26 - World Journal of Gastroenterology
26 - World Journal of Gastroenterology
26 - World Journal of Gastroenterology
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Li GL et al . Biliary complications in rat liver transplantation<br />
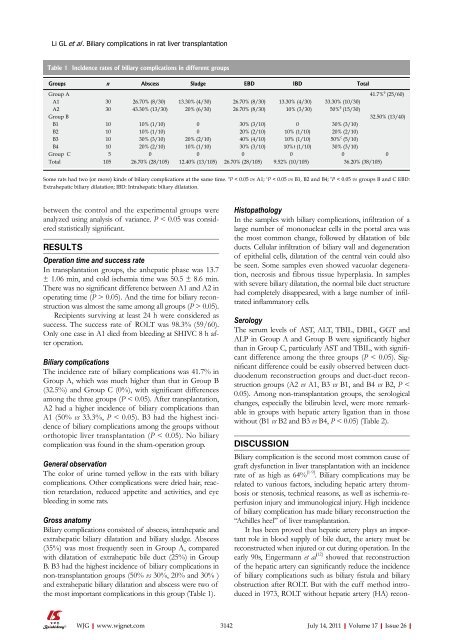
Table 1 Incidence rates <strong>of</strong> biliary complications in different groups<br />
Groups n Abscess Sludge EBD IBD Total<br />
Group A 41.7% e (25/60)<br />
A1 30 <strong>26</strong>.70% (8/30) 13.30% (4/30) <strong>26</strong>.70% (8/30) 13.30% (4/30) 33.30% (10/30)<br />
A2 30 43.30% (13/30) 20% (6/30) <strong>26</strong>.70% (8/30) 10% (3/30) 50% a (15/30)<br />
Group B 32.50% (13/40)<br />
B1 10 10% (1/10) 0 30% (3/10) 0 30% (3/10)<br />
B2 10 10% (1/10) 0 20% (2/10) 10% (1/10) 20% (2/10)<br />
B3 10 30% (3/10) 20% (2/10) 40% (4/10) 10% (1/10) 50% c (5/10)<br />
B4 10 20% (2/10) 10% (1/10) 30% (3/10) 10%t (1/10) 30% (3/10)<br />
Group C 5 0 0 0 0 0 0<br />
Total 105 <strong>26</strong>.70% (28/105) 12.40% (13/105) <strong>26</strong>.70% (28/105) 9.52% (10/105) 36.20% (38/105)<br />
Some rats had two (or more) kinds <strong>of</strong> biliary complications at the same time. a P < 0.05 vs A1; c P < 0.05 vs B1, B2 and B4; e P < 0.05 vs groups B and C EBD:<br />
Extrahepatic biliary dilatation; IBD: Intrahepatic biliary dilatation.<br />
between the control and the experimental groups were<br />
analyzed using analysis <strong>of</strong> variance. P < 0.05 was considered<br />
statistically significant.<br />
RESULTS<br />
Operation time and success rate<br />
In transplantation groups, the anhepatic phase was 13.7<br />
± 1.06 min, and cold ischemia time was 50.5 ± 8.6 min.<br />
There was no significant difference between A1 and A2 in<br />
operating time (P > 0.05). And the time for biliary reconstruction<br />
was almost the same among all groups (P > 0.05).<br />
Recipients surviving at least 24 h were considered as<br />
success. The success rate <strong>of</strong> ROLT was 98.3% (59/60).<br />
Only one case in A1 died from bleeding at SHIVC 8 h after<br />
operation.<br />
Biliary complications<br />
The incidence rate <strong>of</strong> biliary complications was 41.7% in<br />
Group A, which was much higher than that in Group B<br />
(32.5%) and Group C (0%), with significant differences<br />
among the three groups (P < 0.05). After transplantation,<br />
A2 had a higher incidence <strong>of</strong> biliary complications than<br />
A1 (50% vs 33.3%, P < 0.05). B3 had the highest incidence<br />
<strong>of</strong> biliary complications among the groups without<br />
orthotopic liver transplantation (P < 0.05). No biliary<br />
complication was found in the sham-operation group.<br />
General observation<br />
The color <strong>of</strong> urine turned yellow in the rats with biliary<br />
complications. Other complications were dried hair, reaction<br />
retardation, reduced appetite and activities, and eye<br />
bleeding in some rats.<br />
Gross anatomy<br />
Biliary complications consisted <strong>of</strong> abscess, intrahepatic and<br />
extrahepatic biliary dilatation and biliary sludge. Abscess<br />
(35%) was most frequently seen in Group A, compared<br />
with dilatation <strong>of</strong> extrahepatic bile duct (25%) in Group<br />
B. B3 had the highest incidence <strong>of</strong> biliary complications in<br />
non-transplantation groups (50% vs 30%, 20% and 30% )<br />
and extrahepatic biliary dilatation and abscess were two <strong>of</strong><br />
the most important complications in this group (Table 1).<br />
WJG|www.wjgnet.com<br />
Histopathology<br />
In the samples with biliary complications, infiltration <strong>of</strong> a<br />
large number <strong>of</strong> mononuclear cells in the portal area was<br />
the most common change, followed by dilatation <strong>of</strong> bile<br />
ducts. Cellular infiltration <strong>of</strong> biliary wall and degeneration<br />
<strong>of</strong> epithelial cells, dilatation <strong>of</strong> the central vein could also<br />
be seen. Some samples even showed vacuolar degeneration,<br />
necrosis and fibrous tissue hyperplasia. In samples<br />
with severe biliary dilatation, the normal bile duct structure<br />
had completely disappeared, with a large number <strong>of</strong> infiltrated<br />
inflammatory cells.<br />
Serology<br />
The serum levels <strong>of</strong> AST, ALT, TBIL, DBIL, GGT and<br />
ALP in Group A and Group B were significantly higher<br />
than in Group C, particularly AST and TBIL, with significant<br />
difference among the three groups (P < 0.05). Significant<br />
difference could be easily observed between ductduodenum<br />
reconstruction groups and duct-duct reconstruction<br />
groups (A2 vs A1, B3 vs B1, and B4 vs B2, P <<br />
0.05). Among non-transplantation groups, the serological<br />
changes, especially the bilirubin level, were more remarkable<br />
in groups with hepatic artery ligation than in those<br />
without (B1 vs B2 and B3 vs B4, P < 0.05) (Table 2).<br />
DISCUSSION<br />
Biliary complication is the second most common cause <strong>of</strong><br />
graft dysfunction in liver transplantation with an incidence<br />
rate <strong>of</strong> as high as 64% [1-9] . Biliary complications may be<br />
related to various factors, including hepatic artery thrombosis<br />
or stenosis, technical reasons, as well as ischemia-reperfusion<br />
injury and immunological injury. High incidence<br />
<strong>of</strong> biliary complication has made biliary reconstruction the<br />
“Achilles heel” <strong>of</strong> liver transplantation.<br />
It has been proved that hepatic artery plays an important<br />
role in blood supply <strong>of</strong> bile duct, the artery must be<br />
reconstructed when injured or cut during operation. In the<br />
early 90s, Engermann et al [12] showed that reconstruction<br />
<strong>of</strong> the hepatic artery can significantly reduce the incidence<br />
<strong>of</strong> biliary complications such as biliary fistula and biliary<br />
obstruction after ROLT. But with the cuff method introduced<br />
in 1973, ROLT without hepatic artery (HA) recon-<br />
3142 July 14, 2011|Volume 17|Issue <strong>26</strong>|