Impact on Patient Care
Download (PDF, 10.84 MB) - Health Care Improvement Foundation
Download (PDF, 10.84 MB) - Health Care Improvement Foundation
- No tags were found...
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Update <strong>on</strong> Antibacterial Resistance<str<strong>on</strong>g>Impact</str<strong>on</strong>g> <strong>on</strong> <strong>Patient</strong> <strong>Care</strong>John G. Gums, Pharm. D., FCCPProfessor of Pharmacy and MedicineAssociate Chair, Department of Pharmacotherapyand Translati<strong>on</strong>al ResearchDirector of the Antimicrobial Resistance Management (A.R.M.) ProgramUniversity of FloridaHealth <strong>Care</strong> Improvement Foundati<strong>on</strong>Philadelphia, PANovember 12, 20091
Bugs vs. DrugsNew Yorker 20082
Bad Bugs—No Drugs!2 M people will acquire bacterial infecti<strong>on</strong>s in the hospital 90 k will die (4.5%)70% of bacteria will be resistant to at least <strong>on</strong>e drug30% resistant to at least 3 antibiotics!!Review of 15 pharmaceutical companies and 7 major biotechcompanies revealed: 506 drugs in development (phase II/III)5 antibiotics67 cancer-related33 inflammati<strong>on</strong>/pain34 endocrine32 pulm<strong>on</strong>ary diseaseIDSA 20043
Clin Infect Dis 2009;48:1-12E: E.faeciumS: S. aureusK: K. pneum<strong>on</strong>iaA: A. baumaniiP: P. aeruginosaE: E. species4
Major Factors C<strong>on</strong>tributing to theEmergence of Infectious Diseases Internati<strong>on</strong>al travel and commerce Human demographics and behavior Breakdown of public health measuresInstitute of Medicine Report, 1992 CDC5
Antibiotic Producti<strong>on</strong> 15.5 milli<strong>on</strong> kg (17,000 t<strong>on</strong>s) PCN– 3.85 gms/pers<strong>on</strong>s <strong>on</strong> earth– 4.5 milli<strong>on</strong> kg (5,000 t<strong>on</strong>s) TCN 40% used in livestock “Farm-to-Fork” modelWebster P. Lancet 2009;374:772-774JAC 2003; 52:5-76
Historical Perspective Until 1989 vancomycin resistance had not beenreported; Antibacterial-c<strong>on</strong>taining In 1994 14% of hospital-acquiredsoapsenterococci -Meta-analysis were of 27 resistant studies between to vancomycin1980-2006(32% as of 2003) - MMWR 1993;42:597-99-soaps c<strong>on</strong>taining triclosan(0.1%-0.45%) were no more effectivethan plain soap in preventing illness and reducing bacterial levels Not <strong>on</strong> the c<strong>on</strong>fined hands to bacteria - Candida sp.-several J Clin Microbiol studies showed 1994;32:1092-98 evidence of triclosan-adapted crossresistance to antibioticsCID 2007 (September) :45:S137-147 Also seen with mupirocin - JAC 2003; 51:613-17 Vancomycin-dependent Enterococci (VDE) – EID 2004;10(7):1277-817
The Rules of Antibiotic Resistance1. Given enough antibiotic and time, resistance will appear2. Resistance is progressive, moving from low tointermediate to high levels3. Organisms that are resistant to <strong>on</strong>e antibiotic will likelybecome resistant to others ( “cross-resistance”)4. Once selected, drug resistance will not disappear,although it may decline5. Select antibiotics to treat “both” patients!Levy SB NEJM 1998; 338:1376-8.8
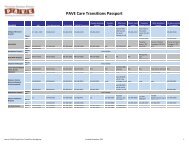
400 + Hospitals21% Teaching79% Community15% North Central30% Northeast2% Northwest16% South Central29% SoutheastGums, JG. University of Floridawww.armprogram.com8% Southwest9
Gums, JG. University of Floridawww.armprogram.comTotal Isolates Compared Nati<strong>on</strong>ally (1990-2009): 30,027,284‣ 2,836,156 Pseudom<strong>on</strong>as aeruginosa isolates‣ 5,558,999 Staphylococcus aureus isolates (incl. MRSA)‣ 220,040 Streptococcus pneum<strong>on</strong>iae isolates‣12,176,916 E. coli isolates‣ 2,907,015 Klebsiella pneum<strong>on</strong>iae isolates10
Escherichia coli Leading nosocomial pathogen (16%) Resistance to amoxicillin 30% in community Hyperproducti<strong>on</strong> of TEM-1 -lactamase.Large quantities of enzyme not suppressedby inhibitors Resistance to:– AMP/SULB = 35%– TIC/CLAV = 14%– PIP/TAZ = 12%11
A.R.M. Program: Escherichia coli(2000-2008)1009080706050403020100AmpicillinAmp/SulbNati<strong>on</strong>alNENJPA12
A.R.M. Program: Escherichia coli(2000-2008)1009080706050403020100Cefazolin Cefuroxime CeftazidimeNati<strong>on</strong>alNENJPA13
A.R.M. Program: Escherichia coli(2000-2008)1009080706050403020100CirprofloxacinLevofloxacinNati<strong>on</strong>alNENJPA14
Klebsiella pneum<strong>on</strong>iae Resistance caused by extended-spectrumcephalosporinases Related to -lactamases (TEM-1, TEM-2, SHV-1)but target 3rd generati<strong>on</strong> cephalosporins Nati<strong>on</strong>al incidence: 14% (variable) Brooklyn,NY-15 hospitals. MDR incidence = 2.5%(2005)vs. 22% (2006) JAC 2007 (May 9)15
A.R.M. Program: Klebsiella Pneum<strong>on</strong>iae(2000-2008)1009080706050403020100Cefazolin Cefuroxime Ceftriax<strong>on</strong>e CefepimeNati<strong>on</strong>alNENJPA16
Pseudom<strong>on</strong>as aeruginosa Inducible, chromosomally-mediated -lactamase Plasmid-mediated -lactamase Loss of an outer membrane protein and plasmidencodedimipenemase c<strong>on</strong>fers resistance toimipenem17
A.R.M. Program: Pseudom<strong>on</strong>as aeruginosa(2000-2008)1009080706050403020100Selective Use PressureAmikacin Gentamicin TobramycinNati<strong>on</strong>alNENJPA18
Gram-Positive OrganismsIf We Only Knew….. August 20, 1999TABLE 1. Cases of community-acquired methicillin-resistant Staphylococcus aureus,byselected characteristics -- Minnesota and North Dakota, 1997-1999 4 Characteristic pediatric Case cases: 1 Case 12m<strong>on</strong>ths-2 Case 3 13 years Case 4 RuralAgeareas7 yearsof Minnesota16 m<strong>on</strong>thsand13 yearsNorth12Dakotam<strong>on</strong>thsSyndrome septic arthritis, severe sepsis necrotizing necrotizingsepsis, pneum<strong>on</strong>ia, pneum<strong>on</strong>ia, pneum<strong>on</strong>ia/ All received β-lactam antibiotics severe sepsis which severe sepsis delayed IDempyemaof MRSAAntimicrobial t/s, tet, cip, gent, t/s, tet, cip, gent, t/s, cep, cip, gent, t/s, tet, cip,susceptibility* ery, clind, vanc ery, clind, vanc ery, clind, vanc gent, ery,clind, vanc All died of systemic MRSA infecti<strong>on</strong>Toxin test+ SEC positive SEC positive SEB positive SEB positive MIC’s to Vanc ≤ 2 mcg/ml and sensitive to multiple* t/s=trimethoprim-sulfamethoxazole, tet=tetracycline, cip=ciprofloxacin, gent=gentamicin,antibioticsery=erythromicin, clind=clindamycin, and vanc=vancomycin.+ SEB=staphylococcal enterotoxin B;SEC=staphylococcal enterotoxinMMWR MMWR 1999;48(32):707-1019
August 1999CA-MRSASCCmec IV or V (rather than I-III)Smaller genome, more mobile, replicates quickerMay displace HA-MRSAVirulence genesPotent toxin PVL (Pant<strong>on</strong>-Valentine leukocidin)20
A.R.M. Program: Staph aureus(2000-2008)1009080706050403020100Nafcillin/OxacillinNati<strong>on</strong>alNENJPA21
Vancomycin IntermediateStaphylococcus aureus (VISA) VISA (MIC = 8 g/cc) May 1996: First reported in Japan July 1997: Perit<strong>on</strong>itis in a l<strong>on</strong>g-term perit<strong>on</strong>eal dialysispatient (Michigan) August 1997: Bloodstream infecti<strong>on</strong> with l<strong>on</strong>g-termMRSA col<strong>on</strong>izati<strong>on</strong> (New Jersey) Report immediately to State Health Department Isolati<strong>on</strong> mandatory C<strong>on</strong>tact FDA for drug therapy opti<strong>on</strong>sState of FloridaMMWR Sept. 5, 1997:46(35)22
Vancomycin ResistantStaphylococcus aureus (VRSA)June 2002--catheter exit site in a 40 y.o. dialysis patient with DM,PVD, & CRF (oxacillin >16 g/cc, vancomycin > 128 g/cc).(MMWR July 5, 2002;51(26):565-67)April 2002--MRSA bacteremia treated with vancomycin and rifampin.Also infected with VRE and K. oxytoca.Resistant isolate c<strong>on</strong>tained the vanA gene from enterococci.September 20, 2002--Pennsylvania: possible osteomyelitis(vancomycin=64 g/cc), c<strong>on</strong>tained mecA and vanA genes.(MMWR Oct. 11, 2002;51(40):902-3) April 23, 2004 – New York: LTCF, urine culture – microscan MIC =4 g/cc, E test = MIC = >256 g/cc; mecA (oxacillin) and vanA(vancomycin) genes present. (MMWR 2004;53(15):322-2323
A.R.M. Program: Staphylococcus aureus(2000-2008)1009080706050403020100ClindamycinErythromycinNati<strong>on</strong>alNENJPA24
% macrolide resistanceRelati<strong>on</strong>ship of Efflux vs.Methylati<strong>on</strong>-Induced Resistance in S. Aureus2000 - 200810080604056% erm58% erm65% erm53% erm36.8 2029.7 35.6effluxmethylati<strong>on</strong>2026.6 25.3 2938.30Nati<strong>on</strong>al NE NJ PA25
CA-MRSA and Clindamycin:Is there inducible resistance?S. aureus soft tissue infecti<strong>on</strong>• Penicillin• Erythromycin• Clindamycin• Levofloxacin• Oxacillin• VancomycinRRSRRSIs this phenotypeauthorizati<strong>on</strong> to prescribeclindamycin?(+) D-test ~ (+erm)(Good chance clindamycin will fail)Frank AL, et al. Pediatr Infect Dis J 2002;21:530-4. Lewis JS, et al. Clin Infect Dis. 2005 Jan 15;40(2):280-5Levin TP, et al. Antimicrob Agents Chemother 2005;49:1222-4. 26
A.R.M. Program: Enterococcus faecium:(2000-2008)1009080706050403020100VancomycinNati<strong>on</strong>alNENJPA27
Penicillin-Resistant Pneumococcus Model of evoluti<strong>on</strong> indicates a slow emergencephase followed by an exp<strong>on</strong>ential growth phase of10 years reaching a stati<strong>on</strong>ary phase when PRP =50% Primary mechanism of resistance is alteredPBP’s, not by producti<strong>on</strong> of -lactamase-lactamase inhibitors do not affect thesusceptibility of these strainsJ Antimicrob Chem 1997;40 (Suppl A):11-1828
A.R.M. Program: Streptococcus pneum<strong>on</strong>iae(2000-2008)1009080706050403020100PenicillinNati<strong>on</strong>alNENJPA29
Campaign to Prevent Antimicrobial Resistance in Healthcare SettingsKey Preventi<strong>on</strong> Strategies• Prevent infecti<strong>on</strong>• Diagnose and treat infecti<strong>on</strong>effectively• Use antimicrobials wisely• Prevent transmissi<strong>on</strong>Clinicians hold the soluti<strong>on</strong>!
Preventing ResistanceUnrealistic patient expectati<strong>on</strong>sNOW ® - Streptococcus pneum<strong>on</strong>iae urinaryantigen test 15 min. for presumptive Dx of Pneumococcalpneum<strong>on</strong>ia (sensitivity = 86%, specificity = 94%, accuracy= 93%) (J Clin Microbiol. 2003;41:2810-13)Snort. Sniffle. Sneeze.No Antibiotics, Please. (FDA/CDC; January 2004)POC CRP testing - CRP>60mg/l - QuikRead31
Strategies for Overcoming ResistanceAvoid exclusive use patterns Use broad-spectrum agents appropriately– Induces resistance– Facilitates cross-resistance– Sustains organism in genesis envir<strong>on</strong>ment New Drug Development– Do they c<strong>on</strong>tribute to the problem?32
Strategies for Overcoming Resistance Rotate agents Alternate between classes rather thanbetween agents within the class Shorten courses rather than lengthen Use targeted regimens as so<strong>on</strong> assusceptibility tests are available(bb guns, not shotguns)NEJM 1994;330:1240-4133
Is the Antibiotic Steward “Ship”Sinking??Junk in, Junk outAntibiograms are old dataData is often not differentiated between urine,systemic, ICU, n<strong>on</strong>-ICU, hospital to hospital, outpatientvs. in-patient, and even duplicate isolates.Data reflects the aggregate not the patient34
Changing the Paradigm: What does thefuture of Antibiotic Stewardship Look Like?35
Hunterd<strong>on</strong> HospitalE. Coli60% antibiotics >5% increase in susceptibility20% antibiotics >5% decrease in susceptibilityKlebsiella pneum<strong>on</strong>ia87% antibiotics >5% increase in susceptibilityPseudom<strong>on</strong>as aeruginosa78% antibiotics >5% increase in susceptibility11% antibiotics >5% decrease in susceptibilityStaphylococcus aureusMRSA rates declined by 23%FinancialTotal cost savings year 1: ~$139,000Total cost savings year 2:~$70,00040
Program Informati<strong>on</strong>A.R.M. ProgramParticipating instituti<strong>on</strong>s receive a customized report profiling trendanalysis within the hospital/system and benchmarking to nati<strong>on</strong>al, regi<strong>on</strong>alor state comparatorsBugs and Drugs ProgramVHA collaborative program that works with individual hospital/systemsproviding a customized analysis of relati<strong>on</strong>ship between antibiotic use andresistance trends, including predictive models.iDOP ProjectInnovative data-mining pilot project evaluating patient-specific variableslinked to antibiotic utilizati<strong>on</strong> and outcomes. Participating instituti<strong>on</strong>sreceive a customized comprehensive and executive report. Need 5 pilotinstituti<strong>on</strong>s.45
Strategies for Overcoming Resistance Increase handwashing 175 individuals (95 women and 80 men) usingpublic restrooms…with and w/o signs 61% of the and 37% of the washed theirhands with soap, in the absence of the sign 97% of the and 35% of the washed theirhands in the presence of the sign.Percept Mot Skills. 2003 Dec;97(3 Pt 1):805-10.46