</strong>ten<br />
report that they are seriously worried. While they perceive<br />
implantology as a safe and prestigious discipline <strong>of</strong>fering great<br />
convenience to patients, they acutely recognize the potential<br />
complications at various stages <strong>of</strong> the treatment. These need to<br />
be carefully assessed, for the sake <strong>of</strong> the patients as well as the<br />
practitioners themselves. The realization that implants can fail<br />
requires the pr<strong>of</strong>ession to take a responsible stance in order to<br />
find appropriate solutions.<br />
While certain postgraduate implantological training courses<br />
are considered excellent, university-level teaching <strong>of</strong> dental<br />
implantology as a whole is generally perceived as inadequate.<br />
Concerns have arisen over the excessive number <strong>of</strong> – not<br />
always well-monitored – courses <strong>of</strong>fered.<br />
This first White Paper on implantology in Spain, to be published<br />
and distributed on request by September, <strong>of</strong>fers a<br />
wealth <strong>of</strong> highly pertinent information, some predictable and<br />
others surprising. The SEI will continue to follow up on the issues<br />
raised in this White Paper in the future. In a highly volatile field,<br />
data and observations can change rapidly, so this study will be a<br />
blueprint for future publications.<br />
We would like to take the opportunity to thank the dental<br />
practitioners who participated in the investigation and the suppliers<br />
who supported the project. Without their help, this project<br />
would have been impossible to carry out.<br />
21
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
The Spanish <strong>Dental</strong> Implant Society (SEI)<br />
conducted prospective study<br />
First White Paper<br />
on Implantology<br />
in Spain<br />
Araceli Morales Sánchez, PhD, MD, DDS,<br />
President <strong>of</strong> the Spanish <strong>Dental</strong> Implant Society (SEI)<br />
The Spanish <strong>Dental</strong> Implant Society (Sociedad Española de Implantes, SEI) has<br />
conducted a prospective study on dental implantology in Spain. The interest<br />
in such a publication has been considerable, given the enormous interest in<br />
dental implants today – not only amongst dental practitioners, but through-<br />
out the entire industry.<br />
21<br />
Spain appears to have the third highest number <strong>of</strong> dental implants <strong>of</strong> any<br />
<strong>European</strong> country – although it is very difficult to come up with precise figures.<br />
This White Paper, however, has established some very interesting facts.<br />
<strong>Dental</strong> implantology has significantly changed the way dental clinics work.<br />
Implant treatment has become more widespread and is increasingly considered<br />
the treatment <strong>of</strong> choice.<br />
Implant treatment is undoubtedly a highly satisfactory therapeutic modality,<br />
<strong>of</strong>fering great clinical benefits to patients and dentists alike. However, concerns<br />
about risks and failures are statistically greater amongst dental practitioners than<br />
normally admitted.<br />
The success rates published in the scientific literature are at odds with the perceptions<br />
generally held by dentists, who <strong>of</strong>ten report that they are seriously worried.<br />
While they perceive implantology as a safe and prestigious discipline <strong>of</strong>fering<br />
great convenience to patients, they acutely recognize the potential complications<br />
at various stages <strong>of</strong> the treatment. These need to be carefully assessed, for<br />
the sake <strong>of</strong> the patients as well as the practitioners themselves. The realization<br />
that implants can fail requires the pr<strong>of</strong>ession to take a responsible stance in<br />
order to find appropriate solutions.<br />
While certain postgraduate implantological training courses are considered<br />
excellent, university-level teaching <strong>of</strong> dental implantology as a whole is<br />
generally perceived as inadequate. Concerns have arisen over the excessive<br />
number <strong>of</strong> – not always well-monitored – courses <strong>of</strong>fered.<br />
This first White Paper on implantology in Spain, to be published and distributed<br />
on request by September, <strong>of</strong>fers a wealth <strong>of</strong> highly pertinent information,<br />
some predictable and others surprising. The SEI will continue to follow<br />
up on the issues raised in this White Paper in the future. In a highly volatile field,<br />
data and observations can change rapidly, so this study will be a blueprint for<br />
future publications.<br />
We would like to take the opportunity to thank the dental practitioners who<br />
participated in the investigation and the suppliers who supported the project.<br />
Without their help, this project would have been impossible to carry out.
22<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Foreword<br />
History <strong>of</strong> the Scientific<br />
Recognition <strong>of</strong> Oral Implantology<br />
When DGZMK, the German umbrella organization for dentistry and dental science, recognized oral implantology as a scientific<br />
discipline on 24 September 1982, implantology had reached the – albeit highly preliminary – end <strong>of</strong> a long and stony path.<br />
Today, many dental clinics are hard to imagine without implant dentistry. For most patients it is the restoration <strong>of</strong> choice; for<br />
many dentists it is an innovative discipline still far from the end <strong>of</strong> its development.<br />
The history <strong>of</strong> BDIZ <strong>EDI</strong> is the history <strong>of</strong> oral implantology.<br />
BDIZ was founded in 1989 by clinical dentists<br />
who, as the BDIZ Expert Manual on Implantology<br />
states, “did not want to watch the development <strong>of</strong><br />
implantology in Germany from the sidelines. Increasing<br />
squabbles concerning indications and payment and<br />
reimbursement issues surrounding implantological<br />
services had greatly displeased them. The lack <strong>of</strong> representation<br />
in and by the dental pr<strong>of</strong>essional bodies<br />
was perceived as a serious deficiency. The evaluation<br />
<strong>of</strong> implantological cases by dental experts unfamiliar<br />
with the new field was also viewed most critically.”<br />
Dr Hans-Jürgen Hartmann <strong>of</strong> Tutzing, co-founder <strong>of</strong><br />
BDIZ <strong>EDI</strong> and its president for many years, reports<br />
about the history <strong>of</strong> the association in good times and<br />
bad – while always striving to achieve free implantology<br />
practiced by free dentists. Things take a less political<br />
turn on page 30. Pr<strong>of</strong>essor Joachim E. Zöller <strong>of</strong> the<br />
University <strong>of</strong> Cologne, BDIZ <strong>EDI</strong> vice president, takes a<br />
Janus view from the standpoint <strong>of</strong> a university teacher<br />
and scientist, not only looking back to the first steps<br />
and the difficulties we were facing but also taking a<br />
glimpse at the future <strong>of</strong> oral implantology.<br />
The famous Tübingen implant – who would be better<br />
suited to report on it than its inventor? Read the<br />
report by Willi Schulte, former pr<strong>of</strong>essor and highly<br />
decorated academic teacher, starting on page 36.<br />
Content<br />
Committed to our tradition – Looking<br />
back on the history <strong>of</strong> the BDIZ <strong>EDI</strong> p. 24<br />
Looking back and looking forward p. 30<br />
The Tübingen implant p. 36
24<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
History <strong>of</strong> the scientific recognition <strong>of</strong> oral implantology<br />
Committed to our Tradition –<br />
Looking Back on the History<br />
<strong>of</strong> the BDIZ <strong>EDI</strong><br />
Dr Hans-Jürgen Hartmann, Founding member <strong>of</strong> the BDIZ <strong>EDI</strong> and<br />
president <strong>of</strong> BDIZ <strong>EDI</strong> from 1993 to 2000<br />
In the early 1980s, oral implantology increasingly had developed into a treatment modality that – as the recognition document<br />
from 1982 described it – “... can be employed as a duly considered alternative to other treatment options...”. The first annual<br />
congress <strong>of</strong> German dental implantologists at Garmisch in southern Bavaria marked the breakthrough for scientific oral<br />
implantology. It was Pr<strong>of</strong>essor Manfred Straßburg <strong>of</strong> the German Society <strong>of</strong> Dentistry and Oral Medicine (Deutsche Gesellschaft<br />
für Zahn-, Mund- und Kieferheilkunde, DGZMK) who first pronounced this scientific recognition.<br />
Oral implantology – developed in clinical dental practice<br />
and predominantly utilized there – gave rise to heated<br />
discussions between dentists in private practice and<br />
their colleagues at the universities. The restorative and<br />
surgical basics we had been taught at the universities<br />
were challenged and modified by oral implantology. We<br />
gained novel insights into masticatory function and the<br />
integration <strong>of</strong> external artifacts into the bone, insights<br />
that we would never have dreamed <strong>of</strong> at dental school.<br />
Implantological topics<br />
were not taken up kindly<br />
As the debate was raging back and forth, the 1988vintage<br />
dental fee schedule was the first to cover<br />
certain implantological services. It became amply clear<br />
at that point that oral implantology was on the verge<br />
<strong>of</strong> becoming an economic factor in clinical dentistry.<br />
As Pr<strong>of</strong>essor Egon Brinkmann wrote in the first issue<br />
<strong>of</strong> the BDIZ yearbook in 1991: “... developments in<br />
implantology have displeased many dentists in private<br />
practice who are active in the field... so that, consequently,<br />
eighteen <strong>of</strong> them assembled in Frankfurt on<br />
30 September 1989 to found the German <strong>Association</strong><br />
<strong>of</strong> Clinical Implantological Dentists as a necessary<br />
and logical consequence <strong>of</strong> the situation.”<br />
The foundation <strong>of</strong> the BDIZ was preceded by copious<br />
conversations, discussions and – sometimes fiery –<br />
debates. It was the managing director <strong>of</strong> SPK Feld-<br />
mühle (later Cerasiv and then CeramTec), Hoch, who<br />
together with Pr<strong>of</strong>essor Brinkmann assembled a group<br />
<strong>of</strong> kindred spirits to sound out the possibility <strong>of</strong><br />
founding an implantological association for dentists in<br />
private practice. Ultimately, a number <strong>of</strong> fellow dentists<br />
joined the ranks, mostly dentists who also worked as<br />
consultants for SPK Feldmühle.<br />
In those turbulent times, when the founding <strong>of</strong> the<br />
association was noted, it was largely dismissed as yet<br />
another implantological society. But this was a misunderstanding,<br />
as the BDIZ did not intend to estab-<br />
Dr Hans-Jürgen<br />
Hartmann<br />
The BDIZ founders (left to right): Dr Rüdiger Oeltermann, Dr Rolf Brandau, Dr Rolf<br />
Briant, Bernd Hölscher, Dr Uwe Ryguschik-Ott, Dr Helmut B. Engels, Pr<strong>of</strong> Egon Brink -<br />
mann, Dr Hans-Joachim Habermehl, Dr Stephan Hausknecht, Dr Hans-Jürgen Hartmann,<br />
Dr Werner Hotz, Dr Heiner Jacoby, Dr Ulrich Kümmerle, Dr Hans-Joachim Foet<br />
and Dr Lothar Winkler.
26<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
lish itself as another scientific society; rather, the goal<br />
was to represent dentists’ political and legal interests.<br />
These interests were hardly, if at all, looked after by<br />
the scientific societies. Issues related to pr<strong>of</strong>essional<br />
law or to fee structures were left to the various State<br />
Chambers <strong>of</strong> Dentists, as they didn’t have any room<br />
within the self-image <strong>of</strong> the scientific societies.<br />
Clear separation between<br />
science and pr<strong>of</strong>essional law<br />
It was a time <strong>of</strong> changes. The large scientific societies,<br />
GOI, AGI and DGZI, were talking mergers. Led by<br />
Pr<strong>of</strong>essor Hubertus Spiekermann, GOI and AGI were<br />
united to form the German Society for Implantology<br />
(Deutsche Gesellschaft für Implantologie, DGI) in 1994.<br />
The small and closely intertwined group <strong>of</strong> leaders <strong>of</strong><br />
the various associations and societies has developed<br />
trustful relationships, a good prerequisite for mergers<br />
and cooperative ventures. A clear separation between<br />
scientific aspects and legal aspects increased the<br />
relative importance <strong>of</strong> the BDIZ, which continued<br />
attracting new members.<br />
For example, BDIZ was instrumental in reopening<br />
the communication channels between maxill<strong>of</strong>acial<br />
surgeons and oral surgeons, ultimately getting them<br />
to return to one table and talk. The political environment<br />
developed in the way that favoured the BDIZ,<br />
with the result that the separation <strong>of</strong> responsibilities<br />
– scientific and legal – was accepted and supported<br />
by the scientific societies. BDIZ became the mouthpiece<br />
<strong>of</strong> all oral implantologists in all matters concerning<br />
pr<strong>of</strong>essional law, insurance politics and fees<br />
and fee schedules.<br />
BDIZ provides an implantological<br />
interpretation <strong>of</strong> the GOZ<br />
The first implantological interpretation <strong>of</strong> the German<br />
fee schedule for dentists, GOZ, was <strong>of</strong>fered by the BDIZ<br />
and ultimately accepted, to a great extent, by the<br />
State Chambers <strong>of</strong> Dentists, even if not without many<br />
rounds <strong>of</strong> discussions and attempts at persuasion. A<br />
committee <strong>of</strong> experts was formed. Also, expert symposia<br />
and lists <strong>of</strong> experts as well as information conferences<br />
for lawyers were conceived and implemented<br />
in collaboration with the Chambers <strong>of</strong> Dentists in order<br />
to spread the implantological expertise. It was also<br />
planned to collect expert opinions, legal decisions and<br />
other pertinent documents. Lastly, it was proposed to<br />
let member dentists contact legal counsel via the BDIZ<br />
to resolve differences with insurance funds and companies<br />
related to dental fee. This idea continues to be<br />
an important one to the state, and the legal firm <strong>of</strong><br />
Ratajczak and partners has implemented the concepts<br />
devised by the BDIZ board at the time.<br />
The struggle by clinical implantologists to have this<br />
services accepted within the framework <strong>of</strong> fee schedules<br />
became more intense, and the fight against<br />
insurance companies became harder. The Contract<br />
Committee, a primary contact point for dentists seeking<br />
fee-related information, was established; it soon<br />
became an important part <strong>of</strong> the BDIZ’s consultancy<br />
work for the benefit <strong>of</strong> all dentists.<br />
Increasing polemics prompted the BDIZ board to<br />
make the insurance companies join in an attempt to<br />
arrive at a common interpretation <strong>of</strong> the fee schedule.<br />
A practical solution was found after many rounds <strong>of</strong><br />
discussion, but unfortunately it never gained the<br />
support <strong>of</strong> the Chambers <strong>of</strong> Dentists nor, ultimately,<br />
<strong>of</strong> the insurance companies themselves, rendering<br />
the labours <strong>of</strong> three years obsolete. But at any rate, the<br />
discussions brought a measure <strong>of</strong> clarity regarding the<br />
concepts embraced by private insurance companies,<br />
concepts that were communicated to the members.<br />
Implantological schedule <strong>of</strong> fees<br />
The idea to develop a separate implantological schedule<br />
<strong>of</strong> fees devised by experts had been born early. It was<br />
ultimately relayed to Germany’s main body <strong>of</strong> dentists,<br />
the German <strong>Dental</strong> <strong>Association</strong> (Bundeszahn ärzte kammer,<br />
BZÄK) by the Baden-Württemberg Chamber <strong>of</strong><br />
Dentists and Dr Peter Kutruff. Working closely with the<br />
legal firm <strong>of</strong> Ratajczak and partners, a managed-care<br />
system with a consolidated schedule <strong>of</strong> fees for oral<br />
implantology was devised, based not least on economic<br />
necessities.<br />
It was quickly noticed that implant quality was giving<br />
dentists trouble. Implants or screws would fracture,<br />
marginal fit was poor, allegedly matching parts would<br />
not fit and so on. This realization caused the BDIZ to<br />
install a Quality and Registration Committee that<br />
worked with the Fraunh<strong>of</strong>er Institute in Freiburg to<br />
define specific quality criteria for dental implants.<br />
The various implant systems were to be tested, at<br />
considerable effort, to test implants for quality under<br />
comparable conditions using neutral test setups. It<br />
did get to the point where the first actual tests were<br />
performed. However, as the <strong>European</strong> Union was<br />
introducing its CE mark at the same time, these landmark<br />
efforts were unfortunately not continued. A<br />
reaction to these developments was the foundation<br />
<strong>of</strong> the <strong>Association</strong> <strong>of</strong> German <strong>Dental</strong> Manufacturers<br />
(Verband der Deutschen <strong>Dental</strong>-Industrie, VDDI).<br />
Pr<strong>of</strong> Dr Dr<br />
Hubertus<br />
Spiekermann
28<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
The BDIZ has never shied away from vehemently<br />
and committedly enacting and defending its decisions,<br />
arrived at in lengthy internal discussions,<br />
against insurance companies, courts, manufacturers,<br />
but also dentists in blatant violation <strong>of</strong> the law with<br />
regard to fee or quality issues.<br />
Focus <strong>of</strong> pr<strong>of</strong>essional activities:<br />
Oral implantology<br />
Minimal implantological education activities in the<br />
1980s and the resistance and delaying tactics on the<br />
part <strong>of</strong> some universities with regard to implantological<br />
curriculum necessitated a different education<br />
and training approach. The underlying framework for<br />
this was created in the early 1990s and integrated<br />
into the work <strong>of</strong> the Committee for Postgraduate and<br />
Continuing Education.<br />
Parallel to this, the possibility was investigated to<br />
organizationally link these education activities to the<br />
State Chambers <strong>of</strong> Dentists, and it was even considered<br />
to take to the courts if no support was forthcoming.<br />
Oral implantology as a formal “focus <strong>of</strong> pr<strong>of</strong>essional<br />
activities” – a German concept denoting a<br />
practical pr<strong>of</strong>essional specialization – met with<br />
resistance on the part <strong>of</strong> the Chambers until a court<br />
broke the impasse in 2001. With the assistance <strong>of</strong><br />
selected dentists, who received discreet support, this<br />
political decision had been fought all the way to the<br />
highest court. It was an unfortunate fact that the<br />
“focus <strong>of</strong> pr<strong>of</strong>essional activities” concept was not to<br />
the liking <strong>of</strong> the Chambers. It had been made amply<br />
clear during the negotiations that the lawsuit would<br />
be withdrawn in the event that the Chambers<br />
acknowledged the focus <strong>of</strong> pr<strong>of</strong>essional activities<br />
status for oral implantology under the conditions<br />
that prevail today. The Chambers felt themselves<br />
under pressure and responded negatively.<br />
The decision <strong>of</strong> the highest court provoked a storm<br />
<strong>of</strong> a magnitude that we as initiators had not expected.<br />
It must be admitted that the Chambers <strong>of</strong> Dentists<br />
were right in some <strong>of</strong> their misgivings. On the other<br />
hand, the Chambers themselves proposed and evaluated<br />
so many different terms, titles, focus designations<br />
and similar that the result was an unhealthy proliferation<br />
in terms <strong>of</strong> both terminology and content, a<br />
development which still continues today.<br />
Once it became clear how the courts would view<br />
the “focus <strong>of</strong> pr<strong>of</strong>essional activities” discussion, BDIZ<br />
took the initiative and started calling for a consensus<br />
conference. The many excellent personal contacts with<br />
other associations ultimately made it possible, after<br />
many rounds <strong>of</strong> negotiation, to unite all scientific<br />
societies, including the maxill<strong>of</strong>acial surgeons, within<br />
that consensus conference, with the objective <strong>of</strong> a<br />
common education, a common curriculum, a common<br />
teaching staff and so on. The inflationary number <strong>of</strong><br />
congresses was seen just as critically as today. Their<br />
number was to be reduced, cooperative efforts with
Pr<strong>of</strong> Dr Egon<br />
Brinkmann<br />
manufacturers were to be undertaken, and, finally, a<br />
level <strong>of</strong> harmonization was aspired with regard to<br />
the issues addressed by the scientific societies.<br />
The consensus conference had as its goal to speak<br />
for all implantological associations, first with regard<br />
to specialist training and later, if sufficient agreement<br />
could be reached, with regard to legal as well as scientific<br />
issues. The entire consensus conference was to be<br />
placed under the auspices <strong>of</strong> the DGZMK – together<br />
with all scientific and pr<strong>of</strong>essional societies.<br />
BDIZ had meanwhile grown to the point where it<br />
became possible to engage in fruitful landmark discussions<br />
with insurance companies and the State<br />
Chambers <strong>of</strong> Dentists. It was our strength in numbers<br />
more than anything else that brought this about.<br />
The Bologna process in the <strong>European</strong> Union, court<br />
decisions on the <strong>European</strong> level and the increasing<br />
political importance <strong>of</strong> the <strong>European</strong> institutions<br />
required a <strong>European</strong> reorientation on the part <strong>of</strong><br />
BDIZ, which added “<strong>European</strong> <strong>Association</strong> <strong>of</strong> <strong>Dental</strong><br />
<strong>Implantologists</strong>” (<strong>EDI</strong>) to its name. The term “scientific<br />
society” was included in the BDIZ <strong>EDI</strong> statutes, putting<br />
it on the same level as the other associations – but<br />
still with the traditional political orientation.<br />
So over the years, the small group <strong>of</strong> 18 dentists<br />
became a fully-fledged association that lacks in nothing<br />
an association needs: its own <strong>of</strong>fice, its publications<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
BDIZ konkret and <strong>EDI</strong> Journal, PR activities, legal support<br />
by a specialized legal adviser and not least annual<br />
congresses that, in addition to matters <strong>of</strong> pr<strong>of</strong>essional<br />
law, now also cover scientific subjects. Recommen -<br />
dations are being issued and international contacts<br />
are being made to <strong>European</strong> scientific and political<br />
associations.<br />
As a founding member, current board member and<br />
past president guiding the association between 1993<br />
and 2000, I would like to take the opportunity to<br />
thank our founder, Pr<strong>of</strong>essor Egon Brinkmann, for his<br />
support. Yet no single person made BDIZ <strong>EDI</strong> what it<br />
is today – but the community <strong>of</strong> those who were<br />
driven by the idea to get something done for the<br />
benefit <strong>of</strong> implantological dentists in private practice.<br />
Thanks are also due to Dr Helmut Engels for his tireless<br />
support and I particularly want to point out that he<br />
contributed personal resources to help BDIZ in times<br />
<strong>of</strong> financial need.<br />
We shied away from no argument. We were afraid<br />
<strong>of</strong> no dispute to promote our common views. It is<br />
clear that the air was not always free <strong>of</strong> tension, and<br />
a tremendous amount <strong>of</strong> discussions was required. I<br />
wish the new president and all those who come after<br />
him the best <strong>of</strong> luck in his <strong>of</strong>fice. I would like to see<br />
BDIZ <strong>EDI</strong> to continue its activities in the energetic<br />
spirit <strong>of</strong> recent years, despite all resistance and all<br />
political hardships, in order to fight for our common<br />
goal: free implantology practiced by free dentists.<br />
29
30<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
History <strong>of</strong> the scientific recognition <strong>of</strong> oral implantology<br />
Pr<strong>of</strong> Joachim E. Zöller<br />
Numerous dentists performing implant treatments<br />
today had not even completed their pr<strong>of</strong>essional<br />
training back in 1982. They are hardly aware <strong>of</strong> the<br />
pioneers who were active at the time, except maybe<br />
from references in various publications. Some dentists<br />
in Germany engaged in dental implantology as<br />
early as 30 or 40 years ago. Pr<strong>of</strong>essor Schulte was<br />
instrumental in promoting recognition <strong>of</strong> dental<br />
implantology by the scientific community. Pr<strong>of</strong>essor<br />
Schulte spearheaded the establishment <strong>of</strong> a dedicated<br />
research institute at the University <strong>of</strong> Tübingen.<br />
The results <strong>of</strong> a multicentre study involving twelve<br />
German universities prepared the ground for dental<br />
implantology becoming a certified discipline <strong>of</strong> dental<br />
science in 1982. As a result, dentists <strong>of</strong>fering<br />
implant treatments were no longer deemed to use<br />
an “unorthodox” approach. Instead, they were<br />
regarded as <strong>of</strong>fering their patients a treatment<br />
modality that was acknowledged as state <strong>of</strong> the art,<br />
both technologically and scientifically.<br />
Aluminium oxide implants and TPS coating<br />
Quite some things have changed in these 25 years.<br />
Aluminium oxide implants were formerly produced<br />
by Friedrichsfeld (today Friadent) or SPK Feldmühle<br />
(whose successor systems are being distributed by<br />
Dentaurum). In addition, the late 1980s saw the<br />
emergence <strong>of</strong> the IMZ system, which became established<br />
as one <strong>of</strong> the most popular systems. Designs<br />
featuring an absorbing element to imitate natural<br />
Looking Back and<br />
Looking Forward<br />
Pr<strong>of</strong>essor Joachim E. Zöller<br />
The German Society <strong>of</strong> Dentistry and Oral Medicine (Deutsche<br />
Gesellschaft für Zahn-, Mund- und Kieferheilkunde, DGZMK) has tradi-<br />
tionally issued reviews <strong>of</strong> current practice. The latest revision, Version<br />
3.0 was published in 2005. This version number reveals that few<br />
groundbreaking changes requiring documentation by scientific stan-<br />
dards have occurred ever since the publication <strong>of</strong> reviews <strong>of</strong> current<br />
practice was first introduced.<br />
tooth mobility were advocated for a long time. More<br />
than a million implants were based on this principle.<br />
Meanwhile, studies have demonstrated that the use<br />
<strong>of</strong> “wearing parts” is not essential to the development<br />
and long-term preservation <strong>of</strong> highly stable<br />
implant-bone interfaces. As a result, few superstructures<br />
continue to be supported by mobile implant<br />
designs.<br />
The surface debate<br />
With the introduction <strong>of</strong> the IMZ system, implant<br />
surfaces treated with a titanium plasma spray (TPS)<br />
started to be widely used. For the first time, a microtextured<br />
implant surface was available <strong>of</strong>fering predictable<br />
success even in situations <strong>of</strong> reduced bone<br />
quality. Today, however, we are struggling with a legacy<br />
<strong>of</strong> peri-implantitis, as this kind <strong>of</strong> surface greatly<br />
favoured the accumulation <strong>of</strong> bacteria and osteo -<br />
blasts in its niches and crypts.<br />
It was not until 15 years after these implants had<br />
been recognized by the scientific community that<br />
the initial success rates could be substantially<br />
improved. Osseointegration was made predictable by<br />
high-temperature etching and sandblasting <strong>of</strong> the<br />
implant surfaces.<br />
Other attempts at optimizing success in reduced<br />
bone showed good initial results, but they were associated<br />
with increased failure rates in the presence <strong>of</strong><br />
inflammation. As a result, few implant systems today<br />
continue to rely on hydroxyapatite-coated surfaces.
32<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Immediate loading<br />
vs. time-efficient treatment<br />
Competition increased as other manufacturers<br />
emerged. Much was made <strong>of</strong> the effectiveness <strong>of</strong> different<br />
surface types in the ensuing campaigns. These<br />
were designed to reach not only the dentists responsible<br />
for treatment decisions, but marketing efforts were<br />
also targeted directly at the patients. Today, the controversy<br />
has largely abated. Surfaces treated by sandblasting<br />
and high-temperature etching have become<br />
something <strong>of</strong> a standard. Their use can be considered<br />
the state <strong>of</strong> the art in the quest for osseointegration.<br />
Any newly developed surfaces will have to stand the<br />
test <strong>of</strong> time, which is not going to be easy given the<br />
very high success rates already on record.<br />
Competing manufacturers, but also implantologists,<br />
have instead embarked on a race for shorter<br />
healing periods and ways <strong>of</strong> <strong>of</strong>fering patients the<br />
benefits <strong>of</strong> immediate restoration. Extensive debates<br />
about these issues are a relatively new phenomenon,<br />
having started only five to seven years ago. Once<br />
again, however, they are based on the efforts and<br />
experience <strong>of</strong> dentists such as Dr Ledermann, who successfully<br />
used a bar design for the immediate restoration<br />
<strong>of</strong> implants 30 years ago. Some <strong>of</strong> the original<br />
techniques have fallen into oblivion, either because<br />
the system components available at the time would<br />
not allow the spectrum <strong>of</strong> indications to be increased<br />
or because the available implants did not have the<br />
properties required for immediate restoration.<br />
Furthermore, any expectations <strong>of</strong> immediately<br />
restoring all implants have turned out to be over -<br />
enthusiastic and are clearly being reconsidered today.<br />
Reduced healing periods <strong>of</strong> six to eight weeks <strong>of</strong>ten do<br />
not justify the extra effort that is required for immediate<br />
restoration. Even temporary restorations can <strong>of</strong>fer<br />
good patient comfort today. Current scientific evidence<br />
on the subject was summarized at the 1 st <strong>European</strong><br />
Consensus Conference <strong>of</strong> the BDIZ <strong>EDI</strong> in 2006.<br />
Challenges in the maxillary<br />
posterior segment<br />
Continuous progress has been made over the past<br />
25 years with regard to treatment options. The first<br />
implants were placed in the maxillary anterior segment<br />
(using the Tübingen implants for immediate<br />
placement) or to support a bar in the mandible<br />
(using titanium implants). These original indications<br />
were followed by maxillary restorations supported by<br />
implants, whose insertion was guided by the principle<br />
<strong>of</strong> utilizing existing bone. Prosthetic handling<br />
became extremely difficult when implants were<br />
inserted in the tuberosity region. Some fellow den-<br />
TPS-coated IMZ implant afflicted with peri-implantitis. A large bone defect is present<br />
on the lingual aspect.<br />
Polarized-light micrograph <strong>of</strong> an<br />
osseointegrated implant. Note the<br />
structure <strong>of</strong> collagen fibers.<br />
Tübingen implant replacing tooth 12.<br />
The radiograph was obtained three<br />
years after prosthetic restoration.<br />
tists lost faith in their manual skills. As augmentation<br />
procedures became established, the era when only<br />
the available bone was utilized gave way to a new era<br />
<strong>of</strong> bone enhancement for implant placement.<br />
Especially in the maxillary posterior region, sinus<br />
floor elevation and augmentation have become an<br />
established procedure recognized by the scientific community.<br />
Surgical access is established by lateral fenestration<br />
and elevation <strong>of</strong> the Schneiderian membrane.<br />
Most authors have used essentially the same approach.<br />
However, very different materials have been used for<br />
sinus filling. Ancillary measures to support wound heal-
34<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Insertion <strong>of</strong> four XiVE-TG implants following augmentation with a free<br />
bone graft harvested from the iliac crest. These implant surfaces are<br />
preconditioned by sandblasting and high-temperature etching.<br />
ing have also varied widely. Meanwhile, approaches<br />
relying on platelet-rich plasma (RPR) in combination<br />
with (autologous, allogeneic or xenogeneic) bone<br />
replacement material have mostly given way to simpler<br />
approaches using microporous bone substitutes based<br />
on hydroxyapatite or tricalcium phosphate.<br />
Augmentation for alveolar<br />
ridge reconstruction<br />
A whole range <strong>of</strong> augmentation techniques to treat<br />
jaw defects have been developed over the past two<br />
decades. Lateral defects can now be treated with<br />
hardly any problems. Important procedures include<br />
bone spreading, bone splitting or guided tissue<br />
regeneration (GTR). New materials and membranes<br />
for GTR are periodically introduced, but they have yet<br />
to succeed in lowering the risks <strong>of</strong> infection and failure<br />
in a significant way. When it comes to the treatment<br />
<strong>of</strong> vertical defects, the highest success rates<br />
have been obtained with autologous bone grafts<br />
(usually harvested from mandibular bone) and by<br />
vertical distraction osteogenesis.<br />
Even advanced cases <strong>of</strong> bone resorption or bone<br />
defects can today be restored to integrity. Extended<br />
techniques <strong>of</strong> reconstruction are used for this purpose,<br />
based on free bone grafts harvested from the<br />
iliac crest. This technique has come to <strong>of</strong>fer predictably<br />
stable results and a low complication rate.<br />
Patients must be prepared, however, to undergo<br />
various surgical interventions that are associated<br />
with individual morbidity. Alternatively, conservative<br />
and cost-effective restorations can be achieved in<br />
some patients, depending on individual conditions<br />
and expectations, by using minimally invasive techniques<br />
such as reduced-diameter implants.<br />
Computer-assisted planning for six Templant implants in the maxilla,<br />
using Galileos s<strong>of</strong>tware (Sirona).<br />
3D diagnostics and implementation<br />
Three-dimensional diagnostics for computer-assisted<br />
template fabrication has been greatly refined over the<br />
past few years. Some systems have reached a level <strong>of</strong><br />
radiation exposure comparable to that incurred with<br />
conventional x-ray films, while <strong>of</strong>fering abundant<br />
information on the entire facial skull. As a result, the<br />
need for extensive mucoperiosteal flaps must be<br />
reconsidered. What used to be a strict requirement is<br />
no longer mandatory for implant placement. Patients<br />
benefit from this development by considerably lower<br />
levels <strong>of</strong> postoperative symptoms.<br />
In this way, the original concept <strong>of</strong> implant planning<br />
by “bone searching” has been revived. Care is<br />
taken to utilize existing bone by deliberate angular<br />
placement <strong>of</strong> implants. Implants inserted in this way<br />
along anatomical structures have been shown to<br />
<strong>of</strong>fer good biochemical stability. Thanks to the large<br />
prosthetic surface areas, only few implants are needed<br />
to support fixed restorations.<br />
Zirconia for implants<br />
Furthermore, these past few years have seen a rediscovery<br />
<strong>of</strong> ceramic materials for oral implants. Ceramics<br />
are known to yield good results for conventional<br />
prosthetic superstructures. Most manufacturers<br />
have succeeded in <strong>of</strong>fering all-ceramic abutments,<br />
although the designs vary.<br />
One-piece zirconia implants require pertinent<br />
experience with the concept <strong>of</strong> immediate restoration.<br />
Without protection by a temporary restoration,<br />
successful osseointegration cannot be achieved. The<br />
use <strong>of</strong> zirconia has significantly improved the<br />
mechanical stability <strong>of</strong> ceramic implants as com-
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Osseointegrated whiteSky implant (bredent) prior to delivering the final<br />
restoration.<br />
pared to the formerly used alumina implants. Zirconia<br />
also has more favourable aging properties. However,<br />
these new ceramic implants are applied very differently<br />
from the concept used in the early days <strong>of</strong><br />
scientific implantology. Highly experienced treatment<br />
teams are required. Their members need to<br />
understand the principles <strong>of</strong> bone-adaptive implant<br />
bed preparation and <strong>of</strong> delivering a temporary<br />
restoration (ideally at the end <strong>of</strong> surgery) for implant<br />
stability. Current scientific evidence on this subject<br />
was summarized at the 2 nd <strong>European</strong> Consensus Conference<br />
<strong>of</strong> the BDIZ <strong>EDI</strong> in 2007.<br />
Summary<br />
To summarize, 25 years <strong>of</strong> scientific implantology in<br />
Germany have been guided by the interaction <strong>of</strong> clinicians,<br />
universities and industry. Not all ideas have<br />
stood the test <strong>of</strong> time. Some <strong>of</strong> them failed despite<br />
enthusiastic propagation and marketing. In a similar<br />
vein, not all innovations presented in recent years<br />
were entirely new. Some <strong>of</strong> them had been used previously<br />
in some form or another. For the next 25 years,<br />
we hope for gentle progress in oral implantology. The<br />
range <strong>of</strong> treatment options available to implantologists<br />
should ensure successful outcomes and patient<br />
satisfaction. Future progress should be based on solid<br />
and responsible product development. Dependable<br />
scientific foundations should be established at universities<br />
and available for application in daily clinical<br />
practice.<br />
35
36<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
History <strong>of</strong> the scientific recognition <strong>of</strong> oral implantology<br />
The Tübingen Implant<br />
Pr<strong>of</strong>essor emeritus Willi Schulte<br />
The recognition <strong>of</strong> oral implantology by the German scientific community – German Socie-<br />
ty <strong>of</strong> Dentistry and Oral Medicine (Deutsche Gesellschaft für Zahn-, Mund- und Kiefer-<br />
heilkunde, DGZMK) – was significantly promoted by the results <strong>of</strong> basic scientific and<br />
applied research in Tübingen over the years 1973 to 1982. The true impetus for this activity<br />
came from an opening-ceremony lecture at the 1972 DGZMK annual conference. Its topic,<br />
“science and clinical practice”, was focused on oral implantology. Its conclusion was that<br />
numerous empirical efforts were being made in clinical practice, creating an urgent need<br />
for university-level research institutes to make scientific efforts toward establishing foun-<br />
dations in implantology [DZZ 28.337 (1973)].<br />
An opportunity arose in 1973 and 1974. The Tübingen<br />
Institute for <strong>Dental</strong> Surgery and Periodontology,<br />
headed by this author, established contact with<br />
physicist Dr G. Heinke, who was then director <strong>of</strong><br />
research at Friedrichsfeld GmbH (later renamed Fria -<br />
tec, today Friadent). German implantology is greatly<br />
indebted to that man. No other name than his will be<br />
mentioned in this article.<br />
The Baden-Württemberg Ministry <strong>of</strong> Economic<br />
Affairs had invited bids for a 5-year interdisciplinary<br />
research program aiming to promote the state’s<br />
ceramics industry with a view to creating jobs. Collaboration<br />
between identified study groups was<br />
required. Disciplines included dentistry, veterinary<br />
medicine, material research and biometrics. Participation<br />
<strong>of</strong> industry was also required. A completely<br />
new product had to be developed. Titanium and aluminium<br />
oxide ceramics had been used for endoprosthetic<br />
applications. Some experience with their use<br />
had also been collected in dental implantology. The<br />
invitation for bids was embraced by this author.<br />
The new paradigm<br />
Back then, dental implant systems were used solely<br />
to restore edentulous jaw segments. In the 1950s and<br />
1960s, we gathered comprehensive experience in<br />
pre-prosthetic surgery, aiming to eliminate the damage<br />
inflicted by tissue-supported dentures. Frustration<br />
had developed in face <strong>of</strong> dissatisfying long-term<br />
results. It was our ambition to develop a completely<br />
new implant system. The goal was<br />
to prevent disuse atrophy <strong>of</strong> the<br />
alveolar ridge following tooth loss<br />
Willi Schulte, former pr<strong>of</strong>essor and<br />
with the possible consequence <strong>of</strong><br />
highly decorated academic teacher.<br />
edentulous jaw segments. Achieving<br />
this goal required continuous loading <strong>of</strong> the bone<br />
by placing an implant either immediately after tooth<br />
loss or soon thereafter. Another objective was that<br />
the newly developed implant should be capable <strong>of</strong><br />
replacing single teeth even in adolescents, for example<br />
after trauma-induced loss <strong>of</strong> anterior teeth. A randomized<br />
study was planned to test implants that<br />
were identical in shape but were fabricated from aluminium<br />
oxide or titanium.<br />
While the ministry accepted the new paradigm as worthy<br />
<strong>of</strong> sponsoring, the use <strong>of</strong> titanium was rejected. The<br />
following new requirements were added for approval:<br />
• For application in humans, it had to be ensured<br />
that no permanent damage was inflicted in the<br />
event <strong>of</strong> treatment failure.<br />
• Patients were not allowed to be charged any fees<br />
for the duration <strong>of</strong> public sponsoring.<br />
• The Tübingen institute was not allowed to employ<br />
any other implant systems for the duration <strong>of</strong><br />
public sponsoring.<br />
• Conventional techniques had to be employed for<br />
the superstructures (e.g. tooth-supported restorations<br />
or dowel crowns).<br />
• The implant manufacturer was barred from introducing<br />
the product on the market before five<br />
years into the research program.
38<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Implementation and design<br />
Some <strong>of</strong> these limitations were disadvantageous,<br />
most importantly those concerning the planned randomized<br />
study. However, it was still our goal to<br />
secure public sponsoring, as the university budget<br />
did not cover our need for human and technical<br />
resources. A number <strong>of</strong> German institutions took<br />
part in developing the “Tübingen implant”: the Institute<br />
for Medical Biometrics in Tübingen; the Institute<br />
<strong>of</strong> Pathology (and animal farm) at the University <strong>of</strong><br />
Heidelberg; the Fraunh<strong>of</strong>er Institute for Mechanics <strong>of</strong><br />
Materials in Freiburg, the Max Planck Institute for<br />
Metal Research in Stuttgart; and the development<br />
department <strong>of</strong> Friedrichsfeld GmbH in Mannheim.<br />
In the 1960s, extensive investigations <strong>of</strong> periodontal<br />
histology had been performed in Tübingen. Other studies<br />
had focused on oral wound healing and specific<br />
hematological reactions for bone regeneration. The<br />
results <strong>of</strong> these studies went into the implant body<br />
design. For a comprehensive overview <strong>of</strong> the research<br />
program, the reader is referred to ZM 74 (19/20), 1981 and<br />
Quint Int 15: 2267, 1984. Numerous references are <strong>of</strong>fered<br />
in these sources. Following basic anatomical studies,<br />
plans for implant placement were originally confined to<br />
specific jaw segments (sites 15 to 25, 34 to 44).<br />
The transmucosal implant element was polished<br />
to a high gloss. In addition to reducing plaque accumulation,<br />
this surface treatment was intended to<br />
ensure the organismic principle <strong>of</strong> ectodermal<br />
integrity in the transmucosal area. In natural teeth,<br />
this integrity is ensured by hemidesmosomal attachment<br />
<strong>of</strong> the inner junctional epithelium to the<br />
cementoenamel junction. However, lack <strong>of</strong> such<br />
attachment can remain without consequences for<br />
decades in the presence <strong>of</strong> recessions because the<br />
epithelium will also become attached to the very<br />
smooth mesodermal cementum.<br />
Based on previous haematological findings about<br />
blood-clot attachment, the enossal surface was blasted<br />
with aluminium oxide particles. The resultant<br />
microtexture was characterized by peaks and valleys<br />
<strong>of</strong> 1 to 5 μm, causing the coagulation and attachment<br />
<strong>of</strong> blood to aluminium oxide surfaces in a matter <strong>of</strong><br />
seconds. Connection was established down to the<br />
molecular level, meeting the quintessential requirement<br />
for speedy organization <strong>of</strong> endosteal tissue!<br />
Both principles were implemented for the first<br />
time and have since been adopted by almost all<br />
implant manufacturers, most notably in recent systems.<br />
Incidentally, the effect <strong>of</strong> surface roughness on<br />
final strength really continues to be an open question.<br />
This conclusion was drawn after we measured<br />
the osseointegration <strong>of</strong> different implant systems in<br />
vivo using the Periotest system.<br />
The implant body was designed<br />
as a conical step cylinder. This<br />
shape was based on the consideration<br />
that implants cannot – as<br />
natural teeth can – introduce<br />
loads into the cranial skeleton by<br />
a push-pull transformation within<br />
the periodontium. Most <strong>of</strong><br />
today’s implants are designed<br />
with threads. However, the ethical<br />
requirements defined by the state<br />
ministry precluded the use <strong>of</strong><br />
threads, since they would have<br />
involved bone loss in the event <strong>of</strong><br />
treatment failure. Rather than<br />
threads, the implant body was<br />
designed to feature lacunae, initially filling with<br />
blood and later with bone. The gross surface (not<br />
including the microstructure) was generally around<br />
55 to 65 percent larger than the surface <strong>of</strong> a natural<br />
root.<br />
The results obtained in animal experiments were<br />
so excellent that, as soon as 1978, the Tübingen/Heidelberg<br />
group won the DGZMK award for<br />
best performance <strong>of</strong> the year. Optimal results were<br />
even obtained in clinical studies, despite entering<br />
uncharted territory. A number <strong>of</strong> rules (frequently<br />
disregarded or highly controversial ever since) were<br />
considered essential. Care was taken to preserve the<br />
marginal gingiva with its fibrous structure and inner<br />
junctional epithelium, requiring careful handling <strong>of</strong> a<br />
periotome to separate the periodontal ligament. Any<br />
reduction <strong>of</strong> the facial alveolar wall and bony interdental<br />
septa was strictly avoided. Instead, the<br />
implant bed was palatally relocated (in relation to<br />
the alveolar axis) and cranially deepened. Finally, an<br />
undisturbed healing period <strong>of</strong> three months was<br />
observed prior to loading the implants.<br />
Excellent statistical results were also obtained. As a<br />
result, another eleven universities agreed to take part<br />
in the clinical studies. These collaborations started in<br />
1977 and were followed up by annual symposia in<br />
Tübingen.<br />
After the phase <strong>of</strong> sponsoring by the Baden-Württemberg<br />
State Ministry <strong>of</strong> Economic Affairs had<br />
ended and Frialit-1 had been introduced in the<br />
market, the German Research Society (Deutsche For -<br />
schungs gesellschaft, DFG) created an opportunity<br />
for the study groups to continue their work. The<br />
research objectives were considerably broadened.<br />
Led by the author, a dedicated research institute was<br />
launched and maintained from 1984 to 1996. Being<br />
the largest effort <strong>of</strong> its kind worldwide, this initiative<br />
The Tübingen<br />
implant.
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
produced over 500 interdisciplinary publications<br />
and countless lectures. Among other findings, these<br />
efforts revealed that aluminium oxide implants susceptible<br />
to fatigue fracture after ten to 15 years in<br />
service, thus defeating original assumptions concerning<br />
their longevity. This realization led to the<br />
development <strong>of</strong> Frialit-2 titanium implants with prefabricated<br />
abutments (Z Zahnärztl Implantol 8: 77-<br />
96, 1992). The dimensions used in the Frialit-1 system<br />
were retained. Threads were now used, some <strong>of</strong><br />
them being extremely flat “bone-saving” designs.<br />
They were introduced (when the limitations<br />
imposed by the state ministry were no longer in<br />
place) because sporadic cases <strong>of</strong> implant rejection<br />
had routinely occurred with the original step cylinders,<br />
due to the organizational pressure occurring in<br />
the first ten days.<br />
Outlook<br />
The first English-language report on the Tübingen<br />
implant was published in 1984. What followed was<br />
an unprecedented surge <strong>of</strong> single-tooth implants<br />
around the world. They have changed the face <strong>of</strong><br />
dentistry like no other development before. Nevertheless,<br />
our own investigations and long-term follow-ups<br />
(over more than 30 years) have revealed that<br />
the highest levels <strong>of</strong> mucosal compatibility and lowest<br />
rates <strong>of</strong> peri-implantitis are reached with ceramic<br />
implants. This observation prompted our own study<br />
group within the research institute to develop an<br />
implant surface with a titanium enossal segment<br />
and a ceramic transmucosal segment. Material<br />
researchers developed a special procedure <strong>of</strong> welding<br />
the ceramic material to the transmucosal “collar”.<br />
Good results were obtained in animal studies. Unfortunately,<br />
these efforts were abandoned when the<br />
research institute was discontinued in 1996.<br />
Even at the time, our study groups would discuss<br />
the use <strong>of</strong> all-zirconia implants. Designs <strong>of</strong> this type<br />
were considered a promising option. These have<br />
meanwhile been introduced in the market. Our experience<br />
clearly indicates that the future belongs to<br />
one-piece zirconia implants placed in single-stage<br />
procedures. Zirconia is considerably more fractureresistant<br />
than aluminium oxide. No metal margins<br />
(as with titanium implants) will become visible as the<br />
gingiva undergoes physiological retraction (0.1 mm<br />
per year). Any aesthetic effects <strong>of</strong> this development<br />
are much less conspicuous with ceramics and can be<br />
readily corrected by changing the superstructure,<br />
even after 15 or 20 years <strong>of</strong> service. However, ceramic<br />
implant designs should always meet one extremely<br />
important requirement: their supragingival element<br />
must be as flat as possible.<br />
39
42<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Interview with Christa Stewens, Bavarian State Minister <strong>of</strong> Labour<br />
and Social Welfare, Family Affairs and Women<br />
Federal Health Fund:<br />
“Dispose <strong>of</strong> it Properly!”<br />
There is hardly a day on which the Federal Health Fund, whose stated objective is to reconcile the differences and financial<br />
clout <strong>of</strong> the various statutory health insurers, does not make the headlines. <strong>EDI</strong> Journal had already reported on this.<br />
Federal Minister for Health Ulla Schmidt and Chancellor Angela Merkel stubbornly cling to the fund and its starting date<br />
<strong>of</strong> 1 January 2009. But they appear to be the only ones. Bavaria, Germany’s largest state by area, will be electing a new state<br />
parliament this autumn – and this election may show the federal government how little appreciation their Federal Health Fund<br />
is getting. BDIZ <strong>EDI</strong> president Christian Berger talked to Christa Stewens, Bavarian State Minister <strong>of</strong> Labour and Social Welfare,<br />
Family Affairs and Women, about the homework that Federal Minister for Health Ulla Schmidt still has to do.<br />
Ms Stewens, your party – the Christian Social Union,<br />
CSU, the regional Bavarian conservative party – has<br />
approved the Federal Health Fund at a federal level.<br />
Why do many within the CSU no longer stand by this<br />
Great Coalition compromise?<br />
We stand by what we have agreed on. But we also<br />
expect the same from our coalition partner. This is<br />
why we will look closely at whether what we agreed<br />
on and what has been defined in the pertinent law is<br />
being both respected and actually implemented. This<br />
also includes the convergence clause, exactly as<br />
defined by the law, but also the correct implementation<br />
<strong>of</strong> the morbidity-based risk adjustment pool and<br />
workable insolvency rules that eliminate any liability<br />
on the part <strong>of</strong> the State <strong>of</strong> Bavaria. To this day, only<br />
fragments <strong>of</strong> the expert opinion on the convergence<br />
clause required by the law – which is supposed to<br />
quantify the effects <strong>of</strong> the Federal Health Fund<br />
before it is realized – have been completed. We cannot<br />
accept that and we will not accept that.<br />
Your ministry has tasked a committee <strong>of</strong> experts led<br />
by Pr<strong>of</strong>essor Udo Steiner, former judge at the Federal<br />
Constitutional Court, to examine the situation <strong>of</strong><br />
physicians and dentists in private practice. What is<br />
their objective, and when can we expect results?<br />
This committee will investigate where and how we<br />
can assist physicians and dentists in private practice.<br />
This is a fairly tall order, because it is the federal government<br />
that creates the legal framework for statutory<br />
health insurance and, consequently, for all contractual<br />
medical providers. The only way Bavaria can<br />
exert its influence is indirectly, through Bundesrat,<br />
the Second Chamber, on a federal level. The expert<br />
committee will therefore mainly be looking for<br />
potential solutions that can be implemented at the<br />
Bavarian level. In addition to the pr<strong>of</strong>essional fees <strong>of</strong><br />
Bavarian physicians, we are also talking about a new<br />
generation <strong>of</strong> physicians and about ensuring adequate<br />
access to general practitioners in rural areas.<br />
The goal is to give recommendations for improving<br />
the situation <strong>of</strong> Bavarian physicians in private practice,<br />
especially general practitioners. A number <strong>of</strong><br />
suggestions will be published by this upcoming<br />
autumn.<br />
Christa Stewens:<br />
Basic tariff may<br />
constitute a<br />
threat.
44<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Physicians and dentists fear that the Federal Health<br />
Fund will indiscriminately level all fees across Germany,<br />
and their representatives in Bavaria fear that<br />
500 million euros may go missing from physicians’<br />
fees and 280 million euros from dentists’ fees. According<br />
to a draft expert opinion to be published shortly,<br />
the “convergence brake” will not have the intended<br />
effect. What are you going to tell the patients if the<br />
quality <strong>of</strong> medical and dental care cannot be maintained<br />
in 2008 and later?<br />
The convergence clause is indispensable for maintaining<br />
the high quality <strong>of</strong> medical care for all<br />
patients in all States. Contrary to the conclusions <strong>of</strong><br />
the expert opinion commissioned by the federal government,<br />
I do believe that this clause can be implemented<br />
in a manner that is in conformance with the<br />
law. We are working on it. However, there is currently<br />
no one who can <strong>of</strong>fer any serious estimates <strong>of</strong> what<br />
the concrete effects <strong>of</strong> the Federal Health Fund will<br />
be. This is one <strong>of</strong> the questions for which I have<br />
demanded an answer ever since day one, but I still<br />
have not received a reply from Ulla Schmidt.<br />
The effects <strong>of</strong> the health reform must be viewed<br />
separately from the effects <strong>of</strong> the reform <strong>of</strong> the fee<br />
structure. The latter affects contract physicians, but<br />
not contract dentists. It is true that the formula<br />
defined in the law, with its uniform standard point<br />
value, will result in a certain amount <strong>of</strong> levelling.<br />
However, the valuation committee has yet to make a<br />
number <strong>of</strong> important decisions, so that we do not<br />
know today what the concrete effects will be. How -<br />
ever, I will do my utmost to ensure that Bavarian<br />
physicians, too, can enjoy reasonable fee increases.<br />
The federal government is obliged to help. After all,<br />
price increases affect everyone, including those who<br />
live and work in Munich and other Bavarian cities.<br />
What effects will the Federal Health Fund have on the<br />
average dentists in private practice? What does it<br />
mean for inpatient and outpatient care?<br />
Any definitive assertions concerning the actual<br />
effects <strong>of</strong> the Federal Health Fund would be pure<br />
speculation today, because a number <strong>of</strong> important<br />
parameters remain undefined. How much are the<br />
premiums going to be? What diseases will be considered<br />
for the risk adjustment pool? There is a lot <strong>of</strong><br />
homework that Ulla Schmidt still has to do.<br />
The beginning <strong>of</strong> this year has seen the introduction<br />
<strong>of</strong> the “basic tariff”. Has this step ushered in the<br />
decline <strong>of</strong> private health insurance in Germany?<br />
The base premium in private health insurance is a<br />
result <strong>of</strong> the political compromise on health reform.<br />
Keeping comprehensive private health insurance<br />
alive was an important agenda for the Bavarian gov-<br />
ernment. We were able to push through this<br />
demand. The pending decision <strong>of</strong> the Federal Constitutional<br />
Court on the complaint brought by the private<br />
health insurers will tell us more.<br />
Have you been able to allay fears that the basic<br />
tariffs, which are intricately linked to the issue <strong>of</strong><br />
portability <strong>of</strong> aging provisions accumulated by private<br />
health insurers on behalf <strong>of</strong> their policyholders,<br />
might bleed the comprehensive private health insurance<br />
tariffs dry?<br />
The portability <strong>of</strong> aging provisions merits well-differentiated<br />
reflection. I myself certainly felt that it<br />
was time to act. The situation today is effectively that<br />
no policyholder <strong>of</strong> a private health insurance company<br />
can switch to another private health insurance<br />
company, because their share <strong>of</strong> the aging provisions<br />
is not transferable. Whether the solution we have<br />
found is ideal is <strong>of</strong> course a matter <strong>of</strong> debate. I can<br />
understand the fears that the basic tariff could<br />
threaten the comprehensive tariffs. In addition, any<br />
subsidies that may be required to support the basic<br />
tariff may penalize policyholders who have signed up<br />
and are paying for the comprehensive tariff. Whether<br />
the courts will find this interference with mutually<br />
agreed contractual agreements to be constitutional<br />
remains to be seen.<br />
The Bavarian State Government seems to have little<br />
influence on the reigning coalition in Berlin when it<br />
comes to the Federal Health Fund. If you had a wish,<br />
what would you do with the fund?<br />
Dispose <strong>of</strong> it properly!<br />
Ms Stewens,<br />
thank you very much for your comments.<br />
Christian Berger:<br />
Bleeding the<br />
comprehensive<br />
private health<br />
insurance tariffs<br />
dry?
46<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
<strong>European</strong> Commission to strengthen patients’ rights<br />
Are we Threatened by<br />
a New Wave <strong>of</strong> Regulations?<br />
Peter Knüpper, solicitor, Munich/Germany<br />
The <strong>European</strong> Court <strong>of</strong> Justice (ECJ) has passed an<br />
extensive body <strong>of</strong> legal decisions on this topic since<br />
1998. In summary, the court has stated that healthcare<br />
services are covered by the freedom to render<br />
services, which is one <strong>of</strong> the four <strong>European</strong> fundamental<br />
freedoms. The free movement <strong>of</strong> goods, persons,<br />
capital and, not least, services have long been<br />
taken for granted by most <strong>of</strong> us. Nevertheless, only<br />
30 percent <strong>of</strong> all EU citizens know that they can<br />
choose to obtain health services in other EU countries,<br />
where the social security system in the patient’s<br />
home country – whether run directly by the state or<br />
in the form <strong>of</strong> an insurance system – has to reimburse<br />
the patient if those services would have been<br />
<strong>of</strong>fered or reimbursed for in the home country.<br />
No prior authorization required<br />
for outpatient services<br />
This is exactly what the draft Directive codifies, with<br />
the result that EU citizens will no longer have to<br />
approach the ECJ in Luxembourg in order to obtain<br />
reimbursement but can confront their national<br />
administrations or health insurance institutions<br />
directly with the new Directive on patients’ rights. It<br />
states, in unison with ECJ decisions, that outpatient<br />
services do not require prior authorization. The same<br />
is true <strong>of</strong> inpatient health services that require a<br />
patient to be admitted overnight or that are included<br />
on a list <strong>of</strong> specific diseases – unless “the financial<br />
balance <strong>of</strong> the Social Security system” were threat-<br />
The <strong>European</strong> Commission finally presented its proposal for a Directive to facilitate the application<br />
<strong>of</strong> <strong>European</strong> patients' rights in relation to cross-border healthcare on 2 July 2008, as part <strong>of</strong> its<br />
Renewed Social Agenda. The proposal is intended to respond to rapid changes in the social and eco-<br />
nomic fields. It intends to promote citizens’ “social well-being” through a mixture <strong>of</strong> measures and<br />
instruments while at the same time harmonizing and modernizing the existing political armamen-<br />
tarium. The proposed Directive covers cross-border health services that patients may obtain outside<br />
their home country – such as the hip joint surgery that a British patient had had performed in<br />
France, bypassing the long waiting lists <strong>of</strong> the British National Health Service.<br />
ened or the planning and rationalization carried out<br />
in the hospital sector were “seriously undermined”<br />
(Article 8 (3) <strong>of</strong> the draft guideline). The prior authorization<br />
system must be limited to what is necessary<br />
and proportionate to avoid such an impact and must<br />
not constitute a means <strong>of</strong> arbitrary discrimination.<br />
The Member States must act to improve the flow <strong>of</strong><br />
information concerning potential healthcare services<br />
in other EU Member States.<br />
The <strong>European</strong> Commission continues to uphold<br />
the sole responsibility <strong>of</strong> the Member States for the<br />
organization and delivery <strong>of</strong> health services and<br />
medical care. The Directive also demands <strong>of</strong> the<br />
Member States to respect the principles <strong>of</strong> universality,<br />
access to quality care, equity and solidarity and<br />
define observe clear standards for quality and safety<br />
and health care. They also have to ensure that “mechanisms<br />
are in place for ensuring that healthcare<br />
providers are able to meet such standards, taking<br />
into account international medical science and generally<br />
recognized good medical practices”. In addition,<br />
EU Member States are tasked to ensure that the<br />
application <strong>of</strong> such standards in practice is regularly<br />
monitored.<br />
National contact points<br />
Healthcare providers will have to “provide all relevant<br />
information to enable patients to make an informed<br />
choice, in particular on availability, prices and outcomes<br />
<strong>of</strong> the healthcare provided”. This also includes
48<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
information on pr<strong>of</strong>essional liability insurance. National<br />
contact points are called upon to provide, in close<br />
cooperation with other national authorities, information<br />
to patients, particularly on cross-border healthcare<br />
and the “guarantees <strong>of</strong> quality and safety”. These contact<br />
points are to help patients protect their rights and<br />
seek appropriate redress in the event <strong>of</strong> harm.<br />
In addition, the EU requires the Member States to<br />
facilitate the development <strong>of</strong> <strong>European</strong> reference networks<br />
intended to help realize the potential <strong>of</strong> <strong>European</strong><br />
cooperation regarding highly specialized healthcare<br />
for patients and for healthcare systems from<br />
innovations in medical science and health technologies.<br />
In addition, the networks are intended to “help to<br />
promote access to high quality and cost-effective<br />
healthcare for all patients with a medical condition<br />
requiring a particular concentration <strong>of</strong> resources or<br />
expertise” and to promote the effective use <strong>of</strong><br />
resources by concentrating them where appropriate.<br />
What does this mean? Will there be a <strong>European</strong><br />
policy <strong>of</strong> subsidies supporting centralized structures<br />
within the EU, comparable with the agricultural sector?<br />
Even if the objective were merely to provide<br />
quality and safety references that assist member<br />
states to “provide a full range <strong>of</strong> highly specialized<br />
services <strong>of</strong> the highest quality”, it is easy to imagine<br />
the type <strong>of</strong> regulatory machinery this would entail.<br />
The same is true <strong>of</strong> the development and operation<br />
<strong>of</strong> a network for health technology assessment,<br />
which the <strong>European</strong> Commission wants to require <strong>of</strong><br />
the Member States. The requirement to collect statistical<br />
data needed for monitoring purposes on the<br />
provision <strong>of</strong> cross-border healthcare, the care provided,<br />
its providers and patients, the cost and the outcomes<br />
(!) and to provide them to the <strong>European</strong> Commission<br />
on an annual basis already afford a glimpse<br />
<strong>of</strong> the new bureaucracy about to be born.<br />
Introduction <strong>of</strong> quality standards<br />
It has been estimated that approximately one percent<br />
<strong>of</strong> all <strong>European</strong>s currently obtain cross-border<br />
health services, not including those who require<br />
treatment on holidays or while working in a different<br />
EU Member State. This cost is borne by the national<br />
health care systems anyway, and the corresponding<br />
rules go back to as far as 1971 (Regulation 1408/71/<br />
EEC), as symbolized by the E 111 form or the <strong>European</strong><br />
health insurance card.<br />
It appears doubtful that such comprehensive<br />
requirements encased in a Directive, dealing with<br />
issues as diverse as patient information, national<br />
contact points, <strong>European</strong> reference centres, information<br />
technology or statistics, should really be necessary.<br />
However, Community institutions are given<br />
broad discretion when it comes to applying a high<br />
level <strong>of</strong> protection. Quite adroitly, the draft Directive<br />
would require the Member States to introduce, e.g.,<br />
certain quality standards, with the <strong>European</strong> Commission<br />
restricting itself to “merely” issuing guidelines.<br />
Obviously, the intention is to resolve the contradiction<br />
between the sovereignty <strong>of</strong> the Member<br />
States in the healthcare sector on one hand and the<br />
common market strategy <strong>of</strong> the EU on the other – a<br />
path that may be juridically feasible but may well<br />
prove politically difficult.<br />
Conclusions<br />
The Patients’ Rights Directive not only determines<br />
that patients may obtain cross-border inpatient and<br />
outpatient medical (elective) services, largely without<br />
prior authorization by the national administrations or<br />
health insurance institutions in their home countries,<br />
and that they may demand reimbursement for these<br />
services from their home social security system.<br />
If the proposed Directive were to be enacted by the<br />
<strong>European</strong> Parliament, the national healthcare systems<br />
would be increasingly harmonized, since the<br />
Member States would be obliged to cooperate and to<br />
implement EU healthcare to a larger extent than previously.<br />
They would ultimately have to adapt their<br />
healthcare policy to the <strong>European</strong> regime – subsidiarity<br />
or no subsidiarity.<br />
What seems to be so problematic is that Europe is<br />
not moving in the direction <strong>of</strong> liberalization but<br />
instead seems to seek redemption by regulation – in<br />
a manner similar to the national healthcare systems.<br />
This is just what we feared when the <strong>European</strong> Parliament<br />
decided to exclude healthcare services from<br />
the scope <strong>of</strong> the general Services Directive in 2006.<br />
We can look forward to the discussions within the<br />
<strong>European</strong> Parliament and the <strong>European</strong> Council over<br />
the next few months regarding the <strong>European</strong> Commission’s<br />
new approach to regulating healthcare<br />
services. Should the Directive fail, the verdict by the<br />
ECJ prevails: Free movement <strong>of</strong> services includes<br />
healthcare services – no restrictions allowed.<br />
Brussels
50<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Fuerteventura 2008<br />
18 th Expert Symposium University<br />
and Clinical Practice<br />
Once again this year, the BDIZ <strong>EDI</strong> University and Clinical Expert Symposium will be held on Fuerteventura – jointly with the<br />
International Interdisciplinary Symposium on Pain and Movement. In 2008, oral implantology and periodontology will be at<br />
the focus <strong>of</strong> this one-week continuing-education event. Date: 25 October – 1 November 2008.<br />
An intensive exchange <strong>of</strong> ideas in a personal environment,<br />
hands-on workshops, a completely renovated<br />
venue – all these will help us to concentrate on<br />
important implantological issues. Being away from<br />
your daily chores and close to the expert speakers –<br />
this is what makes the Fuerteventura expert symposia<br />
so special.<br />
Date: 25 October – 1 November 2008<br />
Registration at: www.schmerzsymposium.de<br />
Travel and registration:<br />
HOLIDAY LAND Reisebüro Garthe & Pflug<br />
Ms Garthe<br />
Triftstrasse 20<br />
60528 Frankfurt<br />
Germany<br />
Phone +49 69 6773670<br />
The following speakers have been signed up:<br />
(Germany unless otherwise noted)<br />
Dr Markus Baumeister, Dortmund<br />
• Treatment planning for reduced-diameter implants<br />
in the aesthetic zone<br />
Christian Berger, Kempten<br />
• Forensic aspects <strong>of</strong> treatment documentation<br />
Dr Fred Bergmann, Viernheim<br />
• What type <strong>of</strong> s<strong>of</strong>t-tissue management for what situation?<br />
Dr Andreas Braun, Bonn<br />
• Antimicrobial photodynamic therapy (aPDT) in chronic periodontitis:<br />
Results <strong>of</strong> an in-vivo study<br />
Dr Christian Foitzik, Darmstadt<br />
• Surgical complications – or complications caused by surgery<br />
Dr Ernst Fuchs, Zürich, Switzerland<br />
• Planning, function and restoration <strong>of</strong> the bioactive container<br />
Dr Ulrich Fürst, Attnang-Puchheim<br />
• Long-term results <strong>of</strong> minimally invasive peri-implantitis therapy<br />
Dr Viktor E. Karapetian, Cologne<br />
• Immediate loading with chairside ceramic crowns<br />
Dr Julia Kenter-Berg, Cologne<br />
• <strong>Dental</strong> low-level laser treatment – evidence-based medicine?<br />
Dr Frank Kistler, Landsberg<br />
• Aesthetics in oral implantology – just a matter <strong>of</strong> planning?<br />
Dr Christian Köneke, Bremen<br />
• Functional complications in implant therapy
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
51<br />
Dr Frank Kornmann, Oppenheim, and MDT Gerhard Stachulla, Augsburg<br />
• Implant planning based on state-<strong>of</strong>-the-art 3D diagnostics<br />
Dr Matthias Krysewski, Gronau<br />
• Solo prophylaxis for dentists and physicians<br />
Dr Thea Lingohr, Cologne<br />
• Preventing jaw atrophy through socket preservation<br />
Dr Daniel Rothamel, Cologne<br />
• Clinical importance <strong>of</strong> growth factors – hocus-pocus or the way <strong>of</strong><br />
the future? Xenogeneic and allogeneic bone blocks – blessing or curse?<br />
Pr<strong>of</strong> Hubert Nentwig, Frankfurt<br />
• Complications caused by minimized implant numbers<br />
and implant dimensions<br />
Dr Jörg Neugebauer, Cologne<br />
• What information does 3D diagnostics provide in the therapy<br />
<strong>of</strong> congenitally missing teeth?<br />
Dr Stefan Reinhardt, Münster<br />
• Planning bone transplants to avoid complications<br />
Dr Bernhard Saneke, Wiesbaden<br />
• Fewer complications in the dental <strong>of</strong>fice through better staff selection?<br />
Dr Sebastian Schmidinger, Seefeld<br />
• Extended diagnostics and its influence on treatment planning in 2008<br />
Dr Jochen Tunkel, Bad Oeynhausen<br />
• Implants at hard- and s<strong>of</strong>t-tissue defects with special regard<br />
to s<strong>of</strong>t-tissue management<br />
MDT Hartmut Scholz, Bonn<br />
• Loose dentures and bar fractures – or stable optimized bar-supported<br />
restorations<br />
Pr<strong>of</strong> Anton Sculean, Nijmegen, Netherlands<br />
• PDT in non-surgical periodontal treatment<br />
Dr Martin Scheer, Cologne<br />
• What mucosal situation can still be considered non-pathological<br />
in oral implant therapy?<br />
Dr Marius Steigmann, Neckargemünd<br />
• S<strong>of</strong>t-tissue management complications<br />
Dr Helmut Steveling, Heidelberg<br />
• 3D planning and implementation: Facilitate systems<br />
Dr Achim Wöhrle, Knittlingen<br />
• How to explain failure to patients<br />
Pr<strong>of</strong> Joachim E. Zöller, Cologne<br />
• Trauma to the dentoalveolar nerve and its consequences
52<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
New service for members<br />
Quintessenz-TV:<br />
Online Video Library<br />
“Your guest at home”! Starting in October 2008, members <strong>of</strong> BDIZ <strong>EDI</strong> will be able to select, from an extensive visual library,<br />
the works <strong>of</strong> a highly diverse group <strong>of</strong> authors on a wide range <strong>of</strong> topics related to dentistry. This gives all those who want to<br />
do so the opportunity to gain new insights and to continue their education at home or at the <strong>of</strong>fice in a manner and at a speed<br />
that suits them. To be able to present this service to its members, BDIZ <strong>EDI</strong> has entered into a cooperative agreement with the<br />
international Quintessence Publishing group.<br />
The comprehensive library <strong>of</strong> videos and presentations<br />
currently covers more than 200 topics<br />
from all fields <strong>of</strong> dentistry. This archive is a true<br />
treasure trove – it spans the range from one <strong>of</strong> the<br />
first dental documentary ever shot (showing Pr<strong>of</strong>essor<br />
Gysi in the year 1926 as he registers a Gothic<br />
arch) all the way to the most recent presentations<br />
<strong>of</strong> internal and external sinus floor elevation<br />
procedures: Continuing education films are available<br />
in full standard TV quality – and since 2007,<br />
Quintessence has been producing all its material<br />
in the state-<strong>of</strong>-the-art 16 : 9 HDTV format.<br />
At the time <strong>of</strong> this writing, the relaunch <strong>of</strong> the<br />
existing quintessenz.tv programme is under way.<br />
Several new convenient user functions will soon<br />
be available (see illustrations). Online tests accessible<br />
through integrated links will allow users to<br />
obtain continuing-education (CE) points according<br />
to BZÄK and DGZMK criteria. 50 tests related to as<br />
many videos are already available on request.<br />
BDIZ <strong>EDI</strong> will be able to use the service without<br />
any extra charge for an initial period <strong>of</strong> twelve<br />
months. The only technical prerequisite is a highspeed<br />
Internet connection to ensure the necessary<br />
bandwidth. Within the next few weeks, BDIZ<br />
<strong>EDI</strong> members will receive a separate letter <strong>of</strong><br />
introduction containing the access data to register<br />
at quintessenz.tv.<br />
1. Embedded video player, 2. Player controls, 3. Full-screen button,<br />
4. About the video, 5. Category/subject selection,<br />
6. Name <strong>of</strong> active category, 7. Video wall for video selection
BDIZ <strong>EDI</strong> congratulates Hinrich Peter Romeike<br />
Implantologist Wins<br />
Two Gold Medals<br />
What does an oral implantologist have in common with an Olympic gold medal<br />
winner? Characteristics such as willpower, precision, technical expertise, but also<br />
social competence and the ability to work in a team. Hinrich Peter Romeike from<br />
little Moholz in the far north <strong>of</strong> Germany has all these virtues. At the Olympic site<br />
<strong>of</strong> Hong Kong he won equestrian gold in both Eventing Team and Eventing Individual<br />
on August 12.<br />
The victorious rider is not only a dentist and oral implantologist<br />
in private practice in Rendsburg but also a member <strong>of</strong> BDIZ<br />
<strong>EDI</strong>. The entire BDIZ <strong>EDI</strong> board extends its congratulations. Hinrich<br />
Peter Romeike and his grey gelding Marius have shown an<br />
exceptional performance and made unexpected but welcome<br />
headlines for the dental pr<strong>of</strong>ession – but they also demon-<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Hinrich Peter Romeike (right), winner <strong>of</strong> two gold<br />
medals in eventing at the 2008 Olympics in Beijing,<br />
in Eventing Team and Eventing Individual.<br />
Back in his home town <strong>of</strong> Moholz, he received a<br />
warm welcome. Schleswig-Holstein’s Prime Minister<br />
Peter Harry Carstensen congratulated him<br />
and his teammate Peter Thomsen (left) and conveyed<br />
the greetings <strong>of</strong> his government.<br />
strated team spirit in helping the entire German team win<br />
Eventing Team Jumping gold.<br />
The BDIZ <strong>EDI</strong> can be proud to have someone like him among<br />
its members. Congratulations, Hinrich Peter Romeike!<br />
53
54<br />
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Belgium/ECJ: National prohibition against<br />
dentists’ advertisements upheld<br />
National regulations that restrict or prohibit advertisement<br />
for dental services are not in violation <strong>of</strong><br />
Community law, according to a <strong>European</strong> Court <strong>of</strong><br />
Justice (ECJ) decision reported by the dental news<br />
service zänd. The judgment had been prompted by<br />
criminal proceedings against a Belgian dentist who<br />
had advertised his laboratory and his dental clinic in<br />
the yellow pages under his full name, something that<br />
is prohibited under Belgian law. The advertisement<br />
contained objective information such as a list <strong>of</strong> services<br />
<strong>of</strong>fered as well as the addresses, phone numbers<br />
and opening hours <strong>of</strong> the two establishments. The<br />
Belgian court that had submitted the question to the<br />
ECJ held the opinion that advertising restrictions for<br />
dentists might violate their freedom <strong>of</strong> competition<br />
pursuant to Articles 10 and 81 <strong>of</strong> the Community<br />
Treaty. “On the other hand, given the heterogeneity <strong>of</strong><br />
the liberal pr<strong>of</strong>essions and the specificity <strong>of</strong> their<br />
markets, one would have to examine closely whether<br />
restrictions in a given market actually restrain competition,”<br />
as the Free <strong>Association</strong> <strong>of</strong> German Dentists<br />
(FVDZ) stated at its Brussels <strong>of</strong>fice. After all, the ECJ<br />
had held that the prohibition did not restrain trade in<br />
that the Belgian law is not covered by any <strong>of</strong> the provisions<br />
<strong>of</strong> Articles 10 and 81 <strong>of</strong> the Community Treaty:<br />
The case at hand did not demonstrate that the law<br />
favoured a cordial agreement or supported, facilitated<br />
or mandated a company decision. Neither had the<br />
law in question lost its character as a legal norm by<br />
virtue <strong>of</strong> the fact that Belgium had transferred<br />
responsibility for economic decisions to certain private<br />
institutions.<br />
Source: Various media<br />
Private health insurance in France:<br />
Covering the deficit<br />
The government <strong>of</strong> France intends to force private<br />
health insurers to cover the deficits <strong>of</strong> the state-run<br />
health-insurance system, which stands at four billion<br />
euros. “If we do not act, this deficits will grow by<br />
another two billion euros each year”, as Minister <strong>of</strong><br />
Health Roselyne Bachelot and Budget Minister Éric<br />
Europe-Ticker<br />
Woerth said in an interview with the French daily Le<br />
Parisien. For this reason, the government intends to<br />
tax the turnover <strong>of</strong> private supplementary health<br />
insurance companies, which would contribute<br />
“approximately one billion euros a year” toward eliminating<br />
the deficit by the year 2011. But the French<br />
government also wants to realize savings in other<br />
areas: They want physicians to stop prescribing<br />
“unnecessarily expensive drugs”, to reduce prices for<br />
certain drugs and medical exams and to improve hospital<br />
organization. Rather than letting the beneficiaries<br />
<strong>of</strong> the state health-insurance system foot the bill,<br />
the government would tax private health insurers, as<br />
Minister <strong>of</strong> Health Bachelot explained. After all,<br />
approximately eight percent <strong>of</strong> all French citizens – or<br />
about four million people – are covered. But political<br />
scientist Bruno Palier <strong>of</strong> the national research Institute<br />
CNRS warned <strong>of</strong> unfairness in the French healthinsurance<br />
system: “Those who can afford it will buy<br />
the best supplementary insurance and, consequently,<br />
the best treatment”, he said to Le Parisien.<br />
Sources: Le Parisien/Deutsches Ärzteblatt<br />
Cancer patients in the UK:<br />
No money for drug treatment<br />
The National Health Service (NHS) in the UK is experiencing<br />
a shortage <strong>of</strong> funds to pay for life-extending<br />
drugs. The affected patients suffer from kidney cancer,<br />
and four life-extending drugs are involved. At up to<br />
£ 35,000 per patient per year, the NHS considers that<br />
the drugs do not <strong>of</strong>fer value for money. Pr<strong>of</strong>essor Peter<br />
Littlejohns, clinical and public health director at the<br />
National Institute for Clinical Excellence (NICE), called<br />
this a difficult decision: “NHS resources are not limitless.”<br />
He admitted that the drugs might prolong the<br />
lives <strong>of</strong> renal cell carcinoma patients by up to half a<br />
year, but without having any actual healing effect. If<br />
these drugs (bevacizumab, sorafenib, sunitinib and<br />
temsirolimus) were provided on the NHS, other<br />
patients would lose out on treatments that are more<br />
useful. Patient representatives denounced the NHS<br />
plans because they would result in many cancer<br />
patients dying faster.<br />
Source: Ärzte-Zeitung
<strong>EDI</strong><br />
<strong>EDI</strong> News<br />
Miniclinics in the US: Treatment at the supermarket<br />
As Americans suffer from the effects <strong>of</strong> the real estate crisis and high oil<br />
prices, instant medical treatment <strong>of</strong> common ailments is booming. Minute-<br />
Clinic, a subsidiary <strong>of</strong> the major US drugstore chain CVS, had 70 clinics in<br />
2006. In March 2008, the 500 th clinic was opened, with the 700 mark expected<br />
to be reached by the end <strong>of</strong> the year. Representatives <strong>of</strong> the medical establishment<br />
warn <strong>of</strong> quality problems, but the demand is skyrocketing. Given<br />
the unability <strong>of</strong> politicians to solve its rampant problems, the US healthcare<br />
system is on the brink <strong>of</strong> collapse. More than 47 million Americans are not<br />
covered by health insurance. As many established practitioners continue to<br />
be highly skeptical, the miniclinic idea is being imitated elsewhere. The<br />
world-famous Mayo Clinic will be founding several <strong>of</strong> these supermarket<br />
clinics by the end <strong>of</strong> 2008 in order to cash in on its legendary name.<br />
Source: Various media<br />
Health insurance in Austria: Imminent bankruptcy<br />
A not insignificant number <strong>of</strong> Austrian health insurers are facing bankruptcy.<br />
The promised temporary state relief in the amount <strong>of</strong> 150 million euros<br />
once promised by the government will not be forthcoming following the<br />
governing coalition’s demise. In any event, the subsidy would have alleviated,<br />
not resolved the financial difficulties. The situation <strong>of</strong> the Vienna Regional<br />
Health Fund (WGKK) is particularly critical because it is up to 543 million<br />
euros in the red. The Vienna Chamber <strong>of</strong> Physicians does not believe that the<br />
bankruptcy <strong>of</strong> the WGKK can be staved <strong>of</strong>f until February 2009, but expects<br />
it to happen as early as this upcoming September, as a spokesman said: “We<br />
do not believe the WGKK will last until February”. As early as this autumn,<br />
patients may be forced to pay for their doctor’s visits themselves. Practitioners<br />
are being told to prepare for a situation without a contract: “We are asking<br />
ourselves whether we will still receive our fees come autumn.”<br />
Source: Various media<br />
Revalidation in the UK: Morale is low in the medical camp<br />
Half <strong>of</strong> all British medical practitioners reject the revalidation process they<br />
have to undergo every five years in order to keep their licenses because this<br />
requirement questions their pr<strong>of</strong>essional qualification. Sixty-five percent <strong>of</strong> all<br />
physicians are convinced that the new revalidation procedures will reduce<br />
morale, according to a current TNS Healthcare survey. In a survey <strong>of</strong> more than<br />
200 GPs across the UK, they found little support for the new procedure: ”71 percent<br />
<strong>of</strong> the physicians believe it will reduce time with patients and almost twothirds<br />
anticipate that it will be no more than a ‘tick box’ exercise. Almost half<br />
are concerned revalidation will serve as a tool to weed out doctors viewed as<br />
difficult to manage or uncooperative.” The new process – which will be drawn<br />
up and piloted over the next 18 months – includes a system for re-licensing the<br />
UK’s 150,000 physicians by testing their basic medical competence.<br />
Source: Zahnärztlicher Nachrichtendienst (zänd)<br />
55
58 <strong>EDI</strong><br />
<strong>European</strong> Law<br />
Proposal for a directive on the application <strong>of</strong> patients’ rights<br />
in cross-border healthcare presented by the <strong>European</strong> Commission on 2 July 2008<br />
<strong>European</strong> Commission Intends to<br />
Provide Legal Certainty for Patients’<br />
Rights in Cross-border Healthcare<br />
On 28 April 1998, the <strong>European</strong> Court <strong>of</strong> Justice (ECJ)<br />
ruled that patients are entitled to receive not only<br />
non-hospital medical services anywhere within the<br />
<strong>European</strong> Community but also to be reimbursed for<br />
their expenses by the statutory health insurers in<br />
their own Member State without prior authorization.<br />
Although the ECJ continues to rule in favour <strong>of</strong><br />
patients, many <strong>of</strong> them are not being reimbursed<br />
and have to pay the cost themselves if they are<br />
unwilling or unable to go to court. A survey 1 has<br />
shown that 30 percent <strong>of</strong> the citizens <strong>of</strong> the <strong>European</strong><br />
Union are not aware <strong>of</strong> the possibility to receive<br />
healthcare outside their Member State <strong>of</strong> affiliation.<br />
This might be a reason why cross-border healthcare<br />
amounts to only 1 percent <strong>of</strong> all healthcare spending<br />
in the EU, i.e. € 10 billion.<br />
The <strong>European</strong> Commission has initiated public<br />
consultations to analyze the problems within crossborder<br />
healthcare and to identify possible legal<br />
instruments best qualified for each <strong>of</strong> the different<br />
issues. The majority <strong>of</strong> the 280 contributors voted in<br />
favour <strong>of</strong> cooperation on the part <strong>of</strong> the <strong>European</strong><br />
healthcare systems on a legislative as well as on a<br />
practical level. Based on these contributions, the<br />
Commission presented, on 2 July 2008, a proposal for<br />
a directive to facilitate the application <strong>of</strong> <strong>European</strong><br />
patients’ rights in relation to cross-border healthcare.<br />
The proposal intends to issue common guidelines to<br />
the Member States to assure that patients’ rights will<br />
be protected.<br />
The Commission’s suggestion is a follows: Based<br />
on the rulings <strong>of</strong> the ECJ, access to cross-border<br />
healthcare is to be simplified and the system <strong>of</strong> preauthorization<br />
reduced to a necessary level. Patients<br />
are to be reimbursed for non-hospital as well as hospital<br />
care without prior authorization. Exceptions can<br />
only be granted within hospital care. A Member State<br />
can require prior authorization for hospital care if it<br />
provides evidence that the treatment, had it been<br />
performed on its territory, would have been covered<br />
by its social security system and that the consequent<br />
outflow <strong>of</strong> patients seriously undermines or is likely<br />
to seriously undermine the financial balance <strong>of</strong> its<br />
social security system.<br />
Member States in which a substantial percentage<br />
<strong>of</strong> all patients receive treatment only after extended<br />
waiting times fear the migration <strong>of</strong> these patients<br />
and potential subsequent instability within their<br />
own healthcare systems. Other Member States are<br />
looking forward to providing treatment for these<br />
patients from areas in the vicinity <strong>of</strong> their borders.<br />
It should not be overlooked that the definition <strong>of</strong><br />
non-hospital and hospital care varies from Member<br />
State to Member State. The proposal defines hospital<br />
care as a benefit that at least requires a patient’s<br />
overnight accommodation, unless the hospital care<br />
concerns certain treatments yet to be listed by the<br />
Commission. Whether all Member States will agree<br />
to this definition is a moot point. If some Member<br />
States have lower or different standards regarding<br />
the overnight-accommodation rule, conflicts may<br />
arise as these States are prevented from requiring<br />
prior authorization.<br />
A potential problem is that the commission plans<br />
to draw up a list <strong>of</strong> specific treatments that are<br />
regarded to constitute hospital care and thereby<br />
being eligible for a prior authorization requirement,<br />
irrespective <strong>of</strong> the mode <strong>of</strong> accommodation. This list<br />
is to include healthcare modalities that require a<br />
highly specialized and cost-intensive medical infrastructure<br />
and medical equipment or healthcare<br />
involving treatments presenting a particular risk to<br />
the patient or the population. It is more than questionable<br />
that the Member States will actually give up<br />
their right to participate in drawing up this list.
60 <strong>EDI</strong><br />
<strong>European</strong> Law<br />
Another challenge all Member States will be facing<br />
is to create a mechanism to assign their healthcare<br />
benefits a specific monetary value in order for<br />
these benefits to become reimbursable. For this<br />
mechanism to become transparent, it will have to<br />
be based on objective, non-discriminatory criteria<br />
announced in advance. If legal certainty is to be provided<br />
in the real <strong>of</strong> cross-border healthcare, the<br />
Member States will also have to find methods to<br />
establish cross-border comparability <strong>of</strong> benefits and<br />
pricing systems.<br />
Furthermore, the proposal intends to reimburse an<br />
insured person for the costs <strong>of</strong> treatment in a foreign<br />
state up to the cost <strong>of</strong> the same or similar treatment<br />
within their national healthcare system, i.e. the treatment<br />
has to be part <strong>of</strong> the service <strong>of</strong>fered to the<br />
insured person in his or her own Member State. In<br />
order to avoid letting the insured person derive a<br />
financial advantage from healthcare provided in<br />
another Member State, reimbursement is to be limited<br />
to the actual cost <strong>of</strong> the healthcare received.<br />
Article 6 <strong>of</strong> the proposal clarifies that only insured<br />
persons are allowed to claim reimbursement for<br />
cross-border healthcare. Article 4 defines the expression<br />
“insured person” with a reference to Article 1 c <strong>of</strong><br />
Council Regulation (EC) No. 883/2004. The proposal<br />
therewith distinguishes between “insured person”<br />
and “family member” as mentioned in Article 1 f <strong>of</strong><br />
Council Regulation (EC) No. 883/2004 but not in the<br />
proposal itself. This may create difficulties because,<br />
for example, family members in Germany can be coinsured<br />
and accordingly should be entitled to reimbursement<br />
for cross-border healthcare as well. Considering<br />
the proposal’s text, this could not be the<br />
case.<br />
In addition, Article 6 <strong>of</strong> the proposal states that the<br />
claim for reimbursement has to be directed against<br />
the Member State <strong>of</strong> affiliation and not its statutory<br />
health insurer. It would be preferable not to obligate<br />
the Member States themselves but to create an obligation<br />
<strong>of</strong> the Member States to ensure reimbursement<br />
by their statutory health insurers.<br />
If reimbursement presupposes that the same or a<br />
similar treatment is being <strong>of</strong>fered and covered in the<br />
insured person’s Member State, it is arguable if and<br />
to what extent the attending physician is allowed to<br />
deviate from the treatment course without the<br />
insured losing his claim for reimbursement. As far as<br />
the proposal is concerned, a patient has the right to<br />
receive any medicinal product authorized for marketing<br />
in the Member State where healthcare is provid-<br />
ed, even if this product is not authorized in the Member<br />
State <strong>of</strong> affiliation. The medicinal product only<br />
has to be considered “an indispensable part <strong>of</strong><br />
obtaining effective treatment in another Member<br />
State”. But if the medicinal product is in fact not<br />
authorized in the patient’s Member State, it cannot<br />
be part <strong>of</strong> any treatment there. In this case, the system<br />
<strong>of</strong> reimbursement might lack a precondition:<br />
“the same or similar” treatment <strong>of</strong>fered and covered<br />
in the Member State <strong>of</strong> affiliation. This will certainly<br />
not become an issue regarding medicinal products<br />
that only bear a different name and/or are provided<br />
by different manufacturers while still containing the<br />
same or a very similar effective substance. But the<br />
question might arise in the context <strong>of</strong> medicinal<br />
products as parts <strong>of</strong> a highly specialized treatment<br />
that, in this form, is not available in every Member<br />
State.<br />
The proposal does not intend to modify the Member<br />
States’ particular national healthcare system.<br />
Member States can impose the same conditions and<br />
criteria <strong>of</strong> eligibility on insured persons seeking<br />
cross-border healthcare as they apply domestically –<br />
as long as these conditions are neither discriminatory<br />
nor an obstacle to freedom <strong>of</strong> movement <strong>of</strong> persons.<br />
For example, many health insurers in Germany<br />
now deduct between 7.5 and 10 percent <strong>of</strong> the reimbursement<br />
for “increased administrative expenses”. It<br />
seems questionable at least that this policy will survive<br />
the coming directive.<br />
To inform patients <strong>of</strong> possible cross-border healthcare<br />
<strong>of</strong>ferings, every Member State has to establish<br />
so-called “national contact points”. These contact<br />
points are to advise patients on the requirements <strong>of</strong><br />
cross-border healthcare, reimbursement systems<br />
and liability questions.<br />
The time and effort the Member States will have to<br />
invest in establishing these contact points will be<br />
substantial. The goal is to gather, summarize and<br />
present all the different healthcare systems and their<br />
legal foundations for a legal layperson, the patient.<br />
The proposal also plans to commit all “healthcare<br />
providers” – which includes physicians – “to provide<br />
all relevant information to enable patients to make<br />
an informed choice, in particular on availability,<br />
prices and outcomes <strong>of</strong> the healthcare provided”. If<br />
this is interpreted as a comparison <strong>of</strong> the costs <strong>of</strong> all<br />
healthcare benefits, an intimate knowledge <strong>of</strong> the<br />
different healthcare systems and their guidelines<br />
regarding conditions <strong>of</strong> treatment and reimbursement<br />
systems will be essential. But the attending<br />
physician cannot be expected to know, for all 27
<strong>EDI</strong> 61<br />
<strong>European</strong> Law<br />
Member States, whether or not patients are eligible<br />
for a certain benefit or if they can claim reimbursement<br />
in their Member States.<br />
Aside from the immense amount <strong>of</strong> time this<br />
information requirement would consume, it certainly<br />
cannot be a physician’s duty to advise patients <strong>of</strong><br />
the numerous requirements <strong>of</strong> cross-border healthcare.<br />
If anything, this task should be performed by<br />
the national contact points.<br />
The <strong>European</strong> Commission also wants to establish<br />
common guidelines concerning the quality and safety<br />
<strong>of</strong> medical care and to increasingly assure the<br />
Member States’ compliance with these guidelines.<br />
The Commission’s intention is to motivate the Member<br />
States to improve their standards <strong>of</strong> quality and<br />
safety and to align themselves with the actual state<br />
<strong>of</strong> medical science to match up the levels <strong>of</strong> provision<br />
within the Member States. Germany has many years<br />
<strong>of</strong> experience with such guidelines, which are almost<br />
invariably out <strong>of</strong> date by the time they are enacted.<br />
This problem will increase if guidelines are to be<br />
developed for all Member States at the same time.<br />
The proposed directive still has to be ratified by the<br />
<strong>European</strong> Parliament and Council. As with the directive<br />
on services, the <strong>European</strong> Parliament will probably<br />
request various amendments. The directive might<br />
therefore not be ratified before a new parliament is<br />
elected in the summer <strong>of</strong> 2009.<br />
Solicitor Nico Gottwald<br />
Ratajczak & Partners<br />
Berlin · Cologne · Essen · Freiburg<br />
Meissen · Munich · Sindelfingen<br />
Posener Straße 1<br />
71065 Sindelfingen, Germany<br />
1 Flash Eurobarometer Series #210, Cross-border<br />
health services in the EU, Analytical report, conducted<br />
by the Gallup Organization, Hungary upon the<br />
request <strong>of</strong> the <strong>European</strong> Commission, the Health<br />
and Consumer Protection Directorate-General (DG<br />
SANCO), 2007.
62 <strong>EDI</strong><br />
<strong>European</strong> Law<br />
<strong>EDI</strong> Journal 1/2008, 44 f. – Supplementary information<br />
Prohibition <strong>of</strong> Age Discrimination<br />
A submission by the Social Court (Sozialgericht) <strong>of</strong><br />
Dortmund, Germany has now given the <strong>European</strong><br />
Court <strong>of</strong> Justice (ECJ) an opportunity to continue<br />
developing its series <strong>of</strong> rulings related to the prohibition<br />
<strong>of</strong> age discrimination and to make a decision on<br />
age limits for dentists.<br />
As reported in <strong>EDI</strong> Journal 1/2008, 45, the Federal<br />
Social Court (Bundessozialgericht) <strong>of</strong> Germany had<br />
not deemed it necessary, when ruling on the legality<br />
<strong>of</strong> a rule that generally bars physicians or dentists<br />
aged 68 or above from engaging in outpatient treatment<br />
covered by the statutory health insurance system,<br />
to submit the issue to the ECJ to request a concrete<br />
interpretation <strong>of</strong> Directive 2000/78/EC (the<br />
anti-discrimination directive). This gap has now been<br />
filled by the Social Court <strong>of</strong> Dortmund, which did not<br />
adopt legal precedent established by the Federal<br />
Social Court. Hence, the Social Court <strong>of</strong> Dortmund<br />
decided on 28 June 2008 to request clarification from<br />
the ECJ concerning the prohibition <strong>of</strong> age discrimination<br />
based on <strong>European</strong> law as it applies to age limits<br />
for dentists within the statutory health insurance<br />
system (S 16 KA 117/07). The Social Court <strong>of</strong> Dortmund<br />
held that the only justification for such an age limit<br />
could be that, according to general life experience,<br />
advancing age goes hand in hand with a reduction in<br />
performance and that this might translate into a<br />
hazard to patients. This was one <strong>of</strong> the reasons why<br />
the Federal Constitutional Court (Bundesverfassungsgericht)<br />
<strong>of</strong> Germany ruled age limits to be constitutional<br />
in 1998; however, this ruling did not relate<br />
to <strong>European</strong> law, especially as it preceded the antidiscrimination<br />
directive. To obtain an opinion on<br />
whether age limits for dentists within the statutory<br />
health insurance system are compatible with the<br />
anti-discrimination directive, the Social Court <strong>of</strong><br />
Dortmund took recourse to the ECJ, which is responsible<br />
for interpreting the provisions <strong>of</strong> <strong>European</strong> law.<br />
The Social Court <strong>of</strong> Dortmund specifically requested<br />
the ECJ to rule on whether the <strong>European</strong> prohibition<br />
against age discrimination precludes the concept <strong>of</strong><br />
a reduction in performance with increasing age, as<br />
assumed by general life experience, as a justification<br />
for enacting age limits.<br />
It should be noted, however, that the idea that<br />
general life experience proves that performance is<br />
reduced with increasing age, as assumed by the<br />
Social Court <strong>of</strong> Dortmund, has not been conclusively<br />
proven. Rather, gerontological and other studies <strong>of</strong><br />
the influence <strong>of</strong> age on productivity have shown that<br />
the age factor has only limited predictive value when<br />
it comes to individual performance (cf. Eichenh<strong>of</strong>er,<br />
Gesetzliche Altersgrenze im Vertrags(zahn)arztrecht:<br />
Kann nach dem AGG alles beim Alten bleiben?, SGb<br />
2007, 580, 582 with references in footnotes 25 and<br />
26). It remains to be seen what position the ECJ will<br />
take with regard to this “general life experience” and<br />
whether it will accept this concept as justification for<br />
age discrimination.<br />
Solicitor Dr Berit Jaeger<br />
Ratajczak & Partners<br />
Berlin · Cologne · Essen · Freiburg ·<br />
Meissen · Munich · Sindelfingen<br />
Posener Straße 1<br />
71065 Sindelfingen<br />
Germany<br />
§
64 <strong>EDI</strong><br />
Case Studies<br />
Anterior maxilla reconstructed with autogenous calvarial bone block grafts<br />
restored with dental implants placed in a flapless image-guided procedure and<br />
immediately loaded with a prefabricated prosthesis – a case report<br />
The Key to Success<br />
Dr Guido Schiroli, MD, DDS, Genoa/Italy, Dr Alessandro Acocella, DDS, and Dr Giuseppe Spinelli,<br />
MD, Florence/Italy<br />
This study describes the use <strong>of</strong> image-guided implantological procedures in a complex case involving the rehabilitation <strong>of</strong> the<br />
anterior maxilla. Trauma to the teeth and alveolar process in the maxillary anterior region may cause severe bone deficiencies,<br />
resulting in ridge atrophy and maxillary retrognathism with loss <strong>of</strong> upper-lip support and undesirable changes <strong>of</strong> the interarch<br />
space, occlusal plane or interarch relationship.<br />
After bone augmentation with autogenous bone blocks harvested from the cranium, endosseous implants were immediately<br />
loaded with a prefabricated splinted bridge using a flapless approach and image-guided surgery. The calvarial area provides<br />
primary stability thanks to a cortical grafting procedure well suited for treating localized alveolar-ridge deficiencies, resulting<br />
in a very low resorption rate and highly dense structure. Image-guided surgery is optimal for determining the correct implant<br />
position and performing a safe flapless procedure. A pre-fabricated prosthesis using the Nobel Guide protocol was placed at<br />
the time <strong>of</strong> surgery for immediate loading and splinting <strong>of</strong> the implants at the previously grafted site. After a standard<br />
healing period, zirconia abutments were connected to the implants, which were then restored with metal-free aesthetic<br />
single-tooth crowns.<br />
Injury to the alveolar ridge <strong>of</strong> the anterior maxilla<br />
<strong>of</strong>ten causes severe deficiencies in the horizontal and<br />
vertical dimensions, leaving inadequate alveolar<br />
bone volume for standard treatment with osseointegrated<br />
implants. In addition, the lack <strong>of</strong> supporting<br />
bone may cause changes in the inter-arch space,<br />
occlusal plane and arch relationship, accompanied by<br />
maxillary retrognathism and a loss <strong>of</strong> upper-lip support.<br />
An adequate bone supply is a prerequisite for<br />
good aesthetic and biomechanical results, especially<br />
in the anterior maxilla. The reconstruction and augmentation<br />
<strong>of</strong> severely resorbed maxillary alveolar<br />
ridges for subsequent implant placement have<br />
become predictable procedures today, with different<br />
grafting materials and techniques being available<br />
[1-12]. The combination <strong>of</strong> autogenous bone grafts<br />
with osseointegrated implants to repair larger<br />
defects requires bone material from extraoral donor<br />
sites such as iliac crest or the calvarium [13-24]. Split<br />
calvarial block grafts have shown very low resorption<br />
rates, fast revascularization and good long-term<br />
results [20-24]. Many authors suggest delaying the<br />
insertion <strong>of</strong> implants for three to six months after<br />
the augmentation procedure and to wait an addi-<br />
tional three to six months before applying functional<br />
load [22-24].<br />
Submerged healing, a waiting period <strong>of</strong> three to six<br />
months before applying a functional load and a surgical<br />
re-entry procedure were long considered a prerequisite<br />
for osseointegration according to the Brånemark<br />
protocol [25]. There were reports that early loading<br />
associated with macromovements induced the<br />
formation <strong>of</strong> fibrous tissue between the implant surface<br />
and the bone [26-30]. However, several studies<br />
were carried out involving immediately loaded<br />
implants in animals and in humans, attesting to the<br />
viability <strong>of</strong> immediate loading with survival rates similar<br />
to those for implants with delayed loading [31-52].<br />
More recently, there have been reports that there is a<br />
continuum <strong>of</strong> implant micromovements ranging<br />
from safe to unsafe and that the threshold <strong>of</strong> unsafe<br />
movements may be between 50 and 150 μm [53-55].<br />
Micromovement below that threshold may be tolerated<br />
by the bone/implant interface, whereas exceeding<br />
the threshold may result in fibrous encapsulation<br />
<strong>of</strong> the implants [53-55]. Good bone quality, primary<br />
stability and rigid splinting <strong>of</strong> the fixtures seem to be<br />
the key to success for immediate-loading protocols.
Fig. 1<br />
Radiological<br />
stent with<br />
radiopaque<br />
teeth derived<br />
from provisional<br />
restoration<br />
shells.<br />
Fig. 2<br />
Adequate<br />
exposure <strong>of</strong> the<br />
donor site.<br />
Fig. 3<br />
Full-thickness<br />
flap exposing<br />
the recipient site<br />
and the residual<br />
alveolar crest.<br />
There are very little data available in literature<br />
regarding the immediate loading <strong>of</strong> implants inserted<br />
in previously grafted sites. Kupeyan et al [56] treated<br />
a patient with immediate loaded implants after<br />
four months <strong>of</strong> graft healing in the posterior maxilla<br />
using bone blocks harvested from the posterior iliac<br />
crest. Chiapasco et al [57] described six cases <strong>of</strong><br />
patients treated with immediately loaded implantsupported<br />
overdentures in severely atrophied<br />
mandibles after reconstruction <strong>of</strong> multi-layered<br />
autogenous calvarial grafts and reported a high<br />
implant survival rate.<br />
Predictable bone reconstruction, correct s<strong>of</strong>t-tissue<br />
management and correct planning <strong>of</strong> the implant<br />
positions are needed to obtain good aesthetic<br />
results, especially in the anterior maxilla.<br />
Teeth-in-an-hour and the Nobel Guide concept<br />
(Nobel Biocare AB, Gothenburg, Sweden) in combination<br />
with Procera planning s<strong>of</strong>tware program make it<br />
possible to preview the suggested implant placement,<br />
showing the exact positions and depths <strong>of</strong> the<br />
implants before surgery and designing a custom surgical<br />
template for implant placement via flapless<br />
surgery and a definitive or temporary prosthesis to<br />
be inserted immediately after surgery [58-62].<br />
The concept described, with its minimally invasive<br />
and simplified surgical procedures, reduces treatment<br />
time and post-surgical discomfort [58-62].<br />
Image-guided implantology results in more predictable<br />
and accurate implant placement [86] and<br />
optimized prosthetics [86].<br />
To our knowledge, the case presented here is the first<br />
case <strong>of</strong> severe post-traumatic localized atrophy <strong>of</strong> the<br />
anterior maxilla treated with calvarial bone grafts, flapless<br />
image-guided surgery and immediate loading.<br />
Clinical case<br />
<strong>EDI</strong> 65<br />
Case Studies<br />
A 23-year-old woman was referred to the Maxill<strong>of</strong>acial<br />
Division <strong>of</strong> the Faculty <strong>of</strong> Medicine (Orthopedic-Traumatologic<br />
Centre, Florence) because <strong>of</strong> traumatic loss<br />
<strong>of</strong> her anterior maxillary teeth and alveolar process<br />
after a motorcycle accident. Panoramic radiographs<br />
and CT scans were performed to exclude the presence<br />
<strong>of</strong> maxill<strong>of</strong>acial fractures. A provisional removable<br />
prosthesis was provided. After five months, the<br />
patient was recalled for a clinical follow-up and for<br />
planning an implant-supported fixed restoration.<br />
The clinical examination revealed severe bone loss<br />
<strong>of</strong> the maxillary anterior alveolar ridge, the absence<br />
<strong>of</strong> a labial sulcus and the loss <strong>of</strong> upper-lip support.<br />
For adequate reconstructive planning and to<br />
assess the residual bone, a CT scan was performed<br />
out with a barium-filled radiological stent (Ivoclar<br />
Vivadent) (Fig. 1), an exact duplicate <strong>of</strong> the provisional<br />
restoration. The digital CT scan (Simplant, Materialise<br />
NV, Belgium) showed a knife-edge ridge with<br />
complete loss <strong>of</strong> the buccal plate, a vertical and horizontal<br />
alveolar-ridge reduction and inadequate conditions<br />
for a conventional implant.<br />
To reconstruct the maxillary anterior alveolar-ridge<br />
defect three-dimensionally, we decided to harvest<br />
bone blocks from the calvarium because <strong>of</strong> their volume<br />
stability.<br />
The bone augmentation procedure was carried out<br />
under general anaesthesia with rhinotracheal intubation.<br />
The initial step involved designing and<br />
reflecting the s<strong>of</strong>t-tissue flap to permit adequate<br />
exposure <strong>of</strong> the recipient site (Fig. 2). The base <strong>of</strong> the<br />
incision must be wider than the crestal incision to<br />
maintain maximum blood supply. Buccal and palatal<br />
intrasulcular incisions were made around the adjacent<br />
teeth, including vestibular divergent releasing<br />
incisions to avoid the interdental papillae. A full<br />
mucoperiosteal flap was raised on the facial and<br />
palatal aspects and retracted (Fig. 3).
66 <strong>EDI</strong><br />
Case Studies<br />
The bone crest was curetted to remove all s<strong>of</strong>t tissue.<br />
While the CT scans provide an excellent image <strong>of</strong><br />
the defect, direct visualization is the only way to accurately<br />
assess its horizontal and vertical dimensions<br />
the amount <strong>of</strong> bone to be harvested from the donor<br />
site. A limited incision in the parietal region revealed<br />
the donor site. No hair needed to be shaved <strong>of</strong>f.<br />
The periosteum was incised and reflected and<br />
bone grafts were outlined using a cutting bur with a<br />
tip diameter <strong>of</strong> 1.5 mm parallel and about 5 cm away<br />
from distant from the midline. Three rectangular<br />
bone grafts 4 x 1 mm in size were designed at the<br />
donor site. The head <strong>of</strong> the round bur was shifted<br />
down to the diploe layer. The oozing <strong>of</strong> blood from<br />
the excision site revealed penetration to the appropriate<br />
anatomical level <strong>of</strong> the skull. The final step was<br />
to use a curved osteotome to free the intended bone<br />
grafts from the donor site, to avoid sourcing any<br />
material from the inner table <strong>of</strong> the skull. Bleeding<br />
from the diploe layer was controlled with bone wax<br />
and the scalp wound was closed using double layer<br />
vertical-mattress resorbable sutures.<br />
The harvested bone was placed in a sterile physiologic<br />
solution or in moist gauze to maintain as much<br />
the vitality <strong>of</strong> the block as possible. The recipient bed<br />
was prepared by perforating with a small, straight<br />
fissure bur. This created bleeding channels in the<br />
recipient bed, assisting the formation <strong>of</strong> neovasculature<br />
from the palatal periosteum. Once the recipient<br />
bed had been prepared, rotary instruments were<br />
used to shape the blocks <strong>of</strong> donor bone to fit the<br />
recipient bed as closely as possible. One block was<br />
adapted and attached on the buccal aspect <strong>of</strong> the<br />
alveolar ridge as a veneer graft, while a second block<br />
was adapted to serve as an onlay graft and attached<br />
to the first calvarial block. To secure the block grafts<br />
in place, two titanium alloy screws per block, at least<br />
1.5 mm in diameter, were used (Fig. 4).<br />
The bone blocks were secured using the lag-screw<br />
technique. With this technique, the hole that is<br />
drilled through the graft is wider than the screw<br />
thread. The bur used to drill the host bone should be<br />
smaller than the diameter <strong>of</strong> the screw. When the<br />
head <strong>of</strong> the screw is tightened against the block, the<br />
graft is compressed onto the host bone surface. The<br />
graft must remain immobile during healing.<br />
Sharp edges <strong>of</strong> the bone blocks were rounded <strong>of</strong>f<br />
with large diamond burs. Gaps around the block<br />
grafts were filled with bone chips harvested from the<br />
donor site. Several authors have reported that resorption<br />
can be reduced by covering the bone graft with<br />
a barrier membrane. However, we believe that barrier<br />
membranes are not necessary with calvarial block<br />
bone grafts, which already show minimal resorption.<br />
Once the graft is secured, closure <strong>of</strong> the s<strong>of</strong>t-tissue<br />
Fig. 4 Panoramic x-ray taken one month after the bone reconstruction: the retention<br />
screws are in place.<br />
Fig. 5 Histologic preparation <strong>of</strong> the external cortical layer<br />
<strong>of</strong> the calvarial graft at implant placement. The picture<br />
shows the typical compact osteonic structures <strong>of</strong> the calvarium,<br />
with signs <strong>of</strong> active remodelling and new vascular<br />
ingrowth. The vital bone containing osteocytes in the<br />
inner core <strong>of</strong> the osteons surrounded lamellar non-vital<br />
bone, suggesting that non-vital bone was recolonized by<br />
blood vessels and osteogenic cells via the Haversian canals (original magnification<br />
x 200; specimens stained with haematoxylin and eosin).<br />
flap requires primary closure without tension. An<br />
incision through the periosteum at the base <strong>of</strong> the<br />
flap usually allows for tissue coverage. Vertical mattress<br />
sutures (Vicryl 3-0) are used to resist any pull on<br />
the wound edges.<br />
The main complication associated with onlay bone<br />
grafts is wound dehiscence with graft exposure. Postoperative<br />
antibiotic and analgesic therapy was routinely<br />
practiced for seven days. Patients were also<br />
given chlorhexidine digluconate (0.2 %) for ten days,<br />
and the sutures were removed after ten to twelve<br />
days. No major complications or evident seromas<br />
were detected at the donor site. After four months <strong>of</strong><br />
healing, the fixation screws were removed under<br />
local anaesthesia, grafts were re-contoured, and the<br />
flap was repositioned to restore an adequate amount<br />
<strong>of</strong> attached gingiva for a better aesthetic result. During<br />
this procedure, a bone biopsy was removed with<br />
a trephine bur and processed for histological testing<br />
to study the vitality, revascularization and remodelling<br />
processes <strong>of</strong> the grafts (Fig. 5). The gingiva was<br />
conditioned by modification <strong>of</strong> the artificial teeth <strong>of</strong><br />
the provisional restoration using composite resin.<br />
After three months <strong>of</strong> s<strong>of</strong>t-tissue healing, an acrylic<br />
radiographic stent was prepared on the base <strong>of</strong> a<br />
diagnostic wax-up <strong>of</strong> the missing teeth according to<br />
the Nobel Guide computer-based planning protocol.<br />
To facilitate the double CT scanning technique and
6 7 8<br />
Fig. 6 Virtual treatment planning. The space between the implants has been<br />
respected as described in the literature.<br />
Fig. 7 Virtual treatment planning. The bone blocks cover and contain the implant bodies.<br />
Fig. 8 Virtual treatment planning. The positions <strong>of</strong> the implants correspond to the<br />
final restorations.<br />
Fig. 10 Provisional restoration, fabricated prior to surgery.<br />
Fig. 12 All implants are placed using the surgical guide and customized<br />
fixture mounts.<br />
subsequent matching <strong>of</strong> the two CT scans in the Procera<br />
s<strong>of</strong>tware, small holes filled with gutta-percha<br />
were inserted in the radiographic guide as reference<br />
points. The first CT scan was performed on the patient<br />
the radiographic stent in place, while a second scan<br />
was performed on the radiographic stent alone. The<br />
resulting CT DICOM files were converted into a file<br />
<strong>EDI</strong> 67<br />
Case Studies<br />
Fig. 9 Stereolithographic surgical stent according to the<br />
Nobel Guide system.<br />
Fig. 11 The abutments are integrated into the provisionals.<br />
format compatible with the Procera s<strong>of</strong>tware. The<br />
insertion <strong>of</strong> four Nobel Speedy Tapered implants<br />
(Nobel Biocare AB, Gothenburg, Sweden) was planned<br />
(Figs. 6 to 8), and a customized surgical template was<br />
developed using a stereolithographic process (Fig. 9).<br />
The surgical stent contained all the necessary information<br />
for creating the stone model, on which a temporary<br />
screw-retained prosthesis was fabricated prior<br />
to surgery (Figs. 10 and 11). On the day <strong>of</strong> surgery the<br />
surgical template was seated intraorally under local<br />
anaesthesia and secured with the anchor pins, verifying<br />
its correct position relative to the opposite arch. A<br />
special drill was used to punch four holes in the<br />
mucosa to access the bone. Low-speed, high-torque,<br />
internally irrigated drills were used to prepare the<br />
osteotomies via sequential cuttings through the surgical<br />
template following the standard protocol <strong>of</strong> the<br />
Nobel guide surgical kit. Finally, implants were placed<br />
at a torque <strong>of</strong> 35 Ncm (Fig. 12).
68 <strong>EDI</strong><br />
Case Studies<br />
Fig. 13 The provisional restoration placed at the time <strong>of</strong> surgery.<br />
Fig. 16 Orthopantomograph three months after implant<br />
insertion. All implants are osseointegrated.<br />
Fig. 18 Aesthetic results after the final restorations were<br />
cemented.<br />
The pre-fabricated temporary prosthesis was connected<br />
to the implants (Fig. 13), and an x-ray control<br />
was performed to assess the position <strong>of</strong> the<br />
implants beneath the bone and the adaptation <strong>of</strong><br />
the prosthesis to the implants (Figs. 14 and 15). Oral<br />
hygiene and postoperative home care instructions<br />
were provided, and the patient was dismissed under<br />
antibiotic and antiphlogistic therapy. Postoperative<br />
pain, bleeding and oedemas were minimal thanks to<br />
the flapless approach. After three months, an<br />
orthopantomograph was taken (Fig. 16), and a clinical<br />
check-up was performed after removal <strong>of</strong> the<br />
temporary prosthesis (Fig. 17).<br />
14 15<br />
Fig. 17 Clinical view before taking the definitive impression.<br />
Fig. 19 Lateral view showing a correct position <strong>of</strong> the<br />
restoration and good lip support.<br />
At three months and at subsequent monthly clinical<br />
examinations, the prosthesis was removed to<br />
ascertain implant mobility, absence <strong>of</strong> pain, paraesthesia,<br />
peri-implant bleeding and infection with suppuration.<br />
At three, six, twelve and 24 months, regular<br />
orthopantomographs and intraoral radiographs were<br />
obtained to detect radiolucent areas and to evaluate<br />
the marginal bone loss around the implants.<br />
At six months, the definitive restorations, consisting<br />
<strong>of</strong> zirconia abutments and zirconia single crowns (Figs.<br />
18 and 19) were inserted. There were no signs or symptoms<br />
<strong>of</strong> pain or peri-implant infection during any <strong>of</strong><br />
the clinical or radiological examinations (Fig. 20).<br />
Fig. 14<br />
X-ray taken at<br />
the time <strong>of</strong><br />
surgery.<br />
Fig. 15<br />
All provisional<br />
abutments fit<br />
the implant<br />
platform.
Fig. 20<br />
Orthopan -<br />
tomograph<br />
three months<br />
after the delivery<br />
<strong>of</strong> the definitive<br />
restoration.<br />
The crater-like peri-implant resorption pattern that<br />
frequently develops after the first few months <strong>of</strong><br />
occlusal loading was not observed (see Fig. 18).<br />
The patient was satisfied with the aesthetics, phonetics<br />
and function <strong>of</strong> her restoration (see Figs. 19 and 20).<br />
Discussion<br />
Implant dentistry has expanded the indications for<br />
fixed dental prosthetics even in the severely compromised<br />
dentition. Nevertheless, several factors are<br />
required to achieve optimal aesthetics and function<br />
in the anterior maxilla, such as the presence <strong>of</strong> adequate<br />
alveolar bone height and width and the quality<br />
<strong>of</strong> bone itself. If these requirements are not met,<br />
ideal implant placement cannot be achieved, jeopardizing<br />
the clinical outcome. If osseous deficiencies<br />
are adequately corrected using predictable ridge<br />
augmentation techniques, this helps achieve prosthetically<br />
ideal implants and a more natural s<strong>of</strong>t-tissue<br />
pr<strong>of</strong>ile, which in turn facilitates favourable crown<br />
anatomies and crown/implant length ratios and,<br />
consequently, aesthetic results.<br />
Several procedures have been proposed to achieve<br />
alveolar ridge augmentation in partially edentulous<br />
patients [1-12]. The use <strong>of</strong> allografts or bone chips in<br />
combination with a barrier membrane is useful<br />
where small bone defects, such as fenestrations or<br />
dehiscences, are present around implants inserted in<br />
post-extractive sites or where so-called self-spacemaking<br />
bony defects are present. Major reconstruction<br />
is needed for vertical and/or lateral augmentation<br />
<strong>of</strong> the alveolar crest. The use <strong>of</strong> particulate autografts<br />
or allografts covered by barrier membranes<br />
seems to produce controversial results. Some authors<br />
have reported that GBR technique is an effective procedure<br />
both in staged approaches [1,63] and concurrently<br />
with implant placement [64,65]. However, the<br />
use <strong>of</strong> allografts results in poor bone quality, while<br />
the use <strong>of</strong> semi-permeable barriers increases the cost<br />
<strong>of</strong> the surgical procedure and presents a higher infection<br />
risk due to wound dehiscence and membrane<br />
<strong>EDI</strong> 69<br />
Case Studies<br />
exposure [66,67]. Like Chiapasco [67], we prefer the<br />
reconstruction <strong>of</strong> narrow ridges with autogenous<br />
bone blocks without membrane in the case <strong>of</strong><br />
extended edentulous areas.<br />
Autogenous bone is still the “gold standard” for<br />
bone reconstruction because <strong>of</strong> its osteogenetic,<br />
osteoinductive and osteoconductive properties. A<br />
bone-block graft is preferred for this type <strong>of</strong> augmentation,<br />
since it provides a source <strong>of</strong> osteogenic cells<br />
as well as a rigid structure for mechanical support.<br />
An advantage <strong>of</strong> monocortical or cortico-trabecular<br />
bone-block grafts is better anatomical correspondence<br />
and adaptability to alveolar ridges. Bone-block<br />
grafts maintain their volume better than particulate<br />
material [68], but the real advantage is that they<br />
can be secured by screws, titanium miniplates or<br />
implants. The anterior iliac crest as a donor site is preferred<br />
by many authors because <strong>of</strong> the large quantity<br />
and high quality <strong>of</strong> the available bone and also<br />
because the harvesting techniques are simple.<br />
Recently, some authors have suggested that iliac<br />
crest bone results in an unacceptably high degree <strong>of</strong><br />
postoperative morbidity and resorption [69,70]. As a<br />
result, the use <strong>of</strong> other donor areas such as the cranium<br />
and mandible has been advocated [20-24, 71-78].<br />
It was found that membranous bone grafts resulted<br />
in higher survival rates and maintained their volume<br />
to a significantly greater extent than endochondral<br />
bone grafts [79,80], which may be related to the<br />
more rapid vascularization <strong>of</strong> membranous bone [81].<br />
Bone harvested from intraoral donor site and calvarial<br />
bone seem to have better osteogenetic and osteoinductive<br />
properties, related to higher concentrations <strong>of</strong><br />
bone morphogenetic proteins (BMP) and growth factors<br />
that may result in a greater capacity for bone<br />
repair and graft retention [82,83]. The pattern <strong>of</strong> onlay<br />
bone-graft resorption seems to be primarily determined<br />
by a graft’s microarchitecture (relative cortical<br />
and cancellous composition) rather than by its embryologic<br />
origin [84]. The calvarium primarily provides<br />
cortical grafts that are well-suited for veneer or onlay<br />
grafting <strong>of</strong> localized alveolar-ridge deficiencies, which<br />
seems to be a highly predictable procedure associated<br />
with a good long-term prognosis <strong>of</strong> implant-supported<br />
rehabilitations [20-24, 71-78].<br />
Advances in fixture design, new implant surfaces<br />
and new surgical techniques have radically changed<br />
the guidelines for clinical treatment with regard to<br />
the best time for implant placement and loading after<br />
grafting. Originally, the Brånemark surgical protocol<br />
stipulated that dental implants were to be submerged<br />
beneath the s<strong>of</strong>t tissue at the time <strong>of</strong> implant<br />
placement and allowed to heal for a minimum <strong>of</strong><br />
three months in the mandible and six months in the<br />
maxilla to achieve osseointegration [25]. Patients
70 <strong>EDI</strong><br />
Case Studies<br />
were also required to refrain from wearing a denture<br />
for at least two weeks after implant placement to<br />
facilitate s<strong>of</strong>t-tissue healing [25]. After the submerged<br />
healing period, a second intervention to uncover the<br />
implants was required. The original concern was that<br />
any implant micromovement might lead to fibroustissue<br />
encapsulation <strong>of</strong> the implant as a reparative<br />
response to physical trauma, resulting in failure to<br />
achieve osseointegration [53-55]. While the importance<br />
<strong>of</strong> the contribution by Brånemark and coworkers<br />
[25] should not be underestimated given the high<br />
success rates and predictable results that have been<br />
documented for more then 30 years, it is important to<br />
note that delayed loading was an empirical principle<br />
that had never been experimentally demonstrated.<br />
The current trend is not to consider implant movement<br />
per se as detrimental to osseointegration, but<br />
rather to consider a threshold <strong>of</strong> acceptable micromovement.<br />
It has been suggested that micromovement<br />
<strong>of</strong> 150 μm or more is excessive and therefore<br />
deleterious for osseointegration, while micromovement<br />
<strong>of</strong> less <strong>of</strong> 50 μm seems to be tolerated [53-55].<br />
During the 1970s, Ledermann [31] introduced the technique<br />
<strong>of</strong> immediately splinting and loading four<br />
transmucosal implants in the edentulous mandible<br />
with a bar-supported overdenture. The underlying<br />
theory was that rigid splinting <strong>of</strong> implants in the<br />
dense bone <strong>of</strong> the mandibular symphysis would prevent<br />
implant micromovement and allow effective<br />
healing and osseointegration under immediate-loading<br />
conditions. Since then, an increasing number <strong>of</strong><br />
publications on immediate loading have been published<br />
citing high success rates in mandibular and<br />
maxillary sites for single-tooth replacement, partial<br />
fixed restorations and full-arch prostheses [31-52].<br />
Most authors agree that good bone quality, primary<br />
stability with insertion torques up to 35-40 Ncm<br />
and rigid splinting <strong>of</strong> implants are important factors<br />
for the long-term survival <strong>of</strong> implants [45]. Several<br />
studies by Piattelli and coworkers [41-43] on both animals<br />
and humans have demonstrated that not only<br />
may immediate loading lead to successful osseointegration,<br />
but it may also increase the quantity <strong>of</strong> bone<br />
in direct contact with the implant surface.<br />
The dense structure <strong>of</strong> cortical calvarial bone grafts<br />
[21-24], which gives implants a high level <strong>of</strong> primary<br />
stability, and the immediate rigid splinting <strong>of</strong> fixtures<br />
with a screw-retained provisional restoration<br />
allowed us to immediate load implants inserted in<br />
previously grafted maxillary sites. The Teeth-in-an-<br />
Hour concept along with the Procera 3D planning<br />
s<strong>of</strong>tware (Nobel Biocare AB, Gothenburg, Sweden)<br />
allowed us to provide patients with fixed well-functioning<br />
restorations on implants in a single one-hour<br />
procedure. By using a custom template created from<br />
the primary CT scan, the provisional teeth can be fabricated<br />
before the implant procedure and inserted at<br />
the same time the implants are placed [58-62]. This<br />
system <strong>of</strong>fers more accurate and safer positioning <strong>of</strong><br />
dental implants via flapless surgery, reducing postoperative<br />
pain, oedema and bleeding [58-62].<br />
Conclusions<br />
The clinical results reported here have shown that<br />
immediate loading is feasible even in grafted anterior<br />
maxillary sites, shortening treatment times in<br />
patients with bone defects.<br />
The therapy is a clinical option even in correctly<br />
diagnosed patients with inadequate bone structure,<br />
provided that a proper reconstructive treatment plan<br />
is made. Patients expect good aesthetic results as<br />
much as they expect functional rehabilitation.<br />
Implant treatment in the aesthetic zone following<br />
injuries or the resection <strong>of</strong> a tumour present both<br />
aesthetic and functional challenges and require the<br />
use <strong>of</strong> the entire scientific, biological and technological<br />
armamentarium, from diagnosis to final therapy.<br />
An accurate CT scan showing the available bone<br />
supply plus the correct identification <strong>of</strong> viable<br />
implant positions using state-<strong>of</strong>-the-art diagnostic<br />
s<strong>of</strong>tware constitute an appropriate approach toward<br />
a three-dimensional determination <strong>of</strong> the bone<br />
quantity required for the implants and their superstructures.<br />
Decisions related to harvesting, donor<br />
sites and bone-block sizes can be made subsequent<br />
to the virtual planning phase.<br />
A computer driven approach seems to be a new<br />
“gold standard” for implant placement, as it assists in<br />
identifying the correct position <strong>of</strong> the implant and<br />
prosthetic platform, respecting adjacent anatomical<br />
structures and creating a correct emergence pr<strong>of</strong>ile <strong>of</strong><br />
the final restorations. In addition, this clinical approach<br />
<strong>of</strong>fers an opportunity to perform a safe and accurate<br />
flapless procedure with favourable outcomes.<br />
The use <strong>of</strong> cortical multi-layered split calvarial bone<br />
grafts with a very low resorption rate and highly dense<br />
structure, high primary stability and rigid connection <strong>of</strong><br />
the implants and accurate computer-guided planning<br />
and implant insertion are the keys to success. However,<br />
more studies and randomized clinical trials are needed<br />
to asses the predictability <strong>of</strong> the procedure.<br />
Contact Address<br />
Dr Alessandro Acocella<br />
Via Dante da Castiglione, 16/A Cercina, Sesto Fiorentino,<br />
Firenze, 5010, ITALY<br />
Phone: +39 333 2317982 (cell.)<br />
alessandroacocella@yahoo.it<br />
A list <strong>of</strong> references<br />
will be supplied by<br />
the editorial <strong>of</strong>fice<br />
on request.
72 <strong>EDI</strong><br />
Product Studies<br />
Clinical and biomechanical outcomes<br />
Platform Switching<br />
Xavier Vela-Nebot, MD, DDS, Xavier Rodríguez-Ciurana, MD, PhD<br />
and Maribel Segalà-Torres, MD, DDS, Barcelona/Spain<br />
After an implant is exposed to the oral environment, the biologic width is re-established and irreversible peri-implant bone loss<br />
occurs. This article looks at the tissues involved in this process and the amount <strong>of</strong> bone loss involved. Platform switching is<br />
proposed as a technique for reducing such bone resorption. The histological and biomechanical advantages <strong>of</strong> platform switching<br />
in implant therapy are assessed.<br />
Throughout the years, two-piece implants have<br />
demonstrated their performance and versatility in<br />
solving all types <strong>of</strong> functional and aesthetic problems.<br />
Numerous authors recommend placing<br />
implants adjacent to natural teeth with the platform<br />
2 to 3 mm below the cementoenamel junction (Fig. 1),<br />
i.e. at the same level as the crestal bone or even<br />
below it, to minimize the risk <strong>of</strong> exposing the metal<br />
<strong>of</strong> the implant collar or the abutment and to achieve<br />
an adequate vertical dimension and an aesthetic<br />
emergence pr<strong>of</strong>ile [1]. Peri-implant bone loss has<br />
been widely documented and quantified and is a<br />
usual radiographic finding. It is common to find a<br />
bone loss <strong>of</strong> 1.5 to 2.5 mm (Fig. 2) on the vertical axis<br />
and 1.5 mm on the horizontal axis, relative to the<br />
implant-abutment junction [2].<br />
Bone remodelling around the implant has traditionally<br />
been divided into three phases [3]:<br />
- Healing (first twelve months). After the surgical<br />
trauma related to drilling and implant insertion,<br />
new bone forms around the immobile implant. In<br />
this phase, the initial blood clot and the traumatized<br />
bone form a new bony callus.<br />
- Remodelling (from the time <strong>of</strong> loading until 18<br />
months). The implant is exposed to the oral environment<br />
and masticatory forces, and the crestal<br />
bone is remodelled according to the magnitude,<br />
direction, and frequency <strong>of</strong> the load. The amount <strong>of</strong><br />
bone loss observed and described in the literature<br />
in these first two phases ranges from 1.5 to 2 mm.<br />
- Stabilization (after 18 months). Stabilization is<br />
achieved after about 18 months from implant<br />
placement; it means that the forces acting on the<br />
implant and the remodelling capacity <strong>of</strong> the bone<br />
around it are in balance. After 18 months, lamellar<br />
bone is considered to have formed around the<br />
implant and true osseointegration is achieved.<br />
Fig. 1 Vertical position <strong>of</strong> the implant platform relative to the neighbouring teeth.<br />
Fig. 2 Common values <strong>of</strong> peri-implant bone loss.<br />
Bone loss in this final phase has been estimated at<br />
0.05 to 0.1 mm/year. This bone loss is similar to that<br />
found around natural teeth. The concepts and values<br />
indicated in the crestal bone remodelling and stabilization<br />
phases are still accepted today.
Fig. 3<br />
Biologic width:<br />
components and<br />
dimensions.<br />
Most bone loss is observed in the healing phase.<br />
This is where classical biomechanical theories are<br />
hard-pressed to explain things such as: the differences<br />
in bone development observed between onepiece<br />
and two-piece implants; the absence <strong>of</strong> bone<br />
loss when the implant is submerged and its appearance<br />
immediately after placing healing screws, even<br />
without loading; and the observation that the<br />
repeated screwing and unscrewing motion <strong>of</strong> the<br />
healing abutment leads to apical migration <strong>of</strong> the<br />
epithelial attachment and results in re-establishment<br />
<strong>of</strong> the bone level [4].<br />
Better knowledge <strong>of</strong> tissue biology and the experience<br />
and information gained in recent years with single-surgery<br />
implants, same-day implants, immediate<br />
loading, etc. have opened up new routes for understanding<br />
the process <strong>of</strong> immediate or early bone<br />
remodelling.<br />
Peri-implant bone loss<br />
We can therefore say today that peri-implant bone<br />
loss in the healing phase:<br />
- Does not seem to be related to implant shape and<br />
occurs with both root-form and cylindrical<br />
implants [5].<br />
- Is not related to when the implant is inserted; it is<br />
observed in both immediate and non-immediate<br />
implant placement [6].<br />
- Does not appear to be related to immediate<br />
implant loading. Some authors state that loads<br />
generating micro-motion <strong>of</strong> less than 120 microns<br />
are even favourable for bone apposition [7].<br />
- Is related to exposure <strong>of</strong> the implant to the oral<br />
environment [8] and is observed after four to five<br />
weeks both in two-stage implants, after uncovering<br />
them, and in single-stage implants when communication<br />
with the oral environment occurs<br />
immediately after implant placement.<br />
Following exposure <strong>of</strong> the implant to the oral environment,<br />
tissue biology ensures the formation <strong>of</strong><br />
connective tissue and an epithelial covering, creating<br />
a band <strong>of</strong> s<strong>of</strong>t tissues that forms a functional unit<br />
with a structural pattern. This is the biologic width<br />
similar to that found in natural teeth [9].<br />
<strong>EDI</strong> 73<br />
Product Studies<br />
Fig. 4 (a) Band <strong>of</strong> inflammatory tissue surrounding the<br />
implant-abutment interface in a cylindrical implant without<br />
platform switching. (b) Re-establishment <strong>of</strong> the biologic width.<br />
This biologic width is traditionally considered to<br />
be composed <strong>of</strong> a sulcus <strong>of</strong> approximately 1 mm,<br />
1 mm <strong>of</strong> junctional epithelium, and 1 mm <strong>of</strong> healthy<br />
supra-periosteal connective tissue. The sum <strong>of</strong><br />
these three structures gives us the known 3 mm<br />
biologic width whose function is defined by each <strong>of</strong><br />
its components (Fig. 3):<br />
- The epithelial components (sulcus and junctional<br />
epithelium) are the first defensive mechanisms for isolation<br />
from the internal medium, acting as a barrier.<br />
- The supra-periosteal connective tissue guarantees<br />
defence, support, nutrition, and filling.<br />
The biologic width thus maintains and ensures the<br />
protection <strong>of</strong> the internal environment by creating a<br />
tight seal around the implants to keep out external<br />
mechanical and biological agents.<br />
Numerous studies have related peri-implant bone<br />
loss to the presence and location <strong>of</strong> the implantabutment<br />
interface, stating that the more apical the<br />
interface is to the alveolar crestal bone, the greater is<br />
the bone loss [10]. It seems apparent that micromovement<br />
[11] between the implant and restorative<br />
components and, specially, bacterial colonization are<br />
the main causes <strong>of</strong> bone loss [12].<br />
When the implant is exposed to the oral environment<br />
(Fig. 4), the defensive epithelial barrier is broken,<br />
allowing bacteria to migrate and colonize the<br />
implant-abutment interface. According to Callan and<br />
co-workers, this occupation takes place in the first 25<br />
days. The bacteria involved in the process are mainly<br />
gram-negatives and anaerobes.<br />
The release <strong>of</strong> collagenase by the bacteria triggers<br />
the connective tissue defensive response, causing<br />
increased vascular patency that facilitates chemotaxis<br />
in defensive cells (polymorphonuclear cells,<br />
plasma cells and macrophages) whose function is to<br />
destroy bacteria. This means that a 1.1 mm band <strong>of</strong><br />
connective tissue around the implant-abutment<br />
interface contains copious amounts <strong>of</strong> inflammatory<br />
infiltrate [13].
74 <strong>EDI</strong><br />
Product Studies<br />
Fig. 5 Platform switching with a 5 mm diameter implant<br />
and a 4.1 mm diameter abutment.<br />
The bacterial lysis resulting from this defensive<br />
action releases endotoxins and osteoclast-activating<br />
factors and lowers the pH, which culminates in the<br />
bone resorption we observe radiographically. Typically,<br />
this bone loss is evident down to the first thread<br />
on the implant. It is an attempt to keep the sterile<br />
internal environment away from the inflammatory<br />
area. Loss <strong>of</strong> peri-implant crestal bone height causes<br />
movement <strong>of</strong> s<strong>of</strong>t tissue as a block (what we call the<br />
biologic width). At the same time, there is an epithelial<br />
migration as the body attempts to isolate the irritant<br />
apically.<br />
This recessive process finishes when the epithelium<br />
recovers its function as a barrier, bonding with<br />
hemidesmosomes to the implant surface in the area<br />
<strong>of</strong> the implant-abutment interface. Underneath,<br />
there is 1 mm <strong>of</strong> supra-periosteal connective tissue<br />
that preserves the defensive properties needed to<br />
keep the internal environment sterile.<br />
What we really see is that the dimensions <strong>of</strong> the<br />
biologic width are being re-established (the sum <strong>of</strong><br />
these areas explains the common bone loss [14]).<br />
Platform switching<br />
In response to this scenario <strong>of</strong> major peri-implant<br />
bone loss (which occurs irreversibly as all two-piece<br />
implants are exposed to the oral environment), the<br />
concept <strong>of</strong> platform switching was developed. Platform<br />
switching consists in creating a discrepancy<br />
between the diameter <strong>of</strong> the implant platform and<br />
the diameter <strong>of</strong> the prosthetic abutment. This is<br />
achieved by using implants with a 5-mm platform<br />
and undersized abutments (4.1 mm). A horizontal distance<br />
<strong>of</strong> 0.45 mm is thus created between the<br />
implant-abutment interface and the peri-implant<br />
tissues [15] (Fig. 5).<br />
When such a configuration is exposed to the oral<br />
environment, the normal reaction occurs: the contact<br />
Fig. 6 Comparison <strong>of</strong> bone loss between implants (a) without platform switching<br />
(control group) and (b) implants with platform switching (study group).<br />
surfaces between implant and abutment are colonized<br />
by gram-negative and anaerobic bacteria, and a<br />
band <strong>of</strong> connective tissue is generated with large<br />
amounts <strong>of</strong> inflammatory infiltrate around it. But the<br />
modification <strong>of</strong> the platform keeps the implant-abutment<br />
interface away from the peri-implant bone,<br />
minimizing the colonization <strong>of</strong> the biologic width<br />
and resulting in a statistically significant reduction in<br />
bone loss: p < 0.0005 [15] (Fig. 6).<br />
Radiographic analysis<br />
The authors have worked with platform switching in<br />
more than 1500 implant cases. The bone loss found<br />
around these implants is similar to that described in<br />
the literature [15], with bone loss in both the vertical<br />
and horizontal axes significantly reduced. The figures<br />
are as follows:<br />
- In implants with a 5-mm platform fitted with abutments<br />
<strong>of</strong> the same diameter (the usual method<br />
without platform switching): The mean vertical<br />
bone loss is 2 to 2.5 mm, and the horizontal bone<br />
loss is 1.5 mm [15].<br />
- In implants with a 5-mm platform fitted with<br />
undersized abutments <strong>of</strong> 4.1 mm (applying the<br />
concept <strong>of</strong> platform switching): Bone loss is up to<br />
70 percent less, with an average <strong>of</strong> 0.76 mm for vertical<br />
loss and 0.72 mm for horizontal loss [15].<br />
- The concept <strong>of</strong> platform switching has been incorporated<br />
in the coronal design <strong>of</strong> the Certain Prevail<br />
implants (Biomet 3i, Palm Beach Gardens, Florida,<br />
USA). The coronal dimensions <strong>of</strong> this implant are a<br />
4.8-mm diameter platform which connects to a<br />
4.1-mm abutment. This leaves a space <strong>of</strong> 0.35 mm<br />
at the edge around the implant-abutment interface.<br />
The Prevail implant platform also has a bevel<br />
<strong>of</strong> 15º, which raises the interface 0.10 mm above<br />
the collar. Taken as a whole, the effect is to move<br />
the implant-abutment interface further from the
Fig. 7 Amounts <strong>of</strong> bone loss in (a) implants without platform switching,<br />
(b) implants with platform switching and (c) Prevail implants.<br />
Fig. 8<br />
Biomechanical<br />
behaviour <strong>of</strong> an<br />
implant without<br />
platform<br />
switching.<br />
Finite element<br />
analysis.<br />
Fig. 9<br />
Biomechanical<br />
behaviour <strong>of</strong> an<br />
implant with<br />
platform<br />
switching.<br />
Finite element<br />
analysis.<br />
Fig. 10<br />
Variations in<br />
crown/implant ratio.<br />
(a) Initial situation<br />
without platform<br />
switching.<br />
(b) Peri-implant<br />
bone loss with platform<br />
switching.<br />
(c) Peri-implant<br />
bone loss without<br />
platform switching.<br />
<strong>EDI</strong> 75<br />
Product Studies<br />
peri-implant bone as done with 5 mm diameter<br />
implants connecting with 4.1 mm abutments.<br />
Worldwide multicentre clinical studies <strong>of</strong> this<br />
implant have shown up to 80 percent reduction in<br />
peri-implant bone loss, with average values <strong>of</strong><br />
0.65 mm on the vertical and the horizontal axis<br />
[16] after three years <strong>of</strong> loading (Fig. 7).<br />
Biomechanical and aesthetic considerations<br />
The use <strong>of</strong> wide-platform implants is indicated for:<br />
1. Improving resistance to occlusal forces. Using an<br />
abutment with the same diameter as the implant<br />
platform distributes the stress uniformly over the<br />
entire implant-abutment contact surface. This is<br />
especially important with wide-platform implants<br />
and is with no doubt a biomechanical advantage,<br />
even though it involves major peri-implant bone<br />
loss, a significant biological disadvantage (Fig. 8).<br />
2. Optimizing the emergence pr<strong>of</strong>ile. Using implants<br />
and abutments <strong>of</strong> the same diameter makes it easier<br />
to match the emergence pr<strong>of</strong>ile <strong>of</strong> implant-supported<br />
restorations with that <strong>of</strong> natural teeth.<br />
Platform switching involves using abutments with<br />
a smaller diameter than that <strong>of</strong> the implant platform.<br />
This limits the advantages <strong>of</strong> wide-diameter<br />
implants that have matching-diameter abutments.<br />
However, it results in better preservation <strong>of</strong> periimplant<br />
bone:<br />
1. Using the Prevail implant reduces the peri-implant<br />
bone loss. This implies a better preservation <strong>of</strong> cortical<br />
bone around the implant platform. Cortical<br />
bone is ten times more resistant to stresses than<br />
medullar bone, especially in front <strong>of</strong> the oblique<br />
forces. The internal connection <strong>of</strong> these implants<br />
increases the implant-abutment contact area.<br />
Although the abutment support on the implant<br />
platform is reduced, the stresses inside the<br />
implant are uniformly and progressively distributed,<br />
which makes the biomechanical behaviour<br />
<strong>of</strong> the Prevail implant superior to that <strong>of</strong> wideplatform<br />
implants and abutments <strong>of</strong> matching<br />
diameter. Results <strong>of</strong> finite-element analysis confirm<br />
this (Fig. 9). The creation <strong>of</strong> the biologic width<br />
causes vertical peri-implant bone loss that alters<br />
the initial crown/implant ratio and even inverts it,<br />
creating an unfavourable situation that reduces<br />
the long-term predictability <strong>of</strong> the restoration<br />
(Fig. 10).<br />
2. The literature on implant-supported restorations<br />
has widely documented the two options for<br />
achieving a good emergence pr<strong>of</strong>ile: using a wideplatform<br />
implant seated at the level <strong>of</strong> the crestal<br />
bone or a narrow-platform implant submerged in
76 <strong>EDI</strong><br />
Product Studies<br />
Fig. 11 Recommended subcrestal seating <strong>of</strong> the implant with platform<br />
switching to achieve a good emergence pr<strong>of</strong>ile.<br />
the crestal bone to compensate for the smaller<br />
platform diameter. With platform switching,<br />
undersized abutments are being used with a wideplatform<br />
implant. The implant thus must be slightly<br />
submerged (by approximately 1 mm) to obtain<br />
the correct emergence pr<strong>of</strong>ile. The Prevail implant<br />
is designed to be seated below the crestal bone. Its<br />
micro- and nanorough NanoTite surface extends<br />
up to the implant collar, which improves the boneimplant<br />
contact index (Fig. 11).<br />
Conclusions<br />
Using platform switching to increase the distance <strong>of</strong><br />
the implant-abutment interface from the crestal<br />
bone minimizes the attack on the biologic width<br />
caused by bacterial colonization. The result is<br />
reduced peri-implant bone loss [15]. This provides several<br />
obvious benefits:<br />
1. Reducing bone loss increases the bone-implant<br />
contact surface and enhances the area <strong>of</strong> the<br />
implant available for osseointegration (Fig. 12).<br />
2. The enhanced osseointegrated area is found mainly<br />
on the cervical third <strong>of</strong> the implant. This is crucial<br />
for preserving peri-implant cortical bone, because<br />
this is the area that best withstands biting forces,<br />
especially the oblique ones, and improves the<br />
crown/implant length ratio. Platform switching<br />
therefore improves the biomechanical properties<br />
<strong>of</strong> implant-supported restorations and their longterm<br />
predictability [17] (see Figs. 8 and 9).<br />
3. Platform switching also helps retain peri-implant<br />
crestal bone, thus providing good support for the<br />
s<strong>of</strong>t tissues. This is extremely important in anterior<br />
restorations in which preserving the buccal plate<br />
and maintaining the peri-implant crestal bone<br />
determines gingival aesthetics and the health <strong>of</strong> the<br />
implant-supported restorations (Figs. 13 and 14).<br />
Fig. 12<br />
Enhanced<br />
osseointegrated<br />
surface<br />
(a) without<br />
platform<br />
switching and<br />
(b) with platform<br />
switching.<br />
Fig. 13<br />
Tooth 11 restored<br />
with a Certain<br />
Prevail implant<br />
after three years<br />
<strong>of</strong> follow-up.<br />
Fig. 14<br />
Tooth 15 restored<br />
with a Certain<br />
Prevail implant<br />
after four years<br />
<strong>of</strong> follow-up.<br />
Note the excellent<br />
preservation<br />
<strong>of</strong> peri-implant<br />
bone, guaranteeing<br />
a good gingival<br />
support.
References<br />
77<br />
[1] Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations<br />
in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxill<strong>of</strong>ac<br />
Implants 2004;19(SUPPL):43-61.<br />
[2] Tarnow DP, Cho SC, Wallace SS. The effect <strong>of</strong> inter-implant distance on the<br />
height <strong>of</strong> inter-implant bone crest. J Periodontol 2000;71:546-549.<br />
[3] Branemark PI, Zarb GA, Albrektsson B. Tissue-integrated prostheses:<br />
osseointegration in clinical dentistry. Quintessence Publishing 1985.<br />
[4] Abrahamson I, Berglundh T, Lindhe J. The mucosal barrier following abutment<br />
dis/reconnection. An experimental study in dogs. J Clin Periodontol<br />
1997;24:568-572.<br />
[5] Daftary F. Dentoalveolar morphology: evaluation <strong>of</strong> natural root form<br />
versus cylindrical implant fixtures. Pract Periodontics Aesthet Dent<br />
1997;9(4):469-77.<br />
[6] Araújo MG, Sukekava F, Wenström JL, Lindhe J. Ridge alterations following<br />
implant placement in fresh extraction sockets: an experimental study in the<br />
dog. Pract Periodontics Aesthet Dent 2000;12(9):817-824.<br />
[7] Romanos G, Toh Ch G, Siar Ch H, Swaminathan D, Ong A H. Histologic and<br />
histomorphometric evaluation <strong>of</strong> peri-implant bone subjected to immediate<br />
loading: an experimental study with macaca fascicularis. Int J Oral Maxill<strong>of</strong>ac<br />
Implants 2002;17:44-51.<br />
[8] Hermann J S, Cochran D L, Nummikoski P V. Crestal bone changes around<br />
titanium implants. A radiographic evaluation <strong>of</strong> unloaded nonsubmerged and<br />
submerged implants in the canine mandible. J Periodontol 1997;68:1117-30.<br />
[9] Gargiulo AW, Wentz FM, Orban B. Dimensions and relations <strong>of</strong> the dentogingival<br />
junction in humans. J Periodontol 1961;32:261-267.<br />
[10] Hermann J S, Buser D, Schenk R K, Schoolfield J D, Cochran D L. Biologic<br />
width around one- and two-piece titanium implants. A histometric evaluation<br />
<strong>of</strong> unloaded nonsubmerged and submerged implants in the canine mandible.<br />
Clin Oral Impl Res 2001;12:559-71.<br />
<strong>EDI</strong> 77<br />
Product Studies<br />
[11] King G N, Hermann J S, Schoolfield J D, Buser D, Cochran D L. Influence <strong>of</strong><br />
the size <strong>of</strong> the microgap on crestal bone levels in non-submerged dental<br />
implants: a radiographic study in the canine mandible. J Periodontol<br />
2002;10:1111-1117.<br />
[12] Callan D P, Cobb C M, Williams K B. DNA probe identification <strong>of</strong> bacteria colonizing<br />
internal surfaces <strong>of</strong> the implant-abutment interface: a preliminary<br />
study. J Periodontol 2005;76:115-120.<br />
[13] Berglundh T, Lindhe J, Ericsson I, Marinello C P, Liljenberg B. S<strong>of</strong>t tissue reactions<br />
to the novo plaque formation at implants and teeth. An experimental<br />
study in the dog. Clin Oral Implant Res 1992;3:1-8.<br />
[14] Berglundh T, Lindhe J. Dimension <strong>of</strong> the peri-implant mucosa. Biological<br />
width revisited. J Clin Periodontol 1996;23:971-3.<br />
[15] Vela X, Rodríguez X, Rodado C, Segalà M. Benefits <strong>of</strong> an implant platform<br />
modification technique to reduce crestal bone resorption. Implant Dent<br />
2006;15(3):313-320.<br />
[16] Calvo JL, Sáez MR, Pardo G, Muñoz E. Immediate provisionalization on a<br />
new implant design for esthetic restoration and preserving crestal bone.<br />
Implant Dent 2007;16(2):155-164.<br />
[17] Kitamura E, Stegaroiu R, Nomura S, Miyakawa O. Biomechanical aspects <strong>of</strong><br />
marginal bone resorption around osseointegrated implants: considerations<br />
based on a three-dimensional finite element analysis. Clin Oral Impl Res<br />
2004;15;401-412.<br />
Contact Address<br />
Barcelona Osseointegration Research Group (BORG)<br />
Sant Martí Nº 43<br />
08470 Sant Celoni (Barcelona)<br />
SPAIN<br />
Phone: +34 619 284474<br />
headquarters@borgroup.net
78 <strong>EDI</strong><br />
Product Studies<br />
Prosthodontic reconstruction <strong>of</strong> the edentulous maxilla with a removable denture<br />
supported on six SynCone abutments<br />
Practice Success with<br />
Telescopic Crowns<br />
Dr Krzyszt<strong>of</strong> Chmielewski, Gdansk/Poland<br />
In the past few years, implantology has developed successfully even under sometimes difficult conditions, for example in<br />
Eastern and Southern <strong>European</strong> countries. This article shows how Dr Krzyszt<strong>of</strong> Chmielewski performs implantology to a very<br />
high standard in Poland and successfully places Ankylos implants.<br />
The different treatment concepts and solutions in<br />
the Ankylos implant system are very obvious. The<br />
benefits derived from the design <strong>of</strong> the implant, its<br />
TissueCare connection and platform-shifting are the<br />
key to long-term success and provide the background<br />
<strong>of</strong> the TissueCare Concept. Reconstruction <strong>of</strong> the<br />
edentulous maxilla is a very common challenge for<br />
us in meeting patient expectations and achieving<br />
long-term stable results.<br />
A removable denture supported by a bar or telescopic<br />
crowns is one solution to give the older<br />
patient a compromise between function, esthetics<br />
and the highly important accessibility for hygiene.<br />
Hygiene can be difficult in elderly patients with a full<br />
arch implant-supported reconstruction <strong>of</strong> the maxilla<br />
for whom even the use <strong>of</strong> dental floss between their<br />
existing natural teeth is problematic. If I can propose<br />
to the patient a treatment which will assist him in<br />
routine oral hygiene and which is very comfortable<br />
and also stable, one <strong>of</strong> my first choices is a removable<br />
denture supported with Ankylos SynCone taper abutments.<br />
The great advantage <strong>of</strong> this taper connection<br />
is reliable friction and precision coming from the production<br />
process. The first time I had an opportunity<br />
<strong>of</strong> holding a SynCone abutment and Gold Cap in my<br />
hands, I was amazed at how well the components fit<br />
together and I had no doubt that they would work in<br />
the mouth as well. To deal with different situations<br />
the abutments come with two different taper conical<br />
heads: 4 and 6 degrees.<br />
The case presented in this article shows how<br />
patient expectations regarding function, esthetics,<br />
hygiene and reasonable treatment costs can be met<br />
(Figs. 1 to 31).<br />
A 62 year old female patient with an edentulous<br />
maxilla and problems due to the mobility <strong>of</strong> her full<br />
upper denture came to my practice seeking a solution<br />
to her problem. After various treatment concepts<br />
were explained, the patient decided on a removable<br />
Fig. 1 OPG during planning with template in the mouth. Fig. 2 Full denture with drilling sleeves mounted.
Fig. 3<br />
Incision on<br />
the top <strong>of</strong><br />
the ridge.<br />
Fig. 4<br />
Drilling through<br />
the template<br />
with 2.0 mm<br />
pilot drill to<br />
mark the drilling<br />
point on the top<br />
<strong>of</strong> the bone.<br />
Fig. 5<br />
Implant sites<br />
prepared.<br />
Fig. 6<br />
Ankylos implant<br />
during placement<br />
in the bone.<br />
Grooves on the<br />
implant carrier<br />
help to submerge<br />
the implant<br />
correctly.<br />
Fig. 7<br />
Six Ankylos<br />
implants in<br />
final positions.<br />
Fig. 8<br />
After six months<br />
<strong>of</strong> healing<br />
re opening <strong>of</strong> the<br />
implant sites and<br />
placement <strong>of</strong><br />
sulcus formers.<br />
Fig. 9<br />
Impression three<br />
weeks after<br />
secondstage surgery.<br />
Closed tray<br />
transfer copings<br />
were used.<br />
Fig. 10<br />
Master cast<br />
after un screwing<br />
<strong>of</strong> the transfer<br />
copings.<br />
3 4<br />
5 6<br />
7 8<br />
9 10<br />
<strong>EDI</strong> 79<br />
Product Studies
80 <strong>EDI</strong><br />
Product Studies<br />
11 12<br />
13 14<br />
15<br />
17 18<br />
16<br />
Fig. 11<br />
15 degrees<br />
angulated<br />
SynCone abutment<br />
with six<br />
degree tape.<br />
Fig. 12<br />
To establish the<br />
correct axis<br />
between the<br />
abutments dedicated<br />
paralleling<br />
pins are used.<br />
Fig. 13<br />
In the first<br />
implant position<br />
on the left side it<br />
was necessary to<br />
customize the<br />
abutment.<br />
Fig. 14<br />
Prefabricated<br />
gold caps placed<br />
on abutments.<br />
Fig. 15<br />
The caps were<br />
milled to reduce<br />
the external size.<br />
To improve adhesion,<br />
the gold<br />
caps were sand<br />
blasted.<br />
Fig. 16<br />
Galvano secondary<br />
cap placed in<br />
the customized<br />
abutment.<br />
Fig. 17<br />
The metal<br />
construction<br />
was additionally<br />
covered with<br />
opaquer.<br />
Fig. 18<br />
Try-in <strong>of</strong> the<br />
construction on<br />
the model.
Fig. 19<br />
Before unscrewing<br />
the abutments<br />
acrylic<br />
jigs were made.<br />
Fig. 20<br />
At every stage<br />
the technician<br />
uses a dynamometric<br />
key.<br />
Fig. 21<br />
Placement <strong>of</strong><br />
the abutments<br />
in the mouth.<br />
Fig. 22<br />
Abutments are<br />
screw-retained<br />
with 15 Ncm<br />
force.<br />
Figs. 23 and 24<br />
Try-in <strong>of</strong> the<br />
caps.<br />
Fig. 25<br />
Try-in <strong>of</strong> the<br />
metal<br />
construction.<br />
Fig. 26<br />
The construction<br />
should be above<br />
the level <strong>of</strong> the<br />
s<strong>of</strong>t tissue to<br />
leave room for<br />
acrylic resin.<br />
19 20<br />
21 22<br />
23 24<br />
25<br />
26<br />
<strong>EDI</strong> 81<br />
Product Studies
82 <strong>EDI</strong><br />
Product Studies<br />
27 28<br />
29 30<br />
Fig. 31 Final result in the patient’s mouth.<br />
denture supported on Ankylos SynCone taper crowns.<br />
Before the surgery, planning took place with an OPG<br />
and to obtain more information regarding the best<br />
implant position I made a surgical template using an<br />
acrylic denture with fixed drilling sleeves. The<br />
patient’s next X-ray was taken with the template in<br />
the mouth. On the OPG I could see the possible positions<br />
for the implants. More than six sleeves were<br />
used in the template to provide more options during<br />
planning. The surgery was then performed, followed<br />
by a six-month healing period. In the meantime, the<br />
patient wore her existing denture as a temporary<br />
restoration. Placing the Ankylos implants 1 mm below<br />
the ridge produces less risk <strong>of</strong> accidental loading by<br />
the temporary denture. After second-stage surgery<br />
and healing <strong>of</strong> the s<strong>of</strong>t tissue, an impression was<br />
taken using the closed tray technique and sent to the<br />
laboratory. On the master cast the technician chose<br />
Fig. 27<br />
SynCone Copings<br />
are fixed to the<br />
metal elements.<br />
Fig. 28<br />
Bite registration<br />
with acrylic resin.<br />
Fig. 29<br />
Impression with<br />
the frame.<br />
Fig. 30<br />
Veneering <strong>of</strong> the<br />
construction with<br />
acrylic resin.
angulated Ankylos SynCone abutments and placed<br />
them in the optimum position to allow space for the<br />
secondary telescopes. The implants were placed in the<br />
maxilla with divergence between the left and right<br />
sides due to the anatomic situation.<br />
In five locations the technician used SynCone abutments<br />
with 15 degree angulation and proper gingival<br />
height, but in position 24 the 22.5 degree angulation<br />
<strong>of</strong> the abutment was not sufficient to obtain the correct<br />
axis. In this position, the technician customized<br />
the abutment. Every customizing <strong>of</strong> a prefabricated<br />
SynCone abutment creates another problem because<br />
it is no longer possible to use prefabricated secondary<br />
telescopic crowns (gold caps). In this case, we<br />
decided to place a Galvano cap as the secondary telescope.<br />
This solution fits well but friction is less predictable<br />
over time compared with prefabricated elements.<br />
From my experience, use <strong>of</strong> one Galvano<br />
among five other prefabricated SynCone elements<br />
has no influence on denture retention.<br />
The next step for the technician was the preparation<br />
<strong>of</strong> the metal frame. The goal <strong>of</strong> this frame is to<br />
strengthen the denture, provide retention for acrylic<br />
veneering and limit the palatal dimension. The external<br />
size <strong>of</strong> the gold caps can be reduced by milling<br />
Contact Address<br />
Dr Krzyszt<strong>of</strong> Chmielewski<br />
Vice President <strong>of</strong> the Polish Academy<br />
<strong>of</strong> Esthetic Dentistry<br />
Implantology and Esthetic Dentistry Clinic<br />
Member <strong>of</strong> the “Omega Gruppe”<br />
Gdansk<br />
POLAND<br />
biuro@kgcdent.pl<br />
<strong>EDI</strong> 83<br />
Product Studies<br />
prior to creation <strong>of</strong> the metal frame. It also helps to<br />
avoid a bulky internal metal construction <strong>of</strong> the denture.<br />
For optimum fitting the gold caps should be<br />
glued to the metal frame in the patient’s mouth.<br />
After that I took an impression <strong>of</strong> the construction<br />
with a custom tray to enable the technician to veneer<br />
the frame with acrylic resin. The final result is very<br />
satisfactory for the patient. The function and esthetics<br />
give the patient’s life a new dimension. The construction<br />
appears to be as rigid as a bridge. The<br />
absence <strong>of</strong> movement, very stable position and<br />
reduced size especially on the palatal side are common<br />
with non-removable constructions but in this<br />
case the patient has a further advantage: she can<br />
remove the denture for cleaning purposes.
84 <strong>EDI</strong><br />
Product Studies<br />
Overview <strong>of</strong> sealing options to prevent peri-implantitis<br />
caused by re-infection from assembled implants<br />
Gap Sealing<br />
Christian Krenkel, Salzburg/Austria<br />
Peri-implantitis denotes inflammatory diseases <strong>of</strong> the hard and s<strong>of</strong>t tissues around dental implants (Fig. 1). A variety <strong>of</strong> etiologic<br />
factors come into play [1-5]. The list <strong>of</strong> causes was formerly led by overload situations, poor gingival conditions and excessive<br />
plaque accumulation. Additional mechanisms were identified more recently, including re-infection from intra-implant spaces<br />
[6]. The dental industry is currently undertaking a variety <strong>of</strong> efforts to eliminate or minimize this pathogenic factor.<br />
The goal is to effectively seal any gaps between implants and superstructures, establishing a barrier that cannot be penetrated<br />
by micro organisms.<br />
Various recent studies have addressed the question<br />
<strong>of</strong> how peri-implantitis can be prevented and treated<br />
[7, 8]. Spurred by these investigations, ways <strong>of</strong> sealing<br />
the internal spaces <strong>of</strong> assembled implants have<br />
increasingly become a focus <strong>of</strong> attention. Intraimplant<br />
gaps and cavities are not a recent discovery<br />
but have always been known to exist in principle.<br />
Numerous practitioners had criticized a putrid smell<br />
that would emanate from implant sites on (deliberate<br />
or incidental) re-entry. However, appropriate<br />
steps to remedy this situation were rarely taken.<br />
Moreover, manufacturers have consistently maintained<br />
that existing implant-abutment interfaces are<br />
safe from leakage. Authors <strong>of</strong> studies on peri-implantitis<br />
first expressed suspicions that infections <strong>of</strong> hard<br />
and s<strong>of</strong>t tissue might be nourished by pathogen colonization<br />
from inside implants [9, 10]. These suspicions<br />
were not, however, supported by hard evidence.<br />
Medications were introduced to treat s<strong>of</strong>t-tissue diseases,<br />
including PerioChip (Dexcel Pharma, Alzenau,<br />
Germany) and Duraplant (Lege Artis Pharma, Dettenhausen,<br />
Germany). They are designed to control<br />
mucosal infections at the subgingival level by intrasulcular<br />
administration. Their active ingredients may<br />
well be effective, yet they presumably cannot resolve<br />
these infections in a lasting fashion unless the<br />
underlying cause is also eliminated.<br />
Schmüdderich was the first to present an analysis<br />
<strong>of</strong> intra-implant pathogen colonization based on<br />
light and electron micrographs [6]. His studies resulted<br />
in a highly innovative sealant characterized by<br />
bactericidal activity in addition to sealing intraimplant<br />
spaces. Schmüdderich’s paper and marketing<br />
for the sealant have apparently set <strong>of</strong>f a spark. The<br />
fact that manufacturers have taken a substantial<br />
interest in hermetic sealing between implants and<br />
their superstructures became clear at the 2007 International<br />
<strong>Dental</strong> Show (IDS) in Cologne, Germany.<br />
Recent studies have corroborated the existence <strong>of</strong><br />
relationships between peri-implantitis and re-infection<br />
from implants [7, 8]. They specifically pointed out<br />
that intra-implant gaps and cavities are very large<br />
from a microbiological viewpoint. Thus the dimensional<br />
proportions are conducive to pathogen colonization.<br />
Intra-implant gaps and cavities<br />
Intra-implant spaces are in direct contact with the<br />
oral cavity (and its microorganisms) via gaps along<br />
the implant threads. Structural drawings <strong>of</strong> implant<br />
manufacturers clearly demonstrate that gaps and<br />
cavities are indeed present (Fig. 2a). Their presence is<br />
also apparent from radiographs, since most current<br />
implants are made <strong>of</strong> radiolucent titanium (Fig. 2b).<br />
Those gaps are so large that they <strong>of</strong>fer no resistance<br />
to pathogen invasion. Figure 3 illustrates the<br />
gap size <strong>of</strong> an implant-abutment interface. Documented<br />
sizes range from 4 to 125 μm [11]. Figure 4 illustrates<br />
the dimensions <strong>of</strong> various intraoral microorganisms<br />
by way <strong>of</strong> comparison. Here the documented<br />
range is 1 to 10 μm [12]. Capillary forces, known to be<br />
inversely related to gap size, also come into play (Fig. 5).<br />
These conditions are ideal for pathogen invasion<br />
and intra-implant survival. Micromovements <strong>of</strong> the
Fig. 1<br />
This implant at<br />
site 36 exhibits<br />
peri-implantitis<br />
and a vertical<br />
bone pocket<br />
extending down<br />
to the apex.<br />
1 2b<br />
2a<br />
Fig. 2a Cross-sectional schematic representation<br />
<strong>of</strong> an implant stack (implant, abutment<br />
and restoration). Red areas indicate<br />
the cavities left upon assembly.<br />
Fig. 3 Scanning electron micrograph (SEM) <strong>of</strong> an implantabutment<br />
interface. The marginal gaps are clearly visible.<br />
abutment during mastication are another factor. They<br />
are associated with a pump-suction effect that will<br />
further promote exchange <strong>of</strong> media between the<br />
intra-implant and peri-implant spaces [13].<br />
Based on current data obtained by scanning electron<br />
microscopy, it seems unlikely that manufacturers<br />
can possibly minimize the gap situation to the<br />
point <strong>of</strong> obtaining an effective seal against pathogen<br />
invasion. Even the greatest manufacturing precision<br />
cannot eliminate the need for interposing some<br />
material to compensate for the surface roughness <strong>of</strong><br />
implants and abutments.<br />
Current sealing techniques<br />
<strong>EDI</strong> 85<br />
Product Studies<br />
Fig. 2b Radiographic view <strong>of</strong> three implants with single-restoration abutments<br />
and fixation screws. Dark shadows indicating the persisting cavities are readily<br />
visible.<br />
Fig. 4 Sizes <strong>of</strong> microorganisms compared to implant marginal<br />
gaps. Intra-implant spaces remain unprotected, since<br />
bacteria can move freely in and out <strong>of</strong> the cavities virtually<br />
without meeting any resistance.<br />
While ingenious attempts have been undertaken to<br />
accomplish sealing, some <strong>of</strong> these approaches have<br />
been less than plausible.<br />
One dental manufacturer (m&k dental Jena, Kahla,<br />
Germany) promises that implant-abutment interfaces
86 <strong>EDI</strong><br />
Product Studies<br />
Fig. 5 Capillary forces<br />
are particularly strong<br />
in narrow gaps. They<br />
will contaminate the<br />
intra-implant cavities<br />
by actively drawing<br />
(microbially charged)<br />
fluids.<br />
Fig. 6 Silicones are another option to seal the intraimplant<br />
spaces.<br />
can be hermetically sealed with a gold foil. Efforts like<br />
this deserve credit for acknowledging that gaps are<br />
present and that they do require sealing. The problem<br />
should not, however, be addressed by establishing<br />
contact between dissimilar metals. Various<br />
authors have shown that this situation will result in<br />
salivary electrolyte streams causing the metals to<br />
corrode by ion migration [14, 15]. The proposed gold<br />
seal will be rather short-lived, not least because an<br />
extremely s<strong>of</strong>t form <strong>of</strong> gold must be used as a<br />
sealant to achieve the desired effect.<br />
Another manufacturer (GDF, Rosbach, Germany)<br />
has introduced a silicone material by the name <strong>of</strong><br />
ImplaSeal (Fig. 6). This self-hardening material works<br />
much like sanitary silicone sealants. It is supplied in<br />
plastic syringes along with several syringe tips. GDF’s<br />
concept introduces another source <strong>of</strong> gap formation,<br />
since the material is bound to contract during setting.<br />
There are also hygienic issues: only the syringe<br />
tips are replaced, while the syringe itself is reusable.<br />
Schmüdderich’s study describing a new sealant has<br />
been mentioned previously in this article. The product<br />
was introduced in 2007 and is being distributed<br />
by Hager & Werken (Duisburg, Germany) under the<br />
trade name <strong>of</strong> GapSeal (Fig. 7). The usefulness <strong>of</strong><br />
GapSeal is supported by current publications [6, 7, 8]<br />
and user reports [16]. The author’s own experience<br />
confirms these findings. All concur in believing that<br />
this product is currently the most effective sealant in<br />
the market, thanks to its logical design in terms <strong>of</strong><br />
consistency (long-term s<strong>of</strong>tness), ingredients (highly<br />
viscous silicone base and thymol), application (autoclavable<br />
applicator) and sterility (sterile carpules for<br />
single use). The material <strong>of</strong>fers excellent positional<br />
stability due to its high viscosity. Being highly resist-<br />
ant to washing out, it can be used even under<br />
cement-retained superstructures. All sterility requirements<br />
are met. The kit supplied is convenient to use<br />
and exhibits a good cost-benefit ratio. GapSeal has<br />
been clinically tested for ten years, <strong>of</strong>fering implantologists<br />
the special advantage <strong>of</strong> having a well-documented<br />
and reliable product at their disposal [8].<br />
Summary and discussion<br />
Fig. 7 GapSeal is a highly viscous material. A special<br />
applicator is used to load the sealant into implant<br />
cavities without air inclusions.<br />
Treatment considerations have resulted in attempts<br />
to prevent peri-implantitis by avoiding its causes. Reinfection<br />
from intra-implant spaces is a key pathogenic<br />
factor. Gaps along the implant-abutment interface<br />
are the pathway <strong>of</strong> such re-infection. They create<br />
a situation in which pathogens are directly exchanged<br />
between the oral cavity and intra-implant cavities.<br />
Efforts have been made to develop sealing techniques.<br />
While some attempts have not been successful,<br />
they should be given credit for acknowledging<br />
that gaps and cavities do exist in assembled<br />
implants. A variety <strong>of</strong> strategies have been used to<br />
establish hermetic sealing against pathogens. This is<br />
a logical goal, as existing conditions have previously<br />
allowed bacteria to migrate into implants, where<br />
they find a favourable environment for survival, such<br />
that they will propagate and subsequently migrate<br />
back into the oral cavity. Implant materials cannot by<br />
themselves ensure an adequate seal, no matter how<br />
carefully an implant system is manufactured. Consequently,<br />
a highly viscous sealant needs to be interposed.<br />
This material should <strong>of</strong>fer maximum bactericidal<br />
activity and resistance to aging. Peri-implantitis<br />
– if only cases maintained by re-infection such as<br />
those described in this article – could be successfully<br />
avoided in this way. Now that the problem has<br />
become apparent, it is expected that manufacturers
will press ahead with eliminating this disadvantage<br />
<strong>of</strong> assembled implants. New products are going to be<br />
<strong>of</strong>fered that will expand the range <strong>of</strong> potential solutions.<br />
GapSeal as a universal sealant has yielded the<br />
best results so far.<br />
References<br />
Contact Address<br />
Christian Krenkel, MD, DMD, PhD<br />
Clinic <strong>of</strong> Oral and Maxill<strong>of</strong>acial Surgery<br />
Paracelsus Medical University<br />
Federal Medical Center Salzburg<br />
Landesklinik Salzburg<br />
Müllner Hauptstrasse 48<br />
A-5020 Salzburg<br />
AUSTRIA<br />
Phone: +43 662 4482-3601<br />
Fax: +43 662 4482-884<br />
c.krenkel@salk.at<br />
www.endodistraction.com<br />
<strong>EDI</strong> 87<br />
Product Studies<br />
[1] Albrektsson, T., Isidor, F.: Consensus report <strong>of</strong> session IV. In: Lang, N. P.,<br />
Karring, T. (Hrsg). Proceedings <strong>of</strong> 1st <strong>European</strong> Workshop on Perio dontology.<br />
London: Quintessence Publishing Co., Ltd. 1994 (365-369).<br />
[2] Ratka-Krüger, P., Horodko, M., Mayer, M.: Ätiologie, Diagnostik, Therapie<br />
und Prävention der Peri-implantitis. ZM 91, 23, 2001 (50-56).<br />
[3] Spiekermann, H.: Peri-implantäre Krankheiten. In: Hrsg. Ratei tschak,<br />
K. H., Wolf, H. F. Implantologie. Georg Thieme Verlag, Stuttgart,<br />
New York 1994 (317-328).<br />
[4] Marinello, C. P., Kundert, E., Andreoni, C.: Die Bedeutung der periimplantären<br />
Nachsorge für Zahnarzt und Patient. Implantologie 1,<br />
1993 (43-57).<br />
[5] Günay, H., Bohnenkamp A.: Peri-implantäre Infektionen, Quintessenz<br />
12, 2006 (1355-1369).<br />
[6] Schmüdderich, W.: Entwicklung eines Materials für die Versie gelung<br />
von Implantatinnenräumen zur Prophylaxe bakterieller Kontamination.<br />
Diss. Med. Dent. Düsseldorf 2001.<br />
[7] Fritzemeier, C. U.: GapSeal – ein Material zur Versiegelung von<br />
Implantatinnenräumen. ZMK 23, 2007 (2-3).<br />
[8] Fritzemeier, C. U., Schmüdderich, W.: Peri-implantitisprophylaxe<br />
durch Versiegelung der Implantatinnenräume mit GapSeal. Im plantologie<br />
15, 2007 (71-79).<br />
[9] Kleisner, J., Marinello, C. P., Kundert, E., Lüthy, H.: Prävention bakte -<br />
riel ler Kontamination von Implantatkomponenten in vivo durch<br />
ein anzuwendendes Metronidazol – Gel. Dent Implantol 2, 4, 1998<br />
(284-296).<br />
[10] Buchmann, R.: Mikrobielle Infekte beseitigen, Überlastungen<br />
verringern. Implantologie Journal 2, 2000 (48-62).<br />
[11] Binon, P., Weir, D., Wantanabe, L., Walker, L.: Implant Component<br />
Compatibility. In: Hrsg. Laney, W. R., Tolman, D. E.: Tissue Integration<br />
in Oral, Orthopedic & Maxill<strong>of</strong>acial Reconstruction, Mayo Medical<br />
Center Rochester, Minnesota, 1990.<br />
[12] Otte, H.-J.: Leitfaden der medizinischen Mikrobiologie, Gustav<br />
Fischer Verlag, Stuttgart, 1965.<br />
[13] Zipprich, H., Weigl, P., Lange, B., Lauer, H.-C.: Erfassung, Ur sa chen<br />
und Folgen von Mikrobewegungen am Implantat-Abutment-<br />
Interface. Implantologie 15, 2007 (31-46).<br />
[14] Battaini, P., Neve, T.: Verhältnis zwischen der elektrochemischen<br />
Korrosion von <strong>Dental</strong>legierungen und ihrer Kompatibilität mit dem<br />
menschlichen Körper. Werksmitteilung der Fa. Rigatti Luchini,<br />
Como 1994.<br />
[15] Fritzemeier, C. U., Steffens, E.: Titan als neues Restaurationsmetall<br />
in der Zahnärztlichen Prothetik und der Mund-, Kiefer- und<br />
Plastischen Gesichtschirurgie. ZWR 101, 1992 (589-595).<br />
[16] Sellmann, H.: „Dicht“ machen. dental:spiegel 27, 2007 (41-42).
88 <strong>EDI</strong><br />
Product Studies<br />
A clinical study on the s<strong>of</strong>t-tissue healing capacity around the treated surfaces <strong>of</strong><br />
one-piece screw implants<br />
S<strong>of</strong>t-tissue Healing Around<br />
Surface-roughened One-piece<br />
Implants<br />
Pr<strong>of</strong> Emanuel A. Bratu, Dr Olimpiu L. Karancsi and Dr Radu Sita, Timisoara/Romania<br />
This study was performed to evaluate the s<strong>of</strong>t-tissue healing capacity around the treated surfaces <strong>of</strong><br />
one-piece screw implants.<br />
Materials and methods<br />
The study comprised six patients, each <strong>of</strong> whom<br />
received one or two fully surface-roughened one-piece<br />
covered screw implants (MIS, Shlomi, Israel), 10 to 13 mm<br />
in length and 3 mm in diameter, in different locations<br />
within the mouth. The baseline examination evaluated<br />
the patients’ medical history and smoking habit, and<br />
included extraoral and intraoral clinical examinations<br />
and Panoramic X-rays. The patients’ bone and s<strong>of</strong>t-tissue<br />
volume were also estimated. Only patients with a<br />
sufficient bone supply were included. The minimum<br />
requirements for implant insertion were 4 mm <strong>of</strong> bone<br />
width and 11 mm <strong>of</strong> bone height. The surgical intervention<br />
was performed under local anaesthesia (Ultracain<br />
DS Forte, Aventis).<br />
Surgical procedure<br />
A crestal incision was performed and full mucoperiosteal<br />
flaps were elevated at the insertion sites. The<br />
bone was cleaned <strong>of</strong> periosteal tissue, and the<br />
implant positions were marked with a round bur. A<br />
2 mm pilot drill marked the depth and angulation <strong>of</strong><br />
the implant. A 2.8 mm enlargement drill was used for<br />
the first 2 mm <strong>of</strong> depth in the cortical crestal bone.<br />
The implants were inserted with a ratchet until the<br />
threads were completely covered by bone. The post -<br />
operative medication included antibiotics (Augmentin<br />
1 g, SmithKline Beecham) for six days and analgesics<br />
(Ketonal forte, 200 mg) for three days. Probing depths<br />
around the implants were taken after suture (Silk, 4-0,<br />
B. Braun). Periotest measurements taken after insertion<br />
yielded values <strong>of</strong> between 2 and –4.<br />
Follow-up<br />
Patients were asked to return after three days. A decision<br />
to perform immediate restoration or to allow<br />
for a healing period was made depending on the<br />
patients’ periotest values. One-half <strong>of</strong> the patients<br />
(with negative periotest values) received provisional<br />
restorations; the other half (with positive values) did<br />
not. The immediate restorations were made <strong>of</strong> acrylic<br />
resin and cemented with provisional Temp-Bond<br />
cement (Kerr).<br />
For the patients who waited three months, probing<br />
depths were again measured after the healing period<br />
and compared to those on the day <strong>of</strong> surgery. Both<br />
patient groups received instructions in oral hygiene<br />
and were told to eat only s<strong>of</strong>t food for two weeks following<br />
their visit. No implant was lost during the study<br />
period. All patients presented with attached healed<br />
gingiva around the implants. The group with provisional<br />
restorations showed faster and better healing<br />
compared with the group with no restorations.<br />
Results<br />
The six patients comprised four men and two women<br />
with a mean age <strong>of</strong> 48 (37 to 60) years. All patients<br />
presented with small edentulous areas rather than<br />
extensive tooth loss. Probing depths varied between<br />
2 and 4 mm at suturing, and between 1 and 2 mm<br />
after three months. No bleeding was observed. There<br />
were no significant differences between male and<br />
female patients. Patients with thicker peri-implant tissue<br />
had smaller probing depths than those with thinner<br />
peri-implant tissue. It was attempted to obtain
Fig. 1<br />
Oral status<br />
at baseline.<br />
Fig. 2<br />
Panoramic X-ray<br />
<strong>of</strong> the initial<br />
status.<br />
Fig. 3<br />
Periotest<br />
values after<br />
insertion.<br />
Fig. 4<br />
Panoramic X-ray<br />
<strong>of</strong> the initial<br />
status.<br />
Fig. 5<br />
Probing depths<br />
after suture<br />
removal,<br />
implant 22.<br />
Fig. 6<br />
Probing depths<br />
after three months<br />
with provisional<br />
restoration in<br />
place, implant 22.<br />
Fig. 7<br />
Probing depths<br />
before cementing<br />
the final restoration,<br />
implant 24.<br />
Fig. 8<br />
Final restoration in<br />
place.<br />
Fig. 9<br />
Panoramic X-ray<br />
after final<br />
restoration<br />
setting.<br />
Fig.10<br />
One-piece<br />
implant (UNO)<br />
in Panoramic<br />
X-ray.<br />
Case 1<br />
1 2<br />
3 4<br />
5 6<br />
7 8<br />
9 10<br />
<strong>EDI</strong> 89<br />
Product Studies
90 <strong>EDI</strong><br />
Product Studies<br />
Case 2<br />
11 12<br />
attached gingiva around the implants (without which<br />
probing depth measurements would have made no<br />
sense). This confirms the theory <strong>of</strong> attached keratinized<br />
gingiva forming around implants.<br />
Discussion<br />
The present clinical study evaluated the stabilization<br />
<strong>of</strong> the s<strong>of</strong>t tissue around surface-roughened implants.<br />
At the first examination following implant insertion,<br />
probing depths were greater than after three months.<br />
This is as expected based on the healing process <strong>of</strong> the<br />
peri-implant tissues. Of clinical importance is the fact<br />
that there was no irritation <strong>of</strong> the s<strong>of</strong>t tissues around<br />
the implants during the healing period. This suggests<br />
that the gingiva recovers well and adheres on a rough<br />
surface, whether or not a patient receives a provisional,<br />
if certain preconditions are met.<br />
Conclusion<br />
The study has shown that if attached gingiva around<br />
the implant can be obtained, there is no absolute<br />
need for a polished implant neck to prevent periimplant<br />
tissue irritation. Also, pocket depths correlate<br />
Nr Age Sex Size Position Periotest<br />
value<br />
with the thickness <strong>of</strong> the mucosa – the thicker the<br />
mucosa, the smaller the depth. However, if the gingiva<br />
is not attached, plaque deposit problems can arise,<br />
and implant failure becomes possible. Initial results<br />
have been promising, but further investigation and<br />
longer observation periods are needed in order to<br />
make a definitive statement on this issue.<br />
Probing depth<br />
Insertion 3 months<br />
1 45 F 3/13 36 -1 4 2<br />
3/13 37 0 3 1,5<br />
2 50 M 3/13 43 -3 3 1,5<br />
3 47 M 3/10 12 +1 3,5 2<br />
4 62 M 3/13 45 -4 4 2<br />
5 51 M 3/10 22 +2 4 1,5<br />
3/13 24 +1 3 2<br />
6 37 F 3/10 14 0 3 1<br />
13<br />
Contact Address<br />
M.I.S. Implant Technologies Ltd<br />
P.O.Box 110, Shlomi 22832, ISRAEL<br />
www.mis-implants.com<br />
Fig. 11<br />
Panoramic<br />
X-ray at patient<br />
presentation.<br />
Fig. 12<br />
Probing depths<br />
after suturing,<br />
implant 36.<br />
Fig. 13<br />
Panoramic<br />
X-ray after<br />
implant<br />
insertion.
92 <strong>EDI</strong><br />
Product Studies<br />
A basis for predictable esthetic transitional contour<br />
Immediate Placement and Loading<br />
Fernando Rojas-Vizcaya, DDS, MS, Chapel Hill/USA<br />
In this complex case, Astra Tech BioManagement Complex supported and preserved the esthetics and functional<br />
results by maintaining marginal bone and healthy peri-implant tissues.<br />
In cases like this, the starting point is always the<br />
desired cervical contour for the new crown. If placing<br />
the implant 3 mm from this contour, the desired biologic<br />
width can be created. But it’s important to<br />
remember that the stability <strong>of</strong> cervical buccal tissue<br />
is the ultimate determinant <strong>of</strong> esthetics. This means<br />
preserving this s<strong>of</strong>t tissue architecture while also<br />
ensuring optimum marginal bone levels. In this case,<br />
the Astra Tech BioManagement Complex is the basis<br />
for predictable esthetic transitional contour.<br />
Complex case, predictable outcome<br />
This complex case <strong>of</strong> immediate placement and<br />
immediate loading in an edentulous maxilla demon-<br />
Fig. 1 Cervical contour design for fully maxillary<br />
rehabilitation – creation <strong>of</strong> the new<br />
esthetic information.<br />
Fig. 4 Surgical stent showing the new cervical<br />
contour.<br />
strates how the BioManagement Complex works in<br />
practice (Figs. 1 to 21). Starting with the desired cervical<br />
contour, the optimal implant three-dimensional<br />
placement is created when using a 2 mm/3 mm depth<br />
rule from the cervical contour <strong>of</strong> the planed crown<br />
indicated by the surgical stent.<br />
Creating the optimal space<br />
Rather than simply placing implants in available bone,<br />
the cervical surgical guide created from the wax-up<br />
allowed the removal <strong>of</strong> bone where necessary to create<br />
the optimal 3 mm space from the planned crown<br />
in the area <strong>of</strong> implants and pontics – while leaving<br />
osseous peaks to support the interdental papillae.<br />
Fig. 2 Before extraction. Fig. 3 After non-traumatic extraction – ready<br />
for immediate placement protocol.<br />
Fig. 5 Implants are to be placed 3 mm from<br />
the cervical contour and 2 mm palatal to it.<br />
Fig. 6 Before placing the implants, bone needs<br />
to be removed.
Fig. 7 Try-in <strong>of</strong> provisional restoration before<br />
bone reduction – the cervical contour is in<br />
contact with the bone.<br />
Fig. 8 Bone is removed using the cervical contour<br />
<strong>of</strong> the surgical stent as reference.<br />
<strong>EDI</strong> 93<br />
Product Studies<br />
Fig. 9 Try-in <strong>of</strong> provisional restoration after<br />
bone reduction – bone is 3 mm from the<br />
cervical contour <strong>of</strong> the planned crowns.<br />
Fig. 10 Localization <strong>of</strong> the ideal three-dimensional implant position using the surgical stent. Fig. 11 Implants are placed and primary stability<br />
is obtained. Osseous peaks are left to support<br />
the interdental papillae.
94 <strong>EDI</strong><br />
Product Studies<br />
Fig. 12 Closure, after abutment placement –<br />
ready for immediate loading.<br />
Fig. 15 New s<strong>of</strong>t tissue contour with mesial<br />
and distal papillae between the implants.<br />
Fig. 18 No black triangles can be seen after 1.5 years – maintenance <strong>of</strong><br />
function and esthetics.<br />
The desired result<br />
Once the desired architecture was established and<br />
implants placed, the BioManagement Complex supported<br />
and preserved the desired result. The provisional<br />
restoration, that had established the transitional<br />
contour, guided the s<strong>of</strong>t tissue during the healing<br />
process and created the interdental papilla.<br />
With acknowledgement to:<br />
Jorge Cid Yáñez, CDT, Lica Pirv, CDT.<br />
Fig. 13 Provisional restoration after immediate<br />
loading protocol.<br />
Fig. 16 Maintenance <strong>of</strong> the initial esthetic<br />
design in the final restoration-position <strong>of</strong> the<br />
zenith and a natural balance <strong>of</strong> the gingival<br />
level.<br />
Fig. 19 Final result.<br />
Figs. 20 and 21 Final results after a full upper arch rehabilitation – frontal and palatine view.<br />
Contact Address<br />
Astra Tech AB<br />
Box 14 · 431 21 Mölndal<br />
SWEDEN<br />
Phone: +46 31 7763000<br />
www.astratechdental.com<br />
Fig. 14 Healthy s<strong>of</strong>t tissue after twelve weeks –<br />
interproximal papillae and space for ovate<br />
pontics.<br />
Fig. 17 Panoramic x-ray showing bone preservation<br />
– note the interproximal bone that<br />
supports the central papilla.
96 <strong>EDI</strong><br />
Business & Events<br />
Astra Tech World Congress 2008<br />
Making New Discoveries<br />
The second Astra Tech World Congress at Gaylord National Resort in Washington, DC<br />
is over and it was yet another success. “Get inspired” and “Making new discoveries”<br />
were the overall messages <strong>of</strong> a congress that delivered four days <strong>of</strong> high-class presen-<br />
tations, discussions, hands-on demonstrations, and awe-inspiring entertainment.<br />
In his opening speech at the world congress, the President<br />
and CEO <strong>of</strong> Astra Tech, Peter Selley, made a point<br />
about the importance <strong>of</strong> scientific documentation in<br />
regard to innovations and new discoveries in implant<br />
dentistry, as it is not enough to design, invent and<br />
market a product, it also has to be documented and<br />
proven safe before it is placed in a patient. Innovation<br />
and competitiveness in implant dentistry must never<br />
put the safety and the well-being <strong>of</strong> the patient at risk.<br />
From the very beginning, the development <strong>of</strong> the<br />
Astra Tech Implant System was built on a very serious<br />
approach to scientific documentation and patient<br />
safety, in combination with curiosity, courage, determination<br />
and search for excellence. Groundbreaking<br />
innovations are the cornerstones <strong>of</strong> the Astra Tech<br />
BioManagement Complex – Conical Seal Design,<br />
MicroThread, OsseoSpeed and Connective Contour.<br />
Exhibition archipelago<br />
The exhibition area, spread out over 6,800 square<br />
meters, provided an ocean <strong>of</strong> knowledge, where it<br />
was possible to go deep beneath the surface and<br />
study all the facts, details and specifics <strong>of</strong> what Astra<br />
Tech <strong>Dental</strong> can <strong>of</strong>fer. The delegates could cruise<br />
between the islands <strong>of</strong> their interests and needs: Scientific<br />
island, Surgical island, Restorative island, and<br />
Training & Education island. By <strong>of</strong>fering product<br />
news, scientific documentation, one-on-one demonstrations,<br />
hands-on training, and Speakers’ Corner<br />
presentations, all visitors were able to make new discoveries<br />
in the exhibition archipelago.<br />
New products<br />
The <strong>of</strong>ficial launch <strong>of</strong> Atlantis, the CAD/CAM solution<br />
for cement-retained, patient-specific abutments,<br />
took place at the congress. By utilizing the Atlantis<br />
VAD (Virtual Abutment Design) s<strong>of</strong>tware, the abutments<br />
are individually designed from the final tooth<br />
shape. The result is an abutment<br />
with outstanding<br />
function and esthetics.<br />
Two new OsseoSpeed<br />
implants were also introduced<br />
at the congress. One is a<br />
short implant ideal for cases<br />
with limited vertical bone height,<br />
that also helps reduce the need for<br />
bone augmentation. The other new<br />
implant, OsseoSpeed 3.0 S, is one <strong>of</strong> the<br />
few two-piece implant solutions on the<br />
market today that is optimal for cases with limited<br />
horizontal space.<br />
Diary <strong>of</strong> a congress delegate<br />
WEDNESDAY, JUNE 4 The congress kicked <strong>of</strong>f today.<br />
The nice weather all <strong>of</strong> a sudden turned into a spectacular<br />
thunderstorm, like inauguration fireworks! The<br />
afternoon started with sixteen pre-congress presentations<br />
that welcomed over 500 attendees. The lectures<br />
and hands-on program <strong>of</strong>fered something for everyone,<br />
from those new to implant dentistry to those<br />
interested in more advanced techniques. There were<br />
also programs in Spanish, Italian, French and Scandinavian<br />
languages. Meanwhile, the poster authors were<br />
busy posting their work – more than 138 posters participated<br />
in the poster competition. It was a great start <strong>of</strong><br />
the congress and I’m looking forward to the remaining<br />
three days <strong>of</strong> 131 internationally renowned researchers<br />
speaking on issues <strong>of</strong> implant dentistry.<br />
THURSDAY, JUNE 5 Finally, the international dental<br />
community assembled for the Grand Opening. Performing<br />
artists started the morning in a very inspiring<br />
way, followed by the President and CEO <strong>of</strong> Astra Tech,<br />
Peter Selley, <strong>of</strong>ficially opening the congress. Eight<br />
world-renowned speakers presented during the<br />
morning session, moderated by the chairman <strong>of</strong> the<br />
Peter Selley<br />
Jan Lindhe<br />
Tomas<br />
Albrekt sson
Scientific Committee, Pr<strong>of</strong>essor Jan Lindhe. The session<br />
covered topics in implant dentistry ranging from the<br />
edentulous patient and oral infection and inflammation<br />
as a risk factor, to special needs patients, treatment<br />
planning, patient quality <strong>of</strong> life, and the future<br />
<strong>of</strong> implant dentistry. For example, Pr<strong>of</strong>essor Lindhe<br />
emphasized the importance <strong>of</strong> implant design for the<br />
preservation <strong>of</strong> s<strong>of</strong>t tissue. Another highlight was<br />
Pr<strong>of</strong>essor Tomas Albrektsson’s presentation<br />
“Implants in dentistry – history and future,” in<br />
which he suggested that it is time to reconsider<br />
the 1986 standard for marginal bone levels<br />
with regard to implant success.<br />
The afternoon featured three parallel sessions.<br />
It was hard to choose between them,<br />
but I managed to listen to parts <strong>of</strong> all three<br />
sessions. The surgical session discussed<br />
pharmacological issues in implant dentistry,<br />
treatment planning protocols, minor s<strong>of</strong>t tissue<br />
procedures, sinus grafting and solutions<br />
for challenging situations, while the restorative<br />
session addressed provisionals, abutment<br />
selection, cemented restorations, and screwretained<br />
restorations. The focus <strong>of</strong> the third session,<br />
„Unlimited possibilities in implant dentistry”,<br />
was implant research, diagnostic technology, and<br />
CAD/CAM and restorative solutions.<br />
After a full day <strong>of</strong> in-depth learning, I attended an<br />
unforgettable evening at the Smithsonian American<br />
Art Museum and the National Portrait Gallery in<br />
downtown Washington, DC. The theme <strong>of</strong> the<br />
evening, “Making new discoveries through art,” gave<br />
the scientific content <strong>of</strong> the morning and afternoon<br />
the best possible ending. Great day!<br />
FRIDAY, JUNE 6 The congress continued in high gear<br />
this morning with “A Good Morning with Astra Tech,”<br />
an innovative and fun morning show where six<br />
speakers discussed controversies in immediate placement<br />
and loading, inter-implant distance, digital<br />
implant dentistry today and tomorrow, and the psychosocial<br />
factors affecting the treatment outcomes<br />
<strong>of</strong> maxill<strong>of</strong>acial conditions. Rich with live music, news<br />
breaks and a dynamic talk show format, the morning<br />
presentations set the stage for another inspirational<br />
day. The lecture by Pr<strong>of</strong>essor Rhonda Jacob from the<br />
Department <strong>of</strong> Neck and Head Surgery at the University<br />
<strong>of</strong> Texas M.D. Anderson Cancer Center, called<br />
“Implants in the rehabilitation <strong>of</strong> head and neck cancer<br />
patients – a hope for the future” truly embodied<br />
the true meaning <strong>of</strong> the expression “quality <strong>of</strong> life”<br />
for this vulnerable patient group. The morning session<br />
ended with an intense and interesting panel discussion<br />
lead by the two moderators Dr Michael Norton,<br />
UK, and Dr Sverker Toreskog, Sweden.<br />
After lunch it was time for seven parallel sessions.<br />
The topics ranged from “Advanced technology in support<br />
<strong>of</strong> implant therapy” and “Implants moving<br />
towards a standard <strong>of</strong> care” to “Prevention and management<br />
<strong>of</strong> complications” and “Frontline research in<br />
implantology.”<br />
After such a busy day, it was great to sit down for<br />
an evening <strong>of</strong> “Making new discoveries through<br />
music, song and dance.” Dinner and a three-act performance<br />
unified the international audience with a<br />
montage <strong>of</strong> orchestral, musical and dance styles.<br />
SATURDAY, JUNE 7 The morning begun with a session<br />
called “Esthetics and the future” in which six speakers<br />
spoke on how biology dictates and implant components<br />
and clinical management support natural esthetic<br />
results. The session covered many different aspects <strong>of</strong><br />
the topic, from the fresh extraction socket to the longterm<br />
success <strong>of</strong> the esthetically restored patient.<br />
The winner <strong>of</strong> the Astra Tech Scientific Award was<br />
also presented during this session – Pr<strong>of</strong>essor John<br />
Brunski <strong>of</strong> the Rensselaer Polytechnic Institute <strong>of</strong> Troy,<br />
New York. Much <strong>of</strong> his work is focused on the properties<br />
<strong>of</strong> the bone-implant interface and reliable models<br />
for predicting implant loading and stress-strain<br />
conditions at interfaces.<br />
A Good Morning with Astra Tech.<br />
<strong>EDI</strong> 97<br />
Business & Events<br />
Let’s not forget the winners <strong>of</strong> the poster competition.<br />
Dr Gustavo Mendonca <strong>of</strong> Brazil won in the<br />
Research category, with Dr Ahmad Hamdan <strong>of</strong> France as<br />
runner-up. In the Clinical application category, Dr Jenni<br />
Rissanen, Finland, took home first prize, while Dr Hans<br />
Bystedt, Sweden, walked away with second prize.<br />
Pr<strong>of</strong>essor Lindhe and Pr<strong>of</strong>essor Albrektsson, two brilliant<br />
minds and legends in their field, delivered the<br />
closing remarks in an inspiring and very humorous<br />
way. A great ending to a congress that delivered 131<br />
internationally renowned speakers and scientists in<br />
the extensive scientific program, 138 exciting and<br />
inspiring posters, sixteen pre-congress courses, four<br />
exhibition islands, three Speakers’ Corners, five award<br />
winners, and delegates from 37 countries.
98 <strong>EDI</strong><br />
Business & Events<br />
BioHorizons Global Symposium 2008<br />
Groundbreaking Technology<br />
The 2008 BioHorizons Global Symposium drew more than 1,000 attendees from 42 countries to San Diego, California for<br />
a three-day scientific program on today’s most important implant and tissue regeneration topics. Each clinician-moderated<br />
session featured a panel discussion <strong>of</strong> audience-submitted questions that kept participants fully engaged in the program.<br />
Members <strong>of</strong> the scientific panel and moderators<br />
included Drs Carl E. Misch, Michael A. Pikos, Maurice<br />
Salama and Michael Reddy. Featured presenters<br />
included Drs Edward P. Allen, Stuart Froum, Michael<br />
McCracken, Craig Misch, Myron Nevins, and Marius<br />
Steigmann.<br />
The keynote session featured presentations on the<br />
ground-breaking Laser-Lok microchannels, BioHorizons’<br />
proprietary surface treatment now <strong>of</strong>fered on<br />
Tapered Internal, Single-stage and Internal implants.<br />
Dr Jack Ricci from NYU presented 15 years <strong>of</strong> in vitro,<br />
animal and human studies conducted at leading universities<br />
around the world on this precision-engineered<br />
surface. Dr Myron Nevins from Harvard University<br />
presented results from his landmark study:<br />
Human Histological Evidence <strong>of</strong> a Connective Tissue<br />
Attachment to a <strong>Dental</strong> Implant.* In this study, Laser-<br />
Lok was shown to attract a physical connective tissue<br />
attachment to a predetermined zone on the implant<br />
while inhibiting epithelial downgrowth and preserving<br />
coronal bone levels. Dr Nevins also showed Laser-<br />
Lok implants placed up to nine-years post-op with<br />
little to no bone loss.<br />
BioHorizons and <strong>Dental</strong> Technologies, Inc. (DTI) also<br />
announced a new Restoration-to-Implant Lifetime<br />
Warranty covering implants, abutments and restorations<br />
when fabricated by a participating DTI Laboratory.<br />
This unique <strong>of</strong>fer, made possible by the recent<br />
merger <strong>of</strong> BioHorizons and DTI, brings incredible<br />
value and practice building potential to the entire<br />
implant team.<br />
R. Steven Boggan, President and CEO, said in<br />
regard to the unprecedented attendance: “Bio-<br />
Horizons continues to be one <strong>of</strong> the fastest growing<br />
implant companies in the industry because <strong>of</strong><br />
unique <strong>of</strong>ferings like Laser-Lok and our Lifetime<br />
Warranty program. The Global Symposium presentations<br />
and attendance are indicative <strong>of</strong> our grow-<br />
ing momentum that stems from science-based<br />
design and synergies with high-tech partners<br />
such as DTI.”<br />
BioHorizons will present the 2009 Global Symposium<br />
from April 30 to May 2, 2009, in Chicago, Illinois.<br />
Attendance will be limited, and another sell-out is<br />
expected, so please register early to ensure your<br />
spot.<br />
* International Journal <strong>of</strong> Periodontics & Restorative<br />
Dentistry, Vol. 28, #2, April 2008.<br />
More Information<br />
BioHorizons<br />
www.biohorizons.com<br />
Myron Nevins,<br />
DDS<br />
Michael A. Pikos,<br />
DDS
The home <strong>of</strong><br />
Gaudí.<br />
CARS 2008<br />
exhibition.<br />
CARS 2008 in Barcelona<br />
Bridging the Gap between<br />
Diagnostics and Computer<br />
Science<br />
The CARS Congress is the most important international<br />
forum for applied advanced information technology in<br />
radiology and surgery. It covers a wide spectrum from<br />
radiological imaging and management (PACS) to computer<br />
science and engineering applications in surgery<br />
(planning, simulation, navigation, robotics etc). Along<br />
with the 22 nd International Congress and Exhibition, CARS<br />
covered a wide range <strong>of</strong> topics: medical imaging, cardiovascular<br />
imaging, maxill<strong>of</strong>acial computer imaging,<br />
image processing and image display, telemedicine and<br />
e-health, computer-aided diagnosis, computer-assisted<br />
radiation therapy, surgical navigation, surgical robotics<br />
and instrumentation, surgical simulation and education,<br />
computer assisted orthopaedic and spinal surgery, computer-assisted<br />
head and neck surgery, image-guided<br />
<strong>EDI</strong> 99<br />
Business & Events<br />
The International Congress <strong>of</strong> CARS (Computer-Assisted Radiology and Surgery) “aims to provide a forum to close<br />
the gap between diagnostic and interventional radiology, surgery and computer science and to encourage inter-<br />
disciplinary research and development activities in an international environment”, says the organizer <strong>of</strong> CARS 2008<br />
in Barcelona, Dr Heinz U. Lemke, Pr<strong>of</strong>essor for Computer-Assisted Surgery at the University <strong>of</strong> Leipzig, Germany.<br />
neurosurgery and minimally invasive cardiovascular and<br />
thoraco-abdominal surgery and not least maxill<strong>of</strong>acial<br />
imaging. From June 25 to 28, CARS 2008 was the meeting<br />
point for international experts, providing balanced<br />
and in-depth information on new diagnostic and therapeutic<br />
procedures including results from multidisciplinary<br />
research and development efforts, treatment<br />
providers’ experiences, patient outcomes, economic and<br />
management considerations and well as scientific<br />
results <strong>of</strong> medical validation. To make the new technologies<br />
available to medical and health care specialists, the<br />
scientific committee headed by CARS president Dr Javier<br />
Herrero Jover had decided to extend the program with a<br />
Clinical Day. This day turned out to be an educative event<br />
where experts from radiological and surgical specialities<br />
presented advanced IT applications in the diagnosis and<br />
therapy <strong>of</strong> highly relevant clinical topics.<br />
The 14 th Computed Maxill<strong>of</strong>acial Imaging Congress<br />
chaired by Dr Allan G Farman (USA) showed what is possible<br />
today in maxill<strong>of</strong>acial surgery, dentistry and dental<br />
implantology. Speakers from the Universities <strong>of</strong> Cologne<br />
and Hannover (Germany) covered the accuracy <strong>of</strong> a<br />
newly developed integrated system for dental implant<br />
planning (Dreiseidler) and the biomechanical effects <strong>of</strong><br />
surgical assisted rapid maxillary expansion by bone<br />
anchored intraoral distraction device: a three-dimensional<br />
finite element analysis (Hassfeld and co-workers).<br />
Renowned speakers from the US gave lectures on contrasting<br />
aspects <strong>of</strong> orbital floor fractures in the setting <strong>of</strong><br />
zygomaticomaxillary complex injuries versus isolated<br />
orbital injury (Marcus and coworkers, University <strong>of</strong><br />
Durham, and Follmar and coworkers, University <strong>of</strong> Baltimore).<br />
At the end, the international party <strong>of</strong> CARS 2008<br />
allowed participants to catch a glimpse <strong>of</strong> tomorrow’s<br />
service robots in surgery and medicine.
100 <strong>EDI</strong><br />
Business & Events<br />
EAO 17 th Annual Scientific Meeting, Warsaw, 18 – 20 September 2008<br />
Clinical Advances and<br />
Predictability with Oral Implants<br />
The <strong>European</strong> <strong>Association</strong> for Osseointegration (EAO) will hold its 17 th Annual Scientific Meeting<br />
at the PKIN Congress Centre in Warsaw, Poland, from 18 to 20 September 2008.<br />
This year the congress will be co-chaired by Dr David<br />
Harris and Dr Andrzej Wojtowicz. The 2008 EAO<br />
meeting has been organized in collaboration with<br />
the National Polish Implantology <strong>Association</strong> (OSIS).<br />
Based on the statistics <strong>of</strong> the previous congress,<br />
this year’s meeting, themed ‘Clinical Advances and<br />
Predictability with Oral Implants’, is expected to welcome<br />
about 3,000 experts from around the world to<br />
share knowledge and experience in the field <strong>of</strong><br />
implant dentistry. The scientific programme will<br />
mainly focus on topics like bio-active surfaces, medical<br />
impairment, oncology, bisphosphonates, extra<br />
oral cases, biomedical imaging, digital planning and<br />
transfer to clinical procedures, navigation and guided<br />
implant placement, gero-implantology, quality <strong>of</strong> life,<br />
simplified treatment protocol, long-term management,<br />
and treatment in the aesthetic zone.<br />
By ensuring exciting three days with worldrenowned<br />
speakers presenting recent advances on<br />
highly relevant scientific and clinical topics in<br />
osseointegration, the Warsaw Meeting will allow<br />
researchers and clinicians to get state-<strong>of</strong>-the-art<br />
information on all the different aspects using<br />
osseointegrated implants in dentistry.<br />
More Information<br />
<strong>European</strong> <strong>Association</strong> for Osseointegration<br />
www.eao.org
Foundation awards prize to young scientists<br />
The camlog foundation<br />
Research Award 2008/2009<br />
Participants will have from the middle <strong>of</strong> 2008 to the<br />
end <strong>of</strong> 2009 to prepare their research papers, which<br />
are to be submitted to the camlog foundation after<br />
their publication in a recognized scientific journal.<br />
The research underlying the expected exceptional<br />
scientific papers must have been conducted in one <strong>of</strong><br />
the countries in which Camlog Biotechnologies AG,<br />
Basel, is represented by its products and services. The<br />
papers may be written in either English or German.<br />
The papers to be submitted are to relate to one <strong>of</strong> the<br />
following three areas:<br />
- Conceptual approaches for sustainable results<br />
in implant dentistry<br />
- Concepts for optimum red-white esthetics<br />
- Convincing long-term results<br />
The papers will be judged and assessed by the scientific<br />
jury, consisting <strong>of</strong> five members <strong>of</strong> the Foundation<br />
board and the Scientific Board <strong>of</strong> the camlog<br />
foundation. The winner <strong>of</strong> the camlog foundation<br />
Research Award 2008/2009 will have the opportunity<br />
<strong>of</strong> presenting his or her paper to a larger audience at<br />
the International Camlog Congress 2010, where<br />
entries will also be invited for the camlog foundation<br />
Research Award 2010/2011. Conditions <strong>of</strong> entry and<br />
the entry form on which entries must be made can be<br />
downloaded from http://www.camlogfoundation.org/.<br />
The camlog foundation is a foundation established<br />
by scientists under Swiss law. It engages in targeted<br />
supporting <strong>of</strong> gifted young scientists, promotion <strong>of</strong><br />
basic and applied research, and continuing training<br />
and education to promote progress in implant dentistry<br />
and related fields to serve the patient. As part<br />
<strong>of</strong> its scientific mission, the camlog foundation has<br />
assumed patronage <strong>of</strong> the International Camlog<br />
Congresses, which take place every two years.<br />
The World <strong>of</strong><br />
<strong>Dental</strong> Edutainment<br />
<strong>EDI</strong> 101<br />
Business & Events<br />
During the International Camlog Congress held in May 2008 in Basel, the President <strong>of</strong> the camlog foundation, Pr<strong>of</strong> Rolf Ewers,<br />
Vienna, announced and invited entries for the camlog foundation Research Award 2008/2009, which <strong>of</strong>fers prizes <strong>of</strong><br />
CHF 10,000 for the winner, CHF 6,000 for the runner up and CHF 4,000 for the third place. Entries are invited from committed<br />
specialists aged under 45 years working in universities, hospitals and surgeries.<br />
More Information<br />
camlog foundation<br />
Margarethenstrasse 38 . CH-4053 Basel . SWITZERLAND<br />
Phone: +41 61 56541-14<br />
foundation@camlog.com . www.camlogfoundation.org<br />
www.dental-online-community.com<br />
The free continuing-education platform<br />
for dentists and dental technicians
102 <strong>EDI</strong><br />
Business & Events<br />
SimPlant Academy World Conference on 3D Digital Dentistry<br />
Successful Outcome<br />
On Friday 30 and Saturday 31 May 2008, clinicians and laboratory technicians from 35 different countries came to Vienna to<br />
participate in Materialise <strong>Dental</strong>’s 7 th edition <strong>of</strong> its SimPlant Academy World Conference on computer guided dentistry.<br />
Set in the comfortable surroundings <strong>of</strong> the Hilton, clinicians attended intensive SimPlant s<strong>of</strong>tware training sessions, hands-on<br />
workshops and various lectures by key opinion leaders.<br />
The SimPlant Academy World Conference kicked <strong>of</strong>f<br />
on Friday morning 30 May with two corporate fora,<br />
one dedicated to Friadent’s ExpertEase and the other<br />
to Biomet 3i’s Navigator technology. Ashok Sethi, BDS,<br />
spoke for the former sponsor and Michael Block,<br />
DMD, acted as a speaker for the second sponsor Biomet<br />
3i. Other sponsors that were also represented at<br />
the SimPlant Academy World Conference were Astra<br />
Tech <strong>Dental</strong> (Facilitate), DeguDent, KaVo, Morita,<br />
NewTom and Planmeca.<br />
The corporate fora in the morning were followed by<br />
a number <strong>of</strong> intensive SimPlant s<strong>of</strong>tware training sessions,<br />
which were designed for all levels <strong>of</strong> users and<br />
were appreciated by many <strong>of</strong> the participants. On this<br />
occasion, Materialise <strong>Dental</strong> took the opportunity to<br />
introduce SimPlant 12, their latest s<strong>of</strong>tware version.<br />
During the afternoon sessions, interactive workshops<br />
provided a terrific practical insight in the whole<br />
process from scanning and planning to guided<br />
implant placement, to the ultimate Immediate Smile.<br />
Delegates got answers on questions such as “how is a<br />
scan prosthesis made” and “what are the differences<br />
between CT & CBCT scanners and what are the<br />
requirements for a good scan”. Several CBCT scanners<br />
were demonstrated by the respective manufacturers.<br />
Treatment planning skills were practiced with real<br />
patient cases and practical sessions with all <strong>of</strong> Materialise<br />
<strong>Dental</strong>’s partners’ surgical kits combined with<br />
genuine SAFE SurgiGuide drill guides taught how surprises<br />
can be eliminated when drilling and placing<br />
implants. SimPlant 12 now also <strong>of</strong>fers the Next Innovation<br />
SurgiGuide drill guide preview, allowing dentists<br />
to customize a SurgiGuide according to their preferences.<br />
And thanks to FastTrack planning, delivery time<br />
<strong>of</strong> SurgiGuide drill guides is significantly reduced.<br />
The Friday training sessions and workshops were<br />
finally concluded with an exquisite dinner at the<br />
Palais Pallavicini, a beautiful classical style palace<br />
which was constructed in the eighteenth century and<br />
is situated in the center <strong>of</strong> Vienna. The comfortable<br />
and relaxed setting invited Materialise <strong>Dental</strong> and<br />
its guests to reflect on an intensive but fruitful day.<br />
Key opinion leaders sharing their<br />
thoughts on 3D Digital Dentistry<br />
Whereas the first day was dedicated to interactive<br />
s<strong>of</strong>tware training sessions and workshops, impressive<br />
lectures by various key opinion leaders marked<br />
the second day <strong>of</strong> the World Conference in Vienna.<br />
Moderator Dr Elmar Frank, Director <strong>of</strong> the SimPlant<br />
Academy in German-speaking countries, guided the<br />
audience and lecturers through a series <strong>of</strong> four different<br />
themes. The first round <strong>of</strong> lectures touched the<br />
subject <strong>of</strong> the interdisciplinary approach <strong>of</strong> 3D Digital<br />
Dentistry. Pr<strong>of</strong>essor Ignace Naert and Pr<strong>of</strong>essor Marc<br />
Quirynen from the K.U.Leuven, Belgium, held a tandem<br />
presentation on “3D Digital Dentistry to optimize<br />
patient care”. A second tandem presentation on “The<br />
interaction between an orthodontist and an oral maxill<strong>of</strong>acial<br />
surgeon in an orthognathic surgery: a case<br />
planning with SimPlant OMS, 3D Dento-Facial-Planner,”<br />
was held by Dr Herman de Jonghe from The<br />
Netherlands and Dr Nico Vrijens from Belgium.<br />
The second round <strong>of</strong> lectures was all about widening<br />
the scope with regard to virtual bone augmentation.<br />
George Mandelaris, DDS, MS, talked about “Sinus floor<br />
augmentation in the atrophic maxilla: a novel<br />
approach using guided surgery with and without<br />
Interactive workshops<br />
provided a<br />
terrific practical<br />
insight in the<br />
whole process from<br />
scanning and planning<br />
to guided<br />
implant placement,<br />
to the ultimate<br />
Immediate Smile.
Dr Dr Steffen Hohl<br />
lecturing on “High<br />
end restorations –<br />
predictability<br />
through virtual<br />
planning.”<br />
<strong>EDI</strong> 103<br />
Business & Events<br />
simultaneous implant placement”, and Dr Andreas<br />
Kullmann touched the subject <strong>of</strong> “Bone augmentation<br />
based on advanced 3D printing technology”.<br />
The third round <strong>of</strong> lectures was about predictable<br />
esthetic planning. Dr Dr Steffen Hohl from Germany<br />
held a lecture about “High end restorations – predictability<br />
through virtual planning”, while Ashok<br />
Sethi, BDS, presented his lecture on “Aesthetics: predicting<br />
improved outcomes with better imaging<br />
modalities and guided surgery”.<br />
In the final round <strong>of</strong> lectures, two other experts went<br />
deeper into the subject <strong>of</strong> facilitating the decision making<br />
process for immediate loading through virtual<br />
imaging. Dr Frank Spiegelberg from Germany talked<br />
about “Immediate Smile following implant placement<br />
in immediate extraction sites”, and Michael Block, DMD,<br />
from the United States provided the icing on the cake<br />
by lecturing on “Immediate provisionalisation in partially<br />
edentulous cases – how to avoid complications”.<br />
In between the different lectures, speakers from<br />
universities and private practices in Austria, France,<br />
Germany, Italy and Turkey presented their innovative<br />
abstracts which had been selected by the scientific<br />
committee. The key opinion leaders that made up<br />
this scientific committee were Scott Ganz, DMD, Pr<strong>of</strong>essor<br />
Ignace Naert, Michael R. Norton, BDS, Ashok<br />
Sethi, BDS, Pr<strong>of</strong>essor Alberto Sicilia and Pr<strong>of</strong>essor<br />
Werner Zechner. Prior to the World Conference, they<br />
had the strenuous task <strong>of</strong> selecting six top abstracts<br />
pertaining to not only research topics involving computer<br />
guided dentistry with SimPlant but also to the<br />
description <strong>of</strong> extraordinary patient cases which had<br />
been treated with the aid <strong>of</strong> SimPlant technology.<br />
At the SimPlant Academy World Conference, Materialise<br />
<strong>Dental</strong> also took the opportunity to inform<br />
participants about their worldwide training schedule.<br />
In addition to these regular trainings, the company<br />
will hold its next clinical course and company visit<br />
on 3 and 4 October at its headquarters in Belgium.<br />
More Information<br />
Materialise <strong>Dental</strong> HQ<br />
www.simplantacademy.org
104 <strong>EDI</strong><br />
Business & Events<br />
Planmeca’s equipment and s<strong>of</strong>tware integration concept will be adopted<br />
in Denmark<br />
An Investment to the Future<br />
Planmeca Oy introduced technologically pioneering dental equipment and s<strong>of</strong>tware integration based on learning environment<br />
for dental education in 2006. Since then the system has successfully been implemented to top-ranking dental schools such as<br />
the Baltimore College <strong>of</strong> <strong>Dental</strong> Surgery, University <strong>of</strong> Maryland <strong>Dental</strong> School (UMB) and the Faculty <strong>of</strong> Dentistry at the<br />
University <strong>of</strong> British Columbia (UBC). Now Planmeca supplies the system to the School <strong>of</strong> Dentistry, University <strong>of</strong> Copenhagen<br />
and the Aarhus School <strong>of</strong> Dentistry also including dental hygienist and dental technician education in both institutions.<br />
The agreement amounts to approximately 9.5 million euros.<br />
Planmeca supplies the School <strong>of</strong> Dentistry, University<br />
<strong>of</strong> Copenhagen and the Aarhus School <strong>of</strong> Dentistry<br />
with 396 digital dental units, 50 digital simulation<br />
workstations, and 600 ultrasonic scalers with LED<br />
light. Planmeca’s solution features a centralised<br />
waterline cleaning system and a centralised suction<br />
hose cleaning system. These features are tailored<br />
especially to fulfil rigorous hygiene demands <strong>of</strong> large<br />
university clinics.<br />
Moreover, the delivery includes a s<strong>of</strong>tware solution<br />
that links digital dental units to the information network<br />
enabling remote monitoring, maintenance, and<br />
management <strong>of</strong> the dental units and instruments.<br />
The intelligent solution preindicates maintenance<br />
routines <strong>of</strong> the unit, which is highly useful in large<br />
facilities. Networking also enables automatic storage<br />
<strong>of</strong> unit and instrument specific data, providing a data<br />
pool for student performance evaluation, quality<br />
assurance, and research purposes.<br />
“Our references make Planmeca a reliable partner<br />
in such extensive projects that require pr<strong>of</strong>ound<br />
understanding <strong>of</strong> clinical workflow as well as special<br />
University <strong>of</strong> Copenhagen<br />
equipment maintenance needs <strong>of</strong> a large institution,”<br />
states Tuomas Lokki, Vice President, Marketing<br />
and Sales.<br />
The delivery is one <strong>of</strong> the largest investments to<br />
dental care in Scandinavia. The first deliveries took<br />
place in August 2008. The entire project will be completed<br />
in 2010.<br />
More Information<br />
Planmeca Oy<br />
Asentajankatu 6<br />
00880 Helsinki<br />
FINLAND<br />
Phone: +358 20 7795 500<br />
www.planmeca.com<br />
Already installed<br />
units at the<br />
University <strong>of</strong><br />
Maryland, USA.
Camlog Invests<br />
in the Future <strong>of</strong><br />
its Wimsheim Site<br />
The symbolic first sod was turned on 5 May to mark the start <strong>of</strong> a signifi-<br />
cant extension to Altatec- und Camlog Vertriebs GmbH’s existing produc-<br />
tion and <strong>of</strong>fice facilities in Wimsheim, Germany, which opened in 2004.<br />
Completion <strong>of</strong> the new buildings and the start <strong>of</strong> production are sched-<br />
uled for June 2009.<br />
The square extension is modular in<br />
concept and will double the effective<br />
area from its present 7,500 square<br />
meters after only four years. In<br />
addition to the expansion <strong>of</strong> the<br />
production, logistics and <strong>of</strong>fice space<br />
made necessary by the company’s<br />
The symbolic first sod was turned on 5 May.<br />
remarkable success, the Camlog<br />
group also has other targets in its<br />
sights. The most important <strong>of</strong> these<br />
are consistently expanding production<br />
in accordance with technical<br />
cybernetic considerations, a<br />
perceptible increase in production<br />
intensity and the ongoing organizational<br />
expansion and adaptation<br />
to the new dimensions into which<br />
the internationally successful Camlog<br />
Group has now grown. One<br />
hundred new jobs are scheduled<br />
to be created in Wimsheim in the<br />
next three years.<br />
<strong>EDI</strong> 105<br />
Business & Events<br />
Jürg Eichenberger, Chief Executive<br />
Officer <strong>of</strong> Camlog Biotechno -<br />
logies AG, stresses that by making<br />
these extensive investments, the<br />
globally operating dental im plant<br />
manufacturer is also making a<br />
clear statement: Camlog is com-<br />
mitting to the long term at<br />
Wimsheim and is thus firmly<br />
declaring its belief in Germany as<br />
a location and in the ‘Made in<br />
Germany’ stamp <strong>of</strong> quality.<br />
More Information<br />
Camlog Biotechnologies AG<br />
Margarethenstrasse 38<br />
CH-4053 Basel<br />
SWITZERLAND<br />
Phone: +41 61 56541-00<br />
info@camlog.com<br />
www.camlog.com
106 <strong>EDI</strong><br />
Product Reports<br />
Natix by Tigran Technologies<br />
More Stable Implants<br />
with Titanium Granules<br />
A new material for supporting bone in-growth around dental implants provides increased stability and is<br />
easy to apply. These promising results are the outcome <strong>of</strong> clinical trials <strong>of</strong> the material when it is used to treat<br />
peri-implantitis and in sinus lifts.<br />
At the EAO Congress in Warsaw, on 18–20 September<br />
2008, the Swedish medical company Tigran Technologies<br />
is presenting the results from ongoing clinical<br />
trials <strong>of</strong> Natix – a new, promising material for dental<br />
use. The material consists <strong>of</strong> irregular titanium<br />
granules that have been optimized in terms <strong>of</strong> porosity,<br />
shape and size, forming the basis for a conducive<br />
environment for bone in-growth.<br />
Peri-implantitis: Peri-implantitis treated with white titanium<br />
granules. No membrane was used in this case.<br />
Courtesy <strong>of</strong> Doctor Caspar Wohlfahrt at the University <strong>of</strong><br />
Oslo, Norway.<br />
Promising results for the treatment<br />
<strong>of</strong> peri-implantitis<br />
Peri-implantitis is a growing problem, and currently<br />
there is no widely established method for supporting<br />
bone in-growth around implants. Caspar Wohlfahrt, a<br />
specialist in periodontology at the University <strong>of</strong> Oslo’s<br />
Institute <strong>of</strong> Clinical Dentistry, is leading the clinical<br />
studies. He recently concluded a pilot study <strong>of</strong> ten<br />
patients, in which the possibility <strong>of</strong> using Tigran’s<br />
porous titanium granules – Natix – in the treatment <strong>of</strong><br />
peri-implantitis was examined; this study has been<br />
submitted for publishing. Caspar Wohlfahrt, who is presenting<br />
the results at the EAO Congress, is impressed<br />
by the material’s characteristics. Histology from two<br />
patients shows bone in-growth next to, through and<br />
between the granules and into the implant.<br />
“We demonstrated well-osseointegrated titanium<br />
granules and in addition the re-osseointegration <strong>of</strong><br />
the implants affected by peri-implantitis – that is,<br />
new bone directly next to the affected implant surface<br />
without fibrous encapsulation between the<br />
bone and implant. This is one <strong>of</strong> the first times reosseointegration<br />
has been proven in a clinical study<br />
when using a bone substitute as a method <strong>of</strong> treatment,”<br />
says Caspar Wohlfahrt.<br />
Sinus lift: Three-year follow-up. The patient was followed for three years after the<br />
abutment operation. The clinical and X-ray examinations show very good results<br />
with healthy gingival margin and a stable marginal bone level. No membrane was<br />
used in this case. Courtesy <strong>of</strong> Associate Pr<strong>of</strong>essor Hans Bystedt, Stockholm, Sweden.
Increased stability for sinus lifts<br />
<strong>EDI</strong> 107<br />
Product Reports<br />
Results from the recently published study “Porous<br />
Titanium Granules Used as Osteoconductive Material<br />
for Sinus Floor Augmentation: A Clinic Pilot Study”<br />
demonstrate the clear benefits <strong>of</strong> the material. Associate<br />
Pr<strong>of</strong>essor Hans Bystedt, who previously worked<br />
as the head <strong>of</strong> the Department <strong>of</strong> Oral and Maxillo -<br />
facial Surgery at Sweden’s Karolinska University Hospital,<br />
is leading the clinical-trial programme and is<br />
hopeful about future use <strong>of</strong> Natix in sinus lifts. The<br />
first time Hans Bystedt used Natix for bone regeneration<br />
was for a sinus lift in 2003, and now he has treated<br />
approximately 40 patients with Natix.<br />
“The method works especially well for direct installations<br />
when the implant is being put in at the same<br />
time as a sinus lift is being done. The advantage <strong>of</strong><br />
treating with Natix is that you get stability straightaway<br />
when you install the implant. Natix is easy to<br />
apply, and there have been no infections.”<br />
Both Caspar Wohlfahrt’s and Hans Bystedt’s experiences<br />
with Natix indicate that the material is easy<br />
to handle. It is easy to place in bone defects and<br />
get the material to lie stable. A blood clot forms<br />
extremely quickly around the granules, which leads<br />
to a stable graft.<br />
More Information<br />
Tigran Technologies AB<br />
Medeon Science Park<br />
20512 Malmö<br />
SWEDEN<br />
Phone: +46 40 650-1665<br />
info@tigran.se<br />
www.tigran.se<br />
The product information produced here editorially is based on information<br />
provided by the manufacturer and has not been checked by the editor<br />
for its accuracy.
108 <strong>EDI</strong><br />
Product Reports<br />
The easy-to-use “two-in-one” solution is well suited<br />
for practitioners seeking a more robust diagnostic<br />
tool, especially implantologists or general practitioners<br />
placing implants. The system’s userfriendly<br />
design and intuitive s<strong>of</strong>tware interface<br />
enable it to be easily implemented in a dental practice,<br />
with a footprint similar to that <strong>of</strong> a traditional<br />
panoramic unit.<br />
The power <strong>of</strong> 3D made easy<br />
KODAK 9000 3D System by Carestream Health<br />
Low-dose Threedimensional<br />
Imaging<br />
Carestream Health, Inc., the exclusive manufacturer <strong>of</strong> KODAK <strong>Dental</strong> Systems, introduced the KODAK<br />
9000 3D Extraoral Imaging System. It enables dental pr<strong>of</strong>essionals to obtain localized, low-doses three-<br />
dimensional (3D) images as well as panoramic examinations at an affordable price – making the power<br />
and utility <strong>of</strong> 3D technology available to most dental pr<strong>of</strong>essionals.<br />
Three-dimensional digital imaging provides highly<br />
detailed images that show actual representations <strong>of</strong><br />
the patient’s anatomy that can be viewed from any<br />
direction. Using this modality, anatomical depth and<br />
relationships between individual features can be precisely<br />
identified and measured for more accurate<br />
diagnoses and treatment.<br />
However in the past, 3D imaging has typically<br />
been complex, expensive to implement, and <strong>of</strong>ten<br />
only performed by radiologists. Moreover, radiation<br />
dose associated with 3D imaging technology were<br />
relatively high. With the introduction <strong>of</strong> the KODAK<br />
9000 3D System, 3D diagnoses are now available to<br />
most dental practices. The system’s localized field <strong>of</strong><br />
view limits irradiation to the region <strong>of</strong> interest and<br />
shows an area <strong>of</strong> approximately three to six teeth in<br />
extraordinary detail, resulting in increased image<br />
accuracy and more detail per tooth. The 3D volume<br />
acquired can be used for any implant treatments,<br />
including both single and multiple site implant<br />
planning. The voxel (VOlume piXEL), which represents<br />
a quantity <strong>of</strong> 3D data similar to a pixel representation<br />
in 2D data, features an edge size (or minimum<br />
slice thickness) <strong>of</strong> 0.076 mm – providing 3D<br />
images that are among the highest resolution in<br />
the industry.<br />
3D exams available on-site<br />
Having 3D exams on-site helps dental pr<strong>of</strong>essionals<br />
provide quicker and more accurate diagnoses, and<br />
reduce the number <strong>of</strong> visits and the treatment time<br />
required significantly. Three-dimensional images<br />
allow implantologists to assess precise bone volume<br />
and quality, to identify anatomical obstacles, take 1:1<br />
measurements and to plan implants using KODAK 3D<br />
Imaging Module – all without having to send the<br />
patient to another imaging facility.<br />
KODAK 3D Imaging Module<br />
comes standard with the Kodak<br />
9000 3D System enabling simple<br />
and efficient manipulation <strong>of</strong> 3D<br />
exams, including an implant planning<br />
module that will simulate<br />
implant placement, take measurements<br />
(both distances and<br />
angles), and locate the mandibular<br />
canal. The high-resolution images and reduced<br />
radiation exposure <strong>of</strong> the KODAK 9000 3D System<br />
also benefit other dental applications, including<br />
endodontics, surgery, impaction, periapical lesion<br />
assessment and TMJ assessment.<br />
The KODAK 9000 3D System is available for sale. A<br />
version <strong>of</strong> the unit including an optional cephalometric<br />
module will be available starting October.<br />
More Information<br />
KODAK <strong>Dental</strong> Systems – Carestream Health<br />
Phone: +800 4567 7654 (Western Europe)<br />
Phone: +49 1805 274-010 (Eastern Europe & other countries)<br />
europedental@cshdental.com<br />
www.my90003d.com<br />
The product information produced here editorially is based on information<br />
provided by the manufacturer and has not been checked by the editor<br />
for its accuracy.<br />
Implant planning<br />
module.
Current Advances<br />
in <strong>Dental</strong> Implantology<br />
Mozo Grau has successfully completed a multicentric prospective implant study,<br />
underlining its continued support <strong>of</strong> scientific methods in dental implantology.<br />
Following up on the previous “Multicentric retrospective<br />
study <strong>of</strong> MG Osseous Implants” published in<br />
2006, which monitored 1001 MG Osseous implants in<br />
247 patients and showing an implant success rate <strong>of</strong><br />
97.8 percent after two years, Dr Serrano Caturla<br />
(Barcelona, Spain) has now concluded a new multicentric<br />
study on almost 1500 MG Osseous implants<br />
from Mozo Grau, this time showing an implant success<br />
rate <strong>of</strong> 98.2 percent after more than two years <strong>of</strong><br />
follow-up. In this study, the cases were prospectively<br />
evaluated.<br />
The design and development <strong>of</strong> the study was<br />
supervised by Scientific Management in O&SS, a<br />
Barcelona company specializing in such studies. The<br />
study included MG Osseous self-tapping, titanium<br />
implants and implants with RBM surface treatment.<br />
Each participating dentist was asked to complete<br />
detailed questionnaires to obtain detailed information<br />
on every patient. Forty-nine cases <strong>of</strong> successful<br />
implants were ultimately<br />
excluded due<br />
to insufficient questionnaire<br />
responses, attesting<br />
to the stringency <strong>of</strong> the<br />
study.<br />
These implants and patients continue<br />
under periodical monitoring, and Dr Serrano would<br />
like to extend the follow-up interval to a minimum <strong>of</strong><br />
five years, which would place this study among the<br />
most extensive long-term studies<br />
on implants.<br />
In early 2008, based on this<br />
information and experience, Mozo<br />
Grau launched the MG InHex<br />
implant with internal connector,<br />
which shares the successful features<br />
<strong>of</strong> the extensively studied<br />
MG Osseous implant.<br />
More Information<br />
Mozo Grau<br />
San Felipe Neri 2<br />
47002 Valladolid<br />
SPAIN<br />
Phone: +34 983 211-312<br />
sales@mozo-grau.com<br />
www.mozo-grau.com<br />
<strong>EDI</strong> 109<br />
Product Reports
110 <strong>EDI</strong><br />
Product Reports<br />
Orthopantomograph OP200 by<br />
Instrumentarium <strong>Dental</strong><br />
All-in-one X-ray Unit<br />
Instrumentarium <strong>Dental</strong> introduced new features in its Orthopantomograph. The new features <strong>of</strong> the<br />
original Orthopantomograph OP200 are designed to make premium dental imaging easier and safer for the<br />
patient – as well as to improve the productivity <strong>of</strong> dental practices.<br />
Optimized Lateral Ceph is designed to minimize the<br />
patient dose. The new Core Lateral Ceph imaging program<br />
decreases the radiation up to 68 percent compared<br />
to typical standard lateral ceph – yet with the<br />
same proven image quality Orthopantomograph has<br />
always been famous for. The starting point <strong>of</strong> the<br />
scan is fully adjustable and therefore enables the<br />
user to allow only the optimal area to be exposed.<br />
Regardless <strong>of</strong> the reduced exposed area all typical<br />
cephalometric tracing landmarks will be included in<br />
the core view. For quick and easy intraoral bitewing<br />
imaging Orthopantomograph OP200 is equipped<br />
with a new imaging program that produces a clear<br />
bitewing-like view <strong>of</strong> molar and premolar regions –<br />
from 1 st premolar to 3 rd molar with one easy exposure.<br />
This new feature <strong>of</strong>fers a comfortable alternative for<br />
patients with a strong gag reflex. Steady positioning<br />
as a very important step towards successful imaging<br />
is ensured with the new fully adjustable headrest. It<br />
<strong>of</strong>fers the strongest and steadiest head support<br />
available and is height adjustable for improved suitability<br />
for both child and adult patients.<br />
Nowadays efficiency is everything. Orthopantomograph<br />
improves the productivity <strong>of</strong> dental practices<br />
with faster operations and carefully designed<br />
automation. Quicker alignments and higher accuracy,<br />
self adjusting fully automatic collimation and easier<br />
unit installation make the unit even more efficient<br />
than before. New OP200 D produces a standard highresolution<br />
panoramic image in just 14,1 seconds. Lateral<br />
ceph scan takes only 5,2 seconds with child patients<br />
and 13,1 seconds with adults. In addition to these new<br />
features, which are now standard in every new unit,<br />
VT-Volumetric Tomography option expands the digital<br />
Orthopantomograph into an advanced tool for<br />
implantology. VT is an innovative digital tomography<br />
imaging tool which enables accurate and reliable<br />
measurements for implant site evaluation. VT produces<br />
a stack <strong>of</strong> cross-sectional slices targeted only on<br />
the region <strong>of</strong> interest. The reconstructed, wide volumetric<br />
view <strong>of</strong>fers 256 slices, from which the optimal<br />
slice or any number <strong>of</strong> slices can be viewed and easily<br />
navigated. Patient dose is kept low by exposing only<br />
the selected region <strong>of</strong> interest. Orthopantomograph<br />
OP200 combines premium quality panoramic,<br />
cephalometric and volumetric tomography imaging<br />
in a true all-in-one X-ray unit.<br />
More Information<br />
Instrumentarium <strong>Dental</strong><br />
Nahkelantie 160<br />
P.O. Box 20, FI-04301 Tuusula<br />
FINLAND<br />
Phone +358 45 7882-2000<br />
www.instrumentariumdental.com<br />
www.vt-cube.com<br />
The product information produced here editorially is based on information<br />
provided by the manufacturer and has not been checked by the editor<br />
for its accuracy.
112 <strong>EDI</strong><br />
Product Reports<br />
Intralift by Satelec<br />
Plug and Spray<br />
The new Intralift method for the ultrasonic generator Piezotome and the ImplantCenter from Satelec (Acteon Group) now<br />
enables dentists to lift the maxillary sinus membrane, by the crestal approach, gently and safely, and fill the new sinus space<br />
with augmentation material – with less room for mistakes and low rupture risk, thanks to the five new TKW instruments.<br />
Designed for ultrasonic drilling and Schneider membrane elevation by hydrodynamic effect, the augmentation material is then<br />
inserted into the osteotomy and compacted. The Intralift procedure thus combines the safety, effectiveness and visibility <strong>of</strong> an<br />
external sinus lift with the minimally-invasive internal sinus lift.<br />
The scope for use <strong>of</strong> piezoelectric ultrasound technology<br />
is constantly increasing. It is therefore not only<br />
suitable for prophylaxis, endodontics and periodontics.<br />
Oral surgeons can also benefit from the<br />
adjustable frequency and the technically-ingenious<br />
tips. With Intralift, Satelec has now introduced a<br />
completely new, minimally-invasive operational<br />
method for internal sinus elevation and bone augmentation.<br />
Minimally-invasive procedure<br />
The particularity <strong>of</strong> this procedure are the five specific<br />
TKW instruments which enable the hydrodynamic<br />
separation <strong>of</strong> the Schneider membrane, by means <strong>of</strong><br />
the modulated surgical mode and irrigation from the<br />
ultrasonic generator. Here, the new ultrasound-based<br />
Intralift method is not only the least invasive operational<br />
procedure currently available, but it is also the<br />
fastest and safest operational procedure for an internal<br />
sinus lift and pre-implant bone augmentation.<br />
Furthermore, it is just as effective as the classic lateral<br />
window technique.<br />
In the case <strong>of</strong> an upper residual bone height <strong>of</strong> less<br />
than 5 mm, bone augmentation should be carried<br />
out after raising the maxillary sinus membrane for<br />
implant placement. According to the surgical protocol<br />
for the Intralift, the new TKW1 to TKW4 diamond<br />
instruments are to be implemented for a stepwise<br />
bone preparation, taking into account bone density<br />
and thickness. With a maximum diameter <strong>of</strong> 2.8 mm,<br />
these tips make an exceptionally gentle cut into the<br />
hard tissue only (selective incision), precisely and free<br />
from bleeding. In this way they will create a microsurgical<br />
access as in the keyhole technique, contrary<br />
to an invasive, external sinus lift.<br />
Hydrodynamic sinus lift<br />
After the stepwise pilot drilling, the smooth TKW5<br />
tip, with internal irrigation to the extremity <strong>of</strong> the tip,<br />
is first inserted in the cavity to lift the Schneider<br />
membrane by hydrodynamic effect. After the elevation,<br />
the TKW5 can be used to insert a collagen fleece<br />
as a protection against possible rupture <strong>of</strong> the sinus<br />
membrane. The augmentation material is then carefully<br />
moved cranially with the tip. If the material is<br />
compacted strongly, the activation <strong>of</strong> this novel plugging<br />
and trumpet instrument, with a low water flow<br />
rate, will cause an automatic dispersion <strong>of</strong> the augmentation<br />
material in the newly formed sinus cavity.<br />
According to the “Plug and Spray” principle, new<br />
material is now alternately inserted, compacted and<br />
then spread using water pressure from the piezoelectrically-activated<br />
TKW5 tip – until a safe primary stability<br />
is achieved for the implant.<br />
Reduced operational trauma<br />
Besides the simple handling for the operator, the new<br />
Intralift is also characterized by a comfortable and<br />
stressless procedure for the patient. Thus the new<br />
minimally-invasive sinus lift proce-<br />
dure causes hardly any post-operative<br />
swelling, pain or bleeding. The<br />
shortened and improved bone regeneration<br />
through piezo surgery is also<br />
certain to convince both parties.<br />
The Intralift TKW1 to TKW5 tips are<br />
now available in a special Intralift<br />
Kit (ref. F87336). They can be used<br />
with both the high-performance<br />
ultrasonic generator Piezotome as<br />
well as the ImplantCenter.<br />
More Information<br />
Satelec-Acteon Equipment<br />
17 avenue Gustave Eiffel<br />
F-33708 Merignac<br />
FRANCE<br />
Phone: +33 556 340607<br />
satelec@acteongroup.com<br />
www.acteongroup.com<br />
The product information produced here editorially<br />
is based on information provided by the<br />
manufacturer and has not been checked by<br />
the editor for its accuracy.
114 <strong>EDI</strong><br />
Product News<br />
Leone Exacone 360°<br />
The anatomical abutments Exacone 360° have got<br />
the ideal characteristics to facilitate the prosthetic<br />
procedure both during the phase <strong>of</strong> choice and customizing<br />
in the laboratory and in the following clinical<br />
procedures.<br />
The main innovation <strong>of</strong> the product, protected by<br />
an international patent, is the realization <strong>of</strong> the apical<br />
hexagon separated from the abutment: this<br />
allows a free positioning to 360° on the model and<br />
makes the correction <strong>of</strong> disparallelism easy by using<br />
the anatomical form <strong>of</strong> the abutment to the utmost.<br />
With the activation <strong>of</strong> the selfblocking<br />
conic connection afterwards,<br />
the abutment will join the<br />
hexagon directed in the selected<br />
position and it will drive the clinician<br />
in the positioning on patient<br />
with the maximum precision.<br />
The anatomical abutments Exacone<br />
360° are available straight or<br />
angled at 15° or 25° to answer all<br />
demands for prosthetic rehabilitation.<br />
An indent on the angled<br />
abutment allows the activation<br />
<strong>of</strong> the connection by exerting a<br />
coaxial force to the axis <strong>of</strong> the<br />
implant. A special flat tip may<br />
be joined to the multi-purpose<br />
handle or contra-angle hand<br />
piece assuring a stable support.<br />
Zimmer <strong>Dental</strong> Instrument Kit System<br />
Zimmer <strong>Dental</strong> Inc. has released the new and<br />
improved Zimmer Instrument Kit System. With its<br />
user-friendly layout and logical color-coding system,<br />
it is designed to enable clinicians to get the most out<br />
<strong>of</strong> the popular Tapered Screw Vent and Zimmer One-<br />
Piece Implants.<br />
The Zimmer Instrument Kit System is an easy to<br />
learn, well organized product family that can be customized<br />
to meet individual clinical needs and maximize<br />
valuable time. A simple color coding system<br />
enables clinicians to intuitively follow surgical sequences,<br />
step-by-step. In addition, the Tapered Screw-<br />
Vent Surgical Kit can be combined with an optional<br />
Zimmer One-Piece Implant Module for streamlined<br />
placement <strong>of</strong> all components <strong>of</strong> the renowned Tapered<br />
Screw-Vent Implant System – thereby creating<br />
a truly centralized, all-in-one kit.<br />
Each Tapered Screw-Vent Surgical Kit includes instruments<br />
needed to place any Tapered Screw-Vent<br />
Implant, including the popular 4.1 mm line. All kit configurations<br />
also leave extra storage space for additional<br />
pieces. An accompanying Staging Block allows users<br />
to place a selection <strong>of</strong> instruments<br />
and implants needed for a procedure<br />
within reach. A separate Zimmer<br />
One-Piece Kit is also available<br />
for new users who want to begin<br />
their experience with Zimmer<br />
<strong>Dental</strong> by treating tight interdental<br />
spaces.<br />
To help clinicians get the most<br />
out <strong>of</strong> the Zimmer Instrument Kit<br />
System, cleaning and sterilization<br />
instructions for instruments and<br />
Driva Drills as well as surgical<br />
sequences are included in a handy<br />
guide that comes with every kit.<br />
Product:<br />
Exacone 360° anatomical<br />
abutments<br />
Indication:<br />
Anatomical abutments<br />
Distribution:<br />
Leone S.p.A.<br />
Via P. a Quaracchi, 50<br />
50019 Sesto Fiorentino (Fi)<br />
ITALY<br />
Phone: +39 055 3044-620<br />
info@leone.it<br />
www.leone.it<br />
Product:<br />
Zimmer Instrument Kit System<br />
Indication:<br />
Instrument kit system<br />
Distribution:<br />
Zimmer <strong>Dental</strong> Inc.<br />
USA<br />
Phone Germany: +49 761 15647-0<br />
Phone Spain: +34 93 84605-43<br />
Phone France: +33 1 451235-66<br />
Phone Italy: +39 043 85555-73<br />
Phone Israel: +972 3 612-4242<br />
www.zimmerdental.com
In case <strong>of</strong> immediate implantation<br />
there is a great risk to contaminate<br />
the jaw bone with connective<br />
tissue fibre <strong>of</strong> the s<strong>of</strong>t tissue.<br />
The new Aesculap Ergoplant<br />
Immediate Implant Retractor<br />
ensures a save implantation by<br />
holding back the alveolar s<strong>of</strong>t<br />
tissue. Thereby working will be<br />
safer, easier and more comfortable.<br />
<strong>EDI</strong> 115<br />
Product News<br />
Aesculap<br />
Ergoplant Immediate Implant Retractor<br />
Product:<br />
Ergoplant Immediate Implant<br />
Retractor<br />
Indication:<br />
Implant retractor<br />
Distribution:<br />
Aesculap AG & CO KG<br />
Am Aesculap-Platz<br />
78352 Tuttlingen<br />
GERMANY<br />
Phone: +49 7461 95-2467<br />
dental@aesculap.de<br />
www.aesculap-dental.com
116 <strong>EDI</strong><br />
Product News<br />
Kohdent Medizintechnik Trinovo<br />
The Micro-Perio Instrument Set Trinovo provides<br />
the dentist with essential instruments for perio -<br />
dontic s<strong>of</strong>t-tissue management and dental surgery.<br />
They allow delicate ablation <strong>of</strong> interstitial papillae<br />
and mucoperiosteal flaps without the risk <strong>of</strong> ripping,<br />
which is always difficult to suture. Thanks<br />
to the instruments’ efficient mode <strong>of</strong> operation,<br />
which show a steadily continuous widening geometry,<br />
every intrusion can be carried out with<br />
extreme precision.<br />
The instruments <strong>of</strong>fer different working tips at<br />
both ends. Through a combination <strong>of</strong> periosteal elevator<br />
and gingiva retractor, the total number <strong>of</strong><br />
required instruments is lessened and, on the other<br />
hand, influences<br />
ergonomic<br />
handling and rapid processing<br />
during surgery. The<br />
Trinovo grip guarantees comfortable<br />
posture and instrument<br />
handling during surgery. The<br />
grip’s pr<strong>of</strong>ile is also remarkable.<br />
The geometry guarantees not<br />
only effective instrument stabilisation,<br />
but also <strong>of</strong>fers the advantage<br />
<strong>of</strong> being completely sterilisable<br />
without having impedimental<br />
retentive recesses.<br />
Hirschmann Instruments<br />
ART Plus and Implant Viewer<br />
Hirschmann Instruments presents the dental<br />
panoramic digital imaging system ART Plus made by<br />
the Finnish company AJAT. The highlight <strong>of</strong> this unit<br />
is its CdTe-CMOS sensor that converts x-rays directly<br />
into electrical signals. ART Plus <strong>of</strong>fers exceptional<br />
image quality and some advanced and unique image<br />
processing features such as the ability to select different<br />
focal planes and convert them. The image area<br />
can be enlarged without any loss in quality. Starting<br />
immediately, Hirschmann Instruments will also market<br />
AJAT’s retr<strong>of</strong>itting kits for converting panoramic<br />
analogue imaging systems to benefit from state-<strong>of</strong>the-art<br />
CdTe sensor technology, allowing the digitiza-<br />
tion <strong>of</strong> legacy systems at competitive<br />
prices.<br />
The Implant Viewer by Anne Solutions,<br />
also marketed by Hirsch -<br />
mann Instruments, is an elegant<br />
s<strong>of</strong>tware solution for exporting reconstructed<br />
DICOM axials to STL<br />
files. DVT diagnostic centres and<br />
dental radiologists can now pass<br />
on the original 3D data to their<br />
customers, which can use the<br />
viewer s<strong>of</strong>tware free <strong>of</strong> charge. The<br />
viewer s<strong>of</strong>tware facilitates multiplanar<br />
representations <strong>of</strong> the selected<br />
jaw region and allows implant<br />
positions to be determined<br />
and distances and angle measurements<br />
to be applied.<br />
Product:<br />
Trinovo<br />
Indication:<br />
Micro-Perio instrument set<br />
Distribution:<br />
Kohdent Roland Kohler Medizintechnik<br />
GmbH & Co. KG<br />
Danningen 9<br />
78579 Neunhausen<br />
GERMANY<br />
Phone: +49 7777 9395-30<br />
info@kohler-medizintechnik.de<br />
www.kohler-medizintechnik.de<br />
Product:<br />
ART Plus<br />
Implant Viewer<br />
Indication:<br />
<strong>Dental</strong> panoramic digital imaging<br />
system<br />
S<strong>of</strong>tware for exporting reconstructed<br />
DICOM axials to STL files<br />
Distribution:<br />
Hirschmann Instruments GmbH<br />
Kramerstr. 17<br />
82061 Neuried<br />
GERMANY<br />
Phone: +49 89 7592206<br />
www.hirschmann-instruments.de
Mozo Grau<br />
Abutments for Immediate Loading<br />
In order to cover the latest<br />
implantological techniques, such<br />
as immediate loading, Mozo Grau<br />
has launched a collection <strong>of</strong> new<br />
abutments suitable for use when<br />
an immediate aesthetic solution<br />
is required by the patient before<br />
the definitive prosthesis is delivered.<br />
These components extend<br />
the range <strong>of</strong> prosthetic options<br />
when restoring MG Osseous and<br />
MG InHex implants.<br />
Designed jointly with experienced<br />
clinical pr<strong>of</strong>essionals, these<br />
abutments have thinner walls,<br />
which makes them suitable for<br />
customization in the patient´s<br />
mouth without presenting an<br />
overheating hazard. Their special<br />
surface facilitates cement adhesion<br />
and improves the retention<br />
<strong>of</strong> the provisional. To facilitate<br />
adjustment, all Mozo Grau components<br />
for immediate loading<br />
are supplied with a plastic cap<br />
that allows the cementation <strong>of</strong><br />
the provisional to the abutment.<br />
This new range for use with<br />
the immediate loading technique<br />
includes castable and titanium<br />
abutments for direct restorations<br />
on implants and for trans epitelial<br />
abutments such as the tapered<br />
abutment. The tapered abutment<br />
is recommended for immediate<br />
loading in the mandible, allowing<br />
the placement and removal <strong>of</strong> a<br />
provisional without adversely<br />
affecting the s<strong>of</strong>t tissues. Its conical<br />
design allows the provisional to be<br />
perfectly adjusted to the implants<br />
even in the presence <strong>of</strong> an axial<br />
divergence <strong>of</strong> 10 to 30 degrees.<br />
The precision <strong>of</strong> all abutments,<br />
together with the self-locking<br />
morse taper connection and the<br />
internal double hex interlock <strong>of</strong><br />
the MG InHex implant, assure a<br />
perfect passive fit <strong>of</strong> the provisionals<br />
for single- and multipletooth<br />
restorations.<br />
Product:<br />
Abutments for immediate loading<br />
Indication:<br />
Provisional for immediate loading<br />
Distribution:<br />
Mozo Grau<br />
San Felipe Neri . 247002 Valladolid . SPAIN<br />
Phone: +34 983 211-312<br />
sales@mozo-grau.com . www.mozo-grau.com<br />
<strong>EDI</strong> 117<br />
Product News
118 <strong>EDI</strong><br />
Product News<br />
Bicon SynthoGraft<br />
SynthoGraft is a synthetic, biocompatible and<br />
resorbable granular ceramic made <strong>of</strong> pure phase<br />
Beta-Tricalcium Phosphate (Ca 3 (PO 4 ) 2 ) for oral and<br />
maxill<strong>of</strong>acial bone regeneration or augmentation.<br />
SynthoGraft was developed to create an augmentation<br />
material that would perform to high levels <strong>of</strong> efficiency<br />
in both rate and quality <strong>of</strong> regeneration. SynthoGraft<br />
has a unique structure that provides stabili-<br />
With the Piezon Master Surgery from EMS the Piezon<br />
method is now also available in dental and oral surgery.<br />
The method is based on piezoceramic ultrasound<br />
waves which generate high-frequency, straight-line<br />
oscillations. These vibrations increase the precision<br />
and safety in surgical applications. Thus the ultrasound<br />
drive enables micrometric incision in the range<br />
<strong>of</strong> 60 to 200 micrometers, in which only a little bone<br />
substance is lost. The ultrasound instruments cut only<br />
hard tissue selectively; s<strong>of</strong>t tissue remains conserved.<br />
In addition, a largely bloodless operation field results<br />
from the high-frequency vibrations with permanent<br />
cooling thus thermal necroses are prevented.<br />
Piezon Master Surgery can be used in periodontal,<br />
oral and maxillary surgery as well as in implantology.<br />
Distinct indications are osteotomy and osteoplasty,<br />
extraction, root tip resection, cystectomy, gaining<br />
bone blocks, sinus lift, nerve transposition, alveolar<br />
ridge cleavage and harvesting autologous bone.<br />
Operation using the touch board is especially simple<br />
and hygienic: One can set both the power and the flow<br />
rate <strong>of</strong> the isotonic solution by brushing one’s finger<br />
over the recessed operating elements. The LED reacts to<br />
ty, while its micro-porosity enables<br />
rapid vascularisation and subsequent<br />
resorption when mixed<br />
with the patient’s own blood.<br />
Several varieties <strong>of</strong> Beta-Tricalcium<br />
Phosphate are now commercially<br />
available, but their bone regenerating<br />
capabilities are not<br />
equal. These differences can affect<br />
not only the rate and quality <strong>of</strong><br />
bone regeneration, but also the<br />
rate <strong>of</strong> resorption and replacement<br />
with autogenous bone during<br />
the healing process.<br />
Additionally, SynthoGraft <strong>of</strong>fers<br />
clinicians and patients the confidence<br />
<strong>of</strong> knowing that they have a<br />
completely synthetic bone graft<br />
material, eliminating the inherent<br />
risks associated with biologicallyderived<br />
bone graft materials.<br />
the stroke <strong>of</strong> the finger with a low<br />
signal – even if your hand is in surgical<br />
gloves and an additional protective<br />
foil is used. Corners, joints<br />
and gaps were dispensed with in<br />
the design for the sake <strong>of</strong> hygiene.<br />
Piezon Master Surgery is <strong>of</strong>fered<br />
as basic system with five<br />
instruments for use in<br />
implant preparations.<br />
Optional systems for<br />
tooth extraction, retrograde<br />
root channel<br />
preparation and operations<br />
on the bone are<br />
also available. All<br />
systems contain<br />
autoclavable<br />
Combi torques<br />
and a Steribox.<br />
Product:<br />
SynthoGraft<br />
Indication:<br />
Oral and maxill<strong>of</strong>acial bone<br />
regeneration or augmentation<br />
Distribution:<br />
Bicon Europe, Ltd.<br />
Phone: +353 61 303-494<br />
www.synthograft.com<br />
www.bicon.com<br />
EMS Electro Medical Systems Piezon Master Surgery<br />
Product:<br />
Piezon Master Surgery<br />
Indication:<br />
Bone cutting using ultrasound<br />
Distribution:<br />
EMS Electro Medical Systems S.A.<br />
Chemin de la Vuarpillière 31<br />
CH-1260 Nyon<br />
SWITZERLAND<br />
Phone +41 22 9944700<br />
welcome@ems-dent.com<br />
www.ems-company.com
Implant Direct SwissPlant Implant<br />
Product:<br />
SwissPlant implant<br />
Indication:<br />
<strong>Dental</strong> implant system<br />
Distribution:<br />
Implant Direct Europe AG<br />
Förrlibuckstrasse 150<br />
8005 Zürich<br />
SWITZERLAND<br />
Phone: +41 848 345534<br />
info-eu@implantdirect.com<br />
www.implantdirect.eu<br />
After the successful start <strong>of</strong> the<br />
<strong>European</strong> business with its own<br />
Spectra system and compatible<br />
implant lines with other implant<br />
manufacturers, Implant Direct is<br />
expanding its product portfolio<br />
with implants and prosthetic<br />
parts that are compatible with<br />
Straumann. The SwissPlant implant<br />
is both surgically and prosthetically<br />
compatible with Straumann<br />
Standard/Standard Plus implants.<br />
This gives Straumann users the<br />
advantage <strong>of</strong> inserting SwissPlant<br />
<strong>EDI</strong> 119<br />
Product News<br />
implants without purchasing another surgical kit.<br />
The SwissPlant implants come with endosteal diameters<br />
<strong>of</strong> 4.1 mm and 4.8 mm, and with implant<br />
lengths <strong>of</strong> 8, 10, 12, 14 and 16 mm, all with the characteristic<br />
blasted, micro-rough surface <strong>of</strong> Implant<br />
Direct. The prosthetic platform includes the traditional<br />
internal octagon <strong>of</strong> Straumann’s implant-prosthetic<br />
connection. The implant has been improved to<br />
include mini-threads in the upper implant body<br />
reducing tensions in crestal bone, as well as double<br />
lead threads in the appical area. Due to the microrough<br />
surface <strong>of</strong> the implant neck it can be used for<br />
one-stage or two-stage procedures, providing a maximum<br />
<strong>of</strong> treatment flexibility. The implant comes in<br />
an innovative All-In-One kit including prosthetic<br />
components such as a cover screw, a healing cap, a<br />
comfort cap, a transfer, and a straight abutment with<br />
a significant price advantage.
120 <strong>EDI</strong><br />
Product News<br />
Dr. Ihde <strong>Dental</strong> SSO Implants<br />
More protection against early<br />
implant loss and a consistently<br />
high primary stability are the<br />
most important advantages <strong>of</strong><br />
the new Dr. Ihde <strong>Dental</strong> SSO<br />
implant surface. At the core <strong>of</strong><br />
this significant innovation there<br />
is an ultra-thin NaCl coating. It<br />
exerts a biocidal effect while<br />
returning to the bone a fair share<br />
<strong>of</strong> the mineral salt that is invariably<br />
lost during preparation <strong>of</strong><br />
the implant bed.<br />
Dr. Ihde <strong>Dental</strong> breaks new<br />
ground when it comes to ensuring<br />
primary implant success. To<br />
date, it has not been possible to<br />
avoid or compensate for the loss<br />
<strong>of</strong> salt that occurs in the bone<br />
Satelec Extraction Kit<br />
The Extraction Kit is the latest addition to the range<br />
<strong>of</strong> ultrasonic surgical tips from Satelec. Compatible<br />
with Piezotome and ImplantCenter power generators,<br />
this new kit <strong>of</strong> six tips has been especially developed<br />
for extractions (total or partial): avulsions,<br />
hemisections and root amputations. The Extraction<br />
Kit presents many clinical advantages for the practitioner:<br />
the slimness <strong>of</strong> these tips associated with<br />
ultrasonic technology facilitates their access inside<br />
the desmodontal space, and thanks to the selective<br />
cut, the tips are inactive on s<strong>of</strong>t tissue and sensitive<br />
anatomical components. Without any inertia, the<br />
regular to-and-fro movement decreases the risk <strong>of</strong><br />
lesions on adjacent teeth and roots. The use <strong>of</strong> this<br />
kit will also provide benefit to patients who will experience<br />
swift and less traumatic treatment that<br />
respects the alveolar plate, as well as less post-operative<br />
pain.<br />
This kit, which is directed mainly towards general<br />
practitioners and stomatologists, consists <strong>of</strong> five LC<br />
tips and one Ninja tip. The LC tips are intended for syndesmotomies<br />
and periradicular osteotomies. With differing<br />
shapes and orientations, they address the morphological<br />
constraints without damaging neighbouring<br />
tissue and anatomical elements. Combined with<br />
during implant-bed preparation – not even by using a<br />
physiological saline solution or Ringer’s lactate for<br />
irrigation. The Osmoactive surface proactively tackles<br />
the salt-loss problem while at the same time creating<br />
the best possible environment for osteoblasts to<br />
develop. A recent study conducted at the University<br />
<strong>of</strong> Würzburg, Germany (to be published shortly) has<br />
shown that implants with an Osmoactive surface<br />
have bactericidal properties yet do not inhibit<br />
osteoblast growth – without requiring the use <strong>of</strong><br />
antibiotics or other unwanted chemicals.<br />
Dr. Ihde <strong>Dental</strong> manufactures 16 crestal<br />
and basal implant systems.<br />
The product catalog is<br />
available in German<br />
and English.<br />
the action <strong>of</strong> ultrasonic microoscillations,<br />
they achieve, with<br />
just a simple sweeping movement<br />
around the tooth, detachment <strong>of</strong><br />
the periodontal ligament in order<br />
to facilitate avulsion <strong>of</strong> the tooth<br />
outside the alveolus. The Ninja<br />
tip with double saw-tooth edges<br />
was developed especially for hemisections<br />
and root amputations.<br />
This tip is also recommended for<br />
sectioning impacted teeth. The<br />
Ninja’s selective and accurate cut<br />
allows the practitioner to achieve<br />
faster and less invasive surgery.<br />
Product:<br />
SSO Implants with<br />
Osmoactive Surface<br />
Indication:<br />
<strong>Dental</strong> implant<br />
Distribution:<br />
Dr. Ihde <strong>Dental</strong> AG<br />
Lindenstrasse 68<br />
8738 Uetliburg/SG<br />
SWITZERLAND<br />
Phone: +41 552 932-323<br />
info@implant.com<br />
www.implant.com<br />
Product:<br />
Extraction Kit<br />
Indication:<br />
Tips for extractions<br />
Distribution:<br />
Satelec-Acteon Equipment<br />
17 avenue Gustave Eiffel<br />
F-33708 Merignac<br />
FRANCE<br />
Phone: +33 556 340607<br />
satelec@acteongroup.com<br />
www.acteongroup.com
122 <strong>EDI</strong><br />
Calendar <strong>of</strong> Events<br />
CALENDAR OF EVENTS<br />
2008/2009 Event Location Date Details/Registration<br />
September Swedental Stockholm, Sweden September 24-27,<br />
2008<br />
FDI Annual World <strong>Dental</strong> Congress<br />
2008<br />
Stockholm, Sweden September 24-27,<br />
2008<br />
October <strong>Dental</strong> Showcase 2008 London, England October 2-4,<br />
2008<br />
Dentex 2008 Brussels, Belgium October 16-18,<br />
2008<br />
Reunión de SEPES 2008 Zaragoza, Spain October 16-18,<br />
2008<br />
November 12 th BDIZ <strong>EDI</strong> Symposium Frankfurt/Main,<br />
Germany<br />
XXIV Congreso Nacional/<br />
XVII Congreso Internacional de S.E.I.<br />
November 7-8,<br />
2008<br />
Oviedo, Spain November 13-15,<br />
2008<br />
Congrès de l’ADF Paris, France November 25-29,<br />
2008<br />
February Chicago <strong>Dental</strong> Society Midwinter<br />
Meeting<br />
March 33 rd International <strong>Dental</strong> Show<br />
(IDS) 2009<br />
<strong>EDI</strong> – Information for Authors<br />
<strong>EDI</strong> – the interdisciplinary journal for prosthetic dental implantology is<br />
aimed at dentists (and technicians) interested in prosthetics implantology.<br />
All contributions submitted should be focused on this aspect in content<br />
and form. Suggested contributions may include:<br />
. Case studies<br />
. Original scientific research<br />
. Overviews<br />
Manuscript Submission<br />
Submissions should include the following:<br />
. two hard copies <strong>of</strong> the manuscript<br />
. a disk copy <strong>of</strong> the manuscript,<br />
. a complete set <strong>of</strong> illustrations<br />
Original articles will be considered for publication only on the condition<br />
that they have not been published elsewhere in part or in whole and are<br />
not simultaneously under consideration elsewhere.<br />
Manuscripts<br />
Pages should be numbered consecutively, starting with the cover page.<br />
The cover page should include the title <strong>of</strong> the manuscript and the name<br />
and degree for all authors. Also included should be the full postal address,<br />
telephone number, fax number, and electronic mail address <strong>of</strong> the contact<br />
author. The second page should contain an abstract that summarizes the<br />
article in approximately 100 words.<br />
Manuscripts can be organized in a manner that best fits the specific goals<br />
<strong>of</strong> the article, but should always include an introductory section, the body<br />
<strong>of</strong> the article and a conclusion.<br />
Figures and Tables<br />
Each article should contain a minimum <strong>of</strong> 20 and a maximum <strong>of</strong> 50 origi -<br />
nal color slides (35 mm) or digital photos, except in unusual circumstances.<br />
The slides will be returned to the author after publication. Slides<br />
should be numbered on the mount in the sequential numerical order in<br />
which they appear in the text (Fig. 1, Fig. 2, etc.).<br />
Chicago, USA February 26 - March 1,<br />
2009<br />
Cologne, Germany March 24-28,<br />
2009<br />
Editors Office: teamwork media GmbH . Hauptstr. 1 . 86925 Fuchstal/Germany<br />
Phone: +49 8243 9692-0 . Fax: +49 8243. 9692-22 . E-mail: service@teamwork-media.de<br />
Stockholm International Fairs<br />
Phone: +46 8749 43-88<br />
www.swedental.org<br />
FDI World <strong>Dental</strong> Federation<br />
congress@fdiworldental.org<br />
www.fdiworldental.org<br />
British <strong>Dental</strong> Trade <strong>Association</strong><br />
www.dentalshowcase.com<br />
C.V. Dentex International S.C.<br />
Phone: +32 2478 1441<br />
www.dentex.be<br />
SEPES – Sociedad Española de Prótesis<br />
Estomatológica<br />
Phone: +34 91 576-5340<br />
www.sepes.org<br />
BDIZ <strong>EDI</strong><br />
Phone: +49 228 9359-244<br />
www.bdizedi.org<br />
S.E.I. – Sociedad Española de Implantes<br />
www.infomed.es/sei<br />
<strong>Association</strong> Dentaire Française<br />
Phone: +33 0158 221710<br />
adf@adf.asso.fr<br />
www.adfcongres.com<br />
Chicago <strong>Dental</strong> Society (CDS)<br />
Phone: +1 312 836-7300<br />
www.cds.org<br />
Koelnmesse GmbH<br />
Phone: +49 180 577-3577<br />
www.ids-cologne.de<br />
Radiographs, charts, graphs, and drawn figures are also accepted.<br />
Figure legends should be brief one or two-line descriptions <strong>of</strong> each figure,<br />
typed on a separate sheet following the references. Legends should be<br />
numbered in the same numerical order as the figures.<br />
Tables should be typed on separate sheets and numbered consecutively,<br />
according to citation in the text. The title <strong>of</strong> the table and its caption<br />
should be on the same sheet as the table itself.<br />
References<br />
Each article should contain a minimum <strong>of</strong> 10 and a maximum <strong>of</strong> 30 references,<br />
except in unusual circumstances. Citations in the body <strong>of</strong> the text<br />
should be made in numerical order. The reference list should be typed on<br />
a separate sheet and should provide complete bibliographical information<br />
in the format exemplified below:<br />
[1] Albrektsson, T.: A multicenter report on osseointegrated oral implants. J<br />
Prosthet Dent 1988; 60, 75-82.<br />
[2] Hildebrand, H. F., Veron, Chr., Martin, P.: Nickel, chromium, cobalt dental<br />
alloys and allergic reactions: an overview. Biomaterials 10, 545-548, (1989)<br />
[3] Johanson, B., Lucas, L., Lemons, J.: Corrosion <strong>of</strong> copper, nickel and gold<br />
dental alloys: an in vitro and in vivo study. J Biomed Mater Res 23, 349,<br />
(1989)<br />
Review Process<br />
Manuscripts will be reviewed by three members <strong>of</strong> the editorial board.<br />
Authors are not informed <strong>of</strong> the identity <strong>of</strong> the reviewers and reviewers<br />
are not provided with the identity <strong>of</strong> the author. The review cycle will be<br />
completed within 60 days. Publication is expected within 9 months.<br />
Page Charges and Reprints<br />
There are no page charges. The publisher will cover all costs <strong>of</strong> production.<br />
The journal will provide the primary author with 20 tear sheets and a free<br />
copy <strong>of</strong> the journal issue in which the article appears.