- Page 1 and 2:
Clinical Practice Guidelines FOR TH
- Page 3:
© The Cancer Council Australia/Aus
- Page 6 and 7:
2.11 Conclusions...................
- Page 8 and 9:
11.2 High ligation ................
- Page 10 and 11:
17.4 Cost effectiveness of follow u
- Page 12 and 13:
Table 14.3 Pathological TNM staging
- Page 14 and 15:
Executive Summary • Colorectal Ca
- Page 16 and 17:
STRENGTH OF RECOMMENDATIONS 2,3 The
- Page 18 and 19:
Should red meat intake be altered t
- Page 20 and 21:
Chapter Recommendations 4 COMMUNICA
- Page 22 and 23:
Chapter 8 Recommendations How shoul
- Page 24 and 25:
Chapter Recommendations Should bowe
- Page 26 and 27:
Chapter Recommendations When should
- Page 28 and 29:
Chapter 17 Recommendations What pos
- Page 30:
Section I Early Colorectal Cancer
- Page 33 and 34:
Adenomatous polyps (adenomas) are b
- Page 35 and 36:
17. South Australian Cancer Registr
- Page 37 and 38:
CHAPTER 2 PRIMARY PREVENTION Studie
- Page 39 and 40:
Colorectal adenomas, especially adv
- Page 41 and 42:
vegetable (3.5 serves/1000 kcals) d
- Page 43 and 44:
mustard greens, swedes and turnips)
- Page 45 and 46:
for protection against Colorectal C
- Page 47 and 48:
Does selenium supplementation reduc
- Page 49 and 50:
the optimal duration of use, and ad
- Page 51 and 52:
References 1. Jass JR. Pathogenesis
- Page 53 and 54: 34. Kushi L, Giovannucci E. Dietary
- Page 55 and 56: 67. Fearon ER, Vogelstein B. A gene
- Page 57 and 58: 100. Il'yasova D, Hodgson ME, Marti
- Page 59 and 60: 133. Meyskens FL, Jr., Gerner EW. D
- Page 61 and 62: CHAPTER 3 POPULATION SCREENING FOR
- Page 63 and 64: studies also demonstrate that age i
- Page 65 and 66: • symptoms • family medical his
- Page 67 and 68: Should screening be recommended? Gu
- Page 69 and 70: Box 3.3 Screening Pathway used in t
- Page 71 and 72: References 1. Young GP, Levin B, Ro
- Page 73 and 74: 33. Alexander F, Weller D. Evaluati
- Page 75 and 76: CHAPTER 4 COMMUNICATION WITH THE PA
- Page 77 and 78: 4.6 Coordination of care Treatment
- Page 79 and 80: • assistance with and care of chi
- Page 81 and 82: 17. National Breast Cancer Centre,
- Page 83 and 84: CHAPTER 5 THE PATIENT WITH SYMPTOMS
- Page 85 and 86: considered (see 8.1.5). Double cont
- Page 87 and 88: 58 The prevention, early detection
- Page 89 and 90: diagnoses prove difficult to confir
- Page 91 and 92: What recommendations are there for
- Page 93 and 94: References 1. Woolf CM. A genetic s
- Page 95 and 96: 34. Australian Health Technology Ad
- Page 97 and 98: CHAPTER 7 HIGH-RISK FAMILIAL COLORE
- Page 99 and 100: offered predictive genetic testing.
- Page 101 and 102: endoscopically uncontrollable numbe
- Page 103: mutation carriers. 52 There is also
- Page 107 and 108: added to transvaginal ultrasound. 8
- Page 109 and 110: category 2, see Chapter 6) but may
- Page 111 and 112: What screening is recommended for e
- Page 113 and 114: References 1. Vasen HF, Griffioen G
- Page 115 and 116: 33. Giardiello FM, Hamilton SR, Kru
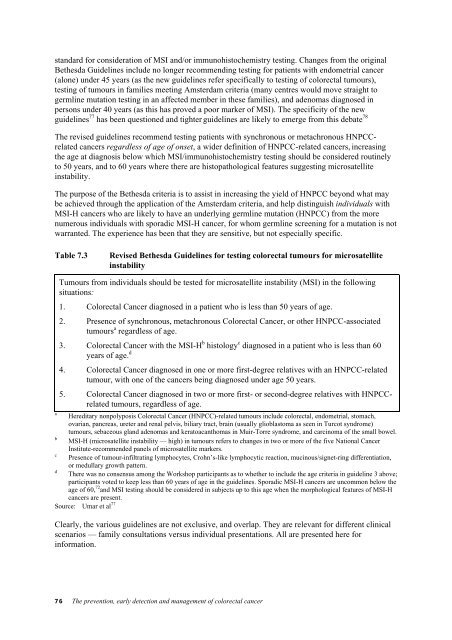
- Page 117 and 118: international criteria for the dete
- Page 119 and 120: 96. Burt RW, Jass JR. Hyperplastic
- Page 121 and 122: 8.1.2 Sigmoidoscopy: rigid versus f
- Page 123 and 124: For radiological imaging of the lar
- Page 125 and 126: 8.2.3 Staging for distant metastase
- Page 127 and 128: The feelings and fears of the patie
- Page 129 and 130: 18. Rex DK, Cutler CS, Lemmel GT et
- Page 131 and 132: 52. Liu SK, Church JM, Lavery IC, F
- Page 133 and 134: 104 The prevention, early detection
- Page 135 and 136: strong family history of Colorectal
- Page 137 and 138: A screening interval of 4-6 years i
- Page 139 and 140: BRAF mutation, particularly when mu
- Page 141 and 142: 18. Jass JR, Young J, Leggett BA. E
- Page 143 and 144: 52. Jass JR, Young J, Leggett BA. H
- Page 145 and 146: 116 The prevention, early detection
- Page 147 and 148: What is the role of the stomal ther
- Page 149 and 150: What happens if a blood transfusion
- Page 151 and 152: References 1. Bass EM, Del Pino A,
- Page 153 and 154: 32. The National Working Party on t
- Page 155 and 156:
CHAPTER 11 ELECTIVE SURGERY FOR COL
- Page 157 and 158:
Total or subtotal colectomy may be
- Page 159 and 160:
11.12 Self-expanding metal stents f
- Page 161 and 162:
18. Gall FP, Tonak J, Altendorf A.
- Page 163 and 164:
134 The prevention, early detection
- Page 165 and 166:
etween 1993 and 1999. The local rec
- Page 167 and 168:
When should local excision of recta
- Page 169 and 170:
What factors influence sphincter pr
- Page 171 and 172:
It has been demonstrated that there
- Page 173 and 174:
References 1. Smith TJ, Hillner BE,
- Page 175 and 176:
36. Vernava AM, III, Moran M, Rothe
- Page 177 and 178:
69. Pimentel JM, Duarte A, Gregorio
- Page 179 and 180:
150 The prevention, early detection
- Page 181 and 182:
A clinical diagnosis of large bowel
- Page 183 and 184:
When should primary anastomosis be
- Page 185 and 186:
17. Deans GT, Krukowski ZH, Irwin S
- Page 187 and 188:
158 The prevention, early detection
- Page 189 and 190:
Table 14.1 Clinicopathological stag
- Page 191 and 192:
The ACPS system embodies the simpli
- Page 193 and 194:
14.4 Translation between staging sy
- Page 195 and 196:
166 The prevention, early detection
- Page 197 and 198:
168 The prevention, early detection
- Page 199 and 200:
16. Shepherd NA, Baxter KJ, Love SB
- Page 201 and 202:
CHAPTER 15 ADJUVANT CHEMOTHERAPY FO
- Page 203 and 204:
isk of death-favouring treatment (H
- Page 205 and 206:
improvement in survival at five yea
- Page 207 and 208:
There has been one trial 55 of intr
- Page 209 and 210:
References 1. National Institute of
- Page 211 and 212:
30. Zaniboni A, Labianca R, Marsoni
- Page 213 and 214:
57. Gastrointestinal Tumour Study G
- Page 215 and 216:
CHAPTER 16 ADJUVANT THERAPY FOR REC
- Page 217 and 218:
preoperative RT 45Gy over 5 weeks s
- Page 219 and 220:
This suggests that a policy of preo
- Page 221 and 222:
Mortality from non-cancer causes wa
- Page 223 and 224:
References 1. Fu KK. Interactions o
- Page 225 and 226:
29. Swedish Rectal Cancer Trial. Im
- Page 227 and 228:
198 The prevention, early detection
- Page 229 and 230:
Rates of intraluminal recurrence an
- Page 231 and 232:
Ultrasonographic screening Ultrason
- Page 233 and 234:
References 1. Nava HR, Pagana TJ. P
- Page 235 and 236:
206 The prevention, early detection
- Page 237 and 238:
• those with a history of psychia
- Page 239 and 240:
References 1. Maisey NR, Norman A,
- Page 241 and 242:
212 The prevention, early detection
- Page 244 and 245:
CHAPTER 19 RECURRENT AND ADVANCED C
- Page 246 and 247:
What are the recommendations for in
- Page 248 and 249:
References 1. National Health and M
- Page 250 and 251:
31. Phillips RK, Hittinger R, Bleso
- Page 252 and 253:
Recurrent and advanced colorectal c
- Page 254 and 255:
(23% compared to 12%, p
- Page 256 and 257:
more patients having disease down-s
- Page 258 and 259:
References 1. Best L, Simmonds P, B
- Page 260 and 261:
30. Fuchs CS, Moore MR, Harker G, V
- Page 262 and 263:
CHAPTER 21 MANAGEMENT OF LIVER AND
- Page 264 and 265:
21.1.3 Imaging controlled destructi
- Page 266 and 267:
Does combination systemic chemother
- Page 268 and 269:
References 1. Woodington FF, Waugh
- Page 270 and 271:
34. Wood BJ, Ramkaransingh JR, Fojo
- Page 272 and 273:
66. Headrick JR, Miller DL, Nagorne
- Page 274 and 275:
Management of liver and other dista
- Page 276 and 277:
years gained can be assessed, which
- Page 278 and 279:
‘If neither of the above cases ap
- Page 280 and 281:
Study Country Study questions Concl
- Page 282 and 283:
Study Country Comparator/ screening
- Page 284 and 285:
Study Country Comparator/ screening
- Page 286 and 287:
Study Country Comparator/ screening
- Page 288 and 289:
Study Country Comparator/ screening
- Page 290 and 291:
Study Country Study questions Concl
- Page 292 and 293:
Three United States studies investi
- Page 294 and 295:
Table 22.6 Results of studies inves
- Page 296 and 297:
Table 22.7 Results of studies inves
- Page 298 and 299:
Table 22.8 Results of studies inves
- Page 300 and 301:
22.9 Treatments 22.9.1 Surgery Seve
- Page 302 and 303:
Study Country Study questions Concl
- Page 304 and 305:
Table 22.10 Results of studies inve
- Page 306 and 307:
Study Country Study questions Concl
- Page 308 and 309:
Study Country Study questions Concl
- Page 310 and 311:
Table 22.11 Summary of findings fro
- Page 312 and 313:
References 1. Australian Institute
- Page 314 and 315:
32. Nakama, H., B. Zhang, and A.S.
- Page 316 and 317:
65. Sieg, A., et al., Screening for
- Page 318 and 319:
97. Durand-Zaleski, I., et al., Eco
- Page 320 and 321:
Cost effectiveness 289
- Page 322 and 323:
References 1. National Health and M
- Page 324:
Appendices
- Page 327 and 328:
“Zorbas et al 2 Multidisciplinary
- Page 329 and 330:
a pathologist-molecular biologist o
- Page 331 and 332:
References 1. Australian Cancer Net
- Page 333 and 334:
Chapter 2 — Primary prevention an
- Page 335 and 336:
Three Cochrane systematic reviews w
- Page 337 and 338:
Dates 1 January 1998 to June 2004 S
- Page 339 and 340:
Dates Update of 1999 document from
- Page 341 and 342:
Search terms MeSH terms were ‘col
- Page 343 and 344:
Chapter 20 — The role of systemic
- Page 345 and 346:
Search terms Colorectal Cancer, soc
- Page 347 and 348:
However, in some cases it was also
- Page 349 and 350:
Professor James St John Gastro ente
- Page 351 and 352:
Working party on emergency surgery
- Page 353 and 354:
Dr Russel Stitz Surgeon, Royal Bris
- Page 355 and 356:
14. Dr Michael Izard Radiation Onco
- Page 357 and 358:
Mrs Avis Mcphee Consumer (June 9 an
- Page 359 and 360:
DVT deep venous thrombosis ECOG Eur
- Page 361 and 362:
TNM tumour, node, metastasis stagin
- Page 363 and 364:
Chemotherapy The use of drugs (whic
- Page 365 and 366:
Malignant Cancerous Malignant cells
- Page 367 and 368:
with a specific disease might survi