Intraocular lens implantation - Optometry Today
Intraocular lens implantation - Optometry Today
Intraocular lens implantation - Optometry Today
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ot<br />
Sponsored by<br />
Emma J. Hollick BA, FRCOphth, MD<br />
<strong>Intraocular</strong> <strong>lens</strong><br />
<strong>implantation</strong><br />
In the 18th century, Casanova first suggested that an<br />
artificial <strong>lens</strong> implant could be inserted into the eye to<br />
replace the crystalline <strong>lens</strong> after cataract extraction 1 .<br />
ABDO has awarded this<br />
article<br />
2 CET credits (GD).<br />
The College of<br />
Optometrists has<br />
awarded this article 2<br />
CET credits. There are<br />
12 MCQs with a pass<br />
mark of 60%.<br />
Theoretically, replacement of the crystalline<br />
<strong>lens</strong> with an artificial <strong>lens</strong> is the optimal form<br />
of aphakic correction, as the majority of<br />
aberrations and distortions from spectacles<br />
derive from their placement anterior to the<br />
pupillary plane. Indeed, image magnification<br />
is a major disadvantage with aphakic<br />
spectacles as they increase the image size by<br />
20-35%, which leads to spatial disorientation.<br />
Other distortions include ring scotomata,<br />
peripheral distortion, the “jack-in-the-box”<br />
phenomenon, and a reduction in useful<br />
peripheral field.<br />
Contact <strong>lens</strong>es bring the refractive<br />
correction nearer to the nodal point of the<br />
eye, with a corresponding decrease in these<br />
distortions. Aphakic contact <strong>lens</strong>es increase<br />
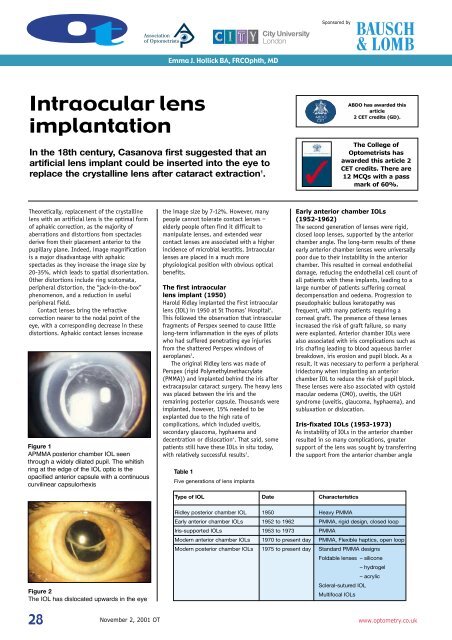
Figure 1<br />
APMMA posterior chamber IOL seen<br />
through a widely dilated pupil. The whitish<br />
ring at the edge of the IOL optic is the<br />
opacified anterior capsule with a continuous<br />
curvilinear capsulorhexis<br />
the image size by 7-12%. However, many<br />
people cannot tolerate contact <strong>lens</strong>es –<br />
elderly people often find it difficult to<br />
manipulate <strong>lens</strong>es, and extended wear<br />
contact <strong>lens</strong>es are associated with a higher<br />
incidence of microbial keratitis. <strong>Intraocular</strong><br />
<strong>lens</strong>es are placed in a much more<br />
physiological position with obvious optical<br />
benefits.<br />
The first intraocular<br />
<strong>lens</strong> implant (1950)<br />
Harold Ridley implanted the first intraocular<br />
<strong>lens</strong> (IOL) in 1950 at St Thomas’ Hospital 2 .<br />
This followed the observation that intraocular<br />
fragments of Perspex seemed to cause little<br />
long-term inflammation in the eyes of pilots<br />
who had suffered penetrating eye injuries<br />
from the shattered Perspex windows of<br />
aeroplanes 3 .<br />
The original Ridley <strong>lens</strong> was made of<br />
Perspex (rigid Polymethylmethacrylate<br />
(PMMA)) and implanted behind the iris after<br />
extracapsular cataract surgery. The heavy <strong>lens</strong><br />
was placed between the iris and the<br />
remaining posterior capsule. Thousands were<br />
implanted, however, 15% needed to be<br />
explanted due to the high rate of<br />
complications, which included uveitis,<br />
secondary glaucoma, hyphaema and<br />
decentration or dislocation 4 . That said, some<br />
patients still have these IOLs in situ today,<br />
with relatively successful results 3 .<br />
Table 1<br />
Five generations of <strong>lens</strong> implants<br />
Early anterior chamber IOLs<br />
(1952-1962)<br />
The second generation of <strong>lens</strong>es were rigid,<br />
closed loop <strong>lens</strong>es, supported by the anterior<br />
chamber angle. The long-term results of these<br />
early anterior chamber <strong>lens</strong>es were universally<br />
poor due to their instability in the anterior<br />
chamber. This resulted in corneal endothelial<br />
damage, reducing the endothelial cell count of<br />
all patients with these implants, leading to a<br />
large number of patients suffering corneal<br />
decompensation and oedema. Progression to<br />
pseudophakic bullous keratopathy was<br />
frequent, with many patients requiring a<br />
corneal graft. The presence of these <strong>lens</strong>es<br />
increased the risk of graft failure, so many<br />
were explanted. Anterior chamber IOLs were<br />
also associated with iris complications such as<br />
iris chafing leading to blood aqueous barrier<br />
breakdown, iris erosion and pupil block. As a<br />
result, it was necessary to perform a peripheral<br />
iridectomy when implanting an anterior<br />
chamber IOL to reduce the risk of pupil block.<br />
These <strong>lens</strong>es were also associated with cystoid<br />
macular oedema (CMO), uveitis, the UGH<br />
syndrome (uveitis, glaucoma, hyphaema), and<br />
subluxation or dislocation.<br />
Iris-fixated IOLs (1953-1973)<br />
As instability of IOLs in the anterior chamber<br />
resulted in so many complications, greater<br />
support of the <strong>lens</strong> was sought by transferring<br />
the support from the anterior chamber angle<br />
Type of IOL Date Characteristics<br />
Figure 2<br />
The IOL has dislocated upwards in the eye<br />
Ridley posterior chamber IOL 1950 Heavy PMMA<br />
Early anterior chamber IOLs 1952 to 1962 PMMA, rigid design, closed loop<br />
Iris-supported IOLs 1953 to 1973 PMMA<br />
Modern anterior chamber IOLs 1970 to present day PMMA, Flexible haptics, open loop<br />
Modern posterior chamber IOLs 1975 to present day Standard PMMA designs<br />
Foldable <strong>lens</strong>es – silicone<br />
– hydrogel<br />
– acrylic<br />
Scleral-sutured IOL<br />
Multifocal IOLs<br />
28<br />
November 2, 2001 OT<br />
www.optometry.co.uk
Sponsored by<br />
Module 3 Part 11<br />
to the iris. The third generation of IOLs,<br />
independently produced by Epstein and<br />
Binkhorst, used the pupillary part of the iris<br />
diaphragm for anatomical fixation. However,<br />
this led to luxation of the <strong>lens</strong> if the pupil<br />
dilated unexpectedly. These pupillary fixated<br />
IOLs are now obsolete. A second development<br />
was the use of a Medallion <strong>lens</strong> fixed to the<br />
iris by a suture, however late degradation of<br />
the suture led to dislocation of the <strong>lens</strong>es. The<br />
next development was the Iris-claw <strong>lens</strong> with a<br />
fixating mechanism based on the capture<br />
of a fold of iris tissue at the two ends of the<br />
IOL.<br />
Modern anterior chamber<br />
IOLs (1970 to present day)<br />
For an anterior chamber <strong>lens</strong> to be safe and<br />
effective there should be minimal contact with<br />
the drainage angle, stability within the<br />
anterior chamber with no movement in the<br />
angle, no iris chafing and no endothelial<br />
touch.<br />
Modern anterior chamber IOLs were<br />
designed to achieve this by using flexible open<br />
loop <strong>lens</strong>es made of PMMA. They have the<br />
advantage of not requiring an intact posterior<br />
capsule for <strong>implantation</strong> and can be implanted<br />
into eyes even after posterior capsule rupture<br />
(occurring during complicated cataract surgery<br />
or after intracapsular surgery). Modern<br />
anterior chamber IOLs allow far better fixation<br />
Table 2<br />
Advantages and disadvantages of the IOL types<br />
www.optometry.co.uk<br />
than the early anterior chamber IOLs and<br />
corneal complications are rare. However, they<br />
are associated with a higher incidence of CMO<br />
and retinal detachment than posterior<br />
chamber IOLs.<br />
Modern posterior chamber<br />
IOLs (1975 to present day)<br />
The first posterior chamber IOLs were made of<br />
PMMA with either PMMA, polypropylene or<br />
polyamide haptics. They require the presence<br />
of a posterior capsule and can either be placed<br />
in the sulcus or the capsular bag. Capsular bag<br />
placement has been shown to be superior to<br />
sulcus placement in terms of centration and<br />
the rate of posterior capsular opacification<br />
(PCO). The advantage of posterior chamber<br />
IOLs is that they are placed in the position of<br />
the original crystalline <strong>lens</strong> leading to a more<br />
physiological situation with optical benefits.<br />
An additional advantage is that posterior<br />
chamber IOLs are situated away from the<br />
delicate structures of the anterior chamber<br />
including the cornea, the aqueous outflow<br />
channels, the iris and the ciliary body. This<br />
leads to a lower incidence of corneal problems,<br />
UGH and pupil block. When the IOL is placed<br />
within the capsular bag, contact with uveal<br />
tissues is completely avoided. The intact<br />
posterior capsule is associated with a<br />
decreased incidence of CMO and retinal<br />
detachment 5 .<br />
Type of IOL Advantages Disadvantages<br />
Ridley PC IOL optical uveitis<br />
secondary glaucoma<br />
hyphaema<br />
decentration/dislocation<br />
Early AC IOLs do not require posterior capsule - corneal complications:<br />
(rigid, closed loop) capsule usually removed therefore (decompensation, oedema,<br />
no PCO<br />
pseudophakic bullous<br />
keratopathy, IOL corneal touch)<br />
CMO, uveitis, UGH<br />
subluxation, dislocation<br />
Iris-supported IOL do not require posterior capsule iris complications: (iris chafing and<br />
erosion, pupil changes, pupillary block,<br />
PAS - Peripheral Anterior Synechiae)<br />
Modern AC IOLs do not require posterior capsule CMO retinal detachment<br />
(flexible, open loop) better fixation corneal complications rare<br />
Modern PC IOLs less corneal problems require intact zonules & posterior capsule<br />
less CMO<br />
less retinal detachment<br />
less UGH<br />
less pupil block<br />
optical<br />
Foldable IOLs small incision expensive<br />
less astigmatism<br />
decentration<br />
quicker rehabilitation<br />
rupture bag when unfolding<br />
safer<br />
spontaneous dislocation<br />
IOL material<br />
PMMA is the gold standard material for use in<br />
IOL manufacturing. It was the first material<br />
to be used, and has withstood the test of<br />
time as the majority of IOLs implanted<br />
worldwide today are still made of it. PMMA<br />
benefits from inducing a minimal intraocular<br />
inflammatory reaction, is not adversely<br />
affected by ultraviolet light and is not<br />
biodegradable in the eye. Because of this, it<br />
maintains a smooth surface even when in<br />
contact with vascular and metabolically<br />
active tissue. PMMA is also relatively<br />
inexpensive. However, one disadvantage is<br />
that it is rigid and so requires a larger<br />
incision for insertion than the newer foldable<br />
materials. Surface modifications of PMMA<br />
with heparin have been found to reduce the<br />
inflammatory cell precipitates found on the<br />
anterior IOL surface post-operatively,<br />
therefore, this <strong>lens</strong> modification is useful in<br />
patients expected to have more precipitation,<br />
such as uveitics.<br />
With the development of small incision<br />
phacoemulsification surgery, a whole new<br />
range of foldable <strong>lens</strong> implant materials have<br />
been developed. Early foldable IOLs, however,<br />
were not successful, because they elbowed<br />
and folded as the capsular bag contracted.<br />
The use of capsulorhexis dramatically reduces<br />
this decentration of foldable materials.<br />
The advantages of foldable IOLs are due<br />
to the smaller incision size required for their<br />
insertion. They are usually self-sealing and<br />
do not require suturing. Smaller incisions<br />
produce less astigmatism, allow quicker<br />
visual rehabilitation with stable refraction<br />
after a couple of weeks compared to six to<br />
eight weeks for larger wounds, and are safer<br />
with less iris prolapse and dehiscence. The<br />
disadvantage of foldable IOLs is that they are<br />
more expensive than PMMA and have a<br />
higher incidence of decentration if a<br />
continuous curvilinear capsulorhexis is not<br />
used.<br />
When a new IOL material is developed, its<br />
biocompatibility needs to be studied. IOL<br />
biocompatibility within the human eye has<br />
three major aspects. These are the effect on<br />
the blood aqueous barrier, the cellular<br />
reaction on the anterior surface of the <strong>lens</strong>,<br />
and the effect on the <strong>lens</strong> capsule. Blood<br />
aqueous barrier changes can be assessed by<br />
the amount of inflammation (flare and cells)<br />
within the anterior chamber, which can be<br />
quantified using the laser flare and cell<br />
meter. Cells on the anterior surface of the<br />
implant can be examined post-operatively<br />
using specular microscopy and have been<br />
used extensively as a method of assessing<br />
the foreign body response to the IOL. The<br />
effect of the IOL on the capsule consists of<br />
<strong>lens</strong> epithelial cell proliferation and<br />
metaplasia leading to anterior and posterior<br />
capsular opacification, and IOL decentration.<br />
PCO occurs in 20-50% of patients two years<br />
after cataract surgery (Figure 3). It leads to a<br />
progressive deterioration in visual acuity and<br />
29
ot<br />
Figure 3<br />
This IOL shows a dramatic amount of<br />
opacification of the posterior capsule.<br />
The patient’s vision was significantly<br />
reduced and they required a Nd: YAG laser<br />
posterior capsulotomy<br />
contrast sensitivity, and in many cases patients<br />
do not seek medical attention, fearing that this<br />
is an untreatable age-related change. PCO can<br />
be relatively easily treated with Nd<br />
(neodymium):YAG laser posterior capsulotomy,<br />
where the Nd:YAG laser is used to make a hole<br />
Table 3<br />
Posterior chamber intraocular <strong>lens</strong> design features<br />
Design feature<br />
Number of pieces<br />
Loop material<br />
Loop shape<br />
Optic design<br />
Surface modification<br />
IOL material<br />
Variations<br />
• One piece (disc or plate haptic)<br />
• Three piece (disc)<br />
Figure 4<br />
A diamond shaped posterior capsulotomy<br />
can be seen in the central posterior<br />
capsule of this patient with significant PCO<br />
in the posterior capsule to clear the visual axis<br />
(Figure 4). This procedure, however, can be<br />
associated with a number of complications such<br />
as pitting of the IOL, intraocular pressure<br />
spikes, inflammation, CMO and retinal<br />
detachment. Many IOL manufacturers are<br />
concentrating their research on ways to prevent<br />
PCO, and there are now certain IOLs which are<br />
associated with a lower incidence of PCO.<br />
• Polypropylene (flexible, possible higher incidence of endophthalmitis)<br />
• PMMA (rigid)<br />
• Polyacrylic<br />
• Angulation (forward angulation increases pressure on posterior capsule<br />
and may decrease PCO, and increases distance of optic from iris.<br />
Less angulation may facilitate insertion)<br />
• J or C loops<br />
• Convex plano, plano convex, biconvex (Biconvex associated with<br />
the least image degradation with decentration and tilt and less PCO)<br />
• Length of the IOL (14mm for sulcus fixation, 12-12.5mm<br />
for in-the-bag fixation)<br />
• Size of optic (4.5-7mm. Larger optics may be better for patients with large<br />
pupils but need bigger incisions. Smaller optics for bag fixation)<br />
• Holes (to facilitate dialling into capsular bag)<br />
• Ridges (designed to facilitate laser capsulotomy, but associated<br />
with more PCO)<br />
• Sharp or round optic edge (less PCO when optic has a square edge than<br />
round, due to barrier to <strong>lens</strong> epithelial cell migration, e.g. Alcon AcrySof IOL;<br />
Pharmacia & Upjohn CeeOn 911; Rayner Centerflex IOLs)<br />
• Binding of hydrogels or heparin to the IOL surface (to make IOL more<br />
hydrophilic, found to reduce inflammatory cell precipitate)<br />
• Surface passivation (to make IOL more hydrophobic and oleophilic,<br />
aiming to repel lipids such as cell membranes and ocular tissues)<br />
• PMMA<br />
• Silicone<br />
• Hydrogel/hydrophilic acrylic<br />
• Hydrophobic acrylic<br />
Silicone elastomers (elastic polymers) are<br />
composed of highly cross-linked polysiloxane<br />
chains. They are compressible and can<br />
therefore be inserted through a small incision<br />
by folding. Silicone <strong>lens</strong>es are homogeneous,<br />
heat-resistant, autoclavable, moldable and<br />
compressible and highly transparent to visible<br />
light. The specific gravity of the material is<br />
low and therefore the <strong>lens</strong> is nearly weightless<br />
in aqueous. Silicone has excellent tensile and<br />
tear strength, and is extraordinarily flexible.<br />
Silicone IOLs can be either three pieces, with<br />
open loop prolene, polyamide or PMMA<br />
haptics, or plate haptic.<br />
Silicone has a lower refractive index<br />
(1.41-1.46) than PMMA (1.49) and<br />
consequently the <strong>lens</strong> is thicker, which may be<br />
an impediment to very high powers. Although<br />
the silicone <strong>lens</strong> is transparent to Nd:YAG<br />
laser radiation, the <strong>lens</strong> can be pitted when<br />
hit by the laser beam 6 . In fact, silicone IOLs<br />
have been shown to have the lowest threshold<br />
for laser-induced damage compared to PMMA<br />
and acrylic IOLs, and to suffer the greatest<br />
damage depth at each energy level tested 7 .<br />
Furthermore, the surface of a silicone IOL is<br />
hydrophobic and it has been shown that a<br />
higher percentage of cellular reactions occur<br />
on hydrophobic surfaces than hydrophilic<br />
ones 8 .<br />
A further disadvantage is that they<br />
become slippery when wet and, as a result,<br />
become difficult to handle. An additional<br />
clinical complication occurs if silicone oil is<br />
used to help re-attach the retina following a<br />
retinal detachment in a pseudophakic patient,<br />
as the oil adheres to silicone IOLs. In<br />
addition, silicone IOLs with flexible haptics or<br />
plate haptic design have a higher incidence of<br />
decentration than other IOL types. Plate<br />
haptic silicone IOLs are also at increased risk<br />
of anterior capsule opening contraction 9 .<br />
Incidences of capsular bag rupture have also<br />
been reported during IOL unfolding, and<br />
spontaneous dislocation of IOLs into the<br />
vitreous after YAG capsulotomy, particularly<br />
with the plate haptic design.<br />
More recent silicone IOLs are made of<br />
second-generation silicone and appear to be<br />
associated with less inflammatory cell<br />
precipitate than the earlier first-generation<br />
<strong>lens</strong>es. A recent silicone IOL design,<br />
CeeOn 911 (Pharmacia & Upjohn) has been<br />
manufactured with a square optic edge, which<br />
has been shown to be associated with a low<br />
incidence of PCO compared to many other IOL<br />
types.<br />
Hydrophilic acrylics include a broad class<br />
of polymer materials which swell extensively<br />
in water but are not water-soluble (previously<br />
referred to as hydrogels). These materials<br />
have variable size and physical properties<br />
according to the state of hydration. An<br />
example is polyhydroxyethylmethacrylate<br />
(PHEMA), which has a 38% water content.<br />
High-water content hydrogels are<br />
cross-linked polymers based on a hydrophilic<br />
monomer. They are soft and resemble living<br />
30<br />
November 2, 2001 OT<br />
www.optometry.co.uk
Sponsored by<br />
Module 3 Part 11<br />
tissues in their physical properties and the<br />
smooth, hydrophilic nature minimises<br />
mechanical friction with ocular tissues and<br />
contributes to superior biocompatibility 10 . This<br />
is reported to produce less damage to the<br />
corneal endothelium after inadvertent touch<br />
on <strong>implantation</strong> than PMMA 11 . The hydrophilic<br />
nature of the <strong>lens</strong> surface causes low<br />
interfacial tension (wettability) of the<br />
hydrogel in aqueous solution and reduces the<br />
tendency of proteins to denature on the<br />
surface of the polymer, thus reducing<br />
biological rejection mechanisms. This possibly<br />
also prevents adhesion between the <strong>lens</strong> and<br />
the capsular bag. As the dimension of the<br />
hydrogel changes in direct proportion to the<br />
degree of water saturation, it enables<br />
<strong>implantation</strong> of a semi-hydrated <strong>lens</strong> through<br />
a small incision, for it to later expand in the<br />
eye as it becomes fully hydrated.<br />
Hydrophilic acrylics have the advantage of<br />
undergoing less damage during YAG laser<br />
capsulotomy. When there is direct impact of<br />
the YAG laser beam on the <strong>lens</strong>, mild to<br />
moderate localised pitting occurs, without the<br />
radial fracturing seen on a PMMA implant. This<br />
is due to the resilience of the material and its<br />
ability to act as a shock absorber rather than<br />
cracking under stress.<br />
Although high water-content polymers are<br />
usually mechanically weak, the hydrogels can<br />
be very strong owing to certain changes of the<br />
polymer produced during the process of<br />
polymerisation. Examples of hydrophilic<br />
acrylic IOLs are the Hydroview <strong>lens</strong>, EasAcryl,<br />
Inject-A, Centerflex and the Memory Lens.<br />
Studies on the Hydroview IOL (Bausch & Lomb)<br />
have shown that it is associated with fewer<br />
surface inflammatory cells than PMMA and a<br />
second-generation silicone IOL. However, a<br />
significant <strong>lens</strong> epithelial cell (LECs) reaction<br />
on the anterior IOL surface was reported in<br />
addition to a higher incidence of PCO 12,13 .<br />
AcrySof (Alcon) is an example of a<br />
hydrophobic acrylic IOL, which has become the<br />
most commonly inserted IOL in the USA. The<br />
AcrySof polymer was developed from the same<br />
backbone used in PMMA. It has a higher<br />
refractive index (1.55) than PMMA or silicone.<br />
This means that <strong>lens</strong> implants made from<br />
AcrySof are thinner, thereby facilitating<br />
folding and insertion through a smaller<br />
incision 14 .<br />
Acrylic polymers change their mechanical<br />
properties with temperature, being hard and<br />
glassy at low temperature, and soft and fluid<br />
at high temperature. This means that an IOL<br />
inserted at room temperature unfolds slowly<br />
and in a controlled manner 14 . This avoids the<br />
rapid, explosive opening which can be seen<br />
with three-piece silicone IOLs which may cause<br />
iatrogenic damage to the capsule or other<br />
anterior segment structures. The AcrySof IOL<br />
is, however, found by many surgeons to be<br />
more difficult to fold than silicone <strong>lens</strong>es, as<br />
the <strong>lens</strong> is more rigid if cool.<br />
In addition, due to its tacky nature, the<br />
AcrySof IOL has a tendency to stick to forceps<br />
or between two parts of the IOL on insertion 15 .<br />
This characteristic may mean that the IOL<br />
sticks to the capsular bag (which is discussed<br />
later and may have advantages), however, the<br />
adhesion means that the IOLs are more<br />
difficult to explant in cases of anisometropia<br />
or incorrect power calculation 16 . The IOLs are<br />
not slippery when wet in contrast to silicone<br />
IOLs.<br />
The AcrySof IOL has been found to be<br />
associated with dramatically reduced rates of<br />
PCO 17 . This is thought to be due to both<br />
mechanical and material features. This was the<br />
first <strong>lens</strong> implant to be manufactured with a<br />
square optic edge, and it is thought that this<br />
edge acts as a barrier to the migration of LECs<br />
onto the posterior capsule, reducing PCO. The<br />
tacky nature of the implant leads to increased<br />
adhesion of the IOL to the capsule which also<br />
probably limits the migration of LECs onto the<br />
posterior capsule.<br />
An IOL may have excellent cytological<br />
biocompatibility (a limited/nil inflammatory<br />
reaction), but poor capsular biocompatibility<br />
(the effect on anterior capsule and PCO), for<br />
example, the Hydroview IOL. Therefore, the<br />
goal is to find an IOL which has both<br />
cytological and capsular biocompatibility.<br />
Design features, such as a sharp optic edge,<br />
and material composition appear to be equally<br />
important. To date, the second-generation<br />
silicone IOLs and AcrySof IOLs appear to have<br />
the best biocompatibility.<br />
Table 4<br />
Advantages and disadvantages of the IOL types<br />
IOL Type Advantages Disadvantages<br />
PMMA Long term experience Rigid so need large incision<br />
Good biocompatibility<br />
Pits with YAG laser<br />
Cheap<br />
High incidence of PCO<br />
The prevalence of <strong>lens</strong> materials in the<br />
1997 survey of the American Society of<br />
Cataract and Refractive Surgery was 38%<br />
acrylic, 20% silicone, and 40% PMMA (Kohnen,<br />
1998). The <strong>implantation</strong> of foldable IOLs in<br />
Australia rose from 1% in 1991 to 67% in<br />
1997 18 .<br />
Multifocal IOLs<br />
Standard IOLs are monofocal and so the loss of<br />
accommodation which increases with age<br />
becomes absolute with surgery, and the need<br />
to correct the resultant presbyopia is apparent.<br />
Multifocal and bifocal IOLs have been designed<br />
in an attempt to provide both distance and<br />
near vision without additional spectacle<br />
correction, as they form separate images of<br />
near and distance objects. The goal of<br />
multifocal implants has been to enable<br />
patients to be less dependent on spectacles<br />
following surgery. Multifocal IOLs are based on<br />
the simultaneous vision principle – if the<br />
power difference between two optical systems<br />
is 3.00DS or more, then the images are<br />
dissimilar enough for the brain to interpret<br />
them as separate.<br />
An example is the ARRAY multifocal IOL by<br />
Allergan which has concentric rings of varying<br />
optical power around a central power for<br />
distance. The rings of power are for near<br />
distances, while the central distance power is<br />
dominant. Fifty per cent of the <strong>lens</strong> is<br />
dedicated to distance vision, 36% to near<br />
Silicone Foldable - small incision Low refractive index - thicker IOLs (first generation silicone)<br />
Fairly low incidence of PCO High refractive index - thinner IOLs (second generation silicone)<br />
(particularly second<br />
Pits with YAG laser<br />
generation silicone)<br />
Rapid unfolding in the eye<br />
Dislocation after YAG<br />
More decentration<br />
More anterior capsule contraction<br />
Slippery when wet<br />
Cannot use with silicone oil<br />
AcrySoft Foldable - small incision Short experience<br />
High refractive index - thin IOLs Tacky surface - sticks to forceps<br />
Very low incidence of PCO More difficult to fold<br />
LEC regression<br />
?Glistenings<br />
Biocompatible<br />
?Glare<br />
Fewer pits with YAG laser<br />
Slow uncontrolled folding<br />
Hydroview Foldable - small incision LECs on anterior IOL surface<br />
Good biocompatibility<br />
High incidence of PCO<br />
- low inflammatory cell reaction<br />
Fewer pits with YAG laser<br />
Controlled unfolding<br />
Less endothelial cell damage<br />
with cornea touch<br />
www.optometry.co.uk<br />
31
ot<br />
vision and 14% to intermediate distances.<br />
One study compared 100 patients implanted<br />
with the ARRAY <strong>lens</strong> in both eyes after<br />
bilateral cataract surgery with 100 patients<br />
with a standard monofocal IOL implanted<br />
bilaterally 19 . It was reported that 41% of<br />
patients with the ARRAY <strong>lens</strong> did not wear<br />
spectacles compared to 12% of patients with<br />
monofocal IOLs. For near tasks, 38% of<br />
multifocal patients did not wear spectacles<br />
compared to 10% of monofocal patients. In<br />
addition, 85% of those with multifocal IOLs<br />
did not wear spectacles for distance compared<br />
to 52% with monofocal IOLs.<br />
The downside was that patients with<br />
multifocal <strong>lens</strong>es were more bothered with<br />
glare and haloes from oncoming headlights at<br />
night and found night driving more difficult<br />
than the patients with monofocal IOLs. This<br />
“halo-effect” can also occur with other<br />
bright/dark contrast situations.<br />
An additional disadvantage of multifocal<br />
<strong>lens</strong>es is that they reduce contrast sensitivity.<br />
This results in loss of sharpness of vision<br />
particularly under poor visibility conditions<br />
such as low light or fog. Therefore, patients<br />
who spend their lives in a twilight<br />
environment and night-time work conditions<br />
may be disturbed by this loss of contrast<br />
sensitivity. Patient selection is a crucial step<br />
when considering whether a multifocal or<br />
monofocal <strong>lens</strong> should be implanted. Suitable<br />
candidates are those whose myopic<br />
astigmatism does not exceed 1.00D, spend<br />
most of their lives in normally lit<br />
environments and have no other ocular<br />
diseases. Bilateral <strong>implantation</strong> results in the<br />
most satisfying outcome, and leaving the<br />
patient emmetropic or slightly hypermetropic<br />
minimises glare and visual disturbances.<br />
Accommodative IOLs<br />
Certain research groups are studying ways of<br />
refilling the capsular bag with flexible IOLs<br />
capable of accommodation. One study<br />
removed <strong>lens</strong>es from a group of rabbits and<br />
primates, and refilled the capsular bag with<br />
an inflatable endocapsular balloon 20 .<br />
Accommodation could be demonstrated<br />
following this technique in primates 21 ,<br />
however, the incidence of PCO was reported to<br />
be very high (94%). The post-operative<br />
amplitude of accommodation was small and<br />
decreased with time, which was likely to be<br />
due to the increase in PCO with capsular<br />
fibrosis leading to a loss of capsular pliability.<br />
The use of a soft injectable liquid to fill<br />
the bag has been attempted in rabbit eyes 22<br />
and primates 23 : after making a minicapsulorhexis,<br />
phacoemulsification was<br />
performed with a tiny tip. Silicone material<br />
was then injected into the capsular bag, and<br />
the bag then closed with a silicone plug.<br />
Some accommodation appeared to be present<br />
postoperatively. However, all eyes suffered<br />
thick PCO soon after surgery. YAG laser<br />
capsulotomy would obviously not be<br />
appropriate as this could annul the attained<br />
accommodation. However, research has<br />
continued in this field and two prototypes will<br />
be marketed for use in humans next year<br />
(see previous CPD article, Outcome in Cataract<br />
Surgery, 05/10/01).<br />
Conclusion<br />
IOL design has developed through the years<br />
and has now become extremely successful<br />
with very few complications. The<br />
complications of corneal decompensation,<br />
glaucoma, hyphaema and uveitis have largely<br />
been resolved with the use of posterior<br />
chamber IOLs placed within the capsular bag.<br />
Similarly, <strong>lens</strong> decentration and dislocation is<br />
much rarer with the in-the-bag positioning of<br />
the <strong>lens</strong> implant with capsulorhexis. However,<br />
one complication remains, despite<br />
improvements in surgical technique – PCO.<br />
Nevertheless, developments in intraocular<br />
<strong>lens</strong> design are having a dramatic effect on<br />
reducing the incidence of PCO.<br />
About the author<br />
Emma Hollick works at Moorfields Eye<br />
Hospital. She recently carried out research at<br />
St Thomas’ Hospital looking at intraocular<br />
<strong>lens</strong> implant biocompatiblity and posterior<br />
capsular opacification.<br />
References<br />
1. Marcher A. Memoirs of Giacomo Casanova<br />
de Seingalt. 8, 45-50, R&R Clarke for<br />
Limited Editions Club 1940.<br />
2. Spalton DJ. Harold Ridley’s first patient.<br />
J Cataract Refract Surg 1999; 25: 156.<br />
3. Letocha CE, Pavlin CJ. Follow-up of three<br />
patients with Ridley intraocular <strong>lens</strong><br />
<strong>implantation</strong>. J Cataract Refract Surg 1999;<br />
25: 587-591.<br />
4. Ridley H. Intra-ocular acrylic <strong>lens</strong>- past,<br />
present and future. Trans Ophthalmol Soc<br />
UK 1964; 84: 5-14.<br />
5. Smith RT, Campbell CJ, Koester CJ et al. The<br />
barrier function in extracapsular cataract<br />
surgery. Ophthalmology 1990; 97: 90-95.<br />
6. Newland TJ, Auffarth GU, Wesendale TA,<br />
Apple DJ. Neodymium: YAG laser damage on<br />
silicone intraocular <strong>lens</strong>es. A comparison of<br />
lesions on explanted <strong>lens</strong>es and<br />
experimentally produced lesions. J Cataract<br />
Refract Surg 1994; 20: 527-533.<br />
7. Newland TJ, McDermott ML, Eliott D,<br />
Hazlett LD, Apple DJ, Lambert RJ, Barett<br />
RP. Experimental neodymium:YAG laser<br />
damage to acrylic,<br />
poly(methylmethacrylate) and silicone<br />
intraocular <strong>lens</strong> materials. J Cataract<br />
Refract Surg 1999; 25: 72-76.<br />
8. Amon M, Menapace R. In vivo<br />
documentation of cellular reactions on <strong>lens</strong><br />
surfaces for assessing the biocompatibility<br />
of different intraocular <strong>lens</strong> implants. Eye<br />
1994: 8: 649-656.<br />
9. Dahlauser KF, Wrolewski KJ, Mader TH.<br />
Anterior capsule contraction with foldable<br />
silicone intraocular <strong>lens</strong>es. J Cataract<br />
Refract Surg 1998; 24: 1216-1219.<br />
10. Blumenthal M. The use of high water<br />
content hydrogels as intraocular <strong>lens</strong>es. In:<br />
Soft implant <strong>lens</strong>es in cataract surgery.<br />
Mazzocco TR, Rajacich GM, Epstein E (eds),<br />
New Jersey, Slack Inc, 1986; pp107-117.<br />
11. Blumenthal M, Yalon M. Interaction of soft<br />
and hard intraocular <strong>lens</strong>es with cat cornea<br />
endothelium. Cornea 1982; 1: 129-132.<br />
12. Hollick EJ, Spalton DJ, and Ursell PG.<br />
Surface cytology on intraocular <strong>lens</strong>es:<br />
Can increased biocompatibility have<br />
disadvantages? Archives Ophthalmol<br />
1999a; 117: 872-878.<br />
13. Hollick EJ, Spalton DJ, Ursell PG, Meacock<br />
WR, Barman SA, Boyce JF. Posterior<br />
capsular opacification with Hydogel, PMMA<br />
and Silicone intraocular <strong>lens</strong>es: two-year<br />
results of a prospective randomised clinical<br />
trial. Am J Ophthalmol 2000;<br />
129: 577-584.<br />
14. Anderson C, Koch DD, Green G, et al. Alcon<br />
AcrySof acrylic intraocular <strong>lens</strong>. In: Martin<br />
RG, Gills JP, Sanders DR, eds, Foldable<br />
<strong>Intraocular</strong> Lenses. Thorofare, NJ, Slack,<br />
1993; 161-177.<br />
15. Komatsu M. Soft acrylic <strong>lens</strong>. In: Tobari I,<br />
ed. Textbook of Ophthalmic Surgery. Vol 2,<br />
Tokyo, Kanehara, 1995; 346-348.<br />
16. Neuhann TH. <strong>Intraocular</strong> folding of an<br />
acrylic <strong>lens</strong> for explantation through a<br />
small incision cataract wound. J Cataract<br />
Refract Surg 1996; 22: 1383-6.<br />
17. Hollick EJ, Spalton DJ, Ursell PG, Pande<br />
MV, Barman SA, Boyce JF, Tilling K. The<br />
effect of PMMA, silicone and polyacrylic<br />
intraocular <strong>lens</strong>es on posterior capsular<br />
opacification three years after cataract<br />
surgery. Ophthalmology 1999b;<br />
106: 49-54.<br />
18. Loughnan M. <strong>Intraocular</strong> <strong>lens</strong> materials<br />
and styles. Aust NZ J Ophthalmol<br />
1997; 25: 251.<br />
19. Javitt MD et al. Outcomes of cataract<br />
surgery with multifocal intraocular <strong>lens</strong><br />
<strong>implantation</strong>: Functional status and quality<br />
of life. Ophthalmology 1997; 104: 589-599.<br />
20. Nishi O, Nakai Y, Mizumoto Y, Yamada Y.<br />
Capsule opacification after refilling the<br />
capsule with an inflatable endocapsular<br />
balloon. J Cataract Refract Surg 1997a,<br />
23: 1548-1555.<br />
21. Nishi O, Nakai Y, Yamada Y, Mizumoto Y.<br />
Amplitudes of accommodation of primate<br />
<strong>lens</strong>es refilled with two types of inflatable<br />
endocapsular balloon. Arch Ophthalmol<br />
1993; 111: 1677-1684.<br />
22. Nishi O, Nishi K, Mano C, Ichihara M,<br />
Honda T. Lens refilling with injectable<br />
silicone in rabbit eyes. J Cataract Refract<br />
Surg 1998a, 24: 975-982.<br />
23. Nishi O, Nishi K, Mano C, Ichihara M,<br />
Honda T. Accommodation amplitude after<br />
<strong>lens</strong> refilling with injectable silicone by<br />
sealing the capsule with a plug in primate<br />
eyes. Arch Ophthalmol 1998b, 116: 1358-<br />
1361.<br />
32<br />
November 2, 2001 OT<br />
www.optometry.co.uk
Sponsored by<br />
Module 3 Part 11<br />
Multiple choice questions<br />
<strong>Intraocular</strong> <strong>lens</strong> <strong>implantation</strong><br />
Please note there is only one correct answer<br />
1. All of the following statements concerning<br />
aphakic spectacle and contact <strong>lens</strong>es are<br />
correct except?<br />
a. Image magnification with aphakic<br />
spectacles is 50%<br />
b. Distortions with aphakic spectacles<br />
include ring scotoma<br />
c. Image magnification with aphakic contact<br />
<strong>lens</strong>es is 7-12%<br />
d. Spatial disorientation with aphakic<br />
spectacles can be a problem<br />
2. All of the following statements concerning<br />
the first IOL are correct except?<br />
a. It was manufactured from<br />
polymethylmethacrylate<br />
b. It was placed in the anterior chamber<br />
c. It had a high rate of complications<br />
d. Some patients can still be seen with these<br />
IOLs in situ today<br />
3. Which one of the following complications<br />
was not seen with early anterior chamber<br />
IOLs?<br />
a. Corneal oedema<br />
b. Uveitis<br />
c. Hyphaema<br />
d. Posterior capsular opacification<br />
4. The main difference between modern<br />
anterior chamber IOLs and early anterior<br />
chamber IOLs was?<br />
a. Material<br />
b. Loop flexibility<br />
c. Optic edge<br />
d. Insertion technique<br />
6. Which one of the following intraocular<br />
<strong>lens</strong>es does not have a square optic edge?<br />
a. AcrySof hydrophobic acrylic<br />
b. Centerflex hydrophilic acrylic<br />
c. CeeOn 911 second-generation silicone<br />
d. Hydroview hydrophilic acrylic<br />
7. Haptics can be made with all of the<br />
following materials except?<br />
a. Polypropylene<br />
b. PMMA<br />
c. Hypromellose<br />
d. Polyamide<br />
8. Binding of which one of the following<br />
materials to the IOL surface will make the<br />
IOL more hydrophilic?<br />
a. Heparin<br />
b. Silicone<br />
c. AcrySof<br />
d. Nitrate<br />
9. All of the following statements about IOL<br />
optics are correct except?<br />
a. The <strong>lens</strong> configuration of the <strong>lens</strong> optic<br />
may be convex plano, plano convex or<br />
biconvex<br />
b. Ridges in the IOL are associated with a<br />
high incidence of PCO<br />
c. The size of the optic varies from 4.5 to<br />
7mm in diameter<br />
d. A small optic may be better tolerated in<br />
patients with large pupils<br />
10. Advantages of foldable IOLs compared to<br />
rigid PMMA IOLs include all of the<br />
following except?<br />
a. Less astigmatism<br />
b. Cheaper<br />
c. Usually no need to suture incision<br />
d. Earlier stability of refraction<br />
11. Which one of the following IOL materials<br />
has been shown to suffer the most pits in<br />
its optic when a Nd:YAG laser posterior<br />
capsulotomy is performed?<br />
a. Silicone<br />
b. Acrylic<br />
c. PMMA<br />
d. Hydrogel<br />
12. All of the following statements regarding<br />
the refractive index of an IOL material are<br />
correct except?<br />
a. The higher the refractive index<br />
the thinner the optic can be<br />
b. Hydrophobic acrylics have a higher<br />
refractive index than either PMMA or<br />
silicone<br />
c. The refractive index depends on the<br />
dioptric power of the <strong>lens</strong><br />
d. IOLs with very high refractive<br />
indices can be inserted through<br />
smaller incisions<br />
5. Which one of the following features is the<br />
least important in the reduction of PCO?<br />
a. Capsular bag placement of the IOL<br />
b. Square optic edge<br />
c. IOL insertion technique<br />
d. IOL material<br />
An answer return form is included in this issue. It should be completed and<br />
returned to: CPD Initiatives (c2983i), OT, Victoria House, 178–180 Fleet Road,<br />
Fleet, Hampshire, GU51 4DA by November 28, 2001.<br />
www.optometry.co.uk<br />
33