Ambulance UK February 2023
Ambulance UK February 2023
Ambulance UK February 2023
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Volume 38 No. 1<br />
<strong>February</strong> <strong>2023</strong><br />
DEDICATED TO THE AMBULANCE SERVICE AND ITS SUPPLIERS<br />
FURTHER<br />
DETAILS ON<br />
PAGES<br />
3 & 17<br />
www.dsmedical.co.uk<br />
ds_medical
O)stJohn<br />
Join the heartbeat<br />
of Western Australia.<br />
Our paramedics are courageous, caring, confident and patient, putting themselves on<br />
the front-line of pre-hospital medical care every day. At St John WA paramedics work<br />
collaboratively across the organisation to provide quality, patient centred care to the<br />
Western Australian community.<br />
The part you'll play<br />
Our paramedics are trained to Advanced Life Support<br />
(ALS) level, which allows them to provide exceptional<br />
emergency care to patients. They are able to insert an<br />
intravenous and intraosseous cannula (drips), administer a<br />
variety of medications, perform advanced airway<br />
management, give intravenous drug therapy for cardiac<br />
arrest patients, and intravenous fluids.<br />
Above all, our paramedics are responsive to the needs of<br />
the patient, administering time-critical interventions and<br />
transportation to specialist definitive care.<br />
St John WA Paramedic eligibility<br />
We currently have an exciting opportunity for Qualified<br />
Paramedics that do not have current Australian working<br />
rights, to be sponsored by St John WA!<br />
• Recent experience employed and working within<br />
a jurisdictional ambulance service in Australia or<br />
internationally (St John New Zealand or London<br />
<strong>Ambulance</strong> Service for example) as a paramedic<br />
for at least two years.<br />
• Hold a full driver's license with no restrictions.<br />
Successful candidates are required to obtain a light<br />
rigid driver's license within the first six months of<br />
employment. Costs associated with obtaining the<br />
required driver's license are the responsibility of the<br />
candidate.<br />
• Candidates that do not hold current Australian working<br />
rights, must meet the visa eligibility requirements, as<br />
outlined by the Department of Home Affairs.<br />
• Be fully vaccinated against COVID-19 and Influenza.<br />
For candidates to successfully be employed as an<br />
ambulance paramedic, they must meet the following<br />
minimum requirements;<br />
• Professional registration as a paramedic with the<br />
Paramedicine Board of Australia.<br />
• Degree in Paramedicine from a recognised AHPRA<br />
approved programs of study course provider or<br />
recognised international education provider.<br />
Ready for a new adventure?<br />
To find out more information and to submit<br />
your application:<br />
search stjohnwa.com.au/directentry<br />
Scan to learn more:
CONTENTS<br />
CONTENTS<br />
<strong>Ambulance</strong> <strong>UK</strong><br />
4 EDITOR’S COMMENT<br />
6 FEATURES<br />
6 How long are we prepared to wait and see if the NHS<br />
improves?<br />
8 Predictive clinical utility of pre-hospital point of care<br />
lactate for transfusion of blood product in patients<br />
with suspected traumatic haemorrhage: derivation<br />
of a decision-support tool<br />
16 NEWSLINE<br />
27 IN PERSON<br />
31 COMPANY NEWS<br />
FURTHER<br />
DETAILS ON<br />
PAGES<br />
3 & 17<br />
This issue edited by:<br />
Sam English<br />
c/o Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
ADVERTISING:<br />
Terry Gardner, Samantha Marsh<br />
CIRCULATION:<br />
Media Publishing Company<br />
Greenoaks, Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
Tel: 01886 853715<br />
E: info@mediapublishingcompany.com<br />
www.ambulanceukonline.com<br />
PUBLISHED BI-MONTHLY:<br />
<strong>February</strong>, April, June, August,<br />
October, December<br />
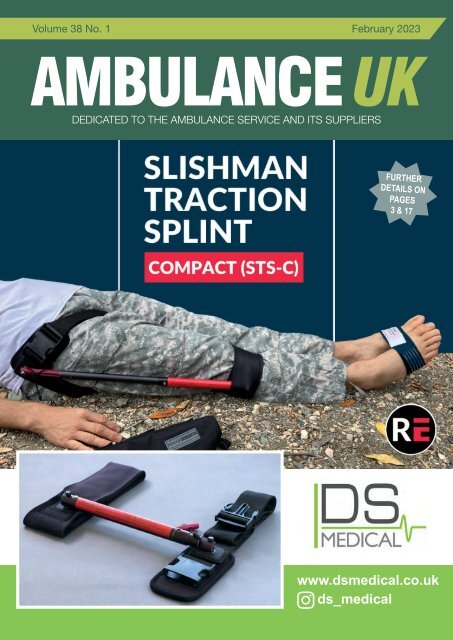
COVER STORY<br />
The Slishman STS-C Compact Traction Splint<br />
New to the <strong>UK</strong> market, exclusively available at DS Medical www.dsmedical.co.uk<br />
The Slishman STS-C Compact Traction Splint is an innovative and effective ds_medical solution<br />
for immobilising and stabilising leg fractures. With its compact design, lightweight<br />
construction, and easy-to-use features, this splint is an essential tool for emergency<br />
responders or medical professionals who needs to immobilise a leg injury.<br />
The traction device is designed with safety in mind. The splint is made from materials<br />
that are strong and durable, and it is designed to withstand the stress and strain of<br />
emergency transportation. The splint also includes safety features that help to prevent<br />
accidental release of the traction mechanism.<br />
How it works, is the distal hitch on the STS-C is applied just proximal to the calf or<br />
patella. Coarse positioning is accomplished using a spring button to extend and lock the<br />
outer tube. Fine traction is accomplished by pulling on the cord, followed by locking with<br />
a downward pull into the V-notch. As all of the traction is controlled at the hip, it is easy<br />
to make adjustments as conditions change, or en route to the hospital.<br />
Features and Benefits are<br />
• Radiolucent<br />
• One size fits all, from small children to large adults<br />
• Single connected device—no loose parts, which may get lost<br />
• Can be applied in under a minute with minimal training<br />
• Application possible even in cases of lower leg/foot amputation<br />
• Includes the Slishman Pressure Wrap to assist with rotational stability<br />
Whether you’re responding to an emergency, hiking in the backcountry, or simply need<br />
to immobilise an injury at home, the Slishman STS-C splint is an excellent choice.<br />
For further information email us on info@dsmedical.co.uk, or visit our website<br />
www.dsmedical.co.uk.<br />
COPYRIGHT:<br />
Media Publishing Company<br />
Greenoaks<br />
Lockhill<br />
Upper Sapey, Worcester, WR6 6XR<br />
PUBLISHERS STATEMENT:<br />
The views and opinions expressed in<br />
this issue are not necessarily those of<br />
the Publisher, the Editors or Media<br />
Publishing Company.<br />
Next Issue April <strong>2023</strong><br />
Subscription Information – <strong>February</strong> <strong>2023</strong><br />
<strong>Ambulance</strong> <strong>UK</strong> is available through<br />
a personal, company or institutional<br />
subscription in both the <strong>UK</strong> and overseas.<br />
<strong>UK</strong>:<br />
Individuals - £24.00 (inc postage)<br />
Companies - £60.00 (inc postage)<br />
Rest of the World:<br />
£60.00 (inc. surface postage)<br />
£84.00 (airmail)<br />
We are also able to process your<br />
subscriptions via most major credit<br />
cards. Please ask for details.<br />
Cheques should be made<br />
payable to MEDIA PUBLISHING.<br />
Designed in the <strong>UK</strong> by me&you creative<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Do you have anything you would like to add or include? Please contact us and let us know.<br />
3
EDITOR’S COMMENT<br />
EDITOR’S COMMENT<br />
Welcome to this issue of A<strong>UK</strong><br />
We have had, and continue to have, a winter of discontent with waiting times surpassing even the worst<br />
predictions. This morning the Government have promised another 800 ambulances before next winter along<br />
with 5000 extra beds and enhanced community resource. It seems like a logical and well thought out plan<br />
but it fails to address the obvious, its fine to have more physical resource but where are the staff to operate<br />
them? This is a fundamental problem in the NHS currently, recruitment and retention are key concerns and<br />
the situation is not helped by those who fail to listen to the concerns of the frontline staff working in todays<br />
high pressure environment.<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
“We should<br />
know that<br />
something is<br />
wrong when<br />
highly qualified<br />
and caring<br />
staff leave<br />
a vocational<br />
career because<br />
they will afford<br />
more and<br />
experience<br />
less stress<br />
by working<br />
in a non<br />
professional<br />
role.”<br />
When I hear of NHS staff having to utilise food banks or hospitals setting up ‘pantries’ to help with the<br />
cost of living issues faced by staff, I am saddened and angry, this is not a problem of <strong>2023</strong> but one which<br />
has festered below the surface for at least the last 10 years. We have watched the pay gap widen yearly,<br />
we have seen the numbers of staff leaving and shortages increase, we have watched unconcerned as the<br />
demand increases year on year and we have heard from the frontline that the situation is worsening.<br />
We should know that something is wrong when highly qualified and caring staff leave a vocational career<br />
because they will afford more and experience less stress by working in a non professional role. Whilst some<br />
may argue that the NHS pension is much better than most private pension schemes and is therefore a<br />
benefit, the age at which this can be claimed continues to rise and I wonder how many of todays staff will<br />
actually reach the end of their careers working in the NHS to enjoy it.<br />
The issues are current, the pressure immense and the only solution is to attract staff to all areas of the NHS<br />
with pay and conditions that ensure recognition of their contribution to our society and provide a living wage<br />
for them and their families. I don’t think that is too much to ask for a service we all pay for and expect to<br />
meet our needs when we have them.<br />
So we roll forward into <strong>2023</strong> and look forward to life’s positives, Easter eggs have appeared on the<br />
supermarket shelves and holiday advertisements are in full flow. Its been chilly the last few weeks but<br />
temperatures are starting to get back to a more <strong>UK</strong> normal. We can but hope that the unrest in the NHS is<br />
resolved and that over the coming months there is peace in Europe again. Here’s hoping all your resolutions<br />
are achieved and best wishes for the year ahead.<br />
Sam English, Co-Editor <strong>Ambulance</strong> <strong>UK</strong><br />
Publishers Statement<br />
For nearly 40 years, thanks to trade support, we have been able to provide <strong>Ambulance</strong> <strong>UK</strong> FREE OF<br />
CHARGE in the knowledge that those receiving our dedicated bi monthly publication enjoy having<br />
something to read during their free time however, return on investment seems to be the buzz word<br />
amongst <strong>Ambulance</strong> Service Suppliers these days, therefore if you enquire about a product advertised,<br />
please mention <strong>Ambulance</strong> <strong>UK</strong> as it will help us confirm to the trade that we are reaching the right<br />
people and providing advertisers with value for money. In respect of our current edition we would like<br />
to thank the following companies for their support as without their contribution towards our print and<br />
postal costs this issue would not have been published - Bluelight <strong>UK</strong>, CSS Europe, DS Medical,<br />
Eberspächer, Intersurgical, Ortus, Synergy business solutions, Vimpex, St Johns Western<br />
Australia.<br />
Terry Gardner<br />
Publisher<br />
4<br />
For more news visit: www.ambulanceukonline.com
FEATURE<br />
HOW LONG ARE WE PREPARED TO<br />
WAIT AND SEE IF THE NHS IMPROVES?<br />
By Ivor Campbell<br />
Waiting times, waiting times…oh how we’re all waiting for the time<br />
when waiting times improve and we can feel confident that the<br />
NHS is working again.<br />
The reality is, however, that without meaningful change, waiting times<br />
are likely only to become longer – at least in the short term.<br />
Besides, there are other metrics that may be more accurate in<br />
measuring quality of care, such as the time patients wait before being<br />
clinically assessed; how long critically ill patients wait before their<br />
treatment is completed; and the proportion of patients who return to<br />
A&E within seven days of their first attendance. Other measures, such<br />
as the time a patient waits to see a clinician, are also now recorded.<br />
Even if they improved, would that necessarily mean we had a properly<br />
functioning health service, or that patients were receiving a better<br />
standard of care?<br />
What is beyond question is that waiting times have become the standard<br />
against which the performance of the NHS and social care service are<br />
measured. With the publication of every new set of statistics, so the<br />
fulmination of the commentariat becomes louder and more hectoring.<br />
Once patients are inside the system, governments continue to rely on<br />
waiting times as a key measure of clinical performance.<br />
There’s a six-week target for the eight key diagnostic tests and<br />
investigations; a 12-week target wait for new outpatient appointments; a<br />
12-week treatment time guarantee; and a waiting target of 18 weeks for<br />
an outpatient appointment, diagnostic test (if required) and treatment (if<br />
appropriate).<br />
Most public angst is reserved for waiting times for A&E departments<br />
because they are the gateway through which most patients enter the<br />
system. A logjam there, can lead to knock-on delays for the ambulance<br />
service, primary care, community-based care, and social services.<br />
In October 2022, the NHS recorded its highest ever waiting times for<br />
A&E admission, with more than one in three patients having to wait<br />
longer than the four-hour target.<br />
Again, we obsess over whether these times are being met and handwring<br />
over the deluge of statistics highlighting missed targets and,<br />
axiomatically, over further evidence of a broken system.<br />
At the end of September 2022, we learned that 7.1million people in<br />
England were waiting to start routine hospital treatment – up by 100,000<br />
on the previous month and the highest number since records began in<br />
August 2007.<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
In Scotland, the situation was worse, with 61.9% of patients attending<br />
casualty departments in the week up to November 27 admitted or<br />
discharged within four hours.<br />
As a result of those failures, we learned that, in the same month, four<br />
patients waited more than 20 hours in the back of ambulances outside<br />
Royal Shrewsbury Hospital, in England.<br />
The average wait for category two, 999 calls for an ambulance —<br />
including for chest pains and strokes — in England and Wales is now 60<br />
minutes, compared with a target of 18 minutes.<br />
When Matt Hancock was Health Secretary, he became so frustrated at<br />
the amount of attention paid to the four-hour waiting target for A&E that<br />
he called for it to be scrapped because, he said, it was longer deemed<br />
to be ‘clinically appropriate.’<br />
While Hancock might be a better guide to the flavour of marsupial<br />
genitalia than to the functioning of a health service, he may have a point<br />
that the practice has its limitations.<br />
The King’s Fund think tank has pointed out that even measuring the<br />
proportion of patients seen within four hours is problematic. Two<br />
separate departments could process the same proportion of patients<br />
within the timescale but have different average waiting times.<br />
Last November it was reported that two women from the North of<br />
Scotland, waited more than three years for an appointment with a<br />
psychiatrist. When Nessie Simpson was eventually seen by a mental<br />
health practitioner, she had to travel 65 miles away from her home in<br />
Fort William.<br />
Most people would agree that having to wait three years for an<br />
appointment, or to sit for more than 20 hours in an ambulance outside<br />
an emergency department, are failures of the system.<br />
But is it necessarily the case that the speed with which a physician gets<br />
through appointments with patients should be the sole criterion upon<br />
which the success or failure of the system should be decided?<br />
A doctor who spends more time with a patient and notices an underlying<br />
issue that has been overlooked by a colleague, who spends less time with<br />
each patient, is obviously doing his or her job more effectively, even if that<br />
means they are costing more in time and resources.<br />
Waiting time statistics don’t show how often someone turns-up with a<br />
minor complaint that is masking something more serious and which is<br />
subsequently detected by a diligent clinician.<br />
Diagnostics is increasingly focused on the personal side of healthcare.<br />
While newspaper headlines fixate about people sitting in ambulances<br />
6<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
or on trollies outside of A&E departments, that is only a fraction of what<br />
hospitals do.<br />
Acute, emergency care may be seen as the ‘sharp-end’ of the health<br />
service, but fewer people die from falling over when drunk or getting<br />
their head stuck in a saucepan than from heart disease, cancers, and<br />
strokes, which take more time to treat and rely on expensive and timeconsuming,<br />
long-term testing.<br />
Intranasal mucosal<br />
atomisation device<br />
At the heart of the dilemma over how to fix the health service is the question<br />
of where best to distribute scarce resources. We have too many patients<br />
with too few resources and our options are therefore to reduce the number<br />
of patients or to increase resources and the latter is not currently viable.<br />
Fewer patients would enter the system if more of them paid for their<br />
treatment privately or if those with less serious conditions avoided<br />
visiting their GP.<br />
In the republic of Ireland, a GP appointment costs around €60 –<br />
with exemptions for pensioners, children under six and people on<br />
low incomes. Patients are also charged if they visit an emergency<br />
department without a GP’s referral.<br />
The Irish system may be unpopular among some, but at least it stops<br />
people turning up because they need a packet of paracetamol.<br />
Its advocates point-out that it prevents misuse of GPs’ time, allowing<br />
them to focus on those who are genuinely ill and that the service<br />
remains free to those who cannot afford to pay.<br />
Critics say such charges, if introduced in the <strong>UK</strong>, would undermine the<br />
founding principle of NHS, of care being free at the point of delivery to<br />
everyone, regardless of their means.<br />
We need to have a grown-up discussion about what would be<br />
acceptable and it may come down to cost. Would those of us who<br />
could afford to, be prepared to pay £20 to see a doctor? Possibly.<br />
Would they be prepared to pay £200? Probably not.<br />
Around 12% of healthcare treatment is already delivered privately. That used<br />
to be called privatisation by stealth but now it is accepted as being part of<br />
the system. People recognise that having the money and spending it on<br />
their health is worth potentially having an extra 10 years of living, pain free.<br />
There are already anomalies of private healthcare existing within the<br />
system. Only the poorest people now receive free dental and ophthalmic<br />
care and private companies routinely provide services for the NHS.<br />
Medication can be quickly<br />
and painlessly delivered with<br />
the DART intranasal mucosal<br />
atomisation device, helping the<br />
patient remain calm in a high<br />
stress situation.<br />
Scan the QR code to find out more:<br />
The system was devised in the late 1940s and, while it has been<br />
revised, many of us are still treated by a system that would be familiar to<br />
patients in the 1950s.<br />
How it will change in the next few years – if it changes at all – will<br />
depend upon public tolerance of a steadily worsening service. In the<br />
meantime, we will all have to wait and see.<br />
Ivor Campbell is Managing Director of Stirlingshire-based Snedden<br />
Campbell, a search company for the medical technology industry.<br />
Quality, innovation and choice<br />
lnteract with us<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
www.intersurgical.co.uk<br />
7
FEATURE<br />
PREDICTIVE CLINICAL UTILITY OF PRE-HOSPITAL POINT OF<br />
CARE LACTATE FOR TRANSFUSION OF BLOOD PRODUCT IN<br />
PATIENTS WITH SUSPECTED TRAUMATIC HAEMORRHAGE:<br />
DERIVATION OF A DECISION-SUPPORT TOOL<br />
J. E. Griggs 1,2* , R. M. Lyon 1,2 , M. Sherriff 4 , J. W. Barrett 2,5 , G. Wareham 1 and E. ter Avest 1,3 on behalf of Air<br />
<strong>Ambulance</strong> Charity Kent Surrey Sussex<br />
Scand J Trauma Resusc Emerg Med (2022) 30:72 https://doi.org/10.1186/s13049-022-01061-x<br />
Abstract<br />
Introduction<br />
Pre-hospital emergency medical teams can transfuse blood products<br />
to patients with suspected major traumatic haemorrhage. Common<br />
transfusion triggers based on physiological parameters have several<br />
disadvantages and are largely unvalidated in guiding pre-hospital<br />
transfusion. The addition of pre-hospital lactate (P-LACT) may overcome<br />
these challenges. To date, the clinical utility of P-LACT to guide prehospital<br />
blood transfusion is unclear.<br />
Background<br />
Over the past decade pre-hospital critical care teams and helicopter<br />
emergency medical services (HEMS) have developed transfusion<br />
protocols and operational capability to transfuse blood products to<br />
patients with suspected traumatic haemorrhagic shock [1, 2]. Clinical<br />
gestalt in combination with clinical variables such as systolic blood<br />
pressure (SBP) and shock index (SI) are used to quantify the severity of<br />
haemorrhagic shock and guide transfusion with blood products, both in<br />
the pre-hospital- and the in-hospital phase of care [3].<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Methods<br />
A retrospective analysis of patients with suspected major traumatic<br />
haemorrhage attended by Air <strong>Ambulance</strong> Charity Kent Surrey Sussex<br />
(KSS) between 8 July 2017 and 31 December 2019. The primary<br />
endpoint was the accuracy of P-LACT to predict the requirement for any<br />
in-hospital (continued) transfusion of blood product.<br />
Results<br />
During the study period, 306 patients with suspected major traumatic<br />
haemorrhage were attended by KSS. P-LACT was obtained in 194<br />
patients. In the cohort 103 (34%) patients were declared Code Red. A<br />
pre-hospital transfusion was commenced in 124 patients (41%) and inhospital<br />
transfusion was continued in 100 (81%) of these patients, in 24<br />
(19%) patients it was ceased. Predictive probabilities of various lactate<br />
cut-off points for requirement of in-hospital transfusion are documented.<br />
The highest overall proportion correctly classified patients were found for<br />
a P-LACT cut-point of 5.4 mmol/L (76.50% correctly classified). Based<br />
on the calculated predictive probabilities, optimal cut-off points were<br />
derived for both the exclusion- and inclusion of the need for in-hospital<br />
transfusion. A P-LACT < 2.5 mmol/L had a sensitivity of 80.28% and a<br />
negative likelihood ratio [LR−] of 0.37 for the prediction of in-hospital<br />
transfusion requirement, whereas a P-LACT of 6.0 mmol/L had a<br />
specificity of 99.22%, [LR−] = 0.78.<br />
Conclusion<br />
Pre-hospital lactate measurements can be used to predict the need<br />
for (continued) in-hospital blood products in addition to current<br />
physiological parameters. A simple decision support tool derived in this<br />
study can help the clinician interpret pre-hospital lactate results and<br />
guide pre-hospital interventions in the major trauma patient.<br />
* Correspondence: Jogriggs@aakss.org.uk<br />
1<br />
Air <strong>Ambulance</strong> Charity Kent Surrey Sussex, Hanger 10 Redhill Aerodrome, Redhill RH1 5YP, <strong>UK</strong><br />
Full list of author information is available at the end of the article<br />
© The Author(s) 2022.<br />
Clinical variables, however, have several disadvantages in guiding<br />
pre-hospital transfusion. First, evidence-based cut-off values to guide<br />
transfusion are lacking. As a result, pre-hospital transfusion trigger<br />
thresholds vary [3, 4]. Second, physiological parameters cannot reliably<br />
determine the degree of occult and temporal haemorrhage as they are<br />
highly influenced by autoregulatory responses [3, 5, 6]. Third, changes<br />
in blood pressure are a late sign of a haemorrhagic shock and by using<br />
SBP or SI as transfusion triggers the transfusion decision point (TDP)<br />
may be delayed beyond the critical window for effective resuscitation<br />
[7]. Finally, other causes mimic the clinical signs of haemorrhagic shock<br />
and may confound decision-making, such as traumatic vasoactive head<br />
injuries [8]. As a result, the sensitivity and specificity of clinical variables<br />
to predict in-hospital transfusion are limited [4, 9–11].<br />
Pre-hospital point of care lactate measurement (P-LACT) has the<br />
potential to overcome some of these shortcomings. Lactate formation<br />
in major trauma patients is the result of tissue hypoperfusion, resulting in<br />
anaerobic glycolysis. Haemorrhage and inadequate ventilation following<br />
a traumatic injury can lead to hypovolemia, hypoxaemia and end-organ<br />
hypoperfusion, resulting in anaerobic glycolysis and lactate formation.<br />
Furthermore, lactate is formed as a result of adrenergic responses to<br />
pain and stress [12–15]. Unlike SBP and SI, P-LACT changes are not<br />
balanced by counter-regulatory mechanisms and can be measured early<br />
at the point of injury [12]. Previous studies have shown that P-LACT<br />
can be used to predict both the need for resuscitative in-hospital care<br />
in trauma patients and the outcome of traumatically injured patients<br />
[1, 9, 10]. To date, the clinical utility of P-LACT to guide blood product<br />
transfusion remains unclear [3, 16].<br />
In this study, we aim to investigate how P-LACT can be used to predict<br />
8<br />
For more news visit: www.ambulanceukonline.com
FEATURE<br />
the need for (continued) in-hospital blood product transfusion in patients<br />
attended by HEMS with suspected major traumatic haemorrhage.<br />
Methods<br />
Study design<br />
We performed a retrospective analysis of all trauma patients with<br />
suspected major haemorrhage attended by Air <strong>Ambulance</strong> Kent Surrey<br />
Sussex (KSS) in whom a P-LACT was measured between 8 July 2017<br />
(when lactate measurements became available to the service) and 31<br />
December 2019. We aimed to investigate the relationship between<br />
clinical variables and measured P-LACT values with the need for<br />
(continued) in-hospital blood product transfusion.<br />
Study setting<br />
KSS HEMS cover three counties in the southeast of England, a region<br />
of 7200km 2 with a resident population of 4.5 million, and a transient<br />
population of 8 million. Two doctor-paramedic teams respond 24/7 in<br />
either a helicopter or rapid response vehicle from one operational base,<br />
attending approximately 2000 patients per year. Tertiary trauma care in the<br />
region is offered at four major trauma centres (MTCs). At the time of the<br />
study KSS carried four units of O Rhesus negative packed red blood cells<br />
(PRBC) in a CRĒDO CUBE (Series 4, 2l Insulation 15, VIP Golden Hour)<br />
and four units of Lyoplas, freeze dried plasma (FDP) on all missions.<br />
Blood products are administered as per KSS Standard Operating<br />
Procedure (SOP) to patients showing signs of severe haemorrhagic<br />
shock. The decision to transfuse blood products is based on clinical<br />
gestalt, considering clinical history, mechanism, physiology and<br />
response to resuscitative efforts. P-LACT is measured as per SOP as an<br />
adjunct to clinical findings to help exclude traumatic major haemorrhage<br />
(cut off < 2.5 mmol/L). Where there is a suspicion of major haemorrhage<br />
and sign of haemodynamic compromise ‘Code Red’ is declared. Code<br />
Red activation enables a titrated transfusion of up to four units of O<br />
Rhesus negative PRBC and 4 units of FDP; administration of 10 mL<br />
Calcium Chloride 10% (after the 2nd unit of PRBC) and Tranexamic Acid<br />
(1 g) through a fluid warmer (Belmont Buddy Lite or Warrior Lite).<br />
In addition, a ‘pre-alert’ to the receiving hospital triggers a predefined<br />
in-hospital major haemorrhage protocol to ensure blood products are<br />
immediately available [17, 18]. Full traceability of blood transfusions<br />
and compliance with Blood Safety and Quality Regulations (2007) and<br />
Medicines and Healthcare Regulatory Agency (MHRA, 2016) is ensured.<br />
Point of care lactate sampling<br />
Lactate was measured from venous blood prior to sodium chloride<br />
(NaCl 0.9%) flush, and drawn into a 2 mL syringe during venepuncture<br />
or after insertion of an intravenous (IV) cannula using the NOVA<br />
StatStrip ® Biomedical Xpress point of care test (POCT) Lactate Meter<br />
system [12]. Samples were taken prior to the initiation of blood product<br />
transfusion. Measurement results were noted, time-stamped and<br />
retrospectively recorded in the KSS electronic patient record system<br />
(HEMSBase 2.0, Medic One Systems Ltd, <strong>UK</strong>).<br />
Outcome measures<br />
The primary endpoint of interest was the accuracy of P-LACT (both<br />
as a continuous variable and at various cut-off points) to predict the<br />
requirement for any (continued) transfusion of blood products inhospital.<br />
Data acquisition<br />
Patient demographics, mechanism of injury and nature of injuries,<br />
presenting physiology, POCT results (including lactate) and treatments<br />
provided by HEMS and other EMS (including blood product) were<br />
retrieved from the dedicated KSS electronic patient clinical record. Inhospital<br />
transfusion data were obtained from electronic health records of<br />
the respective MTC’s and shared with KSS in accordance with existing<br />
data-sharing agreements between KSS and the NHS Trusts.<br />
Ethical considerations<br />
This project was registered with the University of Surrey, and met<br />
National Institute for Healthcare Research (NIHR, <strong>UK</strong>) criteria as a service<br />
evaluation. All the data used for this study were routinely collected as<br />
part of standard pre-hospital and hospital patient data collection. The<br />
project was approved by the KSS Research & Development Committee<br />
and conducted in accordance with Strengthening the Reporting of<br />
Observational Studies in Epidemiology (STROBE) Guidelines [19].<br />
Statistical analysis<br />
Descriptive statistics are given as mean [95% CI] or median [IQR].<br />
Comparisons across groups were made using Fisher’s exact test and<br />
ANOVA Kruskal–Wallis test where appropriate. Sensitivity, specificity,<br />
and positive- and negative likelihood ratios as well as the percentage<br />
correctly classified were calculated for P-LACT values in the range<br />
between 1 and 10 mmol/L. Finally, predicted probabilities [95% CI] of<br />
the occurrence of the defined endpoint were calculated for each of<br />
these values using logistic regression analysis.<br />
Previously published work at KSS in the same patient cohort highlights<br />
an average time from 999 to P-LACT of 66 min [12]. Internal service<br />
evaluation highlights a 999 to hospital time of 1 h 50 min, putting the<br />
HEMS team patient side at between 30 and 45 min.<br />
Study population<br />
Patients were included in the analysis if they had presumed major<br />
haemorrhage as a result of traumatic injuries for which a P-LACT was<br />
measured on scene and for which the patient was transported (by air or<br />
land) to an MTC. Exclusions consisted of patients with traumatic cardiac<br />
arrest (TCA), patients pronounced life extinct (PLE) on scene, patients<br />
with potential haemorrhagic shock from a medical aetiology, patients<br />
transferred to non-MTCs, inter-hospital transfers and patients < 16 years<br />
of age.<br />
Missing values are reported in the results section of the manuscript<br />
according to the STROBE guideline [11]. A p value < 0.05 was regarded<br />
as statistically significant. Statistical analyses were conducted using<br />
Stata 17.0 and SPSS 26.0.<br />
Results<br />
Study population<br />
During the study period KSS attended 306 trauma patients in whom<br />
major traumatic haemorrhage was suspected. 103 of these patients<br />
had signs of haemodynamic compromise for which a Code Red<br />
was declared. Overall, a P-LACT was obtained in a total of 194<br />
patients (47 in whom a Code Red was declared and 147 in whom not).<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Do you have anything you would like to add or include in Features? Please contact us and let us know.<br />
9
FEATURE<br />
Fig. 1 Derived study population and patient inclusion<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
In-hospital transfusion was continued- or started in 126 patients (Fig.<br />
1). 14 of the patients receiving in-hospital transfusion fulfilled criteria<br />
for major transfusion, and 31 fulfilled criteria for massive transfusion.<br />
P-LACT was not measured in 56 (54%) of the patients with a suspicion<br />
of major traumatic haemorrhage.<br />
Baseline characteristics<br />
Patient demographics, mechanism of injury (MOI), presenting<br />
physiology, HEMS interventions and HEMS transfusion of patients<br />
attended with suspected major traumatic haemorrhage are presented<br />
in Table 1, stratified by the primary endpoint the need for (continued)<br />
in-hospital transfusion. Endpoint data were available for 268 (88%)<br />
of patients. Patients who needed in-hospital transfusion were more<br />
frequently injured in an RTC (72%); had a higher heart rate (106 bpm);<br />
a lower systolic blood pressure (88 mmHg); a higher shock index (1.3);<br />
a lower GCS (10/15); a higher overall injury severity score (ISS) and<br />
average P-LACT of 4.60 mmol/L. HEMS critical interventions were more<br />
prevalent in patients who required in-hospital transfusion.<br />
Diagnostic performance of lactate for the prediction of in-hospital<br />
transfusion<br />
The negative likelihood ratio [LR−] gives the change in odds of having<br />
a diagnosis in patients with a negative test. For example, a −LR of 0.1<br />
would indicate a tenfold decrease in the odds of having a condition in<br />
a patient with a negative test result. A -LR of 0.05 would be a 20-fold<br />
decrease in the odds of the condition studied.<br />
Predictive probabilities (95% CI) of cut-off points for every increase in<br />
lactate 1 mmol/L for the need for in-hospital transfusion is reported (Fig.<br />
2). The highest overall percentage of correctly classified patients for a<br />
single cut-off point was found at the inflection point of the curve, cutpoint<br />
5.4 mmol/L. (Table 2). For this cut-point 76.50% of the patients<br />
were correctly classified. However, sensitivity of a lactate < 5.4 mmol/L<br />
(38.03%) was too low to use as a single cut-off value to exclude the<br />
need for in-hospital transfusion.<br />
Sensitivity, specificity, and positive- and negative likelihood ratio’s as<br />
well as the percentage correctly classified subjects for various P-LACT<br />
values in the range between 1 and > 9.6 mmol/L are represented in<br />
Table 2.<br />
The cut-point currently used as an adjunct to exclude major<br />
haemorrhage (P-LACT < 2.5 mmol/L) had a sensitivity of 80.28%,<br />
[LR−] = 0.37 for the prediction of the need for in-hospital transfusion.<br />
However, a P-LACT > 2.5 mmol/L only had a specificity of 52.00%<br />
and was therefore not useful to identify those patients in whom a code<br />
red should be declared and communicated to the receiving hospital.<br />
Specificity increased gradually with increasing P-LACT values until a<br />
value of 6.0 mmol/L and plateaued thereafter. A P-LACT of 6.0 mmol/L<br />
had a specificity of 99.22%, [LR−] = 0.78.<br />
Based on the above findings a decision support tool was devised for the<br />
use of lactate in the pre-hospital phase of care (Fig. 3).<br />
Discussion<br />
In the present study we demonstrate that pre-hospital lactate<br />
measurements can be used to predict the need for (continued) inhospital<br />
blood product. A simple decision support tool can help the<br />
clinician to interpret pre-hospital lactate results and to guide transfusion.<br />
10<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
FEATURE<br />
Table 1 Population characteristics stratified by need for (continued) transfusion of blood products in hospital<br />
All patients (n = 306)<br />
In‐hospital transfusion<br />
(n = 126)<br />
No In‐hospital transfusion<br />
(n = 142)<br />
p value<br />
Demographics<br />
Age, years (SD) 47.4 [21.6] 47.5 [21.7] 47.4 [21.6] .73<br />
Male, (n [%]) 197 [73.5] 90 [71.4] 107 [75.4] .57<br />
Female, (n [%]) 71 [23.2] 36 [28.6] 35 [24.6]<br />
Missing, (n [%]) 38 [3.3]<br />
Mechanism descriptors (n, %)<br />
RTC 162 [52.9] 91 [72.2] 71 [55.6] < 0.001<br />
Accidental Injury 20 [6.5] 16 [12.7] 4 [2.8]<br />
Intentional Self Harm 25 [8.1] 9 [7.14] 16 [11.3]<br />
Assault 19 [6.2] 8 [6.3] 18 [12.6]<br />
Fall 30 [9.8] 4 [3.2] 26 [18.4]<br />
Cyclist 5 [1.6] 0 [0] 5 [3.5]<br />
Motorcyclist 18 [5.9] 4 [3.2] 14 [9.9]<br />
Other 8 [2.6] 2 [1.6] 6 [4.2]<br />
Presenting physiology<br />
TCA (n [%]) 15 [8.5] 14 [10.4] 1 [9.2] < 0.001<br />
HR (mean [SD])<br />
missing<br />
SBP (mean [SD])<br />
missing<br />
Shock Index (mean [SD])<br />
missing<br />
GCS (median [IQR])<br />
missing<br />
P-LACT<br />
Presenting P-LACT (mmol/L) (mean [SD])<br />
missing<br />
Pre-hospital interventions<br />
91 [25.1]<br />
17<br />
106 [34.4]<br />
20<br />
1.0 [0.5]<br />
27<br />
13 [6–15]<br />
3<br />
2.9 [2.4]<br />
84<br />
Demographics, proxy injury and physiological parameters: HR heart rate, SBP systolic blood pressure, SI shock index, GCS Glasgow Coma Scale, PHEA pre-hospital<br />
emergency anaesthesia, PRBC packed red blood cells, FDP freeze-dried plasma, P‐LACT pre-hospital lactate, ICU Intensive Care Unit<br />
When patients are attended by pre-hospital care teams after major<br />
trauma, it can be a challenge to determine which patients suffer from<br />
major haemorrhage due to their injuries. Often this is obvious from the<br />
106 [32.6] 98 [29.6] < 0.001<br />
88 [31.8] 120 [29.5] < 0.001<br />
1.3 [0.6] 0.8 [0.3] < 0.001<br />
10 [3–14]<br />
0<br />
14 [10–15]<br />
3<br />
< 0.001<br />
4.60 [2.4] 3.5 [3.5] < 0.001<br />
PHEA (n [%]) 101 [36.9] 64 [50.4] 37 [25.5] < 0.001<br />
Pre-hospital Code Red 103 [39.9] 89 [70.4] 14 [9.2] < 0.001<br />
Pre-hospital Transfusion 124 [49.0] 100 [79.2] 24 [16.3] < 0.001<br />
PRBC (units, %) mode [range] 0 [4] 0 [3] < 0.001<br />
FDP (units, %) mode [range] 1 [4] 0 [4] < 0.001<br />
PRBC units (n, %)<br />
0 units 169 [60.8] 40 [31.2] 129 [91.5] .68<br />
1 units 44 [17.0] 37 [29.6] 7 [4.3]<br />
2 units 28 [10.1] 24 [19.2] 4 [2.8]<br />
3 units 18 [7.8] 16 [12.8] 2 [1.4]<br />
4 units 9 [4.2] 9 [7.2] 0 [0]<br />
Clinical outcome<br />
Hospital lactate (mmol/L)<br />
Missing (n [%])<br />
ISS (mean [SD])<br />
Missing (n [%])<br />
ICU Length of stay (mean [SD])<br />
Missing (n [%])<br />
Hospital Length of stay (mean [SD])<br />
Missing (n [%])<br />
Survival to discharge<br />
Missing (n [%])<br />
3.4 [2.6]<br />
204 [66.6]<br />
14 [17–41]<br />
82 [27.8]<br />
3 [.00–11.7]<br />
82 [27.8]<br />
16 [5.7 – 31.2]<br />
84 [27.45]<br />
144 (47.1)<br />
97[31.7]<br />
4.4 [3.0] 2.00 [1.0] < 0.001<br />
33 [23.5–43.0] 22 [13–33] < 0.001<br />
4.5 [1.00–16.75] 2 [.0–8.00] < 0.001<br />
18 [3–42] 14 [7–26.0] .50<br />
57 [44.8] 87 [61.0] < 0.001<br />
physical examination (i.e. when external bleeding is present, or when<br />
the patient presents in extremis/ peri-arrest). Sometimes, however, this<br />
is less clear, as patients may be seen early after their injury, with still<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Do you have anything you would like to add or include in Features? Please contact us and let us know.<br />
11
FEATURE<br />
Fig. 2 Predictive probabilities (95% CI) of various cut-off points for the need for in-hospital (continued) transfusion. Predicted probabilities and<br />
Fig. associated 2 Predictive 95% probabilities CIs of In-hospital (95% transfusion CI) of various as a cut-off function points of pre-hospital for the need lactate for in-hospital concentration (continued) transfusion. Predicted probabilities and<br />
associated 95% CIs of In-hospital transfusion as a function of pre-hospital lactate concentration<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Table 2 Diagnostic performance of P-LACT for prediction of<br />
Table in-hospital 2 Diagnostic blood component performance therapy of P-LACT in patients for prediction with traumatic of<br />
in-hospital haemorrhage blood component therapy in patients with traumatic<br />
haemorrhage<br />
Cut‐point Sensitivity Specificity LR+‐ LR− Correctly<br />
Cut‐point (mmol/L) Sensitivity Specificity LR+‐ LR− Correctly classified<br />
(mmol/L)<br />
1 100.00 3.10 1.03 0.00<br />
classified<br />
37.50<br />
1 2 100.00 91.55 3.10 31.78 1.03 1.34 0.00 0.26 37.50 53.00<br />
2 2.5 91.55 80.28 31.78 51.94 1.34 1.67 0.26 0.37 53.00 62.00<br />
2.53 80.28 69.01 51.94 62.78 1.67 1.85 0.37 0.49 62.00 65.00<br />
3 4 69.01 50.34 62.78 82.95 1.85 3.30 0.49 0.52 65.00 73.50<br />
4 5 50.34 39.44 82.95 93.80 3.30 6.36 0.52 0.64 73.50 74.50<br />
5 6 39.44 22.54 93.80 99.22 6.36 29.07 0.64 0.78 74.50 72.00<br />
6 7 22.54 9.86 99.22 99.22 29.07 12.71 0.78 0.90 72.00 67.32<br />
7 8 9.86 7.04 99.22 100.00 12.71 – 0.90 0.91 67.32 67.50<br />
8 9 7.04 1.41 100.00 100.00 – – 0.91 0.98 67.50 65.00<br />
9 > 9 1.41 0.00 100.00 100.00 – – 0.98 1.00 65.00 64.50<br />
> 9 0.00 100.00 – 1.00 64.50<br />
LR+ is the ratio of the probability of a positive test among the truly positive<br />
LR+ subjects is the ratio to the of probability the probability of a positive of a positive test among test among the truly the truly negative positive subjects.<br />
subjects The LR– to is the the probability ratio of the of probability a positive of test a negative among the test truly among negative the truly subjects. positive<br />
The subjects LR– is the to the ratio probability of the probability of a negative of a negative test among test the among truly the negative truly positive subjects<br />
subjects to the probability of a negative test among the truly negative subjects<br />
relatively preserved haemodynamics. In addition, the clinical picture of<br />
major haemorrhage and resultant shock can be mimicked by various<br />
conditions, such as vasoactive head injuries [8]. Clinical variables,<br />
such as blood pressure and heart rate cannot always discriminate<br />
in these instances [4, 10]. Delayed recognition of haemorrhage may<br />
delay appropriate treatment beyond the critical window for effective<br />
resuscitation [7], and/or omitting a pre-alert to the receiving hospital,<br />
leaving clinicians with less time to prepare to receive the patient with<br />
the appropriate resources. However, over-transfusion of patients<br />
with a suspicion of major haemorrhage may occur based on clinical<br />
variables, where a blood transfusion is started in the absence of major<br />
haemorrhage, with resultant deleterious effects [6, 20–22]. This is in-line<br />
with previous reports on the limited sensitivity and specificity of clinical<br />
variables for the prediction of ongoing major haemorrhage [5, 7], even<br />
when these variables are incorporated in sophisticated clinical scoring<br />
systems, such as the Trauma Associated Severe Haemorrhage Score<br />
and Assessment of Blood Consumption Score [3, 23].<br />
In this study, we devise a decision support tool based on P-LACT<br />
measurements to aid clinicians at the transfusion decision point. Lactate<br />
is a well-known independent prognostic marker of in-hospital mortality<br />
in adult trauma patients [24] and previous studies have reported that<br />
P-LACT predicts the need for pre-hospital life-saving intervention beforeand<br />
after admission [15]. The predictive ability of P-LACT for the need<br />
of (continued) transfusion requirement in-hospital however has not been<br />
studied before.<br />
A P-LACT cut-off value of < 2.5 mmol/L had a sensitivity high enough<br />
to exclude the need for in-hospital blood component therapy. This was<br />
also a clinically useful cut-off, as 50% of the patients in our cohort had<br />
a lactate value < 2.5 mmol/L. P-LACT values > 6.0 mmol/L on the other<br />
hand, were highly predictive of the need for (continued) in-hospital<br />
transfusion and requirement of blood components. In combination with<br />
an appropriate trauma mechanism and/or clinical sign congruent with<br />
major haemorrhage, a value > 6.0 mmol/L can almost certainly be used<br />
as a trigger to activate a ‘Code Red’ response to initiate pre-hospital<br />
transfusion, and to pre-alert the receiving hospital. P-LACT values<br />
between 2.5 and 6 mmol/L are not unequivocally diagnostic, which is<br />
in-line with previous studies, wherein it was shown that the aetiology of<br />
elevated P-LACT levels in trauma patients is multifactorial. Other factors<br />
than tissue hypoperfusion, such as increased lactate production due to<br />
catecholamine release as a result of pain, stress, or metabolic needs, or<br />
a decreased lactate clearance due to alcohol intoxication or liver injuries<br />
may play a role. In these instances, serial P-LACT measurements can be<br />
12<br />
For more news visit: www.ambulanceukonline.com
FEATURE<br />
Fig. 3 Division of a decision support tool using P-LACT in patients with suspected major haemorrhage. P-LACT, pre-hospital lactate; *Consider<br />
alternative causes increased lactate production due to catecholamine release as a result of pain, stress or increased metabolic demand, or due to<br />
isolated injuries such as TBI and amputations, or decreased lactate clearance: alcohol intoxication or liver trauma<br />
considered, especially when transport times to hospital are prolonged<br />
and whereby clinicians can aggressively resuscitate a lactate clearance<br />
to < 2.5 mmol/L.<br />
Currently, pre-hospital clinicians often transfuse one or more units of<br />
blood products to patients in whom major haemorrhage is suspected<br />
based on clinical variables. The clinical response is used to establish<br />
the need for further transfusion. However, this is not without risk, as<br />
transfusion related adverse events (although rare) may occur. Potential<br />
deleterious effects may be mitigated, to a certain degree by using<br />
serial P-LACT measurements [6]. The proposed algorithm in this study<br />
may help pre-hospital clinicians to achieve this. It may also attribute<br />
the correct identification of patients who have in-hospital transfusion<br />
requirements and may thereby contribute to the improvement of clinical<br />
pathways for these patients.<br />
Limitations<br />
Our study had several limitations. First, selection bias may have<br />
influenced our results as P-LACT was not measured in 85/306 patients<br />
with suspected major haemorrhage. It is likely that a number of these<br />
patients presented in extremis and the completion of P-LACT would<br />
prolong the time to transfusion, mandating the crews on scene to<br />
prioritize resuscitative interventions above P-LACT measurements. In<br />
these patients however it is unlikely that P-LACT will add much in terms<br />
of decision-making regarding transfusion requirements. This highlights<br />
the challenges of ascertaining the temporality of bleeding in the prehospital<br />
phase of care. For example, identification and differentiation of<br />
the patient whom has active haemorrhage versus the patient who ‘has<br />
bled’. Tailoring of transfusion practice to each of these patients is the<br />
subject of further research. Further, qualitative research may be able<br />
to explore this further in combination with Bayesian theorem. Second,<br />
the P-LACT clinical decision tool developed in this study was derived<br />
from a relatively limited cohort of 221 trauma patients seen by a single<br />
centre. Validation in separate cohorts and other services is warranted<br />
to confirm diagnostic accuracy of the proposed P-LACT cut-off points.<br />
The decision tool should be tested to see if it results in more correctly<br />
classified patients resulting in earlier transfusion in those who need it and<br />
withhold transfusion in those who don’t. Third, in-hospital transfusion<br />
was used as a surrogate for ongoing haemorrhage. However, it is well<br />
known that heuristics and confirmation bias may have influenced the<br />
decision to start or continue in-hospital transfusion. Differences in local<br />
transfusion policies may have influenced this decision too, as patients<br />
were transported to three different MTC’s.<br />
Finally, P-LACT must be adopted within a heuristic approach,<br />
where clinical gestalt developed through pattern recognition, clinical<br />
observation and perception combine to estimate patient transfusion<br />
requirement [25]. We are aware that a single P-LACT is a snapshot<br />
of a dynamic process. The clinical utility of P-LACT is likely found in a<br />
combination of physiological parameters. Future (Bayesian) prediction<br />
modelling to ascertain the value clinicians assign to clinical gestalt at the<br />
transfusion decision point may ascertain the adjunctive value of P-LACT<br />
in combination with physiological parameters [26] in the temporal<br />
management of the bleeding patient.<br />
Conclusion<br />
Pre-hospital lactate measurements can be used to predict the need for<br />
in-hospital blood component therapy. A simple decision support tool<br />
derived in this study can help the clinician interpret pre-hospital lactate<br />
results and guide the need for blood product transfusion.<br />
Abbreviations<br />
KSS: Air <strong>Ambulance</strong> Charity Kent Surrey Sussex; CCP: Critical Care<br />
Paramedic; CI: Confidence Interval; EOC: Emergency Operations<br />
Centre; FDP: Freeze-dried plasma; GCS: Glasgow Coma Score; HEMS:<br />
Helicopter Emergency Medical Service; HR: Heart rate; ICU: Intensive<br />
Care Unit; IQR: Interquartile range; MOI: Mechanism of injury; MTC:<br />
Major Trauma Centre; NIHR: National Institute for Healthcare Research;<br />
PHEA: Pre-hospital emergency anaesthesia; P-LACT : Prehospital<br />
lactate measurement; PRBC: Packed red blood cells; RTC : Road traffic<br />
collision; SBP: Systolic blood pressure; SI: Shock Index; STROBE:<br />
Strengthening the reporting of observational studies in epidemiology<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Do you have anything you would like to add or include in Features? Please contact us and let us know.<br />
13
FEATURE<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
guidelines; TARN: Trauma audit and research network; TDP: Transfusion<br />
decision point; USS: Ultrasound sonography.<br />
Acknowledgements<br />
We acknowledge the South-East Coast <strong>Ambulance</strong> Service NHS<br />
Foundation Trust and associated NHS Hospital Trusts for their ongoing<br />
support.<br />
Author contributions<br />
JG, ETA, RL conceived the study design. MS, JG and ETA performed<br />
statistical analysis. Data analysis and interpretation was performed<br />
by JG and ETA. JG and ETA drafted the manuscript. JB, GW and<br />
RL provided critical revision of the manuscript. All authors read and<br />
approved the final manuscript.<br />
Funding<br />
No funding was received for this study.<br />
Availability of data and materials<br />
The datasets used and/or analysed during the current study are<br />
available from the corresponding author on reasonable request.<br />
Declarations<br />
Ethics approval and consent to participate<br />
Internal service approval was sought from the Research, Audit and<br />
Development Department at KSS. All patient data were collected<br />
routinely as standard and therefore, ethics committee approval was not<br />
required. Patient identifiable data has been anonymised and stored on<br />
electronic devices with technical encryption (Data Protection Act, 1998).<br />
Consent for publication<br />
Not applicable.<br />
Competing interests<br />
JG, ETA, GW and RL are all employees of Air <strong>Ambulance</strong> Kent, Surrey<br />
and Sussex. JB is an employee of South East Coast <strong>Ambulance</strong> Service<br />
NHS Foundation Trust. There were no financial or non-financial conflicts<br />
of interest.<br />
Author details<br />
1<br />
Air <strong>Ambulance</strong> Charity Kent Surrey Sussex, Hanger 10 Redhill<br />
Aerodrome, Redhill RH1 5YP, <strong>UK</strong>. 2 University of Surrey, School of<br />
Health Sciences, Priestley Rd, Guildford GU2 7YH, <strong>UK</strong>. 3 Department of<br />
Emergency Medicine, University Medical Center Groningen, Groningen,<br />
The Netherlands. 4 University of Bristol, Child Dental Health, Bristol<br />
Dental School, Faculty of Health Sciences, Lower Maudlin Street, Bristol<br />
BS1 2LY, <strong>UK</strong>. 5 South East Coast <strong>Ambulance</strong> NHS Foundation Trust,<br />
Neptune House, Gatwick, Surrey RH10 9BG, <strong>UK</strong>.<br />
Received: 30 May 2022 Accepted: 1 December 2022<br />
Published online: 13 December 2022<br />
References<br />
1. Holcomb J. Pragmatic, randomized optimal platelet and plasma ratios [Internet].<br />
clinicaltrials.gov; 2019 Feb [cited 2021 Nov 1]. Report No.: NCT01545232. https://<br />
clinicaltrials.gov/ct2/show/NCT01545232.<br />
2. Huang GS, Dunham CM. Mortality outcomes in trauma patients undergoing prehospital<br />
red blood cell transfusion: a systematic literature review. Int J Burns Trauma.<br />
2017;7(2):17–26.<br />
3. Lewis CT, Naumann DN, Crombie N, Midwinter MJ. Prehospital point-of-care lactate<br />
following trauma: a systematic review. J Trauma Acute Care Surg. 2016;81(4):748–55.<br />
4. Petrosoniak A, Hicks C. Resuscitation resequenced: a rational approach to patients with<br />
trauma in shock. Emerg Med Clin N Am. 2018;36(1):41–60.<br />
5. Convertino VA, Howard JT, Hinojosa-Laborde C, Cardin S, Batchelder P, Mulligan J,<br />
et al. Individual-specific, beat-to-beat trending of significant human blood loss: the<br />
compensatory reserve. Shock Augusta Ga. 2015;44(Suppl 1):27–32.<br />
6. Harris T, Davenport R, Mak M, Brohi K. The evolving science of trauma resuscitation.<br />
Emerg Med Clin N Am. 2018;36(1):85–106.<br />
7. Johnson MC, Alarhayem A, Convertino V, Carter R, Chung K, Stewart R, et al. Comparison<br />
of compensatory reserve and arterial lactate as markers of shock and resuscitation. J<br />
Trauma Acute Care Surg. 2017;83(4):603–8.<br />
8. Gavrilovski M, El-Zanfaly M, Lyon RM. Isolated traumatic brain injury results in significant<br />
pre-hospital derangement of cardiovascular physiology. Injury. 2018;49(9):1675–9.<br />
9. Brown JB, Cohen MJ, Minei JP, Maier RV, West MA, Billiar TR, et al. Pretrauma center red<br />
blood cell transfusion is associated with reduced mortality and coagulopathy in severely<br />
injured patients with blunt trauma. Ann Surg. 2015;261(5):997–1005.<br />
10. Odom SR, Howell MD, Silva GS, Nielsen VM, Gupta A, Shapiro NI, et al. Lactate<br />
clearance as a predictor of mortality in trauma patients. J Trauma Acute Care Surg.<br />
2013;74(4):999–1004.<br />
11. Oyetunji TA, Chang DC, Crompton JG, Greene WR, Efron DT, Haut ER, et al. Redefining<br />
hypotension in the elderly: normotension is not reassuring. Arch Surg Chic Ill 1960.<br />
2011;146(7):865–9.<br />
12. ter Avest E, Griggs J, Wijesuriya J, Russell MQ, Lyon RM. Determinants of prehospital<br />
lactate in trauma patients: a retrospective cohort study. BMC Emerg Med. 2020;20(1):18.<br />
13. Bloom BM, Grundlingh J, Bestwick JP, Harris T. The role of venous blood gas in the<br />
emergency department: a systematic review and meta-analysis. Eur J Emerg Med Off J<br />
Eur Soc Emerg Med. 2014;21(2):81–8.<br />
14. Baxter J, Cranfield KR, Clark G, Harris T, Bloom B, Gray AJ. Do lactate levels in the<br />
emergency department predict outcome in adult trauma patients? A systematic review. J<br />
Trauma Acute Care Surg. 2016;81(3):555–66.<br />
15. Vincent JL, Quintairos e Silva A, Couto L, Taccone FS. The value of blood lactate kinetics<br />
in critically ill patients: a systematic review. Crit Care. 2016;13(20):257.<br />
16. Guyette FX, Meier EN, Newgard C, McKnight B, Daya M, Bulger EM, et al. A comparison<br />
of prehospital lactate and systolic blood pressure for predicting the need for resuscitative<br />
care in trauma transported by ground. J Trauma Acute Care Surg. 2015;78(3):600–6.<br />
17. Rehn M, Weaver A, Eshelby S, Lockey D. London’s air ambulance: 3 year experience with<br />
pre-hospital transfusion. Resuscitation. 2015;1(96):156.<br />
18. Weaver A, Eshelby S, Norton J, Lockey D. The introduction of on-scene blood transfusion<br />
in a civilian physician-led pre-hospital trauma service. Scand J Trauma Resusc Emerg<br />
Med. 2013;21(Suppl 1):S27.<br />
19. von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP, et al.<br />
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE)<br />
statement: guidelines for reporting observational studies. Epidemiol Camb Mass.<br />
2007;18(6):800–4.<br />
20. Bodnar D, Rashford S, Williams S, Enraght-Moony E, Parker L, Clarke B. The feasibility<br />
of civilian prehospital trauma teams carrying and administering packed red blood cells.<br />
Emerg Med J. 2014;31(2):93–5.<br />
21. Miller TE. New evidence in trauma resuscitation—is 1:1:1 the answer? Perioper Med.<br />
2013;3(2):13.<br />
22. Chaiwat O, Lang JD, Vavilala MS, Wang J, MacKenzie EJ, Jurkovich GJ, et al. Early<br />
packed red blood cell transfusion and acute respiratory distress syndrome after trauma.<br />
Anesthesiology. 2009;110(2):351–60.<br />
23. Tonglet ML. Early prediction of ongoing hemorrhage in severe trauma: presentation of the<br />
existing scoring systems. Arch Trauma Res. 2016;5(4):e33377.<br />
24. Salottolo KM, Mains CW, Offner PJ, Bourg PW, Bar-Or D. A retrospective analysis of<br />
geriatric trauma patients: venous lactate is a better predictor of mortality than traditional<br />
vital signs. Scand J Trauma Resusc Emerg Med. 2013;14(21):7.<br />
25. Cantle PM, Cotton BA. Prediction of massive transfusion in trauma. Crit Care Clin.<br />
2017;33(1):71–84.<br />
26. Early Identification of Trauma-induced Coagulopathy: Development and Validation of a<br />
Multivariable Risk Prediction Model—PubMed [Internet]. [cited 2022 Feb 15]. https://<br />
pubmed.ncbi.nlm.nih.gov/31972649/.<br />
Publisher’s Note<br />
Springer Nature remains neutral with regard to jurisdictional claims in<br />
published maps and institutional affiliations.<br />
14<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
MOBILE WORKFORCE<br />
PURCHASING<br />
WORKSHOP<br />
MONITORING<br />
TASKS &<br />
SERVICING<br />
ASSET & INVENTORY<br />
MANAGEMENT<br />
RFID TECHNOLOGY<br />
STOCK<br />
MANAGEMENT<br />
MAKE READY<br />
FLEET<br />
MANAGEMENT<br />
BUSINESS INTELLIGENCE<br />
REPORTING
NEWSLINE<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
‘Golden Hour’ Study<br />
Reaches Major<br />
Trauma Milestone<br />
More than 200 major trauma<br />
patients have been recruited<br />
for a pioneering £10 million<br />
research project looking at<br />
early detectors of probable<br />
susceptibility to in-hospital<br />
infection and / or multi-organ<br />
failure.<br />
The ‘Golden Hour’ study, which<br />
commenced in 2014, is being led<br />
by Research in Emergency and<br />
Acute Care Team at the Queen<br />
Elizabeth Hospital in Birmingham<br />
and is supported by the National<br />
Institute of Health Research<br />
(NIHR). The study aims to improve<br />
patient outcomes by developing<br />
tests to help clinicians treating<br />
those who have suffered a major<br />
trauma to spot the early signs of<br />
whether patients are more likely<br />
to develop a serious infection or<br />
multi-organ failure in hospital in<br />
the days and week following the<br />
initial injury.<br />
The research, which has now<br />
recruited more than half of<br />
the patients required, is being<br />
supported by the critical care<br />
paramedics and pre-hospital<br />
emergency medicine doctors<br />
at Midlands Air <strong>Ambulance</strong><br />
Charity and West Midlands<br />
<strong>Ambulance</strong> Service University<br />
NHS Foundation Trust (WMAS),<br />
who collect blood samples from<br />
appropriate patients during the<br />
first hour of treatment.<br />
Dr Jon Hazeldine, research fellow<br />
at the University of Birmingham,<br />
who is leading the study, explains<br />
the research: “Although the<br />
major and immediate cause of<br />
death following severe trauma<br />
is haemorrhage, many trauma<br />
victims later die following<br />
complications such as multi-organ<br />
dysfunction or sepsis, with the<br />
individual’s immune response to<br />
injury significantly influencing the<br />
chances of developing these lifethreatening<br />
conditions.<br />
“To investigate the immune<br />
response to major trauma the<br />
Golden Hour study analyses blood<br />
samples acquired from trauma<br />
patients at a number of post-injury<br />
time-points. The acquisition of<br />
these samples commences in<br />
the pre-hospital setting, where<br />
patients are enrolled into the<br />
study within 60-minutes of their<br />
injury, a crucial time in which<br />
prompt medical treatment is key<br />
to survival.<br />
“Our collaboration with Midlands<br />
Air <strong>Ambulance</strong> Charity and WMAS<br />
provides us with unique access<br />
to trauma patient blood samples<br />
from the scene of injury, which<br />
enables us to study the immune<br />
system at the earliest possible<br />
opportunity following trauma. This<br />
has yielded new insights into the<br />
post-injury immune response and<br />
has demonstrated the importance<br />
of early blood sampling to truly<br />
understand how trauma alters the<br />
immune system.<br />
“To date, we have recruited more<br />
than 200 patients into the study<br />
and our experiments have shown<br />
that within minutes of injury,<br />
the immune system of trauma<br />
patients is suppressed. Based<br />
on these initial findings, our next<br />
aim is to establish whether, in the<br />
immediate aftermath of a major<br />
injury, there are differences in the<br />
immune responses of patients<br />
who experience poor clinical<br />
outcomes (e.g. the development<br />
of sepsis or multi-organ failure)<br />
compared to those who do not.<br />
If this proves to be the case, then<br />
we would be one step closer to<br />
uncovering potential markers that<br />
could be used to aid in the early<br />
identification and stratification of<br />
patients at risk of poor outcomes,<br />
which could have implications for<br />
their management and treatment.”<br />
Dr Mark Nash, medical director<br />
for Midlands Air <strong>Ambulance</strong><br />
Charity, added: “The first hour<br />
of treatment post-incident is<br />
renowned for being the most<br />
beneficial, giving a patient the<br />
best possible chance of survival<br />
and good recovery. We were<br />
keen to support the Golden Hour<br />
study to assist with patients’<br />
on-going advanced care within<br />
the hospital setting, again giving<br />
those in critical condition the best<br />
chance of a good outcome. The<br />
fact that more than 200 patients<br />
have now been recruited to the<br />
research will help the NIHR to<br />
positively influence in-hospital<br />
care, which will be of great benefit<br />
to patients.”<br />
To find out more about the<br />
Golden Hour study, visit srmrc.<br />
nihr.ac.uk/trials/golden-hour.<br />
Further information on Midlands<br />
Air <strong>Ambulance</strong> Charity is found<br />
at midlandsairambulance.com<br />
and West Midlands <strong>Ambulance</strong><br />
Service is found at wmas.nhs.uk<br />
WAS<br />
<strong>Ambulance</strong> station<br />
welcomes Ukrainian<br />
refugees<br />
Welsh ambulance service<br />
staff have recently welcomed<br />
Ukrainian refugees to their station<br />
Rhyl <strong>Ambulance</strong> Station hosted<br />
Ukrainian refugees who have<br />
settled in the area to teach them<br />
about the Welsh <strong>Ambulance</strong><br />
Service.<br />
As a result of Russia’s invasion<br />
on Ukraine, a large number of<br />
Ukrainian people have been<br />
displaced from their homes.<br />
To welcome them into Rhyl<br />
community, 10 Welsh <strong>Ambulance</strong><br />
staff members gave those families<br />
living in the area a tour of the<br />
station and taught them lifesaving<br />
skills, all through an interpreter.<br />
Dermot O’Leary, Duty Operations<br />
Manager for Conwy and<br />
Denbighshire, who helped arrange<br />
the visit, said: “Humanitarianism<br />
crosses all language barriers.<br />
“It’s been a great experience,<br />
especially seeing the smiles on the<br />
children’s faces as they had a go<br />
at bandaging.<br />
“No words or interpreters are<br />
needed to see enjoyment firsthand.”<br />
The children were able to tour an<br />
emergency ambulance and rapid<br />
response vehicle and learnt how<br />
to perform CPR and how to use a<br />
defibrillator.<br />
Dermot continued: “It was great<br />
to see community engagement in<br />
action, especially from so many<br />
of our staff who willingly gave up<br />
their free time to support the visit.<br />
“Seeing these kids from a wartorn<br />
country being so positive and<br />
upbeat made me really value what<br />
16<br />
For more news visit: www.ambulanceukonline.com
NEWSLINE<br />
I have and realise that despite all<br />
the pressures, we are lucky.”<br />
EEAST<br />
EEAST and Magpas<br />
Air <strong>Ambulance</strong><br />
crews win 999 Hero<br />
category at The<br />
Sun’s Who Cares<br />
Wins awards<br />
Crews from the East of England<br />
<strong>Ambulance</strong> Service NHS<br />
Trust (EEAST) and Magpas<br />
Air <strong>Ambulance</strong> received a<br />
national award for their efforts<br />
in bringing a 13-year-old in<br />
cardiac arrest back to life.<br />
Prime Minister Rishi Sunak<br />
presented the team with the<br />
999 Hero award at the Sun’s<br />
Who Cares Win awards at a<br />
star-studded ceremony at the<br />
Roundhouse in London which<br />
was broadcast on Channel 4 on<br />
Sunday 27th November.<br />
The team won the award for their<br />
work in saving the life of Daisy<br />
Webb, who suffered a cardiac<br />
arrest when walking to school in<br />
Huntingdon in April.<br />
EEAST crew members Grace<br />
Lemin, Harrison Galgut and<br />
Charlie Harris arrived within<br />
minutes of the 999 call from<br />
Tommy Sadler, 15, and his mum<br />
Linda. They discovered Daisy had<br />
had a cardiac arrest, and began<br />
CPR and shocked Daisy’s heart<br />
until her pulse returned.<br />
The crews then handed over care<br />
to colleagues from Magpas Air<br />
<strong>Ambulance</strong>: Dr James Price and<br />
Critical Care Paramedics Steve<br />
Chambers and Thomas Giddings.<br />
The team performed a rapid<br />
general anaesthetic at the incident<br />
scene – a procedure usually only<br />
available in a hospital – to protect<br />
Daisy’s vital functions before<br />
she was transferred by land to<br />
Addenbrooke’s Hospital for further<br />
care. She has since made a full<br />
recovery.<br />
Lesley Hall, Leading Operations<br />
Manager with EEAST who was<br />
also on scene during the incident,<br />
said: “We are all so proud to receive<br />
the award which recognised the<br />
incredible teamwork that saved<br />
Daisy’s life on that day in April.<br />
“We often talk about the chain<br />
of survival in our work and the<br />
actions of everyone involved<br />
changed the course of what could<br />
have happened to Daisy – from<br />
Tommy and Linda calling 999, to<br />
Charlie, Grace and Harrison taking<br />
their swift action to get Daisy’s<br />
heart started and to the seamless<br />
transition of care to the Magpas<br />
Air <strong>Ambulance</strong> critical care team.<br />
“Thanks to everyone involved Daisy<br />
has the rest of life in front of her.<br />
“We all had an amazing evening<br />
meeting so many famous faces<br />
and it was great to receive<br />
recognition for the work that we<br />
do, as the past two years have<br />
been challenging for ambulance<br />
services and the NHS as a<br />
whole.”<br />
Tom Abell, Chief Executive of<br />
East of England <strong>Ambulance</strong><br />
Service, said: “I am really<br />
pleased to hear that Daisy is<br />
recovering well. Everyone at<br />
EEAST is immensely proud of<br />
the team involved in saving<br />
Daisy’s life and receiving the 999<br />
Hero award at The Sun’s Who<br />
Cares Wins awards.<br />
“Our dedicated staff do lifesaving<br />
work like this every day, and<br />
this national recognition for this<br />
wonderful team will hopefully<br />
serve as a boost to their<br />
colleagues who are all working<br />
incredibly hard.”<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
17
NEWSLINE<br />
LAS<br />
Paramedic taught<br />
himself to swim for<br />
new role<br />
A paramedic who failed to get<br />
recruited for a specialist team<br />
at London <strong>Ambulance</strong> Service<br />
taught himself to swim so he<br />
could qualify for the role.<br />
After four years working on<br />
ambulances, Han Tugcu was<br />
keen to join the Hazardous Area<br />
Response Team (HART), a group<br />
of specially recruited and highly<br />
trained paramedics who provide<br />
life-saving medical care in highrisk<br />
and complex emergency<br />
situations, such as industrial<br />
accidents and natural disasters.<br />
To join HART, paramedics must<br />
complete a clinical exam and<br />
a fitness test, which includes<br />
swimming.<br />
However despite growing up in<br />
Sydney, Australia - close to some<br />
of the world’s most beautiful<br />
beaches - Han never learned to<br />
swim as a child.<br />
He said: “I don’t know how I<br />
avoided it but as you get older<br />
it gets harder to learn. It was<br />
embarrassing and I felt annoyed<br />
at myself that I couldn’t do it.<br />
“But I really wanted to join HART –<br />
I love working as a team in the big<br />
complex difficult jobs and I always<br />
like a challenge.”<br />
Han watched YouTube tutorial<br />
videos and visited his local pool<br />
a couple of times to try to teach<br />
himself to swim.<br />
However this challenge proved<br />
too much – Han failed the swim<br />
test and did not get the job,<br />
despite doing well in the rest of his<br />
fitness test and the clinical skills<br />
assessment.<br />
He admitted: “I was very stressed<br />
and very embarrassed not to<br />
complete the timed swim. I was<br />
devastated and disheartened<br />
about it.”<br />
Han was encouraged to improve<br />
his swimming and re-apply for<br />
the HART position. In between<br />
shifts, Han kept going back to<br />
the pool whenever he could, and<br />
when he re-applied a few months<br />
later, he managed to successfully<br />
complete the swimming test.<br />
He has since spent weeks<br />
completing tough water rescue<br />
training in Cardiff as well as<br />
learning all the other skills to<br />
prepare him to treat patients in<br />
perilous situations including fires,<br />
collapsed buildings, under trains<br />
or vehicles, or other in hard-toreach<br />
places.<br />
Training manager Chris Gill said:<br />
“Han has demonstrated incredible<br />
fortitude in overcoming his<br />
non-swimmer status and in less<br />
than a year, deftly participated<br />
in a number of water rescue<br />
scenarios.<br />
“He is a credit to himself and<br />
his team; and an inspiration to<br />
others.”<br />
Like all HART paramedics, Han<br />
is also trained to respond to<br />
chemical incidents, terror attacks<br />
and other high risk jobs.<br />
Care Quality Commission’s<br />
(CQC’s) inspection report of 13<br />
July 2022, which recognised<br />
the improved responsiveness of<br />
the Trust to incidents of alleged<br />
bullying, harassment, and<br />
discrimination. The EHRC was<br />
also encouraged by the Trust’s<br />
commitment to continuous<br />
improvement and the ongoing<br />
actions it plans to take.<br />
The action plan – including formal<br />
monitoring – had been agreed<br />
with the EHRC on 26th April<br />
2021 after a referral from the<br />
Care Quality Commission (CQC)<br />
following the inspection in August<br />
2020. That report found that<br />
the Trust had not done enough<br />
to address serious incidents<br />
of sexual abuse against both<br />
patients and staff.<br />
Since then, the Trust has delivered<br />
an action plan to address the<br />
concerns identified which has<br />
included enhanced training<br />
in appropriate behaviours,<br />
strengthening of the policies for<br />
handling cases of harassment and<br />
abuse, and training for managers<br />
which has led to stronger action<br />
when cases occur.<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
He added: “The opportunities<br />
and variety you get working as a<br />
paramedic in London surprise me<br />
every day.<br />
“My advice if you’re thinking of<br />
joining? You only grow through<br />
challenging yourself.”<br />
EEAST<br />
EHRC concludes<br />
legal agreement with<br />
EEAST<br />
The East of England <strong>Ambulance</strong><br />
Service (EEAST) NHS Trust has<br />
made significant progress in<br />
tackling sexual harassment and<br />
is no longer under the legally<br />
enforceable action plan which<br />
was agreed with the Equality<br />
and Human Rights Commission<br />
(EHRC) in April 2021.<br />
The EHRC acknowledged the<br />
progress made and noted the<br />
While formal monitoring ended at<br />
the conclusion of the agreement<br />
at the end of October, EEAST has<br />
committed to making continuous<br />
improvements to protect its<br />
workforce and ensure a safe and<br />
supportive workplace.<br />
Tom Abell, Chief Executive of<br />
EEAST, said:<br />
“The conclusion of this agreement<br />
with the EHRC shows the<br />
progress that we have made in<br />
tackling long-standing cultural<br />
issues at the Trust.<br />
“I would like to thank all our<br />
people for their hard work during<br />
a time when our service has been<br />
under severe pressure.<br />
“We still have a long way to<br />
go, and we are committed to<br />
continuing this improvement and<br />
building a culture which is a great<br />
place to work for everyone.”<br />
18<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
Over half of NHS<br />
Trusts providing or<br />
planning foodbanks<br />
for staff<br />
New research from NHS<br />
Charities Together suggests<br />
over half of NHS Trusts and<br />
Health Boards could be<br />
providing or planning to provide<br />
foodbanks for their staff, as the<br />
cost of living skyrockets.<br />
In a survey of NHS charities, who<br />
support every Trust and Health<br />
Board in the <strong>UK</strong>, 21% of the 34<br />
who responded said they had an<br />
active foodbank for NHS staff or<br />
are implementing one, and a further<br />
35% are exploring the possibility.<br />
Of the six active foodbanks who<br />
responded, three were newly<br />
opened between October-<br />
December 2022. Across these six<br />
alone, they estimate nearly 5000<br />
NHS staff are making use of them<br />
on a monthly basis, with around<br />
550 of these nurses.<br />
In addition to food banks, over<br />
half of the NHS charities surveyed<br />
(53%) are looking at other food<br />
support for staff – these include<br />
voucher programmes, free<br />
breakfasts, and subsidised meals<br />
in the canteen, where staff can<br />
also bring their families.<br />
Ellie Orton OBE, Chief Executive<br />
of NHS Charities Together, said:<br />
“As the cost of living escalates, like<br />
many employers NHS Trusts and<br />
the charities who support them are<br />
looking at ways to help staff through<br />
the crisis. But with pressures facing<br />
NHS workers already so extreme,<br />
it’s heart-breaking that some are<br />
having to resort to using food banks<br />
to get by.<br />
“Right now hardship funds<br />
and support are the main topic<br />
of interest for NHS charities.<br />
Queries from our members range<br />
from the setting up of Benevolent<br />
Funds and access to travel<br />
bursaries, to the possibility of<br />
providing hot meal vouchers and<br />
other basic support, including<br />
food banks.<br />
“As a sector we are proud to<br />
support the staff and patients of<br />
the NHS however we can, and<br />
sadly today that support is more<br />
important than ever.”<br />
Examples of the response to<br />
increased need amongst staff<br />
include in Liverpool, where<br />
Liverpool Women’s NHS<br />
Foundation Trust’s partnership<br />
with a food poverty charity is<br />
providing around three trollies of<br />
food a week, with other staff also<br />
donating items.<br />
Michelle Turner, Chief People<br />
Officer and Deputy Chief<br />
Executive at Liverpool Women’s<br />
NHS Foundation Trust, said:<br />
“We know with the pressures of<br />
the current financial climate, like<br />
many other people our staff may<br />
be finding things more difficult at<br />
the moment. We decided to set<br />
up a staff pantry to provide help<br />
to anyone who may need it - no<br />
questions asked. The pantry<br />
consists of sealed and dry foods<br />
as well as other essential items<br />
such as sanitary products which<br />
can be accessed by staff 24/7.<br />
The running costs of the pantry is<br />
managed through our staff health<br />
and wellbeing fund as well as<br />
relying on kind donations of items<br />
from staff who are in a position to<br />
donate and donations from other<br />
partners in the city. So far it has<br />
been very well received and we<br />
will continue offering it for as long<br />
as it is needed.”<br />
>>><br />
A WORLD OF COMFORT<br />
CLIMATE CONTROLLED HEALTHCARE<br />
Customised vehicle heating and cooling solutions from Eberspacher.<br />
Simple to use, effective in performance and reliable in operation.<br />
On the move comfort for patient and healthcare professionals.<br />
|<br />
WWW.EBERSPACHER.COM
NEWSLINE<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
In Lothian, Food Pantries have<br />
been set up by the local Unison<br />
branch with support from NHS<br />
Lothian Charity and Edinburgh<br />
and East Lothian Food Projects<br />
to help staff who are struggling<br />
financially because of the<br />
increased prices of gas, electricity,<br />
mortgages and more.<br />
Jane Ferguson, Director of NHS<br />
Lothian Charity, said: “As an NHS<br />
charity, we are committed to<br />
working together with partners<br />
to support our local NHS staff<br />
who are experiencing economic<br />
hardship as a result of this crisis<br />
in whichever way we are able to.<br />
Unison Lothian Health Branch<br />
had been made aware that some<br />
staff were struggling to buy food<br />
for their children or didn’t have<br />
enough for their bus fare to<br />
come into work and, together,<br />
we wanted to do something<br />
to help. With funding from the<br />
Charity for food parcels, Unison<br />
has co-ordinated setting up Food<br />
Pantries at various sites across<br />
Edinburgh, Midlothian, East<br />
Lothian and West Lothian for staff<br />
in need of additional support.”<br />
As the national charity caring for<br />
the NHS, NHS Charities Together<br />
works with a network of over 230<br />
NHS charities providing extra<br />
support in every hospital and<br />
health board in the <strong>UK</strong>. To find<br />
out more about NHS Charities<br />
Together and the work NHS<br />
charities do to support staff,<br />
please visit<br />
www.nhscharitiestogether.co.uk<br />
YAS<br />
Yorkshire <strong>Ambulance</strong><br />
Service staff praised<br />
for long service<br />
Members of staff with a<br />
combined service of 3,280<br />
years have been recognised by<br />
Yorkshire <strong>Ambulance</strong> Service<br />
NHS Trust (YAS) at the Long<br />
Service and Retirement Awards<br />
2022, including one member<br />
of staff who has clocked up an<br />
incredible 50 years.<br />
They gathered for the special<br />
celebration at Pavilions of<br />
Harrogate and were joined by<br />
other guests including Reverend<br />
Brian Hunt, Deputy Lieutenant of<br />
North Yorkshire.<br />
This year’s recipients of awards<br />
for 20, 30, 40 and 50 years’<br />
service include staff from A&E<br />
Operations, the Emergency<br />
Operations Centre, nonemergency<br />
Patient Transport<br />
Service, NHS 111, clinical<br />
education, project management,<br />
and quality improvement.<br />
The honours also included<br />
the Queen’s Long Service and<br />
Good Conduct Medal, which<br />
was awarded to 32 staff on the<br />
day for 20 years’ exemplary<br />
frontline emergency service and<br />
14 retirees were also recognised<br />
for their valuable service to the<br />
Trust and communities across<br />
Yorkshire.<br />
In total, 43 individuals were<br />
congratulated for achieving<br />
20 years’ NHS service and 10<br />
individuals for reaching the 30<br />
years’ service milestone. Seven<br />
staff were recognised for an<br />
incredible 40 years of service.<br />
The longest-serving member of<br />
staff in attendance was Service<br />
Development Project Manager<br />
(Integrated Urgent Care) Bob<br />
Sunley, who picked up an award<br />
for an outstanding 50 years’<br />
service.<br />
Bob started his career with<br />
East Yorkshire County Council<br />
<strong>Ambulance</strong> Service (which later<br />
became Humberside <strong>Ambulance</strong><br />
Service) on 1 March 1971 as an<br />
ambulance cadet, working initially<br />
as an ambulanceman in Beverley<br />
and Bridlington. He also worked<br />
in the control room where he<br />
was Control Superintendent.<br />
After 23 years in operations, he<br />
became Director of Business<br />
Development for Humberside<br />
<strong>Ambulance</strong> Service, before taking<br />
on the role of General Manager<br />
for NHS Direct when it was<br />
hosted by Tees, East and North<br />
Yorkshire <strong>Ambulance</strong> Service<br />
(TENYAS). Latterly, he has been<br />
a huge part of the NHS 111<br />
management team, delivering<br />
many successful projects in the<br />
urgent care service.<br />
Rod Barnes, Chief Executive of<br />
Yorkshire <strong>Ambulance</strong> Service<br />
NHS Trust, said:<br />
“The pressures the service and<br />
wider NHS have faced over the<br />
last three years have been the<br />
most significant of our lifetime<br />
and are likely to be with us for<br />
some time to come. This has<br />
tested our physical and emotional<br />
resilience as never before.<br />
“During these pressured<br />
moments we often don’t spend<br />
enough time simply letting people<br />
know how we feel, saying thankyou<br />
or well done, you’ve done a<br />
great job.<br />
“So, it’s even more important that<br />
we take time at these awards<br />
ceremonies to ensure colleagues<br />
are recognised for the fantastic<br />
work that they do and their<br />
tireless dedication to patient care.<br />
“The commitment, compassion<br />
and teamwork shown by people<br />
across the service in responding<br />
to the pandemic and wider<br />
challenges has been simply<br />
extraordinary and humbling<br />
to witness. Everyone has<br />
consistently gone above and<br />
beyond for our patients, and<br />
they all have so much to be really<br />
proud about.”<br />
The awards ceremony was also<br />
an opportunity for members<br />
of staff who recently retired to<br />
celebrate a lifetime of service to<br />
the NHS. Some of them enjoyed<br />
their jobs so much that they<br />
have come out of retirement and<br />
returned to work.<br />
SWASFT<br />
<strong>Ambulance</strong> service<br />
wins national award<br />
for new system that<br />
helps vulnerable<br />
patients<br />
A new IT system which has<br />
transformed how the South<br />
Western <strong>Ambulance</strong> Service<br />
NHS Foundation Trust<br />
(SWASFT) identifies and helps<br />
vulnerable patients, has won a<br />
national award.<br />
SWASFT teamed up with Exeterbased<br />
Iridium Consulting to create<br />
the Frequent Caller Management<br />
System (FCMS), which has won<br />
the Best Healthcare Management<br />
Solution category in the Health<br />
Tech Digital Awards 2022.<br />
The system was developed in Exeter<br />
and Bristol but serves patients from<br />
across the whole of the South West<br />
region from the Isles of Scilly to<br />
North Gloucestershire.<br />
FCMS is the first system of its<br />
kind in the <strong>UK</strong> that automatically<br />
identifies any individual who meets<br />
the criteria of being a frequent<br />
caller to 999 and who contacts<br />
the ambulance service from within<br />
its geographical area.<br />
Previously, SWASFT’s database<br />
could identify only addresses, not<br />
people – which caused problems<br />
if callers were away from home, or<br />
if they lived in a house of multiple<br />
occupancy.<br />
The bespoke system uses a<br />
unique algorithm to identify<br />
people who contact the service<br />
frequently and enables SWASFT<br />
to provide accurate, up-to-date<br />
information to Multi-Disciplinary<br />
Team meetings about them. Its<br />
data also helps shape specialised<br />
programmes for this group of<br />
20<br />
For more news visit: www.ambulanceukonline.com
NEWSLINE<br />
patients. Together, this enables<br />
them to receive more personalised<br />
care.<br />
Frequent callers, defined as<br />
anyone who calls the ambulance<br />
service five times or more in one<br />
month, are vulnerable because<br />
they often have a complex<br />
mixture of medical, social and<br />
psychological needs. This<br />
means they need the help of a<br />
Multi-Disciplinary Team and can<br />
experience repeated difficulties<br />
when trying to access care and<br />
support.<br />
“Distilling and presenting such<br />
a large dataset into a concise,<br />
more manageable and meaningful<br />
version required new approaches<br />
and solutions, making FCMS a<br />
truly unique application in the<br />
space. It wouldn’t have been<br />
possible without such a close<br />
working relationship with the team<br />
at SWASFT and it is an honour to<br />
see the application being used as<br />
a central tool for managing such<br />
a complex part of the service<br />
SWASFT provides.”<br />
Other benefits of FCMS include:<br />
Jonathan Hammond-Williams,<br />
SWASFT’s Complex Care Lead,<br />
says: “This system helps us to<br />
identify and support some of our<br />
most vulnerable patients. They are<br />
often socially isolated and have<br />
not one but several health needs.<br />
Having multiple problems coming<br />
together forms what can feel like<br />
the perfect storm for them.<br />
“FCMS has revolutionised what<br />
we do. We have gone from<br />
manually counting houses to<br />
automatically providing data to<br />
help improve each individual<br />
patient’s quality of life. It allows<br />
us to track who has called and<br />
why, and to support the wider<br />
healthcare system in getting them<br />
the personalised help they need.<br />
“It was a real team effort to<br />
develop FCMS and I’m so<br />
pleased SWASFT and Iridium<br />
Consulting have earned this<br />
national acknowledgement. I’d<br />
like to thank everyone who has<br />
contributed, both within and<br />
outside the ambulance service”.<br />
Sam Rankin, Director of Iridium<br />
Consulting, says: “We were<br />
delighted when we learnt about<br />
winning the award. Overcoming<br />
the challenges to design and<br />
develop FCMS to support the<br />
ambulance service that serves 20<br />
per cent of England’s land-mass is<br />
something the team at Iridium are<br />
immensely proud of.<br />
• Reducing the number of distinct<br />
frequent callers to SWASFT<br />
from 1,500 a month in 2018<br />
to 925 in 2022, as callers are<br />
supported by more appropriate<br />
services than an emergency<br />
ambulance<br />
• Improving the availability of<br />
ambulances across the South<br />
West to attend life-threatening<br />
emergencies<br />
• Providing a one-stop shop for<br />
health professionals to see all<br />
previous episodes of care, the<br />
reasons for a call, and the actions<br />
completed by the clinicians<br />
involved in their 999 calls<br />
• Enabling improved links<br />
with other parts of the NHS,<br />
including acute hospitals trusts<br />
and mental health trusts.<br />
Jess Taylor, Senior Frequent Caller<br />
Administrator, helped develop the<br />
system. She adds: “FCMS allows<br />
us to put the patient at the centre of<br />
everything we do. A lot of work has<br />
gone into the system, so it’s very<br />
humbling and very exciting to get<br />
that recognition on a national level”.<br />
The system, which became<br />
operational in November 2020,<br />
has also supplied data that has<br />
helped shape services for this<br />
very vulnerable group of patients<br />
across the whole of the South<br />
West, with at least five new<br />
services being developed within<br />
parts of the region as a result.<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Do you have anything you would like to add or include in Newsline? Please contact us and let us know.<br />
21
NEWSLINE<br />
LAS<br />
“Don’t ‘man up’,<br />
get help!” – 999<br />
call handler opens<br />
up about mental<br />
health struggle as he<br />
appeals for men to<br />
seek support<br />
A London <strong>Ambulance</strong> Service<br />
(LAS) emergency call handler<br />
is urging men to seek mental<br />
health support as soon as they<br />
realise something is wrong,<br />
and not shy away from having<br />
that conversation with their<br />
loved ones.<br />
Scott Robertson, 33, who has<br />
worked as an LAS emergency<br />
call coordinator since 2019,<br />
made the appeal to mark<br />
Men’s Mental Health Month in<br />
November 2022.<br />
Scott was diagnosed with<br />
bipolar disorder four years<br />
ago but has suffered from<br />
poor mental health since his<br />
adolescence.<br />
Living with bipolar disorder<br />
means his life can be affected<br />
by extreme mood swings, and<br />
without the appropriate medical<br />
and psychological approach,<br />
he can face periods of severe<br />
emotional highs and lows.<br />
He said: “Living with bipolar<br />
almost feels like my mood is<br />
under a magnifying glass. I take<br />
medications to keep my mood<br />
stable, but there are periods<br />
in which my mental health can<br />
deteriorate.<br />
“Just a couple of months ago,<br />
I had a depressive episode<br />
and had to take some time off<br />
work and throw myself into my<br />
support network, which includes<br />
my husband, brother, and<br />
manager.”<br />
With calls to 999 often being<br />
the first point of care for those<br />
in a mental health crisis, Scott<br />
is witness to the mental health<br />
struggles of many Londoners.<br />
From September 2021 to<br />
August 2022, nearly 186,000<br />
calls with a potential mental<br />
health element were made to<br />
London <strong>Ambulance</strong> Service,<br />
86,758 of which were from male<br />
patients.* Over the past year, our<br />
staff and volunteers attended<br />
18,735 call-outs to patients with<br />
suicidal symptoms or having<br />
attempted suicide, and 9,028 of<br />
these incidents involved a male<br />
patient.**<br />
Scott fears that the number of<br />
men in London suffering from<br />
mental health conditions is<br />
higher than LAS figures may<br />
depict.<br />
“Societal pressures can put men<br />
off from calling for help, he said.<br />
“I felt a sense of shame when<br />
confessing my mental health<br />
condition, because I felt the<br />
pressure to ‘man up’ and meet<br />
the standard of what a man<br />
should be.<br />
“When I was diagnosed with<br />
bipolar I became very secretive<br />
about it. I was ashamed of the<br />
diagnosis and I didn’t want<br />
“If someone calls 999, they want<br />
to reach out and talk about<br />
the problem. When they don’t,<br />
they’re quick enough to tell you<br />
and you change the subject as<br />
necessary.”<br />
Having battled with low mood<br />
for a large part of his life, Scott<br />
wants to normalise the debate<br />
around mental health, especially<br />
amongst men, who can face<br />
stigma when opening up.<br />
Scott’s advice is straightforward:<br />
“Don’t ‘man up’, get help! If<br />
you have a support network<br />
– a group of trusted friends or<br />
family, then give them a chance.<br />
Sometimes you write people off<br />
thinking that they’re not going to<br />
understand. But I’ve found that<br />
the minute you open up, people<br />
do want to understand and want<br />
to support you.<br />
“The more we open up, the more<br />
we discuss mental health, the<br />
more we empower those around<br />
us to do the same and support<br />
each other.”<br />
anyone to know about it. I<br />
If you are having suicidal<br />
swore the people around me to<br />
thoughts, thoughts of harming<br />
secrecy, Scott continued.<br />
yourself or others, or if you do<br />
not feel you can keep yourself<br />
“As a gay man, I felt a bit<br />
and someone else safe call 999<br />
excluded from typical ideas<br />
or go to A&E now.<br />
of masculinity. Being then<br />
diagnosed with a mental health<br />
If you need help urgently for your<br />
condition made me fear that I<br />
mental health, but it’s not an<br />
wouldn’t be taken as seriously<br />
emergency call 111 or use NHS<br />
as a straight, healthy man.”<br />
111 online service.<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
But Scott’s battle with mental<br />
health, which has marked over<br />
half of his life, now acts as an<br />
inspiration to better empathise<br />
with patients who are at crisis<br />
point.<br />
He said: “I experience those<br />
crises myself and I know the<br />
desperation that you can feel<br />
in those situations, so I’m<br />
not frightened to have those<br />
conversations with patients.<br />
If you are experiencing<br />
symptoms such as low mood,<br />
anxiety, and depression call 111<br />
or speak to your GP.<br />
To access more mental health<br />
services, visit www.nhs.uk/<br />
nhs-services/mental-healthservices/.<br />
Your mental health is as important<br />
as your physical health. You will<br />
not be wasting anyone’s time.<br />
22<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
NEWSLINE<br />
New mental health<br />
ambulances scheme<br />
to take pressure off<br />
other emergency<br />
services - Hexagon<br />
comments<br />
The <strong>UK</strong> Government<br />
announced* that a £150<br />
million investment will be<br />
made to support those<br />
experiencing mental health<br />
issues through specialised<br />
mental health ambulances<br />
and other crisis services. The<br />
investment will enable the<br />
procurement of approximately<br />
100 new mental health<br />
ambulances, which will<br />
take specially trained staff<br />
directly to patients in order<br />
to deliver support on the<br />
scene or transfer them to an<br />
appropriate place of care.<br />
With patients facing mental health<br />
problems being twice as likely<br />
to spend 12 hours or more in<br />
emergency departments than<br />
other patients, this funding will<br />
allow 150 new projects centered<br />
on supporting the provision of<br />
mental health crisis response<br />
to enable more convenient and<br />
efficient care for mental health<br />
patients whilst reducing critical<br />
hospital admissions.<br />
Nick Chorley, director of public<br />
safety and security for EMEA at<br />
Hexagon’s Safety, Infrastructure<br />
& Geospatial division, welcomes<br />
these new programmes and<br />
comments on what else needs to<br />
be considered.<br />
“Given the rise in patients<br />
presenting with mental health<br />
issues, it is great to see<br />
programmes being rolled out to<br />
provide better patient care, by<br />
delivering specialist staff who are<br />
more adept in dealing with mental<br />
health emergencies. Equally, it<br />
is essential that specialist and<br />
expensive resources like sworn<br />
police officers or ambulances<br />
that are uniquely able to perform<br />
certain tasks are kept available for<br />
those tasks when they happen and<br />
not tied up on tasks that others<br />
can perform. Nonetheless, whilst<br />
this is a step in the right direction<br />
for improving care of mental<br />
health patients, if the triaging<br />
of appropriate care remains<br />
ineffective, patients will not receive<br />
the help they need, and this<br />
investment will be wasted.<br />
“Indeed, the <strong>UK</strong> Government<br />
must streamline the way<br />
emergency services respond<br />
to patients experiencing mental<br />
health issues by ensuring that<br />
modern technology is available<br />
to accommodate these new<br />
programmes. One of the best<br />
ways that technology can help<br />
this new way of dispatching<br />
personnel to mental health<br />
emergencies is via data analysis.<br />
Utilising analytics from routine<br />
operational data, such as call data<br />
from computer-aided dispatch<br />
systems, emergency centre<br />
managers can gain insights to<br />
help ensure that the right member<br />
of staff is assigned to the job that<br />
they are best placed to deal with.<br />
Operational data and analytics can<br />
also be integrated with artificial<br />
intelligence to offer new levels of<br />
assistive insights to dispatchers,<br />
enabling the best possible level of<br />
care to be provided to the patient at<br />
hand. Not only do these solutions<br />
have the potential to treat mental<br />
health emergencies quicker and<br />
more efficiently, but they can also<br />
save emergency service resources.”<br />
*https://www.gov.uk/<br />
government/news/mental-<br />
health-services-boosted-by-<br />
150-million-government-funding<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
23
NEWSLINE<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
LAS<br />
Paramedic speaks<br />
out after patient<br />
jailed for sexual<br />
assault<br />
A paramedic at London<br />
<strong>Ambulance</strong> Service who<br />
was sexually assaulted by a<br />
patient has spoken out in the<br />
hope it will encourage others<br />
to seek justice – after her<br />
attacker was jailed.<br />
Naveed Ahmed, aged 35, of<br />
Hickling Road, Ilford, was jailed<br />
in November for nine months<br />
after he groped paramedic<br />
Charlotte Miller and exposed<br />
himself.<br />
Charlotte has waived her<br />
right to anonymity, which is<br />
automatically granted to victims<br />
of sexual offences, in the hope it<br />
will encourage others to report<br />
similar crimes.<br />
She said: “My crewmate and I<br />
were encouraging the patient to<br />
get into the ambulance so we<br />
could assess him but he grabbed<br />
my crotch and tried to grab me<br />
again. Then he pulled his pants<br />
down.<br />
“I couldn’t believe it, I was asking<br />
myself if it really happened. I was<br />
frightened and scared. I think the<br />
reason I was so shocked was<br />
because it was so unexpected –<br />
I was there to help him.”<br />
Newly released footage from an<br />
ambulance video camera, shows<br />
Charlotte on her radio calling the<br />
police moments after the assault.<br />
Police officers arrived in less than<br />
a minute and arrested Ahmed<br />
after the incident in Edgware<br />
Road last October.<br />
Charlotte added: “The whole<br />
thing was sickening and<br />
disgusting and really made us<br />
feel quite vulnerable.<br />
“But I would urge everyone to<br />
report these things because I was<br />
well supported by my management<br />
team and by the police.<br />
“It’s only by reporting this sort of<br />
behaviour and helping police to<br />
prosecute that the message will<br />
get through that there are serious<br />
consequences.”<br />
In 2022 there were a total of<br />
49 sexual assaults on London<br />
<strong>Ambulance</strong> Service (LAS) staff or<br />
volunteers. There were a further<br />
516 physical assaults – including<br />
kicking, punching, head-butting<br />
and attacks with a weapon - and<br />
601 reports of verbal abuse or<br />
threats of violence.<br />
The Service has invested more<br />
than £3 million in kitting out its<br />
ambulances with video cameras<br />
aimed at protecting crews. So far,<br />
video captured by the ambulance<br />
cameras has been used in several<br />
successful prosecutions, with 92<br />
submissions of video evidence<br />
since April 2022.<br />
London <strong>Ambulance</strong> Service’s<br />
Chief Paramedic Dr John Martin<br />
said: “Our ambulance crews and<br />
call handlers should be able to<br />
work without fear of violence,<br />
sexual violence or threats.<br />
“They come to work each day<br />
to help others so we will do<br />
everything we can to keep them<br />
safe and ensure they are treated<br />
with the respect they deserve.”<br />
LAS joined ambulance services<br />
across the country to launch a<br />
“Work Without Fear” campaign<br />
to promote a no-violence culture<br />
and help create a safer work<br />
environment for front-line staff and<br />
volunteers.<br />
The Service has dedicated<br />
Violence Reduction Officers who<br />
encourage colleagues to report<br />
all incidents of abuse while also<br />
supporting them through the court<br />
process.<br />
Detective Constable Jorge Sobral,<br />
of the Metropolitan Police, was<br />
part of the team who pursued the<br />
case again Ahmed.<br />
He said: “Our colleagues in the<br />
ambulance service dedicate their<br />
lives to helping people, and it is<br />
not acceptable for them to be<br />
treated like this.<br />
“We will always investigate<br />
crimes like this and I would urge<br />
people to always report this sort<br />
of appalling behaviour to the<br />
police. This was a good result<br />
and will hopefully change people’s<br />
behaviour.”<br />
‘Unusual norovirus<br />
activity’ sees cases<br />
soar 37% higher<br />
than pre-pandemic<br />
average<br />
The <strong>UK</strong>HSA is reporting a 37%<br />
surge in cases of norovirus –<br />
often called winter vomiting<br />
sickness – compared to pre-<br />
Covid levels for the first weeks<br />
of January. As it warns ‘unusual<br />
norovirus activity’ will continue,<br />
a leading testing expert fears<br />
further strains on the NHS.<br />
Cases of norovirus, commonly<br />
known as winter vomiting<br />
sickness, have soared by 37%<br />
compared to the same period<br />
pre-Covid. A report from the <strong>UK</strong><br />
Health Safety Agency (<strong>UK</strong>HSA)<br />
says cases for the first two weeks<br />
in January jumped by 37% over<br />
the five season average prepandemic,<br />
with over 65s reporting<br />
the steepest rise.<br />
A leading testing expert is<br />
concerned that the changing<br />
pattern may indicate a further<br />
surge to come. He cautions that<br />
the virus has not returned to its<br />
overall pre-pandemic seasonal<br />
trend this winter and warns health<br />
professionals to take note of<br />
the <strong>UK</strong>HSA’s observation that<br />
24<br />
For more news visit: www.ambulanceukonline.com
NEWSLINE<br />
‘unusual norovirus activity will<br />
continue throughout the 2022/23<br />
season’.<br />
Dr Quinton Fivelman PhD, Chief<br />
Scientific Officer at London Medical<br />
Laboratory, says: ‘Norovirus is<br />
a very unpleasant virus. As its<br />
common name, winter vomiting<br />
bug, implies, it often causes<br />
sickness and diarrhoea. Other<br />
symptoms can include a fever,<br />
headache and aching arms and<br />
legs. Typically, it doesn’t last very<br />
long and usually goes away in<br />
two to three days, but it can lead<br />
to complications. In particular,<br />
children and the elderly can be<br />
badly affected by this virus and<br />
may require hospital treatment.<br />
‘The obvious concern is that the<br />
NHS has no spare capacity to<br />
deal with a further epidemic this<br />
winter, on top of Covid, flu and<br />
Strep A outbreaks. With industrial<br />
action in the health service set<br />
to escalate, increasing cases<br />
of norovirus couldn’t come at a<br />
worse time.<br />
‘Commonly, the most serious<br />
complication from norovirus is<br />
dehydration, particularly if you<br />
or your child cannot keep fluids<br />
down. In the case of babies and<br />
young children, seek medical<br />
advice if they stop breast or bottle<br />
feeding, or if they show other<br />
signs of dehydration such as<br />
fewer wet nappies.<br />
‘You should call 111 if you (or<br />
your child) have bloody diarrhoea<br />
or bleeding from the bottom,<br />
diarrhoea for more than 7 days or<br />
vomiting for more than 2-3 days.<br />
‘Concerning though this sudden<br />
jump in cases is, the good news<br />
is that it is unlikely that we are<br />
seeing a new mutation, despite<br />
the warning of “unusual” activity.<br />
This winter, the main strain<br />
continues to be genogroup 2 (GII)<br />
that makes up 74% of cases,<br />
with the main genotype being<br />
GII.4, causing 32% of cases. Last<br />
winter, GII caused 90% of cases<br />
and GII.4 specifically 48%.<br />
‘Rather than any new variant,<br />
the main reason for this month’s<br />
spike in cases is likely to be that<br />
immunity against norovirus is<br />
fairly short-lived and during the<br />
pandemic fewer people were<br />
exposed to the virus than normal.<br />
Now everyone is mixing again,<br />
cases are increasing. This virus<br />
spreads very easily and quickly,<br />
more so than the other viruses<br />
causing illness this winter.<br />
‘With our immunity down, it’s<br />
sensible to take precautions to<br />
avoid this unpleasant virus, if<br />
possible. You can catch norovirus<br />
from:<br />
• close contact with someone<br />
with the virus<br />
• touching surfaces or objects<br />
that have the virus on them,<br />
then touching your mouth<br />
• eating food that’s been<br />
prepared or handled by<br />
someone with norovirus<br />
‘As with Covid, washing your<br />
hands frequently with soap and<br />
water is the best way to stop it<br />
spreading. However, it’s important<br />
to note that alcohol hand gels<br />
don’t kill this bug.<br />
‘A general health test might be a<br />
useful course of action for anyone<br />
concerned, to ensure they are<br />
in good health to fight infections<br />
and reduce the likelihood of<br />
needing access to health services<br />
this winter. London Medical<br />
Laboratory’s General Health<br />
Profile Test provides people with a<br />
comprehensive check-up of their<br />
general health, including diabetes<br />
(HbA1c), gout, liver & kidney<br />
function, bone health, iron levels<br />
and a full cholesterol profile. Other<br />
more comprehensive tests check<br />
your vitamin D levels, which are<br />
often low at this time of year, and<br />
any potential thyroid or hormonal<br />
imbalances.<br />
‘They can be taken at home<br />
through the post, or at one of the<br />
many drop-in clinics that offer<br />
these tests across London and<br />
nationwide in over 90 selected<br />
pharmacies and health stores.<br />
If done in-store, a full blood test<br />
can be added that can indicate<br />
a wide range of issues such as<br />
infection, anaemia and leukaemia.<br />
For full details, see: https://www.<br />
londonmedicallaboratory.com/<br />
product/general-health<br />
AAKSS<br />
Tracey Crouch MP<br />
presents the Queen’s<br />
Platinum Jubilee<br />
medals to front<br />
line staff from Air<br />
<strong>Ambulance</strong> Charity<br />
Kent Surrey Sussex<br />
(KSS)<br />
On Friday 25 November Tracey<br />
Crouch, MP for Chatham<br />
and Aylesford, attended the<br />
Rochester headquarters of<br />
Air <strong>Ambulance</strong> Charity Kent<br />
Surrey Sussex (KSS) to present<br />
the Queen’s Platinum Jubilee<br />
Medals to front line staff from<br />
the life-saving charity.<br />
KSS invited Tracey Crouch to<br />
present the medals in recognition<br />
of the exceptional role she played,<br />
in partnership with Air <strong>Ambulance</strong>s<br />
<strong>UK</strong> (AA<strong>UK</strong>), in persuading the<br />
Government to enable eligible staff<br />
from Air <strong>Ambulance</strong> charities to be<br />
included in the medal allocation.<br />
Prior to this campaign, no one<br />
directly employed from the Air<br />
<strong>Ambulance</strong> sector was included in<br />
the awards.<br />
As part of the activity to extend<br />
the award eligibility to Air<br />
<strong>Ambulance</strong> staff, Tracey Crouch<br />
rallied support from 25 MPs<br />
across Kent, Surrey and Sussex.<br />
Together they signed a joint letter<br />
to the Rt Hon Sajid Javid MP, who<br />
was then the Secretary of State<br />
for Health and Social Care.<br />
David Welch, CEO, KSS said:<br />
“KSS wrote to Tracey Crouch<br />
earlier this year to highlight the<br />
exclusion of air ambulance staff<br />
from these awards and she<br />
immediately offered her support.<br />
Her actions resulted in the<br />
Department of Health and Social<br />
Care including eligible Helicopter<br />
Emergency Medical Services staff.<br />
“I couldn’t be prouder of the fact<br />
that 41 paramedics, doctors and<br />
pilots from Team KSS received<br />
their prestigious Platinum Jubilee<br />
Medals today. Without Tracey<br />
Crouch’s support, and the support<br />
from all our local MPs across<br />
Kent, Surrey and Sussex as well<br />
as Air <strong>Ambulance</strong>s <strong>UK</strong>, it would<br />
not have been possible for them<br />
to have received this honour.”<br />
Tracey Crouch MP said: “The<br />
air ambulance is a vital part of<br />
our emergency services ecosystem<br />
and it seemed incredibly<br />
unfair that they were due to be<br />
exempt from recognition. With<br />
their base situated on the border<br />
of my constituency I often see<br />
the helicopter heading off to<br />
or returning from an incident,<br />
knowing that they are called to the<br />
most difficult and challenging of<br />
situations taking the equivalent of<br />
an emergency department right<br />
to the scene. It was my absolute<br />
privilege to co-ordinate a call<br />
for their inclusion in the Queen’s<br />
Platinum Jubilee Medals and I am<br />
humbled to present them to some<br />
absolute heroes.”<br />
KSS provides world-leading<br />
pre-hospital emergency care<br />
whenever and wherever required<br />
to save lives and ensure the<br />
best possible patient outcomes.<br />
Its crews of pilots, doctors and<br />
paramedics responded to 3,051<br />
incidents in 2021, the charity’s<br />
busiest year in its 32-year history<br />
– and so far this year, the service<br />
has been in demand more than<br />
ever before.<br />
>>><br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Do you have anything you would like to add or include in Newsline? Please contact us and let us know.<br />
25
NEWSLINE<br />
Each year, KSS must raise<br />
£15.2M to operate its life-saving<br />
service. 86% of its total income<br />
is raised through the generosity<br />
of KSS’s supporters. For further<br />
information, please visit www.<br />
aakss.org.uk<br />
Galen and College of<br />
Paramedics call for<br />
entries for the Dr John<br />
Hinds Scholarship<br />
Award <strong>2023</strong><br />
Galen, the privately-owned<br />
pharmaceutical sales and<br />
marketing company is<br />
pleased to announce that<br />
applications for the Dr John<br />
Hinds Scholarship Award <strong>2023</strong><br />
are now open across Northern<br />
Ireland and the Republic of<br />
Ireland.<br />
The scholarship, which runs in<br />
association with The College<br />
of Paramedics, is presented<br />
in memory of the late Dr John<br />
Hinds, who was regarded<br />
as an inspirational leader by<br />
paramedics and emergency<br />
medical technicians and those in<br />
pre-hospital care within Ireland.<br />
A world-renowned critical care<br />
physician, Dr Hinds gave a<br />
huge amount of his own time<br />
to educating and supporting<br />
paramedics and ambulance staff<br />
throughout the Island of Ireland.<br />
He died in 2015 following a<br />
motorcycle accident.<br />
The recipient of the scholarship<br />
will win a fully funded place on<br />
the highly coveted Anaesthesia<br />
Trauma and Critical Care (ATACC)<br />
course and have their case<br />
study published in the College<br />
of Paramedics’ magazine,<br />
‘Paramedic INSIGHT’.<br />
Dr Dennise Broderick, Managing<br />
Director & President, Galen, said:<br />
“We are delighted to support this<br />
award for a fourth year, through<br />
our partnership with The College<br />
of Paramedics and pay tribute to<br />
Dr John Hinds’ legacy.<br />
“At Galen, we appreciate now<br />
more than ever the importance<br />
of the work undertaken<br />
by emergency medicine<br />
professionals right across the<br />
island of Ireland. We hope that<br />
through this scholarship we<br />
can support the emergency<br />
medicine sector in a small way,<br />
by providing a unique opportunity<br />
for healthcare professionals to<br />
advance their expertise and gain<br />
access to a globally recognised<br />
training programme.”<br />
Imogen Carter, Executive Officer<br />
for Policy Development at the<br />
College of Paramedics said:<br />
“The College of Paramedics<br />
is proud to host this award in<br />
the name of Dr John Hinds, in<br />
partnership with Galen. We look<br />
forward to receiving many highquality<br />
clinical case studies from<br />
responders across NI and ROI by<br />
the 27th of <strong>February</strong>.”<br />
To apply for the scholarship<br />
award, entrants must submit<br />
a Clinical Case Study that<br />
was experienced in person.<br />
Submissions should be<br />
750–1,000 words, excluding<br />
references and appendices and<br />
be written to protect patient<br />
confidentiality. As a condition of<br />
the award, the case study will<br />
be submitted for publication in<br />
Paramedic INSIGHT magazine<br />
which has over 20,000<br />
subscribers, along with a followup<br />
article that describes their<br />
experience on the ATACC course.<br />
Submissions must be made using<br />
the Dr John Hinds Scholarship<br />
Award Entry Form, available at<br />
the following link: https://galenpharma.com/news-events/news/<br />
john-hinds-scholarship-<strong>2023</strong> and<br />
submitted via email to awards@<br />
collegeofparamedics.co.uk by<br />
4pm on Monday 27th <strong>February</strong><br />
<strong>2023</strong>.<br />
The College Honours and Awards<br />
Committee will then select the<br />
winning piece. The awards<br />
ceremony will take place at the<br />
College of Paramedics National<br />
Conference on 23rd May <strong>2023</strong>.<br />
WAS<br />
Cheryl’s wing walk<br />
for charity<br />
A Welsh <strong>Ambulance</strong> Service<br />
worker is walking along a<br />
biplane wing for charity.<br />
Cheryl Hunter, a Volunteer Car<br />
Service Administrator for the<br />
Trust, will be walking the wing of<br />
a biplane to raise money for St<br />
Kentigern Hospice in memory of<br />
her father, James Miller Irvine.<br />
“But after seeing a picture of<br />
someone wing-walking a couple<br />
of years ago I just thought that I<br />
would love to do it, and why not<br />
fundraise while doing it.”<br />
The 60-year-old, who has<br />
worked for the Trust for 22<br />
years, will be taking on the<br />
aerial adventure for the mayor’s<br />
charity, which last year saw<br />
her husband, councillor Alan<br />
Hunter, the Mayor of Abergele,<br />
swim with sharks all in aid of St<br />
Kentigern Hospice.<br />
Cheryl said: “St Kentigern<br />
Hospice is a North Wales<br />
charity providing specialist<br />
palliative and end of life care,<br />
who do such a brilliant job.<br />
“It has a special place in my<br />
heart as the hospice cared for<br />
my father until the very end.<br />
“They have so much care to<br />
give to their patients but also<br />
provide so much support and<br />
comfort for families.<br />
“They are just fabulous.”<br />
Cheryl’s journey will start from<br />
Leeds East Airport, where the<br />
biplane will reach heights of up<br />
to 700ft and speeds of up to<br />
110mph.<br />
Pennie Walker, Volunteer<br />
Manager for the Trust’s Non-<br />
Emergency Patient Transport<br />
Service, said: “Cheryl is a brave<br />
and courageous woman, and I<br />
am proud that she is part of my<br />
team.<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Cheryl, who is also Mayoress of<br />
Abergele, will take to the skies on<br />
22 April <strong>2023</strong>.<br />
She said: “I’m actually looking<br />
forward to it.<br />
“It’s strange because I would<br />
never do a bungee jump, I would<br />
not put an elastic band around my<br />
ankles and jump off something.<br />
“It takes a lot of willpower to do<br />
something like this.<br />
“I wish her all the best and hope<br />
that she raises a good amount<br />
for St Kentigern Hospice, which<br />
I know is very close to her<br />
heart.”<br />
You can sponsor Cheryl via her<br />
JustGiving page.<br />
26<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
IN PERSON<br />
NWAS News<br />
<strong>Ambulance</strong> Service Deputy<br />
Chief Executive on 2022 New<br />
Year Honours list<br />
of towns in Cumbria including Cockermouth,<br />
Appleby, Keswick, and Kendal which<br />
devastated the area resulting in a mass<br />
evacuation and support systems to be put<br />
in place to look after many hundreds of<br />
members of the public displaced at the time.<br />
EHAAT News<br />
Operations Director for Essex<br />
& Herts Air <strong>Ambulance</strong> retires<br />
after 16 years’ service<br />
Deputy Chief Executive and Director of<br />
Strategy, Partnerships and Transformation<br />
Salman Desai has featured in the 2022<br />
King’s New Year Honours list. Salman will<br />
receive a King’s <strong>Ambulance</strong> Medal in the<br />
New Year.<br />
The King’s <strong>Ambulance</strong> Medal is awarded to<br />
ambulance staff who have shown distinguished<br />
service, exemplary dedication to their role, and<br />
demonstrated outstanding ability, merit and<br />
conduct to their vocation. On being awarded<br />
this honour, Salman said: “I am immensely<br />
proud and truly humbled to receive such an<br />
award after over 25 years’ service. It is an<br />
honour on a personal level but also for North<br />
West <strong>Ambulance</strong> Service (NWAS).<br />
“Helping people and shaping the organisation<br />
to meet and serve the needs of all of our<br />
communities is what motivates me. I have<br />
enjoyed every step of my career so far and<br />
receiving this honour is a true accolade.”<br />
Salman joined the ambulance service in 1997<br />
as a paramedic and has kept his paramedic<br />
registration to date. From 2007-2015 he was<br />
head of service development, undertaking<br />
a number of roles transforming services for<br />
patients. This included working with vulnerable<br />
and disadvantaged groups across Greater<br />
Manchester to prevent deaths from drug use.<br />
In addition to this, he provided commander<br />
support in response to two separate major<br />
incidents in Cumbria.<br />
The first incident was the shootings that<br />
occurred in and around Whitehaven in 2010.<br />
The second incident was the major flooding<br />
Salman joined our board of directors in<br />
2016 as director of strategy and planning<br />
and earlier this year, he was appointed as<br />
deputy chief executive of our trust which is<br />
the second-largest ambulance service in the<br />
country.<br />
Salman has worked hard to redress the<br />
balance of representation from ethnic minority<br />
communities within the ambulance sector,<br />
acting as a trailblazer for equity, equality,<br />
and a better understanding of the personal<br />
challenges that can bring. He recently shared<br />
his experiences with over 300 other leaders at<br />
an <strong>Ambulance</strong> Leadership Forum.<br />
Some of the steps he has taken to make<br />
change include being instrumental in supporting<br />
our Race Equality Network, moving it to a more<br />
formal footing, and ensuring its work is focused<br />
and impactful. Salman chairs our Equality,<br />
Diversity, and Inclusion Committee, driving<br />
improvements in the experience of patients<br />
using our services and staff.<br />
Salman’s portfolio includes patient<br />
experience, and he has established our<br />
diverse Patient and Public Panel ensuring<br />
we listen to and learns from the voice of<br />
our communities, from all ages and all<br />
backgrounds. This work enables service<br />
improvement and helps us address the health<br />
inequalities which have increased during the<br />
pandemic.<br />
Chief Executive Daren Mochrie QAM, said:<br />
“Salman is an exceptional and compassionate<br />
leader who always gives freely of his time to<br />
support and mentor individuals, teams, and<br />
peers across all service lines. He has been<br />
instrumental in developing our newly launched<br />
strategy and supporting myself and the<br />
Board to lead the transformation of the trust<br />
especially so during the past few years of a<br />
COVID pandemic.<br />
“He is both a well-respected leader and an<br />
asset to NWAS and the ambulance service<br />
nationally and I am proud of his achievement.”<br />
Congratulations Salman!<br />
After 16 years with Essex & Herts Air<br />
<strong>Ambulance</strong> (EHAAT) Cliff Gale has retired as<br />
Operations Director.<br />
Cliff joined the charity back in 2007, having spent<br />
30 years with Sussex Police where he gained<br />
hands-on experience managing the police air<br />
operation. Since joining EHAAT he has helped<br />
the charity achieve numerous milestones whilst<br />
setting the foundation for its massive growth.<br />
Cliff has been commended by his colleagues<br />
as helping to create clinical governance in prehospital<br />
care in the early days of air ambulance<br />
services. His achievements have been many,<br />
but probably the most notable are, playing an<br />
instrumental role in expanding the charity’s<br />
operations into Hertfordshire, cementing EHAAT’s<br />
future with its airbases at Earls Colne and North<br />
Weald, and purchasing its first owned helicopter.<br />
Cliff won’t be saying ‘goodbye’ completely though,<br />
as he will continue to work with the charity on a<br />
part-time basis to oversee the implementation<br />
of its carbon reduction strategy alongside other<br />
projects. However, he is handing over the<br />
‘operational reins’ to Paul Curtis who becomes<br />
EHAAT’s new Aviation & Operations Director.<br />
Paul has over 25 years in the aviation<br />
industry piloting helicopters for the military, air<br />
ambulances, the police and for the offshore oil<br />
and gas industries. He has also flown for Jet2.<br />
com, flying Boeing 737’s.<br />
Building on the excellent work already achieved,<br />
Paul, as part of the Executive Team, will be<br />
working alongside the whole EHAAT team,<br />
to help achieve its future strategic goals and<br />
ambitious plans to provide the highest possible<br />
standards of pre-hospital care for its patients.<br />
Jane Gurney, CEO of EHAAT said: “We are<br />
thankful for Cliff’s instrumental impact to the<br />
growth of the charity. His passion, energy,<br />
relentless drive and dedication has been clear,<br />
and his impact has been felt throughout the<br />
whole sector. However, I am hugely excited<br />
that someone as experienced as Paul has<br />
joined our team and I know he will do a<br />
fantastic job at guiding the charity through our<br />
next exciting chapter.”<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
27
IN PERSON<br />
EEAST News<br />
Chair of EEAST to step down<br />
after three years<br />
The Chair of the East of England <strong>Ambulance</strong><br />
Service NHS Trust (EEAST) is to step down<br />
after leading the Trust for three years.<br />
Nicola Scrivings joined EEAST in November<br />
2019 after previous roles with a Community<br />
Services NHS Trust, a Cambridge-based<br />
housing association and national roles with the<br />
Audit Commission and the Health and Care<br />
Professions Council (HCPC).<br />
As Chair, Ms Scrivings has overseen a period<br />
of improvement for the Trust, which has been<br />
recognised by the CQC and NHS England.<br />
She has now decided to step down from<br />
the role but will continue in post until her<br />
replacement is recruited.<br />
Ms Scrivings said:<br />
“It has been a great privilege and experience<br />
to travel alongside such dedicated ambulance<br />
crews and volunteers across the region. I know<br />
how hard everybody works to make sure that<br />
our patients receive the best possible care.<br />
“We set ourselves a vision of ‘outstanding<br />
care, excellent people every hour every day’<br />
and I truly believe we are heading in the right<br />
direction under the guidance of our Chief<br />
Executive and the Board. I wish the new Chair<br />
a successful future with EEAST.<br />
“In the meantime, our Board is very focussed<br />
on working with our partners to address<br />
current performance issues.”<br />
This progress has been recognised by the<br />
CQC and NHSE with acknowledgement that<br />
the first phase of EEAST’s progress towards<br />
‘Good’ is drawing to a close. EEAST now has<br />
a stable Board with professional, committed<br />
members, with a range of combined talents to<br />
lead the Trust to the next level.<br />
Tom Abell, Chief Executive of East of England<br />
<strong>Ambulance</strong> Service NHS Trust said:<br />
“Nicola has made an incredible contribution<br />
to our improvement as an organisation, I<br />
would like to thank her for her dedication,<br />
and commitment to making our organisation<br />
a better place to work for our people and her<br />
passion to improve care for the communities<br />
we serve across the east of England.<br />
”Finding the right successor will take a little<br />
time, and there is a plan for a staged transition<br />
to a new Chair, aiming for appointment of<br />
a Chair Designate in May <strong>2023</strong>. Until that<br />
time Nicola will continue to lead the Board<br />
with pride and support the hard work of<br />
ambulance crews on the frontline, including<br />
our volunteers.”<br />
SCAS News<br />
SCAS has announced two<br />
Non-Executive Appointments<br />
to its Board<br />
South Central <strong>Ambulance</strong> Service NHS<br />
Foundation Trust (SCAS) has announced<br />
two new non-executive appointments to its<br />
board of directors.<br />
Mike McEnaney, who comes with 25 years of<br />
finance director level experience, most recently as<br />
finance director for Oxford Health NHS Foundation<br />
Trust where he had additional responsibility for<br />
procurement, IT, HR and estates, began his initial<br />
three-year term on 1 January <strong>2023</strong>.<br />
than a decade of experience in international<br />
healthcare management. He will begin his initial<br />
three-year term on 20 <strong>February</strong> <strong>2023</strong>.<br />
He has been the global medical director of<br />
Marie Stopes International (MSI) Reproductive<br />
Choices <strong>UK</strong> for the last nine years, one of the<br />
largest providers of contraceptive and safe<br />
abortion care services in the world.<br />
He is part of the MSI executive team and<br />
provides professional clinical oversight globally<br />
for the organisation, which has 10,000 staff<br />
with 4,000 clinicians across 37 countries, as<br />
well as operating as a non-executive director<br />
for three countries.<br />
Prior to joining the SCAS Board, Dr Perera was<br />
an associate non-executive director with the<br />
Dorset County Hospital NHS Foundation Trust<br />
and is a member of working groups including<br />
with the World Health Organisation and<br />
International Federation of Obstetricians and<br />
Gynaecologists (FIGO).<br />
Mr McEnaney replaces Mike Hawker who<br />
has retired from SCAS after three terms<br />
of dedicated service as chair of the audit<br />
committee, while Dr Perera replaces Dr<br />
Henrietta Hughes OBE who left SCAS in<br />
September to take on the national role of the<br />
first Patient Safety Commissioner for England.<br />
Professor Sir Keith Willett, SCAS chair, said:<br />
“I am delighted to welcome both Mike and<br />
Dhammika to the SCAS board.<br />
“Mike brings a breadth of experience and<br />
skills which I know will be incredibly useful in<br />
helping SCAS to achieve its ambitions despite<br />
the economic challenges that we are all<br />
facing, while Dhammika has a very interesting<br />
clinical background which brings very valuable<br />
experience to help us as we continue our<br />
improvement journey.”<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
He has also worked in senior manufacturing<br />
and logistics roles for Honda Motor Company<br />
and Avis Plc and has non-executive director<br />
experience as part of the audit committee at<br />
Oxford Brookes University. He also sits on the<br />
finance committee of NHS Providers and the<br />
board of Akrivia Health (a venture with Oxford<br />
University and the NHS).<br />
He is joined by Dr Dhammika Perera, a<br />
public health professional with over 20 years’<br />
experience as a medical doctor and more<br />
Mike McEnaney and Dr Dhammika Perera<br />
28<br />
For more news visit: www.ambulanceukonline.com
IN PERSON<br />
SECAMB News<br />
Trust announces two new<br />
board appointments<br />
South East Coast <strong>Ambulance</strong> Service<br />
NHS Foundation Trust, (SECAmb), has<br />
announced the appointment of two new<br />
Board members.<br />
Joining the executive team as Chief Medical<br />
Officer is Dr Rachel Oaten, while Max Puller<br />
joins the Board as an Independent Non-<br />
Executive Director for an initial term of three<br />
years. Rachel will join the Trust on 1 <strong>February</strong><br />
with Max taking up his role from 6 <strong>February</strong>.<br />
Dr Oaten replaces Dr Fionna Moore on the<br />
SECAmb’s executive team with Dr Moore<br />
stepping down from her role as Medical<br />
Director for the Trust as announced last year<br />
- SECAmb Medical Director to stand down<br />
after 50 years’ NHS service - NHS South East<br />
Coast <strong>Ambulance</strong> Service. While Fionna is<br />
stepping down from our executive role, she will<br />
remain with the Trust in a part-time clinicallyfocused<br />
advisory role.<br />
Dr Oaten, who qualified as Consultant in<br />
Emergency Medicine in 2017, took up a<br />
post at Salisbury Hospital and in 2018 was<br />
appointed the Clinical Lead role for the<br />
Emergency Department. She also held a parttime<br />
post at East Midlands <strong>Ambulance</strong> Service<br />
in March 2020 where she served as Deputy<br />
Medical Director.<br />
In October 2021 she was appointed Deputy<br />
Clinical Director of Medicine at Salisbury<br />
Hospital. She maintains a clinical hands-on<br />
presence as an Emergency Consultant and<br />
also undertakes shifts working as a Trauma<br />
Team Leader.<br />
Dr Oaten said: “It’s important to me that<br />
everybody delivering care at SECAmb<br />
feels supported and knows that they are<br />
working alongside a chief medical officer<br />
who understands the current pressures and<br />
issues faced by staff and who delivers care in<br />
similar circumstances. I am keen to combine<br />
my acute care and pre-hospital experience to<br />
develop collaborative and effective systembased<br />
ways of working for our patients and<br />
staff.”<br />
Max Puller is currently Director at BCW<br />
Change, the organisational change and<br />
employee experience specialists at global<br />
communications agency, BCW. His role<br />
sees him work with global clients to<br />
deliver successful, sustainable business<br />
transformation and culture change.<br />
His previous roles include Head of Colleague<br />
Communications and Engagement at Tesco<br />
Bank, Employee and Change Communications<br />
Director at Sodexo, and Chief Communications<br />
Officer at the <strong>UK</strong> Ministry of Defence. Prior to<br />
his SECAmb appointment, Max was on the<br />
Board of the Salvation Army where he advised<br />
on reputation, marketing and fundraising<br />
issues.<br />
He said: “I am delighted to join the Board of<br />
SECAmb and excited to work with colleagues<br />
across the Trust as we continue on our<br />
improvement journey. I look forward to adding<br />
to the wealth of expertise and experience<br />
already on the Board, as we work together to<br />
drive positive outcomes for staff and patients<br />
across the region.”<br />
SECAmb Interim Chief Executive Siobhan<br />
Melia said: “I’m pleased we have been able to<br />
make these important appointments. Rachel<br />
and Max both bring a wealth of knowledge and<br />
experience from within and from outside the<br />
NHS. They will be made to feel very welcome<br />
at SECAmb and I look forward to working with<br />
them. I would also like to pay tribute to Fionna<br />
as she steps back from her executive role and<br />
thank her for her immense contribution to the<br />
ambulance sector over so many years.”<br />
SECAmb Chairman David Astley said: “I<br />
welcome both Rachel and Max to SECAmb.<br />
They are both strong appointments. I am<br />
pleased that Fionna is retaining a part-time<br />
role. I have always valued her advice to the<br />
Board and I am also grateful for her leadership<br />
as Interim CEO on two occasions in my time<br />
as Chair.”<br />
WAS News<br />
Coveted award for Welsh<br />
<strong>Ambulance</strong> Service<br />
The Welsh <strong>Ambulance</strong> Service won not<br />
one, but two prestigious awards.<br />
The Trust’s Emergency Communication Nurse<br />
System (ECNS) project team were named the<br />
winner of the Digital and Technology Innovation<br />
Award at last week’s Advancing Healthcare<br />
Awards Wales ceremony, while Advanced<br />
Paramedic Practitioner Ed Harry was highly<br />
commended in the Allied Health Professional of<br />
the Year category.<br />
ECNS is a new telephone consultation tool to<br />
help control room clinicians arrange the most<br />
appropriate care for 999 callers.<br />
Ellen Edwards, Senior Practice Educator and<br />
project team member, said: “It was an absolute<br />
honour to win the Advancing Healthcare Award<br />
for Digital and Technology Innovation.<br />
“The implementation of ECNS onto the Clinical<br />
Support Desk has been a challenge, with<br />
winter pressures, mass recruitment and a<br />
condensed timeline.<br />
“But despite all of this, the team have worked<br />
extremely hard, and this is a testament to<br />
that.”<br />
>>><br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
Do you have anything you would like to add or include? Please contact us and let us know.<br />
29
IN PERSON<br />
For the last four and a half years David has<br />
been working as Managing Director at George<br />
Eliot Hospital NHS Trust, Nuneaton, one of<br />
three District General Hospitals that make up<br />
the Foundation Group. Prior to this, David<br />
was Chief Operating Officer at University<br />
Hospitals Coventry and Warwickshire NHS<br />
Trust, during which time he also supported<br />
NHS Improvement Midlands & East, as Senior<br />
Winter Adviser.<br />
David has a particularly strong patient focus,<br />
underpinned by his clinical background and<br />
active nurse registration. His considerable<br />
expertise in system wide urgent and<br />
emergency care will be extremely valuable in<br />
leading SCAS as it seeks to further integrate<br />
health and social care through its key role as<br />
care navigator.<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
On the award, which was sponsored by<br />
the Welsh Government, the judging panel<br />
felt the ECNS project showed “workforce<br />
sustainability, an extremely high impact to<br />
patients and would be of worldwide interest.”<br />
Penny Durrant, Service Manager for the Clinical<br />
Support Desk said: “I am incredibly proud of<br />
all the staff that have made a contribution to us<br />
winning this award.<br />
“There have been significant changes to the<br />
CSD in the last 12 months with the expansion<br />
in clinician numbers, the introduction of the<br />
Mental Health Practitioners and a new way of<br />
working with the implementation of LowCode,<br />
which operates ECNS.<br />
“This award is evidence of the dedication<br />
and hard work of CSD and its continued<br />
commitment to service improvement and<br />
ultimately patient care.”<br />
Advanced Paramedic Practitioner Ed Harry<br />
was also awarded ‘Highly Commended’ in the<br />
Allied Health Professional of the Year category.<br />
He said: “The only other individual who has<br />
been previously shortlisted from WAST for this<br />
award was Andy Swinburn, our Director of<br />
Paramedicine, so I’m just so grateful to even<br />
be nominated, let alone a runner-up.”<br />
Ed started his career as a paramedic in 2009<br />
and is now an APP who supports various<br />
projects and teams including the clinical<br />
support desk, APP training and ECNS, all while<br />
undertaking a PHD.<br />
Kerry Robertshaw, Professional Development<br />
Lead for Advanced Practice, said: “I nominated<br />
Ed, as his enthusiasm is infectious, and he is one<br />
of those people who just goes above and beyond.<br />
“He does so much incredible work in his own<br />
time – down to transformational projects<br />
that he is working on with the college of<br />
paramedics, to his PHD that is looking at<br />
the impact of Covid-19 on the health and<br />
wellbeing of our ambulance staff.<br />
“He’s really keen that our voice is remembered<br />
during this difficult time.”<br />
The Advancing Health Care Awards are held<br />
every year and is an opportunity to recognise<br />
and celebrate the important and innovative<br />
work of healthcare scientists and allied health<br />
professionals across Wales.<br />
SCAS News<br />
South Central <strong>Ambulance</strong><br />
Service appoints new Chief<br />
Executive Officer<br />
Following a robust recruitment process,<br />
South Central <strong>Ambulance</strong> Service NHS<br />
Foundation Trust (SCAS) has appointed<br />
David Eltringham to the role of Chief<br />
Executive Officer, starting in March <strong>2023</strong>.<br />
David said: “I’m delighted to be joining South<br />
Central <strong>Ambulance</strong> Service as its new Chief<br />
Executive. Every part of the NHS is under<br />
significant pressure at the moment and SCAS<br />
is no exception. When I join the Trust in March,<br />
I’ll be focusing on making sure that we look<br />
after our patients and our staff to the highest<br />
standards. I am committed to developing<br />
those around me to be the very best that they<br />
can be. I think that my expertise in this area<br />
will be of great value to SCAS. I met some<br />
fantastic, skilled and committed people during<br />
the recruitment process and I can’t wait to<br />
become part of the team.”<br />
Professor Sir Keith Willett CBE, Chair at<br />
SCAS, added: “I am excited to welcome<br />
David to the SCAS Board. He brings a wealth<br />
of experience, a passion for working with<br />
ambulance services and a strong track record<br />
in service improvement. This will certainly<br />
support SCAS in the delivery of its ambitious<br />
strategy and ultimately in the delivery of the<br />
best possible care for our patients and their<br />
families.”<br />
30<br />
For further recruitment vacancies visit: www.ambulanceukonline.com
COMPANY NEWS<br />
LogRx Offers a<br />
Better Alternative for<br />
Tracking Controlled<br />
Medications<br />
<strong>Ambulance</strong> companies<br />
contracted with NHS<br />
are subject to reporting<br />
controlled medications. We<br />
all know that it’s an arduous<br />
process: pull out the register<br />
after shift and log the<br />
administration of controlled<br />
drugs and other prescriptiononly<br />
medications.<br />
Most of the time, the reporting<br />
process goes smoothly--<br />
emergency responders are<br />
notoriously meticulous. But we’re<br />
also notoriously busy, working<br />
in high-stress environments. So<br />
even when the coolest heads<br />
prevail, the process of pen-andpaper<br />
logging takes valuable time<br />
and leaves room for human error<br />
(and misuse). LogRx offers a<br />
simplified way to easily track with<br />
accuracy.<br />
Paper Tracking Can Result in<br />
Errors<br />
With access to controlled<br />
medicines come regulations<br />
and tracking requirements.<br />
Unfortunately, many organisations<br />
still rely on paper records to<br />
track, carrying a register in the<br />
medicine bag.<br />
In the stress and pressure of<br />
emergency response, people<br />
can, unfortunately, make<br />
intentional and unintentional<br />
mistakes.<br />
Because the Home Office and<br />
Care Quality Commission (CQC)<br />
regulates the specific medications<br />
emergency responders can<br />
carry and administer, especially<br />
controlled medications, they<br />
must be carefully recorded.<br />
Organisations are subject to<br />
periodic inspections to ensure<br />
that their company is in line with<br />
requirements.<br />
Proper recording of drug<br />
inventories helps organisations<br />
ensure there’s enough on hand<br />
and that it’s not expired or<br />
damaged.<br />
Implementing the right systems<br />
will help your team perform at the<br />
highest level. It protects those<br />
in management from breaching<br />
regulations and responders from<br />
questions about misuse. The<br />
right tools also protect patients—<br />
ensuring that paramedics can<br />
access what they need when<br />
they need it.<br />
A Better Solution for Digitally<br />
Tracking Medications<br />
LogRx is an innovative solution to<br />
ensure accuracy in drug tracking.<br />
The software allows responders<br />
to easily log and manage the<br />
medication inventory with their<br />
handheld devices, like phones or<br />
tablets.<br />
With a quick scan using the<br />
device’s camera, LogRx allows<br />
users to record medication<br />
in a digital log. It provides a<br />
groundbreaking solution for NHS<br />
ambulance teams and other<br />
emergency responders. LogRx<br />
doesn’t require special hardware,<br />
and it’s an extremely affordable<br />
option that saves money on<br />
costly errors and time-consuming<br />
reporting.<br />
LogRx is a tamper-evident<br />
system. Labels with purposebuilt<br />
QR codes ensure accurate<br />
tracking. The system is easy<br />
to use, without a high learning<br />
curve for busy teams. If your<br />
team ventures out of a service<br />
area during their work, they can<br />
still use LogRx and upload the<br />
tracking when they return in<br />
range.<br />
LogRx meets the needs of<br />
ambulance services with<br />
accountability, tracking history,<br />
and organisation. It allows<br />
you to access a full view as a<br />
manager, knowing what is being<br />
administered, where, times, GPS<br />
location, and trends—quickly<br />
identify any areas of concern.<br />
LogRx provides a fail-safe report<br />
for expiring drugs, helping<br />
users know when to replenish<br />
stock and manage inventory.<br />
With a glance, you can monitor<br />
the integrity of your medicine<br />
supply. From the administrative<br />
dashboard, many helpful reports<br />
make the jobs of the appointed<br />
medicine leads easier, especially<br />
when it’s time to report to<br />
the Home Office and CQC<br />
inspections. The cloud-based<br />
administrative dashboard makes<br />
it seamless and simple.<br />
The program was developed<br />
by those working in emergency<br />
response. Initially developed<br />
for use in the U.S., the LogRx<br />
team worked with U.K. field<br />
representatives to ensure<br />
compatibility across devices<br />
and platforms. For the last<br />
several years, many ambulance<br />
services that contract with NHS<br />
have successfully used LogRx<br />
to improve accountability and<br />
efficiency, as well as to reduce<br />
staff hours.<br />
LogRx works internationally with<br />
public and private emergency<br />
response organisations,<br />
ambulance services, fire, police,<br />
veterinary medicine, and wildlife<br />
professionals. To learn more<br />
about LogRx medication tracking<br />
for your organisation, visit<br />
LogRx.com.<br />
As with any paper system, there’s<br />
plenty of margin for error. Logs<br />
can get damaged and misplaced.<br />
In the busyness of emergency<br />
response, it’s easy for people to<br />
forget or become hurried in their<br />
recording. Then when it’s time to<br />
turn in the register, it’s difficult to<br />
decipher.<br />
Not to mention that paper<br />
tracking is more challenging<br />
to oversee. This lack of<br />
transparency can allow for<br />
the misuse and theft of drugs.<br />
AMBULANCE <strong>UK</strong> - FEBRUARY<br />
For the latest <strong>Ambulance</strong> Service News visit: www.ambulancenewsdesk.com<br />
31
Improve workflow with the<br />
A complete modular system that can be split into three parts;<br />
Monitor<br />
defibrillator/monitor.<br />
Patient Box<br />
Defibrillator<br />
The corpuls 3 adapts optimally to your needs.<br />
Discover the clinical flexibility in your hands and optimise patient workflow with the unique user<br />
interface of modular or compact mode during patient monitoring and therapy.<br />
• Enhanced patient safety with extensive data storage and data transmission capability throughout<br />
the patient journey with corpuls.mission and corpuls.manager<br />
• Modular design allows for versatility and better ergonomics throughout the patient care pathway.<br />
• Intuitive touch screen monitor with navigation dial option.<br />
www.corpuls.co.uk<br />
www.theortusgroup.com<br />
Official <strong>UK</strong> supplier of corpuls and Weinmann<br />
medical devices and software.