HRSA Service Category Title - Harris County's New Web Site!
HRSA Service Category Title - Harris County's New Web Site!
HRSA Service Category Title - Harris County's New Web Site!
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
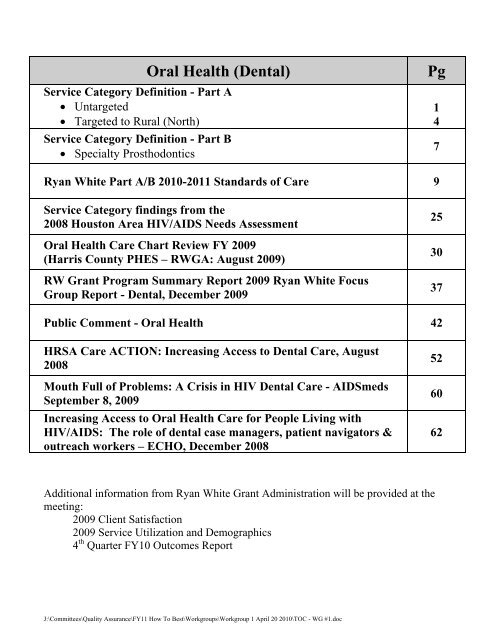
<strong>Service</strong> <strong>Category</strong> Definition - Part A<br />
� Untargeted<br />
� Targeted to Rural (North)<br />
<strong>Service</strong> <strong>Category</strong> Definition - Part B<br />
� Specialty Prosthodontics<br />
Oral Health (Dental) Pg<br />
Ryan White Part A/B 2010-2011 Standards of Care 9<br />
<strong>Service</strong> <strong>Category</strong> findings from the<br />
2008 Houston Area HIV/AIDS Needs Assessment<br />
Oral Health Care Chart Review FY 2009<br />
(<strong>Harris</strong> County PHES – RWGA: August 2009)<br />
RW Grant Program Summary Report 2009 Ryan White Focus<br />
Group Report - Dental, December 2009<br />
Public Comment - Oral Health 42<br />
<strong>HRSA</strong> Care ACTION: Increasing Access to Dental Care, August<br />
2008<br />
Mouth Full of Problems: A Crisis in HIV Dental Care - AIDSmeds<br />
September 8, 2009<br />
Increasing Access to Oral Health Care for People Living with<br />
HIV/AIDS: The role of dental case managers, patient navigators &<br />
outreach workers – ECHO, December 2008<br />
Additional information from Ryan White Grant Administration will be provided at the<br />
meeting:<br />
2009 Client Satisfaction<br />
2009 <strong>Service</strong> Utilization and Demographics<br />
4 th Quarter FY10 Outcomes Report<br />
J:\Committees\Quality Assurance\FY11 How To Best\Workgroups\Workgroup 1 April 20 2010\TOC - WG #1.doc<br />
1<br />
4<br />
7<br />
25<br />
30<br />
37<br />
52<br />
60<br />
62
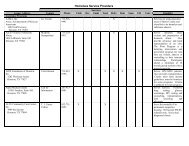
<strong>HRSA</strong> <strong>Service</strong> <strong>Category</strong><br />
<strong>Title</strong>: (RWGA only)<br />
Local <strong>Service</strong> <strong>Category</strong><br />
<strong>Title</strong>:<br />
Budget Type:<br />
(RWGA only)<br />
Budget Requirements or<br />
Restrictions:<br />
(RWGA only)<br />
<strong>HRSA</strong> <strong>Service</strong> <strong>Category</strong><br />
Definition:<br />
(RWGA only)<br />
Local <strong>Service</strong> <strong>Category</strong><br />
Definition:<br />
Target Population (age,<br />
gender, geographic, race,<br />
ethnicity, etc.):<br />
Oral Health<br />
Oral Health<br />
Unit Cost<br />
Not Applicable<br />
Oral health care includes diagnostic, preventive, and therapeutic<br />
services provided by general dental practitioners, dental specialists,<br />
dental hygienists and auxiliaries, and other trained primary care<br />
providers.<br />
Restorative dental services, oral surgery, root canal therapy, fixed<br />
and removable prosthodontics; periodontal services includes<br />
subgingival scaling, gingival curettage, osseous surgery,<br />
gingivectomy, provisional splinting, laser procedures and<br />
maintenance. Oral medication (including pain control) for HIV<br />
patients 15 years old or older must be based on a comprehensive<br />
individual treatment plan.<br />
HIV/AIDS infected individuals residing within the Houston Eligible<br />
Metropolitan Area (EMA).<br />
<strong>Service</strong>s to be Provided: <strong>Service</strong>s must include, but are not limited to: individual<br />
comprehensive treatment plan; diagnosis and treatment of HIVrelated<br />
oral pathology, including oral Kaposi’s Sarcoma, CMV<br />
ulceration, hairy leukoplakia, xerostomia, lichen planus, aphthous<br />
ulcers and herpetic lesions; diffuse infiltrative lymphocytosis;<br />
standard preventive procedures, including oral hygiene instruction,<br />
diet counseling and home care program; oral prophylaxis;<br />
restorative care; oral surgery including dental implants; root canal<br />
therapy; fixed and removable prosthodontics including crowns and<br />
bridges; periodontal services, including subgingival scaling, gingival<br />
curettage, osseous surgery, gingivectomy, provisional splinting,<br />
laser procedures and maintenance. Proposer must have mechanism<br />
in place to provide oral pain medication as prescribed for clients by<br />
<strong>Service</strong> Unit Definition(s):<br />
(RWGA only)<br />
FY 2011 Oral Health: Untargeted – Part A<br />
DRAFT (as of 03-23-10)<br />
the dentist.<br />
A unit of service is defined as one (1) dental visit which includes<br />
restorative dental services, oral surgery, root canal therapy, fixed<br />
and removable prosthodontics; periodontal services includes<br />
subgingival scaling, gingival curettage, osseous surgery,<br />
gingivectomy, provisional splinting, laser procedures and<br />
maintenance. Oral medication (including pain control) for HIV<br />
patients 15 years old or older must be based on a comprehensive<br />
individual treatment plan.<br />
Financial Eligibility: Refer to the RWPC’s approved Financial Eligibility for Houston<br />
Page 1 of 72
EMA <strong>Service</strong>s.<br />
Client Eligibility: HIV-infected adults residing in the Houston EMA meeting financial<br />
eligibility criteria.<br />
Agency Requirements: Agency must document that the primary patient care dentist has 2<br />
years prior experience treating HIV disease and/or on-going HIV<br />
educational programs that are documented in personnel files and<br />
updated regularly.<br />
Staff Requirements: State of Texas dental license; licensed dental hygienist and state<br />
Special Requirements:<br />
(RWGA only)<br />
FY 2011 Oral Health: Untargeted – Part A<br />
DRAFT (as of 03-23-10)<br />
radiology certification for dental assistants.<br />
None.<br />
Page 2 of 72
FY 2011 Oral Health: Untargeted – Part A<br />
DRAFT (as of 03-23-10)<br />
FY 2011 RWPC “How to Best Meet the Need” Decision Process<br />
Step in Process: Council<br />
Recommendations: Approved: Y_____ No: ______<br />
Approved With Changes:______<br />
1.<br />
2.<br />
3.<br />
Step in Process: Steering Committee<br />
Recommendations: Approved: Y_____ No: ______<br />
Approved With Changes:______<br />
1.<br />
2.<br />
3.<br />
Step in Process: Quality Assurance Committee<br />
Recommendations: Approved: Y_____ No: ______<br />
Approved With Changes:______<br />
1.<br />
2.<br />
3.<br />
Step in Process: HTBMTN Workgroup<br />
Recommendations: Financial Eligibility:<br />
1.<br />
2.<br />
3.<br />
Date:<br />
If approved with changes list<br />
changes below:<br />
Date:<br />
If approved with changes list<br />
changes below:<br />
Date:<br />
If approved with changes list<br />
changes below:<br />
Date:<br />
Page 3 of 72
FY 2011 Oral Health: Rural (North) – Part A<br />
DRAFT (as of 03-23-10)<br />
<strong>HRSA</strong> <strong>Service</strong> <strong>Category</strong> Oral Health<br />
<strong>Title</strong>: (RWGA only)<br />
Local <strong>Service</strong> <strong>Category</strong> Oral Health – Rural (North)<br />
<strong>Title</strong>:<br />
Budget Type:<br />
Unit Cost<br />
(RWGA only)<br />
Budget Requirements or Not Applicable<br />
Restrictions:<br />
(RWGA only)<br />
<strong>HRSA</strong> <strong>Service</strong> <strong>Category</strong> Oral health care includes diagnostic, preventive, and therapeutic<br />
Definition:<br />
services provided by general dental practitioners, dental specialists,<br />
(RWGA only)<br />
dental hygienists and auxiliaries, and other trained primary care<br />
providers.<br />
Local <strong>Service</strong> <strong>Category</strong> Restorative dental services, oral surgery, root canal therapy, fixed<br />
Definition:<br />
and removable prosthodontics; periodontal services includes<br />
subgingival scaling, gingival curettage, osseous surgery,<br />
gingivectomy, provisional splinting, laser procedures and<br />
maintenance. Oral medication (including pain control) for HIV<br />
patients 15 years old or older must be based on a comprehensive<br />
individual treatment plan. Prosthodontics services to HIV-infected<br />
individuals including, but not limited to examinations and diagnosis<br />
of need for dentures, diagnostic measurements, laboratory services,<br />
tooth extractions, relines and denture repairs.<br />
Target Population (age, HIV/AIDS infected individuals residing in Houston Eligible<br />
gender, geographic, race, Metropolitan Area (EMA) or Health <strong>Service</strong> Delivery Area (HSDA)<br />
ethnicity, etc.):<br />
counties other than <strong>Harris</strong> County. Comprehensive Oral Health<br />
services targeted to individuals residing in the northern counties of<br />
the EMA/HSDA, including Waller, Walker, Montgomery, Austin,<br />
Chambers and Liberty Counties.<br />
<strong>Service</strong>s to be Provided: <strong>Service</strong>s must include, but are not limited to: individual<br />
comprehensive treatment plan; diagnosis and treatment of HIVrelated<br />
oral pathology, including oral Kaposi’s Sarcoma, CMV<br />
ulceration, hairy leukoplakia, xerostomia, lichen planus, aphthous<br />
ulcers and herpetic lesions; diffuse infiltrative lymphocytosis;<br />
standard preventive procedures, including oral hygiene instruction,<br />
diet counseling and home care program; oral prophylaxis;<br />
restorative care; oral surgery including dental implants; root canal<br />
therapy; fixed and removable prosthodontics including crowns,<br />
bridges and implants;<br />
periodontal services, including subgingival<br />
scaling, gingival curettage, osseous surgery, gingivectomy,<br />
provisional splinting, laser procedures and maintenance. Proposer<br />
must have mechanism in place to provide oral pain medication as<br />
prescribed for clients by the dentist.<br />
<strong>Service</strong> Unit Definition(s): General Dentistry: A unit of service is defined as one (1) dental<br />
(RWGA/TRG only) visit which includes restorative dental services, oral surgery, root<br />
canal therapy, fixed and removable prosthodontics; periodontal<br />
Page 4 of 72
Financial Eligibility:<br />
Client Eligibility:<br />
Agency Requirements:<br />
Staff Requirements:<br />
Special Requirements:<br />
(RWGA only)<br />
FY 2011 Oral Health: Rural (North) – Part A<br />
DRAFT (as of 03-23-10)<br />
services includes subgingival scaling, gingival curettage, osseous<br />
surgery, gingivectomy, provisional splinting, laser procedures and<br />
maintenance. Oral medication (including pain control) for HIV<br />
patients 15 years old or older must be based on a comprehensive<br />
individual treatment plan.<br />
Prosthodontics: A unit of services is defined as one (1)<br />
Prosthodontics visit.<br />
Refer to the RWPC’s approved Financial Eligibility for Houston<br />
EMA/HSDA <strong>Service</strong>s.<br />
HIV-infected adults residing in the rural area of Houston<br />
EMA/HSDA meeting financial eligibility criteria.<br />
Agency must document that the primary patient care dentist has 2<br />
years prior experience treating HIV disease and/or on-going HIV<br />
educational programs that are documented in personnel files and<br />
updated regularly.<br />
<strong>Service</strong> delivery site must be located in one of the northern counties<br />
of the EMA/HSDA area: Waller, Walker, Montgomery, Austin,<br />
Chambers or Liberty Counties<br />
State of Texas dental license; licensed dental hygienist and state<br />
radiology certification for dental assistants.<br />
Must comply with the joint Part A/B standards of care where<br />
applicable.<br />
Page 5 of 72
FY 2011 Oral Health: Rural (North) – Part A<br />
DRAFT (as of 03-23-10)<br />
FY 2011 RWPC “How to Best Meet the Need” Decision Process<br />
Step in Process: Council<br />
Recommendations: Approved: Y_____ No: ______<br />
Approved With Changes:______<br />
1.<br />
2.<br />
3.<br />
Step in Process: Steering Committee<br />
Recommendations: Approved: Y_____ No: ______<br />
Approved With Changes:______<br />
1.<br />
2.<br />
3.<br />
Step in Process: Quality Assurance Committee<br />
Recommendations: Approved: Y_____ No: ______<br />
Approved With Changes:______<br />
1.<br />
2.<br />
3.<br />
Step in Process: HTBMTN Workgroup<br />
Recommendations: Financial Eligibility:<br />
1.<br />
2.<br />
3.<br />
Date:<br />
If approved with changes list<br />
changes below:<br />
Date:<br />
If approved with changes list<br />
changes below:<br />
Date:<br />
If approved with changes list<br />
changes below:<br />
Date:<br />
Page 6 of 72
<strong>Service</strong> <strong>Category</strong> Definition - Ryan White Part B Grant<br />
April 1, 2010 - March 31, 2011<br />
Local <strong>Service</strong> <strong>Category</strong> Oral Health Care – Specialty Prosthodontics (13)<br />
Amount Available<br />
Unit Cost:<br />
To be determined<br />
Budget Requirements or Maximum of 10% of budget for Administrative Costs<br />
Restrictions:<br />
Local <strong>Service</strong> <strong>Category</strong><br />
Definition:<br />
Target Population (age,<br />
gender, geographic, race,<br />
ethnicity, etc.):<br />
Prosthodontics services to HIV infected individuals including but<br />
not limited to examinations and diagnosis of need for dentures,<br />
crowns, bridgework and implants, diagnostic measurements,<br />
laboratory services, tooth extraction, relines and denture repairs.<br />
General dentistry may be provided only if additional unallocated<br />
funds are added to the category during the year.<br />
HIV/AIDS infected individuals residing within the Houston HIV<br />
<strong>Service</strong> Delivery Area (HSDA).<br />
<strong>Service</strong>s to be Provided: <strong>Service</strong>s must include, but are not limited to: fixed and removable<br />
prosthodontics including crowns, bridges and implants.<br />
<strong>Service</strong> Unit Definition(s): A unit of service is defined as one (1) prosthodontics visit.<br />
Financial Eligibility: Income at or below 300% Federal Poverty Guidelines.<br />
Client Eligibility: HIV positive; Adult resident of Houston HSDA<br />
Agency Requirements: Agency must document that the primary patient care dentist has 2<br />
years prior experience treating HIV disease and/or on-going HIV<br />
educational programs that are documented in personnel files and<br />
updated regularly. Dental facility and appropriate dental staff must<br />
maintain Texas licensure/certification and follow all applicable<br />
OSHA requirements for patient management and laboratory<br />
protocol.<br />
Providers and system must be Medicaid/Medicare certified to ensure<br />
that Ryan White funds are the payer of last resort.<br />
Staff Requirements: State dental license.<br />
Special Requirements: Must comply with the Joint Part A/B Standards of care where<br />
applicable.<br />
J:\Committees\Quality Assurance\FY 11 <strong>Service</strong> Definitions - Part B & SS\2011 Svc Cat Defs - Pt B 04-09-2010.doc<br />
Page 7 of 72
������������������������������������������������������<br />
FY 2011 RWPC “How to Best Meet the Need” Decision Process<br />
Step in Process: Council<br />
Recommendations: Approved: Y_____ No: ______<br />
Approved With Changes:______<br />
1.<br />
2.<br />
3.<br />
Step in Process: Steering Committee<br />
Recommendations: Approved: Y_____ No: ______<br />
Approved With Changes:______<br />
1.<br />
2.<br />
3.<br />
Step in Process: Quality Assurance Committee<br />
Recommendations: Approved: Y_____ No: ______<br />
Approved With Changes:______<br />
1.<br />
2.<br />
3.<br />
Step in Process: HTBMTN Workgroup<br />
Recommendations: Financial Eligibility:<br />
1.<br />
2.<br />
3.<br />
Date:<br />
If approved with changes list<br />
changes below:<br />
Date:<br />
If approved with changes list<br />
changes below:<br />
Date:<br />
If approved with changes list<br />
changes below:<br />
Date:<br />
Page 8 of 72
2010-2011 HOUSTON ELIGIBLE METROPOLITAN AREA: RYAN WHITE CARE<br />
ACT PART A/B<br />
STANDARDS OF CARE FOR HIV SERVICES<br />
RYAN WHITE GRANT ADMINISTRATION SECTION<br />
HARRIS COUNTY PUBLIC HEALTH AND ENVIRONMENTAL SERVICES (HCPHES)<br />
TABLE OF CONTENTS<br />
Introduction………………………………………………………………………………………..10<br />
General Standards…………………………………………………………………………….........11<br />
<strong>Service</strong> Specific Standards…………………………………………………………………......... 21<br />
Page 9 of 72
INTRODUCTION<br />
According to the Joint Commission on Accreditation of Healthcare Organization (JCAHO) 2008) 1<br />
, a<br />
standard is a “statement that defines performance expectations structures, or processes that must be in<br />
place for an organization to provide safe, high-quality care, treatment, and services”. Standards are<br />
developed by subject experts and are usually the minimal acceptable level of quality in service delivery.<br />
The Houston EMA Ryan White Grant Administration (RWGA) Standards of Care (SOCs) are based on<br />
multiple sources including RWGA on-site program monitoring results, consumer input, the US Public<br />
Health <strong>Service</strong>s guidelines, Centers for Medicare and Medicaid Conditions of Participation (COP) for<br />
health care facilities, JCAHO accreditation standards, the Texas Administrative Code, Center for<br />
Substance Abuse and Treatment (CSAT) guidelines and other federal, state and local regulations.<br />
Purpose<br />
The purpose of the Ryan White Part A/B SOCs is to determine the minimal acceptable levels of quality in<br />
service delivery and to provide a measurement of the effectiveness of services.<br />
Scope<br />
The Houston EMA SOCs apply to Part A, Part B and State <strong>Service</strong>s, funded <strong>HRSA</strong> defined core and<br />
support services including the following services in FY 2009/10:<br />
• Primary Medical Care<br />
• Vision Care<br />
• Medical Case Management<br />
• Clinical Case Management<br />
• Local AIDS Pharmaceutical<br />
Assistance Program (LPAP)<br />
• Oral Health<br />
• Health insurance<br />
• Hospice Care<br />
• Mental Health <strong>Service</strong>s<br />
• Substance Abuse services<br />
• Home & Community Based <strong>Service</strong>s (Facility-Based)<br />
• Early Intervention <strong>Service</strong>s<br />
• Legal <strong>Service</strong>s<br />
• Medical Nutrition Therapy<br />
• Non-Medical Case Management (<strong>Service</strong> Linkage)<br />
• Food Bank<br />
• Transportation<br />
• Rehabilitation <strong>Service</strong>s<br />
• Linguistic <strong>Service</strong>s<br />
Standards Development<br />
The first group of standards was developed in 1999 following <strong>HRSA</strong> requirements for sub grantees to<br />
implement monitoring systems to ensure subcontractors complied with contract requirements.<br />
Subsequently, the RWGA facilitates annual work group meetings to review the standards and to make<br />
applicable changes. Workgroup participants include physicians, nurses, case managers and executive staff<br />
from subcontractor agencies as well as consumers.<br />
Organization of the SOCs<br />
The standards cover all aspect of service delivery for all funded service categories. Some standards are<br />
consistent across all service categories and therefore are classified under general standards.<br />
These include:<br />
• Staff requirements, training and supervision<br />
• Client rights and confidentiality<br />
• Agency and staff licensure<br />
• Emergency Management<br />
The RWGA funds three case management models. Unique requirements for all three case management<br />
service categories have been classified under <strong>Service</strong> Specific SOCs “Case Management (All <strong>Service</strong><br />
Categories)”. Specific service requirements have been discussed under each service category.<br />
1<br />
The Joint Commission on Accreditation of Healthcare Organization (2008). Comprehensive accreditation manual<br />
for ambulatory care; Glossary<br />
Page 10 of 72
GENERAL STANDARDS<br />
1.0 Staff Requirements<br />
1.1 Staff Screening (Pre-Employment)<br />
Staff providing services to clients shall be screened for<br />
appropriateness by provider agency as follows:<br />
• Personal/Professional references<br />
• Personal interview<br />
• Written application<br />
Criminal background checks, if required by Agency Policy,<br />
must be conducted prior to employment and thereafter for all<br />
staff and/or volunteers per Agency policy.<br />
1.2 Initial Training: Staff/Volunteers<br />
Initial training includes eight (8) hours HIV/AIDS basics<br />
(including one (1) hour HIV/mental health co-morbidity<br />
sensitivity training), safety issues (fire & emergency<br />
preparedness, hazard communication, infection control,<br />
universal precautions), confidentiality issues, role of<br />
staff/volunteers, agency-specific information (e.g. Drug Free<br />
Workplace policy). Initial training must be completed within<br />
60 days of hire.<br />
1.3<br />
Standard Measure<br />
Staff Performance Evaluation<br />
Agency will perform annual staff performance evaluation<br />
1.4 Cultural and HIV Mental Health Co-morbidity Competence<br />
Training/Staff and Volunteers<br />
All staff must receive four (4) hours of cultural competency<br />
training and one (1) hour of HIV/Mental Health co-morbidity<br />
sensitivity training annually.<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Review of personnel and/or volunteer files indicates<br />
compliance<br />
• Documentation of all training in personnel file.<br />
• Specific training requirements are specified in Agency Policy<br />
and Procedure<br />
• Materials for staff training and continuing education are on<br />
file<br />
• Staff interviews indicate compliance<br />
• Completed annual performance evaluation kept in employee’s<br />
file<br />
• Documentation of training is maintained by the agency in the<br />
personnel file<br />
2.0 <strong>Service</strong>s utilize effective management practices such as cost effectiveness, human resources and quality improvement.<br />
2.1 <strong>Service</strong> Evaluation<br />
Agency has a process in place for the evaluation of client<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
Page 11 of 72
services. • Staff interviews indicate compliance.<br />
2.2 Subcontractor Monitoring<br />
Agency that utilizes a subcontractor in delivery of service,<br />
must have established policies and procedures on<br />
subcontractor monitoring that include:<br />
• Fiscal monitoring<br />
• Program<br />
• Quality of care<br />
• Compliance with guidelines and standards<br />
2.3 Staff Guidelines<br />
Agency develops written guidelines for staff, which include,<br />
at a minimum, agency-specific policies and procedures (staff<br />
selection, resignation and termination process, job<br />
descriptions); client confidentiality; health and safety<br />
requirements; complaint and grievance procedures;<br />
emergency procedures; and statement of client rights.<br />
2.4 Work Conditions<br />
Staff/volunteers have the necessary tools, supplies,<br />
equipment and space to accomplish their work.<br />
2.5<br />
Staff Supervision<br />
Staff services are supervised by a paid coordinator or<br />
manager.<br />
2.6 Professional Behavior<br />
Staffs comply with written standards of professional<br />
behavior.<br />
2.7 Communication<br />
There are procedures in place regarding regular<br />
communication with staff about the program and general<br />
agency issues.<br />
• Documentation of subcontractor monitoring<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Personnel file contains a signed statement acknowledging<br />
that staff guidelines were reviewed and that the employee<br />
understands agency policies and procedures<br />
• Inspection of tools and/or equipment indicates that these are<br />
in good working order and in sufficient supply<br />
• Staff interviews indicate compliance<br />
• Review of personnel files indicates compliance<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Staff guidelines include standards of professional behavior<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Review of personnel files indicates compliance<br />
• Review of agency’s complaint and grievance files<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Documentation of regular staff meetings<br />
• Staff interviews indicate compliance<br />
Page 12 of 72
2.8<br />
2.9<br />
Accountability<br />
There is a system in place to document staff work time.<br />
Staff Availability<br />
Staffs are present to answer incoming calls during agency’s<br />
normal operating hours.<br />
3.0 Clients Rights and Responsibilities<br />
3.1 Clients Rights<br />
Agency will provide client with written copy of client rights<br />
and responsibilities, including:<br />
• Informed consent<br />
• Confidentiality<br />
• Grievance procedures<br />
• Duty to warn or report certain behaviors<br />
• Scope of service<br />
• Criteria for end of services<br />
3.2 Confidentiality<br />
Agency has Policy and Procedure regarding client<br />
confidentiality in accordance with RWGA /TRG site visit<br />
guidelines, local, state and federal laws. Providers must<br />
implement mechanisms to ensure protection of clients’<br />
confidentiality in all processes throughout the agency.<br />
There is a written policy statement regarding client<br />
confidentiality form signed by each employee and included in<br />
the personnel file.<br />
3.3<br />
Consents<br />
All consent forms comply with state and federal laws, are<br />
signed by an individual legally able to give consent and must<br />
include the Consent for <strong>Service</strong>s form and a consent for<br />
release/exchange of information for every individual/agency to<br />
whom client identifying information is disclosed, regardless of<br />
whether or not HIV status is revealed.<br />
• Staff time sheets or other documentation indicate compliance<br />
• Published documentation of agency operating hours<br />
• Staff time sheets or other documentation indicate compliance<br />
• Documentation in client’s record<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Clients interview indicates compliance<br />
• Agency’s structural layout and information management<br />
indicates compliance<br />
• Signed confidentiality statement in each employee’s personnel<br />
file<br />
• Agency Policy and Procedure and signed and dated consent<br />
forms in client record<br />
Page 13 of 72
3.4<br />
3.5<br />
Up to date Release of Information<br />
Agency obtains an informed written consent of the client or<br />
legally responsible person prior to the disclosure or exchange<br />
of certain information about client’s case to another party<br />
(including family members) in accordance with the RWGA<br />
<strong>Site</strong> Visit Guidelines, local, state and federal laws. The<br />
release/exchange consent form must contain:<br />
• Name of the person or entity permitted to make the<br />
disclosure<br />
• Name of the client<br />
• The purpose of the disclosure<br />
• The types of information to be disclosed<br />
• Entities to disclose to<br />
• Date on which the consent is signed<br />
• The expiration date of client authorization (no longer<br />
than two years or six (6) months to one (1) year from<br />
last date of service)<br />
• Signature of the client/or parent, guardian or person<br />
authorized to sign in lieu of the client.<br />
• Description of the Release of Information, its<br />
components, and ways the client can nullify it<br />
Released/exchange of information forms must be completed<br />
entirely in the presence of the client. Any unused lines must<br />
have a line crossed through the space.<br />
Grievance Procedure<br />
Agency has Policy and Procedure regarding client grievances<br />
that is reviewed with each client in a language and format the<br />
client can understand and a written copy of which is provided<br />
to each client.<br />
Grievance procedure includes but is not limited to:<br />
• to whom complaints can be made<br />
• steps necessary to complain<br />
• form of grievance, if any<br />
• time lines and steps taken by the agency to resolve the<br />
grievance<br />
• Current Release of Information form with all the required<br />
elements signed by client or authorized person in client’s record<br />
• Signed receipt of agency Grievance Procedure, filed in client<br />
chart<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
Page 14 of 72
3.6<br />
• documentation by the agency of the process<br />
• confidentiality of grievance<br />
• addresses and phone numbers of licensing authorities<br />
and funding sources<br />
Client Rights and Responsibilities Statement<br />
Agency has a Client Rights and Responsibilities Statement that<br />
is reviewed with each client in a language and format the client<br />
can understand and a written copy of which is provided to each<br />
client.<br />
3.7 Client Feedback<br />
Feedback from clients (or from client caregivers, in cases<br />
where clients are unable to give feedback) is obtained about<br />
quality of services annually.<br />
3.8 Patient Safety (Core <strong>Service</strong>s Only)<br />
Agency shall establish mechanisms to implement the<br />
National Patient Safety Goals (NPSG) modeled after the<br />
current Joint Commission accrediatation for Ambulatory<br />
Care (www.jointcommission.org) to ensure patients’ safety.<br />
The NPSG to be addressed include the following:<br />
• “Improve the accuracy of patient identification<br />
• Improve the safety of using medications<br />
• Reduce the risk of Health care-associated infections<br />
• Accurately and completely reconcile medications<br />
across the continuum of care<br />
• Universal Protocol” for preventing Wrong <strong>Site</strong>, Wrong<br />
Procedure and Wrong Person Surgery”<br />
(www.jointcommission.org)<br />
4.0 Accessibility<br />
4.1 Cultural Competence<br />
Agency demonstrates a commitment to provision of services<br />
• Agency Policy and Procedure and signed receipt of Clients<br />
Rights and Responsibilities Statement in client record<br />
• Client feedback mechanism is in place<br />
• Documentation of clients’ evaluation of services is<br />
maintained<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Agency has procedures for obtaining translation services<br />
• Client satisfaction survey indicates compliance<br />
Page 15 of 72
that are culturally sensitive and language competent for Limited<br />
English Proficient (LEP) individuals.<br />
4.2 Client Education<br />
Agency demonstrates capacity for client education and<br />
provision of Information on community resources<br />
4.3 Special <strong>Service</strong> Needs<br />
Agency demonstrates a commitment to assisting individuals<br />
with special needs<br />
4.4 Program Information<br />
Broad-based dissemination of information regarding the<br />
availability of services<br />
4.5<br />
4.6<br />
Proof of HIV Diagnosis<br />
Documentation of the client's HIV status is obtained at or prior<br />
to the initiation of services or registration services.<br />
An anonymous test result may be used to document HIV status<br />
temporarily (up to sixty [60] days). It must contain enough<br />
information to ensure the identity of the subject with a<br />
reasonable amount of certainty.<br />
Client Eligibility<br />
In order to be eligible for services, individuals must meet the<br />
following:<br />
• HIV+<br />
• Residence in the Houston EMA/ HSDA (With prior<br />
approval, clients can be served if they reside outside<br />
of the Houston EMA/HSDA.)<br />
• Income no greater than 300% of the Federal Poverty<br />
level (unless otherwise indicated)<br />
• Policies and procedures demonstrate commitment to the<br />
community and culture of the clients<br />
• Availability of interpretive services, bilingual staff, and staff<br />
trained in cultural competence<br />
• Agency has vital documents including, but not limited to<br />
applications, consents, complaint forms, and notices of rights<br />
translated in client record<br />
• Availability of the blue book and other educational materials<br />
• Documentation of educational needs assessment and client<br />
education in clients’ records<br />
• Agency compliance with the Americans with Disabilities Act<br />
(ADA).<br />
• Review of Policies and Procedures indicates compliance<br />
• Environmental Review<br />
• Format Agency has a written substantiated annual plan to<br />
targeted populations<br />
• Zip code data show provider is reaching clients throughout<br />
service area<br />
• Documentation in client record as per RWGA site visit<br />
guidelines or TRG Policy SG-03<br />
• Documentation of HIV+ status, residence, identification and<br />
income in the client record<br />
• Documentation of ineligibility for third party reimbursement<br />
• Documentation of screening for Third Party Payers in<br />
accordance with TRG Policy SG-06 Documentation of Third<br />
Party Payer Eligibility or RWGA site visit guidelines<br />
Page 16 of 72
• Proof of identification<br />
• Ineligibility for third party reimbursement<br />
4.7 Re-evaluation of Client Eligibility<br />
Agency conducts annual re-evaluation of eligibility for all<br />
clients. At a minimum, agency confirms renewed eligibility<br />
with the CPCDMS and re-screens, as appropriate, for third-<br />
party payers.<br />
4.8 Linkage Into Core <strong>Service</strong>s<br />
Agency staff will provide out-of-care clients with<br />
individualized information and referral to connect them into<br />
ambulatory outpatient medical care and other core medical<br />
services.<br />
4.9 Wait Lists<br />
It is the expectation that clients will not be put on a Wait List<br />
nor will services be postponed or denied due to funding.<br />
Agency must notify the Administrative agency when funds<br />
for service are either low or exhausted for appropriate<br />
measures to be taken to ensure adequate funding is available.<br />
Should a wait list become required, the agency must, at a<br />
minimum, develop a policy that addresses how they will<br />
handle situations where service(s) cannot be immediately<br />
provided and a process by which client information will be<br />
obtained and maintained to ensure that all clients that<br />
requested service(s) are contacted after service provision<br />
resumes;<br />
The A gency w ill n otify The R esource G roup ( TRG) or<br />
RWGA of the following information when a wait list must be<br />
created:<br />
An explanation for the cessation of service; and<br />
A plan for resumption of service. The Sub grantee’s plan<br />
must address:<br />
• Action steps to be taken by Subgrantee to resolve the<br />
service shortfall; and<br />
• Projected date that services will resume.<br />
• Client file contains documentation of re-evaluation of client<br />
residence, income and rescreening for third party payers at<br />
least annually<br />
• Documentation of client referral is present in client file<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Documentation of compliance with TRG’s Policy SG-19 Client<br />
Wait Lists<br />
• Documentation that agency notified their Administrative<br />
Agency when funds for services were either low or exhausted<br />
Page 17 of 72
The A gency w ill r eport to T RG or R WGA in w riting on a<br />
monthly b asis) w hile a c lient w ait l ist i s r equired w ith t he<br />
following information:<br />
• Number of clients on the wait list<br />
• Progress toward completing the plan for resumption of<br />
service<br />
• A revised plan for resumption of service, if necessary<br />
4.10 Intake<br />
The agency conducts an intake to collect required data<br />
including, but not limited, eligibility, appropriate consents and<br />
client identifiers for entry into CPCDMS. Intake process is<br />
flexible and responsive, accommodating disabilities and health<br />
conditions.<br />
When necessary, client is provided alternatives to office visits,<br />
such as conducting business by mail or providing home visits.<br />
Agency has established procedures for communicating with<br />
people with hearing impairments<br />
5.0 Quality Management<br />
5.1 Continuous Quality Improvement (CQI)<br />
Agency demonstrates capacity for an organized CQI program<br />
and has a CQI Committee in place to review procedures and to<br />
initiate Performance Improvement activities.<br />
The Agency shall maintain an up-to-date Quality Management<br />
(QM) Manual. The QM Manual will contain at a minimum:<br />
• The Agency’s QM Plan<br />
• Meeting agendas and/or notes (if applicable)<br />
• Project specific CQI Plans<br />
• Root Cause Analysis & Improvement Plans<br />
• Data collection methods and analysis<br />
• Work products<br />
• Documentation in client record<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Up to date QM Manual<br />
Page 18 of 72
• QM program evaluation<br />
• Materials necessary for QM activities<br />
5.2 Data Collection and Analysis<br />
Agency demonstrates capacity to collect and analyze client<br />
level data including client satisfaction surveys and findings are<br />
incorporated into service delivery. Supervisors shall conduct<br />
and document ongoing record reviews as part of quality<br />
improvement activity.<br />
6.0 Point Of Entry Agreements<br />
6.1 Points of Entry (Core <strong>Service</strong>s Only)<br />
Agency accepts referrals from sources considered to be<br />
points of entry into the continuum of care, in accordance with<br />
HIV <strong>Service</strong>s policy approved by <strong>HRSA</strong> for the Houston<br />
EMA.<br />
7.0 Emergency Management<br />
7.1 Emergency Preparedness<br />
Agency leadership including medical staff must develop an<br />
Emergency Preparedness Plan modeled after the Joint<br />
Commission’s regulations and/or Centers for Medicare and<br />
Medicaid guidelines for Emergency Management. The plan<br />
should, at a minimum utilize “all hazard approach” to ensure<br />
a level of preparedness sufficient to support a range of<br />
emergencies. Agencies shall conduct an annual Hazard<br />
Vulnerability Analysis (HVA) to identify potential hazards,<br />
threats, and adverse events and assess their impact on care,<br />
treatment, and services they must sustain during an<br />
emergency. The agency shall communicate hazards<br />
identified with its community emergency response agencies<br />
and together shall identify the capability of its community in<br />
meeting their needs. The HVA shall be reviewed annually.<br />
7.2<br />
Emergency Preparedness Plan<br />
The emergency preparedness plan shall address the six<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Up to date QM Manual<br />
• Supervisors log on record reviews signed and dated<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Documentation of formal agreements with appropriate Points<br />
of Entry<br />
• Documentation of referrals and their follow-up<br />
• Emergency Preparedness Plan<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Emergency Preparedness Plan<br />
Page 19 of 72
critical areas for emergency management including<br />
• Communication pathways<br />
• Essential resources and assets<br />
• patients’ safety and security<br />
• staff responsibilities<br />
• Supply of key utilities such as portable water and<br />
electricity<br />
• Patient clinical and support activities during<br />
emergency situations. (www.jointcommission.org)<br />
7.3 Emergency Management Drills<br />
Agency shall implement emergency management drills twice<br />
a year either in response to actual emergency or in a planned<br />
exercise. Completed exercise should be evaluated by a<br />
multidisciplinary team including administration, clinical and<br />
support staff. The emergency plan should be modified based<br />
on the evaluation results and retested.<br />
8.0 Building Safety<br />
8.1 Required Permits<br />
All agencies will maintain Occupancy and Fire Marshal’s<br />
permits for the facilities.<br />
• Emergency Management Plan<br />
• Review of Agency’s Policies and Procedures Manual indicates<br />
compliance<br />
• Current required permits on file<br />
Page 20 of 72
Oral Health Care<br />
Oral Health care constitute an essential component of primary health care for PLWHA as poor oral health affects adherence to ARV therapy and<br />
subsequent health outcomes 4<br />
. Thus, there is the need for coordination of services between medical providers and oral health care providers.<br />
The Oral health care standards are based on <strong>HRSA</strong> definition for oral health care, the <strong>New</strong> York State Health Department AIDS Institute<br />
guidelines for HIV and Oral Health and other state and local requirements. The RW HIV/AIDS Treatment Modernization Act of 2006 defines<br />
Oral Health Care as “diagnostic, preventive, and therapeutic services provided by the general dental practitioners, dental specialist, dental<br />
hygienist and auxiliaries and other trained primary care providers”. The Ryan White Part A/B oral health care services include standard<br />
preventive procedures, diagnosis and treatment of HIV-related oral pathology, restorative dental services, oral surgery, root canal therapy, fixed<br />
and removable prosthodontics and oral medication (including pain control) for HIV patients 15 years old or older based on a comprehensive<br />
individual treatment plan.<br />
1.0 Staff Requirements<br />
1.1 Continuing Education<br />
Eight (8) hours of training in HIV/AIDS and clinically-related<br />
issues is required annually for licensed staff.<br />
One (1) hour of training in HIV/AIDS is required annually for all<br />
staff.<br />
1.2 Experience – HIV/AIDS<br />
A minimum of one (1) year documented HIV/AIDS work<br />
experience is preferred for licensed staff.<br />
1.3 Staff Supervision<br />
Supervision of clinical staff shall be provided by a practitioner with<br />
at least two years experience in dental health assessment and<br />
treatment of persons with HIV. All licensed personnel shall<br />
received supervision consistent with the State of Texas license<br />
requirements.<br />
• Materials for staff training and continuing<br />
education are on file<br />
• Documentation of continuing education in<br />
personnel file<br />
• Documentation of work experience in<br />
personnel file<br />
• Review of personnel files indicates<br />
compliance<br />
• Review of agency’s Policies & Procedures<br />
Manual indicates compliance<br />
4<br />
The <strong>New</strong> York State Department of Health AIDS Institute (2000-2009). Clinical guidelines: HIV and oral health. Retrieved 10/02/2009 from www.<br />
http://www.hivguidelines.org/Content.aspx?PageID=263<br />
Page 21 of 72
2.0 Coordination with Primary Care Providers<br />
2.1 HIV Primary Care Provider Contact Information<br />
Agency obtains and documents HIV primary care provider contact<br />
information for each client.<br />
2.2 Consultation for Treatment<br />
Agency consults with client’s medical care providers when<br />
indicated.<br />
2.3 Health History Information<br />
Agency collects and documents health history information for each<br />
client prior to providing care. This information should include, but<br />
not be limited to, the following:<br />
• A baseline current (within the last 6 months) CBC laboratory<br />
test results for all new clients, and an annual update<br />
thereafter<br />
• Current (within the last 6 months) Viral Load and CD4<br />
laboratory test results, when clinically indicated<br />
• Client’s chief complaint, where applicable<br />
• Medication names<br />
• Sexually transmitted diseases<br />
• HIV-associated illnesses<br />
• Allergies and drug sensitivities<br />
• Alcohol use<br />
• Recreational drug use<br />
• Tobacco use<br />
• Neurological diseases<br />
• Hepatitis<br />
• Usual oral hygiene<br />
• Date of last dental examination<br />
• Involuntary weight loss or weight gain<br />
Review of systems<br />
• Documentation of HIV primary care<br />
provider contact information in the client<br />
record. At minimum, agency should collect<br />
the clinic and/or physician’s name and<br />
telephone number<br />
• Documentation of communication in the<br />
client record<br />
• Documentation of health history<br />
information in the client record. Reasons<br />
for missing health history information are<br />
documented<br />
Page 22 of 72
2.4 Client Health History Update<br />
An update to the health history should be made, at minimum, every<br />
six (6) months or at client’s next general dentistry visit whichever<br />
is greater.<br />
2.5<br />
Comprehensive Periodontal Examination<br />
Agency has a written policy and procedure regarding when a<br />
comprehensive periodontal examination should occur.<br />
Comprehensive periodontal examination should be done in<br />
accordance with professional standards and current US Public<br />
Health <strong>Service</strong> guidelines<br />
2.6 Treatment Plan<br />
• A comprehensive, multi disciplinary Oral Health treatment<br />
plan will be developed in conjunction with the patient.<br />
• Patient’s primary reason for dental visit should be addressed<br />
in treatment plan<br />
• Patient strengths and limitations will be considered in<br />
development of treatment plan<br />
• Treatment priority should be given to pain management,<br />
infection, traumatic injury or other emergency conditions<br />
• Treatment plan will be updated as deemed necessary<br />
2.7 Annual Hard/Soft Tissue Examination<br />
The following elements are part of each client’s annual hard/soft<br />
tissue examination and are documented in the client record:<br />
• Charting of caries;<br />
• X-rays;<br />
• Periodontal screening;<br />
• Written diagnoses, where applicable;<br />
• Treatment plan.<br />
Determination of clients needing annual examination should be<br />
based on the dentist’s judgment and criteria outlined in the<br />
• Documentation of health history update in<br />
the client record<br />
• Review of agency’s Policies & Procedures<br />
Manual indicates compliance<br />
• Review of client records indicate<br />
compliance<br />
• Treatment plan dated and signed by both<br />
the provider and patient in patient file<br />
• Updated treatment plan dated and signed by<br />
both the provider and patient in patient file<br />
• Documentation in the client record<br />
• Review of agency’s Policies & Procedures<br />
Manual indicates compliance<br />
Page 23 of 72
agency’s policy and procedure, however the time interval for<br />
all clients may not exceed two (2) years.<br />
2.8 Oral Hygiene Instructions<br />
Oral hygiene instructions (OHI) should be provided annually to<br />
each client. The content of the instructions is documented.<br />
THRESHOLDS<br />
Measurement thresholds will be set at 100%.<br />
IV. IMPLEMENTATION & REPORTING<br />
• Documentation in the client record<br />
Agencies will be required to adhere to the QA guidelines provided by RWGA, or the Part B administrative agency, as applicable.<br />
Page 24 of 72
Findings from the 2008 Houston Area HIV/AIDS Needs Assessment<br />
CORE CORE CORE SERVICES<br />
SERVICES<br />
SERVICES<br />
reported frequently as a barrier. Waiting times were also ranked highly within<br />
subpopulations, except within the out-of-care and youth. Information-related barriers were<br />
ranked highly within the out-of-care, women, African-Americans, the recently released and<br />
substance abusers.<br />
V<br />
DENTIST ENTIST VVISITS<br />
ISITS<br />
<strong>Service</strong> category data were collected in the context of their local definitions, rather<br />
than their official <strong>HRSA</strong> definitions. Although the differences between the local and <strong>HRSA</strong><br />
definitions are minimal, the Data Collection Workgroup felt the local definition approach<br />
would promote a realistic assessment of the Houston HSDA Ryan White care system.<br />
Local definitions for each service category will be included in each summary. A list<br />
of the official <strong>HRSA</strong> service category definitions is provided in Appendix C.<br />
Local Definition<br />
The local definition of dentist visits is defined as:<br />
Restorative dental services, oral surgery, root canal therapy, fixed and removable<br />
prosthodontics; periodontal services includes subgingival scaling, gingival curettage,<br />
osseous surgery, gingivectomy, provisional splinting, laser procedures and maintenance.<br />
Oral medication (including pain control) for HIV patients 15 years old or older must be<br />
based on a comprehensive individual treatment plan.<br />
CPCDMS/ARIES <strong>Service</strong> Utilization Data<br />
Page 25 of 72<br />
<strong>Service</strong> utilization information for most services is based on data from the<br />
Centralized Patient Care Data Management System (CPCDMS) and/or ARIES. The<br />
CPCDMS is a real-time, de-identified client-level computer database application that allows<br />
Ryan White-funded providers, as well as non-Ryan White providers, and other users in the<br />
EMA to share client eligibility information and document service delivery while maintaining<br />
client confidentiality. <strong>Service</strong> providers enter registration, service encounter and medical<br />
update information for each client into the CPCDMS. Client information collected includes<br />
demographic, comorbidity, biological marker, mortality and service utilization data. Since its<br />
inception in June of 2000, over 10,000 clients have been registered in the CPCDMS.<br />
The AIDS Regional Information and Evaluation System (ARIES), implemented in<br />
February 2005, is also a real-time, de-identified client-level computer database application,<br />
the ARIES centralizes client data, service details, and agency and staff information to<br />
maximize the quality of care and services to clients in need. The system was developed<br />
collaboratively for Part B by the State of Texas, County of San Diego, County of San<br />
Bernardino, and State of California. Information from the Centralized Patient Care Data<br />
Management System can be imported into the ARIES system and filtered to produce a<br />
comprehensive picture of service utilization information on both Part B and Part A-funded<br />
providers, as well as other users in the EMA/HSDA<br />
2008 Houston Area HIV/AIDS Needs Assessment
It is important to note that while CPCDMS does represent the majority of PLWHA<br />
receiving Ryan White-funded services in the HSDA, it is incorrect to assume that all 764<br />
survey respondents are enrolled in CPCDMS.<br />
According to the Centralized Patient Care Data Management System (CPCDMS), a<br />
total of 2,219 unduplicated PLWHA received dentist visits through grants billed to Ryan<br />
White Part A and Part B. This total represents 12% of the reported 18,109 PLWHA residing<br />
in the Houston EMA/HSDA.<br />
Access (Easy versus Hard)<br />
At the beginning of the client survey, respondents were given a list of core services<br />
arranged in table format (see Appendix B for copy of client survey). The purpose of the<br />
core service table was to collect information on access and barriers to the listed services.<br />
For each <strong>HRSA</strong>-defined core service, respondents indicated whether they had “some<br />
difficulty” getting the service, if it was “very easy” to get the service, or if they “did not need”<br />
the service within the past year.<br />
The following table shows the level of access to dentist visits reported by all<br />
respondents. It should be noted that the percentages are based on the sum of<br />
respondents within each subpopulation that accessed the service (reported difficulty or<br />
ease). It is also important to remember that the subpopulations are not mutually exclusive<br />
– in other words, the numbers across the subpopulations do not represent unduplicated<br />
respondents. For example, an African-American female reporting a mental health symptom<br />
is included in the Women, African-Americans and Mental Health subpopulations.<br />
Care should also be taken when making comparisons between subpopulations of<br />
very small size. The smaller the subpopulation, the more sensitive percentages become to<br />
changes in the numbers. For example, for very small subpopulations, shifting just one<br />
response can change percentages by as much as 5 points. It is important not to rely solely<br />
on such percentages when planning for services – considering both the proportions and<br />
raw numbers will help ensure a more comprehensive understanding of the results.<br />
Lastly, it should be emphasized that reports of access to a service does not<br />
necessarily mean the respondent received the service. In the client survey, respondents<br />
were asked to report whether they had difficulty getting a service, but the survey did not ask<br />
as a follow-up whether the respondent ultimately received the service despite the<br />
difficulties. So, care should be taken not to equate reports of “very easy” or reports of<br />
“some difficulty” as proxies of service utilization.<br />
2008 Houston Area HIV/AIDS Needs Assessment<br />
DENTIST DENTIST DENTIST VISITS VISITS VISITS<br />
Page 26 of 72
CORE CORE CORE SERVICES<br />
SERVICES<br />
SERVICES<br />
TABLE 15.1: REPORTED ACCESS TO DENTIST VISITS IN THE PAST 12 MONTHS<br />
Total who<br />
attempted<br />
to access<br />
* Subpopulations are not mutually exclusive.<br />
** Percentages may not add up to 100% due to rounding.<br />
%<br />
Very<br />
Easy<br />
The majority (82%) of all 764 survey respondents reported attempting to access<br />
dentist visits during the previous 12 months; a total of 138 (18%) said they did not need this<br />
service. Most subpopulations also reported accessing this service in relatively high<br />
proportions – Latinos access this service in the highest proportion (90%) compared to other<br />
groups. However, the subpopulations with the lowest proportions accessing dentist visits<br />
were substance abusers (79%), the recently released (77%) and the out-of-care (58%).<br />
Overall, the majority of all survey respondents had an easy time accessing dentist<br />
visits – 61% said it was “very easy” to get the service. Among the subpopulations, access<br />
to dentist visits appeared easiest for Latinos (70%), MSM of color (69%) and those in-care<br />
(64%).<br />
By far, the out-of-care subpopulation had the highest proportion (78%) of those who<br />
had some difficulty accessing dentist visits during the past year. Other subpopulations with<br />
relatively higher proportions of difficulty were youth (65%), women (45%) and the recently<br />
released (43%).<br />
Barriers<br />
Survey respondents that reported “some difficulty” getting a service were asked to<br />
describe the barriers they experienced. Respondents could choose from a list of common<br />
barriers, or write their own. The number of possible reported barriers was unlimited, so<br />
respondents were encouraged to list every barrier they encountered when getting a<br />
service. It should also be noted that the number of reported barriers does not indicate<br />
%<br />
Some<br />
Difficulty<br />
%<br />
No<br />
Need<br />
All Respondents (N=764) 626 82% 380 61% 246 39% 138 18%<br />
Subpopulations*<br />
In Care 581 85% 370 64% 211 36% 106 15%<br />
Out-of-Care 45 58% 10 22% 35 78% 32 42%<br />
Women 197 83% 108 55% 89 45% 41 17%<br />
Youth 31 84% 11 35% 20 65% 6 16%<br />
African-Americans 349 81% 214 61% 135 39% 80 19%<br />
Latinos 127 90% 89 70% 38 30% 14 10%<br />
White MSM 83 81% 47 57% 36 43% 20 19%<br />
MSM of Color 179 86% 124 69% 55 31% 29 14%<br />
Recently Released 92 77% 51 55% 41 45% 27 23%<br />
Substance Abuse 196 79% 113 58% 83 42% 52 21%<br />
Mental Health 369 82% 209 57% 160 43% 83 18%<br />
Homeless 64 72% 42 47% 22 25% 25 28%<br />
Page 27 of 72<br />
2008 Houston Area HIV/AIDS Needs Assessment<br />
%
whether the respondent did, or did not, ultimately receive the service – survey respondents<br />
described the barriers they experienced in the process of getting a service.<br />
The following table shows the number of barriers reported for dentist visits. The<br />
numbers in each cell represent how many times respondents faced a certain type of<br />
barrier. The total reported barriers column on the far right represents the total number of<br />
barriers reported for each subpopulation. The cells that are shaded and in bold represent<br />
barriers with the highest number of reports for each subpopulation.<br />
TABLE 15.2: NUMBER OF REPORTED BARRIERS FOR DENTIST VISITS<br />
A B C D E F G H I J K M O Q R S<br />
Total**<br />
Barriers<br />
All Respondents<br />
Subpopulations*<br />
33 58 74 26 15 17 27 87 43 6 10 5 24 1 4 1 431<br />
In Care 26 44 63 16 11 8 25 75 33 4 4 3 18 1 3 1 335<br />
Out-of-Care 7 14 11 10 4 9 2 12 10 2 6 2 6 0 1 0 96<br />
Women 12 21 27 15 7 10 9 29 21 6 6 0 12 1 1 0 177<br />
Youth 6 10 5 3 5 1 3 6 4 2 2 0 3 0 1 0 51<br />
African-Americans 19 36 34 19 8 13 11 49 18 5 8 4 14 0 3 1 242<br />
Latinos 7 8 12 4 3 2 5 15 6 0 1 0 5 0 0 0 68<br />
White MSM 5 5 17 1 2 0 8 14 7 0 0 1 1 0 0 0 61<br />
MSM of Color 7 15 14 3 4 3 5 22 4 0 0 3 7 0 1 0 88<br />
Recently Released 5 10 14 11 2 4 3 13 6 0 3 4 2 0 1 0 78<br />
Substance Abuse 11 19 24 9 1 4 4 33 15 2 5 2 7 0 1 0 137<br />
Mental Health 21 38 55 20 10 13 17 55 32 5 8 2 15 1 4 1 297<br />
Homeless 8 15 13 12 8 7 6 14 3 3 7 0 0 0 1 1 102<br />
* Subpopulations are not mutually exclusive.<br />
** Some barriers may not be shown if no respondents reported them as barriers for this service<br />
Barriers<br />
A The services are not in my area L People at the agency don't speak my language<br />
B I don't know where to get the services M My jail/prison history makes it hard to get services<br />
C I would have to wait too long to get the services N Difficulties with paperwork (volume, confusing process, etc)<br />
D The services cost too much O Substance abuse<br />
E I was told I am not eligible to get the services P Was incarcerated/in jail<br />
F I don't think I'm eligible to get the services Q Personal health issues (too sick, medication resistant, etc)<br />
G The people who run the services are not friendly R Fear, denial or stigma (internal and/or external)<br />
H It's hard to make or keep appointments S Homeless/unstable housing<br />
I It's hard for me to get there T CM left/staff turnover<br />
J There is no one to watch my kids if I go there U Not enough, resources/funds run out too quickly<br />
K I'm afraid someone will find out about my HIV V Immigration status<br />
Overall, there were 431 reports of barriers among respondents who had difficulty<br />
accessing dentist visits during the past year. The barriers reported most often for dentist<br />
visits were related to scheduling appointments, getting to locations of services and waiting<br />
2008 Houston Area HIV/AIDS Needs Assessment<br />
DENTIST DENTIST DENTIST VISITS VISITS VISITS<br />
Page 28 of 72
CORE CORE CORE SERVICES<br />
SERVICES<br />
SERVICES<br />
times. The table below shows 2-3 highlighted barriers reported by subpopulations when<br />
accessing dentist visits. The intent of this table is to highlight the barriers identified most<br />
often by respondents – for the full list of barriers, refer to the table titled, “Number of<br />
reported barriers for Dentist Visits.”<br />
TABLE 15.3: HIGHLIGHTED BARRIERS FOR DENTIST VISITS BY SUBPOPULATION<br />
All Respondents<br />
Subpopulations*<br />
In Care<br />
Out-of-Care<br />
Women<br />
Youth<br />
African-Americans<br />
Latinos<br />
White MSM<br />
MSM of Color<br />
Recently Released<br />
Substance Abuse<br />
Mental Health<br />
Homeless<br />
* Subpopulations are not mutually exclusive.<br />
Barriers (ranked by number of reports)<br />
H – It's hard to make or keep appointments (n=87)<br />
C – I would have to wait too long to get the services (n=74)<br />
H – It's hard to make or keep appointments (n=75)<br />
C – I would have to wait too long to get the services (n=63)<br />
B – I don't know where to get the services (n=14)<br />
H – It's hard to make or keep appointments (n=12)<br />
H – It's hard to make or keep appointments (n=29)<br />
C – I would have to wait too long to get the services (n=27)<br />
B – I don't know where to get the services (n=10)<br />
A – The services are not in my area (n=6)<br />
H – It's hard to make or keep appointments (n=6)<br />
H – It's hard to make or keep appointments (n=49)<br />
B – I don't know where to get the services (n=36)<br />
C – I would have to wait too long to get the services (n=34)<br />
H – It's hard to make or keep appointments (n=15)<br />
C – I would have to wait too long to get the services (n=12)<br />
C – I would have to wait too long to get the services (n=17)<br />
H – It's hard to make or keep appointments (n=14)<br />
H – It's hard to make or keep appointments (n=22)<br />
B – I don't know where to get the services (n=15)<br />
C – I would have to wait too long to get the services (n=14)<br />
C – I would have to wait too long to get the services (n=14)<br />
H – It's hard to make or keep appointments (n=13)<br />
H – It's hard to make or keep appointments (n=33)<br />
C – I would have to wait too long to get the services (n=24)<br />
C – I would have to wait too long to get the services (n=55)<br />
H – It's hard to make or keep appointments (n=55)<br />
B – I don't know where to get the services (n=15)<br />
H – It's hard to make or keep appointments (n=14)<br />
C – I would have to wait too long to get the services (n=13)<br />
D – The services cost too much (n=12)<br />
Page 29 of 72<br />
Within all subpopulations, problems making or keeping appointments ranked high<br />
compared to other barriers. Waiting times were also ranked highly within subpopulations,<br />
except within the out-of-care and youth. Information-related barriers were ranked highly<br />
within African-Americans, women, MSM of color, out-of-care and youth.<br />
2008 Houston Area HIV/AIDS Needs Assessment
Ryan White Part A Quality Management Program–Houston EMA<br />
CONTACT:<br />
Oral Health Care Chart Review<br />
FY 2009<br />
Prepared by <strong>Harris</strong> County Public Health &<br />
Environmental <strong>Service</strong>s – Ryan White Grant Administration<br />
August 2009<br />
Carin Martin, MPA<br />
Project Coordinator–Quality Management Development<br />
<strong>Harris</strong> County Public Health & Environmental <strong>Service</strong>s<br />
Ryan White Grant Administration<br />
2223 West Loop South, RM 417<br />
Houston, TX 77027<br />
713-439-6041<br />
cmartin@hcphes.org<br />
Page 30 of 72
Introduction<br />
Part A funds of the Ryan White Care Act are administered in the Houston Eligible Metropolitan Area (EMA) by the<br />
Ryan White Grant Administration Section of <strong>Harris</strong> County Public Health & Environmental <strong>Service</strong>s. During FY<br />
09, a comprehensive review of client dental records was conducted for services provided between 3/1/07 to<br />
2/28/08. This review included one provider of Adult Oral Health Care that received Part A funding in the<br />
Houston EMA.<br />
The primary purpose of this annual review process is to assess Part A oral health care provided to persons living<br />
with HIV in the Houston EMA. Ryan White Grant Administration manages the review process and analyzes the<br />
subsequent data, while the reviews are conducted by TMF Health Quality Institute (TMF), under contract with<br />
Ryan White Grant Administration. Unlike primary care, there are no federal guidelines published by the U.S Public<br />
Health <strong>Service</strong> for oral health care targeting individuals with HIV/AIDS. Therefore, Ryan White Grant<br />
Administration has adopted general guidelines from peer-reviewed literature that address oral health care for the<br />
HIV/AIDS population, as well as literature published by national dental organizations such as the American Dental<br />
Association and the Academy of General Dentistry, to measure the quality of Part A funded oral health care.<br />
Scope of This Report<br />
This report provides background on the project, supplemental information on the design of the data collection tool,<br />
and presents the pertinent findings of the FY 09 oral health care chart review. In addition to this report, the<br />
reviewed provider will also receive an electronic copy of the raw database in order to facilitate further analysis.<br />
Also, any additional data analysis of items or information not included in this report can likely be provided after a<br />
request is submitted to Ryan White Grant Administration.<br />
The Data Collection Tool<br />
The data collection tool employed in the review was developed through a period of in-depth research and a series of<br />
working meetings between Ryan White Grant Administration and the review contractor, TMF. By studying the<br />
processes of previous dental record reviews and researching the most recent HIV-related and general oral health<br />
practice guidelines, a listing of potential data collection items was developed. Further research provided for the<br />
editing of this list to yield what is believed to represent the most pertinent data elements for oral health care in the<br />
Houston EMA. Topics covered by the data collection tool include, but are not limited to the following: basic client<br />
information, completeness of the health history, hard & soft tissue examinations, oral hygiene prevention, and<br />
periodontal examinations. Contact Ryan White Grant Administration for a copy of the tool.<br />
The Chart Review Process<br />
Page 31 of 72<br />
All charts were reviewed by licensed dentist experienced in identifying documentation issues and assessing<br />
adherence to published guidelines. The reviewer has extensive experience conducting dental chart reviews. The<br />
collected data was recorded directly onto the tool and this information was entered into a preformatted database.<br />
Once all data collection and data entry was completed, the database was forwarded to Ryan White Grant<br />
Administration for analysis. The data collected during this process is intended to be used for service improvement.
The Chart Review Process (cont’d)<br />
The specific parameters established for the data collection process were developed from HIV-related and general<br />
oral health care guidelines available in peer-reviewed literature, and the professional experience of the reviewer on<br />
standard record documentation practices. Table 1 summarizes the various documentation criteria employed during<br />
the review.<br />
Table 1. Data Collection Parameters<br />
Review Area Documentation Criteria<br />
Health History Completeness of Initial Health History: includes but not limited to past medical<br />
history, medications, allergies, substance use, HIV MD/primary care status, physician<br />
contact info, etc.; Completed updates to the initial health history<br />
Hard/Soft Tissue Exam Findings—abnormal or normal, diagnoses, treatment plan, treatment plan updates<br />
Oral Hygiene Prevention Prophylaxis, OHI<br />
Periodontal screening Completeness<br />
Appointments Kept, Not kept, Practitioner<br />
The Sample Selection Process<br />
The sample population was selected from a pool of 2,269 unduplicated clients who accessed Part A oral health care<br />
between 3/1/08 and 2/28/09. The medical charts of 205 of these clients were used in the review, representing 9%<br />
of the pool of unduplicated clients.<br />
In an effort to make the sample population as representative of the actual Part A oral health care population as<br />
possible, the EMA’s Centralized Patient Care Data Management System (CPCDMS) was used to generate a list of<br />
client codes to be reviewed. The demographic make-up (race/ethnicity, gender, age, stage of illness) of clients<br />
accessing oral health services between 3/1/08 and 2/28/09 was determined by CPCDMS, which in turn allowed<br />
Ryan White Grant Administration to generate a sample of specified size that closely mirrors that same demographic<br />
make-up. Randomly-generated client codes were categorized in terms of stage of illness, as delineated by CPCDMS,<br />
in order to allow for assessment of a range of care.<br />
- Asymptomatic CD4 > = 500 - Symptomatic CD4 200-499<br />
- Asymptomatic CD4 200-499 - Symptomatic CD4 < 200<br />
- Asymptomatic CD4 < 200 - AIDS CD4 > = 500<br />
- Symptomatic CD4 > = 500 - AIDS CD4 200-499<br />
- AIDS CD4 < 200<br />
Page 32 of 72<br />
The lists of client codes were usually forwarded to the reviewer and corresponding agencies 5-10 business days<br />
before reviews were scheduled to commence.
Characteristics of the Sample Population<br />
The review sample population was generally comparable to the Part A population receiving oral health care in terms<br />
of race/ethnicity, gender, age and stage of illness. 1<br />
It is important to note that the chart review findings in this<br />
report apply only to those who receive oral health care from a Part A provider and cannot be generalized to all Ryan<br />
White clients or to the broader population of persons with HIV or AIDS. Table 2 compares the review sample<br />
population with the Ryan White Part A oral health care population as a whole.<br />
Table 2. Demographic Characteristics of FY 08 Houston EMA Ryan White Part A Oral Health Care Clients<br />
Sample Ryan White Part A EMA<br />
Race/Ethnicity Number Percent Number Percent<br />
African American 91 44% 1037 46%<br />
White 109 53% 1186 52%<br />
Asian 1 1% 20 1%<br />
Native Hawaiian/Pacific<br />
Islander 1 1% 4
Findings<br />
Appointments<br />
To reduce the number of no-show appointments, the appointment policy at the agency requires patients to call at<br />
least twenty-four hours in advance if their appointment must be canceled or rescheduled. If a patient fails to follow<br />
this policy more than twice, they are no longer eligible for regularly scheduled appointments, but instead are<br />
scheduled for block appointments where groups of patients are scheduled at the same time. While this strategy may<br />
be employed to encourage appointment keeping, it may also create a barrier to oral health care, particularly among<br />
clients facing other life challenges that make appointment keeping very difficult.<br />
At the time of the review, only 6% of records reviewed were for patients who missed more than two appointments.<br />
This rate has continued to decline in recent years. During the 2008 chart review 17% of reviewed records indicated<br />
that would be subject to restricted scheduling.<br />
Unfortunately, this year’s review does demonstrate a marked increase in the racial disparity of those patients<br />
requiring restricted appointments. Historically, there has been little racial difference among individuals who missed<br />
more than two appointments. Last year, of those who missed more than two appointments 43% were African-<br />
Americans. This was slightly less than the percentage that African-Americans represented in the chart review<br />
sample population. However, this year 83% of patients that missed more than 2 appointments were African-<br />
American. This is well over their 44% representation in the sample population.<br />
Additionally, there is also a measure of gender disparity in the restricted scheduling. Fifty percent of those who<br />
missed three or more appointments were females. However, females represent only 26% of the sample population.<br />
These results should be interpreted with caution given the small number of clients in the sample population who<br />
were subject to restricted appointments, and the lack of additional testing to determine whether these differences<br />
are statistically significant.<br />
Clinic Visits<br />
Information gathered during the 2009 chart review included the number of visits during the study period and the<br />
provider type (dentist, hygienist, prosthodontics, other). Generally, utilization of dentists and hygienists was<br />
significant. Of the 1,243 oral health care appointments, 80% of the total number of appointments were conducted<br />
by either a dentist or hygienist. The average number of oral health visits per patient in the sample population was<br />
six. Ninety-eight percent of review patients had an appointment conducted by a dentist at least once during the<br />
review period.<br />
Health History<br />
Page 34 of 72<br />
A complete and thorough assessment of a patient’s medical history is essential among individuals infected with HIV<br />
or anyone who is medically compromised. Such information, such as current medication or any history of<br />
alcoholism for example, offers oral health care providers key information that may determine the appropriateness of<br />
prescriptions, oral health treatments and procedures. The form that is used by the agency to assess patient’s health<br />
history captures a wide range of information; however, for the purposes of this review, this report will focus on the<br />
assessment of information that is of particular importance among HIV/AIDS patients compared to patients in the<br />
general population.<br />
Assessment of Medical History<br />
� 89% (99%-FY 08) of records reviewed for new patients contained an initial assessment of past medical<br />
history. Ninety-eight percent of applicable records documented a health history update every 6 months.<br />
Key highlights are as follows:<br />
o HIV Associated Opportunistic Infections: 98% (98%-FY 08) of records reviewed documented<br />
opportunistic infection status.<br />
o Allergies & Drug Sensitivities: 98% (100%-FY 08) of records reviewed had documentation for<br />
assessing allergies and drug sensitivities located in a prominently in the chart.
Health History cont’d<br />
o Alcohol Use: 0% (25%-FY 08) of records reviewed documented an assessment of alcohol use<br />
during the study period.<br />
o Tobacco Use: 0% (33%-FY 08) of records reviewed documented an assessment of either smoking<br />
status or current use of chewing tobacco/snuff during the study period.<br />
o Street/Illegal Drug Use: 0% (23%-FY 08) of records reviewed documented an assessment of<br />
recreational drug use during the study period.<br />
Health Assessments<br />
o Blood Pressure: 100% of reviewed records documented patient blood pressure at initial visit and<br />
an update of the patient’s blood pressure every 6 months. Additionally, 100% of applicable records<br />
documented blood pressure results prior to an applicable dental procedure.<br />
o Pulse: 100% of reviewed records documented patient pulse at initial visit and an update of the<br />
patient’s pulse every 6 months.<br />
o Risk for infection and bleeding: 100% of applicable records reviewed assessed the patients risk<br />
for infection and bleeding prior to an invasive procedure.<br />
o Need for Antibiotic Prophylaxis: 100% (99%-FY 08) of records reviewed assessed the patients<br />
need for antibiotic prophylaxis.<br />
Patient Medications<br />
� 100% (100%-FY 08) of records reviewed documented a review of patient medications for either HIV or<br />
non-HIV medication.<br />
Primary Care Provider Contact Information<br />
� 100% (100%-FY 08) of records reviewed contained contact information for a primary care provider.<br />
Prevention and Detection of Oral Disease<br />
Page 35 of 72<br />
Maintaining good oral health is so vital to the overall quality of life for individuals living with HIV/AIDS because<br />
the condition of one’s oral health often plays a major role in how well patients are able manage their HIV disease.<br />
Poor oral health due to a lack of dental care may lead to the onset and progression of oral manifestations of HIV<br />
disease, which makes maintaining proper diet and nutrition or adherence to antiretroviral therapy very difficult to<br />
achieve. Furthermore, poor oral health places additional burden on an already compromised immune system.<br />
An intraoral exam was performed in 98% of records reviewed (95%-FY 08). Ninety-eight percent of reviewed<br />
records documented an extraoral exam of the face, head and neck during the study period (95% in FY 08). Onehundred<br />
percent of applicable records documented an x-ray (100% in FY 08 review). Ninety-nine percent of<br />
reviewed records (1% in FY 08 review) documented the clinical chart of teeth was marked and up to date.<br />
One hundred percent of the records reviewed (97% in FY 08 review) documented a statement by the dentist of an<br />
annual patient diagnosis. Ninety-nine percent of reviewed records (91% in FY 08 review) contained a subsequent<br />
treatment plan and/or updates to the treatment plan. One hundred percent of those records documented the<br />
appropriate treatment was done for condition indicated.<br />
Four percent of reviewed records contained documentation of the patient’s need to be seen by a specialist. Of<br />
these records, 78% of applicable records (100%-FY 08) contained documentation that a referral was provided.<br />
The chart review examined assessed patients for the following oral manifestations associated with HIV: xerostomia,<br />
LGE periodontal disease, NUP periodontal disease, and candidiasis. Ninety-two percent of assessed records<br />
documented no pathology for any of these conditions. Three percent of reviewed records (
Conclusions<br />
Overall, oral healthcare services continues it’s trend of consistent, high quality care. The Houston EMA oral<br />
healthcare program has established a strong foundation for preventative care. This is demonstrated in the rates of<br />
intraoral and extraoral exams, 98% for both. The provider has also shown excellent documentation of care with<br />
100% of applicable records documenting an x-ray (100% in FY 06 through FY 08) and 99% of records containing a<br />
marked and up to date clinical tooth chart. Additionally, one hundred percent of the records reviewed (97% in FY<br />
08 review) documented a statement by the dentist of an annual patient diagnosis. Ninety-nine percent of reviewed<br />
records contained a subsequent treatment plan and/or updates to the treatment plan. This rate is an almost 10%<br />
improvement over last year’s review finding of 91%.<br />
This review cycle did suggest a decrease in screening rate for alcohol, tobacco, and recreational drug use (0%-FY<br />
08). These rates were much improved during last year’s chart review. The rates were 2% for FY 07, and increased<br />
to 25%, 33%, and 23% respectively for FY 08 However, during the past year the oral health care provider has<br />
initiated an electronic records system. This may have impacted the chart abstractor’s ability to locate these health<br />
history elements.<br />
Similarly, the rate of necessary specialist referrals showed great improvement in FY 08 at 100%, up from 2% in FY<br />
07. However, FY 09 chart review findings indicate a decrease to 78%. This decrease should be interrupted with<br />
caution, due to the small number of records that required a specialist referral. The 4% of applicable records<br />
indicating a need for a specialist, represents nine charts. Of these nine, two did not document a referral.<br />
Overall, oral healthcare services continues to exhibit excellent performance. We look forward to continued high<br />
levels of care for our patients in future reviews.<br />
Appendix A – Resources<br />
Abel, Stephen N. (and others) eds. Principles of Oral Health Management. Dental Alliance for AIDS/HIV Care,<br />
2000. HAB00230<br />
Periodontal Screening & Recording ®: An Early Detection System. (n.d.). Retrieved May 25, 2004, from<br />
http://www.ada.org/prof/resources/topics/perioscreen/index.asp<br />
Page 36 of 72<br />
Heavy Drinking, Drug Abuse Present Health Complications for Dental Treatment. (December 1, 2003). Retrieved<br />
May 18, 2004 from http://www/agd.org/media/2003/dec/abuse.html
RYAN WHITE GRANT<br />
PROGRAM<br />
SUMMARY REPORT<br />
2009 RYAN WHITE FOCUS<br />
GROUPS<br />
December 2009<br />
Prepared by:<br />
Carin Martin, MPA<br />
Project Coordinator-Quality Management Development<br />
<strong>Harris</strong> County Public Health & Environmental <strong>Service</strong>s<br />
Ryan White Grant Administration Section<br />
2223 West Loop South, RM 417<br />
Houston, TX 77027<br />
713-439-6041<br />
Page 37 of 72
Executive Summary<br />
The following findings highlight the most frequently discussed topics by focus<br />
group participants:<br />
• Most participants are satisfied with transportation benefits provided<br />
through Ryan White funded bus passes. Many of the participants<br />
reported an awareness bus passes should be used exclusively for<br />
transportation to medical appointments.<br />
• Many of the participants reported experiencing long waits for dental<br />
care services, particularly general cleaning appointments.<br />
• Most participants reported receiving their annual Pap screenings as<br />
scheduled.<br />
• Many of the participants emphasized the importance of peer<br />
support/mentoring groups in staying engaged in their own health<br />
maintenance.<br />
• Most participants reported substance abuse, depression and/or<br />
incarceration as barriers to entering care after learning their diagnosis.<br />
Ryan White Grant Program<br />
Summary Report on 2009 Ryan White Consumer Focus Groups<br />
Background<br />
The Houston EMA (Eligible Metropolitan Area) Ryan White Grant<br />
Administration office has conducted consumer satisfaction surveys on an<br />
annual basis since 2003. Since 2008, the Houston Ryan White Grant<br />
Administration office has conducted focus groups at each of the primary care<br />
agencies that receive Ryan White funding to augment the consumer<br />
satisfaction process. The focus groups are conducted to obtain client<br />
perspectives on a variety of core and support services.<br />
In Fall 2009, Ryan White Grant Administration, and <strong>Harris</strong> County Public<br />
Health and Environmental <strong>Service</strong>s staff conducted a series of focus groups<br />
with consumers who utilize Ryan White funded core and support services (as<br />
defined under the Ryan White HIV/AIDS Treatment Modernization Act of 2006).<br />
The data were collected to obtain additional insight into consumers’<br />
perceptions of their experiences with Ryan White funded services. The report<br />
presents common themes that arose from the four focus groups.<br />
Methods and Analyses<br />
Information was obtained on clients perceptions of access to and quality of<br />
care received through the Ryan White funded agencies in a variety of service<br />
areas including, primary care, dental care, transportation, and case<br />
management services, among others.<br />
Page 38 of 72
The Ryan White Project Coordinator collaborated with agency representatives<br />
to recruit clients to participate in the focus groups. The focus groups were<br />
moderated by the Ryan White Project Coordinator. An interpreter was<br />
present at two focus group sessions to ensure full engagement of Spanishspeaking<br />
consumer participants. However, no monolingual Spanish<br />
participants were present at any of the four focus groups. Agencies staff were<br />
prohibited from participating in the focus group sessions to encourage full<br />
disclosure of experiences among focus group participants.<br />
Informed consent forms were obtained from each focus group participant prior<br />
to each focus group session. There were both English and Spanish versions of<br />
the informed consent form available to participants. Each focus group session<br />
was audio taped and transcribed verbatim (to the extent possible). Once the<br />
focus group sessions were transcribed the audiotapes were destroyed to protect<br />
the identity of the focus group participants. Focus group participants were<br />
encouraged to comment however they were informed that it was not necessary<br />
to respond to every question.<br />
A thematic analysis was used to analyze the data. Thematic analysis identifies<br />
patterns in the data and organizes and describes the data in detail (Braun &<br />
Clarke, 2006) 1.<br />
It is important to note that focus group results are not<br />
generalizable to the larger population of consumers who receive Ryan White<br />
funded services.<br />
Characteristics of Focus Group Participants<br />
During the 2009 focus groups, several discussion questions focused on<br />
women’s health issues, specifically Pap screenings. For this reason, most<br />
agency staff recruited exclusively from their female client base. However, one<br />
agency did have mostly male participants. The women in this group indicated<br />
they were comfortable discussing women’s health issue questions in a mixed<br />
gender setting. Additionally, there was a mixture of other characteristics<br />
among focus group participants. There were individuals who had been<br />
diagnosed as long as twenty years ago as well as newly diagnosed individuals.<br />
The education and socioeconomic level of participants also varied. For<br />
example, many participants heavily relied on the Ryan White Program for<br />
transportation services while a few reported owning their own vehicles. The<br />
majority of participants were African American. There were several White<br />
participants. Focus groups consisting of representatives from agency<br />
consumer councils/support groups tended to voice their concerns more readily<br />
than others.<br />
1<br />
Braun, V. & Clarke, V. (2006). Using thematic analysis in psychology. Qualitative Research in<br />
Psychology,3, 77-101.<br />
Page 39 of 72
Dental <strong>Service</strong>s<br />
Findings<br />
Consumers were asked if they aware of any recent changes in Ryan White<br />
Dental services. Those who were aware were asked how the changes have<br />
affected dental services.<br />
In an effort to increase access to dental services, at the beginning of FY 2009,<br />
the Houston EMA began funding a rural oral health care provider.<br />
Additionally, the Houston EMA’s only untargeted oral health care provider<br />
relaxed their rescheduling policy regarding missed client appointments.<br />
• Many of the focus group participants were currently engaged in dental<br />
care, and most of those individuals were aware of changes in the<br />
untargeted provider’s rescheduling policy.<br />
• Participants that were aware of changes in the rescheduling policy were<br />
universally pleased with its impact on access to dental services.<br />
• One participant stated she had already benefited from the more flexible<br />
policy, and that she felt the dental provider were more understanding of<br />
the fact things arise in day-to-day scheduling that make keeping every<br />
appointment difficult for someone living with HIV/AIDS.<br />
• A number of participants that had not been aware of the new policy<br />
commented that they would make an effort to engage in oral health care<br />
services again.<br />
• Most participants were not aware of the new oral health care provider.<br />
The exception to this were patients who received primary medical care<br />
through the same agency that provides rural oral health care.<br />
• Many focus group participants reported long waits for dental care<br />
appointments. One participant commented that she completed her<br />
prerequisite x-ray appointment with the untargeted dental provider and<br />
was told she would be contacted when an appointment was available<br />
for a cleaning. She followed-up for a year. After a year on the waiting<br />
list, she was seen for a cleaning, and told that her x-rays had expired<br />
and needed to be completed again. Participants reported the wait time<br />
at the rural dental provider to be approximately 30 days.<br />
Page 40 of 72
Conclusions<br />
The information obtained through these focus groups provided valuable<br />
insight on consumers’ perceptions of their access to care and experiences with<br />
service providers. Issues such as patient mental health, substance abuse,<br />
stigma, the importance of social support networks and access to medical and<br />
dental appointments were common themes discussed across focus groups.<br />
One of the most notable topics discussed was the profound negative effect<br />
depression and/or substance abuse has on patient retention in medical care.<br />
Depression and substance abuse were given as the chief reasons why patients<br />
were out of care for extended periods of time. This information further<br />
confirms the importance of mental health and substance abuse screenings for<br />
all patients that enter the care system. Mental health and substance abuse<br />
service availability and referral follow-up are equally important aspects of<br />
overcoming barriers to retention in care.<br />
The importance of a support network was also a sentiment that was expressed<br />
across all focus groups. This appeared to be particularly true for patients that<br />
were new to HIV medical care. Participants indicated that in-clinic support<br />
groups were not only excellent resources for information on how to navigate<br />
the care system, but also a network for friends with similar life experiences.<br />
Many consumers comments that the “support groups” were like family,<br />
always available and helpful.<br />
In addition to treatment adherence and retention in care issues, access to<br />
dental services continues to be a significant concern. Many participants were<br />
aware of increased flexibility with our untargeted dental providers<br />
rescheduling policy. Participants also believe that this change enhances their<br />
access to oral health care. However, appointment availability due to system<br />
capacity appears to be a growing problem.<br />
Linkage to and retention in primary medical care is a central focus of quality<br />
improvement for HIV-positive individuals on both a local and national level.<br />
The information provided in the 2009 Houston EMA focus group offers<br />
excellent insight on what areas have the potential of making the greatest<br />
impact on this issue.<br />
Page 41 of 72
Public Comment<br />
for How to Best<br />
Meet the Need<br />
Oral Health<br />
Workgroup<br />
Page 42 of 72
Monday Tuesday Wednesday Thursday Friday Week Totals<br />
Hyg Pts Seen 16 19 15 17 19 86<br />
Hyg Apts<br />
Scheduled<br />
20 20 18 20 20 98<br />
Hyg No Show 4 1 3 3 2 13<br />
X/E Pts Seen 8 20 0 16 6 50<br />
X/E Apts<br />
Scheduled<br />
9 18 0 18 9 54<br />
X/E No Show 2 0 0 3 3 8<br />
Gen Pts Seen 20 27 19 24 26 116<br />
Gen Apts<br />
Scheduled<br />
0<br />
0.00<br />
205<br />
4.10<br />
20 27 17 25 23 112<br />
Gen No Show 5 5 1 2 0 13<br />
Length of General Waiting List in Weeks<br />
Pros Pts Seen 21 9 15 13 10 68<br />
Pros Apts<br />
Scheduled<br />
25 10 17 13 9 74<br />
Pros No Show 5 1 2 0 0 8<br />
Number of Individuals Currently on Pros Waiting List<br />
PVC/Implant<br />
Pts Seen<br />
PVC/Implant<br />
Apts Sched.<br />
PVC/Implant<br />
No Show<br />
Weekly Tally February 1-5<br />
Number of Individuals Currently on Hygiene Waiting List<br />
Length of Hygiene Waiting List in Weeks<br />
Number of Individuals Currently on X/E Waiting List<br />
Length of X/E Waiting List in Weeks<br />
Number of Individuals Currently on Gen Waiting List<br />
Length of Pros Waiting List in Weeks<br />
1 0 2 0 0 3<br />
1 1 2 0 0 4<br />
0 0 0 0 0 0<br />
Number of Individuals Currently on PVC/Implant Waiting List<br />
226<br />
1.95<br />
0<br />
0.00<br />
363<br />
Page 43 of 72
Monday Tuesday Wednesday Thursday Friday Week Totals<br />
Length of PVC/Implant Waiting List in Weeks<br />
Perio Pts Seen 0 0 8 0 0 8<br />
Perio Apts<br />
Scheduled<br />
Perio No<br />
Show<br />
121.00<br />
0 0 7 0 0 7<br />
0 0 1 0 0 1<br />
Number of Individuals Currently on Perio Waiting List<br />
Length of Perio Waiting List in Weeks<br />
Pts Seen 331<br />
Apts<br />
Scheduled<br />
349<br />
No Show 43<br />
No Show Rate 12.32%<br />
Total Number of Individuals Currently on Waiting List<br />
3<br />
0.38<br />
797<br />
Page 44 of 72
Monday Tuesday Wednesday Thursday Friday Week Totals<br />
Hyg Pts Seen 20 15 18 20 20 93<br />
Hyg Apts<br />
Scheduled<br />
20 15 18 20 19 92<br />
Hyg No Show 3 2 2 3 1 11<br />
X/E Pts Seen 17 14 0 17 1 49<br />
X/E Apts<br />
Scheduled<br />
17 18 0 18 0 53<br />
X/E No Show 0 4 0 1 0 5<br />
Gen Pts Seen 16 22 22 20 19 99<br />
Gen Apts<br />
Scheduled<br />
14 24 18 19 18 93<br />
Gen No Show 2 2 0 1 2 7<br />
Pros Pts Seen 29 10 19 11 12 81<br />
Pros Apts<br />
Scheduled<br />
28 11 17 12 14 82<br />
Pros No Show 1 1 1 1 2 6<br />
Number of Individuals Currently on Pros Waiting List<br />
PVC/Implant<br />
Pts Seen<br />
PVC/Implant<br />
Apts Sched.<br />
PVC/Implant<br />
No Show<br />
Weekly Tally February 12<br />
Number of Individuals Currently on Hygiene Waiting List<br />
Length of Hygiene Waiting List in Weeks<br />
Number of Individuals Currently on X/E Waiting List<br />
Length of X/E Waiting List in Weeks<br />
Number of Individuals Currently on Gen Waiting List<br />
Length of General Waiting List in Weeks<br />
Length of Pros Waiting List in Weeks<br />
1 1 2 1 0 5<br />
1 1 2 1 0 5<br />
0 0 0 0 0 0<br />
Number of Individuals Currently on PVC/Implant Waiting List<br />
0<br />
0.00<br />
238<br />
4.86<br />
252<br />
2.55<br />
7<br />
0.09<br />
350<br />
Page 45 of 72
Length of PVC/Implant Waiting List in Weeks<br />
Perio Pts Seen 0 0 8 0 10 18<br />
70.00<br />
Perio Apts<br />
Scheduled<br />
0 0 7 0 11 18<br />
Perio No<br />
Show<br />
0 0 0 0 2 2<br />
Number of Individuals Currently on Perio Waiting List<br />
3<br />
Length of Perio Waiting List in Weeks<br />
Pts Seen 345<br />
Apts<br />
Scheduled<br />
343<br />
No Show 31<br />
No Show Rate 9.04%<br />
Total Number of Individuals Currently on Waiting List<br />
Number of <strong>New</strong> Intakes<br />
0.17<br />
850<br />
9<br />
Page 46 of 72
Monday Tuesday Wednesday Thursday Friday Week Totals<br />
Hyg Pts Seen 20 20 18 20 20 98<br />
Hyg Apts<br />
Scheduled<br />
19 20 18 20 20 97<br />
Hyg No Show 1 1 2 3 2 9<br />
X/E Pts Seen 19 16 0 16 7 58<br />
X/E Apts<br />
Scheduled<br />
18 18 0 18 9 63<br />
X/E No Show 2 2 0 2 2 8<br />
Gen Pts Seen 16 21 15 24 21 97<br />
Gen Apts<br />
Scheduled<br />
16 25 16 21 21 99<br />
Gen No Show 3 5 3 0 4 15<br />
Pros Pts Seen 32 14 17 12 10 85<br />
Pros Apts<br />
Scheduled<br />
29 15 20 12 9 85<br />
Pros No Show 1 1 4 1 1 8<br />
Number of Individuals Currently on Pros Waiting List<br />
PVC/Implant<br />
Pts Seen<br />
PVC/Implant<br />
Apts Sched.<br />
PVC/Implant<br />
No Show<br />
Weekly Tally February 19<br />
Number of Individuals Currently on Hygiene Waiting List<br />
Length of Hygiene Waiting List in Weeks<br />
Number of Individuals Currently on X/E Waiting List<br />
Length of X/E Waiting List in Weeks<br />
Number of Individuals Currently on Gen Waiting List<br />
Length of General Waiting List in Weeks<br />
Length of Pros Waiting List in Weeks<br />
0 0 2 2 0 4<br />
0 0 2 2 0 4<br />
0 0 0 0 0 0<br />
Number of Individuals Currently on PVC/Implant Waiting List<br />
0<br />
0.00<br />
273<br />
4.71<br />
296<br />
3.05<br />
0<br />
0.00<br />
351<br />
Page 47 of 72
Length of PVC/Implant Waiting List in Weeks<br />
Perio Pts Seen 0 0 7 0 6 13<br />
87.75<br />
Perio Apts<br />
Scheduled<br />
0 0 8 0 7 15<br />
Perio No<br />
Show<br />
0 0 2 0 1 3<br />
Number of Individuals Currently on Perio Waiting List<br />
3<br />
Length of Perio Waiting List in Weeks<br />
Pts Seen 355<br />
Apts<br />
Scheduled<br />
363<br />
No Show 43<br />
No Show Rate 11.85%<br />
Total Number of Individuals Currently on Waiting List<br />
Number of <strong>New</strong> Intakes<br />
0.23<br />
923<br />
8<br />
Page 48 of 72
Monday Tuesday Wednesday Thursday Friday Week Totals<br />
Hyg Pts Seen 20 19 15 19 19 92<br />
Hyg Apts<br />
Scheduled<br />
20 20 16 20 20 96<br />
Hyg No Show 2 5 1 3 4 15<br />
X/E Pts Seen 5 14 0 14 0 33<br />
X/E Apts<br />
Scheduled<br />
9 20 0 18 0 47<br />
X/E No Show 4 6 0 4 0 14<br />
Gen Pts Seen 21 27 17 34 26 125<br />
Gen Apts<br />
Scheduled<br />
0<br />
0.00<br />
182<br />
5.52<br />
20 26 18 34 23 121<br />
Gen No Show 4 0 0 1 1 6<br />
Pros Pts Seen 26 11 17 10 11 75<br />
Pros Apts<br />
Scheduled<br />
30 10 17 10 11 78<br />
Pros No Show 7 0 2 1 0 10<br />
Number of Individuals Currently on Pros Waiting List<br />
Length of Pros Waiting List in Weeks<br />
PVC/Implant<br />
Pts Seen<br />
PVC/Implant<br />
Apts Sched.<br />
PVC/Implant<br />
No Show<br />
Weekly Tally February 26<br />
Number of Individuals Currently on Hygiene Waiting List<br />
Length of Hygiene Waiting List in Weeks<br />
Number of Individuals Currently on X/E Waiting List<br />
Length of X/E Waiting List in Weeks<br />
Number of Individuals Currently on Gen Waiting List<br />
Length of General Waiting List in Weeks<br />
1 0 3 0 1 5<br />
1 0 3 0 1 5<br />
0 0 1 0 0 1<br />
Number of Individuals Currently on PVC/Implant Waiting List<br />
281<br />
2.25<br />
0<br />
0.00<br />
352<br />
Page 49 of 72
Length of PVC/Implant Waiting List in Weeks<br />
Perio Pts Seen 0 0 9 0 6 15<br />
Perio Apts<br />
Scheduled<br />
Perio No<br />
Show<br />
70.40<br />
0 0 9 0 10 19<br />
0 0 0 0 4 4<br />
Number of Individuals Currently on Perio Waiting List<br />
Length of Perio Waiting List in Weeks<br />
Pts Seen 345<br />
Apts<br />
Scheduled<br />
366<br />
No Show 50<br />
No Show Rate 13.66%<br />
Total Number of Individuals Currently on Waiting List<br />
Number of <strong>New</strong> Intakes<br />
3<br />
0.20<br />
818<br />
13<br />
Page 50 of 72
February Tally<br />
Week 1 Week 2 Week 3 Week 4 Month Totals<br />
Patients Seen 331 345 355 345 1376<br />
1421<br />
Appointments Scheduled<br />
349 343 363 366<br />
No Show 43 31 43 50 167<br />
No Show Rate 12.32% 9.04% 11.85% 13.66% 11.72%<br />
Total Number of Individuals<br />
Currently on Waiting List<br />
797 850 923 818 818<br />
Number of <strong>New</strong> Intakes 18 9 8 13 48F<br />
Page 51 of 72
INCREASING ACCESS TO DENTAL CARE<br />
You cannot be healthy without oral health<br />
—Oral Health in America: A Report of the Surgeon General 1<br />
Access to oral health care for all people living with HIV/AIDS (PLWHA)<br />
remains a critical—and unmet—goal. Uninsured PLWHA are three times<br />
more likely to have untreated dental and medical needs than are PLWHA<br />
with private insurance. Moreover, oral infections, mouth ulcers, and other<br />
severe dental conditions associated with HIV infections go untreated more<br />
than twice as often as other health problems related to the disease. 2<br />
DID YOU KNOW?<br />
<strong>HRSA</strong>-supported community health centers in 2006 provided oral<br />
health services to some 2.6 million patients.<br />
Approximately 108 million Americans lack dental insurance. 3<br />
More than 500 medications can lead to xerostomia or “dry mouth,”<br />
which can lead to dental decay, periodontal disease, and oral<br />
candidiasis (thrush). 4,5,6<br />
���� Please visit our <strong>Web</strong> site at www.hrsa.gov<br />
ONLINE RESOURCES<br />
Page 52 of 72<br />
AUGUST 2008<br />
Big Barriers: High Costs<br />
HIV Dental Health Issues<br />
Transporting Health<br />
Taking It to the Streets<br />
<strong>HRSA</strong> Part F Dental Programs<br />
http://hab.hrsa.gov/<br />
treatmentmodernization/dental.htm<br />
SPNS Oral Health Initiative Evaluation<br />
Center<br />
www.hdwg.org/echo/front<br />
Oral health in America: A report of the<br />
Surgeon General<br />
http://silk.nih.gov/public/<br />
hck1ocv.@www.surgeon.fullrpt.pdf<br />
HIV Screening in Dental Settings: The<br />
Role of Salivary Diagnostics<br />
www.nationaloralhealthconference.<br />
com/docs/presentations/2007/0430/<br />
Jennifer%20Cleveland%20%20Salivary<br />
%20Diagnostics%20Potential%20<br />
Benefits%20of%20HIV%20Testing%<br />
20in%20Dental%20Settings.pdf
2<br />
DIRECTOR’S NOTES<br />
When the media covers HIV disease, its impact on<br />
dental care and access to oral health services is rarely<br />
discussed. As health care professionals, however, we know<br />
all too well that oral health problems are often the first<br />
manifestations of HIV disease. For HIV-positive persons<br />
who don't know their status, dentists can have an important<br />
role as diagnosticians. For PLWHA who do know their<br />
status, providers must be ever vigilant in linking people to<br />
dental providers and preventing oral health problems.<br />
Dental care in the United States is a luxury many<br />
people cannot afford. In fact, 108 million Americans are<br />
without dental insurance. But for PLWHA, the lack of<br />
proper oral health care can be devastating. Weakened<br />
immune systems can make PLWHA more susceptible to<br />
oral infections and dental problems can interfere with<br />
nutrition and absorption of life-saving HIV medications.<br />
HIV providers across the country are addressing new<br />
oral health issues as they arise—and persist. These may<br />
include “meth mouth,” or the need for more implants and<br />
denture work, as PLWHA continue to age with the disease.<br />
This is why the linkages providers create with one another<br />
are so essential to creating the comprehensive care PLWHA<br />
need if they are going to get healthy—and stay that way.<br />
Deborah Parham Hopson<br />
<strong>HRSA</strong> Associate Administrator for HIV/AIDS<br />
<strong>HRSA</strong> CAREAction<br />
Publisher<br />
U.S. Department of Health and Human <strong>Service</strong>s<br />
Health Resources and <strong>Service</strong>s Administration, HIV/AIDS Bureau<br />
5600 Fishers Lane, Room 7-05<br />
Rockville, MD 20857<br />
Telephone: 301.443.1993<br />
Prepared for <strong>HRSA</strong>/HAB<br />
by Impact Marketing + Communications, www.impactmc.net<br />
Photography<br />
Cover: a patient at the San Francisco Native American Health Center’s<br />
pediatric dental facility. © See Change, www.see-change.net<br />
P. 7, Project coordinator Henry Boza of the Miami Dental Access<br />
Project. © See Change, www.see-change.net<br />
Additional copies are available from the <strong>HRSA</strong> Information Center,<br />
1.888.ASK.<strong>HRSA</strong>, and may be downloaded at www.hab.hrsa.gov.<br />
Page 53 of 72<br />
In addition to common oral health problems,<br />
such as caries (decay) and gingivitis,<br />
PLWHA have a high incidence of rare oral health<br />
issues (see Table 1) because of their weakened<br />
immune systems. 7 Dental problems can also<br />
impede food intake and nutrition, 8 leading to<br />
poor absorption of HIV medications and<br />
increasingly impaired immune function, particularly<br />
because all antiretroviral medications are<br />
given in relation to food intake. 9<br />
Poor oral health conditions can also interfere<br />
with social functioning and limit educational<br />
and career opportunities as a result of the<br />
disfigurement and odor caused by decayed<br />
teeth and gum disease. 10 Completing the circle,<br />
reduced quality of life related to oral health is<br />
associated with poor clinical status and reduced<br />
access to health care. 11<br />
These data are not news to most providers<br />
of HIV/AIDS care to the uninsured. Yet, the<br />
unmet need for oral health services and the<br />
incidence of entirely preventable oral health<br />
problems among underinsured PLWHA remains<br />
persistent. In fact, even people who have medical<br />
insurance, whether or not they have HIV/<br />
AIDS, may have limited or no dental benefits.<br />
Providers who are most successful at helping<br />
PLWHA transcend barriers to good oral<br />
health are applying perhaps one of the most<br />
important lessons learned—and relearned—<br />
since the Ryan White HIV/AIDS Program was<br />
adopted: Eliminating health disparities often<br />
isn’t about doing just one thing; instead, it is<br />
about meeting PLWHA “where they are” and<br />
helping them address the specific barriers they<br />
face.<br />
Big Barriers Extract High Costs<br />
HIV-positive people face challenges in maintaining<br />
oral health that go beyond remembering<br />
to brush and floss their teeth. First among<br />
them may be fear. As much as 20 percent of the<br />
American population does not regularly visit<br />
the dentist because of anxiety, and an estimated<br />
8 to 15 percent of Americans avoid<br />
dental treatment entirely because of this fear. 12<br />
A more systemic issue is that the number of<br />
oral health professionals per capita is declining.<br />
The number of practicing dentists in the United
States has remained stagnant at around 150,000 since<br />
1990, although the U.S. population has grown significantly<br />
since then. 13 The diminishing availability of dentists<br />
exacerbates the shortage of dentists who are experienced<br />
in treating—or willing to treat—PLWHA.<br />
“The number of dentists providing dental care to<br />
HIV-positive patients is inadequate. Consumers consistently<br />
identify oral health as one of their top unmet<br />
needs,” according to Mahyar Mofidi, project director of<br />
the Ryan White HIV/AIDS Program Part F Community-<br />
Based Dental Partnership Program.<br />
PWLHA are among the 108 million Americans without<br />
dental insurance—a number 2.5 times greater than<br />
the number of Americans who lack medical insurance.<br />
14,15 Fewer and fewer people have dental insurance<br />
for a host of reasons, including lack of health literacy,<br />
inadequate coverage from public programs, loss of dental<br />
insurance after retirement, and employer insurance<br />
plans that do not cover dental care. This lack of insurance<br />
is interwoven with many familiar problems for<br />
PLWHA, such as the inability to pay for care and unmet<br />
needs for essentials like transportation, housing, and<br />
child care.<br />
As Steven Toth of the University of Medicine and<br />
Dentistry of <strong>New</strong> Jersey (UMDNJ) explains, poor oral<br />
health carries a stigma. “We had a patient who was very<br />
embarrassed about his smile,” says Toth.“When we saw<br />
him for the first time, he had maybe two teeth. We were<br />
able to give him back his smile, and now his teeth are<br />
reflective of his personality.”<br />
HIV-Specific Dental Health Issues<br />
PLWHA can develop the same oral health problems as<br />
HIV-negative people. But some conditions are seen<br />
almost exclusively in people who are HIV positive (see<br />
Table 1, page 4). In fact, more than one-third of PLWHA<br />
have oral conditions resulting from a weakened<br />
immune system. 20 Oral lesions from candidiasis (thrush),<br />
oral hairy leukoplakia, herpetic ulcers, and Kaposi’s sarcoma,<br />
for example, are often among the first symptoms<br />
of HIV infection. 21<br />
Bacteria are the culprits behind the two most common<br />
oral health conditions affecting everyone, regardless<br />
of HIV status: dental caries and periodontal disease.<br />
22 These bacterial infections that begin in the<br />
mouth can potentially inflict great harm to the heart,<br />
brain, and other organs if not treated, particularly in<br />
PLWHA with severely compromised immune systems. 23<br />
In addition, antiretroviral medications taken by<br />
many PLWHA may cause a reduction in salivary secretions<br />
called xerostomia, commonly referred to as “dry<br />
mouth,”which predisposes people to caries, periodontal<br />
disease, and oral candidiasis. 24,25 In fact, more than 500<br />
medications can lead to dry mouth, and approximately<br />
30 percent of PLWHA have moderate to severe dry<br />
mouth. 26<br />
Saliva neutralizes acids in the mouth from food and<br />
drink and helps prevent microorganisms from adhering<br />
to teeth; in the absence of sufficient saliva, acids and<br />
pathogens have deleterious effects on teeth and gums. 27<br />
Fortunately, dry mouth is easily treated with artificial<br />
“The number of dentists providing dental care to HIV-positive patients is inadequate.<br />
Consumers consistently identify oral health as one of their top unmet needs.”<br />
In addition to large-scale issues, such as cost of services<br />
and access to care, smaller, more personal ones play<br />
a significant role in oral health. People with substance<br />
abuse problems, for example, have an increased incidence<br />
of poor oral hygiene. Some illicit substances<br />
increase cravings for sugary foods and drinks which,<br />
over time, can erode teeth. 16,17 Drugs like ecstasy and<br />
crystal methamphetamine make users more susceptible<br />
to tooth grinding and cause dry mouth. The corrosive<br />
properties of methamphetamine can lead to decayed<br />
oral tissue and severe damage, causing teeth to break,<br />
rot, and discolor. 18,19<br />
Page 54 of 72<br />
saliva products or sugar-free citrus candies, such as<br />
lemon drops, which stimulate saliva production. 28<br />
Steps can be taken to prevent many other oral<br />
health care issues that disproportionately affect PLWHA.<br />
Along with regularly brushing and flossing, PLWHA<br />
should limit smoking and alcohol intake—both of which<br />
are strongly associated with oral cancers, which have a<br />
poorer patient prognosis than other types of cancer. 29<br />
Finally, PLWHA should receive dental examinations<br />
every 6 months. It is preferable if examinations are<br />
conducted by providers familiar with the particular conditions<br />
associated with decreased immune function.<br />
(continued on bottom of page 4)<br />
3
4<br />
TABLE 1. ORAL HEALTH PROBLEMS COMMON AMONG PLWHA<br />
Condition<br />
Aphthous stomatitis<br />
Caries<br />
Herpes simplex<br />
Human papilloma<br />
virus (HPV)<br />
Linear gingival<br />
erythema<br />
Kaposi’s sarcoma<br />
(KS)<br />
Necrotizing<br />
ulcerative<br />
periodontitis<br />
Oral candidiasis<br />
Oral hairy<br />
leukoplakia<br />
Periodontal disease<br />
Description/Cause<br />
Also known as canker sores, this condition is characterized by red sores that can be topped<br />
by a yellow-gray film and are usually found on the tongue or inside of the cheeks and lips 30<br />
Tooth decay caused by bacteria 31<br />
Oral Health Care—A Consumer Priority<br />
Oral health care is considered a core medical service<br />
under the Ryan White HIV/AIDS Treatment Modernization<br />
Act. The Ryan White HIV/AIDS Program tackles oral<br />
Viral infection that causes red sores (“fever blisters”) on the roof of the mouth or on the lips 32<br />
Virus associated with genital and other warts and one of the most common sexually transmitted<br />
infections; can produce serious and hard-to-treat lesions in the mouths of PLWHA 33<br />
Inflammation of the gingiva, the tissue surrounding the neck of the tooth; unique among<br />
people with compromised immune systems 34<br />
Cancer that causes red or purple patches of abnormal tissue to grow under the skin; in the<br />
lining of the mouth, nose, and throat, or in other organs 35<br />
Severe form of periodontal disease (see definition below) in which the gums pull away from<br />
the teeth and form pockets that are infected; if not treated, the bones, gums, and connective<br />
tissue that support the teeth are destroyed 36<br />
A fungal (yeast) infection of the mouth also known as thrush; one of the most common<br />
opportunistic infections among PLWHA, usually appearing when CD4 counts fall below 300 37<br />
White, hairlike growth that usually appears on the side of the tongue or the inside of the<br />
cheeks and lower lip; caused by the Epstein-Barr virus 38<br />
Page 55 of 72<br />
Chronic bacterial inflammation of the gums, ranging from gingivitis, in which gums become<br />
red and swollen and can bleed easily, to serious disease that results in damage to the bone 39<br />
health care on several fronts. In addition to Part F dental<br />
programs, Ryan White Parts A and D address oral health<br />
care and, in 2006, provided approximately $43 million for<br />
oral health care services for nearly 70,000 people.
Currently, three specific dental programs exist within<br />
the Ryan White HIV/AIDS Program: the Community-<br />
Based Dental Partnership Program, the Dental Reimbursement<br />
Program, and the Special Projects of National<br />
Significance (SPNS) HIV/AIDS Oral Health Care Initiative.<br />
The sections that follow describe each program.<br />
Community-Based Dental Partnership Program<br />
The Community-Based Dental Partnership Program provides<br />
dental care and provider training in community<br />
based settings.The program aims to increase oral health<br />
services for PLWHA in underserved communities and to<br />
provide hands-on training for dental school students<br />
and residents in treating PLWHA. The training is particularly<br />
valuable, according to Mofidi, because it is “important<br />
for the students to see how dental care fits into<br />
overall health of PLWHA.”<br />
First funded in 2002, this program supports 12<br />
grantees serving 11 States. In 2006, more than 4,300 HIVpositive<br />
patients received dental care through this program<br />
in a total of 22,000 patient visits—about five visits<br />
per patient, per year. 40<br />
Dental Reimbursement Program<br />
The Dental Reimbursement program is the oldest Ryan<br />
White HIV/AIDS Program dental initiative. It reimburses<br />
schools of dentistry and oral hygiene for a portion of the<br />
costs of providing dental care to PLWHA. In 2006, 65<br />
schools received reimbursements totaling more than<br />
$22.9 million.This program has served more than 32,000<br />
PLWHA and helped train more than 11,000 dental students<br />
and residents in 2006. 41<br />
SPNS HIV/AIDS Oral Health Care Initiative<br />
The Health Resources and <strong>Service</strong>s Administration,<br />
HIV/AIDS Bureau, Special Projects of National Significance<br />
(SPNS) HIV/AIDS Oral Health Care Initiative is<br />
funded through Part F of the Ryan White HIV/AIDS<br />
Program. Launched in 2006, the 5-year, multisite initiative<br />
is developing, implementing, and evaluating innovative<br />
models of oral health care around the country.<br />
Fifteen demonstration sites are being funded in both<br />
urban and nonurban areas where oral health services do<br />
not exist or are inadequate to meet current demand.<br />
The Oral Health Care Initiative includes an evaluation<br />
and technical assistance center—the Evaluation<br />
Center for HIV & Oral Health (ECHO) at the Boston<br />
University School of Public Health. ECHO implements<br />
and coordinates the multisite evaluation of the initiative,<br />
gathers data, and shares lessons learned across the<br />
Page 56 of 72<br />
15 demonstration sites. In addition, it coordinates the<br />
provision of technical assistance through presentations<br />
and trainings by leading experts in HIV oral health care.<br />
ECHO also coordinates semi-annual grantee meetings<br />
to bring grantees together to share their experiences<br />
and lessons from the field, and learn from each other’s<br />
experience in delivering oral health care and evaluating<br />
their service models. (For more information about ECHO,<br />
visit www.hdwg.org/echo/.)<br />
Transporting Clients, Transporting Care<br />
Ann Ferguson is a nurse at the AIDS Care Group in<br />
Chester, Pennsylvania, a SPNS Oral Health Care Initiative<br />
grantee.“Part of the problem for our patients,” she says,<br />
“is the barriers imposed by providers and the general<br />
fear and anxiety associated with dental care.” She points<br />
out other issues too, such as the need for ancillary services.<br />
“We are impressed on a weekly basis by the transportation<br />
needs associated with this program,” says<br />
Ferguson. The AIDS Care Group utilizes a van with a<br />
Global Positioning System (GPS). “It has already logged<br />
20,000 miles on this grant alone.”<br />
Cindee Shapiro echoes the need for transportation<br />
among her clients. Shapiro is vice president of the AIDS<br />
Resource Center of Wisconsin (ARCW) in Green Bay,<br />
another SPNS Oral Health Care Initiative site. About 60<br />
percent of ARCW clients require transportation assistance.<br />
Shapiro says that providing this assistance has<br />
raised clients’ awareness of ARCW’s other services. For<br />
example, she says,“ARCW is experiencing a doubling of<br />
food disbursed through its Green Bay food pantry since<br />
the dental clinic initiated services in April 2007.”<br />
The HIV Alliance of Lane County in Eugene, Oregon,<br />
expected to transport clients all over its 63,000 squaremile<br />
service area when it wrote its SPNS Oral Health Care<br />
Initiative grant application.“We had thought one shuttle<br />
would be fine,” says Dental Program Coordinator<br />
Amanda McCluskey,“but that has not been the case.”<br />
Instead, the HIV Alliance is finding that opening<br />
satellite clinics “is a great way to build capacity and get<br />
involvement in our clinics,” says McCluskey. One satellite<br />
clinic has opened so far; three more are expected to<br />
open this spring, and another two or three over the summer.<br />
The clinics offer cleaning and preventive care from<br />
hygienists, and dentists perform services ranging from<br />
extractions to denture work.<br />
“Partnerships have been the key to the project’s<br />
success,”says McCluskey.“We are partnering with dental<br />
hygiene programs, federally qualified health centers,<br />
community health departments using spaces that<br />
5
already exist,” she explains. “So we are replicating our<br />
model across the State to give clients greater access.”<br />
Taking It to the Streets<br />
Hurricane Katrina devastated the dental school at<br />
Louisiana State University (LSU) in <strong>New</strong> Orleans and<br />
damaged half of all the dental practices in Orleans<br />
Parish. Charity Hospital, which had a large, 28-chair<br />
dental clinic, was lost.<br />
Dental services for city residents after the hurricane<br />
were set up in a military tent in a parking lot with a<br />
single dental chair, recalls Janet Leigh, chair of oral<br />
medicine and radiology at the LSU School of Dentistry<br />
and principal investigator for the Oral Health Initiative<br />
project called “Smile Again, <strong>New</strong> Orleans!” The services<br />
were then moved to the city’s convention center to<br />
allow for increased space. The program moved again,<br />
this time to a vacant department store building, before a<br />
final move to its current location in the Medical Center<br />
of Louisiana at <strong>New</strong> Orleans.<br />
The SPNS grant has provided Leigh’s program with a<br />
mobile unit that can be moved around to areas with<br />
potential patients but no public transportation services.<br />
The project believed the van’s dental services would<br />
attract people already infected with HIV and others at<br />
risk who were unlikely to have been tested or have<br />
accessed care even before the storm.<br />
Sure enough, “The van has helped channel HIV<br />
patients into the medical care they need,” says Leigh. It<br />
also has helped rebuild the HIV outpatient oral health<br />
clinic from three to five chairs. The project has partnered<br />
with Covenant House, a shelter for runaway and troubled<br />
youth; St. Anna’s Episcopal Church, an African<br />
American parish that regularly offers HIV testing; LSU<br />
Behavior Science, an inpatient psychiatric and addiction<br />
program; the Louisiana Office of Public Health; and the<br />
<strong>New</strong> Orleans AIDS Task Force. These partnerships<br />
demonstrate the repeated success <strong>HRSA</strong>-funded programs<br />
have had in maximizing limited resources<br />
through relationships and referral systems with community<br />
based organizations.<br />
Partnering for Lasting Results<br />
The UMDNJ began providing oral health care services to<br />
PLWHA in 1989, and its oral health care services for<br />
PLWHA have been supported by the Ryan White<br />
HIV/AIDS Program for years. Jill York, director of the<br />
UMDNJ’s Special <strong>Service</strong>s Dental Unit, says that the unit<br />
served 616 unduplicated oral health care patients in<br />
2007, accounting for 2,634 patient visits. This success<br />
6<br />
Page 57 of 72<br />
was achieved through a partnership with Access One, an<br />
AIDS service organization serving three counties.<br />
York says that the partnership helps fulfill UMDNJ’s<br />
goal of improving both access to care and primary<br />
health care for PLWHA. At the most fundamental level,<br />
the partnership is successful because it works for all the<br />
players: It creates access to patients for UMDNJ’s Special<br />
<strong>Service</strong>s Dental Unit, and it helps Access One serve its<br />
clients.<br />
The partnership also provides opportunities to train<br />
dental students and medical students, who do a rotation<br />
through the unit’s clinical sites. York is hoping to develop<br />
a national model for oral health care in Ryan White<br />
programs within 5 years and is now conducting followup<br />
interviews with former students to see how they<br />
have implemented what they learned in the program.<br />
“We had a great chance to inspire them,”she says,“so we<br />
want to see how many people are serving the underserved,<br />
particularly HIV patients.”<br />
More than one-half of all the HIV patients seen at<br />
UMDNJ are between 45 and 64 years old. 42 The high percentage<br />
of older PLWHA served in the program demonstrates<br />
how aging with HIV is changing the landscape<br />
not only of primary care but also of dental care.<br />
Partnerships like those spearheaded by the UMDNJ<br />
Special <strong>Service</strong>s Unit are occurring across the country. A<br />
longtime collaboration between the University of<br />
Louisville’s Community-Based Dental Partnership<br />
Program and Ryan White-supported physicians and<br />
social service care coordinators has been the foundation<br />
of its excellent patient care and educational opportunities<br />
for dental students, according to Program Director<br />
Theresa Mayfield. The oral health portion of the program’s<br />
Ryan White grant supports its collaboration with<br />
two clinics—one urban and the other rural. “We have<br />
taught the staff of these clinics, and they have embraced<br />
the need for their clients to receive oral health care,”says<br />
Mayfield. “It is just as important for them to coordinate<br />
for those services as for housing and other services.”<br />
The embrace has been mutual, because medical<br />
providers have realized the value of coordinating their<br />
services with the social service providers. “It takes the<br />
joint effort of medical providers and people doing social<br />
services to make it seamless,” says Mayfield. “You can’t<br />
do it if you don’t have everybody onboard.”<br />
The WINGS Clinic, a Ryan White-supported outpatient<br />
medical clinic for PLWHA at the University of<br />
Louisville, is not just a close partner of the university’s<br />
dental program—it is just down the hallway in the same<br />
building. “Proximity at the school has been mutually
eneficial,” says Clinic Program Director Deborah Wade.<br />
“It has meant that if WINGS Clinic patients have dental<br />
emergencies, or are in pain, we can just walk them right<br />
next door,” adds Wade. “The beauty of that is we have<br />
their records and can tell the dentist their CD4 count,<br />
viral load, whether they’ve been adherent to their medications,<br />
and any background information they might<br />
need as they deliver oral health care.”<br />
Likewise, Wade says the dentists “have trained all our<br />
medical providers on how to do a visual screen at a<br />
medical appointment.” As a result, a medical patient in<br />
the WINGS Clinic who might be experiencing a dental<br />
issue can get an initial assessment in the medical clinic.<br />
It provides a seamless approach to then refer the patient<br />
for dental care. “Now we are pretty much set on autopilot,”<br />
says Wade. “We have all our medical providers do<br />
oral screens as a routine part of each medical visit.”<br />
This collaboration of the WINGS Clinic and the Ryan<br />
White oral health programs has helped educate both<br />
PLWHA and medical providers about the connection<br />
between oral health and general health. “Now we are all<br />
speaking the same language and can communicate better<br />
about patients’ oral health care needs,” says Wade.<br />
Page 58 of 72<br />
The Miami Dental Access Program (MDAP) and Louisiana’s “Smile Again, <strong>New</strong> Orleans!” are two Oral Health Initiative projects using<br />
a mobile van to expand HIV/AIDS dental care into urban communities. MDAP’s Henry Boza is shown above with a prospective client.<br />
At Matthew 25 AIDS <strong>Service</strong>s in Henderson, Kentucky,<br />
Cyndee Burton, the nurse-administrator and cofounder,<br />
says the partnership with the University of<br />
Louisville dental school “has been a Godsend for us.”The<br />
agency has been able to use the relatively small amount<br />
of dental care funding it had before to provide transportation<br />
for dental clients, taking them to either<br />
Louisville or nearby Elizabethtown, Kentucky, for the<br />
specialized care they cannot receive in Henderson.<br />
Clients who receive regular dental care have been<br />
transformed by these important services. In a State<br />
where more than 40 percent of the adult population<br />
experience the loss of more than 5 teeth, receiving<br />
dental care can literally be life changing. 43<br />
“We have one guy who, when he first came in, would<br />
hang his head because his teeth were so bad,” recalls<br />
Burton. “He was a meth user and had gone through<br />
treatment and gotten out. He immediately started volunteering<br />
at our clinic, but I noticed he always did things<br />
in the background. You could never get him to smile.”<br />
That all changed when the patient was referred to the<br />
dental clinic.“He now has the most beautiful teeth, and<br />
he is also one of our leading volunteers,” she marveled.<br />
7
8<br />
REFERENCES<br />
1 U.S. Department of Health and Human <strong>Service</strong>s (HHS). Oral health in<br />
America: A report of the Surgeon General. Rockville, MD: U.S.<br />
Department of Health and Human <strong>Service</strong>s, National Institute of<br />
Dental and Craniofacial Research, National Institutes of Health, 2000.<br />
2 Agency for Healthcare Research and Quality (AHRQ). Dental<br />
problems go unresolved in many HIV patients. April 6, 2001. Rockville,<br />
MD: AHRQ. Available at: www.ahrq.gov/news/press/pr 2001/<br />
dentalhivpr.htm. Accessed April 7, 2008.<br />
3 Centers for Disease Control and Prevention (CDC). Public health &<br />
aging: Retention of natural teeth among older adults—United States,<br />
2002. MMWR. 2003;52:1226-9. Available at: www.cdc.gov/mmwr/<br />
preview/mmwrhtml/mm5250a3.htm. Accessed April 4, 2008.<br />
4 Project Inform. Dealing with drug side effects: Dry mouth. 2008.<br />
Available at: www.projinf.org/info/sideeffects/11.shtml. Accessed<br />
April 6, 2008.<br />
5 Abel S, Reznick D. <strong>New</strong> York/<strong>New</strong> Jersey AETC and Southeast AETC.<br />
Current trends in HIV oral health care. Unpublished presentation to<br />
staff of Health Resources and <strong>Service</strong>s Administration, HIV/AIDS<br />
Bureau, March 28, 2007.<br />
6 Public Broadcasting <strong>Service</strong> (PBS). Frontline: the meth epidemic: How<br />
meth destroys the body. 2006. Available at: www.pbs.org/<br />
wgbh/pages/frontline/meth/body/. Accessed April 6, 2008.<br />
7 Epstein JB. Oral malignancies associated with HIV. J Can Dent Assoc.<br />
2007;73:953-6. Available at: www.cda-adc.ca/jcda/vol-73/issue-10/<br />
953.pdf. Accessed April 9, 2008.<br />
8 Gennaro S, Naidoo S, Berthold P. Oral health and HIV/AIDS. MCN<br />
Am J Matern Child Nurs. 2008;33:50-7.<br />
9 School of Dentistry, Louisiana State University Health Sciences<br />
Center. HIV+ Outpatient Clinic: Overview. 2007. Available at:<br />
www.lsusd.lsuhsc.edu/patient/hiv_clinic1.htm. Accessed April 9,<br />
2008.<br />
10 Abel & Reznick, 2007.<br />
11 Abel & Reznick, 2007.<br />
12 Fischler MS. A tooth fairy’s gift: freedom from fear. <strong>New</strong> York Times.<br />
June 16, 2002. Available at: http://query.nytimes.com/gst/fullpage.<br />
html?res=9A00E7DE173CF935A25755C0A9649C8B63&sec=&spon=<br />
&pagewanted=all/. Accessed April 11, 2008. http://jada.ada.org/cgi/<br />
content/abstract/118/5/591<br />
13 TARGET Center, <strong>HRSA</strong>, HAB. Ryan White National TA call: Oral<br />
health and HIV. Call summary and Transcript. October 25, 2007.<br />
14 CDC, 2002.<br />
15 HHS, 2000.<br />
16 McGrath C, Chan B. Oral health sensations associated with illicit<br />
drug use. Brit Dent J. 2005;198:159-62.<br />
17 PBS, 2006.<br />
18 McGrath & Chan, 2005.<br />
19 PBS, 2006.<br />
20 National Institute of Dental and Craniofacial Research (NIDCR).<br />
Mouth problems and HIV. 2007. Available at: www.nidcr.nih.gov/<br />
NR/rdonlyres/D8E70B65-6F27-46BC-8043-30C309508B5F/0/<br />
Page 59 of 72<br />
MouthProblemsAndHIV.pdf. Accessed April 6, 2008.<br />
21 Gennaro et al., 2008.<br />
22 NIDCR, 2007.<br />
23 Renvert S, Pettersson T, Ohlsson O, Persson GR. Periodontal<br />
bacteria linked to heart disease. J Periodontology. 2006;77:1110-9.<br />
Available at: www.joponline.org/doi/abs/10.1902/jop.2006.050336 .<br />
Accessed April 11, 2008.<br />
24 Project Inform. Dealing with drug side effects: Dry mouth. 2008.<br />
Available at: www.projinf.org/info/sideeffects/11.shtml. Accessed<br />
April 6, 2008.<br />
25CNN. Oral thrush. August 20, 2007. Available at: www.cnn.com/<br />
HEALTH/library/DS/00408.html. Accessed April 7, 2008.<br />
26 Abel & Reznick, 2007.<br />
27 Brosky ME. The role of saliva in oral health: strategies for prevention<br />
and management of xerostomia. J Supportive Oncol.2007;<br />
5:215-25. Available at: http://www.oralcancerfoundation.org/dental/<br />
pdf/mgmnt_of_xerostomia.pdf. Accessed April 11, 2008.<br />
28 NIDCR, 2007.<br />
29 Kerawala C. Oral cancer, smoking and alcohol: A patient’s perspective.<br />
Brit J Oral Maxillofacial Surg. 1999; 37:374-76.<br />
30 NIDCR, 2007.<br />
31 U.S. National Library of Medicine, National Institutes of Health<br />
(NLM). Health topics: Dental cavities. March 18, 2008. Available at:<br />
www.nlm.nih.gov/medlineplus/ency/article/001055.htm. Accessed<br />
April 7, 2008.<br />
32 NIDCR, 2007.<br />
33 Cheah PL, Looi LM. Biology and pathological associations of the<br />
human papillomaviruses: a review. Malays J Pathol. 1998;20:1-10.<br />
34 Southeast AIDS Training and Education Center, Emory University<br />
School of Medicine. Linear gingival erythema. In Clinical management<br />
of the HIV-infected adult. Available at: www.seatec.emory.edu/<br />
clinicalprotocols/chpt5/LinearGingivalErythema.htm. Accessed April<br />
4, 2008.<br />
35 NLM. Health topics: Kaposi’s sarcoma. March 31, 2008. Available at:<br />
www.nlm.nih.gov/medlineplus/kaposissarcoma.html. Accessed<br />
April 6, 2008.<br />
36 NLM. Health topics: Gum disease. March 14, 2008. Available at:<br />
www.nlm.nih.gov/medlineplus/gumdisease.html. Accessed April 6,<br />
2008.<br />
37 NIDCR, 2007.<br />
38 NIDCR, 2007.<br />
39 NLM, March 14, 2008.<br />
40 HIV/AIDS Bureau (HAB). Health Resources and <strong>Service</strong>s Administration.<br />
Ryan White HIV/AIDS Treatment Modernization Act: Dental programs.<br />
n.d. Available at: http://hab.hrsa.gov/<br />
treatmentmodernization/dental.htm. Accessed April 9, 2008.<br />
41 HAB, n.d.<br />
42 University of Medicine and Dentistry of <strong>New</strong> Jersey. Ryan White<br />
HIV/AIDS data report. 2006. Unpublished data.<br />
43 CDC, 2002.
y David Evans<br />
Mouth Full of Problems: A Crisis in HIV Dental Care<br />
AIDSmeds September 8, 2009<br />
Too few people with HIV get the routine oral health care they need to stay healthy. The teetering economy, experts<br />
say, might make the situation a whole lot worse.<br />
Not accessing dental care can be deadly. In early 2007, a 12-year-old boy named Deamonte Driver from suburban<br />
Washington, DC, died of an infection that had spread from an abscess in his mouth to his brain. His family’s<br />
Medicaid had lapsed because of a technicality, so he didn’t get care until his mother took the by then very ill boy<br />
into an emergency room. Experts say an $80 tooth extraction, if done early enough, could have saved his life.<br />
Though Driver’s HIV-status was never reported, and there hasn’t been wide press coverage of a similar story<br />
involving an openly HIV-positive person, David Reznick, DDS, head of the HIV Dental Alliance in Atlanta, says<br />
that all the necessary ingredients to create such a tragedy are already in place—and could be getting worse.<br />
People with HIV are simultaneously more likely than their HIV-negative counterparts to have more frequent and<br />
more serious oral health issues, while being less likely to have the funds and insurance to cover necessary<br />
procedures. The public support that is available for providing clinical oral health care to people with HIV, Reznick<br />
says, is drying up as various states confront catastrophic budget crises. “We’re just not seeing enough [funding]<br />
increases to take care of the people we already serve,” Reznick laments, “So it’s an overwhelming need and no<br />
resources to pay for it.”<br />
Open Wide<br />
Page 60 of 72<br />
People rarely think—at least until their face is horribly swollen and they’re immobilized with pain—that oral health<br />
care can have much of an impact on their overall well-being. According to Reznick, however, a neglected mouth<br />
can lead to more than localized tooth pain: Tooth and gum infections can spread to other parts of the body, and<br />
mouth pain can cause people to go without necessary nutrition—and even cause them to forgo their HIV<br />
medications.<br />
“If you’re in an extraordinary amount of pain, you’re not going to be able to take your medications,” he explains. “If<br />
you don’t have any teeth to chew with, how are you going to get the nutrition you need to stay healthy?”<br />
Reznick also has concerns about chronic inflammation from untreated periodontal disease. A growing number of<br />
studies are illuminating the role of inflammation in a variety of non-AIDS-related health problems such as<br />
cardiovascular disease. The link between gum and heart disease has been proposed in HIV-negative people, and<br />
some evidence suggests it to be true.<br />
For all of these reasons, preventive dental care can have a tremendous influence on a person’s overall well-being.<br />
Unfortunately, many people with HIV don’t know or understand the importance of regular preventive dental care.<br />
According to the Health Resources and <strong>Service</strong>s Administration (<strong>HRSA</strong>), people with HIV who are uninsured are
three times as likely to have untreated dental needs as people with HIV who have insurance. <strong>HRSA</strong> also states,<br />
“Moreover, oral infections, mouth ulcers and other severe dental conditions associated with HIV infections go<br />
untreated more than twice as often as other health problems related to the disease.”<br />
Roadblocks to Care<br />
Reznick says that HIV stigma and cultural habits against seeking dental care are two big reasons that people fail to<br />
go to the dentist regularly even when they have coverage or access to a dentist through public or private benefits.<br />
But even among people who want to go to a dentist as often as is recommended—at least once every six months for<br />
a thorough cleaning and checkup—lack of insurance or comprehensive public benefits can mean going without.<br />
Given the severe budget woes of most states right now, publicly funded dental care is not expanding sufficiently to<br />
meet the growing epidemic. In fact, in many areas it is shrinking.<br />
In most cities and towns, the only options for people without dental insurance are oral care programs covered by the<br />
Ryan White CARE Act or Medicaid. Ryan White, however, has been essentially flat-funded for several years, and<br />
Medicaid dental coverage, already stingy in many states, is beginning to disappear. “Without the Ryan White<br />
dollars, there’s minimal access,” Reznick says. “With states that had adult benefits through Medicaid who have lost<br />
them, it’s caused a gigantic crunch.”<br />
“We’re struggling to keep up with the need,” Reznick explains, “because people are living longer, and more people<br />
are getting tested and entering into the system of care. So we’re literally booked through until November, and I have<br />
eight dental chairs and over three full-time dentists and three hygienists, and we’re having a very difficult time<br />
meeting the need.”<br />
Reznick hopes that policymakers and people living with HIV understand the consequences of too-little access to<br />
good oral health care. Aside from the pain and illness it will almost certainly cause, Reznick contends, it will also<br />
end up costing more money in the long run. He is hoping for increases, rather than additional cuts, to services.<br />
When people don’t get preventive care, Reznick says, “they end up in the emergency department, and that’s going<br />
to cost the public a whole lot more than if they would have kept the benefits in place.”<br />
© Copyright 1996 - 2009 HIVdent.org. All Rights Reserved.�<br />
Page 61 of 72
Increasing Access to Oral Health Care for People Living with HIV/AIDS:<br />
The role of dental case managers, patient navigators and outreach<br />
workers<br />
By Carol Tobias, MMHS; Tim Martinez, DDS; Helene Bednarsh, BS, RDH, MPH;<br />
Jane E. Fox, MPH<br />
While it is common<br />
to find HIV case<br />
managers working<br />
in medical settings<br />
or social service<br />
organizations, the<br />
concept of dental<br />
case management<br />
is relatively new.<br />
Introduction<br />
In 2006 the HIV/AIDS Bureau of the Health Resources and <strong>Service</strong>s<br />
Administration (<strong>HRSA</strong>) funded the Innovations in Oral Health Care<br />
Initiative as a Special Project of National Significance (SPNS). The goal of<br />
this five-year initiative is to expand access to oral health care for HIV-positive<br />
underserved populations in both urban and rural areas across the country.<br />
Nine of the fifteen demonstration sites included in this initiative employ a<br />
dental case manager, patient navigator or outreach worker as part of their<br />
program model.<br />
Case management has been part of the continuum of HIV care in the US<br />
since the early days of the epidemic and was mandated as a service by the<br />
Ryan White CARE Act of 1990 to ensure service coordination and continuity<br />
(Fleishman, 1998). Although there is some variation in the key functions<br />
of case managers across case management programs, the Centers for Disease<br />
Control and Prevention (1997) have identified six core tasks that form the<br />
basis of most of HIV case management programs. These core tasks include:<br />
1.<br />
2.<br />
3.<br />
4.<br />
5.<br />
6.<br />
Client identification, outreach, and engagement;<br />
Medical and psychosocial assessment of need;<br />
Development of a service plan or care plan;<br />
Implementation of the care plan by linking with service delivery systems;<br />
Monitoring of service delivery and reassessment of needs; and<br />
Advocacy on behalf of the client (including creating, obtaining, or<br />
brokering needed client resources).<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
Page 62 of 72<br />
1
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
While it is common to find HIV case managers working in medical settings<br />
(medical case management) or social service organizations (psychosocial case<br />
management), the concept of dental case management is relatively new. Most<br />
of the programs that use dental case managers or related personnel such as<br />
patient navigators or outreach workers [hereafter all referred to as dental<br />
case managers unless otherwise noted] as part of the SPNS initiative do so,<br />
in large part, to increase access to and retention in oral health care. This<br />
report describes the emerging concept of dental case management and how<br />
it is implemented in community settings to expand access to oral health care.<br />
Sections include:<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
•<br />
Methods<br />
Methods<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
The importance of oral health care for people living with HIV<br />
Barriers to care for people living with HIV<br />
The role of dental case managers<br />
How dental case managers improve access to care<br />
How dental case managers are different from HIV case managers<br />
How the dental case manager role can be incorporated into other<br />
practices<br />
In June 2008 the Evaluation Center for HIV Oral Health (ECHO), the<br />
multi-site evaluation and technical support center for the SPNS Oral Health<br />
Initiative, convened a focus group with demonstration site staff who function<br />
as dental case managers to learn more about their roles. Nine individuals<br />
participated in the focus group, six of whom had a formal title or role as a<br />
dental case manager, patient navigator or outreach worker. The other three<br />
individuals, two of whom were research assistants and one of whom was<br />
a research hygienist, participated in the focus group because some of their<br />
functions overlapped with the case managers or outreach workers.<br />
The six core participants worked at three large urban sites (two in San<br />
Francisco and one in <strong>New</strong> York) and three rural sites (Eugene, OR; East<br />
Texas; and Green Bay, WI). We also received written materials from three<br />
additional case managers who work in rural locations (Chester, PA; Cape<br />
Cod, MA; and Middletown, CT).<br />
Page 63 of 72<br />
2
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
Dental case<br />
managers are<br />
critical in helping<br />
patients overcome<br />
the fear, stigma<br />
and other barriers<br />
that inhibit patient<br />
access to oral<br />
health care.<br />
The importance of oral health care for people living with HIV<br />
While good oral health habits are important for all people, they have<br />
particular significance for people living with HIV. Many of the first signs<br />
of HIV infection may occur as oral manifestations that can be identified<br />
during a routine oral examination by a dentist or hygienist. A review of the<br />
patient’s medical history and risk assessment in conjunction with an oral<br />
lesion may prompt the dental team to refer the patient to an HIV testing site<br />
or a medical provider for a comprehensive work-up. This referral is especially<br />
important for patients who do not know their HIV status.<br />
On the other hand, if a person is aware of their HIV status and oral<br />
manifestations are present, this could indicate a change in the immune<br />
system or a failure of the current drug regimen. People may find that treatable<br />
conditions such as gingivitis or early periodontitis can become serious quickly<br />
if the immune system is weak. In addition, medications prescribed to treat<br />
HIV can cause a reduced salivary flow and lead to dry mouth or xerostomia.<br />
Without adequate saliva, which contains protective enzymes, cavities or other<br />
infections may occur. If not treated, oral health complications can make<br />
it difficult to chew or swallow, which in turn can impact nutritional status<br />
or the ability to take HIV medications (Cherry-Peppers, 2003) . This close<br />
and interdependent relationship between physical health and oral health<br />
is reflected in the Presidential Advisory Council on HIV/AIDS report on<br />
Achieving an HIV-Free Generation: Recommendations for a <strong>New</strong> American<br />
HIV Strategy, which recommends that “Oral health be part of core services<br />
available under the Ryan White CARE Act” (DHHS, 2005).<br />
Barriers to care for people living with HIV<br />
Access to oral health care is problematic for many Americans, especially those<br />
living with HIV. With nearly half of all expenditures for dental care coming<br />
straight out of peoples’ pockets (Badner, 2005), and most of the HIV-positive<br />
clients served by Ryan White programs living close to or below the poverty<br />
level, the presence or absence of dental insurance has a major impact on access<br />
to care. For most low-income individuals, the only source of dental insurance<br />
is the Medicaid program; yet only 60% of people who receive Medicaid<br />
benefits live in states that cover adult dental care (Freed, 2005). Even with<br />
Medicaid dental benefits, people often have difficulty finding dentists that<br />
will accept Medicaid payment, and Medicaid dental benefits vary from state<br />
to state.<br />
In addition to the financial issues, people living with HIV face a host of other<br />
barriers to care, including provider shortages (particularly in rural areas),<br />
unwillingness to treat, other competing needs, stigma, discrimination, or<br />
fear of going to the dentist. Unmet needs for oral health care among people<br />
living with HIV are substantially higher than the unmet oral health needs<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
Page 64 of 72<br />
3
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
Dental case<br />
managers are able<br />
to address barriers<br />
to oral health care<br />
in a way that other<br />
HIV-care providers<br />
cannot.<br />
in the general population (Marcus, 2000), and higher than unmet needs for<br />
medical care (Heslin, 2001). Racial and gender disparities also play a role in<br />
access to care, as African Americans, Hispanics, and women are less likely to<br />
receive dental care than other people living with HIV (Dobalian, 2003). This<br />
underscores the importance of developing interventions that address both<br />
the structural and the personal/cultural barriers to oral health care for people<br />
living with HIV.<br />
Another significant barrier to care is the overall lack of awareness about the<br />
importance of regular dental care and the relationship between oral health<br />
and physical health for people living with HIV. This is not just a barrier for<br />
individual patients, who may have never received routine dental care, it is also<br />
a barrier for health care providers and HIV case managers who do not fully<br />
understand the role of oral health in the continuum of HIV care. Thus, HIV<br />
case managers may not include dental care on their screening instruments or<br />
make routine referrals to dental care, or doctors and nurses may not think to<br />
ask patients about their use of dental services.<br />
In the context of the SPNS Oral Health Initiative, where financial barriers<br />
to care were addressed through grant funding, dental case managers play an<br />
important role in addressing many of the other barriers to oral health care.<br />
The role of dental case managers<br />
Nine of the fifteen oral health demonstration programs employ staff as<br />
dental case managers (6), patient navigators (2) or outreach workers (1). In<br />
practice, many of the functions of these staff overlap. For example, all staff,<br />
regardless of title, play an important role in client recruitment, appointment<br />
scheduling and making sure clients have a way to get to the appointment. In<br />
addition, all staff provide some level of patient education about the nature of<br />
the care they will receive, and are instrumental in following up any missed<br />
appointments. Another common function is coordination with (and referral<br />
to, if necessary) other services such as HIV case management, medical care,<br />
or support services. Finally, all of the dental case managers are part of a<br />
team that helps educate other providers in the continuum of HIV care on<br />
the importance of oral health care and how to refer their patients to dental<br />
services. While the above-mentioned functions are common across programs,<br />
both their methods of implementation and other functions may be unique to<br />
a particular patient population or differ based on the location of the program.<br />
Each dental case manager activity is described below with the results from the<br />
focus group used to illuminate the range of activities.<br />
Patient recruitment. A key case management activity is to encourage<br />
patients to come in to receive oral health care. Dental case managers are<br />
critical in helping patients overcome the fear, stigma and other barriers<br />
that inhibit patient access to oral health care. The work involved in patient<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
Page 65 of 72<br />
4
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
I…mostly give them support<br />
to try to come to the [dentist]<br />
appointments. Once they get<br />
over that fear, they start going<br />
in on their own. ….we kind of<br />
team up to see …-do they need<br />
an escort or do they need more<br />
appointment reminders? Do<br />
they have a phone…? One of the<br />
things we are running into is the<br />
….fear of pain.<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
recruitment and appointment scheduling varies greatly across sites.<br />
Most of the dental case managers receive new patients through<br />
referrals from other health or social service providers; the patient has<br />
already decided to seek dental care. Thus, the recruitment work is<br />
actually conducted by building and maintaining relationships with<br />
referral providers rather than with patients directly. However, in two<br />
urban sites that employ patient navigators or outreach workers, these<br />
staff are more directly involved with patient recruitment, actually<br />
doing the work of talking patients into coming to see the dentist,<br />
helping to allay their fears, and offering to accompany new patients<br />
on their first visit to the dentist. In both of these circumstances, the<br />
patient navigator and outreach worker are connected to large HIV<br />
service organizations with a reasonably accessible patient population<br />
that is not already receiving dental care.<br />
I…mostly give them support to try to come to the [dentist] appointments.<br />
Once they get over that fear, they start going in on their<br />
own. ….we kind of team up to see …-do they need an escort or do<br />
they need more appointment reminders? Do they have a phone…?<br />
One of the things we are running into is the ….fear of pain.<br />
Transportation and scheduling. Dental case managers who work<br />
in rural communities that provide services over a broad geographic<br />
area spend much more time arranging or coordinating transportation<br />
for their patients than those who work in urban programs. Some<br />
programs offer gas cards as an incentive for patients to come in for<br />
care, while others use a van to pick patients up and bring them in<br />
to the clinic. Still other programs help arrange car-pools, or try to<br />
arrange Medicaid-financed transportation. With patients coming<br />
to the dental clinic from far distances, the dental case managers also<br />
face scheduling challenges. They may need to schedule a patient<br />
for a large number of procedures on a single day, or they may need<br />
to coordinate the dental visit with a same-day appointment for<br />
medical care and/or HIV case management services. There are some<br />
circumstances in which a patient may need to be scheduled for an<br />
appointment in the afternoon and a subsequent appointment the<br />
following morning. This type of situation requires additional effort<br />
by the case manager to locate and/or book lodging accommodations<br />
for the patient.<br />
….we have a lot of people….with no driver’s license…. in rural<br />
areas it is needed because we don’t have a massive transportation<br />
system here…..One of the other things we are doing….is….setting<br />
up satellite clinics around the state because it’s not practical for us<br />
to drive three hours to pick somebody up for a dental appointment.<br />
Page 66 of 72<br />
5
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
I accompany patients to the<br />
dentist office if they want me to.<br />
That means going in with them<br />
and explaining exactly what<br />
is going down….and why the<br />
dentist is doing that….because<br />
at times the patient doesn’t like<br />
to ask the dentist…..[they feel]<br />
more comfortable with asking me<br />
questions which I love to answer.<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
Visit accompaniment. Two of the urban programs are more likely<br />
to serve immigrant populations that have limited experience with<br />
dental care. These programs offer visit accompaniment services<br />
to help ensure that patients attend their appointments or follow<br />
through on a referral to dental specialty services. A third urban<br />
program serves a population that is largely homeless, many of<br />
whom have mental health or addiction co-morbidities; this<br />
program also offers visit accompaniment services to help get their<br />
new patients in the door for care.<br />
I accompany patients to the dentist office if they want me to.<br />
That means going in with them and explaining exactly what<br />
is going down….and why the dentist is doing that….because<br />
at times the patient doesn’t like to ask the dentist…..[they feel]<br />
more comfortable with asking me questions which I love to<br />
answer.<br />
Visit explanations. Both urban and rural program staff spend<br />
a significant amount of time, particularly with new patients,<br />
explaining what they should expect when they come in for a visit.<br />
This explanation serves several purposes. First, it helps to ease<br />
people’s minds if they are worried about the visit, and it may also<br />
reassure them that the providers they will see are comfortable<br />
treating people with HIV. Second, when the patient arrives for the<br />
appointment, the dental case manager can introduce her/himself<br />
as someone the patient has already spoken with on the phone.<br />
When I used to work in the front office I dealt with a lot of<br />
patient finances and translating for patients. So when it came to<br />
translating for Spanish speaking patients I was already explaining<br />
the treatment plans because the dentist wasn’t able to do<br />
that. So having the patient relationship beforehand…helped<br />
me a lot because I built trust with a lot of patients whether they<br />
were HIV positive or not.<br />
Referrals and translation. Other functions of the dental case<br />
managers at the point of entry into care include enrollment in<br />
benefits, particularly dental benefits if these are available, referrals<br />
to other services, and, in some cases, translation.<br />
Retention services. Retention in dental care begins at the first<br />
visit when the case manager works to build a relationship with<br />
the patient and explains what to expect during the visit. This<br />
relationship is key to patient retention, as the dental case managers<br />
Page 67 of 72<br />
6
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
We have seen within a few<br />
months, when they get teeth,<br />
when they get the partials, they<br />
are able to eat better and they<br />
start gaining weight….<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
check in with patients following their appointments: “How did it<br />
go?” “Do you have the supplies you need?” “Do you want me to<br />
go over what is happening next?” “How are you feeling now?” All<br />
of the case managers provide appointment reminders just prior to<br />
the next appointment, and all follow up with any individual who<br />
misses an appointment. In the typical dental setting, if a patient<br />
fails to show up for an appointment, nothing is done to follow up<br />
to find out why. Instead, the patient’s name is likely to go onto a<br />
no-show list, and if it appears more than two or three times, the<br />
patient may be told to go elsewhere for care. Several of the SPNS<br />
oral health programs with high patient caseloads also had no-show<br />
policies, but they also used missed appointment follow-up as an<br />
opportunity to educate patients about the wait for services and<br />
how advance notice of a missed appointment helps the dental<br />
office accommodate other patients. In addition, most programs<br />
are willing to accommodate patients as walk-ins if they are unable<br />
to keep appointments.<br />
Patient education. All of the case managers provide some level<br />
of oral health education, but the level of education depends on<br />
the clinical background of the staff. Most can explain how HIV<br />
affects the mouth, and things to watch for, as well as basic oral<br />
hygiene techniques. Two of the case managers/navigators are<br />
dental assistants by training, and they are able to provide more<br />
comprehensive education about specific dental procedures and<br />
follow-up care. All of the non-clinical case managers expressed<br />
an interest in receiving more oral health education themselves in<br />
order to share information with their patients. In contrast, the<br />
case managers who are dental assistants by training expressed an<br />
interest in learning more about specific case-management skills.<br />
“Many…..don’t know how to brush their teeth; don’t know that<br />
you need to floss. We have a patient [whose] front teeth were<br />
perfect but behind the teeth was terrible because they learned<br />
that you only brush from one side. So education, education …it<br />
makes a difference cost-wise also.”<br />
Collaboration with HIV case managers. Another way in which<br />
dental case managers improve access to care is through their<br />
collaboration with HIV case managers and medical- and supportservice<br />
providers. Dental case managers can help keep oral health<br />
on the radar screens of other providers by providing resources<br />
and support materials, promoting oral health assessment as part of<br />
comprehensive case management, and training HIV case managers<br />
to advocate for oral health services for their clients.<br />
Page 68 of 72<br />
7
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
My best experience …..a lot of<br />
people haven’t had teeth for years<br />
or haven’t been able ….to smile<br />
for years. So the opportunity to<br />
have that experience is really big<br />
for a lot of people, and [it’s a<br />
relief to] just take care of pain….<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
Background and Qualifications. The formal qualifications for<br />
dental case manager positions vary across programs. Two of<br />
the case managers are trained dental assistants and most have<br />
a bachelor’s degree. However, several of the positions have no<br />
formal education requirements, but require state-specific HIV<br />
training and experience with case management or in human<br />
services. Most of the case managers have a minimum of five years<br />
experience working in HIV care settings or other human services<br />
such as drug treatment, homeless services or domestic violence<br />
shelters. Two of the positions require a valid driver’s license.<br />
How dental case managers improve access to care<br />
Dental case managers are able to address barriers to oral health<br />
care in a way that other HIV-care providers cannot. Most HIV<br />
case managers have a large patient caseload and a series of service<br />
areas to address, many of which may be more pressing than oral<br />
health care. Oral health often gets pushed to the bottom of the<br />
list, if it is on the list to begin with. Dental case managers enable<br />
HIV case managers to focus on other issues within a client’s<br />
service plan without sacrificing access to oral health care. They<br />
arrange transportation, coordinate appointments, provide patient<br />
education and assistance with follow-up care, and help make sure<br />
that people return for their appointments. These are activities that<br />
few HIV case managers can undertake. And in most busy dental<br />
clinics, dentists, hygienists and dental assistants do not have the<br />
time to do all of this either.<br />
“We have seen within a few months, when they get teeth, when<br />
they get the partials, they are able to eat better and they start<br />
gaining weight….”<br />
“My best experience …..a lot of people haven’t had teeth for years<br />
or haven’t been able ….to smile for years. So the opportunity to<br />
have that experience is really big for a lot of people, and [it’s a<br />
relief to] just take care of pain….”<br />
“The best experience is being able to treat those patients…that<br />
are coming from so far away and haven’t gone to a dentist in<br />
so many years because of…access, insurance ….it is really nice<br />
to have them come in and treat them and for them to feel good<br />
about themselves.”<br />
Page 69 of 72<br />
8
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
I got a job that is just awesome.<br />
You know you can give someone<br />
a set of dentures who hasn’t had<br />
any for ten years and has not had<br />
any teeth and…..they hug you.<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
“I got a job that is just awesome. You know you can give someone<br />
a set of dentures who hasn’t had any for ten years and has not<br />
had any teeth and…..they hug you.”<br />
How dental case managers are different from HIV case<br />
managers<br />
Unlike HIV case managers, dental case managers do not conduct<br />
comprehensive psychosocial or health assessments, nor do they<br />
develop, implement and monitor treatment plans. This is<br />
typically the work of the clinical members of the oral health team,<br />
the dentist and the hygienist. Thus, the work of an HIV case<br />
manager is much more comprehensive than the work of a dental<br />
case manager. HIV case managers have to address a broad range<br />
of issues, many of which are immediate needs for their patients<br />
and are not typically related to dental care. Dental case managers<br />
perform fewer tasks per patient and as a result can serve a higher<br />
volume of patients than an HIV case manager can. In addition,<br />
their education role is different – they focus mainly on dental care<br />
rather than on the broader spectrum of HIV care.<br />
In contrast, while an HIV case manager, under the best of<br />
circumstances, may make a referral to dental care, they are not<br />
able to follow up to make sure the patient gets the care he or she<br />
needs. This is something that the dental case manager can do<br />
– arrange the transportation, accompany patients to visits, and<br />
provide the one-to-one attention a patient needs. For dental case<br />
managers, dental care is at the top of the list rather than at the<br />
bottom; they make sure it is available and accessed.<br />
“…the regular HIV case managers have so many things to do.”<br />
How the dental case manager role can be incorporated into<br />
other practices<br />
Nearly all of the dental case managers involved in this<br />
demonstration wore multiple hats. For example, all played<br />
an important role in program evaluation, recruiting study<br />
participants, conducting patient surveys and entering data. Some<br />
of the staff also drove mobile vans, or functioned as receptionist/<br />
front desk staff. In addition, the outreach workers conducted<br />
outreach for other services and the dental assistants assisted with<br />
the dental care. Despite wearing these multiple hats, the case<br />
managers involved in the SPNS initiative served between 150 and<br />
300 patients, depending on the severity of patient needs and the<br />
Page 70 of 72<br />
9
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
You can affect the culture of<br />
care so that you can convince<br />
patients it’s really less costly and<br />
more beneficial if you go [to<br />
the dentist] when there aren’t<br />
problems, go routinely rather<br />
than wait until you are in pain.<br />
You have the time to do that<br />
[affect the culture of care] that a<br />
regular case manager would not<br />
have the time to do.<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
scope of their other duties. Thus, it is quite possible that some of<br />
the functions described above as dental case management could be<br />
incorporated into the roles of other dental clinic staff, especially<br />
receptionists, clinic coordinators, schedulers, translators or dental<br />
assistants.<br />
Within larger organizations, such as AIDS <strong>Service</strong> Organizations<br />
or HIV clinics that provide both medical and dental care, some<br />
of the functions described above could be picked up by HIV case<br />
managers if they are given the time to do this. In organizations<br />
that have multiple case managers, one case manager could be<br />
dedicated to oral health. Ryan White nurse case managers could<br />
be trained to provide basic oral hygiene education and include<br />
oral health as part of their clinical assessments.<br />
Ultimately, many of the tasks performed by dental case managers<br />
are non-reimbursable services and the position or functions<br />
must be funded from general revenue or grants. However, it can<br />
be argued that if the patient education, tracking and retention<br />
functions result in a reduced no-show rate, the position may<br />
pay for itself through additional visit revenue. In clinics where<br />
the dental case manager is a clinician, such as a dental hygienist,<br />
certain patient education services may be billable services. Clinic<br />
billing personnel can review all third party payer reimbursement<br />
codes to identify any codes that are associated with chair-side<br />
patient education as a possible source of revenue. Finally, a case<br />
can be made that the provision of oral hygiene education and early<br />
treatment for conditions such as periodontal disease reduces longterm<br />
costs for dental care. This is a strong argument for including<br />
access to and retention in care services in capitated oral health<br />
care programs where long-term cost savings can help finance<br />
the functions necessary to ensure the provision of early care and<br />
treatment.<br />
“….You can affect the culture of care so that you can convince<br />
patients it’s really less costly and more beneficial if you go [to the<br />
dentist] when there aren’t problems, go routinely rather than<br />
wait until you are in pain. You have the time to do that [affect<br />
the culture of care] that a regular case manager would not have<br />
the time to do.”<br />
Page 71 of 72<br />
10
Increasing Access to Oral Health Care for People Living with HIV/AIDS<br />
References<br />
1.<br />
2.<br />
3.<br />
4.<br />
5.<br />
6.<br />
7.<br />
8.<br />
9.<br />
Badner VM. Ensuring the oral health of patients with HIV. J Am Dent<br />
Assoc. 2005;136(10):1415-7.<br />
Centers for Disease Control and Prevention. (1997, September). HIV<br />
Prevention Case Management: Literature Review and Current Practice.<br />
http://www.cdc.gov/hiv/pubs/pcml/pcml-doc.htm<br />
Cherry-Peppers G, Daniels CO, Meeks V, Sanders CF, Reznik D. Oral<br />
manifestations in the era of HAART. J Natl Med Assoc. 2003;95(2 Suppl<br />
2):21S-32S.<br />
Department of Health and Human <strong>Service</strong>s, Presidential Advisory<br />
Council on HIV/AIDS. Achieving an HIV-free generation:<br />
Recommendations for a new American HIV strategy. 2005.<br />
http://www.pacha.gov/pdf/PACHArev113005.pdf<br />
Dobalian A, Andersen RM, Stein JA, Hays RD, Cunningham WE,<br />
Marcus M. The impact of HIV on oral health and subsequent use of<br />
dental services. J Public Health Dent. 2003;63(2):78-85.<br />
Fleishman, J.A. (1998, July). Research Design Issues in Evaluating the<br />
Outcomes of Case Management for Persons with HIV. Evaluating HIV<br />
Case Management: Invited Research & Evaluation Papers, 25-48.<br />
Freed JR, Marcus M, Freed BA, et al. Oral health findings for HIVinfected<br />
adult medical patients from the HIV Cost and <strong>Service</strong>s<br />
Utilization Study. J Am Dent Assoc. 2005;136(10):1396-405.<br />
Heslin KC, Cunningham WE, Marcus M, et al. A comparison of unmet<br />
needs for dental and medical care among persons with HIV infection<br />
receiving care in the United States. J Public Health Dent. 2001;61(1):14-<br />
21.<br />
Marcus M, Freed JR, Coulter ID, et al. Perceived unmet need for oral<br />
treatment among a national population of HIV-positive medical patients:<br />
social and clinical correlates. Am J Public Health. 2000;90(7):1059-63.<br />
BU School of Public Health, Health & Disability Working Group<br />
December 2008<br />
Page 72 of 72<br />
11