Vol 11-R2- Eyelid
Vol 11-R2- Eyelid
Vol 11-R2- Eyelid
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
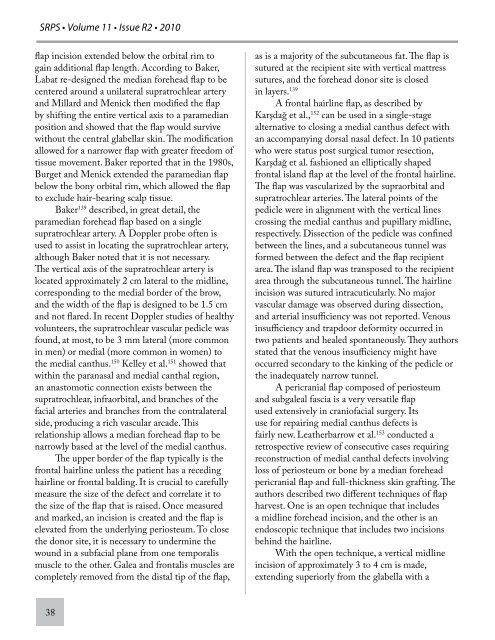
SRPS • <strong>Vol</strong>ume <strong>11</strong> • Issue <strong>R2</strong> • 2010<br />
flap incision extended below the orbital rim to<br />
gain additional flap length. According to Baker,<br />
Labat re-designed the median forehead flap to be<br />
centered around a unilateral supratrochlear artery<br />
and Millard and Menick then modified the flap<br />
by shifting the entire vertical axis to a paramedian<br />
position and showed that the flap would survive<br />
without the central glabellar skin. The modification<br />
allowed for a narrower flap with greater freedom of<br />
tissue movement. Baker reported that in the 1980s,<br />
Burget and Menick extended the paramedian flap<br />
below the bony orbital rim, which allowed the flap<br />
to exclude hair-bearing scalp tissue.<br />
Baker 139 described, in great detail, the<br />
paramedian forehead flap based on a single<br />
supratrochlear artery. A Doppler probe often is<br />
used to assist in locating the supratrochlear artery,<br />
although Baker noted that it is not necessary.<br />
The vertical axis of the supratrochlear artery is<br />
located approximately 2 cm lateral to the midline,<br />
corresponding to the medial border of the brow,<br />
and the width of the flap is designed to be 1.5 cm<br />
and not flared. In recent Doppler studies of healthy<br />
volunteers, the supratrochlear vascular pedicle was<br />
found, at most, to be 3 mm lateral (more common<br />
in men) or medial (more common in women) to<br />
the medial canthus. 150 Kelley et al. 151 showed that<br />
within the paranasal and medial canthal region,<br />
an anastomotic connection exists between the<br />
supratrochlear, infraorbital, and branches of the<br />
facial arteries and branches from the contralateral<br />
side, producing a rich vascular arcade. This<br />
relationship allows a median forehead flap to be<br />
narrowly based at the level of the medial canthus.<br />
The upper border of the flap typically is the<br />
frontal hairline unless the patient has a receding<br />
hairline or frontal balding. It is crucial to carefully<br />
measure the size of the defect and correlate it to<br />
the size of the flap that is raised. Once measured<br />
and marked, an incision is created and the flap is<br />
elevated from the underlying periosteum. To close<br />
the donor site, it is necessary to undermine the<br />
wound in a subfacial plane from one temporalis<br />
muscle to the other. Galea and frontalis muscles are<br />
completely removed from the distal tip of the flap,<br />
38<br />
as is a majority of the subcutaneous fat. The flap is<br />
sutured at the recipient site with vertical mattress<br />
sutures, and the forehead donor site is closed<br />
in layers. 139<br />
A frontal hairline flap, as described by<br />
Karşdağ et al., 152 can be used in a single-stage<br />
alternative to closing a medial canthus defect with<br />
an accompanying dorsal nasal defect. In 10 patients<br />
who were status post surgical tumor resection,<br />
Karşdağ et al. fashioned an elliptically shaped<br />
frontal island flap at the level of the frontal hairline.<br />
The flap was vascularized by the supraorbital and<br />
supratrochlear arteries. The lateral points of the<br />
pedicle were in alignment with the vertical lines<br />
crossing the medial canthus and pupillary midline,<br />
respectively. Dissection of the pedicle was confined<br />
between the lines, and a subcutaneous tunnel was<br />
formed between the defect and the flap recipient<br />
area. The island flap was transposed to the recipient<br />
area through the subcutaneous tunnel. The hairline<br />
incision was sutured intracuticularly. No major<br />
vascular damage was observed during dissection,<br />
and arterial insufficiency was not reported. Venous<br />
insufficiency and trapdoor deformity occurred in<br />
two patients and healed spontaneously. They authors<br />
stated that the venous insufficiency might have<br />
occurred secondary to the kinking of the pedicle or<br />
the inadequately narrow tunnel.<br />
A pericranial flap composed of periosteum<br />
and subgaleal fascia is a very versatile flap<br />
used extensively in craniofacial surgery. Its<br />
use for repairing medial canthus defects is<br />
fairly new. Leatherbarrow et al. 153 conducted a<br />
retrospective review of consecutive cases requiring<br />
reconstruction of medial canthal defects involving<br />
loss of periosteum or bone by a median forehead<br />
pericranial flap and full-thickness skin grafting. The<br />
authors described two different techniques of flap<br />
harvest. One is an open technique that includes<br />
a midline forehead incision, and the other is an<br />
endoscopic technique that includes two incisions<br />
behind the hairline.<br />
With the open technique, a vertical midline<br />
incision of approximately 3 to 4 cm is made,<br />
extending superiorly from the glabella with a