Gastroenterology Today Winter 2023
Gastroenterology Today Winter 2023
Gastroenterology Today Winter 2023
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Volume 34 No. 4 <strong>Winter</strong> <strong>2023</strong>
CONTENTS<br />
CONTENTS<br />
<strong>Gastroenterology</strong> <strong>Today</strong><br />
4 EDITOR’S COMMENT<br />
7 FEATURE Timing of endoscopy in patients with cirrhosis<br />
and acute variceal bleeding: a single-center<br />
retrospective study<br />
19 FEATURE Non-alcoholic fatty liver disease in<br />
hemochromatosis probands with iron<br />
overload and HFE p.C282Y/p.C282Y<br />
26 COMPANY NEWS<br />
This issue edited by:<br />
Aaron Bhakta<br />
c/o Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
ADVERTISING & CIRCULATION:<br />
Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
Tel: 01886 853715<br />
E: info@mediapublishingcompany.com<br />
www.ambulanceukonline.com<br />
PUBLISHED DATES:<br />
March, June, September and December.<br />
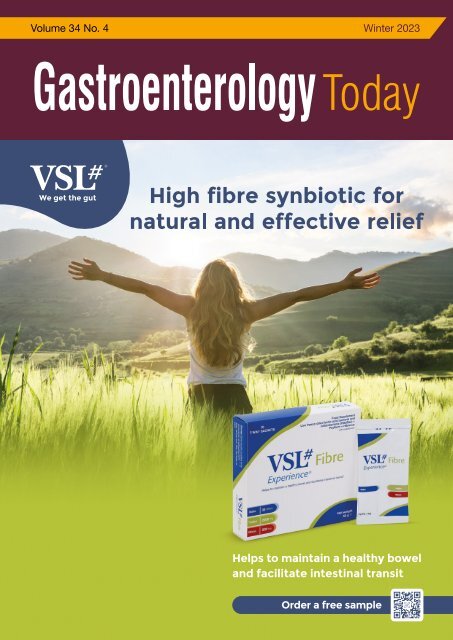
COVER STORY<br />
Have you met the newest member of the VSL# family? Introducing VSL# Fibre!<br />
For the 1 in 7 people in the UK struggling with constipation 1 , VSL# Fibre offers a unique<br />
combination of fibre, poly-biotics and hibiscus extract, to help maintain a healthy bowel<br />
and facilitate intestinal transit.<br />
Combining three natural ingredients, VSL# Fibre is designed to gently relieve symptoms of<br />
constipation, replenish the gut microbiota, and naturally restore a healthy bowel habit:<br />
COPYRIGHT:<br />
Media Publishing Company<br />
Greenoaks<br />
Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company<br />
• Psyllium husk: an effective soluble fibre bulking agent, recommended by NICE for the<br />
management of constipation 2,3<br />
• Live Cultures: 30 Billion CFU across 8 bacterial strains, proven to survive the harsh<br />
conditions of the stomach<br />
• Hibiscus Extract: a natural herbal extract packed with polyphenols 4<br />
Next Issue Spring 2024<br />
Designed in the UK by TGDH<br />
VSL# Fibre ® uses the same 8 diverse strains of bacteria found in one of the World’s<br />
most powerful probiotic – VSL#3, specifically designed to support and enrich the gut<br />
microbiome. Trusted by gastroenterologists from across the UK, VSL#3 has been<br />
extensively researched in both healthy populations and in chronic conditions, with over<br />
30 scientific studies published in the past 5 years alone.<br />
To find out more about the VSL# range, visit the healthcare professional website at<br />
https://www.vsl3.co.uk/pages/vsl-fibre, or request samples of VSL# Fibre by scanning this<br />
QR code.<br />
References:<br />
1. NHS Inform. Constipation. Nov <strong>2023</strong>. Available online at:<br />
https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-andgastrointestinal-tract/constipation#:~:text=It’s%20estimated%20that%20around%20<br />
1,older%20adults%20and%20during%20pregnancy. Accessed Nov <strong>2023</strong>.<br />
2. NICE. Scenario: Constipation in adults. <strong>2023</strong>. Available at:<br />
https://cks.nice.org.uk/topics/constipation/management/adults/ Accessed Nov <strong>2023</strong><br />
3. Jalanka et al. Int. J. Mol. Sci 2019, 20(2) 433 https://doi.org/10.3390/ijms20020433<br />
4. Riaz G and Chopra R. Biomedicine & Pharmacotherapy 2018; 102: 575-586.<br />
https://doi.org/10.1016/j.biopha.2018.03.023<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
3
EDITOR’S COMMENT<br />
FEATURE<br />
EDITOR’S COMMENT<br />
“Data from the<br />
British Liver<br />
Trust shows<br />
that liver<br />
disease is the<br />
only major noncommunicable<br />
disease in<br />
the UK where<br />
death rates<br />
are rising.”<br />
Christmas <strong>2023</strong>.<br />
Chronic liver disease is a significant cause of morbidity and mortality worldwide. Cases of non-alcoholic<br />
related fatty liver disease (NAFLD) and alcohol related cirrhosis are rising in many parts of the world.<br />
As a result, we are seeing more patients presenting to hospital with decompensated cirrhosis and the<br />
associated complications.<br />
One such presentation of decompensated cirrhosis is acute variceal bleeding, for which the initial<br />
management is resuscitation and pharmacological treatment followed by upper endoscopy. A number<br />
of organisations and societies around the world suggest endoscopy within 12 hours of presentation, but<br />
the optimal timing remains a contentious matter as previous studies on the topic failed to reach similar<br />
conclusions. In this edition of <strong>Gastroenterology</strong> <strong>Today</strong> we feature a single-centre retrospective study looking<br />
at this issue.<br />
Aaron Bhakta<br />
Stronger Together<br />
Cantel, Key Surgical and Diagmed are are now part of of STERIS.<br />
Our companies share a a commitment to to provide the the very best<br />
solutions for for our our Customers and we we are are excited to to bring the the<br />
power of of our our teams together, and to to provide a a more extensive<br />
and innovative suite of of offerings to to new and existing<br />
Customers around the the world.<br />
The unique strength of of our our collective organisation will will continue<br />
to to uphold our our mission of of HELPING OUR CUSTOMERS CREATE<br />
A A HEALTHIER AND SAFER WORLD.<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
Publishers Comment<br />
On behalf of everyone involved with the publishing of <strong>Gastroenterology</strong> <strong>Today</strong> I would like to say a big<br />
thank you to our contributors for their input and a special thank you to our advertisers as without their<br />
ongoing support we would not be able to print and despatch copies of this very unique publication to<br />
all <strong>Gastroenterology</strong> Departments and Endoscopy Units. Wishing you all a very happy Christmas and<br />
prosperous 2024.<br />
Terry Gardner<br />
Publisher<br />
GASTROENTEROLOGY TODAY - SUMMER <strong>2023</strong><br />
GASTROENTEROLOGY TODAY - SUMMER <strong>2023</strong><br />
Come join join us us<br />
at at BSG!<br />
Stand A26<br />
The Arena<br />
4<br />
12 12<br />
www.steris.com
FEATURE<br />
TIMING OF ENDOSCOPY IN PATIENTS<br />
WITH CIRRHOSIS AND ACUTE VARICEAL<br />
BLEEDING: A SINGLE-CENTER<br />
RETROSPECTIVE STUDY<br />
Mengyuan Peng 1,2† , Zhaohui Bai 1,3† , Deli Zou 1† , Shixue Xu 1 , Chunmei Wang 1 , Metin Başaranoğlu 4 ,<br />
Cyriac Abby Philips 5 , Xiaozhong Guo 1 , Xiaodong Shao 1* and Xingshun Qi 1,2,3*<br />
Peng et al. BMC <strong>Gastroenterology</strong> (<strong>2023</strong>) 23:219 https://doi.org/10.1186/s12876-023-02766-8<br />
RESEARCH<br />
Abstract<br />
Background The optimal timing of endoscopy in liver cirrhosis<br />
with acute variceal bleeding (AVB) remains controversial in current<br />
guidelines and studies.<br />
Methods Consecutive patients with liver cirrhosis and AVB were<br />
screened. The timing of endoscopy was calculated from the last<br />
presentation of AVB or the admission to endoscopy. Early endoscopy<br />
was defined as the interval < 12 h, < 24 h, or < 48 h. A 1:1 propensity<br />
score matching (PSM) analysis was performed. Five-day failure to<br />
control bleeding and in-hospital mortality were evaluated.<br />
Results Overall, 534 patients were included. When the timing of<br />
endoscopy was calculated from the last presentation of AVB, PSM<br />
analysis demonstrated that the rate of 5-day failure to control bleeding<br />
was significantly higher in early endoscopy group defined as < 48<br />
h (9.7% versus 2.4%, P = 0.009), but not < 12 h (8.7% versus 6.5%,<br />
P = 1.000) or < 24 h (13.4% versus 6.2%, P = 0.091), and that the<br />
in-hospital mortality was not significantly different between early and<br />
delayed endoscopy groups (< 12 h: 6.5% versus 4.3%, P = 1.000;
FEATURE<br />
Peng et al. BMC <strong>Gastroenterology</strong> (<strong>2023</strong>) 23:219<br />
Page 4 of 9<br />
FEATURE<br />
AVB, but not significantly associated with control of bleeding [11].<br />
However, multiple factors, including the definition regarding timing of<br />
endoscopy, presentation of AVB, hemodynamic status, and severity<br />
of liver disease, could not be sufficiently addressed or adjusted in our<br />
meta-analysis.<br />
More recently, a large randomized controlled trial (RCT) did not<br />
demonstrate any significant difference in 30-day mortality between<br />
patients with upper gastrointestinal bleeding treated with urgent<br />
endoscopy (< 6 h) and early endoscopy (6-24 h) [12]. However, these<br />
findings may not be appropriate for the management of AVB, because<br />
most patients included in this RCT were noncirrhotic (91.8%), and the<br />
source of bleeding was mostly non-variceal (82.9%) [12].<br />
Herein, we conducted a retrospective study to further shed light on<br />
whether early endoscopy was beneficial for patients with cirrhosis<br />
and AVB, especially by adjusting for the definitions regarding timing of<br />
endoscopy and early endoscopy, manifestation of AVB, and severity of<br />
liver disease.<br />
Methods<br />
Outcomes<br />
Outcomes of interest included 5-day failure to control bleeding and<br />
in-hospital death.<br />
Definitions<br />
Timing of endoscopy was calculated according to the interval from<br />
the last presentation of AUGIB or the admission to endoscopy.<br />
Accordingly, eligible patients were divided into early and delayed<br />
endoscopy groups according to three different intervals, including<br />
< 12 h versus ≥ 12 h, < 24 h versus ≥ 24 h, and < 48 h versus ≥ 48 h.<br />
AUGIB was defined as hematemesis or melena within 120 h before<br />
admission [2]. Variceal bleeding was defined as: (1) the presence<br />
of active bleeding from varices on endoscopy; (2) signs of recent<br />
bleeding, such as white nipple; or (3) variceal bleeding would also be<br />
considered, if varices were the only lesion in the stomach, and blood<br />
was found in the stomach or endoscopy was performed 24 h after<br />
bleeding [3]. Five-day failure to control bleeding was defined as the<br />
presence of any of the following within 5 days after endoscopy: (1)<br />
vomiting fresh blood or aspirating more than 100 ml fresh blood for<br />
patients with naso-gastric tube placement after 2 h of endoscopy; (2)<br />
reduction of 3 g/L hemoglobin without transfusion; or (3) death [2].<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
Study design<br />
Patients with liver cirrhosis and AVB were screened from our<br />
retrospective database of 982 patients with liver cirrhosis and acute<br />
upper gastrointestinal bleeding (AUGIB) who were consecutively<br />
admitted to our hospital between January 2010 and June 2014 [13, 14]<br />
and our prospective database of 346 patients with liver cirrhosis and<br />
AUGIB who were consecutively admitted to our department between<br />
December 2014 and January 2022 [15, 16]. Age and comorbidities<br />
were not limited.<br />
Exclusion criteria were as follows: (1) patients did not undergo<br />
endoscopy or those with contraindications for endoscopy; (2) patients<br />
underwent endoscopy at other hospitals or emergency department or<br />
outpatient clinics of our hospital; (3) endoscopy was performed beyond<br />
5 days after the last episode of AUGIB; (4) the timing of endoscopy<br />
was ambiguous according to the medical records; and (5) the source<br />
of AUGIB was non-variceal or could not be accurately identified<br />
according to the medical records or endoscopic reports.<br />
The study protocol has been approved by the Medical Ethical<br />
Committee of the General Hospital of Northern Theater Command with<br />
an approval number (Y [2022] 019) and performed according to the<br />
Declaration of Helsinki. Written informed consents were waived due to<br />
the retrospective nature of this study.<br />
Data collection<br />
Primary data extracted included age, gender, clinical manifestations,<br />
etiology of liver disease, presence of hepatocellular carcinoma,<br />
systolic blood pressure, heart rate, hemoglobin, white blood cell,<br />
platelet count, albumin, alanine aminotransferase, blood urea nitrogen,<br />
serum creatinine, sodium, and prothrombin time (PT) at admission.<br />
Active variceal bleeding on endoscopy, source of variceal bleeding,<br />
endoscopic variceal therapy, surgery or interventional treatment, Child-<br />
Pugh score and class, and model for end-stage liver disease (MELD)<br />
score were also recorded.<br />
Management of AUGIB<br />
Generally, the management of AUGIB is in accordance with the current<br />
practice guideline, which primarily includes fluid resuscitation, blood<br />
transfusion, pharmacological treatment, and endoscopic treatment<br />
[1, 8]. Red blood cell transfusion would be given, if patients had a<br />
hemoglobin level of < 60-80 g/L, or they had active bleeding and<br />
were hemodynamically unstable. Pharmacological treatment included<br />
intravenous vasoactive drugs (terlipressin, somatostatin, or octreotide)<br />
and highdose proton pump inhibitors. Timing of endoscopy was<br />
decided at the discretion of attending physicians according to the<br />
patients’ age, consciousness, comorbidities, and hemodynamics.<br />
Endoscopic treatment was performed by experienced endoscopists.<br />
Endoscopic variceal therapy includes endoscopic variceal ligation,<br />
sclerotherapy, and injection of tissue adhesive. Endoscopic variceal<br />
ligation was primarily employed for the treatment of acute esophageal<br />
variceal bleeding, sclerotherapy was considered when ligation was<br />
technically difficult or active variceal bleeding was observed on<br />
endoscopy, and injection of tissue adhesive was primarily used for the<br />
treatment of acute gastric variceal bleeding. Repeat endoscopy was<br />
often recommended 2–4 weeks after the first endoscopic variceal<br />
therapy, with additional endoscopic variceal treatment(s), if necessary.<br />
If endoscopy failed to control bleeding, patients would undergo surgery<br />
or interventional treatment.<br />
Statistical analyses<br />
Continuous variables were presented as mean ± standard deviation<br />
and median (range), and categorical variables were presented as<br />
frequency (percentage). The nonparametric Mann-Whitney U test was<br />
used for continuous variables, and the chi-square test and Fisher’s<br />
exact test were used for categorical variables to explore the difference<br />
between early and delayed endoscopy groups.<br />
Logistic and Cox regression analyses were performed to identify<br />
whether early endoscopy was an independent predictor of 5-day<br />
failure to control bleeding or in-hospital death. Odds ratios (ORs)<br />
Fig. 1 Flowchart of patient selection<br />
in-hospital death (HR = 2.828, 95% CI: 0.706–11.320,<br />
P = 0.142).<br />
In the PSM analysis, 46 patients were matched to each<br />
group (Supplementary Table 2). There was no significant<br />
difference in rate of 5-day failure to control bleeding or<br />
in-hospital mortality between the two groups (Table 2).<br />
< 24 h versus ≥ 24 h. In the overall-analysis, early<br />
endoscopy group was significantly older and had higher<br />
proportions of HCV infection, hematemesis, systolic<br />
blood pressure < 90 mmHg, Child-Pugh class B/C, and<br />
active variceal bleeding on endoscopy and white blood<br />
cell than delayed endoscopy group (Supplementary<br />
Table 3). Early endoscopy group had significantly higher<br />
rate of 5-day failure to control bleeding and in-hospital<br />
mortality than delayed endoscopy group (Table 2).<br />
and hazard ratios (HRs) with 95% confidence intervals (CIs) were<br />
calculated. A 1:1 propensity score matching (PSM) analysis was<br />
performed by using a matching tolerance of 0.02 and greedymatching<br />
algorithm without replacement to compare the rate of 5-day failure<br />
to control bleeding and in-hospital mortality between early and<br />
delayed endoscopy groups. After PSM, the comparability of baseline<br />
characteristics between the groups was re-evaluated. Matching<br />
factors included age, gender, systolic blood pressure < 90mmHg,<br />
heart rate > 100 beats per minute, PT, Child-Pugh score, MELD score,<br />
hematemesis at admission, active variceal bleeding on endoscopy, and<br />
endoscopic variceal therapy. A two-tailed P < 0.05 was considered<br />
statistically significant. All statistical analyses were performed with IBM<br />
SPSS 26.0 (IBM Corp, Armonk, NY, USA).<br />
Results<br />
Patients<br />
Overall, 534 patients with cirrhosis and AVB were included (Fig. 1).<br />
Patient characteristics were shown in Table 1. The median age was<br />
Multivariate logistic regression analysis demonstrated<br />
that the interval from last presentation of AVB to endoscopy<br />
< 24 h was significantly associated with a higher rate<br />
of 5-day failure to control bleeding (OR = 6.065, 95% CI:<br />
2.336–15.749; P < 0.001). Multivariate Cox regression<br />
analysis showed that the interval from last presentation<br />
of AVB to endoscopy < 24 h was not significantly associated<br />
with in-hospital death (HR = 1.400, 95% CI: 0.403–<br />
4.860, P = 0.597).<br />
In the PSM analysis, 97 patients were matched to each<br />
group (Supplementary Table 4). There was no significant<br />
difference in rate of 5-day failure to control bleeding or<br />
in-hospital mortality between the two groups (Table 2).<br />
< 48 h versus ≥ 48 h. In the overall-analysis, early<br />
endoscopy group was significantly older and had significantly<br />
higher proportions of HCV infection,<br />
55.66 years (range: 6.28–92.31 years), and 376 (70.4%) patients<br />
were male. Hematemesis at admission in 332 (62.2%) patients. Most<br />
patients had Child-Pugh class B/C (333/498, 66.9%). Median MELD<br />
score was 10.51 (range: 6.43–38.01). Active bleeding was observed<br />
under endoscopy in 39 (7.4%) patients. The rate of 5-day failure to<br />
control bleeding was 5.1% (n = 27). The in-hospital mortality was<br />
2.4% (n = 13). The causes of death included massive gastrointestinal<br />
bleeding (n = 8), end-stage liver disease with multiple organ failure<br />
(n = 4), and cardiogenic shock (n = 1).<br />
Time to endoscopy according to the interval from the last<br />
presentation of AVB to endoscopy<br />
< 12 h versus ≥ 12 h. In the overall-analysis, early endoscopy group<br />
had significantly higher proportions of hepatitis C virus (HCV) infection<br />
and systolic blood pressure < 90 mmHg and white blood cell than<br />
delayed endoscopy group (Supplementary Table 1). Early endoscopy<br />
group had significantly higher rate of 5-day failure to control bleeding<br />
and in-hospital mortality than delayed endoscopy group (Table 2).<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
8 9
Peng et al. BMC <strong>Gastroenterology</strong> (<strong>2023</strong>) 23:219<br />
FEATURE<br />
Page 5 of 9<br />
Peng et al. BMC <strong>Gastroenterology</strong> (<strong>2023</strong>) 23:219<br />
Page 6 of 9<br />
FEATURE<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
Table 1 Characteristics of included patients<br />
Variables No. Pts Mean ± SD or<br />
Median (Range) or<br />
Frequency (Percentage)<br />
Age (years) 534 55.66 (6.28–92.31)<br />
55.78 ± 11.61<br />
Male 534 376 (70.4%)<br />
Etiology of underlying liver diseases 534<br />
Hepatitis B virus 222 (41.6%)<br />
Hepatitis C virus 47 (8.8%)<br />
Alcohol abuse 150 (28.1%)<br />
Hepatocellular carcinoma 534 48 (9.0%)<br />
Hematemesis 534 332 (62.2%)<br />
Hemodynamics<br />
Heart rate (beats per minute) 534 80.00 (44.00-148.00)<br />
83.36 ± 13.24<br />
Heart rate > 100 beats per minute 534 54 (10.1%)<br />
Systolic blood pressure (mmHg) 533 115.00 (75.00-176.00)<br />
116.07 ± 17.59<br />
Systolic blood pressure < 90mmHg 533 18 (3.4%)<br />
Laboratory tests<br />
Hemoglobin (g/L) 533 73.00 (23.00-158.00)<br />
77.53 ± 22.51<br />
White blood cell (10 12 /L) 533 4.40 (1.00-46.10)<br />
5.45 ± 3.98<br />
Platelet count (10 9 /L) 533 72.00 (15.00-457.00)<br />
87.44 ± 58.82<br />
Total bilirubin (µmol/L) 529 19.90 (3.30-187.40)<br />
25.01 ± 18.35<br />
Albumin (g/L) 524 30.50 (10.00-50.70)<br />
30.57 ± 6.53<br />
Alanine aminotransferase (U/L) 527 22.73 (5.00-1064.00)<br />
32.70 ± 58.03<br />
Blood urea nitrogen (mmol/L) 512 8.03 (1.54–42.83)<br />
8.95 ± 4.79<br />
Serum creatinine (µmol/L) 510 62.00 (25.00-715.00)<br />
69.30 ± 45.29<br />
Sodium (mmol/L) 524 138.5 (109.2-160.10)<br />
138.44 ± 4.22<br />
Prothrombin time (seconds) 510 16.00 (10.50–55.00)<br />
16.85 ± 4.00<br />
Child-Pugh score 498 7.00 (5.00–13.00)<br />
7.47 ± 1.82<br />
Child-Pugh class A/B + C 498 165 (33.1%)/333 (66.9%)<br />
MELD score 502 10.51 (6.43–38.01)<br />
11.92 ± 4.61<br />
Source of variceal bleeding 519 *<br />
Esophageal varices (%) 313 (60.3%)<br />
Gastric varices (%) 77 (14.8%)<br />
Esophageal and gastric varices (%) 129 (24.9%)<br />
Active variceal bleeding on endoscopy 528 # 39 (7.4%)<br />
Endoscopic variceal therapy 534 496 (92.9%)<br />
Surgery or interventional treatment 534 3 (0.6%)<br />
Rate of 5-day failure to control bleeding 534 27 (5.1%)<br />
In-hospital mortality 534 13 (2.4%)<br />
Abbreviations: MELD, model for end-stage liver disease. Notes: * Source of variceal bleeding was unclear in 15 patients because of missing medical records or poor<br />
visual fields under endoscopy; # Active variceal bleeding on endoscopy cannot be identified in 6 patients because of missing endoscopic reports.<br />
Table 2 Outcomes according to the timing of endoscopy defined as the interval from the last presentation of AVB to endoscopy<br />
Overall analysis<br />
< 12h ≥ 12h P value < 24h ≥ 24h P value < 48h ≥ 48h P value<br />
(N = 55) (N = 434)<br />
(N = 114) (N = 357)<br />
(N = 226) (N = 242)<br />
Rate of 5-day failure to control bleeding 6 (10.9%) 14 (3.2%) 0.007 15 (13.2%) 8 (2.2%) < 0.001 20 (8.8%) 5 (2.1%) 0.001<br />
In-hospital mortality 5 (9.1%) 6 (1.4%) < 0.001 6 (5.3%) 6 (1.7%) 0.035 8 (3.5%) 5 (2.1%) 0.332<br />
PSM analysis<br />
hematemesis, systolic blood pressure < 90 mmHg, Child-<br />
Multivariate logistic regression analysis demonstrated that the interval<br />
Pugh class B/C, and active variceal bleeding on endoscopy,<br />
white blood cell, and blood urea nitrogen than<br />
from last presentation of AVB to endoscopy < 12 h was not significantly<br />
associated with 5-day failure to control bleeding (OR = 2.889, 95% CI:<br />
delayed endoscopy group (Supplementary Table 5). Early<br />
0.912–9.151; P = 0.071). Multivariate Cox regression analysis showed<br />
endoscopy group had a significantly higher rate of 5-day<br />
that the interval from last presentation of AVB to endoscopy < 12 h was<br />
failure to control bleeding than delayed endoscopy group,<br />
not significantly associated with in-hospital death (HR = 2.828, 95% CI:<br />
but a statistically similar in-hospital mortality (Table 2).<br />
0.706–11.320, P = 0.142).<br />
Multivariate logistic regression analysis demonstrated<br />
that the interval from last presentation of AVB to endoscopy<br />
< 48 h was significantly associated with a higher rate<br />
In the PSM analysis, 46 patients were matched to each group<br />
(Supplementary Table 2). There was no significant difference in rate of<br />
of 5-day failure to control bleeding (OR = 4.171, 95% CI:<br />
5-day failure to control bleeding or in-hospital mortality between the<br />
1.486–11.708; P = 0.007). Cox regression analysis showed<br />
two groups (Table 2).<br />
that the interval from last presentation of AVB to endoscopy<br />
< 48 h was not significantly associated with in-hospital<br />
death (HR = 0.808, 95% CI: 0.237–2.750, P = 0.733).<br />
< 24 h versus ≥ 24 h. In the overall-analysis, early endoscopy group<br />
was significantly older and had higher proportions of HCV infection,<br />
In the PSM analysis, 165 patients were matched to each<br />
hematemesis, systolic blood pressure < 90 mmHg, Child-Pugh class<br />
group (Supplementary Table 6). Early endoscopy group<br />
B/C, and active variceal bleeding on endoscopy and white blood<br />
had a significantly higher rate of 5-day failure to control<br />
cell than delayed endoscopy group (Supplementary Table 3). Early<br />
bleeding than delayed endoscopy group, but a statistically<br />
endoscopy group had significantly higher rate of 5-day failure to control<br />
similar in-hospital mortality (Table 2).<br />
bleeding and in-hospital mortality than delayed endoscopy group<br />
(Table 2).<br />
Time to endoscopy according to the interval from the<br />
admission to endoscopy<br />
Multivariate logistic regression analysis demonstrated that the interval<br />
< 12 h versus ≥ 12 h. In the overall-analysis, early endoscopy<br />
group was significantly older and had significantly<br />
from last presentation of AVB to endoscopy < 24 h was associated with a higher rate of 5-day failure to control bleeding (OR =<br />
higher proportions of HCV infection, Child-Pugh class<br />
6.065, 95% CI: 2.336–15.749; P < 0.001). Multivariate Cox regression<br />
B/C, and active variceal bleeding on endoscopy, white<br />
analysis showed that the interval from last presentation of AVB to<br />
blood cell, total bilirubin, blood urea nitrogen, Childendoscopy<br />
< 24 h was not significantly associated with in-hospital<br />
Pugh score, and MELD score than delayed endoscopy<br />
death (HR = 1.400, 95% CI: 0.403–4.860, P = 0.597).<br />
group (Supplementary Table 7). There was no significant<br />
difference in rate of 5-day failure to control bleeding or<br />
In the PSM analysis, 97 patients were matched to each group<br />
in-hospital mortality between the two groups (Table 3).<br />
(Supplementary Table 4). There was no significant difference in rate of<br />
5-day failure to control bleeding or in-hospital mortality between the<br />
two groups (Table 2).<br />
< 12h<br />
(N = 46)<br />
≥ 12h<br />
(N = 46)<br />
P value<br />
< 24h<br />
(N = 97)<br />
≥ 24h<br />
(N = 97)<br />
P value<br />
< 48h<br />
(N = 165)<br />
≥ 48h<br />
(N = 165)<br />
Rate of 5-day failure to control bleeding 4 (8.7%) 3 (6.5%) 1.000 13 (13.4%) 6 (6.2%) 0.091 16 (9.7%) 4 (2.4%) 0.009<br />
In-hospital mortality 3 (6.5%) 2 (4.3%) 1.000 4 (4.1%) 3 (3.1%) 1.000 5 (3.0%) 4 (2.4%) 1.000<br />
Abbreviations: AVB, acute variceal bleeding; PSM, propensity score matching<br />
P value<br />
Table 3 Outcomes according to the timing of endoscopy defined as the interval from the admission to endoscopy<br />
Overall analysis<br />
< 12h ≥ 12h P value < 24h ≥ 24h P value < 48h ≥ 48h P value<br />
(N = 75) (N = 453)<br />
(N = 175) (N = 349)<br />
(N = 289) (N = 236)<br />
Rate of 5-day failure to control bleeding 5 (6.7%) 21 (4.6%) 0.451 10 (5.7%) 17 (4.9%) 0.680 13 (4.5%) 13 (5.5%) 0.596<br />
In-hospital mortality 4 (5.3%) 8 (1.8%) 0.055 7 (4.0%) 6 (1.7%) 0.113 8 (2.8%) 5 (2.1%) 0.634<br />
PSM analysis<br />
< 12h<br />
(N = 63)<br />
≥ 12h<br />
(N = 63)<br />
P value<br />
< 24h<br />
(N = 155)<br />
≥ 24h<br />
(N = 155)<br />
P value<br />
< 48h<br />
(N = 199)<br />
≥ 48h<br />
(N = 199)<br />
Rate of 5-day failure to control bleeding 3 (4.8%) 8 (12.7%) 0.205 8 (5.2%) 12 (7.7%) 0.355 9 (4.5%) 12 (6.0%) 0.501<br />
In-hospital mortality 3 (4.8%) 3 (4.8%) 1.000 6 (3.9%) 4 (2.6%) 0.750 4 (2.0%) 5 (2.5%) 1.000<br />
Abbreviations: PSM, propensity score matching<br />
P value<br />
Multivariate logistic regression analysis demonstrated<br />
< 48 h versus ≥ 48 h. In the overall-analysis, early endoscopy group<br />
that the interval from admission to endoscopy < 12 h was<br />
was significantly older and had significantly higher proportions of HCV<br />
not significantly associated with 5-day failure to control<br />
infection, hematemesis, systolic blood pressure < 90 mmHg, Childbleeding<br />
(OR = 0.873, 95% CI: 0.243–3.144; P = 0.836).<br />
Pugh class B/C, and active variceal bleeding on endoscopy, white<br />
blood<br />
Multivariate<br />
cell, and blood<br />
Cox<br />
urea<br />
regression<br />
nitrogen than<br />
analysis<br />
delayed endoscopy<br />
showed that<br />
group<br />
the<br />
(Supplementary<br />
interval from<br />
Table<br />
admission<br />
5). Early<br />
to<br />
endoscopy<br />
endoscopy<br />
group<br />
<<br />
had<br />
12 h<br />
a significantly<br />
was not significantly<br />
higher rate of<br />
associated<br />
5-day failure to<br />
with<br />
control<br />
in-hospital<br />
bleeding than<br />
death<br />
delayed<br />
(HR<br />
endoscopy<br />
= 1.981,<br />
group, 95% CI: but 0.467–8.406, a statistically similar P = 0.354). in-hospital mortality (Table 2).<br />
In the PSM analysis, 63 patients were matched to each<br />
Multivariate group (Supplementary logistic regression Table analysis 8). demonstrated There was that no significant<br />
the interval<br />
from difference last presentation in rate of of AVB 5-day to endoscopy failure to < 48 control h was significantly bleeding or<br />
associated in-hospital with mortality a higher rate between of 5-day the failure two to control groups bleeding (Table(OR<br />
3).<br />
= 4.171, < 2495% h versus CI: 1.486–11.708; ≥ 24 h. P = In 0.007). the Cox overall-analysis, regression analysis early<br />
showed endoscopy that the group interval was from significantly last presentation older of AVB and to endoscopy had significantly<br />
48 h was higher not significantly proportion associated of Child-Pugh with in-hospital class death B/C (HR = and<br />
<<br />
0.808, Child-Pugh 95% CI: 0.237–2.750, score than P delayed = 0.733). endoscopy group (Supplementary<br />
Table 9). There was no significant difference<br />
In in the rate PSM of analysis, 5-day failure 165 patients to control were matched bleeding to each or group in-hospital<br />
(Supplementary mortality between Table 6). the Early two endoscopy groups group (Table had 3). a significantly<br />
higher Multivariate rate of 5-day logistic failure to regression control bleeding analysis than delayed demonstrated<br />
endoscopy<br />
group, that the but interval a statistically from similar admission in-hospital to mortality endoscopy (Table < 2). 24 h was<br />
not significantly associated with 5-day failure to control<br />
Time bleeding to endoscopy (OR = 0.867, according 95% to the CI: interval 0.353–2.132; from the admission P = 0.756).<br />
to Multivariate endoscopy Cox regression analysis showed that the<br />
< interval 12 h versus from ≥ 12 admission h. In the overall-analysis, to endoscopy early < 24 endoscopy h was not group sig-<br />
was significantly associated older and with had significantly in-hospital higher death proportions (HR = of 2.554,<br />
HCV 95% infection, CI: 0.747–8.732, Child-Pugh class P = 0.135). B/C, and active variceal bleeding<br />
on In endoscopy, the PSM white analysis, blood cell, 155 total patients bilirubin, were blood matched urea nitrogen, to each<br />
Child-Pugh group (Supplementary score, and MELD Table score than 10). delayed There was endoscopy no significant group<br />
(Supplementary difference in Table rate 7). of There 5-day was failure no significant to control difference bleeding rate of or<br />
5-day in-hospital failure to mortality control bleeding between or in-hospital the two mortality groups between (Table the 3).<br />
two<br />
<<br />
groups<br />
48 h<br />
(Table<br />
versus<br />
3).<br />
≥ 48 h. In the overall-analysis, early<br />
endoscopy group was significantly older than delayed<br />
Multivariate logistic regression analysis demonstrated that the interval<br />
from admission to endoscopy < 12 h was not significantly associated<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
10 11
FEATURE<br />
FEATURE<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
with 5-day failure to control bleeding (OR = 0.873, 95% CI: 0.243–<br />
3.144; P = 0.836). Multivariate Cox regression analysis showed that<br />
the interval from admission to endoscopy < 12 h was not significantly<br />
associated with in-hospital death (HR = 1.981, 95% CI: 0.467–8.406,<br />
P = 0.354).<br />
In the PSM analysis, 63 patients were matched to each group<br />
(Supplementary Table 8). There was no significant difference in rate of<br />
5-day failure to control bleeding or in-hospital mortality between the<br />
two groups (Table 3).<br />
< 24 h versus ≥ 24 h. In the overall-analysis, early endoscopy group<br />
was significantly older and had significantly higher proportion of Child-<br />
Pugh class B/C and Child-Pugh score than delayed endoscopy group<br />
(Supplementary Table 9). There was no significant difference in rate of<br />
5-day failure to control bleeding or in-hospital mortality between the<br />
two groups (Table 3).<br />
Multivariate logistic regression analysis demonstrated that the interval<br />
from admission to endoscopy < 24 h was not significantly associated<br />
with 5-day failure to control bleeding (OR = 0.867, 95% CI: 0.353–<br />
2.132; P = 0.756). Multivariate Cox regression analysis showed that<br />
the interval from admission to endoscopy < 24 h was not significantly<br />
associated with in-hospital death (HR = 2.554, 95% CI: 0.747–8.732,<br />
P = 0.135).<br />
In the PSM analysis, 155 patients were matched to each group<br />
(Supplementary Table 10). There was no significant difference in rate<br />
of 5-day failure to control bleeding or in-hospital mortality between the<br />
two groups (Table 3).<br />
< 48 h versus ≥ 48 h. In the overall-analysis, early endoscopy group<br />
was significantly older than delayed endoscopy group (Supplementary<br />
Table 11). There was no significant difference in rate of 5-day failure<br />
to control bleeding or in-hospital mortality between the two groups<br />
(Table 3).<br />
Multivariate logistic regression analysis demonstrated that the interval<br />
from admission to endoscopy < 48 h was not significantly associated<br />
with 5-day failure to control bleeding (OR = 0.643, 95% CI: 0.275–<br />
1.506; P = 0.309). Multivariate Cox regression analysis showed that<br />
the interval from admission to endoscopy < 48 h was not significantly<br />
associated with in-hospital death (HR = 1.513, 95% CI: 0.416–5.499,<br />
P = 0.529).<br />
In the PSM analysis, 199 patients were matched to each group<br />
(Supplementary Table 12). There was no significant difference in rate<br />
of 5-day failure to control bleeding or in-hospital mortality between the<br />
two groups (Table 3).<br />
Subgroup analyses<br />
Subgroup analyses were performed according to the manifestations<br />
of AUGIB (hematemesis versus nonhematemesis) and severity of liver<br />
diseases (Child-Pugh class A versus Child-Pugh class B/C). The results<br />
were shown in Supplementary Table 13 and Supplementary Table 14.<br />
Discussion<br />
Based on the data obtained from our center, the benefit of early<br />
endoscopy on the outcomes of patients with liver cirrhosis and AVB<br />
could not be supported. It seems to be contrary to the traditional<br />
concept that early endoscopy could achieve more rapid hemostasis<br />
and hence better outcomes. Notably, early endoscopy may influence<br />
basic resuscitation, leading to ischemic complications, and shorten the<br />
duration of action of vasoactive drugs or antibiotics before endoscopic<br />
treatment for acute gastrointestinal bleeding [17]. Additionally, there<br />
were a significantly larger number of patients with active bleeding in<br />
early endoscopy group. Thus, a large amount of blood and contents<br />
in the non-fasting stomach limits the visual field under endoscopy and<br />
masks the primary source of bleeding, thereby increasing the technical<br />
difficulty as well as risk of aspiration or perforation [18]. By comparison,<br />
delayed endoscopy may be safer and provides clearer visual field,<br />
especially after portal pressure has been sufficiently decreased by the<br />
use of vasoactive drugs [10].<br />
Our finding may be influenced by the definition regarding time<br />
to endoscopy, the manifestation of AVB, or the severity of liver<br />
dysfunction. First, until now, any standard definition regarding time<br />
to endoscopy has not been given by any practice guideline yet [2,<br />
3, 6, 19, 20]. Indeed, the definitions regarding time to endoscopy<br />
are heterogeneous among previous studies. By contrast, in the<br />
present study, both of two major definitions, of which one refers to<br />
the interval from the last presentation of gastrointestinal bleeding to<br />
endoscopy [21], and another refers to the interval from the admission<br />
to endoscopy [9, 22], have been employed. It is true that the number<br />
and percentage of patients assigned to early endoscopy group were<br />
different (55 [10.3%] in < 12 h endoscopy group according to the first<br />
definition versus 75 [14.0%] in < 12 h endoscopy group according to<br />
the second definition). On the other hand, the definitions regarding<br />
early endoscopy are also different among previous studies, including <<br />
6h [23], < 12h [21, 22] and < 24h [24]. Accordingly, the results of overall<br />
analyses based on the interval from the last presentation of AVB to<br />
endoscopy are also heterogeneous that < 12 h and < 24 h endoscopy<br />
group, but not < 48 h endoscopy group, had significantly higher inhospital<br />
mortality than delayed endoscopy group.<br />
Second, patients with cirrhosis and AVB who presented with<br />
hematemesis at admission may have worse prognosis than those<br />
who presented with melena [14]. The results of our subgroup analyses<br />
based on the interval from the last presentation of AVB to endoscopy<br />
demonstrated that early endoscopy was significantly associated<br />
with a higher risk of 5-day failure to control bleeding in patients with<br />
hematemesis, but such an association remains in patients with nonhematemesis.<br />
By contrast, a previous cohort study by Chen et al.<br />
found that 6-week rebleeding rate and mortality were lower in patients<br />
with hematemesis who underwent early endoscopy than those<br />
who underwent delayed endoscopy, but not significantly different<br />
between the two groups in patients without hematemesis [22]. Such a<br />
difference between current and previous studies may be because all<br />
of the patients included in the Chen’s study had active AVB, but active<br />
bleeding was observed endoscopically in only 7.4% of our patients.<br />
Rapid control of active bleeding by early endoscopy is beneficial for<br />
preventing from an injury to the liver and other organs and achieving<br />
better outcomes. It can be speculated that patients with hematemesis<br />
without active bleeding will benefit more from delayed endoscopy after<br />
sufficient medical therapy as compared to early endoscopy.<br />
Third, the severity of liver cirrhosis affects the prognosis of AVB [25].<br />
It has been confirmed that MELD score is an independent predictor<br />
for the prognosis of liver cirrhosis with AVB [26, 27]. Huh et al. found<br />
that early endoscopy, which was defined as the interval from the<br />
last presentation of gastrointestinal bleeding to endoscopy ≤ 12 h,<br />
increased the risk of 6-week rebleeding and death in the low-risk<br />
(MELD score ≤ 17) group, but the timing of endoscopy was not<br />
associated with the prognosis in the high-risk (MELD score > 17)<br />
group [21]. By comparison, according to the results of our subgroup<br />
and PSM analyses, the association between timing of endoscopy and<br />
outcomes was not influenced by Child-Pugh class or score. Thus, the<br />
optimal timing of endoscopy may not be dependent upon the severity<br />
of liver cirrhosis.<br />
Our study has several limitations as follows. First, our study was<br />
retrospective. The selection of emergency endoscopy often depends<br />
on the patients’ conditions, physicians’ decisions, and availability<br />
of endoscopists, which leads to a considerable selection bias.<br />
Specifically, patients with massive hematemesis who were not<br />
effectively treated by drugs were more prone to early endoscopy,<br />
those with hemodynamic instability would undergo delayed endoscopy<br />
after basic resuscitation, and those admitted during off-hours might<br />
undergo delayed endoscopy. Although all procedures were performed<br />
by experienced endoscopists, it may be different in judging the<br />
source of gastrointestinal bleeding and treating AVB under endoscopy<br />
among endoscopists, which influences the prognosis of patients. In<br />
addition, endoscopic findings in the stomach were retrospectively<br />
derived from the patients’ medical records alone, but they seemed<br />
to be insufficient to evaluate whether gastric contents had influenced<br />
the efficacy of gastric variceal treatment under endoscopy. Second,<br />
our study excluded patients who had undergone endoscopy at their<br />
local hospitals and outpatient and emergency departments, those<br />
who were not suitable for endoscopy, as well as those who died<br />
before endoscopy. Such patients should be more severe and critical.<br />
Third, this was a single-center study, which should be validated by a<br />
multi-center study. In addition, our study had a relatively small number<br />
of death events, which might be unpowered to achieve statistically<br />
significant results between early and delayed endoscopy groups.<br />
In conclusion, our study did not confirm an association of timing of<br />
endoscopy with risk of 5-day failure to control bleeding or in-hospital<br />
death in patients with cirrhosis and AVB. Endoscopy after adequate<br />
medical therapy may be more effective than urgent endoscopy. RCTs<br />
with strict eligibility criteria and optimal definitions regarding timing of<br />
endoscopy are needed to confirm the effect of the timing of endoscopy<br />
on prognosis of patients with cirrhosis and AVB in the future.<br />
Abbreviations<br />
AASLD American Association for the Study of Liver Diseases<br />
AUGIB Acute upper gastrointestinal bleeding<br />
AVB Acute variceal bleeding<br />
ESGE European Society of Gastrointestinal Endoscopy<br />
HCV Hepatitis C virus<br />
MELD Model for End-stage Liver Disease<br />
PSM Propensity score matching<br />
PT Prothrombin time<br />
RCT Randomized controlled trial<br />
TIPS Trans-jugular intrahepatic portosystemic shunt<br />
Supplementary Information<br />
The online version contains supplementary material available at<br />
https://doi.org/10.1186/s12876-023-02766-8.<br />
Supplementary Material 1<br />
Acknowledgements<br />
We are indebted to our study team for establishing and updating<br />
our retrospective and prospective databases, including Junna Dai,<br />
Cuihong Zhu, Yun Li, Ying Peng, Zheng Ning, Feifei Hou, Jiancheng<br />
Zhao, Han Deng, Ran Wang, Jing Li, Xintong Zhang, Dan Han, Tingxue<br />
Song, Zhong Peng, Wenchun Bao, Jia Zhu, Yingying Li, Zhaohui Bai,<br />
Xiangbo Xu, Qianqian Li, Kexin Zheng, Yang An, Le Wang, Yanyan<br />
Wu, Fangfang Yi, Li Luo, Yue Yin, Shixue Xu, Yiyan Zhang, Min Ding,<br />
Weiwei Wang, Xueying Wang, and Xiaojie Zheng, of whom all had<br />
worked for our study group.<br />
Author Contribution<br />
MP and XQ were involved in the concept and design of study; MP,<br />
ZB, and XQ were involved in the data curation; MP, ZB, DZ, SX, CW,<br />
XG, XS, and XQ were involved in statistical analysis; MP, ZB, and XQ<br />
were involved in drafting the manuscript; all authors were involved<br />
in writing–review and editing; XG, XS, and XQ were involved in the<br />
supervision of study. All authors have made an intellectual contribution<br />
to the manuscript and approved the submission. All authors read and<br />
approved the final manuscript.<br />
Funding<br />
This work was partially supported by the Young and Middle-aged<br />
Scientific and Technological Innovation Talents Support Plan Project of<br />
Shenyang (RC210011).<br />
Data Availability<br />
The dataset data used to support the findings of this study<br />
are available from the corresponding author at email address<br />
upon request.<br />
Declarations<br />
Ethics approval and consent to participate<br />
The study protocol has been approved by the Medical Ethical<br />
Committee of the General Hospital of Northern Theater Command<br />
with an approval number (Y [2022] 019) and performed according to<br />
the Declaration of Helsinki. Medical Ethical Committee of the General<br />
Hospital of Northern Theater Command waived need for written<br />
informed consents due to the retrospective nature of this study.<br />
Consent for publication<br />
Not applicable.<br />
Competing interests<br />
The authors have no conflict of interests related to this publication.<br />
Author details<br />
1<br />
Department of <strong>Gastroenterology</strong>, General Hospital of Northern Theater<br />
Command (formerly General Hospital of Shenyang Military Area), No.<br />
83 Wenhua Road, Shenyang, Liaoning Province 110840, China<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
12 13
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
FEATURE<br />
2<br />
Postgraduate College, Jinzhou Medical University, Jinzhou, P.R. China<br />
3<br />
Postgraduate College, Shenyang Pharmaceutical University,<br />
Shenyang, P.R. China<br />
4<br />
Department of Internal Medicine, Bezmialem Vakıf University Faculty<br />
of Medicine, İstanbul, Turkey<br />
5<br />
Clinical and Translational Hepatology & Monarch Liver Laboratory,<br />
The Liver Institute, Center of Excellence in Gastrointestinal Sciences,<br />
Rajagiri Hospital, Aluva, Kerala, India<br />
Received: 25 July 2022 / Accepted: 15 April <strong>2023</strong><br />
Published online: 26 June <strong>2023</strong><br />
References<br />
1. Garcia-Tsao G, Bosch J. Management of varices and variceal<br />
hemorrhage in cirrhosis. N Engl J Med. 2010;362(9):823–32.<br />
https://doi.org/10.1056/NEJMra0901512.<br />
2. de Franchis R. Expanding consensus in portal hypertension:<br />
report of the Baveno VI Consensus Workshop: stratifying risk<br />
and individualizing care for portal hypertension. J Hepatol.<br />
2015;63(3):743–52. https://doi.org/10.1016/j.jhep.2015.05.022.<br />
3. Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal<br />
hypertensive bleeding in cirrhosis: risk stratification, diagnosis,<br />
and management: 2016 practice guidance by the American<br />
Association for the Study of Liver Diseases. Hepatology.<br />
2017;65(1):310–35. https://doi.org/10.1002/hep.28906.<br />
4. Hwang JH, Shergill AK, Acosta RD, Chandrasekhara V, Chathadi<br />
KV, Decker GA, et al. The role of endoscopy in the management<br />
of variceal hemorrhage. Gastrointest Endosc. 2014;80(2):221–7.<br />
https://doi.org/10.1016/j.gie.2013.07.023.<br />
5. Colle I, Wilmer A, Le Moine O, Debruyne R, Delwaide J, Dhondt E,<br />
et al. Upper gastrointestinal tract bleeding management: Belgian<br />
guidelines for adults and children. Acta Gastroenterol Belg.<br />
2011;74(1):45–66.<br />
6. Karstensen JG, Ebigbo A, Bhat P, Dinis-Ribeiro M, Gralnek I, Guy<br />
C, et al. Endoscopic treatment of variceal upper gastrointestinal<br />
bleeding: European Society of Gastrointestinal Endoscopy (ESGE)<br />
Cascade Guideline. Endoscopy Int open. 2020;8(7):E990–E997.<br />
https://doi.org/10.1055/a-1187-1154.<br />
7. Tripathi D, Stanley AJ, Hayes PC, Patch D, Millson C, Mehrzad H,<br />
et al. U.K. guidelines on the management of variceal haemorrhage<br />
in cirrhotic patients. Gut. 2015;64(11):1680–704. https://doi.<br />
org/10.1136/gutjnl-2015-309262.<br />
8. Xu X, Ding H, Jia J, Wei L, Duan Z, Linghu E, et al. Guidelines<br />
for the diagnosis and treatment of esophageal and gastric<br />
variceal bleeding in cirrhotic portal hypertension. J Clin Hepatol.<br />
2016;32(02):203–19.<br />
9. Hsu YC, Chung CS, Tseng CH, Lin TL, Liou JM, Wu MS, et al.<br />
Delayed endoscopy as a risk factor for in-hospital mortality in<br />
cirrhotic patients with acute variceal hemorrhage. J Gastroenterol<br />
Hepatol. 2009;24(7):1294–9. https://doi.org/10.1111/j.1440-<br />
1746.2009.05903.x.<br />
10. Yoo JJ, Chang Y, Cho EJ, Moon JE, Kim SG, Kim YS, et al. Timing<br />
of upper gastrointestinal endoscopy does not influence shortterm<br />
outcomes in patients with acute variceal bleeding. World J<br />
Gastroenterol. 2018;24(44):5025–33. https://doi.org/10.3748/wjg.<br />
v24.i44.5025.<br />
11. Bai Z, Wang R, Cheng G, Ma D, Ibrahim M, Chawla S, et<br />
al. Outcomes of early versus delayed endoscopy in cirrhotic<br />
patients with acute variceal bleeding: a systematic review with<br />
meta-analysis. Eur J Gastroenterol Hepatol. 2021;33(1S Suppl<br />
1):e868–76. https://doi.org/10.1097/meg.0000000000002282.<br />
12. Lau JYW, Yu Y, Tang RSY, Chan HCH, Yip HC, Chan SM, et al.<br />
Timing of endoscopy for acute upper gastrointestinal bleeding. N<br />
Engl J Med. 2020;382(14):1299–308. https://doi.org/10.1056/<br />
NEJMoa1912484.<br />
13. An Y, Bai Z, Xu X, Guo X. No benefit of hemostatic drugs on<br />
acute upper gastrointestinal bleeding in cirrhosis. Biomed Res Int.<br />
2020;2020:4097170. https://doi.org/10.1155/2020/4097170.<br />
14. Li Y, Li H, Zhu Q, Tsochatzis E, Wang R, Guo X, et al. Effect of<br />
acute upper gastrointestinal bleeding manifestations at admission<br />
on the in-hospital outcomes of liver cirrhosis: hematemesis<br />
versus melena without hematemesis. Eur J Gastroenterol<br />
Hepatol. 2019;31(11):1334–41. https://doi.org/10.1097/<br />
meg.0000000000001524.<br />
15. Yi F, Guo X, Wang L, Xu X, An Y, Tang Y, et al. Impact of<br />
spontaneous splenorenal shunt on liver volume and longterm<br />
survival of liver cirrhosis. J Gastroenterol Hepatol.<br />
2021;36(6):1694–702. https://doi.org/10.1111/jgh.15386.<br />
16. Yin Y, Li Y, Shao L, Yuan S, Liu B, Lin S, et al. Effect of body<br />
mass index on the prognosis of liver cirrhosis. Front Nutr.<br />
2021;8:700132. https://doi.org/10.3389/fnut.2021.700132.<br />
17. Baradarian R, Ramdhaney S, Chapalamadugu R, Skoczylas L,<br />
Wang K, Rivilis S, et al. Early intensive resuscitation of patients<br />
with upper gastrointestinal bleeding decreases mortality. Am J<br />
Gastroenterol. 2004;99(4):619–22. https://doi.org/10.1111/j.1572-<br />
0241.2004.04073.x.<br />
18. Merola E, Michielan A, de Pretis G. Optimal timing of endoscopy<br />
for acute upper gastrointestinal bleeding: a systematic review and<br />
metaanalysis. Intern Emerg Med. 2021;16(5):1331–40. https://doi.<br />
org/10.1186/s12957-021-02122-8.<br />
19. Reiberger T, Püspök A, Schoder M, Baumann-Durchschein F,<br />
Bucsics T, Datz C, et al. Austrian consensus guidelines on the<br />
management and treatment of portal hypertension (Billroth III).<br />
Wien klin Wochenschr. 2017;129(Suppl3):135–58. https://doi.<br />
org/10.1007/s00508-017-1262-3.<br />
20. EASL Clinical Practice Guidelines for the management of patients<br />
with decompensated cirrhosis. J Hepatol. 2018;69(2):406–60.<br />
https://doi.org/10.1016/j.jhep.2018.03.024.<br />
21. Huh CW, Kim JS, Jung DH, Yang JD, Nam SW, Kwon JH, et al.<br />
Optimal endoscopy timing according to the severity of underlying<br />
liver disease in patients with acute variceal bleeding. Dig Liver Dis.<br />
2019;51(7):993–8. https://doi.org/10.1016/j.dld.2019.01.013<br />
22. Chen PH, Chen WC, Hou MC, Liu TT, Chang CJ, Liao WC, et al.<br />
Delayed endoscopy increases re-bleeding and mortality in patients<br />
with hematemesis and active esophageal variceal bleeding:<br />
a cohort study. J Hepatol. 2012;57(6):1207–13. https://doi.<br />
org/10.1016/j.jhep.2012.07.038.<br />
23. Badave RR, Tantry V, Gopal S, Shenoy S, Shetty A. Very early (<<br />
6 h) endoscopic therapy affects the outcome in acute variceal<br />
bleeding: a retrospective study from tertiary care hospital in<br />
south india. J Clin Exp Hepatol. 2017;7(Suppl 2):65. https://doi.<br />
org/10.1016/j.jceh.2017.05.122.<br />
24. Wang Z, Gao F. Analysis of timing and influencing factors of<br />
endoscopic diagnosis and treatment for cirrhotic patients<br />
with esophageal variceal bleeding. Chin J Gastroenterol.<br />
2018;23(11):673–8.<br />
25. Peng Y, Qi X, Guo X. Child-Pugh versus MELD score for<br />
the assessment of prognosis in liver cirrhosis: a systematic<br />
review and meta-analysis of observational studies.<br />
Medicine. 2016;95(8):e2877. https://doi.org/10.1097/<br />
md.0000000000002877.<br />
26. Bambha K, Kim WR, Pedersen R, Bida JP, Kremers WK,<br />
Kamath PS. Predictors of early re-bleeding and mortality after<br />
acute variceal haemorrhage in patients with cirrhosis. Gut.<br />
2008;57(6):814–20. https://doi.org/10.1136/gut.2007.137489.<br />
27. Reverter E, Tandon P, Augustin S, Turon F, Casu S, Bastiampillai<br />
R, et al. A MELD-based model to determine risk of mortality<br />
among patients with acute variceal bleeding. <strong>Gastroenterology</strong>.<br />
2014;146(2):412–19.e3. https://doi.org/10.1053/j.<br />
gastro.2013.10.018.<br />
Publisher’s Note<br />
Springer Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affiliations.<br />
Revolutionise Your IBD Management:<br />
FEATURE<br />
IBDoc ® Calprotectin Home Test with<br />
Swift, Direct to Patient Delivery<br />
Discover the future of<br />
healthcare at your<br />
doorstep with our<br />
all-new direct to patient<br />
kit delivery for the IBDoc ®<br />
calprotectin self-testing system. This solution<br />
empowers both patients and clinicians, redefining<br />
IBD management.<br />
As pioneers in innovative healthcare<br />
solutions, we're proud to announce our<br />
enhanced approach to home testing logistics.<br />
Alpha Laboratories now presents the<br />
opportunity for direct IBDoc ® kit delivery,<br />
14 right to the patients’ homes.<br />
15<br />
f<br />
f<br />
f<br />
f<br />
Removes requirement for administrative logistics<br />
in sending kits to patients<br />
Improves shelf life and stock level management<br />
Tracked deliveries:<br />
Z<br />
Z<br />
Weekly reports of dispatch requests available<br />
Billing only when kits are sent out<br />
Flexible delivery options (number of kits and location)<br />
02380 483000 • sales@alphalabs.co.uk • www.alphalabs.co.uk<br />
Elevate Your<br />
Healthcare Approach<br />
with Seamless Remote<br />
Testing using the BUHLMANN IBDoc ® :<br />
f Excellent correlation with laboratory<br />
tests and endoscopic findings<br />
f Swift quantitative testing, giving results<br />
the same day for the clinical team and the patient<br />
f Minimized pre-analytical errors thanks to simple<br />
sample preparation<br />
f Individualised kit containing everything the patient<br />
needs for a single test<br />
Elevate your IBD management today<br />
Reach out to us at digestivedx@alphalabs.co.uk<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong>
FEATURE ADVERTORIAL FEATURE<br />
ADVERTORIAL FEATURE<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
BUILDING DREAM<br />
TEAMS IN GREEN<br />
ENDOSCOPY<br />
AN INTERVIEW WITH PROF. SEBASTIAN<br />
Healthcare practitioners and industry members across the<br />
world are thinking about how to mitigate the environmental<br />
footprint of endoscopy. The modus operandi of the<br />
entire endoscopy patient journey is being scrutinized<br />
from evaluating appropriateness of the procedures, the<br />
endoscopy room environment, the instruments that are<br />
used during clinical procedures, to the equipment that is<br />
employed in the reprocessing room.<br />
The growth in society guidelines and position statements<br />
on green endoscopy underlines this movement well.<br />
For example, the European Society of Gastrointestinal<br />
Endoscopy (ESGE) and European Society of<br />
<strong>Gastroenterology</strong> and Endoscopy Nurses and Associates<br />
(ESGENA) 1 published their position statement on reducing<br />
the environmental footprint of gastrointestinal endoscopy.<br />
The British Society of <strong>Gastroenterology</strong> (BSG), Joint<br />
Accreditation Group (JAG) and Centre for Sustainable<br />
Health (CSH) 2 also published a joint consensus on practical<br />
measures for environmental sustainability in endoscopy.<br />
Prof. Shaji Sebastian, Consultant Gastroenterologist, IBD<br />
Unit, Hull University Teaching Hospitals, is the lead author<br />
Prof. Sebastian discussed how to become sustainable in endoscopy with<br />
Prof. Pohl and Prof. Bisschops, during the PENTAX Medical Hygiene Event.<br />
of the BSG, JAG and CSH joint consensus. We recently<br />
spoke with him about the `sustainable future` of endoscopy<br />
and how to create green endoscopy dream teams.<br />
What measures can endoscopy departments implement<br />
to mitigate their environmental footprints?<br />
There are many ‘low-hanging fruits’ that can minimize a<br />
department’s environmental footprint. One of the most important<br />
aspects is reducing unnecessary procedures, as the biggest<br />
amount of waste in endoscopy is the procedure that was not<br />
needed in the first place. The endoscopy services should have<br />
better vetting procedures to determine the appropriateness of<br />
an endoscopy. Additionally, rationalizing the use of endoscopic<br />
biopsies and where possible using enhanced imaging techniques<br />
to reduce the need for biopsies and adopting resect and discard<br />
policies for diminutive polyps can be incorporated within the<br />
endoscopy departments. One US study, analyzing whether biopsy<br />
pots could be reduced or whether their size could be reduced,<br />
found statistical improvement 3 . As practitioners, we must consider<br />
how we can implement such findings across our endoscopy units.<br />
Ambitious targets are being set by national health services<br />
and ministries. What is essential in achieving this?<br />
It is promising to see regulatory bodies set such ambitious targets.<br />
For example, in the United Kingdom we have committed to net zero<br />
by 2040 (Scope 1 and Scope 2 emissions). I fully embrace these<br />
ambitions, as I believe if we don’t reach for the sky, we won’t get off<br />
the ground. The only way we will achieve this is by working together.<br />
We must collectively find sustainable alternatives that reduce the<br />
impact of our endoscopic procedures.<br />
Alongside this, practitioners must provide regulatory bodies with<br />
information and guidance. We must publish practical guidelines,<br />
even in areas where it may be difficult to obtain such evidence.<br />
Think of infection risks, for example. These vary on a case-by-case<br />
basis, which makes it difficult to establish significant findings. As<br />
1<br />
de Santiago ER, Dinis-Ribeiro M, Pohl H, et al. Reducing the environmental footprint of gastrointestinal endoscopy: European Society of gastrointestinal endoscopy<br />
(ESGE) and European Society of gastroenterology and endoscopy nurses and associates (ESGENA) position statement. Endoscopy. 2022;54(08):797-826.<br />
2<br />
Sebastian S, Dhar A, Baddeley R, et al. Green endoscopy: British Society of <strong>Gastroenterology</strong> (BSG), Joint Accreditation Group (JAG) and Centre for<br />
physicians, and reprocessing nurses, we must provide policymakers<br />
with the right clinical evidence, so their legal expertise can guide us<br />
towards the right decisions.<br />
16 Sustainable Health (CSH) joint consensus on practical measures for environmental sustainability in endoscopy. Gut. <strong>2023</strong>;72(1):12-26.<br />
17<br />
3<br />
Gordon IO, Sherman JD, Leapman, M, et al. Life Cycle Greenhouse Gas Emissions of Gastrointestinal Biopsies in a Surgical Pathology Laboratory.<br />
American Journal of Clinical Pathology. 2021; 156(4): 540-549.<br />
Prof. Shaji Sebastian, Consultant<br />
Gastroenterologist, IBD Unit, Hull<br />
University Teaching Hospitals<br />
Listen to the full dialogue:<br />
Patients must be involved in this<br />
as well. We see that they are<br />
becoming more environmentally<br />
aware and weighing up the<br />
impacts of specific interventions.<br />
Sometimes they are even okay<br />
with trading off some of their<br />
comfort, for example by using<br />
slightly less nitrous oxide during<br />
procedures. More and more<br />
of these patients will enter our<br />
hospital doors, and we must<br />
involve them as informed partners<br />
in decision-making.<br />
Industry has a key role to play too mainly working with researchers<br />
and endoscopy teams to come up with products and solutions<br />
which are not only advancing the applications of endoscopy for<br />
clinical care but also those that will support our green initiatives.<br />
How can the field move forward as one?<br />
A cultural change is happening as endoscopic units are<br />
transforming themselves into green endoscopy dream teams.<br />
Companies, such as PENTAX Medical, have sustainability high on<br />
their agenda and are looking to minimize the environmental impact<br />
of their solutions. Holistic thinking is being applied that spans from<br />
supply chain to waste generation considerations, new society<br />
guidelines that are being published and sustainable product design<br />
principles that are being implemented.<br />
Ultimately endoscopy needs to reinvent itself. We simply cannot<br />
go back to business as usual; we need to be part of the solution,<br />
not the problem. The key is for practitioners and industry to<br />
work together, find solutions, and collaborate on this journey for<br />
environmental sustainability. Pictures of our beautiful planet must<br />
be kept in mind during these discussions, and together we must<br />
act in the long-term interest of our children and future generations.<br />
This is why we should care about green endoscopy.<br />
The endoscopic field is embarking on a steadfast<br />
sustainability transformation journey, whereby<br />
systems-level thinking is prioritized. The entire<br />
product development cycle is being reevaluated<br />
and all aspects – from device design, to materials,<br />
distribution and disposal – are being challenged.<br />
Through innovation and collaboration, medical<br />
solutions are increasingly coming to fruition that<br />
minimize the environmental footprint of the field.<br />
PENTAX Medical is a responsible medical devices’<br />
manufacturer, committed to offering holistic hygiene<br />
solutions that embody the “Power of Choice.” This<br />
allows healthcare professionals to select a range<br />
of options, including reusable, semi-disposable,<br />
and single-use endoscopes aimed at optimizing<br />
patient outcomes. By focusing on these core<br />
elements, PENTAX Medical strives to establish new<br />
benchmarks in hygiene, underlining its dedication to<br />
patient safety and infection prevention in endoscopy.<br />
The recently launched PENTAX Medical INSPIRA TM<br />
video processor and AquaTYPHOON TM pre-cleaning<br />
solution exemplify PENTAX Medical commitment<br />
to ensuring environmental responsibility, while<br />
delivering excellence in medical technology. The<br />
video processor upgrades legacy endoscope<br />
portfolios to the latest imaging standard, extending<br />
the life cycle of each endoscope and providing<br />
a future-proof platform for the next generation<br />
medical solutions. Reversely, the AquaTYPHOON TM<br />
revolutionizes pre-cleaning by eliminating<br />
consumables, such as brushes or detergents, and<br />
reducing water consumption by 70%–89% (evaluated<br />
by internal tests against standard manual precleaning<br />
procedures by PENTAX Medical). These<br />
innovations, as well as many others, make PENTAX<br />
Medical the partner of choice for practitioners that<br />
are seeking to balance sustainability and hygiene in<br />
their endoscopy suites.<br />
Imprint:<br />
PENTAX Europe GmbH,<br />
Julius-Vosseler-Str. 104, 22527 Hamburg, Germany<br />
W: https://www pentaxmedical.com<br />
T: +49 40 561 92 0<br />
E: info.emea@pentaxmedical.com<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong>
FEATURE<br />
FEATURE<br />
Three-part single-use<br />
sterile packed liner<br />
system reduces the<br />
potential for crosscontamination<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
CLEANASCOPE <br />
Transport & Short Term Storage System<br />
Confidence is knowing its clean at a glance<br />
Robust reusable tray<br />
easily fits large<br />
endoscopes<br />
Large locking castor wheels<br />
make transport easy and smooth<br />
CLEANASCOPE <br />
Transport & Short<br />
Term Storage System<br />
CLEANASCOPE ® Family<br />
Contact us<br />
Email: hcoperations_steris@steris.com<br />
Transport & Short Term Storage Carts<br />
Tel: (0)116 274 0600<br />
18 19<br />
Cantel Medical (Italy) S.r.l.<br />
Via Laurentina, 169 - 00071 Pomezia (RM) - Italy<br />
Trays fit perfectly into<br />
the contoured tray top to<br />
support workflow<br />
Provides protected<br />
short-term storage<br />
of clean scopes and<br />
equipment<br />
Hard lids available for added protection<br />
when transporting outside department.<br />
Available in 5, 6 and 10 tray options.<br />
NON-ALCOHOLIC FATTY LIVER<br />
DISEASE IN HEMOCHROMATOSIS<br />
PROBANDS WITH IRON OVERLOAD<br />
AND HFE P.C282Y/P.C282Y<br />
James C. Barton 1,2*† , J. Clayborn Barton 2† and Ronald T. Acton 2,3†<br />
Barton et al. BMC <strong>Gastroenterology</strong> (<strong>2023</strong>) 23:137 https://doi.org/10.1186/s12876-023-02763-x<br />
RESEARCH<br />
Abstract<br />
Background The aim of this study was to identify characteristics<br />
of non-alcoholic fatty liver disease (NAFLD) in adults<br />
with HFE p.C282Y/p.C282Y.<br />
Methods We retrospectively studied non-Hispanic white<br />
hemochromatosis probands with iron overload (serum ferritin (SF) ><br />
300 μg/L (M), > 200 μg/L (F)) and p.C282Y/p.C282Y at non-screening<br />
diagnosis who did not report alcohol consumption > 14 g/d, have<br />
cirrhosis or other non-NAFLD liver disorders, use steatogenic<br />
medication, or have diagnoses of heritable disorders that increase<br />
NAFLD risk. We identified NAFLD-associated characteristics using<br />
univariate and multivariable analyses.<br />
Results There were 66 probands (31 men, 35 women), mean age<br />
49 ± 14 (SD) y, of whom 16 (24.2%) had NAFLD. The following<br />
characteristics were higher in probands with NAFLD: median SF<br />
(1118 μg/L (range 259, 2663) vs. 567 μg/L (247, 2385); p = 0.0192);<br />
prevalence of elevated ALT/AST (alanine/aspartate aminotransferase)<br />
(43.8% vs. 10.0%; p = 0.0056); and prevalence of type 2 diabetes<br />
(T2DM) (31.3% vs. 10.0%; p = 0.0427). Mean age, sex, and prevalences<br />
of human leukocyte antigen-A*03 positivity, body mass index ≥ 30.0<br />
kg/m 2 , hyperlipidemia, hypertension, and metabolic syndrome in<br />
probands with/without NAFLD did not differ significantly. Logistic<br />
regression on NAFLD using variables SF, elevated ALT/AST, and T2DM<br />
revealed: SF (p = 0.0318; odds ratio 1.0–1.0) and T2DM (p = 0.0342;<br />
1.1–22.3). Median iron removed to achieve iron depletion (QFe) in<br />
probands with/without NAFLD did not differ significantly (3.6 g (1.4–7.2<br />
g) vs. 2.8 g (0.7–11.0 g), respectively; p = 0.6862).<br />
Conclusions NAFLD in hemochromatosis probands with p.C282Y/p.<br />
C282Y is associated with higher median SF and greater T2DM<br />
†<br />
James C. Barton, J. Clayborn Barton and Ronald T. Acton contributed equally to this work.<br />
*Correspondence:<br />
James C. Barton<br />
bartonjames336@gmail.com<br />
1<br />
Department of Medicine, University of Alabama at Birmingham, Birmingham, AL, USA<br />
2<br />
Southern Iron Disorders Center, Birmingham, AL, USA<br />
3<br />
Department of Microbiology, University of Alabama at Birmingham, Birmingham, AL, USA<br />
prevalence, after adjustment for other factors. NAFLD does not<br />
influence QFe significantly.<br />
Keywords Alanine aminotransferase, Aspartate aminotransferase,<br />
Metabolic syndrome, Obesity, Serum ferritin, Type 2 diabetes<br />
Background<br />
Non-alcoholic fatty liver disease (NAFLD) is a spectrum of liver<br />
abnormalities characterized by steatosis (lipidfilled vacuoles in<br />
hepatocytes), steatohepatitis (steatosis and hepatocyte “ballooning”<br />
with inflammation and necrosis), fibrosis, and cirrhosis [1, 2]. It has<br />
been estimated that 25.2% (95% confidence interval (CI) [22.1, 28.7]) of<br />
persons world-wide have NAFLD [2]. In a metaanalysis of 34 studies,<br />
the prevalence of NAFLD in U.S. whites was 14.4% (95% CI [14.0, 14.8])<br />
[3]. Co-morbid conditions associated with NAFLD include obesity,<br />
type 2 diabetes (T2DM), hyperlipidemia, hypertension, and metabolic<br />
syndrome (MetS) [2].<br />
Hemochromatosis in whites of western European descent is<br />
associated with homozygosity for HFE p.C282Y (rs1800562),<br />
a common missense allele of the homeostatic iron regulator<br />
(chromosome 6p22.2) in linkage disequilibrium with human<br />
leukocyte antigen (HLA)-A*03 [4, 5]. HFE, a non-classical class I<br />
major histocompatibility complex protein, is an upstream regulator<br />
of hepcidin and thus of iron homeostasis [6]. Laboratory phenotypes<br />
of many adults at diagnosis of hemochromatosis and p.C282Y/p.<br />
C282Y include elevated levels of transferrin saturation (TS) and serum<br />
ferritin (SF) [7]. Adults with p.C282Y/p.C282Y have increased risks to<br />
develop iron overload. Severe iron overload occurs predominantly in<br />
men [7, 8]. Non-HFE heritable and environmental variables modify iron<br />
loading in adults with hemochromatosis [5, 7, 9, 10]. Some adults with<br />
p.C282Y/p.C282Y also have hemochromatosis arthropathy, diabetes<br />
mellitus, hypogonadotropic hypogonadism, hepatic cirrhosis, or<br />
cardiomyopathy [7].<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong>
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
FEATURE<br />
The aim of this study was to identify characteristics of non-alcoholic<br />
fatty liver disease (NAFLD) in adults with HFE p.C282Y/p.C282Y.<br />
We performed a retrospective study of clinical and laboratory<br />
characteristics of unrelated non-Hispanic white adults with<br />
hemochromatosis, iron overload, and p.C282Y/p.C282Y at nonscreening<br />
diagnosis. The present probands, with or without NAFLD,<br />
did not report alcohol consumption > 14 g/d, have other liver disorders,<br />
report using steatogenic medication, or have diagnoses of heritable<br />
disorders that increase NAFLD risk. We identified significant NAFLDassociated<br />
characteristics using univariate and multivariable analyses.<br />
We discuss our findings in the context of previous observations of<br />
co-morbid conditions associated with NAFLD in adults who were and<br />
were not selected for HFE genotypes.<br />
Methods<br />
Subjects included<br />
We compiled data on consecutive self-identified non-Hispanic whites<br />
aged ≥ 18 y referred to an Alabama tertiary hematology center<br />
(1989–2005) for evaluation and management of hemochromatosis<br />
who met the following criteria: (a) had HFE p.C282Y/p.C282Y, (b)<br />
had iron overload defined as serum ferritin (SF) > 300 μg/L (M)<br />
or > 200 μg/L (F) [11, 12], (c) underwent HLA-A typing, (d) had no<br />
known cause of secondary iron overload, (e) started and achieved<br />
iron depletion with therapeutic phlebotomy at this center, and (f)<br />
were the first in their respective families to be diagnosed to have<br />
hemochromatosis (probands).<br />
Medical histories were taken from probands and records of referring<br />
physicians. Referring physicians diagnosed and treated probands<br />
with diabetes, hypertension, and hyperlipidemia. Physicians in the<br />
present hematology center evaluated probands for hemochromatosis<br />
arthropathy, hypogonadotropic hypogonadism, cirrhosis, and<br />
cardiomyopathy, as appropriate. All probands underwent medication<br />
review, physical examination, laboratory testing, imaging procedures,<br />
and evaluation of liver and other conditions, as indicated, before<br />
therapeutic phlebotomy was initiated.<br />
Subjects excluded<br />
We excluded probands with any of the following: (a) diagnosis of<br />
hyperferritinemia, hemochromatosis, or HFE p.C282Y/p.C282Y<br />
in family or population screening, (b) diagnosis of any primary or<br />
secondary hematologic disorder, (c) report of alcohol consumption<br />
> 14 g/d drinkequivalent [13], (d) use of steatogenic medication(s)<br />
[14], (e) diagnosis of a heritable disorder that increases NAFLD risk<br />
[15, 16], (f) volunteer whole-blood donation > two units in the year<br />
before hemochromatosis diagnosis, (g) bariatric operations [17], (h)<br />
viral hepatitis B or C infection, (i) hepatic transient fibroelastography<br />
(FibroScan ® , Echosens, Waltham, MA, USA) suggestive of severe<br />
hepatic fibrosis (≥ 9.4 kilopascals) or cirrhosis (≥ 11.0 kilopascals), (j)<br />
biopsy-proven cirrhosis, k) liver transplant, l) diagnosis of malignancy,<br />
m) anti-cancer therapy, n) chronic inflammatory conditions, or o)<br />
selfreported pregnancy.<br />
Laboratory<br />
Blood specimens were collected during mornings without regard<br />
to fasting. TS and SF were measured using standard methods<br />
(Laboratory Corporation of America, Burlington, NC, USA). We defined<br />
these TS and SF phenotypes to be elevated: TS > 50% (men) and TS<br />
> 45% (women); and SF > 300 μg/L (men) and SF > 200 μg/L (women)<br />
[11, 12].<br />
Serum alanine aminotransferase (ALT) and aspartate aminotransferase<br />
(AST) were measured using standard methods (Laboratory<br />
Corporation of America, Burlington, NC, USA). We defined upper limits<br />
of normal for ALT and AST as > 40 IU/L, respectively. We created<br />
a single dichotomous variable representing either elevated ALT or<br />
elevated AST (elevated ALT/AST).<br />
HFE allele analyses were performed as previously described [18].<br />
We demonstrated HFE p.C282Y homozygosity in 1996 or later in all<br />
probands regardless of dates of diagnoses. We defined HLA-A*03 as<br />
the marker of the hemochromatosis ancestral haplotype [18]. Positivity<br />
for A*03 was defined as A*03 homozygosity or heterozygosity.<br />
Liver biopsy<br />
We recommended that probands undergo percutaneous liver<br />
biopsy (or not) in accordance with hemochromatosis diagnosis and<br />
management guidelines of the American Association for the Study of<br />
Liver Diseases [19].<br />
Diagnosis of non-alcoholic fatty liver disease<br />
We diagnosed NAFLD according to the Practice Guideline of the<br />
American Association for the Study of Liver Diseases, American<br />
College of <strong>Gastroenterology</strong>, and the American Gastroenterological<br />
Association [20]. Diagnostic criterion was steatosis detected either<br />
by interpretation of liver biopsy specimens [1, 20], increased hepatic<br />
echogenicity [20, 21], or attenuation difference between liver and<br />
spleen on unenhanced CT scanning images [22], in the absence of<br />
self-report of alcohol consumption > 14 g/d drink-equivalent [13],<br />
cirrhosis or other non-NAFLD liver disorder, use of steatogenic<br />
medication [14], or diagnosis of a heritable disorder associated with<br />
increased NAFLD risk [15, 16].<br />
Definition of fibrosis-four variables and AST-to-platelet<br />
ratio indices<br />
We computed the AST-to-platelet ratio index (APRI) [23] and fibrosisfour<br />
variables (FIB-4) index [24] in all probands. Threshold (or greater)<br />
values of each index are associated with increased risk for advanced<br />
hepatic fibrosis (stage F3, severe fibrosis with architectural distortion<br />
or stage F4, cirrhosis with architectural distortion) [25]. In a previous<br />
study of adults with hemochromatosis, APRI values > 3.25 had a<br />
positive predictive value for cirrhosis of 65% and a specificity of 97%<br />
[26]. FIB-4 index > 1.10 identified adults with HFE p.C282Y/p.C282Y<br />
with advanced fibrosis with 80% sensitivity, 80% specificity, and 81%<br />
accuracy [26].<br />
Definition of iron removed to achieve iron depletion<br />
Iron depletion therapy, defined as the periodic removal of blood to<br />
eliminate storage iron, was performed in all probands as described<br />
elsewhere [27]. Iron depletion therapy was complete when SF was ≤ 20<br />
μg/L [27]. Iron removed by phlebotomy to achieve iron depletion (QFe)<br />
was estimated to be 200 mg Fe per unit of blood (450–500 mL) [27].<br />
Definitions of other conditions<br />
Definitions of hemochromatosis arthropathy, hypogonadotropic<br />
hypogonadism, cirrhosis, and cardiomyopathy are displayed in<br />
Additional file 1 [.docx; Other diagnostic criteria].<br />
We defined obesity as ≥ 30.0 kg/m 2 [28]. We classified diabetes<br />
according to criteria of the American Diabetes Association [29].<br />
We grouped medical histories of essential hypertension or use of<br />
prescription anti-hypertensive drugs in a dichotomous hypertension<br />
variable. We grouped medical histories of hyperlipidemia or<br />
use of prescription lipid-lowering drugs in a dichotomous<br />
hyperlipidemia variable.<br />
We defined metabolic syndrome (MetS) as the concurrence of the<br />
following three attributes: BMI ≥ 30 kg/m 2 ; systolic blood pressure<br />
≥ 130 mm Hg or diastolic blood pressure ≥ 85 mm Hg; and fasting<br />
serum glucose ≥ 100 mg/dL [28, 30, 31]. We grouped positivity for<br />
these three attributes in a dichotomous MetS variable.<br />
Statistics<br />
The dataset for analyses consisted of complete observations at<br />
diagnosis of hemochromatosis, iron overload, and HFE p.C282Y/p.<br />
C282Y in 66 probands. Age, TS, and SF values are displayed to the<br />
nearest integer. Descriptive data are displayed as enumerations,<br />
percentages (with/without 95% CI), means (± 1 standard deviation<br />
(SD)), or medians (range).<br />
Kolmogorov-Smirnov testing demonstrated that age and TS values did<br />
not differ significantly from those which are normally distributed. We<br />
displayed corresponding values as mean ± 1 SD and compared values<br />
using Student’s t test for unpaired data (two-tailed). We displayed other<br />
continuous variables as medians (range) and compared them using<br />
Mann-Whitney U test (twotailed). We compared percentages using<br />
Fisher’s exact test (two-tailed). We did not use a Bonferroni “correction”<br />
for univariate comparisons because many data were not positively<br />
associated and we did not wish to produce “false negative” results [32].<br />
We performed logistic regression on NAFLD by relaxing the “rule” of<br />
ten events per variable [33] and using independent variables identified<br />
in univariate comparisons for which “uncorrected” values of p were ≤<br />
0.1500 (SF, elevated ALT/AST, and T2DM).<br />
We defined p < 0.05 to be significant. We used Excel ® 2000 (Microsoft<br />
Corp., Redmond, WA, USA), GB-Stat ® (v. 10.0, Dynamic Microsystems,<br />
Inc., Silver Spring, MD, USA), and GraphPad Prism 8 ® (2018; GraphPad<br />
Software, San Diego, CA, USA).<br />
Results<br />
General characteristics of probands<br />
There were 31 men (47.0%) and 35 women (53.0%) of mean age 49<br />
± 14 y. NAFLD was diagnosed in 16 probands (24.2%; 95% CI [14.9,<br />
36.6]). All probands underwent one or more imaging procedures that<br />
detect NAFLD [1, 20, 21]. Thirty-five probands (53.0%) underwent liver<br />
biopsy. Of 16 probands with NAFLD, 11 (68.8%) underwent liver biopsy.<br />
Of 50 probands without NAFLD, 24 (48.0%) underwent liver biopsy.<br />
These percentages did not differ significantly (p = 0.1653). Twentyone<br />
probands (31.8%) underwent liver ultrasonography. Percentages of<br />
probands with and without NAFLD evaluated with liver ultrasonography<br />
did not differ significantly (25.0% vs. 34.0%, respectively; p = 0.5562).<br />
Eighteen probands (27.3%) underwent abdominal CT scanning.<br />
Percentages of probands with and without NAFLD evaluated<br />
with liver ultrasonography did not differ significantly<br />
(25.0% vs. 34.0%, respectively; p = 0.5562). Eighteen<br />
probands (27.3%) underwent abdominal FEATURE<br />
CT scanning.<br />
Percentages of probands with and without NAFLD evaluated<br />
with abdominal CT scanning did not differ significantly<br />
(18.8% of probands vs. 30.0%, with and respectively; without NAFLD p = evaluated 0.5245). with Eleven<br />
Percentages<br />
abdominal probands CT (16.7%) scanning did underwent not differ significantly liver evaluations (18.8% vs. 30.0%, with<br />
respectively; two of these p = 0.5245). modalities. Eleven Percentages probands (16.7%) of underwent probands liver with<br />
evaluations and without NAFLD two of these evaluated modalities. with Percentages two modalities of probands did<br />
with not and differ without significantly NAFLD evaluated (25.0% with two vs. modalities 14.0%, did respectively;<br />
not differ<br />
significantly p = 0.4402). (25.0% Two vs. probands 14.0%, respectively; underwent p = 0.4402). fibroelastography<br />
Two probands<br />
underwent as part of fibroelastography experimental or as part pre-marketing of experimental protocols or pre-marketing (n = 2;<br />
protocols<br />
3.0%). Cirrhosis<br />
(n = 2; 3.0%).<br />
was<br />
Cirrhosis<br />
not diagnosed<br />
was not diagnosed<br />
in any proband<br />
in any proband<br />
based<br />
based on clinical, liver on clinical, liver biopsy, or imaging abnormalities.<br />
Three of 16 probands (18.8%) with NAFLD had none of<br />
Three of 16 probands (18.8%) with NAFLD had none of the NAFLD comorbid<br />
conditions we studied. Median SF and prevalences of elevated<br />
the NAFLD co-morbid conditions we studied. Median SF<br />
and prevalences of elevated ALT/AST and T2DM were<br />
ALT/AST and T2DM were greater in probands with than without NAFLD<br />
greater in probands with than without NAFLD (Table 1).<br />
(Table 1).<br />
Table 1 Characteristics of hemochromatosis probands with HFE<br />
p.C282Y/p.C282Y a<br />
Characteristic<br />
Hemochromatosis arthropathy was diagnosed in 24 probands<br />
(36.4%). The prevalence of hemochromatosis arthropathy did not<br />
differ significantly in probands with and without NAFLD (31.3% vs.<br />
38.3%, respectively; p ~ 1.0000). No proband was diagnosed to have<br />
hypogonadotropic hypogonadism, cirrhosis, or cardiomyopathy.<br />
The prevalence of elevated ALT/AST was significantly greater in<br />
probands with than without NAFLD (Table 1). The prevalence of<br />
elevated ALT was greater in probands with than without NAFLD (37.5%<br />
vs. 8.0%, respectively; p = 0.0009). The prevalence of elevated AST<br />
was greater in probands with than without NAFLD (43.8% vs. 4.0%,<br />
respectively; p = 0.0004). Nine of 16 probands with NAFLD (56.3%) did<br />
not have elevated ALT or AST.<br />
NAFLD<br />
(n = 16)<br />
No<br />
NAFLD<br />
(n = 50)<br />
Value<br />
of p<br />
Age at diagnosis, y (± 1 SD) 51 ± 13 49 ± 15 0.6614<br />
Men, % (n) 56.3 (9) 44.0 (22) 0.5659<br />
Mean transferrin saturation, % (± 1 SD) 77 ± 14 83 ± 17 0.1626<br />
Median serum ferritin, µg/L (range) 1118<br />
(259,<br />
2663)<br />
567 (247,<br />
2385)<br />
No proband had APRI > 0.44, although median APRI was greater in<br />
probands with than without NAFLD (0.15 (range 0.07–0.37) vs. 0.10<br />
(range 0.04–0.23); p = 0.0025). Median FIB-4 in probands with and<br />
without NAFLD did not differ significantly (1.10 (range 0.53–3.29) vs.<br />
0.99 (range 0.28–4.99); p = 0.2915). One woman with and another<br />
0.0192<br />
HLA-A*03 positivity, % (n) 75.0 (12) 82.0 (41) 0.7187<br />
Elevated ALT/AST, % (n) 43.8 (7) 10.0 (5) 0.0056<br />
Obesity (BMI ≥ 30.0 kg/m 2 ), % (n) 18.9 (3) 16.0 (8) ~ 1.0000<br />
Diabetes, type 2, % (n) 31.3 (5) 10.0 (5) 0.0427<br />
Hypertension, % (n) 25.0 (4) 18.0 (9) 0.7187<br />
Hyperlipidemia, % (n) 6.3 (1) 12.0 (6) 1.0000<br />
Metabolic syndrome, % (n) 0.0 (0) 4.0 (2) ~ 1.0000<br />
a All observations were recorded at diagnosis. Blood specimens were collected<br />
during mornings without regard to fasting. ALT, alanine aminotransferase; AST,<br />
aspartate aminotransferase; BMI, body mass index; HLA, human leukocyte<br />
antigen; NAFLD, non-alcoholic fatty liver disease; SD, standard deviation. No<br />
proband had hypogonadotropic hypogonadism, cirrhosis, or cardiomyopathy.<br />
respect<br />
NAFLD<br />
No p<br />
was gre<br />
(range<br />
Median<br />
did no<br />
0.99 (r<br />
and an<br />
althoug<br />
reveal c<br />
Co-mor<br />
liver di<br />
The pr<br />
than w<br />
of obe<br />
proban<br />
cantly<br />
Logistic<br />
Logisti<br />
using t<br />
ALT/A<br />
tions:<br />
error 0<br />
1.5973<br />
p = 0.03<br />
NAFLD<br />
(1.094–<br />
Iron rem<br />
Median<br />
not diff<br />
respect<br />
Discus<br />
The p<br />
associa<br />
adults<br />
p.C282<br />
tion > 1<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
20 21
FEATURE<br />
FEATURE<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
woman without NAFLD had FIB-4 > 3.25, although their respective liver<br />
biopsy specimens did not reveal cirrhosis.<br />
Co-morbid conditions associated with non-alcoholic fatty<br />
liver disease<br />
The prevalence of T2DM was greater in probands with than without<br />
NAFLD (Table 1). Respective prevalences of obesity, hypertension,<br />
hyperlipidemia, and MetS in probands with and without NAFLD did not<br />
differ significantly (Table 1).<br />
Logistic regression on non-alcoholic fatty liver disease<br />
Logistic regression on NAFLD, the dependent variable, using the<br />
qualifying independent variables SF, elevated ALT/AST, and T2DM,<br />
revealed two positive associations: SF (p = 0.0318; beta coefficient<br />
0.0011; standard error 0.0005) and T2DM (p = 0.0342; beta coefficient<br />
1.5973; standard error 0.7543). This regression (ANOVA p = 0.0362)<br />
accounted for 11.6% of the variance of NAFLD. Odds ratios were SF<br />
(1.000-1.002) and T2DM (1.094–22.311).<br />
Iron removed by phlebotomy to achieve depletion<br />
Median QFe in probands with and without NAFLD did not differ<br />
significantly (3.6 g (1.4–7.2) vs. 2.8 g (0.7–11.0), respectively;<br />
p = 0.6862).<br />
Discussion<br />
The present study evaluated clinical and laboratory associations of<br />
NAFLD in a cohort of non-screening adults with hemochromatosis,<br />
iron overload, and HFE p.C282Y/p.C282Y who did not report alcohol<br />
consumption > 14 g/d, have cirrhosis or other liver disorders, report<br />
using steatogenic medication, or have diagnoses of heritable disorders<br />
that increase NAFLD risk. The prevalence of NAFLD in the present<br />
cohort was 24.2% (95% CI [14.9, 36.6]). In a meta-analysis of 43<br />
studies with 5,758 NAFLD cases and 14,741 controls from diverse<br />
geographic regions, “a significantly increased risk of NAFLD was<br />
observed for the C282Y polymorphism in the Caucasian population<br />
under all genetic models [34].“ In the same meta-analysis, NAFLD risk<br />
in adults with p.C282Y/p.C282Y and adults with wt/wt (absence of<br />
p.C282Y and p.H63D (rs1799945)) did not differ significantly [34].<br />
Median SF was almost two-fold greater in the present probands with<br />
than without NAFLD. In patients with hemochromatosis and HFE<br />
p.C282Y homozygosity, there was is a significant positive correlation<br />
of phlebotomy-mobilized iron with hepatic iron concentration [35],<br />
although QFe in the present study did not differ significantly in<br />
probands with and without NAFLD. In another study, median SF level<br />
but not hepatic iron concentration was significantly higher in p.C282Y<br />
homozygotes with than without hepatic steatosis [36]. Together,<br />
these observations indicate that NAFLD contributes significantly to<br />
hyperferritinemia but not iron overload in p.C282Y homozygotes.<br />
Prevalences of elevated ALT and elevated AST were greater in the<br />
present probands with than without NAFLD, although 56.3% of<br />
probands with NAFLD had neither elevated ALT nor elevated AST,<br />
and elevated ALT/AST was not significantly associated with NAFLD<br />
in a logistic regression. In a meta-analysis of 11 studies of patients<br />
unselected for HFE genotypes, 25% of patients with NAFLD and 19%<br />
of patients with non-alcoholic steatohepatitis had ALT values within<br />
the reference range [37]. These observations suggest that evaluation<br />
for NAFLD should be considered at diagnosis in all subjects with<br />
hemochromatosis and HFE p.C282Y/p.C282Y, regardless of ALT and<br />
AST levels, although current guidelines for hemochromatosis diagnosis<br />
and management do not recommend evaluation for NAFLD in all<br />
patients with or suspected to have hemochromatosis [19].<br />
The prevalence of obesity (BMI ≥ 30 kg/m 2 ) in the present cohort<br />
(15.2% (95% CI [7.9–26.6]) did not differ significantly in probands with<br />
and without NAFLD. We found no reports of the prevalence of obesity<br />
in screening programs that evaluated participants with HFE p.C282Y/p.<br />
C282Y. It is estimated that the worldwide prevalence of obesity in<br />
subjects with NAFLD is ~ 51% [2].<br />
In a Utah study [38], white men with HFE p.C282Y/p.C282Y aged ≥<br />
40 y had significantly lower mean BMI (26.7 ± 0.5 kg/m 2 ) than control<br />
siblings without p.C282Y/p.C282Y (30.5 ± 1.6 kg/m 2 ) and male 1999–<br />
2002 National Health and Nutrition Examination Survey participants<br />
(28.7 ± 0.3 kg/m 2 ) [38]. Corresponding comparisons in women were<br />
not significant [38]. In a U.S. atherosclerosis risk screening program,<br />
median BMI did not differ significantly in 44 white participants with<br />
p.C282Y/p.C282Y (26.5 kg/m 2 (standard error (SE) 0.1)) and 6768 white<br />
participants with wt/wt (26.9 kg/m 2 (SE 0.1)) [39]. Thus, it is uncertain<br />
whether BMI in adults with p.C282Y/p.C282Y differs from that in adults<br />
in the general U.S. population.<br />
Prevalence of T2DM was greater in the present probands with than<br />
without NAFLD. T2DM was also significantly associated with NAFLD,<br />
after adjustment for other variables. These observations suggest<br />
that presence of T2D at diagnosis in hemochromatosis and HFE<br />
p.C282Y/p.C282Y should prompt evaluations for NAFLD. In a study<br />
of 159 non-screening Alabama adult hemochromatosis probands<br />
with HFE p.C282Y/p.C282Y, predictors of T2DM at hemochromatosis<br />
diagnosis were diabetes reports in first-degree family members (odds<br />
ratio 8.5 (95% CI [2.9, 24.8])) and BMI ≥ 30.0 kg/m 2 (odds ratio 1.1<br />
(95% CI [1.0, 1.2])). In another study, NAFLD was also a significant risk<br />
factor for concurrent or future T2DM diagnoses in adults unselected<br />
for HFE genotypes in the general population [40, 41]. Together, these<br />
observations indicate that NAFLD, diabetes reports in firstdegree<br />
family members, and obesity are associated with T2DM in adults with<br />
p.C282Y/p.C282Y.<br />
The prevalence of hypertension in the present cohort was 19.7%<br />
(95% CI [11.3, 31.7]). The prevalence of hypertension in probands with<br />
and without NAFLD did not differ significantly, although NAFLD is a<br />
possible risk factor for hypertension [42, 43]. In studies of Scandinavian<br />
population cohorts, HFE p.C282Y/p.C282Y and extremely elevated TS,<br />
either separately or combined, were associated with increased risk of<br />
anti-hypertension medication use [44].<br />
The prevalence of hyperlipidemia in the present cohort was 10.6%<br />
(95% CI [4.7, 21.2]). The prevalence of hyperlipidemia in the present<br />
probands with and without NAFLD did not differ significantly. In an<br />
atherosclerosis risk screening study, mean low-density lipoprotein<br />
(LDL) cholesterol was lower in participants with HFE p.C282Y/p.C282Y<br />
than wt/wt [39]. In a primary carebased hemochromatosis and iron<br />
overload screening study, participants with p.C282Y/p.C282Y had<br />
lower total and LDL cholesterol levels than participants with wt/wt<br />
[45]. It has been postulated that lower LDL cholesterol in adults with<br />
p.C282Y/p.C282Y is an effect of excess iron on cholesterol metabolism<br />
and lipoprotein formation in the liver [39]. Triglyceride levels in subjects<br />
with p.C282Y/p.C282Y and wt/wt in two population screening<br />
programs did not differ significantly [39, 45].<br />
MetS was uncommon in the present cohort (3.0% (95% CI [0.5,<br />
11.5])) and the prevalence of MetS in probands with and without<br />
NAFLD did not differ significantly. In a post-screening evaluation of<br />
248 participants with HFE p.C282Y/p.C282Y, the prevalence of MetS<br />
was also relatively low 7.3% (95% CI [4.5, 11.4]) [46]. We attribute the<br />
relatively low prevalence of MetS in the present cohort to relatively low<br />
prevalences of obesity, hypertension, and hyperlipidemia.<br />
Probands with cirrhosis were excluded from the present study,<br />
although < 8% of adults with HFE p.C282Y/p.C282Y diagnosed in<br />
either screening or non-screening cohorts published in the 21st<br />
century have cirrhosis [47]. In a multi-institutional study, cirrhosis in<br />
patients with p.C282Y/p.C282Y was significantly associated with age,<br />
diabetes, daily alcohol intake, and iron removed by phlebotomy, taking<br />
into account the effect of other variables, although the prevalence of<br />
fatty liver/steatosis did not differ significantly in 86 adults with and 282<br />
adults without cirrhosis (27.4% and 33.0%, respectively; p = 0.4400)<br />
[8]. In a large study of healthcare records in UK, Netherlands, Italy and<br />
Spain, the hazard ratio for cirrhosis in patients with NAFLD was 4.73<br />
(95% CI [2.43, 9.19]), although the strongest independent predictor of<br />
cirrhosis was a baseline diagnosis of diabetes [48]. In a study that did<br />
not include subjects with p.C282Y/p.C282Y, SF, age, BMI, and diabetes<br />
were independent predictors of histologic severity and advanced<br />
fibrosis in patients with NAFLD [49]. Together, these observations<br />
suggest that age and diabetes are greater risk factors for cirrhosis in<br />
adults with p.C282Y/p.C282Y than NAFLD.<br />
In summary, the percentage of the present hemochromatosis<br />
probands with NAFLD (24.2%; 95% CI [14.9, 36.6]) was higher than<br />
that of whites in general U.S. populations (14.4%; 95% CI [14.0, 14.8])<br />
[3]. In a metaanalysis of global populations, co-morbid conditions<br />
associated with NAFLD included obesity, T2DM, hyperlipidemia,<br />
hypertension, and MetS [2], whereas T2D alone was significantly<br />
associated with NAFLD in the present hemochromatosis probands.<br />
Referring physicians diagnosed and treated the present probands with<br />
diabetes, hypertension, and hyperlipidemia and thus their evaluations<br />
and diagnostic criteria for these disorders may differ from those of<br />
large population studies. LDL cholesterol [39, 45] and total cholesterol<br />
[45] levels are lower in adults with HFE p.C282Y/p.C282Y than wt/<br />
wt. These factors could account in part for the absence of NAFLD<br />
risk factors we studied in 18.8% of the present probands. It is also<br />
plausible that probands without NAFLD risk factors we studied have<br />
other undiagnosed or undocumented conditions that increase NAFLD<br />
risk, including obstructive sleep apnea [50], hypothyroidism [51, 52],<br />
hypopituitarism [53], or heritable disorder(s) [15, 16].<br />
A strength of the present study is analyses based on observations<br />
of non-screening adults with hemochromatosis, iron overload, and<br />
HFE p.C282Y/p.C282Y, with or without NAFLD, who did not report<br />
alcohol consumption > 14 g/d, have cirrhosis or other liver disorders,<br />
report using steatogenic medication, or have diagnoses of heritable<br />
disorders that increase NAFLD risk. The present study does not<br />
permit a comparison of the sensitivity and specificity of liver biopsy,<br />
ultrasonography, and CT scanning in diagnosing NAFLD. It is also<br />
plausible that the lack of significant difference of the prevalence of<br />
NAFLD co-morbid factors other than T2DM we studied between<br />
probands with and without NAFLD may in part reflect type 2 statistical<br />
error(s). Evaluating subgroups of probands with NAFLD based on ALT/<br />
AST values or liver morphology [2] or alcoholic/non-alcoholic fatty liver<br />
scores/indices, detecting alleles associated with increased NAFLD<br />
risk [15, 16], determining the effects of therapeutic phlebotomy on<br />
ALT and AST levels, treating NAFLD, and evaluating of post-diagnosis<br />
observations other than QFe were beyond the scope of this work.<br />
Conclusions<br />
We conclude that NAFLD in hemochromatosis probands with iron<br />
overload and HFE p.C282Y/p.C282Y is associated with higher median<br />
SF and greater T2DM prevalence, after adjustment for other factors.<br />
NAFLD does not influence QFe significantly.<br />
List of abbreviations<br />
ALD alcoholic liver disease<br />
ALT alanine aminotransferase<br />
ANI alcoholic liver disease/non-alcoholic fatty liver disease index<br />
APRI AST-to-platelet ratio index<br />
AST aspartate aminotransferase<br />
BMI body mass index<br />
CI confidence interval<br />
FIB-4 fibrosis-four variables<br />
HFE homeostatic iron regulator gene<br />
HLA human leukocyte antigen<br />
LDL low-density lipoprotein<br />
MetS metabolic syndrome<br />
NAFLD non-alcoholic fatty liver disease<br />
QFe quantity of iron removed by phlebotomy to achieve iron depletion<br />
SD standard deviation<br />
SE standard error<br />
SF serum ferritin<br />
T2DM type 2 diabetes mellitus<br />
TS transferrin saturation<br />
Supplementary Information<br />
The online version contains supplementary material available at<br />
https://doi.org/10.1186/s12876-023-02763-x.<br />
Supplementary Material 1. Definitions of other conditions<br />
Acknowledgements<br />
Not applicable.<br />
Author contributions<br />
JaCB evaluated probands, conceived this study and its methodology,<br />
curated data, performed analyses, and drafted the manuscript. JClB<br />
conceived study methodology, curated data, performed analyses, and<br />
drafted the manuscript. RTA conceived this study and its methodology,<br />
performed analyses, and drafted the manuscript. Each author<br />
approved the manuscript in its final form.<br />
Funding<br />
The authors received no specific funding for this work.<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
22 23
FEATURE<br />
FEATURE<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
Data Availability<br />
The dataset generated and/or analysed during the current study is<br />
available in the Open Science Framework repository (https://osf.io/<br />
j5gsp/). Data were compiled and displayed in a manner that maintains<br />
proband anonymity. Definitions of hemochromatosis arthropathy,<br />
hypogonadotropic hypogonadism, cirrhosis, and cardiomyopathy are<br />
displayed in Additional file 1 [.docx; Other diagnostic criteria].<br />
Declarations<br />
Ethics approval and consent to participate<br />
This work was performed according to the principles of the Declaration<br />
of Helsinki [43]. Performance of this study was approved by Western<br />
Institutional Review Board, Inc. (submission 2539985–44189619).<br />
The need for obtaining informed consent from participants in this<br />
study was waived by Western Institutional Review Board under United<br />
States Department of Health and Human Services, Office for Human<br />
Research Participants, regulation 45 CFR 46.101(b)(4).<br />
Consent for publication<br />
Not applicable.<br />
Competing interests<br />
None of the authors has a conflict of interest to report.<br />
Received: 13 January <strong>2023</strong> / Accepted: 11 April <strong>2023</strong><br />
Published online: 28 April <strong>2023</strong><br />
References<br />
1. Brunt EM, Tiniakos DG. Histopathology of nonalcoholic fatty liver<br />
disease. World J Gastroenterol. 2010;16:5286–96.<br />
2. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M.<br />
Global epidemiology of nonalcoholic fatty liver disease - Metaanalytic<br />
assessment of prevalence, incidence, and outcomes.<br />
Hepatology. 2016;64:73–84.<br />
3. Rich NE, Oji S, Mufti AR, Browning JD, Parikh ND, Odewole<br />
M, et al. Racial and ethnic disparities in nonalcoholic fatty liver<br />
disease prevalence, severity, and outcomes in the United States: a<br />
systematic review and meta-analysis. Clin Gastroenterol Hepatol.<br />
2018;16:198–210.<br />
4. Feder JN, Gnirke A, Thomas W, Tsuchihashi Z, Ruddy DA, Basava<br />
A, et al. A novel MHC class I-like gene is mutated in patients with<br />
hereditary haemochromatosis. Nat Genet. 1996;13:399–408.<br />
5. Barton JC, Edwards CQ, Acton RT. HFE gene: Structure, function,<br />
mutations, and associated iron abnormalities. Gene. 2015;574:179<br />
– 92.<br />
6. Rishi G, Wallace DF, Subramaniam VN. Hepcidin: regulation of the<br />
master iron regulator. Biosci Rep. 2015;35:e00192.<br />
7. Edwards CQ, Barton JC. Hemochromatosis. In: Greer JP, Rodgers<br />
GM, Glader B, Arber DA, Means RT Jr, List AF, et al. editors.<br />
Wintrobe’s clinical hematology. Philadelphia: Wolters Kluwer; 2019.<br />
pp. 665–90.<br />
8. Barton JC, McLaren CE, Chen WP, Ramm GA, Anderson GJ,<br />
Powell LW, et al. Cirrhosis in hemochromatosis: independent<br />
risk factors in 368 HFE p.C282Y homozygotes. Ann Hepatol.<br />
2018;17:871–9.<br />
9. Wood MJ, Powell LW, Ramm GA. Environmental and genetic<br />
modifiers of the progression to fibrosis and cirrhosis in<br />
hemochromatosis. Blood. 2008;111:4456–62.<br />
10. Martin M, Millan A, Ferraro F, Tetzlaff WF, Lozano CE, Botta E et al.<br />
Leukocyte telomere length is associated with iron overload in male<br />
adults with hereditary hemochromatosis.Biosci Rep. 2020;40.<br />
11. Adams PC, Reboussin DM, Barton JC, McLaren CE, Eckfeldt JH,<br />
McLaren GD, et al. Hemochromatosis and iron-overload screening<br />
in a racially diverse population. N Engl J Med. 2005;352:1769–78.<br />
12. Barton JC, Acton RT, Dawkins FW, Adams PC, Lovato L,<br />
Leiendecker-Foster C, et al. Initial screening transferrin saturation<br />
values, serum ferritin concentrations, and HFE genotypes in whites<br />
and blacks in the Hemochromatosis and Iron Overload Screening<br />
Study. Genet Test. 2005;9:231–41.<br />
13. Bowman SA, Friday JE, Thoerig RC, Moshfegh AJ. Food Patterns<br />
Equivalents Database 2011-12: Methodology and User Guide<br />
[Online]. Food Surveys Research Group, Beltsville Human Nutrition<br />
Research Center, Agricultural Research Service, U. S. Department<br />
of Agriculture, Beltsville, Maryland. http://www.ars.usda.gov/nea/<br />
bhnrc/fsrg. Accessed 2 Jul 2022.<br />
14. Patel V, Sanyal AJ. Drug-induced steatohepatitis. Clin Liver Dis.<br />
2013;17:533–46. vii.<br />
15. Dongiovanni P, Anstee QM, Valenti L. Genetic predisposition<br />
in NAFLD and NASH: impact on severity of liver disease and<br />
response to treatment. Curr Pharm Des. 2013;19:5219–38.<br />
16. Xia MF, Bian H, Gao X. NAFLD and diabetes: two sides of the<br />
same coin? Rationale for gene-based personalized NAFLD<br />
treatment. Front Pharmacol. 2019;10:877.<br />
17. Barton JC. Hemochromatosis, HFE C282Y homozygosity, and<br />
bariatric surgery: report of three cases. Obes Surg. 2004;14:1409–14.<br />
18. Barton JC, Barton JC, Acton RT. HLA-A*03, the hemochromatosis<br />
ancestral haplotype, and phenotypes of referred hemochromatosis<br />
probands with HFE p.C282Y homozygosity. Hereditas.<br />
2022;159:25.<br />
19. Bacon BR, Adams PC, Kowdley KV, Powell LW, Tavill AS.<br />
Diagnosis and management of hemochromatosis: 2011 Practice<br />
Guideline by the American Association for the study of Liver<br />
Diseases. Hepatology. 2011;54:328–43.<br />
20. Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K,<br />
et al. The diagnosis and management of non-alcoholic fatty liver<br />
disease: practice Guideline by the American Association for the<br />
Study of Liver Diseases, American College of <strong>Gastroenterology</strong>,<br />
and the American Gastroenterological Association. Hepatology.<br />
2012;55:2005–23.<br />
21. Khov N, Sharma A, Riley TR. Bedside ultrasound in the diagnosis<br />
of nonalcoholic fatty liver disease. World J Gastroenterol.<br />
2014;20:6821–5.<br />
22. Lee SS, Park SH. Radiologic evaluation of nonalcoholic fatty liver<br />
disease. World J Gastroenterol. 2014;20:7392–402.<br />
23. Lin ZH, Xin YN, Dong QJ, Wang Q, Jiang XJ, Zhan SH, et al.<br />
Performance of the aspartate aminotransferase-to-platelet ratio<br />
index for the staging of hepatitis C-related fibrosis: an updated<br />
meta-analysis. Hepatology. 2011;53:726–36.<br />
24. Sterling RK, Lissen E, Clumeck N, Sola R, Correa MC, Montaner<br />
J, et al. Development of a simple noninvasive index to predict<br />
significant fibrosis in patients with HIV/HCV coinfection.<br />
Hepatology. 2006;43:1317–25.<br />
25. Scheuer PJ. Classification of chronic viral hepatitis: a need for<br />
reassessment. J Hepatol. 1991;13:372–4.<br />
26. Chin J, Powell LW, Ramm LE, Hartel GF, Olynyk JK, Ramm GA.<br />
Utility of serum biomarker indices for staging of hepatic fibrosis<br />
before and after venesection in patients with hemochromatosis<br />
caused by variants in HFE. Clin Gastroenterol Hepatol.<br />
2021;19:1459–68.<br />
27. Adams PC, Barton JC. How I treat hemochromatosis. Blood.<br />
2010;116:317–25.<br />
28. Acton RT, Barton JC, Barton JC. Serum ferritin, insulin resistance,<br />
and metabolic syndrome: clinical and laboratory associations in<br />
769 non-hispanic whites without diabetes mellitus in the HEIRS<br />
Study. Metab Syndr Relat Disord. 2015;13:57–63.<br />
29. American Diabetes Association. 2. Classification and diagnosis of<br />
diabetes: Standards of Medical Care in Diabetes-2020. Diabetes<br />
Care. 2020;43:14–S31.<br />
30. Ford ES. Prevalence of the metabolic syndrome defined by<br />
the International Diabetes Federation among adults in the U.S.<br />
Diabetes Care. 2005;28:2745–9.<br />
31. Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato<br />
KA et al. Harmonizing the metabolic syndrome: a joint interim<br />
statement of the International Diabetes Federation Task Force on<br />
Epidemiology and Prevention; National Heart, Lung, and Blood<br />
Institute; American Heart Association; World Heart Federation;<br />
International Atherosclerosis Society; and International Association<br />
for the Study of Obesity. Circulation. 2009;120:1640-5.<br />
16. Sivero, L. et al. Endoscopic diagnosis and treatment of<br />
32. Armstrong RA. When to use the Bonferroni correction. Ophthalmic<br />
neuroendocrine tumors of the digestive system. Open Med. 11(1),<br />
Physiol Opt. 2014;34:502–8.<br />
33.<br />
369–373.<br />
Vittinghoff<br />
https://doi.org/10.1515/med-2016-0067<br />
E, McCulloch CE. Relaxing the rule of ten<br />
(2016).<br />
events<br />
17. Witteman, per variable B. in J., logistic Janssens, and Cox A. R., regression. Griffi oen, G. Am & J Lamers, Epidemiol. C. B.<br />
Villous 2007;165:710–8.<br />
tumours of the duodenum. An analysis of the literature with<br />
34. emphasis Ye Q, Qian on BX, malignant Yin WL, transformation. Wang FM, Han Neth. T. Association J. Med. 42, between 5 (1993). the<br />
18. Levine,<br />
HFE C282Y,<br />
J. A., Burgart,<br />
H63D polymorphisms<br />
L. J., Batts, K.<br />
and<br />
P. &<br />
the<br />
Wang,<br />
risks<br />
K.<br />
of non-alcoholic<br />
K. Brunner’s<br />
fatty liver disease, liver cirrhosis and hepatocellular carcinoma: an<br />
gland hamartomas: Clinical presentation and pathological features<br />
updated aystematic review and meta-analysis of 5,758 cases and<br />
of 27 cases. Am. J. Gastroenterol. 90, 290–294 (1995).<br />
14,741 controls. PLoS ONE. 2016;11:e0163423.<br />
35. 19. Noguchi, Phatak PD, H. et Barton al. Prevalence JC. Phlebotomy-mobilized of Helicobacter pylori iron as infection a surrogate rate<br />
in for heterotopic liver iron content gastric in mucosa hemochromatosis in histological patients. analysis Hematology. of duodenal<br />
specimens 2003;8:429–32. from patients with duodenal ulcer. Histol. Histopathol.<br />
36. 35(2), Powell 169–176. EE, Ali A, https://doi.org/10.14670/HH-18-142 Clouston AD, Dixon JL, Lincoln DJ, Purdie (2020) DM,<br />
(Epub et al. 2019 Steatosis Jul 2). is a cofactor in liver injury in hemochromatosis.<br />
20. Singhal,<br />
<strong>Gastroenterology</strong>.<br />
S. et al. Anorectal<br />
2005;129:1937–43.<br />
gastrointestinal stromal tumor: A case<br />
37. Ma X, Liu S, Zhang J, Dong M, Wang Y, Wang M, et al.<br />
report and literature review. Case Rep. Gastrointest. Med. 2013,<br />
Proportion of NAFLD patients with normal ALT value in overall<br />
934875 (2013).<br />
NAFLD patients: a systematic review and meta-analysis. BMC<br />
21. Modlin, Gastroenterol. I. M., Lye, 2020;20:10. K. D. & Kidd, M. A 5-decade analysis of 13,715<br />
38. carcinoid Abbas MA, tumors. Abraham Cancer D, Kushner 97, 934–959 JP, McClain (2003). DA. Anti-obesity and<br />
22. Bulur, pro-diabetic A. al. effects Polypoid of hemochromatosis. lesions detected in Obes the upper (Silver Spring).<br />
gastrointestinal 2014;22:2120–2. endoscopy: A retrospective analysis in 19560<br />
39. patients, Pankow a JS, single-center Boerwinkle study E, Adams of a 5-year PC, Guallar experience E, Leiendecker- in Turkey.<br />
N.<br />
Foster<br />
Clin. Istanb.<br />
C, Rogowski<br />
8(2), 178–185.<br />
J, et al. HFE<br />
https://doi.org/10.14744/<br />
C282Y homozygotes have<br />
nci.2020.16779<br />
reduced low-density<br />
(2020).<br />
lipoprotein cholesterol: the atherosclerosis<br />
risk in Communities (ARIC) Study. Transl Res. 2008;152:3–10.<br />
40. 23. Kostiainen, Adams LA, S., Waters Teppo, OR, L. Knuiman & Virkkula, MW, L. Papilloma Elliott RR, of Olynyk the JK.<br />
oesophagus. NAFLD as a Report risk factor of a for case. the development Scand. J. Thorac. of diabetes Cardiovasc. and<br />
Surg. the metabolic 7(1), 95–97. syndrome: https://doi.org/10.3109/14017437309139176<br />
an eleven-year follow-up study. Am J<br />
(1973). Gastroenterol. 2009;104:861–7.<br />
41. 24. Mandard, Tokita Y, A. Maejima M. et al. Y, Shimomura Cancer of the K, esophagus Takenoshita and S, Ishiyama associated N,<br />
lesions: Akuzawa Detailed M, al. pathologic Non-alcoholic study fatty of 100 liver esophagectomy<br />
disease is a risk factor<br />
specimens. for type 2 diabetes Hum. Pathol. in middle-aged 15, 660 (1984). Japanese men and women.<br />
Intern Med. 2017;56:763–71.<br />
42.<br />
25. Levine,<br />
Zhao YC,<br />
J. A.,<br />
Zhao<br />
Burgart,<br />
GJ, Chen<br />
L. J.,<br />
Z,<br />
Batts,<br />
She ZG,<br />
K. P.<br />
Cai<br />
& Wang,<br />
J, Li H.<br />
K.<br />
Nonalcoholic<br />
K. Brunner’s<br />
gland fatty hamartomas: liver disease: an Clinical emerging presentation driver of and hypertension. pathological features<br />
of Hypertension. 27 cases. Am. 2020;75:275–84.<br />
J. Gastroenterol. 90(2), 290–294 (1995).<br />
43. 26. Ma, Kasper M. X. P, & Martin Bourke, A, M. Lang J. S, Management Demir M, Steffen of duodenal HM. Hypertension polyps. Best in<br />
Pract. NAFLD: Res. an Clin. uncontrolled Gastroenterol. burden. 31(4), J Hepatol. 389–399 2021;74:1258–60.<br />
(2017).<br />
44. Ellervik C, Tybjaerg-Hansen A, Appleyard M, Ibsen H,<br />
Nordestgaard BG. Haemochromatosis genotype and iron<br />
Author contributions<br />
overload: association with hypertension and left ventricular<br />
Ç.E., M.Y.: hypertrophy. conception, J Intern design, Med. supervision, 2010;268:252–64. materials, data collection<br />
45. and processing, Adams PC, analysis Pankow and JS, interpretation, Barton JC, Acton literature RT, Leiendecker-<br />
review, writer<br />
and critical Foster review. C, McLaren D.A., B.Y., GD, et K.K. al. O.C., HFE C282Y İ.T., H.T.K.: homozygosity materials, is data<br />
associated with lower total and lowdensity lipoprotein cholesterol:<br />
collection and processing, analysis and interpretation, literature review<br />
the hemochromatosis and Iron overload screening study. Circ<br />
and manuscript Cardiovasc supervision. Genet. 2009;2:34–7.<br />
46. Barton JC, Barton JC, Adams PC, Acton RT. Risk factors for<br />
Competing insulin resistance, interests metabolic syndrome, and diabetes in 248 HFE<br />
C282Y homozygotes identified by population screening in the<br />
The authors declare no competing interests.<br />
HEIRS Study. Metab Syndr Relat Disord. 2016;14:94–101.<br />
47. Barton JC, Acton RT. Diabetes in HFE hemochromatosis. J<br />
Additional Diabetes information Res. 2017;2017:9826930.<br />
48. Correspondence Alexander M, and Loomis requests AK, for van materials der Lei should J, Duarte-Salles be addressed T, Prieto-<br />
Ç.E.<br />
Alhambra D, Ansell D, et al. Risks and clinical predictors of<br />
cirrhosis and hepatocellular carcinoma diagnoses in adults with<br />
Reprints diagnosed and permissions NAFLD: real-world information study is of available 18 million at patients in four<br />
www.nature.com/reprints.<br />
European cohorts. BMC Med. 2019;17:95.<br />
49. Kowdley KV, Belt P, Wilson LA, Yeh MM, Neuschwander-Tetri<br />
BA, Chalasani N, et al. Serum ferritin is an independent predictor<br />
Publisher’s note Springer Nature remains neutral with regard to<br />
of histologic severity and advanced fibrosis in patients with<br />
jurisdictional nonalcoholic claims fatty in published liver disease. maps Hepatology. and institutional 2012;55:77–85. affi liations.<br />
50. Mesarwi OA, Loomba R, Malhotra A. Obstructive sleep apnea,<br />
Open hypoxia, Access and This nonalcoholic article is licensed fatty under liver disease. a Creative Am Commons J Respir Crit Care<br />
Med. 2019;199:830–41.<br />
Attribution 4.0 International License, which permits use, sharing,<br />
51. Lonardo A, Ballestri S, Mantovani A, Nascimbeni F, Lugari S, Targher<br />
adaptation, G. Pathogenesis distribution of and hypothyroidism-induced reproduction in any medium NAFLD: or evidence format, as for a<br />
long as distinct you give disease appropriate entity? credit Dig Liver to the Dis. original 2019;51:462–70. author(s) and the source,<br />
52. provide Manka a link P, to Bechmann the Creative L, Commons Best J, Sydor licence, S, Claridge and indicate LC, Coombes if changes<br />
JD, et al. Low free triiodothyronine is associated with advanced<br />
were made. The images or other third party material in this article are<br />
fibrosis in patients at high risk for nonalcoholic steatohepatitis. Dig<br />
included Dis in Sci. the 2019;64:2351–8.<br />
article’s Creative Commons licence, unless indicated<br />
53. otherwise Itoh E, in a Hizuka credit N, line Fukuda to the material. I, Takano If K. material Metabolic is not disorders included in adult the<br />
article’s growth Creative hormone Commons deficiency: licence a and study your of intended 110 patients use is at not a single permitted<br />
institute in Japan. Endocr J. 2006;53:539–45.<br />
by statutory regulation or exceeds the permitted use, you will need to<br />
obtain permission directly from the copyright holder. To view a copy of this<br />
Publisher’s Note<br />
licence, visit http:// creat iveco mmons. org/ licen ses/ by/4. 0/.<br />
Springer Nature remains neutral with regard to jurisdictional claims in<br />
© The Author(s) <strong>2023</strong><br />
published maps and institutional affiliations.<br />
WHY NOT WRITE FOR US?<br />
<strong>Gastroenterology</strong> <strong>Today</strong> welcomes the submission of<br />
clinical papers and case reports or news that<br />
you feel will be of interest to your colleagues.<br />
Material submitted will be seen by those working within all<br />
UK gastroenterology departments and endoscopy units.<br />
All submissions should be forwarded to info@mediapublishingcompany.com<br />
If you have any queries please contact the publisher Terry Gardner via:<br />
info@mediapublishingcompany.com<br />
GASTROENTEROLOGY TODAY TODAY – WINTER - SUMMER <strong>2023</strong> <strong>2023</strong><br />
24 25 11
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong><br />
COMPANY NEWS<br />
Tune in to PENTAX Medical<br />
Latest Podcast!<br />
Ulrike Beilenhoff (ESGENA Scientific<br />
Secretary) and Prof. dr. Marco<br />
Bruno (Head of the Department of<br />
<strong>Gastroenterology</strong> & Hepatology, Erasmus<br />
Medical Center) reflect on minimizing<br />
the risk of infection in endoscope<br />
reprocessing, touching on pivotal topics<br />
such as the role of manual bedside<br />
cleaning, the risk of biofilm formation,<br />
how to trace a potential infection and the<br />
importance of training. Listen now:<br />
Micro-Tech’s VacStent Gi<br />
We are very pleased to announce that<br />
Micro-Tech’s revolutionary designed<br />
VacStent Gi is now available and being<br />
utilised by NHS England.<br />
The VacStent GI combines two reliable<br />
methods for the treatment of leakage<br />
and anastomotic insufficiency: while the<br />
fully encased stent completely covers the<br />
defects, the wound cavity is drained by<br />
continuous suction.<br />
The VacStent Gi is an innovation in<br />
endoscopic therapy for leaks because it<br />
COMBINES the advantages of the covered<br />
stent with those of improving wound healing<br />
through vacuum drainage.<br />
The innovative product consists of a siliconecoated,<br />
self-expanding super elastic nitinol<br />
stent with a cylindrical polyurethane sponge<br />
on the outside, connected via catheter to<br />
a vacuum source. A continuous suction of<br />
-80 to -120 mm Hg is applied to the sponge.<br />
VacStent GI is as easy to apply as any GI<br />
stent. It won’t dislocate because the suction<br />
keeps it in place, even in difficult topographic<br />
locations of the GI tract. However, it allows for<br />
the open passage of endoscopic instruments,<br />
enteral nutrition, and intestinal contents.<br />
VacStent GI has obtained the CE mark as a<br />
class 2 A medical device. Clinical applications<br />
in the oesophagus have so far been carried<br />
out as part of clinical studies, accompanied<br />
and then unaccompanied implantations.<br />
If you want to know more about our VacStent<br />
Gi or start a product trial, please do get in<br />
touch and we would be happy to assist.<br />
Visit our website on: www.micro-tech-uk.com,<br />
contact us by email sales@micro-tech-uk.com<br />
or call us on (+44) 20 8016 1990.<br />
Searching for New<br />
International Distributors<br />
With a legacy of excellence spanning<br />
over five decades, Alpha Laboratories is<br />
renowned for providing top-tier laboratory<br />
and diagnostic products, to professionals<br />
worldwide. Our commitment to quality,<br />
innovation, and customer satisfaction<br />
has set us apart as a trusted brand,<br />
supporting healthcare, research and<br />
industrial scientists.<br />
Based in the UK, we serve our international<br />
customers through valued relationships<br />
with our overseas distributors. We are now<br />
looking to further expand this family and are<br />
actively seeking new alliances with partners<br />
in France, the Middle East and certain other<br />
markets, including but not limited to, countries<br />
such as USA, India, Singapore, Malaysia<br />
and Indonesia.<br />
I am John Murphy, Alpha Laboratories’<br />
International Business Manager and I extend<br />
a warm invitation to potential distributors<br />
to collaborate with us. Here’s what you<br />
can expect:<br />
• High Quality Products: Access to our<br />
extensive range of renowned laboratory<br />
products, including liquid handling tools,<br />
molecular biology and sample handling<br />
consumables, plus our extensive range of<br />
packaging solutions for UN3373 compliance<br />
for biological sample transport.<br />
• Global Reach: Join a global network of<br />
distributors, benefiting from our established<br />
presence in over 20 countries.<br />
• Training and Support: We provide<br />
comprehensive training, marketing<br />
materials, and ongoing support to help you<br />
excel in your role.<br />
• Innovation: Stay ahead in the industry with<br />
our innovative products and technologies.<br />
• Growth Opportunities: Be part of a<br />
company that’s constantly growing, with a<br />
proven track record of success.<br />
Alpha Laboratories values partnership and<br />
collaboration, and we are excited to welcome<br />
new distributors to help us reach greater<br />
heights. If you are passionate about science,<br />
healthcare, and making a difference, and<br />
would like to join our success story, then this<br />
opportunity is for you.<br />
To learn more about becoming an Alpha<br />
Laboratories international distributor, please<br />
reach out to us at export@alphalabs.co.uk.<br />
Let’s work together to help advance scientific<br />
excellence, globally.<br />
TRIAGE GASTROSCOPY<br />
REFERRALS WITH<br />
GastroPanel® Quick Test<br />
GastroPanel® is a simple and effective noninvasive<br />
test to identify atrophic gastritis<br />
and Helicobacter pylori (H. pylori) prior to<br />
endoscopy.<br />
Atrophic gastritis – a chronic condition of the gastric<br />
mucosa, is considered to be the greatest independent<br />
risk factor for developing gastric cancer and guidelines<br />
recommend that individuals with extensive gastric<br />
atrophy undergo regular endoscopic surveillance<br />
to closely monitor their disease. Early detection<br />
of significant risk is the key to effective patient<br />
management, helping to reduce unnecessary referrals,<br />
and improve survival rates through earlier diagnoses.<br />
GastroPanel helps select cases for<br />
gastroscopy.<br />
GastroPanel is a simple, effective and low cost blood<br />
test that, through extensive validation, has consistently<br />
proven to be effective in the determination of chronic<br />
atrophic gastritis non-invasively. When GastroPanel<br />
is positive, it helps direct appropriate and effective<br />
treatment plans, including, enhanced image endoscopy,<br />
eradication therapy, and surveillance.<br />
GastroPanel measures three stomach biomarkers<br />
from a finger-prick or venous blood sample, enabling<br />
a thorough and objective investigation of the whole<br />
gastric mucosa, non-invasively, giving clinicians more<br />
confidence in their diagnoses and referrals.<br />
Scan to find out more or visit www.biohithealthcare.co.uk/gastropanel<br />
BIOHIT HealthCare Ltd<br />
Pioneer House, Pioneer Business Park, North Road,<br />
Ellesmere Port, Cheshire, United Kingdom CH65 1AD<br />
COMPANY NEWS<br />
GastroPanel measures concentrations of Pepsinogen I, Pepsinogen II,<br />
Gastrin-17 and H. pylori IgG and produces a comprehensive report.<br />
When endoscopy resources and capacity are<br />
stretched.<br />
This patient-friendly blood test can help transform<br />
the referral pathway for upper GI investigations by<br />
identifying those who need enhanced endoscopy<br />
with biopsies. Implementing GastroPanel could help<br />
to relieve the burden on overstretched endoscopy<br />
services, streamline referrals, and reduce costs.<br />
Tel. +44 151 550 4 550<br />
info@biohithealthcare.co.uk<br />
26 27<br />
www.biohithealthcare.co.uk<br />
GASTROENTEROLOGY TODAY – WINTER <strong>2023</strong>
Helicobacter Test INFAI ®<br />
One of the most used<br />
13<br />
C-urea breath tests for the diagnosis<br />
of Hp-infections worldwide<br />
• New line of INFAI packaging and serialization according the EU’s Falsified Medicines Directive<br />
• More than 7.0 million Helicobacter Test INFAI performed worldwide<br />
• Registered in more than 40 countries worldwide<br />
• First approved Hp test for children from the ages of 3 to 11<br />
• Modified Hp test for patients taking PPIs (REFEX)<br />
• Modified Hp test for patients with atrophic gastritis<br />
• Cost-effective CliniPac Basic for hospital and GPs use<br />
INFAI UK Ltd<br />
Innovation Centre, York Science Park<br />
University Road, Heslington<br />
York YO10 5DG UK<br />
Phone: +44 1904 435 228<br />
Fax: +44 1904 435 229<br />
E-Mail: mail@infai.co.uk<br />
Web: www.infai1.com