Second branchial cyst in the parapharyngealspace - Université de ...
Second branchial cyst in the parapharyngealspace - Université de ...
Second branchial cyst in the parapharyngealspace - Université de ...
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
ANL-1153; No of Pages 4<br />
2<br />
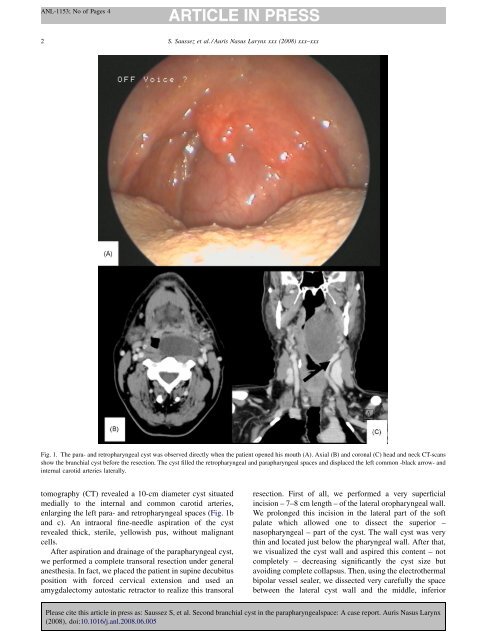
tomography (CT) revealed a 10-cm diameter <strong>cyst</strong> situated<br />
medially to <strong>the</strong> <strong>in</strong>ternal and common carotid arteries,<br />
enlarg<strong>in</strong>g <strong>the</strong> left para- and retropharyngeal spaces (Fig. 1b<br />
and c). An <strong>in</strong>traoral f<strong>in</strong>e-needle aspiration of <strong>the</strong> <strong>cyst</strong><br />
revealed thick, sterile, yellowish pus, without malignant<br />
cells.<br />
After aspiration and dra<strong>in</strong>age of <strong>the</strong> parapharyngeal <strong>cyst</strong>,<br />
we performed a complete transoral resection un<strong>de</strong>r general<br />
anes<strong>the</strong>sia. In fact, we placed <strong>the</strong> patient <strong>in</strong> sup<strong>in</strong>e <strong>de</strong>cubitus<br />
position with forced cervical extension and used an<br />
amygdalectomy autostatic retractor to realize this transoral<br />
S. Saussez et al. / Auris Nasus Larynx xxx (2008) xxx–xxx<br />
Fig. 1. The para- and retropharyngeal <strong>cyst</strong> was observed directly when <strong>the</strong> patient opened his mouth (A). Axial (B) and coronal (C) head and neck CT-scans<br />
show <strong>the</strong> <strong>branchial</strong> <strong>cyst</strong> before <strong>the</strong> resection. The <strong>cyst</strong> filled <strong>the</strong> retropharyngeal and parapharyngeal spaces and displaced <strong>the</strong> left common -black arrow- and<br />
<strong>in</strong>ternal carotid arteries laterally.<br />
resection. First of all, we performed a very superficial<br />
<strong>in</strong>cision – 7–8 cm length – of <strong>the</strong> lateral oropharyngeal wall.<br />
We prolonged this <strong>in</strong>cision <strong>in</strong> <strong>the</strong> lateral part of <strong>the</strong> soft<br />
palate which allowed one to dissect <strong>the</strong> superior –<br />
nasopharyngeal – part of <strong>the</strong> <strong>cyst</strong>. The wall <strong>cyst</strong> was very<br />
th<strong>in</strong> and located just below <strong>the</strong> pharyngeal wall. After that,<br />
we visualized <strong>the</strong> <strong>cyst</strong> wall and aspired this content – not<br />
completely – <strong>de</strong>creas<strong>in</strong>g significantly <strong>the</strong> <strong>cyst</strong> size but<br />
avoid<strong>in</strong>g complete collapsus. Then, us<strong>in</strong>g <strong>the</strong> electro<strong>the</strong>rmal<br />
bipolar vessel sealer, we dissected very carefully <strong>the</strong> space<br />
between <strong>the</strong> lateral <strong>cyst</strong> wall and <strong>the</strong> middle, <strong>in</strong>ferior<br />
Please cite this article <strong>in</strong> press as: Saussez S, et al. <strong>Second</strong> <strong>branchial</strong> <strong>cyst</strong> <strong>in</strong> <strong>the</strong> <strong>parapharyngealspace</strong>: A case report. Auris Nasus Larynx<br />
(2008), doi:10.1016/j.anl.2008.06.005