Measurements of Pulmonary Function Instrument Accuracy - ndd.ch
Measurements of Pulmonary Function Instrument Accuracy - ndd.ch
Measurements of Pulmonary Function Instrument Accuracy - ndd.ch
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
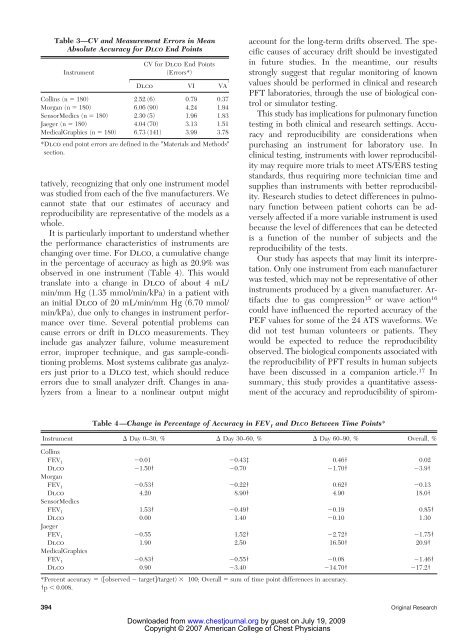
Table 3—CV and Measurement Errors in Mean<br />
Absolute <strong>Accuracy</strong> for DLCO End Points<br />
<strong>Instrument</strong><br />
CV for Dlco End Points<br />
(Errors*)<br />
Dlco VI VA<br />
Collins (n � 180) 2.52 (6) 0.79 0.37<br />
Morgan (n � 180) 6.06 (90) 4.24 1.94<br />
SensorMedics (n � 180) 2.30 (5) 1.96 1.83<br />
Jaeger (n � 180) 4.04 (70) 3.13 1.51<br />
MedicalGraphics (n � 180) 6.73 (141) 3.99 3.78<br />
*Dlco end point errors are defined in the �Materials and Methods�<br />
section.<br />
tatively, recognizing that only one instrument model<br />
was studied from ea<strong>ch</strong> <strong>of</strong> the five manufacturers. We<br />
cannot state that our estimates <strong>of</strong> accuracy and<br />
reproducibility are representative <strong>of</strong> the models as a<br />
whole.<br />
It is particularly important to understand whether<br />
the performance <strong>ch</strong>aracteristics <strong>of</strong> instruments are<br />
<strong>ch</strong>anging over time. For Dlco, a cumulative <strong>ch</strong>ange<br />
in the percentage <strong>of</strong> accuracy as high as 20.9% was<br />
observed in one instrument (Table 4). This would<br />
translate into a <strong>ch</strong>ange in Dlco <strong>of</strong> about 4 mL/<br />
min/mm Hg (1.35 mmol/min/kPa) in a patient with<br />
an initial Dlco <strong>of</strong> 20 mL/min/mm Hg (6.70 mmol/<br />
min/kPa), due only to <strong>ch</strong>anges in instrument performance<br />
over time. Several potential problems can<br />
cause errors or drift in Dlco measurements. They<br />
include gas analyzer failure, volume measurement<br />
error, improper te<strong>ch</strong>nique, and gas sample-conditioning<br />
problems. Most systems calibrate gas analyzers<br />
just prior to a Dlco test, whi<strong>ch</strong> should reduce<br />
errors due to small analyzer drift. Changes in analyzers<br />
from a linear to a nonlinear output might<br />
account for the long-term drifts observed. The specific<br />
causes <strong>of</strong> accuracy drift should be investigated<br />
in future studies. In the meantime, our results<br />
strongly suggest that regular monitoring <strong>of</strong> known<br />
values should be performed in clinical and resear<strong>ch</strong><br />
PFT laboratories, through the use <strong>of</strong> biological control<br />
or simulator testing.<br />
This study has implications for pulmonary function<br />
testing in both clinical and resear<strong>ch</strong> settings. <strong>Accuracy</strong><br />
and reproducibility are considerations when<br />
pur<strong>ch</strong>asing an instrument for laboratory use. In<br />
clinical testing, instruments with lower reproducibility<br />
may require more trials to meet ATS/ERS testing<br />
standards, thus requiring more te<strong>ch</strong>nician time and<br />
supplies than instruments with better reproducibility.<br />
Resear<strong>ch</strong> studies to detect differences in pulmonary<br />
function between patient cohorts can be adversely<br />
affected if a more variable instrument is used<br />
because the level <strong>of</strong> differences that can be detected<br />
is a function <strong>of</strong> the number <strong>of</strong> subjects and the<br />
reproducibility <strong>of</strong> the tests.<br />
Our study has aspects that may limit its interpretation.<br />
Only one instrument from ea<strong>ch</strong> manufacturer<br />
was tested, whi<strong>ch</strong> may not be representative <strong>of</strong> other<br />
instruments produced by a given manufacturer. Artifacts<br />
due to gas compression 15 or wave action 16<br />
could have influenced the reported accuracy <strong>of</strong> the<br />
PEF values for some <strong>of</strong> the 24 ATS waveforms. We<br />
did not test human volunteers or patients. They<br />
would be expected to reduce the reproducibility<br />
observed. The biological components associated with<br />
the reproducibility <strong>of</strong> PFT results in human subjects<br />
have been discussed in a companion article. 17 In<br />
summary, this study provides a quantitative assessment<br />
<strong>of</strong> the accuracy and reproducibility <strong>of</strong> spirom-<br />
Table 4—Change in Percentage <strong>of</strong> <strong>Accuracy</strong> in FEV 1 and DLCO Between Time Points*<br />
<strong>Instrument</strong> � Day 0–30, % � Day 30–60, % � Day 60–90, % Overall, %<br />
Collins<br />
FEV 1 �0.01 �0.43‡ 0.46† 0.02<br />
Dlco �1.50† �0.70 �1.70† �3.9†<br />
Morgan<br />
FEV 1 �0.53† �0.22† 0.62† �0.13<br />
Dlco 4.20 8.90† 4.90 18.0†<br />
SensorMedics<br />
FEV 1 1.53† �0.49† �0.19 0.85†<br />
Dlco 0.00 1.40 �0.10 1.30<br />
Jaeger<br />
FEV 1 �0.55 1.52† �2.72† �1.75†<br />
Dlco 1.90 2.50 16.50† 20.9†<br />
MedicalGraphics<br />
FEV 1 �0.83† �0.55† �0.08 �1.46†<br />
Dlco 0.90 �3.40 �14.70† �17.2†<br />
*Percent accuracy � (�observed � target�/target) � 100; Overall � sum <strong>of</strong> time point differences in accuracy.<br />
†p � 0.008.<br />
394 Original Resear<strong>ch</strong><br />
Downloaded from<br />
www.<strong>ch</strong>estjournal.org by guest on July 19, 2009<br />
Copyright © 2007 American College <strong>of</strong> Chest Physicians