Antimicrobial Drugs
Antimicrobial Drugs
Antimicrobial Drugs
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
M34_ADAM9811_03_SE_CH34.QXD 12/30/09 1:16 PM Page 491<br />
Chapter 34 <strong>Drugs</strong> for Bacterial Infections 491<br />
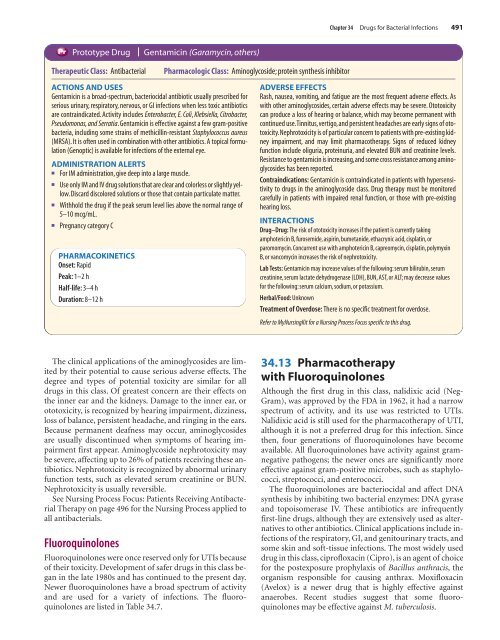
Prototype Drug<br />
Therapeutic Class: Antibacterial<br />
❘ Gentamicin (Garamycin, others)<br />
Pharmacologic Class: Aminoglycoside; protein synthesis inhibitor<br />
ACTIONS AND USES<br />
ADVERSE EFFECTS<br />
Gentamicin is a broad-spectrum, bacteriocidal antibiotic usually prescribed for<br />
serious urinary, respiratory, nervous, or GI infections when less toxic antibiotics<br />
are contraindicated. Activity includes Enterobacter, E. Coli, Klebsiella, Citrobacter,<br />
Pseudomonas, and Serratia. Gentamicin is effective against a few gram-positive<br />
bacteria, including some strains of methicillin-resistant Staphylococcus aureus<br />
(MRSA). It is often used in combination with other antibiotics. A topical formulation<br />
(Genoptic) is available for infections of the external eye.<br />
ADMINISTRATION ALERTS<br />
■ For IM administration, give deep into a large muscle.<br />
■ Use only IM and IV drug solutions that are clear and colorless or slightly yellow.<br />
Discard discolored solutions or those that contain particulate matter.<br />
■ Withhold the drug if the peak serum level lies above the normal range of<br />
5–10 mcg/mL.<br />
■ Pregnancy category C<br />
PHARMACOKINETICS<br />
Onset: Rapid<br />
Peak: 1–2 h<br />
Half-life: 3–4 h<br />
Duration: 8–12 h<br />
Rash, nausea, vomiting, and fatigue are the most frequent adverse effects. As<br />
with other aminoglycosides, certain adverse effects may be severe. Ototoxicity<br />
can produce a loss of hearing or balance, which may become permanent with<br />
continued use.Tinnitus, vertigo, and persistent headaches are early signs of ototoxicity.Nephrotoxicity<br />
is of particular concern to patients with pre-existing kidney<br />
impairment, and may limit pharmacotherapy. Signs of reduced kidney<br />
function include oliguria, proteinuria, and elevated BUN and creatinine levels.<br />
Resistance to gentamicin is increasing,and some cross resistance among aminoglycosides<br />
has been reported.<br />
Contraindications: Gentamicin is contraindicated in patients with hypersensitivity<br />
to drugs in the aminoglycoside class. Drug therapy must be monitored<br />
carefully in patients with impaired renal function, or those with pre-existing<br />
hearing loss.<br />
INTERACTIONS<br />
Drug–Drug: The risk of ototoxicity increases if the patient is currently taking<br />
amphotericin B, furosemide, aspirin, bumetanide, ethacrynic acid, cisplatin, or<br />
paromomycin. Concurrent use with amphotericin B, capreomycin, cisplatin, polymyxin<br />
B, or vancomycin increases the risk of nephrotoxicity.<br />
Lab Tests: Gentamicin may increase values of the following: serum bilirubin, serum<br />
creatinine, serum lactate dehydrogenase (LDH), BUN, AST, or ALT; may decrease values<br />
for the following: serum calcium, sodium, or potassium.<br />
Herbal/Food: Unknown<br />
Treatment of Overdose: There is no specific treatment for overdose.<br />
Refer to MyNursingKit for a Nursing Process Focus specific to this drug.<br />
The clinical applications of the aminoglycosides are limited<br />
by their potential to cause serious adverse effects. The<br />
degree and types of potential toxicity are similar for all<br />
drugs in this class. Of greatest concern are their effects on<br />
the inner ear and the kidneys. Damage to the inner ear, or<br />
ototoxicity, is recognized by hearing impairment, dizziness,<br />
loss of balance, persistent headache, and ringing in the ears.<br />
Because permanent deafness may occur, aminoglycosides<br />
are usually discontinued when symptoms of hearing impairment<br />
first appear. Aminoglycoside nephrotoxicity may<br />
be severe, affecting up to 26% of patients receiving these antibiotics.<br />
Nephrotoxicity is recognized by abnormal urinary<br />
function tests, such as elevated serum creatinine or BUN.<br />
Nephrotoxicity is usually reversible.<br />
See Nursing Process Focus: Patients Receiving Antibacterial<br />
Therapy on page 496 for the Nursing Process applied to<br />
all antibacterials.<br />
Fluoroquinolones<br />
Fluoroquinolones were once reserved only for UTIs because<br />
of their toxicity. Development of safer drugs in this class began<br />
in the late 1980s and has continued to the present day.<br />
Newer fluoroquinolones have a broad spectrum of activity<br />
and are used for a variety of infections. The fluoroquinolones<br />
are listed in Table 34.7.<br />
34.13 Pharmacotherapy<br />
with Fluoroquinolones<br />
Although the first drug in this class, nalidixic acid (Neg-<br />
Gram), was approved by the FDA in 1962, it had a narrow<br />
spectrum of activity, and its use was restricted to UTIs.<br />
Nalidixic acid is still used for the pharmacotherapy of UTI,<br />
although it is not a preferred drug for this infection. Since<br />
then, four generations of fluoroquinolones have become<br />
available. All fluoroquinolones have activity against gramnegative<br />
pathogens; the newer ones are significantly more<br />
effective against gram-positive microbes, such as staphylococci,<br />
streptococci, and enterococci.<br />
The fluoroquinolones are bacteriocidal and affect DNA<br />
synthesis by inhibiting two bacterial enzymes: DNA gyrase<br />
and topoisomerase IV. These antibiotics are infrequently<br />
first-line drugs, although they are extensively used as alternatives<br />
to other antibiotics. Clinical applications include infections<br />
of the respiratory, GI, and genitourinary tracts, and<br />
some skin and soft-tissue infections. The most widely used<br />
drug in this class, ciprofloxacin (Cipro), is an agent of choice<br />
for the postexposure prophylaxis of Bacillus anthracis, the<br />
organism responsible for causing anthrax. Moxifloxacin<br />
(Avelox) is a newer drug that is highly effective against<br />
anaerobes. Recent studies suggest that some fluoroquinolones<br />
may be effective against M. tuberculosis.<br />
# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 491<br />
Title: Pharmacology for Nurses Server: Jobs2<br />
C/M/Y/K<br />
Short / Normal<br />
DESIGN SERVICES OF<br />
S4CARLISLE<br />
Publishing Services