Ambulance UK October 2023
Ambulance UK October 2023
Ambulance UK October 2023
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
Volume 39 No. 5<br />
<strong>October</strong> <strong>2023</strong><br />
DEDICATED TO THE AMBULANCE SERVICE AND ITS SUPPLIERS<br />
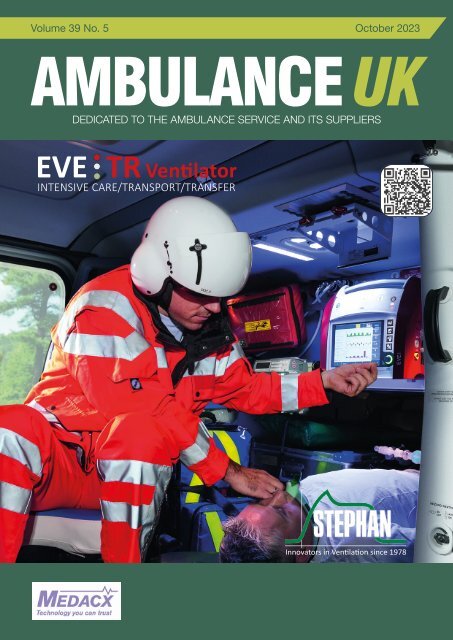
EVE TR Ventilator<br />
INTENSIVE CARE/TRANSPORT/TRANSFER<br />
Innovators in Ventilation since 1978
NEWSLINE<br />
AMBULANCE <strong>UK</strong> - JUNE<br />
82<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For further information visit http://www.synergybusinesssolutions.co.uk
CONTENTS<br />
CONTENTS<br />
<strong>Ambulance</strong> <strong>UK</strong><br />
4 EDITOR’S COMMENT<br />
7 FEATURE<br />
7 FACTORS INFLUENCING ON-SCENE TIME IN A<br />
PHYSICIAN-STAFFED HELICOPTER EMERGENCY<br />
MEDICAL SERVICE (HEMS): A RETROSPECTIVE<br />
OBSERVATIONAL STUDY<br />
18 NEWSLINE<br />
31 IN PERSON<br />
This issue edited by:<br />
Matt House<br />
c/o Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
ADVERTISING:<br />
Terry Gardner, Samantha Marsh<br />
CIRCULATION:<br />
Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
Tel: 01886 853715<br />
E: info@mediapublishingcompany.com<br />
www.ambulanceukonline.com<br />
PUBLISHED BI-MONTHLY:<br />
February, April, June, August,<br />
<strong>October</strong>, December<br />
COVER STORY<br />
Stephan EVE Ventilators bring intensive care ventilation performance to pre-hospital<br />
transport and transfers.<br />
EVE Ventilators are fully independent of mains power or dependence on compressed air.<br />
With inbuilt air-turbine, 8-hour battery use plus ‘hot-swappable 4-hour battery packs for<br />
extended use, lightweight, compact, designed for hospital, intra-hospital transport and<br />
pre-hospital transport. With various ventilator brackets and mounts to support use within<br />
road ambulances, medical helicopter, and medical aircraft.<br />
In an emergency when every second counts; Stephan EVE Ventilators have FAST<br />
‘Safe-Start’ buttons ensuring pre-programmed patient readiness to ventilate at the push<br />
of a button to rapidly deploy safe and optimum ventilation for Neonates, Infants or Paed/<br />
Adults. The pre-use safety checks from power on are completed in 70 seconds; without<br />
the need for any human interaction, the self-test also checks the attached patient circuit<br />
for compliance in use.<br />
COPYRIGHT:<br />
Media Publishing Company<br />
Greenoaks<br />
Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company<br />
Next Issue December <strong>2023</strong><br />
Designed in the <strong>UK</strong> by TGDH<br />
Stephan EVE Ventilators inbuilt air turbine delivers patient ventilation support<br />
without any compromise from tidal volumes of 2ml to 2000ml. Offering both Invasive<br />
and Non-Invasive ventilation [Pressure and Volume modes], 21-100% electronic oxygen<br />
mixing, in addition Low-Flow and High-Flow Oxygen therapy and delivery modes. The<br />
8.4-inch full-colour touchscreen provides a user friendly, tactile user interface supporting<br />
ease of use and intuitive navigation. In addition, there are trend displays/loops and user<br />
configurable displays to personalise operational use. Integrated sensor options are<br />
available for waveform capnography and pulse oximetry.<br />
Manufactured in Germany and Supported throughout the<br />
<strong>UK</strong> by MEDACX Limited a Fritz Stephan GbmH approved<br />
supply and support partner organisation.<br />
Do you have For anything further recruitment you would vacancies like to add visit: or include? www.ambulanceukonline.com<br />
Please contact us and let us know.<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
3
EDITOR’S COMMENT<br />
EDITOR’S COMMENT<br />
Welcome to this issue of A<strong>UK</strong>.<br />
AMBULANCE <strong>UK</strong> <strong>UK</strong> – - OCTOBER JUNE<br />
68<br />
4<br />
“But it isn’t just<br />
about flu or<br />
“The Covid pay anymore, rises<br />
implemented<br />
the weirdly<br />
hot weather<br />
hardly over Summer fi t<br />
the has bill, lead and to<br />
a tripling of<br />
I fear there<br />
pollen induced<br />
is respiratory a real<br />
danger<br />
demand<br />
that<br />
for<br />
many services<br />
recruitment<br />
as well as the<br />
and direct retention effects<br />
of the high<br />
in the NHS<br />
temperatures<br />
will as be well.”<br />
adversely<br />
affected.”<br />
All Well, too I’m quickly offi cially summer retired seems and just to have to indulge given way myself to winter a little, with I’m going Storm to Agnes begin causing by considering havoc as how I write the this<br />
piece. ambulance It always service amuses has evolved me to see since Christmas I started baubles some 35 go years on sale ago. earlier Does and anyone earlier remember in the year the but arrival then I of<br />
began defi brillators think on about the ambulance? the way the At pressures the time on a revolution, the NHS are complete also building with a sooner walkman with recorder seasonal to vaccination ensure<br />
programmes that you used commencing it absolutely in by summer rote. Consider rather than that late now autumn we are in delivering presumably them an remotely attempt by to thwart drone and or mitigate the<br />
that progress particular can easily respiratory be seen. illness The issue. Paramedic But it isn’t syllabus just about was contained flu or covid in anymore a little red the book, weirdly now hot there weather are so<br />
over many summer more skills has and lead knowledge to a tripling requirements of pollen induced no-one respiratory goes on demand duty without for many JRCALC services on their as well smart as the phone.<br />
direct There effects were few of the medicines, high temperatures pain relief was well. limited I wouldn’t to entonox necessarily and the count most myself diffi cult as skill a climate was strapping change<br />
sceptic someone but into it isn’t a Neil something Robertson, I’ve now ever paramedics spent time thinking regularly about administer detail, advanced I recycle drugs and drive and a perform full electric life<br />
car saving but surgical the global interventions. weather related I’m proud catastrophes to have of been this on year that do journey make you and stop continue and think. to follow And with in that interest pause the<br />
for changes thought to comes come. another consideration, a move to full electric ambulances and how that might impact the<br />
NHS, amongst the obvious challenges of cost and infrastructure. Whilst most of the <strong>UK</strong>’s ambulance Trusts<br />
are Summer trialling is some apparently form of here, EV, well there as is near currently as we no get way in of Lancashire, escaping the I’m additional guessing most time in of resource you are looking hours that<br />
comes forward with to holidays the need and for time recharging, with family which or may friends. not It be can as be much a great of a problem time but for at the urban same services time stressful but almost with<br />
certainly the price will increases be for rural we have services seen with across longer all aspects journeys. of I’m life. not The sure pay what rises the implemented answer to the hardly conundrum fi t the bill, is and<br />
but I fear I do there believe is a real it lies danger somewhere that recruitment within the increase and retention in telemedicine in the NHS and will reduced be adversely allocations. affected. This I wonder year’s<br />
emergency how many of services todays show Paramedic clearly cohort demonstrated will be around the rising for interest the next in 30 technology, years. Given AI and the high robotics demands, as potential both<br />
solutions practical and mental, as demonstrated I suspect already that many in the will private move on sector, different AI in particular pastures could and that have there a significant will be far role fewer in<br />
more retiring accurately in the future, targeting especially resource. since Imagine, the current as a NHS 999 retirement call is received age continues the patients to medical increase. history Maybe, is being like<br />
simultaneously many of my peers, interrogated I have seen with the information golden age gathered of ambulance helping predict service. the likely Whatever severity the of future the presentation brings, I hope<br />
and the summer automatically will deliver diverting you the all a incident well earned to the break. most appropriate As for me, I’m resource, looking then for a learning job… from the outcome,<br />
consistently 24/7/365… A stretch of the imagination? We speak to computers that sound like humans all the<br />
time, they don’t tire or need breaks, how long will it be before NHS111 goes fully digital I wonder? Hopefully<br />
no Sam time English, soon as Co-Editor I don’t believe <strong>Ambulance</strong> you could <strong>UK</strong> ever teach a computer to care but it does make you think…<br />
Sam English, Co-Editor <strong>Ambulance</strong> <strong>UK</strong><br />
Publishers Publishers Statement<br />
For<br />
For<br />
nearly<br />
nearly<br />
40<br />
40<br />
years,<br />
years, thanks<br />
thanks<br />
to<br />
to<br />
trade<br />
trade<br />
support,<br />
support,<br />
we<br />
we<br />
have<br />
have<br />
been<br />
been<br />
able<br />
able<br />
to<br />
to<br />
provide<br />
provide<br />
<strong>Ambulance</strong><br />
<strong>Ambulance</strong><br />
<strong>UK</strong><br />
<strong>UK</strong><br />
FREE<br />
FREE OF<br />
CHARGE OF CHARGE in the in knowledge the knowledge that that those those receiving receiving our our dedicated dedicated bi bi monthly monthly publication enjoy enjoy having<br />
something to read during their free time however, return on on investment seems to to be be the the buzz buzz word word<br />
amongst <strong>Ambulance</strong> Service Suppliers these days, days, therefore therefore if you if you enquire enquire about about a product a product advertised, advertised,<br />
please mention <strong>Ambulance</strong> <strong>UK</strong> as it help us confirm to the trade that we are reaching the right<br />
please mention <strong>Ambulance</strong> <strong>UK</strong> as it will help us confi rm to the trade that we are reaching the right<br />
people and providing advertisers with value for money. In respect of our current edition we would<br />
people<br />
like to thank<br />
and providing<br />
the following<br />
advertisers<br />
companies<br />
with<br />
for<br />
value<br />
their<br />
for<br />
support<br />
money.<br />
as<br />
In<br />
without<br />
respect<br />
their<br />
of our<br />
contribution<br />
current edition<br />
towards<br />
we<br />
our<br />
would<br />
print<br />
like<br />
to and thank postal the costs following this issue companies would not for their have support been published as without - Alpha their Laboratories, contribution towards Bluelight our <strong>UK</strong>, print and<br />
postal DS Medical, costs this Eberspaecher, issue would not Ferno have <strong>UK</strong>, been Frontier published Medical, - Bluelight IPRS, <strong>UK</strong>, Medacx, DS Medical, Ortus, St Eberspaecher,<br />
John WA,<br />
EVS, Synergy Ferno, Business Galen, Solutions. Intersurgical, Ortus Medical, Synergy, VCS, Vimpex, Webasto.<br />
Terry Gardner<br />
Terry Publisher Gardner<br />
Publisher<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
For more news visit: www.ambulanceukonline.com
EVE TR Ventilator<br />
INTENSIVE CARE/TRANSPORT/TRANSFER<br />
Innovators in Ventilation since 1978<br />
Technology made in Germany<br />
Supported in the United Kingdom<br />
EVE-TR innovative transport respiratory system for Neonates, Paediatrics & Adults<br />
Invasive & Non-Invasive ventilation Pressure & Volume modes including SIMV, CMV<br />
DuoPAP, NIV, CPAP/nCPAP & ACV. Electronic Oxygen mixing 21-100%, HiFlow 02 2-60 Lpm<br />
Inbuilt Air turbine, 8 hour continuous use plus ‘hot swap battery packs’ to extend use<br />
Independant of air/power. Integral bed/trolley clamps. Compact, Lightweight<br />
with...Fast ‘safe-start’ ventilation at the press of a button<br />
MEDACX LIMITED • ALEXANDER HOUSE • 60-62 STATION ROAD • HAYLING ISLAND • HAMPSHIRE • PO11 0EL<br />
FS 580431<br />
02392 469737<br />
info@medacx.co.uk<br />
www.medacx.co.uk
MAKE A<br />
LEGENDARY<br />
MOVE<br />
Every day is different as a St John WA paramedic, and we have multiple<br />
opportunities available for qualified and experienced <strong>Ambulance</strong> Paramedics<br />
to come join us in beautiful Western Australia.<br />
The offer:<br />
• Visa application support<br />
• Paid for one-way economy airline ticket<br />
• Accommodation upon arrival to<br />
Western Australia<br />
• Additional relocation costs covered<br />
The location:<br />
• Diverse landscape means diverse daily routine<br />
• Safe and stable economy<br />
• Over two-thirds of the year is beautifully clear<br />
and sunny<br />
• Incredible work/life balance with world-class<br />
dining, festivals and more<br />
Don’t have current Australian<br />
working rights? No problem!<br />
For candidates to successfully be employed as<br />
an <strong>Ambulance</strong> Paramedic, they must meet the<br />
following minimum requirements:<br />
• Professional registration as a Paramedic with<br />
the Paramedicine Board of Australia (AHPRA)<br />
or willingness to obtain.<br />
• Recent experience employed and working<br />
within a jurisdictional ambulance service in<br />
Australia or internationally (St John New<br />
Zealand or London <strong>Ambulance</strong> Service for<br />
example) as a paramedic for at least two years.<br />
• Hold a full driver’s license with no restrictions.<br />
Successful candidates are required to obtain<br />
a light rigid driver’s license within the first six<br />
months of employment. Costs associated with<br />
obtaining the required driver’s license are the<br />
responsibility of the candidate.<br />
• Candidates that do not hold current Australian<br />
working rights, must meet the visa eligibility<br />
requirements, as outlined by the Department<br />
of Home Affairs.<br />
Ready to make a<br />
legendary move?<br />
Go on, a career with loads of diversity<br />
and an amazing lifestyle is waiting!<br />
Search stjohnwa.com.au/directentry<br />
Scan to learn more:
FEATURE<br />
FACTORS INFLUENCING ON-SCENE TIME<br />
IN A PHYSICIAN-STAFFED HELICOPTER<br />
EMERGENCY MEDICAL SERVICE (HEMS):<br />
A RETROSPECTIVE OBSERVATIONAL<br />
STUDY<br />
Alexander Fuchs 1,2*† , Markus Huber 1† , Thomas Riva 1 , Stefan Becker 2 , Roland Albrecht 2,3 , Robert Greif 4,5,6 and<br />
Urs Pietsch 2,3,7<br />
Scand J Trauma Resusc Emerg Med (<strong>2023</strong>) 31:20 https://doi.org/10.1186/s13049-023-01085-x<br />
ORIGINAL RESEARCH<br />
Abstract<br />
Keywords: Helicopter emergency medical system, Prehospital onscene<br />
time, Trauma, Helicopter hoist operation, Airway management,<br />
Resuscitation, Paediatric<br />
Background: For helicopter emergency service systems (HEMS),<br />
the prehospital time consists of response time, on-scene time and<br />
transport time. Little is known about the factors that influence on-scene<br />
time or about differences between adult and paediatric missions in a<br />
physician-staffed HEMS.<br />
Methods: We analysed the HEMS electronic database of Swiss Air-<br />
Rescue from 01-01-2011 to 31-12-2021 (N = 110,331). We included<br />
primary missions and excluded missions with National Advisory<br />
Committee for Aeronautics score (NACA) score 0 or 7, resulting in<br />
68,333 missions for analysis. The primary endpoint ‘on-scene time’<br />
was defined as first physical contact with the patient until take-off to<br />
the hospital. A multivariable linear regression model was computed to<br />
examine the association of diagnosis, type and number of interventions<br />
and monitoring, and patient’s characteristics with the primary endpoint.<br />
Results: The prehospital time and on-scene time of the missions<br />
studied were, respectively, 50.6 [IQR: 41.0–62.0] minutes and 21.0<br />
[IQR: 15.0–28.6] minutes. Helicopter hoist operations, resuscitation,<br />
airway management, critical interventions, remote location, night-time,<br />
and paediatric patients were associated with longer on-scene times.<br />
Conclusion: Compared to adult patients, the adjusted on-scene<br />
time for paediatric patients was longer. Besides the strong impact of<br />
a helicopter hoist operation on on-scene time, the dominant factors<br />
contributing to on-scene time are the type and number of interventions<br />
and monitoring: improving individual interventions or performing them in<br />
parallel may offer great potential for reducing on-scene time. However,<br />
multiple clinical interventions and monitoring interact and are not single<br />
interventions. Compared to the impact of interventions, non-modifiable<br />
factors, such as NACA score, type of diagnosis and age, make only a<br />
minor contribution to overall on-scene time.<br />
Introduction<br />
†Alexander Fuchs and Markus Huber have contributed equally and share the first authorship<br />
Critically ill or injured patients require a rapid assessment and stateof-the-art<br />
medical treatment [1]. Furthermore, safe and fast transport<br />
to an appropriate hospital is necessary to prevent the patient from<br />
undergoing an avoidable secondary inter-hospital transfer that<br />
consumes more time [2, 3]. In Switzerland, the emergency medical<br />
system consists of paramedic-staffed ground ambulances and the<br />
emergency, physician-staffed Helicopter Emergency Medical Services<br />
(HEMS). HEMS patient transport is considered safe, ensures short<br />
intervention times and offers access to difficult and remote regions [4–<br />
6]. On-scene HEMS physicians diagnose patient illnesses or conditions<br />
earlier and perform or initiate advanced life-saving critical interventions,<br />
which improve the survival rates of trauma patients [6, 7].<br />
Current international treatment guidelines for critical illnesses or injuries<br />
focus on the first critical hour. However, the association between<br />
prehospital time and survival is unclear [8]. Prehospital time consists<br />
of three parts: (1) the response time, including the flight time from the<br />
base to the patient; (2) the on-scene time; and (3) the time needed<br />
to transport the patient to the hospital. Prolonged on-scene time is<br />
associated with increased in-hospital mortality in trauma patients [9,<br />
10]. By contrast, HEMS transport is an independent factor for improved<br />
survival in paediatric and adult trauma patients [11–13]. Commencing<br />
definitive treatment more rapidly contributes to improved survival,<br />
including for non-trauma patients, especially in stroke, myocardial<br />
infarction, cardiac arrest and sepsis [14–16].<br />
The factors contributing to a mission’s prehospital time in a physicianstaffed<br />
HEMS are unclear. Flight times depend not only on the distance<br />
from the base to the scene and the destination hospital, but also on<br />
the topography and weather conditions. As regards flight safety, these<br />
variables are unchangeable. Thus, we aimed to investigate factors<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
7
FEATURE<br />
Table 1 Intervention and monitoring performed by the helicopter emergency medical system crew listed by sub-units<br />
Basic interventions<br />
and monitoring<br />
Immobilisation and<br />
analgesia<br />
Critical interventions Airway management Resuscitation Other<br />
Intravenous (i.v.) access Vacuum mattress Intraosseous (i.o.) access Tracheal intubation Chest compressions Cervical collar<br />
Peripheral oxygen Sedation Emergency front of<br />
saturation (SpO2 ) neck access (eFONA)<br />
Electrocardiogram<br />
(ECG)<br />
Temperature<br />
Analgesia<br />
Reduction of a fracture<br />
or dislocation<br />
Chest needle decompression<br />
Facemask ventilation Defibrillation Vacuum splinting<br />
Neuromuscular block -<br />
ing agent (NMBA)<br />
Mechanical chest<br />
compression device<br />
Active rewarming (hot<br />
pads)<br />
Transcutaneous paceing Capnography Invasive or non-invasive<br />
blood pressure<br />
Haemostasis Vasopressors Medication (Antiepileptic,<br />
Antiemetic, Tranexam<br />
acid, Antiarrhythmic,<br />
Antihypertensive, etc.)<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
that contribute to extending on-scene time. Furthermore, we were<br />
interested in the differences between paediatric and adult patients.<br />
Methods<br />
Study design and population<br />
The study protocol of this retrospective observational cohort study<br />
was approved by the Ethics Committee of Eastern Switzerland (EKOS<br />
22/021, St. Gallen, Switzerland), which waived the need for informed<br />
consent due to the retrospective study design and anonymised data<br />
analysis. The study was performed in line with the Declaration of<br />
Helsinki and the Swiss Act on Human Research. We followed the<br />
guidelines on Strengthening the Reporting of Observational Studies in<br />
Epidemiology (STROBE) [17].<br />
Setting<br />
Swiss Air-Rescue (Rega) provides 24/7 physician-staffed HEMS<br />
services with 20 helicopters at 14 bases covering an area of more<br />
than 41,000 km2. The bases are distributed throughout the country,<br />
making it possible to reach any location within an average of 15 min<br />
after an alert is received. Swiss Air-Rescue operates a national dispatch<br />
and mission-control centre for HEMS operations and, independently<br />
of the government and hospitals, conducts around 14,000 HEMS<br />
missions annually. An HEMS crew consists of a pilot, a paramedic<br />
and a physician. Swiss Air-Rescue’s HEMS physicians require<br />
board certification in anaesthesiology and certification in prehospital<br />
emergency medicine.<br />
Data collection<br />
We retrospectively screened the Swiss Air-Rescue HEMS electronic<br />
medical record database from 01-01-2011 to 31-12-2021 and included<br />
all primary HEMS missions. We excluded secondary missions,<br />
missions with National Advisory Committee on Aeronautics (NACA)<br />
score 0 and 7 (uninjured or dead patients) and missions lasting longer<br />
than 24 h (search and rescue missions). Patients under the age of 16<br />
years were classified as paediatric, all others as adults. On-scene time,<br />
the primary endpoint, was defined as the landing time of the helicopter<br />
as a surrogate for the first physical contact between the crew and the<br />
patient until the beginning of the transport phase to the hospital with<br />
the lift-off of the helicopter. Secondary endpoints were: prehospital<br />
time, trauma vs. non-trauma and interventions or measurements<br />
influencing on-scene time.<br />
Measurements<br />
The anonymised data was transferred from Swiss Air-Rescue’s<br />
electronic medical records into a dedicated research database. Patient<br />
and mission characteristics included age, sex, location (urban vs.<br />
remote), time of day and type of activity (e.g. traffic, sport, outdoor<br />
activity). The patients’ location was defined as urban when access by<br />
road was given; otherwise remote. The medical data included the NACA<br />
score, Glasgow Coma Scale (GCS), and helicopter hoist operation.<br />
Diagnoses were coded according to the 2019 World Health Organisation<br />
International Classification of Diseases (ICD-10) and grouped into trauma<br />
and non-trauma [18]. Performance of medical interventions or monitoring<br />
by the HEMS crew are listed in Table 1 and were grouped into clinically<br />
meaningful sub-units for the multivariable model.<br />
For pragmatic medical reasons—and deviating from the formal<br />
definition of night flights—daytime missions were defined as those<br />
occurring between 07:00 and 19:00, while night time flights between<br />
19:01 and 06:59. Mission times were defined as follows:<br />
• On-scene time: from first physical contact with the patient until<br />
beginning of the flight to the destination hospital.<br />
• Prehospital time: from the alerting of Swiss Air-Rescue’s national<br />
HEMS dispatch and mission-control centre until arrival at the<br />
destination hospital.<br />
Statistical analysis<br />
In terms of summary measures, categorical variables were<br />
summarised using counts and percentages, while numerical variables<br />
were summarised using the median and interquartile range (IQR).<br />
Data availability is shown for each variable in the corresponding<br />
tables. We used chi-squared or exact Fisher test for unadjusted group<br />
comparisons between child and adult patients of categorical variables,<br />
and unpaired two-sample Wilcoxon test for numerical variables.<br />
For the multivariable linear regression model with the outcome ‘onscene<br />
time’, we included all patients with available measurements and<br />
a diagnosis, but excluded missions with pre-hospital times greater than<br />
24 h. Model fit was evaluated by means of the adjusted R2. The effect<br />
of each variable on the outcome ‘on-scene time’ is illustrated by<br />
estimated marginal means. Separate multivariable linear regression<br />
models were computed for the child and adult sub-groups.<br />
8<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
Figure 1. Study flowchart<br />
Due to the observational character of the study, no formal sample-size<br />
calculation was performed. Statistical analysis was performed using R<br />
[19]. Two-sided P-values are considered here and a P-value < 0.05 was<br />
considered significant.<br />
Results<br />
We screened 110,331 missions, of which 68,333 were used in the final<br />
analysis. Figure 1 shows the study flow chart.<br />
Patients and mission characteristics are summarised in Table 2.<br />
The median age was 50.0 [IQR: 27.0–65.0] years and most patients<br />
were adults (87.1%) and male (64.4%). The majority (52.4%) of all<br />
patients presented NACA scores between IV and VI. Overall, 11.0%<br />
of missions required a helicopter hoist operation (HHO), and the<br />
majority of missions took place during the daytime (86.1%). Across all<br />
included missions, prehospital time and on-scene time were 50.6 [IQR:<br />
41.0;62.0] minutes and 21.0 [15.0;28.6] minutes, respectively.<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
9
FEATURE<br />
Table 2 Baseline characteristics of all patients adjusted to age. Data are given in n (%) or median [Q1;Q3]<br />
All patients Children<br />
Adults<br />
(<<br />
(≥<br />
N = 68,333 N = 8,803 N = 59,530<br />
p<br />
N<br />
Age (years) 50.0 [27.0;65.0] 10.0 [5.00;13.0] 54.0 [36.0;68.0] 0.000 68,333<br />
Sex: < 0.001 68,333<br />
Female 24,317 (35.6%) 3,628 (41.2%) 20,689 (34.8%)<br />
Male 44,010 (64.4%) 5,174 (58.8%) 38,836 (65.2%)<br />
Other 6 (0.01%) 1 (0.01%) 5 (0.01%)<br />
National Advisory Committee for<br />
< 0.001 68,333<br />
Aeronautics (NACA) score:<br />
NACA I–III 32,496 (47.6%) 5,396 (61.3%) 27,100 (45.5%)<br />
NACA IV–VI 35,837 (52.4%) 3,407 (38.7%) 32,430 (54.5%)<br />
Glasgow Coma Scale (GCS): < 0.001 64,918<br />
3 5,106 (7.87%) 307 (3.64%) 4,799 (8.49%)<br />
4 335 (0.52%) 27 (0.32%) 308 (0.55%)<br />
5 318 (0.49%) 34 (0.40%) 284 (0.50%)<br />
6 558 (0.86%) 72 (0.85%) 486 (0.86%)<br />
7 523 (0.81%) 66 (0.78%) 457 (0.81%)<br />
8 519 (0.80%) 76 (0.90%) 443 (0.78%)<br />
9 505 (0.78%) 97 (1.15%) 408 (0.72%)<br />
10 780 (1.20%) 124 (1.47%) 656 (1.16%)<br />
11 869 (1.34%) 122 (1.45%) 747 (1.32%)<br />
12 938 (1.44%) 132 (1.57%) 806 (1.43%)<br />
13 1,892 (2.91%) 262 (3.11%) 1,630 (2.89%)<br />
14 6,238 (9.61%) 737 (8.75%) 5501 (9.74%)<br />
15 46,337 (71.4%) 6,369 (75.6%) 39,968 (70.7%)<br />
Location < 0.001 62,158<br />
Urban 32,283 (51.9%) 3,789 (46.4%) 28,494 (52.8%)<br />
Remote 29,875 (48.1%) 4,381 (53.6%) 25,494 (47.2%)<br />
Helicopter hoist operation (HHO): < 0.001 68,333<br />
No 60,785 (89.0%) 8,527 (96.9%) 52,258 (87.8%)<br />
Yes 7,548 (11.0%) 276 (3.14%) 7,272 (12.2%)<br />
Activity: < 0.001 63,943<br />
Traffic 9,301 (14.5%) 821 (9.5%) 8,480 (15.3%)<br />
Sport (Summer) 4,204 (6.6%) 399 (4.6%) 3,805 (6.9%)<br />
Sport Mountains (Summer) 5,727 (9.0%) 317 (3.7%) 5,410 (9.8%)<br />
Sport (Winter) 16,970 (26.5%) 3,977 (45.8%) 12,993 (23.5%)<br />
Sport Mountains (Winter) 1,197 (1.9%) 13 (0.15%) 1,184 (2.14%)<br />
Water Sports 579 (0.9%) 113 (1.30%) 466 (0.84%)<br />
Other 25,965 (40.6%) 3,046 (35.1%) 22,919 (41.5%)<br />
Time of day: < 0.001 68,333<br />
Daytime (07:00–19:00) 58,842 (86.1%) 7,818 (88.8%) 51,024 (85.7%)<br />
Night-time (otherwise) 9,491 (13.9%) 985 (11.2%) 8,506 (14.3%)<br />
Prehospital time (min) 50.6 [41.0;62.0] 47.0 [39.0;57.0] 51.0 [41.5;63.0] < 0.001 64,899<br />
On-scene time (min) 21.0 [15.0;28.6] 19.0 [14.0;25.0] 21.0 [15.2;29.0] < 0.001 64,765<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
Detailed diagnoses, summarised in Table 3, were available in 53,105<br />
missions (77.7% of all missions). Among these missions, 68.5% and<br />
39.8% of patients were diagnosed with trauma and non-trauma,<br />
respectively. Significantly, Table 3 highlights that multiple trauma<br />
diagnoses were made in 39.3% of trauma patients and multiple nontrauma<br />
diagnoses in 32.9% of non-trauma patients. Note that in this<br />
analysis, we explicitly accounted for the possibility of both trauma and<br />
non-trauma diagnoses in a single patient.<br />
Table 4 summarises the interventions and monitoring conducted,<br />
stratified into the following categories: basic interventions and<br />
monitoring, immobilisation and analgesia, critical interventions, airway<br />
management and resuscitation. Detailed variables were available in<br />
60,278 (88.2%) missions. Intravenous access and SpO2 monitoring<br />
were established in 82.8% and 85.0% of missions, respectively.<br />
Analgesia was given in 50.3% of missions, while intraosseous access<br />
was performed in 0.9% of all missions where the measures were<br />
available. As regards airway management, tracheal intubation and<br />
10<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
Table 3 Diagnoses and on-scene times stratified by age. Data are given in n (%) or median [Q1;Q3]<br />
All patients Children<br />
Adults<br />
(<<br />
(≥<br />
N = 68,333 N = 8,803 N = 59,530<br />
p<br />
N<br />
Diagnosis available: 53,105 (77.7%) 6,889 (78.3%) 46,216 (77.6%) 0.195 68,333<br />
Trauma<br />
Trauma diagnosis: 36,354 (68.5%) 5,647 (82.0%) 30,707 (66.4%) < 0.001 53,105<br />
Number of trauma diagnoses: < 0.001 36,354<br />
1 22,068 (60.7%) 3,779 (66.9%) 18,289 (59.6%)<br />
2 8,435 (23.2%) 1325 (23.5%) 7,110 (23.2%)<br />
3 4,152 (11.4%) 446 (7.90%) 3,706 (12.1%)<br />
4 1,699 (4.7%) 97 (1.7%)<br />
1,602 (5.2%)<br />
Prehospital time (min) 49.0 [39.6;61.0] 46.0 [38.1;55.4] 50.0 [40.0;62.0] < 0.001 34,811<br />
On-scene time (min) 20.0 [15.0;28.0] 18.8 [14.0;24.0] 20.0 [15.0;28.3] < 0.001 34,719<br />
Non-Trauma<br />
Non-trauma diagnosis : 21,144 (39.8%) 1,618 (23.5%) 19,526 (42.2%) < 0.001 53,105<br />
Number of non-trauma diagnoses: < 0.001 21,144<br />
1 14,194 (67.1%) 1,380 (85.3%) 12,814 (65.6%)<br />
2 4,836 (22.9%) 211 (13.0%) 4,625 (23.7%)<br />
3 1,623 (7.68%) 25 (1.55%) 1,598 (8.18%)<br />
4 491 (2.32%) 2 (0.12%)<br />
489 (2.50%)<br />
Type of non-trauma:<br />
Circulatory system 12,037 (56.9%) 199 (12.3%)<br />
11,838 (60.6%) < 0.001 21,144<br />
Respiratory system 1398 (6.6%) 294 (18.2%)<br />
1104 (5.7%) < 0.001 21,144<br />
Nervous system 2545 (12.0%) 342 (21.1%)<br />
2203 (11.3%) < 0.001 21,144<br />
Other 6415 (30.3%) 805 (49.8%)<br />
5610 (28.7%) < 0.001 21,144<br />
Prehospital time (min) 53.0 [44.0;64.0] 50.6 [42.0;60.0] 53.0 [44.0;64.0] < 0.001 19,920<br />
On-scene time (min) 22.0 [16.0;30.0] 21.0 [15.8;28.0] 22.0 [16.2;30.0]<br />
< 0.001 19,922<br />
capnography were performed in 10.3% and 11.4% of all missions,<br />
respectively. Chest compressions were performed as a resuscitation<br />
measure in 2.5% of all missions. Significantly, in 91.5% of all missions<br />
with recorded measures, further measures, as mentioned in Table 1,<br />
were taken beyond those explicitly mentioned in Table 4. While most<br />
patients were immobilised with the vacuum mattress, cervical collar<br />
and vacuum splinting were rarely used.<br />
Data including ICD-10 diagnosis, interventions and monitoring to be<br />
entered into the multivariable regression model with the outcome ‘onscene<br />
time’ were available for 45,060 missions (paediatric n = 5,981,<br />
adults n = 39,079), as summarised in Table 5. In the model, helicopter<br />
hoist operations (HHO) had the largest effect on on-scene time: a<br />
mission requiring HHO adds on average 15.1 (95%-CI 14.7–15.5, p <<br />
0.001) minutes to the overall on-scene time. Table 5 highlights that<br />
each critical intervention and each airway-management measure<br />
adds on average 2.4 (95%CI 2.0–2.9, p < 0.001) minutes and 2.4<br />
(95%-CI 2.3–3.6, p < 0.001) minutes, respectively. Note that separate<br />
regression models were computed for the child and adult sub-groups.<br />
To aid the interpretation and relative size of the regression coefficient,<br />
Fig. 2 illustrates each variable’s estimates of the regression coefficients<br />
(in units of minutes) in decreasing order.<br />
This study explicitly considers the number and types of measures<br />
taken (e.g. airway management measures): the impact of multiple<br />
measures on on-scene time in the child and adult sub-groups is shown<br />
in Fig. 3, which shows that the on-scene time increases linearly as a<br />
function of the number of airway-management, monitoring and criticalintervention<br />
measures.<br />
Discussion<br />
In summary, in Swiss Air-Rescue’s physician-staffed HEMS, adjusted<br />
on-scene and prehospital time for missions with paediatric patients<br />
was slightly longer than in missions with adult patients. Patients in<br />
remote areas that are difficult to access due to the terrain, requiring<br />
an evacuation involving a helicopter hoist, were associated with<br />
the greatest prolongation of on-scene time. Critical interventions,<br />
resuscitation and airway management also influenced the on-scene<br />
time to a varying degree (Fig. 3). Every single intervention and<br />
monitoring measure has a cumulative effect on on-scene time.<br />
An observational study reported median HEMS on-scene times of<br />
only 10 min, which may be explained by a high proportion of treatment<br />
interventions being conducted by ground-based medical teams before<br />
final helicopter transport [20]. A German comparative registry analysis<br />
of trauma patients between 2007 and 2009 showed on-scene times<br />
of around 40 min for HEMS and explained these in terms of a high<br />
proportion of patients requiring airway management [21]. Patient<br />
survival for HEMS transport was improved in this German analysis<br />
compared to the cohort of ground transportation by ambulance. In our<br />
analysis, on-scene time significantly depended on the interventions<br />
and measurements performed. It remains unclear whether—and if so<br />
to what extent—prolonged on-scene time in general influences patient<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
11
FEATURE<br />
Table 4 Available measures of interventions and monitoring stratified by age Data are given in n (%)<br />
All patients<br />
N = 68,333<br />
Children<br />
(<<br />
N = 8,803<br />
Adults<br />
(≥<br />
N = 59,530<br />
p<br />
N<br />
Measure available: 60,278 (88.2%) 7,923 (90.0%) 52,355 (87.9%)<br />
Basic interventions and monitoring<br />
iv access 49,923 (82.8%) 4,761 (60.1%) 45,162 (86.3%)<br />
SpO 2<br />
51,214 (85.0%) 6,353 (80.2%) 44,861 (85.7%)<br />
ECG 30,974 (51.4%) 2,038 (25.7%) 28,936 (55.3%)<br />
Temperature 3,073 (5.10%) 421 (5.31%) 2,652 (5.07%)<br />
Immobilisation & analgesia<br />
Vacuum mattress 24,555 (40.7%) 4,041 (51.0%) 20,514 (39.2%)<br />
Sedation 613 (1.0%) 130 (1.6%) 483 (0.9%)<br />
Analgesia 31,928 (53.0%) 3,627 (45.8%) 28,301 (54.1%)<br />
Reduction of a fracture or dislocation 1,048 (1.7%) 124 (1.6%) 924 (1.8%)<br />
Haemostasis 1,460 (2.4%) 104 (1.3%) 1,356 (2.6%)<br />
Critical interventions<br />
i.o. access 548 (0.9%) 110 (1.4%) 438 (0.8%)<br />
eFONA 14 (0.02%) 1 (0.01%) 13 (0.02%)<br />
Chest needle decompression 182 (0.3%) 8 (0.1%) 174 (0.3%)<br />
transcutaneous paceing 139 (0.2%) 1 (0.01%) 138 (0.3%)<br />
Vasopressors 3,544 (5.9%) 202 (2.6%) 3342 (6.4%)<br />
Airway management<br />
Tracheal intubation 6,210 (10.3%) 421 (5.3%) 5,789 (11.1%)<br />
Facemask ventilation 2,822 (4.7%) 265 (3.3%) 2,557 (4.9%)<br />
NMBA 3,834 (6.4%) 251 (3.2%) 3,583 (6.8%)<br />
Capnography 6,884 (11.4%) 473 (6.0%) 6,411 (12.2%)<br />
Resuscitation<br />
Chest compressions 1,476 (2.5%) 104 (1.3%) 1,372 (2.6%)<br />
Defibrillation 8,68 (1.4%) 22 (0.3%) 846 (1.6%)<br />
Mechanical chest compression device 1,128 (1.9%) 26 (0.3%) 1,102 (2.1%)<br />
Other<br />
Other* 55,131 (91.5%) 6,727 (84.9%) 48,404 (92.5%)<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
0.363<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
0.222<br />
< 0.001<br />
< 0.001<br />
> 0.99<br />
0.001<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
< 0.001<br />
ECG electrocardiogram, eFONA emergency front of neck access, iv intravenous, i.o. intraosseous, NMBA neuromuscular blocking agent, SpO 2<br />
peripheral oxygen saturation<br />
*Including but not limited to: wound dressing, vacuum splinting and cervical collar<br />
68,333<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
60,278<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
outcomes [3]. Fixating solely on shortening on-scene times might not<br />
capture the reality for patients, as life-saving interventions performed at<br />
the prehospital stage substantially reduced mortality in trauma patients<br />
[7, 10]. Discovering the correct diagnosis may reduce the delivery time<br />
for definitive treatment. For example, stroke patients had improved<br />
functional outcomes when treated by a mobile prehospital stroke unit<br />
as compared to traditional treatment in hospital [22].<br />
Helicopters enable missions to rescue patients, especially in remote<br />
and difficult terrain. Given the topography of Switzerland, with the<br />
Alps extending up to 4,634 m and many narrow valleys, these patients<br />
might be impossible to reach by ground ambulances. Many missions<br />
in this analysis involved patients undertaking recreational activities in<br />
the mountains in summer and winter (e.g. skiing, hiking or climbing).<br />
Rescue missions with ground-based evacuation teams could, to<br />
the patient’s disadvantage, easily require several hours just to reach<br />
the patient. A HEMS helicopter operating with a helicopter hoist can<br />
bring a physician to the patient directly and in a timely way, resulting<br />
in immediate access to clinical investigations and interventions [23].<br />
This could be crucial, as an analysis of helicopter hoist missions in<br />
a physician-staffed HEMS reported that nearly 20% of the patients<br />
were severely injured and presented with a NACA score ≥ 4 [6]. Such<br />
helicopter hoist operations can avoid lengthy terrestrial evacuations,<br />
which potentially endanger both patients and rescue crews. Although<br />
our data revealed that helicopter hoist operations were associated with<br />
the greatest prolongation of on-scene time, the additional on-scene<br />
time spent in these HEMS missions results in substantially less rescue<br />
time and likely greater chances of neurologically intact survival, as<br />
compared to traditional ground rescue.<br />
Advanced airway management in a patient with respiratory failure or<br />
the need for a patent airway is a potentially life-saving intervention,<br />
which is performed safely by physician-staffed HEMS services, often<br />
anaesthesiologists [24]. This skill could even be performed in-cabin<br />
as an en-route treatment to optimise time management during<br />
the flight to the hospital [25]. Resuscitation was associated with<br />
prolonged on-scene time. Performing cardiopulmonary resuscitation<br />
in the cabin by HEMS is challenging due to the helicopter’s limited<br />
personnel resources and working space. Nonetheless, mechanical<br />
chest compression devices facilitate high-quality cardiopulmonary<br />
resuscitation in such situations [26]. No evidence, such as outcome<br />
data, is yet available for cases after the use of mechanical resuscitation<br />
12<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
Table 5 The regression coefficient of multivariable linear regression with the outcome on-scene time (in minutes) stratified by age<br />
Outcome: On-scene time (min) All patients Children (< Adults (16 ≥ years)<br />
Characteristic Beta 95% CI p Beta 95% CI p Beta 95% CI p<br />
Helicopter hoist operation (HHO)<br />
No – – – – – –<br />
Yes 15.1 14.7, 15.5 < 0.001 13.0 11.7, 14.3 < 0.001 15.1 14.6, 15.5 < 0.001<br />
Critical interventions (per measure) 2.4 2.0, 2.9 < 0.001 2.7 1.5, 3.9 < 0.001 2.4 1.9, 2.9 < 0.001<br />
Airway management (per measure) 2.4 2.3, 2.6 < 0.001 2.8 2.4, 3.2 < 0.001 2.4 2.2, 2.5 < 0.001<br />
Resuscitation (per measure) 2.1 1.8, 2.5 < 0.001 1.6 0.03, 3.2 0.046 2.2 1.8, 2.5 < 0.001<br />
Basic interventions and monitoring (per<br />
measure)<br />
Location<br />
*including but not limited to: wound dressing, vacuum splinting and cervical collar<br />
1.9 1.7, 2.0 < 0.001 1.5 1.2, 1.8 < 0.001 2.0 1.8, 2.2 < 0.001<br />
(per measure) 1.5 1.4, 1.7 < 0.001 1.1 0.72, 1.4 < 0.001 1.7 1.5, 1.8 < 0.001<br />
Urban – – – – – –<br />
Remote 1.2 0.93, 1.5 < 0.001 − 0.35 − 0.90, 0.20 0.2 1.6 1.3, 1.9 < 0.001<br />
Time of day<br />
Daytime (07:00–19:00) – – – – – –<br />
Night-time (otherwise) 1.0 0.65, 1.3 < 0.001 1.6 0.84, 2.4 < 0.001 0.86 0.49, 1.2 < 0.001<br />
Other measures* (per measure) 0.82 0.75, 0.90 < 0.001 0.71 0.54, 0.87 < 0.001 0.85 0.77, 0.93 < 0.001<br />
Non-trauma (per diagnosis) 0.67 0.49, 0.84 < 0.001 1.2 0.71, 1.8 < 0.001 0.68 0.49, 0.86 < 0.001<br />
Trauma (per diagnosis) 0.41 0.28, 0.55 < 0.001 − 0.13 − 0.45, 0.20 0.4 0.47 0.32, 0.62 < 0.001<br />
National Advisory Committee for Aeronautics<br />
(NACA) score<br />
NACA I–III – – – – – –<br />
NACA IV–VI 0.36 0.05, 0.67 0.021 0.43 − 0.13, 1.0 0.13 0.28 − 0.07, 0.62 0.12<br />
Sex<br />
Female – – – – – –<br />
Male − 0.19 − 0.42, 0.05 0.12 − 0.39 − 0.85, 0.07 0.094 − 0.14 − 0.41, 0.12 0.3<br />
Age category<br />
Children – – – – – –<br />
Adults − 0.83 − 1.2, − 0.49 < 0.001<br />
Model performance<br />
Number of observations (N) 45,060 5,981 39,079<br />
Adjusted R-squared 0.23 0.26 0.23<br />
devices under HEMS conditions. Unfortunately, most of these devices<br />
cannot be used with paediatric patients, as reflected by the low<br />
numbers in our cohort.<br />
Critical interventions were regularly performed and associated with<br />
prolonged on-scene time. Most common in this cohort was the<br />
administration of intravenous vasopressors to maintain perfusion,<br />
intraosseous access and chest needle decompression.<br />
Intravenous access and analgesia were less frequently reported in<br />
children than in adults, even though children had more trauma. Our<br />
findings are in line with a recent observational study in a physicianstaffed<br />
HEMS [27]. Even if missions involving children were rare and<br />
physicians might not be that thoroughly trained in paediatric rescue,<br />
not to mention afraid of the potential risks, the reasons behind this<br />
inequity are unclear and require further investigation. Furthermore, the<br />
adjusted model revealed a slightly longer on-scene time for paediatric<br />
patients, while unadjusted on-scene time was shorter. This might be<br />
explained by statistical confounding, as paediatric patients had lower<br />
NACA scores compared to adults. However, while this finding was<br />
statistically significant, the clinical importance of a prolonged on-scene<br />
time of only 1 min might be negligible.<br />
Modifiable variables, such as the duration of a single measure (e.g. a<br />
critical intervention), have a significantly larger impact on on-scene time<br />
than non-modifiable factors, such as age category, type and number<br />
of diagnoses, and NACA score. Thus, reducing the duration of a single<br />
measure (intervention or monitoring) in these categories or performing<br />
these measures in parallel or during the flight as in-cabin treatment<br />
may hold significant potential to reduce on-scene time.<br />
While the measurements in our model were considered statistically<br />
independent, several measurements affect each other in clinical<br />
practice: A patient with a cardiac arrest is likely to be treated at least<br />
with chest compressions, defibrillation, intravenous or intraosseous<br />
access, vasopressors, intubation and capnography. Considering<br />
the time for all the single measurements, a cardiopulmonary<br />
resuscitation might easily last 10–15 min on-scene. For patients<br />
requiring emergency anaesthesia, baseline monitoring (SpO2,<br />
electrocardiogram, non-invasive blood pressure, and capnography),<br />
intravenous or intraosseous access, several medications (e.g. hypnotic,<br />
opioid, neuromuscular blocking agent, vasopressors), facemask<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
13
FEATURE<br />
Figure 2. Regression coefficients of the multivariable linear regression model with ‘on-scene time’ as the outcome. Mean and 95% confidence<br />
intervals are shown. Separate regression models were computed for (i) all patients, (ii) the child sub-group and (iii) the adult sub-group. HHO<br />
helicopter hoist operations, NACA National Advisory Committee for Aeronautics<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
ventilation, intubation and mechanical ventilation might also result in<br />
at least 10–15 min spent on-scene. In our HEMS, one medical crew<br />
member is responsible for preparing and administering medication<br />
and hemodynamic monitoring, while the other oversees airway<br />
management. These parallel performed tasks might save time spent<br />
on-scene. However, communication is important in such situations to<br />
have shared mental models within the HEMS crew; thus, an airway<br />
checklist is performed as standard operating procedure [28].<br />
Our study has several limitations due to its retrospective and<br />
observational character. Data in some mission reports (i.e. ICD-10<br />
diagnosis or measurement) are missing. The time of arrival on-scene<br />
is the landing time of the helicopter. Thus, the on-scene time might<br />
be slightly overestimated. We considered patients with a NACA score<br />
≥ IV potentially time-critical. However, only the patient’s most severe<br />
NACA score was recorded, which might be resolved by early on-scene<br />
treatment (e.g. airway obstruction, tension pneumothorax, anaphylactic<br />
shock). Our data may be difficult to compare with those from other<br />
topographic areas with less need for helicopter hoist operations.<br />
Unfortunately, our database lacks patient-survival and outcome data,<br />
which we realised is an important point for improvement on this study.<br />
Finally, the study took place over a long period of time which might<br />
have had influence in terms of protocols and practice.<br />
Conclusions<br />
In conclusion, compared to adult patients, the adjusted on-scene and the<br />
prehospital time for children was slightly longer, and children were more<br />
likely to have trauma, but also a lower NACA score. Intravenous access<br />
and analgesia were less frequently established in children. On-scene<br />
time was significantly prolonged in rescue missions with helicopter hoist<br />
operations. Each individual intervention and monitoring measure increases<br />
on-scene time. Thus, performing such interventions in parallel or as<br />
in-cabin treatment could be an option to reduce on-scene time in lifethreatening<br />
patient conditions, but would require special training. However,<br />
multiple clinical interventions and monitoring interact and are not single<br />
interventions. Compared to the impact of interventions, non-modifiable<br />
factors, such as NACA score, type of diagnosis and age, make only a<br />
minor contribution to overall on-scene time. Future research should focus<br />
on the crucial association between on-scene time and patient outcomes<br />
in a physician-staffed HEMS, quality of care for paediatric prehospital<br />
patients and the feasibility of in-cabin treatment.<br />
14<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
Figure 3. Effect plots of the multivariable linear regression model with the outcome ‘on-scene time’ (in minutes), separately for the child and adult<br />
sub-groups. Mean and 95% confidence intervals are shown. Note that the number of diagnoses and measures are considered as factor variables<br />
here to assess the linearity of the association between the number of measures and on-scene time. HHO helicopter hoist operations, NACA National<br />
Advisory Committee for Aeronautics<br />
Abbreviations<br />
HEMS Helicopter Emergency Medical Service<br />
HHO Helicopter Hoist Operation<br />
ICD International Classification of Diseases<br />
NACA National Advisory Committee for Aeronautics<br />
Acknowledgements<br />
None.<br />
Author contributions<br />
AF: conception and design, primary data acquisition, statistical analysis<br />
and interpretation, manuscript drafting. MH: conception, statistical<br />
analysis and interpretation, manuscript drafting. SB, TR and RA: data<br />
interpretation, critical revision of the manuscript. RG: data interpretation,<br />
manuscript drafting and critical revision. UP: conception and design,<br />
primary data acquisition, data interpretation, manuscript drafting and<br />
critical revision, project supervision. All of the authors have read and<br />
approved the final version of the manuscript and agreed to be named<br />
as an author.<br />
Funding<br />
This study did not receive any specific funding.<br />
Availability of data and materials<br />
The dataset analysed in the current study is available from the<br />
corresponding author upon reasonable request and with permission of<br />
the responsible Ethics Committee.<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
15
FEATURE<br />
Declarations<br />
Ethics approval and consent to participate<br />
The study protocol was approved by the responsible Ethics Committee<br />
(Ethics Committee of Eastern Switzerland; EKOS 22/021) and the<br />
need for informed consent was waived due to the retrospective and<br />
anonymised character of the data in this study.<br />
Consent for publication<br />
Not applicable.<br />
Competing interests<br />
RG is the ERC Board Member of ILCOR (International Liaison<br />
Committee on Resuscitation), as well as the ILCOR’s Education,<br />
Implementation and Team Task Force Chair. All other authors declare<br />
that they have no conflicts of interest.<br />
Author details<br />
1Department of Anaesthesiology and Pain Medicine, Inselspital,<br />
Bern University Hospital, University of Bern, Freiburgstrasse, 3010<br />
Bern, Switzerland. 2Swiss Air-Rescue (Rega), Zurich, Switzerland.<br />
3Department of Anaesthesiology and Intensive Care Medicine, Cantonal<br />
Hospital St. Gallen, St. Gallen, Switzerland. 4University of Bern, Bern,<br />
Switzerland. 5School of Medicine, Sigmund Freud University Vienna,<br />
Vienna, Austria. 6European Resuscitation Council (ERC) Research NET,<br />
Niel, Belgium. 7Department of Emergency Medicine, Inselspital, Bern<br />
University Hospital, University of Bern, Bern, Switzerland.<br />
Received: 29 December 2022 Accepted: 6 April <strong>2023</strong><br />
Published online: 14 April <strong>2023</strong><br />
References<br />
1. Oude Alink MB, Moors XRJ, Karrar S, Houmes RJ, Hartog DD, Stolker<br />
RJ. Characteristics, management and outcome of prehospital pediatric<br />
emergencies by a Dutch HEMS. Eur J Trauma Emerg Surg. 2021;<br />
2. Mueller S, Zheng J, Orav EJ, Schnipper JL. Inter-hospital transfer<br />
and patient outcomes: a retrospective cohort study. BMJ Qual Saf.<br />
2019;28(11): e1.<br />
3. Spoelder EJ, Slagt C, Scheffer GJ, van Geffen GJ. Transport<br />
of the patient with trauma: a narrative review. Anaesthesia.<br />
2022;77(11):1281–7.<br />
4. Fuchs A, Schmucki R, Meuli L, Wendel-Garcia PD, Albrecht<br />
R, Greif R, et al. Helicopter inter-hospital transfer for patients<br />
undergoing extracorporeal membrane oxygenation: a retrospective<br />
12-year analysis of a service system. Scand J Trauma Resuscit<br />
Emerg Med. 2022;30(1):33.<br />
5. Meuli L, Zimmermann A, Menges AL, Tissi M, Becker S, Albrecht<br />
R, et al. Helicopter emergency medical service for time critical<br />
interfacility transfers of patients with cardiovascular emergencies.<br />
Scand J Trauma Resuscit Emerg Med. 2021;29(1):168.<br />
6. Pietsch U, Knapp J, Mann M, Meuli L, Lischke V, Tissi M, et al.<br />
Incidence and challenges of helicopter emergency medical service<br />
(HEMS) rescue missions with helicopter hoist operations: analysis<br />
of 11,228 daytime and nighttime missions in Switzerland. Scand J<br />
Trauma Resuscit Emerg Med. 2021;29(1):92.<br />
7. Gomes E, Araujo R, Carneiro A, Dias C, Costa-Pereira A, Lecky<br />
FE. The importance of pre-trauma centre treatment of lifethreatening<br />
events on the mortality of patients transferred with<br />
severe trauma. Resuscitation. 2010;81(4):440–5.<br />
8. Berkeveld E, Popal Z, Schober P, Zuidema WP, Bloemers<br />
FW, Giannakopoulos GF. Prehospital time and mortality in<br />
polytrauma patients: a retrospective analysis. BMC Emerg Med.<br />
2021;21(1):78.<br />
9. Gauss T, Ageron FX, Devaud ML, Debaty G, Travers S, Garrigue D,<br />
et al. Association of prehospital time to in-hospital trauma mortality<br />
in a physician-staffed emergency medicine system. J Am Med<br />
Assoc Surg. 2019;154(12):1117–24.<br />
10. Brown JB, Rosengart MR, Forsythe RM, Reynolds BR, Gestring<br />
ML, Hallinan WM, et al. Not all prehospital time is equal:<br />
influence of scene time on mortality. J Trauma Acute Care Surg.<br />
2016;81(1):93–100.<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
16<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
11. Blasius FM, Horst K, Brokmann JC, Lefering R, Andruszkow H,<br />
Hildebrand F, et al. Helicopter emergency medical service and<br />
hospital treatment levels affect survival in pediatric trauma patients.<br />
J Clin Med. 2021;10(4).<br />
12. Englum BR, Rialon KL, Kim J, Shapiro ML, Scarborough JE, Rice<br />
HE, et al. Current use and outcomes of helicopter transport in<br />
pediatric trauma: a review of 18,291 transports. J Pediatr Surg.<br />
2017;52(1):140–4.<br />
13. Knapp J, Haske D, Bottiger BW, Limacher A, Stalder O, Schmid A,<br />
et al. Influence of prehospital physician presence on survival after<br />
severe trauma: systematic review and meta-analysis. J Trauma<br />
Acute Care Surg. 2019;87(4):978–89.<br />
14. Li T, Cushman JT, Shah MN, Kelly AG, Rich DQ, Jones CMC.<br />
Prehospital time intervals and management of ischemic stroke<br />
patients. Am J Emerg Med. 2021;42:127–31.<br />
15. Herlitz J, Wireklintsundstrom B, Bang A, Berglund A, Svensson<br />
L, Blomstrand C. Early identification and delay to treatment in<br />
myocardial infarction and stroke: differences and similarities.<br />
Scand J Trauma Resuscit Emerg Med. 2010;18:48.<br />
16. Liu VX, Fielding-Singh V, Greene JD, Baker JM, Iwashyna TJ,<br />
Bhattacharya J, et al. The timing of early antibiotics and hospital<br />
mortality in sepsis. Am J Respir Crit Care Med. 2017;196(7):856–63.<br />
17. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche<br />
PC, Vandenbroucke JP. The Strengthening the Reporting of<br />
Observational Studies in Epidemiology (STROBE) statement:<br />
guidelines for reporting observational studies. Lancet.<br />
2007;370(9596):1453–7.<br />
18. World Health Organization (WHO). International Classification of<br />
Diseases (ICD-10) 2019 https://icd.who.int/browse10/2019/en#/<br />
U07.12019. https://icd.who.int/browse10/2019/en#/U07.1.<br />
19. R Core Team. R: A language and environment for statistical<br />
computing. R Foundation for Statistical Computing, Vienna,<br />
Austria. 2021.<br />
20. Osteras O, Heltne JK, Vikenes BC, Assmus J, Brattebo G.<br />
Factors influencing on-scene time in a rural Norwegian helicopter<br />
emergency medical service: a retrospective observational study.<br />
Scand J Trauma Resuscit Emerg Med. 2017;25(1):97.<br />
21. Andruszkow H, Lefering R, Frink M, Mommsen P, Zeckey C, Rahe<br />
K, et al. Survival benefit of helicopter emergency medical services<br />
compared to ground emergency medical services in traumatized<br />
patients. Crit Care. 2013;17(3):R124.<br />
22. Ebinger M, Siegerink B, Kunz A, Wendt M, Weber JE, Schwabauer<br />
E, et al. Association between dispatch of mobile stroke units and<br />
functional outcomes among patients with acute ischemic stroke in<br />
Berlin. J Am Med Assoc. 2021;325(5):454–66.<br />
23. Ausserer J, Moritz E, Stroehle M, Brugger H, Strapazzon G, Rauch<br />
S, et al. Physician staffed helicopter emergency medical systems<br />
can provide advanced trauma life support in mountainous and<br />
remote areas. Injury. 2017;48(1):20–5.<br />
24. Pietsch U, Mullner R, Theiler L, Wenzel V, Meuli L, Knapp J, et al.<br />
Airway management in a Helicopter Emergency Medical Service<br />
(HEMS): a retrospective observational study of 365 out-of-hospital<br />
intubations. BMC Emerg Med. 2022;22(1):23.<br />
25. Knapp J, Venetz P, Pietsch U. In-cabin rapid sequence induction<br />
: experience from alpine air rescue on reduction of the prehospital<br />
time. Anaesthesist. 2021;70(7):609–13.<br />
26. Pietsch U, Reiser D, Wenzel V, Knapp J, Tissi M, Theiler L, et<br />
al. Mechanical chest compression devices in the helicopter<br />
emergency medical service in Switzerland. Scand J Trauma<br />
Resuscit Emerg Med. 2020;28(1):71.<br />
27. Rugg C, Woyke S, Ausserer J, Voelckel W, Paal P, Strohle M.<br />
Analgesia in pediatric trauma patients in physician-staffed Austrian<br />
helicopter rescue: a 12-year registry analysis. Scand J Trauma<br />
Resuscit Emerg Med. 2021;29(1):161.<br />
28. Fuchs A, Frick S, Huber M, Riva T, Theiler L, Kleine-Brueggeney<br />
M, et al. Five-year audit of adherence to an anaesthesia preinduction<br />
checklist. Anaesthesia. 2022.<br />
Publisher’s Note<br />
Springer Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affiliations.<br />
A WORLD OF COMFORT<br />
CLIMATE CONTROLLED HEALTHCARE<br />
Customised vehicle heating and cooling solutions from Eberspacher.<br />
Simple to use, effective in performance and reliable in operation.<br />
On the move comfort for patient and healthcare professionals.<br />
www.eberspaecher-climate.com<br />
Find your<br />
nearest Dealer<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
17
NEWSLINE<br />
opens the new base open for<br />
Magpas Air <strong>Ambulance</strong> to begin<br />
the process of moving their<br />
operations and lifesaving service<br />
to the state-of-the-art airbase and<br />
headquarters.<br />
is a momentous day, however<br />
our hard work continues as we<br />
look to develop our services<br />
further, push to raise the £6million<br />
needed keep us flying every year,<br />
and continue to save lives 24/7.”<br />
HRH The Princess Royal unveils plaque, opening the new<br />
Magpas Air <strong>Ambulance</strong> airbase<br />
Daryl Brown MBE DL, the<br />
charity’s Chief Executive Officer,<br />
said “It was an honour to<br />
welcome our Patron HRH The<br />
Princess Royal to the site of our<br />
new base at Alconbury Weald,<br />
and show her around the building<br />
she’s been so pivotal in helping<br />
us achieve.<br />
Find out more about the charity<br />
today at magpas.org.uk.<br />
<strong>Ambulance</strong> medic<br />
raises money for new<br />
defibrillator in tearful<br />
tribute to brother<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
HRH The Princess<br />
Royal opens<br />
new Magpas Air<br />
<strong>Ambulance</strong> base in<br />
Cambridgeshire<br />
On Tuesday, 12th September<br />
Magpas Air <strong>Ambulance</strong> staff,<br />
clinicians, former patients<br />
and supporters witnessed an<br />
important milestone in the<br />
charity’s history as HRH The<br />
Princess Royal opened the new<br />
charity airbase.<br />
The lifesaving charity has been<br />
working to build its new home<br />
for the past six years: a purposebuilt<br />
airbase, headquarters and<br />
training centre in Alconbury<br />
Weald, Cambridgeshire.<br />
The building, designed by MCW<br />
architects and constructed by<br />
Lindum, includes a dedicated<br />
state-of-the-art training centre<br />
to train the next generation of<br />
pre-hospital emergency doctors<br />
and paramedics; is equipped<br />
for 24/7 operations with wellbeing<br />
and rest facilities for<br />
crew and clinicians; and has<br />
new community and patient<br />
facilities on site—including a new<br />
dedicated space for patients and<br />
their families to visit the charity<br />
and meet with the clinicians that<br />
treated them, away from the<br />
bustle of day-to-day operations.<br />
To ensure it maximises renewable<br />
energy, the building has been<br />
designed with the approach<br />
of ‘be lean, be clean and be<br />
green’. This is achieved through<br />
integrated design measures such<br />
as solar shading and natural<br />
ventilation through louvres, and<br />
PV panels on the roof.<br />
The location of the new airbase<br />
is situated closer to the region’s<br />
major trunk roads, which will<br />
reduce vehicle dispatch times<br />
by up to 15 minutes, and the<br />
co-location of the charity’s<br />
operations and support staff—<br />
who currently work across two<br />
sites—will be more efficient:<br />
reducing charity overheads and<br />
improving environmental impact.<br />
HRH The Princess Royal became<br />
Magpas Air <strong>Ambulance</strong>’s Patron<br />
after she visited the charity’s<br />
previous operations base in<br />
February 2020, and heard about<br />
the need for the service to find a<br />
new home. In 2021, the charity’s<br />
50th year of operations, HRH<br />
launched the Future 50 Appeal<br />
aimed at raising the funding<br />
needed to complete the building.<br />
And in February of this year, HRH<br />
unveiled a cornerstone to mark<br />
the ongoing development of<br />
the project.<br />
However, Tuesday’s visit from The<br />
Princess Royal is undoubtedly<br />
the most exciting yet as HRH<br />
“After she unveiled the plaque,<br />
which will become a treasured<br />
part of our building alongside the<br />
cornerstone, we were delighted<br />
to see her passion for the service<br />
we provide.<br />
“It’s incredibly exciting to see,<br />
what has been a plan for a very<br />
long time, finally come to fruition.<br />
Magpas Air <strong>Ambulance</strong> has<br />
treated over 70,000 patients in<br />
the past 50 years, and this new<br />
building will be fundamental<br />
to our service going forward<br />
saving thousands more lives<br />
and keeping families together for<br />
generations to come.”<br />
Magpas Air <strong>Ambulance</strong> is one<br />
of the first emergency medical<br />
charities of its kind in the <strong>UK</strong>,<br />
initially set up by two GPs in 1971.<br />
The new airbase is an important<br />
milestone in its 50-year pursuit<br />
to improve emergency care<br />
for patients across the region.<br />
However, for the charity that has<br />
experienced the highest number<br />
of activations in six years, the<br />
hard work has just begun. Natalie<br />
Church, the charity’s Director<br />
of Operations who led the new<br />
base development explains,<br />
“In addition to enhancing our<br />
service, the new building provides<br />
so many more opportunities to<br />
increase the understanding of our<br />
work and teach the community<br />
lifesaving skills such as CPR.<br />
For Magaps Air <strong>Ambulance</strong> this<br />
An ambulance medic has<br />
raised money for a new<br />
defibrillator at the temple<br />
where his brother died<br />
suddenly last year.<br />
Ron Dhesi, a long-serving<br />
London <strong>Ambulance</strong> Service<br />
frontline worker, raised £2400 in<br />
just two hours for a defibrillator<br />
that he recently installed at<br />
Woolwich Gurdwara, where his<br />
older brother passed away.<br />
Ron then taught the community<br />
how to use the defibrillator –<br />
which can restart someone’s<br />
heart if it has stopped beating<br />
- and perform life-saving chest<br />
compressions.<br />
Perminder Singh Dhesi, from<br />
Welling, was only 66 when he<br />
went into cardiac arrest after<br />
an afternoon service at the<br />
south east-London Sikh temple<br />
last December.<br />
London <strong>Ambulance</strong> Service<br />
crews tried desperately to save<br />
him but Perminder died shortly<br />
after his collapse.<br />
18<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
Emergency Medical Technician<br />
Ron Dhesi, 64, said:<br />
“We were together on Christmas<br />
day as we normally are every year<br />
– he was absolutely fine, he was a<br />
perfectly healthy man.<br />
“I know from my job that a<br />
cardiac arrest can happen to<br />
anyone, at any time, but you<br />
never expect the worst day to<br />
happen to you.<br />
At Perminder’s funeral, Ron<br />
spoke to the members of the<br />
temple about the vital importance<br />
of having a defibrillator on site.<br />
Within two hours, Ron had<br />
already gathered enough money<br />
to buy a new defibrillator and<br />
convinced the community to learn<br />
life-saving skills.<br />
Ron, who has worked for<br />
London <strong>Ambulance</strong> Service for<br />
20 years, has since delivered a<br />
lifesaving training session at the<br />
Gurdwara with his son Chanbir,<br />
35, who is also a London<br />
<strong>Ambulance</strong> Service paramedic,<br />
and his colleagues Tom Aris and<br />
Simran Pengli.<br />
Welling with emotion talking<br />
about his loss, Ron said:<br />
“My relationship with my brother<br />
was beyond words. Not having<br />
him for the past eight months has<br />
taken a lot out of me.<br />
“He was the sibling that you<br />
dream of. We grew up together,<br />
he stood up for me, fought for<br />
me. He was the one who glued<br />
the family together.<br />
“He loved his grandchildren, but<br />
sadly he missed the birth of his<br />
granddaughter.<br />
“We will never know if my brother<br />
could have been saved if a<br />
defibrillator was there, but this is<br />
all about giving someone the best<br />
chance of survival.”<br />
Ron is now planning training<br />
sessions at other temples in<br />
Greenwich.<br />
Daniel Elkeles, Chief Executive at<br />
London <strong>Ambulance</strong> Service, said:<br />
“Rons’ incredible devotion to<br />
the health and wellbeing of his<br />
community at an incredibly<br />
difficult time for his family is<br />
really inspiring.<br />
“I support his efforts to<br />
encourage people to learn vital<br />
resuscitation skills and help make<br />
London a city of lifesavers: you<br />
could save the life of a loved one.”<br />
Trust working with<br />
partners to improve<br />
care for lower<br />
category call patients<br />
South East Coast <strong>Ambulance</strong><br />
Service NHS Foundation Trust,<br />
(SECAmb), is working with its<br />
partners to establish ways of<br />
improving the care received by<br />
lower category call patients.<br />
Recognising that many of these<br />
patients are often waiting too<br />
long for an ambulance response<br />
or being taken to hospital when<br />
they could be treated elsewhere,<br />
including by community<br />
healthcare providers, SECAmb<br />
is developing an approach that<br />
will see NHS Urgent Community<br />
Response (UCR) teams from<br />
across its region access its<br />
Computer Aided Dispatch<br />
(CAD) system.<br />
UCR teams provide urgent<br />
care to people in their homes<br />
which helps to avoid hospital<br />
admissions and enables people<br />
to live independently for longer.<br />
Through these teams, older<br />
people and adults with complex<br />
STRETCHER &<br />
LOADING SYSTEM<br />
l Mechanical loading system – easy to operate & no electrics to go wrong<br />
l Up to 30 kg lighter weight than other loading systems<br />
l Can be easily loaded on inclines, angles and uneven surfaces<br />
l Powered stretcher with unassisted lift capacity of 50 stone (320 kg)<br />
To book a DEMO and see the AMBULANCE system for yourself email sales.uk@ferno.com call +44 (0) 1274 851 999<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
19
NEWSLINE<br />
health needs who urgently need<br />
care, can get fast access to a<br />
range of health and social care<br />
professionals within two hours.<br />
Access to the system will follow<br />
a 12-week period of working with<br />
SECAmb, with daily ‘touch points’<br />
to establish the types of calls<br />
which would be better assigned<br />
to community teams. The UCR<br />
team is then given access to a<br />
portal that allows them to review<br />
and directly attend appropriate<br />
calls and, in turn, ensure<br />
ambulance clinicians are freer to<br />
respond to calls which require an<br />
ambulance response.<br />
The touch point calls also offer<br />
both providers and SECAmb<br />
with an opportunity to better<br />
understand the range of patients<br />
calling 999 that could potentially<br />
be managed by UCRs earlier in a<br />
patient’s journey.<br />
Operations for Integrated Care<br />
(999 and 111) Scott Thowney<br />
said: “This important work aims<br />
to improve patient care and<br />
provide a more appropriate<br />
service to some of our lower<br />
category call patients who<br />
may not necessarily require an<br />
ambulance response.<br />
“By working more closely with<br />
community providers across our<br />
region, we will ensure that more<br />
patients can be receive timely<br />
treatment and our clinicians<br />
will be freer to respond to<br />
those patients who require an<br />
ambulance response.<br />
“This additional partnership work<br />
will help SECAmb and the wider<br />
NHS ahead of the winter and<br />
ensure we are doing all that we<br />
can to provide the right care for<br />
our patients.”<br />
A cycle paramedic who hops<br />
on her bike to save lives every<br />
day has achieved a top 20<br />
finish at one of the world’s<br />
most renowned cycling<br />
championships.<br />
Carol Reeves, 44, a medic in<br />
London <strong>Ambulance</strong> Service’s<br />
pioneering Cycle Response<br />
Unit (CRU), ranked 19th in<br />
the UCI Gran Fondo World<br />
Championships in August –<br />
the world’s biggest and most<br />
prestigious competition for both<br />
professional and amateur cyclists.<br />
It took Carol just five hours and<br />
10 minutes to cycle 100 miles,<br />
climbing a gruelling 6,000 ft.<br />
She tackled the challenging<br />
roads of Highland Perthshire<br />
outpacing 180 of the world’s best<br />
women riders.<br />
moving to Waterloo to cover an<br />
area in Central London by bike.<br />
This year, Carol qualified at the<br />
Gran Fondo race in Cambridge<br />
and was then invited to represent<br />
Team GB in Glasgow.<br />
Only the top 25% of riders from<br />
27 qualifying events held around<br />
the world were invited to compete<br />
in Scotland.<br />
London <strong>Ambulance</strong> Service’s<br />
Cycle Response Unit is a team of<br />
40 paramedics who ride through<br />
the city’s busiest areas to alleviate<br />
pressures on ambulances.<br />
Cycle paramedics carry 75<br />
kilograms of equipment,<br />
including the same life-saving<br />
equipment as an ambulance like a<br />
defibrillator and electrocardiogram<br />
(ECG) machine.<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
Following this period, the teams<br />
will be able to review 999 calls<br />
awaiting a response and, where<br />
appropriate, respond directly to<br />
lower category 3 and category<br />
4 calls instead of SECAmb<br />
clinicians.<br />
While the work is at an early<br />
stage, referrals to the UCRs are<br />
increasing week on week. Daily<br />
touch point calls are now taking<br />
place with UCRs in Sussex and<br />
Medway and several teams within<br />
Surrey and Kent participating<br />
or scheduled to start in the<br />
coming weeks.<br />
Currently, SECAmb’s ‘hear and<br />
treat rate’ – 999 calls which<br />
are handled with advice over<br />
the phone or referral to another<br />
service – stands at approximately<br />
10 per cent. The service is<br />
looking to increase the rate to<br />
14 per cent – the equivalent to<br />
around 30,000 calls a year, which<br />
would have otherwise received an<br />
ambulance response.<br />
SECAmb Head of Clinical<br />
Hollie Poole, West Sussex Area<br />
Director at Sussex Community<br />
NHS Foundation Trust said:<br />
“I’ve had positive feedback from<br />
our clinicians on the ground.<br />
They’ve told me that the Urgent<br />
Community Response model<br />
and the work that they are<br />
undertaking feels responsive,<br />
relevant and is making a real<br />
difference to our patients.<br />
“This is a fantastic example of<br />
what can be achieved through<br />
collaborative working. As we<br />
continue to work closely together,<br />
I’m excited for the future of UCR<br />
in Sussex.”<br />
Cycle paramedic<br />
breaks into top 20 at<br />
global championship<br />
Carol said: “Getting to the finish<br />
line was a bit like racing to save<br />
the life of a patient. You need to<br />
have the confidence that you are<br />
going to make it.”<br />
Carol, who has been at the<br />
Service for 17 years, cycles an<br />
average of 30 miles per shift. As<br />
a cycle paramedic, she can race<br />
past the capital’s heavy traffic to<br />
get to her patients in an average<br />
of six minutes.<br />
Carol said: “Pedalling fast to get<br />
to emergencies on a bike that has<br />
lots of medical equipment packed<br />
into panniers definitely helped me<br />
prepare for the competition.<br />
“It was amazing to achieve such a<br />
result. All that was going through<br />
my head was: ‘please, don’t<br />
come last!’”<br />
Carol, from Dartford, Kent,<br />
became a keen cyclist 15<br />
years ago, after a career in the<br />
British Army.<br />
In 2006, she started working as a<br />
paramedic in East London, before<br />
Over 50 per cent of the patients<br />
they treat can be discharged at<br />
the scene, freeing up ambulance<br />
crews to attend patients who<br />
need to be taken to hospital.<br />
East of England<br />
<strong>Ambulance</strong> Service<br />
NHS Trust (EEAST)<br />
has taken a<br />
remarkable step<br />
towards prioritising<br />
the mental health<br />
of its staff by<br />
introducing approved<br />
support dogs.<br />
This pawsome new scheme<br />
involves the use of four-legged<br />
friends to provide essential<br />
support and companionship<br />
24/7 to EEAST staff members<br />
after traumatic events.<br />
20<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
EEAST has so far enlisted 17 four-<br />
their own dogs to workstations,<br />
by reducing doctor visits and<br />
Two decommissioned<br />
legged friends, with an additional<br />
50 awaiting assessment. Known<br />
as GoodDOGS, these canine<br />
emergency operation centres,<br />
and offices. Although the<br />
proposal was initially approved,<br />
significantly improving mental<br />
health and overall wellbeing.<br />
ambulances and a Land Rover<br />
have been handed over to the<br />
Ukrainian military courtesy of a<br />
companions are the personal<br />
pets of staff members and have<br />
undergone assessment by a staff<br />
representative, authorised by<br />
Canine Concern, the overseeing<br />
organization.<br />
Those pups approved for<br />
the pandemic hindered its<br />
implementation. When I<br />
learned about Cambridgeshire<br />
Police’s welfare dog project in<br />
2020, I realised it was exactly<br />
what our teams needed. After<br />
consultations and discussions,<br />
I≈decided to revive the<br />
The rollout of the GoodDOGS<br />
scheme commenced in April,<br />
beginning with the recruitment of<br />
the first three dogs. Subsequent<br />
assessment days have been<br />
held in Chelmsford, Longwater,<br />
Bedford EOC, and Melbourn HQ.<br />
Ukrainian doctor and his friends.<br />
This is the third such donation of<br />
decommissioned vehicles and<br />
equipment to be donated by the<br />
service over the last year.<br />
Anatoliy Telpov, who works in the<br />
participation receive their own<br />
identification badges and are<br />
available round the clock to<br />
provide support, especially<br />
after traumatic events, and the<br />
initiative represents a significant<br />
stride in employee wellbeing,<br />
project and introduce our own<br />
GoodDOGS to EEAST.”<br />
The positive effects of interactions<br />
with dogs on human health and<br />
wellbeing are well-established.<br />
Dogs contribute to increased<br />
More former<br />
ambulances sent to<br />
frontline of Ukraine<br />
conflict<br />
Emergency Department of South<br />
Tyneside District Hospital, was<br />
a key member of a group who<br />
drove the fleet close to the border<br />
of Ukraine.<br />
The efforts by Dr Telpov, who<br />
demonstrating the Trust’s<br />
commitment to providing support<br />
to its dedicated and valued<br />
staff members.<br />
physical activity, reduced risks<br />
of cardiovascular disease, and<br />
enhanced immunity to allergies,<br />
particularly in children. According<br />
Former ambulances still<br />
supporting patients in need<br />
after being decommissioned<br />
is from Ivano-Frankivsk, a city<br />
in the west of the country,<br />
follows previous work with NHS<br />
colleague Kelley Storey. She<br />
Amanda Harris, project lead,<br />
said: “The inspiration for this<br />
initiative came from a proposal in<br />
to research conducted by the<br />
University of Lincoln, dogs<br />
play a pivotal role in saving the<br />
<strong>UK</strong> health sector an estimated<br />
North East <strong>Ambulance</strong> Service<br />
has donated more former<br />
ambulance vehicles to the<br />
works for Northumbria Healthcare<br />
NHS Foundation Trust and private<br />
ambulance company, FSNE.<br />
2019 to have staff members bring<br />
£2.45 billion annually, primarily<br />
Ukraine support effort.<br />
Alongside the NEAS vehicles,<br />
Rendering Controlled Drugs Irretrievable for Use<br />
SaferDenature Controlled Drug denaturing kits will render unused, waste<br />
or expired medicines irretrievable prior to disposal via pharmaceutical<br />
waste streams in line with current legislation * .<br />
Suitable for use with tablets, capsules,<br />
liquids, aerosols or patches<br />
The water soluble sachet contains the<br />
formula granules to guard against<br />
accidental spillage and user contamination<br />
Available in volumes from 250ml to 20L to<br />
suit different working environments<br />
Purchase at NHS supply chain: my.supplychain.nhs.uk/catalogue<br />
or www.alphalabs.co.uk/safer-denature<br />
Phone: 023 8048 3000 • www.alphalabs.co.uk<br />
*The misuse of Drugs<br />
Regulations 2001<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
09 Safer Denature - <strong>Ambulance</strong> <strong>UK</strong> - Sept <strong>2023</strong>.indd 1 28/09/<strong>2023</strong> 09:43:02<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
21
NEWSLINE<br />
FSNE donated a 4x4 and<br />
provided funds to pay for fuel and<br />
food for the journey.<br />
checks and now they’re out<br />
there helping. We got some great<br />
feedback from the military, saying<br />
they were a help.”<br />
With the help of Harry Clark,<br />
who works for NEAS, and FSNE<br />
team members James Redshaw,<br />
Katharine Sayer and Stephen<br />
Aitken, all four vehicles were<br />
taken across to mainland Europe<br />
and then to the Polish border to<br />
be handed to Ukrainian military<br />
representatives.<br />
A further two vehicles have also<br />
been donated to the Bravery<br />
Foundation which has also been<br />
used for the Ukraine effort.<br />
Another 7.5 tonne lorry will be<br />
donated in September <strong>2023</strong>.<br />
Graham Tebbutt, managing<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
Simarnam Singh, who also<br />
works as a doctor alongside Dr<br />
Telpov at South Tyneside and<br />
Sunderland NHS Foundation<br />
Trust, and his friends and family<br />
from the Sikh Temple GKMRHK<br />
in South Shields, sponsored ferry<br />
travel, hotels and return flights for<br />
the team.<br />
The vehicles have since<br />
undergone checks in Ukraine<br />
and have been resprayed. They<br />
will now be helping to transport<br />
casualties from the frontline to<br />
where they can be treated.<br />
The doctor and a team of friends<br />
and supporters he works with,<br />
are now seeking out more<br />
4x4 vehicles and quadbikes<br />
to send over in the next wave<br />
of donations.<br />
They hope to raise more funds<br />
and gather together as many<br />
donated vehicles as possible to<br />
send over to Ukraine.<br />
He said: “These vehicles have<br />
gone to help get people to<br />
hospitals from the frontline and<br />
we know they have gone to help<br />
in the South East of the country.<br />
They will be helping every day.<br />
“The journey to take them over to<br />
Ukraine went very well. The team<br />
was absolutely marvellous and<br />
dedicated and they faced long<br />
days and very hot conditions with<br />
no air conditioning.<br />
“All the vehicles got their final<br />
director of NEASUS, the<br />
subsidiary fleet arm of North<br />
East <strong>Ambulance</strong> Service, said:<br />
“It’s great to know that even after<br />
they’ve finished serving the North<br />
East public, our vehicles are<br />
able to continue helping patients<br />
in need.<br />
“My team have been really proud<br />
of being able to play a small role<br />
in this work, and I’d like to thank<br />
them for their support in ensuring<br />
the vehicles were capable of<br />
completing the journey.”<br />
Dr Telpov added: “A special thank<br />
you must go to Kelley for her help<br />
and time with this project.<br />
“Graham has also been a huge<br />
support, without the generous gift<br />
of the ambulances and supplies<br />
it would not have been possible.<br />
“I would like to say a thank you<br />
to Greg Douglas and Melissa<br />
Douglas, the directors of FSNE,<br />
and their team, as well as my<br />
colleague Sim for everything they<br />
have done.<br />
“Now we are working to source<br />
as many 4x4s and quadbikes as<br />
we can, as they can handle the<br />
terrain and can be used to get<br />
people who need help out fast.”<br />
Anyone interested in donating<br />
funds can donate via the<br />
GoFundMe campaign https://<br />
gofund.me/6f85e7e2 and contact<br />
Dr Telpov through the page.<br />
Staff from East of<br />
England <strong>Ambulance</strong><br />
Service (EEAST)<br />
have taken part in<br />
a series of realistic<br />
emergency planning<br />
exercises designed<br />
to prepare them<br />
for emergency<br />
situations that are<br />
not encountered<br />
every day.<br />
One recent exercise at Sutton<br />
Bridge featured a simulated<br />
explosion on a ship and<br />
involved water rescue, rescue<br />
at height and saw EEAST<br />
crews and the Norfolk Fire<br />
and Rescue Service (NFRS)<br />
colleagues working closely<br />
together to practice triage<br />
and treatment of multiple<br />
casualties.<br />
EEAST’s participation was<br />
co-ordinated by Peterborough<br />
Mentoring, Support and Training<br />
Team with additional input from<br />
their Hazardous Area Response<br />
Teams, patient transport and<br />
make-ready teams. Police and<br />
community first responders<br />
also attended.<br />
The EEAST staff who attended<br />
were all on rest days and were<br />
drawn from a wide range<br />
of clinical grades including<br />
BSc students from Anglia<br />
Ruskin University.<br />
These exercises are in addition<br />
to the regular staff training,<br />
and are designed to offer<br />
high-quality, fully-immersive<br />
training to challenge staff with<br />
situations they may not encounter<br />
very often.<br />
Exercises have simulated a wide<br />
range of scenarios, including<br />
burns, heat related illness,<br />
trauma, shootings, drownings,<br />
and a stabbing in a nightclub.<br />
The exercises are open to all,<br />
regardless of clinical grade.<br />
“All we ask is a willingness to<br />
learn and get involved and we’ve<br />
had very positive feedback from<br />
all our attendees,” said Leading<br />
Operations Manager Laura<br />
Kitchen, who has co-ordinated<br />
22<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
the events with other EEAST and<br />
Fire and Rescue colleagues.<br />
“This is a great example of staff<br />
across EEAST working together<br />
and freely giving up their time<br />
to help colleagues, as well as<br />
an excellent example of EEAST<br />
working with other emergency<br />
services and external agencies.<br />
“It also shows that EEAST offers<br />
immersive and high-fidelity<br />
training to staff and students,<br />
which is undoubtedly of value<br />
in terms of recruitment and<br />
staff retention.”<br />
Peterborough Mentoring, Support<br />
and Training Team (MST) was<br />
formed four years ago to support<br />
all staff that were on a Learning<br />
or Preceptorship pathway,<br />
offer support to all staff who<br />
may have clinical questions,<br />
require support and to develop<br />
operational training, irrespective<br />
of their grade.<br />
North West<br />
<strong>Ambulance</strong> Service<br />
helps identify<br />
patients with<br />
undiagnosed high<br />
blood pressure<br />
North West <strong>Ambulance</strong> Service<br />
(NWAS) has successfully<br />
piloted an initiative in Greater<br />
Manchester to help identify<br />
previously unknown cases<br />
of hypertension and is now<br />
working to scale this up to be<br />
rolled out region-wide.<br />
Having high blood pressure, or<br />
hypertension, is a main factor<br />
causing heart attacks and<br />
strokes. Over one third of adults<br />
in England have high blood<br />
pressure, but three in 10 of those<br />
don’t know they have it. Being<br />
aware of having high blood<br />
pressure is a first step to prevent<br />
heart attacks and strokes as this<br />
can be lowered to healthy levels<br />
and therefore reduce the risk.<br />
Using secure email data transfer<br />
of electronic patient records, the<br />
initial pilot involved analysing data<br />
of NWAS patients who had a high<br />
blood pressure reading during<br />
clinical observations on scene.<br />
Where the patient was cared<br />
for in the community without<br />
the need to be taken to hospital<br />
for immediate follow up care,<br />
blood pressure patient data was<br />
shared with the local primary care<br />
network so that patients could<br />
be called for review to confirm<br />
or discard hypertension by their<br />
GP, and a treatment plan initiated<br />
if necessary.<br />
From 71 records shared, the pilot<br />
helped to identify 14 new cases<br />
of hypertension, borderline cases<br />
or cases needing management<br />
review. After analysing these<br />
results, the data suggests that<br />
by sharing high blood pressure<br />
readings with primary care<br />
networks across the region,<br />
around 500 new cases of<br />
hypertension could be diagnosed<br />
using just one month of data.<br />
Work is now ongoing with<br />
integrated care boards and<br />
cardiovascular disease prevention<br />
groups, including GPs and<br />
community pharmacies across<br />
the region to scale up this pilot<br />
and allow the data to be shared<br />
with them in a secure, scalable,<br />
and manageable way.<br />
Medical Director for NWAS,<br />
Chris Grant said: “This project<br />
really highlights how we’re using<br />
advancements, such as our<br />
electronic patient records, to<br />
work together with our partners<br />
within the NHS to make a real<br />
difference to the health of<br />
our patients.<br />
“Learning from this pilot will help<br />
us to improve our data sharing<br />
processes and understand the<br />
potential of this in supporting<br />
prevention in other areas.<br />
pioneering simplicity<br />
new<br />
Repose, a source<br />
of Solace for those<br />
at risk this winter<br />
Pressure damage can develop<br />
within hours during delayed<br />
ambulance handovers<br />
The Repose ® Solace overlay is an<br />
effective pressure redistribution<br />
and reduction support surface for<br />
ambulance stretchers that enhances<br />
comfort and maintains patient dignity<br />
Scan to learn more or<br />
please visit our website<br />
www.frontier-group.co.uk<br />
GP0112_B85_01<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
23
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
Preliminary data analysis has<br />
also indicated hypertension rates<br />
were significantly higher in most<br />
deprived areas, so we’ll pay<br />
particular attention to whether<br />
this work can also support in<br />
reducing health inequalities.”<br />
NWAS is now working with health<br />
and local authority partners from<br />
North East and North Cumbria<br />
Integrated Care System, to<br />
explore ways of automatically<br />
sharing blood pressure data<br />
from all NWAS patients in<br />
North Cumbria who do not<br />
need to be taken to hospital for<br />
further treatment.<br />
Chris continues: “By rolling out<br />
this initiative further, we hope to<br />
identify cases of hypertension<br />
in people who may otherwise<br />
not have known they had high<br />
blood pressure. However, where<br />
possible we encourage people to<br />
get their blood pressure checked<br />
out themselves regularly so that<br />
any risk factors can be managed.”<br />
A blood pressure test is a simple<br />
way of checking if someone’s<br />
blood pressure is too high or too<br />
low. This can be carried out at<br />
a number of places, including<br />
at home – using a patient’s<br />
own digital blood pressure<br />
monitor, a local pharmacy and<br />
GP practice, at an NHS Health<br />
Check appointment (offered to<br />
adults in England aged 40-74),<br />
or even in some opticians and<br />
supermarkets.<br />
Unexpected arrival in<br />
the departure lounge<br />
When a mother suddenly went<br />
into labour in Luton Airport’s<br />
departure lounge, airport staff<br />
and passing air crew all went<br />
to her aid while EEAST 999<br />
call-handler Megan Byrne<br />
talked them through making a<br />
successful and safe delivery.<br />
Megan recently travelled to Luton<br />
Airport where she met in-person<br />
the people she had talked<br />
through delivering the baby - from<br />
EEAST’s <strong>Ambulance</strong> Control<br />
Centre in Norwich.<br />
Megan said: “The 999 alert<br />
was raised by a passing pilot<br />
who followed my instructions to<br />
prepare the mother for delivery.<br />
Melanie Horwood, the Terminal<br />
Duty Officer arrived on scene,<br />
took control of the situation and<br />
began assisting the birth which<br />
was progressing quickly. The<br />
pilot relayed my instructions<br />
onto her until the baby was born<br />
and I could hear it crying in<br />
the background.”<br />
Various members of staff from<br />
Luton Airport offered assistance,<br />
including retail staff and Luton<br />
Airport Fire Department, by<br />
bringing first aid supplies,<br />
blankets and even translating<br />
what was happening to the<br />
mother who didn’t speak English.<br />
The ambulance crew arrived<br />
shortly after and mother and<br />
baby were transported to<br />
Luton and Dunstable Hospital.<br />
They are believed to be doing<br />
well and have returned to their<br />
own country.<br />
Megan has been with EEAST for<br />
four years, having decided while<br />
studying for a geography degree<br />
that she really wanted to work in<br />
an ambulance call centre.<br />
However, this was not the first<br />
baby she had helped deliver over<br />
the phone: “I’ve been quite lucky,<br />
I’ve been involved in delivering<br />
around eight babies,” she said.<br />
“Sometimes callers are in very<br />
obscure locations, such as the<br />
side of the road when people have<br />
not made it to hospital in time. But<br />
never before in an airport.”<br />
Since helping deliver the<br />
baby, Megan has now started<br />
a new role in EEAST, where<br />
she will bring her knowledge<br />
of call handling to our Patient<br />
Safety Teams.<br />
A poignant day as Air<br />
<strong>Ambulance</strong> Charity<br />
Kent Surrey Sussex<br />
remember Graham,<br />
Mark and Tony, 25<br />
years on<br />
On 26th July Air <strong>Ambulance</strong><br />
Charity Kent Surrey Sussex<br />
(KSS) remembered the<br />
dedication and devotion<br />
of crew members Graham<br />
Budden, Mark Darby and Tony<br />
Richardson, three incredible<br />
men who sadly lost their lives<br />
in a helicopter accident whilst<br />
serving with the charity, 25<br />
years ago.<br />
(Wreaths were laid at the<br />
memorial stone at Blue<br />
Bell Hill)<br />
In a private remembrance<br />
ceremony held in the morning,<br />
family members, Team KSS<br />
colleagues, volunteers and<br />
representatives from other<br />
emergency services, gathered at<br />
the memorial stone at Blue Bell<br />
Hill in honour of Graham, Mark<br />
and Tony.<br />
Some of those who gathered<br />
placed wreaths at the base<br />
of the memorial stone in<br />
memory of each crew member,<br />
including Barney Burgess,<br />
Chair of the charity’s Board of<br />
Trustees and Medical Director<br />
Dr Duncan Bootland.<br />
A poignant three-minute silence<br />
at 11am followed, as all who<br />
were gathered paused to reflect<br />
on the ultimate sacrifice made<br />
by Graham, Mark and Tony,<br />
whilst working to save the lives<br />
of others. A helicopter from KSS<br />
then circled overhead three<br />
times to honour the life of each<br />
crew member.<br />
(The Very Reverend John<br />
Richardson, Vicar of Maidstone<br />
led the service)<br />
A Memorial Service was held at<br />
2pm at The Collegiate Church of<br />
All Saints, Maidstone, led by The<br />
Very Reverend John Richardson,<br />
Vicar of Maidstone. The service<br />
was attended by family members,<br />
Team KSS colleagues, volunteers,<br />
supporters, representatives of<br />
other emergency services and<br />
friends of Graham, Mark and<br />
Tony. During the service Graham,<br />
Mark and Tony’s commitment<br />
and service to the charity and<br />
the communities it serves was<br />
honoured. A KSS helicopter<br />
circled in the sky above the<br />
church as guests were departing.<br />
Guests departing from the<br />
memorial service at All Saints<br />
Collegiate Church, Maidstone<br />
Later in the day, a memorial<br />
bench dedicated to Graham,<br />
Mark and Tony to mark the 25th<br />
anniversary was unveiled at<br />
the charity’s Rochester base.<br />
Memorial plaques dedicated to<br />
the three crew members were<br />
also unveiled at both the charity’s<br />
Rochester and Redhill bases.<br />
(The memorial bench in<br />
memory of Graham, Mark<br />
and Tony at the charity’s<br />
Rochester HQ)<br />
Barney Burgess reflected: “It has<br />
been an incredibly poignant day<br />
for the families, Team KSS, our<br />
communities, and all who knew<br />
and loved Graham, Mark and<br />
Tony, as we joined together to<br />
24<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
mark the 25th anniversary. We will<br />
always remember their dedication<br />
and devotion to the charity as we<br />
continue to honour their memory<br />
and legacy of saving lives.<br />
The inspection of the Trust’s<br />
apprenticeship programmes<br />
took place in June <strong>2023</strong> and<br />
included the clinical <strong>Ambulance</strong><br />
Support Worker, which includes<br />
Overall effectiveness – Good<br />
The quality of education –<br />
Good<br />
Behaviour and attitudes –<br />
Outstanding<br />
The areas identified for<br />
improvement are already part of<br />
an ongoing Quality Improvement<br />
Plan being implemented by<br />
the Trust.<br />
“Graham, Mark and Tony are<br />
forever in our hearts and our<br />
thoughts are with their loved<br />
ones, especially today.”<br />
Yorkshire<br />
<strong>Ambulance</strong> Service’s<br />
apprenticeship<br />
provision has been<br />
hailed as good with<br />
outstanding features,<br />
following a full<br />
Ofsted inspection.<br />
The Trust currently has 587<br />
apprentices in both clinical<br />
roles and corporate services<br />
which accounts for 9% of the<br />
workforce (the Government<br />
target is 2.3%).<br />
advanced and emergency driving,<br />
and the Associate <strong>Ambulance</strong><br />
Practitioner roles.<br />
The Ofsted inspectors were<br />
impressed by the behaviour of<br />
the apprentices, their extremely<br />
positive attitudes to learning and<br />
the way in which they support<br />
and constructively challenge each<br />
other to develop their skills.<br />
The inspectors recognised the<br />
expertise of YAS Educators,<br />
the well-planned curriculum<br />
and quality of assessments.<br />
Learner support was deemed<br />
strong with Educators building<br />
the confidence and resilience of<br />
apprentices very effectively.<br />
Personal development –<br />
Outstanding<br />
Leadership and management<br />
– Good<br />
Apprenticeships – Good<br />
Safeguarding – Effective<br />
Dawn Adams, Associate Director<br />
of Education and Organisational<br />
Development (Interim) for<br />
Yorkshire <strong>Ambulance</strong> Service,<br />
said: “I am exceptionally proud<br />
of our apprenticeship provision<br />
in YAS. Our achievement rates<br />
are strong and distinction rates<br />
are excellent. I would like to take<br />
this opportunity to thank all our<br />
apprentices for their hard work<br />
and determination to succeed,<br />
and to thank all those who<br />
support our apprentices; it really<br />
does make a difference.”<br />
The Ofsted report follows on from<br />
the announcement that Yorkshire<br />
<strong>Ambulance</strong> Service was named<br />
as the top-rated NHS trust in<br />
England at number 36 of the Top<br />
100 Apprenticeship Employers.<br />
This list is produced annually by<br />
the Department for Education.<br />
<strong>Ambulance</strong> service<br />
research aims to<br />
support callers<br />
experiencing<br />
loneliness<br />
A collaborative research<br />
project aims to inform<br />
new guidance supporting<br />
people who call ambulance<br />
services frequently.<br />
Specialist Patient<br />
Transport<br />
Services<br />
IPRS MTS supplies general and specialist<br />
patient transport services across the <strong>UK</strong> and<br />
also to and from Europe.<br />
Our Services:<br />
High Dependency Transfers<br />
Secure Mental Health Transfers<br />
Repatriation<br />
Bariatric Transfers<br />
www.IPRSMTS.com<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
25
NEWSLINE<br />
North East <strong>Ambulance</strong> Service<br />
have collaborated on a research<br />
project with Northumbria<br />
University that aims to inform<br />
new guidance for ambulance<br />
trusts supporting people who<br />
call frequently. Frequent callers<br />
can have a combination of<br />
complex mental and physical<br />
health issues, and may also be<br />
experiencing social issues such<br />
as loneliness and isolation.<br />
Gayle Fidler, Emergency<br />
Operations Centre Support<br />
Services Manager for NEAS has<br />
been working with researchers<br />
from Northumbria’s Department<br />
of Social Work, Education<br />
and Community Wellbeing<br />
to interview people who call<br />
frequently, frontline paramedics,<br />
health advisors and senior<br />
clinical advisors from NEAS in<br />
a bid to improve routes to the<br />
right support and interventions<br />
for patients.<br />
Director of Paramedicine at North<br />
East <strong>Ambulance</strong> Service, Andrew<br />
Hodge, said: “Patient care is our<br />
priority so it’s important for us<br />
to understand the nature of our<br />
calls and how we might further<br />
support our patients.<br />
“We are currently undergoing this<br />
research study with Northumbria<br />
University to support patients<br />
who experience loneliness and<br />
isolation and have felt the need to<br />
contact the ambulance service.<br />
“We work closely with other<br />
agencies to ensure that patients<br />
have access to a range of<br />
services that may be able to<br />
support them. Working with<br />
the university on this project,<br />
we hope to understand our<br />
patients better so that we can<br />
often greater support to them<br />
where needed.”<br />
Dr Tracy Collins from<br />
Northumbria, who has a clinical<br />
background in occupational<br />
therapy, is leading the study<br />
which has received funding<br />
support from the National<br />
Institute for Health and Care<br />
Research (NIHR) Clinical<br />
Research Network North East<br />
and North Cumbria’s Targeting<br />
Health Needs award.<br />
She is collaborating with Dr<br />
Jason Scott, a Chartered<br />
Psychologist and national<br />
academic lead for the Frequent<br />
Caller National Network<br />
(FreCaNN), which helps to inform<br />
ambulance service policy and<br />
practice in relation to frequent<br />
callers across the <strong>UK</strong>, and Senior<br />
Research Assistant Lisa Moseley,<br />
who comes from a career in<br />
social work.<br />
“It became clear from our<br />
conversations with colleagues<br />
and practitioners that ambulance<br />
trusts supporting people who<br />
call frequently often have social<br />
needs in addition to medical<br />
needs,” said Dr Collins.<br />
“We’re keen to know more about<br />
individual experiences and allow<br />
those people who do self-identify<br />
as being lonely and socially<br />
isolated to the ambulance service<br />
to have their voices heard. We<br />
need to begin to understand their<br />
unmet needs so we can begin<br />
to make recommendations for<br />
alternative routes of support.”<br />
Due to the sensitive nature of<br />
the topic, only people who self-<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
26<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
identify as lonely and socially<br />
isolated have been interviewed<br />
using open questions which<br />
gather information anonymously<br />
on their circumstances, social<br />
circle and community support<br />
networks. Their lived experience<br />
is being explored alongside the<br />
views of NEAS staff.<br />
Health advisors and paramedic<br />
crews dealing with contacts from<br />
people who call frequently have<br />
been featured in the popular BBC<br />
documentary, <strong>Ambulance</strong>, which<br />
followed and filmed with NEAS<br />
crews during series 9.<br />
The project follows a research<br />
paper published in the British<br />
Paramedic Journal by Dr<br />
Scott, Dr Collins and a group<br />
of expert authors from <strong>UK</strong><br />
ambulance services which<br />
analysed the impact of the<br />
COVID-19 pandemic on people<br />
who call frequently and how<br />
ambulance services in particular<br />
were adapting to suit changing<br />
patient needs.<br />
The team are currently analysing<br />
data from interviews with service<br />
users and staff and hope to be<br />
able to publish the research<br />
findings later this year.<br />
Plans to harness Northumbria’s<br />
research, education and<br />
knowledge exchange expertise<br />
to help meet the health and<br />
social needs of communities<br />
in the region and beyond are<br />
being developed as part of the<br />
University’s Centre for Health and<br />
Social Equity (CHASE).<br />
New route for nurses<br />
to join frontline at<br />
EEAST<br />
A new pathway for nurses to<br />
transfer their skills to frontline<br />
pre-hospital care is open at the<br />
East of England <strong>Ambulance</strong><br />
NHS Trust (EEAST).<br />
Introduced in November 2022,<br />
the new initiative has received<br />
excellent feedback from the<br />
nurses who have already made<br />
the move to pre-hospital practice<br />
at EEAST.<br />
The pre-hospital nurse<br />
practitioners, who must have a<br />
professional registration with the<br />
Nursing and Midwifery Council<br />
(NMC), work on the frontline<br />
alongside paramedics and other<br />
pre-hospital clinicians.<br />
After an induction and training<br />
programme over up to 30 weeks,<br />
the pre-hospital practitioners<br />
work to a similar scope of<br />
practice to a paramedic.<br />
David Young, who qualified as a<br />
nurse in 2001, was part of the first<br />
group of 14 nurses to go through<br />
the programme to become a<br />
pre-hospital nurse practitioner<br />
and is loving his new role on a<br />
frontline ambulance.<br />
Before starting at EEAST, David<br />
was a clinical nurse specialist<br />
in international emergency<br />
assistance and repatriations.<br />
David said:<br />
“Traditionally this type of role was<br />
never open to nurses and I had<br />
considered undertaking further<br />
study to become a paramedic<br />
during my 22 years as a nurse,<br />
but I never found the right time<br />
in my career to make the switch<br />
before this programme.<br />
“This role allows me to apply my<br />
previous nursing experience, but<br />
also to learn some challenging<br />
new skills such as emergency<br />
trauma care, advanced life<br />
support for all age ranges and<br />
emergency obstetric care.<br />
“As a nurse on a frontline<br />
ambulance, every day and every<br />
patient is different; one minute,<br />
we can be responding to a 999<br />
call to a woman in labour to<br />
deliver a baby, then the next<br />
a road traffic collision, cardiac<br />
arrest, or transferring a patient<br />
between hospitals and anything<br />
in between. You never know what<br />
you will be asked to do next,<br />
which is fantastic.<br />
“I love this job. I look forward to<br />
putting on my green uniform,<br />
getting to the station, getting in<br />
the ambulance, and waiting for<br />
control to allocate us a job. It’s<br />
amazing!”<br />
Melissa Dowdeswell, Director<br />
of Nursing and Interim<br />
Chief Operation Officer at<br />
EEAST, said:<br />
“This new programme allows<br />
nurses to transfer their extensive<br />
knowledge, experience and<br />
skills to working in a prehospital<br />
setting working<br />
alongside paramedics and other<br />
frontline clinicians.<br />
“The feedback from nurses on<br />
the programme and the support<br />
provided has been excellent<br />
which is why we are looking to<br />
expand the programme to further<br />
bolster our workforce.<br />
“The specialist skills that prehospital<br />
practitioners bring<br />
to EEAST will help enhance<br />
the service we provide to our<br />
communities.”<br />
London <strong>Ambulance</strong><br />
Service to provide<br />
NHS 111 services to<br />
North Central London<br />
London <strong>Ambulance</strong> Service<br />
(LAS) has been awarded<br />
the contract to provide NHS<br />
111 services, in partnership<br />
with London Central and<br />
West (LCW), to the 1.5 million<br />
people who live within North<br />
Central London.<br />
LAS and LCW will take on<br />
responsibility for 111 and GP<br />
out-of-hours service from<br />
November <strong>2023</strong> covering five<br />
London boroughs – Barnet,<br />
Camden, Enfield, Islington and<br />
Haringey. The new contract<br />
and accompanying new service<br />
model, which is worth £19 million<br />
per year, will have a number of<br />
benefits for patients, including<br />
an increase in ‘consult and<br />
complete’, meaning that patients’<br />
needs are met within two hours.<br />
Daniel Elkeles, Chief Executive<br />
for London <strong>Ambulance</strong> Service,<br />
said: “I’m so pleased that the<br />
North Central London Integrated<br />
Care System awarded their<br />
111 contract to LAS as the lead<br />
provider in partnership with<br />
London Central and West. We<br />
will use the strengths of both<br />
organisations to put in place<br />
more responsive care models<br />
for both the 111 and GP out-ofhours<br />
services.<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
27
NEWSLINE<br />
“Our hard working staff are<br />
experts in receiving and<br />
responding to urgent and<br />
emergency calls, and this latest<br />
development builds on our years<br />
of experience of hosting the<br />
NHS 111 service in other areas<br />
of London. It will allow us to<br />
bring together our emergency<br />
and urgent care services for an<br />
additional 1.5 million people, and<br />
we are very excited to begin.<br />
“This latest development means<br />
we are now the lead or sole<br />
provider of 111 in four of the five<br />
areas of London (South East,<br />
North East, North West and North<br />
Central) with a small role in South<br />
West London, so we’re extending<br />
our footprint to cover all of<br />
London for this service.<br />
“It really is a great example of LAS<br />
working in partnership with other<br />
providers to create a compelling<br />
North West<br />
<strong>Ambulance</strong> Service<br />
boosts resilience<br />
ahead of Winter<br />
As the darker evenings set in<br />
and the temperature drops,<br />
North West <strong>Ambulance</strong> Service<br />
(NWAS) is putting plans in<br />
place to ensure it can continue<br />
to deliver a high-quality<br />
service despite additional<br />
winter demands, including the<br />
recruitment of more than 700<br />
new staff members.<br />
By Christmas, 75 new<br />
paramedics and 32 emergency<br />
medical technicians will have<br />
joined the team, with more due<br />
to be in post by March 2024.<br />
There will be 72 new recruits for<br />
the Patient Transport Service and<br />
250 new call handlers for the 999<br />
and NHS 111 contact centres.<br />
that the high-quality service<br />
expected by our patients is<br />
maintained throughout the<br />
winter period.<br />
“We know that the winter months<br />
will bring with it additional<br />
challenges in terms of more<br />
people needing our help, ongoing<br />
industrial action taking place<br />
across the healthcare system and<br />
an expected increase of seasonal<br />
illnesses, but we are as prepared<br />
as we can be for increased<br />
demands on our service.<br />
North West<br />
<strong>Ambulance</strong> Service<br />
hospital handover<br />
collaboration<br />
shortlisted for<br />
HSJ Award<br />
26 emergency departments. The<br />
work began in <strong>October</strong> 2022<br />
and involved getting together to<br />
come up with innovative ideas<br />
and putting them into action.<br />
There was then an evaluation<br />
process to measure the impact<br />
before coming back together to<br />
share findings and next steps in<br />
May <strong>2023</strong>.<br />
This initiative has been selected<br />
to make the HSJ Awards shortlist<br />
following a thorough judging<br />
process which whittled down a<br />
record-breaking 1,456 entries<br />
to 223 shortlisted projects,<br />
making it the biggest awards<br />
programme in the award’s<br />
43-year history. The high<br />
volume - and exceptional quality<br />
– of applications once again<br />
mirrors the impressive levels of<br />
innovation and care continually<br />
being developed within the <strong>UK</strong>’s<br />
healthcare networks.<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
offer for our commissioners and a<br />
good deal for patients.”<br />
Fred Worth, Chairman of London<br />
Central & West UCC Ltd, said:<br />
“As a GP-led not-for-profit<br />
organisation, we are proud to<br />
play such a vital part in ensuring<br />
patients can access urgent<br />
care quickly. Working with our<br />
partners, we have demonstrated,<br />
over many years, the value that<br />
LCW brings to the healthcare<br />
system and are delighted<br />
to continue to deliver this<br />
service to the patients of North<br />
Central London.”<br />
Patients and members of the<br />
public will also benefit from<br />
having direct access to a<br />
multidisciplinary team of LAS<br />
professionals within the Clinical<br />
Assessment Service which will<br />
mean more timely access to<br />
assessments, greater clinical<br />
oversight and an increased use<br />
of alternative pathways to ensure<br />
access to the right service,<br />
first time.<br />
NWAS is also increasing the<br />
number of clinicians working in<br />
its 999 contact centres. They<br />
help get patients the right care<br />
for their needs by providing<br />
healthcare advice over the<br />
phone or making referrals to an<br />
alternative health or care service<br />
in the community.<br />
An additional 32 emergency<br />
ambulances will be out<br />
responding to patients by<br />
February, increasing the number<br />
of emergency ambulances<br />
operating across the region<br />
to 553.<br />
NWAS will continue to work<br />
closely with local hospitals to<br />
help reduce the amount of time<br />
ambulances spend waiting to<br />
handover patients, allowing<br />
vehicles and crews to be free to<br />
respond to the next emergency.<br />
Chief Operating Officer, Salman<br />
Desai said: “As always, we are<br />
here for the public when they<br />
need us most and we have<br />
robust plans in place to ensure<br />
North West <strong>Ambulance</strong> Service<br />
(NWAS) has been shortlisted<br />
for a Health Service Journal<br />
(HSJ) Award in the Patient<br />
Safety category after working<br />
with North West NHS trusts<br />
in a series of collaborative<br />
events to share ideas and best<br />
practice for improving hospital<br />
handovers.<br />
The improvement collaborative<br />
has helped to reduce the number<br />
of over 60 minute handover<br />
delays in the North West by 47<br />
per cent, only slightly short of the<br />
its target of achieving a 50 per<br />
cent reduction by 31 March <strong>2023</strong>.<br />
The joined-up approach led by<br />
NWAS alongside NHS health<br />
and care quality improvement<br />
organisation Aqua and NHS<br />
England North West included<br />
representatives from 20 NHS<br />
trusts across the region covering<br />
Director of Quality, Innovation and<br />
Improvement, Maxine Power said:<br />
“It’s a fantastic achievement to be<br />
shortlisted for such a prestigious<br />
award. I am exceptionally proud<br />
of what has been achieved by<br />
working together to provide our<br />
patients with a better experience<br />
when they use our services.<br />
A huge well done to all the<br />
passionate people involved who<br />
have worked exceptionally hard to<br />
drive forward change and make a<br />
real difference.”<br />
Some of the improvements that<br />
have been put in place as part<br />
of the collaboration include<br />
managing surges of patients<br />
presenting at hospitals over a<br />
short period, using daily data to<br />
support decision making and<br />
going back to basics by looking<br />
at ways to make improvements to<br />
existing processes.<br />
HSJ editor Alastair McLellan,<br />
adds; “It always gives me great<br />
pleasure to congratulate our<br />
finalists at this stage of the<br />
judging process and this year is<br />
28<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
no exception as we acknowledge<br />
the North West hospital handover<br />
improvement collaborative for<br />
being shortlisted in the category<br />
of Patient Safety.<br />
“It’s been so encouraging to hear<br />
that <strong>2023</strong> has been recordbreaking<br />
in terms of the number<br />
of applicants and, as ever, the<br />
calibre of entries left our panel of<br />
expert judges with some tough<br />
decisions to deliberate over.<br />
However, it’s always important<br />
to remember that the HSJ<br />
Awards are not just a celebration<br />
of success stories but also a<br />
platform to shape the future of<br />
the NHS.<br />
“We can’t wait to welcome our<br />
finalists to the awards ceremony<br />
in November and to recognise<br />
and applaud such impressive<br />
achievements across the sector.”<br />
The official HSJ Awards<br />
ceremony will be held on<br />
16 November <strong>2023</strong> at<br />
Evolution London.<br />
New website given<br />
the Bluelight<br />
Bluelight <strong>UK</strong> Ltd, a trusted<br />
provider of ambulances, is<br />
poised for an exciting journey<br />
ahead. This North West<br />
based ambulance provider is<br />
thrilled to unveil its redesigned<br />
website, marking a significant<br />
milestone in its evolution.<br />
When Bluelight <strong>UK</strong> ventured<br />
into the online realm back<br />
in the early Noughties, the<br />
company held ambitious<br />
aspirations for its ambulance<br />
startup and the impact it<br />
could make.<br />
In the early 2000s, the landscape<br />
of search engine optimisation<br />
and social media was quite<br />
distinct, with platforms like AOL<br />
and Windows Messenger leading<br />
the way. Reflecting on that era,<br />
Bluelight <strong>UK</strong>’s CEO, Simon<br />
Forster, reminisced, “In the early<br />
days, companies like ours relied<br />
on word-of-mouth referrals and<br />
in-person networking, supported<br />
by market-specific advertising.<br />
The technology and social media<br />
landscape we have today were<br />
beyond our reach, limiting our<br />
options for expanding our reach<br />
as a small startup.”<br />
He continued, “Today, platforms<br />
such as LinkedIn, Instagram,<br />
Meta (formerly Facebook), and X<br />
(formerly Twitter) are vying for our<br />
attention. While we still welcome<br />
visits to Bluelight <strong>UK</strong> depots for<br />
our clients, we recognise the<br />
growing demand for high-quality<br />
vehicles with swift turnaround<br />
times. Increasingly, our clients<br />
turn to the web for their vehicle<br />
searches, which is why we<br />
have invested substantially in<br />
revamping our website to cater<br />
to their needs. Collaborating<br />
closely with our designers, we<br />
have found an effective way to<br />
provide a vastly improved user<br />
experience on our website. Our<br />
initial testing has yielded highly<br />
positive results. Our enduring<br />
mission has always been to<br />
deliver value to our clients, and<br />
we believe that our revamped<br />
website will not only save our<br />
clients valuable time but also<br />
offer a seamless ambulance<br />
purchasing experience. We<br />
extend our heartfelt gratitude to<br />
our clients for their unwavering<br />
loyalty and support, eagerly<br />
anticipating the opportunity to<br />
collaborate with even more of<br />
you in the future.”<br />
As Bluelight <strong>UK</strong> approaches its<br />
20th-year anniversary, it stands<br />
as a testament to the dedication<br />
of its founders, Simon and Julie<br />
Forster, who have been part of<br />
the motor industry since 1986.<br />
Julie Forster, Bluelight <strong>UK</strong>’s CFO,<br />
shared, “Our careers began<br />
separately in the motor industry<br />
in 1986, culminating in our<br />
small family-run startup, which<br />
we initiated right on our front<br />
driveway. We take immense pride<br />
in the service we’ve crafted and<br />
are enthusiastic about the future<br />
of Bluelight <strong>UK</strong>.”<br />
Explore their new website for<br />
yourself at www.bluelightuk.<br />
co.uk. Exciting times await!<br />
Student sets heart<br />
on medical career<br />
after his stopped six<br />
times in one day<br />
A student whose heart stopped<br />
six times in a few hours has<br />
thanked the NHS doctors,<br />
nurses and paramedics who<br />
saved his life and pledged to<br />
use his ‘second chance’ to<br />
follow in their footsteps.<br />
Atul Rao, a US citizen, was<br />
studying in London when a<br />
blood clot in his lungs stopped<br />
the blood flow through his heart,<br />
a condition called pulmonary<br />
embolism, and caused him to go<br />
into cardiac arrest.<br />
He was discovered collapsed by<br />
fellow students who raised the<br />
alarm before an Imperial College<br />
London security guard began<br />
to give him chest compressions<br />
(CPR) in the minutes before<br />
London <strong>Ambulance</strong> Service<br />
crews arrived. Paramedics were<br />
able to get his heart beating<br />
again and they took him to<br />
Hammersmith Hospital’s heart<br />
attack centre where scans<br />
confirmed that blood clots in the<br />
lungs were blocking the flow of<br />
blood from the heart.<br />
Staff at Hammersmith Hospital<br />
worked tirelessly through the<br />
night to keep Atul alive and<br />
stabilise him but his heart<br />
stopped a further five times<br />
in that first 24 hours before<br />
clot-busting drugs began to<br />
work and Atul’s heart started<br />
beating reliably.<br />
He was still critically unwell<br />
when he was transported to<br />
St Thomas’ Hospital the next<br />
day in case he needed access<br />
to extracorporeal membrane<br />
oxygenation (ECMO) – a life<br />
support system which can fully<br />
replace the work of the heart and<br />
lungs so that patients have time<br />
to heal. Fortunately, the clotbusting<br />
drugs had begun to work<br />
and with the help of other life<br />
support machines, he was able<br />
to recover without the need for<br />
ECMO. Atul made a remarkable<br />
recovery over the next two<br />
weeks and was discharged from<br />
St Thomas’ Hospital.<br />
Atul, who is from Seattle and<br />
studies at Baylor University in<br />
Texas, visited Hammersmith<br />
Hospital with mum Srividhya<br />
and dad Ajay earlier this month.<br />
They were shown the bed space<br />
where his heart was repeatedly<br />
restarted and spoke to clinicians<br />
about what happened to Atul in<br />
those hours where his life was in<br />
the balance on 27 July. The family<br />
told the doctors, nurses and<br />
paramedics they were ‘thankful<br />
beyond words’ for the efforts they<br />
made to save his life.<br />
Atul told the staff it has helped<br />
him decide what he wants to do<br />
with his life. He is in his final year<br />
of a pre-med degree in his native<br />
USA which would allow him to go<br />
on to a further degree to practice<br />
medicine. But speaking to the<br />
London NHS staff he revealed<br />
that prior to his cardiac arrest, he<br />
had begun to have doubts about<br />
his original career choice.<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
29
NEWSLINE<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
He said:<br />
“Before this happened, I was<br />
starting to wonder if I was doing<br />
the right thing doing medicine<br />
and whether I should be going<br />
into business instead. But the<br />
minute I woke up I knew. I want to<br />
use my time in a productive way. I<br />
want to use my second chance at<br />
life by helping others.”<br />
His mum, Srividhya, a Maths<br />
professor in Seattle, said:<br />
“A really bad thing happened in a<br />
really good place. Everyone who<br />
worked around Atul wanted him<br />
to be well. It’s clear they love and<br />
care about what they do. I feel<br />
blessed to be here and I’m so<br />
thankful and grateful to you for<br />
giving my son back to me.<br />
“I have gained perspective about<br />
life and he gets to see it at such a<br />
young age. His life has changed,<br />
and it’s had a profound impact.”<br />
Atul agrees. Having spent his 21st<br />
birthday in a hospital bed with his<br />
parents and some student friends<br />
he said:<br />
“Most 21-year-olds want to go out<br />
drinking. Given how dangerous<br />
my situation had been, I was<br />
grateful to be here and have<br />
people who love me around<br />
to celebrate.”<br />
Dad Ajay, who works at a<br />
software company, remembered<br />
how London <strong>Ambulance</strong> Service<br />
Advanced Paramedic (APP) Nick<br />
Sillett broke the news that Atul<br />
was critically ill from the scene via<br />
his son’s mobile. He showed Nick<br />
the barely legible notes he took<br />
during the call, his hands shaking,<br />
and spoke of his agonising flight<br />
over to London after knowing<br />
decisions were being made which<br />
could affect whether his son<br />
would live.<br />
Remembering a turning point,<br />
Ajay said:<br />
“At the start Atul was sedated. I<br />
used to call St Thomas’ Hospital<br />
ICU in the mornings after the<br />
doctors’ rounds to ask for news<br />
and one morning they said ‘hold<br />
on’. Then I heard Atul come on<br />
and say ‘hey, dad’. It was the<br />
sweetest ‘hey, dad’ I have ever<br />
heard and I wanted to run to him<br />
right away.”<br />
Thanking the NHS staff, he<br />
added:<br />
“I’m not exaggerating,<br />
Hammersmith and St Thomas’<br />
hospitals have become places<br />
of worship for us. We will be<br />
coming here whenever we come<br />
to London.<br />
“It was the heroic efforts of<br />
London <strong>Ambulance</strong> Service,<br />
the amazing medical teams of<br />
Hammersmith, St Thomas’ and<br />
Royal Brompton that saved him<br />
from this life-threatening series<br />
of events.”<br />
The couple did not have much<br />
time to appreciate London on<br />
this first visit. So concerned<br />
were they about their son in<br />
the immediate aftermath of his<br />
recovery, they walked by Big Ben<br />
for several days on the way to St<br />
Thomas’ Hospital before realising<br />
they were passing the iconic<br />
landmark. Every time they heard<br />
an ambulance pass they say<br />
they were praying for the patients<br />
inside and the medics who would<br />
be caring for them.<br />
APP Nick Sillett, said the reunion<br />
had been very emotional.<br />
“The last time I saw Atul I didn’t<br />
think he was going to survive. To<br />
meet him again and speak with<br />
his parents after giving them such<br />
terrible news was a very special<br />
moment in my 18 years in this<br />
job. Knowing we managed to<br />
save Atul gives me courage and<br />
hope should I encounter that<br />
situation again.<br />
“The LAS crew first on scene<br />
also were the real heroes in<br />
recognising so quickly he was in<br />
cardiac arrest and managed to<br />
give him a chance.”<br />
Dr Louit Thakuria, a Critical<br />
Care Consultant at Imperial<br />
College Healthcare NHS Trust’s<br />
Hammersmith Hospital, said:<br />
“It’s not often you see 20-yearolds<br />
have a cardiac arrest and it’s<br />
even more rare to see someone<br />
who has had six cardiac arrests in<br />
one day make such a miraculous<br />
recovery.<br />
“This was a real team effort and<br />
so many people helped ensure<br />
Atul was able to be here. It’s a<br />
privilege to be a part of that and<br />
hear that you have helped make<br />
such a positive impact.”<br />
Dan Taylor, an intensive care and<br />
ECMO consultant at Guy’s and<br />
St Thomas’ NHS Foundation<br />
Trust, said:<br />
“Atul had a very challenging<br />
combination of problems which<br />
required input from multiple<br />
specialist teams. Thankfully his<br />
heart failure improved and he was<br />
able to avoid ECMO, but he spent<br />
several days critically ill in the<br />
intensive care unit.<br />
“The whole team are delighted<br />
that Atul has made such a great<br />
recovery, and we wish him the<br />
very best in his medical career in<br />
the future.”<br />
There are many known risk<br />
factors that can contribute to<br />
the development of a pulmonary<br />
embolism, like prolonged<br />
air travel. Now that Atul has<br />
recovered from his cardiac<br />
arrests, he is having tests to<br />
investigate the underlying<br />
cause for the formation of this<br />
dangerous blood clot in the<br />
lungs. Once doctors agreed<br />
it was safe, he was allowed to<br />
return home to the US.<br />
His case shows the importance<br />
of receiving good chest<br />
compressions in the immediate<br />
aftermath of a cardiac arrest.<br />
London <strong>Ambulance</strong> Service’s<br />
London Lifesavers campaign<br />
aims to train up thousands of<br />
Londoners with the knowledge<br />
and confidence to act in an<br />
emergency situation until<br />
ambulance crews arrive at<br />
the scene. Evidence shows<br />
that in cardiac arrest, every<br />
second counts and early chest<br />
compressions and defibrillation<br />
can more than double someone’s<br />
chances of survival.<br />
Meanwhile, with support from<br />
Imperial Health Charity, Imperial<br />
College Healthcare are currently<br />
working to develop an ECMO<br />
service at Hammersmith Hospital<br />
to give critically ill patients the<br />
best chance of survival. ECMO is<br />
a highly specialised life-support<br />
machine that can completely<br />
replace the function of the failing<br />
heart and lungs in an emergency.<br />
The charity has funded one<br />
ECMO machine and a training<br />
programme for our ICU and<br />
cardiology teams, and is currently<br />
raising funds to purchase two<br />
additional ECMO machines in<br />
order to provide this life-saving<br />
service for patients.<br />
In England 28,000 patients have<br />
a cardiac arrest that requires<br />
cardiopulmonary resuscitation<br />
(CPR) outside of hospital, and<br />
only 8.6% of those patients<br />
will typically survive(1). Recent<br />
studies have shown that for<br />
some patients who are suitable<br />
for ECMO therapy, the number<br />
of potential survivors could rise<br />
to 43%(2).<br />
Find out more about Imperial<br />
Health Charity’s ECMO Appeal<br />
on the charity’s website.<br />
30<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
IN PERSON<br />
CEO of Essex & Herts Air<br />
<strong>Ambulance</strong> marks 20 years<br />
of loyal service to life saving<br />
charity<br />
In a milestone year for Essex & Herts Air<br />
<strong>Ambulance</strong> (EHAAT) marking 25 years of<br />
saving lives, colleagues and friends have paid<br />
tribute to CEO, Jane Gurney, as she reaches<br />
20 years of loyal service with the charity.<br />
At a special event held on Thursday 17th August<br />
at Earls Colne Business Park, members of the<br />
EHAAT ‘family’ joined Jane in celebrating not<br />
only her contribution to the charity, but also<br />
to the wider air ambulance sector nationally.<br />
As one of the longest-serving CEOs of a <strong>UK</strong><br />
air ambulance, she was also a Director for<br />
the Association of Air <strong>Ambulance</strong>s from 2013<br />
to 2019, and from 2016 to 2020, she was a<br />
Trustee on AA<strong>UK</strong>’s Board, which supports<br />
21 air ambulances around the country. A very<br />
special moment for Jane professionally, was<br />
when she received an honorary degree from the<br />
University of Essex last year, in recognition of her<br />
dedication to expand and improve pre-hospital<br />
care for those in need.<br />
Jane’s career with EHAAT started in 2003, when<br />
she joined the ‘driven and enthusiastic’ small<br />
team that were running Essex Air <strong>Ambulance</strong><br />
(EAA) out of a small side room at Broomfield<br />
Hospital in Chelmsford.<br />
Jane explains, “I remember waiting in EAA’s<br />
reception and overhearing the paramedics<br />
talking about this ‘flying ambulance’. I thought<br />
it was just absolutely amazing and sounded so<br />
inspirational.<br />
“I quickly knew this was something I wanted to<br />
be a part of. They desperately needed income,<br />
and as my previous job was Sponsorship and<br />
Events Manager in media, I knew I had the skills<br />
to help them, so I took on the role of Business<br />
Development Manager.”<br />
Over the following years Jane progressed into<br />
management and was appointed as CEO in<br />
2009. She has led the team and the charity<br />
through many milestones which have included:<br />
the launch of Herts Air <strong>Ambulance</strong> in 2007 and<br />
then its amalgamation with EAA to form Essex<br />
& Herts Air <strong>Ambulance</strong>; the establishment of its<br />
two dedicated airbases and visitor centres at<br />
Earls Colne in 2011, and North Weald in 2021;<br />
the purchase of the charity’s first wholly owned<br />
AW169 helicopter in 2017, and the charity<br />
achieving an ‘outstanding overall’ rating by the<br />
Care Quality Commission in 2022. Another<br />
immensely proud moment was hosting a visit by<br />
the former Earl and Countess of Wessex, Edward<br />
and Sophie, to EHAAT’s North Weald airbase.<br />
During Jane’s tenure, the charity has also<br />
taken massive steps forward in achieving its<br />
aim; to provide the highest possible standards<br />
of pre-hospital clinical care. Highlights have<br />
included: In 2008, doctors becoming part of<br />
the Helicopter Emergency Medical Services<br />
(HEMS) teams flying on missions, enabling more<br />
advanced clinical interventions to be delivered at<br />
the scene; starting to carry blood products on<br />
board in 2019, and more recently the launch of<br />
the Centre for Excellence, which aims to create<br />
a world-leading community through which prehospital<br />
care is developed to achieve the best<br />
possible outcomes for all patients.<br />
Dr Gareth Davies, Senior Medical Advisor<br />
at EHAAT, has been with the charity from its<br />
infancy. He said, “All of those who have worked<br />
with Jane over the years recognise her passion,<br />
drive and commitment. They have witnessed<br />
her compassion and support for the staff and<br />
the respect she has displayed for the partners<br />
in the external health economy. But only a<br />
few of us that are older, will have seen and<br />
recognise Jane’s commitment to our industry<br />
and how she helped shape the world we all<br />
live in today. Jane and a few of her industry<br />
colleagues set about 20 years ago setting the<br />
benchmarks for all the Air <strong>Ambulance</strong> Services<br />
in the <strong>UK</strong> today. What was a few small-scale<br />
charities working alongside NHS ambulance<br />
services 20 years ago is now an industry where<br />
charities are fully blown independent health<br />
care organisations, where only the highest CQC<br />
gradings will suffice. From the earliest days,<br />
Jane has been committed to professionalism at<br />
every level. Always there for her peers and with<br />
a willingness to support new CEO’s coming to<br />
join our community. She has championed the<br />
importance of clinical governance in a way the<br />
NHS still finds difficult today and had the instinct<br />
and vision to support the clinician’s aspiration of<br />
the future with EHAAT’s Centre for Excellence.<br />
It’s been a pleasure to work alongside Jane over<br />
the last 20 years.”<br />
Air <strong>Ambulance</strong>s <strong>UK</strong> CEO, Simmy Akhtar,<br />
said, “Huge congratulations to Jane on her<br />
20th anniversary with Essex & Herts Air<br />
<strong>Ambulance</strong>. Jane devoted six impactful years<br />
as a director of the national organisation and<br />
was passionate about championing and<br />
representing the invaluable work of the air<br />
ambulance community at a national level. Her<br />
tireless efforts have significantly shaped the<br />
Annual Conference and Awards of Excellence<br />
into the remarkable event it stands at today.<br />
Jane’s passion, unwavering commitment, and<br />
remarkable contributions continue to inspire<br />
the air ambulance sector and it is a pleasure<br />
to continue to work alongside Jane as we<br />
continue to collaborate on national issues.”<br />
Jonathan Trower, Chair of Trustees at EHAAT<br />
added, “The fact that the Essex and Herts<br />
Air <strong>Ambulance</strong> Trust has reached its 25th<br />
anniversary in such excellent health is, in<br />
no small measure, down to the determined<br />
leadership of Jane Gurney. So many<br />
congratulations are due to her on the 20th<br />
anniversary of her first employment by the<br />
charity. The progress that we have made over<br />
the last 20 years is remarkable and I know<br />
how much more Jane can achieve in the years<br />
to come”.<br />
However, perhaps the last words should come<br />
from Jane herself. She is humbled by the kind<br />
words and recognition of the impact she has<br />
made saying, “We have come a long way since<br />
our story began, and from our airbases at Earls<br />
Colne and North Weald, today we serve the<br />
communities of Essex, Hertfordshire and the<br />
surrounding areas. We have a Donation Centre<br />
in Stevenage and nine charity shops located<br />
in the very heart of our local communities. We<br />
have grown to over 140 team members and<br />
over 400 volunteers. Last year, we carried out<br />
2,582 missions, 1,346 by air ambulance and<br />
1,235 via our fleet of rapid response vehicles.<br />
“It has been a true privilege to lead Essex<br />
& Herts Air <strong>Ambulance</strong> through so many<br />
milestones over the years, and to work<br />
alongside our amazing supporters, our<br />
dedicated staff and volunteers and our highly<br />
skilled critical care teams. However, it goes<br />
without saying our patients and their families<br />
are the ones who truly inspire me and my team<br />
the most, to continue to deliver our life saving<br />
service today and into the future. Thank you<br />
to everyone who has been on this incredible<br />
journey with me – it has been an amazing<br />
privilege to be part of this very special charity<br />
and myself and the team look forward to many<br />
more rewarding years ahead.”<br />
To find out more or to donate visit<br />
www.ehaat.org.<br />
AMBULANCE <strong>UK</strong> – OCTOBER<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
31
Seamless Synchronisation<br />
Hands Free Resuscitation with the<br />
corpuls3 and corpulscpr.<br />
In the <strong>Ambulance</strong><br />
Emergency transport carries risk<br />
for the patient and the responding<br />
team. With synchronised therapy,<br />
the emergency team can remain<br />
seated whilst in transit. Rhythm<br />
control and shock delivery can be<br />
performed on the corpuls 3 while<br />
the medic is seated.<br />
In tight spaces<br />
Whether in a lift, a stairwell, or<br />
on tricky terrain, synchronised<br />
resuscitation means that therapy<br />
can continue where it wouldn’t<br />
have been possible before. Once<br />
in place, a medic can control the<br />
corpuls 3 monitor, defibrillator and<br />
CPR parameters of the corpuls cpr.<br />
In the air<br />
Patient access is extremely limited<br />
in air rescue. Thanks to the perfect<br />
interaction of the corpuls 3 with<br />
the corpuls cpr, movement within<br />
the cabin is reduced. Synchronised<br />
mechanical chest compressions<br />
can be given, without having to<br />
accept long hands-off times.<br />
• Shorter hands-off time.<br />
• Automated pre-shock compressions.<br />
• Can be used in manual and AED mode.<br />
• Increased safety & minimised interruptions.<br />
• Less resources required.<br />
• Easier operation.<br />
• Data transmission.<br />
• Post mission analysis.<br />
Learn more:<br />
Scan the QR code<br />
with your phone<br />
camera and click<br />
the link.<br />
Or visit:<br />
uqr.to/sync-cpr<br />
www.corpuls.co.uk<br />
Official <strong>UK</strong> supplier of corpuls and Weinmann<br />
medical devices and software.