2021 Head & Neck Cancer Conference
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
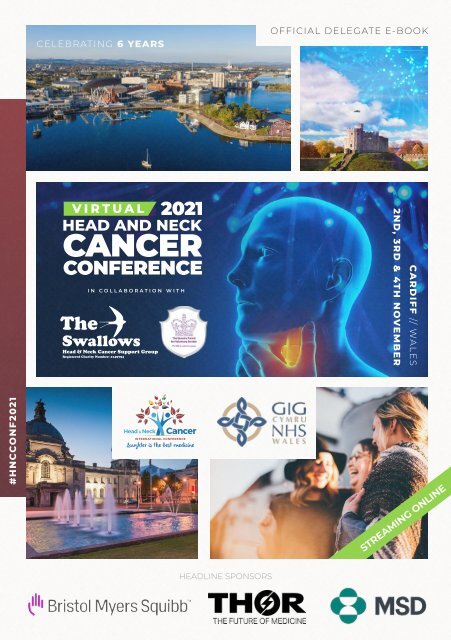
CELEBRATING 6 YEARS<br />
OFFICIAL DELEGATE E-BOOK<br />
CARDIFF // WALES<br />
2ND, 3RD & 4TH NOVEMBER<br />
#HNCCONF<strong>2021</strong><br />
STREAMING ONLINE<br />
HEADLINE SPONSORS
in the everyday<br />
Mucosamin ®<br />
Mouthwash<br />
For use alongside<br />
your daily dental<br />
routine.<br />
Mucosamin ®<br />
Oral Spray<br />
For fast, targeted<br />
relief when and<br />
where it’s needed.<br />
Targeted treatment<br />
for the relief of dry mouth<br />
and oral mucositis<br />
A soothing Mouthwash and convenient Oral Spray<br />
for the effective relief of dry mouth.<br />
• Protects the healthy oral mucosa.<br />
• Relieves the symptoms of dry mouth and oral<br />
mucositis.<br />
• Heals mouth ulcers.<br />
Mucosamin ® products can be used together to<br />
provide a convenient and effective way to help you<br />
with the effects of cancer therapy. Mucosamin ® can be<br />
used before, during and after chemo or radiotherapy.<br />
The Oral Health Foundation recognises that Mucosamin ® Mouthwash and Oral Spray are<br />
useful in helping to relieve the symptoms of dry mouth and oral mucositis, and promote the<br />
healing of the oral mucosa.<br />
Join our social media community for oral mucositis<br />
and dry mouth sufferers and caregivers<br />
@mucosamatters<br />
Always read the label<br />
2<br />
www.mucosamin.co.uk<br />
10104611315 v1.0 Oct 21<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
For more than 125 years, MSD has been inventing for life,<br />
bringing forward medicines and vaccines for many of the<br />
world's most challenging diseases in pursuit of our mission<br />
to save and improve lives. MSD is a trade name of Merck &<br />
Co., Inc., with headquarters in Kenilworth, N.J., U.S.A. We<br />
demonstrate our commitment to patients and population<br />
health by increasing access to health care through farreaching<br />
policies, programs and partnerships.<br />
Today, MSD continues to be at the forefront of research to<br />
prevent and treat diseases that threaten people and animals<br />
— including cancer, infectious diseases such as HIV and<br />
Ebola, and emerging animal diseases — as we aspire to be<br />
the premier research-intensive biopharmaceutical company<br />
in the world.<br />
For more information, visit www.msd-uk.com and connect<br />
with us @MSDintheUK on Twitter, Instagram, LinkedIn,<br />
YouTube and Facebook.
CELEBRATING 6 YEARS<br />
A warm welcome to the <strong>2021</strong><br />
<strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong> <strong>Conference</strong><br />
Welcome to everyone who has joined this year’s 6th Annual International <strong>Head</strong> & <strong>Neck</strong><br />
<strong>Cancer</strong> <strong>Conference</strong>. Due to the Covid pandemic we are once again broadcasting virtually to<br />
a PC near you. We thought long and hard about what to do this year and decided that with<br />
the uncertainty of Covid-19 and the success of last years virtual conference, we would again<br />
go virtual in order to allow as many people as possible to view.<br />
The Covid-19 pandemic has continued to have an impact on the NHS, patients and people<br />
being referred for diagnosis. Mark Lawler from DATA-CAN: The Health Data Research Hub<br />
for <strong>Cancer</strong>, has told us that the NHS will need to work at 130% just to catch up and that it will<br />
take 10 years to get back to where we were prior to pandemic. In 2022 we all need to come<br />
up with innovative ways to get on top of this problem.<br />
This years conference is different to others based on the feedback we received last year.<br />
We have introduced seminars that will allow more interaction between speakers. We’ve<br />
kept our traditional key note speakers who are always so informative, and our hope is that<br />
the mixture of the two styles will work well. A lot of 2020 participants also commented that<br />
they don’t normally get to listen to such high profile speakers, so we were keen to keep the<br />
speaker quality and mix into <strong>2021</strong>.<br />
Caregivers: on day 2 and 3 our wonderful Caregivers are highlighted in two seminars. It is<br />
important that we raise the profile of Caregivers and discuss two of the common themes<br />
that are apparent on a majority of the 24/7 calls we receive; ‘The Psychological Side of<br />
Caregiving’ and ‘Psychological Perspectives on Disease Impact and Coping.’ We hope that<br />
these seminars will shine a light on some of the issues they face.<br />
A big thank you to David Owen, our <strong>2021</strong> <strong>Conference</strong> President. The fantastic city of Cardiff<br />
and Vale University Health Board are our location hosts. David has been instrumental in the<br />
design and content of the programme, and he also introduced some of the great speakers<br />
and panellists we have on the programme this year.<br />
I wish you an enjoyable conference, and please don’t forget to feedback as your thoughts<br />
and comments are so valuable in shaping the conference for 2022. Feel free to email me<br />
directly with your suggestions.<br />
CHRIS CURTIS<br />
World <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong> Ambassador<br />
chris@theswallows.org.uk<br />
HEADLINE SPONSORS<br />
4<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
IS THE BEST<br />
LAUGHTER<br />
MEDICINE<br />
5
David Owens<br />
MBCHB, FRCS(ED), MPHIL, PGDME, FFST(ED)<br />
CONSULTANT OTOLARYNGOLOGIST, UNIVERSITY HOSPITAL OF<br />
WALES. HONORARY SENIOR LECTURER, CARDIFF UNIVERSITY<br />
>> A note from your<br />
conference host<br />
It is our pleasure to welcome you to the 6th Virtual International <strong>Head</strong> and <strong>Neck</strong> <strong>Cancer</strong><br />
<strong>Conference</strong>, organised as always by the Swallows <strong>Head</strong> and <strong>Neck</strong> cancer charity and this<br />
year hosted by The NHS University Health Board in Cardiff, in association with their sister<br />
University Health Boards throughout Wales. We had all hoped to see you in person in Cardiff<br />
this year but, owing to the ongoing global situation in relation to the COVID pandemic, the<br />
organisers, and the Welsh team, could not see a way to make that possible.<br />
<strong>2021</strong> has been another difficult year due to the ongoing COVID-19 pandemic. Its effects<br />
on services, the restricted movement of people and the safety precautions required to<br />
help reduce its spread throughout the population have had a major impact not only on<br />
the medical, psychological and rehabilitative care that people have received, but also, and<br />
importantly, on patient and carer support groups. I hope with the ongoing vaccination<br />
program and the additional boosters being delivered, as well as a greater understanding<br />
of the need for a real international solution, that next year’s conference can be face-to-face,<br />
and we can all finally meet. Although the problems with accessing health care have been<br />
widely reported nationally, I am pleased that, even during the heights of the pandemic,<br />
<strong>Head</strong> and <strong>Neck</strong> services in Wales, including assessment, diagnostics, treatments and all<br />
supportive follow-up care have continued without significant delay. This is a testament to<br />
the determination and conviction of the multidisciplinary teams involved and demonstrates<br />
the importance of head and neck cancer to NHS Wales.<br />
I am sure you will find this year’s meeting as interesting and engaging as all the previous<br />
events, and that you will receive an insight into advances in head and neck cancer care, in<br />
all its medical, surgical, psychological and allied health aspects. The programme, the range<br />
of topics and the speakers involved promise to deliver a fantastic experience for all. I also<br />
hope the meeting gives participants a perspective on head and neck care in Wales and the<br />
journeys of some of the patients and carers.<br />
Enjoy the conference and everything it entails, and hopefully, in the future, come and see<br />
the beautiful city of Cardiff in real life. If you feel you could help the Swallows or indeed have<br />
something to add to future conferences, please do let us know.<br />
6<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
A VIRTUAL WELCOME<br />
FROM<br />
CARDIFF<br />
7
TUES 2-NOV<br />
09:00<br />
- 10:00 Lobby opens<br />
10:00<br />
- 10:30<br />
<strong>Conference</strong> Opening Address<br />
David Owens <strong>Conference</strong> President<br />
10:30<br />
- 11:15<br />
11:15<br />
- 12:45<br />
Importance of Data in the fight against <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong><br />
Professor Mark Lawler (Northern Ireland) Keynote Speaker<br />
Impact on Quality of Life<br />
CHAIR: Chris Curtis, Survivor and CEO of The Swallows Charity (England)<br />
Paul Schneider, Survivor (England)<br />
Ben Sheard, Survivor (England)<br />
Freya Sparks, Clinical Doctoral Research Fellow (England)<br />
12:45<br />
- 13:30<br />
The World of the Biopsy<br />
Dr Ali Khurram (England) Keynote Speaker<br />
13:30<br />
- 15:00<br />
I am Voiceless but not Speechless<br />
CHAIR: Jane Thornton, Speech and Language Therapy (England)<br />
Marianne Kooijman, Survivor (Holland)<br />
Steven Cooper, Survivor (USA)<br />
Tanja Bage, Survivor (England)<br />
Daniela Esteves, <strong>Head</strong> of Nursing Team at ATOS<br />
15:00<br />
- 15:30<br />
Living and learning: a cancer journey through a global pandemic<br />
Niki Shaw, Patient (England) Keynote Speaker<br />
15:30<br />
- 16:30<br />
Showcase: <strong>Head</strong> & <strong>Neck</strong> Services (Wales)<br />
CHAIR: David Owens, <strong>Conference</strong> President<br />
Luke Maxwell<br />
Roger Maggs, 3D printing for dental prosthetics and for surgical precision<br />
Peter Llewelyn<br />
16:30<br />
- 17:15<br />
Reducing the Incidence and Severity of Oral Mucositis with Photobiomodulation<br />
James Carroll, Renowned expert on Photoboimodulation (UK) Keynote Speaker<br />
17:15<br />
- 17:30<br />
Day 1 Closing Address<br />
David Owens <strong>Conference</strong> President<br />
8<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
WEDS 3-NOV<br />
08:00<br />
- 09:00<br />
Lobby opens<br />
09:00<br />
- 09:15<br />
Day 2 Opening Address<br />
David Owens <strong>Conference</strong> President<br />
09:15<br />
- 10:45<br />
10:45<br />
- 11:30<br />
11:30<br />
- 13:00<br />
New Drugs in the fight against <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong><br />
CHAIR: Arthur Lauretano (USA)<br />
Dr Lauren V. Wood, Chief Medical Officer PDS Biotechnology (USA)<br />
Dr Ali Khurram (England)<br />
The gap between dietitians and your home kitchen<br />
Yvonne McClaren, H&N <strong>Cancer</strong> Survivor (Australia) Keynote Speaker<br />
Latest Technology in the fight against H&N <strong>Cancer</strong><br />
CHAIR: Derek Lewthwaite (England)<br />
Naseem Ghazali, <strong>Head</strong> & <strong>Neck</strong> Oncology, and Reconstructive Surgery, (England)<br />
Mr Sandeep Berry, Consultant Otolaryngologist and <strong>Head</strong> & <strong>Neck</strong> Surgeon (Wales)<br />
Brian Pikkula PhD, CSO Forward Science (USA)<br />
13:00<br />
- 13:30<br />
Just one journey amongst millions<br />
Paul Schneider, H&N <strong>Cancer</strong> Survivor (England) Keynote Speaker<br />
13:30<br />
- 15:00<br />
Quality of Life after Hemiglossectomy<br />
CHAIR: Ben Sheard, Survivor (England)<br />
Laura Marsden, Survivor (England)<br />
Barbara Reed, Survivor (England)<br />
Stef Gayhart, Survivor (USA)<br />
15:00<br />
- 16:00<br />
Caregiver (Pt 1) Psychological Perspectives on Caregiving<br />
CHAIR: Derek Lewthwaite (England)<br />
Dr John Donohue, Senior Clinical Psychologist<br />
Debbie Eason, Caregiver (Spain)<br />
Andrew Hyde, Caregiver (England)<br />
16:00<br />
- 17:30<br />
Research Projects in <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong><br />
CHAIR: Dr Elaine Emmerson, The University of Edinburgh (Scotland)<br />
Arutha Kulasinghe, Spatial Biology and Liquid Biopsy Group Leader & Winner<br />
of our Research Award last years conference (Australia)<br />
Miss Kate Hulse, ENT registrar (ST3) (Scotland)<br />
Miss Catriona M Douglas, Consultant ENT/<strong>Head</strong> and <strong>Neck</strong> Surgeon (Scotland)<br />
17:30<br />
- 17:45<br />
Day 2 Closing Address<br />
David Owens <strong>Conference</strong> President<br />
9
THURS 4-NOV<br />
08:00<br />
- 09:00<br />
Lobby opens<br />
09:00<br />
- 09:15<br />
Day 3 Opening Address<br />
David Owens <strong>Conference</strong> President<br />
09:15<br />
- 10:00<br />
Saved… the jaws that are wrecked by radiotherapy - Osteoradionecrosis (ORN)<br />
Mr Vinod Patel, Consultant, Oral Surgery Keynote Speaker<br />
10:00<br />
- 11:30<br />
Proton Therapy in the battle against <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong><br />
CHAIR: Laura Marsden, Survivor (England)<br />
Dr Russell Banner, Consultant Clinical Oncologist at NHS Wales (Wales)<br />
Arthur M. Lauretano, Chief Medical Officer (USA)<br />
Sue Acreman, Consulting Oncology Dietitian Case study<br />
11:30<br />
- 12:00<br />
The Young Tongues - empowering peer support for uncommon cancers (When<br />
the average age of your waiting room is 70+, but you are 31)<br />
Barbara Reed, Survivor (England) Keynote Speaker<br />
12:00<br />
- 13:30<br />
Preventing and treating side effects of <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong><br />
CHAIR: Ben Sheard (England)<br />
Emma Hallam, Consultant Radiographer (England)<br />
Paul Burns, THOR Photomedicine, (England)<br />
Dr Jane Mathlin, Therapeutic Radiographer <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong> (Wales)<br />
13:30<br />
- 14:30<br />
Caregiver (Pt 2) Psychological Perspectives on Disease Impact & Coping<br />
CHAIR: Andrew Hyde (England)<br />
Dr John Donohue, Senior Clinical Psychologist<br />
Isabel Hill, Caregiver<br />
Emily Stuart RD, Nutritionist/Specialist<br />
14:30<br />
- 16:00<br />
New Medicine & Techniques for <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong><br />
CHAIR: Andrew Osafo or Chris Barrow<br />
Mahesh Kumar, Consultant | Dr Tripat K Mahajan, Dental Training<br />
Dr Anthony Kong, Reader & Honorary Consultant Clinical Oncologist (England)<br />
Abdul Ahmed (Consultant in Oral & Maxillofacial Surgery)<br />
Kevin Chiu (Consultant <strong>Head</strong> and <strong>Neck</strong> Clinical Oncologist)<br />
16:00<br />
- 16:30<br />
2022 <strong>Conference</strong> Hosts and location announcement<br />
Chris Curtis, Survivor and CEO of The Swallows Charity (England)<br />
David Owens, <strong>2021</strong> <strong>Conference</strong> President<br />
16:30<br />
- 17:00<br />
Day 3 and <strong>Conference</strong> Closing Address<br />
David Owens <strong>Conference</strong> President<br />
10<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Friends of<br />
The Swallows<br />
Thank you to all our friends<br />
for your ongoing support<br />
11
The conference that<br />
was out of this world...<br />
The start of the Covid-19 pandemic seems a long<br />
time ago now, and it’s safe to say a lot has changed<br />
in the world, both bad and good! We’ve learned to<br />
adapt to things in new ways, developed new skills<br />
during numerous lockdowns and above all found a<br />
new admiration for those working in emergency and<br />
medical services.<br />
When planning started for the 2020 conference, we<br />
chose Edinburgh as our host city and looked forward to<br />
spending a few days in a historical city. Fast forward a few<br />
months and we had to make the hard decision to turn<br />
the conference virtual for the first time in our history.<br />
12<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
New technology, plans flipped<br />
upside down and all hands on deck<br />
resulted in a smooth delivery of our<br />
5th consecutive conference, despite<br />
the challenges of covid.<br />
Supported by our ever-willing<br />
<strong>Conference</strong> President Iain Nixon<br />
and NHS Lothian, we were able to<br />
stream the conference globally on<br />
YouTube to an existing and totally<br />
new audience.<br />
The format of the virtual conference<br />
meant we were able to host a live<br />
in-depth panel Q&A discussion<br />
at the end of each day, hosted by<br />
Arthur Lauretano all the way from<br />
Boston, USA.<br />
Not to be scuppered by the<br />
covid restrictions, Chris Curtis still<br />
managed to produce the now<br />
infamous comedy sketch that<br />
opens each day of the conference.<br />
Once again we had speakers from<br />
various countries, and tackled<br />
subjects such as ‘Living with and<br />
beyond <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong>’ and<br />
‘The importance of collaboration<br />
between the patient, caregiver and<br />
health professionals’ amongst other<br />
important areas.<br />
Here’s to another successful<br />
conference in <strong>2021</strong>.<br />
13
<strong>2021</strong> SPEAKERS<br />
The International <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong> <strong>Conference</strong> is delighted to welcome<br />
a range of health professionals, patients and carers from around the world<br />
to take part in seminars and keynote sessions to dive into the latest and<br />
most interesting topics from the last 12 months.<br />
Your <strong>2021</strong><br />
<strong>Conference</strong> Host<br />
David Owens MBCHB, FRCS(ED), MPHIL, PGDME, FFST(ED)<br />
CONSULTANT OTOLARYNGOLOGIST, UNIVERSITY HOSPITAL OF WALES.<br />
HONORARY SENIOR LECTURER, CARDIFF UNIVERSITY<br />
David is a Consultant ENT surgeon and has been working at<br />
the University Hospital of Wales and as part of the South East<br />
Wales <strong>Head</strong> and <strong>Neck</strong> <strong>Cancer</strong> Network since 2011. He has a<br />
research interest and is involved in a number of trials aimed at<br />
improving treatment and have been involved in studies evaluating<br />
survivorship issue in people following treatment for head and <strong>Neck</strong><br />
<strong>Cancer</strong>. He is immensely proud that Cardiff has been chosen as<br />
host for the event in <strong>2021</strong>.<br />
CATCH DAVID ON: DAY 1 // DAY 2 // DAY 3<br />
Your <strong>Conference</strong><br />
President<br />
Chris Curtis<br />
HEAD & NECK CANCER SURVIVOR<br />
AND CEO OF THE SWALLOWS HEAD & NECK CANCER CHARITY<br />
“How three small words, changed my life forever.” I’m the<br />
founder of The Swallows <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong> Support Group.<br />
My life changed for the better after my diagnosis of <strong>Head</strong> & <strong>Neck</strong><br />
<strong>Cancer</strong>. On Friday 13th May 2011 at 11am my life fell apart with my<br />
diagnosis. I spiralled into a depression so it was suggested I could<br />
get involved with the cancer support network so in November 2011<br />
I joined the group. Fast forward to <strong>2021</strong> and the Swallows <strong>Head</strong> &<br />
<strong>Neck</strong> <strong>Cancer</strong> Charity is thriving and supporting people around the<br />
world, every day.<br />
CATCH CHRIS ON: DAY 1 // DAY 2 // DAY 3<br />
Dr. Arutha Kulasinghe<br />
PHD (CANCER BIOLOGY). BSC HONS (MEDICAL MICROBIOLOGY)<br />
Dr Arutha Kulasinghe is a Peter Doherty NHMRC early career research<br />
fellow at the Queensland University of Technology (QUT) and the<br />
Translational Research Institute. Dr Kulasinghe completed his Bsc<br />
(Hons) in medical microbiology at the University of Pretoria (South<br />
Africa) in 2013 and his PhD in 2017 in the study of micro-metastatic<br />
disease in lung cancer. He now leads the “Spatial biology and liquid<br />
biopsy” group in the <strong>Cancer</strong> and Ageing Research Program (CARP)<br />
at QUT.<br />
CATCH ARUTHA ON: DAY 2<br />
14<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
15<br />
Barbara Reed-Fountain EVENT CONCEPT DESIGNER<br />
Barbara unexpectedly got diagnosed with Squamous Cell Carcinoma<br />
of the Tongue in early 2019 aged 31 at the Norfolk and Norwich<br />
University Hospital. Following a partial hemiglossectomy with partial<br />
neck dissection it was discovered that her stage 1 tumour had spread<br />
in to one lymph node. She took the decision not to proceed with<br />
radiotherapy, but instead opted for a watch and wait approach. After<br />
over two years there is no sign of disease, but regular check ups<br />
continue. Barbara will share her experience of the surgery, what impact<br />
it has had on her physical and mental wellbeing.<br />
CATCH BARBARA ON: DAY 2 // DAY 3<br />
Dr. Ali Khurram BDS, MSC, PHD, MFDS-RCS (EDINBURGH), CILT, FHEA, FDS-RCS (ENGLAND), FRCPATH<br />
SENIOR CLINICAL LECTURER AND CONSULTANT PATHOLOGIST<br />
AT THE UNIVERSITY OF SHEFFIELD<br />
Dr Khurram is involved in the diagnosis of <strong>Head</strong> and neck cancers on<br />
a daily basis and is the clinical lead for the oral pathology diagnostic<br />
service covering most of South Yorkshire. Prior to his training as a<br />
pathologist, he worked as a junior doctor in Oral and Maxillofacial<br />
Surgery and is aware first hand of the devastating nature of these<br />
cancers. He is extremely passionate about raising awareness to aid early<br />
detection and treatment.<br />
CATCH ALI ON: DAY 1<br />
Dr Elaine Emmerson B.SC. (HONS), PH.D.<br />
Elaine graduated from The University of Liverpool in 2004 with a B.Sc.<br />
(Hons) in Genetics, then became a research technician at the University<br />
of Manchester, before beginning a Ph.D. in wound healing in 2006,<br />
receiving her doctorate in 2010. In 2013 Elaine moved to the University<br />
of California San Francisco to begin a Postdoctoral Research Fellow<br />
position. She investigated the interaction between nerves and stem<br />
cells during organ development, using the mouse and human salivary<br />
gland as a model organ.<br />
CATCH ELAINE ON: DAY 2<br />
James Carroll FOUNDER CEO OF THOR PHOTOMEDICINE<br />
James Carroll is an engineer, founder CEO of THOR Photomedicine.<br />
THOR develops Laser and LED Photobiomodulation devices (PBM)<br />
that heal wounds, reduce inflammation and relieve pain. James has coauthored<br />
24 academic papers on PBM, 6 of them with Harvard Medical<br />
School and has co-authored 4 books. He has presented on PBM at the<br />
United Nations Global Health Impact Forum, US Congress on solutions<br />
to the opioid crisis and to policy advisors at the White House.<br />
James took PBM through the NICE guidance process and PBM is now<br />
recommended for preventing or treating oral mucositis.<br />
CATCH JAMES ON: DAY 1
<strong>2021</strong> SPEAKERS<br />
Emma Hallam BSC MSC PGCERTNMP<br />
Emma is a Macmillan Consultant Radiographer at The Nottingham<br />
Radiotherapy Centre. After qualifying in 1998 she specialised in<br />
information and support and in 2013 dedicated her role to support<br />
head and neck cancer patients throughout the treatment pathway.<br />
In 2013 she developed and now leads the Award winning Macmillan<br />
Nottingham Radiotherapy Late Effects Service which has been a truly<br />
humbling experience. Education on late effects and the impact that<br />
such consequences have on a patient’s quality of life is a key element of<br />
Emma’s work.<br />
CATCH EMMA ON: DAY 3<br />
Miss Kate Hulse BSC MBCHB MRCS (ENT)<br />
Kate is an ENT registrar working in the West of Scotland. Kate was<br />
an undergraduate at the University of Glasgow and has since trained<br />
in Manchester, Inverness and Edinburgh. She has recently started a<br />
part-time PhD with the University of Strathclyde alongside full-time<br />
clinical work at the Queen Elizabeth Hospital, Glasgow. Her research is<br />
around health technology in the care of head and neck cancer patients.<br />
Her aim is to create an app which can monitor patients’ physical and<br />
mental well-being and feed back to the appropriate clinical teams, so<br />
patients get the right support at the right time.<br />
CATCH KATE ON: DAY 2<br />
Paul Schneider 2X CANCER SURVIVOR<br />
I’m a 45 year old dad of a beautiful 11 year old daughter, step dad to two<br />
great girls and now fiancee to the most incredible girl I’ve ever met. I<br />
have been working since I was 17 and currently work in a great role for<br />
a UK Telecoms engineering business. I beat Thyroid cancer at 21 and a<br />
parotid cancer diagnosis in December 2020 which lead to emergency<br />
major surgery in January, followed by 6 weeks of radiotherapy.<br />
Nowadays I’ve reignited my DJ hobby and regularly DJ online on the<br />
radio and soon to be playing in nightclubs and other venues again. I<br />
am a house music lover with a strong sense of family values.<br />
CATCH PAUL ON: DAY 1 // DAY 2<br />
Dr Jane Mathlin DAHP, MSC, DCR(T),IP<br />
CONSULTANT RADIOGRAPHER – HEAD &NECK CANCER<br />
I’ve been consultant radiographer for head and neck patients at Velindre<br />
<strong>Cancer</strong> Centre for 3 years. One of the objectives of the role was to introduce<br />
a late side effects clinic for patients treated for head and neck cancers.<br />
I have many years’ experience in the management of side effects of<br />
radiotherapy during after treatment and am an independent prescriber.<br />
I have recently completed a Professional Doctorate looking at the<br />
experience of taste changes during radiotherapy for head & neck cancer.<br />
CATCH JANE ON: DAY 3<br />
16<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
17<br />
Niki Shaw LIVED EXPERIENCE OF THROAT CANCER<br />
KEYNOTE SPEAKER, STRATEGIC MANAGER WITHIN ADULT SOCIAL CARE<br />
Born in Zimbabwe, she moved to England as a child and now lives in<br />
Scotland with her husband. In September 2020, after many months of<br />
tests, investigations, scans and biopsies, Niki was formally diagnosed<br />
with a T3 hypo-pharyngeal squamous cell carcinoma at 38 years old.<br />
She subsequently underwent an intensive six week course of radical<br />
chemo-radiotherapy as an inpatient within the renowned Beatson<br />
<strong>Cancer</strong> Centre (Glasgow) during the COVID-19 pandemic. Niki returned<br />
to work in February <strong>2021</strong> and, in April, a scan revealed a complete<br />
metabolic response to treatment.<br />
CATCH NIKI ON: DAY 1<br />
Mr Sandeep Berry MBBS;MS;DLO(RCS ENG); MRCS(ED); FRCS (ORL-HNS); MPHIL<br />
CONSULTANT ENT HEAD NECK SURGEON<br />
I am a consultant ENT head neck surgeon based at the University<br />
Hospital of Wales, Cardiff and Clinical director for ENT and OMFS and<br />
<strong>Cancer</strong> Lead for Surgical Board. I undertook my head and neck surgery<br />
fellowship in Melbourne, Australia and training for Trans-oral Robotic<br />
surgery in head neck surgery. I was instrumental in setting of the<br />
regional service for Transoral robotic (TORS) for head neck at University<br />
hospital of Wales, Cardiff and am one of the members of the team who<br />
deliver this service.<br />
CATCH SANDEEP ON: DAY 2<br />
Vinod Patel BDS (HONS), MORALSURG RCS ENG, PHD<br />
Mr Patel is a consultant oral surgeon at Guy’s & St Thomas’ Hospital<br />
with a specialist interest in the oral and dental management of cancer<br />
patients. He currently leads the Bone & Jaw Necrosis clinic which has<br />
managed over 450 established osteonecrosis of the jaw cases. Mr<br />
Patel has over 100 peer reviewed publications and completed his PhD<br />
assessing the impact and effect of radiotherapy in oropharyngeal cancer.<br />
CATCH VINOD ON: DAY 3<br />
Steven Cooper LARYNGECTOMEE SURVIVOR<br />
I am a lifelong resident of the state of Maryland, USA. I had my<br />
laryngectomy in February 2019 and a secondary puncture with<br />
Tracheoesophageal Voice Prosthesis (TEP) placement in September<br />
2019. Because of the early help I received from many of the wonderful<br />
members of the Laryngectomee community, I have been instilled<br />
with a heartfelt desire to assist other Laryngectomees in any way<br />
that I can. I’m a board member of the International Association of<br />
Laryngectomees (IAL), the Laryngectomee Club of Montgomery<br />
County Maryland (LCMC) and the Governor’s Advisory Board for<br />
Telecommunications Relay in Maryland, plus much more!<br />
CATCH STEVEN ON: DAY 1<br />
17
<strong>2021</strong> SPEAKERS<br />
Dizzy Marston FOOD WRITER AND TONGUE CANCER THRIVER<br />
In 2019 I was diagnosed with stage 4 advanced oral cancer. I had a<br />
5.5cm tumour invading my tongue. He had to go, but with it he also<br />
took my tongue. I was told that I would never eat or speak again,<br />
unless I used a machine to speak and a tube into my stomach for liquid<br />
nutrition to be pumped through. I refused to accept that my life would<br />
be that drastic, so I pushed myself to learn to swallow, speak and then<br />
finally eat. After many long months of tears, frustration, anger, grit<br />
and determination, I did it - I achieved my objective! In <strong>2021</strong> I launched<br />
‘Eating with Confidence’, a dedicated cook book to help others like me.<br />
CATCH LAURA ON: DAY 2 // DAY 3<br />
Dr Tripat K Mahajan<br />
Tripat studied dentistry at King’s College London and graduated<br />
in 2018. She is currently in a Dental Core Training pathway, gaining<br />
further experience in oral and maxillofacial surgery, restorative and<br />
orthodontic dental specialties. She enjoys keeping up to date with the<br />
latest research and has regularly presented at and attended a variety<br />
of dental conferences. Whilst working in maxillofacial surgery, she saw<br />
how mouth cancer can have a huge effect on oral wellbeing and the<br />
impact it can have on quality of life. She was appointed as a clinical<br />
ambassador for the Mouth <strong>Cancer</strong> Foundation in January <strong>2021</strong>.<br />
CATCH TRIPAT ON: DAY 3<br />
Tanja Båge<br />
On March 16th 2020 I was diagnosed with laryngeal cancer. My<br />
cancer journey really began approximately 2 years before I was<br />
eventually diagnosed when I first started to notice subtle symptoms<br />
of breathlessness and wheezing. After 2 years of mis-diagnosis I<br />
eventually received my diagnosis – adenoid cystic carcinoma in my sub<br />
glottis and trachea. 1 week later I was heading into major life changing<br />
surgery. During surgery they did a total laryngectomy and neck<br />
dissection. I lost the connection between my nose, mouth and lungs<br />
and gained a permanent stoma to breathe through on my neck. I lost<br />
my natural voice. Losing my voice has felt like losing a limb. It is a part<br />
of me that’s gone forever now. I’m here today though, living life and<br />
thankful for every single day.<br />
CATCH TANJA ON: DAY 1<br />
BDS (HONS), MFDS RCSENG, MCGDENT,<br />
PGCERT DENTED<br />
Andrew Hyde BSC, PGCE, LPSH<br />
HEAD & NECK CANCER PATIENT CAREGIVER<br />
Andrew has direct experience of being a caregiver for a <strong>Head</strong> and <strong>Neck</strong><br />
<strong>Cancer</strong> patient. His wife underwent surgery in 2015, 2017 and then a<br />
major operation in 2019. She relied upon him and he had to learn quickly.<br />
He has, through The Swallows <strong>Head</strong> and <strong>Neck</strong> <strong>Cancer</strong> Charity, become<br />
an advocate for caregivers. <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong> patients depend upon<br />
Caregivers looking after ourselves so that they are able to care for them!<br />
CATCH ANDREW ON: DAY 2<br />
18<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
19<br />
Daniela Esteves HEAD OF NURSING AT ATOS CARE – HEAD<br />
AND NECK SPECIALIST NURSE, CRITICAL CARE NURSE BACKGROUND<br />
Daniela has been an Intensive Care Nurse within the NHS for several<br />
years before setting up a community service with Atos Care for patients<br />
with laryngectomy and tracheostomy stomas. Daniela has worked<br />
as a field Nurse in London and the southeast. She has supported<br />
patients at home following surgical treatment of laryngeal cancer<br />
(laryngectomy) and patients who required a tracheostomy tube as part<br />
of their treatment and recovery. Daniela now leads a team of specialist<br />
<strong>Head</strong> and <strong>Neck</strong> Nurses who care for patients with a neck stoma in the<br />
community, covering most of England and Wales. Daniela’s team works<br />
closely with NHS clinicians to support each patient’s transition from<br />
hospital to home with managing their neck airway.<br />
CATCH DANIELA ON: DAY 1<br />
Dr John Donohue CHARTERED CLINICAL PSYCHOLOGIST<br />
Dr Donohue gained his Undergraduate Degree in 1998 from University<br />
College Worcester, UK and Montclair State University, New Jersey,<br />
USA. Following posts in forensic, learning disabilities and child mental<br />
health, he gained his master’s degree in Counselling Psychology with<br />
family therapy and primary care mental health settings experience.<br />
In 2004, he was successful in his application to the clinical psychology<br />
course offered by the University of Coventry, and gained his doctoral<br />
accreditation as a clinical psychologist in 2007. Upon qualification, he<br />
secured a post in Russells Hall Hospital UK, working primarily in the<br />
oncology and clinical haematology wards in the hospital. In 2018 he<br />
returned to his native Ireland and following a short phase in private<br />
practice, became employed as senior clinical psychologist and centre<br />
lead for <strong>Cancer</strong> Care Wests’ satellite service in Co. Donegal. Dr Donohue<br />
is an avid explorer having travelled as far as Antarctica, Kilimanjaro,<br />
Base Camp Everest and Peru.<br />
CATCH JOHN ON: DAY 2 // DAY 3<br />
Dr Russell Banner<br />
CONSULTANT CLINICAL ONCOLOGIST BASED IN SOUTH WALES<br />
Russell’s undergraduate training was at Christ’s College, Cambridge<br />
and then at Guy’s, Kings and St. Thomas’ Medical School in London,<br />
qualifying in 2002. He started his speciality training in Canterbury in<br />
2007 and then transferred to complete his training in South Wales<br />
gaining Fellowship of the Royal College of Radiologists in 2010. Russell<br />
took up his post as a Consultant Clinical Oncologist in the South West<br />
Wales <strong>Cancer</strong> Centre in 2013.<br />
He is enthusiastically research active with Principal Investigator roles<br />
in Swansea for a number of UK-wide randomised clinical research<br />
radiotherapy trials. Russell currently specialises in tumour sites for head &<br />
neck and non-melanoma skin cancers. He is trained in the use of proton<br />
beam therapy, treating patients in the Rutherford <strong>Cancer</strong> Centre, South<br />
Wales since it opened in 2018 and looks forward to further developing<br />
the evidence base for this, including within the ‘TORPEdO’ randomised<br />
clinical trial. Russell was born in London, though his mother ensured that<br />
his first rugby shirt was Welsh!<br />
CATCH RUSSELL ON: DAY 3<br />
19
<strong>2021</strong> SPEAKERS<br />
Abdul Ahmed<br />
After completing both Medical and Dental degrees, Mr Ahmed<br />
completed his surgical training at The Royal London, University college,<br />
Great Ormond Street, and Northwick Park hospitals. Mr Ahmed has a<br />
very innovative practice using the latest technologies in head and neck<br />
reconstructive planning, the use of sentinel node surgery in oral cancer<br />
and Trans Oral Robotic Surgery. He has a strong interest in teaching<br />
and training. He is an Honorary Senior Clinical Lecturer at Queen Mary<br />
University of London. Educational supervisor for the London School of<br />
Surgery, and runs regular courses in Reconstructive Surgery, ATLS, and<br />
Microvascular surgical techniques. Mr Ahmed is part of the faculty for<br />
the Griffin institute for medical research, they provide a wide variety of<br />
course, all aimed at improving the skills and experience of healthcare<br />
professionals to advance patient care. As a clinical researcher, he is<br />
involved in several clinical trials in oncology, and regularly presents in<br />
international meetings.<br />
CATCH ABDUL ON: DAY 3<br />
CONSULTANT IN ORAL & MAXILLOFACIAL SURGERY SPECIALISING<br />
IN RECONSTRUCTIVE HEAD AND NECK SURGERY<br />
Naseem Ghazali BDS, MBBS, MSC, MD, DOHNS, FDSRCS, FRCS(OMFS)<br />
Miss Naseem Ghazali is a Consultant Oral & Maxillofacial Surgeon,<br />
sub-specialsing in <strong>Head</strong> and <strong>Neck</strong> Oncology & Reconstruction, at Royal<br />
Blackburn Teaching Hospital. Miss Ghazali is a credentialed da Vinci<br />
Robot surgeon, and has pioneered minimally invasive surgery on the<br />
robotic platform for H&N <strong>Cancer</strong> at her hospital. She has successfully<br />
established the Transoral Robotic <strong>Head</strong> & <strong>Neck</strong> Surgery (TORS) Service<br />
for East Lancashire NHS Trust within the first year of her appointment<br />
in 2016. This service is currently the only TORS service for the North-<br />
West of England. During this time, she has developed a novel approach<br />
for scarless, benign salivary gland surgery on the robotic platform.<br />
CATCH NASEEM ON: DAY 2<br />
Dr Kevin Chiu<br />
CONSULTANT HEAD AND NECK CLINICAL ONCOLOGIST AT MOUNT VERNON<br />
CANCER CENTRE<br />
Kevin specialises specifically in complex radiotherapy, immunotherapy<br />
and chemotherapy in the management of head and neck cancer.<br />
Dr Chiu obtained his medical degree at the University of Manchester<br />
in 2005. He gained his FRCR qualification in clinical oncology in 2014<br />
and went on to complete a senior head and neck clinical and research<br />
fellowship at Princess Margaret <strong>Cancer</strong> Centre in Toronto in 2017. Since<br />
2019 he has been the Clinical Lead for all Radiation Services at Mount<br />
Vernon <strong>Cancer</strong> Centre, working and collaborating with the London<br />
Radiotherapy Network to improve radiotherapy services. Dr Chiu’s own<br />
clinical practice covers a big geographical area with patients referred<br />
from Hertfordshire, Bedfordshire and Northwest London. Dr Chiu is<br />
the Research Lead for head and neck research at Mount Vernon. His<br />
interests include optimising radiotherapy techniques to improve patients’<br />
outcomes and quality of life, Artificial Intelligence and Clinical Trials.<br />
CATCH KEVIN ON: DAY 3<br />
20<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
21<br />
Miss Catriona M Douglas BSC (MED SCI), MBCHB, MD, FRCS<br />
I am a Consultant <strong>Head</strong> and <strong>Neck</strong> Surgeon based at the Queen Elisabeth<br />
University Hospital, Glasgow, UK. I undertook my clinical training in<br />
Glasgow and the West of Scotland before completing a 1 year fellowship<br />
in <strong>Head</strong> and <strong>Neck</strong> Surgical Oncology at the University of Toronto/Princess<br />
Margaret Oncology Hospital, in Toronto, Canada. I have a research<br />
interest in <strong>Head</strong> and <strong>Neck</strong> cancer and completed my MD in “Biomarkers<br />
that predict treatment response in <strong>Head</strong> and <strong>Neck</strong> <strong>Cancer</strong>” at the<br />
University of Manchester. I have a strong research interest in <strong>Head</strong> and<br />
<strong>Neck</strong> cancer, and have ongoing projects in translational research and<br />
quality of life. I feel very privileged to work with and treat H&N <strong>Cancer</strong><br />
patients, and by doing clinical research I hope that it will improve the<br />
quality of care and life that these patients have.<br />
CATCH CATRIONA ON: DAY 2<br />
Isabell Hill CERTIFICATE OF PRIMARY EDUCATION<br />
HEAD & NECK CANCER PATIENT CAREGIVER<br />
Isabell worked in the education sector as a primary school teacher and<br />
later as an Adult Literacy Tutor. She also spent some years in the Civil<br />
Service but has since retired. She has been a caregiver for my husband<br />
since 2013, and she is a valuable member of The Swallows <strong>Head</strong> & <strong>Neck</strong><br />
Charity Caregiver Project Group.<br />
CATCH ISABELL ON: DAY 3<br />
Yvonne McClaren<br />
AUTHOR, COACH AND FOUNDER OF THE NO FEEDING TUBES MOVEMENT &<br />
THE MIND FOOD BODY PROGRAM<br />
The program is specifically designed to assist others with dysphagia and<br />
a peg feed tube transition back to oral eating. Working as an executive<br />
in the not-for-profit sector and with a love for travel, Yvonne has lived in<br />
Sydney, Melbourne, Bangkok, Kuala Lumpur and for a few months in<br />
Vietnam when she was diagnosed with Oropharyngeal <strong>Cancer</strong> (Tonsil<br />
<strong>Cancer</strong>) in November 2018. Yvonne went on to have a third of her tongue<br />
removed, both tonsils, 30 lymph nodes and 30 chemoradiotherapy<br />
sessions. Yvonne also had a PEG tube feed for 15 months. Yvonne is a<br />
passionate advocate for using real food to transition back to oral eating.<br />
CATCH YVONNE ON: DAY 2<br />
Andrew Osafo BDS DIP SED FIADFE<br />
Andrew graduated from Barts and the London School of Medicine<br />
and Dentistry in 2003 and works in primary and secondary care. He<br />
has a special interest in Minimally Invasive Dentistry, Facial Aesthetics,<br />
Pain free dentistry and Orthodontics. Andrew is also passionate about<br />
health & aesthetics and enjoys helping people get a confidence<br />
boost. Dr Osafo tests products, lectures and writes articles for various<br />
organisations. Andrew is an ambassador for the Mouth <strong>Cancer</strong><br />
Foundation. Dr Andrew received the International Academy for Dental<br />
Facial Esthetics Fellowship. Fellowship in the Academy for Dental Facial<br />
Esthetics is by invitation to those members of the dental industry who<br />
have distinguished themselves.<br />
CATCH ANDREW ON: DAY 3<br />
21
<strong>2021</strong> SPEAKERS<br />
Stephanie Gayhart REGISTERED NURSE (CRITICAL CARE/ICU)<br />
In August 2019, Stephanie was 37 years old and working as an RN<br />
when she found the lump on her tongue. After being told a few<br />
times she was too young and healthy for the worst, an ENT ordered<br />
a CT scan and referred her the next day to a specialist at University<br />
of Maryland in Baltimore, MD, USA. She was diagnosed with Stage III<br />
oral tongue cancer with no predisposing risk factors and underwent<br />
a hemiglossectomy with radial free-flap reconstruction (using cow<br />
collagen, Integra, in a two-step healing process for the flap donation<br />
site), partial neck dissection, and temporary tracheostomy placement.<br />
About two months later she completed 6 weeks of IMRT. She’ll speak<br />
about how the diagnosis and treatment side effects have affected her<br />
quality of life, including her mental and physical well-being and ability<br />
to work.<br />
CATCH STEPHANIE ON: DAY 2<br />
Mark Lawler<br />
ASSOCIATE PRO-VICE CHANCELLOR, PROFESSOR OF DIGITAL HEALTH & CHAIR<br />
IN TRANSLATIONAL CANCER GENOMICS AT QUEEN’S UNIVERSITY BELFAST<br />
His patient centred research and policy work has had international<br />
impact, recognised by a number of national and international awards.<br />
He is Scientific Director of DATA-CAN, the UK’s Health Data Research<br />
Hub for <strong>Cancer</strong>. DATA-CAN’s work on Covid-19 and cancer first<br />
highlighted the significant impact of the pandemic on cancer services<br />
and cancer patients. He co-chairs the European <strong>Cancer</strong> Organisation’s<br />
Special Network on Covid-19 and <strong>Cancer</strong> and leads their TimeToAct<br />
Campaign to ensure that <strong>Cancer</strong> doesn’t become the Forgotten C in<br />
the Fight against <strong>Cancer</strong>.<br />
CATCH MARK ON: DAY 1<br />
Lauren V. Wood, M.D.<br />
CHIEF MEDICAL OFFICER<br />
Dr. Wood joined PDS Biotech as Chief Medical Officer in February 2019.<br />
She has overall responsibility for clinical development of the novel,<br />
immune activating Versamune® platform product pipeline targeting<br />
HPV-related pre-cancer and advanced cancers as well as a broad<br />
spectrum of solid tumors. With 30 years of extensive clinical research<br />
experience at the National Institutes of Health, Dr. Wood most recently<br />
was the Clinical Director of the Vaccine Branch, Center for <strong>Cancer</strong><br />
Research, National <strong>Cancer</strong> Institute (NCI), where she oversaw the<br />
translational development of immune-based therapies for both cancer<br />
and HIV infection and was a co-inventor of two patented therapeutic<br />
cancer vaccine platforms targeting the TARP and HER tumor antigens.<br />
CATCH LAUREN ON: DAY 2<br />
22<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
23<br />
Sue Acreman<br />
RD MSC FBDA, DIP DIETETICS, MSC INTERPROFESSIONAL STUDIES(HEALTH),<br />
POST GRADUATE DIPLOMA IN RESEARCH METHODS, ISM DIP. MANAGEMENT<br />
Sue has been an HCPC registered Dietitian for 47 years and has worked<br />
in Oncology dietetics for over 30 years, she is a fellow of the British<br />
Dietetic Association and a member of its specialist oncology group.<br />
Sue is the oncology dietitian for Rutherford <strong>Cancer</strong> treatment centres<br />
at both Thames Valley and South Wales. Working within the MDT she<br />
provides nutritional support to patients during their treatment and<br />
beyond. Her aim is to help patients meet their nutritional requirements<br />
and maintain their weight which helps improve outcomes and<br />
minimise their risk of developing nutrition-related complication.<br />
CATCH SUE ON: DAY 3<br />
Brian Pikkula<br />
PHD IN BIO-OPTICS, CHIEF SCIENTIFIC OFFICER AND CO-FOUNDER OF<br />
FORWARD SCIENCE<br />
Brian received his bachelor’s degree in biomedical engineering from<br />
Louisiana Tech University and his Ph.D. in bio-optics/bioengineering<br />
from Rice University. Brian has more than 15 years of biomedical<br />
research and medical device development experience. Brian’s career<br />
began at M.D. Anderson <strong>Cancer</strong> Center as Co-Director of a multi-center<br />
clinical study. He went on to work as a Senior Development Scientist<br />
for Remicalm LLC. He also previously worked as a Manager at Medical<br />
Metrics before launching Forward Science with fellow engineer Robert<br />
J. Whitman in 2012, with the goal of changing patients’ lives through<br />
innovative cancer screening technologies.<br />
CATCH BRIAN ON: DAY 2<br />
Arthur M. Lauretano MD, MS, FACS.<br />
OTOLARYNGOLOGIST HEAD AND NECK SURGEON,<br />
MEDICAL DIRECTOR OF OTOLARYNGOLOGY MULTIDISCIPLINARY CLINIC<br />
Arthur is an otolaryngologist head and neck surgeon in Lowell,<br />
Massachusetts. Board certified in Otolaryngology and in Clinical<br />
Informatics, he serves as the Medical Director for the Lowell General<br />
Hospital Multidisciplinary <strong>Head</strong> and <strong>Neck</strong> Clinic and is the former Chief<br />
Medical Officer of Circle Health at Lowell General. He also teaches at<br />
Harvard Medical School, Boston University School of Medicine, and Tufts<br />
University School of Medicine. He is dedicated to quality improvement,<br />
evidence based medicine, and the use of clinical informatics to maximize<br />
the benefits of the health care system.<br />
CATCH ARTHUR ON: DAY 2 // DAY 3<br />
Ben Sheard STAGE 4 CANCER SURVIVOR<br />
Diagnosed with Stage 4 cancer in Sep 2017, Ben was originally only<br />
given 50% chance of survival. At the start of treatment his cancer was<br />
identified in the left tonsil, throat, roof of mouth and lymph nodes. He<br />
went through the sadly all too familiar route of having a PEG fitted,<br />
operations, chemotherapy and radiotherapy and all the challenges they<br />
bring. Despite the challenges Ben’s drive, determination, and inherent<br />
desire to grab life “firmly by the balls” meant he won a new contract<br />
and returned to work in January 2018.<br />
CATCH BEN ON: DAY 2 // DAY 3<br />
23
<strong>2021</strong> SPEAKERS<br />
Derek Lewthwaite ADVOCATE FOR HEAD & NECK CANCER CARERS<br />
Derek is 66 years old and retired, having spent most of my working life<br />
in sales and marketing roles for various manufacturing and distribution<br />
companies in the UK. His wife was diagnosed with mouth cancer in<br />
October 2018 and it was at that time he became aware of The Swallows<br />
Charity as well as the start of his journey as a carer.<br />
It was a relatively short journey as his wife lost her fight against the<br />
cancer in May 2019 but it was packed with ‘highs and lows’ and ‘good<br />
and bad’ experiences of a typical head and neck cancer carer in the UK.<br />
It is from those experiences that he decided to become an advocate<br />
for carers in an effort to try to improve both communication with and<br />
acceptance of head and neck cancer carers within the treatment<br />
system.<br />
CATCH DEREK ON: DAY 2<br />
Freya Sparks BA(HONS), PGDIP, MRES, MRCSLT<br />
Freya is a Clinical Specialist Speech and Language Therapist at Barts<br />
Health, where she has led the speech therapy service for <strong>Head</strong> and <strong>Neck</strong><br />
Oncology and ENT conditions and provides advanced clinical practice.<br />
Freya was awarded an NIHR MRes studentship in 2014, and subsequently<br />
an NIHR pre-doctoral bridging award. She currently holds a Barts Charity<br />
AHP Doctoral Fellowship and is undertaking a PhD at City, University of<br />
London. Her research interests are embedded in clinical practice and<br />
focussed on the rehabilitation of communication and swallowing after<br />
head and neck cancer treatment. Freya’s doctoral study is the VITAL<br />
project, which centres on the development and feasibility testing of a<br />
novel voice therapy approach for people with total laryngectomy.<br />
CATCH FREYA ON: DAY 1<br />
Jane Thornton<br />
BSC (HONS) SPEECH PATHOLOGY AND THERAPY MANCHESTER UNIVERSITY<br />
Jane has been Clinical Lead Speech and Language Therapist for <strong>Head</strong><br />
& <strong>Neck</strong> <strong>Cancer</strong>/Clinical Voice Disorders at Sheffield Teaching Hospital<br />
NHS Foundation Trust since 1996. In that time she has been involved<br />
with developing the service to adults across the entire <strong>Head</strong> and<br />
<strong>Neck</strong> cancer patient pathway. In addition to her day job Jane is also a<br />
Honorary Lecturer at Sheffield University, National Adviser for Royal<br />
College of Speech and Language Therapist, Expert Adviser for National<br />
Institute of Clinical Excellence and has contributed to the writing of<br />
numerous national documents and guidelines including NICE - cancers<br />
of the UADT, National <strong>Cancer</strong> Action Team - rehabilitation pathways<br />
and workforce planning documents.<br />
CATCH JANE ON: DAY 1<br />
24<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
25<br />
Marianne Kooijman<br />
LICENSED LARYNGECTOMEE VOICE TRAINEE AND CANCER SURVIVOR<br />
My journey started in 1989. I had breathing problems which got worse<br />
until I had to be hospitalized. They found a T4 tumour under my right<br />
vocal cord and in November 1989 I had my laryngectomy. 6 weeks after<br />
surgery I spoke my first words and I never stopped speaking. I have<br />
served on the board of local clubs, The Dutch Association as first female<br />
President and for the International Association for Laryngectomees. I<br />
am a licensed laryngectomee trainee which means I am allowed to give<br />
voice lessons to other laryngectomees.<br />
CATCH MARIANNE ON: DAY 1<br />
Anthony Kong MBBS (LONDON) MRCP (UK) FRCR (CLINICAL ONCOLOGY) PHD<br />
Anthony read medicine at Barts and The London School of Medicine<br />
in London and undertook clinical oncology training at Barts and The<br />
Royal Marsden Hospitals after his general internal medicine training.<br />
He did his PhD research at CRUK London Research Institute Lincoln’s<br />
Inn Laboratories, and received a PhD from University College London.<br />
Following his PhD, he was awarded a clinical scientist fellowship and<br />
became a group leader at University of Oxford and an honorary NHS<br />
consultant at Oxford <strong>Cancer</strong> Centre in 2008. He took up a clinical senior<br />
lecturer position at the University of Birmingham in January 2015, and<br />
since July 2019, he has been a clinical reader at King’s College London<br />
and an honorary NHS Consultant in Clinical Oncology at Guy’s and St<br />
Thomas’ NHS Foundation Trust.<br />
CATCH ANTHONY ON: DAY 3<br />
Debbie Eason<br />
CAREGIVER CURRENTLY LIVING IN SPAIN<br />
In 2002 we relocated to Spain and have thoroughly embraced the<br />
Spanish way of life. In February <strong>2021</strong> Stuart was diagnosed with floor<br />
of mouth cancer and our lives changed dramatically. He had major<br />
surgery which was then followed up with 33 sessions of radiotherapy. A<br />
month after the treatment ended, Stu developed another cancerous<br />
tumour which then resulted in a second neck dissection and the<br />
removal of more lymph nodes. His Oncologist recommended<br />
another course of radiotherapy along with chemotherapy, but having<br />
researched the benefits and also taking into consideration the side<br />
effects of both, he decided against the treatment. He is now being<br />
monitored with regular CT scans and appointments with his Oncologist<br />
and Surgeon. Our daughter lives locally and has been amazing<br />
throughout, so strong and supportive. We don’t have any extended<br />
family here but have received support from our friends and a local<br />
<strong>Cancer</strong> Care organisation who have been amazing. It’s been a tough<br />
year, but we’re getting there and are grateful to our medical team,<br />
family and friends for all their love and support.<br />
CATCH DEBBIE ON: DAY 2<br />
25
Preventing Oral Mucositis<br />
A debilitating cancer therapy side effect<br />
Oral Mucositis is a common side effect of chemotherapy and radiotherapy<br />
for cancer. Rapidly divided epithelial cells lining the gastrointestinal tract<br />
break down, leaving the mucosal tissue open to ulceration and infection.<br />
These symptoms usually begin 1–2 weeks after starting cancer treatment.<br />
Oral mucositis is debilitating. It can lead to several problems, including pain<br />
and increased risk of infection due to open sores in the mucosa. It has a<br />
significant effect on the patient’s quality of life and can be dose-limiting<br />
(i.e., requiring a reduction in subsequent chemotherapy doses, or a delay in<br />
radiotherapy treatments).<br />
Signs and symptoms of mucositis include<br />
- Mouth sores on the gums or tongue<br />
- Soreness/pain in the mouth/throat<br />
- Red, shiny, or swollen mouth/gums<br />
- Feeling of dryness, mild burning, or pain<br />
when eating food<br />
- Blood in the mouth<br />
- Difficulty swallowing or talking<br />
- Soft, whitish patches or pus in the<br />
mouth or on the tongue<br />
- Increased mucus or thicker saliva<br />
Preventing Oral Mucositis<br />
Photobiomodulation (PBM) reduces severity and duration of oral mucositis.<br />
The effect of Photobiomodulation (PBM), previously known as Low Level<br />
Laser Therapy (LLLT), on oral mucositis (by laser or LED) has been reported<br />
in 47 randomised controlled clinical trials. These include patients undergoing<br />
chemotherapy, radiotherapy or haematopoietic stem cell transplantation<br />
(HSCT) in both paediatric and adult populations.<br />
The National Institute for Health and Care Excellence have<br />
produced an Interventional Procedure Overview of PBM for<br />
preventing or treating oral mucositis caused by radiotherapy or<br />
chemotherapy—IPG615.<br />
26<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
What is photobiomodulation?<br />
Photobiomodulation (PBM) is the application of light, in the red and near<br />
infrared range, to tissues to reduce inflammation and improve healing. PBM<br />
increases cellular energy (ATP) and reduces free radicals (oxidative stress)<br />
stimulating the body’s natural healing process. Previously, it was primarily<br />
delivered with lasers but recent developments allow for safe and effective<br />
treatments with LED lights integrated into proprietary probes designed for<br />
oral treatments.<br />
What is the treatment like?<br />
The treatment is very gentle and has even been used by St Jude Children’s<br />
Research Hospital on paediatric patients.<br />
An ice-lolly shaped treatment device (the THOR LED Lollipop) is inserted<br />
into the mouth for 1 minute—first on top of the tongue and then beneath<br />
the tongue. Next, a flat circular treatment head (the THOR LED Cluster) is<br />
placed first on each cheek and then the lips—treating each site for 1 minute,<br />
totalling 5 minutes of treatment.<br />
Contact THOR Photomedicine<br />
Call us on 01494 797 100 or email paul.burns@thorlaser.com to learn more<br />
27
Welcome to<br />
The Swallows<br />
<strong>Head</strong> and <strong>Neck</strong> <strong>Cancer</strong> Charity<br />
The Swallows Charity supports all people affected by head and neck cancers; patients, caregivers,<br />
friends or relatives. The patient is the focus for support, help and signposting. However the role of<br />
caregivers and others is vital too, with their own support needs often overlooked. It is our intention<br />
for every person affected by head and neck cancer to have access to support at the point they<br />
need it, by the method of their choice, on a 24/7 basis. This could be by telephone, email or social<br />
media. This is the key growth area for The Swallows and we have expanded our global reach to<br />
provide resources, enabling this 24/7 support to be freely available to all people affected by head<br />
and neck cancers.<br />
It is a proven fact that early diagnosis saves lives. Hence it is important to educate and inform<br />
people globally about a) how to avoid such cancers, and b) how to look for warning signs that<br />
allow for early diagnosis and treatment.<br />
Our support groups<br />
Currently we have several Support Groups in the UK and our unique virtual international monthly<br />
patient and caregiver meeting. Our aim is to increase the number of support groups over the coming<br />
years. The approach we use successfully is to provide a monthly meeting at which both patients and<br />
caregivers can attend to discuss their issues. They are given the opportunity to talk about these matters<br />
collectively or separately in a safe environment.<br />
Our experience and feedback gathered from attendees is that they value this time spent together to<br />
talk about their own specific issues in an open and honest way and to receive support. We find that<br />
separating patients from caregivers for some of this time facilitates a more open and frank exchange<br />
which results in people in similar situations being able to offer much valued support and guidance.<br />
Feedback since 2011 has shown that this approach works very well, and this is the model that we are<br />
now seeking to use with all Swallows Support Groups in the UK and overseas.<br />
Chris Curtis<br />
Chief Executive Officer,<br />
<strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong> Survivor,<br />
Honorary Senior Lecturer within the<br />
School of Health Sciences (UCLan),<br />
The Swallows H&N <strong>Cancer</strong> Support Charity<br />
chris@theswallows.org.uk<br />
www.theswallows.org.uk | info@theswallows.org.uk<br />
justgiving.com/theswallows<br />
24<br />
Patient an<br />
support li<br />
07<br />
725<br />
theswallowscancersupport<br />
@swallowsgroup<br />
28<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Our main activities:<br />
• Providing a wide range of patient & caregiver information books to patients, caregivers, relatives,<br />
GPs, professors, surgeons, clinical nurses, chemists, and dentists. We have a wide range of<br />
material covering awareness of <strong>Head</strong> and <strong>Neck</strong> cancer, early detection, signs and symptoms<br />
of what to look for, self-screening information and human papilloma virus (HPV) awareness<br />
material.<br />
• We offer a unique & dedicated 24/7 support phone line, operated by patients & caregivers for<br />
the patient & caregiver. (This is not a call centre).<br />
• Facilitating an annual <strong>Head</strong> and <strong>Neck</strong> <strong>Cancer</strong> <strong>Conference</strong> at which guest speakers and selected<br />
patients and caregivers from around the world can discuss key topics, key innovations in treatment<br />
methods, greater cooperation between health professionals and how to improve a patient’s cancer<br />
journey.<br />
• We attend overseas conferences to help us raise awareness of our activities to key potential<br />
partners in major industries.<br />
• Within the UK we are involved with health professionals at all levels to help them become more<br />
aware of the patient and caregiver journeys.<br />
• On 27th July each year we participate in World <strong>Head</strong> and <strong>Neck</strong> <strong>Cancer</strong> Day to help generate<br />
awareness to a more global audience.<br />
• We participate at Health and Well-Being events, often providing free oral health checks, in order<br />
to highlight the dangers of smoking, alcohol consumption and general lifestyles in the fight<br />
against head & neck cancer.<br />
• Our website and social media platforms help to educate patients and caregivers<br />
with current and relevant information for head and neck cancers.<br />
• The Swallows Charity shop’s primary purpose is to raise funds. This<br />
brings huge value to the local community which in turn supports local<br />
volunteers and helps boost the local high street.<br />
/7<br />
d Caregiver<br />
ne service:<br />
504<br />
059<br />
Support for all affected by<br />
<strong>Head</strong> and <strong>Neck</strong><br />
<strong>Cancer</strong><br />
29
Caregivers<br />
are important and should not be forgotten…<br />
As a charity that supports patients through their journey, we never forget our caregivers,<br />
and over the last 12 months we have worked on raising the awareness and importance of<br />
our caregivers.<br />
We are looking to launch a unique leaflet written by caregivers, for caregivers offering<br />
help, support, useful tips and sign posting for the caregiver. These will be widely available<br />
through all hospitals and at the point of patient diagnoses.<br />
Along with the new leaflet<br />
we are looking to be able<br />
to offer caregivers ‘a hug in<br />
a box’. This will consist of<br />
some nice goodies to help<br />
them on their journey.<br />
In 2022 it is our plan to<br />
continue to offer support<br />
for caregivers via our 24/7<br />
support line (not a call centre<br />
or message service). We<br />
actually take the call at any<br />
time, any day, whenever<br />
someone may need it.<br />
We will also continue our<br />
regular caregiver meetings<br />
to help them discuss their<br />
challenges, ideas, successes<br />
and so much more.<br />
A caregiver once said, “We are on the same journey<br />
but on different tracks.”<br />
We need to lessen the gap on the tracks and make the journey as one.<br />
If you are interested in getting involved in our caregiver work,<br />
please contact Sharon: sharon@theswallows.org.uk<br />
or call: 07572 493 874.<br />
Sharon Curtis<br />
Caregiver<br />
30<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
If you would like to sponsor the leaflet<br />
or goody box then please contact<br />
sharon@theswallows.org.uk<br />
or call 07572 493 874.<br />
Being a caregiver is the<br />
most satisfying, rewarding<br />
& amazing thing to do, but<br />
hardest job I ever did.<br />
The days when nobody sees the<br />
struggle are so dark and emotionally<br />
draining.<br />
I’ve found myself crying in a corridor<br />
while she slept. (But still in sight)<br />
Screaming in the car where nobody<br />
could hear me.<br />
And I wouldn’t change a day she was<br />
alive (my daughter) but I would change<br />
asking for help.<br />
I wanted to do everything<br />
myself. And I did for 7<br />
years. “<br />
Cheryl<br />
Caregiver to Emma my angel<br />
Our 24/7 Patient and Carer support line<br />
service is answered by a real person<br />
31
Claire’s<br />
Carers Story<br />
My Mum was diagnosed with tonsil cancer a<br />
year ago this month and it has been quite a roller<br />
coaster of a journey. I helped to write her story<br />
some months ago, but to write my own is so much<br />
more difficult as it triggers so many feelings inside<br />
me, which I am trying to get better at managing!<br />
I suppose the first thing I thought about when I was<br />
asked to write this story was the fact that it took<br />
a bit of persuading that I was indeed a carer! In<br />
my mind I have done what any daughter would do<br />
and I have supported my Mum through her cancer<br />
journey and will continue to do so for as long as<br />
she needs me and however much she needs me! I<br />
never saw it as being a carer, I just saw it as being<br />
there for my Mum!<br />
My Mum has been a very lucky lady - she was<br />
diagnosed at an early stage thanks to our eagle eyed<br />
hygienist and fantastic dentist and was lucky enough<br />
to be offered robotic surgery. The outcome has been<br />
amazing to say the least and for a 78 year old woman her<br />
recovery to date has been phenomenal.<br />
Mum had no symptoms so for us to be told she had<br />
cancer was a huge shock. She had smoked for 55 years<br />
and I knew that she wouldn’t get away with it but we<br />
didn’t see this one coming. Her diagnosis completely<br />
floored me and what made it worse was the fact that she<br />
is the person I talk to about worries in life and I couldn’t<br />
tell her about these worries as she had enough of her<br />
own to cope with. I had no outlet and I struggled terribly. I<br />
couldn’t eat and couldn’t think straight. I cried most days<br />
and some days I sobbed rather than cried and I felt like I<br />
wasn’t coping at all. The way I felt scared me.<br />
Mum’s initial proposed treatment was radiotherapy and<br />
when I Googled the side effects it was then that I went<br />
into meltdown...as far as I was concerned my healthy<br />
Mum would undergo gruelling treatment which would<br />
severely affect her quality of life and leave her with life<br />
long side effects. She had no concept of the difficulties<br />
she was facing and so I kept it away from her - she had<br />
enough to worry about. I spent hours and hours every<br />
day and every night scouring the internet for answers and<br />
positive stories and I drove myself daft with it all.<br />
“I kept all of this from Mum and it was<br />
difficult to even look at her at times. I<br />
reached out to various cancer support<br />
charities for information but was left<br />
feeling like there was a lack of honesty;<br />
that they were minimising the situation<br />
and I really believed I couldn’t trust them.”<br />
Then I found the Swallows! My first telephone<br />
conversation with Chris Curtis was the first honest and<br />
frank discussion I had been afforded by anyone. He told<br />
me exactly how tough Mum’s journey could potentially<br />
be but he gave me positivity and lots of ideas. He<br />
also told me about his own story and it gave me hope<br />
for the first time since Mum’s journey began.<br />
He managed to help me to have a night of respite from<br />
the fear, anxiety and worry that had engulfed me since<br />
radiotherapy was discussed as mums treatment option.<br />
At the early diagnosis appointments I felt rushed and<br />
as if nobody afforded us time to talk through options,<br />
prognosis and side effects. Mum was shipped in and out<br />
To read more patient a<br />
32<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
of rooms with little explanation and not much empathy<br />
and I felt like I was in the way and not particularly<br />
welcome. I hated it and I felt like I was an inconvenience<br />
asking questions but this was my Mum’s life and I<br />
was going to fight for it. Mum sat there in a daze at her<br />
appointments and was practically mute which was very<br />
unusual and also so sad to see. Not only that I could<br />
not believe that there were no alternatives. I remember<br />
at an oncology appointment having a support leaflet<br />
thrust into my hand and being told I needed help as<br />
my reaction was “extreme”!! Extreme? This was my<br />
Mum! They hadn’t seen the half of it yet! I cried at that<br />
appointment, rudely referred to radiotherapy as “being<br />
zapped half to death” and begged for an alternative.<br />
That was the first time we heard the words “robotic<br />
surgery”. To this day I don’t think that Mum would have<br />
been offered this fantastic treatment had it not been for<br />
my “extreme” reaction so I don’t regret it one bit!<br />
Mum waited only 3 weeks from her first meeting with<br />
her surgeon until she had her operation. It was over<br />
the Christmas period and it was a difficult time for us all<br />
and I spent New Year’s Eve at home with my husband<br />
in floods of tears. He was disappointed in me and<br />
my demeanour but there was simply nothing I could<br />
do. Mum spent new year with others in our family and<br />
she was certainly not herself either. I spent my time<br />
researching the surgery, it’s success rate, the side<br />
effects and the benefits - my friends have often joked<br />
that I could probably have a good go at doing it myself<br />
but I felt that I needed to be prepared!<br />
Mums recovery from surgery was fast and pretty<br />
impressive! The first few weeks were not so easy. On<br />
the day of her surgery I waited all day for the call to say<br />
she was out of theatre and spent most of it crying!! I<br />
was pathetic to say the least! The staff at the hospital<br />
were amazing and continue to be amazing today - we<br />
have been so lucky to have been referred to them. I<br />
was juggling work and caring for mum and she had<br />
moved into our house to recuperate. She cried with<br />
pain on several mornings (she wasn’t prepared for the<br />
pain of tonsil removal as an adult) and her eating took a<br />
little while to get back to normal. I was quietly confident<br />
but so afraid. It was like having a new baby - every<br />
sound in the night I was up and checking on her. I was<br />
assisting with pain relief in the night and during the day<br />
and just kept praying that she would recover fully.<br />
Fast forward to almost 11 months later and here we<br />
are. Mum is currently free of disease and attending<br />
clinic every 6 weeks. Do I class myself as a carer<br />
now? I do and I am getting used to the concept of it!<br />
I am proud of Mum and her<br />
amazing recovery and I am<br />
proud of having the strength<br />
to speak up for her during that<br />
early appointment (despite how<br />
unpopular I felt when I did it!). We<br />
often talk about how different life would<br />
have been if we hadn’t have met Miss Ghazali and the<br />
wonderful team at Royal Blackburn Hospital and if Mum<br />
hadn’t have been eligible for the surgery. Somebody<br />
finally listened to what we had to say and understood<br />
my view point.<br />
Claire’s Mum, Audrey, has written her own story.<br />
Find it online on The Swallows website.<br />
I could write and talk for hours about this subject but I<br />
really hope that going forward carers are recognised<br />
as cancer sufferers but in a different way. I truly believe<br />
that Mum coped with her illness way better than I did<br />
and think she continues to do so. Watching her go<br />
through the process she been through has been the<br />
most difficult thing I have encountered in my life so far.<br />
Sadly I don’t think that the fear of it returning will ever<br />
go away but her surgeon said something which really<br />
helped us both. “You are now back to being the same<br />
as everyone else, wondering and hoping that you do<br />
not get cancer.” However you are lucky enough to see<br />
a specialist on a regular basis to be checked out and<br />
not everyone gets that!<br />
That way of looking at it has stuck with us both and<br />
along with my family we help Mum to enjoy every<br />
minute of life that the robot gave to her. We make sure<br />
she makes the most of the quality of life that she has<br />
been lucky enough to retain.<br />
Caring for her has been tough but it’s worth it!<br />
nd carer stories or find out more about <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong> support visit: www.theswallows.org.uk<br />
33
Share your<br />
cancer story<br />
We’re looking for patient and carers from<br />
around the world to feature in our next<br />
patient book and on our website.<br />
Please send approximately 500 words and supporting images to:<br />
info@theswallows.org.uk<br />
24/7 34Patient and Carer support line VIRTUAL service: HEAD 07504 & NECK 725 059 CANCER www.theswallows.org.uk<br />
CONFERENCE <strong>2021</strong>
We are pleased to meet you at the<br />
<strong>2021</strong> Virtual<br />
<strong>Head</strong> & <strong>Neck</strong><br />
<strong>Cancer</strong> <strong>Conference</strong><br />
Seminar<br />
New Medicine & Techniques<br />
for <strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong><br />
Sponsored by Sensius<br />
35
Radiotherapy treatment:<br />
When patients undergo radiotherapy<br />
treatment, they often experience a range<br />
of side effects including (but not limited to);<br />
xerostomia (dry mouth), mucositis (mouth<br />
ulcers), taste changes and changes to<br />
secretions (producing thick saliva). These<br />
side effects can impact eating and drinking,<br />
a person’s appetite and interest in food.<br />
Throughout radiotherapy treatment the<br />
side effects that a patient experiences can<br />
change and so the diet can be adapted as<br />
treatment progresses.<br />
Pain<br />
Including a variety of foods in the diet is<br />
important to provide nutrition. Patients<br />
are advised to focus on their calorie and<br />
protein intake to help maintain their weight<br />
and muscle mass. If the radiotherapy is<br />
causing pain in the mouth and throat, then<br />
eating can become more challenging. We<br />
recommend that our patients continue a<br />
textured diet for as long as they are able,<br />
but if eating is becoming unmanageable<br />
then soft foods are encouraged. Often<br />
people start to avoid spicy and acidic foods<br />
as these can cause a burning/ stinging<br />
sensation. The tolerance to these foods<br />
varies from person to person.<br />
Tips to help with pain:<br />
• Choose softer textures (avoiding foods<br />
which have a rough edge)<br />
• Try different temperatures and check<br />
which suits you<br />
• Avoid acidic or spicy foods<br />
• Take pain relief prior to eating (as guided by<br />
your medical team or clinical nurse specialist)<br />
Xerostomia (Dry mouth)<br />
When patients experience xerostomia<br />
dry foods can be more challenging, often<br />
patients find it more manageable to have<br />
additional sauces with foods. Also sipping<br />
on fluids while eating can help patients get<br />
foods down. Often steaming is advised prior<br />
to meals so that patients can clear any thick<br />
secretions and add moisture<br />
Written by Alysia Burrows,<br />
Dietitian at the Royal Marsden Hospital<br />
to their mouth prior to eating.<br />
Tips to help with xerostomia:<br />
• Steam regularly throughout the day<br />
• Sip on fluids when eating<br />
• Add sauces, gravies, and dressings to<br />
foods to add moisture<br />
• Choose soft/ moist foods/avoid dry options<br />
• Use sprays of water and olive oil to add<br />
moisture to the mouth<br />
• Try artificial saliva’s<br />
Increased secretions<br />
Some people will experience an increase<br />
in thick, sticky secretions while having<br />
radiotherapy. A build-up of these thick<br />
secretions can sometimes cause nausea<br />
which can impact eating. It is beneficial<br />
to steam regularly. The medical team<br />
and clinical nurse specialist may also<br />
recommend mouthwashes to help you<br />
clear the secretions and anti-sickness<br />
medications to reduce the nausea.<br />
Taste changes<br />
Experiencing taste changes while having<br />
radiotherapy treatment is common but<br />
how the taste is altered can vary from<br />
person to person. To increase the flavours<br />
in foods, techniques such as adding herbs<br />
and garlic to foods can make foods more<br />
palatable. Some people can taste strong<br />
flavours or will notice they have more<br />
affinity to taste savoury rather than sweet<br />
flavours or vice versa.<br />
Tips to help with taste changes*:<br />
• Choose foods with a stronger flavour<br />
• Add pickles or chutneys (if tolerated)<br />
• Trial sweet foods and savoury foods<br />
and check if one is easier to taste<br />
• Trial foods at differing temperatures<br />
• Add sauces to foods<br />
• Marinade foods to increase flavour<br />
• Add herbs and seasonings<br />
• Focus on foods which are palatable<br />
for you<br />
• If you cannot taste any flavours focus<br />
on setting a routine to prompt eating<br />
36<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
37<br />
DIET SOLUTIONS<br />
Protein Sources:<br />
When eating think about whether you could<br />
add additional foods to increase the protein<br />
and calorie content. For example, adding<br />
cheese to mash potato, lentils to a sauce, nut<br />
butters to a smoothie or on a snack.<br />
Maintaining weight and muscle mass<br />
during treatment may be difficult however<br />
is an important part of recovery. Focus<br />
on incorporating protein and calorie rich<br />
foods into your diet.<br />
Examples of protein rich foods:<br />
Meats, Fish, Beans and pulses, Eggs, Dairy<br />
products, Quorn, soy products, Nuts.<br />
Nourishing drinks:<br />
If eating is becoming more difficult then<br />
nourishing drinks are beneficial. Milk<br />
based drinks such as hot chocolate, malt<br />
drinks, homemade milkshakes or a glass<br />
of full fat milk will increase the daily intake<br />
of calories and protein which in turn can<br />
help to prevent or reduce weight loss and<br />
muscle loss.<br />
Soft foods include:<br />
Texture modification is often necessary<br />
during radiotherapy treatment and<br />
people tend to have softer foods as the<br />
weeks pass. This can make eating more<br />
comfortable, which in turn encourages<br />
a larger intake. This is paramount in<br />
maintaining nutritional status.<br />
An example of soft meal options:<br />
Breakfast: Porridge, scrambled egg,<br />
yoghurts, pancakes etc.<br />
Main meals: shepherd’s pie, fish pie,<br />
casseroles, carbonara, spaghetti dish,<br />
risotto, soft noodles with a tender meat etc.<br />
Desserts: sponge puddings, rice pudding,<br />
custard, trifle, ice cream, crème caramel,<br />
mousse etc.<br />
Nutritional supplements:<br />
To increase a person’s calorie and protein<br />
intake often nutritional supplements are<br />
prescribed. The nutritional supplements<br />
are nutrient dense. They are available in<br />
different varieties so that a supplement<br />
which is suitable can be found for each<br />
person. Some of the supplements are milk<br />
based and others are juice based. Often<br />
the low volume, high protein supplements<br />
are used as a first line as people tend to<br />
manage smaller volumes with more ease.<br />
The nutritional supplements are very<br />
important when oral intake is reduced,<br />
and they may be prescribed multiple<br />
times a day.<br />
Artificial feeding:<br />
Some patients will require a feeding tube<br />
to support their nutrition throughout<br />
treatment. A nasogastric tube or<br />
gastrostomy tube may be inserted. This<br />
decision would be made with the patient<br />
if required.<br />
After Radiotherapy:<br />
It often takes a few weeks post<br />
radiotherapy before the side effects start<br />
to improve and this is a gradual process.<br />
As the pain improves the variety of foods<br />
which people can eat often increases and<br />
this in turn improves their calorie and<br />
protein intake. For those on nutritional<br />
supplements these can then be weaned<br />
down, with the aim of stopping them.<br />
*For more information regarding taste changes see www.lifekitchen.co.uk
Try for<br />
yourself -<br />
Book a<br />
FREE<br />
TASTING<br />
SESSION<br />
SAVOUR THE FLAVOURS<br />
OF CHRISTMAS<br />
Wiltshire Farm Foods is part<br />
of the apetito family, providers<br />
of award winning meals to<br />
hospitals. apetito.co.uk<br />
We take huge care<br />
over every dish, so<br />
you can be confident<br />
your patients can<br />
enjoy great food.<br />
<strong>Head</strong> Chef<br />
We want everyone to be able to enjoy a festive dinner<br />
with their families this Christmas. That’s why we’ve<br />
added to our award winning Softer Foods range with<br />
our Christmas menu!<br />
There’s no contract, so your patients can simply order<br />
as much or as little as they like - we can even put their<br />
dishes away into their freezer for them on delivery.<br />
Pop straight into the microwave or oven from frozen<br />
and voilà - a nutritious meal that’s delicious to eat and<br />
safe to swallow.<br />
Over 80 dishes made in line with IDDSI standards,<br />
including breakfast, snacks and deserts.<br />
A dedicated range for those<br />
with swallowing difficulties.<br />
Smaller portioned,<br />
calorie dense options.<br />
Friendly local drivers<br />
they’ll get to know.<br />
No contract or commitment.<br />
Reassurance that your patients<br />
are eating well at home.<br />
Level 4 - Purée Meals<br />
Level 5 - Minced Meals<br />
Level 6 - Soft &<br />
Bite-Sized Meals<br />
38<br />
To order brochures for your patients or request a free tasting session<br />
visit: wff.link/HCPrequest or call 0800 066 3702<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Suffering with Dry Mouth?<br />
Get some soothing relief!<br />
Due to the impact on a person’s quality of life,<br />
clinicians often prescribe a Dry Mouth Spray like<br />
Saliveze, to help relieve symptoms.<br />
Benefits of Saliveze include:<br />
• pH neutral<br />
• Vegan friendly<br />
• Soothing relief<br />
• Mild minty taste<br />
• Sugar-free<br />
• On prescription<br />
©2020 Wyvern Medical Ltd. Image of mouth is for illustration purposes<br />
For more information or<br />
request a sample call us on<br />
01531 631105 or visit<br />
www.wyvernmedical.co.uk<br />
Soothing Dry Mouth Spray<br />
39
Tips for swallowing during<br />
radiotherapy<br />
Patients experience a wide range of symptoms during radiotherapy (RT) treatment.<br />
As the symptoms can vary day on day and week on week, it is important that you<br />
have regular reviews with your multi-disciplinary team to manage symptoms as they<br />
arise. Your team may include your Oncologist, Clinical Nurse Specialist, Dietitian and<br />
Speech and Language Therapist (SLT). We encourage patients to flag their concerns or<br />
changes in symptoms early to enable us to best support you through your treatment.<br />
Swallow management<br />
Your swallow function can be affected by the cancer<br />
itself, the symptom burden of the cancer such as pain or<br />
due to RT side effects. SLTs assess your swallow prior to RT<br />
commencing and will continue to monitor your swallow during and after RT. SLTs offer guidance on how<br />
to manage potential swallowing difficulties, which we refer to as dysphagia. Some patients have difficulty<br />
swallowing their saliva, liquids and food during and after RT. If we are concerned about your swallow, we<br />
may advice you to have a videofluroscopy or Fibreoptic Endoscopic Evaluation of Swallowing (FEES) which<br />
can assess the safety and efficiency of your swallow. Once your swallow has been assessed we can provide<br />
you with a tailored rehabilitation plan. Some patients have difficulty swallowing safely which can result<br />
in a chest infection, other patients can develop swallowing difficulties long after RT has finished, we call<br />
this late effects. At 6 years following RT, Paterson et al. (2018) reported half of patients enjoyed a normal<br />
diet and one fifth of patients had aspiration, which increased their risk of chest infections. Long-term<br />
dysphagia was reported as a serious concern following RT in this study.<br />
Ways to manage your dysphagia may include; engaging in regular swallow exercises, compensatory<br />
strategies or having a modified diet such as a soft diet. Patients may be advised to have a feeding tube to<br />
supplement their oral intake during RT, these patients will still be encouraged to swallow regularly, it may<br />
be just small amounts of water or their saliva. To prevent muscle loss and scaring which can result in long<br />
term dysphagia it is essential to continue swallowing throughout RT.<br />
Exercise<br />
Swallowing exercises are recommended as part of your treatment. We recommend you start the exercises<br />
the day you meet with your SLT. Your SLT will explain how to do the exercises and why it is important to<br />
them. The evidence for the exercises is not robust but from our clinical experience we feel they are an<br />
important part of keeping the swallowing musculature flexible and strong during RT to enable you to<br />
enjoy eating again after RT and reduce the risk of long-term swallowing difficulty. The recommendation<br />
40<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
is to complete the exercises 3 to 5 times a day, each exercise is repeated 5 times. We are aware that all the<br />
recommendations can seem burdensome and time consuming, patients often report the importance of<br />
setting up a routine early to promote self-care.<br />
We encourage all patients to maintain general physical exercise during RT. Studies from prostate cancer<br />
and breast cancer show that patients who exercise for 50 minutes three times a week for 5 to 8 weeks<br />
depending on the study report better quality of life and less fatigue than the group who did not exercise<br />
(Hojan et al, 2017., Monga et al 2007., Hwang et al, 2008).<br />
Pain<br />
As pain is often reported as the number one symptom affecting a patient’s ability to continue with oral<br />
intake, it is of upmost importance that your pain is well controlled. Proactive management of pain relief<br />
is needed. We promote regular,<br />
consistent use of analgesia<br />
from the onset of discomfort on<br />
swallowing. Taking pain relief<br />
20-30 minutes before your meal<br />
may enable you to continue a<br />
solid diet for longer. We are always<br />
pleased to hear that a patient<br />
increased their pain relief in order<br />
to eat rather than decreased their<br />
texture due to poorly controlled<br />
pain, working with your Clinical<br />
Nurse Specialist and Oncologists is<br />
essential for this.<br />
Mouth care<br />
An excellent resource for mouth<br />
care advice is UK_OM_Guidelines.<br />
pdf (ukomic.co.uk).<br />
RT can directly affect the oral cavity resulting in acute changes such as ulceration and swelling<br />
and long term changes such as dryness. These side effects often impact a patients ability to eat<br />
and drink. This can also impact patient well-being. With as many as 97% of all patients receiving<br />
radiotherapy (with or without chemotherapy) for head and neck cancers suffering some degree of<br />
oral mucusoitis (Kostler et al., 2001) weekly assessment by trained professionals is needed. When<br />
patients have their mucusoitis managed correctly they can continue to enjoy an oral diet.<br />
General advice during RT is; brush teeth twice daily with high fluoride toothpaste, salt water rinses, sip<br />
water throughout the day and minimise foods that can irritate your mouth such as spicy foods or acidic<br />
foods.<br />
Secretion management<br />
Dry Mouth due to RT can affect a patients ability to eat, appetite and taste. We recommend sipping water,<br />
rigorous mouth care, steaming and/ or nebulisers, saline mouth rinses and salivary products such as<br />
artificial saliva spray may be indicated. Managing your dry mouth, which we refer to as xerostomia, before<br />
oral intake with sips of water and steam inhalation may increase your comfort at meal times.<br />
During RT and in the weeks following RT you may experience thick saliva which can negatively affect your<br />
swallowing. Patients report feeling nauseous as a result of their thick secretions. As it is more difficult to<br />
swallow when secretions are thick, you have a reduced appetite and altered taste, it is important to clear<br />
your secretions with steam inhalation before a meal. Sipping water during the day and remaining active<br />
also helps with this.<br />
References available<br />
on request.<br />
Written by Lauren Leigh-Doyle<br />
Highly Specialist Speech and Language Therapist at<br />
the Royal Marsden NHS Foundation Trust.<br />
41
Welcome to Atos Care<br />
The only integrated care and distribution service for people with a<br />
laryngectomy and tracheostomy in the UK.<br />
Atos Care is a comprehensive support service, dedicated to<br />
making life easier for people living with a neck stoma.<br />
The Atos Circle of Care<br />
Best Start: Get off to the best start in life after a<br />
laryngectomy or tracheostomy.<br />
• Enhanced support for your first six months from<br />
our Welcome Team of CQC Registered Nurses<br />
• A welcome pack and a welcome call<br />
• Practical tools and equipment to make life easier,<br />
including a complimentary care bag containing a<br />
range of helpful items<br />
• Regular liaison with clinicians for joined up care<br />
Connection hub: Stay connected to those who<br />
know and understand.<br />
• A dedicated Customer Care Representative<br />
• Personalised service - you choose how and when<br />
you hear from us<br />
• CQC Registered Nurses to support you in<br />
your daily routines, in close partnership and<br />
communication with clinicians<br />
• Educational events in the community for people<br />
with similar experiences<br />
Care delivered: Bringing the right products and<br />
care your way.<br />
• Easy and convenient ordering<br />
• Optional convenient monthly reminders<br />
• Electronic Prescription Service<br />
• Rapid, reliable delivery<br />
• Discreet packaging<br />
• Convenience orders by subscription<br />
Call us:<br />
0800 783 1659<br />
Email us:<br />
info@atos-care.co.uk<br />
Visit our website:<br />
www.atos-care.co.uk<br />
42<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
We’re here - right where<br />
you need us!<br />
Supporting patients on their<br />
cancer journey, from diagnosis<br />
through to treatment and<br />
recovery, we provide access to<br />
the latest treatments, including<br />
proton beam therapy.<br />
Across our UK network of centres,<br />
our consultants, specialists and staff<br />
provide an all-encompassing cancer<br />
care service. Treatments and services<br />
include imaging, chemotherapy,<br />
immunotherapy, radiotherapy,<br />
proton beam therapy and ongoing<br />
supportive care.<br />
0800 210 0402<br />
therutherford.com<br />
All our registered centres undergo a registration inspection by the independent healthcare regulators of each country (Healthcare Inspectorate<br />
Wales, Care Quality Commission) to ensure that the quality and safety of services meet the required standards of care. In addition, ongoing 43<br />
inspections are undertaken, and where these have taken place, full reports are made available on our website.
the role of the<br />
Physiotherapist<br />
For 34 years, it has been my privilege and joy<br />
to be a physiotherapist – learning every day<br />
from people who trust me with their body<br />
and experience. People who have had lifechanging<br />
surgery, radiotherapy, chemo and<br />
reconstructive work.<br />
For clarity, I use the words “people/person/<br />
someone” to refer to the person undergoing<br />
treatment and care.<br />
Ideally, you meet someone before their<br />
initial medical treatment, both to explain the<br />
role of a physio and explore what the person<br />
may want and need. Describe what the<br />
person might expect in the way of sensation<br />
and function, suggest helpful positionings,<br />
exercises, breathing, swallowing, chewing<br />
and communicating techniques. Hopefully,<br />
this is done in collaboration with a speech<br />
and language therapist (SALT). Explanation<br />
around the anatomy involved can be very<br />
helpful for some people. And also, and this is<br />
important, find out who the person is, what<br />
their hopes and needs are and see how they<br />
move before treatment has begun.<br />
After surgery, there is much we can offer as<br />
physios, but I understand from the people<br />
I work with that they rarely see a physio<br />
in hospital, although often have exercises<br />
from the SALT. Even simple things like how<br />
to move in and out of bed or negotiate<br />
the toilet or staircase with drains, can<br />
make a difference in those first days. SALT<br />
exercises and their useful advice and follow<br />
up is usually described positively and may<br />
be continuing after acute intervention<br />
(support) has lessened. This can be a great<br />
psychological encouragement as well as of<br />
practical benefit. Sometimes, people just<br />
want to know what’s “normal,” after their<br />
familiar body, the place where they live has<br />
become an unpredictable stranger.<br />
If your recovery starts on ITU, you are likely<br />
to see physios. They may be maintaining<br />
airways, optimising respiratory function<br />
and moving people’s limbs if they are<br />
unconscious or unable to move freely.<br />
In the early post surgery/radiotherapy days,<br />
the correct movements and exercises are<br />
important. As are relaxation, nourishing and<br />
sustaining breathing and posture (how we<br />
rest and function in comfort) Suggestions<br />
around pacing, placement of pillows,<br />
visualisation and revisiting anatomy can<br />
be helpful. (shock and trauma may mean<br />
people may need to have information<br />
several times).<br />
44<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Some people who have been treated without surgery, or with robotic surgery may still need physio even<br />
though their scarring and tightness may be unseen.<br />
Significant lymphoedema (swelling caused by the congestion of lymphatic fluid, the flow of which<br />
having been disrupted by surgery and/or radiotherapy) may indicate referral to a specialist lymphoedema<br />
therapist or nurse. Treatment options may include manual therapy, use specialist equipment, compression<br />
garments and advice for skincare and selfcare.<br />
Some people may find it increasingly difficult to open their mouth, have stiffness, weakness or altered<br />
sensation. As time passes, tightness in scarring may affect facial appearance and function.<br />
The fascia, the connective tissue under the skin, embracing almost everything and enabling smooth<br />
gliding of one structure over another can become scarred and stuck after surgery and/or radiotherapy. The<br />
light touch techniques we (and other suitably-trained bodyworkers) can use both externally and intraorally<br />
can have an enormous impact on function, movement, comfort and appearance.<br />
We are integrated beings. Tethering and restriction of one place affects other parts of the body. This maybe<br />
what brings the person to physio. Soreness in the spine or arms due to altered movement or suboptimal<br />
mechanics. Or changes in arm movements affecting walking patterns.<br />
The specialist light touch, sheer and vibrational techniques are not a miracle, but the people I work with<br />
sometimes describe them as such. Being able to swallow more easily, turn the head without an eye being<br />
pulled closed or regaining more subtlety of facial expression can be life changing. During treatment,<br />
people may experience “scratchiness” “pinching” or sharp sensations, but it doesn’t need to hurt to be<br />
effective. Others may say, “this is bliss.” Afterwards, people often describe feeling “lighter” or “freer” and<br />
there may be more sparkle in their eyes. Over a course of treatment, people may have less pain, improved<br />
flexibility and increased confidence in their body.<br />
Exercises are important, but they need to be the correct ones for that individual at the right time.<br />
1-3 exercises done well and attentively may be enough. It is my job to suggest and demonstrate well<br />
something that feels enhancing for the person. I need to explain why it matters that they do it. Often it is<br />
more about movement than exercise. This is not just semantics. Language and intent matter.<br />
What we say, how we say it and why we say it all matter. A person whose life has been in significant peril<br />
will be paying great attention. As professionals, we need to be both confident and cautious, checking what<br />
is and is not alright for this person trusting us with their precious body. Unless we ask, we have no idea of<br />
their previous history – and even if we ask, they may never feel at liberty to say. And they may no longer<br />
have a fluent voice!<br />
During an initial assessment, when I ask what someone loves doing, I am often reminded of the person<br />
who said, “sex, eating and swimming. And I can’t do any of those, now.” As part of a team, it is a physio’s role,<br />
to try to facilitate the person’s way forward to a fulfilling life, so that the person has not endured significant<br />
challenging and life-changing treatment to simply survive.<br />
Changes in sensation, energy, appearance, saliva, speech and movement may mean that intimacy and sex<br />
are changed.<br />
Communication is essential, but not always easy.<br />
The physio’s role is seen as primarily physical therapy, and three of our four core elements respiratory,<br />
exercise and massage, can all make a significant difference<br />
to someone who has undergone treatment for head or<br />
neck cancer. However, it is essential to truly engage with the<br />
person as well as their physical body if we are to be of help.<br />
Please feel free to contact me at<br />
www.leahthephysio.co.uk if you have any questions or<br />
know you can help me deepen my understanding.<br />
Written by<br />
Leah Dalby<br />
MCSP<br />
Physiotherapist<br />
45
The power of protons<br />
It was only a few years ago that<br />
we celebrated the arrival of proton<br />
beam therapy in the UK. Previously<br />
a treatment that cancer patients had<br />
to travel abroad for, today the power<br />
of protons can be accessed through<br />
a complementary mix of private and<br />
public facilities across the country.<br />
This transformation has been led by Rutherford<br />
Health, who first treated a patient with high energy<br />
proton beam therapy in April 2018. That milestone<br />
ushered in an era of progress that has helped<br />
establish the UK as a world leader in precision<br />
medicine. Whilst it is not suitable for all patients or<br />
all cancers, proton beam therapy can be a highly<br />
effective treatment for a range of head and neck<br />
cancers.<br />
<strong>Head</strong> and neck cancer – a term used to describe<br />
any tumour that affects the areas including<br />
forehead, eyes, nose, mouth, sinuses and any<br />
glands or lymph nodes – is the eighth most<br />
common cancer in the UK. There are about 12,000<br />
new cases of head and neck cancer each year.<br />
There is also a gender difference here in the UK –<br />
in men, it is the fourth most common cancer, while<br />
in women it is the thirteenth.<br />
The head and neck region contains many important<br />
organs which are located closely to each other. When<br />
considering treatment options, it is therefore essential<br />
to factor in the impact on neighbouring organs.<br />
Damage to healthy tissue in the mouth and throat<br />
can have long-term impacts, from chewing problems,<br />
dryness, loss of hearing, and more.<br />
Proton beam therapy is a type of radiotherapy that<br />
delivers heavily charged protons in a more targeted<br />
manner to reduce damage to peripheral tissue and<br />
organs.<br />
The precision of proton beam therapy allows for the<br />
effective treatment of many complicated head and<br />
neck tumors, while minimising the radiation dose to<br />
vital structures such as the eyes, mouth and brain. As<br />
an extremely targeted treatment, it has the ability<br />
to stop radiating beyond a tumour site, making it<br />
possible to treat the cancerous area whilst reducing<br />
the radiation dose delivered to the normal healthy<br />
tissue surrounding it.<br />
This means, in principal, proton beam therapy can<br />
reduce the risk of severe side effects when compared<br />
to conventional radiotherapy, delivering an enhanced<br />
quality of life for patients.<br />
46<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
More information on the Rutherford <strong>Cancer</strong> Centres can be found on our website: www.therutherford.com<br />
These are the main benefits of treating head and<br />
neck cancer with proton beam therapy:<br />
• Associated side effects are reduced, allowing<br />
for quicker recovery<br />
• Possible reduction of the experience of longterm<br />
dry mouth and swallowing dysfunction<br />
• Targeting the treatment area and avoiding<br />
vital organs and sensitive areas in the head and<br />
neck area that don’t need radiation - such as<br />
the eyes, brain etc<br />
• It is highly accurate in targeting a treatment<br />
area. It can be used to treat hard-to-reach<br />
tumours, while lowering radiation exposure to<br />
surrounding healthy tissue and vital organs.<br />
The role of Rutherford Health’s network of advanced<br />
proton beam therapy facilities – located in Newport,<br />
Reading, Liverpool and Northumberland – has been<br />
central to the UK closing the gap when it comes to<br />
proton therapy provision. Our network represents<br />
the lion’s share of proton therapy capacity in the<br />
UK and our highly successful oncologist training<br />
programme has led to the UK benefiting from<br />
an ‘innovation dividend’ through the creation of<br />
a better skilled healthcare workforce which also<br />
includes therapy radiographers and physicists.<br />
The Rutherford <strong>Cancer</strong> Centres are at the forefront<br />
of particle therapy and precision radiotherapy<br />
research, working with some of the world’s top<br />
academic institutions and advanced medical<br />
technology providers. Thanks to these efforts<br />
the UK is now a key contributor to thought<br />
leadership on proton beam therapy globally. In<br />
addition to proton beam therapy, each Rutherford<br />
<strong>Cancer</strong> Centre provides CT, MRI, Radiotherapy,<br />
Chemotherapy, Infusion Therapy, and<br />
Immunotherapy, as well as a suite of diagnostic,<br />
planning and support services for all patients.<br />
Rutherford Health is a network of cancer centres across<br />
the UK offering the most advanced cancer treatments and<br />
diagnostic services. It has four centres in Wales, Reading,<br />
Northumberland and Liverpool and offers chemotherapy,<br />
immunotherapy, radiotherapy and high energy proton<br />
beam therapy. The centre in Wales was the first to introduce<br />
high energy proton beam therapy to the UK in 2018.<br />
47
Hidden Figures: The role of a Pathologist<br />
in a head and neck cancer patient journey<br />
By Dr Ali Khurram- Consultant Pathologist<br />
& Senior Lecturer, University of Sheffield<br />
What is pathology?<br />
Pathology is a branch of medical science that involves study of<br />
diseases. There are numerous branches of the specialty involving<br />
examination of micro-organisms and viruses, autopsy and bodily<br />
fluids. Histopathology is the branch of pathology which deals with<br />
examination of biopsy/tissue specimens under a microscope and<br />
these are the people involved in your diagnosis and treatment.<br />
You may not be aware of the fact that that Pathologists not only<br />
play a play role in improving understanding of diseases and<br />
research but are also at the forefront of developing and using<br />
cutting edge technologies to identify patterns in the tissue to aid<br />
patient treatment.<br />
What role does a Pathologist play in<br />
a patient’s journey?<br />
The role of a pathologist in a patient’s journey is<br />
multifold with involvement every step of the way.<br />
a. Prior to treatment<br />
When you are sent to a hospital to have an initial<br />
biopsy, that is the first stage when a pathologist<br />
gets involved. The piece of tissue that is removed,<br />
undergoes a series of steps to preserve it in a<br />
life-like state and thin slices are cut and coloured<br />
followed by placement on a glass slide which<br />
can then be viewed under the microscope by a<br />
pathologist.<br />
The light shining under the slide on the<br />
microscope allows the pathologist (with the help<br />
of magnifying lenses) to meticulously analyse<br />
features within the tissue including presence of<br />
abnormal, pre-cancerous or cancerous cells.<br />
These microscopic findings are then shared<br />
with the surgeons and oncologists and form the<br />
foundation of your future treatment.<br />
Figure 1 - Left image showing stained/coloured tissue on a glass slide. Right image<br />
shows the slide placed on a microscope with a light shining through.<br />
Figure 2 - A stained image as it appears under<br />
the microscope showing presence of oral/mouth<br />
cancer cells.<br />
48<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
. During treatment<br />
A pathologist’s role during your treatment is<br />
absolutely critical. If the surgeons decide to<br />
remove the cancer, the tissue is sent to the<br />
lab where it is appropriately sampled by a<br />
pathologist. In some instances, lymph nodes<br />
of the neck may also be removed along with<br />
the cancer which are also all analysed by<br />
the pathologist along with the cancer. A wide<br />
range of features are assessed to determine<br />
the aggressiveness of the cancer and whether<br />
the surgical margins are clear. This information<br />
is then presented to all the patient care team<br />
to decide the need for further surgery or<br />
adjuvant radio- or chemotherapy.<br />
Figure 3 - An oral/mouth cancer resection specimen and how<br />
information may be shared by a pathologist.<br />
c. After treatment<br />
Even after your treatment, if there are any suspicious<br />
areas or the surgeons/oncologists want to determine<br />
the response to treatment, repeat biopsies may be<br />
performed which are assessed by the pathologist and<br />
compared with the features seen previously. This may<br />
necessitate further surgical or oncological treatment.<br />
Identification of pre-cancer (dysplasia)<br />
In addition to diagnosing head neck cancer,<br />
pathologists also play a key role in identification<br />
of the presence of pre-cancer (or dysplasia). This<br />
is crucial as early detection of such lesions can<br />
prevent development into cancer reducing the need<br />
for extensive surgery and improving the quality of<br />
life and prognosis for patients. For this purpose, a<br />
pathologist examines the tissue for the presence<br />
of a number of features including the shape, size<br />
and colour of the cells as well as the shape of the<br />
mouth or throat lining to establish the grade/risk of a<br />
pre-cancer.<br />
Special techniques and methods<br />
Pathology is a technologically advanced specialty<br />
and the reporting pathologist will also undertake any<br />
further relevant tests (e.g. for HPV or molecular or<br />
genetic testing) vital to your diagnosis and treatment<br />
plan (i.e. HPV positive cancers may not always<br />
require surgery as the first line of treatment). Other<br />
related information such as clinical photographs or<br />
radiological imaging may also be assessed by the<br />
Pathologist to obtain contextual information.<br />
Figure 4 - p16 positivity (brown colour) in a tonsillar cancer<br />
to determine HPV presence.<br />
Dr Ali Khurram<br />
BDS, MSc., PhD, MFDS RCS (Edinburgh), CiLT, FHEA, FDS RCS (England), FRC Path<br />
Senior Clinical Lecturer and Consultant Pathologist<br />
Dr Ali Khurram is a Senior Clinical Lecturer and Consultant Pathologist at the University of<br />
Sheffield, UK. His postdoctoral training was funded by the National Institute for Health Research<br />
(NIHR), UK as a part of which he also trained as a Diagnostic Oral and Maxillofacial Pathologist.<br />
Following the successful completion of FRCPath in 2016, he was appointed as a Senior Clinical<br />
Lecturer and Consultant Pathologist at the School of Clinical Dentistry, University of Sheffield.<br />
49
It helps when you<br />
speak to someone who<br />
understands you<br />
Our 24/7 Patient and Carer<br />
support line service is<br />
answered by a real person<br />
50<br />
Alternatively visit our website<br />
www.theswallows.org.uk<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Facts about...<br />
MOUTH<br />
CANCER<br />
What is Mouth <strong>Cancer</strong><br />
This is the general term given to the variety of<br />
malignant tumours that develop in the mouth,<br />
(oral cavity). The Mouth <strong>Cancer</strong> Foundation<br />
promotes awareness of all head and neck cancers<br />
i.e. throat (pharynx), voice box (larynx), salivary<br />
glands, nose, nasal, sinuses, lips and skin.<br />
Symptoms<br />
...................................................<br />
• An ulcer or white or red patch anywhere in the mouth<br />
that does not heal within 3 weeks.<br />
• A lump or swelling anywhere in the mouth, jaw or neck<br />
that persists for more than 3 weeks.<br />
• Difficulty swallowing, chewing or moving the jaw or tongue.<br />
• Numbness of tongue or other area of the mouth.<br />
• A feeling that something is caught in the throat.<br />
• A chronic sore throat or hoarseness that persists<br />
more than 6 weeks.<br />
• Unexplained loosening of teeth.<br />
1 person every 3 HOURS is lost to Mouth cancer<br />
Over 8300 new cases in the UK each year<br />
Each year 2700 + lives are lost to Mouth <strong>Cancer</strong><br />
Worldwide Mouth <strong>Cancer</strong> affects 650,000 per year<br />
Risk Factors<br />
...................................................<br />
• Tobacco use is the main cause of mouth cancer.<br />
• Drinking alcohol to excess can increase risks four fold.<br />
• Drinking and smoking together can make mouth cancer<br />
up to 30 times more likely to develop.<br />
• Poor diet and social deprivation is linked to a third of<br />
all cancer cases.<br />
• The Human Papilloma Virus (HPV), transmitted through<br />
oral sex, could overtake tobacco and alcohol as the main<br />
risk factor within the next decade.<br />
• Exposure to the sun is a cause of skin cancer which can<br />
affect the lips and face.<br />
Mouth <strong>Cancer</strong> is TWICE as common in men<br />
78% off cases occur in the Over 55 age group<br />
Incidence has risen by 49% over the past 10 years<br />
5 year SURVIVAL rate has hardly improved in last few decades<br />
To make a donation or for FREE information visit<br />
www.mouthcancerfoundation.org<br />
Advice Line: 01924 950 950 • <strong>Head</strong> Office +44 (0) 208 940 5680<br />
Alternatively you can email info@mouthcancerfoundation.org<br />
JOIN OUR WALK FOR<br />
MOUTH CANCER<br />
SCAN TO<br />
WATCH<br />
OUR<br />
YOUTUBE<br />
VIDEO<br />
51
What does quality of life mean<br />
to the healthcare professional?<br />
On preparing to write this article, a short<br />
poll of healthcare colleagues revealed some<br />
expected answers to the question of ‘what<br />
does quality of life mean to you?’ Responses<br />
centred on familiar themes, each essential<br />
in living well beyond or with cancer: eating<br />
and drinking, communicating, managing<br />
pain and dry mouth, participating in social<br />
activities and wellbeing. One response stood<br />
out above all others, however. A succinct<br />
response from an experienced clinician<br />
who simply stated that ‘quality of life means<br />
whatever the patient says it means.’ With<br />
these sage words in mind, we begin by<br />
addressing why quality of life matters to<br />
the healthcare professional and how it is<br />
approached in clinical practice.<br />
Incidence of head and neck cancer has increased<br />
by 20% in the UK within the last decade (<strong>Cancer</strong><br />
Research UK, <strong>2021</strong>), however one and five-year<br />
survival rates have also increased over a similar<br />
timeframe (Macmillan, 2017). Whilst increase in<br />
survival is clearly a favourable statistic, the quality<br />
of that life in survivorship must be considered. It<br />
is essential that the experience of survivorship is a<br />
positive one; optimised through management of<br />
the impact of cancer treatment.<br />
Following a diagnosis of head and neck cancer, 53%<br />
of patients report a decrease in quality of life (Rogers<br />
et al, 2012). Assessment of quality of life ensures that<br />
the impact of treatments and the cancer itself is<br />
acknowledged and understood. It is our role as<br />
healthcare professionals to explore this in a patientcentred<br />
way and to identify individualised support<br />
needs based on the lived<br />
experience.<br />
In response to the need<br />
for greater focus on longterm<br />
cancer support,<br />
the National <strong>Cancer</strong><br />
Survivorship Initiative<br />
(NCSI) was implemented<br />
in 2010 (Richards et<br />
al, 2011). The NCSI is a<br />
partnership between the<br />
Department of Health<br />
and Macmillan <strong>Cancer</strong><br />
Support and its aim is to<br />
Figure 1: The Recovery<br />
ensure cancer survivors,<br />
Package (Macmillan, 2013)<br />
and those living with<br />
cancer, receive the support they require to continue<br />
a healthy and active life. Through the work of the<br />
NCSI, the Recovery Package was developed. All<br />
cancer patients should<br />
have access to The<br />
Recovery Package,<br />
which consists of holistic<br />
needs assessment,<br />
treatment summary,<br />
ongoing education and<br />
support events and<br />
a GP led cancer care<br />
review at six months.<br />
Additionally, the package<br />
provides healthcare<br />
professionals with a<br />
structured approach to<br />
delivery of holistic care,<br />
in collaboration with the<br />
patient.<br />
The practice of<br />
healthcare professionals<br />
in relation to quality of<br />
life is informed by several<br />
guidelines. National<br />
Institute for Clinical<br />
Excellence guidance on<br />
supportive and palliative<br />
care (NICE, 2004) advises<br />
that throughout the<br />
cancer pathway, physical,<br />
financial, spiritual,<br />
psychological and social<br />
wellbeing should be<br />
assessed and supported.<br />
The requirement<br />
to undertake this<br />
assessment at several points along the cancer<br />
pathway is highly relevant as quality of life may vary<br />
at different stages, therefore assessment should be<br />
a dynamic, ongoing process adapted to changing<br />
needs.<br />
The British Association of <strong>Head</strong> and <strong>Neck</strong> Oncologists<br />
(BAHNO, 2020) echo the NICE guidance, stipulating<br />
that repeated holistic needs assessment should<br />
be undertaken to identify needs and manage or<br />
signpost to alternative services.<br />
Beyond oncological and surgical treatment, longterm<br />
rehabilitation needs are provided by nursing<br />
and allied health professionals (AHPs). Detailed<br />
guidance for AHPs is provided in the <strong>Cancer</strong><br />
Rehabilitation Pathways (Macmillan, 2018) and<br />
NHS England guidance which advocate holistic<br />
needs assessment throughout cancer care, noting<br />
that ‘timely, holistic and personalised care improves<br />
quality of life’ (NHS England, 2018).<br />
52<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
A challenge for the<br />
healthcare professional is<br />
how to put these guidelines<br />
into clinical practice. Within<br />
the context of the finite<br />
resources of NHS services<br />
and the time limitations of<br />
under-resourced outpatient<br />
clinics, how do we ensure<br />
that care meets the<br />
required standards and the<br />
individual’s quality of life<br />
needs are met?<br />
In this regard, a multitude<br />
of assessment tools are<br />
established in practice to<br />
gain information about<br />
quality of life and treatment<br />
outcomes as reported by the<br />
patient. Assessment tools<br />
are useful for the clinician as<br />
they provide (in many cases)<br />
a validated measure which<br />
can be used quickly and<br />
at various stages, allowing<br />
problems to be identified<br />
and the impact of support<br />
measured. They also<br />
fulfil the requirements of<br />
cancer data reporting and<br />
research. However, a review<br />
of quality of life assessments<br />
by Ojo et al (2012), noted<br />
that ‘there is no gold<br />
standard questionnaire’ and<br />
concluded that there is work<br />
to be done to ensure that<br />
measures translate to being<br />
clinically useful in practice<br />
and truly representative of patient experience.<br />
This is pertinent as, despite the unquestionable<br />
utility of quality of life assessment tools, there is the<br />
risk that healthcare professionals may only ask the<br />
questions that we want to know the answer to. By<br />
assessing quality of life only in this way the patient<br />
lacks agency to lead discussion towards the support<br />
they want and they may feel that their concerns are<br />
not reflected accurately within the confines of the<br />
assessment tool. As healthcare professionals we<br />
must therefore question if we are truly addressing<br />
what matters to the patient or if we are projecting<br />
only our own opinions of what we think quality of<br />
life looks like.<br />
The Patient Concerns Inventory for <strong>Head</strong> and <strong>Neck</strong><br />
(PCI) (Rogers et al, 2009) is a holistic assessment<br />
tool which seeks to address this by supporting<br />
the patient to discuss concerns that may be less<br />
immediately identifiable within an outpatient<br />
appointment. The PCI takes the form of a patientled<br />
prompt list of discussion areas, covering physical<br />
and functional wellbeing, treatment related, social<br />
care and well-being, psychological, emotional<br />
and spiritual wellbeing.<br />
The patient<br />
is therefore placed<br />
at the centre of<br />
the consultation<br />
and empowered to<br />
take active control<br />
of what they would<br />
like to discuss.<br />
The PCI has been<br />
shown to make<br />
consultations feel<br />
more personal and<br />
importantly does<br />
not significantly<br />
i n c r e a s e<br />
consultation time<br />
(Rogers et al, 2009).<br />
T h e s e<br />
developments,<br />
and the increasing<br />
Figure 2: The Patient<br />
Concerns Inventory for<br />
<strong>Head</strong> and <strong>Neck</strong><br />
awareness of long-term quality of life issues in<br />
strategy and guidelines, demonstrate a growing<br />
appetite to ‘get things right’ from the patient’s<br />
perspective.<br />
We have briefly reviewed what quality of life means<br />
to the healthcare professional and identified that<br />
there are several contributing factors. The competing<br />
demands of clinical pressures and collecting essential<br />
data on clinical outcomes must be balanced with our<br />
responsibilities towards the patient and compliance<br />
with clinical practice guidelines.<br />
It is essential that assessment is holistic and<br />
dynamic to respond to the fluctuating quality of<br />
life at all stages of cancer pathway. Alongside the<br />
available assessment tools we must work hard to<br />
identify what quality of life means to each individual<br />
and ensure that we tailor our interventions towards<br />
optimisation of a patient directed agenda. The<br />
hope is that greater alignment between the<br />
patient and the healthcare professional can achieve<br />
meaningful outcomes that benefit quality of life.<br />
References are available on request.<br />
Written by<br />
Freya Sparks<br />
BA(HONS), PGDIP, MRES MRCSLT<br />
Clinical Specialist Speech and<br />
Language Therapist at Barts Health<br />
53
Introducing Provox Life<br />
• Better pulmonary performance<br />
• Enables 24/7 HME use<br />
• Reduction of mucus<br />
• Reduced coughing<br />
Home<br />
HME<br />
Go<br />
HME<br />
Night<br />
HME<br />
Energy<br />
HME<br />
Protect<br />
HME<br />
FreeHands<br />
HME<br />
Standard<br />
Adhesive<br />
Sensitive<br />
Adhesive<br />
Stability<br />
Adhesive<br />
Night<br />
Adhesive<br />
Breathe better, whatever you do<br />
The Provox Life TM system was developed on the<br />
basis of thorough research, and is designed to<br />
address the challenges that you experience with<br />
HMEs and attachments.<br />
Designed for people with a laryngectomy, the<br />
system offers a complete, flexible solution that<br />
allows you to experience a personalised routine,<br />
no matter where you are on your recovery<br />
journey.<br />
Please visit our website at www.atos-care.co.uk<br />
or call us on 0800 783 1659 for more information<br />
on how Provox Life TM can improve your quality<br />
of life.<br />
The next generation solution<br />
consists of:<br />
• Six high performing HMEs that offer<br />
improved humidification and<br />
breathability<br />
• Four newly designed adhesives for a<br />
wider range of skin types and stoma<br />
contours with improved materials and<br />
new SecureFit TM coupling<br />
• HMEs that are compatible with all<br />
adhesives in the Provox Life TM range<br />
to offer you a personalised routine<br />
Call us:<br />
0800 783 1659<br />
Email us:<br />
provoxlife@atos-care.co.uk<br />
Visit our website:<br />
www.atos-care.co.uk<br />
54<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
55
THE IMPORTANCE OF RESEARCH IN THE<br />
FIGHT AGAINST HEAD AND NECK CANCER<br />
<strong>Head</strong> and neck cancer (HNC) encompasses<br />
cancers of the larynx, pharynx, oesophagus,<br />
trachea, mouth, tongue, nose, salivary glands<br />
and tonsils, and collectively are the 8th most<br />
common cancer in the UK with over 12,000<br />
new cases diagnosed every year. Survival<br />
rates range from 19% to 59%, depending on<br />
the location and type of cancer [1]. Crucially,<br />
these improvements in survival have been<br />
made possible in large part to significant<br />
investment into research. Here, I describe<br />
some of the pivotal advancements that<br />
have led to improvements in treatment and<br />
scientific discovery, and my perspectives on<br />
the future of HNC research.<br />
Historic Treatment of HNC<br />
Early discovery of HNC<br />
Archaeological evidence has shown that<br />
HNC was evident as early as 3000 BCE<br />
in Egypt (The Ebers Papyrus) and Peru.<br />
Treatment consisted of poultices, composed<br />
of cow’s fat, wax and earth. Following this, the<br />
Greek physician Hippocrates was amongst<br />
the first to describe, in detail, the diagnosis<br />
and surgical treatment of head and neck<br />
cancer, in the fourth and fifth centuries BC.<br />
However, it was the Greek physician Galen,<br />
who lived during the 2nd Century, who<br />
changed the attitude to HNC, due to his<br />
humoral theory; suggesting that incurable<br />
cancers form from residues of black bile, and<br />
curable ones from excesses of yellow bile.<br />
His view that cancer was a systemic disease<br />
caused by imbalances of the humours, led<br />
to a decline in surgical intervention to treat<br />
HNC. Crucially, it wasn’t until the 17th Century<br />
when scientific discovery really began<br />
informing HNC treatment.<br />
Discovery of the causes of HNC<br />
We now know that a number of<br />
environmental effects influence to incidence<br />
of HNC. However, it wasn’t until the 18th<br />
Century, that the London physician John Hill<br />
hypothesised that the use of tobacco was<br />
associated with the occurrence of HNC, and<br />
issued the statement “with respect to cancers<br />
of the nose, they are as dreadful and as fatal<br />
as any others … It is evident therefore that no<br />
man should venture upon snuff who is not<br />
sure that he is not so far liable to a cancer:<br />
and no man can be sure of that”. Smoking<br />
tobacco superseded the use of snuff in the<br />
late 18th Century; however, despite there<br />
being much research into the links between<br />
tobacco use and cancer in the following years,<br />
it was 1964 before a national commission in<br />
the US concluded that cigarette smoking<br />
was a significant cause of laryngeal cancer.<br />
The subsequent drive to highlight the harms<br />
of tobacco has had a very positive influence<br />
on the incidence of HNC, due in no small part<br />
to substantial research.<br />
Scientific research to inform<br />
treatment<br />
The expanded use of the microscope in<br />
pathology in the 19th Century opened up<br />
insights in into cancer, specifically with the<br />
knowledge of Rudolf Virchow, who described<br />
the cellular composition of tumours and<br />
the stages in tumour development that<br />
we use to this day. This allowed better<br />
diagnosis and informed subsequent<br />
treatment options. In addition, at the turn<br />
of the century (1895) the discovery of X-rays<br />
was announced and the phenomenon<br />
of radioactivity was described (also 1895).<br />
These scientific discoveries were followed<br />
by the discovery of radium by the Curies<br />
in 1898. Thus, the 20th century introduced<br />
the use of ionising radiation (radiotherapy)<br />
in 1951 and, later, chemotherapy in 1966, as<br />
therapeutic alternatives to, or in combination<br />
with, surgery. Radiotherapy went through 4<br />
stages to become the therapy we all know<br />
today, as scientists and physicians began to<br />
better understand radiation biology. By the<br />
second and third phases the emphasis was<br />
on selective destruction of the tumour while<br />
preserving local tissue, employing accurate<br />
planning of treatment with respect to<br />
anatomical fields and dosimetry. To this day,<br />
radiotherapy follows these same rules and<br />
provides a life-saving treatment for many<br />
thousands of HNC patients every year.<br />
Surgical practice in HNC treatment<br />
While surgery was originally utilised to<br />
remove a tumour, it had fallen out of favour<br />
in the 2nd Century. However, by the late 19th<br />
Century and into the 20th Century modern<br />
surgical practice, with much improved<br />
survival, was commonplace, with particular<br />
success attributable to Henry Butlin of St.<br />
Bartholomew’s Hospital. His careful notekeeping<br />
and follow-up of patients (in 1898 he<br />
was able to trace all but seven of 102 patients<br />
he had treated) showed that survival<br />
following HNC surgery improved from 5% to<br />
28%, and later, to 42%. He also identified that<br />
metastases often occurred in HNC patients,<br />
due to spread to and from the lymph nodes.<br />
He subsequently proposed and practised<br />
nodal dissection during his surgeries to<br />
reduce the chance of cancer spread and<br />
metastases. In later years, improvements<br />
in anaesthesia, a better understanding<br />
of infection and the widespread use of<br />
antibiotics and blood replacement made<br />
surgery a much safer procedure.<br />
56<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Modern HNC prevention and treatment<br />
The association between viruses and HNC<br />
Once upon a time, HNC, and indeed all cancers, were<br />
considered to be caused by external factors, such as<br />
the use of tobacco and alcohol. In 1932, the Human<br />
Papilloma virus (HPV) was discovered; however, it<br />
wasn’t until the 1980s that the link between HPV and<br />
cervical cancer was published, against the popular<br />
dogma, leading to the principal scientist Harald zur<br />
Hausen being awarded the Nobel Prize for Physiology<br />
and Medicine in 2008. Vaccines have become<br />
commonplace in our society to protect against viral<br />
diseases, and cancer caused by viruses should be no<br />
exception. In 2006, the first HPV vaccine was approved<br />
for use to prevent HPV-related cervical cancer, and is<br />
now routinely administered to school-aged girls. In<br />
more recent years, a role for HPV in a subset of head<br />
and neck cancers, mostly cancers of the oropharynx,<br />
has been identified [2]. This led to the appeal that<br />
school-aged boys also be vaccinated against HPV in<br />
order to provide them with the equivalent protection<br />
as girls, an appeal that was won in 2018 in the UK.<br />
Crucially, recent research has demonstrated that HPV<br />
vaccination has reduced the incidence and mortality<br />
from cervical cancer in women by 90% [3], and with<br />
time we expect to see the same trend with HNC in<br />
both men and women. In support of this, a study of<br />
more than 7,000 young women in Costa Rica found<br />
that the prevalence of HPV infection was significantly<br />
lower in those vaccinated, compared to those who<br />
were not vaccinated [4].<br />
Genetic testing as a tool to treat HNC<br />
The advent of genetic testing and precision medicine<br />
has accelerated the development of targeted<br />
therapies for the treatment of HNC. For example, the<br />
epidermal growth factor receptor (EGFR) inhibitor<br />
cetuximab was the first approved targeted therapy<br />
for HNC [5], after extensive research. More recently,<br />
HPV, EGFR, and LOH have become examples of<br />
biomarkers that can have diagnostic, prognostic, or<br />
therapeutic value in HNC research and treatment.<br />
In recent years, The <strong>Cancer</strong> Genome Atlas Research<br />
Network have discovered genomic differences,<br />
specifically alterations of the gene FGFR3 and<br />
mutations in the PIK3CA gene in HPV+ HNC, that<br />
could have significant clinical implications. These<br />
genes may play roles in pathways that control cell<br />
growth and proliferation, and for which therapies<br />
are either already available or are currently in<br />
development.<br />
Improvements in cancer imaging<br />
The ability to “visualise” cancer has greatly improved<br />
treatment options and improve quality of life. In<br />
2016, improvements in imaging techniques allowed<br />
clinicians to identify patients who may be able to<br />
avoid surgical dissection. An advanced imaging<br />
technique, known as PET-CT, has been shown to<br />
successfully identify both structural and metabolic<br />
abnormalities in tumours. Patients who underwent<br />
PET-CT imaging after chemoradiation to determine<br />
if they still needed to have surgery had overall survival<br />
rates similar to those of patients who underwent<br />
planned neck dissection and chemoradiation, while<br />
PET-CT imaging also resulted in fewer operations and<br />
was more cost-effective [6]. Collectively, this approach<br />
to treatment both saves lives and vastly improves<br />
patient quality of life.<br />
Conclusions and future approaches<br />
The distance we have come in human history in our<br />
fight to treat HNC is evident in this timeline, from a 5%<br />
survival expectancy following surgery to close to 100%<br />
nowadays. Collectively, this highlights the importance<br />
of research in the progressing with treatments and<br />
methods to detect cancer. However, while survival<br />
rates can be as good as 59%, for some HNC subtypes<br />
it is still as low as 19%. How do we improve this to<br />
100%? The boom in the use of immunotherapy, the<br />
method by which the patient’s own immune system<br />
is “reprogrammed” to attack cancer cells specifically,<br />
is a promising area of study. However, such research<br />
is costly and requires great skill in the research<br />
workforce. Thus, we collectively need to recognise the<br />
importance of research as we strive to improve the<br />
diagnosis, treatment and lives of those diagnosed<br />
with HNC, and to make our voices heard, especially to<br />
those who control the purse strings. While HNC is the<br />
8th most common cancer in the UK with over 12,000<br />
new cases diagnosed every year, research into HNC<br />
accounts for less than 1% of the total amount spent<br />
annually on cancer research in the UK [7]. Thus, it is<br />
not surprising that HNC survival and quality of life are<br />
lagging behind other cancers.<br />
Furthermore, we shouldn’t overlook our collective<br />
voice when it comes to political decisions. Applications<br />
for European funding have already fallen by 40% since<br />
the decision to leave the EU [8] and a number of highprofile<br />
eminent scientists wrote an open letter to the<br />
Prime Minister in late 2020, highlighting the need for a<br />
compromise with EU leaders to continue benefitting<br />
from EU funding and for the UK to remain a scientific<br />
leader that we have come to know it to be [9].<br />
Moreover, UK science relies on attracting international<br />
talent, something that shouldn’t be overlooked when<br />
discussing the UK’s position on immigration. We all<br />
have the power to use our collective voice for good<br />
when it comes to improving research into this vastly<br />
underappreciated disease.<br />
References are available on request.<br />
Written by<br />
Dr Elaine Emmerson<br />
B.Sc. (Hons), Ph.D.<br />
The Centre for Regenerative Medicine,<br />
The University of Edinburgh<br />
57
Dry Mouth?<br />
Don’t Don’t ignore it. it.<br />
R<br />
Dry Dry Mouth Mouth (Xerostomia), is a distressing a distressing and and debilitating debilitating<br />
condition condition that that can can have have a profound a profound impact impact on a on person’s a person’s<br />
quality quality of life. of life.<br />
Keeping Keeping hydrated hydrated is very is very important, important, but but this this alone alone is is<br />
often often not not enough. enough. Therefore, Therefore, to help to help relieve relieve Dry Dry Mouth Mouth<br />
symptoms, symptoms, clinicians clinicians often often prescribe prescribe a saliva a saliva substitute. substitute.<br />
Due Due to its to long its long history history in clinically clinically proven proven Dry Dry Mouth Mouth<br />
relief, relief, they they often often choose choose A.S A.S Saliva Saliva Orthana Orthana to get to get the the<br />
best best results results for their for their patients. patients.<br />
Unlike Unlike most most other other Dry Dry Mouth Mouth products, products, ours ours are are pH pH<br />
neutral. neutral. This This important, is important, as any as any increase increase acidity in acidity<br />
levels levels can can result result in additional in additional mouth mouth soreness soreness and and<br />
accelerated accelerated tooth tooth decay. decay.<br />
The A.S The Saliva A.S Saliva Orthana Orthana Range Range<br />
Dry Mouth Dry Mouth relief relief<br />
• Clinically • Clinically proven proven<br />
• Easy • Easy to use to & use long-lasting & long-lasting<br />
• Pump • Pump action action spray, spray, no propellent no propelle<br />
• Creates • Creates a protective a protective oral oral coating coati<br />
• Mild • Mild flavoured flavoured and pH and neutral pH neutra<br />
Available Available in 50ml in oral 50ml pump oral spray, pump 500ml spray, 500ml refill and refill and • Based on natural mucin<br />
lozenges, lozenges, see our see website our website for more for details.<br />
• Based on natural mucin<br />
more details.<br />
• On • prescription On prescription<br />
58<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Relieve it! it!<br />
Dry Dry Mouth Mouth Relief Relief<br />
nt<br />
ng<br />
l<br />
Unlike Unlike most most other other Dry Dry Mouth Mouth products, products, ours ours are are pH pH<br />
neutral. neutral. This This important, is important, as any as any increase increase acidity in acidity levels levels<br />
can can result result in additional in additional mouth mouth soreness soreness and and accelerated accelerated<br />
tooth tooth decay. decay.<br />
For For more more information information on Dry on Dry Mouth Mouth and and our our range, range, or or<br />
request request a sample a sample call call us 01264 us 01264 332172 332172 or visit or visit<br />
www.CCMed.co.uk<br />
FOLLOW FOLLOW US: US:<br />
@DryMouth_Relief<br />
59
Targeted treatment for oral mucositis and dry mouth<br />
Protects Relieves Heals<br />
the healthy oral mucosa<br />
the symptoms of dry<br />
mouth and oral mucositis<br />
mouth ulcers<br />
Mucosamin ® Mouthwash and Mucosamin ® Oral Spray help to relieve and treat<br />
the symptoms of oral mucositis and dry mouth caused by cancer treatment<br />
(radiotherapy and chemotherapy).<br />
Available as a soothing mouthwash and a convenient oral spray to provide relief<br />
when you need it most.<br />
Helps to protect the healthy lining of your mouth (oral mucosa).<br />
Reduces and relieves the symptoms of dry mouth.<br />
Provides pain relief.<br />
Supports healing of mouth ulcers (oral lesions).<br />
Hyaluronic acid (HA)<br />
✓ Hydrating and lubricating properties<br />
✓ Leads to greater saliva production<br />
✓ Supports wound healing<br />
Amino acids<br />
(glycine, L-proline, L-leucine and L-lysine HCl)<br />
✓ Promote the formation of collagenkey<br />
for tissue healing<br />
✓ Necessary for wound repair<br />
60<br />
Always read the label.<br />
10104611312 v1.0 Oct 21<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Mouthwash<br />
For use alongside your<br />
daily dental routine.<br />
Oral Spray<br />
For fast, targeted relief<br />
when and where it’s<br />
needed.<br />
Mucosamin ® products can be used together to provide a convenient and effective<br />
way to help you with the effects of cancer therapy. Mucosamin ® can be used before,<br />
during and after chemo or radiotherapy.<br />
Where is Mucosamin ® available from?<br />
If you are undergoing chemotherapy or radiotherapy for a head or neck cancer,<br />
your healthcare professional can prescribe Mucosamin ® Mouthwash and Oral<br />
Spray for you. Alternatively, you can buy directly from pharmacies or find online at<br />
Amazon.co.uk<br />
On prescription In pharmacies Online at amazon.co.uk<br />
The Oral Health Foundation recognises that Mucosamin ® Mouthwash and<br />
Oral Spray are useful in helping to relieve the symptoms of dry mouth<br />
and oral mucositis, and promote the healing of the oral mucosa.<br />
@mucosamatters<br />
A social media community for oral mucositis and dry mouth sufferers and caregivers.<br />
www.mucosamin.co.uk<br />
Always read the label.<br />
10104611312 v1.0 Oct 21<br />
61
Supporting you at every<br />
stage of your journey<br />
back to work<br />
Written by patients & caregivers<br />
for patients and caregivers<br />
To order your copy of the Back to Work Guide,<br />
email: chris@theswallows.org.uk<br />
62<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Specialists in<br />
<strong>Cancer</strong> Innovation<br />
Treatments for<br />
<strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong><br />
ORALID<br />
OralID is manufactured by Forward Science, a<br />
company that was founded with the vision to<br />
create a simpler, efficient, and more affordable<br />
oral cancer screening device. OralID uses the<br />
same proven fluorescence technology as other<br />
oral exam devices, with no up-front costs and<br />
lower overall lifetime costs.In addition, unlike any<br />
other device on the market, OralID has no perpatient<br />
cost during use.<br />
SalivaMAX® is a supersaturated calcium phosphate<br />
powder that when dissolved in water, creates a solution<br />
with a high concentration of electrolytes similar to<br />
that of natural saliva. SalivaMAX is an artificial saliva<br />
that is used to relieve acute and chronic symptoms of<br />
xerostomia. Supersaturated calcium phosphate rinses<br />
have been clinically proven to reduce the symptoms<br />
of xerostomia (dry mouth) due to medications,<br />
dysfunction of the salivary glands, Sjögren’s syndrome,<br />
chemotherapy, and radiation treatment.<br />
SalivaMAX®<br />
Orapeutic<br />
Orapeutic is a medical device that has been<br />
designed to provide relief. and protection.<br />
Orapeutic provides a protective barrier<br />
over the wound preventing irritation and<br />
contamination.<br />
Find out more at<br />
www.healthcaresupplysolutions.co.uk
Speak<br />
in your<br />
own<br />
words<br />
Voice banking<br />
services for<br />
those affected<br />
by <strong>Head</strong> &<br />
<strong>Neck</strong> <strong>Cancer</strong><br />
Register at:<br />
www.speakunique.co.uk<br />
Please email Chris (chris@theswallows.org.uk)<br />
once registered with full names, email address,<br />
mobile number, and full address so we can allocate<br />
our code to the booking.<br />
own words<br />
for communication aids.<br />
The Swallows Charity and SpeakUnique<br />
working in collaboration to deliver voice<br />
to our patients. Voice Banking solutions<br />
for all speech needs.<br />
What is<br />
Voice Banking?<br />
In your<br />
After recommending someone to<br />
SpeakUnique. He was able to bank<br />
his voice the weekend before his<br />
surgery. He is in the top 0.3% of a<br />
company with 305,000 employees<br />
and is VERY happy with the results.<br />
He’s been able to conduct business<br />
and to record your voice, please visit<br />
SpeakUnique<br />
about information more For<br />
info@speakunique.co.uk.<br />
us an email at<br />
drop Alternatively<br />
using Speak Unique!<br />
Don’t Just Take Our Word For It<br />
SpeakUnique voices:<br />
of our users say about their<br />
some what Here’s<br />
a voice which is recognisably mine, which means I am<br />
using work at people with communicate to able am “I<br />
comfortable continuing with part-time paid employment”<br />
with my degraded voice on a couple of days says he<br />
me heard only has and London in lives who son “My<br />
played the voice to him”<br />
if someone<br />
me as straightaway it recognise would<br />
“My grandchildren said, ‘It sounds just like Gramps!’ ”<br />
only recorded half the phrases, so it seems little short of<br />
I and recording, the made I when breathless bit a was “I<br />
miraculous that the synthetic voice is so close to my voice”<br />
research project, partly because it seemed such a<br />
banking<br />
voice a in participated I ago years “Several<br />
speaking. I had no idea then that I would have a<br />
public<br />
enjoyed I because partly and innovation, great<br />
diagnosed with Motor Neuron Disease, and my speech<br />
was I year last But, recordings. those of need personal<br />
me to have been able to acquire a synthetic voice based<br />
to<br />
important hugely been has It affected. badly been has<br />
Contact Us<br />
www.speakunique.co.uk.<br />
Steven Cooper<br />
Voice Banking is a term given to the process of recording your voice<br />
and using this recording to generate a personalised synthetic voice.<br />
This synthetic voice can then be used on a device, where it converts<br />
text to speech, allowing an individual to communicate with a voice that<br />
is identifiably their own, even when natural speech is not possible.<br />
to be able to retain some of my personal identity.”<br />
difference<br />
a such makes It recordings. voice own my on<br />
Traditionally voice banking has only been available to people who<br />
know they are going to lose their voice but have not yet developed<br />
speech symptoms. SpeakUnique are the only service who can also<br />
offer voice banking to those with impaired speech through our Voice<br />
Repair service, and offer a bespoke Voice Design service for those<br />
with no speech so they can choose how they sound.<br />
How does SpeakUnique work?<br />
SpeakUnique offer voice banking technology to allow people to retain<br />
their identity and communicate in a voice that is their own, even when<br />
natural speech is not possible. Sign up today to submit your recordings<br />
and hear your synthetic voice tomorrow. Listen to samples of your voice<br />
before downloading it. Your synthetic voice can be used on Apple, and<br />
Android devices using the SpeakUnique app, or on Windows devices,<br />
accessed through third party software (must be purchased separately).<br />
A Voice Build synthetic voice is £220 however there will be no<br />
charge as you will be refered from The Swallows <strong>Head</strong> & <strong>Neck</strong><br />
<strong>Cancer</strong> Charity.<br />
Personalised synthetic voices<br />
64<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Contact Us<br />
and to record your voice, please visit<br />
SpeakUnique<br />
about information more For<br />
www.speakunique.co.uk.<br />
info@speakunique.co.uk.<br />
us an email at<br />
drop Alternatively<br />
The process<br />
Easy as 1, 2, 3...<br />
own words<br />
your In<br />
for communication aids.<br />
voices<br />
synthetic Personalised<br />
The Process<br />
We can build your synthetic voice from just a short<br />
recording of your speech. All you need to get started is a<br />
computer or laptop, an external microphone (not the one<br />
built into your computer) and a quiet room.<br />
1. Grant forms available by sending an email to<br />
sharon@theswallows.org.uk<br />
2. Complete the application form and send to<br />
sharon@theswallows.org.uk to process.<br />
3. Acceptance is within 24 hours.<br />
4. During this time register on the SpeakUnique website<br />
– in the “How did you hear about us” box, please enter<br />
The Swallows.<br />
5. Record your voice (follow simple instructions on the<br />
website – step by step “How to” guides can be found<br />
at: www.speakunique.co.uk/resources-and-support/<br />
support-documents/)<br />
For recording we recommend:<br />
a. Patient is in a quiet room.<br />
b. Use a quality mic. The quality of the recording will<br />
impact the quality of the synthetic voice, so it is<br />
important to use a good microphone, be in a quiet<br />
room and make sure there isn’t too much echo.<br />
c. Take time when reading the words.<br />
6. On acceptance of the grant, we will inform<br />
SpeakUnique to issue the voice and The Swallows<br />
reimburse SpeakUnique direct. We will need to share<br />
the user’s name and email address with SpeakUnique<br />
so they can match the funding to the patient.<br />
7. Following the successful use of the voice, we ask for a<br />
testimonial and a report from the team (to help us get<br />
this as standard process of the pathway and funded by<br />
the NHS).<br />
8. If the process is urgent due to operation time-line, then<br />
please highlight this on your initial email and grant form,<br />
we can then fast track the process.<br />
9. As we are a charity, if the patient can afford the £200<br />
fee, then please ask them to pay as this will leave funds<br />
free for other patients that cannot. In this case, payment<br />
will be made to The Swallows to ensure that there is<br />
no confusion about who is paying for the voice with<br />
SpeakUnique.<br />
The Swallows Charity<br />
Remember, this special rate is only available<br />
via the Swallows.<br />
Register at:<br />
www.speakunique.co.uk<br />
65
Expert Hand. Human Touch.<br />
Protect what matters most<br />
A bit about me and my background<br />
My name is Shahin Master, I’m an associate<br />
solicitor for Irwin Mitchell based in<br />
Manchester. I was a dental surgeon and<br />
practised dentistry before qualifying as a<br />
solicitor in 2010.<br />
I’ve worked as a dentist in general practice,<br />
in the community dental service treating<br />
children and adults with special needs and in<br />
a dental hospital. I’ve also worked as a senior<br />
house officer in an oral medicine team based<br />
in a city centre hospital in London, where I<br />
was involved in seeing patients who’d been<br />
referred urgently with suspected head and<br />
neck cancer.<br />
Putting my experience to work<br />
As part of the dedicated Dental Negligence<br />
team at Irwin Mitchell I often see delays in<br />
the diagnosis of oral cancer, nerve injuries,<br />
substandard dental implant treatment and<br />
periodontal disease cases. I’ve acted for<br />
clients and their families who’ve suffered the<br />
devastating effects of head and neck cancer as<br />
a result of negligent care and I’m committed<br />
to making a positive difference.<br />
My team work hard to ensure that our clients<br />
are able to get the support and answers<br />
they need. We recognise the impact that<br />
a diagnosis has not only on the individual<br />
affected but also their families.<br />
66<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
I’m very passionate about raising awareness<br />
of the importance of the early detection of<br />
head and neck cancer, because I’ve seen firsthand,<br />
through the work I do, what impact<br />
this can have on prognosis.<br />
Shahin Master<br />
Associate Solicitor<br />
Erica’s story<br />
Erica* visited her dentist because she was<br />
concerned about a lump in her mouth, and<br />
after a number of appointments, she was<br />
diagnosed with an abscess.<br />
She went on to suffer with loosening of<br />
her lower teeth and as a result had to have<br />
some extracted. Despite this her symptoms<br />
persisted and worsened. Eventually she was<br />
referred to hospital where she underwent a<br />
biopsy and was diagnosed with advanced<br />
squamous cell carcinoma of her lower jaw.<br />
Erica then had to undergo extensive surgery,<br />
which included resection of her lower jaw and<br />
reconstruction. She’s been left unable to eat<br />
via her mouth and has to be peg fed.<br />
A helping hand<br />
Erica instructed us to pursue a medical<br />
negligence claim against her former dentist on<br />
her behalf, for failing to refer her to hospital<br />
in a timely manner under the two week<br />
referral rule. It was admitted that she should<br />
have been referred to hospital for further<br />
investigation earlier and that failure to do so<br />
constituted negligence.<br />
It was also admitted that had she been<br />
referred earlier, she would have been<br />
diagnosed earlier, which would have resulted<br />
in less extensive surgery and she wouldn’t<br />
have had to have her lower jaw resected.<br />
We were able to secure compensation<br />
for Erica, which allows her to pay for the<br />
professional care she now requires due to<br />
her ongoing condition. She’s been able to<br />
purchase the equipment she needs to live<br />
as independently as possible. Erica’s also<br />
gained access to private speech and language<br />
therapy.<br />
Erica has suffered psychologically as well<br />
as physically as a result of all she’s been<br />
through. Thankfully she’s been able to access<br />
specifically tailored therapy to help her cope<br />
with the devastating consequences of her late<br />
diagnosis and treatment.<br />
In these challenging times, Irwin Mitchell is<br />
here to protect what matters most to you. Visit<br />
irwinmitchell.com to find out more.<br />
*Erica is not our client’s real name and has been used to<br />
uphold her preferred anonymity.<br />
irwinmitchell.com<br />
Authorised and regulated by the Solicitors Regulation Authority.<br />
67
A new clinical<br />
trial for people<br />
diagnosed with<br />
head and<br />
neck cancer.<br />
The TrilynX Clinical Trial is evaluating a liquid investigational medication, xevinapant (Debio 1143),<br />
to see if it may improve the effectiveness of chemotherapy and radiation therapy when taken<br />
together for squamous cell carcinoma of the head and neck.<br />
Key Eligibility Criteria<br />
• At least 18 years of age (or equivalent majority age in your country)<br />
• Diagnosed with squamous cell carcinoma of the oropharynx, hypopharynx and/or larynx that has not spread to other<br />
parts of the body<br />
• Unable to have surgery to remove the cancer and have not received other cancer treatments<br />
• HPV-positive oropharynx patients are not eligible<br />
About xevinapant (Debio 1143)<br />
• May optimize the effectiveness of chemoradiotherapy (CRT) when administered together<br />
• A potential first-in-class oral antagonist of IAPs (inhibitor of apoptosis proteins), that sensitizes tumor cells to radiochemo<br />
therapy by promoting programmed cell death and fostering anti-tumor immunity<br />
• Granted breakthrough therapy designation by the FDA in early 2020<br />
About Debiopharm<br />
Debiopharm is a global biopharmaceutical company<br />
headquartered in Switzerland whose main area of expertise<br />
is oncology. Debiopharm is committed to bringing innovative,<br />
Copyright © 2020 Debiopharm<br />
life-saving treatments to people with cancer. For more<br />
TrilynX H&N <strong>Conference</strong> Poster_Global-English_<br />
V1_21OCT2020<br />
information 68 about Debiopharm, visit VIRTUAL debiopharm.com. HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Severn Healthcare have a long and proud history of supplying market leading products to<br />
support the laryngectomee community with their communication and stoma care needs.<br />
Covid 19 reinforced to all of us the importance of stoma protection for neck breathers. Stoma<br />
care, managing a laryngectomy tube or stoma button, changing a baseplate or cleaning a<br />
voice prosthesis (or valve) in as clean an environment as possible remains vitally important.<br />
Information and support that is easy to access remains a priority for the laryngectomy<br />
community.<br />
Severn Healthcare would therefore like to extend an invitation to you to visit the<br />
Laryngectomy Forum which can be found at: www.severnhealthcare.com<br />
In an effort to provide helpful information, postings are being made by Speech and Language<br />
Therapists, professional organisations, individuals within the laryngectomee community and<br />
their support groups.<br />
INSTRUCTIONS TO NAVIGATE TO THE FORUM:<br />
1. On any internet browser please type ‘SEVERN HEALTHCARE TECHNOLOGIES’<br />
2. Next click on ‘FORUM’<br />
3. Click the ‘SIGN-UP’ button in the top right-hand corner and create an account<br />
Alternatively, if you already have an account then please sign-in<br />
4. Once you have registered/signed-in then please browse the Forum posts and feel<br />
free to add any of your own comments<br />
5. The Forum has two groups. One is designated for Clinicians, the other is a general<br />
discussion group which every member has access to<br />
69
<strong>Head</strong> and <strong>Neck</strong><br />
<strong>Cancer</strong> Early<br />
Recurrence<br />
Detection Study<br />
Study Type: Non-interventional cohort study<br />
Planned enrolment: 200 participants<br />
Primary Purpose: Early Detection of Recurrence (funded by <strong>Cancer</strong> Research UK)<br />
Official Title: A prospective cohort study of patients with radically treated newly diagnosed<br />
locally advanced HPV negative head and neck cancer to develop and validate a<br />
multimodal signature to risk-stratify for recurrence<br />
Projected Start Date: November <strong>2021</strong><br />
Estimated Primary Completion Date: November 2024<br />
Recruitment Method/Participating Sites: Patients will be assessed and recruited<br />
from 3 sites; University College London Hospital (UCLH), London, Guys and St Thomas’<br />
Hospitals (GSTT), London and North Middlesex Hospital<br />
Investigators: Professor Tony Ng (KCL), Dr Martin Forster (UCL)<br />
Figure 1: Background<br />
<strong>Head</strong> and neck cancer is the 8th most common cancer in the UK, with 12,000 new cases diagnosed<br />
yearly. Most patients are diagnosed when the cancer is present in the head and neck area but has not<br />
spread to other organs. Doctors aim to cure the patient with either surgery and/or radiotherapy and<br />
chemotherapy as initial treatment. Despite this treatment, the cancer recurs within the first year in about<br />
3 in 10 patients (figure 1), and patients remain under surveillance (scans and clinic appointments, figure<br />
2) after initial treatment to detect whether the cancer has returned. There is no standardised programme<br />
for this surveillance, and so this varies between hospitals and clinicians (within both the public and private<br />
sectors) leading to inconsistencies. Here we can see a window of need to develop a strategy to help more<br />
accurately follow up patients.<br />
70<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Figure 2: Current pathway for surveillance and window of opportunity for risk stratifying patients<br />
Summary and Design<br />
The patients recruited into the study would be at a higher risk of recurrence based on factors related to the<br />
tumour ((Fig 3) e.g. size, involvement of lymph nodes). These samples will be taken before, during and after<br />
their initial treatment.<br />
Fig 3: Inclusion/Exclusion Criteria<br />
This study aims to predict the likelihood<br />
for the cancer to return after initial<br />
treatment by using a combination of<br />
blood, saliva, urine and stool tests along<br />
with modern imaging techniques (MRI<br />
based). We then aim to extract key<br />
information, such as changes in the<br />
stiffness of tumour, distribution and types<br />
of immune cells, genetic material, and<br />
even bacteria and their influence on the<br />
immune cells, in response to their initial<br />
treatment. A complex statistical model will<br />
then be used to put together these factors<br />
and link them to predict the likelihood for<br />
cancer recurrence. The data from these<br />
tests will be used by the research team to find markers to help doctors diagnose cancer relapse early<br />
on and to more accurately group high and low risk head and neck cancers. This is likely to improve the<br />
chances of cure in cases where relapse is diagnosed early.<br />
A successful predictive model may benefit future patients in<br />
two ways:<br />
• by generating a more personalised surveillance<br />
programme, with more intensive assessments for<br />
patients at higher risk, we may detect recurrence earlier.<br />
• patients at higher risk may benefit from extra treatment<br />
to reduce the chance of recurrence.<br />
Written by<br />
Dr Sanjena Mithra MRCP(UK), MBChB<br />
Specialist Registrar in Medical Oncology / Clinical<br />
Research Fellow, University College London<br />
71
TRUSTED NUTRITION FOR EVERY<br />
STAGE OF LIFE<br />
Abbott is a global healthcare leader that helps people live more<br />
fully at all stages of life. Our portfolio of life-changing<br />
technologies spans the spectrum of healthcare, with leading<br />
businesses and products in diagnostics, medical devices,<br />
nutritionals and branded generic medicines. Our 109,000<br />
colleagues serve people in more than 160 countries.<br />
Connect with us at www.abbott.com, on LinkedIn at<br />
www.linkedin.com/company/abbott-/, on Facebook at<br />
www.facebook.com/Abbott and on Twitter @AbbottNews.<br />
UK-N/A-2100384 October <strong>2021</strong><br />
All my best,<br />
Jim Lauder<br />
Call us at 800-388-8642 or e-mail me at jklvoice@aol.com.<br />
72<br />
We carry most of what you may need. What we don't carry, we usu<br />
will be happy to refer you to a distributor.<br />
At Lauder - The ElectroLarynx Company our most important goal is to make available the very best<br />
speech aids and laryngectomee products to our customers at fair prices.<br />
Our company began when my father Col. Edmund Lauder self-published his book, "Self Help for the<br />
Laryngectomee." Col. Lauder was himself a Laryngectomee; thus bringing needed experience and clari<br />
to the project. Throughout the years, this book has become an indispensable guide for laryngectomee<br />
We have ways of<br />
and those who care for them.<br />
making you talk...<br />
• voice amplifiers and • batteries.<br />
• books • tapes • electrolarynges (sales and service)<br />
Our products include:<br />
In 1990, when I was planning to print and update my father's book<br />
customers by offering the best products available today for the lar<br />
Our company began when my father Col. Edmund Lauder self-pub<br />
Laryngectomee." Col. Lauder was himself a Laryngectomee; thus b<br />
to the project. Throughout the years, this book has become an ind<br />
and those who care for them.<br />
At Lauder - The ElectroLarynx Company our most important goa<br />
speech aids and laryngectomee products to our customers at fair<br />
In 1990, when I was planning to print and update my father's book, I felt I could further serve his<br />
customers by offering the best products available today for the laryngectomee.<br />
Our most important goal is to make available the<br />
very best speech Our aids products and include: laryngectomee products<br />
to our customers at fair prices.<br />
• books • tapes • electrolarynges (sales and service)<br />
Our products include: • voice amplifiers and • batteries.<br />
Electrolarynges We carry (sales most of and what service) you may • need. Books What we don't carry, we usually know where you can get it and<br />
Tapes • Voice will be amplifiers happy to refer you • Batteries<br />
to a distributor.<br />
Call us at 800-388-8642 or e-mail me at jklvoice@aol.com.<br />
We carry most of what you may need. What we don’t,<br />
we usually know All where my best, you get it and will be happy<br />
to refer you to Jim a distributor.<br />
Lauder<br />
LAUDER ENTERPRISES INC.<br />
All my best,<br />
Jim Lauder<br />
Call for<br />
www.electrolarynx.com<br />
Catalog 800-388-8642<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong><br />
Email me at 4754 jklvoice@aol.com Shavano Oak, Suite | 4754 104 • Shavano San Antonio, Oak, TX 78249-4027 Suite 104 | • San www.electrolarynx.com<br />
Antonio, TX 78249-4027
<strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong><br />
The Symptoms<br />
Look out for the warning signs<br />
Persistent<br />
sore throat<br />
Foul breath<br />
Hoarseness or<br />
voice changes<br />
Swelling of<br />
throat<br />
Lump, bump or<br />
mass without pain<br />
White or red<br />
patch<br />
Persistent nasal<br />
obstructions or congestions<br />
If you have any of these symptoms contact your<br />
medical practitioner immediately<br />
<strong>Head</strong> to www.theswallows.org.uk to find out more<br />
73
What is the Impact of<br />
<strong>Head</strong> and <strong>Neck</strong> <strong>Cancer</strong> upon Sexuality?<br />
Why research this topic area?<br />
The experience of having a cancer<br />
diagnosis and receiving treatment for it has<br />
been shown to negatively impact sexual<br />
functioning and satisfaction (Moreno et<br />
al., 2012). There is a lack of research into<br />
whether living with HNC may influence<br />
sexuality which is surprising due to the<br />
loss of function that can accompany in<br />
HNC, particularly in surgically invasive<br />
treatments such as a partial or total<br />
laryngectomy (Rhoten et al., 2013; Singer et<br />
al., 2008). The impact of loss of/alteration to<br />
physical functioning could have especially<br />
heightened implications in HNC due<br />
to the significance of the affected areas<br />
to sexual identity, such as the ability to<br />
communicate with others (Rhoten et<br />
al., 2013) and the influence physical and<br />
psychological changes can have on levels<br />
of distress (McCabe-White et al., <strong>2021</strong>).<br />
HNC may also provide specific functional<br />
challenges related to sexuality, such as the<br />
loss/reduction of lip and tongue function<br />
following particular types of HNC which<br />
could impact on kissing, sexual arousal<br />
and ability to perform oral sex (Rogers et<br />
al., 2014). Other functional disturbances<br />
can occur such as fatigue, difficulties with<br />
eating, sight and smell and problems with<br />
achieving a desired facial expression when<br />
communicating non-verbally (Rhoten,<br />
2016). These changes can be experienced as<br />
aversive and embarrassing by the patient,<br />
leading them to socially withdraw from<br />
other or cope in ways that could impact on<br />
their health e.g. engaging in risky sexual<br />
activity, meaning that the ability to create<br />
new intimate relationships as well as<br />
maintaining current relationships can be<br />
reduced (Rhoten et al., 2013).<br />
Research also suggests that patients do<br />
not always know whether it is appropriate<br />
to ask questions about sex during medical<br />
appointments, suggesting that any<br />
difficulties relating to sexuality are not being<br />
routinely addressed and resolved (Low et<br />
al., 2009). The Holistic Needs Assessment -<br />
which is a short questionnaire that has been<br />
routinely used in practice since 2009 - does<br />
discuss relationship concerns but sex and<br />
sexuality is not explicitly acknowledged.<br />
Research into HNC’s possible impact on<br />
sexuality is particularly important to develop<br />
as more people now survive HNC and more<br />
patients are now diagnosed with HNC at<br />
younger ages. This is significant as these<br />
patients may live for a longer time than<br />
patients with HNC have previously, meaning<br />
that concerns around sexuality may be of<br />
increased concern.<br />
What is the project and what are its aims?<br />
The project consisted of a mixed-methods sequential explanatory design with a<br />
quantitative online survey phase first, followed by a qualitative semi-structured<br />
interview phase.<br />
The primary aim of the study was to investigate the impact of HNC on sexuality in terms<br />
of sexual function, satisfaction, identity, and relationships. A secondary aim was to assess<br />
whether psychological flexibility and other coping responses predict sexuality and quality<br />
of life in the context of HNC – and whether psychological flexibility and other coping<br />
responses moderate the relationship between cancer appraisals and sexuality/QoL<br />
outcomes. A tertiary aim was to explore what the clinical need is for individuals with HNC<br />
in terms of psychological support/care provision around sexuality.<br />
74<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
How is the project progressing?<br />
Regarding recruitment, 58 participants took part in the online survey<br />
stage and 18 participants attended a semi-structured interview. The<br />
data that has resulted from this is in the process of being analysed.<br />
If you have experienced <strong>Head</strong><br />
and <strong>Neck</strong> <strong>Cancer</strong>, it is still possible<br />
to take part in this survey by<br />
accessing the below link or<br />
scanning the QR code:<br />
During the course of this research, we have<br />
published a Systematic Literature Review in<br />
Psycho-Oncology entitled ‘Factors associated<br />
with psychological distress for couples facing<br />
head and neck cancer: A systematic literature<br />
review’. This research identified multiple factors<br />
associated with psychological distress for<br />
couples facing HNC. The strongest correlates<br />
for distress were psychological factors such as<br />
coping responses.<br />
What’s next?<br />
Following data analysis, I will be writing up my<br />
thesis for submission in February, following<br />
which we aim to publish the results in a<br />
peer-reviewed journal. I will then speak at the<br />
International <strong>Head</strong> and <strong>Neck</strong> <strong>Cancer</strong> <strong>Conference</strong><br />
2022 to share the results of my research.<br />
References are available on request.<br />
By Linda McCabe, Dr. Anna<br />
Tickle, Dr. Nima Moghaddam,<br />
and Dr. Sanchia Biswas<br />
75
76<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
77
A new chapter for<br />
Oracle <strong>Cancer</strong> Trust<br />
Oracle <strong>Cancer</strong> Trust is the UK’s leading national charity dedicated<br />
to funding pioneering research into head and neck cancer which<br />
is now, as many of you know, one of the fastest growing cancer<br />
types in the UK and the sixth most common form of cancer<br />
worldwide. There is also growing awareness of the prevalence<br />
of these cancers in younger populations. This is being seen in<br />
laryngeal cancer areas as well as in HPV-related oral cancers.<br />
‘Today HPV related oral cancers account for up<br />
to 70% of oral cancer cases.’<br />
And the last two years haven’t helped. Speaking to<br />
ocologists, surgeons and other medical practitioners<br />
there seem to be higher levels of late stage diagnosis<br />
and this alongside a significant slow down in cancer<br />
research. <strong>Head</strong> and neck cancer remains one of the<br />
most poorly funded cancers and receives almost 50%<br />
less research funding compared to breast cancer.<br />
So there is more work than ever for charities like<br />
Oracle, The Swallows and others to achieve. Taking<br />
up the helm of this challenge at Oracle is new CEO,<br />
Tamara Kahn. “I’m really pleased to be joining Oracle<br />
and helping to grow understanding and awareness<br />
of head & neck cancers. I really think that Oracle<br />
<strong>Cancer</strong> Trust’s history of funding high potential<br />
medical research projects is remarkable and I hope<br />
that we can continue to fund key diagnosis and<br />
treatment research projects. I also think that there is<br />
an opportunity for us to do more to bring together<br />
the patient, research and medical communities and<br />
to raise awareness of diagnosis and best practice<br />
treatment options. Ensuring that all patients have<br />
equal access and outcomes is something we want<br />
to strive for. And key to this is working with other<br />
organisations who have similar objectives and a<br />
common purpose and I see The Swallows <strong>Head</strong> &<br />
<strong>Neck</strong> <strong>Cancer</strong> Support Group as a key partner.<br />
78<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
“It has been a very<br />
challenging two years for<br />
our community but by<br />
working closely I am sure we<br />
can both better understand<br />
needs and raise critically needed funds.”<br />
Oracle’s primary role in that is focusing on providing financial and operational<br />
support that allows for the discovery of newer and kinder treatments by funding<br />
the riskier but high potential early-stage research. Without this early-stage<br />
research new discoveries simply wouldn’t happen. Oracle has<br />
funded research at some of the UK’s leading scientific research<br />
institutions including The Institute of <strong>Cancer</strong> Research, Bart’s/<br />
Queen Mary’s University, Newcastle University, The Royal Marsden<br />
Hospital, Brunel University and The University of Sunderland.<br />
Over the past twenty years Oracle has invested over £10m<br />
in research funding and made notable breakthroughs in<br />
discovering immunotherapy treatments, advances in radiotherapy<br />
techniques, drug development, speech, preserving swallowing<br />
and taste following radiotherapy as well as numerous studies<br />
on imaging and quality of life studies. And a lot of this research<br />
has contributed directly and indirectly to greater understanding<br />
and personalised approaches to treatment so that patients can<br />
hopefully have fewer treatment related side-effects and continue<br />
to get access to newer and kinder treatments.<br />
As stated above, we really are more than ever looking to engage with our wider head and<br />
neck cancer community, including supporters, scientists, partners, other charities and support<br />
organisations helping head and neck cancer patients, medical practitioners and corporate<br />
partners. Tamara and the Oracle <strong>Cancer</strong> Trust team would be delighted to meet if you have<br />
time so please get in touch.<br />
ceo@oraclecancertrust.org. | www.oraclecancertrust.org<br />
79
Did you ever feel like your HME filter was too noticeable?<br />
Kapitex understands that life isn’t all about your Laryngectomy stoma, you<br />
need a product which gives you the confidence to protect the airway in the<br />
most discrete way possible.<br />
PHONIQ® Low Profile HME<br />
The slim design of the Low Profile HME filter makes it less<br />
noticeable on the neckline. The filter fits securely into the<br />
PHONIQ® baseplate, laryngectomy tube or stoma button<br />
ring without protruding over the top and provides the<br />
performance data to match the PHONIQ® DigiClose<br />
HME range.<br />
LAPFT0005 PHONIQ Low Profile HME 30<br />
PHONIQ® Low Profile Shower Shield<br />
With a clear lightweight polycarbonate casing that<br />
snaps into place for a secure fit to the PHONIQ®<br />
Low Profile HME Filter.<br />
LAPPB0002 PHONIQ Low Profile Shower Shield 2<br />
Lower the profile, not the<br />
performance!<br />
For a no obligation free trial please email sales@kapitex.com<br />
80<br />
www.kapitex.com<br />
Kapitex Healthcare Ltd, Unit 1, Erivan Park, Sandbeck Way,<br />
WestYorkshire, LS22 7DN Tel: 01937 580211 Email: sales@kapitex.com<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Our<br />
charity<br />
shop needs<br />
your donations<br />
We are always in need of:<br />
Find us at:<br />
The Michael Stenhouse<br />
Centre, 68-70 Waterloo<br />
Road, South Shore,<br />
Blackpool, FY4 1AB<br />
Call us on: 01253 428 940<br />
or email: info@theswallows.org.uk<br />
Drop off items in the shop, or our<br />
dedicated free parking area at the rear of the shop<br />
Clothing<br />
Furniture<br />
Bric-a-brac<br />
Household<br />
Toys<br />
Most items accepted<br />
24/7 Patient and Carer support line service: 07504 725 059<br />
81<br />
www.theswallows.org.uk
BRIDGING THE GAP <<br />
The Swallows<br />
<strong>Head</strong> & <strong>Neck</strong> <strong>Cancer</strong> Charity<br />
YOUR<br />
HOSPITAL<br />
TEAM<br />
PATIENT<br />
& CAREGIVER<br />
AT HOME<br />
> 24/7 support line<br />
> Monthly Meetings<br />
> Support Boxes<br />
> Voice Banking<br />
Our 24/7 support line:<br />
Email: info@theswallows.org.uk<br />
82 VIRTUAL www.theswallows.org.uk<br />
HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Centre for Regenerative Medicine<br />
‘Virtual’ Behind-the-Scenes Tour<br />
Have you ever wondered what happens inside a research laboratory?<br />
Who are the people working on new treatments for head and neck cancer?<br />
Meet members of Dr Elaine Emmerson’s research team who will take you on a<br />
special behind the scenes virtual tour of the Centre for Regenerative Medicine,<br />
a world leading medical research facility based at the University of Edinburgh.<br />
Elaine’s lab are researching ways to regenerate salivary<br />
glands (regrow and restore function), following damage<br />
caused by radiotherapy. Their hope is to develop a new<br />
treatment for head and neck cancer patients who are<br />
suffering from chronic dry mouth.<br />
Hear more about the ground-breaking research happening<br />
within the laboratory and get to know the scientists working<br />
behind the scenes.<br />
Dr Elaine Emmerson<br />
Wednesday 4 November, 15:30 – 16:30<br />
Further information contact: Dr Elaine Emmerson, The Centre for Regenerative Medicine, Institute<br />
for Regeneration and Repair, The University of Edinburgh, Edinburgh BioQuarter, 5 Little France Drive,<br />
Register: https://regenerativemedicineroom.eventbrite.co.uk<br />
Edinburgh, EH16 4UU | email: elaine.emmerson@ed.ac.uk<br />
83
•Soothes pain 1<br />
•Reduces the incidence of<br />
moist desquamation (MD) 2<br />
Apply from Day 1<br />
Soothes & cools the skin<br />
Non-sticky<br />
Easy to apply<br />
www.flenhealth.co.uk<br />
Scan here for more info<br />
Reference<br />
1. Korting HC, Schollmann C, White RJ. Management of minor acute cutaneous wounds: importance<br />
of wound healing in a moist environment. Journal of the European Academy of Dermatology and<br />
Venereology : JEADV. 2011;25(2):130-7<br />
2. Censabella S, Claes S, Orlandini M et al (2017) Efficacy of a hydroactive colloid gel versus historical<br />
controls for the prevention of radiotherapy-induced moist desquamation in breast cancer patients.<br />
Eu Jnl0ncNsg 29:1-7<br />
84<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Sarah’s Story<br />
“Being told that one has <strong>Cancer</strong> is not much fun, and when I was diagnosed nearly 18<br />
months ago it was inevitably a shock. This was compounded by the certainty of an<br />
operation (double mastectomy), possibility of chemotherapy and almost certainty of<br />
Radiotherapy.<br />
The Chemo I escaped, the operation went well, but it was the anticipation of the<br />
Radiotherapy which, for me, presented the worst fears. It was not a fear of ‘nuclear<br />
medicine’, it was the side-effects: I was almost promised these...blistering, weeping skin,<br />
bright red and extremely itchy patches around the treated areas.<br />
It was just before I started Radiotherapy, however, that I was introduced to someone who<br />
had travelled an identical path to mine, and she swore by Flamigel RT. It was prescription<br />
only and our GP, himself a ‘skin man’, agreed that Flamigel RT was the route to take. About<br />
four days into my Radiotherapy I switched from E45 to Flamigel RT. And I have not looked<br />
back...<br />
I have had NONE of the promised nasties, no weeping skin, no blistering effects like<br />
sunburn. Yes, three weeks after I finished treatment two angry red patches appeared<br />
around my collar bone but they only itch a tiny bit, easily soothed by a quick application of<br />
Flamigel, and I expect them to go away soon. Most importantly, of course, it WORKS and I<br />
had none of the miseries that I had anticipated.<br />
I sincerely hope that Flamigel RT will soon be widely and easily available to ALL those<br />
unfortunate enough to have to undergo the rigours of Radiotherapy.”<br />
Sarah Rendall<br />
For Radiotherapy Induced Dermatitus<br />
•Soothes pain 1<br />
•Reduces the incidence of<br />
moist desquamation (MD) 2<br />
Scan here for more info<br />
Reference<br />
1. Korting HC, Schollmann C, White RJ. Management of minor acute cutaneous wounds: importance of<br />
wound healing in a moist environment. Journal of the European Academy of Dermatology and<br />
Venereology : JEADV. 2011;25(2):130-7<br />
2. Censabella S, Claes S, Orlandini M et al (2017) Efficacy of a hydroactive colloid gel versus historical<br />
controls for the prevention of radiotherapy-induced moist desquamation in breast cancer patients. Eu<br />
Jnl0ncNsg 29:1-7<br />
Apply from Day 1<br />
Soothes & cools the skin<br />
Non-sticky<br />
Easy to apply<br />
85
Coping with<br />
Dry Mouth<br />
for <strong>Head</strong> & <strong>Neck</strong><br />
<strong>Cancer</strong> Patients<br />
Living with<br />
dry mouth<br />
Dry mouth is one of the most<br />
common complications during<br />
and after radiotherapy for<br />
head and neck cancer, and<br />
it is important to understand<br />
how to keep on top of your<br />
oral health to avoid further<br />
complications.<br />
Radiotherapy or<br />
chemotherapy to the head<br />
and neck can damage your<br />
salivary glands, causing a dry<br />
mouth. Your salivary glands<br />
may gradually recover but it<br />
can take 6 months or even<br />
longer to start noticing an<br />
improvement.<br />
If your mouth is dry from<br />
treatment you may notice<br />
some of the following<br />
ORALIEVEsymptoms:<br />
A need to drink water<br />
which can lead to frequent<br />
urination and interrupted<br />
sleep<br />
Increased tooth decay or<br />
bleeding gums<br />
Difficulty in tasting and<br />
swallowing food<br />
Cracked or chapped lips<br />
Bad breath or a rough<br />
tongue<br />
A sore or sensitive mouth<br />
Thick, viscous, sticky saliva<br />
86<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
Why water alone<br />
isn’t enough<br />
One of the most frequently<br />
used saliva substitutes is water.<br />
Water can be used as a saliva<br />
replacement however, it does<br />
not moisten, lubricate and<br />
replace what your mouth has<br />
lost after undergoing head and<br />
neck cancer treatment.<br />
Furthermore, it has been<br />
reported that patients who<br />
compensate through frequent<br />
sips of water often show a<br />
decrease in sleep quality due<br />
to the increased frequency<br />
of urination.<br />
The importance of saliva<br />
It helps protect your teeth<br />
from the acids and sugars<br />
in your diet, helping to<br />
prevent tooth decay<br />
It helps remove bacteria<br />
and residual food from<br />
your mouth which can<br />
cause tooth decay and<br />
gum disease by flushing<br />
it into the gut<br />
The anti-microbial<br />
mechanisms help to<br />
control the balance of<br />
bacteria in the mouth<br />
It helps keep the tissues of<br />
your mouth including your<br />
tongue, lips, cheeks and<br />
gums healthy<br />
It helps you to swallow<br />
and digest food and even<br />
facilitates taste<br />
87
Top tips for dry mouth<br />
Add ice to drinks or try sucking ice<br />
cubes to soothe a dry mouth<br />
Consider the use of a<br />
moisturising gel or spray<br />
You may find eating cold food<br />
more soothing than hot food<br />
Avoid very dry foods, which can<br />
stick to the top of your mouth<br />
ORALIVE<br />
Keep food moist with gravies<br />
and sauces to aid swallowing<br />
If your mouth is sore avoid salty<br />
or spicy food that may sting, or<br />
rough-textured food such as toast<br />
Clean your mouth after eating with<br />
a soft brush and a mild toothpaste<br />
and choose an alcohol free fluoride<br />
mouthwash with a mild flavour to<br />
aid with cleansing<br />
If you wear dentures remove them<br />
for as long as you can at night<br />
and clean them with a specialist<br />
cleanser<br />
88<br />
Tell your doctor or pharmacist about your dry mouth and<br />
ask your dentist for oral health advice<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
ORALIEVE<br />
relief range<br />
comfort range<br />
To find out more about<br />
Oralieve and their dry mouth<br />
product range, visit:<br />
www.oralieve.co.uk<br />
89
Look, listen<br />
and observe with the elderly<br />
It is suspected that <strong>Cancer</strong> referrals during the pandemic in 2020 fell by 350,000 compared to 2019 (Lancet<br />
<strong>2021</strong>), indeed one of England’s biggest NHS Trusts reports that mouth cancer referrals have fallen by 65%<br />
since the beginning of the lockdown. (Dentistry <strong>2021</strong>). The pandemic was a challenging time for many, but<br />
the elderly and the people who care for them faced many challenges. With many residential homes being<br />
forced into complete lockdown, access to healthcare support often proved difficult due to the sheer pressure<br />
the system was under. As <strong>Cancer</strong> Research UK reports that the peak rate in <strong>Head</strong> and <strong>Neck</strong> cancers<br />
in 2018-2019 was in the 70-74 age group, it therefore makes it essential that assessing and checking for<br />
mouth cancers in the elderly age group a priority.<br />
This however has its own challenges as there are currently 850,000 people in the UK with Dementia.<br />
Alzheimer UK reports that 7.1% of all people over the age of 65 years have Dementia.<br />
It is essential to maintain good oral hygiene for people living with Dementia as it can impact on their overall<br />
well-being. By carrying out daily care this can help prevent problems like painful cavities and infections,<br />
which can cause pain and issues with eating, drinking and communicating. (Dementia UK)<br />
People living with dementia are susceptible to a high rate of tooth decay and gum disease. One reason for<br />
this is as the dementia progresses, they may find it challenging to perform day to day basic activities and<br />
perform oral care. Oral issues can get left untreated as the individual may find it difficult to express that<br />
they have a tooth ache or pain.<br />
Each and every person is entitled to a clean mouth. It is important that the person living with dementia<br />
is supported with oral care and when needed ensure mouth care is continued when they are unable or<br />
reluctant to do it for themselves. (Dementia UK)<br />
• Each person should have their natural teeth brushed at least twice a day.<br />
• Try and use the cleaning products they are used too, however consider<br />
a foam free toothpaste as the person may not be able to swallow or spit<br />
out.<br />
• Use the residents choice of toothbrush, this may even be an electric<br />
toothbrush. As the dementia progresses it may be useful to change to<br />
a small headed toothbrush for easier access.<br />
• Cleaning denture by manually brushing and removing food debris.<br />
Remove dentures at night.<br />
(Mouth <strong>Cancer</strong> Foundation)<br />
Providing basic mouth care for this group of individuals can in some cases prove be extremely difficult as<br />
the dementia progresses, in some case people close their lips, move their head, clench their teeth together<br />
and sometimes even bite. There are many tips and advice around providing mouth care for challenging<br />
individuals, for example, giving short and clear instructions, the “watch me” technique (Alzheimer’s Association)<br />
or use a distraction technique (BGS)<br />
All residents in a care setting should have an oral health assessment when they first move into their home,<br />
this involves input from family and friends who have previously cared for the individual. This information is<br />
recorded in the care plan and is vital as it helps keeping on top of any changes.<br />
90<br />
VIRTUAL HEAD & NECK CANCER CONFERENCE <strong>2021</strong>
How to spot changes in the mouth in the elderly<br />
smell<br />
listen<br />
look<br />
Have you noticed any bad odour coming from the mouth?<br />
Have you noticed a change in the sound of their voice?<br />
A sore throat or a cough that isn’t clearing up? Has the<br />
resident complained that they feel something is stuck<br />
in their throat?<br />
Have a close look at the resident’s whole face and throat.<br />
Have you noticed any bumps, unusual lumps, changes<br />
in marks on the skin, moles that have changed in size<br />
or colour, any red or white patches or ulcers inside the<br />
mouth? Have the dentures unexpectable become looser<br />
or ill fitting?<br />
observe<br />
Have you noticed a change in the resident’s<br />
behaviour? Drooling from the mouth,<br />
unexplained weight loss, problems with eating?<br />
It is vitally important that the carer observer a resident and notices any changes in their behaviour, even<br />
some small change can be an important sign. There should be a documented referral pathway so that<br />
carers can report any concerns and then refer to the dental and hospital team as soon as possible. It is<br />
important to stress even noticing a small change can mean addressing any problem early and hopefully<br />
saving a life.<br />
Mouth cancer does not discriminate and will visit the elderly and people living with such conditions as<br />
dementia. It is therefore essential that effective oral care and assessing the oral condition of the individual<br />
is embedded into their care and care plan. This is also important for people living in their own homes with<br />
support from family and carers. It is therefore crucial that staff, carers and family members are offered<br />
support around spotting any potential issues and how to act on this.<br />
Written by<br />
Emma Riley<br />
Healthcare Services Director<br />
at RIS Products<br />
www.ris.healthcare.co.uk<br />
91