Download the PDF
Download the PDF
Download the PDF
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ot<br />
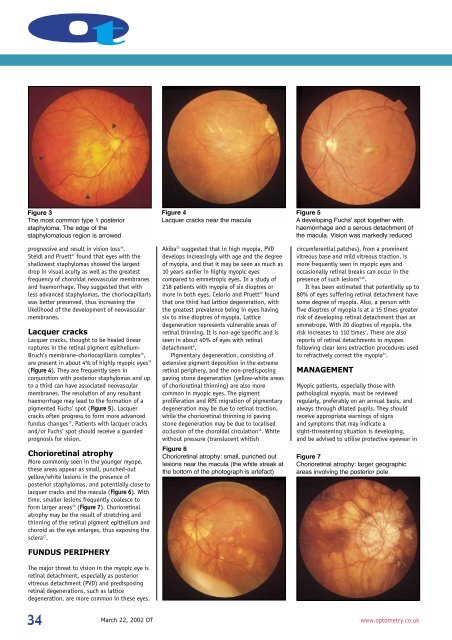
Figure 3<br />
The most common type 1 posterior<br />
staphyloma. The edge of <strong>the</strong><br />
staphylomatous region is arrowed<br />
progressive and result in vision loss 16 .<br />
Steidl and Pruett 17 found that eyes with <strong>the</strong><br />
shallowest staphylomas showed <strong>the</strong> largest<br />
drop in visual acuity as well as <strong>the</strong> greatest<br />
frequency of choroidal neovascular membranes<br />
and haemorrhage. They suggested that with<br />
less advanced staphylomas, <strong>the</strong> choriocapillaris<br />
was better preserved, thus increasing <strong>the</strong><br />
likelihood of <strong>the</strong> development of neovascular<br />
membranes.<br />
Lacquer cracks<br />
Lacquer cracks, thought to be healed linear<br />
ruptures in <strong>the</strong> retinal pigment epi<strong>the</strong>lium-<br />
Bruch’s membrane-choriocapillaris complex 18 ,<br />
are present in about 4% of highly myopic eyes 19<br />
(Figure 4). They are frequently seen in<br />
conjunction with posterior staphylomas and up<br />
to a third can have associated neovascular<br />
membranes. The resolution of any resultant<br />
haemorrhage may lead to <strong>the</strong> formation of a<br />
pigmented Fuchs’ spot (Figure 5). Lacquer<br />
cracks often progress to form more advanced<br />
fundus changes 19 . Patients with lacquer cracks<br />
and/or Fuchs’ spot should receive a guarded<br />
prognosis for vision.<br />
Chorioretinal atrophy<br />
More commonly seen in <strong>the</strong> younger myope,<br />
<strong>the</strong>se areas appear as small, punched-out<br />
yellow/white lesions in <strong>the</strong> presence of<br />
posterior staphylomas, and potentially close to<br />
lacquer cracks and <strong>the</strong> macula (Figure 6). With<br />
time, smaller lesions frequently coalesce to<br />
form larger areas 20 (Figure 7). Chorioretinal<br />
atrophy may be <strong>the</strong> result of stretching and<br />
thinning of <strong>the</strong> retinal pigment epi<strong>the</strong>lium and<br />
choroid as <strong>the</strong> eye enlarges, thus exposing <strong>the</strong><br />
sclera 21 .<br />
FUNDUS PERIPHERY<br />
The major threat to vision in <strong>the</strong> myopic eye is<br />
retinal detachment, especially as posterior<br />
vitreous detachment (PVD) and predisposing<br />
retinal degenerations, such as lattice<br />
degeneration, are more common in <strong>the</strong>se eyes.<br />
Figure 4<br />
Lacquer cracks near <strong>the</strong> macula<br />
Akiba 22 suggested that in high myopia, PVD<br />
develops increasingly with age and <strong>the</strong> degree<br />
of myopia, and that it may be seen as much as<br />
10 years earlier in highly myopic eyes<br />
compared to emmetropic eyes. In a study of<br />
218 patients with myopia of six dioptres or<br />
more in both eyes, Celorio and Pruett 23 found<br />
that one third had lattice degeneration, with<br />
<strong>the</strong> greatest prevalence being in eyes having<br />
six to nine dioptres of myopia. Lattice<br />
degeneration represents vulnerable areas of<br />
retinal thinning. It is non-age specific and is<br />
seen in about 40% of eyes with retinal<br />
detachment 9 .<br />
Pigmentary degeneration, consisting of<br />
extensive pigment deposition in <strong>the</strong> extreme<br />
retinal periphery, and <strong>the</strong> non-predisposing<br />
paving stone degeneration (yellow-white areas<br />
of chorioretinal thinning) are also more<br />
common in myopic eyes. The pigment<br />
proliferation and RPE migration of pigmentary<br />
degeneration may be due to retinal traction,<br />
while <strong>the</strong> chorioretinal thinning in paving<br />
stone degeneration may be due to localised<br />
occlusion of <strong>the</strong> choroidal circulation 16 . White<br />
without pressure (translucent whitish<br />
Figure 6<br />
Chorioretinal atrophy: small, punched out<br />
lesions near <strong>the</strong> macula (<strong>the</strong> white streak at<br />
<strong>the</strong> bottom of <strong>the</strong> photograph is artefact)<br />
Figure 5<br />
A developing Fuchs’ spot toge<strong>the</strong>r with<br />
haemorrhage and a serous detachment of<br />
<strong>the</strong> macula. Vision was markedly reduced<br />
circumferential patches), from a prominent<br />
vitreous base and mild vitreous traction, is<br />
more frequently seen in myopic eyes and<br />
occasionally retinal breaks can occur in <strong>the</strong><br />
presence of such lesions 9,16 .<br />
It has been estimated that potentially up to<br />
80% of eyes suffering retinal detachment have<br />
some degree of myopia. Also, a person with<br />
five dioptres of myopia is at a 15 times greater<br />
risk of developing retinal detachment than an<br />
emmetrope. With 20 dioptres of myopia, <strong>the</strong><br />
risk increases to 110 times 7 . There are also<br />
reports of retinal detachments in myopes<br />
following clear lens extraction procedures used<br />
to refractively correct <strong>the</strong> myopia 24 .<br />
MANAGEMENT<br />
Myopic patients, especially those with<br />
pathological myopia, must be reviewed<br />
regularly, preferably on an annual basis, and<br />
always through dilated pupils. They should<br />
receive appropriate warnings of signs<br />
and symptoms that may indicate a<br />
sight-threatening situation is developing,<br />
and be advised to utilise protective eyewear in<br />
Figure 7<br />
Chorioretinal atrophy: larger geographic<br />
areas involving <strong>the</strong> posterior pole<br />
34<br />
March 22, 2002 OT<br />
www.optometry.co.uk