Download the PDF
Download the PDF
Download the PDF
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
Peter G. Swann BSc (Hons), MAppSc, FCOptom, FAAO and Katrina L. Schmid BAppSc (Optom) (Hons), GradCertEd (Higher Ed), PhD<br />
Fundus changes in myopia<br />
An overview<br />
Myopia is <strong>the</strong> most common of <strong>the</strong><br />
refractive errors. Due to this, and <strong>the</strong><br />
fact that many patients have a<br />
relatively low degree of myopia, with<br />
no deleterious ocular changes, <strong>the</strong>re<br />
is perhaps a tendency to regard<br />
myopia as a simple refractive<br />
condition without considering <strong>the</strong><br />
serious visual problems which can<br />
arise. This article describes <strong>the</strong><br />
changes which can occur in <strong>the</strong><br />
ocular fundus due to axial myopia. A<br />
treatment to slow or arrest <strong>the</strong> axial<br />
elongation of <strong>the</strong> eye and, thus, <strong>the</strong>se<br />
complications is required. Band-aid<br />
approaches such as spectacles or<br />
refractive surgery, which do not<br />
prevent <strong>the</strong> elongation of <strong>the</strong> eye, will<br />
have no beneficial effect in terms of<br />
preventing such consequences.<br />
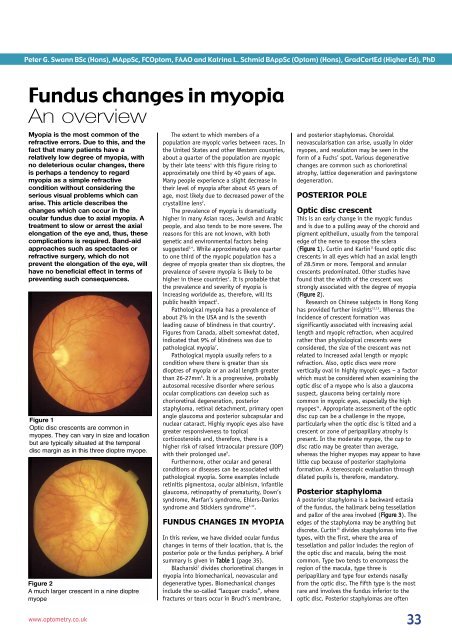
Figure 1<br />
Optic disc crescents are common in<br />
myopes. They can vary in size and location<br />
but are typically situated at <strong>the</strong> temporal<br />
disc margin as in this three dioptre myope.<br />
Figure 2<br />
A much larger crescent in a nine dioptre<br />
myope<br />
The extent to which members of a<br />
population are myopic varies between races. In<br />
<strong>the</strong> United States and o<strong>the</strong>r Western countries,<br />
about a quarter of <strong>the</strong> population are myopic<br />
by <strong>the</strong>ir late teens 1 with this figure rising to<br />
approximately one third by 40 years of age.<br />
Many people experience a slight decrease in<br />
<strong>the</strong>ir level of myopia after about 45 years of<br />
age, most likely due to decreased power of <strong>the</strong><br />
crystalline lens 2 .<br />
The prevalence of myopia is dramatically<br />
higher in many Asian races, Jewish and Arabic<br />
people, and also tends to be more severe. The<br />
reasons for this are not known, with both<br />
genetic and environmental factors being<br />
suggested 3,4 . While approximately one quarter<br />
to one third of <strong>the</strong> myopic population has a<br />
degree of myopia greater than six dioptres, <strong>the</strong><br />
prevalence of severe myopia is likely to be<br />
higher in <strong>the</strong>se countries 4 . It is probable that<br />
<strong>the</strong> prevalence and severity of myopia is<br />
increasing worldwide as, <strong>the</strong>refore, will its<br />
public health impact 5 .<br />
Pathological myopia has a prevalence of<br />
about 2% in <strong>the</strong> USA and is <strong>the</strong> seventh<br />
leading cause of blindness in that country 6 .<br />
Figures from Canada, albeit somewhat dated,<br />
indicated that 9% of blindness was due to<br />
pathological myopia 7 .<br />
Pathological myopia usually refers to a<br />
condition where <strong>the</strong>re is greater than six<br />
dioptres of myopia or an axial length greater<br />
than 26-27mm 8 . It is a progressive, probably<br />
autosomal recessive disorder where serious<br />
ocular complications can develop such as<br />
chorioretinal degeneration, posterior<br />
staphyloma, retinal detachment, primary open<br />
angle glaucoma and posterior subcapsular and<br />
nuclear cataract. Highly myopic eyes also have<br />
greater responsiveness to topical<br />
corticosteroids and, <strong>the</strong>refore, <strong>the</strong>re is a<br />
higher risk of raised intraocular pressure (IOP)<br />
with <strong>the</strong>ir prolonged use 9 .<br />
Fur<strong>the</strong>rmore, o<strong>the</strong>r ocular and general<br />
conditions or diseases can be associated with<br />
pathological myopia. Some examples include<br />
retinitis pigmentosa, ocular albinism, infantile<br />
glaucoma, retinopathy of prematurity, Down’s<br />
syndrome, Marfan’s syndrome, Ehlers-Danlos<br />
syndrome and Sticklers syndrome 6,10 .<br />
FUNDUS CHANGES IN MYOPIA<br />
In this review, we have divided ocular fundus<br />
changes in terms of <strong>the</strong>ir location, that is, <strong>the</strong><br />
posterior pole or <strong>the</strong> fundus periphery. A brief<br />
summary is given in Table 1 (page 35).<br />
Blacharski 7 divides chorioretinal changes in<br />
myopia into biomechanical, neovascular and<br />
degenerative types. Biomechanical changes<br />
include <strong>the</strong> so-called “lacquer cracks”, where<br />
fractures or tears occur in Bruch’s membrane,<br />
and posterior staphylomas. Choroidal<br />
neovascularisation can arise, usually in older<br />
myopes, and resolution may be seen in <strong>the</strong><br />
form of a Fuchs’ spot. Various degenerative<br />
changes are common such as chorioretinal<br />
atrophy, lattice degeneration and pavingstone<br />
degeneration.<br />
POSTERIOR POLE<br />
Optic disc crescent<br />
This is an early change in <strong>the</strong> myopic fundus<br />
and is due to a pulling away of <strong>the</strong> choroid and<br />
pigment epi<strong>the</strong>lium, usually from <strong>the</strong> temporal<br />
edge of <strong>the</strong> nerve to expose <strong>the</strong> sclera<br />
(Figure 1). Curtin and Karlin 11 found optic disc<br />
crescents in all eyes which had an axial length<br />
of 28.5mm or more. Temporal and annular<br />
crescents predominated. O<strong>the</strong>r studies have<br />
found that <strong>the</strong> width of <strong>the</strong> crescent was<br />
strongly associated with <strong>the</strong> degree of myopia<br />
(Figure 2).<br />
Research on Chinese subjects in Hong Kong<br />
has provided fur<strong>the</strong>r insights 12,13 . Whereas <strong>the</strong><br />
incidence of crescent formation was<br />
significantly associated with increasing axial<br />
length and myopic refraction, when acquired<br />
ra<strong>the</strong>r than physiological crescents were<br />
considered, <strong>the</strong> size of <strong>the</strong> crescent was not<br />
related to increased axial length or myopic<br />
refraction. Also, optic discs were more<br />
vertically oval in highly myopic eyes – a factor<br />
which must be considered when examining <strong>the</strong><br />
optic disc of a myope who is also a glaucoma<br />
suspect, glaucoma being certainly more<br />
common in myopic eyes, especially <strong>the</strong> high<br />
myopes 14 . Appropriate assessment of <strong>the</strong> optic<br />
disc cup can be a challenge in <strong>the</strong> myope,<br />
particularly when <strong>the</strong> optic disc is tilted and a<br />
crescent or zone of peripapillary atrophy is<br />
present. In <strong>the</strong> moderate myope, <strong>the</strong> cup to<br />
disc ratio may be greater than average,<br />
whereas <strong>the</strong> higher myopes may appear to have<br />
little cup because of posterior staphyloma<br />
formation. A stereoscopic evaluation through<br />
dilated pupils is, <strong>the</strong>refore, mandatory.<br />
Posterior staphyloma<br />
A posterior staphyloma is a backward ectasia<br />
of <strong>the</strong> fundus, <strong>the</strong> hallmark being tessellation<br />
and pallor of <strong>the</strong> area involved (Figure 3). The<br />
edges of <strong>the</strong> staphyloma may be anything but<br />
discrete. Curtin 15 divides staphylomas into five<br />
types, with <strong>the</strong> first, where <strong>the</strong> area of<br />
tessellation and pallor includes <strong>the</strong> region of<br />
<strong>the</strong> optic disc and macula, being <strong>the</strong> most<br />
common. Type two tends to encompass <strong>the</strong><br />
region of <strong>the</strong> macula, type three is<br />
peripapillary and type four extends nasally<br />
from <strong>the</strong> optic disc. The fifth type is <strong>the</strong> most<br />
rare and involves <strong>the</strong> fundus inferior to <strong>the</strong><br />
optic disc. Posterior staphylomas are often<br />
www.optometry.co.uk<br />
33
ot<br />
Figure 3<br />
The most common type 1 posterior<br />
staphyloma. The edge of <strong>the</strong><br />
staphylomatous region is arrowed<br />
progressive and result in vision loss 16 .<br />
Steidl and Pruett 17 found that eyes with <strong>the</strong><br />
shallowest staphylomas showed <strong>the</strong> largest<br />
drop in visual acuity as well as <strong>the</strong> greatest<br />
frequency of choroidal neovascular membranes<br />
and haemorrhage. They suggested that with<br />
less advanced staphylomas, <strong>the</strong> choriocapillaris<br />
was better preserved, thus increasing <strong>the</strong><br />
likelihood of <strong>the</strong> development of neovascular<br />
membranes.<br />
Lacquer cracks<br />
Lacquer cracks, thought to be healed linear<br />
ruptures in <strong>the</strong> retinal pigment epi<strong>the</strong>lium-<br />
Bruch’s membrane-choriocapillaris complex 18 ,<br />
are present in about 4% of highly myopic eyes 19<br />
(Figure 4). They are frequently seen in<br />
conjunction with posterior staphylomas and up<br />
to a third can have associated neovascular<br />
membranes. The resolution of any resultant<br />
haemorrhage may lead to <strong>the</strong> formation of a<br />
pigmented Fuchs’ spot (Figure 5). Lacquer<br />
cracks often progress to form more advanced<br />
fundus changes 19 . Patients with lacquer cracks<br />
and/or Fuchs’ spot should receive a guarded<br />
prognosis for vision.<br />
Chorioretinal atrophy<br />
More commonly seen in <strong>the</strong> younger myope,<br />
<strong>the</strong>se areas appear as small, punched-out<br />
yellow/white lesions in <strong>the</strong> presence of<br />
posterior staphylomas, and potentially close to<br />
lacquer cracks and <strong>the</strong> macula (Figure 6). With<br />
time, smaller lesions frequently coalesce to<br />
form larger areas 20 (Figure 7). Chorioretinal<br />
atrophy may be <strong>the</strong> result of stretching and<br />
thinning of <strong>the</strong> retinal pigment epi<strong>the</strong>lium and<br />
choroid as <strong>the</strong> eye enlarges, thus exposing <strong>the</strong><br />
sclera 21 .<br />
FUNDUS PERIPHERY<br />
The major threat to vision in <strong>the</strong> myopic eye is<br />
retinal detachment, especially as posterior<br />
vitreous detachment (PVD) and predisposing<br />
retinal degenerations, such as lattice<br />
degeneration, are more common in <strong>the</strong>se eyes.<br />
Figure 4<br />
Lacquer cracks near <strong>the</strong> macula<br />
Akiba 22 suggested that in high myopia, PVD<br />
develops increasingly with age and <strong>the</strong> degree<br />
of myopia, and that it may be seen as much as<br />
10 years earlier in highly myopic eyes<br />
compared to emmetropic eyes. In a study of<br />
218 patients with myopia of six dioptres or<br />
more in both eyes, Celorio and Pruett 23 found<br />
that one third had lattice degeneration, with<br />
<strong>the</strong> greatest prevalence being in eyes having<br />
six to nine dioptres of myopia. Lattice<br />
degeneration represents vulnerable areas of<br />
retinal thinning. It is non-age specific and is<br />
seen in about 40% of eyes with retinal<br />
detachment 9 .<br />
Pigmentary degeneration, consisting of<br />
extensive pigment deposition in <strong>the</strong> extreme<br />
retinal periphery, and <strong>the</strong> non-predisposing<br />
paving stone degeneration (yellow-white areas<br />
of chorioretinal thinning) are also more<br />
common in myopic eyes. The pigment<br />
proliferation and RPE migration of pigmentary<br />
degeneration may be due to retinal traction,<br />
while <strong>the</strong> chorioretinal thinning in paving<br />
stone degeneration may be due to localised<br />
occlusion of <strong>the</strong> choroidal circulation 16 . White<br />
without pressure (translucent whitish<br />
Figure 6<br />
Chorioretinal atrophy: small, punched out<br />
lesions near <strong>the</strong> macula (<strong>the</strong> white streak at<br />
<strong>the</strong> bottom of <strong>the</strong> photograph is artefact)<br />
Figure 5<br />
A developing Fuchs’ spot toge<strong>the</strong>r with<br />
haemorrhage and a serous detachment of<br />
<strong>the</strong> macula. Vision was markedly reduced<br />
circumferential patches), from a prominent<br />
vitreous base and mild vitreous traction, is<br />
more frequently seen in myopic eyes and<br />
occasionally retinal breaks can occur in <strong>the</strong><br />
presence of such lesions 9,16 .<br />
It has been estimated that potentially up to<br />
80% of eyes suffering retinal detachment have<br />
some degree of myopia. Also, a person with<br />
five dioptres of myopia is at a 15 times greater<br />
risk of developing retinal detachment than an<br />
emmetrope. With 20 dioptres of myopia, <strong>the</strong><br />
risk increases to 110 times 7 . There are also<br />
reports of retinal detachments in myopes<br />
following clear lens extraction procedures used<br />
to refractively correct <strong>the</strong> myopia 24 .<br />
MANAGEMENT<br />
Myopic patients, especially those with<br />
pathological myopia, must be reviewed<br />
regularly, preferably on an annual basis, and<br />
always through dilated pupils. They should<br />
receive appropriate warnings of signs<br />
and symptoms that may indicate a<br />
sight-threatening situation is developing,<br />
and be advised to utilise protective eyewear in<br />
Figure 7<br />
Chorioretinal atrophy: larger geographic<br />
areas involving <strong>the</strong> posterior pole<br />
34<br />
March 22, 2002 OT<br />
www.optometry.co.uk
potentially hazardous circumstances. Patients<br />
at risk for subretinal neovascular membrane<br />
formation should be given a take-home Amsler<br />
grid for daily testing. The increased incidence<br />
of associated conditions, such as glaucoma,<br />
must be remembered.<br />
About <strong>the</strong> authors<br />
Peter Swann is Associate Professor and<br />
Katrina Schmid Senior Lecturer in <strong>the</strong> School<br />
of Optometry, Queensland University of<br />
Technology, Brisbane, Australia. Professor<br />
Swann has a particular interest in eye disease,<br />
and Dr Schmid in <strong>the</strong> aetiology of myopia.<br />
References<br />
1. Sperduto RD, Seigel D, Roberts J, Rowland<br />
M. (1983) Prevalence of myopia in <strong>the</strong><br />
United States. Arch. Ophthalmol. 101:<br />
405-407.<br />
2. Lee KE, Klein BEK, Klein R. (1999) Changes<br />
in refractive error over a 5-year interval in<br />
<strong>the</strong> Beaver Dam Eye study. Invest<br />
Ophthalmol. Vis. Sci. 40: 1645-1649.<br />
3. Wu MM, Edwards MH. (1999) The effect of<br />
having myopic parents: an analysis of<br />
myopia in three generations. Optom. Vis.<br />
Sci. 76: 387-392.<br />
4. Wu HM, Seet B, Yap EP et al. (2001) Does<br />
education explain ethnic differences in<br />
myopia prevalence? A population-based<br />
study of young adult males in Singapore.<br />
Optom. Vis. Sci. 78: 234-239.<br />
5. Rose K, Smith W, Morgan I, Mitchell P.<br />
(2001) The increasing prevalence of<br />
myopia: implications for Australia.<br />
Clin. Exp. Ophthalmol. 29: 116-120.<br />
6. Alexander LJ. (1994) Primary care of <strong>the</strong><br />
posterior segment. Appleton & Lange,<br />
Connecticut.<br />
7. Blacharski PA. (1988) Pathologic<br />
progressive myopia, in DA Newsome Ed.,<br />
Retinal dystrophies and degenerations.<br />
Raven Press, New York.<br />
8. Miller DG, Singerman LJ. (2001) Natural<br />
history of choroidal neovascularization in<br />
high myopia. Curr. Opinion Ophthalmol.<br />
12: 222-224.<br />
9. Kanski JJ. (1994) Clinical Ophthalmology<br />
3rd ed, Butterworth-Heinemann, Oxford.<br />
10. Marr JE, Halliwell-Ewen J, Fisher B et al.<br />
(2001) Associations of high myopia in<br />
childhood. Eye 15: 70-74.<br />
11. Curtin BJ, Karlin DB. (1971) Axial length<br />
measurements and fundus changes of <strong>the</strong><br />
myopic eye. Am. J. Ophthalmol. 71: 42-53.<br />
12. Hendicott P, Lam C. (1991) Myopic<br />
crescent, refractive error and axial length<br />
in Chinese eyes. Clin. Exp. Optom. 74: 168-<br />
174.<br />
13. Lam AKC, Cheng KKH, Lam RK et al. (1996)<br />
Optic disc ovalness, refractive error and<br />
axial length of Hong Kong Chinese.<br />
Clin. Exp. Optom. 79: 167-172.<br />
14. Mitchell P, Hourihan F, Sandbach J, Wang<br />
JJ. (2000) The relationship between<br />
glaucoma and myopia. Ophthalmology 106:<br />
2010-2015.<br />
15. Curtin BJ. (1977) The posterior staphyloma<br />
of pathologic myopia.<br />
Trans. Am. Ophthalmol. Soc. 75: 67-86.<br />
16. Hoffman DJ, Heath DA. (1987) Staphyloma<br />
and o<strong>the</strong>r risk factors in axial myopia.<br />
J. Am. Optom. Assoc. 58: 907-913.<br />
17. Steidl SM, Pruet RC. (1997) Macular<br />
complications associated with posterior<br />
staphyloma. Am. J. Ophthalmol. 123:<br />
181-187.<br />
18. Klein RM, Curtin BJ. (1975) Lacquer crack<br />
lesions in pathologic myopia.<br />
Am. J. Ophthalmol. 79: 386-392.<br />
19. Ohno-Matsui K, Tokoro T. (1996) The<br />
progression of lacquer cracks in pathologic<br />
myopia. Retina 16: 29-37.<br />
20. Ito-Ohara M, Seko Y, Morita H et al. (1998)<br />
Clinical course of newly developed or<br />
progressive patchy chorioretinal atrophy in<br />
pathological myopia. Ophthalmologica<br />
212: 23-29.<br />
21. Morse PH. (1989) Vitreoretinal disease 2nd<br />
ed, Year Book Medical Publishers, Chicago.<br />
22. Akiba J. (1993) Prevalence of posterior<br />
vitreous detachment in high myopia.<br />
Ophthalmology 100: 1384-1388.<br />
23. Celorio JM, Pruett RC. (1991) Prevalence of<br />
lattice degeneration and its relation to<br />
axial length in severe myopia.<br />
Am. J. Ophthalmol. 111: 20-23.<br />
24. Ripandelli G, Billi B, Fedeli S. (1996)<br />
Retinal detachment after clear lens<br />
extraction in 41 eyes with high axial<br />
myopia. Retina 16: 3-6.<br />
25. Pierro L, Camesasca FI, Mischi M, Brancato<br />
R. (1992) Peripheral retinal changes and<br />
axial myopia. Retina 12: 12-17.<br />
Table 1 Summary of potential ocular fundus changes in high myopia<br />
FUNDUS CHANGE LOCATION AETIOLOGY PREVALENCE<br />
EFFECT ON VISION<br />
MAY LEAD TO<br />
Optic disc<br />
crescent<br />
Posterior pole<br />
Biomechanical<br />
Observed in most myopes,<br />
100% of eyes with axial length<br />
≥28.5mm 11<br />
None, unless o<strong>the</strong>r pathology<br />
also present<br />
----<br />
Posterior<br />
staphyloma<br />
Posterior pole<br />
Biomechanical<br />
Observed in 76% of myopes,<br />
-3 to -38D 16<br />
Can be progressive and result<br />
in vision loss<br />
Choroidal neovascular<br />
membranes<br />
Lacquer cracks<br />
Posterior pole<br />
Biomechanical<br />
Observed in 4% of high<br />
myopes >6D 19<br />
Guarded prognosis for vision<br />
Choroidal neovascular<br />
membranes<br />
Chorioretinal<br />
atrophy<br />
Posterior pole<br />
Degenerative<br />
Observed more commonly in<br />
younger high myopes, 23% of<br />
myopic eyes with axial length<br />
>24.5mm 11<br />
Guarded prognosis for vision<br />
if at <strong>the</strong> macula<br />
Associated with posterior<br />
staphylomas, lacquer cracks<br />
Fuchs’ spot<br />
Macula<br />
Neovascular<br />
Observed in 5-10% of eyes<br />
with axial length ≥26.5mm 11<br />
Guarded prognosis for vision<br />
Associated with posterior<br />
staphylomas, lacquer cracks<br />
Lattice<br />
degeneration<br />
Periphery<br />
Degenerative<br />
Observed in 13-30% of<br />
myopes 23,25<br />
None, unless secondary<br />
pathology occurs<br />
Retinal detachment<br />
Pigmentary<br />
degeneration<br />
Periphery<br />
Degenerative<br />
Observed in 17% of myopes 25<br />
None<br />
----<br />
Paving stone<br />
degeneration<br />
Periphery<br />
Degenerative<br />
Observed in 27% of myopes 25<br />
None<br />
----<br />
White without<br />
pressure<br />
Periphery<br />
Biomechanical<br />
Observed in 23% of myopes 25<br />
None, unless secondary<br />
pathology occurs<br />
Occasionally retinal tears<br />
Prevalence values should only be used as an indication of how common <strong>the</strong>se changes are in <strong>the</strong> myopic eye.<br />
Reported prevalence values vary greatly between studies, due to differences in <strong>the</strong> age of subjects and severity of <strong>the</strong> myopia.<br />
www.optometry.co.uk 35