Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
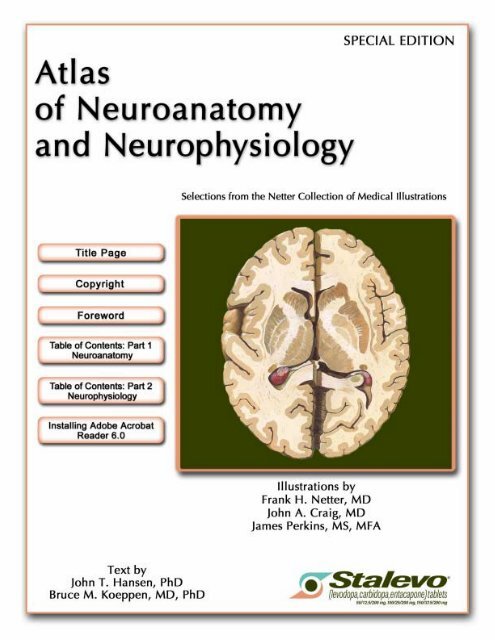
<strong>Atlas</strong> of<br />
<strong>Neuro</strong>anatomy and<br />
<strong>Neuro</strong>physiology<br />
Selections from the Netter Collection of Medical Illustrations<br />
Illustrations by<br />
Frank H. Netter, MD<br />
John A. Craig, MD<br />
James Perkins, MS, MFA<br />
Text by<br />
John T. Hansen, PhD<br />
Bruce M. Koeppen, MD, PhD
<strong>Atlas</strong> of <strong>Neuro</strong>anatomy and <strong>Neuro</strong>physiology<br />
Selections from the Netter Collection of Medical Illustrations<br />
Copyright ©2004 Icon Custom Communications. All rights reserved.<br />
The contents of this book may not be reproduced in any form without written<br />
authorization from Icon Custom Communications. Requests for permission<br />
should be addressed to Permissions Department, Icon Custom Communications,<br />
295 North St., Teterboro NJ 07608, or can be made at www. Netterart.com.<br />
NOTICE<br />
Every effort has been taken to confirm the accuracy of the information presented.<br />
Novartis, the publisher or the authors cannot be held responsible for errors or for<br />
any consequences arising from the use of the information contained herein, and<br />
make no warranty, expressed or implied, with respect to the contents of the publication.<br />
Printed in U.S.A.
Foreword<br />
Frank Netter: The Physician, The Artist, The Art<br />
This selection of the art of Dr. Frank H. Netter on neuroanatomy and neurophysiology is drawn<br />
from the <strong>Atlas</strong> of Human Anatomy and Netter’s <strong>Atlas</strong> of Human Physiology. Viewing these pictures<br />
again prompts reflection on Dr. Netter’s work and his roles as physician and artist.<br />
Frank H. Netter was born in 1906 in New York City. He pursued his artistic muse at the Sorbonne,<br />
the Art Student’s League, and the National Academy of Design before entering medical school at<br />
New York University, where he received his M.D. degree in 1931. During his student years, Dr.<br />
Netter’s notebook sketches attracted the attention of the medical faculty and other physicians, allowing<br />
him to augment his income by illustrating articles and textbooks. He continued illustrating as a<br />
sideline after establishing a surgical practice in 1933, but ultimately opted to give up his practice in<br />
favor of a full-time commitment to art. After service in the United States Army during the Second<br />
World War, Dr. Netter began his long collaboration with the CIBA Pharmaceutical Company (now<br />
Novartis Pharmaceuticals). This 45-year partnership resulted in the production of the extraordinary<br />
collection of medical art so familiar to physicians and other medical professionals worldwide.<br />
When Dr. Netter’s work is discussed, attention is focused primarily on Netter the artist and only<br />
secondarily on Netter the physician. As a student of Dr. Netter’s work for more than forty years, I can<br />
say that the true strength of a Netter illustration was always established well before brush was laid to<br />
paper. In that respect each plate is more of an intellectual than an artistic or aesthetic exercise. It is<br />
easy to appreciate the aesthetic qualities of Dr. Netter’s work, but to overlook its intellectual qualities<br />
is to miss the real strength and intent of the art. This intellectual process requires thorough understanding<br />
of the topic, as Dr. Netter wrote: “Strange as it may seem, the hardest part of making a medical<br />
picture is not the drawing at all. It is the planning, the conception, the determination of point of<br />
view and the approach which will best clarify the subject which takes the most effort.”<br />
Years before the inception of “the integrated curriculum,” Netter the physician realized that a<br />
good medical illustration can include clinical information and physiologic functions as well as anatomy.<br />
In pursuit of this principle Dr. Netter often integrates pertinent basic and clinical science elements<br />
in his anatomic interpretations. Although he was chided for this heresy by a prominent<br />
European anatomy professor, many generations of students training to be physicians rather than<br />
anatomists have appreciated Dr. Netter’s concept.<br />
The integration of physiology and clinical medicine with anatomy has led Dr. Netter to another,<br />
more subtle, choice in his art. Many texts and atlases published during the period of Dr. Netter’s<br />
career depict anatomy clearly based on cadaver specimens with renderings of shrunken and shriveled<br />
tissues and organs. Netter the physician chose to render “live” versions of these structures—not<br />
shriveled, colorless, formaldehyde-soaked tissues, but plump, robust organs, glowing with color!<br />
The value of Dr. Netter’s approach is clearly demonstrated by the plates in this selection.<br />
John A. Craig, MD<br />
Austin, Texas
This volume brings together two distinct but related aspects of the work of Frank<br />
H. Netter, MD, and associated artists. Netter is best known as the creator of the<br />
<strong>Atlas</strong> of Human Anatomy, a comprehensive textbook of gross anatomy that has<br />
become the standard atlas for students of the subject. But Netter’s work included<br />
far more than anatomical art. In the pages of Clinical Symposia, a series of monographs<br />
published over a period of more than 50 years, and in The Netter Collection<br />
of Medical Illustrations, this premier medical artist created superb illustrations of<br />
biological and physiological processes, disease pathology, clinical presentations,<br />
and medical procedures.<br />
As a service to the medical community, Novartis Pharma has commissioned this<br />
special edition of Netter’s work, which includes his beautiful and instructive illustrations<br />
of nervous system anatomy as well as his depictions of neurophysiological<br />
concepts and functions. We hope that readers will find Dr. Netter’s renderings of<br />
neurological form and function interesting and useful.
Part 1 <strong>Neuro</strong>anatomy<br />
Cerebrum—Medial Views . . . . . . . . . . . . . . . . . 2<br />
Cerebrum—Inferior View. . . . . . . . . . . . . . . . . . 3<br />
Basal Nuclei (Ganglia). . . . . . . . . . . . . . . . . . . . 4<br />
Thalamus . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 5<br />
Cerebellum . . . . . . . . . . . . . . . . . . . . . . . . . . . . 6<br />
Brainstem. . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 7<br />
Fourth Ventricle and Cerebellum . . . . . . . . . . . 8<br />
Accessory Nerve (XI) . . . . . . . . . . . . . . . . . . . . 9<br />
Arteries to Brain and Meninges . . . . . . . . . . . 10<br />
Arteries to Brain: Schema . . . . . . . . . . . . . . . . 11<br />
Arteries of Brain: Inferior Views . . . . . . . . . . . 12<br />
Cerebral Arterial Circle (Willis) . . . . . . . . . . . 13<br />
Arteries of Brain: Frontal View and Section . . 14<br />
Arteries of Brain:<br />
Lateral and Medial Views. . . . . . . . . . . . . . . 15<br />
Arteries of Posterior Cranial Fossa . . . . . . . . . 16<br />
Veins of Posterior Cranial Fossa . . . . . . . . . . . 17<br />
Deep Veins of Brain. . . . . . . . . . . . . . . . . . . . . 18<br />
Subependymal Veins of Brain . . . . . . . . . . . . . 19<br />
Hypothalamus and Hypophysis . . . . . . . . . . . 20<br />
Arteries and Veins<br />
of Hypothalamus and Hypophysis . . . . . . . . 21<br />
Relation of Spinal Nerve Roots to Vertebrae . . . 22<br />
Autonomic Nervous System:<br />
General Topography. . . . . . . . . . . . . . . . . . . 23<br />
Spinal Nerve Origin: Cross Sections. . . . . . . . 24<br />
Olfactory Nerve (I): Schema . . . . . . . . . . . . . . 25<br />
Optic Nerve (II)<br />
(Visual Pathway): Schema . . . . . . . . . . . . . . 26<br />
Oculomotor (III), Trochlear (IV)<br />
and Abducent (VI) Nerves: Schema. . . . . . . 27<br />
Trigeminal Nerve (V): Schema . . . . . . . . . . . . 28<br />
Facial Nerve (VII): Schema . . . . . . . . . . . . . . . 29<br />
Vestibulocochlear Nerve (VIII): Schema. . . . . 30<br />
Glossopharyngeal Nerve (IX): Schema . . . . . . 31<br />
Vagus Nerve (X): Schema . . . . . . . . . . . . . . . . 32<br />
Accessory Nerve (XI): Schema . . . . . . . . . . . . 33<br />
Hypoglossal Nerve (XII): Schema . . . . . . . . . . 34<br />
Nerves of Heart . . . . . . . . . . . . . . . . . . . . . . . . 35<br />
Autonomic Nerves<br />
and Ganglia of Abdomen. . . . . . . . . . . . . . . 36<br />
Nerves of Stomach and Duodenum . . . . . . . . 37<br />
Nerves of Stomach<br />
and Duodenum (continued) . . . . . . . . . . . . 38<br />
Nerves of Small Intestine . . . . . . . . . . . . . . . . 39<br />
Nerves of Large Intestine . . . . . . . . . . . . . . . . 40<br />
Nerves of Kidneys,<br />
Ureters and Urinary Bladder . . . . . . . . . . . . 41<br />
Nerves of Pelvic Viscera: Male . . . . . . . . . . . . 42<br />
Nerves of Pelvic Viscera: Female . . . . . . . . . . 43<br />
Median Nerve . . . . . . . . . . . . . . . . . . . . . . . . . 44<br />
Ulnar Nerve . . . . . . . . . . . . . . . . . . . . . . . . . . . 45<br />
Radial Nerve in Arm<br />
and Nerves of Posterior Shoulder . . . . . . . . 46<br />
Radial Nerve in Forearm . . . . . . . . . . . . . . . . . 47<br />
Sciatic Nerve and Posterior<br />
Cutaneous Nerve of Thigh . . . . . . . . . . . . . . 48<br />
Tibial Nerve . . . . . . . . . . . . . . . . . . . . . . . . . . . 49<br />
Common Fibular (Peroneal) Nerve. . . . . . . . . 50
NEUROANATOMY<br />
Cerebrum: Medial Views<br />
Sagittal section of<br />
Cingulate gyrus<br />
brain in situ<br />
Cingulate sulcus<br />
Medial frontal gyrus<br />
Sulcus of corpus callosum<br />
Fornix<br />
Septum pellucidum<br />
Interventricular<br />
foramen (Monro)<br />
Interthalamic<br />
adhesion<br />
Thalamus and<br />
3rd ventricle<br />
Subcallosal<br />
(parolfactory)<br />
area<br />
Anterior<br />
commissure<br />
Subcallosal<br />
gyrus<br />
Hypothalamic<br />
sulcus<br />
Lamina<br />
terminalis<br />
Supraoptic<br />
recess<br />
Optic chiasm<br />
Tuber cinereum<br />
Hypophysis (pituitary gland)<br />
Mammillary body<br />
Cerebral peduncle<br />
Pons<br />
Medial surface of cerebral<br />
hemisphere: brainstem excised<br />
Cingulate gyrus<br />
Mammillothalamic<br />
fasciculus<br />
Mammillary body<br />
Uncus<br />
Optic nerve (II)<br />
Olfactory tract<br />
Collateral sulcus<br />
Rhinal sulcus<br />
Medial occipitotemporal gyrus<br />
Occipitotemporal sulcus<br />
Lateral occipitotemporal gyrus<br />
Paracentral sulcus<br />
Central sulcus (Rolando)<br />
Paracentral lobule<br />
Marginal sulcus<br />
Corpus callosum<br />
Precuneus<br />
Superior sagittal sinus<br />
Choroid plexus<br />
of 3rd ventricle<br />
Stria medullaris<br />
of thalamus<br />
Parietooccipital<br />
sulcus<br />
Cuneus<br />
Habenular<br />
commissure<br />
Cerebral aqueduct<br />
(Sylvius)<br />
Pineal body<br />
Posterior<br />
commissure<br />
Calcarine<br />
sulcus<br />
Straight sinus<br />
in tentorium<br />
cerebelli<br />
Great cerebral vein<br />
(Galen)<br />
Superior colliculus<br />
Inferior colliculus<br />
Tectal (quadrigeminal) plate<br />
Cerebellum<br />
Superior medullary velum<br />
4th ventricle and choroid plexus<br />
Inferior medullary velum<br />
Medulla oblongata<br />
Genu<br />
Rostrum<br />
Trunk<br />
Splenium<br />
of<br />
corpus callosum<br />
Isthmus of cingulate gyrus<br />
Parietooccipital sulcus<br />
Cuneus<br />
Calcarine sulcus<br />
Lingual gyrus<br />
Crus<br />
Body<br />
Column<br />
of fornix<br />
Fimbria of hippocampus<br />
Dentate gyrus<br />
Parahippocampal gyrus<br />
2
Cerebrum: Inferior View<br />
NEUROANATOMY<br />
Sectioned brainstem<br />
Frontal pole of cerebrum<br />
Straight gyrus<br />
Olfactory sulcus<br />
Orbital sulci<br />
Longitudinal cerebral fissure<br />
Genu of corpus callosum<br />
Lamina terminalis<br />
Olfactory bulb<br />
Orbital gyri<br />
Temporal pole<br />
Lateral sulcus (Sylvius)<br />
Inferior temporal sulcus<br />
Inferior temporal gyrus<br />
Olfactory tract<br />
Optic chiasm<br />
Optic nerve (II) (cut)<br />
Hypophysis<br />
(pituitary gland)<br />
Anterior<br />
perforated substance<br />
Optic tract<br />
Tuber cinereum<br />
Inferior (inferolateral)<br />
margin<br />
of cerebrum<br />
Rhinal sulcus<br />
Uncus<br />
Inferior<br />
temporal gyrus<br />
Occipitotemporal<br />
sulcus<br />
Lateral occipitotemporal<br />
gyrus<br />
Collateral sulcus<br />
Parahippocampal gyrus<br />
Medial occipitotemporal gyrus<br />
Calcarine sulcus<br />
Isthmus of cingulate gyrus<br />
Apex of cuneus<br />
Occipital pole of cerebrum<br />
Longitudinal cerebral fissure<br />
Cerebral aqueduct<br />
Splenium of corpus callosum<br />
Mammillary body<br />
Posterior perforated<br />
substance (in<br />
interpeduncular<br />
fossa)<br />
Cerebral crus<br />
Lateral geniculate<br />
body<br />
Substantia nigra<br />
Medial geniculate<br />
body<br />
Red nucleus<br />
Pulvinar of thalamus<br />
Superior colliculus (of<br />
corpora quadrigemina)<br />
3
NEUROANATOMY<br />
Basal Nuclei (Ganglia)<br />
Horizontal sections<br />
through cerebrum<br />
A<br />
B<br />
Genu of corpus callosum<br />
Head of caudate nucleus<br />
Lateral ventricle<br />
Septum pellucidum<br />
Anterior limb<br />
Genu<br />
Posterior limb<br />
of internal<br />
capsule<br />
Column of fornix<br />
Insula<br />
(island of Reil)<br />
Interthalamic<br />
adhesion<br />
Putamen<br />
Globus pallidus<br />
3rd ventricle<br />
External capsule<br />
Lentiform<br />
nucleus<br />
Thalamus<br />
Claustrum<br />
Crus of fornix<br />
Retrolenticular part<br />
of internal capsule<br />
Choroid plexus<br />
of lateral ventricle<br />
Tail of caudate nucleus<br />
Splenium of<br />
corpus callosum<br />
Hippocampus and fimbria<br />
Occipital (posterior) horn<br />
of lateral ventricle<br />
Habenula<br />
Organization of<br />
basal nuclei (ganglia)<br />
A<br />
B<br />
Pineal body<br />
Caudate<br />
nucleus<br />
Putamen Globus<br />
pallidus<br />
Cleft for internal capsule<br />
Striatum<br />
Corpus<br />
striatum<br />
Basal nuclei<br />
(ganglia)<br />
Lentiform<br />
nucleus<br />
Caudate<br />
nucleus<br />
Levels of<br />
sections<br />
above<br />
Body<br />
Head<br />
A<br />
B<br />
Lentiform nucleus<br />
(globus pallidus medial<br />
to putamen)<br />
Amygdaloid body<br />
Thalamus<br />
Pulvinar<br />
Medial geniculate body<br />
Lateral geniculate body<br />
Tail of caudate nucleus<br />
Interrelationship of thalamus, lentiform nucleus, caudate<br />
nucleus and amygdaloid body (schema): left lateral view<br />
A<br />
B<br />
4
Thalamus<br />
NEUROANATOMY<br />
Interventricular foramen (Monro)<br />
Tela choroidea (cut edge)<br />
of 3rd ventricle<br />
3rd ventricle<br />
Choroid plexus<br />
Superior thalamostriate vein<br />
Pes hippocampi<br />
Temporal (inferior) horn<br />
of lateral ventricle<br />
Internal cerebral vein<br />
Dentate gyrus<br />
Collateral eminence<br />
Hippocampus<br />
Fimbria of hippocampus<br />
Posterior commissure<br />
Habenular commissure<br />
Pineal body<br />
Collateral trigone<br />
Calcar avis<br />
Occipital (posterior) horn<br />
of lateral ventricle<br />
Calcarine sulcus<br />
Corpus callosum (cut)<br />
Head of caudate nucleus<br />
Septum pellucidum<br />
Columns of fornix<br />
Anterior tubercle<br />
Stria terminalis<br />
Interthalamic adhesion<br />
Lamina affixa<br />
Stria medullaris<br />
Habenular trigone<br />
Pulvinar (retracted)<br />
Lateral geniculate body<br />
Medial geniculate body<br />
Brachium of superior colliculus<br />
Brachium of inferior colliculus<br />
Superior colliculus<br />
Inferior colliculus<br />
Cerebellum<br />
Internal<br />
medullary<br />
lamina<br />
MD<br />
M<br />
CM<br />
VPM<br />
LP<br />
VPL<br />
Pulvinar<br />
Intralaminar<br />
nuclei<br />
Reticular nucleus<br />
Interthalamic<br />
adhesion<br />
3rd ventricle<br />
Internal<br />
Median<br />
Medial<br />
LP<br />
VP<br />
Lamina<br />
LD<br />
medullary lamina<br />
VPL VPM VI<br />
Anterior<br />
VL<br />
VA<br />
3rd ventricle<br />
Median nuclei<br />
External<br />
medullary<br />
lamina<br />
Schematic section<br />
through thalamus<br />
(at level of broken<br />
line shown in figure<br />
at right)<br />
Thalamic nuclei<br />
CM Centromedian<br />
LD Lateral dorsal<br />
LP Lateral posterior<br />
M Medial<br />
MD Medial dorsal<br />
VA Ventral anterior<br />
VI Ventral intermedial<br />
VL Ventral lateral<br />
VP Ventral posterior<br />
VPL Ventral posterolateral<br />
VPM Ventral posteromedial<br />
Pulvinar<br />
Lateral geniculate body<br />
Medial geniculate body<br />
Schematic representation of thalamus<br />
(external medullary lamina and<br />
reticular nuclei removed)<br />
Lateral nuclei<br />
Medial nuclei<br />
Anterior nuclei<br />
5
NEUROANATOMY<br />
Cerebellum<br />
Superior<br />
vermis<br />
Anterior cerebellar notch<br />
Central lobule (II & III)<br />
Culmen (IV & V)<br />
Declive (VI)<br />
Folium (VII A)<br />
Posterior cerebellar notch<br />
Superior surface<br />
Anterior lobe<br />
Quadrangular lobule (H IV-V)<br />
Primary fissure<br />
Horizontal fissure<br />
Simple lobule (H VI)<br />
Posterior lobe<br />
Postlunate fissure<br />
Superior semilunar<br />
(anseriform) lobule (H VII A)<br />
Horizontal fissure<br />
Inferior semilunar<br />
(caudal) lobule (H VII B)<br />
Superior vermis<br />
Central lobule<br />
Lingula (I)<br />
Superior medullary velum<br />
Flocculus (H X)<br />
4th ventricle<br />
Inferior medullary velum<br />
Inferior<br />
vermis<br />
Nodule (X)<br />
Uvula (IX)<br />
Pyramid (VIII)<br />
Tuber (VII B)<br />
Posterior cerebellar notch<br />
Inferior surface<br />
Anterior lobe<br />
Wing of central lobule<br />
Superior<br />
Middle Cerebellar peduncles<br />
Inferior<br />
Flocculonodular lobe<br />
Posterolateral (dorsolateral)<br />
fissure<br />
Retrotonsillar fissure<br />
Posterior lobe<br />
Tonsil<br />
Biventer lobule (H VIII)<br />
Secondary (postpyramidal)<br />
fissure<br />
Horizontal fissure<br />
Inferior semilunar<br />
(caudal) lobule (H VII B)<br />
Decussation of<br />
superior cerebellar peduncles<br />
4th ventricle<br />
Superior medullary velum<br />
Cerebral crus<br />
Medial longitudinal fasciculus<br />
Nuclear layer of<br />
medulla oblongata<br />
Cerebellar<br />
nuclei<br />
Fastigial<br />
Globose<br />
Dentate<br />
Emboliform<br />
Superior cerebellar<br />
peduncle<br />
Lingula (I)<br />
Vermis<br />
Section in plane of superior cerebellar peduncle<br />
6
Brainstem<br />
NEUROANATOMY<br />
Posterolateral view<br />
Pulvinars of thalami<br />
Pineal body<br />
Superior colliculi<br />
Inferior colliculi<br />
Trochlear nerve (IV)<br />
Superior medullary velum<br />
Superior cerebellar peduncle<br />
Rhomboid fossa of<br />
4th ventricle<br />
Glossopharyngeal (IX) and<br />
vagus (X) nerves<br />
Cuneate tubercle<br />
Gracile tubercle<br />
Dorsal roots of<br />
1st spinal nerve (C1)<br />
Cuneate fasciculus<br />
Gracile fasciculus<br />
Thalamus (cut surface)<br />
Lateral geniculate body<br />
Optic tract<br />
Medial geniculate body<br />
Brachia of superior and inferior colliculi<br />
Cerebral crus<br />
Pons<br />
Trigeminal nerve (V)<br />
Middle cerebellar peduncle<br />
Vestibulocochlear nerve (VIII)<br />
Facial nerve (VII)<br />
Inferior cerebellar peduncle<br />
Hypoglossal nerve (XII)<br />
Accessory nerve (XI)<br />
Olfactory tract<br />
Anterior view<br />
Optic chiasm<br />
Optic tract<br />
Tuber cinereum<br />
Cerebral crus<br />
Lateral geniculate body<br />
Posterior perforated substance<br />
Pons<br />
Middle cerebellar peduncle<br />
Olive<br />
Pyramid<br />
Ventral roots of 1st spinal nerve (C1)<br />
Decussation of pyramids<br />
Anterior perforated substance<br />
Infundibulum (pituitary stalk)<br />
Mammillary bodies<br />
Temporal lobe (cut surface)<br />
Oculomotor nerve (III)<br />
Trochlear nerve (IV)<br />
Trigeminal nerve (V)<br />
Abducent nerve (VI)<br />
Facial nerve (VII) and<br />
intermediate nerve<br />
Vestibulocochlear nerve (VIII)<br />
Flocculus of cerebellum<br />
Choroid plexus of 4th<br />
ventricle<br />
Glossopharyngeal nerve (IX)<br />
Vagus nerve (X)<br />
Hypoglossal nerve (XII)<br />
Accessory nerve (XI)<br />
7
NEUROANATOMY<br />
Fourth Ventricle and Cerebellum<br />
Posterior view<br />
3rd ventricle<br />
Pulvinar of thalamus<br />
Pineal body<br />
Superior colliculus<br />
Inferior colliculus<br />
Trochlear nerve (IV)<br />
Superior medullary velum<br />
Superior<br />
Cerebellar peduncles Middle<br />
Inferior<br />
Lateral recess<br />
Superior fovea<br />
Sulcus limitans<br />
Inferior fovea<br />
Trigeminal tubercle<br />
Hypoglossal trigone<br />
Vagal trigone<br />
Obex<br />
Gracile fasciculus<br />
Habenular trigone<br />
Medial<br />
Geniculate bodies<br />
Lateral<br />
Dorsal median sulcus<br />
Superior cerebellar peduncle<br />
Locus ceruleus<br />
Medial eminence<br />
Facial colliculus<br />
Vestibular area<br />
Lateral funiculus<br />
Cuneate fasciculus<br />
Dentate nucleus<br />
of cerebellum<br />
Striae medullares<br />
Tenia of 4th ventricle<br />
Cuneate tubercle<br />
Gracile tubercle<br />
Dorsal median sulcus<br />
Median sagittal section<br />
Body of fornix<br />
Thalamus (in<br />
3rd ventricle)<br />
Interventricular<br />
foramen (Monro)<br />
Anterior commissure<br />
Lamina terminalis<br />
Hypothalamic sulcus<br />
Cerebral peduncle<br />
Cerebral aqueduct (Sylvius)<br />
Superior colliculus<br />
Tectal (quadrigeminal) plate<br />
Inferior colliculus<br />
Pons<br />
Medial longitudinal fasciculus<br />
4th ventricle<br />
Choroid plexus of 4th ventricle<br />
Medulla oblongata<br />
Median aperture (foramen of Magendie)<br />
Decussation of pyramids<br />
Central canal of spinal cord<br />
Interthalamic adhesion<br />
Posterior commissure<br />
Habenular commissure<br />
Pineal body<br />
Splenium of corpus callosum<br />
Great cerebral vein (Galen)<br />
Choroid plexus of 4th ventricle<br />
Tonsil of cerebellum<br />
Lingula (I)<br />
Central lobule (II-III)<br />
Culmen (IV-V)<br />
Declive (VI)<br />
Folium (VII A)<br />
Superior medullary velum<br />
Inferior medullary velum<br />
Tuber (VII B)<br />
Pyramid (VIII)<br />
Uvula (IX)<br />
Nodulus (X)<br />
Vermis of<br />
cerebellum<br />
Vermis of<br />
cerebellum<br />
8
Accessory Nerve (XI): Schema<br />
NEUROANATOMY<br />
Nucleus ambiguus<br />
Vagus nerve (X)<br />
Cranial root of accessory nerve (joins vagus nerve<br />
and via recurrent laryngeal nerve supplies muscles of<br />
larynx, except cricothyroid)*<br />
Spinal root of<br />
accessory nerve<br />
Jugular foramen<br />
Foramen<br />
magnum<br />
Superior ganglion<br />
of vagus nerve<br />
Accessory nerve (XI)*<br />
Inferior ganglion<br />
of vagus nerve<br />
C1 spinal nerve<br />
C2 spinal nerve<br />
Accessory nerve<br />
(to sternocleidomastoid<br />
and trapezius muscles)<br />
Sternocleidomastoid muscle (cut)<br />
C3 spinal nerve<br />
C4 spinal nerve<br />
Trapezius muscle<br />
*Recent evidence suggests that the accessory nerve lacks a cranial root and has no connection to the vagus nerve.<br />
Verification of this finding awaits further investigation.<br />
Efferent fibers<br />
Proprioceptive fibers<br />
9
NEUROANATOMY<br />
Arteries to Brain and Meninges<br />
Mastoid branch of<br />
left occipital artery<br />
Anterior inferior<br />
cerebellar artery<br />
Posterior inferior<br />
cerebellar artery<br />
Left middle meningeal artery<br />
Posterior cerebral artery<br />
Superior cerebellar artery<br />
Basilar artery<br />
Left labyrinthine<br />
(internal acoustic) artery<br />
Posterior meningeal<br />
branch of left ascending<br />
pharyngeal artery<br />
Left and right<br />
vertebral arteries<br />
(intracranial part)<br />
Posterior meningeal<br />
branch of vertebral<br />
artery<br />
Anterior meningeal<br />
branch of vertebral artery<br />
Posterior auricular artery<br />
Occipital artery<br />
Middle cerebral artery<br />
Anterior cerebral artery<br />
Anterior communicating artery<br />
Ophthalmic artery<br />
Posterior<br />
communicating<br />
artery<br />
Cavernous sinus<br />
Lingual artery<br />
Middle<br />
meningeal<br />
artery<br />
Maxillary<br />
artery<br />
Superficial<br />
temporal<br />
artery<br />
External<br />
carotid<br />
artery<br />
Facial artery<br />
Internal carotid artery<br />
Carotid sinus<br />
Carotid body<br />
Vertebral artery<br />
(cervical part)<br />
Transverse process of C6<br />
Deep cervical artery<br />
Supreme intercostal<br />
artery<br />
Costocervical trunk<br />
Subclavian artery<br />
Ascending pharyngeal artery<br />
Superior laryngeal artery<br />
Superior thyroid artery<br />
Common carotid artery<br />
Ascending cervical artery (cut)<br />
Inferior thyroid artery<br />
Thyrocervical trunk<br />
Brachiocephalic trunk<br />
Internal thoracic artery<br />
10
Arteries to Brain: Schema<br />
NEUROANATOMY<br />
Anterior cerebral artery<br />
Middle cerebral artery<br />
1<br />
Anterior communicating artery<br />
Ophthalmic artery<br />
Posterior communicating artery<br />
Caroticotympanic branch<br />
of internal carotid artery<br />
Posterior cerebral artery<br />
Superior cerebellar artery<br />
Anterior tympanic artery<br />
Middle meningeal artery<br />
Maxillary artery<br />
Basilar artery<br />
Anterior inferior<br />
cerebellar artery<br />
4<br />
3<br />
3<br />
3<br />
3<br />
4<br />
5<br />
5<br />
5<br />
5<br />
2<br />
1<br />
1<br />
1<br />
Supraorbital artery<br />
Supratrochlear artery<br />
Lacrimal artery<br />
Dorsal nasal artery<br />
Middle meningeal artery<br />
Angular artery<br />
Superficial temporal artery<br />
Posterior auricular artery<br />
Facial artery<br />
Occipital artery<br />
Lingual artery<br />
Ascending pharyngeal artery<br />
Posterior inferior<br />
cerebellar artery<br />
External carotid artery<br />
Internal carotid artery<br />
5<br />
5<br />
5<br />
Anterior spinal artery<br />
Spinal segmental<br />
medullary branches<br />
Vertebral artery<br />
Common carotid artery<br />
Superior thyroid artery<br />
Common carotid artery<br />
5<br />
Deep cervical artery<br />
Transverse cervical artery<br />
Vertebral artery<br />
Ascending cervical artery<br />
Suprascapular artery<br />
Supreme intercostal artery<br />
Costocervical trunk<br />
Inferior thyroid artery<br />
Thyrocervical trunk<br />
Subclavian artery<br />
Subclavian artery<br />
Internal thoracic artery<br />
Brachiocephalic trunk<br />
Aorta<br />
Arch<br />
Descending<br />
Ascending<br />
Anastomoses<br />
1 Right–Left<br />
2 Carotid–Vertebral<br />
3 Internal carotid–External carotid<br />
4 Subclavian–Carotid<br />
5 Subclavian–Vertebral<br />
11
NEUROANATOMY<br />
Arteries of Brain: Inferior Views<br />
Medial frontobasal (orbitofrontal) artery<br />
Anterior communicating artery<br />
Anterior cerebral artery<br />
Distal medial striate artery<br />
(recurrent artery of Heubner)<br />
Internal carotid artery<br />
Anterolateral central (lenticulostriate) arteries<br />
Middle cerebral artery<br />
Lateral frontobasal (orbitofrontal) artery<br />
Prefrontal artery<br />
Anterior choroidal artery<br />
Posterior communicating artery<br />
Posterior cerebral artery<br />
Superior cerebellar artery<br />
Basilar artery<br />
Pontine arteries<br />
Labyrinthine (internal acoustic) artery<br />
Anterior inferior cerebellar artery<br />
Vertebral artery<br />
Anterior spinal artery<br />
Posterior inferior cerebellar artery (PICA) (cut)<br />
Posterior spinal artery<br />
Distal medial striate artery<br />
(recurrent artery of Heubner)<br />
Anterior communicating artery<br />
Anterior cerebral artery<br />
Middle cerebral artery<br />
Posterior communicating artery<br />
Anterior choroidal artery<br />
Optic tract<br />
Posterior cerebral artery<br />
Cerebral crus<br />
Lateral geniculate body<br />
Posterior medial choroidal artery<br />
Posterior lateral choroidal artery<br />
Choroid plexus of lateral ventricle<br />
Medial geniculate body<br />
Pulvinar of thalamus<br />
Lateral ventricle<br />
Cerebral arterial<br />
circle (Willis)<br />
(broken line)<br />
12
Cerebral Arterial Circle (Willis)<br />
NEUROANATOMY<br />
Vessels dissected out: inferior view<br />
Anterior cerebral artery<br />
(A 2 segment)<br />
Anterior communicating artery<br />
Anterior cerebral artery<br />
(A 1 segment)<br />
Ophthalmic artery<br />
Internal carotid artery<br />
Distal medial striate artery<br />
(recurrent artery of Heubner)<br />
Anteromedial central (perforating)<br />
arteries<br />
Hypothalamic artery<br />
Anterolateral central<br />
(lenticulostriate) arteries<br />
Middle cerebral artery<br />
Posterior communicating artery<br />
Posterior cerebral artery<br />
(P 2 segment)<br />
(P 1 segment)<br />
Superior cerebellar artery<br />
Basilar artery<br />
Pontine arteries<br />
Anterior inferior cerebellar artery<br />
Superior hypophyseal artery<br />
Inferior hypophyseal artery<br />
Anterior choroidal artery<br />
Thalamotuberal<br />
(premammillary) artery<br />
Posteromedial central<br />
(perforating) arteries<br />
Thalamoperforating artery<br />
Posteromedial central<br />
(paramedian) arteries<br />
Labyrinthine (internal acoustic) artery<br />
Vertebral artery<br />
Vessels in situ: inferior view<br />
Anterior cerebral artery<br />
Hypothalamic artery<br />
Internal carotid artery<br />
Superior hypophyseal artery<br />
Middle cerebral artery<br />
Inferior hypophyseal artery<br />
Posterior communicating artery<br />
Efferent hypophyseal veins<br />
Posterior cerebral artery<br />
Anterior communicating artery<br />
Optic chiasm<br />
Cavernous sinus<br />
Infundibulum (pituitary stalk)<br />
and long hypophyseal portal veins<br />
Adenohypophysis (anterior<br />
lobe of pituitary gland)<br />
<strong>Neuro</strong>hypophysis (posterior<br />
lobe of pituitary gland)<br />
Posteromedial central<br />
(perforating) arteries<br />
Superior cerebellar artery<br />
Basilar artery<br />
13
NEUROANATOMY<br />
Arteries of Brain: Frontal View and Section<br />
Prefrontal artery<br />
Corpus callosum<br />
Anterolateral central<br />
(lenticulostriate) arteries<br />
Lateral frontobasal<br />
(orbitofrontal) artery<br />
Precentral (pre-rolandic)<br />
and central (rolandic)<br />
sulcal arteries<br />
Anterior parietal<br />
(postcentral sulcal)<br />
artery<br />
Posterior parietal<br />
artery<br />
Branch to<br />
angular gyrus<br />
Temporal branches<br />
(anterior, middle<br />
and posterior)<br />
Middle cerebral artery<br />
and branches<br />
(deep in lateral cerebral<br />
[sylvian] sulcus)<br />
Anterior communicating artery<br />
Posterior communicating artery<br />
Anterior inferior cerebellar artery<br />
Posterior spinal artery<br />
Corpus striatum<br />
(caudate and lentiform nuclei)<br />
Anterolateral central<br />
(lenticulostriate) arteries<br />
Insula (island of Reil)<br />
Limen of insula<br />
Precentral (pre-rolandic),<br />
central (rolandic) sulcal<br />
and parietal arteries<br />
Lateral cerebral (sylvian) sulcus<br />
Temporal branches of<br />
middle cerebral artery<br />
Temporal lobe<br />
Middle cerebral artery<br />
Internal carotid artery<br />
Paracentral artery<br />
Medial frontal branches<br />
Pericallosal artery<br />
Callosomarginal artery<br />
Polar frontal artery<br />
Anterior cerebral<br />
arteries<br />
Medial frontobasal<br />
(orbitofrontal) artery<br />
Distal medial striate<br />
artery (recurrent<br />
artery of Heubner)<br />
Internal carotid<br />
artery<br />
Anterior choroidal<br />
artery<br />
Posterior cerebral<br />
artery<br />
Superior cerebellar artery<br />
Basilar and pontine arteries<br />
Labyrinthine (internal<br />
acoustic) artery<br />
Vertebral artery<br />
Posterior inferior cerebellar artery<br />
Anterior spinal artery<br />
Falx cerebri<br />
Callosomarginal arteries<br />
and<br />
Pericallosal arteries<br />
(branches of anterior<br />
cerebral arteries)<br />
Trunk of corpus callosum<br />
Internal capsule<br />
Septum pellucidum<br />
Rostrum of corpus callosum<br />
Anterior cerebral arteries<br />
Distal medial striate artery<br />
(recurrent artery of Heubner)<br />
Anterior communicating artery<br />
Optic chiasm<br />
14
Arteries of Brain: Lateral and Medial Views<br />
NEUROANATOMY<br />
Precentral (pre-rolandic) sulcal artery<br />
Prefrontal sulcal<br />
artery<br />
Anterior parietal (postcentral sulcal) artery<br />
Central (rolandic) sulcal artery<br />
Posterior parietal artery<br />
Branch to angular gyrus<br />
Terminal branches<br />
of posterior<br />
cerebral artery<br />
Terminal branches of<br />
anterior cerebral<br />
artery<br />
Lateral frontobasal<br />
(orbitofrontal) artery<br />
Left middle<br />
cerebral artery<br />
Left anterior<br />
cerebral artery<br />
Anterior communicating artery<br />
Right anterior cerebral artery<br />
Left internal carotid artery<br />
Polar temporal artery<br />
Occipitotemporal<br />
branches<br />
Posterior temporal branch<br />
Middle temporal branch<br />
Superior and inferior terminal branches (trunks)<br />
Anterior temporal branch<br />
Medial<br />
frontal<br />
branches<br />
Callosomarginal<br />
artery<br />
Polar frontal artery<br />
Right anterior<br />
cerebral artery<br />
Posterior<br />
Intermediate<br />
Anterior<br />
Pericallosal artery<br />
Paracentral artery<br />
Cingular branches<br />
Right posterior cerebral artery<br />
Precuneal artery<br />
Dorsal branch<br />
to corpus callosum<br />
Parietooccipital branch<br />
Calcarine branch<br />
Medial frontobasal<br />
(orbitofrontal)<br />
artery<br />
Anterior<br />
communicating artery (cut)<br />
Distal medial striate artery<br />
(recurrent artery of Heubner)<br />
Right internal carotid artery<br />
Medial occipital artery<br />
Posterior temporal branch<br />
Anterior temporal branch<br />
Posterior communicating artery<br />
Note: Anterior parietal (postcentral sulcal) artery also occurs as separate anterior parietal and postcentral sulcal arteries<br />
15
NEUROANATOMY<br />
Arteries of Posterior Cranial Fossa<br />
Thalamogeniculate arteries<br />
Anterior choroidal artery<br />
Crura of fornix<br />
Anterolateral central<br />
(lenticulostriate) arteries<br />
Heads of caudate nuclei<br />
Septum pellucidum<br />
Corpus callosum<br />
Anterior<br />
cerebral arteries<br />
Longitudinal<br />
cerebral<br />
fissure<br />
Lateral and medial geniculate bodies of left thalamus<br />
Choroid plexuses of lateral ventricles<br />
Pulvinars of left and right thalami<br />
Splenium of corpus callosum<br />
Occipital (posterior) horn of right lateral ventricle<br />
Right dorsal branch to corpus callosum<br />
(posterior pericallosal artery)<br />
Parietooccipital Branches of<br />
right posterior<br />
Calcarine cerebral artery<br />
Superior<br />
colliculi<br />
Optic nerve (II)<br />
Ophthalmic artery<br />
Anterior<br />
cerebral artery<br />
Middle<br />
cerebral artery<br />
Posterior<br />
communicating artery<br />
Thalamoperforating arteries<br />
Left internal carotid artery<br />
Basilar artery<br />
Pontine arteries<br />
Labyrinthine (internal acoustic) artery<br />
Posterior cerebral artery<br />
Superior cerebellar artery<br />
III<br />
Anterior inferior cerebellar artery<br />
Anterior meningeal branch of vertebral artery<br />
Temporal branches of posterior cerebral artery<br />
Anterior spinal artery<br />
VI<br />
IV<br />
V<br />
VIII<br />
VII<br />
IX<br />
X<br />
XI<br />
Posterior medial<br />
choroidal artery<br />
to choroid plexus<br />
of 3rd ventricle<br />
Posterior lateral<br />
choroidal artery<br />
Lateral (marginal) branch<br />
Inferior vermian artery<br />
(phantom)<br />
Choroidal branch to 4th ventricle<br />
(phantom) and<br />
Cerebellar tonsillar branch<br />
of posterior inferior cerebellar artery<br />
Outline of 4th ventricle (broken line)<br />
Posterior meningeal branch of vertebral artery<br />
Posterior inferior cerebellar artery (PICA)<br />
Left posterior spinal artery<br />
Left vertebral artery<br />
Superior<br />
vermian<br />
branch<br />
16
Veins of Posterior Cranial Fossa<br />
NEUROANATOMY<br />
Left superior and inferior colliculi<br />
Basal vein (Rosenthal)<br />
Posterior mesencephalic vein<br />
Medial geniculate body<br />
Lateral geniculate body<br />
Left thalamus<br />
(cut surface)<br />
Optic tract<br />
Inferior thalamostriate<br />
veins<br />
Deep middle<br />
cerebral<br />
vein (cut)<br />
Anterior<br />
cerebral<br />
vein<br />
Optic<br />
nerve (II)<br />
Lateral<br />
mesencephalic vein<br />
Left pulvinar<br />
Right pulvinar<br />
Internal cerebral veins<br />
Splenium of corpus callosum<br />
Great cerebral vein (Galen)<br />
Dorsal vein of corpus callosum<br />
Inferior sagittal sinus<br />
Straight sinus<br />
Falx cerebri<br />
Tentorium<br />
cerebelli (cut)<br />
Confluence of sinuses<br />
Left transverse<br />
sinus (cut)<br />
Superior<br />
sagittal<br />
sinus<br />
Anterior pontomesencephalic<br />
vein<br />
Trigeminal nerve (V)<br />
Transverse pontine vein<br />
Petrosal vein (draining<br />
to superior petrosal sinus)<br />
Lateral pontine vein<br />
Anteromedian medullary vein<br />
Vein of lateral recess of 4th ventricle<br />
Superior, middle and<br />
inferior cerebellar peduncles<br />
Anterior spinal vein<br />
L<br />
CL<br />
N<br />
T<br />
C<br />
4th ventricle<br />
U<br />
C<br />
Posterior spinal vein<br />
P<br />
D<br />
F<br />
TU<br />
Preculminate vein<br />
Precentral cerebellar vein<br />
Superior retrotonsillar vein<br />
(Inferior retrotonsillar)<br />
vein of cerebellomedullary<br />
cistern<br />
Superior<br />
vermian<br />
vein<br />
Inferior<br />
vermian vein<br />
Falx cerebelli (cut)<br />
and occipital sinus<br />
Inferior cerebellar<br />
hemispheric veins<br />
Intraculminate vein<br />
Superior cerebellar vein (inconstant)<br />
Parts of cerebellum<br />
L Lingula TU Tuber<br />
CL Central lobule P Pyramid<br />
C Culmen U Uvula<br />
D Declive N Nodule<br />
F Folium T Tonsil<br />
17
NEUROANATOMY<br />
Deep Veins of Brain<br />
Longitudinal cerebral fissure<br />
Anterior cerebral veins<br />
Rostrum of corpus callosum<br />
Septum pellucidum<br />
Anterior vein of septum pellucidum<br />
Head of caudate nucleus<br />
Anterior vein of caudate nucleus<br />
Transverse veins of caudate nucleus<br />
Interventricular foramen (Monro)<br />
Columns of fornix<br />
Superior thalamostriate vein<br />
Superior choroid vein and<br />
choroid plexus of lateral ventricle<br />
Thalamus<br />
Tela choroidea of 3rd ventricle<br />
Lateral direct vein<br />
Posterior vein of caudate nucleus<br />
Internal cerebral veins<br />
Basal vein (Rosenthal)<br />
Great cerebral vein (Galen)<br />
Inferior sagittal sinus<br />
Straight sinus<br />
Tentorium cerebelli<br />
Transverse sinus<br />
Confluence of sinuses<br />
Superior sagittal sinus<br />
Dissection: superior view<br />
Uncal vein<br />
Anterior cerebral vein<br />
Superficial middle cerebral vein<br />
(draining to sphenoparietal sinus)<br />
Deep middle cerebral vein<br />
Optic chiasm<br />
Cerebral crus<br />
Basal vein (Rosenthal)<br />
Lateral geniculate body<br />
Medial geniculate body<br />
Inferior<br />
cerebral<br />
veins<br />
Pulvinar of thalamus<br />
Splenium of corpus callosum<br />
Great cerebral vein (Galen)<br />
Inferior<br />
anastomotic<br />
vein (Labbé)<br />
Dissection: inferior view<br />
18
Subependymal Veins of Brain<br />
NEUROANATOMY<br />
Posterior veins of septum pellucidum<br />
Superior thalamic veins<br />
Superior choroid vein<br />
Transverse veins of caudate nucleus<br />
Superior thalamostriate vein<br />
Lateral ventricle<br />
Anterior vein of<br />
caudate nucleus<br />
Anterior vein of<br />
septum pellucidum<br />
Genu of<br />
corpus<br />
callosum<br />
Lateral direct vein<br />
Posterior terminal vein of caudate nucleus<br />
(posterior part of thalamostriate vein)<br />
Internal cerebral veins (right and left)<br />
Medial (atrial) vein of lateral ventricle<br />
Lateral (atrial) vein of lateral ventricle<br />
Splenium of corpus callosum<br />
Great cerebral vein<br />
(Galen)<br />
Dorsal vein of corpus<br />
callosum<br />
Inferior sagittal<br />
sinus<br />
Internal<br />
occipital vein<br />
Straight sinus<br />
Occipital<br />
(posterior)<br />
horn of<br />
lateral<br />
ventricle<br />
Interventricular<br />
foramen (Monro)<br />
Anterior commissure<br />
Interthalamic adhesion<br />
Anterior cerebral vein<br />
Optic chiasm<br />
3rd ventricle<br />
Cerebellum<br />
Deep middle cerebral vein<br />
Inferior thalamostriate veins<br />
Basal vein (Rosenthal)<br />
Temporal (inferior) horn of lateral ventricle<br />
Posterior mesencephalic vein<br />
Hippocampal and inferior ventricular veins<br />
Cerebral aqueduct<br />
4th ventricle<br />
Lateral and median apertures of 4th ventricle<br />
Superior vermian vein<br />
Veins on lateral wall of ventricle<br />
Veins on medial wall and floor of ventricle<br />
All other veins<br />
19
NEUROANATOMY<br />
Hypothalamus and Hypophysis<br />
Septum pellucidum<br />
Thalamus<br />
Fornix<br />
Hypothalamic sulcus<br />
Anterior commissure<br />
Principal<br />
nuclei of<br />
hypothalamus<br />
Paraventricular<br />
Posterior<br />
Dorsomedial<br />
Supraoptic<br />
Ventromedial<br />
Arcuate<br />
(infundibular)<br />
Mammillary<br />
Optic chiasm<br />
Infundibulum (pituitary stalk)<br />
Hypophysis (pituitary gland)<br />
Mammillothalamic tract<br />
Dorsal longitudinal<br />
fasciculus and other<br />
descending pathways<br />
Lamina terminalis<br />
Paraventricular hypothalamic nucleus<br />
Hypothalamic<br />
sulcus<br />
Supraoptic hypothalamic nucleus<br />
Supraopticohypophyseal tract<br />
Tuberohypophyseal tract<br />
Hypothalamohypophyseal tract<br />
Infundibulum (pituitary stalk)<br />
Mammillary<br />
body<br />
Arcuate (infundibular) nucleus<br />
Adenohypophysis<br />
(anterior lobe of<br />
pituitary gland)<br />
Pars tuberalis<br />
Fibrous trabecula<br />
Pars intermedia<br />
Pars distalis<br />
Cleft<br />
Median eminence<br />
of tuber cinereum<br />
Infundibular<br />
stem<br />
Infundibular<br />
process<br />
<strong>Neuro</strong>hypophysis<br />
(posterior lobe<br />
of pituitary gland)<br />
20
Arteries and Veins of Hypothalamus and Hypophysis<br />
NEUROANATOMY<br />
Hypothalamic vessels<br />
Primary plexus of<br />
hypophyseal portal system<br />
Superior<br />
hypophyseal<br />
artery<br />
Artery of trabecula<br />
Trabecula (fibrous tissue)<br />
Efferent hypophyseal vein<br />
to cavernous sinus<br />
Long hypophyseal portal veins<br />
Short hypophyseal portal veins<br />
Efferent hypophyseal vein<br />
to cavernous sinus<br />
Secondary plexus<br />
of hypophyseal<br />
portal system<br />
<strong>Neuro</strong>hypophysis<br />
(posterior lobe of<br />
pituitary gland)<br />
Adenohypophysis<br />
(anterior lobe of<br />
pituitary gland)<br />
Capillary plexus of<br />
infundibular process<br />
Efferent hypophyseal vein<br />
to cavernous sinus<br />
Efferent hypophyseal<br />
veins to cavernous sinus<br />
Inferior hypophyseal artery<br />
21
NEUROANATOMY<br />
Relation of Spinal Nerve Roots to Vertebrae<br />
Cervical<br />
enlargement<br />
Lumbar<br />
enlargement<br />
Base<br />
of skull<br />
C1<br />
C2<br />
C3<br />
C4<br />
C5<br />
C6<br />
C7<br />
T1<br />
T2<br />
T3<br />
T4<br />
T5<br />
T6<br />
T7<br />
T8<br />
T9<br />
T10<br />
C1<br />
C2<br />
C3<br />
C4<br />
C5<br />
C6<br />
C7<br />
C8<br />
T1<br />
T2<br />
T3<br />
T4<br />
T5<br />
T6<br />
T7<br />
T8<br />
T9<br />
T10<br />
T11<br />
T11<br />
T12<br />
T12<br />
L1<br />
L1<br />
L2<br />
C1 spinal nerve exits<br />
above C1 vertebra<br />
C8 spinal nerve<br />
exits below<br />
C7 vertebra<br />
(there are 8 cervical<br />
nerves but only<br />
7 cervical vertebrae)<br />
Conus medullaris<br />
(termination of<br />
spinal cord)<br />
S1<br />
S2<br />
L4<br />
L5<br />
Lumbar disc protrusion does not usually affect<br />
nerve exiting above disc. Lateral protrusion<br />
at disc level L4–5 affects L5 spinal nerve, not<br />
L4 spinal nerve. Protrusion at disc level L5–S1<br />
affects S1 spinal nerve, not L5 spinal nerve<br />
L4<br />
L4<br />
L5<br />
L4<br />
Internal terminal<br />
filum (pial part)<br />
L3<br />
L4<br />
L2<br />
L3<br />
L4<br />
Cauda equina<br />
L5<br />
L5<br />
External<br />
terminal filum<br />
(dural part)<br />
S2<br />
S3<br />
Termination of<br />
S4 dural sac<br />
S5<br />
Coccygeal nerve<br />
Coccyx<br />
L5<br />
L5<br />
Sacrum<br />
S1<br />
Cervical nerves<br />
Thoracic nerves<br />
Lumbar nerves<br />
Sacral and coccygeal nerves<br />
S1<br />
S2<br />
S3<br />
S4<br />
S5<br />
Coccygeal nerve<br />
Medial protrusion at disc level L4–5 rarely affects<br />
L4 spinal nerve but may affect L5 spinal nerve<br />
and sometimes S1–4 spinal nerves<br />
22
Autonomic Nervous System: General Topography<br />
NEUROANATOMY<br />
Oculomotor nerve (III)<br />
Facial nerve (VII)<br />
Glossopharyngeal nerve (IX)<br />
Vagus nerve (X)<br />
Internal carotid nerve and plexus<br />
Superior cervical sympathetic ganglion<br />
C4 spinal nerve<br />
Middle cervical sympathetic ganglion<br />
Vertebral ganglion<br />
Cervicothoracic (stellate) ganglion<br />
Cervical (sympathetic)<br />
cardiac nerves<br />
Sympathetic trunk<br />
Superior<br />
Middle<br />
Inferior<br />
Thoracic (sympathetic) cardiac nerves<br />
6th intercostal nerve<br />
(ventral ramus of T6<br />
spinal nerve)<br />
Sympathetic trunk<br />
6th thoracic sympathetic ganglion<br />
Gray and white rami communicantes<br />
Greater splanchnic nerve<br />
Lesser splanchnic nerve<br />
Least splanchnic nerve<br />
Aorticorenal ganglion<br />
Lumbar splanchnic nerves (sympathetic)<br />
Gray rami communicantes<br />
Sacral splanchnic nerves (sympathetic)<br />
Pelvic splanchnic nerves<br />
(sacral parasympathetic<br />
outflow)<br />
Sciatic nerve<br />
Inferior hypogastric<br />
(pelvic) plexus<br />
Sympathetic fibers<br />
Parasympathetic fibers<br />
Ciliary ganglion<br />
Pterygopalatine ganglion<br />
Otic ganglion<br />
Chorda tympani nerve<br />
Lingual nerve<br />
Submandibular ganglion<br />
Pharyngeal and superior laryngeal branches<br />
of vagus nerve<br />
Recurrent laryngeal branch of vagus nerve<br />
Superior cervical<br />
Inferior cervical<br />
Thoracic<br />
Cardiac plexus<br />
Anterior<br />
Posterior<br />
Esophageal plexus<br />
Cardiac branches<br />
of vagus nerve<br />
Pulmonary plexuses<br />
Thoracic aortic plexus<br />
Anterior vagal trunk<br />
Posterior vagal trunk<br />
Celiac ganglion<br />
Celiac trunk and plexus<br />
Superior mesenteric ganglion<br />
Superior mesenteric artery<br />
and plexus<br />
Intermesenteric<br />
(abdominal aortic) plexus<br />
Inferior mesenteric ganglion<br />
Inferior mesenteric artery<br />
and plexus<br />
Superior hypogastric plexus<br />
Parasympathetic branch from<br />
inferior hypogastric plexus to<br />
descending colon<br />
Hypogastric nerves<br />
Rectal plexus<br />
Vesical plexus<br />
Prostatic plexus<br />
23
NEUROANATOMY<br />
Spinal Nerve Origin: Cross Sections<br />
Section through thoracic vertebra<br />
Aorta<br />
Fat in epidural space<br />
Sympathetic ganglion<br />
Ventral root<br />
White and gray rami<br />
communicantes<br />
Spinal nerve<br />
Ventral ramus<br />
(intercostal nerve)<br />
Dorsal ramus<br />
Body of vertebra<br />
Dura mater<br />
Arachnoid mater*<br />
Subarachnoid space<br />
Pia mater*<br />
Recurrent<br />
meningeal<br />
branches of<br />
spinal nerve<br />
Pleura<br />
Lung<br />
Spinal sensory<br />
(dorsal root) ganglion<br />
Dorsal root<br />
Lateral horn of<br />
gray matter of spinal cord<br />
Section through lumbar vertebra<br />
Sympathetic<br />
ganglion<br />
Dura mater<br />
Lateral branch<br />
Medial branch<br />
of dorsal<br />
ramus<br />
of spinal<br />
nerve<br />
Gray ramus<br />
communicans<br />
Fat in<br />
epidural<br />
space<br />
Arachnoid mater<br />
Ventral root<br />
Spinal nerve<br />
Internal vertebral<br />
(epidural) venous plexus<br />
Ventral ramus (contributes to lumbar plexus)<br />
Dorsal ramus<br />
Dorsal and ventral<br />
roots of lumbar and<br />
sacral spinal nerves<br />
forming cauda equina<br />
Spinal sensory (dorsal root) ganglion<br />
Dorsal root<br />
Conus medullaris<br />
*Leptomeninges<br />
24
Olfactory Nerve (I): Schema<br />
NEUROANATOMY<br />
Olfactory bulb cells: schema<br />
Efferent fibers to<br />
olfactory bulb<br />
Afferent fibers from bulb<br />
to central connections<br />
and contralateral bulb<br />
Granule cell (excited by<br />
and inhibiting to mitral<br />
and tufted cells)<br />
Mitral cell<br />
Recurrent process<br />
Tufted cell<br />
Periglomerular<br />
cell<br />
Glomerulus<br />
Olfactory<br />
nerve fibers<br />
Subcallosal (parolfactory) area<br />
Septal area and nuclei<br />
Fibers from<br />
Fibers to<br />
Contralateral<br />
olfactory bulb<br />
Anterior commissure<br />
Medial<br />
olfactory stria<br />
Olfactory cells<br />
Olfactory tract<br />
Olfactory mucosa<br />
Olfactory nerves (I)<br />
Olfactory bulb<br />
Cribriform plate of ethmoid bone<br />
Anterior olfactory nucleus<br />
Olfactory trigone<br />
and olfactory tubercle<br />
Lateral olfactory stria<br />
Lateral olfactory tract nucleus<br />
Anterior perforated substance<br />
Amygdaloid body (phantom)<br />
Piriform lobe<br />
Uncus<br />
Hippocampal<br />
fimbria<br />
Dentate gyrus<br />
Parahippocampal gyrus<br />
25
NEUROANATOMY<br />
Optic Nerve (II) (Visual Pathway): Schema<br />
G<br />
A<br />
B<br />
H<br />
G<br />
B<br />
A<br />
H<br />
Overlapping<br />
visual fields<br />
Central darker<br />
circle represents<br />
macular zone<br />
Lighter shades<br />
represent<br />
monocular fields<br />
Each quadrant<br />
a different color<br />
R R C<br />
C<br />
Projection on<br />
left retina<br />
Projection on<br />
right retina<br />
P<br />
Choroid<br />
Periphery<br />
P<br />
Choroid<br />
Macula<br />
Optic nerves (II)<br />
Optic chiasm<br />
Structure of retina: schema<br />
A Amacrine cells<br />
B Bipolar cells<br />
C Cones<br />
G Ganglion cells<br />
H Horizontal cells<br />
P Pigment cells<br />
R Rods<br />
Projection on left<br />
dorsal lateral<br />
geniculate nucleus<br />
Optic tracts<br />
Lateral<br />
geniculate<br />
bodies<br />
Projection on right<br />
dorsal lateral<br />
geniculate nucleus<br />
Optic radiation<br />
Optic radiation<br />
Calcarine<br />
sulcus<br />
Calcarine<br />
sulcus<br />
Projection on left<br />
occipital lobe<br />
Projection on right<br />
occipital lobe<br />
26
Oculomotor (III), Trochlear (IV) and Abducent (VI) Nerves: Schema<br />
NEUROANATOMY<br />
Long ciliary nerve<br />
Short ciliary nerves<br />
Anterior ethmoidal nerve<br />
Superior oblique muscle<br />
Levator palpebrae<br />
superioris muscle<br />
Superior<br />
rectus muscle<br />
Ciliary ganglion<br />
Posterior ethmoidal nerve<br />
Sensory root of ciliary ganglion<br />
Sympathetic root of ciliary ganglion<br />
Superior division of<br />
oculomotor nerve<br />
Frontal nerve (cut)<br />
Lacrimal nerve (cut)<br />
Nasociliary nerve<br />
Abducent nucleus<br />
Trochlear nucleus<br />
Oculomotor nucleus<br />
Accessory oculomotor<br />
(Edinger-Westphal)<br />
nucleus (parasympathetic)<br />
Trochlear nerve (IV)<br />
Oculomotor nerve (III)<br />
Ophthalmic nerve (V 1 )<br />
Infraorbital nerve<br />
Zygomatic nerve (cut)<br />
Inferior oblique muscle<br />
Ciliary muscle<br />
Dilator muscle of pupil<br />
Sphincter muscle of pupil<br />
Efferent fibers<br />
Afferent fibers<br />
Sympathetic fibers<br />
Parasympathetic fibers<br />
Pterygopalatine<br />
ganglion<br />
Inferior division of<br />
oculomotor nerve<br />
Medial rectus muscle<br />
Inferior rectus muscle<br />
Parasympathetic root<br />
of ciliary ganglion<br />
Abducent<br />
nerve (VI)<br />
Mandibular nerve (V 3 )<br />
Internal carotid artery<br />
and nerve plexus<br />
Maxillary nerve (V 2 )<br />
Lateral rectus muscle and<br />
abducent nerve (turned back)<br />
Cavernous plexus<br />
Common tendinous ring<br />
27
NEUROANATOMY<br />
Trigeminal Nerve (V): Schema<br />
Efferent fibers<br />
Afferent fibers<br />
Proprioceptive fibers<br />
Parasympathetic fibers<br />
Sympathetic fibers<br />
Frontal nerve<br />
Ciliary ganglion<br />
Posterior ethmoidal nerve<br />
Long ciliary nerve<br />
Short ciliary nerves<br />
Anterior ethmoidal nerve<br />
Supraorbital nerve<br />
Supratrochlear nerve<br />
Infratrochlear nerve<br />
Internal nasal branches<br />
and<br />
External nasal branches<br />
of anterior ethmoidal nerve<br />
Maxillary nerve (V 2 )<br />
Meningeal branch<br />
Zygomaticotemporal<br />
nerve<br />
Zygomaticofacial nerve<br />
Zygomatic nerve<br />
Infraorbital nerve<br />
Pterygopalatine<br />
ganglion<br />
Superior<br />
alveolar<br />
branches of<br />
infraorbital nerve<br />
Nasal branches<br />
(posterior superior<br />
lateral, nasopalatine<br />
and posterior<br />
superior medial)<br />
Nerve (vidian) of<br />
pterygoid canal<br />
(from facial nerve [VII]<br />
and carotid plexus)<br />
Pharyngeal branch<br />
Greater and lesser<br />
palatine nerves<br />
Ophthalmic nerve (V 1 )<br />
Tentorial (meningeal) branch<br />
Nasociliary nerve<br />
Lacrimal nerve<br />
Sensory root of<br />
ciliary ganglion<br />
Trigeminal nerve (V) ganglion and nuclei<br />
Motor nucleus<br />
Mesencephalic nucleus<br />
Principal sensory nucleus<br />
Spinal tract and nucleus<br />
Facial nerve (VII)<br />
Chorda<br />
tympani nerve<br />
Deep temporal nerves<br />
(to temporalis muscle)<br />
Lateral pterygoid<br />
and masseteric nerves<br />
Tensor veli palatini and<br />
medial pterygoid nerves<br />
Buccal nerve<br />
Mental nerve<br />
Inferior dental plexus<br />
Lingual nerve<br />
Submandibular<br />
ganglion<br />
Mylohyoid nerve<br />
Mandibular nerve (V 3 )<br />
Inferior<br />
alveolar nerve<br />
Otic ganglion<br />
Tensor tympani nerve<br />
Superficial<br />
temporal branches<br />
Articular branch<br />
and anterior<br />
auricular nerves<br />
Auriculotemporal nerve<br />
Parotid branches<br />
Meningeal branch<br />
Lesser petrosal nerve (from<br />
glossopharyngeal nerve [IX])<br />
28
Facial Nerve (VII): Schema<br />
NEUROANATOMY<br />
Greater petrosal nerve<br />
Deep petrosal nerve (from internal carotid plexus)<br />
Lesser petrosal nerve<br />
Nerve (vidian) of pterygoid canal<br />
Otic ganglion<br />
Pterygopalatine ganglion<br />
Facial muscles<br />
Facial nerve (VII)<br />
Geniculate ganglion<br />
Internal carotid plexus<br />
(on internal carotid artery)<br />
Internal acoustic meatus<br />
Intermediate nerve<br />
Motor nucleus of facial nerve<br />
Superior salivatory nucleus<br />
Solitary tract nucleus<br />
Frontal belly (frontalis)<br />
of occipitofrontalis<br />
Orbicularis oculi<br />
Corrugator supercilii<br />
Zygomaticus major<br />
Zygomaticus minor<br />
Procerus<br />
Levator labii<br />
superioris<br />
Levator labii<br />
superioris<br />
alaeque nasi<br />
Levator<br />
anguli oris<br />
Nasalis<br />
Temporal<br />
branches<br />
Depressor<br />
septi nasi<br />
Orbicularis<br />
oris<br />
Depressor<br />
anguli oris<br />
Depressor labii<br />
inferioris<br />
Mentalis<br />
(Risorius)<br />
(not shown)<br />
Buccinator<br />
Platysma<br />
Taste:<br />
of<br />
anterior 2 ⁄3<br />
tongue<br />
Zygomatic<br />
Marginal<br />
mandibular<br />
branch<br />
branches<br />
Buccal<br />
branches<br />
Sublingual gland<br />
Submandibular gland<br />
Efferent fibers<br />
Submandibular ganglion<br />
Afferent fibers<br />
Parasympathetic fibers Lingual nerve (from trigeminal nerve)<br />
Sympathetic fibers<br />
Chorda tympani nerve<br />
Cervical branch<br />
Tympanic nerve (Jacobson)<br />
(from glossopharyngeal nerve)<br />
Glossopharyngeal nerve (IX)<br />
Digastric muscle (posterior belly)<br />
Stylohyoid muscle<br />
Nerve to stapedius muscle<br />
Stylomastoid foramen<br />
Tympanic plexus<br />
Occipital<br />
branch of<br />
posterior<br />
auricular<br />
nerve<br />
Branches to auricular muscles<br />
Posterior auricular nerve<br />
Caroticotympanic nerve (from internal carotid plexus)<br />
Occipital<br />
belly<br />
(occipitalis) of<br />
occipitofrontalis<br />
muscle<br />
29
NEUROANATOMY<br />
Vestibulocochlear Nerve (VIII): Schema<br />
Afferent fibers<br />
Geniculum of facial nerve<br />
(site of geniculate ganglion)<br />
Greater petrosal nerve<br />
Facial canal<br />
Tympanic cavity<br />
Chorda tympani nerve<br />
Head of malleus<br />
Cochlear (spiral) ganglion<br />
Incus<br />
Vestibular nerve<br />
Cochlear nerve<br />
Motor root of facial nerve<br />
and intermediate nerve<br />
Vestibulocochlear<br />
nerve (VIII)<br />
Medulla oblongata<br />
(cross section)<br />
Medial<br />
Internal<br />
acoustic<br />
meatus<br />
Ampulla of lateral<br />
semicircular duct<br />
Ampulla of superior<br />
semicircular duct<br />
Vestibular<br />
nuclei<br />
(diagrammatic)<br />
Superior<br />
Inferior<br />
Lateral<br />
Anterior<br />
Posterior<br />
Cochlear<br />
nuclei<br />
Inferior cerebellar<br />
peduncle (to cerebellum)<br />
Saccule<br />
Utricle<br />
Ampulla of posterior<br />
semicircular duct<br />
Vestibular ganglion<br />
Superior division<br />
Inferior division<br />
of vestibular nerve<br />
30
Glossopharyngeal Nerve (IX): Schema<br />
NEUROANATOMY<br />
Efferent fibers<br />
Spinal tract and spinal nucleus of trigeminal nerve<br />
Afferent fibers<br />
Solitary tract nucleus<br />
Parasympathetic fibers Tympanic nerve (Jacobson)<br />
Nucleus ambiguus<br />
Tympanic cavity and plexus<br />
Inferior salivatory nucleus<br />
Stylomastoid foramen<br />
Geniculate ganglion<br />
of facial nerve<br />
Caroticotympanic nerve (from internal carotid plexus)<br />
Greater petrosal nerve<br />
Deep petrosal nerve<br />
Nerve (vidian) of pterygoid canal<br />
Lesser petrosal nerve<br />
Pterygopalatine ganglion<br />
Mandibular nerve (V 3 )<br />
Otic ganglion<br />
Auriculotemporal nerve<br />
Parotid gland<br />
Tubal branch of tympanic plexus<br />
Pharyngotympanic (auditory)<br />
tube and pharyngeal opening<br />
Stylopharyngeus muscle (and branch<br />
Glossopharyngeal<br />
from glossopharyngeal nerve)<br />
nerve (IX)<br />
Jugular foramen<br />
Communication to auricular<br />
branch of vagus nerve<br />
Superior and<br />
Inferior ganglia of<br />
Glossopharyngeal nerve<br />
Taste and<br />
somatic<br />
sensation:<br />
posterior<br />
1<br />
⁄3 of tongue<br />
Communication to facial nerve (VII)<br />
Vagus nerve (X)<br />
Superior cervical<br />
sympathetic ganglion<br />
Sympathetic trunk<br />
Carotid branch of<br />
glossopharyngeal nerve<br />
Pharyngeal plexus<br />
Pharyngeal, tonsillar and lingual<br />
branches of glossopharyngeal nerve<br />
Pharyngeal branch of vagus nerve<br />
Internal carotid artery<br />
Carotid sinus<br />
Carotid body<br />
Common carotid artery<br />
External carotid artery<br />
31
NEUROANATOMY<br />
Vagus Nerve (X): Schema<br />
SEE ALSO PLATE 160<br />
Glossopharyngeal nerve (IX)<br />
Meningeal branch of vagus nerve<br />
Auricular branch of vagus nerve<br />
Pharyngotympanic (auditory) tube<br />
Levator veli<br />
palatini muscle<br />
Salpingopharyngeus<br />
muscle<br />
Palatoglossus muscle<br />
Palatopharyngeus<br />
muscle<br />
Superior pharyngeal<br />
constrictor muscle<br />
Stylopharyngeus muscle<br />
Middle pharyngeal constrictor muscle<br />
Inferior pharyngeal constrictor muscle<br />
Cricothyroid muscle<br />
Trachea<br />
Esophagus<br />
Right subclavian artery<br />
Right recurrent laryngeal nerve<br />
Heart<br />
Hepatic branch of anterior<br />
vagal trunk (in lesser omentum)<br />
Celiac branches from anterior<br />
and posterior vagal trunks<br />
to celiac plexus<br />
Celiac and superior mesenteric<br />
ganglia and celiac plexus<br />
Hepatic plexus<br />
Gallbladder<br />
and bile ducts<br />
Liver<br />
Pyloric branch<br />
from hepatic plexus<br />
Pancreas<br />
Duodenum<br />
Ascending colon<br />
Cecum<br />
Appendix<br />
Jugular foramen<br />
Posterior nucleus of vagus<br />
nerve (parasympathetic<br />
and visceral afferent)<br />
Solitary tract nucleus (visceral<br />
afferents including taste)<br />
Spinal tract and spinal<br />
nucleus of trigeminal nerve<br />
(somatic afferent)<br />
Nucleus ambiguus<br />
(motor to pharyngeal<br />
and laryngeal muscles)<br />
Cranial root of<br />
accessory nerve*<br />
(see next plate)<br />
Vagus nerve (X)<br />
Superior ganglion of vagus nerve<br />
Inferior ganglion of vagus nerve<br />
Pharyngeal branch of vagus nerve (motor to muscles of<br />
palate and lower pharynx; sensory to lower pharynx)<br />
Communicating branch of vagus nerve to<br />
carotid branch of glossopharyngeal nerve<br />
Pharyngeal plexus<br />
Superior laryngeal nerve:<br />
Internal branch (sensory and parasympathetic)<br />
External branch (motor to cricothyroid muscle)<br />
Superior cervical cardiac branch of vagus nerve<br />
Inferior cervical cardiac branch of vagus nerve<br />
Thoracic cardiac branch of vagus nerve<br />
Left recurrent laryngeal nerve (motor to muscles of larynx<br />
except cricothyroid; sensory and parasympathetic to<br />
larynx below vocal folds; parasympathetic, efferent and<br />
afferent to upper esophagus and trachea)<br />
Pulmonary plexus<br />
Cardiac plexus<br />
Esophageal plexus<br />
Anterior vagal trunk<br />
Gastric branches of anterior vagal trunk<br />
(branches from posterior trunk behind stomach)<br />
Vagal branches (parasympathetic motor,<br />
secretomotor and afferent fibers) accompany<br />
superior mesenteric artery and its branches<br />
usually as far as left colic (splenic) flexure<br />
Small intestine<br />
Efferent fibers<br />
Afferent fibers<br />
Parasympathetic fibers<br />
32
Accessory Nerve (XI): Schema<br />
NEUROANATOMY<br />
SEE ALSO PLATE 28<br />
Nucleus ambiguus<br />
Vagus nerve (X)<br />
Cranial root of accessory nerve (joins vagus nerve<br />
and via recurrent laryngeal nerve supplies muscles of<br />
larynx, except cricothyroid)*<br />
Spinal root of<br />
accessory nerve<br />
Jugular foramen<br />
Foramen<br />
magnum<br />
Superior ganglion<br />
of vagus nerve<br />
Accessory nerve (XI)*<br />
Inferior ganglion<br />
of vagus nerve<br />
C1 spinal nerve<br />
C2 spinal nerve<br />
Accessory nerve<br />
(to sternocleidomastoid<br />
and trapezius muscles)<br />
Sternocleidomastoid muscle (cut)<br />
C3 spinal nerve<br />
C4 spinal nerve<br />
Trapezius muscle<br />
*Recent evidence suggests that the accessory nerve lacks a cranial root and has no connection to the vagus nerve.<br />
Verification of this finding awaits further investigation.<br />
Efferent fibers<br />
Proprioceptive fibers<br />
33
NEUROANATOMY<br />
Hypoglossal Nerve (XII): Schema<br />
Hypoglossal nerve (XII)<br />
(in hypoglossal canal)<br />
Meningeal branch<br />
Intrinsic<br />
muscles<br />
of tongue<br />
Superior<br />
longitudinal<br />
Transverse<br />
and vertical<br />
Inferior<br />
longitudinal<br />
Styloglossus<br />
muscle<br />
Hypoglossal nucleus<br />
Occipital condyle<br />
Inferior ganglion of<br />
vagus nerve<br />
Ventral rami of<br />
C1, 2, 3 form<br />
ansa cervicalis<br />
of cervical plexus<br />
Superior cervical<br />
sympathetic<br />
ganglion<br />
Genioglossus<br />
muscle<br />
Geniohyoid muscle<br />
Hyoglossus muscle<br />
Superior root of<br />
ansa cervicalis<br />
Internal carotid artery<br />
Inferior root of ansa cervicalis<br />
Thyrohyoid muscle<br />
Omohyoid muscle<br />
(superior belly)<br />
Sternohyoid muscle<br />
Ansa cervicalis<br />
Internal jugular vein<br />
Common carotid artery<br />
Sternothyroid muscle<br />
Omohyoid muscle (inferior belly)<br />
Efferent fibers<br />
Afferent fibers<br />
34
Nerves of Heart<br />
NEUROANATOMY<br />
Superior cervical<br />
sympathetic ganglion<br />
Vagus nerve (X)<br />
(Conjoined sympathetic and<br />
vagal) superior cervical cardiac nerves<br />
Middle cervical<br />
sympathetic ganglion<br />
Middle cervical<br />
(sympathetic) cardiac nerve<br />
Phrenic nerve<br />
Inferior cervical<br />
(vagal) cardiac nerve<br />
Vertebral ganglion<br />
Inferior thyroid artery<br />
Vertebral artery<br />
Cervicothoracic<br />
(stellate) ganglion<br />
Ansa subclavia<br />
Recurrent<br />
laryngeal nerve<br />
Superior cervical<br />
sympathetic ganglion<br />
Vagus nerve (X)<br />
Superior cervical<br />
(sympathetic) cardiac nerve<br />
Superior cervical<br />
(vagal) cardiac nerve<br />
Middle cervical<br />
sympathetic ganglion<br />
Phrenic nerve<br />
Middle cervical<br />
(sympathetic) cardiac nerve<br />
Inferior cervical<br />
(vagal) cardiac nerve<br />
Vertebral ganglion<br />
Cervicothoracic<br />
(stellate) ganglion<br />
Inferior cervical<br />
sympathetic<br />
cardiac nerves<br />
Inferior cervical<br />
(sympathetic) cardiac nerves<br />
Thoracic cardiac branch<br />
of vagus nerve<br />
4th thoracic<br />
sympathetic ganglion<br />
Thoracic (sympathetic)<br />
cardiac branches<br />
Cardiac plexus<br />
3rd thoracic<br />
sympathetic ganglion<br />
Thoracic (sympathetic)<br />
cardiac branches<br />
Thoracic cardiac<br />
branch of<br />
vagus nerve<br />
Recurrent laryngeal<br />
nerve<br />
Phrenic nerve (cut)<br />
35
NEUROANATOMY<br />
Autonomic Nerves and Ganglia of Abdomen<br />
Right sympathetic trunk<br />
Thoracic duct<br />
Right greater<br />
and lesser<br />
splanchnic<br />
nerves<br />
Right phrenic nerve<br />
Inferior phrenic<br />
arteries and plexuses<br />
Right greater<br />
and lesser<br />
splanchnic<br />
nerves<br />
Right suprarenal<br />
plexus<br />
Right aorticorenal<br />
ganglion<br />
Right least<br />
splanchnic nerve<br />
Right renal<br />
artery and plexus<br />
Right<br />
sympathetic trunk<br />
White and gray<br />
rami communicantes<br />
Cisterna chyli<br />
Gray ramus communicans<br />
3rd lumbar ganglion<br />
of sympathetic trunk<br />
2nd and 3rd lumbar<br />
splanchnic nerves<br />
Right ureter and plexus<br />
Right testicular (ovarian)<br />
artery and plexus<br />
4th lumbar splanchnic nerve<br />
1st sacral ganglion<br />
of sympathetic trunk<br />
Gray rami communicantes<br />
Anterior,<br />
Posterior<br />
vagal trunks<br />
Left gastric artery<br />
and plexus<br />
Celiac ganglia<br />
Left greater<br />
splanchnic nerve<br />
Left lesser<br />
splanchnic nerve<br />
Splenic artery<br />
and plexus<br />
Common hepatic<br />
artery and plexus<br />
Superior mesenteric<br />
ganglion and plexus<br />
Left aorticorenal<br />
ganglion<br />
Left sympathetic<br />
trunk<br />
Intermesenteric<br />
(aortic) plexus<br />
Inferior mesenteric<br />
ganglion<br />
Left colic artery<br />
and plexus<br />
Inferior mesenteric<br />
artery and plexus<br />
Left common iliac<br />
artery and plexus<br />
Superior rectal<br />
artery and plexus<br />
Superior hypogastric<br />
plexus<br />
Internal and external<br />
iliac arteries and<br />
plexuses<br />
Right and left<br />
hypogastric nerves<br />
to inferior hypogastric<br />
(pelvic) plexus<br />
Left sacral plexus<br />
Pelvic splanchnic<br />
nerves<br />
36
Nerves of Stomach and Duodenum<br />
NEUROANATOMY<br />
Right and left inferior phrenic arteries and plexuses<br />
Anterior and posterior layers of lesser omentum<br />
Branch from hepatic plexus to<br />
cardia via lesser omentum<br />
Right greater splanchnic<br />
nerve<br />
Hepatic branch of anterior vagal trunk<br />
Anterior vagal trunk<br />
Celiac branch of posterior vagal trunk<br />
Celiac branch of anterior vagal trunk<br />
Left gastric artery and plexus<br />
Vagal<br />
branch<br />
from<br />
hepatic<br />
plexus<br />
to<br />
pyloric<br />
part of<br />
stomach<br />
Hepatic plexus<br />
Right gastric<br />
artery and plexus<br />
Anterior gastric<br />
branch of anterior<br />
vagal trunk<br />
Left greater splanchnic<br />
nerve<br />
Left lesser splanchnic<br />
nerve<br />
Splenic artery and plexus<br />
Celiac ganglia and plexus<br />
Plexus on gastro-omental<br />
(gastroepiploic) arteries<br />
Superior mesenteric artery and plexus<br />
Plexus on inferior pancreaticoduodenal artery<br />
Plexus on first jejunal artery<br />
Plexus on anterior superior and anterior<br />
inferior pancreaticoduodenal arteries<br />
(posterior pancreaticoduodenal arteries<br />
and plexuses not visible in this view)<br />
37
NEUROANATOMY<br />
Nerves of Stomach and Duodenum (continued)<br />
Plexus on gastro-omental<br />
(gastroepiploic) arteries<br />
Hepatic plexus<br />
Right gastric<br />
artery and<br />
plexus<br />
Posterior gastric branch of posterior vagal trunk<br />
Hepatic branch of anterior vagal trunk via lesser omentum<br />
Branch from hepatic plexus to cardia via lesser omentum<br />
Right inferior phrenic artery and plexus<br />
Posterior vagal trunk<br />
Celiac branch of posterior vagal trunk<br />
Celiac branch of anterior vagal trunk<br />
Left gastric artery and plexus<br />
Left inferior phrenic artery and plexus<br />
Celiac ganglia and plexus<br />
Greater, lesser and least<br />
splanchnic nerves<br />
Aorticorenal ganglia<br />
Splenic artery and plexus<br />
Greater,<br />
Lesser,<br />
Least<br />
splanchnic<br />
nerves<br />
View<br />
with<br />
stomach<br />
reflected<br />
cephalad<br />
Right phrenic nerve<br />
Phrenic ganglion<br />
Branch from right inferior phrenic<br />
plexus to cardia of stomach<br />
Right and left inferior phrenic<br />
arteries and plexuses<br />
Anterior vagal trunk<br />
Posterior vagal trunk<br />
Plexus on<br />
anterior superior<br />
and anterior inferior<br />
pancreaticoduodenal<br />
arteries<br />
Plexus on gastroduodenal artery<br />
Plexus on posterior superior<br />
and posterior inferior<br />
pancreaticoduodenal arteries<br />
Superior mesenteric ganglion and plexus<br />
Right greater,<br />
lesser<br />
and least<br />
splanchnic nerves<br />
Celiac ganglia<br />
Right aorticorenal<br />
ganglion<br />
Celiac branches<br />
of anterior<br />
and posterior<br />
vagal trunks<br />
Left gastric<br />
artery and plexus<br />
Left greater,<br />
lesser and least<br />
splanchnic nerves<br />
Superior mesenteric ganglion and plexus<br />
Left aorticorenal ganglion<br />
38
Nerves of Small Intestine<br />
NEUROANATOMY<br />
Recurrent branch of left inferior phrenic<br />
artery and plexus to esophagus<br />
Anterior vagal trunk<br />
Posterior vagal trunk<br />
Hepatic branch of anterior<br />
vagal trunk (courses in lesser<br />
omentum, removed here)<br />
Celiac branches of anterior<br />
and posterior vagal trunks<br />
Inferior phrenic arteries and plexuses<br />
Left gastric artery and plexus<br />
Hepatic plexus<br />
Greater splanchnic nerves<br />
Right gastric artery and plexus (cut)<br />
Celiac ganglia and plexus<br />
Gastroduodenal artery and plexus<br />
Lesser splanchnic nerves<br />
Least splanchnic nerves<br />
Aorticorenal ganglia<br />
Superior mesenteric ganglion<br />
Intermesenteric (aortic) plexus<br />
Inferior pancreaticoduodenal<br />
arteries and plexuses<br />
Superior mesenteric<br />
artery and plexus<br />
Middle colic artery and plexus (cut)<br />
Right colic artery and plexus<br />
Ileocolic artery and plexus<br />
Superior mesenteric<br />
artery and plexus<br />
Peritoneum (cut edge)<br />
Mesenteric branches<br />
Mesoappendix (contains<br />
appendicular artery and<br />
nerve plexus)<br />
39
NEUROANATOMY<br />
Nerves of Large Intestine<br />
Anterior vagal trunk and hepatic branch<br />
Posterior vagal trunk<br />
Celiac branches of anterior<br />
and posterior vagal trunks<br />
Right inferior phrenic artery and plexus<br />
Right greater<br />
splanchnic nerve<br />
Celiac ganglia and plexus<br />
Right lesser and<br />
least splanchnic<br />
nerves<br />
Right aorticorenal<br />
ganglion<br />
Superior<br />
mesenteric<br />
ganglion<br />
Middle colic<br />
artery<br />
and plexus<br />
Inferior<br />
pancreaticoduodenal<br />
arteries<br />
and plexuses<br />
Right colic<br />
artery<br />
and plexus<br />
Ileocolic<br />
artery<br />
and plexus<br />
Cecal and<br />
appendicular<br />
arteries<br />
and plexuses<br />
Right internal<br />
iliac artery<br />
and plexus (cut)<br />
Sacral sympathetic trunk<br />
Right sacral plexus<br />
Pelvic splanchnic nerves<br />
Middle rectal artery and plexus<br />
Right inferior hypogastric<br />
(pelvic) plexus<br />
Vesical plexus<br />
Rectal plexus<br />
Urinary bladder<br />
Marginal artery and plexus<br />
Esophagus<br />
Left inferior phrenic<br />
artery and plexus<br />
Left gastric artery<br />
and plexus<br />
Left greater<br />
splanchnic<br />
nerve<br />
Left suprarenal<br />
plexus<br />
Left lesser and<br />
least splanchnic<br />
nerves<br />
Left aorticorenal<br />
ganglion<br />
Left renal artery<br />
and plexus<br />
1st left lumbar<br />
splanchnic nerve<br />
Left lumbar<br />
sympathetic trunk<br />
Intermesenteric<br />
(aortic) plexus<br />
Left colic artery<br />
and plexus<br />
Inferior<br />
mesenteric<br />
ganglion, artery<br />
and plexus<br />
Sigmoid<br />
arteries<br />
and plexuses<br />
Superior<br />
hypogastric<br />
plexus<br />
Superior<br />
rectal<br />
artery<br />
and plexus<br />
Right and left<br />
hypogastric<br />
nerves<br />
Rectosigmoid<br />
artery and<br />
plexus<br />
Nerves from inferior hypogastric (pelvic)<br />
plexuses to sigmoid colon, descending<br />
colon and left colic (splenic) flexure<br />
40
Nerves of Kidneys, Ureters and Urinary Bladder<br />
NEUROANATOMY<br />
Anterior vagal trunk<br />
Posterior vagal trunk<br />
Greater splanchnic nerve<br />
Celiac ganglia and plexus<br />
Lesser splanchnic nerve<br />
Superior mesenteric ganglion<br />
Least splanchnic nerve<br />
Aorticorenal ganglion<br />
Renal plexus and ganglion<br />
2nd lumbar splanchnic nerve<br />
Renal and upper ureteric branches<br />
from intermesenteric plexus<br />
Intermesenteric (aortic) plexus<br />
Testicular (ovarian) artery and plexus<br />
Inferior mesenteric ganglion<br />
Sympathetic trunk and ganglion<br />
Middle ureteric branch<br />
Superior hypogastric plexus<br />
Sacral splanchnic nerves<br />
(branches from upper sacral<br />
sympathetic ganglia to<br />
hypogastric plexus)<br />
Gray ramus communicans<br />
Hypogastric nerves<br />
Sacral plexus<br />
Pudendal nerve<br />
Pelvic splanchnic nerves<br />
Inferior hypogastric (pelvic) plexus<br />
with periureteric loops and<br />
branches to lower ureter<br />
Rectal plexus<br />
Vesical plexus<br />
Prostatic plexus<br />
41
NEUROANATOMY<br />
Nerves of Pelvic Viscera: Male<br />
Anterior vagal trunk<br />
Posterior vagal trunk<br />
and<br />
Celiac branch<br />
Inferior phrenic arteries and plexuses<br />
Left gastric artery and gastric plexus<br />
Celiac ganglia, plexus and trunk<br />
Left aorticorenal ganglion<br />
Superior mesenteric ganglion<br />
Superior mesenteric artery and plexus<br />
Intermesenteric (aortic) plexus<br />
Inferior mesenteric ganglion,<br />
artery and plexus<br />
Ureter and ureteric plexus<br />
Superior hypogastric plexus<br />
Superior rectal artery and plexus<br />
Hypogastric nerves<br />
Nerve from inferior<br />
hypogastric plexus<br />
to sigmoid and descending<br />
colon (parasympathetic)<br />
Sacral splanchnic nerves<br />
(sympathetic)<br />
Inferior hypogastric<br />
(pelvic) plexus<br />
Obturator nerve<br />
and artery<br />
Ductus deferens<br />
and plexus<br />
Vesical plexus<br />
Rectal plexus<br />
Prostatic plexus<br />
Cavernous nerves<br />
of penis<br />
T10 spinal nerve (anterior ramus)<br />
White and gray rami communicantes<br />
Greater<br />
Lesser<br />
Least<br />
Gray<br />
White<br />
Lumbosacral trunk<br />
Diaphragm<br />
Gray rami communicantes<br />
Sympathetic trunk and ganglia<br />
5th lumbar splanchnic nerve<br />
L5 spinal nerve (anterior ramus)<br />
Gray rami communicantes<br />
S1 spinal nerve<br />
(anterior ramus)<br />
Sacral plexus<br />
Pudendal nerve<br />
Levator ani muscle<br />
Splanchnic<br />
nerves<br />
Left renal artery<br />
and plexus<br />
L1 spinal nerve<br />
(anterior ramus)<br />
Rami<br />
communicantes<br />
1st, 2nd, 3rd lumbar splanchnic nerves<br />
Pelvic splanchnic<br />
nerves<br />
(parasympathetic)<br />
Piriformis muscle<br />
Gluteus maximus<br />
muscle and sacrotuberous<br />
ligament<br />
(Ischio-)coccygeus<br />
muscle and<br />
sacrospinous ligament<br />
Inferior anal (rectal) nerve<br />
Perineal nerve<br />
Dorsal nerve of penis<br />
Posterior scrotal nerves<br />
42
Nerves of Pelvic Viscera: Female<br />
NEUROANATOMY<br />
Sympathetic trunk<br />
and L2 ganglion<br />
Abdominal aorta<br />
Inferior vena cava<br />
Peritoneum<br />
White and<br />
gray rami<br />
communicantes<br />
Lumbar<br />
splanchnic<br />
nerves<br />
Extraperitoneal<br />
(subserous)<br />
fascia<br />
Common<br />
iliac vessels<br />
and plexus<br />
Ureter<br />
Intermesenteric<br />
(aortic) plexus<br />
Gray rami<br />
communicantes<br />
L5 spinal<br />
nerve<br />
Ovarian artery<br />
and plexus<br />
Superior<br />
hypogastric<br />
plexus<br />
Sacral<br />
promontory<br />
Right<br />
hypogastric<br />
nerve (cut)<br />
Right and<br />
left sacral<br />
sympathetic<br />
trunks and<br />
ganglia<br />
Piriformis<br />
muscle<br />
Sacral<br />
splanchnic<br />
nerves<br />
(sympathetic)<br />
Pudendal<br />
nerve<br />
S2<br />
S3<br />
S4<br />
S5<br />
S1<br />
Superior<br />
hypogastric<br />
plexus<br />
Common<br />
iliac artery<br />
and plexus<br />
Ureter<br />
Internal<br />
iliac artery<br />
and plexus<br />
External<br />
iliac artery<br />
and plexus<br />
Left hypogastric nerve<br />
Inferior hypogastric (pelvic) plexus<br />
Uterine (fallopian) tube<br />
Ovary<br />
Right and left<br />
hypogastric nerves<br />
Uterus<br />
Sigmoid<br />
colon<br />
Right sympathetic trunk<br />
Pelvic<br />
splanchnic<br />
nerves<br />
(parasympathetic)<br />
Symphyseal surface of pubis<br />
Urinary bladder<br />
Vesical plexus<br />
(Ischio-)coccygeus muscle<br />
Uterovaginal plexus<br />
Rectal plexus<br />
Uterus (retracted)<br />
Rectum (retracted)<br />
43
NEUROANATOMY<br />
Median Nerve<br />
Anterior view<br />
Note: Only muscles innervated by median nerve shown<br />
Musculocutaneous nerve<br />
Median nerve (C5, 6, 7, 8, T1)<br />
Inconstant contribution<br />
Pronator teres muscle (humeral head)<br />
Articular branch<br />
Flexor carpi radialis muscle<br />
Palmaris longus muscle<br />
Pronator teres muscle (ulnar head)<br />
Flexor digitorum superficialis muscle<br />
(turned up)<br />
Medial<br />
Posterior<br />
Lateral<br />
Medial cutaneous<br />
nerve of arm<br />
Medial cutaneous<br />
nerve of forearm<br />
Axillary nerve<br />
Radial nerve<br />
Ulnar nerve<br />
Cords of<br />
brachial<br />
plexus<br />
Flexor digitorum profundus muscle<br />
(lateral part supplied by median<br />
[anterior interosseous] nerve;<br />
medial part supplied by ulnar nerve)<br />
Anterior interosseous nerve<br />
Flexor pollicis longus muscle<br />
Pronator quadratus muscle<br />
Palmar branch of median nerve<br />
Cutaneous<br />
innervation<br />
Thenar<br />
muscles<br />
Abductor pollicis brevis<br />
Opponens pollicis<br />
Superficial head of<br />
flexor pollicis brevis<br />
(deep head<br />
supplied by<br />
ulnar nerve)<br />
1st and 2nd<br />
lumbrical muscles<br />
Communicating branch<br />
of median nerve with<br />
ulnar nerve<br />
Common palmar<br />
digital nerves<br />
Palmar view<br />
Dorsal branches to<br />
dorsum of middle and<br />
distal phalanges<br />
Proper palmar<br />
digital nerves<br />
Posterior (dorsal) view<br />
44
Ulnar Nerve<br />
NEUROANATOMY<br />
Anterior view<br />
Note: Only muscles innervated<br />
by ulnar nerve shown<br />
Ulnar nerve (C7, 8, T1)<br />
(no branches above elbow)<br />
Inconstant contribution<br />
Medial epicondyle<br />
Cutaneous<br />
innervation<br />
Articular branch<br />
(behind condyle)<br />
Flexor digitorum profundus<br />
muscle (medial part only;<br />
lateral part supplied by<br />
anterior interosseous<br />
branch of median nerve)<br />
Palmar view<br />
Flexor carpi ulnaris muscle<br />
(drawn aside)<br />
Posterior<br />
(dorsal) view<br />
Dorsal branch of ulnar nerve<br />
Palmar branch<br />
Flexor pollicis brevis muscle<br />
(deep head only; superficial<br />
head and other thenar muscles<br />
supplied by median nerve)<br />
Superficial branch<br />
Deep branch<br />
Adductor pollicis muscle<br />
Palmaris brevis<br />
Abductor digiti minimi<br />
Flexor digiti minimi brevis<br />
Opponens digiti minimi<br />
Hypothenar muscles<br />
Common palmar digital nerve<br />
Communicating branch of median nerve with<br />
ulnar nerve<br />
Palmar and dorsal interosseous muscles<br />
3rd and 4th lumbrical muscles (turned down)<br />
Proper palmar digital nerves<br />
(dorsal digital nerves are from dorsal branch)<br />
Dorsal branches to dorsum of middle and distal phalanges<br />
45
NEUROANATOMY<br />
Radial Nerve in Arm and Nerves of Posterior Shoulder<br />
Dorsal scapular nerve (C5)<br />
Posterior view<br />
Supraspinatus muscle<br />
Suprascapular nerve (C5, 6)<br />
Levator scapulae<br />
muscle (supplied<br />
also by branches<br />
from C3 and C4)<br />
Deltoid muscle<br />
Teres minor muscle<br />
Axillary nerve (C5, 6)<br />
Rhomboid<br />
minor muscle<br />
Rhomboid<br />
major muscle<br />
Superior lateral<br />
cutaneous nerve of arm<br />
Radial nerve<br />
(C5, 6, 7, 8, T1)<br />
Inconstant contribution<br />
Inferior lateral<br />
cutaneous nerve of arm<br />
Infraspinatus muscle<br />
Teres major muscle<br />
Lower subscapular nerve (C5, 6)<br />
Posterior cutaneous nerve of arm<br />
(branch of radial nerve in axilla)<br />
Triceps brachii muscle<br />
Long head<br />
Lateral head<br />
Medial head<br />
Posterior cutaneous<br />
nerve of forearm<br />
Lateral intermuscular<br />
septum<br />
Brachialis muscle (lateral<br />
part; remainder of muscle<br />
supplied by musculocutaneous<br />
nerve)<br />
Brachioradialis muscle<br />
Triceps brachii tendon<br />
Medial epicondyle<br />
Olecranon<br />
Anconeus muscle<br />
Extensor digitorum muscle<br />
Extensor carpi radialis<br />
longus muscle<br />
Extensor carpi<br />
radialis brevis<br />
muscle<br />
Extensor carpi ulnaris muscle<br />
46
Radial Nerve in Forearm<br />
NEUROANATOMY<br />
Radial nerve (C5, 6, 7, 8, T1)<br />
Inconstant contribution<br />
Superficial (terminal) branch<br />
Deep (terminal) branch<br />
Lateral epicondyle<br />
Posterior view<br />
Anconeus muscle<br />
Brachioradialis muscle<br />
Extensor carpi radialis longus muscle<br />
Supinator muscle<br />
Extensor carpi radialis brevis muscle<br />
Extensor carpi ulnaris muscle<br />
Extensor digitorum muscle and<br />
extensor digiti minimi muscle<br />
Extensor indicis muscle<br />
Extensor-supinator<br />
group of muscles<br />
Extensor pollicis longus muscle<br />
Abductor pollicis longus muscle<br />
Extensor pollicis brevis muscle<br />
Posterior interosseous nerve<br />
(continuation of deep branch of<br />
radial nerve distal to supinator muscle)<br />
Superficial branch of radial nerve<br />
From axillary nerve<br />
Superior lateral<br />
cutaneous nerve<br />
of arm<br />
Inferior lateral<br />
cutaneous nerve<br />
of arm<br />
From radial nerve<br />
Posterior cutaneous<br />
nerve of arm<br />
Posterior cutaneous<br />
nerve of forearm<br />
Superficial branch of<br />
radial nerve and dorsal<br />
digital branches<br />
Dorsal digital nerves<br />
Cutaneous innervation from<br />
radial and axillary nerves<br />
47
NEUROANATOMY<br />
Sciatic Nerve and Posterior Cutaneous Nerve of Thigh<br />
Posterior cutaneous<br />
nerve of thigh<br />
(S1, 2, 3)<br />
Inferior cluneal nerves<br />
Perineal branches<br />
Greater sciatic foramen<br />
Sciatic nerve (L4, 5, S1, 2, 3)<br />
Tibial division<br />
of sciatic nerve<br />
Common fibular (peroneal)<br />
division of sciatic nerve<br />
Long head (cut) of<br />
biceps femoris muscle<br />
Short head of<br />
biceps femoris muscle<br />
Cutaneous innervation<br />
Adductor magnus muscle<br />
(also partially supplied<br />
by obturator nerve)<br />
Semitendinosus muscle<br />
Semimembranosus muscle<br />
Long head (cut)<br />
of biceps femoris<br />
muscle<br />
Common fibular<br />
(peroneal) nerve<br />
Tibial nerve<br />
Articular branch<br />
Plantaris muscle<br />
Articular<br />
branch<br />
Lateral sural<br />
cutaneous nerve<br />
Posterior<br />
cutaneous nerve<br />
of thigh<br />
Medial sural<br />
cutaneous nerve<br />
Gastrocnemius muscle<br />
Sural nerve<br />
Soleus muscle<br />
Tibial nerve<br />
Medial<br />
calcaneal branches<br />
Medial and lateral<br />
plantar nerves<br />
Sural<br />
communicating<br />
branch<br />
Lateral calcaneal<br />
branches<br />
Lateral dorsal<br />
cutaneous nerve<br />
From sciatic<br />
nerve<br />
Common fibular<br />
(peroneal) nerve<br />
via lateral sural<br />
cutaneous nerve<br />
Medial sural<br />
cutaneous nerve<br />
Superficial fibular<br />
(peroneal) nerve<br />
Sural nerve<br />
Tibial nerve<br />
via medial<br />
calcaneal<br />
branches<br />
48
Tibial Nerve<br />
NEUROANATOMY<br />
Tibial nerve<br />
(L4, 5, S1, 2, 3)<br />
Medial sural<br />
cutaneous nerve (cut)<br />
Articular branches<br />
Plantaris muscle<br />
Gastrocnemius<br />
muscle (cut)<br />
Nerve to popliteus muscle<br />
Popliteus muscle<br />
Interosseous nerve of leg<br />
Common fibular (peroneal) nerve<br />
Lateral sural cutaneous nerve (cut)<br />
From<br />
tibial nerve<br />
Articular branch<br />
Medial calcaneal<br />
branches<br />
(S1, 2)<br />
Medial<br />
plantar nerve<br />
(L4, 5)<br />
Lateral<br />
plantar nerve<br />
(S1, 2)<br />
Saphenous nerve<br />
(L3, 4)<br />
Sural nerve<br />
(S1, 2) via<br />
lateral calcaneal<br />
and lateral dorsal<br />
cutaneous<br />
branches<br />
Cutaneous innervation of sole<br />
Soleus muscle (cut and<br />
partly retracted)<br />
Flexor digitorum<br />
longus muscle<br />
Tibialis posterior muscle<br />
Flexor hallucis<br />
longus muscle<br />
Sural nerve (cut)<br />
Lateral calcaneal branch<br />
Medial<br />
calcaneal branch<br />
Flexor retinaculum (cut)<br />
Lateral dorsal<br />
cutaneous nerve<br />
Flexor<br />
retinaculum<br />
(cut)<br />
Tibial<br />
nerve<br />
Medial<br />
calcaneal<br />
branch<br />
Medial plantar<br />
nerve<br />
Flexor digitorum<br />
brevis muscle<br />
and nerve<br />
Abductor hallucis<br />
muscle and nerve<br />
Flexor hallucis<br />
brevis muscle<br />
and nerve<br />
1st lumbrical<br />
muscle and<br />
nerve<br />
Common<br />
plantar<br />
digital<br />
nerves<br />
Proper<br />
plantar<br />
digital<br />
nerves<br />
Lateral calcaneal<br />
branch of sural nerve<br />
Lateral plantar<br />
nerve<br />
Nerve to abductor<br />
digiti minimi muscle<br />
Quadratus plantae<br />
muscle and nerve<br />
Abductor digiti<br />
minimi muscle<br />
Deep branch to<br />
interosseous<br />
muscles,<br />
2nd, 3rd and 4th<br />
lumbrical muscles<br />
and<br />
Adductor hallucis<br />
muscle<br />
Superficial<br />
branch to<br />
4th interosseous<br />
muscle<br />
and<br />
Flexor digiti minimi<br />
brevis muscle<br />
Common and<br />
Proper plantar<br />
digital nerves<br />
Note: Articular branches not shown<br />
49
NEUROANATOMY<br />
Common Fibular (Peroneal) Nerve<br />
Common fibular<br />
(peroneal) nerve<br />
(phantom)<br />
Biceps femoris tendon<br />
Common fibular (peroneal)<br />
nerve (L4, 5, S1, 2)<br />
Lateral sural cutaneous nerve (phantom)<br />
Articular branches<br />
Recurrent articular nerve<br />
Extensor digitorum longus muscle (cut)<br />
Head of fibula<br />
Fibularis (peroneus)<br />
longus muscle (cut)<br />
Deep fibular (peroneal) nerve<br />
Tibialis anterior muscle<br />
Superficial fibular<br />
(peroneal) nerve<br />
Cutaneous innervation<br />
Branches of lateral<br />
sural cutaneous nerve<br />
Extensor digitorum<br />
longus muscle<br />
Fibularis (peroneus)<br />
longus muscle<br />
Fibularis (peroneus)<br />
brevis muscle<br />
Extensor hallucis<br />
longus muscle<br />
Lateral sural<br />
cutaneous nerve<br />
Medial dorsal cutaneous nerve<br />
Superficial fibular<br />
(peroneal) nerve<br />
Intermediate dorsal<br />
cutaneous nerve<br />
Inferior extensor<br />
retinaculum (partially cut)<br />
Lateral dorsal cutaneous nerve<br />
(branch of sural nerve)<br />
Lateral branch of<br />
deep fibular<br />
(peroneal) nerve to<br />
Extensor hallucis brevis<br />
and<br />
Extensor digitorum brevis<br />
muscles<br />
Medial branch of<br />
deep fibular<br />
(peroneal) nerve<br />
Deep<br />
fibular<br />
(peroneal)<br />
nerve<br />
Dorsal digital nerves<br />
Sural nerve<br />
via lateral dorsal<br />
cutaneous branch<br />
50
Part 2 <strong>Neuro</strong>physiology<br />
Organization of the Brain: Cerebrum. . . . . . . 52<br />
Organization of the Brain: Cell Types. . . . . . . 53<br />
Blood-Brain Barrier . . . . . . . . . . . . . . . . . . . . . 54<br />
Synaptic Transmission:<br />
Morphology of Synapses . . . . . . . . . . . . . . . 55<br />
Synaptic Transmission:<br />
<strong>Neuro</strong>muscular Junction . . . . . . . . . . . . . . . 56<br />
Synaptic Transmission:<br />
Visceral Efferent Endings . . . . . . . . . . . . . . . 57<br />
Synaptic Transmission:<br />
Inhibitory Mechanisms . . . . . . . . . . . . . . . . 58<br />
Synaptic Transmission:<br />
Chemical Synaptic Transmission . . . . . . . . . 59<br />
Synaptic Transmission:<br />
Temporal and Spatial Summation . . . . . . . . 60<br />
Cerebrospinal Fluid (CSF):<br />
Brain Ventricles and CSF Composition . . . . 61<br />
Cerebrospinal Fluid (CSF):<br />
Circulation of CSF . . . . . . . . . . . . . . . . . . . . 62<br />
Spinal Cord: Ventral Rami. . . . . . . . . . . . . . . . 63<br />
Spinal Cord: Membranes and Nerve Roots . . 64<br />
Peripheral Nervous System . . . . . . . . . . . . . . . 65<br />
Autonomic Nervous System: Schema. . . . . . . 66<br />
Autonomic Nervous System:<br />
Cholinergic and Adrenergic Synapses . . . . . 67<br />
Hypothalamus . . . . . . . . . . . . . . . . . . . . . . . . . 68<br />
Limbic System . . . . . . . . . . . . . . . . . . . . . . . . . 69<br />
The Cerebral Cortex . . . . . . . . . . . . . . . . . . . . 70<br />
Descending Motor Pathways . . . . . . . . . . . . . 71<br />
Cerebellum: Afferent Pathways. . . . . . . . . . . . 72<br />
Cerebellum: Efferent Pathways . . . . . . . . . . . . 73<br />
Cutaneous Sensory Receptors. . . . . . . . . . . . . 74<br />
Cutaneous Receptors:<br />
Pacinian Corpuscle. . . . . . . . . . . . . . . . . . . . 75<br />
Proprioception and Reflex Pathways: I . . . . . . 76<br />
Proprioception and Reflex Pathways: II . . . . . 77<br />
Proprioception and Reflex Pathways: III . . . . 78<br />
Proprioception and Reflex Pathways: IV. . . . . 79<br />
Sensory Pathways: I. . . . . . . . . . . . . . . . . . . . . 80<br />
Sensory Pathways: II . . . . . . . . . . . . . . . . . . . . 81<br />
Sensory Pathways: III. . . . . . . . . . . . . . . . . . . . 82<br />
Visual System: Receptors. . . . . . . . . . . . . . . . . 83<br />
Visual System: Visual Pathway . . . . . . . . . . . . 84<br />
Auditory System: Cochlea . . . . . . . . . . . . . . . . 85<br />
Auditory System: Pathways . . . . . . . . . . . . . . . 86<br />
Vestibular System: Receptors . . . . . . . . . . . . . 87<br />
Vestibular System: Vestibulospinal Tracts. . . . 88<br />
Gustatory (Taste) System: Receptors . . . . . . . 89<br />
Gustatory (Taste) System: Pathways . . . . . . . . 90<br />
Olfactory System: Receptors . . . . . . . . . . . . . . 91<br />
Olfactory System: Pathway . . . . . . . . . . . . . . . 92
NEUROPHYSIOLOGY<br />
Organization of the Brain: Cerebrum<br />
Precentral sulcus<br />
Central sulcus (Rolando)<br />
Precentral gyrus<br />
Postcentral gyrus<br />
Postcentral sulcus<br />
Superior parietal lobule<br />
Inferior parietal lobule<br />
Supramarginal gyrus<br />
Angular gyrus<br />
Parietooccipital<br />
sulcus<br />
Frontal pole<br />
Occipital pole<br />
Calcarine sulcus<br />
Lateral sulcus<br />
(Sylvius)<br />
Temporal pole<br />
Superior temporal gyrus<br />
Middle temporal gyrus<br />
Inferior temporal gyrus<br />
Frontal lobe<br />
Parietal lobe<br />
Temporal lobe<br />
Occipital lobe<br />
Insula (island of Reil)<br />
©<br />
FIGURE 2.1<br />
ORGANIZATION OF THE BRAIN: CEREBRUM •<br />
The cerebral cortex represents the highest center for sensory and<br />
motor processing. In general, the frontal lobe processes motor,<br />
visual, speech, and personality modalities. The parietal lobe<br />
processes sensory information; the temporal lobe, auditory and<br />
memory modalities; and the occipital lobe, vision. The cerebellum<br />
coordinates smooth motor activities and processes muscle position.<br />
The brainstem (medulla, pons, midbrain) conveys motor and sensory<br />
information and mediates important autonomic functions. The spinal<br />
cord receives sensory input from the body and conveys somatic and<br />
autonomic motor information to peripheral targets (muscles, viscera).<br />
52
Organization of the Brain: Cell Types<br />
NEUROPHYSIOLOGY<br />
Multipolar (pyramidal)<br />
cell of cerebral<br />
motor cortex<br />
Astrocyte<br />
Motor<br />
endplate<br />
Multipolar somatic<br />
motor cell of nuclei<br />
of cranial nn.<br />
Multipolar cell<br />
of lower brain<br />
motor centers<br />
Oligodendrocyte<br />
Corticospinal<br />
(pyramidal) fiber<br />
Axodendritic ending<br />
Axosomatic ending<br />
Axoaxonic ending<br />
Multipolar somatic<br />
motor cell of<br />
anterior horn<br />
of spinal cord<br />
Collateral<br />
Striated<br />
(somatic)<br />
muscle<br />
Renshaw interneuron<br />
(feedback)<br />
Myelinated somatic motor<br />
fiber of spinal nerve<br />
Interneurons<br />
Blood vessel<br />
Interneuron<br />
Astrocyte<br />
Multipolar visceral<br />
motor (autonomic)<br />
cell of spinal cord<br />
Autonomic preganglionic<br />
(sympathetic or parasympathetic)<br />
nerve fiber<br />
Myelin sheath<br />
Autonomic postganglionic<br />
neuron of sympathetic or<br />
parasympathetic ganglion<br />
Satellite cells<br />
Unmyelinated nerve fiber<br />
Schwann cells<br />
Bipolar cell of cranial n.<br />
Unipolar cell of<br />
sensory ganglia of<br />
cranial nn.<br />
Satellite cells<br />
Schwann cell<br />
Free nerve endings<br />
(unmyelinated fibers)<br />
Encapsulated ending<br />
Specialized ending<br />
Muscle spindle<br />
Unipolar sensory cell<br />
of dorsal spinal<br />
root ganglion<br />
Satellite cells<br />
Myelinated afferent<br />
fiber of spinal nerve<br />
Myelin sheath<br />
Red: Motor neuron<br />
Blue: Sensory neuron<br />
Purple: Interneuron<br />
Gray: Glial and<br />
neurilemmal cells<br />
and myelin<br />
Note: Cerebellar cells<br />
not shown here<br />
Myelin sheath<br />
Schwann cells<br />
Motor endplate with<br />
Schwann cell cap<br />
Striated<br />
(voluntary)<br />
muscle<br />
Endings on<br />
cardiac muscle<br />
or nodal cells<br />
Beaded<br />
varicosities<br />
and endings on<br />
smooth muscle<br />
and gland cells<br />
Unmyelinated fibers<br />
Free nerve endings<br />
Encapsulated ending<br />
Muscle spindle<br />
©<br />
FIGURE 2.2<br />
ORGANIZATION OF THE BRAIN: CELL TYPES •<br />
<strong>Neuro</strong>ns form the functional cellular units responsible for<br />
communication, and throughout the nervous system, they are<br />
characterized by their distinctive size and shapes (e.g., bipolar,<br />
unipolar, multipolar). Supporting cells include the neuroglia<br />
(e.g., astrocytes, oligodendrocytes), satellite cells, and other specialized<br />
cells that optimize neuronal function, provide maintenance<br />
functions, or protect the nervous system.<br />
53
NEUROPHYSIOLOGY<br />
Blood-Brain Barrier<br />
Tight<br />
junction<br />
proteins<br />
Cell<br />
membrane<br />
Basement<br />
membrane<br />
Cytoplasm<br />
Red<br />
blood<br />
cell<br />
Capillary<br />
lumen<br />
Astrocyte<br />
foot processes<br />
Tight<br />
junction<br />
Capillary<br />
endothelial<br />
cell<br />
Astrocyte<br />
©<br />
FIGURE 2.3<br />
BLOOD-BRAIN BARRIER •<br />
The blood-brain barrier (BBB) is the cellular interface between the<br />
blood and the central nervous system (CNS; brain and spinal cord).<br />
It serves to maintain the interstitial fluid environment to ensure<br />
optimal functionality of the neurons. This barrier consists of the<br />
capillary endothelial cells with an elaborate network of tight junctions<br />
and astrocytic foot processes that abut the endothelium and<br />
its basement membrane. The movement of large molecules and<br />
54<br />
other substances (including many drugs) from the blood to the<br />
interstitial space of the CNS is restricted by the BBB. CNS endothelial<br />
cells also exhibit a low level of pinocytotic activity across the<br />
cell, so specific carrier systems for the transport of essential substrates<br />
of energy and amino acid metabolism are characteristic of<br />
these cells. The astrocytes help transfer important metabolites from<br />
the blood to the neurons and also remove excess K and neurotransmitters<br />
from the interstitial fluid.
Synaptic Transmission: Morphology of Synapses<br />
NEUROPHYSIOLOGY<br />
Dendrite<br />
Node<br />
Axon<br />
Dendrites<br />
Myelin sheath<br />
Numerous boutons (synaptic knobs)<br />
of presynaptic neurons terminating<br />
on a motor neuron and its dendrites<br />
Enlarged section<br />
of bouton<br />
Axolemma<br />
Mitochondria<br />
Glial process<br />
Synaptic vesicles<br />
Synaptic cleft<br />
Presynaptic membrane<br />
(densely staining)<br />
Postsynaptic membrane<br />
(densely staining)<br />
Postsynaptic cell<br />
Axon (axoplasm)<br />
©<br />
FIGURE 2.4<br />
MORPHOLOGY OF SYNAPSES •<br />
<strong>Neuro</strong>ns communicate with each other and with effector targets at<br />
specialized regions called synapses. The top figure shows a typical<br />
motor neuron that receives numerous synaptic contacts on its cell<br />
body and associated dendrites. Incoming axons lose their myelin<br />
sheaths, exhibit extensive branching, and terminate as synaptic<br />
boutons (synaptic terminals or knobs) on the motor neuron. The<br />
lower figure shows an enlargement of one such synaptic bouton.<br />
Chemical neurotransmitters are contained in synaptic vesicles,<br />
which can fuse with the presynaptic membrane, release the transmitters<br />
into the synaptic cleft, and then bind to receptors situated<br />
in the postsynaptic membrane. This synaptic transmission results in<br />
excitatory, inhibitory, or modulatory effects on the target cell.<br />
55
NEUROPHYSIOLOGY<br />
Synaptic Transmission: <strong>Neuro</strong>muscular Junction<br />
Structure of <strong>Neuro</strong>muscular Junction<br />
Active zone<br />
Schwann cell process<br />
Acetylcholine<br />
receptor sites<br />
Myelin sheath<br />
Neurilemma<br />
Axoplasm<br />
Schwann cell<br />
Mitochondria<br />
Basement membrane<br />
Nucleus of Schwann cell<br />
Presynaptic membrane<br />
Active zone<br />
Synaptic vesicles<br />
Synaptic trough<br />
Basement membrane<br />
Sarcolemma<br />
Nucleus of<br />
muscle cell<br />
Myofibrils<br />
Synaptic cleft<br />
Postsynaptic<br />
membrane<br />
Junctional fold<br />
Sarcoplasm<br />
Acetylcholine receptor sites<br />
©<br />
FIGURE 2.5<br />
STRUCTURE OF THE NEUROMUSCULAR JUNCTION •<br />
Motor axons that synapse on skeletal muscle form expanded terminals<br />
called neuromuscular junctions (motor endplates). The motor<br />
axon loses its myelin sheath and expands into a Schwann<br />
cell–invested synaptic terminal that resides within a trough in the<br />
muscle fiber. Acetylcholine-containing synaptic vesicles accumulate<br />
adjacent to the presynaptic membrane and, when appropriately<br />
stimulated, release their neurotransmitter into the synaptic<br />
cleft. The transmitter then binds to receptors that mediate depolarization<br />
of the muscle sarcolemma and initiate a muscle action<br />
potential. A single muscle fiber has only one neuromuscular junction,<br />
but a motor axon can innervate multiple muscle fibers.<br />
56
Synaptic Transmission: Visceral Efferent Endings<br />
NEUROPHYSIOLOGY<br />
Visceral Efferent Endings<br />
A. Smooth muscle<br />
Smooth muscle cells (cut)<br />
Schwann cell cap enclosing<br />
nerve axons<br />
Mucous cells<br />
Schwann cell<br />
cap enclosing<br />
nerve axons<br />
B. Gland (submandibular)<br />
Sympathetic terminal<br />
ending<br />
Varicosity<br />
Schwann<br />
cell cap<br />
⎧<br />
⎪⎪⎨⎪⎪⎩<br />
⎧<br />
⎪⎪⎨⎪⎪⎩<br />
⎧<br />
⎪⎪⎨⎪⎪⎩<br />
Axon<br />
C. <strong>Neuro</strong>secretory<br />
(posterior pituitary)<br />
Pituicyte processes<br />
Axon<br />
Schwann cell cap<br />
Smooth muscle cells<br />
Varicosities<br />
Terminal endings<br />
Serous cells<br />
Parasympathetic<br />
terminal ending<br />
Schwann cell<br />
cap enclosing<br />
nerve axons<br />
Varicosity<br />
Capillary<br />
Endothelium<br />
Mast cell<br />
Fibroblast<br />
<strong>Neuro</strong>secretory<br />
vesicles<br />
Collagen space<br />
Basement membrane<br />
©<br />
FIGURE 2.6<br />
VISCERAL EFFERENT ENDINGS •<br />
<strong>Neuro</strong>nal efferent endings on smooth muscle (A) and glands (B<br />
and C) exhibit unique endings unlike the presynaptic and postsynaptic<br />
terminals observed in neuronal and neuromuscular junction<br />
synapses. Rather, neurotransmitter substances are released<br />
into interstitial spaces (A and B) or into the bloodstream (C, neurosecretion)<br />
from expanded nerve terminal endings. This arrangement<br />
allows for the stimulation of numerous target cells over a<br />
wide area. Not all smooth muscle cells are innervated. They are<br />
connected to adjacent cells by gap junctions and can therefore<br />
contract together with the innervated cells.<br />
57
NEUROPHYSIOLOGY<br />
Synaptic Transmission: Inhibitory Mechanisms<br />
E<br />
(Excitatory<br />
fiber)<br />
I<br />
(Inhibitory<br />
fiber)<br />
E<br />
(Excitatory<br />
fiber)<br />
Motor<br />
neuron<br />
Motor<br />
neuron<br />
Axon<br />
I<br />
(Inhibitory<br />
fiber)<br />
Axon<br />
A. Only E fires<br />
90-mV spike<br />
in E terminal<br />
mV<br />
20<br />
90 mV A′. Only E fires<br />
mV<br />
EPSP in<br />
motor neuron<br />
70<br />
60<br />
70<br />
EPSP in<br />
motor<br />
neuron<br />
60<br />
70<br />
B. Only I fires<br />
Long-lasting<br />
partial<br />
depolarization<br />
in E terminal<br />
No response in<br />
motor neuron<br />
60<br />
70<br />
70<br />
B′. Only I fires<br />
Motor<br />
neuron<br />
hyperpolarized<br />
70<br />
80<br />
C. I fires before E<br />
Partial<br />
depolarization<br />
of E terminal<br />
reduces spike<br />
to 80 mV, thus<br />
releasing less<br />
transmitter<br />
substance<br />
Smaller EPSP in<br />
motor neuron<br />
20<br />
70<br />
60<br />
70<br />
80 mV<br />
C′. I fires before E<br />
Depolarization<br />
of motor<br />
neuron less<br />
than if only<br />
E fires<br />
60<br />
70<br />
80<br />
©<br />
FIGURE 2.7<br />
SYNAPTIC INHIBITORY MECHANISMS •<br />
Inhibitory synapses modulate neuronal activity. Illustrated here is presynaptic inhibition (left panel) and postsynaptic inhibition (right<br />
panel) at a motor neuron.<br />
58
Synaptic Transmission: Chemical Synaptic Transmission<br />
NEUROPHYSIOLOGY<br />
Excitatory<br />
⎧<br />
⎪⎪⎨⎪⎪⎩<br />
⎧<br />
⎪⎪⎨⎪⎪⎩<br />
Synaptic<br />
vesicles<br />
in synaptic<br />
bouton<br />
Presynaptic<br />
membrane<br />
Inhibitory<br />
<br />
<br />
<br />
<br />
<br />
<br />
Na Current<br />
K <br />
<br />
<br />
<br />
<br />
Transmitter<br />
substances<br />
Synaptic cleft<br />
Postsynaptic<br />
membrane<br />
<br />
<br />
<br />
<br />
<br />
<br />
Cl <br />
<br />
<br />
<br />
<br />
When impulse reaches excitatory synaptic<br />
bouton, it causes release of a transmitter<br />
substance into synaptic cleft. This increases<br />
permeability of postsynaptic membrane to<br />
Na and K . More Na moves into postsynaptic<br />
cell than K moves out, due to greater<br />
electrochemical gradient<br />
At inhibitory synapse, transmitter substance released<br />
by an impulse increases permeability of<br />
the postsynaptic membrane to Cl . K moves<br />
out of post-synaptic cell but no net flow of Cl <br />
occurs at resting membrane potential<br />
Synaptic bouton<br />
Resultant net ionic current flow is in a direction<br />
that tends to depolarize postsynaptic cell.<br />
If depolarization reaches firing threshold, an<br />
impulse is generated in postsynaptic cell<br />
Potential (mV)<br />
65<br />
Potential<br />
70 0 4 8 12 16<br />
msec<br />
Current flow and potential change<br />
Resultant ionic current flow is in direction that tends to<br />
hyperpolarize postsynaptic cell. This makes depolarization<br />
by excitatory synapses more difficult—more depolarization<br />
is required to reach threshold<br />
msec<br />
12 16<br />
75<br />
Current<br />
Potential<br />
Potential (mV)70 0 4 8<br />
Current flow and potential change<br />
©<br />
FIGURE 2.8<br />
CHEMICAL SYNAPTIC TRANSMISSION •<br />
Chemical synaptic transmission between neurons may be excitatory<br />
or inhibitory. During excitation (left column), a net increase in<br />
the inward flow of Na compared with the outward flow of K <br />
results in a depolarizing potential change (excitatory postsynaptic<br />
potential [EPSP]) that drives the postsynaptic cell closer to its<br />
threshold for an action potential. During inhibition (right column),<br />
the opening of K and Cl channels drives the membrane potential<br />
away from threshold (hyperpolarization) and decreases the probability<br />
that the neuron will reach threshold (inhibitory postsynaptic<br />
potential [IPSP]) for an action potential.<br />
59
NEUROPHYSIOLOGY<br />
Synaptic Transmission: Temporal and Spatial Summation<br />
Temporal and Spatial Summation<br />
of Excitation and Inhibition<br />
Excitatory fibers<br />
mV<br />
Excitatory fibers<br />
mV<br />
–70<br />
–70<br />
Axon<br />
Axon<br />
Inhibitory fibers<br />
A. Resting state: motor nerve cell shown with synaptic boutons of<br />
excitatory and inhibitory nerve fibers ending close to it<br />
Inhibitory fibers<br />
B. Partial depolarization: impulse from one excitatory fiber has<br />
caused partial (below firing threshold) depolarization of motor<br />
neuron<br />
Excitatory fibers<br />
mV<br />
–70<br />
Excitatory fibers<br />
mV<br />
–70<br />
Inhibitory fibers<br />
Axon<br />
C. Temporal excitatory summation: a series of impulses in one<br />
excitatory fiber together produce a suprathreshold depolarization<br />
that triggers an action potential<br />
Inhibitory fibers<br />
Axon<br />
D. Spatial excitatory summation: impulses in two excitatory fibers<br />
cause two synaptic depolarizations that together reach firing<br />
threshold triggering an action potential<br />
Excitatory fibers<br />
mV<br />
Excitatory fibers<br />
mV<br />
–70<br />
–70<br />
Axon<br />
Axon<br />
Inhibitory fibers<br />
E. Spatial excitatory summation with inhibition: impulses from<br />
two excitatory fibers reach motor neuron but impulses from<br />
inhibitory fiber prevent depolarization from reaching threshold<br />
Inhibitory fibers<br />
E. (continued): motor neuron now receives additional excitatory<br />
impulses and reaches firing threshold despite a simultaneous<br />
inhibitory impulse; additional inhibitory impulses might still<br />
prevent firing<br />
©<br />
CHART 2.1<br />
SUMMARY OF SOME NEUROTRANSMITTERS AND WHERE WITHIN THE CENTRAL AND PERIPHERAL NERVOUS<br />
SYSTEM THEY ARE FOUND<br />
Transmitter<br />
Acetylcholine<br />
Biogenic amines<br />
Norepinephrine<br />
Dopamine<br />
Serotonin<br />
Amino acids<br />
-Aminobutyric<br />
acid (GABA)<br />
Glutamate<br />
Purines<br />
Adenosine<br />
Adenosine<br />
triphosphate (ATP)<br />
Location<br />
<strong>Neuro</strong>muscular junction, autonomic endings<br />
and ganglia, CNS<br />
Sympathetic endings, CNS<br />
CNS<br />
CNS, GI tract<br />
CNS<br />
CNS<br />
CNS<br />
CNS<br />
Transmitter<br />
Gas<br />
Nitric oxide<br />
Peptides<br />
-Endorphins<br />
Enkephalins<br />
Antidiuretic<br />
hormone<br />
Pituitary-releasing<br />
hormones<br />
Somatostatin<br />
<strong>Neuro</strong>peptide Y<br />
Vasoactive<br />
intestinal peptide<br />
Location<br />
CNS, GI tract<br />
CNS, GI tract<br />
CNS<br />
CNS (hypothalamus/posterior<br />
pituitary)<br />
CNS (hypothalamus/anterior<br />
pituitary)<br />
CNS, GI tract<br />
CNS<br />
CNS, GI tract<br />
CNS, Central nervous system; GI, gastrointestinal.<br />
FIGURE 2.9<br />
TEMPORAL AND SPATIAL SUMMATION •<br />
<strong>Neuro</strong>ns receive multiple excitatory and inhibitory inputs. Temporal<br />
summation occurs when a series of subthreshold impulses in<br />
one excitatory fiber produces an action potential in the postsynaptic<br />
cell (panel C). Spatial summation occurs when subthreshold<br />
impulses from two or more different fibers trigger an action potential<br />
(panel D). Both temporal and spatial summation can be modulated<br />
by simultaneous inhibitory input (panel E). Inhibitory and<br />
excitatory neurons use a wide variety of neurotransmitters, some of<br />
which are summarized here.<br />
60
Cerebrospinal Fluid (CSF): Brain Ventricles and CSF Composition<br />
NEUROPHYSIOLOGY<br />
Left lateral phantom view<br />
Right lateral ventricle<br />
Frontal (anterior) horn<br />
Central part<br />
Temporal (inferior) horn<br />
Occipital (posterior) horn<br />
Left<br />
lateral<br />
ventricle<br />
Cerebral aqueduct (Sylvius)<br />
4th ventricle<br />
Left lateral aperture<br />
(foramen of Luschka)<br />
Left interventricular<br />
foramen (Monro)<br />
3rd ventricle<br />
Left lateral recess<br />
Median aperture<br />
(foramen of Magendie)<br />
Central canal of spinal cord<br />
©<br />
CHART 2.2<br />
CSF COMPOSITION<br />
CSF<br />
Blood Plasma<br />
Na (mEq/L) 140–145 135–147<br />
K (mEq/L) 3 3.5–5.0<br />
Cl − (mEq/L) 115–120 95–105<br />
HCO 3− (mEq/L) 20 22–28<br />
Glucose (mg/dL) 50–75 70–110<br />
Protein (g/dL) 0.05–0.07 6.0–7.8<br />
pH 7.3 7.35–7.45<br />
FIGURE 2.10<br />
BRAIN VENTRICLES AND CSF COMPOSITION •<br />
CSF circulates through the four brain ventricles (two lateral ventricles<br />
and a third and fourth ventricle) and in the subarachnoid<br />
space surrounding the brain and spinal cord. The electrolyte composition<br />
of the CSF is regulated by the choroid plexus, which<br />
secretes the CSF. Importantly, the CSF has a lower [HCO 3 ] than<br />
plasma and therefore a lower pH. This allows small changes in<br />
blood PCO 2 to cause changes in CSF pH, which in turn regulates<br />
the rate of respiration (see Chapter 5).<br />
61
NEUROPHYSIOLOGY<br />
Cerebrospinal Fluid (CSF): Circulation of CSF<br />
Dura mater<br />
Choroid plexus of lateral<br />
ventricle (phantom)<br />
Cistern of corpus callosum<br />
Superior sagittal sinus<br />
Subarachnoid space<br />
Arachnoid granulations<br />
Arachnoid<br />
Interventricular<br />
foramen (Monro)<br />
Choroid plexus of 3rd ventricle<br />
Cerebral aqueduct (Sylvius)<br />
Lateral aperture (foramen of Luschka)<br />
Choroid plexus of 4th ventricle<br />
Dura mater<br />
Median aperture<br />
(foramen of Magendie)<br />
Arachnoid<br />
Subarachnoid space<br />
Central canal of spinal cord<br />
©<br />
FIGURE 2.11<br />
CIRCULATION OF CEREBROSPINAL FLUID •<br />
CSF circulates through the four brain ventricles (two lateral ventricles<br />
and a third and fourth ventricle) and in the subarachnoid<br />
space surrounding the brain and spinal cord. Most of the CSF is<br />
reabsorbed into the venous system through the arachnoid granulations<br />
and through the walls of the capillaries of the central nervous<br />
system and pia mater.<br />
62
Spinal Cord: Ventral Rami<br />
NEUROPHYSIOLOGY<br />
Base of skull<br />
C1 spinal nerve<br />
C8 spinal nerve<br />
T1 spinal nerve<br />
C1 vertebra (atlas)<br />
Cervical plexus<br />
Brachial plexus<br />
Intercostal<br />
nerves<br />
1st rib<br />
Spinal dura mater<br />
Filaments<br />
of spinal<br />
nerve roots<br />
(T7 and T8)<br />
T12 spinal<br />
nerve<br />
12th rib<br />
L1<br />
vertebra<br />
Conus medullaris<br />
L1 spinal nerve<br />
Cauda equina<br />
S1 spinal nerve<br />
Sacrum (cut away)<br />
Termination of<br />
dural sac<br />
Coccygeal nerve<br />
Lumbar plexus<br />
L5 vertebra<br />
Sacral plexus<br />
Sciatic nerve<br />
Coccyx<br />
©<br />
FIGURE 2.12<br />
SPINAL CORD AND VENTRAL RAMI IN SITU •<br />
The spinal cord gives rise to 31 pairs of spinal nerves that distribute<br />
segmentally to the body. These nerves are organized into plexuses<br />
that distribute to the neck (cervical plexus), upper limb (brachial<br />
plexus), and pelvis and lower limb (lumbosacral plexus). Motor<br />
fibers of these spinal nerves innervate skeletal muscle, and sensory<br />
fibers convey information back to the central nervous system from<br />
the skin, skeletal muscles, and joints.<br />
63
NEUROPHYSIOLOGY<br />
Spinal Cord: Membranes and Nerve Roots<br />
Posterior view<br />
Ventral root of spinal nerve<br />
Dorsal root of spinal nerve<br />
Spinal sensory (dorsal root) ganglion<br />
Ventral ramus of spinal nerve<br />
Dorsal ramus of spinal nerve<br />
Dura mater<br />
Arachnoid mater<br />
Subarachnoid space<br />
Pia mater overlying spinal cord<br />
Filaments of dorsal root<br />
Membranes removed: anterior view<br />
(greatly magnified)<br />
Gray matter<br />
White matter<br />
Filaments of dorsal root<br />
Dorsal root of spinal nerve<br />
Filaments of ventral root<br />
Spinal sensory (dorsal<br />
root) ganglion<br />
Dorsal ramus of<br />
spinal nerve<br />
Ventral ramus of<br />
spinal nerve<br />
Ventral root of spinal nerve<br />
Spinal nerve<br />
Gray and white rami<br />
communicantes<br />
©<br />
FIGURE 2.13<br />
SPINAL MEMBRANES AND NERVE ROOTS •<br />
The spinal cord gives rise to 31 pairs of spinal nerves that distribute<br />
segmentally to the body. Motor fibers of these spinal nerves innervate<br />
skeletal muscle, and sensory fibers convey information back<br />
to the central nervous system from the skin, skeletal muscles, and<br />
joints.<br />
The spinal cord is ensheathed in three meningeal coverings: the<br />
outer, tough dura mater; the arachnoid mater; and the pia mater,<br />
which intimately ensheaths the cord itself. CSF bathes the cord and<br />
is found in the subarachnoid space.<br />
64
Peripheral Nervous System<br />
NEUROPHYSIOLOGY<br />
Posterior horn<br />
Dorsal root ganglion<br />
Sensory neuron cell body<br />
Dorsal root<br />
Anterior horn<br />
Motor neuron cell body<br />
Ventral root<br />
Peripheral nerve<br />
Axon<br />
Myelin sheath<br />
Motor neuron<br />
Sensory neuron<br />
<strong>Neuro</strong>muscular<br />
junction<br />
Skin<br />
Muscle<br />
with<br />
©<br />
FIGURE 2.14<br />
PERIPHERAL NERVOUS SYSTEM •<br />
The peripheral nervous system (PNS) consists of all of the neural<br />
elements outside of the CNS (brain and spinal cord) and provides<br />
the connections between the CNS and all other body organ systems.<br />
The PNS consists of somatic and autonomic components. The<br />
somatic component innervates skeletal muscle and skin and is<br />
shown here (see Figure 2.15 for the autonomic nervous system).<br />
The somatic component of the peripheral nerves contains both<br />
motor and sensory axons. Cell bodies of the motor neurons are<br />
found in the anterior horn gray matter, whereas the cell bodies of<br />
sensory neurons are located in the dorsal root ganglia.<br />
65
NEUROPHYSIOLOGY<br />
Autonomic Nervous System: Schema<br />
Oculomotor nerve (III)<br />
Facial nerve (VII)<br />
Glossopharyngeal nerve (IX)<br />
Medulla oblongata<br />
Vagus nerve (X)<br />
Sweat<br />
gland<br />
Peripheral<br />
blood vessel<br />
C1<br />
Arrector (smooth)<br />
muscle of hair follicle<br />
Note: Above three<br />
structures are shown at<br />
only one level but<br />
occur at all levels<br />
C2<br />
C3<br />
C4<br />
C5<br />
C6<br />
C7<br />
C8<br />
T1<br />
T2<br />
T3<br />
T4<br />
T5<br />
T9<br />
T10<br />
T7<br />
T8<br />
T11<br />
T12<br />
T6<br />
L1<br />
L2<br />
L3<br />
L4<br />
L5<br />
Note: Blue-shaded S1<br />
areas indicate zones of<br />
parasympathetic S2<br />
outflow from CNS S3<br />
S4<br />
S5<br />
Coccygeal<br />
Gray rami<br />
communicantes<br />
Gray and white rami communicantes<br />
Gray rami communicantes<br />
Greater<br />
Lesser<br />
Least<br />
Lumbar<br />
splanchnic<br />
nerves<br />
⎧<br />
⎨<br />
⎩<br />
Splanchnic<br />
nerves<br />
Pelvic<br />
splanchnic<br />
nerves<br />
Intracranial vessels<br />
Ciliary ganglion<br />
Eye<br />
Pterygopalatine ganglion<br />
Lacrimal glands<br />
Otic ganglion<br />
Parotid glands<br />
Submandibular ganglion<br />
Sublingual and<br />
submandibular glands<br />
Peripheral cranial<br />
and facial vessels<br />
Larynx<br />
Trachea<br />
Bronchi<br />
Lungs<br />
Heart<br />
Stomach<br />
Liver<br />
Gallbladder<br />
Bile ducts<br />
Pancreas<br />
Suprarenal glands<br />
Kidneys<br />
Intestines<br />
Descending colon<br />
Sigmoid colon<br />
Rectum<br />
Prostate<br />
External genitalia<br />
Urinary bladder<br />
Pulmonary plexus<br />
Cardiac plexus<br />
Celiac ganglion<br />
Aorticorenal ganglion<br />
Superior mesenteric<br />
ganglion<br />
Inferior mesenteric<br />
ganglion<br />
Superior hypogastric<br />
plexus<br />
Inferior<br />
hypogastric<br />
plexus<br />
Sympathetic<br />
fibers<br />
Presynaptic<br />
Postsynaptic<br />
Parasympathetic<br />
fibers<br />
Presynaptic<br />
Postsynaptic<br />
Antidromic<br />
conduction<br />
©<br />
FIGURE 2.15<br />
AUTONOMIC NERVOUS SYSTEM: SCHEMA •<br />
The autonomic nervous system is composed of two divisions: the<br />
parasympathetic division derived from four of the cranial nerves<br />
(CN III, VII, IX, and X) and the S2-S4 sacral spinal cord levels, and the<br />
sympathetic division associated with the thoracic and upper lumbar<br />
spinal cord levels (T1-L2). The autonomic nervous system is a twoneuron<br />
chain, with the preganglionic neuron arising from the central<br />
nervous system and synapsing on a postganglionic neuron located in<br />
66<br />
a peripheral autonomic ganglion. Postganglionic axons of the autonomic<br />
nervous system innervate smooth muscle, cardiac muscle, and<br />
glands. Basically, the sympathetic division mobilizes our body (“fight<br />
or flight”) while the parasympathetic division regulates digestive and<br />
homeostatic functions. Normally, both divisions work in concert to<br />
regulate visceral activity (respiration, cardiovascular function, digestion,<br />
and associated glandular activity).
Autonomic Nervous System: Cholinergic and Adrenergic Synapses<br />
NEUROPHYSIOLOGY<br />
Medulla<br />
oblongata<br />
Glossopharyngeal<br />
nerve (IX)<br />
Internal carotid nerve<br />
Vagus nerve (X)<br />
Parotid<br />
gland<br />
Larynx<br />
Trachea<br />
Bronchi<br />
Lungs<br />
Heart<br />
Cervical<br />
sympathetic<br />
ganglia<br />
Striated muscle<br />
Sweat glands<br />
Thoracic<br />
part of<br />
spinal cord<br />
Gray ramus<br />
communicans<br />
White ramus<br />
communicans<br />
Celiac<br />
ganglion<br />
Hair follicles<br />
Peripheral arteries<br />
Upper<br />
lumbar<br />
part of<br />
spinal cord<br />
(L1-2 [3])<br />
Superior<br />
mesenteric<br />
ganglion<br />
Suprarenal<br />
gland<br />
Visceral<br />
arteries<br />
Gastrointestinal<br />
tract<br />
Inferior<br />
mesenteric ganglion<br />
Sacral<br />
part of<br />
spinal cord<br />
Pelvic splanchnic nerves<br />
C Cholinergic synapses<br />
A Adrenergic synapses<br />
Urinary bladder<br />
Urethra<br />
Prostate<br />
Sympathetic<br />
fibers<br />
Presynaptic<br />
Postsynaptic<br />
Parasympathetic<br />
fibers<br />
Presynaptic<br />
Postsynaptic<br />
Somatic fibers<br />
Antidromic conduction<br />
©<br />
FIGURE 2.16<br />
CHOLINERGIC AND ADRENERGIC SYNAPSES: SCHEMA •<br />
The autonomic nervous system (ANS) is a two-neuron chain, with<br />
the preganglionic neuron arising from the central nervous system<br />
and synapsing on a postganglionic neuron located in a peripheral<br />
autonomic ganglion. Acetylcholine is the neurotransmitter in both<br />
the sympathetic and parasympathetic ganglia. The parasympathetic<br />
division of the ANS releases acetylcholine at its postganglionic<br />
synapses and is characterized as having cholinergic (C) effects,<br />
whereas the sympathetic division releases predominantly noradrenaline<br />
(norepinephrine) at its postganglionic synapses, causing<br />
adrenergic (A) effects (except on sweat glands, where acetylcholine<br />
is released). Although acetylcholine and noradrenaline are the<br />
chief transmitter substances, other neuroactive peptides often are<br />
colocalized with them and include such substances as gammaaminobutyric<br />
acid (GABA), substance P, enkephalins, histamine,<br />
glutamic acid, neuropeptide Y, and others.<br />
67
NEUROPHYSIOLOGY<br />
Hypothalamus<br />
Lateral<br />
ventricle<br />
Septum<br />
pellucidum<br />
Fornix<br />
Corpus callosum<br />
Medial<br />
forebrain<br />
bundle<br />
Lateral<br />
preoptic<br />
nucleus<br />
Anterior<br />
commissure<br />
Medial<br />
preoptic<br />
nucleus<br />
From<br />
Thalamus<br />
hippocampal<br />
formation<br />
Interthalamic<br />
Lateral<br />
adhesion<br />
hypothalamic area<br />
Paraventricular nucleus<br />
Anterior hypothalamic area<br />
Dorsal hypothalamic area<br />
Dorsomedial nucleus<br />
Mamillothalamic tract<br />
Posterior area<br />
Periventricular<br />
nucleus<br />
Nucleus<br />
intercalatus<br />
Olfactory<br />
tract<br />
Optic (II)<br />
nerve<br />
Optic chiasm<br />
Anterior<br />
lobe of<br />
pituitary<br />
Fornix<br />
Ventromedial<br />
nucleus<br />
Mamillary<br />
complex<br />
Tuberohypophyseal tract<br />
Red nucleus<br />
Oculomotor (III) nerve<br />
Supraoptic nucleus<br />
Supraopticohypophyseal<br />
tract<br />
Posterior lobe of pituitary<br />
Cerebral<br />
peduncle<br />
Dorsal<br />
longitudinal<br />
fasciculus<br />
Descending<br />
hypothalamic<br />
connections<br />
Pons<br />
Reticular<br />
formation<br />
©<br />
CHART 2.3<br />
MAJOR FUNCTIONS OF THE HYPOTHALAMUS<br />
Hypothalamic Area<br />
Preoptic and anterior<br />
Posterior<br />
Lateral<br />
Ventromedial<br />
Supraoptic (subfornical organ and organum vasculosum)<br />
Paraventricular<br />
Periventricular<br />
*Stimulation of the center causes the responses listed.<br />
Major Functions*<br />
Heat loss center: cutaneous vasodilation and sweating<br />
Heat conservation center: cutaneous vasoconstriction and shivering<br />
Feeding center: eating behavior<br />
Satiety center: inhibits eating behavior<br />
ADH and oxytocin secretion (sensation of thirst)<br />
ADH and oxytocin secretion<br />
Releasing hormones for the anterior pituitary<br />
FIGURE 2.17<br />
SCHEMATIC RECONSTRUCTION OF THE HYPOTHALAMUS •<br />
The hypothalamus, part of the diencephalon, controls a number of<br />
important homeostatic systems within the body, including temperature<br />
regulation, food intake, water intake, many of the endocrine<br />
systems (see Chapter 8), motivation, and emotional behavior. It<br />
receives inputs from the reticular formation (sleep/wake cycle<br />
information), the thalamus (pain), the limbic system (emotion, fear,<br />
anger, smell), the medulla oblongata (blood pressure and heart<br />
rate), and the optic system, and it integrates these inputs for regulation<br />
of the functions listed.<br />
68
Limbic System<br />
NEUROPHYSIOLOGY<br />
Genu of corpus callosum<br />
Head of caudate nucleus<br />
Columns of fornix<br />
Body of fornix<br />
Thalamus<br />
Uncus<br />
Crura of fornix<br />
Fimbria of hippocampus<br />
Hippocampus<br />
Commissure of fornix<br />
Splenium of corpus callosum<br />
Lateral ventricle<br />
Columns<br />
of fornix<br />
Body of fornix<br />
Commissure<br />
of fornix<br />
Crura of fornix<br />
Mamillary<br />
bodies<br />
Amygdaloid bodies<br />
Hippocampus<br />
with fimbria ©<br />
FIGURE 2.18<br />
HIPPOCAMPUS AND FORNIX •<br />
The limbic system includes the hypothalamus and a collection of<br />
interconnected structures in the telencephalon (cingulate, parahippocampal,<br />
and subcallosal gyri), as well as the amygdala and hippocampal<br />
formation. The limbic system functions in linking emotion<br />
and motivation (amygdala), learning and memory (hippocampal<br />
formation), and sexual behavior (hypothalamus).<br />
69
NEUROPHYSIOLOGY<br />
The Cerebral Cortex<br />
Premotor; orientation;<br />
eye and head<br />
movements<br />
Motor<br />
Ms I<br />
Ms II<br />
Sm I<br />
Sm II<br />
Sensory<br />
Sensory<br />
analysis<br />
Prefrontal;<br />
inhibitory control<br />
of behavior;<br />
higher<br />
intelligence<br />
Visual III<br />
Visual II<br />
Visual I<br />
Motor control<br />
of speech<br />
Language;<br />
reading; speech<br />
Auditory I<br />
Auditory II<br />
Premotor<br />
Motor<br />
Ms I<br />
Ms II<br />
Sm I<br />
Sm III<br />
?<br />
Sensory<br />
Prefrontal;<br />
inhibitory control<br />
of behavior;<br />
higher<br />
intelligence<br />
Visual III<br />
Visual II<br />
Visual I<br />
Cingulate gyrus<br />
(emotional behavior)<br />
and cingulum<br />
Corpus callosum<br />
Hippocampal commissure<br />
©<br />
Olfactory<br />
Anterior commissure<br />
FIGURE 2.19<br />
CEREBRAL CORTEX: LOCALIZATION OF FUNCTION AND ASSOCIATION PATHWAYS •<br />
The cerebral cortex is organized into functional regions. In addition<br />
to specific areas devoted to sensory and motor functions, there<br />
are areas that integrate information from multiple sources. The<br />
cerebral cortex participates in advanced intellectual functions,<br />
including aspects of memory storage and recall, language, higher<br />
cognitive functions, conscious perception, sensory integration, and<br />
planning/execution of complex motor activity. General cortical<br />
areas associated with these functions are illustrated.<br />
70
Descending Motor Pathways<br />
NEUROPHYSIOLOGY<br />
Motor<br />
cortex<br />
Internal<br />
capsule<br />
Hip<br />
Knee<br />
Ankle<br />
Toes<br />
Trunk<br />
Shoulder<br />
Elbow<br />
Wrist<br />
Fingers<br />
Thumb<br />
Neck<br />
Brow<br />
Eyelid<br />
Nares<br />
Lips<br />
Tongue<br />
Larynx<br />
Lateral aspect of<br />
cerebral cortex to show<br />
topographic projection<br />
of motor centers on<br />
precentral gyrus<br />
Midbrain<br />
Pons<br />
Medulla<br />
Basis<br />
pedunculi<br />
Basis<br />
pontis<br />
Pyramids<br />
Motor system<br />
Fibers originate in motor cortex and<br />
descend via posterior limb of internal<br />
capsule to basis pedunculi of midbrain<br />
Longitudinal bundles branch upon<br />
entering basis pontis and rejoin to<br />
enter pyramids of medulla<br />
At lower medulla, bulk of fibers cross<br />
median plane to form lateral<br />
corticospinal tract; some fibers<br />
continue downward in ipsilateral<br />
lateral corticospinal tract; others<br />
descending ipsilateral anterior<br />
corticospinal tract<br />
Medulla<br />
Above midthoracic<br />
level<br />
Decussation<br />
of pyramids<br />
Synapse occurs at spinal level: Lateral<br />
corticospinal fibers synapse on<br />
ipsilateral anterior horn cells; anterior<br />
corticospinal fibers synapse on<br />
contralateral anterior horn cells<br />
Motor<br />
endplate<br />
Spinal<br />
cord<br />
Below midthoracic<br />
level<br />
Anterior corticospinal tract<br />
Lateral corticospinal tract<br />
Motor<br />
endplate<br />
©<br />
FIGURE 2.20<br />
CORTICOSPINAL TRACTS •<br />
The corticospinal, or pyramidal, tract is the major motor tract that<br />
controls voluntary movement of the skeletal muscles, especially<br />
skilled movements of distal muscles of the limbs. All structures<br />
from the cerebral cortex to the anterior horn cells in the spinal<br />
cord constitute the upper portion of the system (upper motor neuron).<br />
The anterior horn cells and their associated axons constitute<br />
the lower portion of the system (lower motor neuron).<br />
71
NEUROPHYSIOLOGY<br />
Cerebellum: Afferent Pathways<br />
Superior cerebellar peduncle<br />
Middle cerebellar peduncle<br />
Cortical input<br />
Nucleus<br />
reticularis<br />
tegmenti<br />
pontis<br />
Pontine nuclei<br />
(contralateral)<br />
Spinal input<br />
Inferior olive<br />
Leg<br />
Arm Face<br />
To contralateral cerebellar cortex<br />
Primary fissure<br />
Upper part<br />
of medulla<br />
oblongata<br />
Spinal input<br />
Vestibular nerve<br />
and ganglion<br />
Lower part<br />
of medulla<br />
oblongata<br />
Cortical input<br />
Lateral reticular<br />
nucleus<br />
Spinal input<br />
Cervical part<br />
of spinal cord<br />
Motor interneuron<br />
Rostral<br />
spinocerebellar<br />
tract<br />
Spinal border cells<br />
Motor interneuron<br />
Lumbar part<br />
of spinal cord<br />
Clarke’s column<br />
Ventral spinocerebellar<br />
tract<br />
Vestibular<br />
nuclei<br />
To nodule and flocculus<br />
Inferior cerebellar peduncle<br />
Reticulocerebellar<br />
tract<br />
Cuneocerebellar<br />
tract<br />
Gracile nucleus<br />
Main cuneate<br />
nucleus (relay<br />
for cutaneous<br />
information)<br />
External cuneate nucleus<br />
(relay for proprioceptive<br />
information)<br />
From skin (touch<br />
and pressure)<br />
From muscle (spindles<br />
and Golgi tendon organs)<br />
From skin and<br />
deep tissues<br />
(pain and Golgi<br />
tendon organs)<br />
From skin (touch<br />
and pressure)<br />
and from muscle<br />
(spindles and<br />
Golgi tendon<br />
organs)<br />
Dorsal spinocerebellar tract<br />
Leg zone<br />
Arm zone<br />
Face zone<br />
2nd spinal<br />
projection<br />
area (gracile<br />
lobule)<br />
Archicerebellum<br />
(vestibulocerebellum)<br />
Paleocerebellum<br />
(spinocerebellum)<br />
Functional Subdivisions of Cerebellum<br />
Hemisphere Vermis<br />
Intermediate<br />
Lateral<br />
part part<br />
Lingula<br />
Flocculus<br />
Nodule<br />
Neocerebellum<br />
(pontocerebellum)<br />
Uvula<br />
Pyramid<br />
Vermis<br />
Middle vermis<br />
Hemisphere<br />
Anterior lobe<br />
Primary<br />
fissure<br />
Middle<br />
(posterior)<br />
lobe<br />
Posterolateral<br />
fissure<br />
Flocculonodular<br />
lobe<br />
Schema of<br />
theoretical<br />
“unfolding”<br />
of cerebellar<br />
surface in<br />
derivation of<br />
above diagram<br />
FIGURE 2.21<br />
CEREBELLAR AFFERENT PATHWAYS •<br />
©<br />
72<br />
The cerebellum plays an important role in coordinating movement. It<br />
receives sensory information and then influences descending motor<br />
pathways to produce fine, smooth, and coordinated motion. The<br />
cerebellum is divided into three general areas: archicerebellum (also<br />
called vestibulocerebellum) paleocerebellum (also called spinocerebellum)<br />
and the neocerebellum (also called the cerebrocerebellum).<br />
The archicerebellum is primarily involved in controlling posture and<br />
balance, as well as the movement of the head and eyes. It receives<br />
afferent signals from the vestibular apparatus and then sends efferent<br />
fibers to the appropriate descending motor pathways. The paleocerebellum<br />
primarily controls movement of the proximal portions of the<br />
limbs. It receives sensory information on limb position and muscle<br />
tone and then modifies and coordinates these movements through<br />
efferent pathways to the appropriate descending motor pathways. The<br />
neocerebellum is the largest portion of the cerebellum, and it coordinates<br />
the movement of the distal portions of the limbs. It receives<br />
input from the cerebral cortex and thus helps in the planning of<br />
motor activity (e.g., seeing a pencil and then planning and executing<br />
the movement of the arm and hand to pick it up).
Cerebellum: Efferent Pathways<br />
NEUROPHYSIOLOGY<br />
Excitatory<br />
endings<br />
Inhibitory<br />
endings of<br />
Purkinje<br />
cells<br />
Motor and<br />
premotor<br />
cerebral<br />
cortex<br />
Ventral anterior and<br />
ventral lateral nuclei<br />
of thalamus<br />
Mesencephalic reticular formation<br />
Dentate nucleus<br />
Cerebellar<br />
cortex<br />
Globose nuclei<br />
Emboliform nucleus<br />
Red nucleus<br />
Fastigial nucleus<br />
Internal capsule<br />
Cerebral peduncle<br />
Decussation of superior<br />
cerebellar peduncles<br />
Descending fibers from<br />
superior cerebellar<br />
peduncles<br />
Hook bundle of Russell<br />
Section<br />
A–B<br />
viewed<br />
from<br />
below<br />
Vestibular<br />
nuclei<br />
Section<br />
B–C<br />
viewed<br />
from<br />
above<br />
Inferior cerebellar<br />
peduncle<br />
Inferior olive<br />
Lateral reticular nucleus<br />
Medulla oblongata<br />
Pontomedullary reticular formation<br />
A<br />
Planes of<br />
section:<br />
red arrows<br />
indicate<br />
C<br />
direction<br />
of view<br />
B<br />
©<br />
FIGURE 2.22<br />
CEREBELLAR EFFERENT PATHWAYS •<br />
The cerebellum plays an important role in coordinating movement.<br />
It influences descending motor pathways to produce fine, smooth,<br />
and coordinated motion. The archicerebellum is primarily involved<br />
in controlling posture and balance and movement of the head and<br />
eyes. It sends efferent fibers to the appropriate descending motor<br />
pathways. The paleocerebellum primarily controls movement of<br />
the proximal portions of the limbs. It modifies and coordinates<br />
these movements through efferent pathways to the appropriate<br />
descending motor pathways. The neocerebellum coordinates the<br />
movement of the distal portions of the limbs. It helps in the planning<br />
of motor activity (e.g., seeing a pencil and then planning and<br />
executing the movement of the arm and hand to pick it up).<br />
73
NEUROPHYSIOLOGY<br />
Cutaneous Sensory Receptors<br />
Basal<br />
epithelial<br />
cells<br />
Hair follicle<br />
Free nerve endings<br />
Hair shaft<br />
Melanocyte<br />
Arrector muscle of hair<br />
Sebaceous gland<br />
Cuticle<br />
Internal sheath<br />
External sheath<br />
Glassy<br />
membrane<br />
Connective<br />
tissue layer<br />
Hair cuticle<br />
Sweat gland<br />
Hair matrix<br />
Papilla of hair follicle<br />
Pacinian<br />
corpuscle<br />
Artery<br />
Detail of Merkel’s disc<br />
Meissner’s corpuscle<br />
Pore of sweat gland<br />
Vein<br />
Sensory nerves<br />
Elastic fibers<br />
Skin ligaments<br />
(retinacula cutis)<br />
Motor<br />
(autonomic)<br />
nerve<br />
Desmosomes<br />
Cutaneous<br />
nerve<br />
Stratum corneum<br />
Stratum<br />
lucidum<br />
Stratum<br />
spinosum<br />
Dermal<br />
papilla<br />
(of papillary<br />
layer)<br />
Reticular<br />
layer<br />
Stratum<br />
granulosum<br />
Subcutaneous<br />
artery and vein<br />
Cross section<br />
Stratum<br />
basale<br />
Epidermis Dermis Subcutaneous tissue<br />
Basement membrane<br />
Axon terminal<br />
Mitochondrion<br />
Schwann cell<br />
Cytoplasmic<br />
protrusion<br />
Merkel<br />
cell<br />
Mitochondria<br />
Lobulated<br />
nucleus<br />
Expanded<br />
axon terminal<br />
Granulated<br />
vesicles<br />
Axon<br />
©<br />
Schwann<br />
cell<br />
Schwann cells<br />
Detail of free nerve ending<br />
FIGURE 2.23<br />
SKIN AND CUTANEOUS RECEPTORS •<br />
Cutaneous receptors respond to touch (mechanoreceptors), pain<br />
(nociceptors), and temperature (thermoreceptors). Several different<br />
types of receptors are present in skin. Meissner’s corpuscles have<br />
small receptive fields and respond best to stimuli that are applied<br />
at low frequency (i.e., flutter). The pacinian corpuscles are located<br />
in the subcutaneous tissue and have large receptive fields. They<br />
respond best to high-frequency stimulation (i.e., vibration).<br />
Merkel’s discs have small receptive fields and respond to touch and<br />
pressure (i.e., indenting the skin). Ruffini’s corpuscles have large<br />
receptive fields, and they also respond to touch and pressure. Free<br />
nerve endings respond to pain and temperature.<br />
74
Cutaneous Receptors: Pacinian Corpuscle<br />
NEUROPHYSIOLOGY<br />
Pacinian Corpuscle<br />
as Pressure Transducer<br />
To amplifier<br />
Pressure<br />
Generator potential<br />
Action potential<br />
A. Sharp “on and off” changes in pressure at start and end<br />
1st node<br />
Pressure Na + of pulse applied to lamellated capsule are transmitted to<br />
Myelin sheath central axon and provoke generator potentials, which in<br />
Lamellated capsule<br />
turn may trigger action potentials; there is no response to a<br />
slow change in pressure gradient. Pressure at central core<br />
Central core<br />
Unmyelinated axon terminal<br />
and, accordingly, generator potentials are rapidly dissipated<br />
by viscoelastic properties of capsule (Action potentials may<br />
be blocked by pressure at a node or by drugs)<br />
Pressure<br />
To amplifier<br />
Generator potential<br />
B. In absence of capsule, axon responds to slow as well<br />
as to rapid changes in pressure. Generator potential<br />
dissipates slowly, and there is no “off” response<br />
Action potential<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
Pressure applied to axon terminal directly or<br />
via capsule causes increased permeability of<br />
membrane to Na + , thus setting up ionic<br />
generator current through 1st node<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
<br />
If resultant depolarization at 1st node is great<br />
enough to reach threshold, an action potential<br />
appears which is propagated along nerve fiber<br />
©<br />
FIGURE 2.24<br />
PACINIAN CORPUSCLE •<br />
Pacinian corpuscles are mechanoreceptors that transduce mechanical<br />
forces (displacement, pressure, vibration) into action potentials<br />
that are conveyed centrally by afferent nerve fibers. As the viscoelastic<br />
lamellae are displaced, the unmyelinated axon terminal<br />
membrane’s ionic permeability is increased until it is capable of<br />
producing a “generator potential.” As demonstrated in the figure,<br />
pacinian corpuscles respond to the beginning and end of a<br />
mechanical force while the concentric lamellae dissipate slow<br />
changes in pressure. In the absence of the capsule, the generator<br />
potential decays slowly and yields only a single action potential.<br />
75
NEUROPHYSIOLOGY<br />
Proprioception and Reflex Pathways: I<br />
Spinal Effector Mechanisms<br />
Dorsal horn<br />
interneuron<br />
From motor neuron<br />
Proprioceptive fibers<br />
Dorsal horn interneuron<br />
From<br />
cutaneous<br />
receptor<br />
From<br />
muscle<br />
spindle<br />
Flexor reflex interneuron<br />
Dorsal horn interneuron<br />
Dorsal root<br />
ganglion<br />
Ventral root<br />
To motor neuron<br />
motor axon<br />
To motor neuron<br />
Schematic representation of motor neurons<br />
In cervical<br />
enlargement of<br />
spinal cord<br />
Flex ors<br />
Extensors<br />
In lumbar<br />
enlargement<br />
of spinal cord<br />
Fle<br />
xors<br />
Exte nsors<br />
©<br />
FIGURE 2.25<br />
PROPRIOCEPTION: SPINAL EFFECTOR MECHANISM •<br />
Position sense or proprioception involves input from cutaneous<br />
mechanoreceptors, Golgi tendon organs, and muscle spindles<br />
(middle figure of upper panel). Both monosynaptic reflex pathways<br />
(middle figure of upper panel) and polysynaptic pathways involving<br />
several spinal cord segments (top and bottom figures of upper<br />
panel) initiate muscle contraction reflexes. The lower panel shows<br />
the somatotopic distribution of the motor neuron cell bodies in the<br />
ventral horn of the spinal cord that innervate limb muscles (flexor<br />
and extensor muscles of upper and lower limbs).<br />
76
Proprioception and Reflex Pathways: II<br />
NEUROPHYSIOLOGY<br />
Alpha motor neurons to extrafusal<br />
striated muscle end plates<br />
Gamma motor neurons to intrafusal<br />
striated muscle end plates<br />
Ia (A) fibers from annulospiral<br />
endings (proprioception)<br />
II (A) fibers from flower spray<br />
endings (proprioception);<br />
from paciniform corpuscles (pressure)<br />
and pacinian corpuscles (pressure)<br />
III (A) fibers from free nerve endings<br />
and from some specialized endings<br />
(pain and some pressure)<br />
IV (unmyelinated) fibers from free<br />
nerve endings (pain)<br />
Ib (A) fibers from Golgi tendon<br />
organs (proprioception)<br />
Alpha motor neuron to extrafusal<br />
muscle fiber end plates<br />
A fibers from<br />
Golgi-type<br />
endings<br />
A fibers from<br />
paciniform corpuscles<br />
and Ruffini terminals<br />
A and C fibers<br />
from free nerve<br />
endings<br />
Gamma motor neuron to intrafusal<br />
muscle fiber and plates<br />
II (A) fiber from flower spray endings<br />
Ia (A) fiber from annulospiral endings<br />
Detail of<br />
muscle spindle<br />
Sheath<br />
Lymph space<br />
Nuclear bag fiber<br />
Nuclear chain fiber<br />
Extrafusal<br />
muscle fiber<br />
Intrafusal<br />
muscle fibers<br />
©<br />
Efferent fibers<br />
Afferent fibers<br />
FIGURE 2.26<br />
MUSCLE AND JOINT RECEPTORS •<br />
Muscle spindles and Golgi tendon organs send afferent signals to<br />
the brain to convey the position of limbs and help coordinate muscle<br />
movement. Muscle spindles convey information on muscle tension<br />
and contraction (dynamic forces) and muscle length (static<br />
forces). The nuclear bag fibers respond to both dynamic and static<br />
forces, whereas the nuclear chain fibers respond to static forces.<br />
Intrafusal fibers maintain appropriate tension on the nuclear bag<br />
and nuclear chain fibers. If the muscle tension is too great (e.g.,<br />
overstretching of muscle or too heavy a load), activation of the<br />
Golgi tendon organ causes a reflex relaxation of the muscle.<br />
77
NEUROPHYSIOLOGY<br />
Proprioception and Reflex Pathways: III<br />
Ib fibers<br />
Ia fibers <br />
Extrafusal muscle fiber<br />
Intrafusal muscle fiber<br />
Alpha motor neurons <br />
Gamma motor neurons<br />
Golgi<br />
tendon<br />
organ<br />
A. Passive stretch. Both intrafusal and extrafusal muscle fibers stretched;<br />
spindles activated. Reflex via Ia fibers and alpha motor neurons causes<br />
secondary contraction (basis of stretch reflexes, such as knee jerk).<br />
Stretch is too weak to activate Golgi tendon organs<br />
Ib fibers <br />
Ia fibers<br />
Alpha activation<br />
from brain<br />
Extrafusal muscle fiber<br />
Intrafusal muscle fiber<br />
Inhibitory interneuron<br />
Alpha motor neurons <br />
Gamma motor neurons<br />
Golgi<br />
tendon<br />
organ<br />
B. Active contraction. Central excitation of alpha motor neurons<br />
only causes contraction of extrafusal muscle fibers with consequent<br />
relaxation of intrafusal fibers; spindles not activated. Tension is low;<br />
does not adjust to increased resistance. Tendon organ activated,<br />
causing relaxation<br />
Alpha and<br />
Ib fibers <br />
gamma<br />
activation<br />
from brain<br />
Ia fibers <br />
Extrafusal muscle fiber<br />
Intrafusal muscle fiber<br />
Alpha motor neurons <br />
Gamma motor neurons <br />
Golgi<br />
tendon<br />
organ<br />
C. Active contraction with gamma coactivation. Intrafusal as well as<br />
extrafusal fibers contract; spindles activated, reinforcing contraction<br />
stimulus via Ia fibers in accord with resistance. Tendon organ<br />
activated, causing relaxation if load is too great<br />
©<br />
FIGURE 2.27<br />
PROPRIOCEPTIVE REFLEX CONTROL OF MUSCLE TENSION •<br />
Interaction of the muscle spindle and Golgi tendon organ during passive stretch of a muscle (panel A) and during a contraction (panels B<br />
and C).<br />
78
Proprioception and Reflex Pathways: IV<br />
NEUROPHYSIOLOGY<br />
A. Afferent inhibition<br />
From extensor spindle<br />
receptor (Ia, II fibers)<br />
From flexor spindle<br />
(Ia, II fibers)<br />
Axoaxonic presynaptic<br />
inhibitory synapse<br />
To extensors<br />
B. Stretch reflex<br />
(reciprocal inhibition)<br />
From extensor spindle<br />
receptor (Ia, II fibers)<br />
Axosomatic or<br />
axodendritic<br />
inhibitory<br />
synapse<br />
Excitatory<br />
synapse<br />
To extensors<br />
To flexors<br />
C. Recurrent inhibition<br />
D. Tendon organ reflex<br />
From extensor tendon<br />
organ (Ib fibers)<br />
Inhibitory synapse<br />
Renshaw cells<br />
Collaterals<br />
To synergistic<br />
muscles<br />
Excitatory synapse<br />
To extensors<br />
To flexors<br />
E. Flexor withdrawal reflex<br />
Nociceptive fibers<br />
Ipsilateral<br />
flexion<br />
Contralateral<br />
extension<br />
Inhibitory synapse<br />
Excitatory synapse<br />
To extensors<br />
To flexors<br />
Excitatory synapse<br />
Inhibitory synapse<br />
To extensors<br />
To flexors<br />
©<br />
FIGURE 2.28<br />
SPINAL REFLEX PATHWAYS •<br />
Summary of the spinal reflex pathways.<br />
79
NEUROPHYSIOLOGY<br />
Sensory Pathways: I<br />
Cerebral cortex:<br />
postcentral gyrus<br />
Posterior limb of<br />
internal capsule<br />
Ventral posterolateral<br />
(VPL) nucleus of<br />
thalamus<br />
Mesencephalon<br />
(cerebral peduncles)<br />
Medial lemniscus<br />
Spinothalamic tract<br />
Gracile nucleus<br />
Cuneate nucleus<br />
Lower part of<br />
medulla oblongata<br />
Reticular formation<br />
Cervical part<br />
of spinal cord<br />
Lateral<br />
spinothalamic tract:<br />
pain, temperature<br />
Ventral (anterior)<br />
spinothalamic tract:<br />
touch, pressure<br />
Fasciculus gracilis<br />
Fasciculus cuneatus<br />
Dorsal (posterior) spinal<br />
root ganglion<br />
Proprioception,<br />
position<br />
Touch,<br />
pressure,<br />
vibration<br />
Pain,<br />
temperature<br />
Lateral cervical nucleus<br />
Spinocervical tract<br />
Large<br />
myelinated<br />
fibers<br />
Small<br />
myelinated<br />
and unmyelinated<br />
fibers<br />
Lumbar part<br />
of spinal cord<br />
©<br />
FIGURE 2.29<br />
SOMESTHETIC SYSTEM OF THE BODY •<br />
Pain, temperature, and pressure sensations below the head ultimately<br />
are conveyed to the primary somatosensory cortex (postcentral<br />
gyrus) by the anterolateral system (spinothalamic and spinoreticular<br />
tracts). The fasciculus gracilis and cuneatus of the spinal<br />
lemniscal system convey proprioceptive, vibratory, and tactile sensations<br />
to the thalamus (ventral posterolateral nucleus), whereas<br />
the lateral cervical system mediates some touch, vibratory, and<br />
proprioceptive sensations (blue and purple lines show these dual<br />
pathways). Ultimately, these fibers ascend as parallel pathways to<br />
the thalamus, synapse, and ascend to the cortex.<br />
80
Sensory Pathways: II<br />
NEUROPHYSIOLOGY<br />
Cerebral cortex:<br />
postcentral gyrus<br />
Ventral posteromedial (VPM)<br />
nucleus of thalamus<br />
Internal capsule<br />
Midbrain<br />
(cerebral<br />
peduncles)<br />
Ventral<br />
trigeminal<br />
lemniscus<br />
Pontine<br />
reticular<br />
formation<br />
Pons<br />
Dorsal trigeminal lemniscus<br />
Trigeminal mesencephalic nucleus<br />
Trigeminal motor nucleus<br />
Principal sensory trigeminal nucleus<br />
Touch, pressure<br />
Pain, temperature<br />
Proprioception<br />
Trigeminal (semilunar) ganglion<br />
Ophthalmic n.<br />
Maxillary n.<br />
Sensory root<br />
and<br />
Motor root of mandibular n.<br />
Medullary<br />
reticular<br />
formation<br />
Spinal<br />
trigeminal<br />
tract<br />
Spinal<br />
trigeminal<br />
nucleus<br />
Cervical<br />
part of<br />
spinal<br />
cord<br />
Facial (VII) n.<br />
Vagus (X) n.<br />
Dorsolateral fasciculus (of Lissauer)<br />
Substantia gelatinosa (Iamina II)<br />
©<br />
FIGURE 2.30<br />
SOMESTHETIC SYSTEM OF THE HEAD •<br />
Nerve cells bodies for touch, pressure, pain, and temperature in<br />
the head are in the trigeminal (semilunar) ganglion of the trigeminal<br />
(CN V) nerve (blue and red lines in figure). <strong>Neuro</strong>nal cell bodies<br />
mediating proprioception reside in the mesencephalic nucleus<br />
of CN V (purple fibers). Most relay neurons project to the contralateral<br />
VPM nucleus of the thalamus and thence to the postcentral<br />
gyrus of the cerebral cortex, where they are somatotopically<br />
represented.<br />
81
NEUROPHYSIOLOGY<br />
Sensory Pathways: III<br />
C2<br />
C3<br />
C4<br />
C5<br />
T1<br />
T2<br />
T3<br />
T4<br />
T5<br />
T6<br />
T7<br />
T8<br />
T9<br />
T10<br />
T11<br />
T12<br />
L1<br />
S2, 3<br />
L2<br />
L3<br />
L4<br />
T1<br />
C8<br />
C6<br />
Schematic demarcation of<br />
dermatomes shown as distinct<br />
segments. There is actually<br />
considerable overlap between<br />
any two adjacent dermatomes<br />
C5<br />
C7<br />
C6<br />
C7<br />
C6<br />
C7<br />
C8<br />
S3<br />
S4<br />
S5<br />
C7 C8<br />
C8<br />
L5<br />
L1<br />
L2<br />
L3<br />
C2<br />
C3<br />
C4<br />
C5<br />
C6<br />
T1<br />
T2<br />
T3<br />
T4<br />
T5<br />
T6<br />
T7<br />
T8<br />
T9<br />
T10<br />
T11<br />
T12<br />
L1<br />
L2<br />
L3<br />
L4<br />
L5<br />
S1<br />
S2<br />
S1<br />
S2<br />
L5<br />
S1 S2<br />
L5<br />
S1<br />
L4<br />
L4<br />
S1<br />
L5<br />
L4<br />
Levels of principal dermatomes<br />
C5 Clavicles<br />
C5, 6, 7 Lateral parts of upper limbs<br />
C8, T1 Medial sides of upper limbs<br />
C6 Thumb<br />
C6, 7, 8 Hand<br />
C8 Ring and little fingers<br />
T4 Level of nipples<br />
T10 Level of umbilicus<br />
T12 Inguinal or groin regions<br />
L1, 2, 3, 4 Anterior and inner surfaces of lower limbs<br />
L4, 5, S1 Foot<br />
L4 Medial side of great toe<br />
S1, 2, L5 Posterior and outer surfaces of lower limbs<br />
S1 Lateral margin of foot and little toe<br />
S2, 3, 4 Perineum<br />
©<br />
FIGURE 2.31<br />
DERMATOMES •<br />
Sensory information below the head is localized to specific areas<br />
of the body, which reflect the distribution of peripheral sensory<br />
fibers that convey sensations to the spinal cord through the dorsal<br />
roots (sensory nerve cell bodies reside in the corresponding dorsal<br />
root ganglion). The area of skin subserved by afferent fibers of one<br />
dorsal root is called a dermatome. This figure shows the dermatome<br />
segments and lists key dermatome levels used by clinicians.<br />
Variability and overlap occur, so all dermatome segments<br />
are only approximations.<br />
82
Visual System: Receptors<br />
NEUROPHYSIOLOGY<br />
A. Eyeball<br />
Suspensory<br />
ligament<br />
Iris Lens<br />
Cornea<br />
Ciliary<br />
body<br />
B. Section<br />
through retina<br />
Inner limiting<br />
membrane<br />
Axons at surface<br />
of retina passing<br />
via optic nerve,<br />
chiasm, and tract<br />
to lateral<br />
geniculate body<br />
Ora<br />
serrata<br />
Anterior<br />
chamber<br />
Posterior<br />
chamber<br />
containing<br />
aqueous humor<br />
Vitreous humor<br />
Retina<br />
Choroid<br />
Sclera<br />
Fovea<br />
Optic nerve<br />
Ganglion cell<br />
Müller cell<br />
(supporting glial<br />
cell)<br />
Amacrine cell<br />
Bipolar cell<br />
Horizontal cell<br />
Rod<br />
Cone<br />
Pigment cells<br />
of choroid<br />
Synaptic<br />
ending<br />
depolarized<br />
C. Rod in dark D. Rod in light<br />
Synaptic<br />
ending<br />
fully<br />
polarized<br />
Synaptic bar<br />
Photons<br />
of light<br />
Nucleus<br />
Rhodopsin<br />
Lumirhodopsin<br />
Current<br />
flow<br />
Na +<br />
permeability<br />
increased<br />
Retinene<br />
+<br />
Opsin<br />
Vitamin A<br />
Metabolic<br />
energy<br />
Circulation<br />
Metarhodopsin<br />
Retinene<br />
+<br />
Opsin<br />
Vitamin A<br />
Centriole<br />
(basal body)<br />
Na +<br />
permeability<br />
decreased<br />
©<br />
FIGURE 2.32<br />
VISUAL RECEPTORS •<br />
The rods and cones of the retina transduce light into electrical signals.<br />
As illustrated for the rod, light is absorbed by rhodopsin, and<br />
through the second messenger cGMP (not shown), Na channels<br />
in the membrane close and the cell hyperpolarizes. Thus, in the<br />
dark the cell is depolarized, but it is hyperpolarized in the light.<br />
This electrical response to light is distinct from other receptor<br />
responses, in which the response to a stimulus results in a depolarization<br />
of the receptor cell membrane.<br />
83
NEUROPHYSIOLOGY<br />
Visual System: Visual Pathway<br />
G<br />
A<br />
B<br />
H<br />
G<br />
B<br />
A<br />
H<br />
Overlapping<br />
visual fields<br />
Central<br />
darker<br />
circle<br />
represents<br />
macular<br />
zone<br />
Lightest<br />
shades<br />
represent<br />
monocular<br />
fields<br />
Each<br />
quadrant<br />
a different<br />
color<br />
R R C<br />
C<br />
Projection on<br />
left retina<br />
Projection on<br />
right retina<br />
P<br />
P<br />
Choroid Choroid<br />
Periphery Macula<br />
Structure of retina (schematic):<br />
A Amacrine cells<br />
B Bipolar cells<br />
C Cones<br />
G Ganglion cells<br />
H Horizontal cells<br />
P Pigment cells<br />
R Rods<br />
Projection on left<br />
dorsal lateral<br />
geniculate nucleus<br />
Optic<br />
(II) nerves<br />
Optic chiasm<br />
Optic tracts<br />
Lateral<br />
geniculate<br />
bodies<br />
Projection on right<br />
dorsal lateral<br />
geniculate nucleus<br />
Calcarine<br />
fissure<br />
Projection<br />
on left<br />
occipital lobe<br />
Projection<br />
on right<br />
occipital lobe<br />
©<br />
FIGURE 2.33<br />
RETINOGENICULOSTRIATE VISUAL PATHWAY •<br />
The retina has two types of photoreceptors: cones that mediate<br />
color vision and rods that mediate light perception but with low<br />
acuity. The greatest acuity is found in the region of the macula of<br />
the retina, where only cones are found (upper left panel). Visual<br />
signals are conveyed by the ganglion cells whose axons course in<br />
the optic nerves. Visual signals from the nasal retina cross in the<br />
optic chiasm while information from the temporal retina remains in<br />
the ipsilateral optic tract. Fibers synapse in the lateral geniculate<br />
nucleus (visual field is topographically represented here and<br />
inverted), and signals are conveyed to the visual cortex on the<br />
medial surface of the occipital lobe.<br />
84
Auditory System: Cochlea<br />
NEUROPHYSIOLOGY<br />
A. Membranous<br />
labyrinth within<br />
bony labyrinth<br />
(path of sound<br />
waves)<br />
Cochlear nerve<br />
Utricle<br />
Saccule<br />
Semicircular<br />
canals<br />
Scala vestibuli<br />
Cochlear duct<br />
(scala media)<br />
Scala tympani<br />
B. Section<br />
through turn<br />
of cochlea<br />
Efferent<br />
nerve fibers<br />
Afferent<br />
nerve fibers<br />
Spiral ganglion<br />
Round window<br />
Scala vestibuli<br />
(perilymph);<br />
weakly<br />
positive +80 mV<br />
Scala tympani<br />
(perilymph); 0 mV<br />
Oval window and stapes<br />
Vestibular (Reissner’s)<br />
membrane<br />
Cochlear duct (scala media;<br />
endolymph)<br />
Tectorial membrane<br />
Spiral ligament<br />
Bone<br />
Outer hair cells; 60 mV<br />
Basilar membrane<br />
Inner hair cell; 60 mV<br />
C. Spiral organ<br />
of Corti<br />
Hair cells<br />
Inner Outer<br />
Tectorial membrane<br />
Stereocilia<br />
Rods<br />
and<br />
tunnel<br />
of Corti<br />
Basilar membrane<br />
Supporting cells<br />
Spiral lamina Afferent nerve fibers<br />
Spiral ganglion<br />
Efferent nerve fibers<br />
As basilar membrane moves up, hairs are deflected outward, causing<br />
depolarization of hair cells and increased firing of afferent nerve fibers<br />
©<br />
FIGURE 2.34<br />
COCHLEAR RECEPTORS •<br />
The cochlea transduces sound into electrical signals. This is<br />
accomplished by the hair cells, which depolarize in response to<br />
vibration of the basilar membrane. The basilar membrane moves in<br />
response to pressure changes imparted on the oval window of the<br />
cochlea in response to vibrations of the tympanic membrane.<br />
85
NEUROPHYSIOLOGY<br />
Auditory System: Pathways<br />
Acoustic area of<br />
temporal lobe cortex<br />
Medial geniculate body<br />
Brachium of<br />
inferior<br />
colliculus<br />
Inferior<br />
colliculus<br />
Midbrain<br />
Lateral<br />
lemnisci<br />
Medulla<br />
oblongata<br />
Nuclei of<br />
lateral<br />
lemnisci<br />
Correspondence<br />
between cochlea<br />
and acoustic area<br />
of cortex:<br />
Low tones<br />
Middle tones<br />
High tones<br />
Dorsal cochlear nucleus<br />
Inferior cerebellar peduncle<br />
Ventral cochlear nucleus<br />
Cochlear division of<br />
vestibulocochlear nerve<br />
Dorsal<br />
acoustic stria<br />
Reticular formation<br />
Trapezoid body<br />
Intermediate acoustic stria<br />
Superior olivary complex<br />
Inner Outer<br />
Spiral ganglion<br />
Hair cells<br />
©<br />
FIGURE 2.35<br />
AUDITORY PATHWAYS •<br />
The cochlea transduces sound into electrical signals. Axons convey<br />
these signals to the dorsal and ventral cochlear nuclei, where it is<br />
tonotopically organized. Following a series of integrated relay<br />
pathways, the ascending pathway projects to the thalamus (medial<br />
geniculate bodies) and then the acoustic cortex in the transverse<br />
gyrus of the temporal lobe, where information is tonotopically represented<br />
(low, middle, and high tones).<br />
86
Vestibular System: Receptors<br />
NEUROPHYSIOLOGY<br />
Vestibular ganglion<br />
Vestibular<br />
and cochlear<br />
divisions of<br />
vestibulocochlear n.<br />
Maculae<br />
Saccule<br />
Utricle<br />
Cochlear duct<br />
(scala media)<br />
A. Membranous labyrinth<br />
Superior semicircular<br />
canal<br />
Cristae within<br />
ampullae<br />
Horizontal semicircular<br />
canal<br />
Posterior semicircular<br />
canal<br />
B. Section of crista<br />
Opposite wall<br />
of ampulla<br />
Gelatinous cupula<br />
Hair tufts<br />
Hair cells<br />
Nerve fibers<br />
Basement<br />
membrane<br />
C. Section of macula<br />
Otoconia<br />
Gelatinous otolithic<br />
membrane<br />
Hair tuft<br />
Hair cells<br />
Supporting cells<br />
Basement membrane<br />
Nerve fibers<br />
D. Structure and innervation<br />
of hair cells<br />
Hair cell (type I)<br />
Supporting cells<br />
Afferent nerve<br />
calyx<br />
Efferent nerve<br />
ending<br />
Basement<br />
membrane<br />
Kinocilium<br />
Stereocilia<br />
Cuticle<br />
Excitation<br />
Inhibition<br />
Basal body<br />
Cuticle<br />
Kinocilium<br />
Stereocilia<br />
Basal body<br />
Hair cell (type II)<br />
Supporting cell<br />
Efferent nerve<br />
endings<br />
Afferent nerve<br />
endings<br />
Myelin sheath<br />
Myelin sheath<br />
©<br />
FIGURE 2.36<br />
VESTIBULAR RECEPTORS •<br />
The vestibular apparatus detects movement of the head in the form<br />
of linear and angular acceleration. This information is important for<br />
the control of eye movements so that the retina can be provided<br />
with a stable visual image. It is also important for the control of<br />
posture. The utricle and saccule respond to linear acceleration,<br />
such as the pull of gravity. The three semicircular canals are<br />
aligned so that the angular movement of the head can be sensed in<br />
all planes. The sensory hair cells are located in the maculae of the<br />
utricle and saccule and in the cristae within each ampullae.<br />
87
NEUROPHYSIOLOGY<br />
Vestibular System: Vestibulospinal Tracts<br />
Excitatory<br />
endings<br />
Inhibitory<br />
endings<br />
Ascending fibers in medial<br />
longitudinal fasciculi<br />
Superior<br />
Medial<br />
Lateral<br />
Inferior<br />
Vestibular nuclei<br />
Upper<br />
limb<br />
Rostral<br />
Trunk<br />
Ventral<br />
Dorsal<br />
To<br />
cerebellum<br />
Caudal<br />
Lower<br />
limb<br />
Somatotopical<br />
pattern in lateral<br />
vestibular nucleus<br />
Motor neuron<br />
(controlling<br />
neck muscles)<br />
Vestibular<br />
ganglion<br />
and<br />
nerve<br />
Medial vestibulospinal<br />
fibers in medial<br />
longitudinal fasciculi<br />
Lateral<br />
vestibulospinal<br />
tract<br />
Fibers from cristae<br />
(rotational stimuli)<br />
Excitatory<br />
endings<br />
to back<br />
muscles<br />
? ?<br />
Excitatory<br />
interneuron<br />
Inhibitory<br />
interneuron<br />
Fibers from maculae<br />
(gravitational stimuli)<br />
Lower<br />
part of<br />
cervical<br />
spinal cord<br />
To axial<br />
muscles<br />
Lumbar part of<br />
spinal cord<br />
?<br />
Inhibitory<br />
ending<br />
To flexor muscles<br />
To extensor muscles<br />
Inhibitory ending<br />
?<br />
To axial muscles<br />
Excitatory ending<br />
Lateral vestibulospinal tract<br />
Inhibitory interneuron<br />
Excitatory synapse<br />
To flexor muscles<br />
To extensor muscles<br />
©<br />
FIGURE 2.37<br />
VESTIBULOSPINAL TRACTS •<br />
Sensory input from the vestibular apparatus is used to maintain stability<br />
of the head and to maintain balance and posture. Axons convey<br />
vestibular information to the vestibular nuclei in the pons, and<br />
then secondary axons distribute this information to five sites: spinal<br />
cord (muscle control), cerebellum (vermis), reticular formation<br />
(vomiting center), extraocular muscles, and cortex (conscious perception).<br />
This figure shows only the spinal cord pathways.<br />
88
Gustatory (Taste) System: Receptors<br />
NEUROPHYSIOLOGY<br />
A. Tongue<br />
Foliate<br />
papillae<br />
B. Section<br />
through<br />
vallate<br />
papilla<br />
Taste buds<br />
Duct of<br />
gustatory<br />
(Ebner’s)<br />
gland<br />
Fungiform<br />
papillae<br />
Vallate papillae<br />
Microvilli<br />
Taste pore<br />
Taste cells<br />
C. Taste bud<br />
Epithelium<br />
Basement membrane<br />
Nerve plexus<br />
Nerve fibers<br />
emerging from<br />
taste buds<br />
Desmosomes<br />
Epithelium<br />
Large nerve fiber<br />
Granules<br />
Basement membrane<br />
Small nerve fiber<br />
Fibroblast<br />
Schwann cell<br />
Microvilli<br />
Intercellular space Large nerve fiber<br />
Collagen<br />
D. Detail of taste pore E. Detail of base of receptor cells<br />
©<br />
FIGURE 2.38<br />
TASTE RECEPTORS •<br />
Taste buds on the tongue respond to various chemical stimuli. Taste<br />
cells, like neurons, normally have a net negative charge internally<br />
and are depolarized by stimuli, thus releasing transmitters that depolarize<br />
neurons connected to the taste cells. A single taste bud can<br />
respond to more than one stimulus. The four traditional taste qualities<br />
that are sensed are sweet, salty, sour, and bitter.<br />
89
NEUROPHYSIOLOGY<br />
Gustatory (Taste) System: Pathways<br />
Ventral posteromedial (VPM)<br />
nucleus of thalamus<br />
Sensory cortex (just below<br />
face area)<br />
Lateral hypothalamic area<br />
Amygdala<br />
Mesencephalic<br />
nucleus<br />
and<br />
Motor nucleus<br />
of trigeminal n.<br />
Pontine taste area<br />
Trigeminal (V) n.<br />
Maxillary n.<br />
Mandibular n.<br />
Pons<br />
Greater petrosal n.<br />
Geniculate ganglion<br />
Pterygopalatine<br />
ganglion<br />
Facial (VII) n.<br />
and<br />
Nervus inermedius<br />
Rostral part of nucleus<br />
of solitary tract<br />
Glossopharyngeal (IX) n.<br />
Lower<br />
part of<br />
medulla<br />
oblongata<br />
Otic<br />
ganglion<br />
Chorda<br />
tympani<br />
Fungiform papillae<br />
Foliate papillae<br />
Valiate papillae<br />
Lingual n.<br />
Petrosal (inferior)<br />
ganglion of<br />
glossopharyngeal n.<br />
Epiglottis<br />
Larynx<br />
Nodose (inferior)<br />
ganglion of vagus n.<br />
Vagus (X) n.<br />
Superior laryngeal n.<br />
©<br />
FIGURE 2.39<br />
TASTE PATHWAYS •<br />
Depicted here are the afferent pathways leading from the taste receptors to the brainstem and, ultimately, to the sensory cortex in the<br />
postcentral gyrus.<br />
90
Olfactory System: Receptors<br />
NEUROPHYSIOLOGY<br />
Olfactory<br />
bulb<br />
A. Distribution<br />
of olfactory<br />
epithelium<br />
(blue area)<br />
Cribriform plate<br />
of ethmoid bone<br />
Lateral nasal wall<br />
Septum<br />
B. Schema of<br />
section through<br />
olfactory mucosa<br />
Cribriform plate<br />
Schwann cell<br />
Olfactory gland<br />
Unmyelinated<br />
olfactory axons<br />
Basement<br />
membrane<br />
Sustentacular<br />
cells<br />
Endoplasmic<br />
reticulum<br />
Nucleus<br />
Olfactory cells<br />
Dendrites<br />
Terminal bars<br />
(desmosomes)<br />
Olfactory rod<br />
(vesicle)<br />
Villi<br />
Cilia<br />
Mucus<br />
©<br />
FIGURE 2.40<br />
OLFACTORY RECEPTORS •<br />
The sensory cells that make up the olfactory epithelium respond to<br />
odorants by depolarizing. Like taste buds, an olfactory cell can<br />
respond to more than one odorant. There are six general odor<br />
qualities that can be sensed: floral, ethereal (e.g., pears), musky,<br />
camphor (e.g., eucalyptus), putrid, and pungent (e.g., vinegar, peppermint).<br />
91
NEUROPHYSIOLOGY<br />
Olfactory System: Pathway<br />
Efferent fibers<br />
Afferent fibers<br />
Granule cell (excited by<br />
and inhibiting to mitral<br />
and tufted cells)<br />
Mitral cell<br />
Recurrent process<br />
Tufted cell<br />
Periglomerular<br />
cell<br />
Glomerulus<br />
Olfactory<br />
nerve fibers<br />
Fibers from contralateral olfactory bulb<br />
Fibers to contralateral olfactory bulb<br />
Anterior commissure<br />
Medial olfactory stria<br />
Olfactory trigone and<br />
olfactory tubercle<br />
Anterior perforated<br />
substance<br />
Lateral olfactory<br />
stria<br />
Lateral olfactory<br />
tract nucleus<br />
Piriform lobe<br />
Uncus<br />
Amygdala<br />
(in phantom)<br />
Entorhinal area<br />
Olfactory epithelium<br />
Olfactory nerves<br />
Olfactory bulb<br />
Olfactory tract<br />
Anterior olfactory nucleus<br />
Cribriform plate of ethmoid bone<br />
©<br />
FIGURE 2.41<br />
OLFACTORY PATHWAY •<br />
Olfactory stimuli are detected by the nerve fibers of the olfactory<br />
epithelium and conveyed to the olfactory bulb (detailed local circuitry<br />
shown in upper left panel). Integrated signals pass along the<br />
olfactory tract and centrally diverge to pass to the anterior commissure<br />
(some efferent projections course to the contralateral olfactory<br />
bulb, blue lines) or terminate in the ipsilateral olfactory trigone<br />
(olfactory tubercle). Axons then project to the primary olfactory<br />
cortex (piriform cortex), entorhinal cortex, and amygdala.<br />
92
Installing Adobe Acrobat Reader<br />
The images and text included in this atlas are contained in a Portable Document Format (pdf)<br />
file and can be viewed with Adobe Acrobat Reader. A copy of Acrobat Reader 6.0 is included<br />
on this CD. You will need to install or upgrade to Acrobat Reader 5.0 or later in order to<br />
have full functionality.<br />
Please follow these instructions:<br />
Windows<br />
1. Choose Run from the Start menu and then click Browse.<br />
2. Navigate to the Acrobat Reader folder on the <strong>Neuro</strong><strong>Atlas</strong> CD.<br />
3. Double-click the setup.exe file to open the Acrobat Reader Installer.<br />
4. Follow the onscreen instructions.<br />
Macintosh OS X<br />
1. Double-click the Acrobat Reader folder on the <strong>Neuro</strong><strong>Atlas</strong> CD.<br />
2. Copy the Adobe Reader 6.0 folder to the Applications folder.<br />
3. To complete the installation, double-click the Adobe Reader 6.0 file in your Applications<br />
folder.<br />
Note: If you are using Macintosh 9.2 or earlier, you should go to the following URL to download the Adobe<br />
Acrobat Reader. http://www.adobe.com/products/acrobat/readstep2.html<br />
Running the <strong>Atlas</strong> of <strong>Neuro</strong>anatomy and <strong>Neuro</strong>physiology<br />
Windows<br />
1. Insert the CD into the CD-ROM drive.<br />
2. If Acrobat Reader 5.0 or greater is not already installed on your computer, follow the installation<br />
instructions above.<br />
3. Choose Run from the Start menu and type x:\ (where x is the letter of your CD-ROM drive).<br />
4. Under Files of Type, click All Files.<br />
5. Double-click the <strong>Neuro</strong> <strong>Atlas</strong>.pdf file to open the program.<br />
6. For best viewing results in Acrobat Reader 5.0, use the Edit menu to access the Preferences.<br />
Select General and open the Display preferences to activate the Smooth Line Art option.<br />
Macintosh<br />
1. Insert the CD into the CD-ROM drive.<br />
2. If Acrobat Reader 5.0 or greater is not already installed on your computer, follow the installation<br />
instructions above.<br />
3. Double-click the <strong>Neuro</strong> <strong>Atlas</strong>.pdf file to open the program.<br />
4. For best viewing results in Acrobat Reader 5.0, use the Edit menu to access the Preferences.<br />
Select General and open the Display preferences to activate the Smooth Line Art option.<br />
All rights reserved. No material on this CD-ROM may be reproduced in any electronic format, including information<br />
storage and retrieval systems, without permission in writing from the publisher. Send requests for permissions<br />
to Permissions Editor, Icon Custom Communications, 295 North St., Teterboro NJ 07608, or visit<br />
http://store.netterart.com/requestform1.htm.