Ambulance UK April 2024
Ambulance UK April 2024
Ambulance UK April 2024
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
FEATURE<br />
FEATURE<br />
DISCUSSION: Discussion: WHERE Where IS Is the THE Occlusion? OCCLUSION?<br />
Jerry W. Jones, MD FACEP FAAEM<br />
Jerry W. Jones, MD FACEP FAAEM<br />
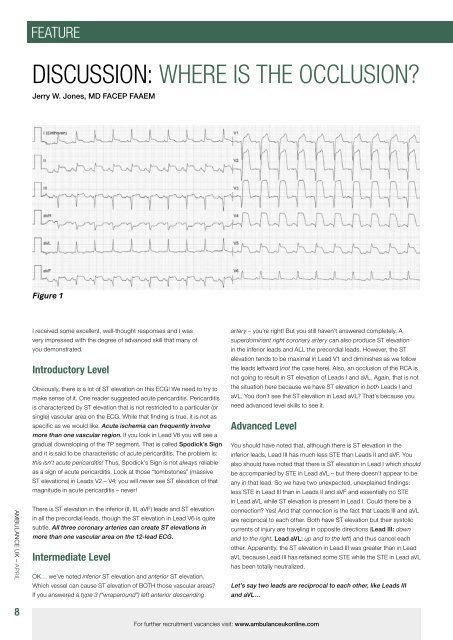
Figure 1<br />
Figure 1 (repeated)<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
8<br />
I received<br />
some excellent,<br />
some<br />
well-thought<br />
excellent,<br />
responses<br />
well-thought<br />
and I was<br />
responses<br />
artery – you’re<br />
and<br />
right!<br />
I<br />
But<br />
was<br />
you still<br />
very<br />
haven’t<br />
impressed<br />
answered completely.<br />
with<br />
A<br />
the<br />
very impressed with the degree of advanced skill that many of<br />
superdominant right coronary artery can also produce ST elevation<br />
degree of advanced skill that many of you demonstrated.<br />
you demonstrated.<br />
subtle. All three coronary arteries can create ST elevations in<br />
more than one vascular area on the 12-lead ECG.<br />
There is ST elevation in the inferior (II, III, aVF) leads and ST elevation in all the precordial<br />
other. Apparently, the ST elevation in Lead III was greater than in Lead<br />
Intermediate leads, though Level the ST elevation in Lead V6 is quite aVL because subtle. Lead All III has three retained coronary some STE while arteries the STE in Lead can aVL<br />
has been totally neutralized.<br />
create ST elevations in more than one vascular area on the 12-lead ECG.<br />
OK… we’ve noted inferior ST elevation and anterior ST elevation.<br />
in the inferior leads and ALL the precordial leads. However, the ST<br />
elevation tends to be maximal in Lead V1 and diminishes as we follow<br />
the leads leftward (not the case here). Also, an occlusion of the RCA is<br />
Introductory Level<br />
not going to result in ST elevation of Leads I and aVL. Again, that is not<br />
Obviously,<br />
Introductory<br />
there is a lot of ST<br />
Level<br />
elevation on this ECG! We need to try to the situation here because we have ST elevation in both Leads I and<br />
make sense of it. One reader suggested acute pericarditis. Pericarditis aVL. You don’t see the ST elevation in Lead aVL? That’s because you<br />
is Obviously, characterized by there ST elevation is a that lot is of not ST restricted elevation to a particular on (or this ECG! need advanced We need level skills to to try see to it. make sense of it. One<br />
single)<br />
reader<br />
vascular<br />
suggested<br />
area on the ECG.<br />
acute<br />
While<br />
pericarditis.<br />
that finding is true,<br />
Pericarditis<br />
it is not as<br />
is characterized by ST elevation that is not<br />
specific as we would like. Acute ischemia can frequently involve<br />
restricted<br />
more than one<br />
to<br />
vascular<br />
a particular<br />
region. If you<br />
(or<br />
look in<br />
single)<br />
Lead V6 you<br />
vascular<br />
will see a<br />
area<br />
Advanced<br />
on the ECG.<br />
Level<br />
While that finding is true, it is<br />
gradual not as downsloping specific of the as TP we segment. would That like. is called Acute Spodick’s ischemia Sign You should can have frequently noted that, although involve there is ST more elevation than in the one<br />
and it is said to be characteristic of acute pericarditis. The problem is: inferior leads, Lead III has much less STE than Leads II and aVF. You<br />
vascular region. If you look in Lead V6 you will see a gradual downsloping of the TP<br />
this isn’t acute pericarditis! Thus, Spodick’s Sign is not always reliable also should have noted that there is ST elevation in Lead I which should<br />
as segment. a sign of acute That pericarditis. is Look called at those Spodick’s “tombstones” (massive Sign and be accompanied it is said by STE to in be Lead characteristic aVL – but there doesn’t of appear acute to be<br />
ST elevations) in Leads V2 – V4; you will never see ST elevation of that<br />
pericarditis. The problem is: this isn’t acute pericarditis!<br />
any in that lead.<br />
Thus,<br />
So we have<br />
Spodick’s<br />
two unexpected,<br />
Sign<br />
unexplained<br />
is not<br />
findings:<br />
always<br />
magnitude in acute pericarditis – never!<br />
less STE in Lead III than in Leads II and aVF and essentially no STE<br />
reliable as a sign of acute pericarditis. Look at those<br />
in Lead aVL<br />
“tombstones”<br />
while ST elevation is present<br />
(massive<br />
in Lead<br />
ST<br />
I. Could<br />
elevations)<br />
there be a<br />
There<br />
in Leads<br />
is ST elevation<br />
V2 –<br />
in<br />
V4;<br />
the inferior<br />
you<br />
(II,<br />
will<br />
III, aVF)<br />
never<br />
leads and<br />
see<br />
ST elevation<br />
ST elevation connection? of that Yes! magnitude And that connection in is acute the fact that pericarditis Leads III and aVL –<br />
in all the precordial leads, though the ST elevation in Lead V6 is quite are reciprocal to each other. Both have ST elevation but their systolic<br />
never!<br />
currents of injury are traveling in opposite directions (Lead III: down<br />
and to the right, Lead aVL: up and to the left) and thus cancel each<br />
Which vessel can cause ST elevation of BOTH those vascular areas? Let’s say two leads are reciprocal to each other, like Leads III<br />
If you answered a type 3 (“wraparound”) left anterior descending and aVL…<br />
For further recruitment vacancies visit: www.ambulanceukonline.com<br />
Intermediate Level<br />
If one lead has acute ischemia with ST elevation and the other<br />
remains nonischemic, the nonischemic lead will act reciprocally<br />
and manifest the reciprocal changes of ST depression.<br />
However, if BOTH leads manifest acute ischemia with ST elevation, supports (but doesn’t prove) an occlusion proximal to D1 and distal to<br />
anterior<br />
then based on<br />
descending<br />
their relative locations<br />
artery<br />
to each<br />
–<br />
other,<br />
you’re<br />
the ST<br />
right!<br />
elevations<br />
But<br />
S1.<br />
you<br />
If haven’t<br />
still haven’t<br />
noticed it, look<br />
answered<br />
again before continuing.<br />
completely. A<br />
will cancel each other and it is possible that both leads will have<br />
3 (“wraparound”) LAD. Most people – between 75% to 80% – have<br />
and infarctions.<br />
located in the inferior wall caused by the occlusion of the LAD. So<br />
maybe it is and maybe it isn’t proximal to S1.<br />
OK… we’ve noted inferior ST elevation and anterior ST elevation. Which vessel can cause<br />
As advanced ECG nerds, you should have noticed something that<br />
ST elevation of BOTH those vascular areas? If you answered a type 3 (“wraparound”) left<br />
superdominant right coronary artery can also produce ST elevation in the inferior leads and<br />
normal-appearing ST segments!<br />
The first septal perforator supplies blood to the right bundle branch.<br />
ALL the precordial leads. However, the ST elevation Occlusions tends proximal to to S1 be will often maximal result in acute in Lead RBBB – a V1 very and<br />
Which artery is occluded and at which level is the<br />
ominous sign during an occlusion of the LAD. There is no RBBB<br />
diminishes as we follow the leads leftward (not the case here). Also, an occlusion of the<br />
occlusion located?<br />
present on this ECG. While that adds to the likelihood that the<br />
RCA is not going to result in ST elevation of Leads I and aVL. Again, that is not the situation<br />
occlusion is distal to S1 and proximal to D1, it unfortunately doesn’t<br />
The<br />
here<br />
infarct<br />
because<br />
related artery<br />
we<br />
(IRA)<br />
have<br />
– often<br />
ST<br />
referred<br />
elevation<br />
to as the “culprit”<br />
in both<br />
artery<br />
Leads<br />
prove<br />
I<br />
it.<br />
and aVL. You don’t see the ST elevation<br />
is the left anterior descending artery (LAD). In this case, it is a Type<br />
in Lead aVL? That’s because you need advanced level skills to see it.<br />
There is another issue with occlusions of a Type 3 (“wraparound”)<br />
a Type 3 LAD. It is by far the most common type of LAD and, when LAD: the ischemia causing the ST elevation in Leads I and aVL can<br />
occluded, can result in very complex, difficult-to-see acute ischemias – at times – perfectly cancel the ST elevation in Leads II, III and aVF!<br />
Advanced Level<br />
This will leave you with signs of acute ischemia only in the precordial<br />
leads. Now, the ischemic changes in the precordial leads of this ECG<br />
So, can we tell where the level of the infarction is located? We can are extremely impressive – but in other ECGs they may not be. In fact,<br />
definitely You should say that it have is proximal noted to the that, first diagonal although branch there (D1) is ST the precordial elevation leads in may the show inferior nothing more leads, than hyperacute Lead III T waves has<br />
because of the ST elevation that involves Leads V2 to V5, and the which could be missed by someone not as astute and skilled as you.<br />
much less STE than Leads II and aVF. You also should have noted that there is ST elevation<br />
ST elevation in Lead I (and presumably, Lead aVL). We used to think So, a proximal occlusion of a Type 3 (“wraparound”) LAD may appear<br />
that in Lead if ST elevation I which were present should in Lead be V1, accompanied then the occlusion was by STE like in a Lead minor, distal aVL occlusion – but when there – in doesn’t fact – it is quite appear large! to be<br />
automatically any in that proximal lead. to the So first we septal have perforator two branch unexpected, (S1). While unexplained findings: less STE in Lead III than<br />
that is often, if not usually the case, it still doesn’t represent 100% And remember: most people have a Type 3 (“wraparound”) LAD.<br />
in Leads II and aVF and essentially no STE in Lead aVL while ST elevation is present in Lead<br />
assurance of a proximal location. We normally confirm an occlusion Exactly the kind of comforting thought that keeps you on your toes,<br />
proximal I. Could to S1 there by presence be a connection? of ST depression in the Yes! inferior And leads, that isn’t connection it? The next time is you the see fact a patient that with Leads ACS type III chest and pain aVL –<br />
but we don’t have that opportunity here because of the acute ischemia but the ECG appears normal – remember this!<br />
are reciprocal to each other. Both have ST elevation but their systolic currents of injury are<br />
traveling in opposite directions (Lead III: down and to the right, Lead aVL: up and to the left)<br />
and thus cancel each other. For further Apparently, recruitment vacancies the ST visit: elevation www.ambulanceukonline.com<br />
Lead III was greater than in Lead<br />
AMBULANCE <strong>UK</strong> – APRIL<br />
9