Download the PDF
Download the PDF
Download the PDF
You also want an ePaper? Increase the reach of your titles
YUMPU automatically turns print PDFs into web optimized ePapers that Google loves.
ot<br />
Richard G. Lindsay BScOptom, MBA, FAAO DipCL<br />
Recurrent corneal erosion syndrome<br />
Recurrent corneal erosion (RCE) syndrome is a condition which is characterised by a<br />
disturbance at <strong>the</strong> level of <strong>the</strong> corneal epi<strong>the</strong>lial basement membrane resulting in<br />
defective adhesion and recurrent breakdown of <strong>the</strong> epi<strong>the</strong>lium 1 .<br />
RCE syndrome may occur secondary to<br />
corneal injury or else spontaneously 2 . In <strong>the</strong><br />
latter case, <strong>the</strong>re is often some predisposing<br />
factor, such as diabetes or a corneal<br />
dystrophy 1-3 . Management of <strong>the</strong> problem is<br />
usually aimed at regenerating or repairing<br />
<strong>the</strong> epi<strong>the</strong>lial basement membrane so as to<br />
restore <strong>the</strong> adhesions between <strong>the</strong><br />
epi<strong>the</strong>lium and <strong>the</strong> anterior stroma.<br />
Aetiology<br />
The corneal epi<strong>the</strong>lial basement membrane<br />
complex is responsible for <strong>the</strong> tight adhesion<br />
of <strong>the</strong> epi<strong>the</strong>lial basal cell layer to <strong>the</strong><br />
underlying stroma. The primary abnormality<br />
with RCE syndrome is poor adhesion of <strong>the</strong><br />
epi<strong>the</strong>lium to Bowman’s layer due to a<br />
failure to establish or maintain normal<br />
adhesion complexes. Multiple recurrences are<br />
common, because <strong>the</strong> basal epi<strong>the</strong>lial cells<br />
require at least 8 to 12 weeks to regenerate<br />
or repair <strong>the</strong> epi<strong>the</strong>lial basement membrane 2 .<br />
The most common cause of RCE syndrome<br />
is trauma to <strong>the</strong> cornea. In <strong>the</strong>se cases,<br />
patients will generally give a history of<br />
previous oblique corneal abrasion with an<br />
object such as a fingernail, piece of paper or<br />
twig 4 . The original injury is generally well<br />
recalled by <strong>the</strong> patient as it is usually<br />
followed by several days of pain, watering<br />
and photophobia. The first recurrence may<br />
<strong>the</strong>n not occur for quite a few months after<br />
<strong>the</strong> original trauma. Epi<strong>the</strong>lial injuries where<br />
<strong>the</strong> basement membrane is preserved are<br />
unlikely to be followed by recurrent corneal<br />
erosions.<br />
RCE syndrome can also occur<br />
spontaneously, although in this situation<br />
<strong>the</strong>re is often some predisposing factor. For<br />
example, many corneal dystrophies are<br />
associated with recurrent corneal erosions.<br />
Epi<strong>the</strong>lial basement membrane dystrophy<br />
(EBMD, also known as Cogan’s microcystic<br />
dystrophy or map-dot-fingerprint dystrophy)<br />
is commonly associated with RCE syndrome,<br />
with about half <strong>the</strong> patients with recurrent<br />
epi<strong>the</strong>lial erosions exhibiting EBMD 3 . O<strong>the</strong>r<br />
corneal dystrophies which can lead to<br />
recurrent erosions include Reis-Bücklers’<br />
dystrophy (a dystrophy occurring at <strong>the</strong><br />
level of Bowman’s layer, also known as<br />
ring-shaped dystrophy), stromal dystrophies<br />
such as granular and lattice, and Fuchs’<br />
endo<strong>the</strong>lial dystrophy 4 .<br />
Spontaneous recurrent erosions, with an<br />
autosomal dominant inheritance pattern,<br />
have been described in 40 members of one<br />
family 3 . RCE syndrome also appears to be<br />
more common in patients with diabetes<br />
mellitus (due to basement membrane<br />
thickening and abnormal adhesion<br />
complexes) as well as in post-operative<br />
patients who have undergone ocular surgical<br />
procedures such as cataract extraction (with<br />
intraocular lens implantation) or refractive<br />
surgery 2 .<br />
Consequently, for patients who present<br />
with signs and symptoms of RCE syndrome, a<br />
careful history and examination of <strong>the</strong><br />
corneae should be undertaken to ensure<br />
<strong>the</strong>re are no underlying factors which may<br />
have predisposed <strong>the</strong> patient to this<br />
condition. This applies even in cases where<br />
<strong>the</strong>re is a history of injury to <strong>the</strong> cornea – a<br />
defect in <strong>the</strong> epi<strong>the</strong>lial basement membrane<br />
complex may have been present before <strong>the</strong><br />
initial trauma 3 .<br />
Presentation<br />
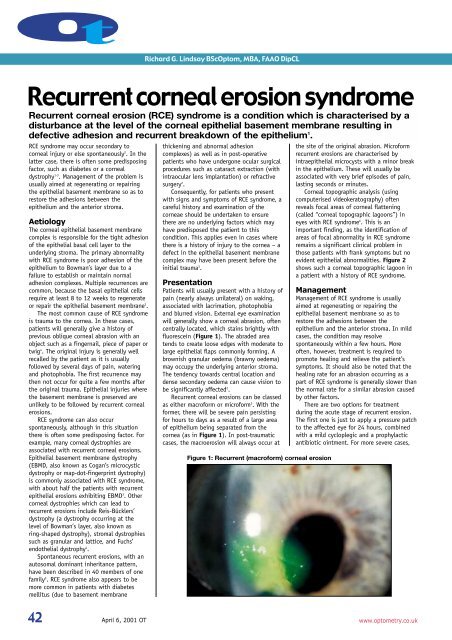
Patients will usually present with a history of<br />
pain (nearly always unilateral) on waking,<br />
associated with lacrimation, photophobia<br />
and blurred vision. External eye examination<br />
will generally show a corneal abrasion, often<br />
centrally located, which stains brightly with<br />
fluorescein (Figure 1). The abraded area<br />
tends to create loose edges with moderate to<br />
large epi<strong>the</strong>lial flaps commonly forming. A<br />
brownish granular oedema (brawny oedema)<br />
may occupy <strong>the</strong> underlying anterior stroma.<br />
The tendency towards central location and<br />
dense secondary oedema can cause vision to<br />
be significantly affected 2 .<br />
Recurrent corneal erosions can be classed<br />
as ei<strong>the</strong>r macroform or microform 5 . With <strong>the</strong><br />
former, <strong>the</strong>re will be severe pain persisting<br />
for hours to days as a result of a large area<br />
of epi<strong>the</strong>lium being separated from <strong>the</strong><br />
cornea (as in Figure 1). In post-traumatic<br />
cases, <strong>the</strong> macroerosion will always occur at<br />
Figure 1: Recurrent (macroform) corneal erosion<br />
<strong>the</strong> site of <strong>the</strong> original abrasion. Microform<br />
recurrent erosions are characterised by<br />
intraepi<strong>the</strong>lial microcysts with a minor break<br />
in <strong>the</strong> epi<strong>the</strong>lium. These will usually be<br />
associated with very brief episodes of pain,<br />
lasting seconds or minutes.<br />
Corneal topographic analysis (using<br />
computerised videokeratography) often<br />
reveals focal areas of corneal flattening<br />
(called “corneal topographic lagoons”) in<br />
eyes with RCE syndrome 6 . This is an<br />
important finding, as <strong>the</strong> identification of<br />
areas of focal abnormality in RCE syndrome<br />
remains a significant clinical problem in<br />
those patients with frank symptoms but no<br />
evident epi<strong>the</strong>lial abnormalities. Figure 2<br />
shows such a corneal topographic lagoon in<br />
a patient with a history of RCE syndrome.<br />
Management<br />
Management of RCE syndrome is usually<br />
aimed at regenerating or repairing <strong>the</strong><br />
epi<strong>the</strong>lial basement membrane so as to<br />
restore <strong>the</strong> adhesions between <strong>the</strong><br />
epi<strong>the</strong>lium and <strong>the</strong> anterior stroma. In mild<br />
cases, <strong>the</strong> condition may resolve<br />
spontaneously within a few hours. More<br />
often, however, treatment is required to<br />
promote healing and relieve <strong>the</strong> patient’s<br />
symptoms. It should also be noted that <strong>the</strong><br />
healing rate for an abrasion occurring as a<br />
part of RCE syndrome is generally slower than<br />
<strong>the</strong> normal rate for a similar abrasion caused<br />
by o<strong>the</strong>r factors.<br />
There are two options for treatment<br />
during <strong>the</strong> acute stage of recurrent erosion.<br />
The first one is just to apply a pressure patch<br />
to <strong>the</strong> affected eye for 24 hours, combined<br />
with a mild cycloplegic and a prophylactic<br />
antibiotic ointment. For more severe cases,<br />
42<br />
April 6, 2001 OT<br />
www.optometry.co.uk
where <strong>the</strong>re is extensive disadhesion of <strong>the</strong><br />
epi<strong>the</strong>lium, mechanical debridement of <strong>the</strong><br />
loose epi<strong>the</strong>lium is required. Debridement<br />
provides for a smoo<strong>the</strong>r epi<strong>the</strong>lial basement<br />
membrane which can <strong>the</strong>n be resurfaced with<br />
a healthy epi<strong>the</strong>lium. Debridement of loose<br />
epi<strong>the</strong>lium assists healing and resolves pain<br />
sooner, but does nothing to prevent<br />
recurrences. This is not that surprising, as<br />
with RCE syndrome <strong>the</strong> problem is more one<br />
of epi<strong>the</strong>lial adherence ra<strong>the</strong>r than epi<strong>the</strong>lial<br />
resurfacing 3 . Pressure patching will always be<br />
required following debridement and it is<br />
often suggested that <strong>the</strong> patient should be<br />
patched bilaterally to completely immobilise<br />
<strong>the</strong> eyes 2 . Patching should only be done for<br />
up to 72 hours and if <strong>the</strong> corneal abrasion<br />
has not resolved within this time, <strong>the</strong>n <strong>the</strong><br />
use of a <strong>the</strong>rapeutic (bandage) soft contact<br />
lens should be considered.<br />
Prophylactic treatment of RCE syndrome is<br />
aimed more at preventing recurrences of <strong>the</strong><br />
corneal erosions. Fluid accumulating beneath<br />
<strong>the</strong> epi<strong>the</strong>lium during <strong>the</strong> night – caused by<br />
<strong>the</strong> tears becoming hypotonic during sleep –<br />
leading to disadhesion of <strong>the</strong> epi<strong>the</strong>lium,<br />
and adherence of <strong>the</strong> epi<strong>the</strong>lium to <strong>the</strong><br />
tarsal conjunctiva, are thought to be <strong>the</strong> two<br />
major factors leading to recurrence.<br />
A lubricating ointment – such as<br />
Lacrilube® (Allergan) – can be used as a<br />
prophylactic treatment in <strong>the</strong> management of<br />
RCE syndrome, through application at<br />
bedtime to prevent adhesion between <strong>the</strong><br />
corneal epi<strong>the</strong>lium and <strong>the</strong> eyelid during<br />
sleep 3 . However, using just a lubricating<br />
agent as a prophylactic treatment for RCE<br />
syndrome may not always be successful, as<br />
this does little to prevent <strong>the</strong> fluid intake by<br />
<strong>the</strong> cornea during <strong>the</strong> night, which is<br />
generally believed to cause <strong>the</strong> disadhesion<br />
of <strong>the</strong> epi<strong>the</strong>lium 3,5 . In view of this, an<br />
alternative approach to prophylaxis is to use<br />
an ophthalmic ointment, such as Muro 128®<br />
(Bausch & Lomb), which also incorporates a<br />
hypertonic agent to promote corneal<br />
desiccation.<br />
Ano<strong>the</strong>r form of prophylaxis for RCE<br />
syndrome is to use a bandage contact lens.<br />
This form of treatment will generally be<br />
adopted when application of <strong>the</strong> hypertonic<br />
ointment (or drops) has been unsuccessful in<br />
preventing recurrences. A thin medium to<br />
high-water content, loosely fitting<br />
<strong>the</strong>rapeutic soft contact lens worn on a<br />
continuous (extended wear) basis for at least<br />
two months will protect <strong>the</strong> epi<strong>the</strong>lium while<br />
it reattaches itself to <strong>the</strong> basement<br />
membrane. The new silicone hydrogel contact<br />
lenses – with <strong>the</strong>ir greatly increased oxygen<br />
transmissibility – are also a good option in<br />
this regard, as <strong>the</strong>y have <strong>the</strong> potential to<br />
promote faster corneal healing through <strong>the</strong><br />
delivery of higher levels of oxygen to <strong>the</strong><br />
cornea during extended wear.<br />
The wearing of a <strong>the</strong>rapeutic contact lens<br />
may precipitate corneal erosions in some<br />
patients. The o<strong>the</strong>r major problem with this<br />
form of treatment relates to <strong>the</strong> risks<br />
associated with <strong>the</strong> extended wear of a soft<br />
contact lens 7 , especially when that lens is<br />
worn continuously for 60 days or more. In<br />
particular, <strong>the</strong> risk of corneal infection is<br />
greatly increased by <strong>the</strong> wearing of a soft<br />
contact lens on a continuous basis 8 , so<br />
consideration should be given to using a<br />
prophylactic antibiotic medication in<br />
combination with <strong>the</strong> contact lens for <strong>the</strong><br />
duration of <strong>the</strong> extended wear.<br />
The nightly administration of an<br />
ophthalmic ointment or eyedrop (preferably<br />
<strong>the</strong> former), which incorporates both a<br />
lubricating agent (to prevent adhesion<br />
between <strong>the</strong> corneal epi<strong>the</strong>lium and <strong>the</strong><br />
eyelid) and a hypertonic agent (to produce<br />
corneal desiccation), is certainly a more<br />
conservative treatment option with less<br />
associated risk compared to a bandage<br />
contact lens used on an extended wear basis.<br />
To be successful, patients should be advised<br />
that application of <strong>the</strong> ointment may need<br />
to be continued for a period of between 4 to<br />
12 weeks.<br />
In severe cases, where nei<strong>the</strong>r a bandage<br />
contact lens or a hypertonic agent is<br />
successful in preventing frequent recurrences,<br />
<strong>the</strong>re are a number of o<strong>the</strong>r treatment<br />
options. Anterior stromal puncture is very<br />
effective in managing post-traumatic<br />
macroerosions. Multiple micropunctures made<br />
in <strong>the</strong> anterior stroma incite focal scarring<br />
leading to more secure epi<strong>the</strong>lial adhesion.<br />
Alternatively, superficial epi<strong>the</strong>lial<br />
keratectomy involves debriding <strong>the</strong><br />
epi<strong>the</strong>lium, usually just in <strong>the</strong> affected area,<br />
also with subsequent scarification. The<br />
resultant scarring with <strong>the</strong>se procedures<br />
means that treatment near or on <strong>the</strong> visual<br />
axis should be avoided if possible 1,3 .<br />
Photo<strong>the</strong>rapeutic keratectomy (PTK) is<br />
often effective when ano<strong>the</strong>r treatment has<br />
failed. PTK can be used in resistant cases of<br />
recurrent erosions to smooth <strong>the</strong><br />
subepi<strong>the</strong>lial corneal surface, creating a<br />
substrate more conducive to epi<strong>the</strong>lial<br />
migration and adhesion 9 . The treatment<br />
involves mechanical debridement of <strong>the</strong><br />
epi<strong>the</strong>lium followed by a plano ablation of<br />
usually less than 10 microns. This may be<br />
combined with a refractive ablation in<br />
suitable ametropic patients. The ablation<br />
zone diameter is generally determined by <strong>the</strong><br />
Figure 2:<br />
Computerised videokeratography<br />
showing a typical topographic<br />
lagoon – a small focal (blue) area of<br />
corneal flattening just slightly<br />
superotemporal to <strong>the</strong> corneal vertex –<br />
in a patient with RCE syndrome<br />
extent of changes to <strong>the</strong> epi<strong>the</strong>lial basement<br />
membrane.<br />
The prognosis for a patient with RCE<br />
syndrome is generally quite good. The<br />
condition will usually heal if <strong>the</strong> underlying<br />
cause is properly diagnosed and remediated<br />
(if this is possible). If <strong>the</strong> condition is<br />
chronic, <strong>the</strong> patient must be instructed on<br />
appropriate prophylactic measures and<br />
advised of <strong>the</strong> need for indefinite<br />
continuation of procedures. Most<br />
importantly, patients should be reassured<br />
that most cases of RCE heal eventually or are<br />
controllable without visual loss.<br />
About <strong>the</strong> author<br />
Richard G. Lindsay is a Senior Fellow at <strong>the</strong><br />
Department of Optometry and Vision<br />
Sciences, University of Melbourne, Victoria,<br />
Australia, and an optometrist in private<br />
practice in East Melbourne.<br />
References<br />
1. Kanski, J. (1994) ‘Clinical<br />
Ophthalmology’. 3rd ed. Butterworths,<br />
London, 135-136.<br />
2. Catania, L. (1995) ‘Primary Care of <strong>the</strong><br />
Anterior Segment’. 2nd ed. Appleton &<br />
Lange, Conneticut, 237-241.<br />
3. Brown, N. and Bron, A. (1976)<br />
“Recurrent erosion of <strong>the</strong> cornea”. Brit.<br />
J. Ophthal. 60: 84-96.<br />
4. Waring, G.O., Rodrigues, M.M. and<br />
Laibson, P.R. (1978) “Corneal<br />
dystrophies. 1. Dystrophies of <strong>the</strong><br />
epi<strong>the</strong>lium, Bowman’s layer and stroma”.<br />
Surv. Ophthalmol. 23: 71-122.<br />
5. Chandler, P.A. (1945) “Recurrent erosion<br />
of <strong>the</strong> cornea”. Am. J. Ophthalmol.<br />
28: 355-367.<br />
6. McGhee, C.N.J., Bryce, I.G., Anastas, C.N.,<br />
Webber, S.K., Burvill, M. and Murray, A.T.<br />
(1996) “Corneal topographic lagoons: a<br />
potential new marker for post-traumatic<br />
recurrent corneal erosion syndrome”. Aust.<br />
NZ J. Ophthal. 24: 27-31.<br />
7. Bruce, A.S. and Brennan, N.A. (1990)<br />
“Corneal pathophysiology with contact<br />
lens wear”. Surv. Ophthalmol. 35: 25-58.<br />
8. Brennan, N.A. and Coles, M.L.C. (1997)<br />
“Extended wear in perspective”. Optom.<br />
Vis. Sci. 74: 609-623.<br />
9. Harkins, T. (1995) “The excimer laser and<br />
photo<strong>the</strong>rapeutic keratectomy”.<br />
Clin. Eye Vis. Care 7: 103-106.<br />
www.optometry.co.uk 43