Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume 38 No. 4<br />
<strong>August</strong> <strong>2023</strong><br />
DEDICATED TO THE AMBULANCE SERVICE AND ITS SUPPLIERS<br />
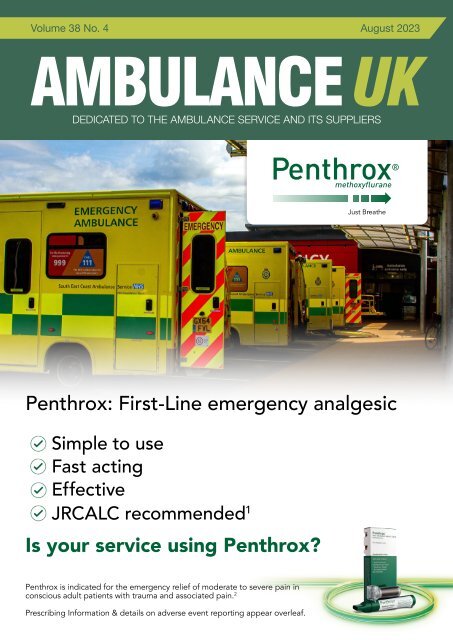
Penthrox: First-Line emergency analgesic<br />
Simple to use<br />
Fast acting<br />
Effective<br />
JRCALC recommended 1<br />
Is your service using Penthrox?<br />
Penthrox is indicated for the emergency relief of moderate to severe pain in<br />
conscious adult patients with trauma and associated pain. 2<br />
Prescribing Information & details on adverse event reporting appear overleaf.
QUESTIONS?<br />
PENTHROX 99.9%, 3 ml inhalation vapour, liquid (methoxyflurane): Please refer to the Summary<br />
of Product Characteristics (SmPC) before prescribing. Abbreviated Prescribing Information.<br />
Presentation: Each bottle of PENTHROX contains 3 ml of methoxyflurane 99.9%, a clear, almost<br />
colourless, volatile liquid, with a characteristic fruity odour. Each PENTHROX combination pack<br />
consists of one bottle of 3 ml PENTHROX, one PENTHROX Inhaler and one Activated Carbon (AC)<br />
chamber. Indications: Emergency relief of moderate to severe pain in conscious adult patients with<br />
trauma and associated pain. Dosage and administration: PENTHROX should be self-administered<br />
under supervision of a person trained in its administration, using the hand held PENTHROX Inhaler. It<br />
is inhaled through the custom-built PENTHROX inhaler. Adults: One bottle of 3 ml PENTHROX as a<br />
single dose, administered using the device provided. A second bottle should only be used where<br />
needed. The frequency at which PENTHROX can be safely used is not established. The following<br />
administration schedule is recommended: no more than 6 ml in a single day, administration on<br />
consecutive days is not recommended and the total dose to a patient in a week should not exceed 15<br />
ml. Onset of pain relief is rapid and occurs after 6-10 inhalations. Patients are able to titrate the amount<br />
of PENTHROX inhaled and should be instructed to inhale intermittently to achieve adequate analgesia.<br />
Continuous inhalation of a bottle containing 3 ml provides analgesic relief for up to 25-30 minutes;<br />
intermittent inhalation may provide longer analgesic relief. Patients should be advised to use the<br />
lowest possible dose to achieve pain relief. Renal impairment: Methoxyflurane may cause renal failure<br />
if the recommended dose is exceeded. Caution should be exercised for patients diagnosed with<br />
clinical conditions that would pre-dispose to renal injury. Hepatic impairment: Cautious clinical<br />
judgement should be exercised when PENTHROX is to be used more frequently than on one occasion<br />
every 3 months. Paediatric population: PENTHROX should not be used in children and adolescents<br />
under 18 years. For detailed information on the method of administration refer to the SmPC.<br />
Contraindications: Use as an anaesthetic agent. Hypersensitivity to methoxyflurane, any fluorinated<br />
anaesthetic or to any of the excipients. Patients who are known to be or genetically susceptible to<br />
malignant hyperthermia. Patients or patients with a known family history of severe adverse reactions<br />
after being administered with inhaled anaesthetics. Patients who have a history of showing signs of<br />
liver damage after previous methoxyflurane use or halogenated hydrocarbon anaesthesia. Clinically<br />
significant renal impairment. Altered level of consciousness due to any cause including head injury,<br />
drugs or alcohol. Clinically evident cardiovascular instability. Clinically evident respiratory depression.<br />
Warnings and Precautions: To ensure the safe use of PENTHROX as an analgesic the lowest effective<br />
dose to control pain should be used and it should be used with caution in the elderly or other patients<br />
with known risk factors for renal disease, and in patients diagnosed with clinical conditions which may<br />
pre-dispose to renal injury. Methoxyflurane causes significant nephrotoxicity at high doses.<br />
Nephrotoxicity is thought to be associated with inorganic fluoride ions, a metabolic breakdown<br />
product. When administered as instructed for the analgesic indication, a single dose of 3 ml<br />
methoxyflurane produces serum levels of inorganic fluoride ions below 10 micromol/l. In the past<br />
when used as an anaesthetic agent, methoxyflurane at high doses caused significant nephrotoxicity,<br />
which was determined to occur at serum levels of inorganic fluoride ions greater than 40 micromol/l.<br />
Nephrotoxicity is also related to the rate of metabolism. Factors that increase the rate of metabolism<br />
such as drugs that induce hepatic enzymes can increase the risk of toxicity with methoxyflurane as well<br />
as sub-groups of people with genetic variations that may result in fast metaboliser status.<br />
Methoxyflurane is metabolised in the liver, therefore increased exposures in patients with hepatic<br />
impairment can cause toxicity. PENTHROX should be used with care in patients with underlying<br />
hepatic conditions or with risks for hepatic dysfunction. Previous exposure to halogenated hydrocarbon<br />
anaesthetics (including methoxyflurane when used as an anaesthetic agent), especially if the interval<br />
is less than 3 months, may increase the potential for hepatic injury. Potential effects on blood pressure<br />
and heart rate are known class-effects of high-dose methoxyflurane used in anaesthesia and other<br />
anaesthetics. Caution is required with use in the elderly due to possible reduction in blood pressure.<br />
Potential CNS effects such as sedation, euphoria, amnesia, ability to concentrate, altered sensorimotor<br />
co-ordination and change in mood are known class-effects. The possibility of CNS effects may be<br />
seen as a risk factor for potential abuse, however reports are very rare in post-marketing use.<br />
Respiratory depression has also been reported with analgesic doses. Respiration should be monitored<br />
due to the risk of respiratory depression and hypoxia. PENTHROX is not appropriate for providing<br />
relief of break-through pain/exacerbations in chronic pain conditions or for the relief of trauma related<br />
pain in closely repeated episodes for the same patient. PENTHROX contains the excipient, butylated<br />
Adverse events should be reported. Reporting forms and information can be found at www.mhra.gov.uk/yellowcard. Adverse events should also be reported to Galen Limited on<br />
028 3833 4974 and select the customer services option, or e-mail customer.services@galen-pharma.com. Medical information enquiries should also be directed to Galen Limited.<br />
Before administering PENTHROX, make sure you have read and fully understood the SmPC and educational materials, which provide important information about how to safely use<br />
the device to minimise risk of serious side effects. PENTHROX educational materials and training on its administration are available from Galen on request.<br />
References: 1. JRCALC Guidelines. Available at: https://www.jrcalc.org.uk/guidelines/ 2. Penthrox <strong>UK</strong> Summary of Product Characteristics. March <strong>2023</strong><br />
MAT-PEN-<strong>UK</strong>-000719 Date of preparation: July <strong>2023</strong><br />
www.penthrox.co.uk/<br />
healthcare/contact<br />
or scan the QR code above.<br />
hydroxytoluene (E321) which may cause local skin reactions (e.g. contact dermatitis), or irritation to the<br />
eyes and mucous membranes. To reduce occupational exposure to methoxyflurane, the PENTHROX<br />
Inhaler should always be used with the AC Chamber which adsorbs exhaled methoxyflurane. Multiple<br />
use of PENTHROX Inhaler without the AC Chamber creates additional risk. Elevation of liver enzymes,<br />
blood urea nitrogen and serum uric acid have been reported in exposed maternity ward staff when<br />
methoxyflurane was used in the past at the time of labour and delivery. There have been reports of<br />
non-serious and transient reactions such as dizziness, headache, nausea or malaise, and reports of<br />
hypersensitivity reactions to methoxyflurane or other ingredients in healthcare professionals exposed<br />
to PENTHROX. Measurements of exposure levels to methoxyflurane in hospital staff showed levels<br />
significantly lower than those associated with nephrotoxicity. Interactions: Methoxyflurane is<br />
metabolised by the CYP 450 enzymes, particularly CYP 2E1, CYP 2B6 and to some extent CYP 2A6. It<br />
is possible that enzyme inducers (such as alcohol or isoniazid for CYP 2E1 and phenobarbital or<br />
rifampicin for CYP 2A6 and carbamazepine, efavirenz, rifampicin or nevirapine for CYP 2B6) which<br />
increase the rate of methoxyflurane metabolism might increase its potential toxicity and they should<br />
be avoided concomitantly with methoxyflurane. Concomitant use of methoxyflurane with medicines<br />
(e.g. contrast agents and some antibiotics) which are known to have a nephrotoxic effect should be<br />
avoided as there may be an additive effect on nephrotoxicity; tetracycline, gentamicin, colistin,<br />
polymyxin B and amphotericin B have known nephrotoxic potential. Sevoflurane anaesthesia should<br />
be avoided following methoxyflurane analgesia, as sevoflurane increases serum fluoride levels and<br />
methoxyflurane nephrotoxicity is associated with raised serum fluoride. Concomitant use of<br />
PENTHROX with CNS depressants, such as opioids, sedatives or hypnotics, general anaesthetics,<br />
phenothiazines, tranquillisers, skeletal muscle relaxants, sedating antihistamines and alcohol may<br />
produce additive depressant effects. If opioids are given concomitantly with PENTHROX, the patient<br />
should be observed closely. When methoxyflurane was used for anaesthesia at the higher doses of<br />
40–60 ml, there were reports of drug interaction with hepatic enzyme inducers (e.g. barbiturates)<br />
increasing metabolism of methoxyflurane and resulting in a few reported cases of nephrotoxicity;<br />
reduction of renal blood flow and hence anticipated enhanced renal effect when used in combination<br />
with drugs (e.g. barbiturates) reducing cardiac output; and class effect on cardiac depression, which<br />
may be enhanced by other cardiac depressant drugs, e.g. intravenous practolol during cardiac<br />
surgery. Fertility, pregnancy and lactation: No clinical data on effects of methoxyflurane on fertility<br />
are available. Studies in animals have shown reproduction toxicity. As with all medicines care should<br />
be exercised when administered during pregnancy especially the first trimester. There is insufficient<br />
information on the excretion of methoxyflurane in human milk. Caution should be exercised when<br />
methoxyflurane is administered to a nursing mother. Effects on ability to drive and use machines:<br />
Methoxyflurane may have a minor influence on the ability to drive and use machines. Patients should<br />
be advised not to drive or operate machinery if they are feeling drowsy or dizzy. Undesirable effects:<br />
The common non-serious reactions are CNS type reactions such as dizziness and somnolence and are<br />
generally easily reversible. Serious dose-related nephrotoxicity has only been associated with<br />
methoxyflurane when used in large doses over prolonged periods during general anaesthesia. The<br />
following adverse drug reactions have either been observed in PENTHROX clinical trials in analgesia,<br />
with analgesic use of methoxyflurane following post-marketing experience or are linked to<br />
methoxyflurane use in analgesia found in post-marketing experience and in scientific literature (refer<br />
to the SmPC for further details): Very common (≥1/10): dizziness; common (≥1/100 to
CONTENTS<br />
CONTENTS<br />
<strong>Ambulance</strong> <strong>UK</strong><br />
4 EDITOR’S COMMENT<br />
6 FEATURE<br />
6 NINE GOLDEN CODES: IMPROVING THE ACCURACY<br />
OF HELICOPTER EMERGENCY MEDICAL SERVICES<br />
(HEMS) DISPATCH—A RETROSPECTIVE,<br />
MULTI‐ORGANISATIONAL STUDY IN THE EAST<br />
OF ENGLAND<br />
14 NEWSLINE<br />
42 IN PERSON<br />
46 COMPANY NEWS<br />
This issue edited by:<br />
Matt House<br />
c/o Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
ADVERTISING:<br />
Terry Gardner, Samantha Marsh<br />
CIRCULATION:<br />
Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
Tel: 01886 853715<br />
E: info@mediapublishingcompany.com<br />
www.ambulanceukonline.com<br />
PUBLISHED BI-MONTHLY:<br />
February, April, June, <strong>August</strong>,<br />
October, December<br />
COPYRIGHT:<br />
Media Publishing Company<br />
Greenoaks<br />
Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
COVER STORY<br />
VCS Invest in <strong>UK</strong>’s largest dedicated ambulance and police vehicle factory<br />
VCS, the <strong>UK</strong>’s leading manufacturer of emergency services vehicles, have invested more<br />
than £5 million in a new manufacturing facility for ambulances, police, and specialist<br />
vehicle conversions in Bradford. The new factory ensures the <strong>UK</strong>’s supply of world-class<br />
emergency vehicles by creating the country’s largest dedicated manufacturing facility and<br />
trebling VCS’s previous production capacity to nearly 1500 vehicles annually.<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company<br />
Next Issue October <strong>2023</strong><br />
Designed in the <strong>UK</strong> by TGDH<br />
The Bradford-based company, which started with fi ve staff members in 2009, will have<br />
the capacity to grow its workforce to more than 150 owing to the new facility. Meanwhile,<br />
a dedicated training academy within the new site means that the company can recruit<br />
more local people without emergency services sector experience, providing a further<br />
boost to the local community.<br />
The new facility helps future-proof the <strong>UK</strong>’s emergency services fl eet, with a new<br />
dedicated R&D facility that doubles its engineering capability. This builds upon the<br />
company’s reputation for creating the lightest vehicle conversions available – in turn<br />
aiding fuel effi ciency and reducing emissions – without compromising on vehicle quality<br />
and reliability.<br />
This investment follows a period of exceptional growth for VCS, which posted a 30%<br />
increase in turnover over two years. The company currently sits in fi rst place on the<br />
NHS framework for ambulance convertors, while it also plans to target new international<br />
markets in the coming years.<br />
Do you have For anything further recruitment you would vacancies like to add visit: or include? www.ambulanceukonline.com<br />
Please contact us and let us know.<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
3
EDITOR’S COMMENT<br />
EDITOR’S COMMENT<br />
Welcome to this issue of A<strong>UK</strong>.<br />
One of my sons is twenty six. We call him The Boy. He’s had a few jobs in his time, and a few interests have<br />
come and gone, as they do. However, since a very young age, the one constant in his life has been football.<br />
From his early years, he has had a passion for it. Whether that is gaining an encyclopedic knowledge of the<br />
game; playing football consantly on the console, or playing it himself for school and then a local team; it has<br />
been a huge part of his life.<br />
“As time<br />
goes on, and<br />
I become<br />
reflective<br />
on what is<br />
important in life,<br />
I find myself<br />
coming back to<br />
the philosophy<br />
that “you only<br />
get one life to<br />
play football”.<br />
Try it, you may<br />
just find that it<br />
helps you make<br />
one or two<br />
decisions.”<br />
I was discussing some new potential jobs with The Boy recently. The change would have meant better<br />
money and prospects. However, it would also have interferred with his football training and practice nights.<br />
During the conversation he said “Dad, you only get one life to play football”.<br />
I relayed this to some friends last weekend. We were trying to persuade one of them to attend a course<br />
he has been hoping to start for some years. The trouble is, the course is three weeks long, and he was<br />
concerned about taking time off work. There are all the important meetings; the emails that need attention;<br />
and various projects he has a hand in. All of this, he felt, meant he couldn’t take three weeks off work. I told<br />
him about The Boy’s philosophy to football, and said that while not a football course, the same rationale<br />
could be applied.<br />
The work will always be there to prevent you doing things if you let it. It is important to recognise and<br />
understand that. After all, it is that work that inevitably pays the bills and allows you the freedom to do the<br />
other things that you need to do in life. In some ways, ambulance people often see their work as a vocation,<br />
so work does take up a lot of their time and interest even when not actually working. However, we all have<br />
something outside of work that is important to us. That might be family, or some other interest. It’s the thing,<br />
or things, that help make us who we are.<br />
As time goes on, and I become reflective on what is important in life, I find myself coming back to the<br />
philosophy that “you only get one life to play football”. Try it, you may just find that it helps you make one<br />
or two decisions.<br />
Matt House, Co-Editor <strong>Ambulance</strong> <strong>UK</strong><br />
Publishers Statement<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For nearly 40 years, thanks to trade support, we have been able to provide <strong>Ambulance</strong> <strong>UK</strong> FREE<br />
OF CHARGE in the knowledge that those receiving our dedicated bi monthly publication enjoy having<br />
something to read during their free time however, return on investment seems to be the buzz word<br />
amongst <strong>Ambulance</strong> Service Suppliers these days, therefore if you enquire about a product advertised,<br />
please mention <strong>Ambulance</strong> <strong>UK</strong> as it help us confirrm to the trade that we are reaching the right<br />
people and providing advertisers with value for money. In respect of our current edition we would like<br />
to thank the following companies for their support as without their contribution towards our print and<br />
postal costs this issue would not have been published - Bluelight <strong>UK</strong>, DS Medical, Durabook,<br />
Eberspaecher, EVS, Ferno, Galen, IPRS, Medacx, Mer Fleet Services, Ortus, St John W.A.,<br />
Stryker, VCS, Vimpex, Webasto.<br />
Terry Gardner<br />
Publisher<br />
4<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
EVE TR Ventilator<br />
INTENSIVE CARE/TRANSPORT/TRANSFER<br />
Innovators in Ventilation since 1978<br />
Technology made in Germany<br />
Supported in the United Kingdom<br />
EVE-TR innovative transport respiratory system for Neonates, Paediatrics & Adults<br />
Invasive & Non-Invasive ventilation Pressure & Volume modes including SIMV, CMV<br />
DuoPAP, NIV, CPAP/nCPAP & ACV. Electronic Oxygen mixing 21-100%, HiFlow 02 2-60 Lpm<br />
Inbuilt Air turbine, 8 hour continuous use plus ‘hot swap battery packs’ to extend use<br />
Independant of air/power. Integral bed/trolley clamps. Compact, Lightweight<br />
with...Fast ‘safe-start’ ventilation at the press of a button<br />
MEDACX LIMITED • ALEXANDER HOUSE • 60-62 STATION ROAD • HAYLING ISLAND • HAMPSHIRE • PO11 0EL<br />
FS 580431<br />
02392 469737<br />
info@medacx.co.uk<br />
www.medacx.co.uk
FEATURE<br />
NINE GOLDEN CODES: IMPROVING<br />
THE ACCURACY OF HELICOPTER<br />
EMERGENCY MEDICAL SERVICES<br />
(HEMS) DISPATCH—A RETROSPECTIVE,<br />
MULTI‐ORGANISATIONAL STUDY IN<br />
THE EAST OF ENGLAND<br />
Christopher T. Edmunds 1,4 *, Kate Lachowycz 1,4 , Sarah McLachlan 2,3 , Andrew Downes 1 , Andrew Smith 5 ,<br />
Rob Major 1,4 and Edward B. G. Barnard 1,6,7<br />
Scand J Trauma Resusc Emerg Med (<strong>2023</strong>) 31:27 https://doi.org/10.1186/s13049-023-01094-w<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
ORIGINAL RESEARCH<br />
Abstract<br />
Background: Helicopter Emergency Medical Services (HEMS) are a<br />
limited and expensive resource, and should be intelligently tasked. HEMS<br />
dispatch was identified as a key research priority in 2011, with a call to<br />
identify a ‘general set of criteria with the highest discriminating potential’.<br />
However, there have been no published data analyses in the past decade<br />
that specifically address this priority, and this priority has been reaffirmed<br />
in <strong>2023</strong>. The objective of this study was to define the dispatch criteria<br />
available at the time of the initial emergency call with the greatest HEMS<br />
utility using a large, regional, multi-organizational dataset in the <strong>UK</strong>.<br />
Methods: This retrospective observational study utilized dispatch<br />
data from a regional emergency medical service (EMS) and three<br />
HEMS organisations in the East of England, 2016–2019. In a logistic<br />
regression model, Advanced Medical Priority Dispatch System<br />
(AMPDS) codes with ≥ 50 HEMS dispatches in the study period were<br />
compared with the remainder to identify codes with high-levels of<br />
HEMS patient contact and HEMS-level intervention/drug/diagnostic<br />
(HLIDD). The primary outcome was to identify AMPDS codes with a ><br />
10% HEMS dispatch rate of all EMS taskings that would result in 10–20<br />
high-utility HEMS dispatches per 24-h period in the East of England.<br />
Data were analysed in R, and are reported as number (percentage);<br />
significance was p < 0.05.<br />
Results: There were n = 25,491 HEMS dispatches (6400 per year), of<br />
which n = 23,030 (90.3%) had an associated AMPDS code. n = 13,778<br />
(59.8%) of HEMS dispatches resulted in patient contact, and n = 8437<br />
(36.6%) had an HLIDD. 43 AMPDS codes had significantly greater<br />
rates of patient contact and/or HLIDD compared to the reference<br />
group. In an exploratory analysis, a cut-off of ≥ 70% patient contact<br />
rate and/or ≥ 70% HLIDD (with a > 10% HEMS dispatch of all EMS<br />
taskings) resulted in 17 taskings per 24-h period. This definition derived<br />
nine AMPDS codes with high HEMS utility.<br />
Conclusion: We have identified nine ‘golden’ AMPDS codes, available at<br />
the time of initial emergency call, that are associated with high-levels of<br />
whole-system and HEMS utility in the East of England. We propose that<br />
<strong>UK</strong> EMS should consider immediate HEMS dispatch to these codes.<br />
Keywords: Air ambulances, Emergency medical dispatch, Emergency<br />
medical services, Prehospital emergency care.<br />
Background<br />
Physician-staffed prehospital teams have existed for over 50 years.<br />
In 1967, there were 20,000 motor vehicle collision deaths in Germany,<br />
leading to emergency doctors demanding earlier and better treatment<br />
of injured patients. In response, the first Helicopter Emergency Medical<br />
Service (HEMS) ‘Christoph 1’ became operational in Munich in 1970<br />
[1]. Since then, over 2.2 million HEMS missions have taken place in<br />
Germany, and similar physician-staffed HEMS have been developed,<br />
predominantly in Europe and Australasia.<br />
The primary rationale for HEMS is the rapid deployment of a specialist<br />
team over a large geographic area, with the assumption that physicians<br />
working alongside paramedics infer better patient outcomes compared<br />
to paramedics alone. The latter point is multi-factorial, and includes<br />
higher-level decision-making [2, 3], and interventions that are either<br />
physician-level specific or require drugs that legally require their<br />
presence [3–5]; an example in the <strong>UK</strong> is prehospital emergency<br />
anaesthesia (PHEA) [6, 7]. There is contradictory evidence that<br />
physician-staffed teams are associated with better patient outcomes<br />
following trauma [8–14], and out-ofhospital cardiac arrest [15–18].<br />
However, the heterogeneity of systems makes conclusive synthesis of<br />
these data inappropriate, and physician-staffed HEMS remain a key<br />
component of many emergency medical systems (EMS).<br />
HEMS are a limited and expensive resource [19–21]. It is therefore<br />
important to ensure that these teams are intelligently dispatched [22],<br />
which may in time also lead to a better understanding of which patients<br />
6<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
have the greatest likelihood of benefit—these concepts are somewhat<br />
inter-dependent. HEMS dispatch was identified as a key research<br />
priority in 2011, with a call to identify a ‘general set of criteria with the<br />
highest discriminating potential’ [23]. It has again been identified as a key<br />
research priority in <strong>2023</strong> suggesting limited progress in this area over the<br />
last decade [24]. Since 2011, London’s Air <strong>Ambulance</strong> has reported that<br />
call-interrogation and crew request dispatch models were more accurate<br />
for HEMS utilization compared to an immediate dispatch model based<br />
on mechanism of injury. However, this was at the expense of delaying<br />
dispatch [25], which is likely to dilute HEMS benefit. There is also <strong>UK</strong><br />
data that suggests non-clinical dispatchers may improve HEMS dispatch<br />
accuracy when using a bespoke algorithm [21]. However, clinicians in<br />
dispatch systems often undertake additional roles; for example, remote<br />
clinical advice to EMS. Overall, there is a paucity of data that could<br />
be used to increase the accuracy of HEMS dispatch [26, 27], possibly<br />
owing to the intrinsic complexity of these systems.<br />
Therefore, the challenge lies in increasing the accuracy of HEMSappropriate<br />
taskings using information available from the initial<br />
emergency call. The positives of which may include: better patient<br />
outcomes (by reducing under-triage), greater availability of HEMS<br />
for those with the highest chance of benefit (by reducing over-triage)<br />
[28], reducing costs associated with helicopter dispatch [29], and<br />
reducing unnecessary emergency aviation risk to medical teams [30].<br />
The objective of this study was to define the dispatch criteria available<br />
at the time of the initial emergency call with the greatest HEMS utility<br />
using a large, regional, multi-organisational dataset in the <strong>UK</strong>.<br />
Methods<br />
Emergency medical system<br />
The East of England is a 20,000 km2 geographic area, containing a<br />
population of 6.3 million people (June 2021) [31]. The statutory regional<br />
EMS is the East of England <strong>Ambulance</strong> Service NHS Trust (EEAST),<br />
which receives approximately 4000 calls per day, and has been<br />
previously described [18]. EEAST is supported by three HEMS charities<br />
operating from five operational bases: East Anglian Air <strong>Ambulance</strong><br />
(EAAA) [32], Magpas Air <strong>Ambulance</strong> (Magpas) [33], and Essex & Herts<br />
Air <strong>Ambulance</strong> (EHAAT) [34]. The core of each team consists of a<br />
prehospital-trained physician and a critical care paramedic (CCP) with<br />
a minimum of three years’ postgraduate experience and role-specific<br />
training [6]. Occasionally, HEMS resources may be staffed by one or<br />
two CCPs without a physician. During the study period, HEMS teams<br />
typically responded by helicopter during the day and rapid response<br />
vehicle (RRV) at night, during periods of aircraft unavailability, and<br />
when an RRV dispatch was thought to be advantageous.<br />
Dispatch system<br />
EEAST uses the Advanced Medical Priority Dispatch System (AMPDS,<br />
Priority Dispatch Corporation, Salt Lake City, Utah, USA, version<br />
13.3). AMPDS provides a scripted caller interrogation protocol to<br />
prioritise calls and allocate EMS resources to incidents via the linked<br />
ProQA (Priority Dispatch Corp., ProQAv 5.1.1.44) software system.<br />
The data end-point is a ‘number-letternumber’ sequence (AMPDS<br />
code) that describes the category, severity (in reference to the speed<br />
and configuration of EMS response required, A to E), and sub-type<br />
of the incident. For example, a cardiac or respiratory arrest (patient<br />
not breathing) would be coded as ‘09-E-01’; ‘09’ is the AMPDS<br />
code category of ‘cardiac or respiratory arrest’, ‘E’ is a capability of<br />
‘Advanced Life Support and special units’ with a response of ‘hot<br />
(multiple units) plus other first responders’, and the ‘01’ sub-type of<br />
this code refers to ‘not breathing at all’.<br />
AMPDS codes are available either during or directly after the<br />
initial emergency call, and therefore present an appropriate target<br />
in modelling HEMS dispatch utility using immediately available<br />
information. These codes are typically set within the initial call handling<br />
process, but they can be manually changed if more information<br />
becomes available during the triage process.<br />
HEMS are dispatched at the discretion of the EEAST Critical Care Desk<br />
(CCD), which is routinely staffed by a HEMS-dispatcher and a clinicallyactive<br />
CCP. However, at times CCD may be staffed by a dispatcher<br />
without a CCP. CCD personnel continuously review EEAST emergency<br />
calls 24 h per day, with the aim of identifying incidents believed to<br />
be most appropriate for HEMS, either as an ‘immediate’ dispatch<br />
based on AMDPS codes and other information in the Computer Aided<br />
Dispatch (CAD) system, or as an ‘interrogate’ (additional information<br />
from the caller), as well as responding to EMS requests for a HEMS<br />
co-response (crew request).<br />
Data inclusion criteria<br />
All HEMS dispatches by EEAST (EAAA, Magpas, EHAAT) during a fouryear<br />
period (2016–2019) where an AMPDS code was available. In order to<br />
ensure that AMPDS codes with the highest system utility were identified,<br />
EEAST provided complete system (EMS and HEMS) AMPDS code<br />
dispatches for a 12-month period (2021)—the ‘EMS reference group’.<br />
Data collection<br />
All services use HEMSbase (MedicOne Systems Ltd, <strong>UK</strong>) electronic<br />
medical record software. The following data were extracted from<br />
HEMSbase. HEMS taskings: incident type, call result (stand down,<br />
or patient attended), callsign (helicopter, or RRV), job timings (day—<br />
0700– 1900, or night—1900–0700), CCD team composition (CCP<br />
team, or dispatcher alone), and the EEAST unique case identification<br />
number (CAD date/number). The following data were additionally<br />
collected for all patients attended by HEMS: patient age and gender,<br />
all drugs given, all interventions performed, and attendance result<br />
(air conveyance, ground escort, scene assist (HEMS team did not<br />
accompany patient to hospital), and stood down (before mobile, en<br />
route or at scene). The CAD number/ dates were shared with EEAST<br />
in order to obtain the AMPDS codes. Combined data from the three<br />
HEMS were collated into Excel data sheets and stored on a secure<br />
server protected by double-authenticator security and only accessible<br />
to the team working on the project; all data were anonymised.<br />
Definitions<br />
HEMS-level intervention/drug/diagnostic (HLIDD)—all HEMS-delivered<br />
actions were compared against Schedule 17 of the <strong>UK</strong> Human<br />
Medicines Regulations 2012 (exemption for registered paramedics<br />
from the restrictions on administration of prescription-only medicines)<br />
[35, 36], and the Joint Royal Colleges <strong>Ambulance</strong> Liaison Committee<br />
(JRCALC) clinical guidelines October 2022 [37], to identify a list of<br />
HLIDD; additionally, we included helicopter conveyance to hospital.<br />
A list of HLIDDs is in Additional file 1. Not all HLIDDs are routinely<br />
delivered by every HEMS in this region.<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
7
FEATURE<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
Patient contact was defined as clinical contact with the patient by a<br />
member of the HEMS team. Stand-down was defined as no clinical<br />
contact (either stood-down before mobile, en route, or at scene).<br />
AMPDS codes were defined as the complete three-part data (09-E-<br />
01). AMPDS categories were defined as the first data descriptor of the<br />
AMPDS code (09). High system utility was predefined as AMPDS codes<br />
that had > 10% HEMS dispatch rate of all EMS taskings in the EMS<br />
reference group (2021), in order to ensure that codes identified in the<br />
primary outcome had significant whole-system frequency; for example,<br />
code 09E01 was found to comprise of 13.7% of all HEMS tasking by<br />
EEAST.<br />
Owing to the lack of previously published data in the area of HEMS<br />
dispatch we planned to undertake an exploratory analysis for<br />
the primary outcome of paired ‘patient contact rate’ and ‘HLIDD’<br />
proportions (60%, 70%, 80%, 90%) to identify codes that would<br />
result in an optimal number of high-utility HEMS dispatches in a 24-h<br />
period. This was pre-defined as 10–20 HEMS dispatches (two to four<br />
dispatches on average for each of the five HEMS teams in the East<br />
of England). The authors derived optimal dispatch frequency through<br />
consensus based on operational experience, which also takes into<br />
account the potential limitations to activity (weather, fuel, equipment<br />
and drug restocking during a duty period).<br />
Primary outcome<br />
The primary outcome was to identify AMPDS codes with a > 10%<br />
HEMS dispatch rate of all EMS taskings that would result in 10–20<br />
high-utility HEMS dispatches per 24-h period in the East of England.<br />
Secondary outcomes<br />
The secondary outcomes were to identify plausible associations with<br />
the chance of patient contact and the chance of an HLIDD using<br />
individual logistic regression models for the ten most frequently HEMSdispatched<br />
AMPDS categories. The pre-specified variables of interest<br />
were: age, sex, time of day (day, night), HEMS transport platform<br />
(helicopter, RRV), and CCD team composition (dispatcher and CCP,<br />
lone dispatcher).<br />
Data analysis<br />
For the primary outcome, the EMS reference group data were<br />
interrogated to identify AMPDS codes with a > 10% HEMS dispatch<br />
rate in 2021. In the HEMS dispatch data (2016–2019), codes were<br />
identified that resulted in ≥ 50 HEMS dispatches in the four-year<br />
period. Codes with < 50 HEMS dispatches were used as the reference<br />
group in two logistic regression models. The first model identified<br />
codes with a significantly high rate of patient contact compared with<br />
the reference group (using a binary outcome of 1 = patient seen, 0 =<br />
stand down). A second logistic regression analysis identified codes<br />
with a significantly high rates of HLIDD compared with the reference<br />
group (using a binary outcome of 1 = HLIDD, 0 = no HLIDD) for jobs<br />
where a patient was seen. We then undertook an exploratory analysis<br />
to determine the optimal patient contact and/or HLIDD proportions<br />
(with a > 10% HEMS dispatch rate of all EMS taskings) that would<br />
result in 10–20 high-utility HEMS dispatches in 24 h.<br />
For the secondary outcomes, all variables in the HEMS dispatch data<br />
(2016–2019) were included in further individual logistic regression<br />
models for each of the ten most prevalent AMPDS categories with<br />
two outcomes— patient contact and HLIDD. Age was separated into<br />
bins (< 16, 16–55, > 55 years old) based on clinically pragmatic ranges<br />
(all other variables were binary). Taskings that resulted in more than<br />
one patient being treated were excluded from the analysis of age and<br />
sex. A logistic regression model was built for each of the ten AMPDS<br />
categories, starting with all variables followed by sequential elimination,<br />
to retain only those with significance for the outcome (patient contact<br />
and/or HLIDD). For all models, the assumptions of logistic regression<br />
were tested, checking for linear relationships in the logit of the<br />
outcomes, unduly influential values and multicollinearity. Plausible<br />
interactions were tested with likelihood ratio tests to determine the<br />
final best model. Missing data were handled as ‘missing at random’.<br />
Significance was predefined as p < 0.05 throughout.<br />
Data have been reported as number (percentage), and median<br />
[interquartile-range] as appropriate. Results of logistic regression have<br />
been reported as an adjusted odds ratios (OR) with 95% confidence<br />
intervals (95%CI), both derived from coefficients in the logistic<br />
regression model. Data manipulation and statistical analyses were<br />
performed using the R statistical programming language (R Core Team<br />
[2018]; R: A language and environment for statistical computing [R<br />
Foundation for Statistical Computing, Vienna, Austria]).<br />
Results<br />
During the four-year study period there were n = 25,491 HEMS<br />
dispatches (6400 per year), of which n = 20,030 (90.3%) had an<br />
associated AMPDS code, Fig. 1.<br />
HEMS dispatches<br />
Approximately half of all HEMS dispatches were immediate, and the<br />
majority occurred when the dispatch team included a CCP. More<br />
dispatches occurred during the day shift (0700–1900) compared to<br />
the night shift, and the HEMS transport platform was a helicopter in<br />
more than half of cases. The 23,030 HEMS dispatches included n =<br />
678 unique AMPDS codes, and the most prevalent AMPDS categories<br />
were cardiac/respiratory, road traffic collisions (RTC), and falls, Table 1.<br />
HEMS dispatches with patient contact<br />
N = 13,778 (59.8%) of HEMS dispatches resulted in patient contact,<br />
and therefore the stand-down rate was approximately 40%. The<br />
median age was 49 [29–65] years and included n = 1060 (7.7%)<br />
patients under 16 years old (n = 63 missing age data). There were<br />
n = 9109 (66.1%) male patients and five (0.04%) were recorded<br />
as transgender (n = 86 missing gender data). n = 8437 (61.2%) of<br />
missions with patient contact resulted in use of HLIDD for at least<br />
one patient, and a total of n = 8967 patients received an HLIDD—this<br />
number is greater than the ‘missions with patient contact that resulted<br />
in an HLIDD’ number as some missions included treatment of more<br />
than one patient, Table 2.<br />
Primary outcome<br />
A small proportion, n = 84 (12.4%), of AMPDS codes resulted in ≥ 50<br />
HEMS dispatches per code, but represented more than three-quarters<br />
of all HEMS dispatches (n = 18,240, 79.2%) as total number.<br />
43 AMPDS codes were identified that had significantly greater rates of<br />
patient contact and/or HLIDD compared to the reference group. These<br />
codes were associated with 11,640 (50.5%) HEMS dispatches in the<br />
8<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
study period. In the exploratory analysis, a cut-off of ≥ 70% patient<br />
contact rate and/or ≥ 70% HLIDD (with a > 10% HEMS dispatch of all<br />
EMS taskings) resulted in 17 taskings per 24-h period. Additional file 2<br />
includes the sensitivity analysis to explore the impact of thresholds on<br />
estimated tasking numbers per 24-h period. This definition derived nine<br />
‘golden’ AMPDS codes with a high whole-system and HEMS utility,<br />
and an optimal frequency of HEMS dispatches, Table 3.<br />
A complete description of the 43 AMPDS codes with significantly<br />
high rates of patient contact or HLIDD is in Additional file 3.<br />
Secondary outcomes<br />
The ten most prevalent AMPDS categories of HEMS dispatch were<br />
analysed, n = 19,384 (84.2%) of taskings. Only variables that had<br />
significance in the univariate models for each AMPDS category (not<br />
presented) were included in the multivariate analyses.<br />
HEMS at night (compared to day) and dispatch by RRV (compared to<br />
helicopter) both had a significantly lower chance of patient contact and<br />
HLIDD for several AMPDS categories. The exception to this was road<br />
traffic collisions, which had significantly higher rates of patient contact<br />
at night compared day.<br />
The presence of a CCP in the CCD team had no effect on the chance<br />
of patient contact or HLIDD, other than for penetrating injury codes<br />
(stab/gunshot, 27-X-XX) for which a CCP on the desk was associated<br />
with an increased chance of patient contact but had no effect on the<br />
chance of HLIDD.<br />
Age < 16 years old (compared to 16–55 years old) was associated with<br />
a lower chance of HLIDD for the majority of categories, and age > 55<br />
years old had a greater chance of HLIDD for cardiac/respiratory and<br />
traumatic injury categories, and lower for burns. Male sex (compared<br />
Figure 1. HEMS dispatches in the East of England (2016–2019)<br />
with complete AMPDS code data. HEMS patient contact, and<br />
HEMS-level intervention/drug/diagnostic (HLIDD). HEMS<br />
Helicopter Emergency Medical Service. AMPDS Advanced<br />
Medical Priority Dispatch System. Stand-down—the HEMS team<br />
were not required and were cancelled before patient contact<br />
Table 1. A description of HEMS dispatches in the East of England<br />
2016–2019, n = 23,030<br />
n (%)<br />
Dispatch type<br />
Immediate 12,463 (54.1)<br />
Interrogate 5428 (23.6)<br />
Crew request 4918 (21.4)<br />
Dispatch characteristics<br />
CCP in dispatch team 20,912 (90.8)<br />
Day shift (0700-1900) 16,552 (71.7)<br />
Helicopter 14,750 (64.1)<br />
RRV 8280 (36.0)<br />
AMPDS category (category number)<br />
Cardiac/respiratory (09) 5299 (23.0)<br />
RTC (29) 4951 (21.5)<br />
Falls (17) 2491 (10.8)<br />
Stab/gunshot (27) 1532 (6.7)<br />
Unconscious/fainting (31) 1204 (5.2)<br />
Convulsions/fitting (12) 1183 (5.1)<br />
Traumatic injuries (30) 1114 (4.8)<br />
Breathing problems (06) 902 (3.9)<br />
Burns (07) 361 (1.6)<br />
Chest pain (10) 347 (1.5)<br />
Other (>10 in rank order) 3646 (15.8)<br />
CCP Critical Care Paramedic, RRV rapid response vehicle (car), AMPDS<br />
Advanced Medical Priority Dispatch System, RTC road traffic collision<br />
Table 2 Patients attended by HEMS in the East of<br />
England (2016–2019) who received a HEMS-level<br />
intervention/drug/diagnostic (HLIDD), n = 8967. Only including<br />
HLIDD received by > 400 patients<br />
HLIDD N %<br />
Endotracheal tube 3883 43.3<br />
Advanced analgesia 2576 28.7<br />
Conveyed by helicopter 2463 27.5<br />
PHEA 2194 24.5<br />
POCUS (Cardiac) 1070 11.9<br />
Gastric Tube 1047 11.7<br />
Procedural sedation 867 9.7<br />
Oesophageal Temperature Probe 842 9.4<br />
Intravenous antimicrobial 771 8.6<br />
Thoracostomy 651 7.3<br />
Intravenous electrolyte 643 7.2<br />
Splintage 558 6.2<br />
POCUS (FAST) 513 5.7<br />
POCUS (Lung) 492 5.5<br />
Radial arterial line 471 5.3<br />
HLIDD HLIDD HEMS-level intervention/drug/diagnostic (complete list at<br />
Additional file 1); advanced analgesia includes intravenous fentanyl and<br />
inhaled methoxyflurane (Penthrox); PHEA prehospital emergency<br />
anaesthesia (drug-assisted intubation); POCUS point-of-care ultrasound;<br />
gastric tube includes oro and nasogastric decompression tubes;<br />
intravenous electrolyte includes magnesium, calcium chloride, and<br />
sodium bicarbonate; intravenous antimicrobial includes coamoxiclav,<br />
ceftriaxone, and acyclovir<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
9
FEATURE<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
with female sex) was associated with a greater chance of HLIDD<br />
for cardiac/respiratory, road traffic collisions and convulsions/fitting<br />
categories, Tables 4 and 5.<br />
Discussion<br />
We have used large, multi-organisational, data to identify nine ‘golden’<br />
AMPDS codes with significant utility in improving the accuracy of<br />
HEMS dispatch with respect to patient contact rates and HEMS-level<br />
intervention/ drug/diagnostic rates. In addition, we have demonstrated<br />
some important associations with these outcomes for age, sex, time of<br />
day, HEMS transport type, AMPDS categories, and the presence of a<br />
clinician (a critical care paramedic) in the dispatch team.<br />
There is a distinct paucity of published data in the area of HEMS<br />
dispatch despite this being an expensive and limited resource where<br />
research has been identified as a priority for the last decade. It is likely<br />
that this is due to a combination of factors, which includes the volume,<br />
complexity, and availability of data in these systems. We have therefore<br />
had to make pragmatic consensus decisions on appropriate data<br />
definitions, together with an exploratory analysis of HEMS dispatches<br />
per 24-h time period to determine the optimal cut-off for specificity<br />
of the primary outcome, which has a ≤ 30% over-triage rate. By<br />
happenstance, this over-triage rate is compliant with the American<br />
College of Surgeon’s Committee on Trauma (ACS CoT) guideline for the<br />
triage of prehospital major trauma (25–35% over-triage) [38]. However,<br />
as we were only able to determine the patient contact and HLIDD rates<br />
for patients that HEMS were dispatched to we are unable to determine<br />
the under-triage rate (i.e. what proportion of EMS dispatches should<br />
have had a HEMS patient contact and/or HLIDD, but did not). Arguably,<br />
this is a more important metric when considering the performance of a<br />
triage system, and the ACS CoT recommends an under-triage rate of <<br />
5% [38]. It is very likely that under-triage in <strong>UK</strong> EMS for HEMS patient<br />
contact and HLIDD is much higher than 5%, but there are no data<br />
that verify this assumption. However, we have been able to identify<br />
an easily applied method to reduce the over-triage rate from > 40%<br />
(HEMS stand-down rate in our complete data) to ≤ 30%, whilst also<br />
assisting the very early identification of emergency calls with a greater<br />
chance of leading to HEMS-level actions. We believe that these data<br />
are unique in addressing the paucity of HEMS dispatch data [26], and<br />
the associated 2011 and <strong>2023</strong> prehospital research priority [23].<br />
The main controversy in this area of research is whether there<br />
is patient-centered benefit from HEMS compared to EMS-only<br />
attendance. Whilst the existing evidence is perhaps equivocal [8–18],<br />
a key factor in robustly answering this question (and in providing<br />
optimal patient care across a system) is ensuring that HEMS are<br />
dispatched to the right patients (i.e., those who are most likely to<br />
benefit), which may be aetiology-dependent [12, 15]. Exact aetiology<br />
is often not available at the time of the initial emergency call, which<br />
therefore necessitates using a time-sensitive surrogate, which in the<br />
case of this study was AMPDS codes. Overall, there is a low level of<br />
evidence supporting the accuracy of dispatch systems in identifying<br />
acuity [27]. However, we have been able to rely on the pragmatic<br />
judgement of prehospital clinicians in the need for HEMS patient<br />
contact and HEMS interventions, the frequency of which we have been<br />
able to use to identify an optimal number (for operational delivery)<br />
of AMPDS codes associated with the highest levels of HEMS utility.<br />
We cannot control for the major constraint of not knowing the undertriage<br />
rate for these codes, and they should be prospectively tested<br />
in multiple settings to confirm their utility. The expectation is that<br />
identification of high-utility AMPDS codes is a step towards a better<br />
understanding of the benefit of HEMS.<br />
We observed that night and RRV taskings, compared to day and<br />
helicopter respectively, are both associated with lower patient contact<br />
and HLIDD rates overall. This effect has been previously described<br />
in the <strong>UK</strong> and Norway [19, 39], in contrast to The Netherlands where<br />
no day-night effect has been reported [28]. The lower rates for RRV<br />
taskings, even after adjusting for time-of-day remain unexplained, but<br />
it may be that standing-down a road vehicle response is perceived<br />
to be more acceptable that re-routing a helicopter. Our data also<br />
suggests that the absence of a clinician in dispatch has no effect on<br />
the chance of HEMS patient contact for most taskings, with the notable<br />
exception of the stab/gunshot call category. Furthermore, there was<br />
no signal across any of the ten most prevalent AMPDS categories that<br />
this variable had any effect on the chance of a HLIDD (including stab/<br />
gunshot). This somewhat agrees with previous <strong>UK</strong> HEMS data [21], but<br />
as there was a CCP in dispatch for > 90% of HEMS taskings, this may<br />
represent a type-2 error (small numbers), and we are also unable to<br />
control for the likelihood that non-clinical dispatchers have learned from<br />
co-dispatching with a CCP for the vast majority of duties. Therefore, we<br />
do not believe that our data support nonclinician HEMS dispatch.<br />
We observed significantly higher rates of HLIDD in patients > 55 years<br />
old in two AMPDS categories: cardiac/ respiratory, traumatic injuries.<br />
The first of these is likely to represent a higher acuity of age-related<br />
aetiology in these categories, and the latter is likely to reflect the Silver<br />
Trauma phenomenon [40]. Older age has previously been identified<br />
in <strong>UK</strong> HEMS as a potentially useful dispatch criteria [41], and our data<br />
provide support for this in a more specific and actionable way. In the<br />
East of England, we have used the nine ‘golden’ codes to better inform<br />
clinicians on the Critical Care Desk in their decisions around HEMS<br />
dispatch. It is anticipated that this will reduce the over-triage rate by<br />
approximately 10% (as per our retrospective findings). It may also<br />
be useful to utilize these codes as a framework for key performance<br />
indicators in HEMS dispatch.<br />
The major limitation of this study is that we were only able to<br />
interrogate data for taskings that HEMS had been dispatched on.<br />
Table 3 AMPDS codes with a significantly greater chance of HEMS<br />
patient contact and/or HEMS-level intervention/drug/ diagnostic<br />
(HLIDD) compared to the reference group (2016– 2019). Nine<br />
‘golden’ codes had a ≥ 70% rate of patient contact and/or HLIDD<br />
(2016–2019) and were > 10% of EEAST incidents<br />
AMPDS code category<br />
Burns<br />
Cardiac/respiratory<br />
Convulsions/fitting<br />
Falls<br />
RTC<br />
AMPDS code<br />
07-C-03<br />
09-E-01<br />
12-D-01<br />
17-D-02P, 17-D-06, 17-D-06P<br />
29-D-06, 29-D-06 V, 29-D-07<br />
AMPDS Advanced Medical Priority Dispatch System, HEMS helicopter<br />
emergency medical service, EEAST East of England <strong>Ambulance</strong> Service NHS<br />
Trust, RTC road traffic collision<br />
10<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
Table 4 Variables associated with significant high or low rates of HEMS patient contact (multivariate model)<br />
AMPDS category/n<br />
Night (ref: day)<br />
RRV (ref: helicopter)<br />
Adjusted odds ratio (95% confidence interval)<br />
Dispatch desk<br />
CCP (ref: no<br />
CCP)<br />
06–Breathing problems<br />
n = 902<br />
07—Burns<br />
n = 361<br />
09—Cardiac/respiratory<br />
n = 5299<br />
10–Chest pain<br />
n = 347<br />
12—Convulsions/fitting<br />
n = 1183<br />
17—Falls<br />
n = 2491<br />
27—Stab/gunshot<br />
n = 1532<br />
29—RTC<br />
n = 4951<br />
30—Traumatic injuries<br />
n = 1114<br />
31—Unconscious/fainting<br />
n = 1204<br />
0.6 (0.4–0.8) ns ns<br />
0.5 (0.3–0.9) 0.5 (0.3–0.8) ns<br />
0.8 (0.7–0.9) 0.8 (0.7–0.9) ns<br />
0.3 (0.1–0.4) ns ns<br />
ns ns ns<br />
0.5 (0.4–0.7) 0.8 (0.6–0.9) ns<br />
0.7 (0.6–0.9) ns 1.6 (1.1–2.5)<br />
0.8 (0.7–0.9) 0.8 (0.7–0.9) ns<br />
ns 0.5 (0.4–0.7) ns<br />
0.6 (0.5–0.8) ns ns<br />
HEMS Helicopter Emergency Medical Service, AMPDS Advanced Medical Priority Dispatch System, RRV rapid response vehicle, CCP critical<br />
care paramedic, ns not significant (p-value ≥ 0.05). An odds ratio < 1 is a reduced chance of the outcome (not highlighted bold); an odds<br />
ratio > 1 is an increased chance of the outcome (highlighted bold)<br />
Table 5 Variables associated with significant high or low rates of HEMS-level intervention/drug/diagnostic (multivariate model)<br />
AMPDS category / n<br />
Night (ref: day)<br />
Night<br />
(ref: day)<br />
RRV (ref:<br />
helicopter)<br />
Dispatch desk<br />
CCP (ref: no<br />
CCP)<br />
Male<br />
(ref: female)<br />
Age < 16 years<br />
(ref:<br />
16–55 years)<br />
Age > 55 years<br />
(ref:<br />
16–55 years)<br />
06—Breathing problems<br />
n = 493<br />
07—Burns<br />
n = 200<br />
09—Cardiac/respiratory<br />
n = 3128<br />
10—Chest pain<br />
n = 277<br />
12—Convulsions/fitting<br />
n = 760<br />
17—Falls<br />
n = 1785<br />
27—Stab/gunshot<br />
n = 549<br />
29—RTC<br />
n = 3018<br />
30—Traumatic injuries<br />
n = 786<br />
31—Unconscious/fainting<br />
n = 682<br />
ns 0.4 (0.3–0.6) ns ns 0.1 (0.1–0.3) ns<br />
0.3 (0.1–0.6) ns ns ns 0.5 (0.2–0.9) 0.4 (0.2–0.9)<br />
ns 0.7 (0.6–0.8) ns 1.2 (1.1–1.4) 0.6 (0.5–0.9) 1.3 (1.1–1.5)<br />
ns 0.3 (0.2–0.6) ns ns ns ns<br />
ns ns ns 1.4 (1.1–1.9) 0.5 (0.3–0.7) ns<br />
0.7 (0.6–0.9) 0.6 (0.5–0.8) ns ns 0.4 (0.3–0.6) ns<br />
ns 0.3 (0.2–0.4) ns ns ns ns<br />
1.3 (1.0–1.5) 0.5 (0.4–0.6) ns 1.5 (1.2–1.8) ns ns<br />
0.5 (0.3–0.9) 0.6 (0.3–0.9) ns ns 0.6 (0.4–0.9) 1.4 (1.1–2.1)<br />
ns 0.7 (0.5–0.9) ns ns 0.1 (0.1–0.3) ns<br />
HEMS Helicopter Emergency Medical Service, AMPDS Advanced Medical Priority Dispatch System, RRV rapid response vehicle, CCP critical<br />
care paramedic, ns not significant (p-value ≥ 0.05). An odds ratio < 1 is a reduced chance of the outcome (not highlighted bold); an odds<br />
ratio > 1 is an increased chance of the outcome (highlighted bold)<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
11
FEATURE<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
Therefore, it is possible that patients not attended by HEMS in the<br />
study period would have had AMPDS codes assigned that would<br />
meet the utility criteria. However, the large data capture over four<br />
years for three HEMS organsiations operating five teams somewhat<br />
mitigates this. Some AMPDS codes that are used very infrequently,<br />
and were therefore excluded from this analysis, are likely to be<br />
important when considering HEMS dispatch. Examples include<br />
codes relating to major or mass casualty incidents, and there are<br />
others (for example: ‘34—automatic crash notification’) that may<br />
become more important in the future as technology develops [42].<br />
Our data are likely to have generalizability to HEMS systems that<br />
operate a physician-paramedic model in mixed urban and rural<br />
geographies that use AMPDS for dispatch. However, these data<br />
have less utility in non-AMPDS dispatch systems (for example, those<br />
using NHS Pathways in some regions of the <strong>UK</strong>) without robust<br />
mapping of AMPDS and non-AMPDS codes. In addition, whilst the<br />
East of England includes a broad mix of urban and rural populations,<br />
it is very flat. Therefore, our data may have reduced generalizability<br />
in more mountainous geographies where the limitations of patient<br />
accessibility, weather, and potentially a different epidemiology<br />
of disease and trauma may have a different impact on important<br />
dispatch codes.<br />
We have identified nine ‘golden’ AMPDS codes, available at the time<br />
of initial emergency call, that are associated with high-levels of wholesystem<br />
and HEMS utility in the East of England. We propose that <strong>UK</strong><br />
EMS should consider immediate HEMS dispatch to these codes, or<br />
automated notification to HEMS dispatchers when these codes are<br />
generated from emergency calls within a robust governance framework.<br />
Abbreviations<br />
HEMS Helicopter Emergency Medical Services<br />
EMS Emergency medical service<br />
AMPDS Advanced Medical Priority Dispatch System<br />
HLIDD HEMS-level intervention/drug/diagnostic<br />
PHEA Prehospital emergency anaesthesia<br />
EEAST East of England <strong>Ambulance</strong> Service NHS Trust<br />
EAAA East Anglian Air <strong>Ambulance</strong><br />
Magpas Magpas Air <strong>Ambulance</strong><br />
EHAAT Essex & Herts Air <strong>Ambulance</strong><br />
CCP Critical Care Paramedic<br />
RRV Rapid Response Vehicle<br />
RTC Road traffic collisions<br />
POCUS Point of Care Ultrasound<br />
ACS CoT American College of Surgeon’s Committee on Trauma<br />
Supplementary Information<br />
The online version contains supplementary material available at https://<br />
sjtrem.biomedcentral.com/articles/10.1186/s13049-023-01094-w.<br />
Additional file 1. HEMS-level intervention/drug/diagnostic. A list of all<br />
HLIDDs used within this study.<br />
Additional file 2. Sensitivity analysis to explore impact of thresholds<br />
on estimated tasking numbers/24 h. Demonstration of the impact of<br />
specific thresholds for intervention and/or patient contact on code<br />
availability.<br />
Additional file 3. AMPDS codes with significantly high rates of patient<br />
contact and/or HLIDD. A table listing the p value for both HLIDD and<br />
patient contact for specific codes.<br />
Acknowledgements<br />
We acknowledge the assistance of EEAST in aiding with providing core<br />
data to allow the analysis in the paper to be undertaken.<br />
Author contributions<br />
The authors confirm contribution to the paper as follows: study<br />
conception and design: CTE, KL, RM, EBGB; data collection: CTE,<br />
KL, AS, AD, SM; analysis and interpretation of results: CTE, KL, EBGB;<br />
manuscript preparation: CTE, KL, RM, EBGB. KL is the data guarantor.<br />
All authors approved the final version of the manuscript.<br />
Funding<br />
No funding was provided for this work.<br />
Availability of data and materials<br />
Data are available on reasonable request.<br />
Declarations<br />
Ethics approval and consent to participate<br />
This study met the Health Research Authority criteria for a service<br />
evaluation. The protocol was approved by the Anglian Ruskin<br />
University School Research Ethics Panel for Allied Health, Nursing<br />
& Midwifery & Medicine (ref no. AHSREP- 21-032), and registered<br />
with the EAAA Department of Research, Audit, Innovation, and<br />
Development (RAID), Reference Number: EAAA 2021/028.<br />
Consent for publication<br />
Patients and the public were not involved in the design, analysis,<br />
or reporting of this research.<br />
Competing interests<br />
We have no competing interests to declare.<br />
Author details<br />
1 Department of Research, Audit, Innovation, and Development, East<br />
Anglian Air <strong>Ambulance</strong>, Gambling Close, Norwich Airport, Norwich<br />
NR6 6EG, <strong>UK</strong>. 2 Essex & Herts Air <strong>Ambulance</strong> Trust, Colchester,<br />
Essex, <strong>UK</strong>. 3 Anglia Ruskin University, Cambridge, <strong>UK</strong>. 4 University of<br />
East Anglia, Norwich, <strong>UK</strong>. 5 Magpas Air <strong>Ambulance</strong>, Huntingdon, <strong>UK</strong>.<br />
6 Academic Department of Military Emergency Medicine, Royal Centre<br />
for Defence Medicine (Research & Clinical Innovation), Birmingham,<br />
<strong>UK</strong>. 7 Emergency Department, Cambridge University Hospitals NHS<br />
Foundation Trust, Cambridge, <strong>UK</strong>.<br />
Received: 24 February <strong>2023</strong> Accepted: 7 June <strong>2023</strong><br />
Published online: 12 June <strong>2023</strong><br />
References<br />
1. ADAC Air Rescue [Internet]. [cited 2019 Aug 6]. Available from:<br />
https://arts. eu/ blog/ adac- air- rescue<br />
2. Roberts K, Blethyn K, Foreman M, Bleetman A. Influence of air<br />
ambulance doctors on on-scene times, clinical interventions,<br />
decision-making and independent paramedic practice. Emerg<br />
Med J. 2009;26:128.<br />
3. Schuppen H van, Bierens J. Understanding the prehospital<br />
physician controversy. Step 2. Eur J Emerg Med. 2015;22:384–90.<br />
4. Bernard SA, Nguyen V, Cameron P, Masci K, Fitzgerald M,<br />
Cooper DJ, et al. Prehospital rapid sequence intubation improves<br />
functional outcome for patients with severe traumatic brain injury.<br />
Ann Surg. 2010;252:959–65.<br />
5. Lendrum R, Perkins Z, Chana M, Marsden M, Davenport R,<br />
Grier G, et al. Pre-hospital resuscitative endovascular balloon<br />
occlusion of the aorta for exsanguinating pelvic haemorrhage.<br />
Resuscitation. 2018;135:6–13.<br />
6. Price J, Lachowycz K, Steel A, Moncur L, Major R, Barnard<br />
EBG. Intubation success in prehospital emergency anaesthesia:<br />
a retrospective observational analysis of the Inter-Changeable<br />
Operator Model (ICOM). Scand J Trauma Resusc Emerg<br />
Medicine. 2022;30:44.<br />
7. Lockey DJ, Crewdson K, Davies G, Jenkins B, Klein J, Laird C,<br />
et al. AAGBI: safer pre-hospital anaesthesia 2017. Anaesthesia.<br />
2017;72:379–90.<br />
12<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
8. Garner A, Rashford S, Lee A, Bartolacci R. Addition of physicians<br />
to paramedic helicopter services decreases blunt trauma<br />
mortality. Aust Nz J Surg. 1999;69:697–701.<br />
9. Iirola TT, Laaksonen MI, Vahlberg TJ, Pälve HK. Effect of<br />
physician-staffed helicopter emergency medical service on blunt<br />
trauma patient survival and prehospital care. Eur J Emerg Med.<br />
2006;13:335–9.<br />
10. Morrison JJ, Oh J, DuBose JJ, O’Reilly DJ, Russell RJ,<br />
Blackbourne LH, et al. En-route care capability from point of<br />
injury impacts mortality after severe wartime injury. Ann Surg.<br />
2013;257:330–4.<br />
11. Hartog DD, Romeo J, Ringburg AN, Verhofstad MHJ, Lieshout<br />
EMMV. Survival benefit of physician-staffed Helicopter<br />
Emergency Medical Services (HEMS) assistance for severely<br />
injured patients. Inj. 2015;46:1281–6.<br />
12. Garner AA, Mann KP, Fearnside M, Poynter E, Gebski V. The<br />
Head Injury Retrieval Trial (HIRT): a single-centre randomised<br />
controlled trial of physician prehospital management of severe<br />
blunt head injury compared with management by paramedics<br />
only. Emerg Med J. 2015;32:869.<br />
13. Andruszkow H, Schweigkofler U, Lefering R, Frey M, Horst K,<br />
Pfeifer R, et al. Impact of helicopter emergency medical service<br />
in traumatized patients: Which patient benefits most? PLoS ONE.<br />
2016;11: e0146897.<br />
14. Maddock A, Corfield AR, Donald MJ, Lyon RM, Sinclair N,<br />
Fitzpatrick D, et al. Prehospital critical care is associated with<br />
increased survival in adult trauma patients in Scotland. Emerg<br />
Med J. 2020;37:141–5.<br />
15. von Vopelius-Feldt J, Brandling J, Benger J. Systematic review<br />
of the effectiveness of prehospital critical care following out-ofhospital<br />
cardiac arrest. Resuscitation. 2017;114:40–6.<br />
16. Böttiger BW, Bernhard M, Knapp J, Nagele P. Influence of<br />
EMS-physician presence on survival after out-of-hospital<br />
cardiopulmonary resuscitation: systematic review and metaanalysis.<br />
Crit Care. 2016;20:4. 17. von Vopelius-Feldt J, Benger<br />
JR. Should physicians attend out-of-hospital cardiac arrests?<br />
Resuscitation. 2016;108:A6-7.<br />
18. Barnard EBG, Sandbach DD, Nicholls TL, Wilson AW, Ercole<br />
A. Prehospital determinants of successful resuscitation after<br />
traumatic and non-traumatic out-of-hospital cardiac arrest.<br />
Emerg Med J. 2019;36:333.<br />
19. Evans EG, Hudson A, McWhirter E, Lyon R. A review of the<br />
activation triggers and reasons for stand downs of a Helicopter<br />
Emergency Medical Service (HEMS). Scand J Trauma Resusc<br />
Emerg Medicine. 2014;22:P5.<br />
20. Taylor C, Jan S, Curtis K, Tzannes A, Li Q, Palmer C, et al. The<br />
cost-effectiveness of physician staffed Helicopter Emergency<br />
Medical Service (HEMS) transport to a major trauma centre in<br />
NSW. Australia Inj. 2012;43:1843–9.<br />
21. Munro S, Joy M, de Coverly R, Salmon M, Williams J, Lyon<br />
RM. A novel method of non-clinical dispatch is associated<br />
with a higher rate of critical Helicopter Emergency Medical<br />
Service intervention. Scand J Trauma Resusc Emerg Medicine.<br />
2018;26:84.<br />
22. Wilson MH, Habig K, Wright C, Hughes A, Davies G, Imray CHE.<br />
Prehospital emergency medicine. Lancet. 2016;386:2526–34.<br />
23. Fevang E, Lockey D, Thompson J, Lossius HM. The top five<br />
research priorities in physician-provided pre-hospital critical care:<br />
a consensus report from a European research collaboration.<br />
Scand J Trauma Resusc Emerg Medicine. 2011;19:57.<br />
24. Ramage L, McLachlan S, Williams K, (PHOTON) PTO<br />
research N. Determining the top research priorities in <strong>UK</strong><br />
prehospital critical care: a modified Delphi study. Emerg Med<br />
J. <strong>2023</strong>;emermed-2022–212622.<br />
25. Wilmer I, Chalk G, Davies GE, Weaver AE, Lockey DJ. Air<br />
ambulance tasking: mechanism of injury, telephone interrogation<br />
or ambulance crew assessment? Emerg Med J. 2015;32:813.<br />
26. Eaton G, Brown S, Raitt J. HEMS dispatch: a systematic review.<br />
Trauma. 2018;20:3–10.<br />
27. Bohm K, Kurland L. The accuracy of medical dispatch—a<br />
systematic review. Scand J Trauma Resusc Emerg Medicine.<br />
2018;26:94.<br />
28. Berkeveld E, Sierkstra TCN, Schober P, Schwarte LA, Terra M,<br />
de Leeuw MA, et al. Characteristics of helicopter emergency<br />
medical services (HEMS) dispatch cancellations during a sixyear<br />
period in a Dutch HEMS region. Bmc Emerg Medicine.<br />
2021;21:50.<br />
29. Röper J, Krohn M, Fleßa S, Thies K-C. Costing of helicopter<br />
emergency services—a strategic simulation based on the<br />
example of a German rural region. Heal Econ Rev. 2020;10:34.<br />
30. Baker SP, Grabowski JG, Dodd RS, Shanahan DF, Lamb MW,<br />
Li GH. EMS helicopter crashes: What influences fatal outcome?<br />
Ann Emerg Med. 2006;47:351–6.<br />
31. Statistics O for N. Population and household estimates, England<br />
and Wales: Census 2021. 2022.<br />
32. Price J, Sandbach DD, Ercole A, Wilson A, Barnard EBG. Endtidal<br />
and arterial carbon dioxide gradient in serious traumatic<br />
brain injury after prehospital emergency anaesthesia: a<br />
retrospective observational study. Emerg Med J. 2020;37:674–9.<br />
33. Steel A, Haldane C, Cody D. Impact of videolaryngoscopy<br />
introduction into prehospital emergency medicine practice: a<br />
quality improvement project. Emerg Med J. 2021;38:549–55.<br />
34. McLachlan S, Bungay H, Wallman S, Christian MD, Ley E, Fenton<br />
R. Scoping the demand for night operation of essex & herts<br />
air ambulance: a prospective observational study. Air Medical<br />
J. 2021;40:28–35.<br />
35. England E. Paramedics and medicines: legal considerations.<br />
J Paramedic Pract. 2016;8:408–15.<br />
36. The Human Medicines Regulations 2012 [Internet]. [cited<br />
<strong>2023</strong> Jan 6]. Available from: https://www.legislation.gov.uk/<br />
uksi/2012/1916/schedule/17/made<br />
37. (AACE) A of ACE, Committee JRCAL. JRCALC Clinical Guidelines<br />
2022. 2022.<br />
38. Surgeons AC of, Trauma C on. Resources for the optimal care<br />
of the injured patient. Chicago: American College of Surgeons;<br />
2014.<br />
39. Østerås Ø, Brattebø G, Heltne J-K. Helicopter-based emergency<br />
medical services for a sparsely populated region: a study of<br />
42,500 dispatches. Acta Anaesth Scand. 2016;60:659–67.<br />
40. Alshibani A, Alharbi M, Conroy S. Under-triage of older trauma<br />
patients in prehospital care: a systematic review. Eur Geriatr Med.<br />
2021;12:903–19.<br />
41. Griggs JE, Barrett JW, Avest ET, de Coverly R, Nelson M,<br />
Williams J, et al. Helicopter emergency medical service dispatch<br />
in older trauma: Time to reconsider the trigger? Scand J Trauma<br />
Resusc Emerg Medicine. 2021;29:62.<br />
42. Ponte G, Ryan GA, Anderson RWG. An estimate of the<br />
effectiveness of an in-vehicle automatic collision notification<br />
system in reducing road crash fatalities in South Australia. Traffic<br />
Inj Prev. 2016;17:258–63.<br />
Publisher’s Note<br />
Springer Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affiliations.<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
13
NEWSLINE<br />
‘Phenomenal results’<br />
achieved by first<br />
paramedic degree<br />
apprenticeship group<br />
The first cohort of East of<br />
England <strong>Ambulance</strong> Service<br />
(EEAST) staff to qualify<br />
as paramedics through<br />
a new apprenticeship<br />
degree programme with the<br />
University of Cumbria have<br />
been celebrated at a special<br />
ceremony after achieving<br />
‘phenomenal results’.<br />
The group of 20, who graduated<br />
at the University of Cumbria<br />
in June, were presented with<br />
a certificate to mark their<br />
achievements on completing the<br />
Level 6 Degree Apprenticeship<br />
Paramedic Programme at a<br />
ceremony at The Athenaeum in<br />
Bury St Edmunds.<br />
Over 80 per cent on the<br />
programme achieved an upperclass<br />
honours degree with five of<br />
the group achieving a first and 11<br />
achieving a 2:1.<br />
EEAST was one of seven<br />
ambulance services to sign<br />
up to the new BSc (Hons)<br />
apprenticeship paramedic degree<br />
course in 2021. The course<br />
was devised by the University<br />
of Cumbria for existing patientfacing<br />
staff, such as emergency<br />
care assistants, ambulance<br />
technicians and associate<br />
ambulance practitioners.<br />
The course takes two years to<br />
complete, compared to three for<br />
a traditional degree in paramedic<br />
science, and allows staff to<br />
continue to work in frontline roles<br />
at EEAST while studying.<br />
This opens an important career<br />
progression pathway for staff who<br />
want to become a paramedic but<br />
feel that university is not the right<br />
option for their circumstances.<br />
Katie Burst, Head of Education<br />
& Learner Experience at EEAST,<br />
said the success will mean more<br />
future paramedics qualifying<br />
through this partnership with the<br />
University of Cumbria.<br />
Katie said:<br />
“We are all delighted and proud<br />
of the success achieved by the<br />
first group on this new apprentice<br />
paramedic degree programme<br />
with the University of Cumbria.<br />
“The feedback on the course<br />
has been excellent and the<br />
partnership with the University of<br />
Cumbria has worked so well.<br />
“The Trust sees this programme<br />
as an important pathway<br />
for developing our staff to<br />
becoming paramedics and we<br />
are fully committed to expanding<br />
availability.”<br />
Hanna Stevens, principal<br />
lecturer in paramedic<br />
apprenticeships at the<br />
University of Cumbria, said:<br />
“The first group of students all<br />
worked exceptionally hard and<br />
they have produced phenomenal<br />
results, with 80 per cent<br />
achieving an upper class degree<br />
honours.<br />
“That is testament to the<br />
partnership working from all<br />
involved who have helped make<br />
this course such a success.<br />
“We look forward to working<br />
with EEAST on this exciting<br />
educational pathway for many<br />
years to come.”<br />
Lee Sweetlove, 36, a student<br />
on the course, said:<br />
“I found the course really<br />
challenging but also very<br />
rewarding. I describe it as<br />
hiking up a steep mountain but<br />
at the top the views are worth the<br />
effort.<br />
“We are now registered<br />
healthcare professionals, and it<br />
has opened up so many career<br />
pathways, so it is a really exciting<br />
time to be a paramedic.<br />
“I always wanted to progress my<br />
career and become a paramedic,<br />
expanding my skillset to be able<br />
to help more patients. I worked<br />
for the Trust as a technician<br />
initially and, if I had decided to<br />
take the traditional route, I would<br />
have had to spend three years at<br />
university and pay for that course.<br />
“By gaining this qualification<br />
through the Trust and the<br />
apprenticeship pathway, you<br />
are still able to earn a salary. I<br />
was able to get married and we<br />
were able to buy our first house<br />
together while I was on the<br />
course.<br />
“For me, this was definitely the<br />
better route. I have built lots of<br />
confidence and experience as I<br />
have been mainly working on the<br />
ambulance with a mentor and<br />
putting my university learning into<br />
practice.’’<br />
The Trust is currently running<br />
three courses on this apprentice<br />
paramedic degree each year<br />
and the pathway is expected to<br />
provide the Trust with 500 newly<br />
qualified paramedics over the<br />
next seven years.<br />
Nine new electric<br />
vehicles introduced<br />
to boost community<br />
response<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
We are pleased to announce<br />
the introduction of nine new<br />
electric vehicles into our fleet<br />
which will be provided to nine<br />
of our Community Response<br />
schemes across the East<br />
Midlands.<br />
This exciting development follows<br />
funding secured from charity<br />
grants in 2022 to help support<br />
several different projects at East<br />
Midlands <strong>Ambulance</strong> Service as<br />
14<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
part of its Community Response<br />
Volunteer Strategy.<br />
Midlands <strong>Ambulance</strong> Service<br />
said:<br />
With the help of the NHS<br />
Charities Together grant, we<br />
have been able to purchase nine<br />
of the new vehicles to support<br />
the vital work carried out by<br />
our Community Responder<br />
schemes, so they can continue<br />
providing lifesaving care to our<br />
communities.<br />
All the electric vehicles have<br />
sat-nav fitted as standard and<br />
our Community First Responders<br />
(CFR) will be able to re-charge the<br />
vehicles at numerous charging<br />
points across the region. In<br />
addition to the normal kit carried<br />
by our CFRs these vehicles are<br />
equipped with a Raizor lifting<br />
chair enabling our volunteers to<br />
assist patients following a fall.<br />
By investing in our fleet and<br />
replacing older vehicles with<br />
electric ones, it also supports<br />
EMAS’ goal to deliver greener,<br />
sustainable healthcare and is<br />
part of our ongoing commitment<br />
to becoming a net zero trust by<br />
2040.<br />
James Hornby, Service Delivery<br />
Manager for Community<br />
Response at East Midlands<br />
<strong>Ambulance</strong> Service said:<br />
“Thanks to the funding secured,<br />
we have been able to provide<br />
these state-of-the-art vehicles<br />
to our Community Response<br />
schemes across the region.<br />
“These nine vehicles join the<br />
other eight electric vehicles which<br />
our schemes have and will help<br />
ensure our volunteers, who make<br />
a huge and valued contribution<br />
at EMAS can continue to make a<br />
difference to the lives of people<br />
within our communities across<br />
the region.”<br />
Cara Turton-Chambers,<br />
Sustainability, Energy and<br />
Compliance Manager at East<br />
“It’s great to see that our EV CFR<br />
fleet is expanding. The NHS has a<br />
big challenge ahead to reach net<br />
zero by 2040. However, at EMAS<br />
we know this transition is not only<br />
best for the planet, but best for<br />
our patients and service users.<br />
“Climate change is a health<br />
emergency and action to slow<br />
climate change, helps create a<br />
healthy future. As well as lower<br />
carbon emissions, these vehicles<br />
will have no tail pipe emissions<br />
and so as we respond we aren’t<br />
worsening air pollution, further<br />
helping keep people healthy.<br />
“Projects like this support the<br />
implementation of our Green Plan<br />
and the wider NHS’ journey to<br />
deliver greener, more sustainable<br />
healthcare.”<br />
This investment will see every<br />
division in the East Midlands<br />
region (Derbyshire, Leicester,<br />
Leicestershire and Rutland,<br />
Lincolnshire, Northamptonshire<br />
and Nottinghamshire) receive one<br />
of the electric vehicles.<br />
In May <strong>2023</strong> EMAS launched its<br />
new five-year strategy (<strong>2023</strong>-<br />
2028) and five new strategic<br />
ambitions to help the organisation<br />
achieve its overall vision. This<br />
investment supports ambition<br />
5 – ‘We will work in partnership<br />
to reduce health inequalities<br />
and improve the health of<br />
our population, and ensure<br />
sustainability’.<br />
We began the introduction of<br />
electric vehicles into our fleet<br />
as early as 2017.<br />
In 2022, we replaced all Non-<br />
Emergency Patient Transport<br />
Service (NEPTS) cars in<br />
Derbyshire with fully-electric<br />
cars; reducing our emissions<br />
by 96 tonnes of carbon dioxide<br />
equivalent (tCO2e) per year.<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
15
NEWLINE<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
EEAST represented<br />
at Westminster<br />
Abbey service to<br />
mark NHS 75th<br />
Birthday<br />
Staff at the East of England<br />
<strong>Ambulance</strong> Service NHS Trust<br />
(EEAST) joined colleagues from<br />
across the NHS at a service at<br />
Westminster Abbey to mark the<br />
NHS’s 75th Birthday.<br />
Terry Hicks, head of operations<br />
for Cambridgeshire and<br />
Peterborough, Zoe Martindale,<br />
Philip Bygrave, and Chaplain<br />
Tony Mills all made the journey to<br />
attend the service on Wednesday,<br />
July 5.<br />
The event, which was attended<br />
by Their Royal Highnesses The<br />
Duke and Duchess of Edinburgh<br />
and senior political leaders,<br />
started with a procession of<br />
the George Cross, which was<br />
presented to the NHS in 2022 by<br />
Her Majesty The Queen.<br />
The Cross was carried by nurse<br />
May Parsons, who administered<br />
the world’s first COVID vaccine.<br />
May was joined by Kyle Dean-<br />
Curtis, 17, St John <strong>Ambulance</strong><br />
cadet of the year, and Enid<br />
Richmond, 91, who worked for<br />
the NHS at the time it launched.<br />
Zoe Martindale is an<br />
improvement manager for the<br />
Emergency Operations Centre<br />
which handles incoming 999<br />
emergency calls. She said:<br />
“I felt extremely honoured and<br />
privileged to be invited to attend<br />
the service to celebrate the<br />
75th anniversary of the NHS at<br />
Westminster Abbey. It was a<br />
really moving experience and I felt<br />
lucky and honoured to have been<br />
picked to attend”,<br />
“Attending the service gave<br />
me an opportunity to reflect on<br />
the past 15 years that I have<br />
spent working for the Trust,<br />
and although it’s not always<br />
been easy, I’m still so incredibly<br />
proud and grateful to wear my<br />
uniform and I look forward to<br />
what the future holds for all of us<br />
here within the EOC and across<br />
EEAST.”<br />
Philip Bygrave is a Make Ready<br />
Group lead for King’s Lynn and<br />
Peterborough, which prepares<br />
ambulances and other vehicles<br />
ready for deployment. He said:<br />
“Attending the service on behalf<br />
of EEAST was a great honour<br />
and it was humbling to be with so<br />
many people who have dedicated<br />
so much to the NHS. I have<br />
worked in the ambulance service<br />
for 23 years and was in patientfacing<br />
roles before joining the<br />
Make Ready Service at EEAST<br />
in 2020. Knowing that you are<br />
making a difference to patients’<br />
lives is extremely rewarding and<br />
makes you feel proud to work in<br />
the NHS.”<br />
Welsh <strong>Ambulance</strong><br />
Service awarded<br />
prestigious<br />
environmental<br />
management<br />
standard<br />
THE Welsh <strong>Ambulance</strong> Service<br />
has been recognised for its<br />
commitment to reduce its<br />
environmental footprint and<br />
improve its performance.<br />
The Trust has been awarded<br />
the prestigious ISO 14001<br />
Environmental Management<br />
Systems Standard by British<br />
Standards Institution after a<br />
rigorous five-day inspection of its<br />
environmental governance system.<br />
ISO 14001 is an internationally<br />
recognised standard for<br />
environmental management<br />
systems, which supports<br />
organisations in identifying,<br />
managing, monitoring and<br />
controlling environmental<br />
processes.<br />
The Welsh <strong>Ambulance</strong> Service<br />
is currently the only ambulance<br />
service in the <strong>UK</strong> to hold this<br />
standard.<br />
Richard Davies, the Trust’s<br />
Assistant Director of Capital<br />
and Estates, said: “To retain<br />
accreditation is a massive<br />
achievement.<br />
“It’s a validation of the great work<br />
headed by the Estates team<br />
and especially Environment and<br />
Sustainability Manager Nicci<br />
Stephens and Environment and<br />
Sustainability Support Officer<br />
Sharon Jones.<br />
“A massive thanks are owed to<br />
the team who have supported<br />
and delivered on this, we are all<br />
extremely proud.”<br />
The Trust introduced a<br />
catalogue of new initiatives in<br />
its bid to secure ISO 14001,<br />
which includes new plug-in<br />
hybrid rapid response cars to<br />
replace the older diesel-powered<br />
vehicles, 270 speed-limited<br />
non-emergency patient transport<br />
vehicles installed with solar<br />
panels to minimise the need for<br />
mains charging, continued the<br />
use of video conferencing to<br />
reduce travel time, emissions and<br />
cost, installed new renewable<br />
energy systems and reduced<br />
its reliance on fossil fuels by<br />
installing low carbon heating.<br />
Leading the work has been<br />
Environment and Sustainability<br />
Manager Nicci Stephens, who<br />
said: “I am so pleased to say that<br />
after five days of auditing, the<br />
Welsh <strong>Ambulance</strong> Service has<br />
kept the ISO 14001 accreditation<br />
for <strong>2023</strong>.<br />
“The accreditation provides<br />
assurance to the Trust’s<br />
management and employees, as<br />
well as external stakeholders that<br />
the environmental impacts of the<br />
Trust are being measured and<br />
improved.<br />
“The assessor noted that during<br />
their visit, the Trust demonstrated<br />
that the environmental<br />
management systems in place<br />
continue to support the strategic<br />
direction of the organisation<br />
and achieve objectives relating<br />
to improving environmental<br />
performance, which we are very<br />
proud of.<br />
“In order to support the Welsh<br />
Government’s ambition of a<br />
net zero carbon public sector<br />
by 2030, we have developed a<br />
decarbonisation plan and are<br />
working towards the NHS Wales<br />
decarbonisation target reduction<br />
of 34%.”<br />
The Trust was accredited following<br />
an audit which took place at a<br />
sample of stations and office<br />
buildings across Wales during May.<br />
16<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
Seamless Synchronisation<br />
Hands Free Resuscitation with the<br />
corpuls3 and corpulscpr.<br />
In the <strong>Ambulance</strong><br />
Emergency transport carries risk<br />
for the patient and the responding<br />
team. With synchronised therapy,<br />
the emergency team can remain<br />
seated whilst in transit. Rhythm<br />
control and shock delivery can be<br />
performed on the corpuls 3 while<br />
the medic is seated.<br />
In tight spaces<br />
Whether in a lift, a stairwell, or<br />
on tricky terrain, synchronised<br />
resuscitation means that therapy<br />
can continue where it wouldn’t<br />
have been possible before. Once<br />
in place, a medic can control the<br />
corpuls 3 monitor, defibrillator and<br />
CPR parameters of the corpuls cpr.<br />
In the air<br />
Patient access is extremely limited<br />
in air rescue. Thanks to the perfect<br />
interaction of the corpuls 3 with<br />
the corpuls cpr, movement within<br />
the cabin is reduced. Synchronised<br />
mechanical chest compressions<br />
can be given, without having to<br />
accept long hands-off times.<br />
• Shorter hands-off time.<br />
• Automated pre-shock compressions.<br />
• Can be used in manual and AED mode.<br />
• Increased safety & minimised interruptions.<br />
• Less resources required.<br />
• Easier operation.<br />
• Data transmission.<br />
• Post mission analysis.<br />
Learn more:<br />
Scan the QR code<br />
with your phone<br />
camera and click<br />
the link.<br />
Or visit:<br />
uqr.to/sync-cpr<br />
Attending the Emergency Services Show?<br />
Visit us at stand K150 to learn more.<br />
www.corpuls.co.uk<br />
Official <strong>UK</strong> supplier of corpuls and Weinmann<br />
medical devices and software.
ADVERTORIAL FEATURE<br />
Brand new<br />
ambulance service,<br />
IPRS MTS launched<br />
A brand-new specialist<br />
patient transport service IPRS<br />
MTS has recently launched<br />
operations in Gatwick, West<br />
Sussex, offering a wide-range<br />
of specialised ambulance<br />
transportation services across<br />
the United Kingdom and to<br />
and from Europe with plans<br />
for rapid expansion.<br />
IPRS MTS is the latest member of<br />
the IPRS Group, an organisation<br />
with over 27 years’ experience<br />
delivering a wide-range of awardwinning<br />
clinical products and<br />
services to both the public and<br />
private sectors.<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
A strong emphasis on clinical<br />
excellence, compliance, and an<br />
exceptional patient experience<br />
is at the heart of all IPRS<br />
Group services with IPRS MTS<br />
embracing this to provide a firstclass<br />
service to all clients and<br />
patients in their care.<br />
Martyn Jackson, CEO of the IPRS<br />
Group, is excited by the launch of<br />
IPRS MTS and is confident that<br />
the new start-up will be another<br />
successful member of the group.<br />
He said, “It’s very exciting to<br />
finally launch IPRS MTS as it’s<br />
been something we’ve been<br />
working on for a long time now<br />
in the background and it’s great<br />
that the news is out, and we have<br />
began delivering our services.<br />
We firmly believe that our<br />
experience in repatriation<br />
positions us favourably to build<br />
upon it through our new venture.<br />
We have already assembled a<br />
team with extensive expertise<br />
in this field, and I am greatly<br />
enthused about the growth<br />
prospects of this organisation.”<br />
IPRS MTS has developed<br />
four distinct medical transport<br />
services consisting of transfers of<br />
high-dependency patients from<br />
the ICU, secure transportation<br />
services for individuals suffering<br />
mental health issues, bariatric<br />
transfers for patients requiring<br />
medical assistance during and<br />
non-emergency repatriation<br />
services to and from Europe.<br />
IPRS MTS collaborate directly<br />
with NHS trusts, commissioning<br />
bodies, private ambulance<br />
services, and the general public<br />
to fulfil the unique transportation<br />
requirements of patients.<br />
The success of IPRS MTS will be<br />
built on three key pillars which all<br />
services will be delivered upon.<br />
Exceptional clinical quality, utilising<br />
technology and delivering services<br />
in a manner that is sustainable.<br />
Providing the highest standard of<br />
clinical care is key to IPRS MTS.<br />
Each member of their paramedic<br />
team is registered with the Health<br />
Practice Associates Council<br />
with all colleagues undergoing<br />
extensive training upon joining<br />
to ensure that all patients under<br />
their care receive an optimal<br />
level of care and compassion in<br />
every journey.<br />
Technology and innovation<br />
lie at the core of IPRS MTS’s<br />
operations. To facilitate a safe<br />
and comfortable service, they<br />
possess a fleet of ambulances<br />
equipped with state-of-the-art<br />
medical equipment utilised by<br />
their paramedics to provide<br />
exemplary care. For the secure<br />
transportation of patients with<br />
mental health conditions, they<br />
employ vehicles fitted with<br />
Home Office Category B cells<br />
and seating arrangements that<br />
allow for assessments and<br />
conversation throughout the<br />
journey. All services undergo<br />
rigorous auditing to preserve<br />
the highest quality standards<br />
possible and maintain patient<br />
satisfaction.<br />
Delivering services is a<br />
sustainable manner is important<br />
to IPRS MTS, the organisation<br />
will be constantly looking for<br />
more sustainable ways to deliver<br />
their services and have aligned<br />
themselves to the Greener NHS<br />
Programme. Sustainability is<br />
extremely important across the<br />
IPRS Group who have planted<br />
over 3,000 trees, capturing more<br />
than 1,200 tonnes of CO2.<br />
Phil Bayliss, the Director of<br />
IPRS MTS, is excited by the<br />
launch saying, “I am thrilled to<br />
announce the launch of IPRS<br />
MTS. We are enthusiastic about<br />
delivering our services to the<br />
market and truly believe that our<br />
offerings are unparalleled. We<br />
align ourselves with the Greener<br />
NHS program, embrace cuttingedge<br />
technology, and maintain a<br />
strong focus on clinical expertise.<br />
Being a part of IPRS MTS is truly<br />
exciting, and I eagerly anticipate<br />
the growth of the organisation in<br />
the months and years ahead.”<br />
IPRS MTS is currently recruiting<br />
for a variety of clinical roles<br />
at varying levels of expertise.<br />
Despite IPRS MTS being a new<br />
company, they are part of IPRS<br />
Group who have won numerous<br />
employer awards including<br />
winning Best Employer in the<br />
Healthcare Industry at the 2021<br />
Best Employers Eastern Region<br />
along with being named a<br />
Platinum Employer.<br />
18<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWLINE<br />
Chief Paramedic<br />
awarded top<br />
ambulance medal in<br />
the King’s Birthday<br />
Honours<br />
The Chief Paramedic at<br />
London <strong>Ambulance</strong> Service<br />
has been awarded His Majesty<br />
the King’s <strong>Ambulance</strong> Service<br />
Medal for distinguished service<br />
as part of the monarch’s<br />
Birthday Honours.<br />
A paramedic since 2002, Dr John<br />
Martin has had a phenomenal<br />
career at the forefront of the field,<br />
dedicating his life to improving<br />
patient care and developing the<br />
expertise of clinicians within the<br />
profession.<br />
Dr Martin joined the London<br />
<strong>Ambulance</strong> Service in March<br />
2021 in a newly-created Chief<br />
Paramedic role which brought<br />
together responsibility for both<br />
clinical quality at the Trust and<br />
for ensuring paramedics and<br />
ambulance clinicians have access<br />
to world-class training, education<br />
and professional development.<br />
With over 650 apprentices at<br />
the Service, John has helped<br />
LAS become the biggest<br />
apprentice provider in the NHS<br />
and spearheaded work to<br />
protect our staff from violence<br />
and aggression, including the<br />
installation of crew safety systems<br />
and body worn cameras.<br />
LAS Chief Executive Daniel<br />
Elkeles said: “John epitomises<br />
what it is to be a highly<br />
compassionate, respected and<br />
inclusive NHS leader. He also<br />
exemplifies what it is to be a<br />
professional paramedic, using<br />
every opportunity to develop the<br />
profession for the benefit of staff<br />
and the patients they care for.<br />
“His leadership and foresight has<br />
turbocharged the development<br />
of the country’s paramedic<br />
workforce, improving the quality<br />
of care received by thousands<br />
of patients across the country.<br />
These achievements will deliver<br />
lasting improvements for the<br />
paramedic profession.”<br />
Dr Martin has also been President<br />
of the College of Paramedics<br />
since 2017, and has been active<br />
in developing the College of<br />
Paramedics for many years, all of<br />
which he has volunteered to do in<br />
his own time.<br />
In May <strong>2023</strong>, he finished his<br />
second term as the College’s<br />
president. Under his tenure,<br />
membership has grown by<br />
2,000% and the College is close<br />
to achieving a Royal Charter<br />
and continuous professional<br />
development is now a mandatory<br />
part of paramedic practice.<br />
Dr John Martin said: “I am hugely<br />
honoured and humbled to receive<br />
this medal on behalf of London<br />
<strong>Ambulance</strong> Service and the<br />
paramedic profession.<br />
“I’m proud to have been a<br />
paramedic for over 20 years<br />
and work with such dedicated<br />
and talented clinicians at LAS,<br />
ambulance services and the<br />
wider NHS to ensure that our<br />
patients get the best possible<br />
care in their time of need.”<br />
In 2006 Dr Martin led the<br />
curriculum guidance development<br />
for paramedics, paving the way<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
19
Specialist<br />
Patient Transport<br />
Services<br />
Our Services:<br />
High Dependency Transfers<br />
Secure Mental Health Transfers<br />
Repatriation<br />
Bariatric Transfers<br />
www.IPRSMTS.com
COMPANY NEWS<br />
NEWLINE<br />
for enhanced education and<br />
paramedic practice, which is now<br />
Webasto<br />
embedded across<br />
heating<br />
the United<br />
and Kingdom. air conditioning<br />
systems<br />
His other roles in the NHS<br />
have included Consultant<br />
Webasto heating and air<br />
conditioning<br />
Paramedic at East<br />
systems<br />
of England<br />
are<br />
used<br />
<strong>Ambulance</strong><br />
by front<br />
Service,<br />
line fleets<br />
and director<br />
with<br />
roles at<br />
systems<br />
Cambridgeshire<br />
designed<br />
and<br />
to<br />
Peterborough<br />
meet exacting,<br />
NHS Foundation<br />
tailored<br />
requirements. Trust – where he Our led the products Trust’s<br />
are response designed to the to COVID-19 provide<br />
exceptional pandemic. performance and<br />
service.<br />
<strong>Ambulance</strong> crews<br />
Not only do we provide<br />
use hard-hitting<br />
the virtual crew, we reality can also achieve to a<br />
reduction better in spot idling times signs which of<br />
in turn lowers fuel consumption,<br />
sexual abuse and<br />
decreases overall operating<br />
domestic violence<br />
comfortable working climates for<br />
costs and helps us to remain<br />
<strong>Ambulance</strong> crews are using<br />
virtual reality (VR) headsets<br />
to immerse themselves in<br />
traumatic situations such as<br />
domestic focused towards violence improving to better the<br />
prepare environment. them for real-life<br />
situations where vulnerable<br />
people Webasto are products in need have of help. been a<br />
mainstay for one of the largest<br />
London fleets in the <strong>Ambulance</strong> <strong>UK</strong> for many Service years,<br />
(LAS) based has on an developed impressive training reliability<br />
using record headsets and ease which of operational are loaded<br />
with function. true-to-life scenarios to<br />
help clinicians understand the<br />
impact A parts of locator various and types replacement of abuse<br />
and part trauma service are on the available physical to ensure and<br />
mental your own wellbeing people get of vulnerable the best<br />
adults operational and children. efficiency from the<br />
fleet. Clear and concise training<br />
The material, simulated with regular scenarios updates include are<br />
scenes also offered domestic either at violence, Webasto’s<br />
sexual training exploitation, academy, or drug at your abuse,<br />
child own depot grooming, locations modern to suit slavery your<br />
and needs. gang intimidation and give<br />
users a 360 degree view.<br />
For many large fleets, demands<br />
Alan placed Taylor, on both Head crew of and vehicle<br />
Safeguarding, said: “The<br />
immersive experience allows<br />
ambulance staff to see things<br />
from a patient’s perspective and<br />
to help understand the fear so<br />
they can be truly extremely empathise arduous, with their so it<br />
patient. is of vital importance that both<br />
remain fully optimised to respond<br />
“This when gives it really our matters. crews a When greater<br />
understanding considering these of how demands vulnerable and<br />
patients agreeing may on a display build specification signs of<br />
trauma for your and frontline means ambulance, they can<br />
better rapid response, protect children and patient and adults<br />
at transport risk.” service vehicles we<br />
will only specify products that<br />
<strong>Ambulance</strong> meet the exacting clinicians standards are often<br />
the and first performance people to expected identify a from<br />
vulnerable Webasto. adult or child and they<br />
make safeguarding referrals to<br />
the<br />
Webasto<br />
appropriate<br />
is the largest<br />
agency<br />
producer<br />
if they<br />
are concerned about abuse or<br />
of auxiliary heaters and air<br />
neglect.<br />
conditioning in Europe. Let us<br />
take you through the options.<br />
LAS is the first ambulance<br />
For an informal chat, call David<br />
service in the country to use<br />
Stafford on 01302 381141<br />
the technology for safeguarding<br />
or email david.stafford@<br />
training.<br />
webasto.com<br />
Paramedic Patrick Hunter<br />
(pictured) said: “I thought I was<br />
unshockable but this was really<br />
sobering to watch. I was shocked<br />
but necessarily so. Seeing things<br />
Not only do we<br />
from a child’s perspective helps<br />
us to understand how integral<br />
provide comfortable<br />
safeguarding is to our practice.<br />
working climates for<br />
the crew, we can also<br />
“Sometimes children won’t<br />
engage with us or might seem<br />
achieve a reduction<br />
rude but this training shows that<br />
in idling times<br />
behind certain behaviour there<br />
may be a very vulnerable child in<br />
which in turn lowers<br />
need of our help.”<br />
fuel consumption,<br />
The videos and technology<br />
decreases overall<br />
were developed by a company<br />
operating costs and<br />
called Antser, one of the<br />
leading health and social care<br />
helps us to remain<br />
technology providers in the <strong>UK</strong>.<br />
focused towards<br />
improving the<br />
environment.<br />
The advantages of<br />
Engine-off Technology<br />
AMBULANCE <strong>UK</strong> - JUNE<br />
A ready-for-duty driver at all times<br />
n Extreme cold is exceptionally strenuous and<br />
exhausting for vehicle drivers. Engine-Off<br />
Heating systems assure a pleasant work<br />
climate and maximum comfort, even in the<br />
coldest conditions.<br />
Environmentally friendly<br />
n The automatic Engine-Off Technology<br />
benefits the environment too. In a double<br />
sense. Thanks to the many engine pauses -<br />
and to the fact that only this new technology<br />
makes use of environment friendly start-stop<br />
systems possible. With a constantly warm<br />
engine, restart comes off without a hitch.<br />
Diesel particulate filters stay clean<br />
longer<br />
n When idling, the combustion temperature<br />
for efficient operation of the filters is too<br />
low. So they soil and wear out much faster.<br />
Engine-Off Climate systems prolong the life<br />
of particulate filters.<br />
Up to 90% less fuel consumption<br />
n In comparison with idling, considerably less<br />
fuel is consumed when the engine is not<br />
running. This can pay off in savings of up<br />
to 90%.<br />
Less wear-and-tear, less<br />
maintenance<br />
n Less idling also means less engine wear and<br />
tear. Engine running times are reduced and,<br />
due to fewer operating hours (up to 60%),<br />
less maintenance is required while achieving<br />
higher resale value.<br />
www.webasto.co.uk<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
94<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
21
You live it. We built it.<br />
The industry’s first connected ambulance cot.<br />
Nobody knows what works in the field better than you. That’s why<br />
we reimagined our proven design to redefine your partner on scene—<br />
focusing on what matters most to help you get the job done.<br />
Introducing Stryker’s new Power-PRO TM 2<br />
powered ambulance cot.<br />
Lighter. Faster. Stronger.*<br />
*In comparison with Power-PRO XT<br />
This document is intended solely for the use of healthcare professionals. A healthcare professional must always rely on his or her own<br />
professional clinical judgment when deciding whether to use a particular product when treating a particular patient. Stryker does not<br />
dispense medical advice and recommends that healthcare professionals be trained in the use of any particular product before using it.<br />
The information presented is intended to demonstrate the breadth of Stryker product offerings. A healthcare professional must always<br />
refer to the package insert, product label and/or instructions for use before using any Stryker product. Products may not be available in all<br />
markets because product availability is subject to the regulatory and/or medical practices in individual markets. Please contact your Stryker<br />
representative if you have questions about the availability of Stryker products in your area. Stryker Corporation or its divisions or the<br />
corporate affiliated entities own, use or have applied for the following trademarks or service marks: Power-LOAD, Power-PRO, Power-PRO 2.<br />
All other trademarks are trademarks of their respective owners. Class I, Stryker.<br />
3800 E. Centre Avenue<br />
Portage, MI 49002 USA<br />
stryker.com<br />
Copyright © 2022 Stryker.<br />
SMACC Number: 2022-32460<br />
02/2022
NEWLINE<br />
The scenarios are filmed using<br />
actors and will help clinicians<br />
when they make safeguarding<br />
referrals and ultimately help<br />
protect patients.<br />
LAS is hoping bespoke scenarios<br />
could also be developed for call<br />
handlers as they can also help<br />
identify patients at risk when<br />
taking 999 calls.<br />
The Service is also considering<br />
using VR technology for<br />
clinical education. It already<br />
has immersive training suites<br />
at its education centres where<br />
simulated scenarios play out.<br />
Two EEAST clinicians<br />
have talked about<br />
how being a reservist<br />
in the armed forces<br />
has enhanced both<br />
their clinical skills<br />
and developed their<br />
confidence and<br />
professional abilities.<br />
Gavin Smith, a paramedic and<br />
former Leading Operations<br />
Manager for EEAST has also<br />
enjoyed a career in both the<br />
Army and the Royal Air Force<br />
as a regular and reservist<br />
which has spanned 33 years.<br />
Since joining the Trust in 2015, he<br />
has maintained a position within<br />
the Royal Auxiliary Air Force,<br />
initially in a Chemical, Biological,<br />
Radiological and Nuclear (CBRN)<br />
specialist role, and more latterly,<br />
as a field gunner in an Immediate<br />
Operational Response (IOR) role.<br />
“These are just a few of the skills<br />
that my service career has given<br />
me,” said Gavin, “Others include<br />
linguistics, cultural awareness,<br />
intelligence, communications,<br />
investigatory, report generation<br />
as well as a myriad of others<br />
- nearly all have been directly<br />
transferable or have found some<br />
use during my time within the<br />
<strong>Ambulance</strong> Service<br />
“Personally, my journey through<br />
the <strong>Ambulance</strong> Service has been<br />
as a direct result of my time within<br />
the armed forces, and I have<br />
found that EEAST have been<br />
truly supportive in allowing me to<br />
continue both roles side-by-side.<br />
Sadly, Gavin who now works in<br />
an investigation role for EEAST,<br />
said he will be stepping down<br />
as a reservist shortly, but he<br />
would recommend it to others<br />
considering becoming a reservist:<br />
“Given the choice, I would<br />
continue forever, however, there<br />
of course comes a point where<br />
the mind is willing but the body<br />
less so!<br />
“Sometimes the journey to<br />
become a reservist may be<br />
arduous, other times it may be<br />
fun, but at all times, you will<br />
become part of a camaraderie<br />
and a team that is like no other -<br />
and when you return to your dayto<br />
day role, the skills you learn will<br />
be as valued as those that you<br />
already possess and will bring to<br />
your reservist role - whatever that<br />
may be!”<br />
Mia Gill has been working for<br />
EEAST since 2016. As a reservist<br />
with the Royal Army Medical<br />
Corps she is a recognised<br />
paramedic and a combat medical<br />
technician (CMT (P)).<br />
She said:<br />
“I am incredibly proud to be a<br />
part of both organisations which<br />
have had a positive impact on<br />
my life and as a professional. I<br />
feel both roles really complement<br />
A WORLD OF COMFORT<br />
CLIMATE CONTROLLED HEALTHCARE<br />
Customised vehicle heating and cooling solutions from Eberspacher.<br />
Simple to use, effective in performance and reliable in operation.<br />
On the move comfort for patient and healthcare professionals.<br />
See us on Stand No. E150 at The Emergency Services Show, NEC<br />
www.eberspaecher-climate.com<br />
Find your<br />
nearest Dealer<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
23
MAKE A<br />
LEGENDARY<br />
MOVE<br />
Every day is different as a St John WA paramedic, and we have multiple<br />
opportunities available for qualified and experienced <strong>Ambulance</strong> Paramedics<br />
to come join us in beautiful Western Australia.<br />
The offer:<br />
• Visa application support<br />
• Paid for one-way economy airline ticket<br />
• Accommodation upon arrival to<br />
Western Australia<br />
• Additional relocation costs covered<br />
The location:<br />
• Diverse landscape means diverse daily routine<br />
• Safe and stable economy<br />
• Over two-thirds of the year is beautifully clear<br />
and sunny<br />
• Incredible work/life balance with world-class<br />
dining, festivals and more<br />
Don’t have current Australian<br />
working rights? No problem!<br />
For candidates to successfully be employed as<br />
an <strong>Ambulance</strong> Paramedic, they must meet the<br />
following minimum requirements:<br />
• Professional registration as a Paramedic with<br />
the Paramedicine Board of Australia (AHPRA)<br />
or willingness to obtain.<br />
• Recent experience employed and working<br />
within a jurisdictional ambulance service in<br />
Australia or internationally (St John New<br />
Zealand or London <strong>Ambulance</strong> Service for<br />
example) as a paramedic for at least two years.<br />
• Hold a full driver’s license with no restrictions.<br />
Successful candidates are required to obtain<br />
a light rigid driver’s license within the first six<br />
months of employment. Costs associated with<br />
obtaining the required driver’s license are the<br />
responsibility of the candidate.<br />
• Candidates that do not hold current Australian<br />
working rights, must meet the visa eligibility<br />
requirements, as outlined by the Department<br />
of Home Affairs.<br />
Ready to make a<br />
legendary move?<br />
Go on, a career with loads of diversity<br />
and an amazing lifestyle is waiting!<br />
Search stjohnwa.com.au/directentry<br />
Scan to learn more:
NEWLINE<br />
each other and EEAST are so<br />
supportive in allowing me time to<br />
conduct my military exercises.<br />
“The military has helped me<br />
gain confidence and grow into<br />
an individual with integrity and<br />
discipline. This has helped me in<br />
my civilian role as a paramedic<br />
as I have the confidence to air<br />
my opinions, and act as a better<br />
advocate for my patients. I have<br />
also developed my trauma skills<br />
greatly, which I have utilised when<br />
attending patients and mentoring<br />
students and colleagues. I have<br />
evolved from a timid young<br />
individual to a confident and<br />
knowledgeable clinician.”<br />
Pioneering mental<br />
health joint response<br />
unit shortlisted<br />
for prestigious<br />
NHS Parliamentary<br />
Awards<br />
A ground-breaking scheme at<br />
London <strong>Ambulance</strong> Service<br />
(LAS) which pairs a mental<br />
health professional with a<br />
paramedic to treat people<br />
experiencing a mental health<br />
crisis has been shortlisted<br />
for the prestigious NHS<br />
Parliamentary Awards.<br />
The Service’s mental health joint<br />
response unit allows a more<br />
tailored response to a patient’s<br />
mental and physical needs,<br />
ensuring vulnerable patients get<br />
the treatment they need at home<br />
or through local community<br />
services, and wherever<br />
possible avoids unnecessary<br />
visits to hospital emergency<br />
departments.<br />
More than 17,000 people have<br />
been helped by this specialised<br />
team since January 2020 when<br />
the service expanded across<br />
the capital. Ensuring equity of<br />
access to care is a key focus at<br />
LAS and, thanks to the expertise<br />
of this joint team, just 16% of<br />
patients experiencing a mental<br />
health crisis have needed to<br />
be taken to an emergency<br />
department.<br />
Alison Blakely, Director of<br />
Clinical Pathways and Clinical<br />
Transformation at London<br />
<strong>Ambulance</strong> Service, said:<br />
“I’m delighted that the team<br />
have been nominated for their<br />
incredible work. Thanks to their<br />
expertise, we can ensure that<br />
we can provide a response that<br />
meets each patients’ individual<br />
needs and sees their mental<br />
health treated with the same<br />
level of importance as their<br />
physical wellbeing.<br />
“This importantly helps patients<br />
receive the best possible care<br />
away from busy emergency<br />
departments that may not be<br />
conductive to their recovery.”<br />
The unit, which was launched as<br />
a single car in south east London<br />
in November 2018 before<br />
expanding to six response cars,<br />
was nominated for the honour by<br />
eight London MPs.<br />
Dr Rosena Allin-Khan MP,<br />
Shadow Minister for Mental<br />
Health and Labour MP for<br />
Tooting, who nominated the<br />
team for the award, said:<br />
“I am thrilled to see the London<br />
<strong>Ambulance</strong> Service’s mental<br />
health joint response unit has<br />
been shortlisted for an award.<br />
Every patient deserves the<br />
very best standard of care,<br />
and through this team, patients<br />
experiencing a mental health<br />
crisis are being directed to the<br />
services that work best for<br />
them. This is a well-deserved<br />
recognition of the brilliant<br />
efforts that these mental health<br />
professionals put in every day.”<br />
Members of the mental health<br />
team also work in our 999<br />
control rooms, supporting<br />
colleagues answering calls<br />
from members of the public<br />
who are experiencing a mental<br />
health crisis, guiding teams<br />
who are dispatching LAS crews<br />
to patients, and providing<br />
patients with direct telephone<br />
assessments.<br />
The team works closely with<br />
local mental health trusts to<br />
ensure the patients they support<br />
receive the care they need from<br />
community services in the most<br />
efficient way possible. The<br />
scheme has benefited from close<br />
collaboration between LAS and<br />
mental health trusts to ensure<br />
the patient gets the right care in<br />
the right place, first time.<br />
The NHS Parliamentary Awards<br />
launched in 2018 to celebrate<br />
the NHS’ 70 birthday and<br />
recognise the outstanding<br />
contribution of staff, volunteers<br />
and others working in the health<br />
and care sector. Now in its sixth<br />
year, the awards have been an<br />
overwhelming success with<br />
more than 700 nominations<br />
being submitted by over half of<br />
MPs representing constituencies<br />
in England last year alone.<br />
The MPs who nominated the<br />
mental health response team<br />
are: Ellie Reeves (Labour,<br />
Lewisham West and Penge), Lyn<br />
Brown (Labour, West Ham), Sir<br />
Keir Starmer (Labour, Holborn<br />
and St Pancras), Catherine<br />
West (Labour, Hornsey and<br />
Wood Green), Feryal Clark<br />
(Labour, Enfield North), Stephen<br />
Hammond (Conservative,<br />
Wimbledon), Rosena Allin-Khan<br />
(Labour, Tooting) and Marsha De<br />
Cordova (Labour, Battersea).<br />
The winners will be announced<br />
at an Awards Ceremony on the<br />
health service’s 75th anniversary<br />
on Wednesday 5 July <strong>2023</strong>, to<br />
which all nominees, their relevant<br />
MPs and other key figures will<br />
be invited. The ceremony will be<br />
held at the Queen Elizabeth II<br />
Centre in Westminster.<br />
SECAmb thanks<br />
colleagues and their<br />
families this Armed<br />
Forces Day<br />
South East Coast <strong>Ambulance</strong><br />
Service NHS Foundation<br />
Trust (SECAmb) would like<br />
to pay tribute and thank all<br />
colleagues and their families<br />
with links to the armed forces.<br />
The Trust is proud to have close<br />
links with the armed forces with<br />
of its staff and volunteers either<br />
having served in a previous<br />
career or continuing to serve<br />
as a reservist alongside their<br />
ambulance service role.<br />
SECAmb signed up to the<br />
Armed Forces Covenant<br />
in 2018. The covenant is a<br />
commitment to member of<br />
the reserves, armed forces,<br />
veterans, or family members<br />
and outlines how the Trust will<br />
support them, officially, as<br />
a military-friendly employer.<br />
Further details on the<br />
covenant can be found on the<br />
Trust’s website here: Armed<br />
Forces Covenant - NHS South<br />
East Coast <strong>Ambulance</strong> Service<br />
(secamb.nhs.uk)<br />
In 2022, SECAmb was proud<br />
to achieve an Armed Forces<br />
Silver Award. The award is a<br />
progression on the Bronze<br />
Award it was granted in 2018/19<br />
and is evidence of the Trust’s<br />
commitment to employing and<br />
supporting those with a current<br />
or previous role in the armed<br />
forces.<br />
SECAmb Chief Executive,<br />
Simon Weldon, said: “I would<br />
like to thank each and every<br />
colleague who has a previous<br />
link to the armed forces or who<br />
is a reservist. We are proud<br />
of our strong links with the<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
25
www.vcs-limited.com<br />
0800 304 7958<br />
The next generation of front-line<br />
emergency service vehicles<br />
Manufactured in the <strong>UK</strong>'s largest dedicated emergency vehicle<br />
manufacturing facility.<br />
Capacity to design, manufacture and deliver over 1500 vehicles<br />
annually to NHS trusts across the country.<br />
New dedicated R&D facility doubles our engineering capability.<br />
In-house academy dedicated to the training of new and existing staff<br />
to maintain our exceptional vehicle standards.
NEWLINE<br />
armed forces and I am keen to<br />
ensure this continues and that<br />
our associations are further<br />
strengthened in the years ahead.<br />
“I would also like to thank the<br />
families of our colleagues who have<br />
links to the armed forces. They play<br />
a vital and difficult role in supporting<br />
their loved ones in managing the<br />
dual challenge of managing a career<br />
in both sectors.”<br />
AMBULANCE<br />
WORKERS SUFFER<br />
AT LEAST 9,500<br />
VIOLENT ATTACKS<br />
IN RECENT YEARS,<br />
GMB INVESTIGATION<br />
SHOWS<br />
Almost 1,250 recorded sexual<br />
assaults and true number likely<br />
to be far higher, says GMB Union<br />
South East Coast <strong>Ambulance</strong><br />
Service NHS Foundation Trust,<br />
(SECAmb), is to trial three fullyelectric<br />
vehicles as part of its plans<br />
to reduce carbon emissions and<br />
introduce zeroemission vehicles<br />
on to its fleet.<br />
<strong>Ambulance</strong> workers been subject<br />
to at least 9,500 violent attacks<br />
in the line of duty over the last<br />
five years, a GMB investigation<br />
has revealed.<br />
Attacks, which saw blue light<br />
crews bitten, head-butted, spat<br />
at and struck with weapons, took<br />
place more than 9,565 times<br />
from the financial year 2017/18<br />
to 21/22. [1]<br />
A total of 1,248 of these were<br />
sexual assaults.<br />
The true numbers of assaults<br />
are likely to be far higher as only<br />
eight out of 13 ambulance trusts<br />
across England, Scotland, Wales<br />
and Northern Ireland responded<br />
to GMB’s Freedom of Information<br />
Act request.<br />
<strong>Ambulance</strong> workers took to<br />
the stage at GMB’s annual<br />
congress in Brighton on Sunday<br />
4 June to discuss the attacks<br />
they face daily, as well as the<br />
national NHS strikes they took<br />
part in and much needed<br />
reform to ambulance worker<br />
retirement age.<br />
GMB’s ambulance members<br />
successfully changed the law in<br />
2018 when the Assaults Against<br />
Emergency Workers (Offences)<br />
Act made assaults on ambulance<br />
workers an aggravating factor for<br />
sentencing. [2]<br />
Rachel Harrison, GMB National<br />
Secretary, said:<br />
“<strong>Ambulance</strong> workers go to work<br />
every day to save lives.<br />
“Despite this, thousands of them<br />
are bitten, attacked, spat at and<br />
even sexually assaulted.<br />
“No one should have to put up<br />
with that, least of all those who<br />
are there to protect us.<br />
“GMB members helped change<br />
the law but more needs to be<br />
done.<br />
“We demand full enforcement<br />
of the Protect the Protectors<br />
legislation, investment in better<br />
systems to flag offenders, and<br />
much better support for the<br />
victims of violence.”<br />
[1] <strong>Ambulance</strong> service<br />
2018/2019 1,597<br />
2019/20201,924<br />
2020/2021 1,871<br />
2021/2022 2,141<br />
2022/<strong>2023</strong> 2,032<br />
Total9,565<br />
The EMERGENCY SERVICES SHOW <strong>2023</strong> Stand D180<br />
THE POWER TO DEMO<br />
Come and see the developments on the VIPER Stretcher<br />
and Loading System and the latest VENICE PowerTraxx,<br />
also this year the COMPACT PowerTraxx will be in action -<br />
the next evolution <strong>Ambulance</strong> Stair Chair and already under<br />
evaluation by various NHS Trusts.<br />
OUR NEW RESCUE SLED THE XTRIC8<br />
& THE TIROL WHEEL KIT BOTH READY<br />
FOR ACTION<br />
For complete product information and specifications<br />
go to ferno.com email sales.uk@ferno.com call +44 (0) 1274 851 999<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
27
NEWLINE<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
*SWAST provided figures per<br />
calendar year, rather than<br />
financial year<br />
[2] MPs back tougher measures<br />
in Protect the Protectors Bill<br />
| GMB<br />
Heroic acts, heartwarming<br />
tales and<br />
long service were<br />
celebrated at West<br />
Midlands <strong>Ambulance</strong><br />
Service’s annual<br />
awards ceremonies<br />
on Thursday June 15.<br />
The Staff Long Service &<br />
Excellence Awards and<br />
Excellence in the Community<br />
Awards were held at The<br />
Copthorne Hotel in Brierley<br />
Hill with almost 700 guests<br />
attending across the two<br />
events. Guests included the<br />
Deputy-Lieutenant of the West<br />
Midlands, Ian Sargeant, and<br />
the High Sheriff of the County<br />
of West Midlands, Wade Lyn.<br />
This year, 56 members of staff<br />
were recognised for having given<br />
20 years of service to WMAS,<br />
15 staff were commended for<br />
25 years’ service, 14 received<br />
certificates for 30 years’ service,<br />
three members of staff were<br />
honoured for 35 years in the<br />
Trust whilst two celebrated<br />
the incredible landmark of 40<br />
years of service. Other awards<br />
to be handed out included<br />
Chief Officer Commendations,<br />
Student Paramedic of the Year,<br />
Mentor Awards, Apprenticeship<br />
Awards, Community Initiative<br />
and Partnership Awards; St John<br />
<strong>Ambulance</strong> Awards; CFR Long<br />
Service Awards and the CFR of<br />
the Year.<br />
Trust Chief Executive, Anthony<br />
Marsh, said: “In the aftermath<br />
of the pandemic, the continuing<br />
cost of living crisis and everything<br />
else that is presenting us all with<br />
CFR Volunteer of the Year, Jean Morgan<br />
(Credit: West Midlands <strong>Ambulance</strong> Service ).<br />
challenges at the moment, it is<br />
fantastic to have the opportunity<br />
to celebrate some of the<br />
incredible achievements of our<br />
staff, volunteers and members of<br />
the public.<br />
“We are extremely lucky to have<br />
such a professional workforce<br />
and team of volunteers who have<br />
a desire to always do their very<br />
best for the patient.<br />
“There were so many stories of<br />
people going above and beyond,<br />
in all sorts of situations, and to<br />
everyone who was recognised<br />
at these fantastic events, I would<br />
like to say a big well done, and<br />
thank you.”<br />
Deputy-Lieutenant of the West<br />
Midlands, Ian Sargeant, said:<br />
“Being at the awards made me<br />
extremely happy. There are lots<br />
of others words I could use here,<br />
but ‘happy’ is the right one.<br />
“That is because an organisation<br />
such as West Midlands<br />
<strong>Ambulance</strong> Service only works if<br />
everybody comes together, from<br />
those on the frontline to those<br />
behind the scenes, and everyone<br />
in between.<br />
“We’ve heard about tales of<br />
commitment to care, loyalty,<br />
bravery and dedication and it was<br />
an honour to be present to see<br />
some outstanding members of<br />
staff recognised.”<br />
High Sheriff of the County of<br />
West Midlands, Wade Lyn, said:<br />
“It is so important people are<br />
recognised for the excellence<br />
they show, and we have seen<br />
people from across the region<br />
celebrated, which is fantastic.<br />
“There are so many selfless<br />
people recognised at these<br />
events, all of whom are a real<br />
inspiration to their communities.<br />
By celebrating heroes we<br />
recognise the positive impact they<br />
make and encourage others to<br />
follow in their footsteps, which is<br />
so important. Well done to you all.”<br />
Prof Ian Cumming, WMAS<br />
Chairman, said: “It is important<br />
we recognise our staff, volunteers<br />
and members of the community<br />
because they all do remarkable<br />
things, day in, day out, despite the<br />
NHS facing some of the toughest<br />
challenges every seen. I send a<br />
huge and heartfelt thank you to<br />
them all for everything they do.”<br />
The Trust’s awards were<br />
sponsored by Coventry<br />
University, University of<br />
Wolverhampton, University of<br />
Worcester, Mills and Reeve,<br />
Medskills Academy, Birmingham<br />
City University, Jays Sourcing,<br />
Staffordshire University, VCS Ltd,<br />
DS Medical, G4S, Advantage<br />
Storing and Handling Ltd and<br />
Defibshop.<br />
SCAS re-signs Armed<br />
Forces Covenant<br />
South Central <strong>Ambulance</strong><br />
Service NHS Foundation<br />
Trust (SCAS) has reiterated<br />
its commitment to support<br />
members of the armed<br />
forces community, including<br />
reservists and veterans, by<br />
signing up once again to the<br />
Armed Forces Covenant.<br />
SCAS was the first ambulance<br />
trust in the country to sign up to<br />
the covenant in 2014 and a formal<br />
re-signing took place at the<br />
Trust’s North Harbour Resource<br />
Centre in Portsmouth on<br />
Wednesday, 5 July. Signatories<br />
to this latest commitment<br />
were Dr John Black, medical<br />
director for SCAS and retired<br />
lieutenant colonel, and Surgeon<br />
Commodore Stuart Collett<br />
CBE KHP.<br />
By signing the covenant,<br />
organisations give a formal<br />
commitment to ensure that<br />
members of the armed<br />
forces community are never<br />
disadvantaged through service life.<br />
Serving personnel, veterans and<br />
their families can sometimes be<br />
affected by the frequent house<br />
moves, separation from loved<br />
ones and support networks,<br />
and unfamiliarity with civilian life<br />
meaning they can find themselves<br />
on the back foot when accessing<br />
public goods and services, such<br />
as healthcare.<br />
Dr Black said: “It was a privilege<br />
to once again sign the Armed<br />
Forces Covenant on behalf of<br />
SCAS as a demonstration of our<br />
support to serving personnel,<br />
veterans, reservists and their<br />
families.<br />
“As well as taking into account<br />
the needs of the armed forces<br />
community in the development<br />
of our services and policies,<br />
I am also delighted that we<br />
continue to offer veterans and<br />
reservists a range of employment<br />
opportunities within SCAS.”<br />
28<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWLINE<br />
The covenant was signed at the<br />
end of a recruitment event hosted<br />
at the North Harbour Resource<br />
Centre by SCAS and the Career<br />
Transition Partnership (CTP).<br />
The CTP has been the official<br />
provider of resettlement support<br />
for leavers from the Armed<br />
Forces for over 20 years.<br />
At the event, SCAS opened its<br />
doors to serving members of<br />
the armed forces community as<br />
well as recent leavers, who were<br />
able to hear about the career<br />
opportunities in the emergency,<br />
NHS 111, patient transport and<br />
support services that SCAS<br />
provides. They were also able<br />
to speak to a number of military<br />
veterans who had already made<br />
the transition into SCAS and<br />
were enjoying successful and<br />
rewarding second careers.<br />
Laura Farrow, recruitment<br />
manager and military champion<br />
at SCAS, said: “Thank you to<br />
everyone who took the time to<br />
visit and from the conversations<br />
I had with attendees, people left<br />
with a deeper understanding<br />
about the services we provide<br />
and were excited about the<br />
opportunities we can offer them<br />
after they have finished their<br />
military service.<br />
“SCAS has over 150 veterans,<br />
reservists and military champions<br />
working in the organisation,<br />
some of whom enjoyed spending<br />
time showing visitors around our<br />
vehicles and equipment, and<br />
talking to them about their own<br />
real life experiences.<br />
“I am sure that today’s event,<br />
along with others we have<br />
planned, and the formal re-signing<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
29
NEWLINE<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
of the Armed Forces Covenant will<br />
continue to keep SCAS at the front<br />
of many people’s minds when<br />
considering a career after leaving<br />
the armed forces.”<br />
Welsh <strong>Ambulance</strong><br />
Service colleagues<br />
praised for long<br />
service<br />
THE Welsh <strong>Ambulance</strong> Service<br />
celebrated its long-serving<br />
staff and volunteers at an<br />
awards ceremony in North<br />
Wales yesterday.<br />
Colleagues with 20, 30, 40<br />
and 50 years of service were<br />
presented with medals at<br />
Deganwy’s Quay Hotel in an<br />
event to recognise length of<br />
service.<br />
Colleagues with 20 years<br />
in the Emergency Medical<br />
Service were also presented<br />
with a Long Service and Good<br />
Conduct Medal by the King’s<br />
representative in Clwyd, High<br />
Sheriff Kate Hill-Trevor.<br />
Among the recipients at<br />
yesterday’s event was urgent care<br />
assistant Trefor Lloyd Jones from<br />
Caernarfon, who was recognised<br />
for a half-century of service.<br />
Trefor joined the NHS in 1972 aged<br />
17, starting his career as a filing<br />
clerk at the Caernarfonshire and<br />
Anglesey (C&A) Hospital in Bangor.<br />
He worked his way up to clerical<br />
officer before joining Gwynedd<br />
<strong>Ambulance</strong> Service in 1977.<br />
Trefor said: “There was no such<br />
thing as a paramedic back then<br />
– I joined as an ‘ambulance man’<br />
and that’s what we all were.<br />
“I did two weeks of training at<br />
the ambulance headquarters in<br />
Bodfan at Eryri Hospital, then six<br />
weeks at Wrenbury Hall in Crewe,<br />
and then I was qualified.<br />
“Back then, we did both<br />
emergencies and nonemergencies,<br />
so taking people to<br />
clinic appointments.<br />
“There was also a standby shift,<br />
which meant the duty ambulance<br />
driver would take the vehicle home<br />
and he’d get a call on his landline<br />
telephone from control if there was<br />
an emergency in the night.”<br />
Later qualifying as an Emergency<br />
Medical Technician, Trefor says<br />
a lot has changed in the last<br />
50 years.<br />
“In the 1970s, we were essentially<br />
just providing basic life support,<br />
and not a lot else,” he said.<br />
“We didn’t have the skills or<br />
equipment back then – in fact,<br />
the only equipment we had was<br />
a stretcher, splints, blankets<br />
and a ‘minuteman’ to help with<br />
resuscitation.<br />
“Our ‘ambulance’ was a Ford<br />
Transit with two stretchers in the<br />
back and a small blue light on<br />
the roof.<br />
“The standard of care has<br />
improved fantastically, but we’ve<br />
had no choice but to evolve<br />
because demand on the service<br />
has also increased drastically.<br />
“There’d be some nights where<br />
you wouldn’t turn the wheel of the<br />
ambulance, but these days, it can<br />
be job after job after job.”<br />
Trefor’s wife Julie recalls: “In the<br />
80s, I remember getting calls at<br />
home from the control room to say<br />
‘Trefor’s had a dirty job – please<br />
could you have a bath ready?’<br />
“I’d have to run a hot bath and<br />
make sure the washer was empty<br />
so his dirty clothes could go<br />
straight in.<br />
“I’d also have a bowl of hot water<br />
and Savlon antiseptic by the back<br />
door for his stethoscope to go in<br />
and any loose change from his<br />
pocket.<br />
30<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWLINE<br />
“This was at the time of the<br />
meningitis outbreak, but there<br />
was no such thing then as PPE.<br />
“The ambulance service also<br />
gave us six vouchers a year<br />
for Johnson Cleaners, so we<br />
could take Trefor’s uniform to be<br />
laundered and dry cleaned.”<br />
Trefor added: “If we had a<br />
‘dirty’ job, we’d have to mix two<br />
chemicals together in a bowl<br />
and leave it in the back of the<br />
ambulance with the doors locked<br />
for it to have a reaction and<br />
disinfect everything.”<br />
Trefor, 68, whose nickname<br />
locally is ‘Trefor <strong>Ambulance</strong>’, is<br />
these days working part-time as<br />
an Urgent Care Assistant.<br />
He said: “Caernarfon is such a<br />
small community that everyone<br />
knows everyone.<br />
“Often, you’ll have people coming<br />
up to you to say ‘You helped my<br />
mam’ or ‘You helped my auntie.’<br />
“One time, a woman came up to<br />
me and said ‘You see that boy<br />
there – you helped to deliver him.’<br />
“He must have been about<br />
11-years-old but I did remember<br />
it – it’s a nice feeling.”<br />
Trefor, a father-of-four and a<br />
grandfather-of-five, has even<br />
inspired his two sons to follow in<br />
his footsteps.<br />
His eldest son Gareth, 44,<br />
works for the Royal Air Force in<br />
Bedford and is also a Community<br />
First Responder for the East of<br />
England <strong>Ambulance</strong> Service.<br />
His youngest son Dewi, 33,<br />
is a paramedic at the Welsh<br />
<strong>Ambulance</strong> Service in Bargoed,<br />
who next week takes up a new<br />
role as a Cymru High Acuity<br />
Response Unit Paramedic.<br />
Trefor added: “Of the 27<br />
colleagues who did their training<br />
back in 1977, I’m the last one<br />
standing, but I enjoy it as much<br />
now as I did on day one.”<br />
Almost 200 colleagues across the<br />
Trust have been invited to receive<br />
a Long Service Award this year.<br />
Patient-facing colleagues at<br />
yesterday’s event included<br />
paramedics, emergency medical<br />
technicians, call handlers,<br />
allocators and operations<br />
managers, while a practice<br />
educator, project support officer<br />
and a safeguarding specialist were<br />
among the corporate colleagues.<br />
Recipients came from all four<br />
corners of North Wales, including<br />
Holyhead, Bangor, Llanfairfechan,<br />
Rhyl, St Asaph, Wrexham, Ruthin,<br />
Dolgellau and Dobshill, Flintshire.<br />
Chief Executive Jason Killens<br />
said: “Working for the ambulance<br />
service is not just any job – it’s a<br />
job that makes a real difference.<br />
“Often when people are at their<br />
lowest ebb, our staff are the<br />
people to whom they turn, and<br />
it takes remarkable people to do<br />
the remarkable job they do, day<br />
in, day out.<br />
“It’s mindboggling to think that<br />
all the Long Service Awards we<br />
presented yesterday amount to<br />
more than 600 years of service.”<br />
Chair Colin Dennis added: “The<br />
reason the Welsh <strong>Ambulance</strong><br />
Service is what it is rests with its<br />
people who work tirelessly, 24/7,<br />
to serve the people of Wales.<br />
“All our staff and volunteers<br />
play a part in saving lives and<br />
I am extremely proud of their<br />
achievements.<br />
“Congratulations to all of our<br />
recipients.”<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
31
NEWLINE<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
NHS Charities<br />
Together Patrons The<br />
Prince and Princess<br />
of Wales surprise<br />
health workers with<br />
75th anniversary<br />
party – even helping<br />
make the cake!<br />
Marking the 75th anniversary<br />
of the NHS on Wednesday 5th<br />
July, Their Royal Highnesses<br />
The Prince and Princess of<br />
Wales have surprised NHS<br />
staff and patients from across<br />
the <strong>UK</strong> with a very special NHS<br />
Big Tea party – even arriving<br />
early to help lay the tables, put<br />
finishing touches on a birthday<br />
cake, and debate the age-old<br />
question: jam or cream first.<br />
Hosted by NHS Charities Together<br />
– the national charity caring for<br />
the NHS, of which Their Royal<br />
Highnesses are Patrons – and<br />
television presenter Mel Giedroyc,<br />
the event was attended by<br />
members of the workforce and<br />
patients representing myriad<br />
achievements of the NHS and NHS<br />
charities over the last 75 years. It<br />
was held in the wellbeing garden of<br />
St Thomas’ Hospital in London – a<br />
wellbeing initiative funded by Guy’s<br />
and St Thomas’ Charity.<br />
The Prince and Princess met<br />
with guests ranging from Aneira<br />
Thomas, the first baby born on<br />
the NHS, to pioneers in research<br />
and those on the frontline tackling<br />
Covid-19. The guest list honoured<br />
staff past and present, including<br />
three generations of NHS workers<br />
from one family – inspired by<br />
grandmother and former nurse of<br />
nearly 50 years, Blanche Hines,<br />
who was part of the Windrush<br />
generation.<br />
Their Royal Highnesses<br />
discussed current challenges and<br />
thanked staff for the work they<br />
continue to do, and – in the spirit<br />
of the tea party – even attempted<br />
to settle the long-standing scone<br />
debate regarding jam or cream<br />
first, with The Princess voting for<br />
jam, and Prince William preferring<br />
whatever is closest. They<br />
concluded their visit with a video<br />
message for the entire NHS:<br />
“Wishing everyone a very happy<br />
75th birthday for the NHS.<br />
Thank you so much for all<br />
you do.”<br />
Ellie Orton OBE, Chief<br />
Executive of NHS Charities<br />
Together, said: “We want to<br />
say a huge thank you to our<br />
Royal Patrons, and everyone<br />
who’s helped celebrate the 75th<br />
anniversary of our beloved NHS<br />
this year. As the national charity<br />
caring for the NHS, NHS Charities<br />
Together is here for anyone who<br />
wants to give something back to<br />
its people, who all give so much<br />
to us, and that extra support<br />
has never been so important.<br />
It includes providing staff<br />
psychologists, counselling, peer<br />
support training and so much<br />
more.<br />
“It’s not too late to arrange<br />
your own NHS Big Tea party<br />
and raise vital funds to support<br />
NHS charities – find out<br />
how you can get involved at<br />
nhscharitiestogether.co.uk.”<br />
Dr Neil Rees, a Consultant<br />
Clinical Psychologist leading<br />
the staff wellbeing programme<br />
at Guy’s and St Thomas’, which<br />
has benefited from NHS charity<br />
funding, said: “The Prince of<br />
Wales was very mindful of the<br />
support that’s been given by<br />
NHS charities and how essential<br />
that is, and really understood<br />
the issues and complexities<br />
– particularly with the current<br />
challenges we’re facing. The<br />
pandemic shone a light on the<br />
needs of staff, but he was keen<br />
to talk about how we maintain the<br />
care roles like mine provide, and<br />
how charities play a major role in<br />
that. It was incredibly special to<br />
be recognised in that way.”<br />
Eurovision and former Great-<br />
British Bake Off presenter<br />
Mel Giedroyc was the host<br />
for the event on behalf of<br />
NHS Charities Together, and<br />
said: “The NHS is part of our<br />
DNA in this country so it was<br />
an utter privilege to be involved<br />
in this NHS Big Tea surprise to<br />
celebrate 75 years of the NHS<br />
and NHS charities. People were<br />
so delighted and it was just a<br />
quintessentially lovely, British day,<br />
celebrating our health service<br />
that we all love so much. I hope<br />
we will continue to love and take<br />
care of it for the next 750 years,<br />
because it’s something truly<br />
precious – and what would we do<br />
without it? I have it to thank for<br />
my hernia operations!”<br />
The Prince and Princess of<br />
Wales became Royal Patrons<br />
for NHS Charities Together in<br />
December 2020, during the<br />
height of the Covid-19 pandemic.<br />
Since then, their support for<br />
the charity has helped to shine<br />
a light on the incredible and<br />
ongoing contribution of the NHS<br />
workforce and the role of NHS<br />
charities in helping the NHS go<br />
further for everyone.<br />
Now entering its sixth year, the<br />
NHS Big Tea brings the nation<br />
together to celebrate the NHS<br />
and raise funds to provide the<br />
extra support needed for staff,<br />
patients, and volunteers. All<br />
funds raised from the NHS Big<br />
Tea contribute to key projects<br />
supporting the incredible NHS<br />
workforce, the long-term recovery<br />
of the NHS following Covid-19,<br />
and projects improving care for<br />
patients and communities.<br />
To find out more about the<br />
work of NHS charities, or how<br />
you can host your own NHS<br />
Big Tea event pack, please visit<br />
www.nhscharitiestogether.<br />
co.uk<br />
Six new community<br />
first responder cars<br />
for the South Western<br />
<strong>Ambulance</strong> Service<br />
thanks to NHS<br />
Charities Together<br />
Thanks to a £128,000 grant<br />
from NHS Charities Together,<br />
patient care provided by<br />
South Western <strong>Ambulance</strong><br />
Service NHS Foundation Trust<br />
volunteer Community First<br />
Responders, will be boosted<br />
by the arrival of six new Dacia<br />
Dusters response vehicles.<br />
The new vehicles were officially<br />
presented to the ambulance<br />
service at an event at Buckfast<br />
Abbey in Devon, on the last day of<br />
Volunteers’ Week.<br />
Every day, volunteers from across<br />
the South West support the South<br />
Western <strong>Ambulance</strong> Service NHS<br />
Foundation Trust (SWASFT) by<br />
attending emergencies within<br />
their local communities ahead<br />
of an emergency ambulance.<br />
Sometimes the difference is<br />
providing reassurance; sometimes<br />
it is saving someone’s life.<br />
In the last 12 months, Community<br />
First Responders were mobilised<br />
approximately 24,000 times, to<br />
medical emergencies such as:<br />
cardiac arrests, chest pains,<br />
breathing difficulties and patients<br />
who had fallen.<br />
The grant was secured by the<br />
South Western <strong>Ambulance</strong><br />
Charity as part of a collaborative<br />
project with the Trust’s<br />
Volunteering and Community<br />
Services team and delivered with<br />
the support of the Fleet team.<br />
Each car has been converted and<br />
equipped with a full Community<br />
First Responder kit including<br />
a defibrillator and observation<br />
equipment. Each car also carries<br />
a Raizer lifting chair to assist<br />
32<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
TESTED<br />
ADVANCED<br />
AMBULANCE SEATING<br />
patients who have had a fall.<br />
Will Warrender, Chief Executive<br />
of SWASFT, said: “The funding<br />
received by the South Western<br />
<strong>Ambulance</strong> Charity is enabling us<br />
to better support our volunteers,<br />
who, in turn provide incredible<br />
support to the communities<br />
they serve.<br />
“The six cars that are being<br />
provided through the charity<br />
will enable Community First<br />
Responders to respond to<br />
emergencies across a wider<br />
geographic area and support the<br />
training of new volunteers through<br />
observer shifts.”<br />
Zoe Larter, Head of South<br />
Western <strong>Ambulance</strong> Charity, said:<br />
“We would like to thank NHS<br />
Charities Together for awarding<br />
us this grant. It’s really going to<br />
make a huge difference and help<br />
improve the patient care delivered<br />
by our dedicated volunteers.”<br />
Ellie Orton OBE, Chief Executive<br />
of NHS Charities Together,<br />
said: “NHS Charities Together<br />
is the national charity caring for<br />
the NHS, and we’re delighted<br />
to support South Western<br />
<strong>Ambulance</strong> Charity with this<br />
project. Our ambulance services<br />
are facing pressures on a colossal<br />
scale, and CFRs provide vital<br />
support when every second<br />
counts. We hope these new<br />
response vehicles will help them<br />
reach vulnerable patients even<br />
faster in emergency incidents –<br />
and ultimately help save lives.”<br />
SWASFT has over 500 active<br />
volunteers who support the<br />
service in patient-facing and<br />
non-patient facing roles. To find<br />
out about volunteering roles at the<br />
Trust and to express an interest,<br />
please visit - https://www.swast.<br />
nhs.uk/welcome/community-firstresponders/volunteer-recruitment.<br />
The cars will enhance the<br />
work of the Community First<br />
Responders in their communities<br />
by supporting operational<br />
requirements in the following<br />
ways:<br />
• Additional response vehicles<br />
to extend Community First<br />
Responder capacity and<br />
improve patient experience<br />
• Provided a response vehicle<br />
that allows two Community<br />
First Responders to respond<br />
together to patients across the<br />
South West<br />
• Volunteer training activities,<br />
such as experienced crew<br />
members taking out new<br />
volunteers on familiarisation<br />
shifts<br />
• For double-crewed shifts to<br />
enhance skills or to enable work<br />
with other professionals<br />
Cars may also be used to target<br />
specific types of incidents, e.g. as<br />
a Falls Vehicle or Welfare Support<br />
Car, or to work alongside a skilled<br />
professional such as with the<br />
Mental Health Team or Home<br />
Treatment Team.<br />
M1 SEATS APPROVED TO LATEST<br />
R44.04 CHILD SEAT STANDARDS<br />
Contact us for further<br />
information and brochures<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
33
NEWLINE<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
A Day in the Life Of<br />
… a 999 call handler<br />
mentor<br />
After 15 years of answering<br />
emergency ambulance calls,<br />
Suman Legah has heard it all,<br />
and now she spends most<br />
of her days mentoring and<br />
inspiring the next generation<br />
of 999 call handlers. We joined<br />
her to see what a day in her life<br />
is like.<br />
“<strong>Ambulance</strong> service, is the patient<br />
breathing?”<br />
One ring of the phone is all our<br />
Emergency Medical Dispatchers<br />
have before they speak directly<br />
to someone in their hour of need,<br />
and the first call of today is for an<br />
elderly lady who has had a fall<br />
in a Lincolnshire care home and<br />
suffered a nasty head injury.<br />
Emergency call handler and<br />
mentor Suman Legah carefully<br />
and calmly takes all the details<br />
needed for an ambulance to be<br />
dispatched, before talking the<br />
concerned carer through how to<br />
stop the bleeding with a clean, dry<br />
towel. Suman reassures the caller<br />
an ambulance will be sent as soon<br />
as possible and ends the call to<br />
take the next one.<br />
The phone rings again, this time<br />
a General Practitioner (GP) with a<br />
patient experiencing chest pain,<br />
followed by a call for an elderly<br />
lady stranded on the toilet for 10<br />
hours having been found by her<br />
carers when they arrived for their<br />
morning visit.<br />
Suman explains that while she’s<br />
taken some very traumatic calls<br />
over the years, it’s actually these<br />
elderly patients who concern her<br />
the most.<br />
She said: “It’s the older callers<br />
that get me – the little Dorises – if<br />
people aren’t looking out for each<br />
other now, what is it going to<br />
be like for me when I’m older. It<br />
makes you think.<br />
“I once took a call from the police<br />
who had forced entry to an elderly<br />
woman’s house and found she<br />
had been on the floor for two<br />
weeks – no medication, no food,<br />
no water – no-one had checked<br />
up on her. But she was still alive!<br />
“As it was a fall, the call was<br />
automatically categorised as a<br />
Category 3, so I immediately went<br />
over to our Clinical Assessment<br />
Team to ask them to upgrade it<br />
given the circumstances so we<br />
could get there as quickly as<br />
possible.”<br />
The two EMAS 999 control<br />
rooms – one in Bracebridge Heath<br />
in Lincolnshire and one near<br />
Nuthall in Nottinghamshire – take<br />
challenging calls every day, and<br />
so Suman explains that anyone<br />
looking to join as a 999 call<br />
handler needs to be emotionally<br />
resilient to cope with such calls.<br />
Suman said: “I’ve taken calls from<br />
people who have seen loved ones<br />
stabbed, or drivers who have<br />
come across traumatic road traffic<br />
collisions where the patient’s limbs<br />
have come off due to the force of<br />
the impact. It’s the picture painted<br />
in your mind by the caller which<br />
can be difficult.<br />
“You also get the callers who<br />
shout and swear at you – it gets<br />
easier over the years, but I am<br />
human too.<br />
“All I can do is my best for each<br />
caller, which means taking control<br />
of the situation, getting the<br />
information I need to send help<br />
to them, and providing them with<br />
reassurance until an ambulance<br />
crew can arrive.”<br />
To help her process and reflect<br />
on the calls she answers, Suman<br />
walks around 16,000 steps a day<br />
– including walks before her 6am<br />
shift starts, in her 45-minute meal<br />
break, and to help her wind down<br />
when she gets home to Ilkeston in<br />
Derbyshire.<br />
She said: “I don’t sleep much and<br />
I’m an early riser so I’m up before<br />
4am and do some yoga, prayer,<br />
read, have a shower and a cup of<br />
tea, and then come to work about<br />
half an hour early.<br />
“Then I park up, do a few laps<br />
around the headquarters site as<br />
I love walking, and then I set my<br />
desk up, log in, and I’m ready to<br />
take on whatever comes my way.<br />
“After work I use the time to<br />
think about what I could have<br />
done better, but without beating<br />
myself up.”<br />
Before becoming a 999 call<br />
handler, Suman travelled the world<br />
as a buyer for big-name brands<br />
such as BHS, Asda and Tesco.<br />
After getting married, she stopped<br />
travelling and looked for a more<br />
local role and began working in<br />
the control room at EMAS.<br />
She said: “I was very intimidated<br />
coming to work in the office as<br />
everyone knew more than me<br />
and I kept worrying ‘what if I<br />
kill someone?’.<br />
“Back then you only had three<br />
shifts with a mentor and then you<br />
were taking calls by yourself. Now<br />
we mentor new colleagues for<br />
around 10 to 12 shifts. I make sure<br />
they feel confident and reassured<br />
and know they can still always<br />
come to me to ask anything they<br />
are not sure about.”<br />
Suman’s first solo shift was tough,<br />
especially as the first call she ever<br />
answered was for someone who<br />
had taken their own life and there<br />
was little she could do to help<br />
them.<br />
She said: “In my mind I hadn’t<br />
helped because the patient had<br />
died, and there wasn’t much<br />
support back then for us. I went<br />
home and cried, and then carried<br />
my resignation letter in my bag<br />
with me for six months.<br />
“However, it turned out I needed<br />
to give the job a chance, and<br />
within six months it all started<br />
coming together and I was asked<br />
to become a mentor for new<br />
colleagues.<br />
“Now I say to my mentees that<br />
they need to give the role six to<br />
nine months, and then one day it<br />
will all suddenly click in your head,<br />
and you’ll walk in buzzing, and<br />
you won’t need to ask anyone<br />
anything.”<br />
Throughout her EMAS career to<br />
date, Suman estimates that she’s<br />
mentored somewhere between 30<br />
and 40 people, and every single<br />
one of them have passed their<br />
Emergency Medical Dispatcher<br />
certification.<br />
However, she is clear that people<br />
applying for the role need to be a<br />
certain type of person and willing<br />
to work bank holidays, weekends,<br />
days and nights as part of a shift<br />
pattern.<br />
Suman added: “This job isn’t<br />
for everyone. You need to be<br />
confident and assertive, and<br />
you cannot get upset after every<br />
traumatic call. At the end of the<br />
day, if you are not alert enough<br />
and practising active listening with<br />
each caller to catch something<br />
which may indicate that someone<br />
is seriously unwell, then someone<br />
could die.<br />
“This is a really serious job, and<br />
I need to feel confident that all<br />
my colleagues around me in the<br />
control room are able to do the<br />
right thing for our patients.<br />
“We need to be following the<br />
script for compliance, but<br />
without it sounding like we are<br />
reading from a script, still making<br />
it personal for them, and still<br />
thinking outside the box when we<br />
34<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWLINE<br />
need to in order to do the right<br />
(Gorseinon), Tamsin Turner<br />
the island, but if you think the<br />
hosted the visit.<br />
thing for that patient.”<br />
(Pembroke Dock), Callum<br />
domestic calls would be in any<br />
Paramedics<br />
switch gears at TT<br />
motorsport festival<br />
PARAMEDICS from the Welsh<br />
<strong>Ambulance</strong> Service have been<br />
supporting the world-famous<br />
TT motorsport festival in the<br />
Isle of Man.<br />
McNamara (Holyhead), Aimee<br />
Griffiths (Dobshill), Amanda Binks<br />
(Aberystwyth) and Lesley Spanner<br />
(Gorseinon) were picked to attend.<br />
The team were led across the<br />
two-week period by Dorian<br />
James, operations manager<br />
in Powys.<br />
Dorian said: “The TT is a fantastic<br />
learning experience, and you<br />
way dull, you couldn’t be more<br />
wrong.<br />
“The island’s Mountain Road has<br />
no speed limit and unfortunately,<br />
lots of race-goers and tourists had<br />
accidents here, so what we saw<br />
was predominantly trauma jobs.<br />
“We worked really closely with the<br />
Isle of Man <strong>Ambulance</strong> Service<br />
and Great North Air <strong>Ambulance</strong>,<br />
He said: “We had an absolutely<br />
brilliant welcome from the Isle of<br />
Man <strong>Ambulance</strong> Service.<br />
“From the managers to the ‘makeready’<br />
staff, they couldn’t do<br />
enough for us.<br />
“We presented them with a Welsh<br />
dragon plaque at the end of the<br />
trip as a token of our appreciation.<br />
Every May and June, the world’s<br />
greatest road racers gather on<br />
the Isle of Man to test themselves<br />
against the 37.73 mile ‘Mountain<br />
Course’ carved out of the island’s<br />
public roads.<br />
The festival attracts 40,000 visitors<br />
annually, and when the Isle of<br />
Man <strong>Ambulance</strong> Service made an<br />
appeal for mutual aid, the Welsh<br />
<strong>Ambulance</strong> Service answered.<br />
acquire so many new skills.<br />
“For example, we learnt in<br />
our induction how to perform<br />
a surgical airway procedure<br />
and how to use a ‘Lucas-3’<br />
device to deliver mechanical<br />
chest compressions, a piece of<br />
equipment which only high acuity<br />
paramedics in Wales are trained<br />
to use.<br />
which flew patients from the island<br />
to the <strong>UK</strong> mainland.<br />
“Callum even got opportunity to<br />
spend time on the air ambulance<br />
and ended up in Liverpool and<br />
Northern Ireland during some<br />
of the transfers.<br />
“It was a completely different way<br />
of working there.”<br />
“I’d encourage all of my WAST<br />
colleagues to think about applying<br />
next year.”<br />
Clare Langshaw, the Welsh<br />
<strong>Ambulance</strong> Service’s Head<br />
of Emergency Preparedness,<br />
Resilience and Response,<br />
said: “Mutual aid arrangements<br />
like this not only enable us<br />
to deliver services across<br />
geographic boundaries but it’s<br />
“Our job was to attend the<br />
Dorian has extended a thanks to<br />
also a wonderful opportunity for<br />
Paramedics Sarah Raddenbury<br />
‘business as usual’ activity on<br />
the Isle of Man colleagues who<br />
individuals to develop their skills<br />
Helping to Power the<br />
Healthcare Services<br />
Now’s the time to<br />
electrify blue light fleets.<br />
Electrifying the response vehicles of the ambulance services will have a major<br />
positive impact on reducing emissions.<br />
Mer are experts in this field. Counting London <strong>Ambulance</strong> Service and NTW<br />
Solutions as clients, we have the experience to deliver on your EV goals.<br />
Take charge and talk to us today<br />
03300 562 562<br />
Click to visit us online today<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
35
NEWLINE<br />
and get a whole new perspective<br />
on things.<br />
“It helps to strengthen<br />
relationships with our partner<br />
agencies, as well as introduce us<br />
to new people and new ideas.”<br />
Judith Bryce, Assistant Director of<br />
Operations for National Operations<br />
and Support, said: “This is the<br />
second year that we’ve supported<br />
the TT event, and each year,<br />
colleagues come back with bags<br />
of enthusiasm having experienced<br />
something completely different,<br />
and lots of ideas for improvement<br />
based on what they observed.<br />
“We’re proud and grateful to these<br />
seven colleagues for flying the flag<br />
for Wales in such a professional<br />
way.”<br />
Will Bellamy, Head of the Isle of<br />
Man <strong>Ambulance</strong> Service, added:<br />
“I’d like to take this opportunity<br />
to offer my personal thanks to<br />
Dorian, Sarah, Tamsin, Callum,<br />
Aimee, Amanda and Lesley for<br />
their invaluable support during the<br />
TT fortnight, and for their tireless<br />
devotion in keeping both Manx<br />
residents and visitors to the island<br />
as safe as possible.<br />
“It was a great opportunity for our<br />
teams to be able to learn from<br />
their Welsh colleagues too.<br />
Chief Executive Jason Killens<br />
(Credit: Wales Online)<br />
King’s <strong>Ambulance</strong> Service Medal<br />
for distinguished service, it was<br />
announced tonight.<br />
Meanwhile, Volunteer Car Service<br />
Driver Ian Cross has been<br />
awarded a British Empire Medal<br />
for services to the Trust.<br />
The King’s Birthday Honours<br />
List recognises the outstanding<br />
achievements of people across<br />
the <strong>UK</strong>, from all walks of life.<br />
Colin Dennis, Chair of the Welsh<br />
<strong>Ambulance</strong> Service, said: “We’re<br />
beyond thrilled that Jason and<br />
of highly skilled, engaged and<br />
healthy people, and it shines<br />
through in all he does.<br />
“These awards recognise the<br />
dedication of some of our very<br />
best ambulance professionals,<br />
and I’d like to extend a huge<br />
congratulations to Jason and Ian.”<br />
Jason began his career as an<br />
Emergency Medical Technician<br />
at London <strong>Ambulance</strong> Service,<br />
where he held various senior<br />
leadership roles, including<br />
Executive Director of Operations.<br />
“I’ve had 27 years in ambulance<br />
services in the <strong>UK</strong> and Australia<br />
and I love it as much now as I did<br />
on day one.<br />
“<strong>Ambulance</strong> work for me is all<br />
about doing the best we can for<br />
our people and our patients, so the<br />
King’s <strong>Ambulance</strong> Service Medal is<br />
as much for them as it is for me.<br />
“A huge congratulations also to<br />
Ian, who is an integral cog in the<br />
wheel of our non-emergency<br />
service.”<br />
Ian Cross, a civil servant from<br />
Pontypool, volunteers two days<br />
per week to take patients to their<br />
hospital appointments, including<br />
dialysis, oncology and outpatient<br />
appointments.<br />
Ian, who is severely deaf, is usually<br />
accompanied by his hearing dog<br />
Buddy, a 10-year-old Cocker<br />
Spaniel trained to assist Ian by<br />
alerting him to important sounds,<br />
like smoke alarms.<br />
In 2022/23, Volunteer Car Service<br />
Drivers made 51,924 journeys<br />
across Wales and covered more<br />
than one and a half million miles in<br />
their own vehicles.<br />
Ian, 53, said: “I couldn’t believe<br />
it when the letter landed on my<br />
doormat.<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
“I look forward to welcoming<br />
more colleagues from the Welsh<br />
<strong>Ambulance</strong> Service to the island<br />
in 2024!”<br />
Welsh <strong>Ambulance</strong><br />
Service staff<br />
recognised in King’s<br />
Birthday Honours List<br />
TWO Welsh <strong>Ambulance</strong> Service<br />
staff have been recognised in<br />
His Majesty the King’s Birthday<br />
Honours List.<br />
Chief Executive Jason Killens has<br />
been awarded the prestigious<br />
Ian have been recognised in<br />
King Charles’ first Birthday<br />
Honours List.<br />
“We’re incredibly proud of all<br />
colleagues who go the extra mile<br />
for patients, at all levels, including<br />
hard-working volunteers like Ian.<br />
“Jason meanwhile has a near<br />
30-year ambulance service career,<br />
his talent and tenacity as a Chief<br />
Executive taking him literally<br />
around the globe.<br />
“He’s passionate about the<br />
delivery of high quality patient care<br />
in partnership with a workforce<br />
He was appointed the Chief<br />
Executive of the South Australia<br />
<strong>Ambulance</strong> Service in 2015 before<br />
joining the Welsh <strong>Ambulance</strong><br />
Service as Chief Executive<br />
in 2018.<br />
He is an Honorary Professor at<br />
Swansea University’s College<br />
of Human and Health Sciences,<br />
and the Chief Executive lead for<br />
Operations at the Association of<br />
<strong>Ambulance</strong> Chief Executives.<br />
Jason, 48, said: “I’m proud and<br />
delighted to be recognised in the<br />
King’s Birthday Honours List.<br />
“I saw ‘On His Majesty’s Service’<br />
and thought: ‘Oh no, I’m in<br />
trouble.’<br />
“I was shaking like a leaf and it<br />
gave me goose bumps to read –<br />
I have goose bumps talking about<br />
it even now.<br />
“Poor old Buddy was wondering<br />
where his tea was because I just<br />
kept re-reading the letter.<br />
“The fact that it’s the King’s first<br />
Birthday Honours List makes<br />
me especially proud, and I’m<br />
really looking forward to the<br />
presentation of the medal.”<br />
36<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWLINE<br />
To learn more about becoming<br />
a Volunteer Car Service Driver,<br />
visit: Become a Volunteer<br />
Car Service Driver - Welsh<br />
<strong>Ambulance</strong> Services NHS Trust<br />
Secretary of State for Wales,<br />
David TC Davies, said: “It is<br />
incredibly inspiring to hear<br />
about the extraordinary and<br />
invaluable work of so many people<br />
from across Wales who have<br />
deservedly been recognised in the<br />
King’s Birthday Honours.<br />
“Welsh recipients from a wide<br />
range of fields have been<br />
recognised, whether it’s for<br />
their commitment to their local<br />
community, their contribution<br />
to sport, education, culture or<br />
health – and I’m thrilled that<br />
their endeavours have been<br />
commended.<br />
“I would like to congratulate all the<br />
recipients being honoured and<br />
thank each and every one for their<br />
contribution.”<br />
LGBT+ staff survey<br />
finds EEAST ‘a<br />
modern and inclusive<br />
organisation’<br />
Chief executive recognises<br />
progress, but says there is<br />
‘much further to go’.<br />
The East of England <strong>Ambulance</strong><br />
Service is publishing the results<br />
of an independent survey of<br />
colleagues who identify as LGBT+.<br />
https://www.eastamb.nhs.uk/<br />
about-us/equality-and-diversitysurveys.htm<br />
This follows independent surveys<br />
of BME staff and employees living<br />
with a disability and is part of<br />
the Trust’s on-going programme<br />
to making EEAST an inclusive<br />
environment for everyone.<br />
65% of LGBT staff took part<br />
and shared their views. 72% of<br />
respondents reported that they<br />
consider the Trust to be ‘a modern<br />
and inclusive organisation, which<br />
recognises and embraces people<br />
of all sexual orientations and<br />
different gender identities.’<br />
Tom Abell, CEO of EEAST, said:<br />
“We have made good progress in<br />
improving the culture at EEAST as<br />
evidenced by our improved Care<br />
Quality Commission report and<br />
the lifting of CQC and European<br />
Human Rights Commission<br />
conditions. We are also optimistic<br />
that our results from our recent<br />
staff survey show that we are<br />
beginning to move in the right<br />
direction.<br />
“However, we still have much<br />
further to go in making our<br />
Trust an inclusive environment<br />
for everyone. The key areas<br />
to improve include ensuring<br />
that our staff are confident that<br />
complaints or concerns raised<br />
within EEAST are taken seriously<br />
and not dismissed, trivialised,<br />
or explained away, and that we<br />
tackle ignorance that can lead to<br />
discrimination.<br />
“We have a three-year plan to<br />
make EEAST a more inclusive<br />
place to work and have a skilled<br />
team in the Strategy, Culture and<br />
Education Directorate to drive<br />
forward this plan. We will work<br />
with our employee networks to<br />
ensure that the voice of our people<br />
is represented and valued in all<br />
our plans.”<br />
Ground-breaking<br />
degree turns out first<br />
qualified paramedics<br />
A group of London <strong>Ambulance</strong><br />
Service medics are celebrating<br />
completing a new twoyear<br />
university degree in<br />
paramedicine.<br />
The 45 students are the first<br />
London <strong>Ambulance</strong> Service<br />
cohort to graduate from<br />
the University of Cumbria’s<br />
Paramedicine Course.<br />
The new programme, which is<br />
fully-funded for the students and<br />
started in 2021, aims to make<br />
becoming a paramedic more<br />
accessible and allows clinicians<br />
who are already on the frontline to<br />
continue to work while they earn<br />
their degree.<br />
Lee Knowles, 50, from East<br />
London, was a driving instructor<br />
until the age of 46. He started<br />
working on ambulances four<br />
years ago and is one of the frontline<br />
workers to benefit from the<br />
programme.<br />
He said: “I got my paramedic<br />
registration this month (July) as I<br />
turned 50. At my age, to be given<br />
the opportunity to go back to<br />
university, debt-free, was amazing.<br />
It has opened many doors for me.<br />
“I left school at 16, with good<br />
enough GCSEs. But 30 years<br />
ago, I would have never thought<br />
I would have joined an ambulance<br />
service and even possibly become<br />
a qualified paramedic.”<br />
Donna Buckman, 35, from Surrey,<br />
worked as a florist before joining<br />
the Service at 30. She said the<br />
course was a challenging but<br />
rewarding experience:<br />
“I don’t think I would have<br />
considered a degree without this<br />
opportunity.<br />
“I was diagnosed with dyslexia<br />
years ago and more recently with<br />
dyscalculia. I knew that would be<br />
a challenge, but I tried not to let<br />
that get in the way.<br />
“When I saw I had finished with<br />
a first, I was shocked. I didn’t<br />
know I could do it because I<br />
found the academic side of<br />
things challenging. I hope my<br />
achievement inspires other<br />
neurodivergent people to not give<br />
up on their dreams.”<br />
Jamie Haig, 47, from North<br />
London, became an ambulance<br />
worker in 2019 after a career in IT.<br />
He said: “I went through a period<br />
in my life when I needed change.<br />
I became an Emergency Medical<br />
Technician four years ago and that<br />
change was wonderful – I wish I’d<br />
done it 20 years ago.<br />
“But as fantastic as the Technician<br />
job was, I wanted to qualify as<br />
a paramedic. It was great to be<br />
back in the classroom, I loved the<br />
academic challenge. This degree<br />
has opened up a huge number of<br />
options for me. I have nothing but<br />
gratitude for this job.”<br />
Dr John Martin, Chief Paramedic<br />
at London <strong>Ambulance</strong> Service,<br />
joined the celebrations at<br />
University of Cumbria and said:<br />
“Huge congratulations to the<br />
graduates – it’s incredibly<br />
inspiring to see them get to<br />
this milestone. Studying for a<br />
university degree while working<br />
on the frontline can be extremely<br />
challenging, so everyone should<br />
be immensely proud!<br />
“We know demand on our<br />
services continues to grow and<br />
the need to secure a pipeline<br />
of paramedics is a key priority.<br />
This degree has created a new<br />
route, helping our staff gain the<br />
same standards of education as<br />
those who take the usual degree<br />
route, while continuing to work on<br />
the frontline.<br />
“It has also proved to be an<br />
amazing opportunity for those<br />
who may have thought university<br />
wasn’t for them and we hope it will<br />
help us attract a more diverse pool<br />
of talent from the local area.”<br />
The new degree programme<br />
runs alongside the successful<br />
Associate <strong>Ambulance</strong> Practitioner<br />
apprenticeship, which is a route to<br />
becoming an Emergency Medical<br />
Technician (EMT) without any prior<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
37
NEWLINE<br />
medical qualifications. Following<br />
the apprenticeship, frontline<br />
workers can move onto the<br />
two-year degree course without<br />
pausing their careers.<br />
In 2022, London <strong>Ambulance</strong><br />
Service launched the most<br />
ambitious recruitment programme<br />
in its history. In the last year, 1600<br />
people have joined the Service<br />
including 900 frontline ambulance<br />
staff and 370 call handlers. The<br />
increased numbers mean the<br />
Service now has around 400<br />
ambulances on the road every<br />
day responding to 999 calls – 100<br />
more than pre-pandemic levels.<br />
Last year, London <strong>Ambulance</strong><br />
Service was ranked as the top<br />
NHS employer for apprenticeships<br />
in the country by the Department<br />
for Education – ahead of big<br />
name companies like Tesco<br />
and Amazon.<br />
Magpas Air<br />
<strong>Ambulance</strong> signs<br />
the Armed Forces<br />
Covenant, alongside<br />
armed forces<br />
personnel and the<br />
Lord Lieutenant of<br />
Cambridgeshire,<br />
Julie Spence OBE<br />
Cambridgeshire-based charity<br />
Magpas Air <strong>Ambulance</strong><br />
received a Gold Award in the<br />
Defence Employer Recognition<br />
Scheme for its support of<br />
Armed Forces personnel<br />
on 12 July. It’s a coveted<br />
achievement, with only a<br />
handful of businesses in the<br />
<strong>UK</strong> receiving the award—which<br />
is the highest badge of honour<br />
available in the scheme and<br />
recognises the positive role that<br />
employers play in supporting<br />
the Armed Forces community.<br />
Not only does it make the charity<br />
one of a small percentage<br />
of companies across the <strong>UK</strong><br />
to achieve this, Magpas Air<br />
<strong>Ambulance</strong> has also become the<br />
first air ambulance in the <strong>UK</strong> to<br />
receive the Gold Award too.<br />
The Defence Employer<br />
Recognition Scheme confirmed<br />
the charity was to receive the<br />
Gold Award after Magpas Air<br />
<strong>Ambulance</strong> made a series<br />
of pledges and worked for<br />
accreditations to demonstrate<br />
the charity’s support for<br />
their colleagues in the forces<br />
over the past few years. This<br />
included signing the Armed<br />
Forces Covenant in 2021, which<br />
represents a promise to those<br />
who serve or have served—and<br />
their families—that they will be<br />
supported and treated fairly by<br />
the charity.<br />
Magpas Air <strong>Ambulance</strong>’s Chief<br />
Executive Daryl Brown MBE<br />
DL, who is also Honorary<br />
Commander for the US Air<br />
Force, 423rd Medical Squadron<br />
of the 501st Combat Support<br />
Wing, summarises, “Magpas Air<br />
<strong>Ambulance</strong> has a really strong<br />
relationship with the Armed<br />
Forces, with a number of our<br />
founding doctors coming from<br />
army and RAF backgrounds. For<br />
over 50 years, this partnership<br />
has thrived—with Magpas Air<br />
<strong>Ambulance</strong> continuing to host<br />
many Armed Forces doctors,<br />
paramedics and flight crew—and<br />
some of our non-clinical staff<br />
are current or former service<br />
personnel, including two trustees.<br />
“As a charity we have signed up<br />
to the Armed Forces Covenant<br />
and we’re incredibly proud of<br />
our colleagues who have and<br />
continue to serve in the Armed<br />
Forces, as well as their families,<br />
and will always ensure they are<br />
treated fairly and get the support<br />
they need from Magpas Air<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
38<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWLINE<br />
<strong>Ambulance</strong>. As well as signing<br />
the Armed Forces Covenant<br />
and working with the Defence<br />
Employer Recognition Scheme,<br />
we also have a partnership with<br />
our local medical reserve force<br />
(254 medical regiment), and<br />
are proud to have a reservists<br />
policy—which has been<br />
developed in consultation with<br />
our Armed Forces personnel. We<br />
also work closely with the US Air<br />
Force bases and international<br />
forces located in our region.<br />
We hope all of this supports<br />
our current workforce and will<br />
encourage other members of the<br />
forces to join this 24/7 lifesaving<br />
service.”<br />
Natalie Church, Magpas<br />
Air <strong>Ambulance</strong> Director of<br />
Operations, continues “One of<br />
our charity’s greatest strengths<br />
is our dedication to education<br />
and training—including learning<br />
from other services, such as<br />
the Armed Forces. The Magpas<br />
Air <strong>Ambulance</strong> medical team<br />
regularly utilise procedures and<br />
equipment that are used on<br />
the battlefield and endorsed<br />
by our military staff to enhance<br />
patient care.<br />
“The skills and experience of<br />
our Armed Forces personnel<br />
complement our lifesaving<br />
service, and in return Magpas<br />
Air <strong>Ambulance</strong> provides these<br />
clinicians with the opportunity<br />
to not only maintain but further<br />
develop their clinical expertise<br />
in the field when they’re not on<br />
active operations.”<br />
Magpas Air <strong>Ambulance</strong>, the<br />
charity that saves lives 24/7<br />
across the whole of the east of<br />
England by bringing pre-hospital<br />
emergency care to critically ill<br />
and injured patients is not state<br />
funded and relies on generous<br />
public donations to continue<br />
saving lives. To find out more<br />
about the service, just visit:<br />
https://magpas.org.uk/.<br />
Great-grandad<br />
recalls ambulance<br />
career as<br />
paramedics<br />
transport him back<br />
to the sixties<br />
A 98-year-old man with<br />
dementia was able to recall<br />
events from his career on<br />
London ambulances when two<br />
paramedics visited his care<br />
home in a 1960s ambulance<br />
and wearing uniform dating<br />
back to that time.<br />
Albert Gibbs, a Normandy<br />
veteran from the Second World<br />
War who worked on ambulances<br />
in London between 1965 and<br />
1990, now lives in Essex and<br />
often refers back to his time as an<br />
ambulance worker, but memory<br />
loss means many important<br />
events from his career have<br />
been forgotten.<br />
However, when London<br />
<strong>Ambulance</strong> Service paramedics<br />
Craig Henty and Terence<br />
Thomson visited him recently in<br />
an original 1967 Morris Wadhams<br />
ambulance and period uniforms,<br />
it took him right back to his days<br />
as a medic.<br />
He immediately said: “I wore the<br />
same uniform and the same hat.<br />
Then, he added: “I recognise<br />
your badge. It’s from the northeast<br />
sector, where I used to<br />
work. I was stationed at Ilford,<br />
but sometimes also worked<br />
in Romford.”<br />
Before visiting, Craig and Terence<br />
had researched material from<br />
Albert’s time in the ambulance<br />
through the Service’s Historic<br />
Collection and traced thank-you<br />
letters from patients Albert had<br />
cared for, as well as pictures of a<br />
work holiday he had organised.<br />
Albert said: “I had a holiday club<br />
that people called ‘Gibbs Tours’.<br />
I once arranged a weekend in<br />
Benidorm and got 43 people to<br />
go, including ambulance workers,<br />
nurses, doctors, and their<br />
families. It was a good weekend!”<br />
Reminiscing about some<br />
important jobs he attended, he<br />
said: “I delivered five babies and<br />
saved a person who fell under<br />
a train.<br />
“I had a good time and a lot of<br />
laughs at the Service, especially<br />
when I rang the ambulance<br />
bell on the Woolwich ferry. We<br />
weren’t allowed to do that, but I<br />
did it once and then sped down<br />
the ferry. It got me into some<br />
troubles!”<br />
Craig Henty, London <strong>Ambulance</strong><br />
Service Paramedic and Head of<br />
Historic Collections, commented:<br />
“I sat with Albert in the back of<br />
the ambulance for a chat and it<br />
felt as if we had just finished a<br />
job together.<br />
“His mannerism and familiarity<br />
with the vehicle are classic<br />
of someone who works in an<br />
ambulance. He even rested his<br />
feet on the rail in front of him and<br />
that’s exactly what an ambulance<br />
crew would do.<br />
“I was amazed to see that<br />
the experience brought him<br />
right back.”<br />
Head Nurse at Elizabeth House<br />
Care Home Tracy McGuinness<br />
explained that people with<br />
dementia can benefit from visual<br />
and sensory cues to stimulate<br />
their brain and trigger their<br />
memory.<br />
She said: “It was emotional to<br />
see Albert recall his time as an<br />
ambulance worker.<br />
“We encourage our patients to relive<br />
important experiences from<br />
their lives as that keeps their brain<br />
engaged and can reduce their<br />
cognitive decline. We try to keep<br />
their mind ticking and give them<br />
purpose.”<br />
Albert Gibbs’ daughter Elaine<br />
Dettmar said: “My dad served in<br />
the ambulance service for many<br />
years and that was a huge part of<br />
his life – it was moving to help him<br />
re-live it.<br />
“As he talked and engaged with<br />
the pictures more memories were<br />
coming out.”<br />
Throughout his 25-year<br />
ambulance career, Albert Gibbs<br />
saw the development of what<br />
grew to be known as ‘London<br />
<strong>Ambulance</strong> Service’, which<br />
today is the busiest emergency<br />
ambulance service in the world.<br />
On the year he became a medic,<br />
in 1965, a London-wide service<br />
was formed in the capital after<br />
nine existing services merged<br />
together, comprising nearly 1,000<br />
vehicles and 2,500 staff.<br />
In 1974, when the National Health<br />
Service was reorganised, the<br />
Service was transferred from the<br />
control of local government to<br />
the South West Thames Regional<br />
Health Authority.<br />
Service managers continued to<br />
report to South West Thames<br />
until 1 April 1996, when the<br />
organisation became an NHS<br />
trust. London <strong>Ambulance</strong> Service<br />
as we know it today officially<br />
came into being.<br />
This year, the NHS celebrates<br />
75 years since post-war<br />
reorganisation led to the National<br />
Health Service Act of 1948. As<br />
part of this, for the first time,<br />
there was a requirement for<br />
ambulances to be available for<br />
all those who needed them.<br />
London <strong>Ambulance</strong> Service<br />
collects original items that trace<br />
the history of the Service in its<br />
Historic Collection. This includes<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
39
NEWLINE<br />
horse carriages and blitz<br />
ambulances from the Second<br />
World War, as well as medical<br />
equipment, uniforms, and medals<br />
of historical significance.<br />
NHS 111 staff to<br />
move into new<br />
ambulance centre<br />
in Gillingham<br />
Staff from South East Coast<br />
<strong>Ambulance</strong>’s NHS 111 service<br />
will begin to move into a new<br />
multi-purpose ambulance and<br />
contact centre in Gillingham<br />
this week.<br />
The staff, who are currently<br />
based in Ashford, Kent, are<br />
expected to move in to the<br />
building from Wednesday, 28<br />
June. They will join their 999<br />
frontline operations colleagues<br />
who moved into the building<br />
earlier this month with both teams<br />
being joined later this year by<br />
their 999 Emergency Operations<br />
Centre (EOC) colleagues.<br />
The multi-purpose centre, in<br />
Bredgar Road, Gillingham,<br />
will consist of a Make Ready<br />
Centre, EOC, and NHS 111<br />
contact centre. It will be the first<br />
ambulance centre in the country<br />
to bring all three functions<br />
together under one roof.<br />
people across both 999 and 111<br />
services.<br />
John J O’Sullivan, Associate<br />
Director for Integrated Care (999<br />
& 111) at SECAmb said: “I’m<br />
really pleased that our NHS 111<br />
teams will be joining their frontline<br />
colleagues at the new centre this<br />
week. This is an important move<br />
as we continue to evolve and<br />
share best practice across our<br />
999 and 111 functions.<br />
“I would like to thank all those<br />
involved in this project which is a<br />
significant undertaking and which<br />
will be of real benefit to the Trust<br />
and our patients. I wish everyone<br />
well in their new home.”<br />
Resuscitation<br />
Council <strong>UK</strong> raise<br />
awareness of the<br />
urgent need for a<br />
rehabilitation plan<br />
for survivors of<br />
cardiac arrest at<br />
Westminster event<br />
On Monday 19 June,<br />
Resuscitation Council <strong>UK</strong><br />
(RC<strong>UK</strong>) hosted a parliamentary<br />
event to raise awareness of the<br />
urgent need to have a recovery<br />
plan to ensure people who have<br />
a cardiac arrest get the follow<br />
up care they urgently need.<br />
Cross party MPs and Lords<br />
attended the successful event,<br />
where they heard powerful<br />
testimonies from cardiac arrest<br />
survivors, who spoke about their<br />
challenging individual and family<br />
experiences, and the significant<br />
barriers to recovery and quality of<br />
life post-arrest. They highlighted<br />
the absence of a formal care<br />
pathway for post cardiac arrest<br />
care across the <strong>UK</strong>.<br />
A cardiac arrest is the ultimate<br />
medical emergency, when the<br />
heart stops beating, and the<br />
individual is clinically dead. Yet<br />
cardiac arrest survivors are not<br />
offered the same well-established<br />
rehabilitation services that stroke,<br />
and heart attack survivors get.<br />
My Right To Cardiac Arrest<br />
Recovery campaign raises<br />
awareness of the lack of support<br />
available for individuals who have<br />
experienced a cardiac arrest and<br />
aims to achieve a formal care plan<br />
for cardiac arrest survivors, which is<br />
consistently applied across the <strong>UK</strong>.<br />
Lord Aberdare said: “I was<br />
delighted to attend Resuscitation<br />
Council <strong>UK</strong>’s parliamentary event<br />
on Monday 19th June: ‘My Right<br />
to Cardiac Arrest Recovery’.<br />
“I spoke to many cardiac arrest<br />
survivors and their families,<br />
who told me that as a result<br />
of a cardiac arrest, they often<br />
struggle with anxiety, depression,<br />
and post-traumatic stress. They<br />
explained that the support<br />
available for cardiac arrest<br />
care is inconsistent across the<br />
<strong>UK</strong>, and there needs to be a<br />
formal care pathway, similar to<br />
what heart attack and stroke<br />
survivors receive.<br />
“I support this campaign and<br />
believe everyone has the right to<br />
make their best possible recovery<br />
after a cardiac arrest.”<br />
To ensure cardiac arrest survivors<br />
receive the care and support they<br />
need, RC<strong>UK</strong> are asking people<br />
to sign a petition to get MPs to<br />
prioritise this very important issue.<br />
James Cant, CEO at<br />
Resuscitation Council <strong>UK</strong>, said:<br />
“It is great to have everyone<br />
in one room to get this very<br />
important conversation going,<br />
so we can begin to implement<br />
change.<br />
“Currently, we are failing people<br />
who survive a cardiac arrest -<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
Integrating both 999 and<br />
111 services is a key part of<br />
SECAmb’s aim to deliver more<br />
joined up integrated care and<br />
to increase efficiency. The<br />
development will also bring the<br />
east of SECAmb’s region in<br />
line with its West Emergency<br />
Operations Centre (including NHS<br />
111), based in Crawley, which<br />
opened in 2017.<br />
The new centre will provide<br />
the Trust with greater contact<br />
centre capacity and provide<br />
greater resilience and operational<br />
flexibility. It will also bring local<br />
recruitment opportunities for<br />
40<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWLINE<br />
there is no personalised care plan<br />
for rehabilitation for these patients,<br />
they are often sent home with<br />
severe neurological, physical, and<br />
emotional difficulties, missing out<br />
on the vital services they need to<br />
help them recover.<br />
“Please take a spare moment to<br />
sign our petition or write to your<br />
local MP, as a cardiac arrest can<br />
happen to anyone and anytime –<br />
meaning it could be a loved one,<br />
so although you may not think<br />
this concerns you now, it may do<br />
in the future.”<br />
Data suggests that as little as<br />
29% of survivors of out of hospital<br />
cardiac arrest are assessed for<br />
neurological rehabilitation in their<br />
post-cardiac arrest care, and<br />
psychological reviews are only<br />
offered to 20% of survivors.<br />
RC<strong>UK</strong> is developing a new set<br />
of guidelines for cardiac arrest<br />
survivors, aimed at ensuring<br />
consistent, effective, and<br />
sustainable care for cardiac arrest<br />
survivors and their families.<br />
For more information or to<br />
request for an interview or<br />
case studies please call<br />
Tom Shearsmith, Media and<br />
Campaign Officer by email tom.<br />
shearsmith@resus.org.uk<br />
<strong>Ambulance</strong> employee<br />
responded to<br />
emergency call while<br />
working from home<br />
A member of East of England<br />
<strong>Ambulance</strong> Service who<br />
abandoned an online meeting<br />
to help save a man’s life has<br />
been commended.<br />
George Barber, acting Chief of<br />
Staff for the Trust, was working<br />
from home in a meeting with the<br />
Emergency Operations Centre<br />
in January, when the call came<br />
through the GoodSam app for<br />
first responders.<br />
Mr Barber, who is qualified as<br />
an emergency care assistant,<br />
checked the Trust’s computeraided<br />
despatch system, and saw<br />
the nearest ambulance was still<br />
some distance away.<br />
He left the meeting and jumped<br />
into his car, arriving at the leisure<br />
centre in Saffron Walden to find a<br />
man had gone into cardiac arrest<br />
in the pool.<br />
Mr Barber said: “I arrived to find<br />
police giving good quality CPR<br />
and confirmed with control that it<br />
was both a cardiac arrest and that<br />
critical care were still attending.<br />
Then I supported doing CPR and<br />
maintaining the patient’s airway,<br />
and I had to pull the patient further<br />
out of the water before they were<br />
shocked due to safety.”<br />
The patient eventually regained<br />
partial consciousness before<br />
being taken to hospital, where he<br />
made a full recovery.<br />
Mr Barber, who has gone on<br />
to become a community first<br />
responder for EEAST, has<br />
been given the Chief Officer<br />
Commendation for his actions.<br />
He is just one of 131 people who<br />
received an award as part of<br />
the Trust’s annual ceremony on<br />
Wednesday, July 4.<br />
The ceremony honours courage<br />
and swift action in medical<br />
emergencies by blue-light<br />
colleagues and members of<br />
the public. It also recognises<br />
outstanding commitment,<br />
long service and dedication by<br />
members of EEAST staff.<br />
Tom Abell, chief executive, said:<br />
“George recognised this was<br />
an opportunity to save a life<br />
and instantly stepped out of his<br />
everyday role. Without a doubt, his<br />
actions helped bring this patient<br />
back from the brink of death.<br />
WHY NOT WRITE FOR US?<br />
<strong>Ambulance</strong> <strong>UK</strong> welcomes the submission of<br />
clinical papers and case reports or news that<br />
you feel will be of interest to your colleagues.<br />
Material submitted will be seen by those working within the public and private<br />
sector of the <strong>Ambulance</strong> Service, Air <strong>Ambulance</strong> Operators, BASICS Doctors etc.<br />
All submissions should be forwarded to info@mediapublishingcompany.com<br />
If you have any queries please contact the publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
41
IN PERSON<br />
EEAST NEWS<br />
Essex & Herts Air<br />
<strong>Ambulance</strong>’s Centre for<br />
excellence takes shape<br />
with key appointments<br />
In a significant step forward in delivering<br />
its vision, to create a world-leading<br />
community through which prehospital care<br />
is developed to achieve the best possible<br />
outcomes for all patients, local life-saving<br />
charity, Essex & Herts Air <strong>Ambulance</strong><br />
(EHAAT), has made four key appointments<br />
to its Centre for Excellence.<br />
The Centre for Excellence is underpinned<br />
by its four pillars: Research and Scholarship,<br />
Innovation, Education and Training, and<br />
Community, which support three overarching<br />
clinical domains of cardiac arrest, head injury<br />
and patient experience and outcomes. Together<br />
these create a framework where working<br />
collaboratively, the highest possible standards of<br />
pre-hospital clinical care can be reached.<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
Advanced Paramedic Practitioner, Lisa<br />
Burrell, has joined the Centre for Excellence<br />
team as Education and Training Lead. A<br />
busy mother of three, she brings a wealth<br />
of experience to the new role, and also runs<br />
a MSc in Advanced Clinical Practice at St<br />
George’s, University of London.<br />
Lisa’s role in the Centre for Excellence will<br />
be primarily focused on embracing the<br />
training needs and professional development<br />
of EHAAT’s clinical teams, and the wider<br />
medical community. Working alongside<br />
colleagues, she will also be responsible for<br />
creating a strategy which focuses on sharing<br />
best practice, to ensure prehospital care<br />
is developed to make a real difference to<br />
patients and their families.<br />
Lisa said: “I am thrilled to join such a highly<br />
motivated and talented team. EHAAT has a<br />
strong reputation for leading development<br />
in prehospital critical care, and it is a great<br />
privilege to be part of the innovative journey<br />
going forward with the Centre for Excellence.”<br />
Consultant Neurosurgeon, Professor Chris<br />
Uff, has been appointed as the Centre for<br />
Excellence Academic Lead for Head Injury.<br />
Keen triathlete and violin maker, Professor Uff<br />
is head of neuro trauma and neurovascular<br />
surgery at The Royal London Hospital and<br />
Major Trauma Centre in East London. His role<br />
will see him working with the clinical teams<br />
at EHAAT, and linking up with other partner<br />
organisations, to understand more about head<br />
injury and what new and innovative treatment<br />
options are available to reduce the lasting<br />
effects of what can be a catastrophic injury.<br />
Professor Uff said: “I’m delighted to join the<br />
EHAAT team as academic head injury lead.<br />
Working with such diverse and unique talent<br />
places us in an enviable position to deliver<br />
outstanding and innovative care to our<br />
patients.”<br />
Adam Carr, who has been with EHAAT since<br />
2013 as a Critical Care Paramedic and more<br />
recently Head of Patient & Family Liaison,<br />
has been promoted into the new role of<br />
Community Lead (Clinical) at the Centre for<br />
Excellence. In this new role, Adam will deliver<br />
and oversee a co-ordinated community<br />
training programme covering CPR and<br />
defibrillators, so that the public are better able<br />
to make life-saving interventions in the crucial<br />
minutes following an incident.<br />
Adam said: “Being given the opportunity and<br />
resources to set up the ‘Community’ pillar<br />
of EHAATs Centre for Excellence is such a<br />
huge and exciting opportunity for me. Over<br />
my time with EHAAT, I have seen, on a regular<br />
basis, the difference bystander CPR makes to<br />
the outcome of our patients. For this reason,<br />
one of my main initial projects is going to be<br />
ensuring CPR and AED (defibrillator) training<br />
is accessible and available to as many of the<br />
good people of Essex and Hertfordshire as<br />
possible. I genuinely believe this will benefit<br />
our local communities and beyond, I can’t<br />
wait to get started!”<br />
Dr Sarah McLachlan has been appointed<br />
as Centre for Excellence Research Lead.<br />
Having worked with EHAAT for the last five<br />
years, she is also a Senior Research Fellow in<br />
Health Sciences Research at Anglia Ruskin<br />
University. Sarah’s new role at EHAAT will be<br />
focused on building and leading a team to<br />
deliver the charity’s research and scholarship<br />
strategy. She will also lead on research<br />
collaborations with other organisations, as<br />
well as patients and members of the public.<br />
Sarah said: “I am delighted to have the<br />
privilege of leading the implementation of<br />
our exciting Centre for Excellence research<br />
and scholarship strategy. The strategy<br />
focuses on enhancing our understanding of<br />
patients’ experiences and outcomes, and<br />
producing high quality evidence to help drive<br />
continual improvements in the care that we<br />
provide, especially around head injury and<br />
cardiac arrest.”<br />
42<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
IN PERSON<br />
Dr Gareth Grier, Project Lead at the Centre<br />
for Excellence, is delighted to welcome<br />
Sarah, Lisa, Chris, and Adam to the Centre<br />
for Excellence team. He said: “Our vision for<br />
the Centre for Excellence is bold, innovative<br />
and sits at the heart of the community. With<br />
Chris, Sarah, Adam and Lisa on board, and<br />
their combined knowledge and experience,<br />
I have no doubt that we will be able to take<br />
constructive steps in our aim to create a world<br />
leading community, where clinical excellence<br />
sits at the centre of our ambition, ensuring<br />
prehospital care is developed to make a real<br />
difference in achieving the best possible<br />
outcomes for patients and their families in our<br />
region and beyond.”<br />
To support, donate and find out more about<br />
EHAAT and the Centre for Excellence visit<br />
https://www.ehaat.org.<br />
NEWS<br />
New Medical Director,<br />
Dr Andy Lockyer<br />
Prior to his appointment as Medical Director<br />
at GWAAC, Dr Lockyer among other activities<br />
completed several fundraising challenges,<br />
organised a Women in PHEM event to<br />
encourage female Doctors to consider this<br />
career path, and was Blood Transfusion<br />
Clinical Governance Lead for three years.<br />
“It will be a great honour to serve GWAAC<br />
going forward. The organisation has seen<br />
a few challenges over the years including<br />
the move to our current airbase and the<br />
pandemic. I can see a real opportunity to<br />
progress the medical team. We have an<br />
incredibly talented team of people; I want to<br />
harness this as best as possible so we remain<br />
a cutting-edge critical care service, with all the<br />
latest developments that we can provide.”<br />
Dr Andy Lockyer, Medical Director, Great<br />
Western Air <strong>Ambulance</strong> Charity<br />
As GWAAC’s Medical Director, Dr Lockyer<br />
will take leadership of all aspects of GWAAC’s<br />
medical team, including performance,<br />
standards, overseeing audit processes, and<br />
staffing. He will represent all GWAAC Doctors<br />
and work closely alongside Advanced Clinical<br />
Practitioner in Critical Care, Vicki Brown,<br />
who is the lead for GWAAC’s Specialist<br />
Paramedics in Critical Care.<br />
Jonny joins the Trust from North West<br />
<strong>Ambulance</strong> Service, where he is currently the<br />
Chief of Digital and Innovation.<br />
Prior to that, he spent 15 years in the private<br />
sector, including as a Business Intelligence<br />
Director at Health Management Ltd and Client<br />
Intelligence Manager at Capita.<br />
Chief Executive Jason Killens said: “The<br />
Welsh <strong>Ambulance</strong> Service has undergone<br />
significant transformation over the last couple<br />
years and is today celebrated as one of the<br />
most innovative of its kind internationally.<br />
“We want this to continue, and Jonny’s<br />
appointment is testament to just how<br />
committed we are to using digital technology<br />
to enhance our services.<br />
“Jonny brings a wealth of expert knowledge<br />
and experience, and we look forward to him<br />
joining the #TeamWAST family.”<br />
Jonny’s priorities on entering the Trust<br />
will be to deliver and evolve the digital<br />
strategy, create the right conditions for<br />
digital innovation and review the technology<br />
adoption and training approach.<br />
He will also develop a pipeline of development<br />
NEWS<br />
Welsh <strong>Ambulance</strong> Service<br />
appoints new Director of<br />
Digital<br />
opportunities, harness partnerships to help us<br />
become a digital exemplar organisation and<br />
ensure our cyber security continues to meet<br />
and overcome daily challenges.<br />
Jonny said: “I am absolutely thrilled to be<br />
joining the Welsh <strong>Ambulance</strong> Service as its<br />
new Director of Digital.<br />
“I’m excited to be a part of such a forwardthinking<br />
organisation and as I settle into the<br />
Dr Lockyer joined GWAAC in 2016 when he<br />
started his pre-hospital emergency medicine<br />
(PHEM) training. He qualified as a Critical Care<br />
role, I am eager to support the organisation<br />
through delivery of our digital innovations and<br />
solutions.<br />
Doctor in 2017 and achieved the Fellowship in<br />
Immediate Medical Care in 2019.<br />
He has been a Consultant in Emergency<br />
Medicine at the Bristol Royal Infirmary since<br />
2018, where he is the Clinical Lead for major<br />
incident planning, public health, major trauma,<br />
education, and global health. He is also the<br />
BRI’s Global Emergency Medicine Program’s<br />
lead consultant, for which he won their <strong>2023</strong><br />
Unsung Hero award, and a Trustee of the<br />
related international medical charity.<br />
THE Welsh <strong>Ambulance</strong> Service has<br />
appointed a new Director of Digital.<br />
Jonny Sammut has been appointed to<br />
oversee an ambitious digital services strategy<br />
which will support the delivery of patient care<br />
and improve the experience of staff.<br />
“I believe that digital has a big part to play in<br />
further enhancing the care we provide to our<br />
patients and the day-to-day experience of our<br />
colleagues.<br />
“I’m looking forward to solving everyday<br />
problems and building on our digital<br />
ecosystem by exploring state-of-the-art<br />
technologies and data-driven insights.<br />
“I am excited to embark on this journey.”<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
43
IN PERSON<br />
Jonny is the successor of Andy Haywood,<br />
who joined the Trust in 2020 as its first ever<br />
Director of Digital.<br />
Since Andy’s departure for pastures new last<br />
year, Leanne Smith, Assistant Director for<br />
Data and Analytics, has been carrying the<br />
portfolio on an interim basis.<br />
Jonny will join the Trust officially in September.<br />
NEWS<br />
NHS England appoints Chief<br />
Information Officer<br />
transformations throughout his career, and so<br />
brings a wealth of experience and expertise to<br />
the role of Chief Information Officer.<br />
“I’ve found John’s measured, insightful, and<br />
outcomes-oriented approach to problem<br />
solving invaluable since he joined NHS<br />
England.<br />
“I know the whole team will continue to value<br />
his wise and caring leadership style, as we<br />
adopt the latest technology to transform the<br />
NHS and improve care for patients.”<br />
NEWS<br />
London <strong>Ambulance</strong> Service<br />
chief paramedic appointed<br />
as visiting professor in<br />
Paramedic Science<br />
“The paramedic role has evolved dramatically<br />
over the last two decades and there is now an<br />
incredible wealth of experience, and expertise<br />
within the profession, as well as career<br />
development and board-level opportunities.”<br />
In 2021 Dr Martin was appointed the first<br />
Chief Paramedic at London <strong>Ambulance</strong><br />
Service, a newly created role which brings<br />
together responsibility for clinical quality and<br />
for ensuring paramedics and ambulance<br />
clinicians have access to world-class training,<br />
education and professional development.<br />
In this role, he has overseen accountability<br />
for emergency preparedness, resilience and<br />
response during Her Majesty the Queen’s<br />
funeral.<br />
He was invited to be the paramedic advisor to<br />
the emergency medical committee during the<br />
London 2012 Olympics games, supporting<br />
expert provision on the field of play.<br />
Also among his many career highlights, Dr<br />
Martin has given evidence in both the House<br />
of Lords and at the Commons Health and<br />
NHS England has appointed a new Chief<br />
Information Officer to oversee digital<br />
technology across the health service.<br />
John Quinn has been offered the role<br />
following a rigorous recruitment process.<br />
His key responsibilities will include running<br />
and evolving the NHS’s critical technical<br />
infrastructure and managing cyber security for<br />
national services.<br />
The most senior paramedic at London<br />
<strong>Ambulance</strong> Service (LAS) has been<br />
appointed to a prestigious teaching post<br />
at his former university where he will share<br />
his experience with the next generation of<br />
Social Care Select Committee.<br />
Daniel Elkeles, Chief Executive at London<br />
<strong>Ambulance</strong> Service, said:<br />
“John is a fantastic role-model for others in the<br />
NHS and I’m so pleased that he continues to<br />
inspire the next generation of paramedics and<br />
leaders in the London <strong>Ambulance</strong> Service and<br />
wider ambulance workforce.<br />
John has been filling the role on a temporary<br />
basis since February and was previously<br />
the Executive Director of IT Operations and<br />
Enterprise Services at NHS Digital.<br />
He also spent eight years in leadership roles<br />
at the Medicines and Healthcare products<br />
Regulatory Agency (MHRA), including as the<br />
Executive Director for Technology, Digital Data<br />
and Delivery during the pandemic.<br />
paramedics.<br />
Chief Paramedic Dr John Martin has been<br />
appointed visiting professor in Paramedic<br />
Science at the University of Hertfordshire. It<br />
is the second honour this week for Dr John<br />
Martin who was awarded His Majesty’s<br />
the King’s <strong>Ambulance</strong> Service Medal for<br />
distinguished service in the monarch’s<br />
Birthday Honours last weekend.<br />
“We are very lucky to have someone who is<br />
so passionate and inclusive about developing<br />
others starting out in the profession and<br />
helping to shape the skills and knowledge<br />
that our medics need to serve the people of<br />
London.”<br />
Many graduates of the University of<br />
Hertfordshire go on to have successful<br />
careers at London <strong>Ambulance</strong> Service.<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
He spent the earlier part of his career in<br />
the Department for Education in Digital,<br />
Technology, Project Delivery and Knowledge<br />
Management roles.<br />
Dr Tim Ferris, National Director of<br />
Transformation at NHS England, said:<br />
“John has led significant digital<br />
Dr John Martin, Chief Paramedic and Deputy<br />
Chief Executive at London <strong>Ambulance</strong><br />
Service, said:<br />
“Being a paramedic is an incredible and<br />
satisfying career and I’m delighted to return to<br />
the University of Hertfordshire as a professor<br />
where I completed my original Paramedic<br />
Science degree over 20 years ago.<br />
Each year we recruit around 500 paramedics,<br />
50 percent of whom are recruited through<br />
apprenticeships and Paramedic Science<br />
degrees in the <strong>UK</strong>, with the rest of the<br />
paramedic workforce recruited internationally<br />
and from other NHS organisations. The<br />
Service is hoping to recruit over 1,400<br />
frontline staff, including paramedics, as part of<br />
its 2022-23 recruitment programme.<br />
44<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
19-20 SEPTEMBER <strong>2023</strong><br />
PREPARING OUR EMERGENCY<br />
SERVICES FOR EVERY RESPONSE<br />
500+<br />
EXHIBITORS<br />
10,000+<br />
PRODUCTS AND SOLUTIONS<br />
CPD<br />
ACCREDITED CONTENT<br />
16,000+<br />
VISITORS<br />
NEW LAUNCH<br />
REGISTER FOR YOUR FREE PASS<br />
WWW.EMERGENCY<strong>UK</strong>.COM
COMPANY NEWS<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
Mer helps NHS trust<br />
take a lead on fleet<br />
electrification<br />
An NHS trust is taking a<br />
leading role in transitioning its<br />
fleet to electric vehicles (EVs)<br />
after a major project to install<br />
charging infrastructure.<br />
London, <strong>UK</strong>, 05 July <strong>2023</strong> –<br />
Cumbria, Northumberland, Tyne<br />
and Wear NHS Foundation Trust<br />
has been able to accelerate its<br />
fleet electrification after Mer<br />
installed charge points at 13<br />
of its sites. Mer worked on the<br />
project with NTW Solutions<br />
Ltd, which is the subsidiary<br />
responsible for support services<br />
to the Trust. NTW Solutions<br />
provides the Trust with estates<br />
and facilities management, car<br />
leasing, finance, workforce and<br />
procurement services.<br />
Lee Cant, Commercial Director<br />
of NTW Solutions, said: “Working<br />
with Mer to procure these<br />
chargers has been an enabler<br />
for us to move forward with our<br />
decarbonisation strategy. We<br />
benchmark ourselves against<br />
other trusts in the region and<br />
we know that we are out in front<br />
in terms of fleet electrification<br />
thanks in part to this project.”<br />
NTW Solutions runs a fleet<br />
of 1,400 lease cars for Trust<br />
employees as well as around 90<br />
service vehicles ranging from<br />
pool cars to vans and trucks.<br />
“In total 40 percent of the lease<br />
cars are now fully electric or plugin<br />
hybrids, while about a quarter<br />
of the service fleet is the same,”<br />
added Lee. “Some of the service<br />
vehicles are larger and they<br />
need full payloads for operations<br />
like laundry, so they won’t be<br />
electrified yet, we’ll concentrate<br />
for now on the lighter vans.”<br />
Mer won a competitive tender<br />
to deliver the charge points after<br />
meeting all the key criteria. One<br />
of the main priorities for the Trust<br />
was the ability to set different<br />
tariffs – free charging for fleet<br />
vehicles, a preferential rate for<br />
staff, and a higher rate for visitors.<br />
Working with Mer<br />
to procure these<br />
chargers has been<br />
an enabler for us to<br />
move forward with<br />
our decarbonisation<br />
strategy. We<br />
benchmark ourselves<br />
against other trusts<br />
in the region and we<br />
know that we are out<br />
in front in terms of<br />
fleet electrification<br />
thanks in part to this<br />
project..<br />
“It was imperative that we could<br />
set different rates for public<br />
charging, staff charging, and also<br />
for our fleet service vehicles,”<br />
said Lee. “It was important to be<br />
able to differentiate for different<br />
use cases and also to have<br />
different methods of accessing<br />
the chargers, from contactless<br />
payment to RFID cards and key<br />
fobs.<br />
“We were also keen on having a<br />
viable management system that<br />
we could extract data from, in<br />
order to ascertain which chargers<br />
were the most popular and<br />
identify where we might need<br />
additional infrastructure to meet<br />
demand.<br />
“Mer has been fantastic;<br />
they have gone above and<br />
beyond in terms of customer<br />
service. Working with them<br />
has significantly increased the<br />
speed of electrification and the<br />
decarbonisation of our fleet.<br />
“We had a lot of wards that were<br />
not prepared to go electric until<br />
there were chargers on site. For<br />
example, we have a 24/7 crisis<br />
service that operates around the<br />
clock so needs constant access<br />
to the vehicles. With the mileage<br />
that they do and the size of the<br />
area they cover, they needed<br />
reliable charging infrastructure on<br />
site to give them that confidence<br />
to go electric.<br />
“It has enabled us to change our<br />
policy so that all new vehicles<br />
added to the fleet have to be<br />
electric unless there is a very<br />
good operational reason why they<br />
can’t be EVs.”<br />
Scott Duncan, associate<br />
consultant at Mer, said: “We<br />
are proud to be helping the<br />
Trust with the decarbonisation<br />
of its fleet. This was a complex<br />
but rewarding project to install<br />
chargers across multiple<br />
locations. The Trust is making<br />
full use of the smart charger<br />
technology to set different tariffs<br />
for various use cases and utilise<br />
Mer’s proprietary back-office<br />
software for data analytics.”<br />
For more information visit https://<br />
uk.mer.eco/emergency-services/<br />
Durabook upgrades<br />
its U11I fully rugged<br />
tablet to better<br />
support emergency<br />
services<br />
Durabook, the global rugged<br />
mobile solutions specialist,<br />
has significantly upgraded<br />
its U11I fully-rugged tablet to<br />
offer unparalleled versatility<br />
for emergency service crews<br />
performing their critical work.<br />
Not oema With its 12th Gen Intel ®<br />
CPU processor and architectural<br />
innovations, the U11I is the most<br />
versatile 11-inch rugged tablet,<br />
exceeding standard requirements<br />
and elevating the user experience<br />
for mobile workforces and<br />
response teams.<br />
Performance is up to 225% faster<br />
than its predecessor, ideal for<br />
ambulance workers operating<br />
in time-critical situations, while<br />
its Coolfinity fanless thermal<br />
solution offers increased<br />
dependability and reduced<br />
downtime so crews are assured<br />
of optimal performance in any<br />
conditions.<br />
Designed for endurance, the<br />
tablet is certified to withstand<br />
drops of up to 6 feet and<br />
remains functional in the extreme<br />
temperatures conducive to<br />
emergency services work.<br />
Additionally, its ultra-long battery<br />
life of up to 10 hours, plus an<br />
optional extra 20 hours, means<br />
emergency services crews can<br />
trust it to last an entire shift.<br />
Performance is up<br />
to 225% faster than<br />
its predecessor,<br />
ideal for ambulance<br />
workers operating<br />
in time-critical<br />
situations, while its<br />
Coolfinity fanless<br />
thermal solution<br />
offers increased<br />
dependability and<br />
reduced downtime so<br />
crews are assured of<br />
optimal performance<br />
in any conditions.<br />
The U11I is equipped with<br />
advanced wireless capabilities<br />
for powerful yet simple and<br />
flexible connectivity. Response<br />
teams benefit from increased<br />
throughput, simultaneous<br />
connections and improved<br />
consistency in dense areas so,<br />
wherever they are, they can<br />
connect with the hospital to<br />
46<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
COMPANY NEWS<br />
receive critical patient data for<br />
rapid diagnosis and treatment.<br />
“The upgraded U11I tablet<br />
far exceeds expectations by<br />
boosting productivity and<br />
offering unparalleled versatility<br />
and reliability, which is critical<br />
for emergency services teams<br />
operating in the most challenging<br />
situations.” said Twinhead CEO<br />
Fred Kao.<br />
For more information on how<br />
the U11I can enhance your<br />
organisation’s operations, visit<br />
www.durabook.com, or contact<br />
marketing@durabook.com<br />
Mer x <strong>Ambulance</strong> <strong>UK</strong><br />
Healthcare services are<br />
actively supporting the net<br />
zero transition. Electrifying<br />
emergency service fleets is a<br />
fundamental part of meeting<br />
key sustainability goals in the<br />
coming years.<br />
With the transition to zeroemission<br />
emergency vehicles<br />
comes the need for the right<br />
kind of charging infrastructure,<br />
to ensure the vehicles are ready<br />
and available to respond to<br />
unforeseeable situations at all<br />
times. No two emergency fleets<br />
are the same, and neither is the<br />
charging infrastructure required<br />
to power the fleet.<br />
Fleet managers do not have to<br />
think about how, when and where<br />
their fleets will charge alone. Mer,<br />
a leading EV charging company<br />
backed by Statkraft, Europe’s<br />
largest renewable energy<br />
generator, supports healthcare<br />
teams transition their emergency<br />
fleets to electric by providing<br />
suitable, reliable EV charging<br />
infrastructure.<br />
As a leading supplier of EV<br />
charging to <strong>UK</strong> public services<br />
and with more than 10 years’<br />
experience in the industry, Mer<br />
provides free consultancy for<br />
Fleet managers do<br />
not have to think<br />
about how, when and<br />
where their fleets will<br />
charge alone. Mer, a<br />
leading EV charging<br />
company backed by<br />
Statkraft, Europe’s<br />
largest renewable<br />
energy generator,<br />
supports healthcare<br />
teams transition<br />
their emergency<br />
fleets to electric by<br />
providing suitable,<br />
reliable EV charging<br />
infrastructure.<br />
NHS and ambulance services.<br />
Mer offers expert guidance on<br />
infrastructure requirements,<br />
operation models and power<br />
connections. It’s Operator<br />
Portal offers clear visibility<br />
of charger health, availability<br />
and functionality, and the<br />
company provides full aftercare,<br />
maintenance, and 24/7 support<br />
once the infrastructure has been<br />
installed.<br />
Mer is hosting a webinar to help<br />
personnel in the healthcare<br />
services understand how to build<br />
an EV charging infrastructure<br />
portfolio that is reliable, future-fit<br />
and attentive to the demands of<br />
their specific fleet.<br />
To learn more about how Mer<br />
can help you transition your<br />
emergency service fleet to<br />
electric, attend its Electrifying the<br />
Emergency Services webinar.<br />
Link: https://uk.mer.eco/<br />
emergency-services/?utm_<br />
medium=editorial&utm_<br />
source=ambulanceuk&utm_<br />
campaign=Emergency%20<br />
Services<br />
Webasto heating<br />
and air conditioning<br />
systems<br />
Webasto heating and air<br />
conditioning systems are used<br />
by front line fleets with systems<br />
designed to meet exacting,<br />
tailored requirements. Our<br />
products are designed<br />
to provide exceptional<br />
performance and service.<br />
Not only do we provide<br />
comfortable working climates for<br />
the crew, we can also achieve a<br />
reduction in idling times which<br />
in turn lowers fuel consumption,<br />
decreases overall operating<br />
costs and helps us to remain<br />
focused towards improving the<br />
environment.<br />
Webasto products have been a<br />
mainstay for one of the largest<br />
fleets in the <strong>UK</strong> for many years,<br />
based on an impressive reliability<br />
record and ease of operational<br />
function.<br />
Not only do we<br />
provide comfortable<br />
working climates for<br />
the crew, we can also<br />
achieve a reduction<br />
in idling times<br />
which in turn lowers<br />
fuel consumption,<br />
decreases overall<br />
operating costs and<br />
helps us to remain<br />
focused towards<br />
improving the<br />
environment.<br />
A parts locator and replacement<br />
part service are available to<br />
ensure your own people get<br />
the best operational efficiency<br />
from the fleet. Clear and concise<br />
training material, with regular<br />
updates are also offered either at<br />
Webasto’s training academy, or at<br />
your own depot locations to suit<br />
your needs.<br />
For many large fleets, demands<br />
placed on both crew and vehicle<br />
can be extremely arduous, so it<br />
is of vital importance that both<br />
remain fully optimised to respond<br />
when it really matters. When<br />
considering these demands and<br />
agreeing on a build specification<br />
for your frontline ambulance,<br />
rapid response, and patient<br />
transport service vehicles we<br />
will only specify products that<br />
meet the exacting standards<br />
and performance expected from<br />
Webasto.<br />
Webasto is the largest producer<br />
of auxiliary heaters and air<br />
conditioning in Europe. Let us<br />
take you through the options.<br />
For an informal chat, call David<br />
Stafford on 01302 381141 or<br />
email david.stafford@<br />
webasto.com<br />
AMBULANCE <strong>UK</strong> – AUGUST<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
47
Data Driven Vehicle Telematics & Asset Monitoring<br />
Prior to deployment, during the mission and post event.<br />
Vehicle<br />
Maintenance<br />
Reduce<br />
unnecessary<br />
VOR time.<br />
Role<br />
Equipment<br />
Detailed status<br />
and activity<br />
logs.<br />
Fuel<br />
Consumption<br />
Increase mpg<br />
and reduce<br />
emissions.<br />
Make Ready<br />
Improve vehicle<br />
turnaround<br />
times.<br />
Equipment<br />
Compliance<br />
Comply with<br />
device servicing<br />
schedules.<br />
Inventory<br />
Monitoring<br />
Monitor real<br />
time equipment<br />
inventories.<br />
Consumables<br />
Management<br />
Manage<br />
consumable item<br />
replenishment.<br />
The Insight Platform provides unrivalled levels of data for fleet and asset management, as well<br />
as CCTV capability. Whether you’re aiming for a net zero fleet or want to know where your most<br />
valuable assets are at any given time, to understanding compliance levels of key assets or replay any<br />
crashes/ incidents in real time, the Insight Platform can help.<br />
Visit us at stand K150 to learn how our technology benefits<br />
multiple clients across <strong>UK</strong> <strong>Ambulance</strong> Trusts, and other<br />
mission critical sectors.<br />
www.theortusgroup.com<br />
E: hello@ortus.co.uk<br />
T: 0845 459 4705