Antimicrobial Drugs
Antimicrobial Drugs
Antimicrobial Drugs
Create successful ePaper yourself
Turn your PDF publications into a flip-book with our unique Google optimized e-Paper software.
M34_ADAM9811_03_SE_CH34.QXD 12/30/09 1:16 PM Page 482<br />
482 Unit 5 The Immune System<br />
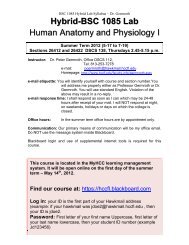
Resistant<br />
organism<br />
Antibiotic<br />
Time<br />
➤ Figure 34.2 Acquired resistance<br />
1. Infection<br />
2. Antibiotic kills all organisms<br />
except the resistant one.<br />
3. Resistant organism that<br />
remained has rapidly divided<br />
to infect the client. Antibiotic<br />
is no longer effective.<br />
Health care providers play important roles in delaying the<br />
emergence of resistance. The following are five principles<br />
recommended by the CDC:<br />
● Prevent infections whenever possible. It is always easier<br />
to prevent an infection, than to treat one. This includes<br />
teaching the patient the importance of getting<br />
immunizations.<br />
● Use the right drug for the infection. Infections should be<br />
cultured so that the offending organism can be identified<br />
and the correct drug chosen (see Section 34.6).<br />
● Restrict the use of antibiotics to those conditions<br />
deemed medically necessary. Antibiotics should only be<br />
prescribed when there is a clear rationale for their use.<br />
● Advise the patient to take anti-infectives for the full<br />
length of therapy, even if symptoms disappear before the<br />
regimen is finished. Prematurely stopping antibiotic<br />
therapy allows some pathogens to survive, thus<br />
promoting the development of resistant strains.<br />
● Prevent transmission of the pathogen by using proper<br />
infection control procedures. This includes the use of<br />
standard precautions and teaching patients methods of<br />
proper hygiene for preventing transmission in the home<br />
and community settings.<br />
In most cases, antibiotics are given when there is clear evidence<br />
of bacterial infection. Some patients, however, receive<br />
antibiotics to prevent an infection, a practice called<br />
prophylactic use, or chemoprophylaxis. Examples of patients<br />
who might receive prophylactic antibiotics include those<br />
who have a suppressed immune system, those who have experienced<br />
deep puncture wounds such as from dog bites, or<br />
those who have prosthetic heart valves and are about to have<br />
medical or dental procedures.<br />
34.6 Selection of an<br />
Effective Antibiotic<br />
The selection of an antibiotic that will be effective against a<br />
specific pathogen is an important task of the health care<br />
provider. Selecting an incorrect drug will delay proper treatment,<br />
giving the microorganisms more time to invade.<br />
Prescribing ineffective antibiotics also promotes the development<br />
of resistance, and may cause unnecessary adverse<br />
effects in the patient.<br />
Ideally, laboratory tests should be conducted to identify the<br />
specific pathogen prior to beginning anti-infective therapy.<br />
Lab tests may include examination of urine, stool, spinal<br />
fluid, sputum, blood, or purulent drainage for microorganisms.<br />
Organisms isolated from the specimens are grown in the<br />
laboratory and identified. After identification, the laboratory<br />
tests several different antibiotics to determine which is most<br />
effective against the infecting microorganism. This process of<br />
growing the pathogen and identifying the most effective antibiotic<br />
is called culture and sensitivity (C&S) testing.<br />
Because antibiotic therapy alters the composition of infected<br />
fluids, samples should be collected prior to starting<br />
pharmacotherapy. However, laboratory testing and identification<br />
may take several days and, in the case of viruses, several<br />
weeks. If the infection is severe, therapy is often begun<br />
with a broad-spectrum antibiotic, one that is effective against a<br />
wide variety of different microbial species. After laboratory<br />
testing is completed, the drug may be changed to a narrowspectrum<br />
antibiotic, one that is effective against a smaller group<br />
of microbes or only the isolated species. In general, narrowspectrum<br />
antibiotics have less effect on normal host flora,<br />
thus causing fewer side effects. For mild infections, laboratory<br />
identification is not always necessary; skilled health<br />
care providers are often able to make an accurate diagnosis<br />
based on patient signs and symptoms.<br />
In most cases, antibacterial therapy is best conducted using<br />
a single drug. Combining two antibiotics may actually<br />
decrease each drug’s efficacy, a phenomenon known as<br />
antagonism. If incorrect combinations are prescribed, the<br />
use of multiple antibiotics also has the potential to promote<br />
resistance. Multidrug therapy is warranted, however, if several<br />
different organisms are causing the patient’s infection<br />
or if the infection is so severe that therapy must be started<br />
before laboratory tests have been completed. Multidrug<br />
therapy is clearly warranted in the treatment of tuberculosis<br />
or in patients infected with HIV.<br />
One common adverse effect of anti-infective therapy is the<br />
appearance of secondary infections, known as superinfections,<br />
# 102887 Cust: PE/NJ/CHET Au: ADAMS Pg. No. 482<br />
Title: Pharmacology for Nurses Server: Jobs2<br />
C/M/Y/K<br />
Short / Normal<br />
DESIGN SERVICES OF<br />
S4CARLISLE<br />
Publishing Services