Download the PDF
Download the PDF
Download the PDF
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
where <strong>the</strong>re is extensive disadhesion of <strong>the</strong><br />
epi<strong>the</strong>lium, mechanical debridement of <strong>the</strong><br />
loose epi<strong>the</strong>lium is required. Debridement<br />
provides for a smoo<strong>the</strong>r epi<strong>the</strong>lial basement<br />
membrane which can <strong>the</strong>n be resurfaced with<br />
a healthy epi<strong>the</strong>lium. Debridement of loose<br />
epi<strong>the</strong>lium assists healing and resolves pain<br />
sooner, but does nothing to prevent<br />
recurrences. This is not that surprising, as<br />
with RCE syndrome <strong>the</strong> problem is more one<br />
of epi<strong>the</strong>lial adherence ra<strong>the</strong>r than epi<strong>the</strong>lial<br />
resurfacing 3 . Pressure patching will always be<br />
required following debridement and it is<br />
often suggested that <strong>the</strong> patient should be<br />
patched bilaterally to completely immobilise<br />
<strong>the</strong> eyes 2 . Patching should only be done for<br />
up to 72 hours and if <strong>the</strong> corneal abrasion<br />
has not resolved within this time, <strong>the</strong>n <strong>the</strong><br />
use of a <strong>the</strong>rapeutic (bandage) soft contact<br />
lens should be considered.<br />
Prophylactic treatment of RCE syndrome is<br />
aimed more at preventing recurrences of <strong>the</strong><br />
corneal erosions. Fluid accumulating beneath<br />
<strong>the</strong> epi<strong>the</strong>lium during <strong>the</strong> night – caused by<br />
<strong>the</strong> tears becoming hypotonic during sleep –<br />
leading to disadhesion of <strong>the</strong> epi<strong>the</strong>lium,<br />
and adherence of <strong>the</strong> epi<strong>the</strong>lium to <strong>the</strong><br />
tarsal conjunctiva, are thought to be <strong>the</strong> two<br />
major factors leading to recurrence.<br />
A lubricating ointment – such as<br />
Lacrilube® (Allergan) – can be used as a<br />
prophylactic treatment in <strong>the</strong> management of<br />
RCE syndrome, through application at<br />
bedtime to prevent adhesion between <strong>the</strong><br />
corneal epi<strong>the</strong>lium and <strong>the</strong> eyelid during<br />
sleep 3 . However, using just a lubricating<br />
agent as a prophylactic treatment for RCE<br />
syndrome may not always be successful, as<br />
this does little to prevent <strong>the</strong> fluid intake by<br />
<strong>the</strong> cornea during <strong>the</strong> night, which is<br />
generally believed to cause <strong>the</strong> disadhesion<br />
of <strong>the</strong> epi<strong>the</strong>lium 3,5 . In view of this, an<br />
alternative approach to prophylaxis is to use<br />
an ophthalmic ointment, such as Muro 128®<br />
(Bausch & Lomb), which also incorporates a<br />
hypertonic agent to promote corneal<br />
desiccation.<br />
Ano<strong>the</strong>r form of prophylaxis for RCE<br />
syndrome is to use a bandage contact lens.<br />
This form of treatment will generally be<br />
adopted when application of <strong>the</strong> hypertonic<br />
ointment (or drops) has been unsuccessful in<br />
preventing recurrences. A thin medium to<br />
high-water content, loosely fitting<br />
<strong>the</strong>rapeutic soft contact lens worn on a<br />
continuous (extended wear) basis for at least<br />
two months will protect <strong>the</strong> epi<strong>the</strong>lium while<br />
it reattaches itself to <strong>the</strong> basement<br />
membrane. The new silicone hydrogel contact<br />
lenses – with <strong>the</strong>ir greatly increased oxygen<br />
transmissibility – are also a good option in<br />
this regard, as <strong>the</strong>y have <strong>the</strong> potential to<br />
promote faster corneal healing through <strong>the</strong><br />
delivery of higher levels of oxygen to <strong>the</strong><br />
cornea during extended wear.<br />
The wearing of a <strong>the</strong>rapeutic contact lens<br />
may precipitate corneal erosions in some<br />
patients. The o<strong>the</strong>r major problem with this<br />
form of treatment relates to <strong>the</strong> risks<br />
associated with <strong>the</strong> extended wear of a soft<br />
contact lens 7 , especially when that lens is<br />
worn continuously for 60 days or more. In<br />
particular, <strong>the</strong> risk of corneal infection is<br />
greatly increased by <strong>the</strong> wearing of a soft<br />
contact lens on a continuous basis 8 , so<br />
consideration should be given to using a<br />
prophylactic antibiotic medication in<br />
combination with <strong>the</strong> contact lens for <strong>the</strong><br />
duration of <strong>the</strong> extended wear.<br />
The nightly administration of an<br />
ophthalmic ointment or eyedrop (preferably<br />
<strong>the</strong> former), which incorporates both a<br />
lubricating agent (to prevent adhesion<br />
between <strong>the</strong> corneal epi<strong>the</strong>lium and <strong>the</strong><br />
eyelid) and a hypertonic agent (to produce<br />
corneal desiccation), is certainly a more<br />
conservative treatment option with less<br />
associated risk compared to a bandage<br />
contact lens used on an extended wear basis.<br />
To be successful, patients should be advised<br />
that application of <strong>the</strong> ointment may need<br />
to be continued for a period of between 4 to<br />
12 weeks.<br />
In severe cases, where nei<strong>the</strong>r a bandage<br />
contact lens or a hypertonic agent is<br />
successful in preventing frequent recurrences,<br />
<strong>the</strong>re are a number of o<strong>the</strong>r treatment<br />
options. Anterior stromal puncture is very<br />
effective in managing post-traumatic<br />
macroerosions. Multiple micropunctures made<br />
in <strong>the</strong> anterior stroma incite focal scarring<br />
leading to more secure epi<strong>the</strong>lial adhesion.<br />
Alternatively, superficial epi<strong>the</strong>lial<br />
keratectomy involves debriding <strong>the</strong><br />
epi<strong>the</strong>lium, usually just in <strong>the</strong> affected area,<br />
also with subsequent scarification. The<br />
resultant scarring with <strong>the</strong>se procedures<br />
means that treatment near or on <strong>the</strong> visual<br />
axis should be avoided if possible 1,3 .<br />
Photo<strong>the</strong>rapeutic keratectomy (PTK) is<br />
often effective when ano<strong>the</strong>r treatment has<br />
failed. PTK can be used in resistant cases of<br />
recurrent erosions to smooth <strong>the</strong><br />
subepi<strong>the</strong>lial corneal surface, creating a<br />
substrate more conducive to epi<strong>the</strong>lial<br />
migration and adhesion 9 . The treatment<br />
involves mechanical debridement of <strong>the</strong><br />
epi<strong>the</strong>lium followed by a plano ablation of<br />
usually less than 10 microns. This may be<br />
combined with a refractive ablation in<br />
suitable ametropic patients. The ablation<br />
zone diameter is generally determined by <strong>the</strong><br />
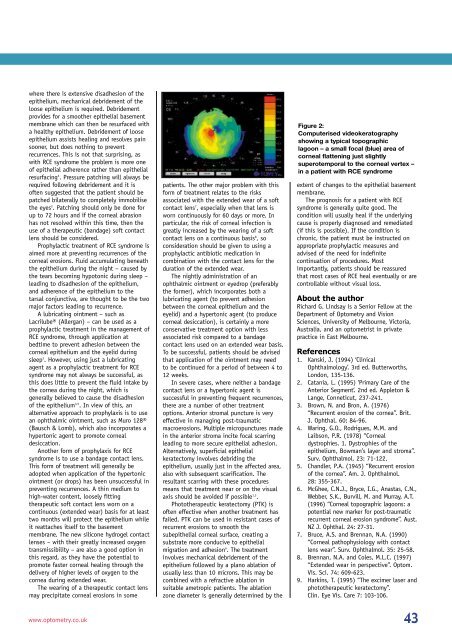
Figure 2:<br />
Computerised videokeratography<br />
showing a typical topographic<br />
lagoon – a small focal (blue) area of<br />
corneal flattening just slightly<br />
superotemporal to <strong>the</strong> corneal vertex –<br />
in a patient with RCE syndrome<br />
extent of changes to <strong>the</strong> epi<strong>the</strong>lial basement<br />
membrane.<br />
The prognosis for a patient with RCE<br />
syndrome is generally quite good. The<br />
condition will usually heal if <strong>the</strong> underlying<br />
cause is properly diagnosed and remediated<br />
(if this is possible). If <strong>the</strong> condition is<br />
chronic, <strong>the</strong> patient must be instructed on<br />
appropriate prophylactic measures and<br />
advised of <strong>the</strong> need for indefinite<br />
continuation of procedures. Most<br />
importantly, patients should be reassured<br />
that most cases of RCE heal eventually or are<br />
controllable without visual loss.<br />
About <strong>the</strong> author<br />
Richard G. Lindsay is a Senior Fellow at <strong>the</strong><br />
Department of Optometry and Vision<br />
Sciences, University of Melbourne, Victoria,<br />
Australia, and an optometrist in private<br />
practice in East Melbourne.<br />
References<br />
1. Kanski, J. (1994) ‘Clinical<br />
Ophthalmology’. 3rd ed. Butterworths,<br />
London, 135-136.<br />
2. Catania, L. (1995) ‘Primary Care of <strong>the</strong><br />
Anterior Segment’. 2nd ed. Appleton &<br />
Lange, Conneticut, 237-241.<br />
3. Brown, N. and Bron, A. (1976)<br />
“Recurrent erosion of <strong>the</strong> cornea”. Brit.<br />
J. Ophthal. 60: 84-96.<br />
4. Waring, G.O., Rodrigues, M.M. and<br />
Laibson, P.R. (1978) “Corneal<br />
dystrophies. 1. Dystrophies of <strong>the</strong><br />
epi<strong>the</strong>lium, Bowman’s layer and stroma”.<br />
Surv. Ophthalmol. 23: 71-122.<br />
5. Chandler, P.A. (1945) “Recurrent erosion<br />
of <strong>the</strong> cornea”. Am. J. Ophthalmol.<br />
28: 355-367.<br />
6. McGhee, C.N.J., Bryce, I.G., Anastas, C.N.,<br />
Webber, S.K., Burvill, M. and Murray, A.T.<br />
(1996) “Corneal topographic lagoons: a<br />
potential new marker for post-traumatic<br />
recurrent corneal erosion syndrome”. Aust.<br />
NZ J. Ophthal. 24: 27-31.<br />
7. Bruce, A.S. and Brennan, N.A. (1990)<br />
“Corneal pathophysiology with contact<br />
lens wear”. Surv. Ophthalmol. 35: 25-58.<br />
8. Brennan, N.A. and Coles, M.L.C. (1997)<br />
“Extended wear in perspective”. Optom.<br />
Vis. Sci. 74: 609-623.<br />
9. Harkins, T. (1995) “The excimer laser and<br />
photo<strong>the</strong>rapeutic keratectomy”.<br />
Clin. Eye Vis. Care 7: 103-106.<br />
www.optometry.co.uk 43