Ambulance UK April 2024
Ambulance UK April 2024
Ambulance UK April 2024
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume 39 No. 8<br />
<strong>April</strong> <strong>2024</strong><br />
DEDICATED TO THE AMBULANCE SERVICE AND ITS SUPPLIERS
CONTENTS<br />
MAKE A<br />
LEGENDARY<br />
MOVE<br />
CONTENTS<br />
4 EDITOR’S COMMENT<br />
6 FEATURE<br />
6 5 WAYS TO MISS AN ACUTE MYOCARDIAL INFARCTION<br />
8 DISCUSSION: WHERE IS THE OCCLUSION?<br />
10 NEWSLINE<br />
30 IN PERSON<br />
<strong>Ambulance</strong> <strong>UK</strong><br />
This issue edited by:<br />
Matt House<br />
c/o Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
ADVERTISING:<br />
Terry Gardner, Samantha Marsh<br />
CIRCULATION:<br />
Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
Tel: 01886 853715<br />
E: info@mediapublishingcompany.com<br />
www.ambulanceukonline.com<br />
Every day is different as a St John WA paramedic, and we have multiple<br />
opportunities available for qualified and experienced <strong>Ambulance</strong> Paramedics<br />
to come join us in beautiful Western Australia.<br />
The offer:<br />
• Visa application support<br />
• Paid for one-way economy airline ticket<br />
• Accommodation upon arrival to<br />
Western Australia<br />
• Additional relocation costs covered<br />
Don’t have current Australian<br />
working rights? No problem!<br />
For candidates to successfully be employed as<br />
an <strong>Ambulance</strong> Paramedic, they must meet the<br />
following minimum requirements:<br />
• Professional registration as a Paramedic with<br />
the Paramedicine Board of Australia (AHPRA)<br />
or willingness to obtain.<br />
• Recent experience employed and working<br />
within a jurisdictional ambulance service in<br />
Australia or internationally (St John New<br />
Zealand or London <strong>Ambulance</strong> Service for<br />
example) as a paramedic for at least two years.<br />
• Hold a full driver’s license with no restrictions.<br />
Successful candidates are required to obtain<br />
a light rigid driver’s license within the first six<br />
months of employment. Costs associated with<br />
obtaining the required driver’s license are the<br />
responsibility of the candidate.<br />
• Candidates that do not hold current Australian<br />
working rights, must meet the visa eligibility<br />
requirements, as outlined by the Department<br />
of Home Affairs.<br />
The location:<br />
• Diverse landscape means diverse daily routine<br />
• Safe and stable economy<br />
• Over two-thirds of the year is beautifully clear<br />
and sunny<br />
• Incredible work/life balance with world-class<br />
dining, festivals and more<br />
Ready to make a<br />
legendary move?<br />
Go on, a career with loads of diversity<br />
and an amazing lifestyle is waiting!<br />
Search stjohnwa.com.au/directentry<br />
Scan to learn more:<br />
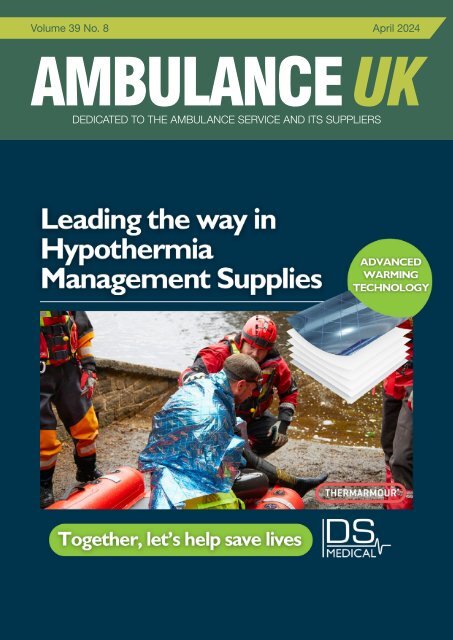
COVER STORY<br />
Why does hypothermia matter?<br />
Clinicians are well aware that hypothermia is one of the lethal triad. Checking for,<br />
alleviating, and monitoring the effects of hypothermia are all crucial during first<br />
assessments of a trauma casualty through to their handover at A&E.<br />
What’s the challenge with current solutions?<br />
Whilst traditional foil blankets are somewhat effective at reflecting and trapping body heat,<br />
they have limited insulative properties. Used alone, single layer foil blankets will typically<br />
not provide sufficient warmth to prevent hypothermia from setting in between pre-hospital<br />
services and A&E.<br />
On the other hand, blankets that rely solely on-air capture technology, whilst demonstrably<br />
effective in emergency situations, are cumbersome in size and design so may not be<br />
practical to remain with the patient from incident to A&E.<br />
Why switch to THERMARMOUR?<br />
Simple to use: THERMARMOUR blankets are clinically proven to maintain normothermia<br />
using convective and reflective technology - they are effective as soon as they are placed<br />
around the casualty.<br />
Adaptable: THERMARMOUR blankets are X-ray compatible, can be pre-warmed where<br />
required and can easily be folded, reshaped, or cut to fit patient needs. They are water<br />
and wind proof and will begin the warming process in any environment…<br />
Work without a secondary heat source: THERMARMOUR’s unique multi layered design<br />
creates an immediate thermal envelope around the casualty, capturing heat using the<br />
body’s own warmth, limiting the need for active warming interventions from incident to<br />
A&E assessment.<br />
Cost-Effective: THERMARMOUR is a cost effective and practical alternative to traditional<br />
air capture technology.<br />
Available at https://dsmedical.co.uk/blankets/thermarmour-emergency-blanket-2m-x-1-<br />
PUBLISHED BI-MONTHLY:<br />
February, <strong>April</strong>, June, August,<br />
October, December<br />
COPYRIGHT:<br />
Media Publishing Company<br />
Greenoaks<br />
Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company<br />
Next Issue June <strong>2024</strong><br />
Designed in the <strong>UK</strong> by TGDH<br />
Do you have For anything further recruitment you would vacancies like to add visit: or include? www.ambulanceukonline.com<br />
Please contact us and let us know.<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
3
EDITOR’S COMMENT<br />
EDITOR’S COMMENT<br />
“It feels like<br />
we have had<br />
another long<br />
winter, which<br />
has brought<br />
with it, its<br />
fair share of<br />
challenges<br />
across the<br />
<strong>Ambulance</strong><br />
Sector”<br />
Welcome to the latest edition of <strong>Ambulance</strong> <strong>UK</strong>. As I write this, I’m seeing the first signs of spring. When I<br />
took my dog out for his walk this morning, the sky was blue, and I didn’t have to dress up in multiple layers<br />
just to keep warm. The first daffodils are blooming and the trees in the garden are showing the first signs<br />
of blossom.<br />
It feels like we have had another long winter, which has brought with it its fair share of challenges across the<br />
ambulance sector. Yet despite this, people have stepped up and worked hard. We are seeing more joinedup<br />
work as other areas of the NHS work with the ambulance sector to help us find alternatives to emergency<br />
departments and seek solutions to the hospital delays that have plagued us in recent years. I think I seem<br />
to be seeing other providers coming to us with suggestions for improvements or offering answers. These<br />
include changes to the same day emergency care (SDEC), which will make referrals easier, direct lines to<br />
consultants for advice on patient disposition, and single points of contact for ambulance referrals into other<br />
out of hospital providers.<br />
These are just a few of the initiatives that are being worked through. Some are re-works of existing or<br />
historical processes, whereas some are entirely new ideas. It’s good to see that, whatever the motivation,<br />
people are working together to help. From my perspective, the difference this time is that we are starting to<br />
find that the people external to the ambulance service are thinking of system-wide solutions more than they<br />
have done in the past. I am aware that there are external factors that have influenced this move, but it is still<br />
gratefully received.<br />
We are certainly not out of the woods yet, but we are definitely moving in the right direction. For our part, we<br />
need to assess honestly what we are doing and not be afraid to stop things or change direction when they<br />
are not adding benefit, while increasing or adding the things that are.<br />
So, as we see the first of the blue skies this year and the thermometer reaching double figures, we plan for<br />
time away from work. Let’s also look forward to a better year at work. I hope the work we and our partners<br />
are all doing will help provide our clinicians with much better options for their patients.<br />
Finally, I would just like to congratulate the College of Paramedics on being granted the Charter of<br />
Incorporation by His Majesty King Charles III. This is an important milestone for the profession. Well done!<br />
Matt House, Co-Editor <strong>Ambulance</strong> <strong>UK</strong><br />
PREPARING OUR EMERGENCY<br />
SERVICES FOR EVERY RESPONSE<br />
16,000+<br />
VISITORS<br />
600+<br />
EXHIBITORS<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
4<br />
Publishers Statement<br />
For nearly 40 years, thanks to trade support, we have been able to provide <strong>Ambulance</strong> <strong>UK</strong> FREE<br />
OF CHARGE in the knowledge that those receiving our dedicated bi monthly publication enjoy<br />
having something to read during their free time however, return on investment seems to be the buzz<br />
word amongst <strong>Ambulance</strong> Service Suppliers these days, therefore if you enquire about a product<br />
advertised, please mention <strong>Ambulance</strong> <strong>UK</strong> as it help us confirm to the trade that we are reaching<br />
the right people and providing advertisers with value for money. In respect of our current edition we<br />
would like to thank the following companies for their support as without their contribution towards our<br />
print and postal costs this issue would not have been published - Alpha Labs, APG, Bluelight <strong>UK</strong>,<br />
DS Medical, IAM Roadsmart, ORTUS, Proact Medical, St Johns WA, WEL Medical.<br />
Terry Gardner<br />
Publisher<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
20,000+<br />
PRODUCTS &<br />
SOLUTIONS<br />
FIND OUT MORE<br />
EMERGENCY<strong>UK</strong>.COM<br />
CO-LOCATED WITH
FEATURE<br />
5 WAYS TO MISS AN ACUTE<br />
MYOCARDIAL INFARCTION<br />
Jerry W. Jones, MD FACEP FAAEM<br />
1. You stop looking too soon!<br />
If you were at home with your 2½ year old son or grandson and<br />
you suddenly noticed that he wasn’t in the room with you, you<br />
would go looking for him. Let’s say your home has ten rooms. You<br />
check eight rooms, but he isn’t in any of them. Would you stop<br />
looking for him and just assume he’s OK because he wasn’t in any<br />
of those rooms? Of course not! But that’s what too many people<br />
do when they order a 12-lead ECG for a patient with suspicious<br />
chest pain. They fail to “look in all the rooms.” They all too often<br />
take the advice of colleagues who say, “Well, if it’s not on the 12-<br />
lead ECG, you’re probably not going to find it in any of the other<br />
leads!” (I once overheard a resident tell a medical student this!)<br />
Probably? Think about that word for a moment – probably. It’s a<br />
word you use when you don’t know the answer to a question.<br />
If the patient is having chest pain consistent with an acute<br />
coronary syndrome and the initial 12-lead ECG is non-diagnostic<br />
– look in the posterior leads and the right-sided leads. It is NOT<br />
necessary to have an inferior MI for there to be an inferobasal<br />
(formerly posterior) infarction OR a right ventricular<br />
infarction. An occlusion of the left circumflex artery can easily<br />
cause an inferobasal infarction without an inferior infarction. And<br />
did you know that isolated right ventricular infarctions (without<br />
a concurrent inferior infarction) can occur in up to 5% of ALL<br />
myocardial infarctions?<br />
I can remember a number of times when, as the attending<br />
physician coming on-duty in the emergency department, the offgoing<br />
doctor would tell me about a patient with chest pain who<br />
was having a non-STEMI waiting for a CCU bed. The ECG showed<br />
no changes. The ECG? Singular? The first thing I did was to order<br />
a second ECG which occasionally resulted in my alerting the cath<br />
lab immediately.<br />
Bottom Line: If the first ECG is non-diagnostic, yet you are still<br />
suspicious of an acute MI – repeat the 12-lead ECG every 20<br />
minutes for at least 3 times!<br />
3. Adhering to the STEMI paradigm.<br />
OK… this one is a bit controversial because not everyone has<br />
accepted the Occlusion Myocardial Infarction (OMI) concept<br />
(but I certainly do!).<br />
If you aren’t familiar with OMI, it’s an approach to diagnosing<br />
acute myocardial infarctions by looking for evidence of acute<br />
coronary occlusion rather than an arbitrary, fixed deviation of<br />
the ST segment. Adhering to a fixed measurement to decide if a<br />
patient gets emergent reperfusion or medical management has<br />
one major flaw – you’re going to miss an unacceptable number<br />
of complete or near-complete acute coronary occlusions with<br />
transmural ischemia (25 – 30%) which would definitely benefit from<br />
emergent reperfusion.<br />
resulting in STE in Leads I and aVL which oppose simultaneous<br />
STE in Leads II, III and aVF). And that does NOT include all the<br />
ECGs that do have ST elevation but don’t quite meet the STEMI<br />
criteria and which are neither repeated nor pursued any further<br />
after being diagnosed as “non-STEMIs.”<br />
Bottom Line: If you are not familiar with all these ECG<br />
presentations, you’d better look them up! Better yet, enroll<br />
in The Masterclass in Advanced Electrocardiography<br />
(https://medicusofhouston.com).<br />
5. Depending on the ECG machine<br />
interpretation.<br />
I really don’t have much to say here but I will be brutally blunt: if<br />
part of your job involves ordering ECGs on acutely ill patients and<br />
making medical decisions based on those ECGs, and your ECG<br />
interpretation skills are so poor that you must depend completely<br />
on the ECG machine interpretation, you should find someone with<br />
better skills to see those patients.<br />
Bottom Line: If you are making immediate medical<br />
management decisions based on the ECGs that you are<br />
ordering, you must be able to read those ECGs with a high<br />
level of skill and confidence. If you are depending on the ECG<br />
machine interpretation to direct your management of the<br />
patient, you are betting the patient’s LIFE on a machine that is<br />
notorious for giving incorrect interpretations!<br />
FEATURE<br />
I teach ADVANCED electrocardiography because when a patient’s<br />
LIFE is in YOUR hands, introductory knowledge is simply not enough!<br />
Come join us and be a PARTICIPANT… never just an audience!<br />
WEBSITE: https://medicusofhouston.com<br />
EMAIL: jwjmd@medicusofhouston.com<br />
WHY NOT WRITE FOR US?<br />
Bottom Line: If the initial 12-lead ECG is non-diagnostic,<br />
keep looking using posterior and right-sided leads.<br />
2. Once again, you stopped too soon!<br />
Returning to our allegory of the missing toddler, let’s say you<br />
check the remaining two rooms and you still don’t find him. Some<br />
rooms have more than one door by which one can enter or leave.<br />
The GOOD news: By abiding by the OMI concept, you will miss<br />
fewer acute myocardial infarctions!<br />
The “SO-SO” news: There are no specific algorithms or criteria<br />
to guide you. You are going to have to depend on more advanced<br />
ECG interpretation skills than you did by simply following a “cookbook”<br />
method of diagnosis.<br />
<strong>Ambulance</strong> <strong>UK</strong> welcomes the submission of<br />
clinical papers and case reports or news that<br />
you feel will be of interest to your colleagues.<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
He could have gone out one door as you were entering the other.<br />
And children that age love to hide, so you need to go back through<br />
some of those rooms and look more thoroughly rather than<br />
just glancing.<br />
But too many healthcare providers managing patients with very<br />
credible chest pain don’t take that “second look in all the rooms.”<br />
The repolarization changes indicating acute ischemia (ST elevation)<br />
may not show up immediately and it is not too unusual for a patient<br />
who is indeed having an acute MI to have an initial ECG that shows<br />
nothing – even to an experienced electrocardiographer. It’s also<br />
possible that the reciprocal change may appear before the primary<br />
change of acute ischemia! What IS unusual, however, is for NO<br />
Bottom Line: You are going to need advanced ECG<br />
interpretation skills.<br />
4. Thinking that ST elevation is the only way<br />
to diagnose an acute MI!<br />
There are a number of acute myocardial infarctions that don’t<br />
always manifest with ST elevation: Wellens Syndrome, De Winter<br />
T waves, acute inferobasal (formerly “posterior”) infarctions,<br />
right ventricular infarctions, some proximal occlusions of the left<br />
circumflex artery (resulting in STE in Leads I and aVL which oppose<br />
simultaneous STE in Leads II, III and aVF) and some proximal<br />
Material submitted will be seen by those working within the public and private<br />
sector of the <strong>Ambulance</strong> Service, Air <strong>Ambulance</strong> Operators, BASICS Doctors etc.<br />
All submissions should be forwarded to<br />
If you have any queries please contact the publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
info@mediapublishingcompany.com<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
signs of an acute MI to appear at all during the next hour or two.<br />
occlusions of a “wraparound” left anterior descending artery (also<br />
6<br />
7<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
FEATURE<br />
DISCUSSION: Discussion: WHERE Where IS Is the THE Occlusion? OCCLUSION?<br />
Jerry W. Jones, MD FACEP FAAEM<br />
Jerry W. Jones, MD FACEP FAAEM<br />
Figure 1<br />
Figure 1 (repeated)<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
8<br />
I received<br />
some excellent,<br />
some<br />
well-thought<br />
excellent,<br />
responses<br />
well-thought<br />
and I was<br />
responses<br />
artery – you’re<br />
and<br />
right!<br />
I<br />
But<br />
was<br />
you still<br />
very<br />
haven’t<br />
impressed<br />
answered completely.<br />
with<br />
A<br />
the<br />
very impressed with the degree of advanced skill that many of<br />
superdominant right coronary artery can also produce ST elevation<br />
degree of advanced skill that many of you demonstrated.<br />
you demonstrated.<br />
subtle. All three coronary arteries can create ST elevations in<br />
more than one vascular area on the 12-lead ECG.<br />
There is ST elevation in the inferior (II, III, aVF) leads and ST elevation in all the precordial<br />
other. Apparently, the ST elevation in Lead III was greater than in Lead<br />
Intermediate leads, though Level the ST elevation in Lead V6 is quite aVL because subtle. Lead All III has three retained coronary some STE while arteries the STE in Lead can aVL<br />
has been totally neutralized.<br />
create ST elevations in more than one vascular area on the 12-lead ECG.<br />
OK… we’ve noted inferior ST elevation and anterior ST elevation.<br />
in the inferior leads and ALL the precordial leads. However, the ST<br />
elevation tends to be maximal in Lead V1 and diminishes as we follow<br />
the leads leftward (not the case here). Also, an occlusion of the RCA is<br />
Introductory Level<br />
not going to result in ST elevation of Leads I and aVL. Again, that is not<br />
Obviously,<br />
Introductory<br />
there is a lot of ST<br />
Level<br />
elevation on this ECG! We need to try to the situation here because we have ST elevation in both Leads I and<br />
make sense of it. One reader suggested acute pericarditis. Pericarditis aVL. You don’t see the ST elevation in Lead aVL? That’s because you<br />
is Obviously, characterized by there ST elevation is a that lot is of not ST restricted elevation to a particular on (or this ECG! need advanced We need level skills to to try see to it. make sense of it. One<br />
single)<br />
reader<br />
vascular<br />
suggested<br />
area on the ECG.<br />
acute<br />
While<br />
pericarditis.<br />
that finding is true,<br />
Pericarditis<br />
it is not as<br />
is characterized by ST elevation that is not<br />
specific as we would like. Acute ischemia can frequently involve<br />
restricted<br />
more than one<br />
to<br />
vascular<br />
a particular<br />
region. If you<br />
(or<br />
look in<br />
single)<br />
Lead V6 you<br />
vascular<br />
will see a<br />
area<br />
Advanced<br />
on the ECG.<br />
Level<br />
While that finding is true, it is<br />
gradual not as downsloping specific of the as TP we segment. would That like. is called Acute Spodick’s ischemia Sign You should can have frequently noted that, although involve there is ST more elevation than in the one<br />
and it is said to be characteristic of acute pericarditis. The problem is: inferior leads, Lead III has much less STE than Leads II and aVF. You<br />
vascular region. If you look in Lead V6 you will see a gradual downsloping of the TP<br />
this isn’t acute pericarditis! Thus, Spodick’s Sign is not always reliable also should have noted that there is ST elevation in Lead I which should<br />
as segment. a sign of acute That pericarditis. is Look called at those Spodick’s “tombstones” (massive Sign and be accompanied it is said by STE to in be Lead characteristic aVL – but there doesn’t of appear acute to be<br />
ST elevations) in Leads V2 – V4; you will never see ST elevation of that<br />
pericarditis. The problem is: this isn’t acute pericarditis!<br />
any in that lead.<br />
Thus,<br />
So we have<br />
Spodick’s<br />
two unexpected,<br />
Sign<br />
unexplained<br />
is not<br />
findings:<br />
always<br />
magnitude in acute pericarditis – never!<br />
less STE in Lead III than in Leads II and aVF and essentially no STE<br />
reliable as a sign of acute pericarditis. Look at those<br />
in Lead aVL<br />
“tombstones”<br />
while ST elevation is present<br />
(massive<br />
in Lead<br />
ST<br />
I. Could<br />
elevations)<br />
there be a<br />
There<br />
in Leads<br />
is ST elevation<br />
V2 –<br />
in<br />
V4;<br />
the inferior<br />
you<br />
(II,<br />
will<br />
III, aVF)<br />
never<br />
leads and<br />
see<br />
ST elevation<br />
ST elevation connection? of that Yes! magnitude And that connection in is acute the fact that pericarditis Leads III and aVL –<br />
in all the precordial leads, though the ST elevation in Lead V6 is quite are reciprocal to each other. Both have ST elevation but their systolic<br />
never!<br />
currents of injury are traveling in opposite directions (Lead III: down<br />
and to the right, Lead aVL: up and to the left) and thus cancel each<br />
Which vessel can cause ST elevation of BOTH those vascular areas? Let’s say two leads are reciprocal to each other, like Leads III<br />
If you answered a type 3 (“wraparound”) left anterior descending and aVL…<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
Intermediate Level<br />
If one lead has acute ischemia with ST elevation and the other<br />
remains nonischemic, the nonischemic lead will act reciprocally<br />
and manifest the reciprocal changes of ST depression.<br />
However, if BOTH leads manifest acute ischemia with ST elevation, supports (but doesn’t prove) an occlusion proximal to D1 and distal to<br />
anterior<br />
then based on<br />
descending<br />
their relative locations<br />
artery<br />
to each<br />
–<br />
other,<br />
you’re<br />
the ST<br />
right!<br />
elevations<br />
But<br />
S1.<br />
you<br />
If haven’t<br />
still haven’t<br />
noticed it, look<br />
answered<br />
again before continuing.<br />
completely. A<br />
will cancel each other and it is possible that both leads will have<br />
3 (“wraparound”) LAD. Most people – between 75% to 80% – have<br />
and infarctions.<br />
located in the inferior wall caused by the occlusion of the LAD. So<br />
maybe it is and maybe it isn’t proximal to S1.<br />
OK… we’ve noted inferior ST elevation and anterior ST elevation. Which vessel can cause<br />
As advanced ECG nerds, you should have noticed something that<br />
ST elevation of BOTH those vascular areas? If you answered a type 3 (“wraparound”) left<br />
superdominant right coronary artery can also produce ST elevation in the inferior leads and<br />
normal-appearing ST segments!<br />
The first septal perforator supplies blood to the right bundle branch.<br />
ALL the precordial leads. However, the ST elevation Occlusions tends proximal to to S1 be will often maximal result in acute in Lead RBBB – a V1 very and<br />
Which artery is occluded and at which level is the<br />
ominous sign during an occlusion of the LAD. There is no RBBB<br />
diminishes as we follow the leads leftward (not the case here). Also, an occlusion of the<br />
occlusion located?<br />
present on this ECG. While that adds to the likelihood that the<br />
RCA is not going to result in ST elevation of Leads I and aVL. Again, that is not the situation<br />
occlusion is distal to S1 and proximal to D1, it unfortunately doesn’t<br />
The<br />
here<br />
infarct<br />
because<br />
related artery<br />
we<br />
(IRA)<br />
have<br />
– often<br />
ST<br />
referred<br />
elevation<br />
to as the “culprit”<br />
in both<br />
artery<br />
Leads<br />
prove<br />
I<br />
it.<br />
and aVL. You don’t see the ST elevation<br />
is the left anterior descending artery (LAD). In this case, it is a Type<br />
in Lead aVL? That’s because you need advanced level skills to see it.<br />
There is another issue with occlusions of a Type 3 (“wraparound”)<br />
a Type 3 LAD. It is by far the most common type of LAD and, when LAD: the ischemia causing the ST elevation in Leads I and aVL can<br />
occluded, can result in very complex, difficult-to-see acute ischemias – at times – perfectly cancel the ST elevation in Leads II, III and aVF!<br />
Advanced Level<br />
This will leave you with signs of acute ischemia only in the precordial<br />
leads. Now, the ischemic changes in the precordial leads of this ECG<br />
So, can we tell where the level of the infarction is located? We can are extremely impressive – but in other ECGs they may not be. In fact,<br />
definitely You should say that it have is proximal noted to the that, first diagonal although branch there (D1) is ST the precordial elevation leads in may the show inferior nothing more leads, than hyperacute Lead III T waves has<br />
because of the ST elevation that involves Leads V2 to V5, and the which could be missed by someone not as astute and skilled as you.<br />
much less STE than Leads II and aVF. You also should have noted that there is ST elevation<br />
ST elevation in Lead I (and presumably, Lead aVL). We used to think So, a proximal occlusion of a Type 3 (“wraparound”) LAD may appear<br />
that in Lead if ST elevation I which were present should in Lead be V1, accompanied then the occlusion was by STE like in a Lead minor, distal aVL occlusion – but when there – in doesn’t fact – it is quite appear large! to be<br />
automatically any in that proximal lead. to the So first we septal have perforator two branch unexpected, (S1). While unexplained findings: less STE in Lead III than<br />
that is often, if not usually the case, it still doesn’t represent 100% And remember: most people have a Type 3 (“wraparound”) LAD.<br />
in Leads II and aVF and essentially no STE in Lead aVL while ST elevation is present in Lead<br />
assurance of a proximal location. We normally confirm an occlusion Exactly the kind of comforting thought that keeps you on your toes,<br />
proximal I. Could to S1 there by presence be a connection? of ST depression in the Yes! inferior And leads, that isn’t connection it? The next time is you the see fact a patient that with Leads ACS type III chest and pain aVL –<br />
but we don’t have that opportunity here because of the acute ischemia but the ECG appears normal – remember this!<br />
are reciprocal to each other. Both have ST elevation but their systolic currents of injury are<br />
traveling in opposite directions (Lead III: down and to the right, Lead aVL: up and to the left)<br />
and thus cancel each other. For further Apparently, recruitment vacancies the ST visit: elevation www.ambulanceukonline.com<br />
Lead III was greater than in Lead<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
9
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
Air ambulance<br />
charity and property<br />
developers join<br />
forces to save lives<br />
Great Western Air <strong>Ambulance</strong><br />
Charity (GWAAC) has joined<br />
hands with YTL Developments<br />
to make Brabazon the first<br />
heart-safe community in the<br />
South West.<br />
Brabazon is the new<br />
neighbourhood for Bristol that is<br />
being built on the historic former<br />
Filton Airfield, where GWAAC<br />
used to have its Emergency<br />
Air Base.<br />
The partnership is a<br />
groundbreaking commitment to<br />
community health and safety.<br />
YTL Developments will pay for<br />
and install defibrillators around<br />
the neighbourhood through<br />
GWAAC’s Great Western Hearts<br />
defibrillator programme. The<br />
lifesaving devices will be placed in<br />
strategic locations at 300-metre<br />
intervals across Brabazon. The<br />
aim is for residents of Brabazon<br />
to have an accessible defibrillator<br />
within a three-minute-return walk,<br />
helping to increase the chance<br />
of survival for someone suffering<br />
a cardiac arrest nearby by up<br />
to 70%.<br />
In addition, YTL Developments<br />
will also donate £100 for every<br />
house sold in the remainder of<br />
the first phase and the entirety of<br />
the second phase of new homes<br />
at Brabazon.<br />
Anna Perry, Chief Executive of<br />
GWAAC, says: “Our team of<br />
Paramedics and Consultant<br />
Doctors treat the most serious<br />
trauma and medical emergencies<br />
across the region. But we can't<br />
do this by ourselves. As a charity,<br />
we can only remain ready to<br />
respond thanks to the generosity<br />
of community and business<br />
partnerships like this with YTL<br />
Developments.<br />
“Through this partnership, the<br />
neighbourhood will benefit from<br />
a defibrillator within 300m of<br />
every house. Every resident<br />
will be given the opportunity to<br />
learn how to use these devices,<br />
alongside CPR. With this support<br />
in place, we could see survival<br />
rates for anyone suffering an outof-hospital<br />
cardiac arrest jump<br />
from less than 10% to nearly 70%.<br />
“Not only this, but the donations<br />
GWAAC receive for every house<br />
sale will support everyone across<br />
Bristol if they ever suffer medical<br />
emergency. The funds will help<br />
ensure our ‘flying hospital’ can<br />
come to those who need it most.<br />
YTL Developments are helping to<br />
give people the best chance on<br />
their worst day. “<br />
GWAAC is one of three major<br />
charity partners with YTL<br />
Developments<br />
As Brabazon is one of the largest<br />
construction projects in the South<br />
West, YTL Developments has<br />
also forged a partnership with:<br />
• Lighthouse Construction<br />
Industry Charity, to help<br />
support mental health within<br />
the industry<br />
• Southern Brooks, a charity<br />
providing community<br />
development opportunities and<br />
health and wellbeing services<br />
that support individuals and<br />
communities<br />
“We’re committed to building<br />
thriving communities that work<br />
not only for today but for many<br />
generations to come. Our three<br />
charity partnerships are designed<br />
to form a comprehensive strategy<br />
that supports the mental health,<br />
physical safety and social<br />
wellbeing of our staff, our supply<br />
chain, residents and neighbours.<br />
Our partnership with the Great<br />
Western Air <strong>Ambulance</strong> Charity<br />
will be a <strong>UK</strong> first in providing<br />
a heart-safe community. With<br />
the support of the Lighthouse<br />
Club, we are seeking to tackle<br />
the scourge of poor mental<br />
health. And our partnership<br />
with Southern Brooks is already<br />
supporting new residents<br />
both at Brabazon and across<br />
North Bristol.<br />
"These three charity partnerships<br />
epitomise our Vision for<br />
Brabazon. We want to live up to<br />
the legacy of the community that<br />
built Concorde, stewarding this<br />
historic landmark and create an<br />
inclusive new community that<br />
will drive local prosperity for the<br />
next century.”<br />
Jon McDiarmid, Sales Director at<br />
YTL Developments<br />
London’s Air<br />
<strong>Ambulance</strong> Charity<br />
announces most<br />
successful gala in<br />
its history, raising<br />
£1.2 million.<br />
London’s Air <strong>Ambulance</strong><br />
Charity hosted its largest ever<br />
single fundraising event on<br />
7 February raising a record<br />
£1.2 million at its gala at<br />
Raffles London.<br />
The charity is called to London’s<br />
most severe trauma cases,<br />
delivering life-saving emergency<br />
medical care at the roadside and<br />
conducting procedures usually<br />
only seen in a hospital.<br />
The money raised will go directly<br />
to support the charity’s ongoing<br />
appeal, “Up Against Time”. The<br />
campaign, the largest in the<br />
charity’s 35 year history, aims to<br />
raise £15 million to fund two new<br />
helicopters by Autumn <strong>2024</strong>.<br />
Support has never been more<br />
needed. Despite the sum raised<br />
at the gala, the charity still needs<br />
to raise more than £5 million,<br />
with just eight months left of<br />
the appeal.<br />
The gala was attended by the<br />
charity’s royal Patron, His Royal<br />
Highness The Prince of Wales.<br />
The Prince met with doctors,<br />
pilots and paramedics from the<br />
service, speaking to the team<br />
about their life-saving work. As<br />
a former air ambulance pilot<br />
himself, His Royal Highness has<br />
seen the difference advanced<br />
trauma teams can make when<br />
time is short.<br />
The Prince also met Milana, an<br />
inspirational patient whose life<br />
was saved by the London’s Air<br />
<strong>Ambulance</strong> team in January<br />
2022. Later in the evening, Milana<br />
gave a powerful speech to the<br />
assembled guests, sharing her<br />
experience and talking movingly<br />
about her rehabilitation - for more<br />
information on Milana’s story<br />
see below.<br />
The event, held at Raffles London<br />
at The OWO, was hosted by Tania<br />
Bryer and Mark-Francis Vandelli<br />
and attended by a number of<br />
VIP guests, including Top Gun<br />
star Tom Cruise and Arsenal<br />
manager Mikel Arteta and saw<br />
entertainment from disco legends<br />
Sister Sledge.<br />
During a speech at the Gala<br />
Dinner, His Royal Highness<br />
The Prince of Wales said:<br />
“We gather tonight to help<br />
as many people as possible<br />
benefit from top class care in<br />
the silhouette of London’s Air<br />
<strong>Ambulance</strong>’s flying lifelines.<br />
As a former pilot for East Anglia<br />
Air <strong>Ambulance</strong>, I know just how<br />
vital the work of air ambulance<br />
teams across the country<br />
is, and the truly life-saving<br />
difference it can make to deliver<br />
urgent medical care wherever<br />
injury strikes.<br />
Here in London, the current<br />
aircraft have served magnificently.<br />
But our capital city needs a new<br />
fleet. And we are Up Against<br />
Time. The clue really is in the<br />
Appeal’s name. By September,<br />
we need the two new red birds -<br />
decked with the latest kit such as<br />
night vision - in our skies.<br />
You wouldn’t be here if you<br />
needed much persuading, I<br />
know. But just wait to hear<br />
Milana’s story later of how the<br />
Air <strong>Ambulance</strong>, and its incredible<br />
teams, have given her a second<br />
chance at life.<br />
Anyway, an enormous thank you<br />
to all for being here tonight and<br />
for supporting such a wonderful<br />
cause. You are all, each and<br />
every one of you, lifesavers.”<br />
Jonathan Jenkins, CEO of<br />
London’s Air <strong>Ambulance</strong><br />
Charity said;<br />
“Every day London’s Air<br />
<strong>Ambulance</strong> is up against time<br />
to save lives in London. Our<br />
helicopters get to the scene<br />
within 11 minutes to deliver<br />
lifesaving care. But it has become<br />
increasingly difficult to operate<br />
them. We have a discontinued<br />
model and there is a lack of spare<br />
parts available worldwide.<br />
We cannot operate an emergency<br />
service if we need to wait for<br />
months to replace a part. When a<br />
life is on a line, we simply cannot<br />
afford to lose time.<br />
That is why the support at this<br />
evening’s event will help save<br />
lives in London; by raising this<br />
money we move closer to our<br />
fundraising target of £15million so<br />
we can replace our helicopters.<br />
We are honoured to have the<br />
support of HRH The Prince of<br />
Wales and have him attend the<br />
Gala tonight. We would like to<br />
thank our Patron, and those<br />
who made the evening possible,<br />
including our Philanthropy Board<br />
and sponsors Chopard, Hinduja<br />
Foundation, Corsair, Akademy<br />
Club and Viaro Energy. Their<br />
belief in our cause means we can<br />
continue to be there for everyone<br />
in London, whenever they<br />
need us.”<br />
London’s Air <strong>Ambulance</strong> delivers<br />
an advanced trauma team, made<br />
up of a doctor and paramedic,<br />
to bring the hospital to the scene<br />
via helicopter or rapid response<br />
car when time is of the essence.<br />
The expert teams can reach<br />
anywhere in London in under<br />
11 minutes.<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
10<br />
11<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
Primarily funded by charitable<br />
donations, the service is also<br />
run in partnership with Barts<br />
Health NHS Trust and the<br />
London <strong>Ambulance</strong> Service<br />
NHS Trust. Barts Health NHS<br />
Trust provides the doctors, some<br />
financial support and the helipad<br />
facilities at The Royal London<br />
Hospital. The London <strong>Ambulance</strong><br />
Service NHS Trust provides the<br />
paramedics and the emergency<br />
infrastructure to dispatch the<br />
service 24 hours a day.<br />
Milana’s story<br />
On 17 January 2022, Milana – a<br />
mother of two – accidentally fell<br />
from a great height in London.<br />
Her life took a turn that no one<br />
could prepare for.<br />
London’s Air <strong>Ambulance</strong> was<br />
dispatched and arrived at her<br />
side within minutes, the first on<br />
scene. Our advanced trauma<br />
team found Milana barely<br />
alive. She was critically injured,<br />
extremely pale, breathing very<br />
quickly with only palpable central<br />
pulses, cold and in a lot of pain.<br />
She also had no recordable blood<br />
pressure and her heart rate was<br />
over twice the normal rate.<br />
The crew sited intravenous<br />
access to administer strong<br />
painkillers. They suspected<br />
Milana was severely bleeding<br />
internally in her abdomen and<br />
from a life-threatening pelvic<br />
fracture. She had broken her<br />
ribs on her left side, puncturing<br />
her lung, and had broken her left<br />
ankle to such an extent it was<br />
stopping the blood supply to<br />
her foot. The team also noticed<br />
that Milana was not moving her<br />
lower limbs at all. They suspected<br />
she had unfortunately suffered a<br />
spinal cord injury.<br />
Once off the ground onto a<br />
trolley bed, having had a pelvic<br />
splint applied, Milana received a<br />
blood transfusion – something<br />
only London’s Air <strong>Ambulance</strong>’s<br />
team can administer on scene<br />
in London. The team also<br />
administered a roadside general<br />
anaesthetic to take over her<br />
breathing and performed a<br />
surgical procedure to the left<br />
side of her chest to re-inflate<br />
her punctured lung. Both these<br />
procedures ensured Milana could<br />
get maximum oxygen to her vital<br />
organs, especially her brain.<br />
The team then rang the nearest<br />
major trauma centre and<br />
declared a code red. A code<br />
red is an early warning to the<br />
receiving hospital team, to<br />
prepare them for a patient who is<br />
severely injured and has got lifethreatening<br />
bleeding. On the way<br />
to hospital the crew performed<br />
an ultrasound scan of Milana’s<br />
abdomen which confirmed their<br />
suspicion of internal bleeding.<br />
The team accompanied Milana to<br />
hospital, where they handed her<br />
over to an awaiting trauma team.<br />
“When I woke up from my coma,<br />
I thought I was in a nightmare.<br />
Doctors were telling me what had<br />
happened, but I didn’t believe<br />
it was real,” said Milana. “I was<br />
waiting for someone to pinch me<br />
to wake me up properly so I could<br />
return to my normal life.”<br />
For the following 10 months,<br />
Milana remained in hospital. Her<br />
spinal cord injury had resulted<br />
in paralysation from her waist<br />
down. “For the first three months<br />
I struggled to accept this new<br />
reality. But when I realised it was<br />
real, I said to myself I have to<br />
work out how to do this.<br />
“First I have to heal physically and<br />
then find my way out of hospital<br />
and back home. I have to return<br />
home to my boys.”<br />
Through 12 surgeries and months<br />
of intensive rehabilitation, Milana<br />
worked tirelessly on her recovery<br />
with dedication and tenacity.<br />
“I had to find a new way of living.<br />
I had to learn how to do the<br />
daily things you don’t even think<br />
about in a wheelchair, like getting<br />
dressed and getting onto a bed.<br />
But I wanted to do it for my<br />
children, I wanted to be at home<br />
with them for Christmas. They<br />
were my driving force.<br />
“An inspiring woman said to me<br />
that it is not the accident that<br />
happens to you that defines<br />
you, but how you respond to<br />
the challenges.”<br />
Surrounded by unconditional love<br />
and fuelled by determination to<br />
overcome the challenges ahead<br />
of her, Milana progressed through<br />
rehab and returned home to her<br />
family, where she lives today.<br />
“I vividly remember my first breath<br />
of fresh air after removing my<br />
respiratory breathing tube and<br />
seeing my first sunrise since the<br />
accident – so many shades of<br />
pink, orange and blue. We can<br />
get caught up in life sometimes,<br />
but I was reminded never to take<br />
anything for granted.<br />
“Something really dreadful<br />
happened that day, but at the<br />
same time, a miracle happened<br />
and from that point onwards so<br />
many stars aligned to help me<br />
survive. London’s Air <strong>Ambulance</strong><br />
being first on the spot and<br />
then the NHS for the following<br />
months. I am grateful for every<br />
day, minute and second. Being<br />
alive is a privilege and I am<br />
so thankful to all the medical<br />
teams that have given me the<br />
opportunity to be here. The<br />
courage and professionalism of<br />
London’s Air <strong>Ambulance</strong>’s crew<br />
was incredible.”<br />
After a year of being back at<br />
home, living her life with her<br />
children and husband, Milana is<br />
full of thanks for everyone who<br />
has been a part of her journey.<br />
“Two things made this impossible<br />
journey possible for me. The<br />
immense love I received from<br />
my husband, my children, my<br />
parents, brother, sister and<br />
friends. And of course all the<br />
doctors and nurses that attended<br />
to me. London’s Air <strong>Ambulance</strong>:<br />
the first to arrive and help me.<br />
Those first minutes were the most<br />
crucial. The charity made my<br />
recovery possible.”<br />
Milana was already aware of<br />
London’s Air <strong>Ambulance</strong> Charity<br />
before her accident – she had<br />
attended one of our events in<br />
2019 and subsequently joined the<br />
charity’s gala committee.<br />
“I was taken aback by the charity<br />
when I first heard about it. It’s an<br />
inspirational service – you really<br />
do save lives.”<br />
She played an instrumental role in<br />
organising the 2022 gala – which<br />
went on to raise over £1 million on<br />
the night – but hadn’t been able<br />
to attend as was still in hospital<br />
at the time. Instead, she followed<br />
the evening through a video call<br />
from her hospital bed!<br />
“I am best placed to say that this<br />
really can happen to anyone. I<br />
wouldn’t wish it to happen to<br />
anybody ever. But if it does, we<br />
need to make sure London’s Air<br />
<strong>Ambulance</strong> can be there to save<br />
their life too.”<br />
In February <strong>2024</strong>, just two years<br />
after her accident, Milana spoke<br />
at our <strong>2024</strong> gala, bravely sharing<br />
her journey with the guests.<br />
“Speaking at the gala is part of<br />
my journey, another milestone<br />
for me,” she beamed. “This is an<br />
opportunity to say thank you to<br />
everyone who supported me.<br />
“Something tragic happened to<br />
me. But from that point onwards,<br />
so much good happened and I<br />
am so thankful to London’s Air<br />
<strong>Ambulance</strong> Charity for that.<br />
“There is no rewind button in life,<br />
so we have to look forward and<br />
that is what I’m doing. Together,<br />
tonight, we can make sure that<br />
London’s Air <strong>Ambulance</strong> Charity<br />
is able to give another person<br />
that chance.”<br />
Royal Engineers from<br />
Kinloss Barracks join<br />
forces with HELP<br />
Appeal helipad charity<br />
for first time to bring<br />
lifesaving helipad to<br />
Isle of Gigha.<br />
Once completed the HELP<br />
Appeal and 39 Engineer<br />
Regiment could construct<br />
more helipads in Scotland to<br />
speed up remote communities’<br />
access to hospitals in medical<br />
emergencies.<br />
For the first time, the Corps of<br />
Royal Engineers, and the HELP<br />
(Helicopter Emergency Landing<br />
Pads) Appeal, the only helipad<br />
charity in the country, will be<br />
working together to build a<br />
much-needed emergency helipad<br />
on the community owned Isle<br />
of Gigha.<br />
Gigha is located on the most<br />
southerly Hebridean Islands,<br />
three miles west of the Kintyre<br />
peninsula and around a threehour<br />
drive from Glasgow followed<br />
by a 20-minute sailing on a<br />
ferry. Whilst there is a regular<br />
ferry service, Gigha is still a<br />
remote and rural community,<br />
and its inaccessibility can be<br />
problematic particularly during a<br />
medical emergency. By having<br />
Rendering Controlled Drugs Irretrievable for Use<br />
SaferDenature Controlled Drug denaturing kits will render unused, waste or expired medicines<br />
irretrievable prior to disposal via pharmaceutical waste streams in line with current legislation * .<br />
Simple, easy-to-use, instructions on every kit<br />
Small 250ml kit for convenient use in the field<br />
Suitable for use with tablets, capsules, liquids,<br />
aerosols or patches<br />
The water soluble sachet contains the<br />
formula granules to guard against accidental<br />
spillage and user contamination<br />
Larger kit volumes available for expired<br />
stock clearance<br />
a permanent, purpose-built<br />
helipad at Gigha Airfield, the<br />
Scottish Air <strong>Ambulance</strong> and<br />
larger coastguard helicopters can<br />
land and take off at any time on<br />
the island, transporting critically ill<br />
patients to the most appropriate<br />
major trauma centre or A&E<br />
hospital on the mainland.<br />
Jane Millar, from The Isle of Gigha<br />
Heritage Trust, approached the<br />
HELP Appeal for support. By a<br />
happy co-incidence the charity<br />
had also been contacted by 39<br />
Engineer Regiment in Kinloss,<br />
Scotland, asking if there was<br />
a helipad project it could be<br />
involved with to gain exercise<br />
experience of building emergency<br />
platforms. 39 Engr Regiment<br />
are the MOD’s high readiness<br />
air support Engineer force and<br />
the regiment strive to improve<br />
its understanding of helicopter<br />
infrastructure so it can react<br />
without delay to the needs of<br />
defence across the world.<br />
Purchase at NHS supply chain:<br />
my.supplychain.nhs.uk/catalogue or www.alphalabs.co.uk/safer-denature<br />
Phone: 023 8048 3000 • www.alphalabs.co.uk<br />
In 2002, the Gigha islanders<br />
managed to purchase the<br />
island for £4 million under the<br />
Community Right to Buy scheme.<br />
They now own it through the<br />
Isle of Gigha Heritage Trust,<br />
which has teamed up with the<br />
HELP Appeal and 39 Engineer<br />
Regiment to coordinate the<br />
project. Currently the island<br />
operates on a “landing strip” of<br />
grass, which is a highly unsuitable<br />
surface for its volunteer<br />
ambulance service when<br />
escorting patients to a helicopter.<br />
It can become waterlogged and<br />
muddy delaying their transfer to<br />
lifesaving treatment at a hospital<br />
on the mainland.<br />
Robert Bertram, the HELP<br />
Appeal’s Chief Executive has<br />
agreed to fund the cost of the<br />
project - £150,000 - and 39<br />
Engineer Regiment in conjunction<br />
with local contractors, will<br />
build the helipad. It will be<br />
operational by <strong>April</strong> <strong>2024</strong>. Once<br />
*The misuse of Drugs<br />
Regulations 2001<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
12<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
01 Safer Denature - <strong>Ambulance</strong> <strong>UK</strong> - Jan <strong>2024</strong>.indd 1 10/01/<strong>2024</strong> 14:27:14<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
13
NEWSLINE<br />
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
completed the HELP Appeal<br />
and 39 Engineer Regiment<br />
could construct more helipads<br />
in Scotland to speed up remote<br />
communities’ access to hospitals<br />
in medical emergencies. The<br />
HELP Appeal is also dedicated<br />
to partnering with other Royal<br />
Engineer regiments, to make<br />
helipads a reality on islands<br />
across England and Wales.<br />
Robert Bertram, Chief Executive<br />
of the HELP Appeal says: “Gigha<br />
needs this helipad now as there<br />
is only one surgery on the Island<br />
with no Doctor, so thanks to our<br />
supporters, funding is available<br />
immediately and with the Royal<br />
Engineers on board I’ve no<br />
doubt that construction will be<br />
as efficient as possible ensuring<br />
it opens this Spring. Once built,<br />
the community will never have to<br />
fear that ground conditions will<br />
let them down again and they<br />
can be sure of a swift transfer off<br />
the island to hospital whenever<br />
they need it. I’m excited that this<br />
unique partnership will provide<br />
lifesaving access to hospital in<br />
an emergency.”<br />
Captain Paddy Bryden of<br />
39 Engr Regt says: “53 Field<br />
Squadron, is part of 39 Engineer<br />
Regiment, and we are delighted<br />
to be involved with this project.<br />
Our role in supporting military<br />
helicopters has many similarities<br />
to the construction of civilian<br />
helicopter infrastructure, and<br />
this opportunity offers valuable<br />
training for our specialist<br />
tradespeople. As a Regiment<br />
we are grateful to be afforded<br />
the opportunity to give back<br />
to our rural areas and having<br />
been born and raised in the<br />
Highlands myself, I recognise the<br />
disproportionally positive impact<br />
improved infrastructure can have<br />
on communities such as Gigha.<br />
We hope there might be future<br />
training opportunities for the Regt<br />
to work with the HELP Appeal<br />
team when our schedule allows.”<br />
Jane Millar, Business<br />
Development Manager of the<br />
Isle of Gigha Heritage Trust says:<br />
“We are completely amazed by<br />
this opportunity with the HELP<br />
Appeal and Royal Engineers. The<br />
issues with the existing airfield<br />
have been raised for years, but<br />
there never seemed to be a viable<br />
solution for the community Trust<br />
to take forward. We know how<br />
difficult the current situation has<br />
been for our local emergency<br />
services, so this project will<br />
hugely support their work, and<br />
ensure safe access to hospital for<br />
our community. To receive this<br />
level of support from the HELP<br />
Appeal and the Royal Engineers<br />
has been incredible.”<br />
Gigha resident, Maurice Forster,<br />
53, agrees after he was airlifted<br />
to the HELP Appeal funded<br />
Queen Elizabeth University<br />
Hospital helipad in Glasgow<br />
in December 2023 following a<br />
medical emergency. Maurice<br />
was taken to intensive care<br />
immediately after landing. He<br />
says, “The emergency services<br />
were amazing, as was the<br />
coordinator between them all.<br />
Within 20 minutes, I had arrived in<br />
Glasgow. The Air <strong>Ambulance</strong> is a<br />
crucial service, and a permanent<br />
landing pad in Gigha will make<br />
it even more seamless for<br />
our community.”<br />
The HELP Appeal has funded<br />
or is funding 15 helipads in<br />
Scotland, including at the Queen<br />
Elizabeth University Hospital in<br />
Glasgow, Raigmore Hospital<br />
in Inverness, Edinburgh Royal<br />
Infirmary and Campbeltown<br />
Hospital. The charity has also<br />
donated £200,000 towards<br />
portable landing lights for<br />
Scotland’s Air <strong>Ambulance</strong> Service<br />
for 20 island locations across<br />
Scotland. It has funded 45<br />
helipads across the <strong>UK</strong>, which<br />
have seen over 27,000 landings.<br />
Midlands Air<br />
<strong>Ambulance</strong> Charity<br />
Hosts European<br />
Trauma Course<br />
Twenty-four doctors and<br />
advanced clinical practitioners<br />
from across the country<br />
travelled to Midlands Air<br />
<strong>Ambulance</strong> Charity’s new<br />
airbase and headquarters,<br />
to join 15 faculties from<br />
across <strong>UK</strong> & Ireland at the<br />
European Trauma Course (ETC)<br />
in September.<br />
The three-day course, at the<br />
charity’s new facility on the<br />
Shropshire / Staffordshire border,<br />
brought together clinicians from<br />
key hospital specialties involved<br />
in the immediate stabilisation of<br />
major trauma patients on arrival<br />
in hospital, focusing on technical<br />
and non-technical skills required<br />
to optimise patient care. Running<br />
for over ten years, the course<br />
covers key aspects of trauma<br />
management, such as advanced<br />
airway management, head injury,<br />
paediatric injury, spinal injury<br />
and more.<br />
Hosted in Midlands Air<br />
<strong>Ambulance</strong> Charity’s new<br />
clinical training suite, the course<br />
included scenario workshops,<br />
each focusing on specific areas<br />
of trauma, growing in complexity<br />
to meet patient needs as the<br />
course progressed. In addition,<br />
the charity’s immersive simulation<br />
suite, supported by The Kildare<br />
Trust, was utilised throughout<br />
the training, using the charity’s<br />
facilities and equipment that is<br />
some of the best available in<br />
the industry.<br />
Adam Low, pre-hospital<br />
emergency medicine doctor at<br />
Midlands Air <strong>Ambulance</strong> Charity<br />
and Medical Director for this<br />
European Trauma Course, said:<br />
“The ETC provides a valuable<br />
team-based approach to<br />
immediate trauma management,<br />
providing an environment to<br />
learn technical and non-technical<br />
skills that are integral to real life<br />
situations. It was a privilege to<br />
be able to host the course-at our<br />
state-of-the-art clinical training<br />
suite, inviting fellow advanced<br />
clinical practitioners for training<br />
to support the wider quality of<br />
trauma care nationally.”<br />
After receiving a positive response<br />
from the group of delegates that<br />
attended, the charity is hoping to<br />
host another European Trauma<br />
Course in spring <strong>2024</strong>.<br />
Learn more about the<br />
European Trauma Course at<br />
europeantraumacourse.com<br />
To make an inquiry about booking<br />
a bespoke training course at<br />
Midlands Air <strong>Ambulance</strong> Charity,<br />
please contact education@<br />
midlandsairambulance.com.<br />
Learn more about the charity by<br />
visiting midlandsairambulance.<br />
com or by following the charity on<br />
social media.<br />
EEAST team first in<br />
country to win global<br />
quality certification<br />
A team at the East of England<br />
<strong>Ambulance</strong> Service NHS<br />
Trust (EEAST) has won an<br />
international quality standard.<br />
EEAST has a dedicated team<br />
that maintains the Trust’s medical<br />
devices. Medical devices are<br />
lifesaving essentials such as:<br />
• defibrillators,<br />
• ventilators,<br />
• patient monitoring,<br />
• and oxygen equipment.<br />
The certification process provides<br />
an enhanced level of assurance<br />
to patients, staff and volunteers.<br />
It includes an audit of the quality<br />
and documentation systems for<br />
the whole lifecycle of the Trust’s<br />
medical devices - from purchase,<br />
deployment, servicing and<br />
ultimately disposal.<br />
EEAST is the first ambulance<br />
service in the <strong>UK</strong> to receive<br />
the global ISO 13485:2016<br />
accreditation for medical devices.<br />
Katie Birkenhead, Head of<br />
Medical Devices said:<br />
“This certification is a fantastic<br />
achievement for the team,<br />
they have all worked incredibly<br />
hard and it is a credit to their<br />
commitment.<br />
“ISO accreditation has been<br />
an ambition of mine for many<br />
years, and I’m proud that we’ve<br />
successfully delivered our goal.”<br />
Picture: Andrew Macdonald –<br />
Clinical Engineering Manager;<br />
Matt Kent – Clinical Engineering<br />
Technician; Charlotte Ennew<br />
– Medical Devices Assurance<br />
Manager; Neil Hogg – Clinical<br />
Engineering Technician and<br />
Paige Hogg – Clinical Engineering<br />
Support with their ISO<br />
certification.<br />
Falls partnership for<br />
<strong>Ambulance</strong> Service<br />
and Cambridgeshire<br />
Fire and Rescue<br />
Service<br />
People who have fallen in<br />
their homes will benefit from<br />
a new partnership between<br />
Cambridgeshire Fire and<br />
Rescue Service and East of<br />
England <strong>Ambulance</strong> Service<br />
NHS Trust.<br />
The partnership is a 12-month<br />
pilot which will see four<br />
Community Wellbeing Officers<br />
work across Cambridgeshire<br />
responding to calls from people<br />
who have fallen.<br />
The Community Wellbeing<br />
Officers completed a three-week<br />
emergency responder training<br />
with EEAST to learn the skills<br />
required for their role.<br />
Falls can account for up to 20%<br />
of the ambulance service’s calls<br />
and although some patients will<br />
require hospital treatment, many<br />
simply need to be helped to their<br />
feet and checked over to make<br />
sure they are safe to be left at<br />
home. Currently, if a person falls<br />
at home and has no injuries, they<br />
could have a long wait for an<br />
ambulance to become available.<br />
The new partnership aims to free<br />
up ambulance crews to attend<br />
the most seriously ill people in<br />
Cambridgeshire and this new<br />
programme aims to send a<br />
Community Wellbeing Officer<br />
within an hour of the call.<br />
Cambridgeshire Fire Service<br />
Station Commander Scott<br />
Fretwell, Community Risk<br />
Manager said: “We are excited<br />
to be working in partnership<br />
with East of England <strong>Ambulance</strong><br />
Service Trust to introduce<br />
community wellbeing officers.<br />
“The collaboration will help to<br />
save lives, enhance patient<br />
experience and subsequently<br />
improve community welfare.<br />
When they are not responding to<br />
calls, the community wellbeing<br />
officers will be visiting homes of<br />
the most vulnerable people in our<br />
communities to help them stay<br />
safe from fire and other risks such<br />
as slips and falls.<br />
“We are looking forward to<br />
seeing the positive impact of<br />
this new partnership over the<br />
coming months.”<br />
Tom Barker, EEAST Community<br />
Response Manager said:<br />
“We’re delighted to be part<br />
of this collaboration with<br />
Cambridgeshire Fire and Rescue<br />
Service which aims to improve<br />
the speed of response and<br />
increase support for people who<br />
have fallen in their homes.<br />
“The people we’ll be responding<br />
to are the vulnerable members of<br />
our communities who will not only<br />
benefit from a quicker response<br />
to help them back on their feet,<br />
but also the person-centred<br />
home safety check that will be<br />
carried out at the same time.<br />
“I am confident that this<br />
programme will see real benefits,<br />
for not only for the ambulance<br />
service, but more importantly to<br />
our vulnerable members of our<br />
community who we want to make<br />
sure are safe in their homes.”<br />
How the scheme will work<br />
When a call is received by EEAST<br />
via 999 or 111 to a person who<br />
has fallen it will be clinically<br />
assessed by the EEAST control<br />
room. If the patient doesn’t have<br />
any injuries, it will be assigned<br />
to the Community Wellbeing<br />
Officers. The officers, who will<br />
be working in pairs, will then be<br />
dispatched to the address to<br />
safely get the patient off the floor.<br />
The officers will then discuss the<br />
patient’s condition with a clinician<br />
in the EEAST control room to<br />
ensure the patient can be safely<br />
left at home.<br />
Once the officers have assisted<br />
the patient, they will also carry<br />
out a tailored home safety check<br />
to ensure their smoke alarms<br />
are working and will also help to<br />
reduce risk of fire or further falls<br />
(loose rug, old slippers, steps<br />
without hand rails).<br />
The aim of the partnership is to<br />
allow paramedics to be available<br />
for serious medical emergencies,<br />
while making vulnerable residents<br />
safer in their homes.<br />
Photo caption: Joshua Berrisford,<br />
Tom Barker, Jo Fletcher, Scott<br />
Fretwell and Megan Cantwell<br />
Successful jockey<br />
finds “second<br />
calling” with the<br />
ambulance service<br />
A former professional jockey<br />
who rode for Her Late Majesty<br />
Queen Elizabeth II and football<br />
legend Sir Alex Ferguson has<br />
found his “second calling” with<br />
the East of England <strong>Ambulance</strong><br />
Service (EEAST).<br />
Thomas Brown, 31, rode 123<br />
winners as a jockey with his<br />
biggest success coming in 2016<br />
on a horse called Educate in<br />
the prestigious John Smith’s<br />
Cup at York – the feature race<br />
on a raceday which attracted<br />
over 35,000 people and was<br />
broadcast live on Channel 4.<br />
One of Thomas’ other winners<br />
was for Sir Alex Ferguson at<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
14<br />
15<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
Ascot and he also achieved a<br />
third place aboard a horse in<br />
the royal silks when he was an<br />
apprentice jockey.<br />
But injuries saw Thomas give up<br />
his jockey’s licence in 2017 and<br />
a knee injury in a football match<br />
in 2022 left him unable to ride<br />
horses for three months.<br />
During his rehabilitation he<br />
considered a career outside of<br />
horse racing and consulted with<br />
a career adviser at JETS – the<br />
Jockeys Education and Training<br />
Scheme. They identified a career<br />
with the ambulance service to<br />
help fulfil Thomas’ desire to be<br />
outside meeting new people<br />
every day and providing a similar<br />
adrenaline rush to being a jockey.<br />
JETS arranged for Thomas<br />
to meet EEAST paramedics<br />
providing medical cover at<br />
a raceday at Newmarket so<br />
he could find out more about<br />
working for the ambulance<br />
service.<br />
They told Thomas he could<br />
retrain to work for the ambulance<br />
service without a university<br />
degree, as internal career<br />
pathways within EEAST would<br />
allow him to progress from<br />
an entry level position as an<br />
emergency care assistant to<br />
become a paramedic.<br />
Thomas successfully applied<br />
to become an emergency<br />
care assistant working in the<br />
Bury St Edmunds area and<br />
started in March 2023. He was<br />
on the road in an ambulance<br />
working alongside a qualified<br />
paramedic after six weeks of<br />
intensive training.<br />
Celebrating his year anniversary<br />
at EEAST, Thomas says he<br />
looks forward to every shift and<br />
his ambition is to become an<br />
emergency medical technician<br />
and then a paramedic.<br />
He said:<br />
“I feel incredibly proud to wear<br />
the green uniform and work for<br />
the ambulance service.<br />
“I had some great days as a<br />
jockey, but it feels like I have<br />
found my second calling at<br />
EEAST and I’m loving every<br />
minute of it.<br />
Successful jockey finds<br />
“second calling” with the<br />
ambulance service<br />
“To see the difference you make<br />
to patients is incredible. It’s a<br />
good feeling when you see the<br />
relief on a patient’s face when<br />
you arrive on scene and it’s even<br />
better when you make them<br />
more comfortable.<br />
“Becoming a paramedic is the<br />
eventual goal but I’m taking<br />
things one step at a time and<br />
enjoying learning new skills from<br />
supportive colleagues who want<br />
you to do well.<br />
“Working in the ambulance<br />
service has matured me a lot and<br />
given me a wider perspective<br />
on life.”<br />
Jemma Varela, head of clinical<br />
operations in Suffolk and North<br />
East Essex, said:<br />
“Thomas is an excellent example<br />
of someone starting in the<br />
ambulance service later in life<br />
and seeing a career pathway to<br />
progress and do well at EEAST.<br />
“Working for the ambulance<br />
service is incredibly rewarding<br />
and it’s great that Thomas loves<br />
his job and feels he has found his<br />
second calling.”<br />
Thomas is sharing his story of<br />
how he joined EEAST at the start<br />
of National Careers Week. He will<br />
be taking part in a Q&A session<br />
on EEAST’s Instagram account<br />
on Thursday 7th March from<br />
12pm to 2pm alongside a fellow<br />
emergency care assistant.<br />
He also speaks at seminars to<br />
young apprentice jockeys about<br />
his riding career and his second<br />
career with the ambulance<br />
service, discussing the skills he<br />
was able to transfer from horse<br />
racing to the ambulance service.<br />
He said: “JETS has given me<br />
so much help in supporting me<br />
into a career that I love, so it’s<br />
important I give something back<br />
to them by sharing my experience<br />
and what I have learned from it.<br />
“When I was starting out in<br />
racing aged 16, I never thought<br />
of anything other than being a<br />
jockey. I now encourage people<br />
to think about your options if<br />
a career as a jockey doesn’t<br />
work out.”<br />
Pilot programme<br />
gives volunteers<br />
a pathway to join<br />
East of England<br />
<strong>Ambulance</strong> Service<br />
A new programme run by the<br />
East of England <strong>Ambulance</strong><br />
Service provides a direct route<br />
for volunteers to start a career<br />
with the ambulance service.<br />
The ‘Volunteer to Career’<br />
programme provides training for<br />
people to get the skills needed to<br />
begin full time roles at EEAST.<br />
And the course now has its<br />
first success stories, with<br />
graduates Grant Harvey and<br />
Matt Sharp taking up new roles<br />
as emergency care assistants<br />
in Ipswich and Hellesdon<br />
respectively in <strong>April</strong>.<br />
Grant and Matt were two of 11<br />
people on the NHS Englandfunded<br />
pilot programme and<br />
joined EEAST as volunteer<br />
community first responders after<br />
receiving induction training.<br />
The students then shadowed<br />
ambulance crews and call<br />
handlers in an emergency<br />
operations centre to see which<br />
role would suit them best, before<br />
being trained to kickstart a career<br />
in that role.<br />
In Matt and Grant’s case it was<br />
a career in frontline operations<br />
that appealed most and they<br />
undertook more clinical training to<br />
complete the course.<br />
Grant also completed the<br />
four-week course to drive an<br />
ambulance on blue lights – the<br />
certificate in emergency response<br />
ambulance driving (CERAD) – so<br />
will be ready to hit the ground<br />
running when he joins the Trust<br />
in <strong>April</strong>.<br />
The programme offers no<br />
guarantee of a job, but everyone<br />
on the course is supported<br />
throughout and secures<br />
qualifications that enhance their<br />
career prospects.<br />
Matt joined the programme from<br />
the care industry having long<br />
wanted to pursue a career with<br />
the ambulance service, while<br />
Grant had previously been a<br />
lorry driver.<br />
The programme has support from<br />
Helpforce, a charity which aims to<br />
accelerate the growth and impact<br />
of volunteering in health and care.<br />
It is hoped that the early success<br />
of the programme will lead to<br />
it being continued and provide<br />
another pathway for people to<br />
join EEAST.<br />
Vikki Darby, a leadership<br />
development manager at EEAST<br />
who led up the programme, was<br />
delighted to hear the news that<br />
Grant and Matt had secured jobs.<br />
She said:<br />
“It has been a privilege to support<br />
everyone on the pilot of the<br />
Volunteer to Career programme<br />
and I was ecstatic to hear Matt<br />
and Grant had been successful in<br />
their applications to join the Trust.<br />
“The teamwork across the<br />
organisation to help launch<br />
this programme has been<br />
phenomenal and ensured it has<br />
been a success.<br />
“Grant and Matt securing jobs at<br />
EEAST shows that the pathway<br />
works and we are looking to<br />
continue and develop this<br />
programme.”<br />
Grant said:<br />
“I would recommend this<br />
programme to anyone who is<br />
thinking about working in the<br />
ambulance service.<br />
“It takes a lot of effort and<br />
sacrifices as there are many hours<br />
of studying, but it gives you a real<br />
sense of achievement when you<br />
have completed all the courses.<br />
“The support from everyone<br />
involved with the programme<br />
has been fantastic and it gives<br />
volunteers a real insight into<br />
working at the ambulance service<br />
before committing to the job<br />
full time.”<br />
Matt said:<br />
“The support from Vikki and<br />
her team this on programme<br />
is exceptional. I can’t thank<br />
them enough.<br />
“The course was challenging but<br />
very rewarding and you always<br />
felt supported.<br />
Save more lives with<br />
the SPR<br />
“I feel incredibly lucky to be the<br />
first to have gone through this<br />
route to secure a job.”<br />
Photo caption: From volunteers<br />
to a career at the ambulance<br />
service, Matt Sharp (left) and<br />
Grant Harvey who have secured<br />
jobs at EEAST after completing<br />
the Volunteer to Career<br />
programme; they are pictured<br />
with Vikki Darby, leadership<br />
development manager.<br />
£1 million boost for<br />
wireless innovations<br />
to improve patient<br />
care<br />
Highest<br />
IP66<br />
Rating<br />
Trials of new wireless<br />
technologies to help improve<br />
patient care and strengthen<br />
connectivity in A&Es and<br />
ambulance bays are set to<br />
launch across seven NHS<br />
trusts, following new funding<br />
from NHS England.<br />
Around £1million in total has been<br />
awarded to seven trusts as part<br />
of NHS England’s Wireless Trials<br />
programme, which seeks to make<br />
the most of cutting-edge wireless<br />
technologies to provide the best<br />
care and experiences for patients,<br />
while freeing up more staff time to<br />
spend with their patients.<br />
Manchester University NHS<br />
Foundation Trust will trial an<br />
innovative approach of combining<br />
satellite and cloud-based wireless<br />
solutions to enhance connectivity<br />
across their 10 hospital sites and<br />
wider community services.<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
16<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
WEL Medical Half Page.indd 1 11/01/<strong>2024</strong> 10:23<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
17
NEWSLINE<br />
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
Mid Cheshire and Princess<br />
Alexandra Hospital NHS trusts<br />
will use the funding to install<br />
wireless trackers on medical<br />
equipment and hospital beds,<br />
which allow real-time monitoring<br />
and location tracking so that staff<br />
can easily find what they need,<br />
when they need it.<br />
The North West and East of<br />
England ambulance services<br />
trusts will also roll out improved<br />
wireless connections in A&E and<br />
ambulance areas, speeding up<br />
the transfer of essential patient<br />
care data from ambulances<br />
to hospitals.<br />
Another project run by Sussex<br />
Community NHS Foundation<br />
Trust will introduce a new<br />
app that allows staff to take<br />
observations on tablets and<br />
smartphones by a patient’s<br />
bedside, reducing the time spent<br />
typing up patient notes and<br />
providing more time to spend<br />
with patients.<br />
A trial at the Countess of Chester<br />
NHS Foundation Trust will<br />
wirelessly link modern diagnostic<br />
devices with the trust’s electronic<br />
patient records system, speeding<br />
up assessment time for patients.<br />
Stephen Koch, Executive<br />
Director of Platforms, NHS<br />
England, said: “I have been<br />
impressed with the innovative<br />
ideas coming from the system<br />
and we are delighted to be able<br />
to award this funding to the<br />
successful trialists to develop<br />
new or improved wireless<br />
solutions for the NHS.<br />
“We’ll be monitoring the<br />
outcomes of the trials and are<br />
very hopeful that a number of<br />
these will be able to be scaled<br />
more broadly across the health<br />
and social care system saving<br />
clinical time, improving patient<br />
care and saving money for<br />
the system.”<br />
Dan Prescott, Group<br />
Chief Information Officer,<br />
Manchester University NHS<br />
Foundation Trust, said: “As<br />
one of the country’s largest NHS<br />
trusts, it’s essential that we can<br />
provide continuous patient care<br />
with minimum disruptions. With<br />
the Wireless Trial we’re aiming to<br />
create a reliable, fast and secure<br />
network access solution to<br />
address unexpected connectivity<br />
issues, even in areas of poorconnectivity.<br />
This is vital in<br />
supporting key initiatives for our<br />
staff and giving our patients the<br />
best possible care.”<br />
Previous wireless trials included<br />
the development of University<br />
College London Hospitals’ Find<br />
and Treat service, which uses<br />
high-tech tools and software<br />
to provide real-time remote<br />
diagnosis and referrals on board<br />
a mobile health unit. The service<br />
provides remote screening,<br />
testing and treatment for<br />
vulnerable, homeless, and highrisk<br />
people in London.<br />
Another trial led to South London<br />
and Maudsley NHS Foundation<br />
Trust becoming the first<br />
5G-connected hospital in the <strong>UK</strong>.<br />
This Wireless Trials programme<br />
aims to provide NHS<br />
organisations with the capability<br />
they need to deliver the<br />
challenging digital ambitions set<br />
out in the NHS Long Term Plan.<br />
The trialists will benefit from<br />
funding for their project, advice<br />
and guidance from NHS England,<br />
and the opportunity to collaborate<br />
with like-minded organisations.<br />
NHS England will also capture<br />
best practice from successful<br />
trialists and share this across the<br />
wider NHS.<br />
Applications for the next series of<br />
wireless trials will open later this<br />
year. More details are available on<br />
the Connectivity Hub.<br />
College of<br />
Paramedics<br />
Granted Charter<br />
of Incorporation<br />
The College of Paramedics is<br />
thrilled to announce that we<br />
have been granted the Charter<br />
of Incorporation by His Majesty<br />
King Charles III.<br />
The Royal Charter was granted<br />
to the College in recognition<br />
of its objectives to inspire<br />
and enable all paramedics to<br />
participate in the profession<br />
within an environment based on<br />
safety, collegiality, inclusiveness,<br />
mental and physical wellbeing<br />
and innovation.<br />
The issue of the Royal Charter<br />
represents an important<br />
milestone in the development<br />
of the College of Paramedics,<br />
provides recognition for the<br />
profession, gives strength to our<br />
professional voice and leadership<br />
and offers our members a<br />
moment of immense pride.<br />
It also cements the College<br />
in perpetuity, meaning that<br />
there will always be a College<br />
of Paramedics for the future,<br />
supporting and guiding the<br />
profession forevermore.<br />
Chief Executive of the College<br />
of Paramedics, Tracy Nicholls<br />
said: “I am delighted we have<br />
been able to achieve this on<br />
behalf of our members, and to<br />
strengthen the College for the<br />
future. Gaining the Royal Charter<br />
is the first step towards being<br />
granted the title ‘Royal’ but our<br />
journey to increase leadership<br />
and development across our<br />
profession has a solid foundation<br />
for future chartered titles and<br />
more scope for development<br />
of paramedics.”<br />
President of the College of<br />
Paramedics, Jon Price said: “I am<br />
extremely proud that the College<br />
of Paramedics has received this<br />
level of recognition, and this<br />
represents a monumental effort<br />
from a large number of people<br />
who have tirelessly worked with<br />
the College since its inception to<br />
get us to this point.<br />
“The College has been<br />
recognised as a well-run charity<br />
whose purpose brings value,<br />
not only to its members but<br />
the nation as a whole. It is also<br />
recognition for every paramedic<br />
in the <strong>UK</strong> and beyond, in<br />
whatever professional setting<br />
you work, that your contribution<br />
to the profession is absolutely<br />
acknowledged and valued.”<br />
The College of Paramedics began<br />
life as the British Paramedic<br />
Association on December 14,<br />
2001, when it was established<br />
as the professional body for<br />
paramedics in the <strong>UK</strong>. Three<br />
years later, the organisation<br />
rebranded itself the College of<br />
Paramedics and within 15 years<br />
of its inception, the College had<br />
10,000 members. This figure has<br />
continued to grow over the years<br />
and today stands at more than<br />
20,000 members.<br />
Since its early days, the<br />
College has been instrumental<br />
in developing the paramedic<br />
profession and was responsible<br />
for writing the first standards<br />
of proficiency for paramedics<br />
in 2004, introducing the British<br />
Paramedic Journal, presenting<br />
the first paramedic curriculum<br />
framework in 2006, raising<br />
the threshold for entry to the<br />
Health and Care Professions<br />
Council’s register to degree<br />
status and achieving independent<br />
prescribing for paramedics.<br />
More recently, thanks to the<br />
College’s work with Public Health<br />
England and NHS England Public<br />
Health Commissioning and<br />
Operations, it was announced<br />
in September 2023 that primary<br />
care paramedics would be able<br />
to undertake the training required<br />
to become sample takers in<br />
the NHS Cervical Screening<br />
Programme.<br />
Several of these achievements<br />
occurred under the presidency<br />
of Dr John Martin, who has been<br />
a member of the College since<br />
2004 and was president between<br />
2017 and 2023, and who has<br />
been invaluable in guiding the<br />
College on its path to Royal<br />
Charter status.<br />
Dr John Martin, currently<br />
Chief Executive of South<br />
Western <strong>Ambulance</strong> Service,<br />
on secondment from his<br />
role as Chief Paramedic and<br />
Quality Officer and Deputy<br />
Chief Executive at London<br />
<strong>Ambulance</strong> Service said: “This<br />
is a fantastic acknowledgment<br />
that paramedics have become<br />
a key part of society delivering<br />
as a trusted profession to<br />
patients. The recognition through<br />
a Royal Charter confirms this<br />
proactmedical.co.uk<br />
and means the College of<br />
Paramedics will now be in place<br />
to support ongoing development<br />
for generations to come. It’s<br />
excellent news!”<br />
HELP Appeal makes<br />
fifth £250,000<br />
donation to British<br />
Association for<br />
Immediate Care<br />
(BASICS)<br />
Since 2019, its donations have<br />
enabled 79 grants to be made<br />
to BASICS’ schemes across<br />
the country<br />
Over the past five years, the<br />
HELP Appeal has donated a<br />
total of £1,250,000 to the British<br />
Association for Immediate Care<br />
(BASICS), which distributes<br />
individual grants to schemes,<br />
made up of medical, nursing and<br />
paramedic volunteers, who give<br />
up their free time to be on call to<br />
help NHS <strong>Ambulance</strong> Services.<br />
Thanks to the HELP Appeal,<br />
79 grants have been made to<br />
schemes, which have been used<br />
to purchase:<br />
• 8 Response vehicles<br />
• 172 Covert blue light and<br />
siren systems for emergency<br />
responders<br />
• 28 Safety equipment for<br />
vehicles, such as tyres,<br />
equipment cages and<br />
safety cameras<br />
• 32 Communications and<br />
satellite navigation equipment<br />
• 236 Personal protective<br />
equipment including helmets,<br />
flame retardant/all-weather<br />
high-vis safety wear and boots<br />
• 64 Specialist equipment bags<br />
• 21 Advanced monitor/<br />
defibrillators<br />
• Specialist monitoring<br />
Metal Max COMBI 50 Laryngoscope System<br />
equipment<br />
• 23 Ultrasound equipment<br />
• 25 Emergency driver training<br />
• 150 Specialist pre-hospital<br />
training<br />
The HELP Appeal’s latest (and<br />
fifth) donation of £250,000 will be<br />
distributed amongst 14 schemes<br />
in <strong>2024</strong> to help cover the cost<br />
of PPE, covert blue light and<br />
siren systems for emergency<br />
responders to ensure teams can<br />
arrive quickly at an emergency<br />
incident, kit bags and clinical<br />
equipment including defibrillators,<br />
ultrasound machines and cardiac<br />
resuscitation devices. The latest<br />
schemes to receive a grant are:<br />
• BASICS Devon<br />
• BASICS Essex<br />
• BEEP Doctors (Cumbria)<br />
• Beds and Herts Emergency<br />
Critical Care Scheme<br />
• BRAVO Medics (Bristol<br />
and Avon)<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
18<br />
19<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
• East Midlands Immediate<br />
Care Scheme<br />
• MERS Accident and Rescue<br />
(Midlands)<br />
• North East Immediate Care<br />
Scheme<br />
• North Staffordshire BASICS<br />
• North West Pre-Hospital<br />
Critical Care Charity<br />
• Suffolk Emergency Medical<br />
Charity<br />
• Swift Medics (Wiltshire,<br />
Swindon and Bristol)<br />
• SCAS BASICS (Hampshire)<br />
• West Yorkshire Medical<br />
Response Team<br />
Tony Kemp, Chief Officer of<br />
the British Association for<br />
Immediate Care, says:<br />
“As volunteers, our teams have<br />
little time to dedicate to the<br />
essential task of fundraising,<br />
neither do they have the skillsets<br />
and experience. The annual HELP<br />
Appeal donations are an absolute<br />
lifeline providing much needed<br />
vehicle, training and specialist<br />
equipment to our volunteer 999<br />
responders. Today, critical and<br />
enhanced care as provided by<br />
BASICS responders is much more<br />
costly as it requires much more<br />
advanced specialist equipment<br />
both for the patient’s benefit and<br />
to keep our volunteers safe and<br />
well prepared for their role.”<br />
Robert Bertram, Chief<br />
Executive of the HELP<br />
Appeal adds:<br />
“Thanks to our supporters’<br />
generosity, we have been able<br />
to focus on saving time and<br />
lives by enabling grants to be<br />
made to these incredible teams<br />
of medical volunteers who help<br />
in emergency incidents – often<br />
being first on the scene to treat<br />
a critically ill patient. The new<br />
equipment and PPE that will be<br />
purchased, can only strengthen<br />
their services across the country<br />
helping to save even more lives.”<br />
Mersey Care<br />
becomes first NHS<br />
Trust to eliminate<br />
Hepatitis C for more<br />
than six months<br />
The team, based at Brook<br />
Place in Liverpool, has now<br />
been free of Hepatitis C within<br />
their service users for the<br />
last eight months. It’s a virus<br />
which can cause serious and<br />
potentially life-threatening<br />
damage to the liver and is<br />
particularly common among<br />
more deprived communities,<br />
including those who have a<br />
history of substance abuse.<br />
They reached such a consistency<br />
by testing almost everyone<br />
registered with the service, no<br />
matter what risks they have<br />
been exposed to, and regularly<br />
reviewing their risk status and<br />
date of their last test.<br />
“All our Brook Place staff<br />
have been retrained on Hep<br />
C understanding, testing and<br />
offering harm reduction advice<br />
and risk of re-infection prevention<br />
information,” explained Hayley<br />
Curran, Recovery Co-ordinator<br />
at Brook Place. “That includes<br />
giving out safe needle exchange<br />
cards that we created and<br />
offering advice on not sharing<br />
equipment like toothbrushes,<br />
razors and pipes.<br />
“It’s a remarkable achievement<br />
and has taken a lot of hard work<br />
from everyone who works in the<br />
team. We know the virus is at its<br />
lowest levels in this country for 10<br />
years, but the discipline required<br />
to eliminate it from our service<br />
users for eight months is really<br />
exceptional.”<br />
Maintaining the elimination of<br />
Hep C has been a collaborative<br />
approach with Gilead Sciences,<br />
Hepatitis C U Later, the Hepatitis<br />
C Trust and Mersey Care’s<br />
Operational Delivery Network<br />
nurse, who is based at the<br />
Royal site of Liverpool University<br />
Hospital. The joined up approach<br />
has proved vital in providing the<br />
best standard of care to patients.<br />
According to the latest figures<br />
provided by the <strong>UK</strong> Health<br />
Security Agency (<strong>UK</strong>HSA) last<br />
year, Hepatitis C is most common<br />
among some of the most<br />
deprived areas in the country,<br />
so eliminating the virus helps<br />
towards Mersey Care’s aim of<br />
reducing health inequalities.<br />
This helps improve the service<br />
users’ physical health and<br />
increases positive outcomes,<br />
which also aids their recovery<br />
from substance abuse by<br />
becoming more in control of their<br />
health and care provided.<br />
The highly specialist team at<br />
Brook Place also provide a wide<br />
variety of services and are not,<br />
despite common belief, just<br />
a substitute prescriber. They<br />
provide a recovery focused<br />
service to people living in<br />
Liverpool who have problems<br />
using opiates and deliver<br />
clinics for Chronic Obstructive<br />
Pulmonary Disease (COPD),<br />
Spirometry testing, Hep C testing,<br />
sexual health and wound care.<br />
NHS apprenticeship<br />
‘truly changed<br />
my life’<br />
A former greengrocer has<br />
described how an NHS<br />
apprenticeship “truly changed”<br />
his life and set him on the path<br />
to becoming a nurse.<br />
At the start of National<br />
Apprenticeship Week, Steven<br />
Jewell, aged 42, who left school<br />
at 15 with no qualifications,<br />
told how he recently completed<br />
the Registered Nursing Degree<br />
Apprenticeship and now works at<br />
Lancashire and South Cumbria<br />
NHS Foundation Trust.<br />
After a range of jobs, including<br />
owning a greengrocer shop, he<br />
changed careers and joined the<br />
NHS as a healthcare support<br />
worker, before starting his<br />
apprenticeship.<br />
The NHS is the nation’s biggest<br />
trainer of apprentices, with more<br />
than 20,000 starting last year.<br />
Apprentices are a crucial part of<br />
the NHS Long Term Workforce<br />
Plan and NHS England aims to<br />
triple the number being trained by<br />
2030, so they make up more than<br />
one in five new recruits.<br />
Steven said: “Without the<br />
apprenticeship, I would never<br />
have been able to go to university<br />
or be in the position I am today.<br />
At nearly 40, being afforded the<br />
opportunity to earn a salary while<br />
taking a degree level course with<br />
blended work-placed learning,<br />
truly changed my life.<br />
“The apprentice route has<br />
enabled me to go from<br />
greengrocer to registered<br />
mental health nurse in just over<br />
four years. I am now in a job I<br />
love, helping other people, as<br />
well as changing my life for the<br />
better. Don’t ever think you are<br />
too old or not smart enough.<br />
Apprenticeships provide all of us<br />
with equal opportunities to our<br />
peers, and enable us to change<br />
course in life - we just have to<br />
want it.”<br />
Apprenticeships offer routes into<br />
many of the more than 350 NHS<br />
careers, meaning people can<br />
“earn while they learn” - working<br />
for their local NHS, but without<br />
having to go to university first.<br />
This includes a range of higher<br />
or degree apprenticeships<br />
(equivalent to foundation, full<br />
Bachelor’s or Master’s degrees),<br />
including nursing.<br />
And the Medical Doctor Degree<br />
Apprenticeship pilot, due to<br />
be launched this year, is the<br />
first of its kind in the world and<br />
an important step forward in<br />
helping to attract a wider range<br />
of candidates to medicine. It will<br />
initially be delivered with three<br />
Higher Education Institutes.<br />
NHS apprenticeships also include<br />
a variety of entry-level roles<br />
including support staff – helping<br />
employers attract talent from<br />
local communities and ensuring<br />
people from all backgrounds<br />
get the chance to pursue a<br />
rewarding career.<br />
With the increased focus on data<br />
and move to electronic patient<br />
records there is also a focus on<br />
digital apprenticeships to attract<br />
new talent into tech roles in the<br />
NHS, with opportunities ranging<br />
from Data Technician to Artificial<br />
Intelligence Data Specialist.<br />
Professor Mark Radford,<br />
Director of Long Term<br />
Workforce Plan Delivery<br />
and Education, and Deputy<br />
Chief Nursing Officer at NHS<br />
England, said:<br />
“Apprentices are at the heart of<br />
our Long Term Workforce Plan,<br />
to put staffing on a sustainable<br />
footing and improve patient care.<br />
“Apprenticeships are a fantastic<br />
tool, not only to attract new talent<br />
to the NHS but also to develop the<br />
skills of the existing workforce.<br />
“Our ambition for apprenticeships<br />
is to continue to build on the<br />
fantastic success of the expansion<br />
to date and provide an alternative<br />
route to careers such as nursing<br />
and Allied Health Professions.<br />
Working with UCAS from 2025<br />
young people will also be able to<br />
apply for apprenticeships at the<br />
same time as traditional degree<br />
programmes.”<br />
Health Minister Andrew<br />
Stephenson said:<br />
“I am delighted to see the NHS<br />
has emerged as the country’s<br />
top trainer of apprentices – with<br />
over 20,000 starting last year -<br />
showing just how many people<br />
continue to value a career in the<br />
health service.<br />
“Apprentices are an integral part<br />
of the NHS’ Long Term Workforce<br />
Plan. We’re committed to<br />
boosting training for clinical staff<br />
through apprenticeships over the<br />
coming years, as we continue<br />
to deliver long term change for a<br />
brighter future.<br />
“The introduction of the<br />
groundbreaking Medical Doctor<br />
Degree Apprenticeship will further<br />
widen participation from underrepresented<br />
backgrounds —<br />
inspiring more people to pursue<br />
their dreams while allowing them<br />
to earn while they learn.”<br />
Minister for Skills,<br />
Apprenticeships and Higher<br />
Education Robert Halfon said:<br />
“The NHS serves the nation’s<br />
health needs every single day and<br />
apprenticeships are a crucial way<br />
for the health service to get the<br />
staff it vitally needs. NHS England<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
20<br />
21<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
is one of our Top 100 apprentice<br />
employers, and embraces both<br />
apprenticeships and T Levels<br />
as great ways to get skilled<br />
healthcare workers.<br />
“Apprenticeships are crucial<br />
to giving people from all<br />
backgrounds the chance to<br />
climb the ladder of opportunity<br />
and it’s fantastic news that they<br />
plan to recruit one in five of their<br />
employees as apprentices by<br />
2030. The NHS understand the<br />
apprenticeship levy and use it<br />
well, and I hope more employers<br />
follow their lead and experience<br />
the benefits of apprentices for<br />
themselves.”<br />
Jennifer Coupland, chief<br />
executive of the Institute for<br />
Apprenticeships and Technical<br />
Education (IfATE), said:<br />
“It’s brilliant to see that so many<br />
people are reaping the benefits<br />
of world class apprenticeships,<br />
designed by employers. They<br />
are popular across the country<br />
and with a really good variety of<br />
occupations.”<br />
NHS staff experience<br />
improving, according<br />
to world’s largest<br />
workforce survey<br />
The experiences of staff<br />
working in the NHS in England<br />
have improved across a range<br />
of important areas, including<br />
to new results from the world’s<br />
largest workforce survey.<br />
Compared to the previous<br />
survey in 2022, staff are<br />
markedly more likely to say<br />
that they would recommend<br />
their organisation as a place<br />
to work; that they would be<br />
happy with the standard of<br />
care provided if a friend or<br />
relative needed treatment; and<br />
that they have the right support<br />
and resources to do their jobs.<br />
However, results for many key<br />
measures of staff experience<br />
remain below pre-Covid levels.<br />
Results from the NHS Staff<br />
Survey, which was coordinated<br />
by the independent charity<br />
Picker on behalf of NHS<br />
England, included responses<br />
from more than 700,000 NHS<br />
staff working across more than<br />
200 organisations. The survey<br />
included all directly employed<br />
staff in secondary and tertiary<br />
care organisations, ranging from<br />
consultants to care assistants<br />
and from porters to paramedics.<br />
Questions in the survey cover<br />
all aspects of work experiences,<br />
with a particular focus on those<br />
described by NHS England’s<br />
People Promise.<br />
The survey showed large<br />
improvements in a range of<br />
important areas. Two headline<br />
measures that had fallen since<br />
2020 showed signs of recovery:<br />
the proportion of staff who would<br />
recommend their organisation<br />
as a place to work jumped<br />
3.7% points to 61.1%, whilst<br />
the 65.0% said that they would<br />
be happy with the standard<br />
of care provided by their<br />
organisation if a friend or relative<br />
needed treatment, a 2.0% point<br />
improvement on 2022. Results<br />
for both measures remain below<br />
the pre-Covid levels recorded<br />
in 2019, which were 63.4% and<br />
71.5% respectively – but NHS<br />
providers will be encouraged<br />
by the scale of improvements<br />
in 2023.<br />
Some of the most striking<br />
improvements in the survey<br />
were around workload and<br />
resources. After declines on<br />
most of these questions in<br />
2021 and 2022, results are now<br />
equal to or higher than they<br />
were before the pandemic in<br />
2019. For example, 46.7% of<br />
staff said that they are “able to<br />
meet all the conflicting demands<br />
on their time at work”; a 3.7%<br />
improvement from 2022, and<br />
0.7% higher than in 2019. There<br />
was an even bigger improvement<br />
in the proportion who said that<br />
there are enough staff in their<br />
organisation for them to do their<br />
job properly – up 6.0% points<br />
from 26.4% in 2022 to 32.4% in<br />
2023. The concern remains that<br />
only a minority of staff agreed<br />
with these statements – but the<br />
improvements are substantial<br />
and demonstrate good progress<br />
in an area that has long been<br />
challenging.<br />
The 2023 survey was conducted<br />
during September, October, and<br />
November 2023. This was several<br />
months after freshly agreed<br />
pay deals were implemented<br />
for most staff groups – but<br />
at a time when junior doctors<br />
and consultant remained in<br />
dispute. Overall, satisfaction with<br />
pay improved by 5.6% points<br />
compared to 2022 – but remains<br />
low at 31.2%. Perhaps reflecting<br />
ongoing disputes, trends differ<br />
for different staff groups: whilst<br />
most are now more satisfied with<br />
pay than in 2022, the proportion<br />
of medical and dental staff who<br />
were satisfied with their pay fell by<br />
4.5% points to 32.0% - continuing<br />
a steep decline from a high of<br />
56.9% in 2020.<br />
This year, the survey included<br />
a new question asking staff<br />
whether they had “been the<br />
target of unwanted behaviour of<br />
a sexual nature in the workplace”,<br />
either from patients and the<br />
public or from colleagues.<br />
The definition of “unwanted<br />
behaviour” is broad, including<br />
inappropriate conversations and<br />
‘jokes’ as well as touching and<br />
assault. Overall, 8.7% of staff –<br />
equivalent to more than 120,000<br />
people when scaled to the size<br />
of the workforce – reported<br />
being the target of unwanted<br />
sexual behaviour from patients<br />
and the public. Unsurprisingly,<br />
this figure was much higher for<br />
staff in roles that are frequently<br />
patient-facing (11.5%), and there<br />
was significant variation between<br />
different staff groups. The<br />
highest rates were reported by<br />
ambulance technicians (36.1%)<br />
and paramedics (32.2%).<br />
Commenting on the findings,<br />
Chris Graham, Chief Executive<br />
at Picker, said: “The results<br />
from the 2023 NHS Staff<br />
Survey provide welcome good<br />
news for providers, as they<br />
show frequently substantial<br />
improvements across many<br />
of the most important areas<br />
of workforce experience. This<br />
follows a period of time where<br />
staff experience had suffered in<br />
the wake of the pandemic, and<br />
– whilst in many cases results<br />
have not yet returned to the prepandemic<br />
level – it is encouraging<br />
to see these improvements in<br />
staff engagement and wellbeing.<br />
“With more than 700,000<br />
responses nationally, the<br />
survey is a goldmine of insight<br />
for organisations wishing to<br />
understand the experiences of<br />
their staff. Beneath the national<br />
level, it offers detailed evidence<br />
on the experiences of different<br />
staff and demographic groups<br />
within trusts – and we encourage<br />
all providers to delve deep into<br />
the data to understand how<br />
different parts of their workforce<br />
experience working life. There<br />
is much room for further<br />
improvement and an opportunity<br />
to build on progress over the<br />
last year to make the NHS the<br />
best possible place to work.<br />
This should be a top priority for<br />
organisations, both because<br />
better workforce experience<br />
is associated with a range of<br />
positive outcomes – including<br />
better patient experiences,<br />
lower sickness absence rates,<br />
and higher staff retention – and<br />
because the people working hard<br />
to deliver a person centred health<br />
service deserve to see that care<br />
reciprocated.”<br />
Critically ill<br />
grandmother thanks<br />
medics for ‘gift of<br />
life’ and chance<br />
to meet her first<br />
granddaughter<br />
A woman who survived a<br />
cardiac arrest has thanked<br />
paramedics for giving her<br />
the chance to meet the<br />
granddaughter born as she<br />
fought for her life.<br />
At an emotional reunion at<br />
Isleworth <strong>Ambulance</strong> Station,<br />
Sue Whitham, 62, who lives<br />
in Hanworth in west London,<br />
thanked the ambulance crews<br />
and 999 call handler who came<br />
to her rescue when she suffered<br />
a sudden cardiac arrest at home.<br />
Sue left work one night at St<br />
Mary’s University in Twickenham<br />
telling colleagues ‘I think my<br />
granddaughter will be born this<br />
weekend’. She promised to call<br />
with news, but that night her<br />
heart suddenly stopped beating.<br />
She said: “Thankfully my husband<br />
Julian knew how to do chest<br />
compressions and instinctively<br />
knew that I wasn’t breathing.<br />
Within seconds he saw I was<br />
turning blue.<br />
“Fortunately we had our phones<br />
nearby so my son Jordan and his<br />
partner Emma could call as we<br />
were expecting their daughter<br />
Sienna to be born at any moment<br />
and we were on standby to look<br />
after their little boys.”<br />
Julian dialled 999 and call handler<br />
Mattie Wright was there for him<br />
on the other end of the line to<br />
offer life-saving advice. She<br />
counted with him so he could<br />
perform chest compressions<br />
on Sue.<br />
Julian said: “Within seconds I<br />
JOIN THE TEAM<br />
knew Sue was gone and I could<br />
tell there was no sign of life. Mattie<br />
was brilliant and her calming voice<br />
encouraged me to keep going<br />
with chest compressions.”<br />
Isleworth, Hanwell and New<br />
Malden ambulance crews<br />
including Jade Bank, Jack<br />
Denham, George Simpson,<br />
Annie Davies and Nichaela Coyle<br />
arrived at the scene quickly.<br />
Advanced paramedic Andy<br />
Parker was also dispatched to<br />
assist in stabilising Sue.<br />
Julian added: “The crews took<br />
over resuscitation and a couple of<br />
them took me into another room<br />
and kept me away so I couldn’t<br />
see what was going on. I was in<br />
a terrible state of shock.”<br />
It took an hour to stabilise Sue<br />
before ambulance crew George<br />
and Annie took her to St George’s<br />
Hospital in Tooting.<br />
PARAMEDICS, TECH’S & ECA’S<br />
FOR FRONTLINE WORK FROM OUR PLYMOUTH BASE<br />
GREAT RATES OF PAY FREE ACCOMMODATION<br />
LEARNING & DEVELOPMENT OPPORTUNITIES<br />
Email the HR Team on hr@alliance-pioneer.co.uk<br />
or call them on 01752 717722 for more information.<br />
Hawthorne House, 25 Darklake View,<br />
Estover, Plymouth, PL6 7TL<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
22<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
23
NEWSLINE<br />
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
Sue suffered another cardiac<br />
arrest on her way to St George’s<br />
and was immediately taken to the<br />
hospital’s heart centre. She had<br />
tiny tubes, called stents, inserted<br />
into the blood vessels around her<br />
heart to allow the blood to keep<br />
flowing through.<br />
Doctors on the intensive care unit<br />
put Sue into a medically-induced<br />
coma for several weeks so they<br />
could drop her body temperature<br />
down to allow her recover.<br />
Sue said: “When I was brought<br />
out of the coma I didn’t know<br />
what had happened to me and<br />
couldn’t believe I had a fourweek-old<br />
granddaughter.<br />
“I didn’t even know Sienna had<br />
been born as I thought I had<br />
woken up the next day. It’s an<br />
absolute miracle that I’m here.<br />
I’ve been told my heart failed<br />
several times and I’m so grateful<br />
the ambulance crews didn’t give<br />
up on me.<br />
“I was determined to get strong<br />
again so I could walk Sienna in<br />
the park and shop for baby things,<br />
which four months on, I can now<br />
do. The hospital medics at St<br />
George’s were also incredible.”<br />
Sue, who already has four little<br />
grandsons she adores, added:<br />
“I’ve been gifted another life. I had<br />
longed for a granddaughter and<br />
when we found out about her I<br />
was just so excited for a little girl.”<br />
Mattie Wright, 999 Emergency<br />
Call Handler at London<br />
<strong>Ambulance</strong> Service, said: “I was<br />
utterly overjoyed to hear of Sue’s<br />
incredible recovery, and it was an<br />
honour to be able to meet Sue<br />
and her family. I definitely cried<br />
when I met them.<br />
“I hope Sue, Julian and their<br />
newly expanded family enjoy<br />
every single moment they can<br />
squeeze from life.”<br />
Julian said: “It was wonderful to<br />
meet Mattie and the paramedics<br />
who helped saved Sue. As a<br />
family, we are eternally grateful<br />
to them.”<br />
Sam Wilcox, Community<br />
Defibrillation Manager at<br />
London <strong>Ambulance</strong> Service,<br />
said “Knowing what to do when<br />
someone is in cardiac arrest and<br />
having the confidence to act<br />
quickly will save lives.<br />
“The first few minutes before an<br />
ambulance arrives can make all<br />
the difference. Over 75 percent of<br />
cardiac arrests happen at home,<br />
so by learning these simple<br />
skills, you could save someone<br />
you love.”<br />
Dr Jonathan Aron, Consultant<br />
in Intensive Care Medicine at<br />
St George’s Hospital, said: “It’s<br />
wonderful to hear that Sue has<br />
continued to do so well since<br />
leaving our care, and it was a<br />
privilege to have played such<br />
a vital part in her treatment<br />
and recovery.<br />
“Patients who have suffered<br />
heart attacks and acute heart<br />
failure like Sue need immediate<br />
attention. This was an incredible<br />
response from everyone – from<br />
Sue’s family, to the call handler<br />
and paramedics, to the multiple<br />
teams of staff at St George’s<br />
and beyond.”<br />
Two ambulance<br />
medics a day kicked,<br />
punched, and spat at<br />
in London<br />
Physical violence against<br />
ambulance crews in London<br />
has soared by nearly 40% in<br />
the past year, shocking new<br />
figures can reveal.<br />
Fresh data released by London<br />
<strong>Ambulance</strong> Service in February<br />
has laid bare the appalling<br />
increase in abuse against<br />
ambulance staff, with cases<br />
surging from 523 in 2022 to<br />
728 in 2023. That’s a 39 per<br />
cent increase.<br />
The staggering figures show<br />
instances of kicking, punching,<br />
spitting or attacking with a<br />
weapon affect two ambulance<br />
medics a day.<br />
Pauline Cranmer, Chief<br />
Paramedic at London <strong>Ambulance</strong><br />
Service, said:<br />
“These shocking figures reveal a<br />
very, very sad state of affairs.<br />
“Our ambulance crews and<br />
call handlers work tirelessly<br />
day in and day out to care for<br />
Londoners and treat each patient<br />
with respect. Abuse of any form<br />
can have a profound impact on<br />
our staff and won’t be tolerated.<br />
“On the whole, abusive patients<br />
are just a small number of the<br />
people our medics see every day,<br />
and sometimes violent behaviour<br />
arises as a consequence of a<br />
medical condition. However, I<br />
want to urge the public to treat<br />
our staff with kindness and<br />
respect while they go about their<br />
very busy shifts.<br />
“We have invested £3 million in<br />
fitting our ambulances with safety<br />
systems to protect our staff and<br />
created a dedicated violence<br />
reduction team to encourage<br />
reporting and ensure abusers are<br />
brought to justice.<br />
“Staff and volunteers feel<br />
increasingly confident to come<br />
forward and trust they will be<br />
supported through our own<br />
teams and the courts.”<br />
Last November, London<br />
<strong>Ambulance</strong> Service called for<br />
violence against ambulance<br />
staff to stop when it released<br />
video footage of a paramedic<br />
getting pushed out the back of an<br />
ambulance by an abusive patient.<br />
The paramedic was shown<br />
crashing to the ground and<br />
landing hard on his elbow as the<br />
patient walked straight past him,<br />
displaying no reaction.<br />
The patient was promptly<br />
arrested and has since been<br />
convicted and ordered to pay the<br />
paramedic compensation.<br />
The London <strong>Ambulance</strong> Service<br />
paramedic said: “I’m glad this<br />
went to court because it reminds<br />
people this is an unacceptable<br />
way to treat us and needs to<br />
be stopped.<br />
“We come to work to help<br />
people, not for this. I always wear<br />
a body-worn camera now and I<br />
make sure I’m never alone with<br />
some patients who I think might<br />
be a risk.”<br />
The Service has dedicated<br />
Violence Reduction Officers who<br />
encourage colleagues to report<br />
all incidents of abuse while also<br />
supporting them through the<br />
court process. Over 70% of staff<br />
who experience abuse currently<br />
report it and the Trust continues<br />
to improve its reporting culture.<br />
While many offenders never to<br />
go to court on medical grounds,<br />
there have been 38 successful<br />
prosecutions since <strong>April</strong> 2023.<br />
As part of the £3 million<br />
investment in safety measures,<br />
the Service fit its ambulances<br />
with panic buttons linked to<br />
a recording device and new<br />
monitors that can help staff see<br />
the outside of the vehicle, as well<br />
an electronic tracking to help<br />
police arrive even faster.<br />
C<br />
M<br />
Y<br />
CM<br />
MY<br />
CY<br />
CMY<br />
K<br />
In recent years, LAS joined<br />
ambulance services across<br />
the country to launch a “Work<br />
Without Fear” campaign to<br />
promote a no-violence culture<br />
and help create a safer work<br />
environment for front-line staff<br />
and volunteers. The campaign<br />
encourages staff and volunteers<br />
to report all incidents of abuse<br />
and violence rather than accept it<br />
as ‘part of the job’.<br />
Celebrating 10 years<br />
of MERIT doctors<br />
in the ambulance<br />
service<br />
The beginning of March<br />
marked the 10th anniversary<br />
of North West <strong>Ambulance</strong><br />
Service’s (NWAS) Medical<br />
Emergency Response Incident<br />
Team (MERIT).<br />
comprises a committed group<br />
of doctors who support incident<br />
commanders during major, mass<br />
casualty, and complex incidents<br />
across the region.<br />
MERIT doctors contribute to<br />
command and clinical decisionmaking<br />
processes. The team<br />
provides medical advice,<br />
coordinates on-scene medical<br />
assets, and helps us get the right<br />
care to patients involved in largescale<br />
incidents.<br />
Bringing together a diverse range<br />
of specialties, each team member<br />
offers expert knowledge and<br />
experience in their respective<br />
practice areas. Supporting NWAS’<br />
response to incidents such as<br />
uncontrolled chemical releases,<br />
large-scale road traffic collisions,<br />
fires, or civil disorders, MERIT<br />
doctors work on an on-call basis<br />
to provide medical expertise<br />
The team, set <strong>Ambulance</strong> up in <strong>UK</strong>.pdf March 1 2014, 20/03/<strong>2024</strong> 10:25:56 across the region at any time.<br />
Save lives -<br />
spread the road<br />
safety message<br />
Reflecting on a decade of service,<br />
MERIT Manager Dr Craig Hooper<br />
remarked: “People may not<br />
necessarily be aware that there<br />
are doctors who work within<br />
the ambulance service. The<br />
past 10 years have showcased<br />
MERIT’s invaluable contribution in<br />
responding to complex, largescale<br />
incidents. The dedicated<br />
team work seamlessly with our<br />
command and clinical leadership<br />
colleagues. They provide<br />
essential advice and ensure<br />
medical resources are given to<br />
those in need.”<br />
NWAS was among the first<br />
ambulance services in the nation<br />
to establish a bespoke team of<br />
As ambulance crew with a professional driving or riding qualification, join our road safety<br />
community. Become an IAM RoadSmart member to access a range of benefits and influence<br />
road users with your skills, knowledge, and experience.<br />
JOIN TODAY<br />
Visit iamroadsmart.net/ambulanceuk<br />
or call us on 0300 303 1134.<br />
@IAMRoadSmart<br />
@iam_roadsmart<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
24<br />
25<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
doctors of this nature.<br />
One of the longest-serving<br />
MERIT doctors, Dr Theo Weston,<br />
added: “Working within MERIT<br />
for ten years complements my<br />
other medical practices, offering<br />
valuable insights and allowing me<br />
to contribute meaningfully to the<br />
ambulance service. It has been<br />
a privilege to be part of such an<br />
important and national leading<br />
organisation - there are very<br />
few similar schemes like MERIT<br />
throughout the country and it<br />
has been great to be a part of<br />
that journey.”<br />
Each MERIT doctor possesses<br />
a certificate of completion of<br />
training in either general practice<br />
or specialties such as emergency<br />
medicine, anaesthesia, critical<br />
care, and surgery.<br />
Find further information<br />
about MERIT by visiting<br />
nwas.nhs.uk/careers.<br />
Pic caption - MERIT doctor<br />
(centre) getting involved in<br />
incident command training<br />
SECAmb NHS<br />
Staff Survey<br />
shows significant<br />
improvements<br />
South East Coast <strong>Ambulance</strong><br />
Service NHS Foundation Trust,<br />
(SECAmb), is pleased to see<br />
significant improvements in its<br />
results in the yearly national<br />
NHS Staff Survey.<br />
The 2023 survey, published<br />
by NHS England today,<br />
(7 March), saw SECAmb record<br />
improvements across all nine<br />
themes explored by the survey’s<br />
questions and improved<br />
scores to almost all individual<br />
questions. The Trust’s scores<br />
have also improved more,<br />
year-on-year, than others in the<br />
ambulance sector.<br />
Close to 2,800 colleagues, (some<br />
60 per cent of staff), completed<br />
the voluntary survey – the fourth<br />
consecutive year more than 60<br />
per cent have participated.<br />
The results include:<br />
• 62 per cent said they were<br />
enthusiastic about their job – an<br />
increase of 5 per cent on 2022<br />
• 60 per cent of staff said that<br />
care of patients/service users is<br />
a top priority – an improvement<br />
of 8 per cent since 2022<br />
• 53 per cent said they felt safe<br />
to speak up about anything that<br />
concerns them – also an 8 per<br />
cent improvement on 2022<br />
• 62 per cent of staff said that,<br />
if a friend or relative needed<br />
treatment, they would be<br />
happy with the standard of<br />
care provided – a 10 per cent<br />
improvement on 2022<br />
While welcoming the marked<br />
improvements in results,<br />
SECAmb recognises the need<br />
for further work across all areas<br />
of the Trust and is committed<br />
to evaluating the results of<br />
the survey to drive further<br />
improvements.<br />
SECAmb Chief Executive, Simon<br />
Weldon, said: “I’d like to thank<br />
each and every colleague who<br />
took the time to complete the<br />
survey. While we want to hear<br />
everyone’s views throughout the<br />
year, the national staff survey is an<br />
extremely valuable tool where we<br />
can gain feedback, of any kind, to<br />
ensure we continue to improve,<br />
and respond to the things that are<br />
important to our staff.<br />
“There is much to be positive about<br />
in these results but I recognise that<br />
there is still a lot of work to be done<br />
to ensure we are where we need to<br />
be as an organisation for both our<br />
staff and patients.<br />
“I would like to take this<br />
opportunity to thank colleagues<br />
for everything they do, dayin,<br />
day-out, to respond to our<br />
patient’s needs. They should<br />
be very proud of the work they<br />
do and I am committed to<br />
ensuring their work environment<br />
is everything it should be so that<br />
they can thrive in their roles.”<br />
The SECAmb results in full can be<br />
found via the following link: NHS<br />
Staff Survey Benchmark report<br />
2023 (nhsstaffsurveys.com)<br />
Clinical hubs<br />
benefiting patients<br />
and reducing<br />
demand on A&E<br />
Two clinical co-ordination hubs<br />
set up as trials by South East<br />
Coast <strong>Ambulance</strong> Service NHS<br />
Foundation Trust, (SECAmb),<br />
in partnership with NHS Trusts<br />
in Kent, have been extended<br />
having delivered positive<br />
early results.<br />
The hubs, established in Autumn<br />
last year, in the Trust’s Paddock<br />
Wood and Ashford operational<br />
areas, involve multi-discipline<br />
teams from across the Kent<br />
healthcare system joining<br />
SECAmb Paramedic Practitioners<br />
to ensure 999 calls are receiving<br />
the most appropriate response.<br />
By reviewing appropriate 999<br />
calls, the hubs are helping<br />
to reduce pressure on A&E<br />
by guiding patients to the<br />
most appropriate service and<br />
supporting ambulance crews at<br />
the scene of an incident.<br />
Based at the Trust’s Ashford and<br />
Paddock Wood Make Ready<br />
Centres, SECAmb teams are<br />
joined by emergency department<br />
consultants and clinicians from<br />
East Kent Hospitals University<br />
NHS Foundation Trust, Maidstone<br />
and Tunbridge Wells NHS Trust<br />
and urgent care teams, including<br />
the Home Treatment Service at<br />
Kent Community Health NHS<br />
Foundation Trust.<br />
In the 15 weeks since the<br />
beginning of October last<br />
year, the West Kent Clinical<br />
Coordination Hub has made<br />
more than 1,400 contacts with<br />
crews and discharged more<br />
than 200 patients on scene. It<br />
has help avoid conveyance to<br />
an emergency department for<br />
more than 500 patients where<br />
the original plan was to convey;<br />
supported 79 medical Same<br />
Day Emergency Care (SDEC)<br />
referrals and 19 surgical SDEC<br />
referrals; arranged 90 GP in ED<br />
appointments; and referred 191<br />
patients directly into a home<br />
treatment team.<br />
The Ashford Integrated Care<br />
Hub has enjoyed similar success<br />
since its launch at the beginning<br />
of November 2023. Over the<br />
last three months it has made<br />
more than 1,500 contacts with<br />
ambulance crews and discharged<br />
more than 600 patients on<br />
scene. It has also arranged more<br />
appropriate care for more than<br />
800 patients who were due to<br />
attend an emergency department.<br />
The hub has supported more than<br />
100 medical SDEC referrals and<br />
more than 100 Urgent Community<br />
Response (UCR) referrals. Some<br />
180 GP in emergency department<br />
appointments have been arranged<br />
and the team has referred<br />
approximately 250 patients directly<br />
into a home treatment team.<br />
SECAmb Operations Manager<br />
for Ashford, Nakai Redman<br />
said: “The first three months the<br />
hub has been in operation have<br />
been extremely encouraging.<br />
The results have shown that<br />
by having a multi-discipline<br />
approach to reviewing 999 calls,<br />
we can improve the response and<br />
ultimately the care we provide the<br />
local community.<br />
“We have also seen a significant<br />
improvement in work satisfaction<br />
from colleagues as they finding<br />
they are more often being sent<br />
to emergencies where they can<br />
make a difference and help<br />
patients with the support of<br />
shared decision making.”<br />
SECAmb Practice Development<br />
Lead and the Trust’s lead at<br />
the Paddock Wood hub, Sean<br />
Edwards said: “Our clinical<br />
coordination hub is a true<br />
collaboration between acute<br />
and community services that<br />
is directly benefitting patients,<br />
ensuring they can be seen in<br />
the right place, first time for<br />
their condition, and reducing<br />
unnecessary ED attendances.<br />
Furthermore, <strong>Ambulance</strong> crews<br />
have access to senior clinicians<br />
to aid in complex decision<br />
making, ensuring patient safety<br />
and improving the quality of care<br />
we can provide our patients in<br />
West Kent.”<br />
New cards to help<br />
deliver instant<br />
patient feedback<br />
Patients will soon be able to<br />
instantly provide feedback on<br />
the care given to them with the<br />
introduction of new feedback<br />
cards on every South East<br />
Coast <strong>Ambulance</strong> Service<br />
(SECAmb) ambulance.<br />
The small business cards, which<br />
are expected to be on board<br />
ambulances in the coming<br />
weeks, feature a QR code<br />
allowing patients to scan it with<br />
a smart device, if they have one.<br />
The QR code will then take them<br />
to SECAmb’s Patient Experience<br />
Questionnaire which is also<br />
hosted on its website.<br />
Giving a card means that if a<br />
patient doesn’t have a smart<br />
device or they don’t feel well<br />
enough to provide their feedback<br />
at the time they are being cared<br />
for, they can take the card with<br />
them and provide their feedback<br />
at a later time.<br />
The cards provide an additional<br />
way of gathering patient<br />
feedback with the only previous<br />
way for people to officially<br />
provide feedback being through<br />
contacting the Trust’s patient<br />
experience team.<br />
Recognising that obtaining<br />
feedback via the questionnaire<br />
from patients is very reliant on<br />
them having a smart device or a<br />
computer, it is not the only way<br />
patients can share their views as<br />
we still welcome people’s letters,<br />
cards and calls to our patient<br />
experience team who ensure<br />
patient feedback is captured and<br />
shared appropriately. Details of<br />
how to get in touch can be found<br />
on the Trust’s website: Patient<br />
Advice & Liaison - PALS - NHS<br />
South East Coast <strong>Ambulance</strong><br />
Service (secamb.nhs.uk) or by<br />
calling 0300 1239 242<br />
SECAmb Patient Engagement<br />
Lead, Vikki Baldock said: “Having<br />
this instant feedback will be really<br />
valuable and is just one approach<br />
we are taking to give patients to<br />
communicate with us about the<br />
service they receive.<br />
“We understand that this<br />
approach may exclude some<br />
groups of people so we<br />
absolutely continue to welcome<br />
the more traditional approach of<br />
getting in touch with our patient<br />
experience team.<br />
“The questionnaire offers an<br />
informal approach to providing<br />
feedback as people are not<br />
required to provide personal<br />
information about themselves<br />
unless they wish to, and for which<br />
there is a free-text field to allow<br />
for this.”<br />
SECAmb recently introduced its<br />
community forums which have<br />
allowed patients to share their<br />
experiences about our services<br />
as well has learn more about<br />
what we’re doing to improve the<br />
care we provide.<br />
Anyone who would like to learn<br />
more about SECAmb’s patient<br />
engagement work or would<br />
like to get involved, is asked to<br />
email engagementteam@<br />
secamb.nhs.uk<br />
Volunteer film<br />
highlights<br />
importance of<br />
bystander CPR<br />
A short film highlighting the<br />
importance of bystander<br />
CPR and the use of public<br />
access defibrillators has been<br />
produced by Tonbridge and<br />
Tunbridge Wells Community<br />
First Responder, (CFR), team.<br />
The volunteer team is one of<br />
close to 60 teams which is<br />
trained by and works with South<br />
East Coast <strong>Ambulance</strong> Service,<br />
with responders attending certain<br />
emergencies and providing vital,<br />
often life-saving care to patients.<br />
The awareness film was<br />
produced in partnership with<br />
local video production company,<br />
Digitom, based in Tunbridge<br />
Wells, after the CFR team<br />
successfully applied to be the<br />
company’s Charity of the Year –<br />
part of which includes benefiting<br />
from a free video production<br />
package to promote their cause.<br />
The film sees a reconstruction<br />
where a man collapses in a<br />
shopping centre and requires<br />
cardiopulmonary resuscitation,<br />
(CPR), and a shock from a public<br />
access defibrillator to save his life.<br />
The film concludes with a twist,<br />
when it’s revealed its narrator<br />
is 27-year-old cardiac-arrest<br />
survivor and local Maidstone<br />
resident Frankie Turner.<br />
Frankie’s life was saved by the<br />
quick-thinking of husband,<br />
Nathan, who commenced<br />
CPR and the attending<br />
ambulance clinicians.<br />
Data shows that sadly fewer than<br />
10 per cent of patients survive<br />
to 30 days after experiencing an<br />
out-of-hospital arrest.<br />
Prompt bystander CPR and early<br />
defibrillation is key to increasing<br />
out-of-hospital cardiac arrest<br />
survival rates.<br />
Tonbridge and Tonbridge Wells<br />
CFR Team Leader, Fergus<br />
Chalmers, features in the film. He<br />
is passionate about increasing<br />
awareness of the importance<br />
of bystander CPR and breaking<br />
down anxiousness around using<br />
a public defibrillator.<br />
Fergus said: “We were delighted<br />
to be selected as Digitom’s<br />
Charity of the Year and be given<br />
the opportunity to work with<br />
them to create this awareness<br />
film of what people should do<br />
should they discover someone in<br />
cardiac arrest.<br />
“As a team we teach many<br />
members of the public how to<br />
save a life and it is a skill everyone<br />
should possess and we hope this<br />
film helps others learn and have<br />
the confidence to act.<br />
“In the event of someone not<br />
breathing, it is vital that chest<br />
compressions are commenced<br />
as quickly as possible, someone<br />
calls 999 and, if directed to do so,<br />
collects a defibrillator and follows<br />
the instructions of the 999 call<br />
operator and the machine itself.<br />
“Out-of-hospital cardiac arrests<br />
are a community issue, and<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
26<br />
27<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
anyone could be called upon in<br />
their lives to play a key role in an<br />
attempt to save a person’s life.”<br />
Frankie added: “It was an honour<br />
to be involved in this awareness<br />
video, the message is so<br />
important and something I have<br />
become passionate about in the<br />
last year following my cardiac<br />
arrest. You genuinely never know<br />
when you’ll need to perform CPR,<br />
and this video is great for helping<br />
people understand how straight<br />
forward and vital CPR and the<br />
use of a public defibrillator is.<br />
“The current survival rates of<br />
out-of-hospital cardiac arrests are<br />
shocking, I hope this video gives<br />
people the confidence to help<br />
should they ever be faced with a<br />
similar situation.”<br />
To watch the follow this link:<br />
https://youtu.be/oywaqEXre4c<br />
‘Is going home in one<br />
piece too much to<br />
ask?’ – Paramedic<br />
steps down after<br />
assault<br />
A PARAMEDIC who was<br />
verbally abused and spat at as<br />
she tried to help a patient has<br />
decided to leave her job.<br />
Julie Owen, a Welsh <strong>Ambulance</strong><br />
Service Paramedic in Colwyn<br />
Bay, said the attack by a patient’s<br />
daughter has left her ‘hyper<br />
aware’ of threats.<br />
While Julie has undergone<br />
counselling, she says she is no<br />
longer interested in the job she<br />
once loved.<br />
The 56-year-old said: “I’ve<br />
suffered violence and aggression<br />
of many kinds over my 20-year<br />
career, and I guess this is the last<br />
one I’m prepared to deal with.<br />
“They build up and up, and one<br />
day just become too much.<br />
“I feared for my life that night, and<br />
the impact on me was something<br />
I didn’t expect.<br />
“Is going home in one piece too<br />
much to ask?”<br />
Julie and her colleague Emma<br />
Griffiths, an Emergency Medical<br />
Technician, were responding to<br />
a medical emergency in Shotton<br />
when the patient’s daughter<br />
became aggressive.<br />
Emma, 49, who also has 20 years’<br />
service, said: “We could hear<br />
shouting and screaming before<br />
we’d even entered the property.<br />
“As we tried to treat the patient,<br />
her daughter took exception<br />
to the fact we’d asked her<br />
not to light a cigarette around<br />
the oxygen cylinder, which<br />
is flammable.<br />
“At one point she tried to block<br />
the doorway with her hand, and<br />
when I asked her to move it,<br />
she started shouting about how<br />
useless we were and called me a<br />
fat, blonde bimbo.<br />
“She was jumping up and<br />
down like a lunatic and<br />
was unstoppable.<br />
“I’ve been verbally abused many<br />
times over my career, but this<br />
was my first physical assault.<br />
“It shook me up because we<br />
were there to help.<br />
“Assault should never be part of<br />
the job.”<br />
Julie said: “She was verbally<br />
abusive throughout, and when<br />
we went to get pain relief for her<br />
mum, she became physically<br />
aggressive too.<br />
“She threw glass at us, spat at us<br />
and came right up to our faces<br />
trying to punch us.”<br />
Julie and Emma called for<br />
police back-up and the patient’s<br />
daughter was arrested.<br />
Julie said: “Thank goodness the<br />
police responded so quickly and<br />
came to our aid.<br />
“It’s unacceptable to assault any<br />
emergency worker – they’re there<br />
to help.<br />
“I love my job as a paramedic<br />
but since the incident have lost<br />
interest in it and am hyper aware<br />
of what I could be facing in the<br />
community.<br />
“To that end, I’ve decided to hang<br />
up my boots and secure another<br />
role in the service which means I’ll<br />
have less patient-facing contact.<br />
“It’s a very sad way for me to end<br />
my career as a road paramedic.”<br />
On 29 February <strong>2024</strong> at Mold<br />
Magistrates’ Court, a 33 year old<br />
female was jailed for 20 weeks<br />
having previously admitted<br />
three offences of assaulting an<br />
emergency worker and one of<br />
using threatening or abusive<br />
words or behaviour.<br />
She was also ordered to pay<br />
£50 in compensation to each of<br />
the victims.<br />
To her colleagues in the<br />
ambulance service, Julie had<br />
this message.<br />
“Violence and aggression<br />
should never be part of the job,”<br />
she said.<br />
“Don’t just put up with it because<br />
one day it’ll come back and bite<br />
you, just like it did me.<br />
“Staff should report any form<br />
of violence, even if it’s just a<br />
verbal threat, because if it goes<br />
unreported and no action is<br />
taken, your colleagues could find<br />
themselves in the same situation<br />
days later – or worse.”<br />
Jason Killens, Chief Executive of<br />
the Welsh <strong>Ambulance</strong> Service,<br />
said: “It’s heartbreaking to hear<br />
that Julie, who will have helped<br />
thousands of patients during<br />
her 20-year career, has decided<br />
to step down from her patientfacing<br />
role.<br />
“What’s also frustrating is that<br />
Julie and Emma were there to<br />
help this person’s mother, so to<br />
obstruct them in the course of<br />
that and exhibit such obnoxious<br />
behaviour just beggars belief.<br />
“Violence and aggression<br />
against emergency workers is<br />
unacceptable and we will always<br />
seek prosecution for those that<br />
choose to harm our people.<br />
“<strong>Ambulance</strong> workers are there<br />
to help people, but they can’t<br />
fight for someone’s life if they’re<br />
fighting for their own.”<br />
Wesley Williams, a District<br />
Inspector at North Wales Police,<br />
added: “Every single day,<br />
emergency service workers are<br />
often dealing with challenging<br />
situations and putting themselves<br />
in harm’s way to keep the public<br />
safe and to save lives.<br />
“Being assaulted is not and<br />
should never be regarded as ‘part<br />
of the job’.<br />
“Assault is a traumatic offence that<br />
causes great distress to anyone,<br />
and it is no different when the<br />
victim is an emergency worker.<br />
“It is wholly unacceptable for<br />
them to be threatened, attacked,<br />
verbally abused or spat at – and<br />
those responsible should face the<br />
full force of the law.”<br />
The Welsh <strong>Ambulance</strong> Service<br />
is a member of the NHS Wales<br />
Anti-Violence Collaborative,<br />
which was set up to improve the<br />
reporting of incidents and better<br />
support victims through the<br />
prosecution process.<br />
Jonathan Webb, Chair of the<br />
Collaborative, which includes<br />
NHS Wales, Welsh police forces,<br />
the Crown Prosecution Service,<br />
Welsh Government and staff<br />
support organisations, said:<br />
“Any form of abuse or violence<br />
against emergency workers is<br />
unacceptable.<br />
“The partners of the Anti-Violence<br />
Collaborative are actively working<br />
on initiatives to reduce violence<br />
and aggression encountered<br />
by colleagues.”<br />
The Welsh <strong>Ambulance</strong> Service<br />
is also running a campaign to<br />
reduce the number of assaults on<br />
emergency workers in Wales.<br />
Pledge your support on social<br />
media using the hashtag<br />
#WithUsNotAgainstUs or<br />
#GydaNiNidYnEinHerbyn.<br />
ParOARmedics<br />
Atlantic Challenge<br />
<strong>2024</strong><br />
In December <strong>2024</strong> team<br />
parOARmedics is taking on a<br />
3000 mile unsupported row<br />
across the Atlantic Ocean.<br />
The team, comprised of newly<br />
qualified Yorkshire paramedics<br />
Ethan Chapman, Tom Dowdy,<br />
and Ken Bordt are hoping to<br />
raise awareness and money<br />
for three incredible charities:<br />
The <strong>Ambulance</strong> Staff Charity<br />
(TASC), MacMillan Cancer<br />
and The Stroke Association,<br />
highlighting the incredible work<br />
they do in the community and<br />
supporting staffing to continue<br />
to allow these charities to<br />
support local communities<br />
and ambulance staff on a<br />
daily basis.<br />
The team will set off from La<br />
Gomera (Canary Islands) and<br />
finish in English Harbour, Antigua.<br />
This gruelling challenge dubbed<br />
“The Worlds toughest Row”<br />
will see the team battle various<br />
mental and physical challenges<br />
during this arduous crossing<br />
that could see the team rowing<br />
continuously for up to 40 days.<br />
The team will have to battle<br />
through sleep deprivation, 25 ft<br />
waves, whilst rowing 3hrs on and<br />
3hrs off maintaining a watch night<br />
and day for passing cargo ships,<br />
rogue waves that could capsize<br />
them and random marlin strikes.<br />
The team will also have to carry<br />
all their equipment and provisions<br />
for the entire journey as they are<br />
not allowed any reprovisioning<br />
along the way, a mighty task<br />
as the gents will be consuming<br />
between 5500 and 6500 calories<br />
daily to maintain the energy<br />
levels required to row up to 12<br />
hours daily.<br />
The team have now completed<br />
all their mandatory classroom<br />
training covering topics such as<br />
essential seamanship, navigation<br />
and sea survival training. Their<br />
sights are now set firmly on<br />
completing the required open<br />
water rowing hours and over the<br />
next few months their focus will be<br />
taking to open water to row, row,<br />
row and then row some more.<br />
They will be practicing various<br />
drills from cooking on board,<br />
navigating, radio communications<br />
and maintaining the ship to vital<br />
skills such as deploying their paraanchor,<br />
man overboard drills and<br />
other potentially life saving skills<br />
in order to ensure an efficient and<br />
safe as crossing come December.<br />
Alongside this physical<br />
preparation, the team are<br />
continuing to fundraise for the<br />
campaign and are always on<br />
the lookout for any individuals<br />
or companies that would like<br />
to help them to get to the start<br />
line and be part of this amazing<br />
campaign. The team have various<br />
sponsorship and support options<br />
available for all levels of support<br />
and they are keen to hear from<br />
anyone who would like to be<br />
part of their campaign to discuss<br />
how we can work together on<br />
this amazing project. The team<br />
have a website dedicated to the<br />
challenge as well as an active<br />
presence on social media where<br />
you can follow their preparations<br />
leading up to the race and<br />
eventually follow their progress<br />
across the Atlantic during the<br />
actual race.<br />
To find out more, support the<br />
team or get in touch, follow<br />
them on SM and check out<br />
their website.<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
28<br />
29<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
IN PERSON<br />
COMPANY NEWS<br />
oversaw the merger of the college with the<br />
then University of Glamorgan.<br />
He was also Director of Finance and<br />
Corporate Services at Sport Wales, Director<br />
of Finance at Aberystwyth University and<br />
Assistant Director of Finance at Cardiff<br />
Metropolitan University.<br />
(Health and Social Care), focusing on<br />
managing a range of key relationships related<br />
to the health and social care portfolio.<br />
Since 2019, he has been acting as Nominated<br />
Advisor to Welsh Government for Respiratory<br />
Innovation Wales.<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
30<br />
Welsh <strong>Ambulance</strong> Service<br />
appoints new Non-Executive<br />
Directors<br />
THE Welsh <strong>Ambulance</strong> Service has<br />
appointed two new Non-Executive<br />
Directors to its Board.<br />
Welsh Government’s Minister for Health and<br />
Social Services has appointed Peter Curran<br />
as a Non-Executive Director (Finance) and<br />
Ian Mathieson as a Non-Executive Director<br />
(Academic).<br />
Peter began his four-year term on 01<br />
February, while Ian will take up post on<br />
01 <strong>April</strong>.<br />
Colin Dennis, the Chair of the Welsh<br />
<strong>Ambulance</strong> Service, said: “Congratulations<br />
to Peter and Ian on their respective<br />
appointments.<br />
“Overseeing the work of the only all-Wales<br />
emergency service comes with a unique set<br />
of challenges, but Peter and Ian come with a<br />
wealth of experience and expertise to help us<br />
navigate these.<br />
“I speak for the whole Board when I say we<br />
are looking forward to working with Peter and<br />
Ian to realise our strategic ambitions.”<br />
Peter Curran is a Fellow of the Chartered<br />
Institute of Public Finance and Accountancy,<br />
with an Economics degree from<br />
Aberystwyth University.<br />
He has acted as a Chief Finance Officer for<br />
more than 20 years in a number of sectors.<br />
He was the Vice Principal (Resources) at the<br />
Royal Welsh College of Music and Drama,<br />
where he led the development of awardwinning<br />
new performance spaces and<br />
Peter holds a number of non-executive roles,<br />
including at Taff Housing Association, and is<br />
Trustee at Action for Children and National<br />
Youth Arts Wales.<br />
He is also an independent member of Y Coleg<br />
Cymraeg Cenedlaethol’s Audit and Risk<br />
Committee and an Honorary Fellow of the<br />
Royal Welsh College of Music and Drama.<br />
Peter took semi-retirement in July 2023,<br />
having previously served as the Chief Finance<br />
Officer for the Office of the South Wales<br />
Police and Crime Commissioner for five years.<br />
He said: “It is a privilege to be appointed to<br />
the Board of Welsh <strong>Ambulance</strong> Service.<br />
“Whilst there are undoubtedly challenges<br />
ahead, I am looking forward to applying<br />
my experience to add value to the Trust’s<br />
activities and help it achieve its strategic<br />
objectives in what is a critical public service<br />
in Wales.”<br />
Meanwhile, Ian Mathieson trained as a<br />
podiatrist in Edinburgh and was appointed to<br />
his first academic post at Cardiff Metropolitan<br />
University in 1996.<br />
He undertook a PhD focusing on lower<br />
limb biomechanics, and helped to develop<br />
various Master’s courses, including in<br />
advanced practice.<br />
Ian became Director of Learning and Teaching<br />
and Deputy Dean for Health Sciences at<br />
Cardiff Metropolitan University in 2013,<br />
assuming responsibility for a wide range<br />
of disciplines.<br />
He moved to the University of South Wales in<br />
2020 and helped the Faculty of Life Sciences<br />
and Education extend its health portfolio to<br />
include physiotherapy, occupational therapy<br />
and operating department practice.<br />
In 2022, he became Associate Dean,<br />
Partnerships and Business Development<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
And since 2020, he has been Convenor of the<br />
Council of Deans of Health Wales.<br />
Ian said: “I am delighted to have this<br />
opportunity to serve on WAST’s Board and<br />
to support it to realise its ambitious but<br />
achievable strategic plans.<br />
“WAST is making a central contribution to the<br />
transformation of the way our health and care<br />
services are delivered and I look forward to<br />
being a part of its ongoing work.”<br />
The Trust’s Board is comprised of a Chair,<br />
Vice Chair, six Non-Executive Directors, the<br />
Chief Executive and five Executive Directors.<br />
A further four Directors and two Trade Union<br />
partners also attend the Board.<br />
The tenure of current Non-Executive Director<br />
(Finance) Martin Turner will draw to a close as<br />
Peter takes up post next month.<br />
Meanwhile, the term of current Non-Executive<br />
Director (Academic) Paul Hollard will end as<br />
Ian takes up post in <strong>April</strong>.<br />
Colin said: “We are extremely lucky to have<br />
secured the services of Paul and Martin.<br />
“Paul joined the Board in 2016 and Martin<br />
in 2018.<br />
“Both have chaired Committees of the Board,<br />
including latterly the People and Culture<br />
Committee and Audit Committee respectively,<br />
and have made sterling contributions to the<br />
Board over the recent years, including through<br />
the most difficult period in our history – the<br />
Covid-19 pandemic.<br />
“While Paul will remain with us for a little while<br />
longer, we would like to wish both of them all<br />
the very best for the future and thank them for<br />
their support and service.”<br />
CO-LOCATED WITH<br />
THE HOME OF<br />
TECHNOLOGY<br />
INNOVATION FOR<br />
THE EMERGENCY<br />
SERVICES<br />
Register for your FREE pass<br />
www.emergencytechshow.com<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
150+<br />
EXHIBITORS<br />
8,000+<br />
VISITORS<br />
10,000+<br />
PRODUCTS AND SOLUTIONS<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
CPD<br />
ACCREDITED CONTENT<br />
31
Seamless Synchronisation<br />
Hands Free Resuscitation with the<br />
corpuls3 and corpulscpr.<br />
In the <strong>Ambulance</strong><br />
Emergency transport carries risk<br />
for the patient and the responding<br />
team. With synchronised therapy,<br />
the emergency team can remain<br />
seated whilst in transit. Rhythm<br />
control and shock delivery can be<br />
performed on the corpuls 3 while<br />
the medic is seated.<br />
In Tight Spaces<br />
Whether in a lift, a stairwell, or<br />
on tricky terrain, synchronised<br />
resuscitation means that therapy<br />
can continue where it wouldn’t<br />
have been possible before. Once<br />
in place, a medic can control the<br />
corpuls 3 monitor, defibrillator and<br />
CPR parameters of the corpuls cpr.<br />
In the Air<br />
Patient access is extremely limited<br />
in air rescue. Thanks to the perfect<br />
interaction of the corpuls 3 with<br />
the corpuls cpr, movement within<br />
the cabin is reduced. Synchronised<br />
mechanical chest compressions<br />
can be given, without having to<br />
accept long hands-off times.<br />
• Shorter hands-off time<br />
• Automated pre-shock compressions<br />
• Can be used in manual and AED mode<br />
• Increased safety & minimised interruptions<br />
• Less resources required<br />
• Easier operation<br />
• Data transmission<br />
• Post mission analysis<br />
Learn more:<br />
Scan the QR code<br />
with your phone<br />
camera and click<br />
the link.<br />
Or visit:<br />
uqr.to/sync-cpr<br />
www.theortusgroup.com