sign130
sign130
sign130
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
1.3.3 BRAIN INjURy SEVERITy<br />
Long term prognosis in people with brain injuries correlates to different extents with various factors including<br />
levels of consciousness, duration of post-traumatic amnesia, age, gender and pre-injury education and<br />
employment. The most widely used index of injury severity is the Glasgow Coma Score (GCS) which classifies<br />
injuries into mild, moderate or severe categories based on level of consciousness post injury (see Table 1). It<br />
should be noted that severity of symptoms associated with an injury may not correlate perfectly with severity<br />
of injury as defined by GCS, so that patients with a severe brain injury may experience many of the same<br />
symptoms as patients with a mild injury, although these may be longer lasting or result in greater disability.<br />
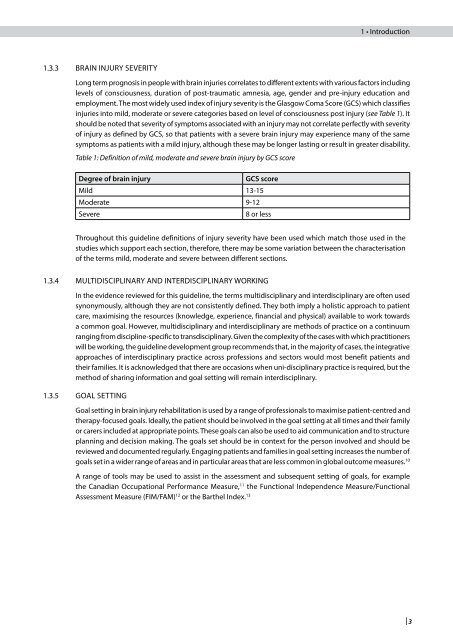
Table 1: Definition of mild, moderate and severe brain injury by GCS score<br />
Degree of brain injury GCS score<br />
Mild 13-15<br />
Moderate 9-12<br />
Severe 8 or less<br />
Throughout this guideline definitions of injury severity have been used which match those used in the<br />
studies which support each section, therefore, there may be some variation between the characterisation<br />
of the terms mild, moderate and severe between different sections.<br />
1.3.4 MULTIDISCIPLINARy AND INTERDISCIPLINARy WORkING<br />
In the evidence reviewed for this guideline, the terms multidisciplinary and interdisciplinary are often used<br />
synonymously, although they are not consistently defined. They both imply a holistic approach to patient<br />
care, maximising the resources (knowledge, experience, financial and physical) available to work towards<br />
a common goal. However, multidisciplinary and interdisciplinary are methods of practice on a continuum<br />
ranging from discipline-specific to transdisciplinary. Given the complexity of the cases with which practitioners<br />
will be working, the guideline development group recommends that, in the majority of cases, the integrative<br />
approaches of interdisciplinary practice across professions and sectors would most benefit patients and<br />
their families. It is acknowledged that there are occasions when uni-disciplinary practice is required, but the<br />
method of sharing information and goal setting will remain interdisciplinary.<br />
1.3.5 GOAL SETTING<br />
1 • Introduction<br />
Goal setting in brain injury rehabilitation is used by a range of professionals to maximise patient-centred and<br />
therapy-focused goals. Ideally, the patient should be involved in the goal setting at all times and their family<br />
or carers included at appropriate points. These goals can also be used to aid communication and to structure<br />
planning and decision making. The goals set should be in context for the person involved and should be<br />
reviewed and documented regularly. Engaging patients and families in goal setting increases the number of<br />
goals set in a wider range of areas and in particular areas that are less common in global outcome measures. 10<br />
A range of tools may be used to assist in the assessment and subsequent setting of goals, for example<br />
the Canadian Occupational Performance Measure, 11 the Functional Independence Measure/Functional<br />
Assessment Measure (FIM/FAM) 12 or the Barthel Index. 13<br />
| 3