Gastroenterology Today Spring 2022
Gastroenterology Today Spring 2022
Gastroenterology Today Spring 2022
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
NEWS<br />
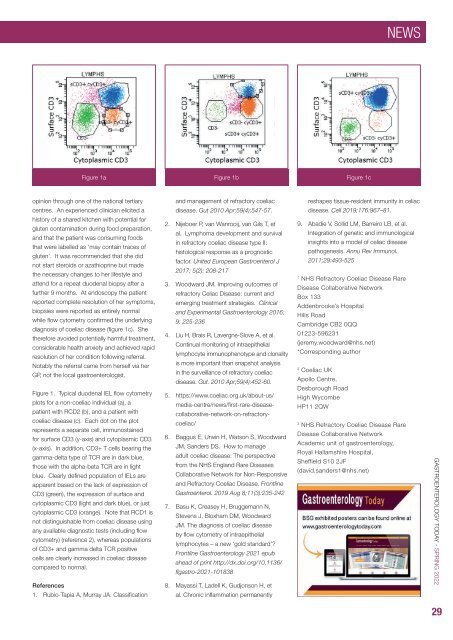
Figure 1a Figure 1b Figure 1c<br />
opinion through one of the national tertiary<br />
centres. An experienced clinician elicited a<br />
history of a shared kitchen with potential for<br />
gluten contamination during food preparation,<br />
and that the patient was consuming foods<br />
that were labelled as ‘may contain traces of<br />
gluten’. It was recommended that she did<br />
not start steroids or azathioprine but made<br />
the necessary changes to her lifestyle and<br />
attend for a repeat duodenal biopsy after a<br />
further 9 months. At endoscopy the patient<br />
reported complete resolution of her symptoms,<br />
biopsies were reported as entirely normal<br />
while flow cytometry confirmed the underlying<br />
diagnosis of coeliac disease (figure 1c). She<br />
therefore avoided potentially harmful treatment,<br />
considerable health anxiety and achieved rapid<br />
resolution of her condition following referral.<br />
Notably the referral came from herself via her<br />
GP, not the local gastroenterologist.<br />
Figure 1. Typical duodenal IEL flow cytometry<br />
plots for a non-coeliac individual (a), a<br />
patient with RCD2 (b), and a patient with<br />
coeliac disease (c). Each dot on the plot<br />
represents a separate cell, immunostained<br />
for surface CD3 (y-axis) and cytoplasmic CD3<br />
(x-axis). In addition, CD3+ T cells bearing the<br />
gamma-delta type of TCR are in dark blue,<br />
those with the alpha-beta TCR are in light<br />
blue. Clearly defined population of IELs are<br />
apparent based on the lack of expression of<br />
CD3 (green), the expression of surface and<br />
cytoplasmic CD3 (light and dark blue), or just<br />
cytoplasmic CD3 (orange). Note that RCD1 is<br />
not distinguishable from coeliac disease using<br />
any available diagnostic tests (including flow<br />
cytometry) (reference 2), whereas populations<br />
of CD3+ and gamma delta TCR positive<br />
cells are clearly increased in coeliac disease<br />
compared to normal.<br />
References<br />
1. Rubio-Tapia A, Murray JA. Classification<br />
and management of refractory coeliac<br />
disease. Gut 2010 Apr;59(4):547-57.<br />
2. Nijeboer P, van Wanrooij, van Gils T, et<br />
al. Lymphoma development and survival<br />
in refractory coeliac disease type II:<br />
histological response as a prognostic<br />
factor. United European Gastroenterol J<br />
2017; 5(2): 208-217<br />
3. Woodward JM. Improving outcomes of<br />
refractory Celiac Disease: current and<br />
emerging treatment strategies. Clinical<br />
and Experimental <strong>Gastroenterology</strong> 2016;<br />
9: 225-236<br />
4. Liu H, Brais R, Lavergne-Slove A, et al.<br />
Continual monitoring of intraepithelial<br />
lymphocyte immunophenotype and clonality<br />
is more important than snapshot analysis<br />
in the surveillance of refractory coeliac<br />
disease. Gut. 2010 Apr;59(4):452-60.<br />
5. https://www.coeliac.org.uk/about-us/<br />
media-centre/news/first-rare-diseasecollaborative-network-on-refractorycoeliac/<br />
6. Baggus E, Urwin H, Watson S, Woodward<br />
JM, Sanders DS. How to manage<br />
adult coeliac disease: The perspective<br />
from the NHS England Rare Diseases<br />
Collaborative Network for Non-Responsive<br />
and Refractory Coeliac Disease. Frontline<br />
Gastroenterol. 2019 Aug 8;11(3):235-242<br />
7. Basu K, Creasey H, Bruggemann N,<br />
Stevens J, Bloxham DM, Woodward<br />
JM. The diagnosis of coeliac disease<br />
by flow cytometry of intraepithelial<br />
lymphocytes – a new ‘gold standard’?<br />
Frontline <strong>Gastroenterology</strong> 2021 epub<br />
ahead of print http://dx.doi.org/10.1136/<br />
flgastro-2021-101838<br />
8. Mayassi T, Ladell K, Gudjonson H, et<br />
al. Chronic inflammation permanently<br />
reshapes tissue-resident immunity in celiac<br />
disease. Cell 2019;176:967–81.<br />
9. Abadie V, Sollid LM, Barreiro LB, et al.<br />
Integration of genetic and immunological<br />
insights into a model of celiac disease<br />
pathogenesis. Annu Rev Immunol.<br />
2011;29:493-525<br />
1<br />
NHS Refractory Coeliac Disease Rare<br />
Disease Collaborative Network<br />
Box 133<br />
Addenbrooke’s Hospital<br />
Hills Road<br />
Cambridge CB2 0QQ<br />
01223-596231<br />
(jeremy.woodward@nhs.net)<br />
*Corresponding author<br />
2<br />
Coeliac UK<br />
Apollo Centre,<br />
Desborough Road<br />
High Wycombe<br />
HP11 2QW<br />
3<br />
NHS Refractory Coeliac Disease Rare<br />
Disease Collaborative Network<br />
Academic unit of gastroenterology,<br />
Royal Hallamshire Hospital,<br />
Sheffield S10 2JF<br />
(david.sanders1@nhs.net)<br />
GASTROENTEROLOGY TODAY - SPRING <strong>2022</strong><br />
29