Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
British Journal of Ophthalmology 1996; 80: 267-269<br />
LETTERS TO THE EDITOR<br />
<strong>Benign</strong> <strong>fleck</strong> <strong>retina</strong><br />
EDITOR,-We report a case of <strong>fleck</strong>ed <strong>retina</strong>l<br />
dystrophy in a child of mixed Australian aboriginal<br />
and white descent. Both fundi showed<br />
widespread discrete yellow-white <strong>fleck</strong> lesions<br />
at the level of <strong>retina</strong>l pigment epithelium,<br />
extending to the far periphery but sparing the<br />
macular region. Visual acuity was normal and<br />
the electroretinogram showed no abnormality.<br />
To our knowledge no other family members<br />
are affected, and there is no history of<br />
consanguinity between the parents. The phenotype<br />
appears similar to the 'benign familial<br />
<strong>fleck</strong> <strong>retina</strong>' described by Aish and Dajani,1<br />
and we believe this to be the first published<br />
report of such a case since the original<br />
description in 1980.<br />
CASE REPORT<br />
A 12-year-old girl was referred after her<br />
optometrist noted areas of <strong>retina</strong>l abnormality<br />
on ophthalmoscopy after a routine refraction.<br />
She complained of occasional headaches, but<br />
had no specific ocular symptoms and was in<br />
good general health. Drug or substance abuse<br />
was denied. There was no history of maternal<br />
illness or nutritional deficiency during pregnancy,<br />
and the patient was born at full term.<br />
Visual and general development were reportedly<br />
normal during infancy and early childhood,<br />
and the mother noted no signs of poor<br />
daytime or night vision in any of her three<br />
children.<br />
The child was of mixed ethnic origin, the<br />
non-consanguineous parents both being of<br />
mixed Australian aboriginal and white<br />
descent, and there was no family history of<br />
ocular or systemic disease other than the<br />
recent development of maturity onset diabetes<br />
mellitus in the mother.<br />
General examination found no evidence of<br />
skin depigmentation or vitiligo. Visual<br />
acuities were 6/9 right with +0 50 DS/- 1-00<br />
DCX 180 degrees, 6/6 left with +0 50 DS.<br />
Slit-lamp examination of anterior segments<br />
and vitreous was normal. Funduscopy<br />
revealed a striking pattern of multiple yellowwhite<br />
<strong>fleck</strong>s situated at a level deep to the <strong>retina</strong>l<br />
vessels, affecting both fundi in a<br />
symmetrical pattern (Fig 1). The lesions were<br />
distributed in a concentric pattern around the<br />
posterior fundus but sparing the optic disc,<br />
papillomacular bundle, and the peripapillary<br />
area for a distance of 1 disc diameter except<br />
inferiorly, where there was involvement to the<br />
margin of the optic disc. No part of the equatorial,<br />
peripheral, or far peripheral <strong>retina</strong> was<br />
spared. The shape of the <strong>fleck</strong>s was highly<br />
variable. The most centrally located lesions<br />
were roughly round or oblong in shape, and<br />
approximately the diameter of a third order<br />
arteriole. With increasing distance from the<br />
central macula, the <strong>fleck</strong>s tended to become<br />
much larger and confluent, up to 1/2 disc<br />
diameter in size across the largest dimension.<br />
The more peripheral <strong>fleck</strong>s showed greater<br />
variability in shape, with linear, geographical,<br />
or amoeboid outlines and smooth sinuous<br />
margins. On stereoscopic slit-lamp biomicroscopy,<br />
the <strong>fleck</strong> lesions appeared flat, with<br />
no evidence of accumulated material within<br />
or anterior to <strong>retina</strong>l pigment epithelial cells.<br />
There was no evidence of pigment migration,<br />
although several of the larger lesions enclosed<br />
areas of normnally pigmented <strong>retina</strong>, giving the<br />
Downloaded from<br />
bjo.bmj.com on July 1, 2013 - Published by group.bmj.com<br />
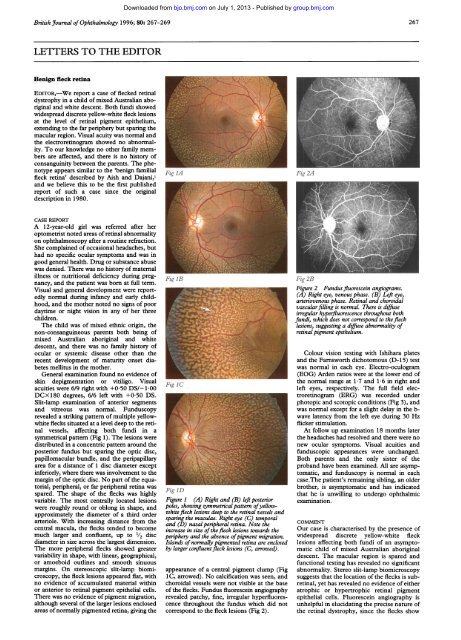
Fig IA Fig 2A<br />
Fig 11 Pig 2B<br />
Figure 2 Fundusfluorescein angiograms.<br />
(A) Right eye, venous phase. (B) Left eye,<br />
arteriovenous phase. Retinal and choroidal<br />
vascularfilling is normal. There is diffuse<br />
irregular hyperfluorescence throughout both<br />
fundi, which does not correspond to the <strong>fleck</strong><br />
lesions, suggesting a diffuse abnormality of<br />
<strong>retina</strong>l pigment epithelium.<br />
Fig IC<br />
Fig ID<br />
Figure 1 (A) Right and (B) left posterior<br />
poles, showing symmetrical pattern ofyellowwhite<br />
<strong>fleck</strong> lesions deep to the <strong>retina</strong>l vessels and<br />
sparing the maculae. Right eye (C) temporal<br />
and (D) nasal peripheral <strong>retina</strong>. Note the<br />
increase in size of the<strong>fleck</strong> lesions towards the<br />
periphery and the absence ofpigment migration.<br />
Islands of normally pigmented <strong>retina</strong> are enclosed<br />
by larger confluent<strong>fleck</strong> lesions (C, arrowed).<br />
appearance of a central pigment clump (Fig<br />
1C, arrowed). No calcification was seen, and<br />
choroidal vessels were not visible at the base<br />
of the <strong>fleck</strong>s. Fundus fluorescein angiography<br />
revealed patchy, fine, irregular hyperfluorescence<br />
throughout the fundus which did not<br />
correspond to the <strong>fleck</strong> lesions (Fig 2).<br />
267<br />
Colour vision testing with Ishihara plates<br />
and the Farnsworth dichotomous (D- 15) test<br />
was normal in each eye. Electro-oculogram<br />
(EOG) Arden ratios were at the lower end of<br />
the normal range at 1-7 and 1-6 in right and<br />
left eyes, respectively. The full field electroretinogram<br />
(ERG) was recorded under<br />
photopic and scotopic conditions (Fig 3), and<br />
was normal except for a slight delay in the bwave<br />
latency from the left eye during 30 Hz<br />
flicker stimulation.<br />
At follow up examination 18 months later<br />
the headaches had resolved and there were no<br />
new ocular symptoms. Visual acuities and<br />
funduscopic appearances were unchanged.<br />
Both parents and the only sister of the<br />
proband have been examined. All are asymptomatic,<br />
and funduscopy is normal in each<br />
case.The patient's remaining sibling, an older<br />
brother, is asymptomatic and has indicated<br />
that he is unwilling to undergo ophthalmic<br />
examination.<br />
COMMENT<br />
Our case is characterised by the presence of<br />
widespread discrete yellow-white <strong>fleck</strong><br />
lesions affecting both fundi of an asymptomatic<br />
child of mixed Australian aboriginal<br />
descent. The macular region is spared and<br />
functional testing has revealed no significant<br />
abnormality. Stereo slit-lamp biomicroscopy<br />
suggests that the location of the <strong>fleck</strong>s is sub<strong>retina</strong>l,<br />
yet has revealed no evidence of either<br />
atrophic or hypertrophic <strong>retina</strong>l pigment<br />
epithelial cells. Fluorescein angiography is<br />
unhelpful in elucidating the precise nature of<br />
the <strong>retina</strong>l dystrophy, since the <strong>fleck</strong>s show
268<br />
Z A B<br />
_- +<br />
400<br />
D 200<br />
(0<br />
0 0<br />
z<br />
' -200<br />
-400<br />
200<br />
D 100<br />
0)<br />
0 0<br />
z<br />
C-100<br />
-200<br />
Z A B<br />
L+A in<br />
White light scotopic stimulation<br />
Right eye<br />
[9, GY1867. V12]<br />
10 sweeps<br />
Z<br />
400 r-<br />
A EB<br />
200<br />
-200<br />
-400 _<br />
White light photopic stimulation<br />
[11, GY1867. V12]<br />
10 sweeps<br />
100 ms<br />
0<br />
Z A B I<br />
200 r<br />
100<br />
0<br />
-100<br />
-200 _<br />
*- i \<br />
Figure 3 Fullfield Ganzfeld electroretinogram (ERG). Upper traces show scotopic ERG elicited by<br />
a single whiteflash in the dark adapted eye: A-wave latency 25-5 ms RE, 2517 ms LE (normal range<br />
24-4-28-1 ms), amplitude 121-0 ,uVRE, 131-0 ,AVLE (normal range 561-1-85-2 pV). B-wave<br />
latency 48-0 ms RE, 47-8 ms LE (43-8-53-1 ms) and amplitude 548-0 ,uVPRE, 616-0 ,uVLE<br />
(348-0-679-6 p.V'). Lower traces show photopic ERG response to a single white flash: A-wave<br />
latency 16-6 ms in each eye (normal range 16-5-18-9 ms) and amplitude 27-0 ,uVRE, 28-0 p.V<br />
LE. B-wave latency 30-7 ms RE, 31-0 ms LE (27-5-31-8 ms)and amplitude 121-0 puVRE, 151-0<br />
,uVLE (39-1-207-1 ttf'). All normal range values represent mean (2 SD).<br />
neither a 'window defect' suggesting depigmentation,<br />
nor hypofluorescence, which<br />
might suggest an abnormal accumulation<br />
of material within <strong>retina</strong>l pigment epithelium<br />
cells. Instead, the mild generalised<br />
irregular hyperfluorescence suggests merely<br />
a diffuse abnormality of <strong>retina</strong>l pigment<br />
epithelium.<br />
The occurrence of a marbelised fundus in<br />
asymptomatic patients is rare. Aish and<br />
Dajani have described an Arab Palestinian<br />
family with clinical features which appear to<br />
closely resemble those of our patient.' In this<br />
pedigree, the parents were phenotypically<br />
normal first cousins. Seven out of 10 of their<br />
offspring showed massive invasion of both<br />
fundi by bright white or yellow <strong>fleck</strong> lesions<br />
situated behind the <strong>retina</strong>l blood vessels, and<br />
always sparing the macula. Visual findings<br />
were normal in all cases. The probable mode<br />
of inheritance within this family was autosomal<br />
recessive, since both sexes were involved,<br />
and the consanguineous parents were unaffected.<br />
Krogh et al have described an asymptomatic<br />
31-year-old woman with normal<br />
visual acuity, with bilateral <strong>retina</strong>l <strong>fleck</strong>s in the<br />
mid periphery of both eyes.2 The <strong>fleck</strong>s<br />
became more dense in the periphery, where<br />
they formed a palisade pattern quite unlike<br />
that of our case. Functional testing revealed<br />
an absent EOG light rise in one eye but was<br />
otherwise normal. More recently, a case of<br />
bilateral 'breadcrumb' <strong>fleck</strong>ed retinopathy<br />
with normal fluorescein angiography and<br />
normal electrophysiological findings has been<br />
reported in a 9-year-old girl. However, this<br />
child also had an idiopathic seizure disorder<br />
which had been controlled medically for 6<br />
years, subnormal intelligence, gross motor<br />
and developmental delay, and esotropia.3 The<br />
size and shape of the <strong>retina</strong>l <strong>fleck</strong>s in this case<br />
are not described in detail, but the published<br />
photographs appear to demonstrate a more<br />
uniform size and more irregular margins to<br />
the <strong>fleck</strong>s than in our patient, with a more<br />
linear distribution of <strong>fleck</strong>s and a greater<br />
area of normal appearing <strong>retina</strong> between the<br />
<strong>fleck</strong>s.<br />
A marbelised fundus appearance has also<br />
been reported as a rare finding in Leber's<br />
congenital amaurosis.46 In this variant,<br />
Downloaded from<br />
bjo.bmj.com on July 1, 2013 - Published by group.bmj.com<br />
yellowish lesions are seen deep to the <strong>retina</strong>l<br />
vessels in a periarteriolar distribution, and<br />
there may be associated systemic abnormalities,<br />
including medullary cystic renal disease<br />
(juvenile nephronophthisis).7 The other clinical<br />
features and absent ERG response of<br />
Leber's amaurosis make confusion with our<br />
case unlikely. However, it is interesting to<br />
note in such cases that a marbelised fundus<br />
may be incidental to visual functional abnormalities.<br />
We suggest that our case represents either<br />
a new mutation of the condition described,<br />
or possibly an autosomal recessive disorder,<br />
since both parents are phenotypically<br />
normal.<br />
We wish to thank the Department of Medical<br />
Technology and Physics, Sir Charles Gairdner<br />
Hospital, for performing the electrophysiological<br />
testing.<br />
TIMOTHY W ISAACS<br />
IAN L McALLISTER<br />
MATTHEW S WADE<br />
Department of Ophthalmology,<br />
Royal Perth Hospital,<br />
Wellington Street,<br />
Perth, Western Australia 6001,<br />
Australia<br />
Correspondence to: Mr Timothy W Isaacs, Lions<br />
Eye Institute, 2 Verdun Street, Nedlands, Western<br />
Australia, WA 6009, Australia.<br />
Accepted for publication 11 October 1995<br />
1 Aish SFS, Dajani B. <strong>Benign</strong> familial <strong>fleck</strong> <strong>retina</strong>.<br />
BrJ Ophthalmol 1980; 64: 652-9.<br />
2 Krogh E, Reersted P, Holm K. Flecked <strong>retina</strong><br />
syndrome with palisade appearance in the<br />
periphery. A case study with a family investigation.<br />
Int Ophthalmol 1980; 2: 77-80.<br />
3 Protzko EE, Schatz H, Raymond WR 4th,<br />
McDonald HR, Johnson RN. Bread crumb<strong>fleck</strong>ed<br />
retinopathy. Retina 1992; 12: 21-3.<br />
4 Franceschetti A, Forni S. Degenerescence tapetoretinienne<br />
(type Leber) avec aspect marbre du<br />
fond de l'oeil peripherique. Ophtalmologica<br />
1958; 135: 610-8.<br />
5 Chew E, Deutman A, Pinckers A, Aan De Kerk<br />
A. Yellowish <strong>fleck</strong>s in Leber's congenital<br />
amaurosis. BrJ_ Ophthalmol 1984; 68: 727-31.<br />
6 Schroeder R, Mets MB, Maumenee IH. Leber's<br />
congenital amaurosis. Retrospective review of<br />
43 cases and a new fundus finding in two cases.<br />
Arch Ophthalmol 1987; 105: 356-9.<br />
7 Ticho B, Sieving PA. Leber's congenital amaurosis<br />
with marbelized fundus and juvenile<br />
nephronophthisis. Am Ophthalmol 1989; 107:<br />
426-8.<br />
Letters<br />
Brown's syndrome as a complication of<br />
Left eye I<br />
r. ,,% %, I- - -- t 1. -1<br />
19, GY1867. V12I<br />
cardiopulmonary resuscitation<br />
EDITOR,-Brown's syndrome is a well<br />
150 ms<br />
[1 GY1867. Vl12]<br />
100 ms<br />
_ I<br />
recognised ocular motility disorder which may<br />
be congenital or acquired. Regardless of<br />
aetiology it manifests itself clinically with<br />
restriction to both active and passive elevation<br />
in adduction, minimal or only slight limitation<br />
to elevation in abduction, occasionally a<br />
downshoot of the affected eye in adduction<br />
and, in more severely affected cases, a primary<br />
position hypotropia with an associated abnormal<br />
head posture. The head posture consists<br />
of a chin-up head position with a face turned<br />
away from the affected side or a variable head<br />
tilt. Other features less commonly seen are a<br />
'V' pattern resulting from divergence in<br />
upgaze and widening of the palpebral fissure<br />
on adduction.1<br />
CASE REPORT<br />
We report a case of acquired Brown's syndrome<br />
in a 2-year-old girl without a history of<br />
ocular motility defects, who accidentally fell<br />
into the family swimming pool and was found<br />
cyanotic, face down in the water. Her mother,<br />
trained in cardiopulmonary resuscitation,<br />
rescued her from the pool and successfully<br />
resuscitated her using nasal compression,<br />
mouth to mouth ventilation, and cardiac<br />
massage. The patient was transferred to the<br />
Children's Hospital of Pittsburgh and, after a<br />
short period of artificial ventilation, made a<br />
full recovery. A computed tomography brain<br />
scan did not reveal any abnormality.<br />
After hospitalisation it was noted that the<br />
child had developed a mild chin-up head<br />
posture. One week later her vision was 20/30<br />
in each eye using Allen figures, she was<br />
orthophoric in the primary position of gaze,<br />
had a chin-up head posture without head tilt<br />
or face turn, and ocular versions revealed<br />
limitation of elevation in adduction (Fig 1).<br />
There was no evidence of superior oblique<br />
muscle overaction or downshoot in adduction.<br />
In addition, the right superior rectus<br />
muscle did not demonstrate overaction and<br />
there was some divergence in upgaze which<br />
helped to differentiate this entity from an isolated<br />
left inferior oblique paresis. She demonstrated<br />
100 seconds of arc stereoacuity and<br />
had normal fusion for both distance and near<br />
using the Worth 4 dot test in the primary<br />
position of gaze. Magnetic resonance imaging<br />
of the orbits was normal and did not reveal<br />
any evidence of trochlear disinsertion or<br />
swelling. The orbital floor was intact. When<br />
the patient was considered sufficiently mature<br />
we performed forced duction testing under<br />
local anaesthesia which confirmed the diagnosis.<br />
The patient was 3 years old at this time.<br />
We did not feel it necessary to subject the<br />
patient to general anaesthesia when she first<br />
presented in order to confirm the diagnosis,<br />
particularly in light of her near drowning<br />
event.<br />
This patient has been followed for 18<br />
months and the restriction to elevation in<br />
adduction has improved significantly. As the<br />
patient did not have a significant head tilt and<br />
was orthophoric in primary position surgical<br />
intervention was not required.<br />
COMMENT<br />
Acquired Brown's syndrome has been<br />
reported following traumatic events occurring<br />
in the region of the trochlea; these include<br />
peribulbar anaesthesia,2 orbital surgery,3<br />
orbital roof fracture with superior oblique
Email alerting<br />
service<br />
Notes<br />
<strong>Benign</strong> <strong>fleck</strong> <strong>retina</strong>.<br />
T W Isaacs, I L McAllister and M S Wade<br />
Br J Ophthalmol 1996 80: 267-268<br />
doi: 10.1136/bjo.80.3.267<br />
Updated information and services can be found at:<br />
http://bjo.bmj.com/content/80/3/267.citation<br />
These include:<br />
To request permissions go to:<br />
http://group.bmj.com/group/rights-licensing/permissions<br />
To order reprints go to:<br />
http://journals.bmj.com/cgi/reprintform<br />
To subscribe to BMJ go to:<br />
http://group.bmj.com/subscribe/<br />
Downloaded from<br />
bjo.bmj.com on July 1, 2013 - Published by group.bmj.com<br />
Receive free email alerts when new articles cite this article. Sign up in<br />
the box at the top right corner of the online article.