SHOT Annual Report 2009 - Serious Hazards of Transfusion
SHOT Annual Report 2009 - Serious Hazards of Transfusion
SHOT Annual Report 2009 - Serious Hazards of Transfusion
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
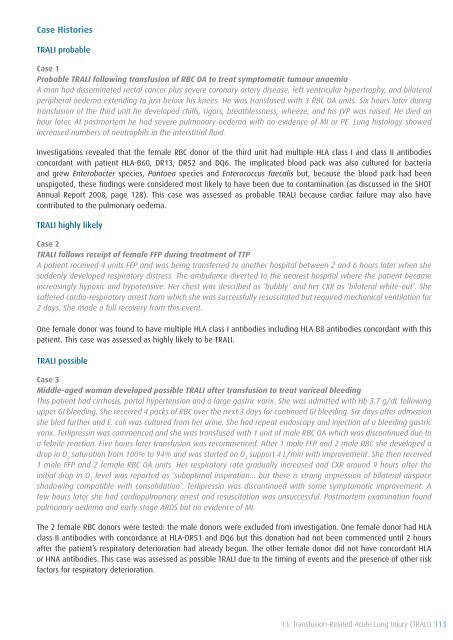
Case Histories<br />
TRALI probable<br />
Case 1<br />
Probable TRALI following transfusion <strong>of</strong> RBC OA to treat symptomatic tumour anaemia<br />
A man had disseminated rectal cancer plus severe coronary artery disease, left ventricular hypertrophy, and bilateral<br />
peripheral oedema extending to just below his knees. He was transfused with 3 RBC OA units. Six hours later during<br />
transfusion <strong>of</strong> the third unit he developed chills, rigors, breathlessness, wheeze, and his JVP was raised. He died an<br />
hour later. At postmortem he had severe pulmonary oedema with no evidence <strong>of</strong> MI or PE. Lung histology showed<br />
increased numbers <strong>of</strong> neutrophils in the interstitial fluid.<br />
Investigations revealed that the female RBC donor <strong>of</strong> the third unit had multiple HLA class I and class II antibodies<br />
concordant with patient HLA-B60, DR13, DR52 and DQ6. The implicated blood pack was also cultured for bacteria<br />
and grew Enterobacter species, Pantoea species and Enterococcus faecalis but, because the blood pack had been<br />
unspigoted, these findings were considered most likely to have been due to contamination (as discussed in the <strong>SHOT</strong><br />
<strong>Annual</strong> <strong>Report</strong> 2008, page 128). This case was assessed as probable TRALI because cardiac failure may also have<br />
contributed to the pulmonary oedema.<br />
TRALI highly likely<br />
Case 2<br />
TRALI follows receipt <strong>of</strong> female FFP during treatment <strong>of</strong> TTP<br />
A patient received 4 units FFP and was being transferred to another hospital between 2 and 6 hours later when she<br />
suddenly developed respiratory distress. The ambulance diverted to the nearest hospital where the patient became<br />
increasingly hypoxic and hypotensive. Her chest was described as ‘bubbly’ and her CXR as ‘bilateral white-out’. She<br />
suffered cardio-respiratory arrest from which she was successfully resuscitated but required mechanical ventilation for<br />
2 days. She made a full recovery from this event.<br />
One female donor was found to have multiple HLA class I antibodies including HLA B8 antibodies concordant with this<br />
patient. This case was assessed as highly likely to be TRALI.<br />
TRALI possible<br />
Case 3<br />
Middle-aged woman developed possible TRALI after transfusion to treat variceal bleeding<br />
This patient had cirrhosis, portal hypertension and a large gastric varix. She was admitted with Hb 3.7 g/dL following<br />
upper GI bleeding. She received 4 packs <strong>of</strong> RBC over the next 3 days for continued GI bleeding. Six days after admission<br />
she bled further and E. coli was cultured from her urine. She had repeat endoscopy and injection <strong>of</strong> a bleeding gastric<br />
varix. Terlipressin was commenced and she was transfused with 1 unit <strong>of</strong> male RBC OA which was discontinued due to<br />
a febrile reaction. Five hours later transfusion was recommenced. After 1 male FFP and 2 male RBC she developed a<br />
drop in O 2<br />
saturation from 100% to 94% and was started on O 2<br />
support 4 L/min with improvement. She then received<br />
1 male FFP and 2 female RBC OA units. Her respiratory rate gradually increased and CXR around 9 hours after the<br />
initial drop in O 2<br />
level was reported as ‘suboptimal inspiration... but there is strong impression <strong>of</strong> bilateral airspace<br />
shadowing compatible with consolidation’. Terlipressin was discontinued with some symptomatic improvement. A<br />
few hours later she had cardiopulmonary arrest and resuscitation was unsuccessful. Postmortem examination found<br />
pulmonary oedema and early stage ARDS but no evidence <strong>of</strong> MI.<br />
The 2 female RBC donors were tested: the male donors were excluded from investigation. One female donor had HLA<br />
class II antibodies with concordance at HLA-DR51 and DQ6 but this donation had not been commenced until 2 hours<br />
after the patient’s respiratory deterioration had already begun. The other female donor did not have concordant HLA<br />
or HNA antibodies. This case was assessed as possible TRALI due to the timing <strong>of</strong> events and the presence <strong>of</strong> other risk<br />
factors for respiratory deterioration.<br />
13. <strong>Transfusion</strong>-Related Acute Lung Injury (TRALI) 113