ESRD NETWORK 6 2011 ANNUAL REPORT
ESRD NETWORK 6 2011 ANNUAL REPORT
ESRD NETWORK 6 2011 ANNUAL REPORT
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
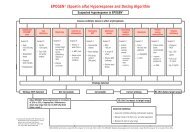
Background and OverviewSoutheastern Kidney Council Sanction ProcessThe Centers for Medicare and Medicaid services (CMS) published the sanction regulations in theApril 15, 2008 Conditions for Coverage for <strong>ESRD</strong>. Under contract with CMS, the <strong>ESRD</strong> Networks’responsibilities for sanctions or alternative sanction recommendations and referrals include thefollowing:Recommending to CMS sanctions or alternative sanctions for facilities/providers that do notcomply with Network goals and/or are not providing appropriate medical care;Providing the necessary documentation to support the recommendation; and,Referring to the QIO or the State Office of the Inspector General information collected whileconducting contract activities that indicate that a physician may be failing to meet his/herobligation to provide quality care or involved in Medicare fraud.Role of the NetworkCongress and CMS charge the Southeastern Kidney Council, as the Network 6 contractor, toprotect <strong>ESRD</strong> Medicare beneficiaries by monitoring and improving care provided and ensuringfacilities meet the Network goals. Network 6 believes that prompt identification and resolution ofquality issues through a collaborative, collegial approach best serves the patients. Network 6creates measurable goals, notifies providers of the expectations/deliverables in meeting thosegoals, and provides on-going technical assistance and education for <strong>ESRD</strong> providers to supportthem in reaching the goals and providing the highest level of care possible. When SKC identifiesfacilities as having opportunities to improve, the Network provides intensive technical assistance toaddress and resolve the issues. If quality issues continue despite this intensive intervention and thefacility fails to meet Network goals, Network 6 will pursue sanctions to protect the beneficiariesand/or enforce CMS requirements and standards.The Conditions for Coverage for <strong>ESRD</strong>, excerpted below, allow for alternative sanctions for anyprovider that does not participate in the activities and pursue the goals of the Network. Every year,each facility in the Network 6 area signs a Quality of Care Commitment with the Network (found inthe CMS National Goals and Network Activities section of this report) which states the expectationsof the Network. This includes providing the highest quality of care, cooperating with the MedicalReview Board in quality improvement projects, cooperating with the Network in the resolution ofcomplaints, submitting data and improvement plans as requested. Facilities selected for focusedreview sign an additional agreement to ensure they understand the goals and the performancematrix for expected deliverables and outcomes.The Network 6 is committed to rapid identification and correction of problems. The severity of theissue and the pace at which the facility improves determines the rate at which SKC requestsinterventions and sanctions. Generally, this will not exceed one year, but may be much shorter forcritical issues or repeat issues.Network 6 will refer any regulatory issues to the State Survey Agency. Network 6 will refer allissues that are specific to the physician(s) or involve Medicare fraud to the Quality ImprovementOrganization (QIO), state Medical Board and/or the Office of the Inspector General (OIG).P a g e | 91