Child research
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
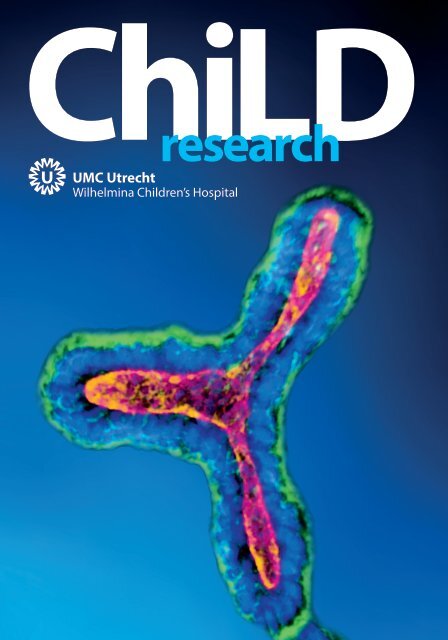
ChiLD<br />
<strong>research</strong>
Colophon<br />
<strong>Child</strong> Health magazine, edition 2019<br />
Publisher<br />
This magazine is published by UMC Utrecht,<br />
Strategic Program <strong>Child</strong> Health<br />
Editors<br />
Celine Uit de Weerd-Bakker, Anneke van der Brug<br />
Magazine concept, design and art direction<br />
UMC Utrecht Design & productions;<br />
Barbara Hagoort, Laura Langenbach<br />
Contributors<br />
Kors van der Ent, Anneke van der Brug, Berent Prakken,<br />
Mireille Bekker, Kitty Bloemenkamp, Jeroen Dudink,<br />
Floris Groenendaal, Manon Benders, Helen Torrance,<br />
Frank Broekmans, Gijs van Haaften, Hans Kristian Ploos<br />
van Amstel, Albertien van Eerde, Marc Lilien, Hans Breur,<br />
Peter van Tintelen, Sabine Fuchs, Peter van Hasselt,<br />
Judith Jans, Nanda Verhoeven, Jeffrey Beekman,<br />
Saskia van Mil, Bas Vastert, Jorg van Loosdregt,<br />
Femke van Wijk, Louis Bont, Patricia Bruijning,<br />
Marry van den Heuvel-Eibrink, Roelie Wösten-van Asperen,<br />
Hanneke van Santen, Jaap van Laar, Nico Wulffraat,<br />
Harry Heijerman, Kathelijn Fisscher, Roger Schutgens,<br />
Elise van de Putte, Tim Takken, Janjaap van der Net,<br />
Marianne Boes, Marjolijn Ketelaar, Sanne Nijhof,<br />
Martha Grootenhuis, René Eijkemans, Niels Eijkelkamp,<br />
Freek Hoebeek, Joost Frenkel, Cyrus Park.<br />
colofon<br />
Copy editors<br />
Sarah Opitz, Cyrus Park<br />
Coordination photography<br />
UMC Utrecht Design & Productions; Jelle Westerhoff<br />
Photography / contributing photographers<br />
UMC Utrecht Design & Productions;<br />
Rudi Hovig, Ed van Rijswijk, Thomas Dobber, Ivar Pel<br />
Getty Images, Unsplash<br />
Illustrations<br />
Barbara Hagoort, Laura Langenbach<br />
Print<br />
Revon<br />
Contact<br />
Anneke van der Brug<br />
Program manager <strong>Child</strong> Health<br />
abrug@umcutrecht.nl<br />
0031 6 16 36 11 51<br />
www.umcutrecht.nl/childhealth<br />
childhealth@umcutrecht.nl<br />
2 UMC Utrecht - <strong>Child</strong> <strong>research</strong><br />
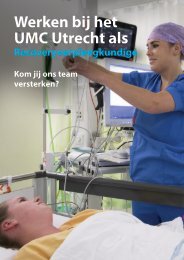
The photographs on the<br />
coverpage and this page<br />
show microscopic pictures<br />
of intestinal organoids used<br />
by several <strong>research</strong> groups<br />
of the <strong>Child</strong> Health Program
UMC UTRECHT I WILHELMINA CHILDREN’S HOSPITAL<br />
<br />
<strong>Child</strong> Health<br />
in Utrecht<br />
<br />
In the 17th and 18th centuries, medical care for children was in the hands of general<br />
physicians and surgeons. It was not until the second half of the 19th century that<br />
doctors began to focus on caring for sick children and formed the basis for current<br />
pediatric medicine.<br />
The Wilhelmina <strong>Child</strong>ren’s Hospital was founded in 1888 and<br />
is one of the oldest children’s hospitals in the world. From the<br />
very beginning, excellent medical care and new medical<br />
developments went hand-in-hand, working closely with the<br />
Utrecht University. In 1997, the children’s hospital merged<br />
with the Academic Hospital Utrecht and the medical faculty<br />
of Utrecht University to form the University Medical Center<br />
Utrecht (UMC Utrecht).<br />
Today, the UMC Utrecht is one of the largest academic<br />
centers in the Netherlands. Patient care and biomedical<br />
<strong>research</strong> are closely linked, which creates an environment<br />
where scientific advancements quickly move from bench to<br />
bedside. The UMC Utrecht finds itself in the middle of a<br />
vibrant biomedical <strong>research</strong> community: Utrecht Life<br />
Sciences. This represents a strategic alliance in education,<br />
<strong>research</strong> and entrepreneurship in the domain of the life<br />
sciences in the Utrecht area, located in the very heart of<br />
the Netherlands.<br />
The UMC Utrecht’s strategy ‘Connecting U’ concentrates<br />
<strong>research</strong> into six programs, each with a focused number of<br />
disease targets and patient care is integrated into these<br />
programs. Care and <strong>research</strong> for sick children are still at the<br />
heart of the organization, and one of the six <strong>research</strong><br />
programs is ‘<strong>Child</strong> Health’. This Program is an integrated<br />
framework for child-centered interdisciplinary <strong>research</strong>,<br />
aligning patients, clinicians, investigators and resources, so<br />
that it can lead by filling significant gaps to improve the lives<br />
of children during childhood and thereafter.<br />
This magazine gives you an insight into the program and<br />
introduces you to our <strong>research</strong>ers and their subjects.<br />
We invite you to contact them and work together -<br />
because children are our future!<br />
I believe the children are our<br />
<br />
future<br />
Teach them well and let them lead the way<br />
Show them all the beauty they possess inside<br />
Give them a sense of pride to make it easier.<br />
- Whitney Houston, 1985<br />
Kors van der Ent Chair of <strong>Child</strong> Health<br />
Program UMC Utrecht.<br />
Care for chronic diseases in the future<br />
asks for rigorous changes in our<br />
old-fashioned health care systems.<br />
- Kors van der Ent<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 3
06Contents<br />
The <strong>Child</strong> Health Program<br />
Ante- and<br />
perinatal<br />
damage<br />
Congenital<br />
and hereditary<br />
disorders<br />
Severe<br />
inflammatory<br />
disorders<br />
Postoncology<br />
When you<br />
save the<br />
mother,<br />
you save<br />
the family.<br />
- Kitty Bloemenkamp<br />
Your DNA<br />
at the<br />
center<br />
of care.<br />
- Hans Kristian and<br />
Ploos van Amstel<br />
Prevention is<br />
better than<br />
treatment.<br />
- Patricia Bruijning<br />
<br />
Our mission in<br />
pediatric oncology<br />
<strong>research</strong> is to<br />
improve cure rates<br />
for all children and<br />
to enhance quality<br />
of survival.<br />
- Marry van den Heuvel-Eibrink<br />
10 16 22<br />
30<br />
32<br />
Strategic Themes<br />
40 Unique Resources<br />
32<br />
36<br />
38<br />
Lifecycle<br />
Interdisciplinarity<br />
Mental & Physical Health<br />
40 Patients cohorts<br />
41<br />
45<br />
Facilities & Expert Knowledge<br />
Clinical Trials<br />
46 Education and Talent<br />
4 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
CHILD HEALTH PROGRAM UMC UTRECHT<br />
Collaborations<br />
& networks<br />
Visualization network of collaboration partners of <strong>Child</strong> Health - based<br />
on co-authorship of 1324 articles and reviews in Web of Science<br />
published in 2016-2018. The graph shows the 100 organizations that<br />
<strong>Child</strong> Health most frequently collaborates with. Bubble size is<br />
proportional to number of publications, line thickness to the number<br />
of papers co-authored by <strong>research</strong>ers from the respective organizations.<br />
connections are only shown between organizations that co-published<br />
10 or more papers.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 5
The <strong>Child</strong> Health Program<br />
of the UMC Utrecht<br />
UMC Utrecht is one of the top-ranked academic medical centers<br />
in Europe in which patient care and biomedical <strong>research</strong> are<br />
closely linked. Partners, for example the Hubrecht Institute, can<br />
be found at a close distance, and collaboration with the Faculties<br />
of Veterinary Medicine and Science at Utrecht University<br />
reinforces the relationship between animal and human health<br />
and the environment. The UMC Utrecht has been awarded<br />
international accreditation on quality of care, <strong>research</strong> and<br />
education by the Joint Commission International (JCI).<br />
Our program, <strong>Child</strong> Health, is one of six<br />
hospital-wide strategic <strong>research</strong> programs.<br />
The diseases we focus on are characterized<br />
by their influence on an individual’s entire<br />
lifespan as they often start at the<br />
beginning of life, or even before birth, and<br />
can have consequences far into adulthood.<br />
Within our <strong>Child</strong> Health program, we<br />
ensure that our ‘Cycle of Life’ approach is<br />
strongly intertwined with innovation.<br />
Goals<br />
We focus on healthy development of a<br />
child, from pre-conception to adulthood.<br />
We’ve established an interdisciplinary<br />
child-centered <strong>research</strong> community that<br />
aligns with the European Commission’s<br />
philosophy of Responsible Research and<br />
Innovation (RRI) and aims to:<br />
Anneke van der Brug, MSc is the <strong>Child</strong> Health Program<br />
manager. She enjoys stimulating (clinical) <strong>research</strong>ers working<br />
together in multidisciplinary <strong>research</strong> and is eager to continuously<br />
think up opportunities to promote excellent scientific results.<br />
abrug@umcutrecht.nl<br />
Kors van der Ent, MD PhD is chair of the <strong>Child</strong> Health<br />
Program. He is an experienced pediatric pulmonologist with<br />
special interest for chronic diseases, like cystic fibrosis. Besides<br />
top-notch science he is mainly focused on what really matters for<br />
patients and their families.<br />
cent@umcutrecht.nl<br />
• Improve pediatric disease outcomes<br />
within a lifespan context.<br />
• Cure congenital and hereditary diseases<br />
by unravelling pathogenesis; by developing<br />
diagnostic and prognostic markers<br />
and tools; and by developing and implementing<br />
novel therapeutics and lifestyle<br />
interventions.<br />
• Improve resilience and quality of life for<br />
children and their relatives during childhood<br />
and thereafter.<br />
6 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
CHILD HEALTH PROGRAM UMC UTRECHT<br />
By collaborating<br />
we can multiply<br />
our<br />
<br />
success.<br />
- Anneke van der Brug<br />
Societal impact<br />
In the past few decades, the field of<br />
pediatrics has been successful in<br />
combating disease and the life expectancy<br />
of many disorders has significantly<br />
improved. Unfortunately, although children<br />
may survive their disease, they’re<br />
burdened with long-term physical and<br />
mental consequences. This requires drastic<br />
changes for future healthcare: Pediatrics<br />
should focus on the development of children<br />
towards healthy and balanced adults.<br />
Our <strong>Child</strong> Health Program is dedicated to<br />
developing disease prevention strategies,<br />
as well as safe treatment options for<br />
children, which requires intensive<br />
collaboration and cross-fertilization<br />
between our basic and clinical scientists.<br />
But most importantly, our program is<br />
constantly interacting with children<br />
themselves and with the environment in<br />
which they grow up, including their family,<br />
school, sports clubs and broader living<br />
environment. Our program is an active<br />
participant in the midst of a child’s society.<br />
<br />
Research<br />
Areas<br />
The <strong>Child</strong> Health Program of the University<br />
Medical Center links top referent care for<br />
pediatric patient groups to interdisciplinary<br />
<strong>research</strong>. This ranges from fundamental to<br />
translational to longitudinal applied medical<br />
<strong>research</strong>. All chronic diseases within the focus of<br />
our program are similar in that they emerge<br />
early, in the beginning of life and can have<br />
consequences far into adulthood. Our <strong>research</strong><br />
areas high lighted in this magazine are:<br />
Ante- and perinatal damage<br />
This program has a life-cycle character hosting several<br />
Centers of Excellence. It provides high quality care and<br />
<strong>research</strong> through the periconceptional, antenatal and<br />
perinatal phases up to neonatal intensive care, aiming for<br />
the best long-term outcome of child health. Women,<br />
babies and their families are the center of our service as<br />
we strive for excellence and innovation.<br />
Congenital and hereditary disorders<br />
Many disorders of genetic origin are rare and require<br />
academic specialist care. The <strong>Child</strong> Health Program<br />
focuses in particular on congenital diseases of the heart,<br />
liver and kidney and plays a key role in respective<br />
European Reference Networks.<br />
Severe inflammatory disorders<br />
We host several Centers of Excellence for children with<br />
sustained severe inflammatory disorders, such as Juvenile<br />
Idiopathic Arthritis, Cystic Fibrosis, Inflammatory Bowel<br />
Disease and Recurrent Respiratory Tract Infections.<br />
Post-oncology<br />
Treatment of cancer in children can result in severe<br />
physical and psychosocial consequences later in life. The<br />
<strong>Child</strong> Health Program closely collaborates with the<br />
Princes Máxima Center to improve long term outcomes of<br />
cancer treatment.<br />
Let’s collaborate on a culture<br />
of trust and innovation.<br />
- Kors van der Ent<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 7
Berent Prakken,<br />
Acting Dean:<br />
}What I most appreciate about<br />
the <strong>Child</strong> Health program is that<br />
it thrives to deliver top notch<br />
science and translate it into<br />
societal impact.~<br />
Partnering with society<br />
Today, scientific discovery and societal needs<br />
go hand-in-hand. One does not preclude the<br />
other. Because of this, there’s a great deal of<br />
cooperation between the <strong>Child</strong> Health Program<br />
with external social partners such as the<br />
municipality of Utrecht, the Trimbos Institute<br />
for Mental Health, the Jantje Beton Charity and<br />
a large number of patient organizations.<br />
Together, we ensure that basic science and<br />
clinical science harmonize to revolutionize<br />
patient care, and we’re motivated by both<br />
acquiring and applying knowledge.<br />
Team sport<br />
There’s a reason why we do what we do. We’re<br />
curious, we’re motivated, we’re passionate. We<br />
push our <strong>research</strong> beyond conventional<br />
questions. If we discover an important new<br />
gene, we don’t stop with a beautiful genetics<br />
paper. Instead, we continue hunting for the<br />
protein it encodes, and for its function. This<br />
feeds our passion for healing patients and we<br />
cannot do this alone. Fortunately, we don’t have<br />
to. From the molecular biologist discovering a<br />
molecule to the translational scientist<br />
investigating methods of delivery, to the<br />
physician making a diagnosis, to the<br />
psychologist encouraging adherence, to a<br />
treatment regimen, to the patient foundation<br />
focused on patient experiences. We’re all in this<br />
together. It’s no longer just a handful of<br />
<strong>research</strong>ers, but really a team sport.<br />
Berent Prakken<br />
Professor , Pediatric Immunology, Acting Dean,<br />
Education, Director, Biomedical Education Center<br />
3 Strategic Themes<br />
The <strong>research</strong> areas within the <strong>Child</strong> Health<br />
Program are cross-linked by three Strategic<br />
Themes that are represented in all <strong>research</strong> areas.<br />
1. Life-cycle <strong>research</strong><br />
Prognosis of pediatric diseases have improved dramatically<br />
over the past few decades. For example, the life expectancy<br />
of children with cystic fibrosis has increased from about 10<br />
years in the 1950s to almost 50 years in current times. The<br />
first heart surgery in children was performed in at the end<br />
of the 1940s, when the lifespan was very short. Today, heart<br />
surgery is routine and most children with congenital heart<br />
disease are operated on and therefore have a normal life<br />
expectancy. Advances in cancer <strong>research</strong> and care are also<br />
providing a better and longer quality of life for children<br />
with cancer.<br />
The advancements in survival rates and success of<br />
combating acute complications have, in turn, changed care<br />
requirements of pediatric patients. New long-term<br />
complications of diseases are emerging, for example,<br />
cardiac arrhythmias can develop in adults after pediatric<br />
heart surgery and 40% of children with cystic fibrosis<br />
develop diabetes in adulthood. In addition, the effects of<br />
drug treatment in children with, for example, juvenile<br />
rheumatoid arthritis on the function of the liver, kidneys<br />
and lungs in adulthood are unknown. Research in<br />
chronically ill children demands parallel focus on longterm<br />
health for adults.<br />
bprakken@umcutrecht.nl<br />
8 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
CHILD HEALTH PROGRAM UMC UTRECHT<br />
2. Interdisciplinary innovation loops<br />
Our <strong>Child</strong> Health Program has created a scientific infrastructure<br />
that integrates various fields of biomedical <strong>research</strong> connected<br />
to groups of children with chronic diseases and their parents/<br />
relatives. Advancing <strong>research</strong> for the benefit of these children<br />
requires an interdisciplinary approach including basic,<br />
translational and applied medical <strong>research</strong>.<br />
Patient problems, new technologies and societal developments<br />
continuously raise new <strong>research</strong> questions. Our<br />
coherent, interdisciplinary <strong>research</strong> strategy enables us to<br />
answer these <strong>research</strong> questions and discover meaningful<br />
outcomes for patients, their families and society. Therefore, all<br />
of our scientists and professionals who are involved in the care<br />
of our sick children, collaborate closely and share the same<br />
ambition to find the best solutions for our young patients. In<br />
addition, we’re dedicated to communicating our findings to<br />
our patients, relatives and the public; there is clear value in<br />
collecting feedback and properly evaluating our <strong>research</strong> as<br />
these will inevitably lead to new <strong>research</strong> questions. It is<br />
through this innovation loop that societal issues are considered<br />
when defining <strong>research</strong> directions, and where we can<br />
accelerate scientific results quickly from bench to bedside.<br />
I am daily impressed<br />
<br />
by<br />
the talent of the people<br />
who already work and<br />
study at these<br />
organizations. We must<br />
ensure that they can<br />
thrive and contribute to<br />
solving the social<br />
problems that our<br />
world faces.<br />
- Professor Anton Pijpers,<br />
President Utrecht University<br />
3. Physical – mental interaction<br />
Physical restrictions in childhood can have profound<br />
influence on the psychosocial development and identity<br />
formation in adulthood. Pain and discomfort in early life<br />
can affect basic trust in children. Deprivation from<br />
parents, families and friends during early life might<br />
influence social adaptations. Absence from school and<br />
inability to participate in sports might have a negative<br />
impact on the development of resilience in adolescence.<br />
It’s not enough to only pay attention to the physical<br />
health of children. On the other hand, psychological<br />
problems during childhood can have major adverse<br />
effects on medical treatment and the course of a disease.<br />
For example, denial of symptoms and poor adherence to<br />
therapy can highly influence outcome of chronic diseases.<br />
Therefore, we pay particular attention to the development<br />
of children with chronic diseases and study determinants<br />
of, for example, pain and fatigue at both the basic science<br />
and clinical care levels. This can help to develop and<br />
evaluate intervention programs. Our ultimate goal in this<br />
strategic theme is to empower and to engage children<br />
and their relatives to be fit for their future.<br />
Health and happiness are broad concepts. Chronically<br />
ill children indicate that they feel happy too though<br />
they are ill. By support from the environment and the feeling<br />
just to be able to participate, at school and at<br />
<br />
home.<br />
- Jan van Zanen, mayor of Utrecht<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 9
ANTE- AND PERINATAL DAMAGE<br />
Reproductive care<br />
before, during and after birth<br />
kbloemen@umcutrecht.nl mbekker3@umcutrecht.nl<br />
Mireille Bekker, MD, PhD<br />
is a maternal fetal medicine<br />
specialist with an interest in<br />
fetal medicine, counseling,<br />
patient empowerment and<br />
eHealth in obstetric care. She’s<br />
a member of the board of the<br />
national NIPT consortium that<br />
performs nationwide implementation<br />
studies (Trials by<br />
Dutch laboratories for<br />
Evaluation of Non-Invasive<br />
Prenatal Testing). Mireille is the<br />
project leader of several<br />
<strong>research</strong> projects regarding<br />
home telemonitoring and<br />
other eHealth strategies in<br />
obstetric health care.<br />
Kitty Bloemenkamp. MD,<br />
PhD is and has been a PI of<br />
several randomized controlled<br />
trials, observational studies<br />
and experimental studies in<br />
the field of maternal health.<br />
She is the Chairman of Nethoss<br />
(Netherlands Obstetric Survey<br />
Study), National Enquiry of<br />
Maternal Death Review,<br />
Netherlands and of INOSS<br />
(International Network of<br />
Obstetric Survey Systems).<br />
Improving the health of women and<br />
children is a global public health issue.<br />
This mission was adopted by all United<br />
Nations Member States in 2015 and<br />
addresses sustainable development to<br />
ensure healthy lives and promote wellbeing<br />
at all ages.<br />
In this <strong>research</strong> area of <strong>Child</strong> Health, we focus on reproductive,<br />
maternal, newborn and child health. More specifically, we develop<br />
novel clinical strategies to innovate and improve the quality of care for<br />
the mother, fetus and child by integrating <strong>research</strong> with clinical care.<br />
This includes translational <strong>research</strong>, advanced imaging technologies,<br />
creating and integrating patient registries, diagnosis accompanied by<br />
genetic testing, eHealth, auditing to evaluate impact and value-based<br />
health care approaches. This is done in close collaboration with our<br />
colleagues in the fields of fertility, gynaecology and neonatology.<br />
In this way we investigate the entire lifecycle from preconception and<br />
complicated pregnancy to delivery, postpartum and consequences of<br />
these complications later in life.<br />
eHealth and high-risk pregnancy<br />
eHealth converges healthcare and technology, and is allowing our<br />
patients to actively participate in their own healthcare regimens. It also<br />
provides our physicians up-to-date information about our patients, in<br />
real-time, making diagnosis and treatment more efficient and<br />
accurate. And with the availability of mobile phones and internetbased<br />
applications, we can reach women and their babies in<br />
improverished areas.<br />
We often use eHealth methods in our <strong>research</strong> and care, and to share<br />
our findings. For example, women with high-risk pregnancies need to<br />
visit the hospital frequently, which may become burdensome on both<br />
the mother and unborn child. We’re currently running two studies,<br />
Safe@home and HOTEL, using smart telemonitoring systems. In the<br />
SAFE@home study, we monitor pregnant women at home for high-risk<br />
factors, for example high blood pressure and diabetes, reducing the<br />
number of visits they need to make to the doctor. In the HOTEL study,<br />
the fetal condition is monitored at home by a fetal cardiotocography<br />
device instead of hospital admission or daily visits.<br />
10 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
ANTE- AND PERINATAL DAMAGE<br />
Life<br />
starts<br />
in the<br />
uterus.<br />
- Mireille Bekker<br />
<br />
Empowering women and their doctors<br />
Through previous eHealth studies on maternal health, we’ve<br />
discovered a need for reliable registration methods and audit<br />
processes for maternal and neonatal mortality. In addition, morbidity<br />
must be recorded in order to assess strategies on improving health<br />
conditions for women and their babies. Our goal is to translate our<br />
findings, as well as eHealth technologies, to help women, and their<br />
doctors monitor their pregnancies outside of the hospital in low to<br />
middle income countries. We aim to improve the quality of care for<br />
women and their families, and empower them through novel<br />
healthcare systems.<br />
<br />
When you save<br />
the mother, you<br />
save the family.<br />
- Kitty Bloemenkamp<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 11
Building better brains<br />
Improvements in fetal and neonatal care<br />
have significantly reduced mortality in<br />
preterm infants and critically ill term infants.<br />
Unfortunately, half of the infants admitted to<br />
the neonatal intensive care unit (NICU)<br />
experience long-term neurodevelopmental<br />
problems, including cognitive deficits, motor<br />
disabilities and psychiatric diseases. This<br />
creates a lifelong burden, both socially and<br />
financially, for the affected individuals and<br />
their families.<br />
We’re on a mission to “build better brains”<br />
for vulnerable infants. Adverse early life events<br />
such as preterm birth, neonatal cardiac and<br />
non-cardiac surgery and hypoxic-ischemic<br />
encephalopathy can have a profound effect on<br />
brain development. Our neonatal neurology<br />
<strong>research</strong> group studies these events in relation to<br />
the developing infant brain by combining<br />
routine clinical neuroimaging (ultrasound and<br />
MRI), neuromonitoring (aEEG and NIRS) and<br />
neurodevelopmental follow-up.<br />
Babies get stressed too<br />
Premature infants are suddenly thrust into the<br />
bleak and sterile environment of the NICU and<br />
expected to thrive. During this period, exposure<br />
to stressful stimuli causes significant<br />
neurobiological changes affecting brain volume,<br />
DNA methylation and the hypothalamicpituitary-adrenal-axis.<br />
We’re investigating the<br />
effects of early stress on brain development and<br />
are optimizing neonatal care by enriching the<br />
extra-uterine environment and increasing<br />
parental involvement. Together with our national<br />
(Hippo-trial) and international <strong>research</strong> partners<br />
(University of Leuven, Kings College London,<br />
SickKids Toronto), we’re investigating how stress,<br />
such as painful procedures, and stress relievers,<br />
such as skin-to-skin care and sleep, can influence<br />
brain connectivity in order alleviate the<br />
harshness of premature birth and to further<br />
improve our care.<br />
Good sleep, healthy brains<br />
When babies sleep, their brains are actively<br />
developing. A preterm newborn spends most of<br />
his or her time in ‘active sleep’ (REM sleep),<br />
which coincides with heightened synaptogenesis<br />
and brain plasticity. It’s difficult to<br />
visually recognize sleep stages in preterm<br />
infants. However, to optimize sleep (and to set<br />
up intervention studies) we’re studying ways to<br />
automatically detect sleep stages. To do this,<br />
we’re using deep learning algorithms to<br />
recognize neonatal sleep stages based on<br />
monitor values. And together with two technical<br />
Universities (Delft and Eindhoven) we’re developing<br />
advanced wireless biomedical sensors<br />
(e.g. low frequency radar devices) to record<br />
sleep stages.<br />
Personalizing treatment<br />
Within our team, we’ve improved current<br />
neuroprotective treatments. One example is<br />
therapeutic hypothermia for infants with<br />
hypoxic-ischemic encephalopathy, and we’re<br />
optimizing patient selection for this treatment<br />
by studying pharmacokinetics of neurotropic<br />
medication. Additional therapies are also<br />
explored (Benders).<br />
The foundation for optimal brain development<br />
starts peri-conceptionally and lasts well beyond<br />
the teenage years. This calls for an interdisciplinary<br />
approach and together with our<br />
national and international colleagues, we’re<br />
improving the long-term neurodevelopmental<br />
outcome for infants with challenges in longterm<br />
brain development. We’re proud that our<br />
investigations can contribute to new European<br />
standards of care (e.g. ENCFI standards) and we<br />
benchmark our outcome using the International<br />
Consortium for Health Outcomes Measurements<br />
(ICHOM) standards.<br />
<br />
Floris Groenendaal,<br />
MD, PhD is a neonatologist<br />
whose goal is to improve<br />
diagnostics of early brain<br />
injury, using MRI/MRS and<br />
aEEG. In collaboration with<br />
the Laboratory of<br />
Neuro-immunology and<br />
Develop-mental Origins of<br />
Disease, UMC Utrecht, he’s<br />
explored novel neuroprotective<br />
strategies. Floris<br />
introduced therapeutic<br />
hypothermia in The<br />
Netherlands, and performed<br />
pharmacokinetics during<br />
cooling.<br />
Jeroen Dudink, MD, PhD<br />
is a neonatologist with<br />
expertise in neonatal<br />
neuroimaging. He studies<br />
the relation between<br />
neonatal sleep and early<br />
brain development. Together<br />
with technical Universities<br />
and commercial partners, he<br />
develops new devices to<br />
automatically recognize<br />
sleep stages. Furthermore,<br />
Jeroen studies the relation<br />
between neonatal cerebellar<br />
injury and long-term<br />
outcome.<br />
Better baby brains -<br />
the challenge goes on.<br />
- Floris Groenendaal<br />
fgroenen@umcutrecht.nl<br />
jdudink@umcutrecht.nl<br />
12 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
ANTE- AND PERINATAL DAMAGE<br />
A brighter future for<br />
high-risk neonates<br />
mbenders@umcutrecht.nl<br />
Manon Benders, MD,<br />
PhD focuses on neonatal<br />
imaging of brain<br />
development and predicting<br />
outcome. She also<br />
investigates neuroprotective<br />
and neuro-regenerative<br />
strategies to reduce<br />
brain injury.<br />
The early years – starting from prebirth<br />
– is a critical period in a child’s<br />
development, as they form bonds with<br />
their parents, develop language skills<br />
and other cognitive functions, and<br />
establish behavioral patterns. Given the<br />
strong link between perinatal<br />
complications and adverse adolescent<br />
outcomes, we focus on developing<br />
interventions that may prevent, or at<br />
least reduce, perinatal life adversities.<br />
We have an outstanding Neonatal<br />
Neurology team that specializes in the<br />
development of objective biological<br />
measures in the developing brain in<br />
relation to long-term outcome (lifespan<br />
approach). We’ve established an<br />
integrated approach to study this, and<br />
by combining basic and translational<br />
developmental neuroscience, neuromonitoring<br />
and MRI analysis, we’ve<br />
developed perinatal neuro-protective<br />
and neural rescue strategies for the<br />
human fetus and infants. Because of our<br />
strong collaborative approach, we’ve<br />
became an internationally recognized<br />
center of expertise by the Committee of<br />
Rare Diseases of the National Federation<br />
of University Hospitals in the Netherlands<br />
and are part of the EpiCARE, a European<br />
Research Network for rare and complex<br />
epilepsies.<br />
CRUCIAL clinical trial<br />
There is an urgent need for<br />
neuroprotective strategies for infants<br />
with congenital heart disease (CHD) as<br />
they often experience long-term<br />
neurodevelopmental impairments.<br />
Perinatal <br />
improvement<br />
is multiplying<br />
health gain<br />
later on.<br />
- Manon Benders<br />
To investigate this, we recently launched a<br />
multicenter CRUCIAL-trial (CeRebrUm and<br />
Cardiac protection with Allopurinol) in<br />
neonates with CHD who require cardiac<br />
surgery with cardiopulmonary bypass.<br />
We’re investigating the effects of postnatal<br />
and perioperative allopurinol<br />
administration on postoperative brain<br />
injury in CHD neonates. Patients will be<br />
screened using fetal MRI and included<br />
before birth, requiring extensive<br />
collaboration with obstetricians,<br />
neonatologists, cardiologists, pediatric<br />
intensivists and pediatric thoracic<br />
surgeons. Our primary outcome is based<br />
on fetal, postnatal and post-operative MRI<br />
analysis in close collaboration with<br />
quantitative MRI analysts at the Image<br />
Sciences Institute, UMC Utrecht. Longterm<br />
outcome is a secondary objective of<br />
this study, evaluated by psychologists and<br />
occupational therapists, for which we<br />
collaborate with pediatric rehabilitation<br />
and psychiatry. Additional therapies are<br />
also explored within our team<br />
(Dudink and Groenendaal).<br />
In addition to our goals of improving<br />
long-term outcome in high-risk neonates,<br />
we subscribe to the philosophy of open<br />
science. Through the YOUth study<br />
(uu.nl/youthcohort), a large longitudinal<br />
cohort study that collects information<br />
about brain and behavioral development,<br />
we’re able to broadly share anonymous<br />
information about our healthy and highrisk<br />
neonates.<br />
Big Data for small Babies<br />
Premature babies admitted to the<br />
neonatology intensive care unit are closely<br />
monitored as they are susceptible to<br />
infection. Over the past decade, we’ve<br />
collected a vast amount of data and a<br />
group led by Daniel Vijlbrief, PhD, uses<br />
machine learning on this data in order to<br />
improve diagnosis and treatment options<br />
regarding sepsis for preterm babies.<br />
Preparing our future talent<br />
Within our team, we have a culture of<br />
collaboration and this extends to young<br />
clinicians and <strong>research</strong>ers with high<br />
potential. They have opportunities to learn<br />
and train through our educational<br />
programs and to contribute to our overall<br />
societal impact through our outreach<br />
activities. Our multidisciplinary approach<br />
will lead to earlier diagnosis, tailored<br />
treatments and enable us to create new<br />
and better interventions to transform<br />
children’s lives.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 13
Protecting<br />
fertilityFor many,<br />
parent is one of the happiest<br />
days in life. Unfortunately,<br />
1 in 6 couples who want to<br />
conceive, fail to do so. This<br />
infertility has many different<br />
causes and we focus on<br />
reduced ovarian reserve<br />
and late effects of childhood<br />
cancer treatment.<br />
becoming a<br />
<br />
Helen Torrance and Frank Broekmans<br />
work at the Center for Reproductive<br />
Medicine which is an international<br />
and national expert center and global<br />
leader in the field of reproduction.<br />
Both care and <strong>research</strong> are aimed at<br />
optimizing the chances of a healthy<br />
conception and thereby the chances<br />
of a healthy child.<br />
14 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
ANTE- AND PERINATAL DAMAGE<br />
Helen Torrance MD,<br />
PhD specializes in<br />
reproductive medicine.<br />
She combines clinical<br />
and scientific <strong>research</strong><br />
related to fertility.<br />
Her current interests<br />
include future fertility<br />
for children with<br />
chronic disease and<br />
optimizing successful<br />
implantation.<br />
htorranc@umcutrecht.nl<br />
Changing IVF protocols<br />
Ovarian ageing and reduced ovarian reserve have been a main topic of<br />
<strong>research</strong> at the Center for Reproductive Medicine for more than 20 years,<br />
and we’ve answered many diagnostic, prognostic, etiologic and therapeutic<br />
questions. One of our most recent multicenter randomized controlled trials<br />
studied the efficacy of individual hormonal treatment for IVF. We<br />
demonstrated that high doses of hormones in women with a reduced<br />
ovarian reserve actually do not increase her chances of having a baby.<br />
Our findings have helped change long-standing IVF practice in which<br />
high-dose hormones were prescribed for infertility. This is especially<br />
important as there are concerns that IVF impacts the long-term health of the<br />
children conceived through this technique. Although still unclear,<br />
high hormone doses may be a causal factor.<br />
Caring for the entire reproductive life cycle<br />
Ovarian ageing can have a clear cause, be idiopathically or be iatrogenically<br />
caused by, for example, cancer treatment. We collaborate with the Princess<br />
Maxima Center to provide both care and <strong>research</strong> for children with cancer,<br />
focusing on early fertility counselling and fertility preservation.<br />
can be devastating.<br />
We’re Infertility<br />
improving care for these<br />
patients so more people can enjoy<br />
the exceptional path of parenthood.<br />
- Helen Torrance<br />
This type of lifecycle medicine and care is also important for children with<br />
other childhood diseases that used to be lethal but are now considered<br />
chronic diseases. These children need follow-up care directly related to their<br />
condition and sadly, disease progression and exposure to medication during<br />
childhood and adolescence may affect their reproductive system.<br />
More <strong>research</strong> into current and future fertility of these patients is needed.<br />
Mapping out infertility<br />
If patients have concerns about future fertility, then fertility counselling and<br />
fertility preservation should be offered to all individuals at risk as becoming<br />
a parent may significantly contribute to a long-term improved quality of life.<br />
From 2019 onwards, we expect to complement existing long-term child<br />
health follow-up databases with fertility parameters so that early<br />
determinants can be connected to late fertility outcome. Our team will start<br />
by including girls with chronic hematologic conditions (for example,<br />
Diamond Blackfan anemia, sickle cell anemia or thalassemia; in collaboration<br />
with the department of haematology (Bartels) and will then extend this<br />
concept to other childhood diseases.<br />
Frank Broekmans<br />
MD, PhD is devoted to<br />
the mysteries behind<br />
ageing ovaries. He<br />
focuses on assessing<br />
fertility in childhood<br />
disease survivors with<br />
the goal of preventing<br />
early life onset genetic<br />
disease. His group<br />
conducts Preimplantation<br />
Genetic Diagnostic<br />
testing of embryos<br />
created by Assisted<br />
Reproductive<br />
Technology.<br />
fbroekma@umcutrecht.nl<br />
time to be proactive - to provide<br />
preventative It’s<br />
care for infertility and<br />
to avoid reproductive consequences<br />
of childhood disease. - Frank Broekmans<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 15
CONGENITAL AND HEREDITARY DISORDERS<br />
ghaaften@umcutrecht.nl<br />
Finding genetic<br />
variations<br />
<br />
Your DNA<br />
at the<br />
center of<br />
care.<br />
- Hans Kristian<br />
Ploos van Amstel<br />
Gijs van Haaften,<br />
PhD focuses on<br />
understanding<br />
the genetics and<br />
biology of monogenic<br />
disorders, with<br />
a focus on metabolic,<br />
craniofacial and<br />
cardiac disorders.<br />
Genetic testing can identify<br />
aberrations and changes in our<br />
genetic information. This can<br />
help confirm or rule out<br />
suspected genetic diseases, it<br />
can identify hereditary genetic<br />
conditions and determine<br />
whether an unborn infant has<br />
a certain disorder. With the<br />
event of advanced genome<br />
sequencing technologies,<br />
genetic testing is becoming<br />
more routine in medical care.<br />
The Department of Genetics within the<br />
<strong>Child</strong> Health Program focuses on<br />
developing technologies for genetic<br />
diseases, in particular, on genome-wide<br />
detection of genetic variations. We aim to<br />
establish the relationship between<br />
clinical presentation, gene expression<br />
and protein function of both morbid<br />
genes (genes that are causally linked to<br />
disease) and candidate morbid genes.<br />
To address this, two national cooperative<br />
studies have been initiated and Hans<br />
Kristiaan Ploos van Amstel leads the<br />
diagnostic lab.<br />
WGS-based approach to<br />
understanding genetic diseases<br />
Whole genome sequencing (WGS)<br />
can identify almost all disease-causing<br />
mutations and has broad applicability in<br />
diagnostics, treatment and drug response.<br />
It has been therefore hypothesized<br />
whether a “one-test-fits-all” could be<br />
implemented to diagnose rare genetic<br />
disorders. This would increase diagnostic<br />
yield in a shortened time frame, reduce<br />
complexity and costs, result in early access<br />
to personalized patient care and reduce<br />
co-morbidity and mortality. We’re<br />
currently performing a study with patients<br />
from the neonatal intensive care unit and<br />
with neurodevelopmental disorders.<br />
A new blood test for prenatal<br />
genetic diagnosis<br />
Our second study is in collaboration with<br />
Wouter de Laat, PhD at the Hubrecht<br />
Institute. Together, we’ve developed<br />
a Monogenic Non-Invasive Prenatal<br />
Diagnosis (MG-NIPD), a new highly<br />
sensitive blood test, to detect<br />
monogenetic disorders during the early<br />
stages (8-10 weeks) of pregnancy.<br />
MG-NIPD can detect genetic diseases<br />
that have a small genetic variation, and<br />
may replace traditional, more invasive<br />
methods such as amniocentesis and<br />
chronic villus sampling. We’re currently<br />
validating and optimizing the MG-NIPD<br />
in at-risk families as a safe and reliable<br />
alternative for prenatal diagnosis.<br />
Understanding the biology of<br />
genetic disease<br />
For many genetic diseases, the precise<br />
genetic cause is not understood, and by<br />
studying genes and their functions in<br />
human health and disease, we gain<br />
insights into patient care and novel<br />
biological processes. We focus on the<br />
biology and genetics of rare diseases,<br />
with a particular interest in metabolic,<br />
craniofacial and cardiac anomalies;<br />
this area of investigation is led by<br />
Gijs van Haaften.<br />
A recent example is the discovery that<br />
germline mutations in histone H4 cause<br />
a developmental syndrome by altering<br />
DNA damage response and cell cycle<br />
control. We model patient mutations to<br />
study effects on gene and protein<br />
function, and use several approaches<br />
including patient cells, cell lines in<br />
which we introduce the patient-specific<br />
mutated allele and the zebrafish<br />
developmental model.<br />
We recently described a method to<br />
engineer the zebrafish genome at the<br />
single nucleotide level, using the geneediting<br />
technology CRISPR/Cas9 in<br />
combination with homology-directed<br />
repair. This allows us to generate precise<br />
models for human genetic disorders.<br />
We’re currently investigating whether<br />
certain therapies can reverse<br />
cardiovascular defects with the goal of<br />
translating our findings to patients<br />
in the future.<br />
jploos@umcutrecht.nl<br />
Hans Kristian<br />
Ploos van Amstel,<br />
PhD focuses his<br />
<strong>research</strong> on impro -<br />
ving detection and<br />
interpretation of<br />
genomic variations<br />
and on identifying<br />
disease genes.<br />
He strives to<br />
diagnosis, prognosis<br />
and treatment. He is<br />
chair of the Dutch<br />
Society for Clinical<br />
Genetic Laboratory<br />
Diagnostics (VKGL).<br />
16 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
CONGENITAL AND HEREDITARY DISORDERS<br />
truly connected<br />
interdisciplinary<br />
Our<br />
network<br />
enables swift transition<br />
from bedside to bench<br />
and back, directly<br />
supporting improvement<br />
of care for vulnerable<br />
patients.<br />
- Marc Lilien<br />
Kidney<br />
and Urinary tract<br />
An end stage renal disease patient is<br />
referred to the outpatient clinic for<br />
hereditary renal disease: The patient is<br />
diagnosed with an autosomal dominant<br />
renal disease. Recently, his first child was<br />
born with an autosomal dominant renal<br />
disease. This does not recur in a kidney<br />
graft. His eldest (at 50% risk) was<br />
subsequently evaluated at the pediatric<br />
hereditary renal disease outpatient clinic.<br />
Wishing to further establish their family,<br />
the couple was informed about their<br />
options and chose to try to conceive using<br />
preimplantation genetic diagnosis.<br />
aeerde@umcutrecht.nl<br />
mlilien@umcutrecht.nl<br />
Albertien van Eerde<br />
MD, PhD is clinical<br />
geneticist at the UMC<br />
Utrecht who specializes<br />
in nephrogenetics. She’s<br />
the coordinator of the<br />
Expert Center for<br />
Hereditary and Congenital<br />
Renal and Urinary<br />
Tract Disorders, which is<br />
accredited both<br />
nationally and by the EU<br />
(through ERKNET).<br />
Marc Lilien MD,<br />
PhD is a pediatric<br />
nephrologist at the<br />
Wilhelmina <strong>Child</strong>ren’s<br />
Hospital and has<br />
expertise in renal<br />
ciliopathies and renal<br />
tuberous sclerosis<br />
phenotypes.<br />
Our <strong>research</strong> in the kidney and urinary tract<br />
focuses on clinical expertise in the nationally<br />
accredited Center of Expertise for Hereditary and<br />
Congenital Nephrologic and Urologic Disorders.<br />
The Expert Center ensures optimal care and<br />
<strong>research</strong> for families with renal disease and spans<br />
infancy to adulthood, including preconception<br />
and prenatal care. It encompasses (pediatric)<br />
nephrology, (pediatric) urology, clinical and<br />
laboratory genetics, obstetrics, nephropathology,<br />
radiology, and we participate in ERKnet:<br />
the European Reference Network for Rare<br />
Kidney Disease.<br />
The case above is a good clinical example of the<br />
interdisciplinary nature of our work. When a<br />
diagnosis is challenging or undetermined, we<br />
incorporate genetic testing and functional follow<br />
up. This has proven effective for the ITGA3 gene.<br />
For insights into cystinosis-related phenotypes,<br />
we collaborate with Roos Masereeuw, PhD at<br />
Utrecht University who is an expert on how<br />
pharmacologics affect molecular pathways, and<br />
to further investigations into new candidate<br />
genes we collaborate with the Antignac’s group<br />
in Paris.<br />
We also perform cohort-based <strong>research</strong>. Albertien<br />
has shown that NPHP1 gene deletions can cause<br />
adult renal disease, which comprises about 0.5%<br />
of adult end stage renal disease at all ages. This<br />
challenges the paradigm that nephronophthisis is<br />
primarily a pediatric renal disease, and has<br />
consequences for follow up into adulthood and<br />
kidney donation, especially by siblings. We both<br />
actively participate in the AGORA cohort (for<br />
example, patients with congenital anomalies of<br />
the kidney and urinary tract and renal ciliopathies).<br />
Marc has recently published a detailed overview<br />
of renal ciliopathy phenotypes, and steps towards<br />
early biomarkers.<br />
With a recently acquired Dutch Kidney Foundation<br />
grant, Albertien will further establish a registry of<br />
patients with rare renal diseases, and will build a<br />
Kidney Gene Regulatory Network. We both also<br />
want to further the understanding of “renal<br />
sensitivity”: What drives the variability in severity<br />
in patients with similar genetic predisposition or<br />
toxic exposure.<br />
Genetic diagnoses have an effect in the full circle<br />
of life. And they are too often missed, especially in<br />
adult nephrology. Together, our <strong>research</strong> activities<br />
create synergy and we’re able to create impact for<br />
instance, by developing informational material<br />
(like online movies) for patients, by conceiving a<br />
national guideline for genetic testing in (pediatric)<br />
nephrology and by teaching pediatricians,<br />
nephrologists and geneticists, nationally and<br />
internationally. We often work together with the<br />
Dutch Kidney Patient Association.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 17
Congenital and genetic<br />
heart disorders<br />
Roughly 1 in 100 children<br />
have a congenital cardiac<br />
abnormality and about 1<br />
in 200 individuals have a<br />
gene mutation predisposing<br />
him or her to an inherited<br />
cardiac disorder including<br />
a cardiomyopathy or<br />
arrhythmia syndrome.<br />
More and more genes and<br />
mutations underlying these<br />
different cardiac disorders<br />
have been identified. Our<br />
departments of Genetics<br />
and Pediatric Cardiology<br />
are focused on elucidating<br />
these genetic defects and<br />
our discoveries advance<br />
both patient and family<br />
care, as well as <strong>research</strong>.<br />
Congenital heart<br />
defects have the<br />
highest prevalence<br />
of all congenital<br />
defects.<br />
- Hans Breur<br />
<br />
hbreur@umcutrecht.nl<br />
Hans Breur MD, PhD<br />
Pediatric cardiologist is<br />
one of the founders of<br />
the Congenital Heart<br />
Disease LifeSpan<br />
Program in which all<br />
patients with severe<br />
congenital heart disease<br />
undergo extensive and<br />
lifelong cardiac and<br />
neurocognitive<br />
follow-up, and where<br />
interventions are<br />
developed to improve<br />
outcome.<br />
In patient and family care, the results of a<br />
genetic test can be used for genetic<br />
counseling as it provides important<br />
information on inheritance patterns and<br />
aids with determining recurrence risk<br />
with a potential for prenatal diagnostics.<br />
In cases of a late onset autosomal<br />
dominantly inherited disease,<br />
presymptomatic genetic testing<br />
(where a genetic mutation may be<br />
detected before an individual presents<br />
with clinical symptoms) in family<br />
members can be facilitated with these<br />
genetic discoveries. Given the autosomal<br />
inheritance, this may lead to 50% fewer<br />
family members who require follow-up<br />
by a cardiologist.<br />
Unfortunately, clinical variability is still<br />
poorly understood: Individuals with an<br />
identical mutation can be symptomless<br />
for decades while close family members<br />
may encounter signs of the disease at an<br />
early age. And we still don’t know which<br />
factors contribute to disease<br />
development at what phase in life. Our<br />
<strong>research</strong>ers and clinicians collaborate<br />
with several patient organizations and<br />
together, we’re identifying factors that<br />
influence the development and<br />
progression of these disorders. From this,<br />
we can better determine risk and develop<br />
personalized treatments. In our<br />
diagnostic and therapeutic work-up we<br />
use cutting edge imaging techniques like<br />
3-D rotational angiography.<br />
Organizing our data<br />
In the Netherlands we closely collaborate<br />
with all other centers involved in<br />
Congenital and Cardiogenetic Disease<br />
within the Dutch National Working Group<br />
on cardiogenetic diseases.<br />
Within this multidisciplinary network of<br />
clinical and molecular geneticists,<br />
cardiologists, pediatric cardiologists and<br />
pathologists, we aim to improve<br />
diagnostics and care for these patients.<br />
We’ve initiated several large-scale patient<br />
registries, including the national<br />
18 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
CONGENITAL AND HEREDITARY DISORDERS<br />
jtintel3@umcutrecht.nl<br />
Peter van Tintelen,<br />
MD, PhD<br />
Chair, Department of<br />
Genetics<br />
is a clinical geneticist<br />
who set up cardiogenetics<br />
<strong>research</strong> at<br />
the UMC Groningen. In<br />
2018, he returned to<br />
Utrecht to become<br />
Chair of the Department<br />
of Genetics. The<br />
main focus of his<br />
<strong>research</strong> is understanding<br />
clinical variability<br />
in inherited cardiac<br />
disease.<br />
The worldwide impact<br />
of congenital heart disease is<br />
greater than cancer when<br />
looking at years lost to disability.<br />
Arrhythmogenic Cardiomyopathy Registry<br />
(www.acmregistry.nl) which contains data<br />
from over 1000 patients and family<br />
members, and the PLN Cardiomyopathy<br />
Registry, which has enrolled over 800<br />
patients who carry an identical mutation.<br />
Using these data, we’re able to improve<br />
risk prediction for patients and<br />
their families.<br />
Lifelong care for our patients<br />
All patients with a severe congenital<br />
heart defect enroll in our Congenital<br />
Heart Disease Life Span Program. In this<br />
program, life-long structured cardiac<br />
and neurocognitive follow-up starting<br />
from pre-natal diagnosis onwards, is<br />
combined with an extensive <strong>research</strong><br />
program including blood and tissue<br />
biobanking for all patients. A stateof-the-art<br />
pipeline including whole<br />
One in 250 children have a<br />
mutation predisposing for<br />
an inherited cardiomyopathy<br />
or arrhythmia syndrome.<br />
- Peter van Tintelen<br />
genome sequencing and zebrafish<br />
modeling (together with the Hubrecht<br />
institute) allows us to study the origin of<br />
congenital heart disease. Patients with<br />
inherited cardiomyopathies and<br />
arrhythmias enroll in our multidisciplinary<br />
life cycle follow-up, where families are<br />
counselled and treated by both the adult<br />
and pediatric cardiologists as well as a<br />
clinical geneticist.<br />
With current excellent survival rates,<br />
our focus needs to shift from mortality<br />
to quality of life.<br />
- Hans Breur<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 19
Better care for the rare<br />
Gastroenterology - Hepatology - Metabolic Diseases<br />
Metabolic diseases comprise a group of more than 1000 rare genetic diseases in which<br />
a metabolic pathway is perturbed. These conditions often have devastating<br />
consequences for patients and their families, and may involve a diagnostic odyssey,<br />
prognostic uncertainty and absence of treatment options. Our multidisciplinary<br />
<strong>research</strong>, in which laboratory and clinical scientists closely collaborate, aims to increase<br />
knowledge on these diseases in a number of ways.<br />
<br />
Let’s make use of<br />
the unprecedented<br />
technological possibilities<br />
to improve<br />
patient care in<br />
terms of diagnostics<br />
and (personalized)<br />
therapies.<br />
- Sabine Fuchs<br />
Disease discovery<br />
In undiagnosed patients with a<br />
metabolic phenotype, whole exome<br />
sequencing, metabolomics and deep<br />
phenotyping are combined to elucidate<br />
existing and new defects. When we find<br />
a candidate gene with related changes in<br />
the metabolome or phenotype of a<br />
patient, we perform functional studies in<br />
cells or organoids from the patient or<br />
after CRISPR-Cas9 gene-editing or in<br />
animal models like the zebrafish to<br />
identify and characterize new genetic<br />
metabolic diseases. In recent years, we<br />
have collaboratively described two new<br />
defects in the malate aspartate shuttle,<br />
two defects in glutamate metabolism<br />
and a defect in ketone utilization.<br />
This approach has also elucidated 8<br />
inborn errors outside the classical<br />
boundaries of metabolism (STX3,<br />
NSMCE3, UNC13A, ANKZF1, PET117<br />
(complex iv), KIAA1109, TRAPPC2L,<br />
SMARCC2). In all families involved, these<br />
discoveries have led to long-awaited<br />
diagnoses and prenatal screening<br />
possibilities, and in some, to successful<br />
treatment of affected children.<br />
Pathogenesis of disease<br />
We focus on defects in vitamin B6 and<br />
amino acid metabolism. To pave the way<br />
for better treatments, our team<br />
investigates pathogenic mechanisms in<br />
these defects making use of deep<br />
phenotyping, metabolomics and model<br />
systems. We’ve published a zebrafish<br />
model of pyridoxine dependent epilepsy,<br />
a mouse model of pyridoxal phosphatase<br />
deficiency and a new cause of vitamin<br />
B6-dependent epilepsy: pyridoxal<br />
phosphate binding protein deficiency.<br />
Similarly, these strategies have<br />
contributed to the discernment and<br />
publishing of a common clinical<br />
phenotype for amino acid tRNAsynthetase<br />
deficiencies, putatively based<br />
on a common disease mechanism.<br />
Follow-up of treatment<br />
Patients with lysosomal storage disease<br />
can be treated with stem cell therapy.<br />
Although this can be successful, residual<br />
disease is substantial. To address this, we<br />
make use of a unique standardized<br />
multidisciplinary follow-up facility<br />
(Sylvia Toth Center; also used for deepphenotyping)<br />
to investigate the natural<br />
history of these diseases, and clinical and<br />
biochemical follow-up of patients who<br />
have been transplanted. Examples of<br />
novel biochemical markers include the<br />
analysis of iduronidase in blood spots<br />
and saliva, analysis of glycosaminoglycans<br />
in tear drops by mass spectrometry and<br />
analysis of vacuoles in lymphocytes as a<br />
marker for neuronal ceroid lipofuscinosis.<br />
Organoid <strong>research</strong><br />
In close collaboration with groups at the<br />
Hubrecht Institute, we generate liver and<br />
intestinal organoids from patient-derived<br />
adult stem cells. These organoids<br />
represent a unique patient-specific in<br />
vitro model that we use to elucidate<br />
disease mechanisms, develop novel<br />
therapeutic strategies (including<br />
organoid transplantations) and test these<br />
strategies in a personalized manner.<br />
This led to the identification of novel<br />
causes of secretory diarrhea (due to<br />
deficiencies of STX3 and DGAT1).<br />
Furthermore, we’re in the process of<br />
evaluating small molecule therapy for<br />
genetic cholestatic diseases, such as<br />
progressive familial intrahepatic cholestasis.<br />
20 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
CONGENITAL AND HEREDITARY DISORDERS<br />
nverhoev@umcutrecht.nl<br />
Nanda Verhoeven<br />
PhD has a special<br />
interest in disorders<br />
of vitamin B6 and amino<br />
acid metabolism and<br />
the discovery of new<br />
diseases in this area.<br />
Nanda is Head Laboratory<br />
Metabolic Diseases.<br />
sfuchs@umcutrecht.nl<br />
Sabine Fuchs MD,<br />
PhD is a pediatrician in<br />
metabolic diseases,<br />
pharmacist and basic<br />
scientist with a lab in<br />
the Hubrecht institute,<br />
with the aim to improve<br />
care for patients with<br />
metabolic/liver diseases<br />
by unraveling disease<br />
mechanisms (in patient<br />
derived organoids) to<br />
develop and test novel<br />
treatment strategies,<br />
including liver stem cell<br />
transplantations.<br />
phassel2@umcutrecht.nl<br />
Peter van Hasselt MD,<br />
PhD focuses on translational<br />
<strong>research</strong> aimed at<br />
creating 'better care for<br />
the rare' by 1) elucidating<br />
the genetic cause; 2)<br />
describing effects of<br />
treatment on the natural<br />
disease course; 3)<br />
improving early recognition<br />
and/or preventive<br />
measures; and 4)<br />
creating novel diseaseseverity<br />
markers.<br />
jjans@umcutrecht.nl<br />
Judith Jans PhD<br />
focuses on the development<br />
and introduction of<br />
untargeted metabolomics<br />
in diagnostics to<br />
elucidate novel genetic<br />
metabolic diseases and<br />
improve current<br />
diagnostic practice. She<br />
aspires to fully integrate<br />
genomics and metabolomics<br />
data to advance<br />
patient care.<br />
<br />
Ask yourself how the present<br />
situation compares to your ideal<br />
situation, and how it helps you<br />
see how to decrease the gap.<br />
- Peter van Hasselt<br />
<br />
A solid diagnosis<br />
is the foundation<br />
on which care and<br />
treatment can<br />
be built.<br />
- Nanda Verhoeven<br />
In our labs, technology development is a<br />
driving force for the above-mentioned<br />
projects. We’ve developed a direct<br />
infusion high-resolution mass spectrometric<br />
pipeline for untargeted metabolomics.<br />
We’ve validated this approach<br />
in blood spots and plasma from a number<br />
of patients with known genetic metabolic<br />
diseases and demonstrated that this<br />
method is capable of correctly<br />
establishing diagnoses. This approach is<br />
promising for disease discovery,<br />
identification of biomarkers and for<br />
<strong>research</strong> on pathogenic processes. In<br />
addition, we employ frontline geneediting,<br />
organoid technologies and<br />
animal models for in vitro modeling. The<br />
strong clinical embedding, with an<br />
interest in patients with novel genetic<br />
metabolic defects, deep phenotyping<br />
and use of the human phenotype<br />
ontology informs our <strong>research</strong> on the<br />
clinical presentation and natural course<br />
of known and novel disease entities.<br />
In the Netherlands, we collaborate with<br />
the five other University Medical Centers<br />
in a national initiative, United for<br />
Metabolic Diseases. This multidisciplinary<br />
consortium consists of pediatricians,<br />
internists, clinical geneticists, laboratory<br />
specialists and scientists in the field of<br />
genetic metabolic disease and patient<br />
organizations. We aim to improve<br />
registration, education, technology and<br />
e-health and to find a diagnosis for 500<br />
undiagnosed patients, both children and<br />
adults, by combining multi-omics<br />
technologies and bioinformatics. The<br />
first patients were included in<br />
March/May 2019.<br />
<br />
Significant<br />
advances in<br />
diagnostics can<br />
be made when<br />
we successfully<br />
combine the<br />
diverse strengths<br />
of metabolomics<br />
and genomics.<br />
- Judith Jans<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 21
SEVERE INFLAMMATORY DISORDERS<br />
Cystic Fibrosis:<br />
personalized treatment<br />
for all patients<br />
<br />
We are honored to be<br />
selected to participate in the<br />
HIT-CF Europe consortium and<br />
join forces with key thought<br />
leaders to explore the potential of<br />
a personalized medicine<br />
approach as a possible new<br />
frontier for CF therapy.<br />
- Meenu Chhabra, President and Chief<br />
Executive Officer of Proteostasis<br />
22 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
SEVERE INFLAMMATORY DISORDERS<br />
The UMC Utrecht hosts the largest<br />
expertise center for Cystic Fibrosis (CF) in<br />
the Netherlands, giving care to about onethird<br />
of more than 1500 Dutch CF<br />
patients. Our multidisciplinary team, led<br />
by Kors van der Ent, MD (pediatric<br />
pulmonologist) and Harry Heijerman, MD,<br />
PhD (adult pulmonologist) covers the<br />
entire spectrum of care from heel prick<br />
screening to lung transplantation. In<br />
addition, we have our own clinical <strong>research</strong><br />
team, which supports investigator-driven<br />
and pharmaceutical-driven clinical trials.<br />
These trials have focused on treatment of<br />
pulmonary inflammation and infection<br />
(microbiome studies) and on the effects<br />
of CFTR-modulators.<br />
Chloride Concentration and intestinal current<br />
measurements.<br />
Organoids in drug discovery<br />
Preclinically, organoids are used to identify and<br />
develop CFTR-modulating drugs and to explore<br />
mechanisms associated with differences in CFTR<br />
function. Pharmaceutical companies use intestinal<br />
organoids in their drug development pipeline<br />
and initial high-throughput-screening has<br />
resulted in the discovery of different chemical<br />
structures as potential CFTR-modulating drugs.<br />
Organoids are used to test both the potency of<br />
single drugs and to compare the efficacy of<br />
combination treatments. Our group also<br />
highlighted the translational potential of<br />
organoids, demonstrating that genotype-specific<br />
effects of CFTR-modulators correlate with clinical<br />
trial data at group level.<br />
Our CF Center leads the cystic fibrosis core<br />
network of the European Reference Network<br />
LUNG (ERN-LUNG), a network of European<br />
healthcare providers dedicated to ensuring and<br />
promoting excellence in care and <strong>research</strong> for the<br />
benefit of patients affected by rare respiratory<br />
diseases. We’re also a member of the Clinical Trial<br />
Network of the European CF Society, and have<br />
participated in the European CF Patient Registry<br />
for more than 10 years, enabling quality control<br />
and studying long-term patient outcomes.<br />
A formal collaboration agreement between the<br />
UMC Utrecht and the Dutch CF Patient<br />
organization was signed in 2016 and joint<br />
initiatives between patients and caregivers have<br />
been developed.<br />
Organoid technology<br />
Our CF Center Utrecht has its own <strong>research</strong> lab<br />
headed by Jeffrey Beekman, PhD, and the close<br />
collaboration between basic science and clinical<br />
care in Utrecht has led to a highly translational<br />
<strong>research</strong> profile. His <strong>research</strong> group developed an<br />
adult stem cell-based culture and assay<br />
technology (organoids) to model human<br />
pulmonary disease and in particular, CF.<br />
Organoids are three-dimensional, multi-cellular<br />
structures that recapitulate tissue features of the<br />
parental organ and are usually grown from donor<br />
tissue fragments. As organoids are functional<br />
expressions of individual genomes, they’re<br />
particularly useful for understanding how genetic<br />
factors contribute to individual disease. Intestinal<br />
organoids have been at the forefront of these<br />
developments as culture methodology was first<br />
developed for this tissue source. For CF, human<br />
intestinal organoids can be grown from intestinal<br />
crypt fragments isolated from rectal biopsies.<br />
We’ve shown that organoid measurements reflect<br />
residual CFTR function and correlate with<br />
predicted severity of the CF genotype and other<br />
biomarkers of CFTR function, including Sweat<br />
Promising drug treatments for CF<br />
Recent proof-of-concept in two patients with<br />
ultra-rare mutations showed clear in vitro-in vivo<br />
correlation in response to treatment with the drug<br />
ivacaftor. A subsequent study found that intestinal<br />
organoid measurements with the drugs curcumin,<br />
genistein, ivacaftor and lumacaftor/ivacaftor<br />
correlated with in vivo responses in pulmonary<br />
function and sweat chloride concentrations on the<br />
individual level. These techniques have<br />
revolutionized CF care, especially in patients with<br />
ultra-rare mutations. New mutation class-specific<br />
drugs are currently only being tested in patients<br />
with well-described, very common mutations.<br />
As a result, market authorization and<br />
reimbursement of these drugs is only granted in<br />
these specific subsets of patients. Nevertheless,<br />
other patients with less common mutations might<br />
also benefit from them.<br />
Using organoids to predict<br />
treatment response<br />
In our group, Kors coordinates an EU-funded<br />
consortium study (www.HITCF.org) which aims to<br />
develop a path for access to therapies for<br />
individual patients or patient groups who show<br />
positive response to the therapy in an organoid<br />
test, and to pave the way for organoid-based<br />
personalized medicine. Our organoid studies in<br />
CF focus on pre-treatment selection of patients<br />
with ultra-rare CFTR-variants and biopsies of<br />
patients with ultra-rare CFTR mutations are<br />
collected all over Europe and bio-banked in<br />
Utrecht. Currently four pharmaceutical companies<br />
deliver their lead CFTR-modulating compounds<br />
for screening and ultimately clinical trials in<br />
pre-selected patient groups are foreseen, in close<br />
collaboration with the European Medical Agency<br />
and MoCA (Mechanisms of Coordinated Access<br />
to Orphan Medicinal Products).<br />
cent@umcutrecht.nl<br />
jbeekman@umcutrecht.nl<br />
Kors van der Ent,<br />
MD, PhD initiated the<br />
CF-Center Utrecht in<br />
1997. He is a co-developer<br />
of the Utrecht<br />
organoid model for CF.<br />
Kors is coordinator of<br />
the H2020 HIT-CF<br />
program and core<br />
network leader for CF<br />
in the European<br />
Reference Network<br />
(ERN-LUNG).<br />
Jeffrey Beekman,<br />
PhD heads a <strong>research</strong><br />
program focused on<br />
development of<br />
personalized medicine<br />
for CF. His work aims<br />
to develop new<br />
diagnostics and<br />
therapeutics to enable<br />
individually optimized<br />
treatments.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 23
We are extremely excited to be<br />
participating in the HIT-CF <strong>research</strong><br />
project, which has the potential to<br />
lead to treatment options for many<br />
CF patients, based on their<br />
<br />
functional responses in the lab.<br />
- Dr. Gregory Williams, Chief Operating Officer, Eloxx Pharmaceuticals<br />
The patient not only<br />
thinks along, but<br />
decides. The patient<br />
perspective must be<br />
considered for care<br />
and <strong>research</strong>.<br />
What is important<br />
for CF patients and<br />
what <strong>research</strong> is<br />
needed?<br />
- Jacquelien Noordhoek, Director,<br />
Dutch CF Foundation<br />
Ethics<br />
and innovation<br />
are natural partners,<br />
In fact, you would like<br />
doctors and <strong>research</strong>ers to<br />
always think about the ethical<br />
and social impact of their<br />
innovation at an early stage.<br />
<br />
Patients can think along about the design<br />
of the technology and become<br />
co-designers.<br />
- Annelien Bredenoord, Professor,<br />
Ethics of Biomedical Innovation<br />
My experience gave me new insights. For example, how important it is for doctors to express<br />
their confidence in me as a parent. As a mother you are defeated and powerless, you dare not<br />
attach yourself for fear of loss. It is also very supportive if the doctor fulfills the role of a mental<br />
coach and encourages you. Parents must play a central role; parental love is the best medicine.<br />
Benjamin is now eight years old. He is healthy and goes to school. I often drive past the<br />
Wilhelmina <strong>Child</strong>ren's Hospital - and I always have a deep sense of gratitude.<br />
- Anne Marie Louwerse, mother of Benjamin, who was born at barely 25 weeks.<br />
<br />
~<br />
24 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
SEVERE INFLAMMATORY DISORDERS<br />
Inflammatory<br />
Bowel Disease<br />
Inflammatory bowel disease (IBD) is a complex disorder associated with a<br />
dysregulated immune response to environmental triggers in a genetically<br />
susceptible host. The incidence of IBD is increasing around the world:<br />
Approximately 25% of patients with IBD present before the age of 20, with an<br />
annual pediatric incidence of 0.5 to 23/100,000 person-years in Northern and<br />
Western Europe. The cause of this increase is poorly understood, but proposed to<br />
include increased antibiotic use, changes in diet and the adoption of prepared<br />
foods that include emulsifiers and surfactants, all of which contribute to<br />
alterations in the gut microbiome.<br />
Saskia van Mil,<br />
PhD Associate<br />
Professor<br />
studies the roles<br />
of microbiota, bile<br />
acids and their<br />
receptors in health<br />
and chronic<br />
infla-mmatory<br />
diseases, e.g.<br />
Inflammatory<br />
Bowel Disease<br />
and non- alcoholic<br />
steatohepatitis.<br />
smil2@umcutrecht.nl<br />
Small bugs can make a big difference<br />
In children with Crohn’s disease, exclusive<br />
enteral nutrition is the therapy of choice for<br />
remission induction with remission rates<br />
comparable to steroids, indicating that nutrition<br />
plays an important role in IBD activity. Even<br />
though several dietary factors have been<br />
implicated in the pathogenesis of IBD, their<br />
relative importance and exact role is unknown.<br />
Current <strong>research</strong> on the interactions between<br />
food, microbiome and IBD are based on crosssectional<br />
cohort studies, which do not catch the<br />
changes in diet and microbiome prior to the<br />
development of an IBD flare. In addition,<br />
microbiome <strong>research</strong> has focused on the<br />
difference in the microbial species between IBD<br />
patients and controls, and in IBD patients in and<br />
out of an inflammatory episode. The most<br />
imminent questions that we are currently<br />
investigating are: what are the metabolic<br />
functions of these differentially present<br />
microbes, how do those functions affect host<br />
metabolism and IBD activity and what are the<br />
effects of dietary changes?<br />
Our <strong>research</strong> contributes to the cycle of life<br />
theme of <strong>Child</strong> Health, by gaining a better<br />
understanding of the nutrition-microbiome-bile<br />
acid-host health axis, and pursuing development<br />
of non-invasive biomarkers and novel therapies<br />
for IBD.<br />
acids act as<br />
hormones Bile<br />
and dictate<br />
microbiome composition<br />
and host metabolism.<br />
- Saskia van Mil<br />
25% IBD cases<br />
diagnosed during<br />
<strong>Child</strong>hood<br />
A potential therapeutic target<br />
In addition, our previous work has contributed<br />
to our current knowledge on bile acids as a<br />
treatment target for IBD. Bile acids activate the<br />
bile acid receptor FXR, which regulates the fate<br />
of dietary components; it also counteracts<br />
inflammation and controls the composition and<br />
abundance of gut bacteria. In IBD patients, the<br />
expression and function of FXR is suppressed.<br />
In collaboration with TES Pharma, we’re<br />
developing tissue and gene-selective FXR<br />
ligands for the treatment of IBD.<br />
Up to 1 in 4 cases of IBD are<br />
diagnosed during childhealth<br />
6x<br />
To develop<br />
More<br />
likely<br />
Colorectal<br />
cancer<br />
IBD patients are six times<br />
more likely to develop<br />
colorectal cancer.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 25
RSV & Rotavirus:<br />
so much in common<br />
Translational<br />
<strong>research</strong> is<br />
needed to<br />
improve the<br />
health of<br />
children.<br />
- Louis Bont<br />
<br />
lbont@umcutrecht.nl<br />
Louis Bont, MD, PhD<br />
has an interest in understanding,<br />
preventing and treating<br />
respiratory syncytial virus<br />
(RSV) bronchiolitis. He was<br />
one of the founders of the<br />
TULIPS program, which<br />
furthers the career of<br />
multidisciplinary early stage<br />
<strong>research</strong>ers in the field of<br />
child health.<br />
Infant mortality is a major global health threat and the most<br />
prevalent clinical syndromes are diarrhea and respiratory<br />
infection. According to a Global Burden of Diseases study<br />
conducted by the Institute for Health Metrics and Evaluation<br />
at Washington University, rotavirus and respiratory syncytial<br />
virus (RSV) are the primary causes of infant diarrhea and<br />
infection, respectively.<br />
In a retrospective case series, we’ve demonstrated that indeed, most children<br />
dying from an RSV infection are younger than 6 months of age. The World Health<br />
Organization has prioritized vaccine development for rotavirus and RSV infections;<br />
rotavirus vaccines have now been introduced and it’s expected that RSV vaccines will<br />
soon follow.<br />
RSV is the<br />
second<br />
cause of<br />
death<br />
during<br />
infancy<br />
worldwide<br />
Within the <strong>Child</strong> Health Program, we also prioritize rotavirus and RSV, which have<br />
much in common. Both are RNA viruses with exclusive tropism for the epithelium.<br />
Although each virus itself is genetically diverse, it appears that, while genetic diversity<br />
is needed to escape the immune system, it doesn’t contribute to disease severity.<br />
<strong>Child</strong>ren with co-morbidities, such as preterm birth, have the highest risk of a severe<br />
course of disease, including death.<br />
Developing a vaccine is complicated<br />
Viruses are excellent at evading our immune system, which makes developing an<br />
effective vaccine challenging. An early formalin-inactivated RSV vaccine developed<br />
the 1960s was a disappointment. Rather than prevent infection, it augmented RSV<br />
disease in vaccine recipients upon natural infection in the community; two immunized<br />
infants died upon infection and the clinical trial was abruptly ended. Several decades<br />
later, the first rotavirus vaccine Rotashield® was approved for infant gastroenteritis.<br />
Unfortunately, it increased susceptibility to intussuception, a rare form of bowel<br />
obstruction where the bowel folds upon itself. Upon investigation, it was concluded<br />
that Rotashield® did contribute to or increased the risk of intussuception and the<br />
vaccine was withdrawn from the market.<br />
26 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
SEVERE INFLAMMATORY DISORDERS<br />
Viruses also infect older patients<br />
RSV and rotavirus infections also cause severe disease throughout life.<br />
An RSV infection during infancy is associated with recurrent wheeze and asthma.<br />
We conducted a multicenter, double-blind, randomized placebo-controlled MAKI<br />
clinical trial and showed that RSV is causally-related to infant wheeze. In older<br />
adults, RSV is associated with similar incidence and severity compared with<br />
influenza. Rotavirus can cause acute gastroenteritis throughout life, but is especially<br />
severe in immunocompromised adults and frail elderly. In general, increased<br />
awareness of severe RSV and rotavirus infection in adults is needed.<br />
pbruijni@umcutrecht.nl<br />
Patricia Bruijning, MD,<br />
PhD focuses on vaccinepreventable<br />
diseases, which is a<br />
central theme in epidemiological<br />
<strong>research</strong>. She aims to<br />
optimize vaccination strategies<br />
for infants and children with a<br />
special focus on medicallyvulnerable<br />
pediatric<br />
populations.<br />
It takes a village<br />
Our aim in <strong>Child</strong> Health is to contribute to the development and implementation of<br />
vaccines against RSV and rotavirus. We conduct our <strong>research</strong> as part of large<br />
national and international consortia, including RIVAR, RESCEU, ReSViNET and RSV<br />
GOLD. The RIVAR-program (Risk-Group Infant Vaccination against Rotavirus) aims to<br />
implement a hospital-based rotavirus vaccination program for high-risk infants;<br />
the IMI-funded RESCEU project informs the European Union of the RSV burden in<br />
Europe before future introduction of RSV vaccines; Louis Bont is the founding<br />
chairman of the ReSViNET Foundation, which brings together a global network of<br />
stakeholders in order to decrease the vurden of RSV infection; and The Bill and<br />
Melinda Gates Foundation-funded RSV GOLD project studies clinical characteristics<br />
of children dying from RSV infection. By defining age distribution of RSV-related<br />
deaths we can guide impact analysis of future maternal RSV vaccines.<br />
Together with our collaborators in other areas, including Linde Meyaard, PhD<br />
(immune dysfunction in HIV), Jeanette Leusen, PhD (therapeutic antibodies) and<br />
Jose Borghans, PhD (leukocyte dynamics), we’re characterizing virus transmission<br />
dynamics and conducting health economic evaluations of vaccination strategies.<br />
We’re gaining a better understanding of disease pathogenesis, and developing<br />
effective and affordable preventive interventions and immunodiagnostic tools.<br />
<br />
Prevention is better than treatment.<br />
- Patricia Bruijning<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 27
Pediatric Rheumatology:<br />
Collaboration is essential<br />
The Pediatric Rheumatology Department, Wilhelmina <strong>Child</strong>ren’s<br />
Hospital is comprised of both basic science and clinical <strong>research</strong> groups.<br />
These include a joint pediatric rheumatology <strong>research</strong> group, led by<br />
Bas Vastert, MD, PhD and Jorg van Loosdregt-Vastert, PhD; a translational<br />
immunology lab headed by Femke van Wijk, PhD; and <strong>research</strong> by several<br />
clinical pediatric rheumatology groups, including Joost Swart, MD, PhD,<br />
Nico Wulffraat, MD, PhD and Sytze de Roock, PhD (Juvenile Idiopathic<br />
Arthritis, JIA) and Annet van Royen, MD, PhD (Juvenile Dermatomyositis).<br />
Together, we have a longstanding track record of studying<br />
chronic inflammatory disorders in children.<br />
bvastert@umcutrecht<br />
Bas Vastert, MD,<br />
PhD is a pediatric<br />
rheuma-tologist with<br />
expertise in translational<br />
immunology. He’s<br />
passionate about<br />
developing novel,<br />
biologically informed<br />
therapeutic strategies<br />
to personalize the<br />
treatment for juvenile<br />
idiopathic arthritis.<br />
This truly translational <strong>research</strong> collaboration, where basic immunological scientists and clinician<br />
scientists work together, lies at the heart of the acknowledgement of our department as a EULAR<br />
Center of Excellence in pediatric rheumatology – we’re only the 2nd pediatric rheumatology<br />
center worldwide. And thanks to the efforts of Nico, who has led several European Union funded<br />
collaborations including Pharmachild (European Pharmacovigilance register) and SHARE<br />
(developing evidence and consensus based guidelines on rare pediatric rheumatic diseases),<br />
our ability to have a real impact on patient care is excellent.<br />
Juvenile Idiopathic Arthritis (JIA)<br />
We cover a broad spectrum of chronic inflammatory diseases in children, with a particular interest<br />
in JIA, a chronic autoimmune disease characterized by arthritis and clinical presentation of<br />
systemic inflammation. In addition, we’re focused on finding off-label uses for existing drugs or<br />
alternative combinations of drugs in order to improve treatment strategies, and we perform<br />
clinical trials based on the fundamental <strong>research</strong> we perform in our labs.<br />
In 2014, we reported the first prospective cohort study of a first-line therapy with recombinant<br />
IL-1Ra in children with new-onset JIA; the majority of patients responded quickly and could stop<br />
treatment within one year. Based on <strong>research</strong> in our department, we postulate that timing of<br />
recombinant IL-1Ra administration could be change disease progression. Since then, we’ve<br />
initiated a the Early Stop of targeted Treatment in Systemic JIA (ESTIS), a ZonMw Rational<br />
Pharmacotherapy-sponsored clinical trial, where we’re testing IL-18 as a therapy response<br />
biomarker in systemic JIA in a multicenter clinical trial in the Netherlands.<br />
Another example of off-label use is nicotinamide, also known as vitamin B3, which is used as a<br />
dietary supplement and to treat acne and skin cancers. Most recently, we’ve planned a study to test<br />
whether nicotinamide can act as a regulatory T-cell-inducing compound in a stop strategy of<br />
biologicals and/or methotrexate (a chemotherapeutic agent and immune system suppressant),<br />
which are used as maintenance treatments in non-systemic JIA.<br />
From an immunology perspective<br />
We’re also understanding epigenetic and epitranscriptomic regulatory mechanisms that modulate<br />
immune homeostasis and might be dysregulated in chronic inflammatory (autoimmune) diseases<br />
like JIA. We’re using JIA as a model to study fundamental immune-regulatory mechanisms, and<br />
by combining our findings and observations from both the lab and the clinic, we can gain<br />
insight into the complex interplay between the molecules and pathways involved in<br />
pediatric inflammatory conditions.<br />
We also focus on juvenile dermatomyositis (JDM) from an immunological point of view, where we’re<br />
identifying distinctive and overlapping molecular mechanisms in order to develop early precision<br />
treatment approaches. Together Annet and Femke, have discovered and validated a novel robust<br />
jloosdre@umcutrecht.nl<br />
Jorg van Loosdregt,<br />
PhD is a fundamental<br />
immunologist who<br />
aims to translate<br />
fundamental discoveries<br />
into novel<br />
therapeutic strategies.<br />
He loves collaborating<br />
with experts in other<br />
fields of <strong>research</strong>.<br />
28 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
SEVERE INFLAMMATORY DISORDERS<br />
<br />
Here in the city of Utrecht, we work together with all<br />
kinds of organizations to ensure that children who<br />
want to exercise within their means enjoy sports.<br />
And that children coming from the hospital can work<br />
out at a sports club nearby. We do this with partner<br />
organizations in the ‘Sport op Maat’-network and the<br />
Wilhelmina <strong>Child</strong>ren's Hospital.<br />
- Victor Everhardt, counciler of Utrecht<br />
<br />
Translational immunology<br />
is much<br />
more than a linear<br />
process; it’s based<br />
on perpetuating<br />
circles of knowledge<br />
and implementation,<br />
fueled by different<br />
disciplines.<br />
- Femke van Wijk<br />
fwijk@umcutrecht.nl<br />
Femke van Wijk,<br />
MD, PhD focuses on<br />
the role of T cells in<br />
(tissue) homeostasis<br />
and chronic inflammation.<br />
She enjoys<br />
training and mentoring<br />
young scientists.<br />
marker for disease activity in JDM that can guide precision treatment; this is now being tested<br />
in a large international multicenter setting. In other studies. Femke has also contributed to the<br />
understanding of immune regulation in JIA, by proposing the paradigm of human T-cell<br />
resistance to regulation. Together with the pediatric rheumatology <strong>research</strong> group, she’s<br />
recently described a role for regulatory T-cell programming in JIA joint inflammation.<br />
Surprisingly, this regulatory T-cell signature is not only present in JIA and rheumatoid arthritis,<br />
but also in tumors, demonstrating conservation of developmental pathways across different<br />
diseases.<br />
The close-knit interaction of our team members, together with our breadth of expertise, allows<br />
us to expand our current understanding of the intricate mechanisms that facilitate inflammation<br />
in the joints of JIA patients. As translational scientists, we rely on both clinical and lab<br />
observations to ask the right questions and design smart experimental and clinical studies.<br />
Our ultimate aim is to identify novel therapeutic targets for the treatment of this disease.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 29
POST-ONCOLOGY<br />
Improving care for<br />
oncology PICU patients<br />
Marry van den<br />
Heuvel-Eibrink MD,<br />
PhD Pediatric Oncologist<br />
focuses on renal<br />
tumors and (genetic)<br />
variation of toxicity in<br />
childhood cancer.<br />
Roelie Wösten-van<br />
Asperen MD, PhD is<br />
a pediatric intensivist<br />
whose <strong>research</strong> focuses<br />
on pediatric cancer<br />
patients admitted to<br />
PICU. She is the chair of<br />
the PICU Oncology Kids<br />
in Europe Research<br />
group (POKER)<br />
rasperen@umcutrecht.nl m.m.vandenheuvel-eibrink@prinsesmaximacentrum.nl<br />
Survival rates for children with<br />
cancer have improved over the past<br />
20 years; however, intensified<br />
concomitant treatment has resulted<br />
in the fact that 40% of patients<br />
require at least one pediatric<br />
intensive care unit (PICU) admission<br />
throughout their disease course,<br />
and PICU mortality rates are higher<br />
(around 30%) compared to those of<br />
other PICU subcohorts. In addition,<br />
PICU mortality has remained<br />
relatively unchanged over the past<br />
decades, in contrast to the <strong>research</strong>led<br />
improvements observed in<br />
adults with cancer admitted to<br />
intensive care unit.<br />
Identifying critically ill pediatric cancer<br />
patients. It’s crucial to timely identify critically<br />
ill hospitalized cancer patients in order to<br />
prevent further clinical deterioration by<br />
providing early-required treatment. In this<br />
high-risk population, we need tools that<br />
differentiate early between ‘relatively well’<br />
and ‘critically ill’ patients (requiring PICU<br />
admission). We’ve launched an interdisciplinary<br />
<strong>research</strong> project between the PICU,<br />
Wilhelmina <strong>Child</strong>ren’s Hospital and the<br />
Princess Máxima Center, which aims to<br />
determine the predictive value of the<br />
Bedside Pediatric Early Warning Score<br />
(BedsidePEWS) for the identification of<br />
<br />
PICU mortality rates of<br />
pediatric cancer patients<br />
are far higher when<br />
compared to current<br />
mortality rates of the<br />
general PICU population.<br />
- Roelie Wösten-van Asperen<br />
critically ill pediatric cancer patients and, if<br />
necessary, to optimize the score for its use in<br />
this specific patient population. This will<br />
facilitate timely identification, referral to and<br />
treatment at the PICU and result in improved<br />
survival and reduced morbidity.<br />
PICU Oncology Kids in Europe Research<br />
group (POKER) There is little to no data on<br />
changes in clinical conditions in pediatric<br />
cancer patients preceding PICU admission;<br />
there is also no outcome data available. More<br />
<strong>research</strong> is needed to improve our ability to<br />
timely recognize clinical deterioration and to<br />
appropriately treat our patients. Recognizing<br />
the need for international collaboration on<br />
this issue, we established the PICU Oncology<br />
Kids in Europe Research group (POKER),<br />
comprising of 10 PICUs which belong to large<br />
pediatric oncological centers in seven<br />
different countries (the Netherlands,<br />
Belgium, Denmark, Germany, Switzerland,<br />
United Kingdom and France), and is endorsed<br />
by the European Society for Pediatric and<br />
Neonatal Intensive Care. As a first step,<br />
POKER aims to obtain consensus in<br />
determining the top <strong>research</strong> and core<br />
outcome priorities for pediatric cancer<br />
patients in a PICU for the next 10 years.<br />
Our mission in<br />
pediatric oncology<br />
<strong>research</strong> is to<br />
improve cure rates<br />
for all children and<br />
to enhance quality<br />
of survival.<br />
- Marry van den Heuvel-Eibrink<br />
30 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
POST-ONCOLOGY<br />
The endocrine<br />
system and cancer<br />
Hanneke van<br />
Santen, MD PhD<br />
is a pediatric endocrinologist<br />
with a focus on<br />
damaged endocrine<br />
systems in children.<br />
Endocrine effects of<br />
cancer treatment in<br />
childhood, thyroid<br />
tumors and craniopharyngioma.<br />
In 2013, she moved to<br />
Utrecht to support the<br />
new Princes Máxima<br />
initiative and coordinate<br />
endocrine care for<br />
children with cancer.<br />
hsanten@umcutrecht.nl<br />
It’s estimated that about 80% of pediatric<br />
cancer survivors reach the 5-year mark;<br />
however, about 50% of all patients<br />
experience an endocrine adverse event.<br />
Endocrine disorders in children with cancer<br />
can be caused by the tumor itself or by<br />
treatment. <strong>Child</strong>ren need an intact endocrine<br />
system for normal growth and to recover<br />
from their treatment. With early detection,<br />
endocrine disorders can be treated, and the<br />
balance or deficiency restored.<br />
Unfortunately, these disorders aren’t always<br />
diagnosed in time because they aren’t<br />
recognized or understood and ultimately, we<br />
must also find ways to prevent endocrine<br />
damage.<br />
I focus on early and late endocrine effects of<br />
childhood cancer treatment with a special<br />
interest in the thyroid and pituitary gland,<br />
and at improving care for children with<br />
thyroid cancer and craniopharyngioma.<br />
Rare tumors and hormonal changes<br />
Located in the brain, the hypothalamus and<br />
the pituitary gland are the main regulators of<br />
the endocrine system. If damaged, children<br />
present with a variety of clinical signs caused<br />
by hormonal deficiencies, including small<br />
stature, delay of puberty, tiredness, disturbed<br />
day-night rhythm, temperature instability<br />
and hypothalamic obesity.<br />
Tumors in this area during childhood are rare,<br />
necessitating centralization of care and an<br />
experienced multi-disciplinary team to<br />
ensure optimal treatment and outcome.<br />
I also study hormonal disorders during<br />
cancer treatment, which is challenging<br />
because hormones may be altered because<br />
of drug toxicity or because a child is ill<br />
(adaptive regulatory mechanism). The first<br />
requires hormone replacement therapy,<br />
while the second does not. To date, no<br />
prospective studies have been performed in<br />
children with cancer to differentiate between<br />
hormonal changes during childhood cancer<br />
and adaptive hormonal changes.<br />
THYRO-Dynamics Study<br />
We’re supported by the Foundation KIKA<br />
(<strong>Child</strong>ren Cancer-free Foundation, for The<br />
THYRO-Dynamics study, where we will<br />
prospectively measure thyroid hormones in<br />
children treated at the Princess Máxima<br />
Center (PMC). We will gain insight into the<br />
prevalence and causes of true thyroid<br />
dysfunction versus changes regarded as<br />
adaptation. Our findings will lead to better<br />
diagnostics, earlier treatment and better<br />
outcome for children during and after<br />
treatment. This new study illustrates the<br />
unique collaboration between the<br />
Wilhelmina <strong>Child</strong>ren’s Hospital and the<br />
Prinses Máxima Center.<br />
<br />
All children with (chronic)<br />
diseases, deserve screening and<br />
timely treatment of endocrine<br />
deficiencies, so they can grow<br />
and develop just as their peers.<br />
- Hanneke van Santen<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 31
STRATEGIC THEMES: LIFECYCLE<br />
The life-course approach<br />
eputte@umcutrecht.nl<br />
Elise van de Putte,<br />
MD, PhD is a pediatrician<br />
specialized in<br />
social pediatrics and a<br />
Professor of Lifecycle<br />
Pediatrics. Her<br />
<strong>research</strong> is focused on<br />
well-being, participation<br />
and social inclusion<br />
in chronically ill<br />
children.<br />
The <strong>Child</strong> Health Program can be characterized by a unique life-course approach for our<br />
different patient groups. Our aim is to enable chronically ill children to develop and realize<br />
their potential. We support them in adaptation and self-management to meet the social,<br />
physical and emotional challenges they may encounter. A child with a chronic disease<br />
experiences the cumulative impact of all these challenges over time, with direct effect on<br />
his or her health and development. We operationalize this approach within Social Pediatrics<br />
Department in the PROactive life-course cohort study.<br />
PROactive life-course cohort study<br />
In this study, we collect data from young chronic patients (2-25 years old) and their parents using a<br />
comprehensive set of questionnaires. The aim of this <strong>research</strong> project is to study the relationship<br />
between chronic disease and fatigue, pain, societal participation and wellbeing – assessed from both a<br />
child’s and parent’s perspective. Specifically, the project aims to unravel the complex interplay of<br />
protective and risk factors that affect the development of these chronic patients, their societal<br />
participation and their wellbeing. Modern digital tools enable us to report these factors on both the<br />
individual and group level.<br />
Most pediatric patient groups participate in this life-course cohort study: patients with severe<br />
inflammatory disorders (juvenile idiopathic arthritis, cystic fibrosis, irritable bowel disease), children<br />
after oncology treatment and patients with congenital diseases (kidney, heart). A particular strength of<br />
this study is the integration of biological, psychological, social and behavioral data with a focus on<br />
well-being, including health, social inclusion and participation, and with fatigue and chronic pain as<br />
important proxies for these outcome measures. Clinical data are collected from the electronic patient<br />
file in the <strong>research</strong> data platform and are combined with the data from questionnaires that are filled<br />
out using a web-portal (www.hetklikt.nu). Since 2017, we’ve already included 1000 children and we<br />
expect to double this number by the end of 2019.<br />
<br />
The availability and cross-linking with large scale cohort studies outside the hospital, such as the<br />
Whistler, Piama and Youth cohorts, enable us to further understand the cumulative impact of the<br />
challenges that chronically ill children encounter.<br />
Investing in the child creates a<br />
threefold gain: in their present, in<br />
their future as adults and in their<br />
children, our next generation.<br />
- Elise van de Putte<br />
32 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
STRATEGIC THEMES: LIFECYCLE<br />
Let’s try to<br />
help patients<br />
manage their<br />
own disease.<br />
- Jaap van Laar<br />
<br />
Jaap van Laar, MD, PhD is an<br />
academic rheumatologist, and his<br />
professional goal has always been to<br />
explore new roads to improve patient<br />
care. He was PI of the landmark ASTIStrial<br />
and currently runs a productive<br />
<strong>research</strong> program that focuses on<br />
developing innovative therapies for<br />
systemic sclerosis and rheumatoid<br />
arthritis.<br />
jlaar@umcutrecht.nl<br />
Nico Wulffraat, MD, PhD is a<br />
pediatric immunologist and<br />
rheumatologist who works on JIA<br />
and stem cell transplantation. He leads<br />
studies on autologous stem cell<br />
transplant in JIA, vaccination<br />
development and drug treatment trials.<br />
nwulffra@umcutrecht.nl<br />
Pediatric and adult<br />
rheumatology:<br />
2 sides of the same coin<br />
Whilst the outcomes of young adults with rheumatic diseases such as juvenile idiopathic arthritis (JIA) has<br />
markedly improved since the introduction of biologicals and more intensive treatment regimens, they still face<br />
multiple challenges in daily life. Not only do they need to develop strategies to cope with pain, fatigue and<br />
disability, they also need to prepare for an uncertain future in terms of jobs, relationships and long-term<br />
outcome of their condition. Surprisingly few studies have addressed long-term multidomain outcomes in JIA<br />
and there is a pressing need for new observational studies of JIA patients, even those with optimally controlled<br />
disease. There is even less data available for patients with connective tissue diseases and immunodeficiencies.<br />
Basic fundamental questions remain unanswered. How is the immune system shaped by recurrent bouts of<br />
rheumatic disease and infections and what are the long-term clinical sequelae?<br />
Reuma2Go: managing disease smartly<br />
The successful conduct of long-term studies on<br />
pharmacovigilance and immune health not only requires<br />
smooth transitional care from pediatric rheumatology to adult<br />
rheumatology, but also harmonisation of data collection,<br />
integration of electronic patient records and development of<br />
tailor-made solutions (such as the use of smart mobile apps).<br />
We are currently setting up a prolonged transition of care plan<br />
supported by an E-Health tool called Reuma2Go. It is our<br />
ambition to promote self-management. With adequate selfassessment,<br />
patients can, for instance, reduce the number of<br />
outpatient visits when in remission.<br />
Predicting treatment response<br />
Even more relevant is the search for biomarkers predicting<br />
response to medication and long-term prognosis. For this we<br />
have set up a multicenter program (a multi “omics” approach)<br />
in which all Canadian and Dutch academic pediatric<br />
rheumatology centers participate. Patient engagement is<br />
critical for the successful implementation of such ambitious<br />
projects. Ultimately new digital technologies and advances in<br />
disease monitoring should help put patients in the driver’s seat<br />
with respect to managing their own disease.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 33
Transitioning care as<br />
child becomes adult<br />
Cystic Fibrosis (CF) is the most prevalent hereditary disease in<br />
Western countries. CF was first described just before World War<br />
II. At that time, all patients died during early childhood because<br />
of severe lung damage as a result of untreatable airway<br />
infections. Until the 1970s, CF was mainly a pediatric disease<br />
which required intensive treatment with antibiotics, chest<br />
physiotherapy and food supplements. With improvement of<br />
prognosis, new complications emerged: About one third of<br />
patients developed CF-related liver disease during late childhood<br />
and more than half acquired CF-related diabetes in early<br />
adulthood. Of those born in the 1980s, about 75% survived into<br />
adulthood. In addition to the increasing complexity of patient<br />
care, CF was no longer only a pediatric disease, as it permeated<br />
into the fields of adult lung specialists, gastro-enterologists and<br />
endocrinologists. Current mean life expectancy has risen up to<br />
almost 50 years of age and thus, care issues like male infertility,<br />
child birth and labor participation are reality for most patients.<br />
With the recent introduction of modulators of the CF<br />
Transmembrane Conductance Regulator (CFTR) protein, survival<br />
will further improve for many patients.<br />
Care needs to include the transition from child to adulthood<br />
The transition from a monodisciplinary deadly disease in children<br />
to a multidisciplinary complex chronic disease in older adults<br />
requires far-reaching changes in health care systems. For many<br />
years, ‘transition programs’ were developed to bridge the gaps<br />
between pediatric and adult knowledge and culture of care, but<br />
they were hampered by logistical and financial barriers. Such<br />
programs have never been successful and evaluations show that<br />
patients are dissatisfied and lost in follow-up. Transition<br />
programs focus on adapting the patient to the existing health<br />
care system, without considering changing care needs and<br />
prognosis. In addition, the current system impedes further<br />
knowledge development and innovation because ‘early<br />
determinants’ in childhood are disconnected from ‘late<br />
outcomes’ in adulthood.<br />
Our solution<br />
This is why, for years, the CF Center Utrecht has been using the<br />
concept of life-course care. <strong>Child</strong>ren and adults are followed and<br />
treated within a single team working with one continuous<br />
patient file and database, and where <strong>research</strong> focuses on<br />
improving the entire life-course perspective. This concept is<br />
accomplishing what the transition programs failed to do.<br />
cent@umcutrecht.nl<br />
hheijer2@umcutrecht.nl<br />
Kors van der Ent, MD,<br />
PhD initiated the Cystic<br />
Fibrosis Center Utrecht in<br />
1997 and is a co-developer<br />
of the Utrecht organoid<br />
model for CF. Kors is the<br />
coordinator of the European<br />
Union Horizon 2020 HIT-CF<br />
Program and the core-network<br />
leader for CF in the<br />
European Reference<br />
Network (ERN-LUNG)<br />
Harry Heijerman, MD,<br />
PhD is adult chest physician<br />
who founded (1989) and<br />
chaired the adult CF Center<br />
in The Hague and is also<br />
founding editor of The<br />
Journal of Cystic Fibrosis<br />
and CF Research News, of<br />
which he is currently<br />
Editor-in-Chief.<br />
34 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
STRATEGIC THEMES: LIFECYCLE<br />
Living better with a<br />
clotting disorder<br />
In 1964, Simon van Creveld founded a special clinic for children with hemophilia, a rare<br />
congenital disease. Patients with hemophilia lack clotting factors VIII or IX,<br />
characterized by bleeding in the joints, which leads to crippling joint arthropathy in<br />
adulthood. During the 1960s, these patients were admitted to the hospital for months<br />
and received multidisciplinary care with a physiotherapist, nurse, psychologist and<br />
teacher. Since then, treatment has improved and the Van Creveldkliniek has evolved<br />
into an outpatient clinic for patients of all ages with congenital clotting disorders. It’s<br />
now part of the UMC Utrecht, but maintains its unique concept of multidisciplinary care<br />
provided by a designated team. We provide care for approximately 50% of all patients<br />
with congenital clotting disorders in the Netherlands.<br />
rschutge@umcutrecht.nl<br />
kfische2@umcutrecht.nl<br />
Roger Schutgens, MD, PhD is an adult<br />
hematologist and epidemiologist. He is<br />
Head of the Van Creveldkliniek, Center for<br />
Benign Hematology, Thrombosis and<br />
Hemostasis. He is Chair of the<br />
Anticoagulation Committee at the<br />
UMC Utrecht, Secretary of the Dutch<br />
Society of Hemophilia Treaters and<br />
Secretary of the Dutch Society for<br />
Thrombosis and Hemostasis.<br />
Kathelijn Fischer, MD, PhD is a<br />
pediatric hematologist and clinical<br />
epidemiologist. At the Van Creveldkliniek<br />
(part of the UMC Utrecht), she combines<br />
clinical care for children with clotting<br />
disorders with multidisciplinary <strong>research</strong>.<br />
Concomitantly, she is the epidemiologist<br />
for two European Hemophilia Registries<br />
(EUHASS and PedNet) and section editor<br />
for ‘Thrombosis and Haemostasis’.<br />
Collecting interdisciplinary data<br />
Our <strong>research</strong> focuses on patients with hemophilia, where care and <strong>research</strong><br />
are combined: All patients with severe hemophilia are seen annually within<br />
our multidisciplinary clinic, and their medical file includes documen tation<br />
of treatment and bleeds, laboratory tests, physical assess ment,<br />
questionnaires about physical activities and quality of life, and consultation<br />
with a hemophilia nurse and social worker. Provision of lifelong care<br />
provides the opportunity to see the effects of pediatric treatment through<br />
to adulthood and provides crosstalk between adult and pediatric specialists.<br />
Data from patient medical files, available since the 1970s, combined with<br />
annual multi disciplinary assessment, have established a longitudinal cohort<br />
study with repeated outcome assessments.<br />
Over the years, we’ve used these data to <strong>research</strong> effective replacement<br />
therapy, to understand the natural history of hepatitis C infections, to<br />
conduct a prospective study on cardiovascular disease and to investigate<br />
the value of various imaging techniques.<br />
Can patients with clotting disorders do sports?<br />
One current <strong>research</strong> project is a prospective study on sports participation<br />
and injuries. We started this because many patients are discouraged from<br />
participating in sports, because of perceived bleeding risk. At baseline, we<br />
test strength, endurance and coordination. Then sports participation and<br />
injuries are assessed for a year. The rate of injuries will be compared to<br />
general population data and we will use results of baseline tests to counsel<br />
patients on injury risk in a sports outpatient clinic.<br />
Our <strong>research</strong> projects strive to improve lifelong multidisciplinary care<br />
for patients with hemophilia and other clotting disorders.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 35
STRATEGIC THEMES: INTERDISCIPLINARITY<br />
Janjaap<br />
van der Net,<br />
PhD is a pediatric<br />
physiotherapist and<br />
clinical health scientist,<br />
whose special interest is<br />
motor-proficiency and<br />
physical literacy in<br />
childhood chronic<br />
conditions.<br />
Tim Takken, PhD is<br />
medical physiologist<br />
and a special interest in<br />
clinical pediatric<br />
exercise physiology.<br />
t.takken@umcutrecht.nl<br />
jnet@umcutrecht.nl<br />
Become competent now,<br />
to be confident later<br />
A family-centered and interdisciplinary showcase for <strong>Child</strong> Health <strong>research</strong><br />
At the Center for <strong>Child</strong> Development, Exercise and Physical<br />
Literacy, we study Activity & Health in <strong>Child</strong>hood Chronic<br />
Conditions. This is done in close collaboration with the<br />
Psychosocial Depart ment of the Wilhelmina <strong>Child</strong>ren’s Hospital,<br />
which focuses on Empowerment and Resilience in <strong>Child</strong>hood<br />
Chronic Conditions. Embedded within the <strong>Child</strong> Health<br />
Program is this complementary, interdisciplinary approach to<br />
studying health in childhood chronic conditions from a social,<br />
behavioral and physical activity perspective.<br />
Studying health within the context of disease<br />
An inspiring example is the Congenital Heart Disease-Lifespan<br />
study (CHD-Ls), a program in which health, rather than disease<br />
alone, in children with a congenital heart disease (CHD) and<br />
their families is longitudinally studied from as early as 20 weeks<br />
of gestation into their 40s. we focus on a family-centered and<br />
patient-centered perspective and on the physical, cognitive<br />
and emotional development and health in children with CHD<br />
and their family members.<br />
Nested within the CHD-Ls study is the CRUCIAL TRIAL, a<br />
collaboration between obstetrics, pediatric cardiology and<br />
cardiosurgery, neonatal and pediatric intensive care medicine,<br />
as well as pediatric physiotherapy, exercise physiology and<br />
pediatric psychology. This trial aims to minimize cerebral<br />
damage and increase cardiac health during pregnancy,<br />
perinatally and in early childhood to improve neuro-cognitive<br />
and motor-development as well as long-term health-related<br />
fitness in children with a congenital heart disease.<br />
Promoting physical activity in children with<br />
a chronic condition<br />
With survival rates increasing in childhood conditions (e.g.<br />
cystic fibrosis, childhood cancer and more recently, spinal<br />
muscular atrophy), as well as more efficient disease control (e.g.<br />
pediatric rheumatic conditions and hemophilia), there is an<br />
increasing desire from children and their families to be able to<br />
fully participate in an active healthy lifestyle. We therefore<br />
joined the Active Healthy Kids Global Alliance, together with<br />
Mark Tremblay, PhD, and expert in exercise science at the<br />
University of Ottawa, Canada, and produced the Dutch Physical<br />
Activity Report Card for <strong>Child</strong>ren and Youth. In this<br />
interdisciplinary and societal project, we collaborated with<br />
many national societal organizations and mapped health<br />
policies on local, municipal, provincial and national levels to<br />
improve active healthy living in children with a chronic<br />
condition. Together with the Department of Preventive<br />
Medicine and Youth from the municipality of Utrecht, we’re<br />
currently implementing a program “WKZsportief” to improve<br />
physical literacy, and to enhance participation in sports and<br />
active recreation in children with chronic conditions. Our motto<br />
for this approach is: become competent now, to be confident<br />
later.<br />
36 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
STRATEGIC THEMES: INTERDISCIPLINARITY<br />
Empowering the entire family<br />
Center of Excellence for Rehabilitation Medicine<br />
(De Hoogstraat Rehabilitation)<br />
Advances in medical technology, diagnosis and treatment have increased the life expectancy<br />
of various childhood disorders. Pediatric rehabilitation aims to optimize autonomy, selfmanagement<br />
and participation of children with developmental disabilities and their families.<br />
Our interdisciplinary program focuses on developmental trajectories, identification of children<br />
at risk for physical and mental health problems and interventions to mitigate those risks.<br />
Because families are central in the lives and development of children, we also focus on family<br />
empowerment.<br />
Patients and families are involved throughout our <strong>research</strong> process, from idea to<br />
implementation, and we have a strong collaboration with patient organizations, including<br />
Cerebral Palsy Netherlands (CP Nederland; formerly known as BOSK). A good example is our<br />
study on sleep, nutrition and physical activity of children with Brain Based Developmental<br />
Disabilities. Together with Neonatology, we’ve developed clinical care pathways to guide<br />
clinicians with assessment and early identification of problems in these areas, based on<br />
systematic data collection. We seek to understand the quantity and quality of sleep and its<br />
relationship with development. In partnership with parents, we’re developing a support<br />
program, including an instructional video and online knowledge translation resources, to<br />
educate and empower families so they can support the development and health of their child.<br />
mketela2@umcutrecht.nl<br />
We collaborate with<br />
patients and families in all<br />
stages of <strong>research</strong>.<br />
- Marjolijn Ketelaar<br />
<br />
Marjolijn Ketelaar,<br />
PhD focuses on the<br />
development of children<br />
with developmental<br />
disabilities, and<br />
empowerment of<br />
families to optimize<br />
autonomy and<br />
participation.<br />
Novel insights into cancer immunotherapy<br />
mboes@umcutrecht.nl<br />
Marianne Boes,<br />
PhD focuses on<br />
immunodeficiencies<br />
and immune activation<br />
with a special<br />
interest in immune<br />
checkpoints and<br />
developing immunotherapy<br />
for cancer<br />
patients.<br />
Immunotherapy based on checkpoint blocking antibodies (anti CTLA4, anti PD-1) has<br />
revolutionized treatment for patients suffering from well-responding cancers such as<br />
melanoma and non-small cell lung cancer, which are tumors with acquired mutational loads.<br />
Neuroblastoma accounts for 15% of childhood cancer mortality, yet susceptibility to<br />
checkpoint blockade-based immunotherapy is not evident. Because the level of expression<br />
of major histocompatibility (MHC) Class-I molecules is low, neuroblastoma tumors evade a<br />
major immune defense strategy based on MHC-restricted cytotoxic T cells. In our opinion,<br />
induction of MHC-I membrane expression is prerequisite for optimal efficacy of T-cell therapy<br />
in neuroblastoma and should be incorporated into treatment regimens.<br />
My team initiated an interdisciplinary collaboration with colleagues at the Netherlands<br />
Cancer institute to screen for targets that upregulate MHC-I display at the neuroblastoma cell<br />
surface, yielding TNIP1 and N4BP1. Validation experiments in neuroblastoma revealed<br />
increased MHC-I antigen presentation capacity and induced recognition by neuroblastoma<br />
tumor-antigen specific T-cells. Supporting our findings, patients expressing high levels of<br />
TNIP1 and N4BP1 in neuroblastoma have lowered MHC-I tumor surface display and have<br />
worse survival probability. Use of these targets in therapy has the potential to augment<br />
current treatments in innovative ways that will improve clinical outcomes for neuroblastoma<br />
cancer patients.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 37
STRATEGIC THEMES: MENTAL & PHYSICAL HEALTH<br />
<br />
mgroote5@umcutrecht.nl<br />
Healthy play, better coping<br />
the importance of monitoring and acting on psychosocial development<br />
A child living with a chronic disease carries this burden, whether<br />
he or she is ill or well at any given time. It affects his or her everyday<br />
life. Chronic disease extends beyond the actual illness itself and<br />
has a negative impact on a child’s physical, social, emotional and<br />
cognitive development. Lower psychological well-being of and<br />
decreased social participation by chronically ill patients is<br />
demonstrated in conditions such as cystic fibrosis, autoimmune<br />
disorders, cardiac disorders, cancer and premature birth. We study<br />
play and focus on innovative gaming approaches as coping and<br />
healthy developmental tools for children with chronic conditions.<br />
For children, play is essential<br />
Play behavior is essential for the healthy development of an individual and<br />
hospitalization, pain, fatigue and social isolation limit opportunities to engage in<br />
social play. Play allows children to experiment with their behavioral and social<br />
repertoire and to practice physical and communication skills; it facilitates the<br />
development of social competence, emotional capacities, resilience, creativity and<br />
of problem-solving skills. Therefore, impaired play may have long-lasting<br />
consequences for these children as they grow up, in addition to the direct physical<br />
effects of their disease. Unfortunately, direct empirical evidence demonstrating<br />
the importance of play is lacking.<br />
Patient reported outcomes like fatigue and pain represent the<br />
struggles patients experience on a day-to-day basis.<br />
Martha Grootenhuis,<br />
PhD studied<br />
psychology and<br />
worked at the Emma<br />
<strong>Child</strong>ren’s Hospital<br />
from 1992-2015.<br />
Thereafter, she moved<br />
to Utrecht to become<br />
Principal Investigator<br />
in the Princess Máxima<br />
Center. Martha is<br />
founder of the<br />
Pediatric Psycho-<br />
Oncology Committee<br />
of the International<br />
Society of Pediatric<br />
Oncology (SIOP).<br />
- Sanne Nijhof<br />
Healthy Play, Better Coping<br />
We participate in a new multidisciplinary <strong>research</strong> project focused on play and<br />
applied games in children with chronic or life-threatening conditions: Healthy Play,<br />
Better Coping. In this consortium we investigate various ways to stimulate or<br />
modify play behavior and how to assess its effects on patient-reported outcomes.<br />
We hypothesize that helping children better adapt to the stress of their chronic<br />
condition will promote their short-and long-term cognitive, social, emotional and<br />
psychomotor development. To do this, we focus on preventative programs,<br />
applied games (games created with a specific purpose other than pure<br />
entertainment) and other interactive technologies, such as video games and<br />
virtual reality. Our network combines expertise from various collaborators,<br />
including several partners within Utrecht University (Dynamics of Youth theme,<br />
Game Research Graduate Program, Behavioral Neuroscience Department, Faculty<br />
of Veterinary Medicine); the Princes Máxima Center; and the Trimbos Institute for<br />
Mental Health. Our integrated systematic approach will help young patients better<br />
cope with the consequences of their illness by stimulating healthy social play and<br />
an overall healthy development.<br />
Social and emotional development of teenagers<br />
We investigate social and emotional development based on lifespan studies in<br />
young patients and their families. Sanne was involved in a randomized clinical trial<br />
FITNET (Fatigue In Teenagers on the interNET), which demonstrated the<br />
effectiveness of internet-based cognitive behavioral treatment for adolescents<br />
with chronic fatigue syndrome. Based on outcomes of the trial, Sanne has extended<br />
her experience with severe fatigue to new somatic domains, including<br />
snijhof@umcutrecht.nl<br />
Sanne Nijhof, MD, PhD<br />
is a pediatrician and<br />
clinical <strong>research</strong>er with<br />
focus on social<br />
pediatrics and<br />
patient-reported<br />
outcomes, like fatigue<br />
and pain. She is driven<br />
by the hypothesis that<br />
(chronic) childhood<br />
diseases influence all<br />
aspects of a child’s life<br />
- not only the physical,<br />
but also the social, emotional,<br />
educational and<br />
economical. Sanne<br />
co-developed personalized<br />
digital tools to<br />
assess and treat the<br />
associated psychosocial<br />
consequences of<br />
chronic disease.<br />
38 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
STRATEGIC THEMES: MENTAL & PHYSICAL HEALTH<br />
<strong>Child</strong>hood<br />
cancer affects the<br />
whole family.<br />
Screening<br />
<br />
and<br />
monitoring help to<br />
prevent traumatic stress<br />
and provide timely<br />
interventions.<br />
- Martha Grootenhuis<br />
rheumatology, pulmonology and oncology. Together with Elise<br />
van de Putte, MD, PhD, she’s translated insights into tailored<br />
e-health interventions: FitNet-plus, a web-based portal for<br />
cognitive behavioral therapy; and PROfeel, a smartphone app<br />
where children can log their complaints in real-time.<br />
Martha’s group has longitudinally studied several pediatric<br />
populations. Her studies demonstrate, for example, that young<br />
adults who grow up with a childhood chronic disease achieve<br />
fewer milestones, or achieve them later than their peers across<br />
different domains (i.e. autonomy, psychosexual and social). A<br />
delayed social development, including limited participation in<br />
sports, was related to a lower quality of life in adulthood. This<br />
underlines the urgent need to address social development<br />
earlier in life.<br />
Together with Elise van Putte, MD, PhD, we collaborate in the<br />
PROactive study (Patient Reported Outcomes in Adolescents<br />
with Chronic/life-threatening disease and Tailored<br />
InterVentions in a digital Environment). PROactive enables the<br />
early detection of a disturbed psychosocial development and<br />
prompts subsequent interventions, that considers the<br />
perspective of both the child and his or her family, and aims to<br />
improve self-management and growth towards independency<br />
in adulthood. In particular, we have a special focus on fatigue<br />
and social/sports activities.<br />
Early interventions will empower our chronically ill patients<br />
and help them cope with the psychosocial effects of their<br />
physical condition. We expect that, through health play and<br />
game interventions, our patients will develop into healthy<br />
resilient adults.<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 39
UNIQUE RESOURCES<br />
Patients cohorts<br />
in the child health program<br />
The <strong>Child</strong> Health program focusses on the longterm outcomes of patients with chronic diseases.<br />
Within the program an extensive number of longitudinal patient cohorts are being studied, many of<br />
them covering birth, pediatric and adult care. We invite you to collaborate with us and to add or use<br />
these cohort data for your own <strong>research</strong>. For full description of the cohorts we refer to our website:<br />
www.umcutrecht.nl/childhealth<br />
Congenital<br />
heart<br />
diseases<br />
Wilson<br />
diseases<br />
Progressive<br />
familiar<br />
intrahepatic<br />
cholestasis<br />
Mixed<br />
endocrine<br />
diseases<br />
Post cancer<br />
treatment<br />
Mixed<br />
metabolic<br />
diseases<br />
Pregnant<br />
women<br />
with fetal<br />
abnormality<br />
Congenital<br />
kidney<br />
diseases<br />
Extremely<br />
preterm<br />
infants<br />
Cystic Fibrosis<br />
Perinatal<br />
brain<br />
damage<br />
Juvenile<br />
rheumatic<br />
arthritis<br />
Syncytial<br />
40 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
UNIQUE RESOURCES<br />
Facilities<br />
& Expert Knowledge<br />
You can find some examples of our facilities & expert knowledge on the next<br />
pages. Lease check our website for lots more! www.umcutrecht.nl/childhealth<br />
Metabolic diagnostics<br />
We use an in-house developed direct infusion mass spectrometry pipeline to<br />
investigate the metabolome in patients’ body fluids and cells and to<br />
characterize model systems like cell lines, knock out mice and zebrafish.<br />
Validation of interesting findings is performed by targeted mass spectrometry<br />
by a range of dedicated platforms. This approach greatly contributes to<br />
diagnostics, disease-discovery and elucidation of pathogenic mechanisms.<br />
For more information please contact Judith Jans, jjans@umcutrecht.nl<br />
or Nanda Verhoeven, nverhoev@umcutrecht.nl<br />
Cardiac 3D imaging<br />
We are world leading in 3D imaging of the heart in young children. We have<br />
a state of the art catheterization laboratory with 3 dimensional rotational<br />
angiography that is able to obtain high resolution 3D images in small<br />
infants. Also fetal and neonatal MRI scanning of heart and brain is being<br />
performed. Furthermore we have a 3D printer that is able to convert any 3D<br />
dataset into a 3D model within 24 hours. 3D datasets and 3D prints can be<br />
further analyzed using our (MRI compatible) computational fluid dynamics<br />
lab and software.<br />
For more information please contact Hans Breur, hbreur@umcutrecht.nl<br />
Organoids<br />
We work with organoids from different disciplines. Sabine Fuchs’<br />
laboratory participates in the RMCU (Regenerative Medicine Center<br />
Utrecht) in the Hubrecht Institute. Her main facility involves liver and<br />
intestinal organoid <strong>research</strong>, including functional assays and frontline<br />
gene-editing technologies. Clinically, we have a unique multidisciplinary<br />
standardized diagnostic/follow-up facility (Sylvia Toth Center) in the<br />
Wilhelmina <strong>Child</strong>ren’s Hospital for evaluation of diseases of unknown<br />
origin, or for the follow-up of novel treatment strategies.<br />
Jeffrey Beekmans’ laboratory focuses on<br />
translational <strong>research</strong> with stem cells in cystic<br />
fibrosis. He leads a <strong>research</strong> group that<br />
develops stem cell based culture and assay<br />
technology to model human pulmonary<br />
disease, and currently mostly focusses on<br />
(personalized) treatment of cystic fibrosis.<br />
For more information please contact<br />
Jeffrey Beekman, jbeekman@umcutrecht.nl<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 41
Facilities<br />
& Expert Knowledge<br />
Zebrafish model<br />
Creation of a zebrafish<br />
model, including gene<br />
knockout and knockin<br />
of variants. Zebra fish<br />
modeling<br />
(Hubrecht Institute,<br />
prof. Jeroen Bakkers)<br />
For information, please contact<br />
Gijs van Haaften,<br />
ghaaften@umcutrecht.nl<br />
meijkema@umcutrecht.nl<br />
René Eijkemans,<br />
MD, PhD focuses on<br />
clinical prediction<br />
models and machine<br />
learning in high<br />
dimensional data. He<br />
has worked in many<br />
clinical areas, in<br />
particular, in reproductive<br />
medicine.<br />
Applied big data analysis &<br />
machine learning<br />
In infants, Respiratory syncytial virus (RSV) is the<br />
leading cause of lower respiratory tract infections<br />
and is responsible for up to 80% of acute<br />
bronchiolitis cases. Several risk factors for<br />
developing severe RSV disease in infants have<br />
been identified. Nevertheless, this knowledge<br />
only allows us to predict approximately 50% of all<br />
severe RSV infections in young children. Currently,<br />
we cannot predict whether an infant will progress<br />
to severe disease, or clear the virus without<br />
extensive medical care. Consequently, many<br />
infants are hospitalized for observation, and a<br />
significant number do not progress to a severe<br />
disease condition. Thus, medical care for infants<br />
with an RSV infection could be more efficient and<br />
patient-tailored with accurate prediction. We<br />
investigated whether a genomic prognostic<br />
signature exists that can predict the course of<br />
RSV infection with high accuracy. We used early<br />
onset blood transcriptome profiles from 39<br />
hospitalized infants who were followed until<br />
recovery and whose level of disease severity was<br />
determined retrospectively. Applying support<br />
vector machine learning on age by sex<br />
standardized transcription data, an 84-gene<br />
signature was identified that discriminated<br />
hospitalized infants with eventually mild or<br />
moderate RSV infection from infants suffering<br />
from severe RSV disease with a validated AUC of<br />
0.971 on the experimental data. We conclude that<br />
this 84-gene signature may serve as the basis to<br />
develop a prognostic test to support clinical<br />
management of RSV patients, making the care for<br />
these patients more patient-tailored.<br />
We are drowning<br />
in information<br />
and starving for<br />
knowledge.<br />
- Rutherford D. Roger<br />
<br />
42 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
UNIQUE RESOURCES<br />
Understanding and<br />
treating chronic pain:<br />
Neuro-Immunology of pain<br />
Chronic pain affects more than 20% of the<br />
population and is a huge clinical and<br />
societal problem. Current therapies often<br />
fail because of their limited effectiveness,<br />
or because of severe side effects such as<br />
addition (opioids). We aim to understand<br />
how chronic pain develops in children and<br />
adults and identify potential differences<br />
between these groups. Our goal is to<br />
translate novel insights into ways to predict<br />
who will develop chronic pain to enable<br />
earlier pain treatment to prevent the<br />
development of chronic pain and to<br />
develop novel treatments. Based on<br />
recently identified neuro-immune<br />
interactions in chronic pain we have<br />
developed an interleukin-4 and<br />
interleukin-10 fusion protein of that shows<br />
remarkable effects in resolving pain; this is<br />
being further developed for clinical use.<br />
Why does pain persist?<br />
Pain normally serves as a warning sign of<br />
inflammation and damage that disappears<br />
when these conditions are resolved.<br />
However, pain persists even after cessation<br />
of inflammation or damage in many<br />
patients with inflammatory diseases, for<br />
example, children with rheumatic disease.<br />
The mechanisms for persisting pain are<br />
poorly understood. We hypothese that this<br />
persisting pain results from failing pain<br />
resolution programs caused by aberrant<br />
immune and nervous system interactions.<br />
For example, we’ve identified macrophages<br />
as key regulators of the resolution<br />
of inflammatory pain through interactions<br />
with sensory neurons. However, sensory<br />
neurons are also able to change<br />
macrophage function, such that<br />
macrophages switch to maintenance of<br />
chronic pain, independent of the original<br />
inflammation or damage. We study how<br />
these systems interact and contribute to<br />
pain. We’ve determined that various antiinflammatory<br />
cytokines signal to sensory<br />
neurons and glia cells to prevent<br />
development of long-lasting pain and also<br />
identified new pain genes such as<br />
FAM173b.<br />
Using a multidisciplinary approach<br />
to pain<br />
Pain is a multidisciplinary problem and<br />
therefore we work together with scientist<br />
from different disciplines (e.g. neuroscientists<br />
and immunologists) and<br />
clinicians (e.g. pediatric rheumatologists<br />
and anesthesiologists) within and outside<br />
(for the UMC Utrecht (as an example, see<br />
www.bonepain.eu). We use various<br />
preclinical chronic pain models including<br />
inflammatory, neuropathic, chemotherapy,<br />
visceral, diabetes, and osteoarthritis pain<br />
models. Moreover, we perform studies in<br />
relevant patient populations such as<br />
juvenile idiopathic arthritis and<br />
osteoarthritis. With our efforts, we’re<br />
taking the next step in outsmarting<br />
chronic pain.<br />
neijkelk@umcutrecht.nl<br />
Niels Eijkelkamp,<br />
PhD is an expert in the<br />
field of neuroimmunology.<br />
His <strong>research</strong> topics<br />
include understanding<br />
chronic pain and the<br />
development of novel<br />
therapeutic approaches.<br />
pain, a<br />
neglected Chronic<br />
global<br />
health problem, is<br />
not a symptom of<br />
disease but a<br />
pathologic entity<br />
that requires<br />
mechanism-based<br />
new and specific<br />
therapies.<br />
- Niels Eijkelkamp<br />
Pediatric exercise and muscle lab<br />
Special equipped to measure al relevant parameters of health related<br />
fitness, including Bio Impedance measures and nutritional status.<br />
Including a platform to measure real-time –Spectrometry (7T) of<br />
exercise metabolism and Near Infrared Spectography (NIRS) in<br />
muscles.<br />
For more information please contact Janjaap van der Net, jnet@umcutrecht.nl<br />
or Tim Takken, ttakken@umcutrecht.nl<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 43
Facilities<br />
& Expert Knowledge<br />
Functional brain measurements<br />
1. State-of-the-art neonatal and infant MRI scanning<br />
(3 tesla and recently 7 tesla) including advanced<br />
postprocessing (e.g. DTI, MRS, Segmentations<br />
(volumetric measurements)).<br />
2. State-of-the-art cerebral ultrasound.<br />
3. State-of-the-art neuromonitoring (aEEG, NIRS,<br />
sleep assessments).<br />
4. A dedicted highly specialized<br />
neurodevelopmental follow up group<br />
For more information please contact<br />
Jeroen Dudink, jdudink@umcutrecht.nl<br />
Translational <strong>research</strong><br />
for early stages of life<br />
What happens early in life can have detrimental effects<br />
later on. The Department for Developmental Origins of<br />
Disease provides unique resources to the <strong>Child</strong> Health<br />
Program and we focuse on causes, consequences of and<br />
cures for adverse events that occur during early life stages.<br />
We collaborate with patient organizations and clinical<br />
investigators in the Neonatology, Obstetrics and Pediatric<br />
Departments, UMC Utrecht to ensure that we develop<br />
interventions that truly matter to our patients and families.<br />
Using cutting edge techniques and biotechnological<br />
innovations, in collaboration with technical universities in<br />
Eindhoven and Delft, we combine molecular, anatomical,<br />
physiological and behavioral expertise and investigate<br />
intra-uterine processes and interventions to prevent<br />
cardiovascular and neurodevelopmental disorders later in<br />
life (led by Titia Lely, MD, PhD); the developing connectivity<br />
of neuronal networks that enable social play, motor<br />
learning and cognition (led by Freek Hoebeek, PhD); and<br />
novel neuroprotective and neuroregenerative<br />
interventions including stem cells, nutrition and growth<br />
factors for perinatal brain injury (led by Cora Nijboer, PhD).<br />
<br />
Translational<br />
<strong>research</strong> not<br />
only spans<br />
fundamental to<br />
clinical science,<br />
but also forms<br />
the bridge<br />
allowing <strong>Child</strong><br />
Health experts<br />
to innovate<br />
therapies.<br />
- Freek Hoebeek<br />
fhoebeek@umcutrecht.nl<br />
Freek Hoebeek,<br />
PhD focuses on<br />
neuroscience and<br />
building multidisciplinary<br />
<strong>research</strong> teams.<br />
He is the UMC Utrecht<br />
Chair of Translational<br />
Research of Early Life<br />
Events in 2018.<br />
44 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
UNIQUE RESOURCES<br />
Clinical Trials<br />
Changing lives through trials<br />
An important aspect of <strong>research</strong> in<br />
pregnant women and children is the<br />
design and performance of clinical studies<br />
and trials. To do this in the best way, we’ve<br />
taken an approach which translates basic,<br />
fundamental science into clinical<br />
application, by developing innovative,<br />
patient-centric biomarkers and<br />
therapeutics. We also collaborate with<br />
public and private sectors to bring a<br />
spectrum of innovative treatments, not<br />
easily or readily available, to children in<br />
need. By working with scientists, clinicians,<br />
institutes, and industry, the sum of its parts<br />
is truly greater than what could be<br />
achieved alone.<br />
The UMC Utrecht U-TRIAL initiative helps<br />
<strong>research</strong>ers within this strategic theme<br />
bring their <strong>research</strong> ideas to the forefront.<br />
Together with patient organizations,<br />
health authorities, industry partners and<br />
Julius Clinical (the academic <strong>research</strong><br />
organization spin-off of the UMC Utrecht),<br />
investigators are stimulated to develop<br />
new and impactful clinical hypotheses<br />
which can be tested within a bold, highquality<br />
framework. In doing so, we deliver<br />
essential clinical results and thereby<br />
treatments to quickly and effectively<br />
improve the health of pregnant women<br />
and children.<br />
cpark@umcutrecht.nl<br />
Cyrus Park, MSc, MBA<br />
Strategic Advisor – Trial<br />
Development U-TRIAL<br />
initiative to stimulate<br />
innovative, impactful<br />
clinical <strong>research</strong> to benefit<br />
UMC Utrecht and society.<br />
Clinical Trials in UMC Utrecht<br />
1,546<br />
studies<br />
1,335<br />
medical conditions<br />
Pediatric Clinical Trials in UMC Utrecht<br />
315 trials in children<br />
226<br />
interventional<br />
89<br />
observational<br />
169<br />
industry<br />
funded<br />
collaborations<br />
146<br />
other funded<br />
collaborations<br />
Source: clinicaltrials.gov<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 45
EDUCATION AND TALENT<br />
Attracting and<br />
advancing talent<br />
Berent Prakken, acting dean: <strong>Child</strong> Health has a strong focus<br />
on education, and for a very good reason: Education holds the<br />
key to our future. Our education program is aimed at different<br />
audiences ranging from patients to health professionals and<br />
scientists. We specifically support targeted programs for talent<br />
management that help young <strong>research</strong>ers focus their efforts<br />
towards real and sustainable societal impact.<br />
<br />
<br />
Education<br />
holds the<br />
key to our<br />
future.<br />
- Berent Prakken<br />
<br />
There are no better<br />
teachers for<br />
upcoming physicians<br />
than patients and<br />
their loved ones.<br />
- Joost Frenkel<br />
46 UMC Utrecht - <strong>Child</strong> <strong>research</strong>
EDUCATION AND TALENT<br />
TULIPS program<br />
New <strong>research</strong>ers within the <strong>Child</strong> Health<br />
program are actively stimulated to<br />
participate in the national TULIPS program<br />
(Training Upcoming Leaders in Pediatric<br />
Science), an initiative of the Dutch Society<br />
for <strong>Child</strong>care. The vision of TULIPS is that<br />
high-quality <strong>research</strong> is required to<br />
improve child health. TULIPS has the<br />
mission to empower young clinician<br />
scientists to become international<br />
competitive <strong>research</strong>ers. Therefore, TULIPS<br />
provides distinct, selective 2-year curricula<br />
for PhD students and Postdoctoral fellows.<br />
Both curricula provide interactive training<br />
sessions and weekend educational retreats<br />
to create opportunities for collaboration<br />
and to enhance competences required to<br />
become successful in Pediatric Science.<br />
bprakken@umcutrecht.nl<br />
Berent Prakken, MD, PhD<br />
Pediatric Immunology,<br />
Acting Dean, Education<br />
Director Biomedical<br />
Education Center<br />
Summer Schools<br />
The <strong>Child</strong> Health program hosts several<br />
Summer Schools during the summer.<br />
These educational activities introduce<br />
global child health to young doctors and<br />
master’s students and stimulate working<br />
together in an international environment.<br />
The Summer School on translational<br />
medicine is organized together with<br />
students from the international Apollo<br />
Society (https://www.apollosociety.eu/)<br />
and hosts an impressive international<br />
faculty. By organizing joint events between<br />
summer schools, we are building a lasting<br />
network of young <strong>research</strong>ers.<br />
EUREKA Institute<br />
The Eureka Institute of Translational<br />
Medicine is the result of a close<br />
collaboration between the UMC Utrecht,<br />
various other top universities (Stanford<br />
University, Duke/NUS Medical School,<br />
University of Arizona, University of Miami,<br />
University College London and the<br />
University of Toronto), <strong>research</strong> institutions<br />
(TIP, Center for Translational Molecular<br />
Medicine), foundations (Dutch Arthritis<br />
Foundation) and industry (Nutricia<br />
Research). Nature Medicine and Nature<br />
Biotechnology have supported the<br />
program, in addition to providing learning<br />
materials. The Eureka Institute was initiated<br />
to develop an international community of<br />
translational medicine professionals<br />
equipped to catalyze the application of<br />
discoveries for the benefit of human<br />
health. The Institute offers a unique<br />
translational medicine course, the<br />
International Certificate Program and<br />
within this framework we’ve developed a<br />
special program for <strong>research</strong>ers appointed<br />
within <strong>Child</strong> Health. This program<br />
stimulates new <strong>research</strong>ers in crucial areas,<br />
such as teambuilding and collaboration;<br />
critical thinking and problem solving;<br />
translational medicine and valorization. In<br />
collaboration with the Eureka Institute, we<br />
also organize masterclasses with internationally<br />
renowned facilitators for young<br />
talent in <strong>Child</strong> Health.<br />
jfrenkel@umcutrecht.nl<br />
Joost Frenkel, MD, PhD<br />
is a pediatric rheumatologist<br />
with a keen interest in<br />
mechanisms of inflammaton.<br />
He is an excellent<br />
clinical teacher, putting<br />
patients and families center<br />
stage. Current <strong>research</strong><br />
involves both patientcentered<br />
education and<br />
disorders affecting the<br />
innate immune system.<br />
<br />
Boost Grants<br />
One of the main strategic themes of the<br />
<strong>Child</strong> Health program is interdisciplinary<br />
<strong>research</strong>. To stimulate young investigators<br />
to share their <strong>research</strong> experiences with<br />
colleagues outside their own professional<br />
expertise, we have launched annual Boost<br />
Grants. Young investigators within the<br />
program are asked to submit <strong>research</strong><br />
proposals in collaboration with one or<br />
more investigators in the program with<br />
whom they have never worked before.<br />
Each year, this produces 15-20 new<br />
<strong>research</strong> ideas that are presented and<br />
discussed during general <strong>Child</strong> Health<br />
meetings. The three best ideas are<br />
rewarded with an amount of 15,000 Euros<br />
to start the project and generate pilot data<br />
for future larger grant applications.<br />
Doctors must understand a patient’s<br />
perspective to establish a balanced<br />
relationship. This calls for novel education,<br />
both in the classroom and at the bedside -<br />
education that gives patients a voice that<br />
physicians hear, so they can jointly reach a<br />
shared decision.<br />
- Joost Frenkel<br />
UMC Utrecht - <strong>Child</strong> <strong>research</strong> 47
Science<br />
for life