ECR 2013 â Final Programme - myESR.org
ECR 2013 â Final Programme - myESR.org
ECR 2013 â Final Programme - myESR.org
- No tags were found...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
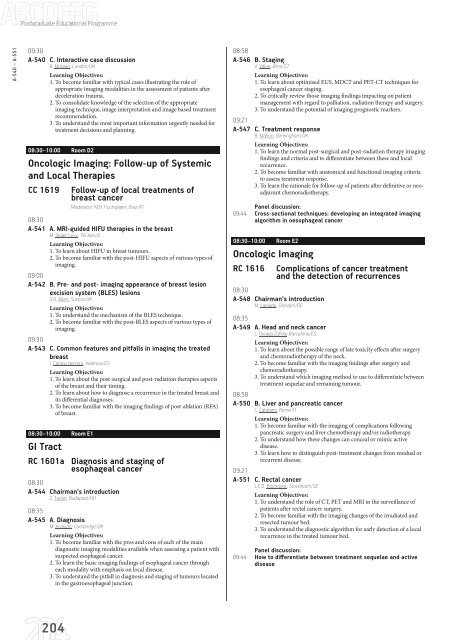
Postgraduate Educational <strong>Programme</strong>A-540 – A-55109:30A-540 C. Interactive case discussionR. M<strong>org</strong>an; London/UKLearning Objectives:1. To become familiar with typical cases illustrating the role ofappropriate imaging modalities in the assessment of patients afterdeceleration trauma.2. To consolidate knowledge of the selection of the appropriateimaging technique, image interpretation and image based treatmentrecommendation.3. To understand the most important information urgently needed fortreatment decisions and planning.08:30–10:00 Room D2Oncologic Imaging: Follow-up of Systemicand Local TherapiesCC 1619 Follow-up of local treatments ofbreast cancerModerator: M.H. Fuchsjäger; Graz/AT08:30A-541 A. MRI-guided HIFU therapies in the breastM. Sklair-Levy; Tel Aviv/ILLearning Objectives:1. To learn about HIFU in breast tumours.2. To become familiar with the post-HIFU aspects of various types ofimaging.09:00A-542 B. Pre- and post- imaging appearance of breast lesionexcision system (BLES) lesionsS.D. Allen; Sutton/UKLearning Objectives:1. To understand the mechanism of the BLES technique.2. To become familiar with the post-BLES aspects of various types ofimaging.09:30A-543 C. Common features and pitfalls in imaging the treatedbreastJ. Camps Herrero; Valencia/ESLearning Objectives:1. To learn about the post-surgical and post-radiation therapies aspectsof the breast and their timing.2. To learn about how to diagnose a recurrence in the treated breast andits differential diagnoses.3. To become familiar with the imaging findings of post-ablation (RFA)of breast.08:30–10:00 Room E1GI TractRC 1601a Diagnosis and staging ofesophageal cancer08:30A-544 Chairman‘s introductionZ. Tarján; Budapest/HU08:35A-545 A. DiagnosisM. Krokidis; Cambridge/UKLearning Objectives:1. To become familiar with the pros and cons of each of the maindiagnostic imaging modalities available when assessing a patient withsuspected esophageal cancer.2. To learn the basic imaging findings of esophageal cancer througheach modality with emphasis on local disease.3. To understand the pitfall in diagnosis and staging of tumours locatedin the gastroesophageal junction.08:58A-546 B. StagingV. Válek; Brno/CZLearning Objectives:1. To learn about optimised EUS, MDCT and PET-CT techniques foresophageal cancer staging.2. To critically review those imaging findings impacting on patientmanagement with regard to palliation, radiation therapy and surgery.3. To understand the potential of imaging prognostic markers.09:21A-547 C. Treatment responseB. Mahon; Birmingham/UKLearning Objectives:1. To learn the normal post-surgical and post-radiation therapy imagingfindings and criteria and to differentiate between these and localrecurrence.2. To become familiar with anatomical and functional imaging criteriato assess treatment response.3. To learn the rationale for follow-up of patients after definitive or neoadjuvantchemoradiotherapy.Panel discussion:09:44 Cross-sectional techniques: developing an integrated imagingalgorithm in oesophageal cancer08:30–10:00 Room E2Oncologic ImagingRC 1616 Complications of cancer treatmentand the detection of recurrences08:30A-548 Chairman‘s introductionM. Laniado; Dresden/DE08:35A-549 A. Head and neck cancerL. Oleaga Zufiría; Barcelona/ESLearning Objectives:1. To learn about the possible range of late toxicity effects after surgeryand chemoradiotherapy of the neck.2. To become familiar with the imaging findings after surgery andchemoradiotherapy.3. To understand which imaging method to use to differentiate betweentreatment sequelae and remaining tumour.08:58A-550 B. Liver and pancreatic cancerC. Catalano; Rome/ITLearning Objectives:1. To become familiar with the imaging of complications followingpancreatic surgery and liver chemotherapy and/or radiotherapy.2. To understand how these changes can conceal or mimic activedisease.3. To learn how to distinguish post-treatment changes from residual orrecurrent disease.09:21A-551 C. Rectal cancerL.C.O. Blomqvist; Stockholm/SELearning Objectives:1. To understand the role of CT, PET and MRI in the surveillance ofpatients after rectal cancer surgery.2. To become familiar with the imaging changes of the irradiated andresected tumour bed.3. To understand the diagnostic algorithm for early detection of a localrecurrence in the treated tumour bed.Panel discussion:09:44 How to differentiate between treatment sequelae and activedisease204